

Thank you for joining todays webinar!
Thank You to Our Sponsors!





Webinar Video Replay & Slides


As follow up to todays webinar, we will have the speaker slides and a video replay available. They will be provided shortly after the webinar concludes and posted to our website.





• Open the Q&A window, allowing you to ask questions to the host and panelists. It will be sent to our moderator and panelists for discussion. • If you have a question that does not get answered today, you can contact our Infoline at 800-452-CURE (2873) US & Canada, 1-818-4877455, or email infoline@myeloma.org. Audience Q&A
Feedback Survey


At the close of the meeting a feedback survey will pop up. This will also be emailed to you shortly after the workshop. Please take a moment to complete this survey. We Want to Hear From You!
Psychosocial Care: Common Support Needs and Coping Skills
 Elaine Wheat Dawson, PsyD
Elaine Wheat Dawson, PsyD

Welcome!
Care across the continuum



• Different support needs emerge at different stages of treatment • Assessing needs for support “early and often” is the goal *Lamerset al., 2013
New diagnosis/Early treatment
• Historically, the support needs at the time of multiplemyeloma diagnosis has been minimallystudied*


• Acceptance of psychosocial help tends to be higher at earlier phases of diagnosis, so this is a crucial window to receive/offer help
• Informational needs tend to be high during this stage (including education about diagnosis)
• The actual diagnostic process can be lengthy, and therefore particularly stressful Shock/overwhelm
•
New



diagnosis/Early treatment continued • Previous study found that approximately 50% of multiple myeloma patients were interested in psychosocial supports at diagnosis.* • Most common requests were: 1. Relaxation techniques 2. Counseling 3. Peer support groups 4. Psychotherapy 5. Support for family members 6. Social service assistance *Lamers et al. (2013)


Treatment • Support for symptom burden of treatment (includingpain) • Can impact quality of life • May experience unplanned hospital stays (or planned stays, including transplant) • Fear: Treatment effectiveness
Remission


• “Extended survivorship” (Mullan; “Celebration, uncertainty, and transition”) or Chronic Survivorship • Fear: Relapse • Continued pain management for some • Quality of life can be impacted by late effects (neuropathy, weight gain, pain, more)

Emotional Health
Cancer is stressful


Common symptoms


• It’s normal to experience distress and feel as if you’re on an “emotional rollercoaster” • An increase in anxiety and depressive symptoms is common • They also influence a person’s unmet support needs* • Anxiety: worry, uneasiness, restlessness, difficulty concentrating, racing thoughts, difficulty sleeping, muscle tension • Depression: low mood, diminished pleasure or interest, fatigue/low energy, difficulty concentrating, worthlessness, guilt, hopelessness, helplessness, irritability/frustration *Cho & Yoo, 2020
Common for



symptoms
caregivers • Caregivers/care partners tend to endorse high rates of distress, psychological symptoms (anxiety in particular, depression)* • This remains true across disease trajectory • Despite this, only a small portion of caregivers of patients with advanced cancer access mental health services* *O’Donnell, 2022; Vanderweker et al. (2005)
Fear of


the unknown • Uncertainty is a common experience in cancer care (from time of diagnosis) • This is a “core theme” for caregivers, as well.* • Shakes our confidence, sense of control • Tip: Focus on what you can control, and one task at a time. • Seek guidance for questions that can be answered *Quinoa-Salanova et al., 2019


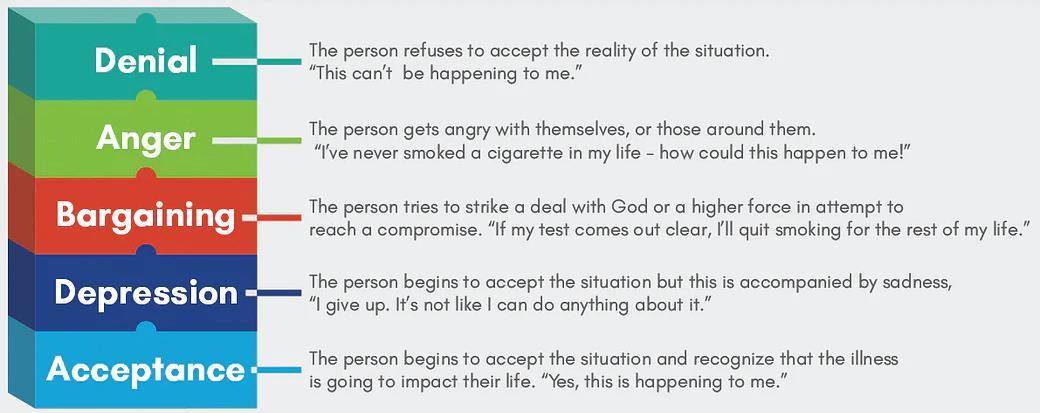
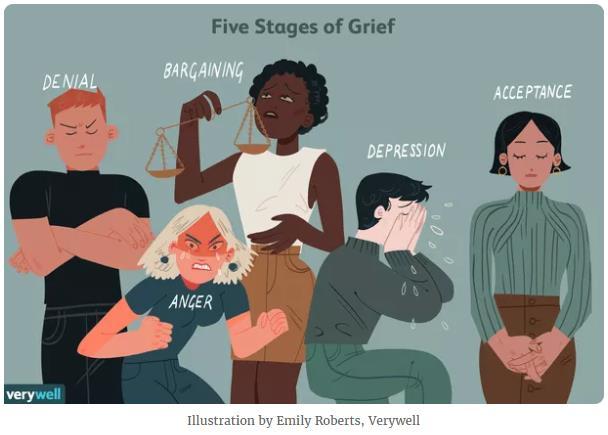
• We experience loss(es) during cancer treatment.
Grief
Emotion identification
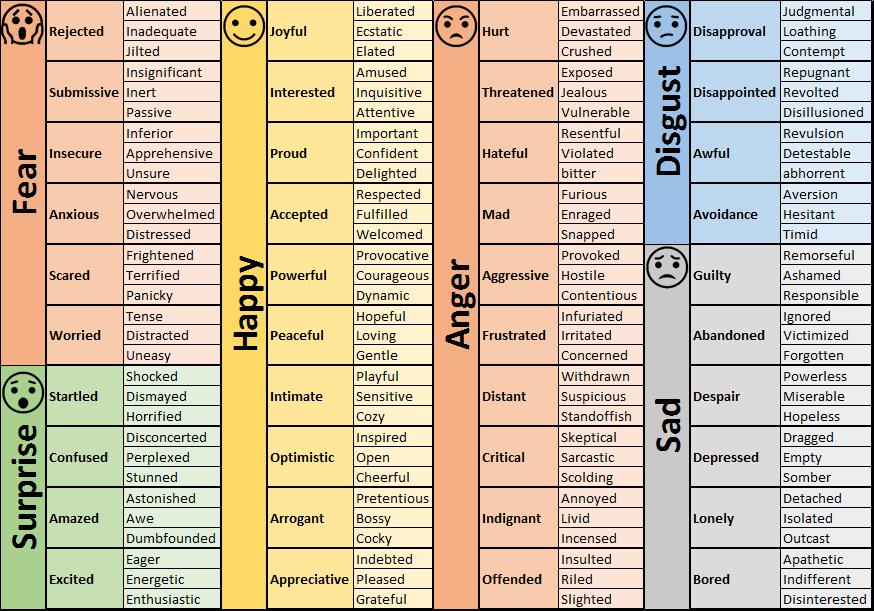

• I often introduce the importance of recognizing and naming your emotions They are temporary, and some teach us things (or signal things to us) Journaling can be very helpful


•
•
Living with Pain

Pain• Causes can vary: Neuropathy, steroid toxicity, lytic lesions or fractures, post-transplant symptoms

• Pain (aka persistent stressor) causes a “Fight or Flight” response in the body.
• Our sympathetic nervous system governs this process, including parts of your brain, and it helps us prepare to face a threat
• However, chronic pain prolongs this response to the point that it is no longer adaptive or helpful, and the body then has less time to recover


Pain continued
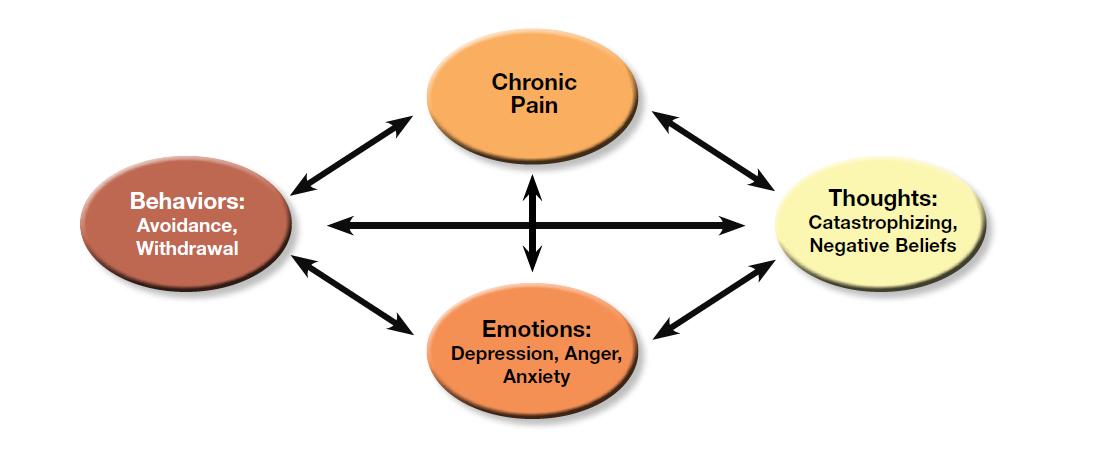
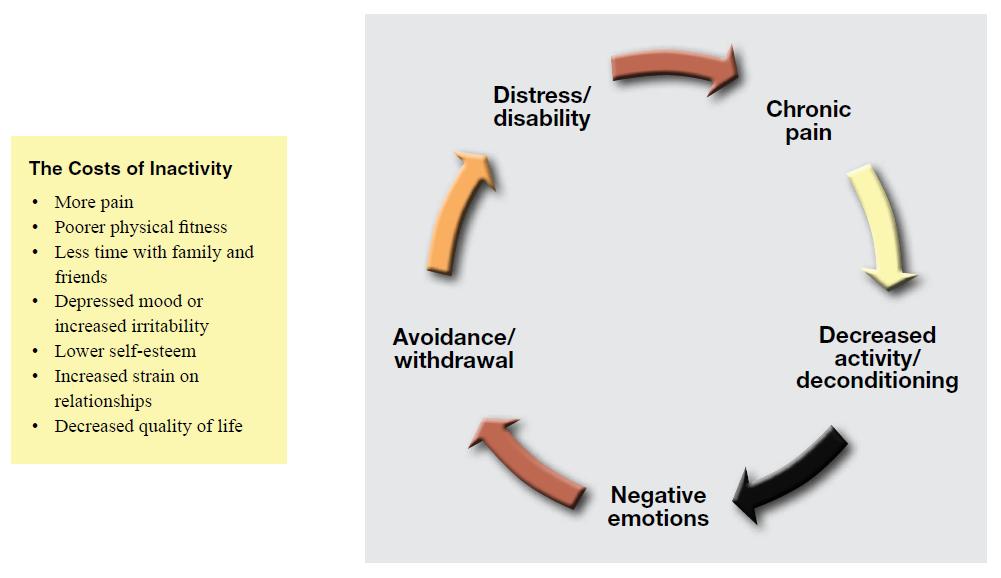
• Among other things, we may unconsciously tense our muscles, reduce our involvement in activities, and have frequent negative thoughts related to pain.*
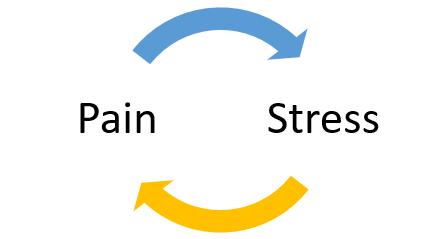
• We know that stress and pain have a bi-directional relationship: perceptions of pain intensify stress, and stress (including emotional distress like anxiety and depression) intensifies perceptions of pain.

*Benson, 1975

Impacts of pain


*Murphy et al.

Coping Tools
Relaxation Skills


• With practice, we can use relaxation techniques to return our bodies to more relaxed states → reducing perceived intensity of our pain • Our parasympathetic nervous system helps calm our bodies after a threat; it eases the fight-or-flight response • We are capable of developing some control over this process and engaging this system as a way to manage stress and/or pain • Benefits of relaxation skills include decreased muscle tension and fatigue, improved sleep, and increased energy* *Laevsky et al., 2011; Persson et al., 2008
Deep Breathing
• Slows your breathing rate, increases oxygen intake, and increases energy
• Breaths are smoother, slower, and deeper than what you’d usually do throughout the day. It’s one of the easiest, quickest ways to decrease tension in your body.



• Allows more room for the lungs to fill with air by breathing into your diaphragm
• Meditation has been practiced in cultures all over the world. (It can be practiced independently of any spirituality or religion.)


• There are many different types of meditation



Meditation • Training in awareness and focused attention
Mindfulness



• The goal of mindfulness is intentional, non-judgmental present moment awareness • Mindfulness encourages you to notice unwanted or uncomfortable thoughts, emotions and pain without trying to change them or make them go away • Connect to your body and your inner world at this moment



Guided Imagery • Create mental images to foster a relaxed state • Choose a location to mentally visit during the exercise • Only rule: Choose a place that is peaceful and calm • The key to developing a deeply immersive experience is to give full attention to the specific details of the scene (incorporate your senses)
IMF


Supports • There are wonderful resources (mindfulness meditation, yoga) on the Mind, Body & Wellness page • Also: Webinar titled “Building Your Resilience During Challenging Times”
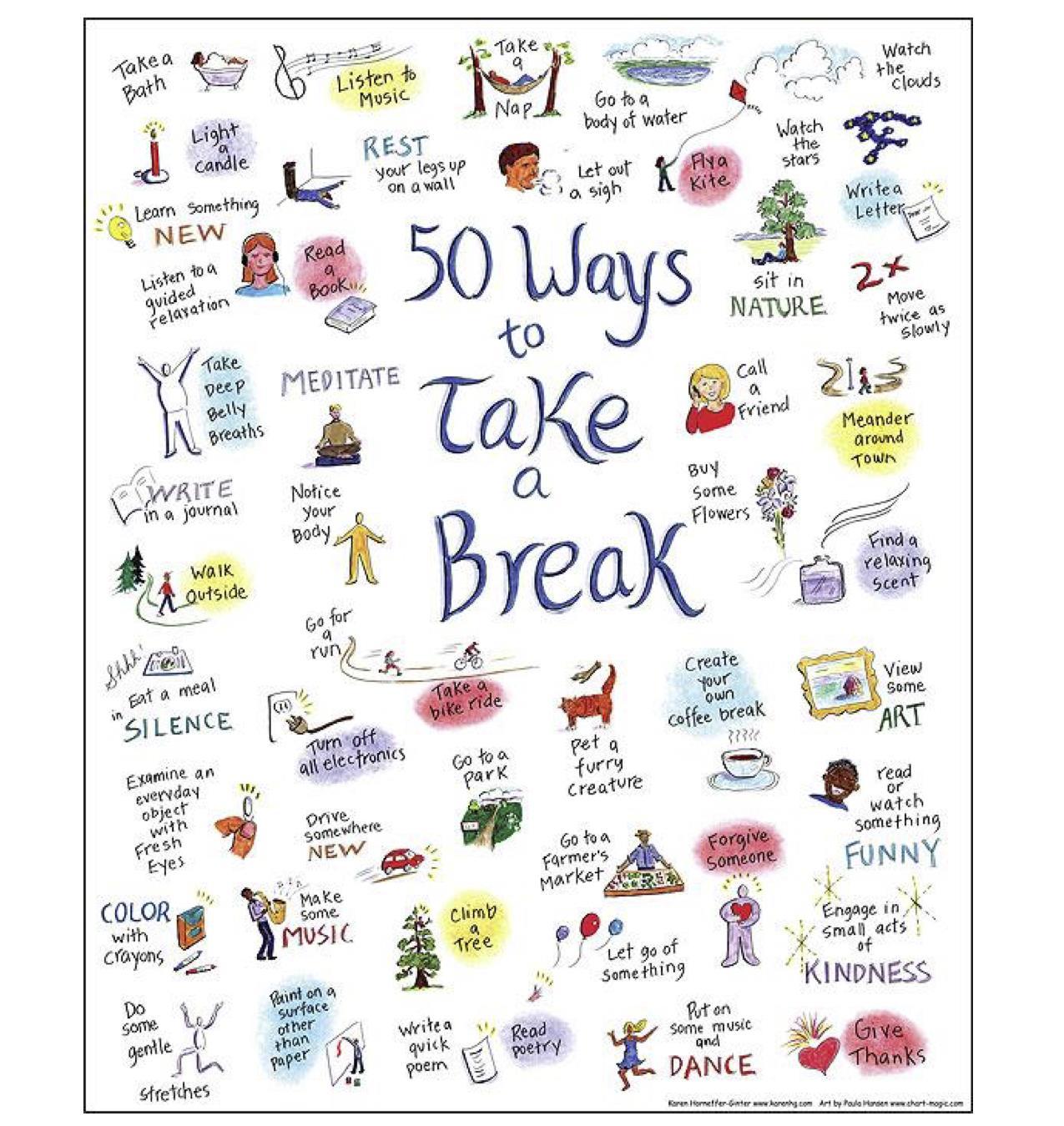
Enjoyable activities



Cognitive coping

• Negative thoughts are often automatic and outside of a person’s awareness, but they may still significantly impact emotions and behaviors
• Research shows that negative thoughts are directly associated with pain perception* We all have automatic thoughts that can be unhelpful or helpful Notice them the experts”, Fear Fact proceed anyway?

•
•
• “Look to
vs.
• Can I
*Lawrence et al., 2011
Peer Connection/Support





• One of the highestrequested resources at start of treatment

• Can be helpful to hear others’ experiences, perspectives (see the IMF “PatientStories” section of the Mind, Body & Wellness page) or the Support Groups page)
Communication with medical team



• Continue to report symptoms to your physician, even if it feels repetitive. • Some studies have shown that individuals will experience “resignation” about poorly managed symptoms,to the extent that they stop mentioning them at appointments* • But self-management is a crucial aspect of multiple myelomacare • Take notes re: questions, symptoms and bring these notes to your appointments • Ask a question until you understand the answer *Cormican et al 2018)
Communication with loved ones


• Ask for help when needed (asking for help doesn’t mean you’ve lost all independence, or that it will be this way forever) • Be specific in the type of ways family or friends can help you • You can even prepare a mental or physical list of tasks, organized by familiarity. When someone offers help, you can choose something from the list • Consider an online program like Caring Bridge or Care Pages to communicate support needs (and/or medical updates) • Clarify what you can do right now, or what you want to continue doing (Setting family expectations) • Openly talk about any changes treatment may cause to your routine at home
Care partner communication tips


• of about other than can help with of it to

Silence doesn’t need to be uncomfortable. Silence can give space for thinking deeply and continuation
thought • Talking
subjects
cancer
a sense
normalcy & reduce overwhelm • At times, your loved one may find
hard
be “positive.” Sadness, anger, and fear are normal. Encourage them to share, even if it seems negative *Adapted from the American Cancer Society and Cancer Care
Other Psychosocial Supports

Other of


sources
support • Psychiatry • Social Work • Groups (for patients, caregivers) • Spiritual care • Financial counselors • Dieticians/Nutritionists • Educational resources • Patient Advocacy
The big picture
Biological

Psychological
Social Spiritual


Discussion
Bernstein, E.E., Curtiss, J.E., Wu, G.W.Y., Barreira, P.J., & McNally, R.J. (2018) Exercise and emotion dynamics: An experience sampling study. Emotion, 19:4, 637 644. Cho, Y.R., Yoo, Y S. (2020) Factors influencing supportive care needs of multiple myeloma patients treated with chemotherapy. Supportive Care in Cancer, 28: 1783 1791. Coleman, E.A., Goodwin, J.A., Coon, S.K., Richards, K., Enderlin, C., Kennedy, R., Stewart, C.B., McNatt, P., Lockhart, K., Anaissie, E.J., Barlogie, B. (2011) Fatigue, sleep, pain, mood, and performance status in patients with multiple myeloma. Cancer Nursing, 34:3, 219 227. Cormican, O., Dowling, M. (2018) Living with relapsed myeloma: Symptoms and self care strategies. Journal of Clinical Nursing, 27: 1713 1721. Kurtin, S. (2017) Living with multiple myeloma: A continuum based approach to cancer survivorship. Seminars in Oncology Nursing, 33, 3, 348 361. Laevsky et al, 2011
Lamers, J., Hartmann, M., Goldschmidt, H., Brechtel, A., Hillengass, J., Herzog, W. (2013) Psychosocial support in patients with multiple myeloma at time of diagnosis: who wants what? Psycho oncology, 22, 2313 2320.

O’Donnell, E., Shapiro, Y., Yee, A., Nadeem, O., Laubach, J., Branagan, A., Anderson, K., Mo, C., Munshi, N., Ghobrial, I., Sperling, A., Agyemang, E., Burke, J., Harrington, C., Hu, B., Richardson, P., Raje, N., El Jawahri, A. (2022) Quality of life, psychological distress, and prognostic perceptions in caregivers of patients with multiple myeloma. Blood Advances. Persson et al, 2008
Quinoa Salanova C., Porta Sales, J., Monforte Royo, C., Edo Gual, M. (2019) The experiences and needs of primary family caregivers of patients with multiple myeloma: A qualitative analysis. Palliative Medicine, 33(5), 500 509.
Murphy, J.L., McKellar, J.D., Raffa, S.D., Clark, M.E., Kerns, R.D., & Karlin, B.E. Cognitive behavioral therapy for chronic pain among veterans: Therapist manual. Washington, DC: U.S. Department of Veterans Affairs. Vanderwerker, L.C., Laff, R.E., Kadan Lottick, N.S., McColl, S., Prigerson, H.G. (2005) Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. Journal of Clinical Oncology, 23, 28, 6899 6907.
References





• Open the Q&A window, allowing you to ask questions to the host and panelists. It will be sent to our moderator and panelists for discussion. • If you have a question that does not get answered today, you can contact our Infoline at 800-452-CURE (2873) US & Canada, 1-818-4877455, or email infoline@myeloma.org. Audience Q&A
Feedback Survey


At the close of the meeting a feedback survey will pop up. This will also be emailed to you shortly after the workshop. Please take a moment to complete this survey. We Want to Hear From You!
Thank You to Our Sponsors!





Thank you for Joining Todays Webinar


