1
Myeloma 101 and Frontline Therapy Craig Cole, MD Michigan State University



2
The Application of Science: Multiple Myeloma 101 and Frontline Therapy International
Myeloma Foundation




Pacific Northwest Regional Community Workshop
Saturday November 19th, 2022
Craig Emmitt Cole, M.D. Assistant Professor Director of Clinical Research Department of Internal Medicine Division of Hematology/Oncology; Hematology Section Michigan State University College of Human Medicine Karmanos Cancer Institute
Discussion How common is multiple myeloma Spectrum of plasma cell disorders Diagnosis of myeloma and labs Staging and risk stratification The Science behind the treatments! Up front therapy strategies: induction, transplant, and maintenance Bone support “New Stuff” 4 drug induction therapy Perspectives in the advancement of myeloma science and survival
Today’s

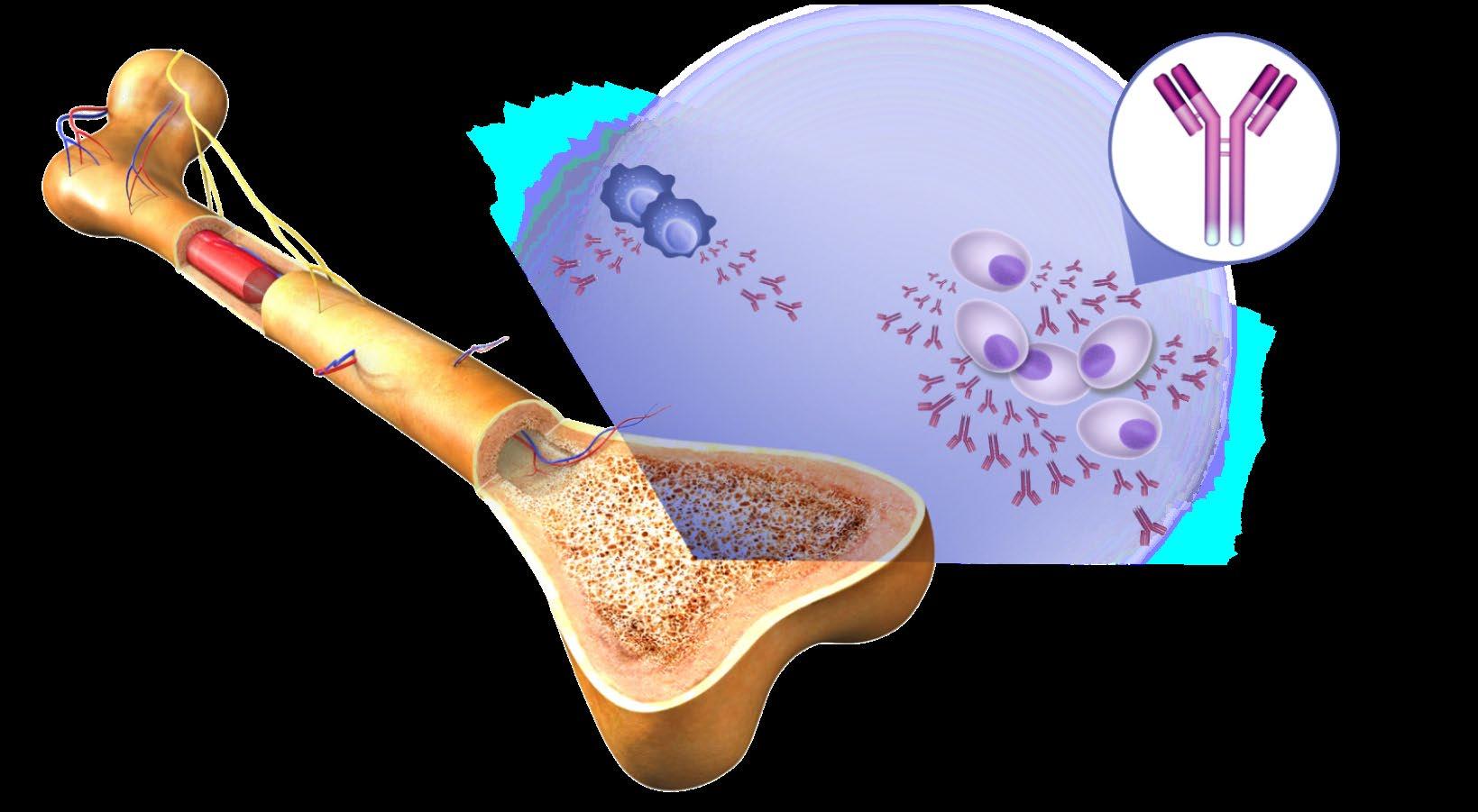




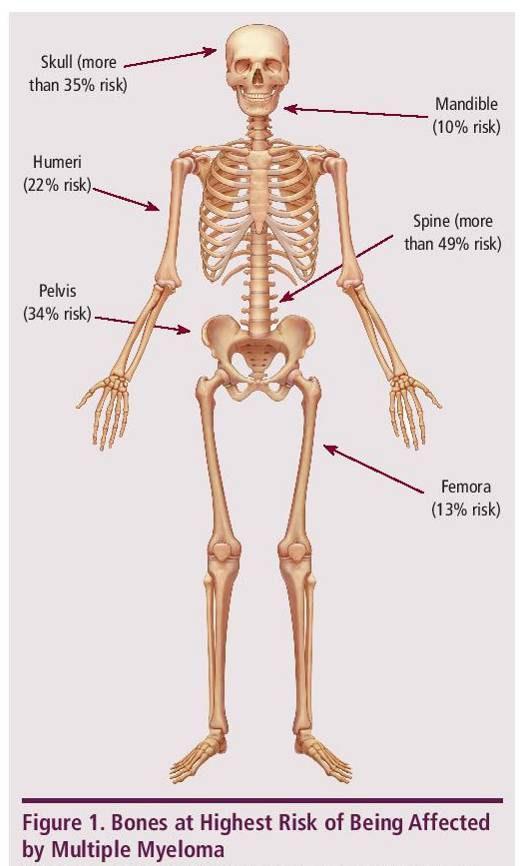
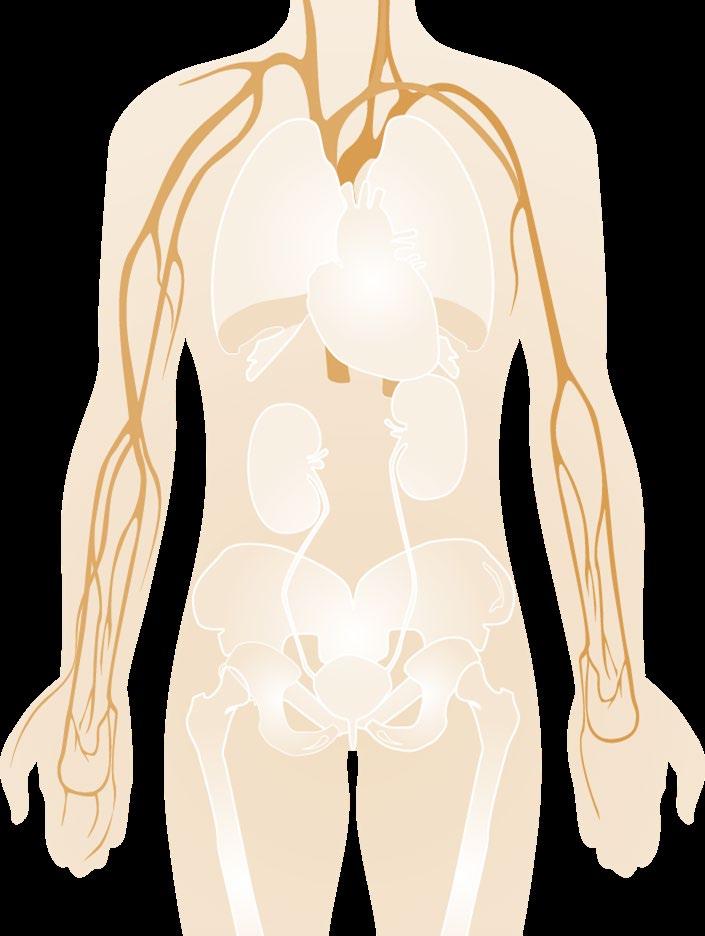
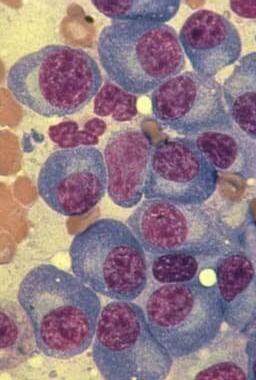
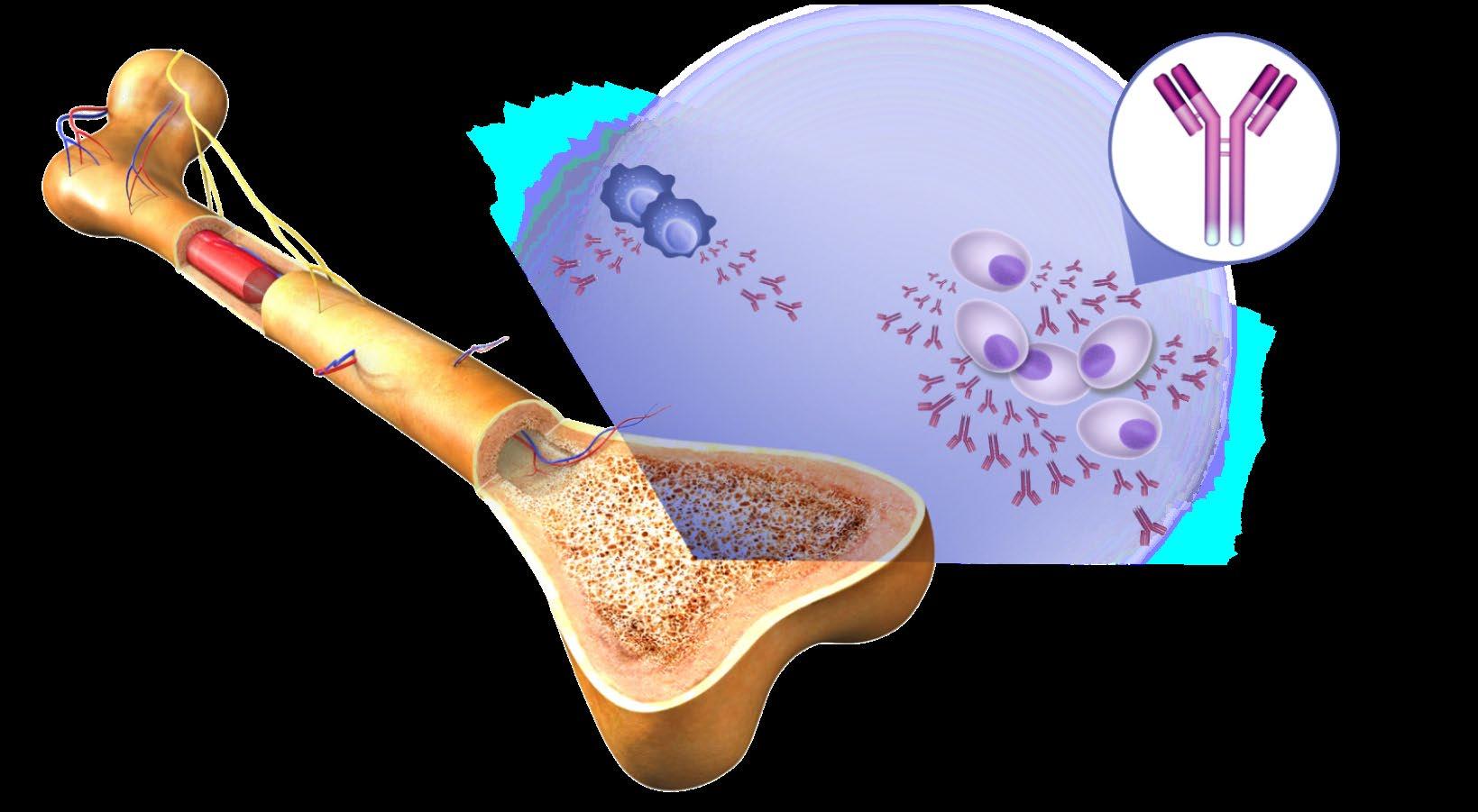
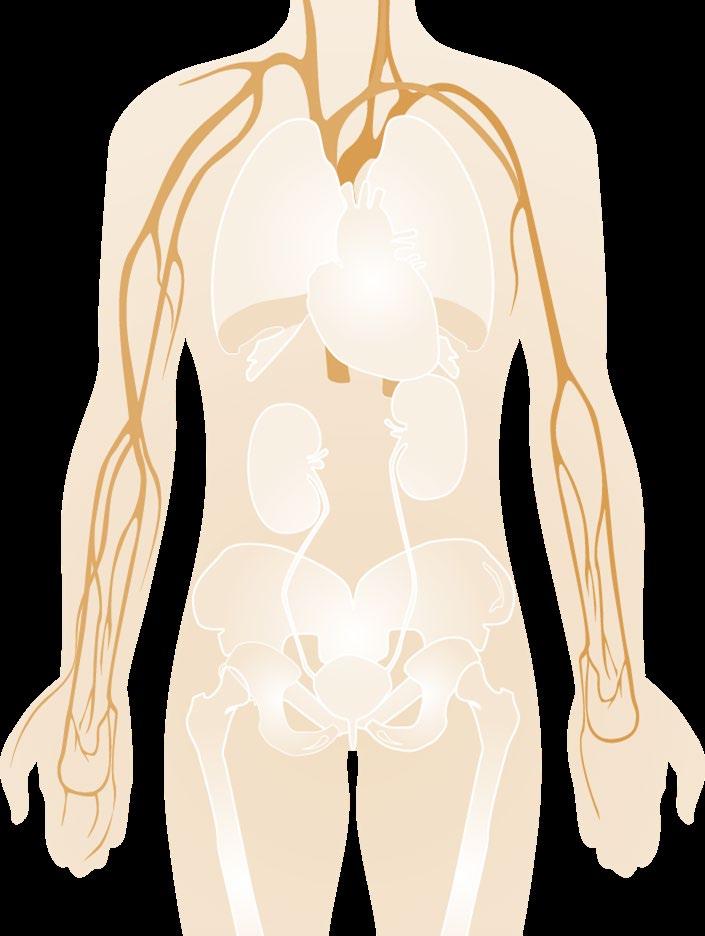
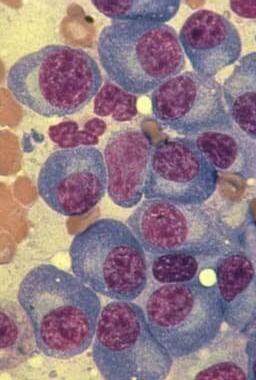
Large amounts of M proteins Multiple Myeloma is a Cancer of the Bone Marrow Plasma Cells Normal plasma cells Bone Bone marrow Antibodies BONES • Surrounding bone where Myeloma cells grow is damaged/ weakened • Myeloma cells activate bone destruction blood calcium levels Calcium high Renal (kidney) failure Anemia Bone destruction Mutated Cancer Cell BLOOD • Myeloma is a cancer of the blood • Myeloma crowds out normal blood forming cells, causing anemia Monoclonal (M) proteins Multiple Myeloma cells
Common Symptoms Multiple Myeloma


About Low Blood Counts • Anemia is present in 60% at diagnosis • May lead to anemia and infection
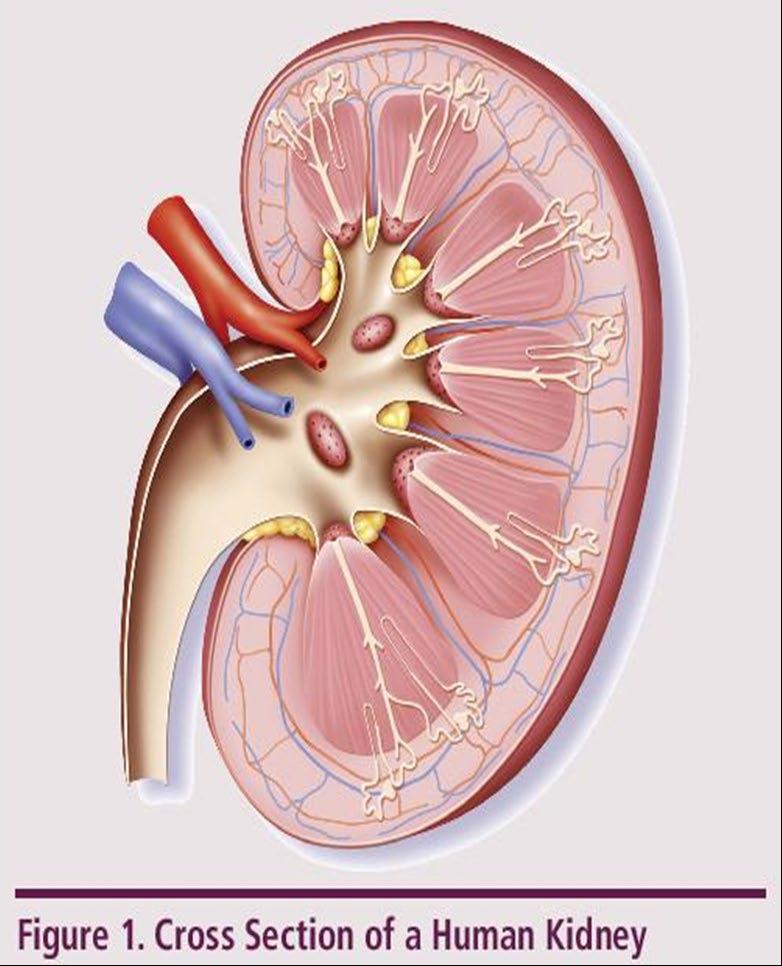
20% Weakness Fatigue Infection Decreased Kidney Function • Occurs in over half of myeloma patients Bone Damage • Affects 85% of patients • Leads to fractures Bone Turnover • Leads to high levels of calcium in blood (hypercalcemia)
myeloma Weakness Bone pain Loss of appetite Weight loss C: Calcium elevation (>11 mg/dL) R: Renal- low kidney function; (serum creatinine >2 mg/dL) A: Anemia –low red blood count (Hb <10 g/dL) B: Bone disease (≥1 lytic lesions on skeletal radiography, CT, or PET-CT)

10% to
of patients with newly diagnosed
Campbell K. Nurs Times. 2014;110:12. will not have any symptoms.
Multiple Myeloma Fast Facts





Leukemia & Lymphoma Society. Facts and Statistics. http://www.lls.org/facts and statistics/facts and statistics overview#Myeloma.
SEER Cancer Stat Facts: Myeloma. National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/statfacts/html/mulmy.html
North American Association of Central Cancer Registries (NAACCR), 2021 http://www.naaccr.org/DataandPublications/CINAPubs.aspx
Multiple Myeloma 2nd most common blood cancer 34,920 new cases of myeloma in 2021 138,451 U.S. patients living with myeloma in 2021 Myeloma is most frequently diagnosed in people 65 to 74 years old Black Incidence: 14.1/100,000 White Incidence: 6.1/100,000


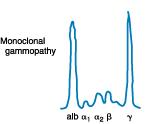
M protein over 3 g/dL (serum) or over 500 mg/24 hrs (urine) AND Plasma cells in Bone Marrow 10%–60% AND No CRAB or “SLiM” high risk features M protein under 3 g/dL AND Plasma cells in Bone Marrow <10% AND No CRAB or “SLiM” high risk features MGUS Monoclonal Gammopathy of Uncertain Significance Smoldering Myeloma Multiple Myeloma 10% risk of progression/year to active myeloma 1% risk of progression/year to multiple myeloma or related conditions Spectrum of Plasma Cell Disorders and Myeloma Malignant Plasma cells seen on any biopsy (usually bone marrow) AND ≥1 “CRAB” feature OR have >1 SLiM ‘high risk” features: C: Calcium elevation (>11 mg/dL) R: Renal- low kidney function; (serum creatinine >2 mg/dL) A: Anemia –low red blood count (Hb <10 g/dL) B: Bone disease (≥1 lytic lesions on skeletal radiography, CT, or PET-CT) S: >60% Plasma Cells on Bone Marrow biopsy Li: Serum light chain ratio >100 M: >1 lytic lesions on MRI (or PET/ CT scan) High Risk Smoldering M protein over 2 g/dL AND Plasma cells in Bone Marrow 20%–60% AND Free Lt Chain Ratio >20 “Evolving type”SMM Increase >10% protein w/in 6mo AND No CRAB or “SLiM” high risk features >46% risk of progression in 2 yr to active myeloma Observation Clinical Trials Observation Clinical Trials Close Observation Clinical Trials ?? Treatment?? Front Line Treatment Clinical Trials









Diagnosing Myeloma: Learn Your Labs! CBC • Number of red blood cells, white blood cells, and platelets CoMP • Measure levels of albumin, calcium, and creatinine. Assess function of kidney, liver, and bone status (alkaline phosphatase) and the extent of disease. Immuno Fixation • Identify the type of abnormal antibody proteins: IgG, IgA, κ,or λ Serum Protein EP • Detect the presence and level of M protein = how much myeloma Serum FreeLight Chain • Freelite test measures free light chains (kappa or lambda) in blood = how much myeloma Urine Protein EP • Detect Bence-Jones proteins (otherwise known as myeloma light chains) in urine (present or not present) 24 hr Urine Analysis • Determine the presence and levels of M protein and Bence Jones protein in the urine = how much myeloma LDH Lactate Dehydrogenase • Determine the level of myeloma cell production and extent of MM : USED FOR STAGE Beta2 MicroG • Determine the level of a protein that indicates the presence/extent of MM and kidney function: USED FOR STAGE

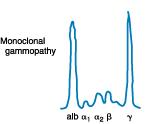















IgG Kappa M-Protein IgG Kappa M-Protein Serum Protein EP • Detect the presence and level of M protein = how much myeloma Monoclonal protein Treatment • Freelite test measures free light chains (kappa or lambda) in blood = how much myeloma Serum FreeLight Chain Kappa Lt. Chain Lambda Lt. Chain Kappa Lt. Chain MM Positive Kappa Monoclonal Serum Light Chains Treatment Ratio: 1
Types of Monoclonal Protein (M Protein) in Multiple Myeloma
• IgG+kappa • IgG+lambda • IgA+kappa • IgA+lambda • etc… • 80% of myeloma cases
Jones protein
• 18% of all myeloma cases
• Renal failure more common in light chain multiple myeloma; creatinine >2 mg/dL in 1/3 of cases
protein present
• Less than 3% of cases of multiple myeloma
Diagnosis of Multiple Myeloma
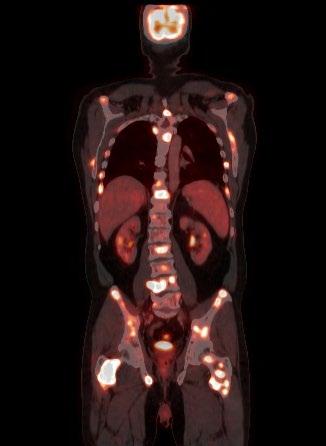
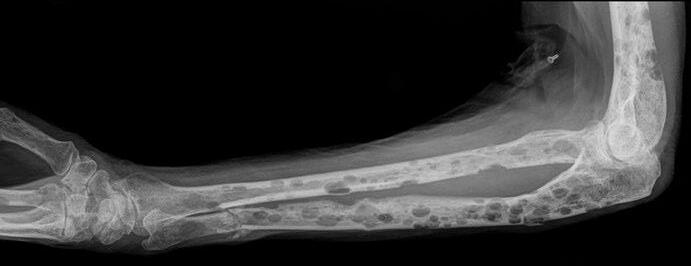
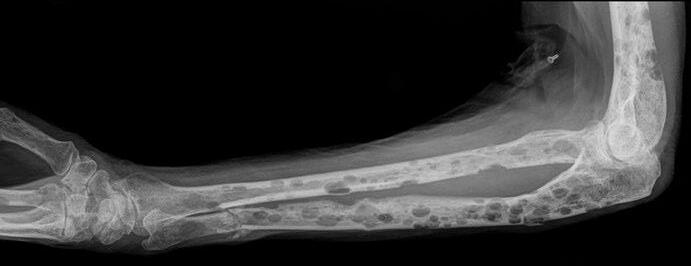
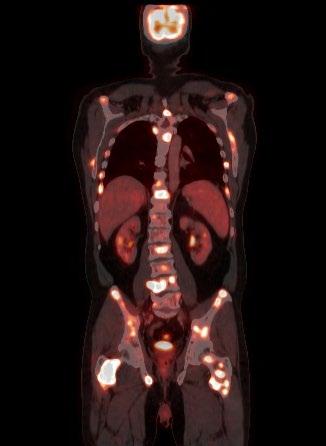
Conventional X-rays reveal punched-out lytic lesions, osteoporosis, or fractures in 75% of patients.
FDG PET/CT appears to be more sensitive (85%) than skeletal survey for the detection of small lytic bone lesions.
2003. Nanni C
Journal of Nuclear Medicine and Molecular Imaging
33:2006
Leukemia. 2009 • Diagnosis is confirmed with bone marrow demonstrating greater than 10% involvement by malignant plasma cells with either CRAB or SLiM Malignant Plasma cells seen on biopsy AND ≥1 “CRAB” feature OR have >1 SLiM ‘high risk” features: C: Calcium elevation (>11 mg/dL) R: Renal- low kidney function; (serum creatinine >2 mg/dL) A: Anemia –low red blood count (Hb <10 g/dL) B: Bone disease (≥1 lytic lesions on skeletal radiography, CT, or PET-CT) S: >60% Plasma Cells on Bone Marrow biopsy Li: Serum light chain ratio >100 M: >1 lytic lesions on MRI (or PET/ CT scan)
•
•
Kyle RA et al. Mayo Clin Proc Jan;78(1):
et al. European
Vol.
Dimopoulos MA, et al.
Staging
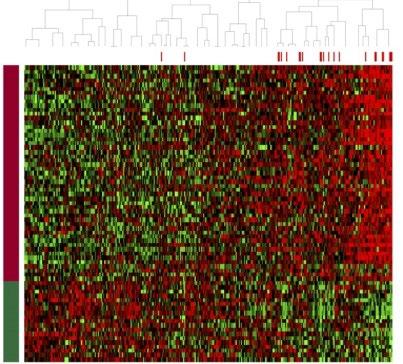
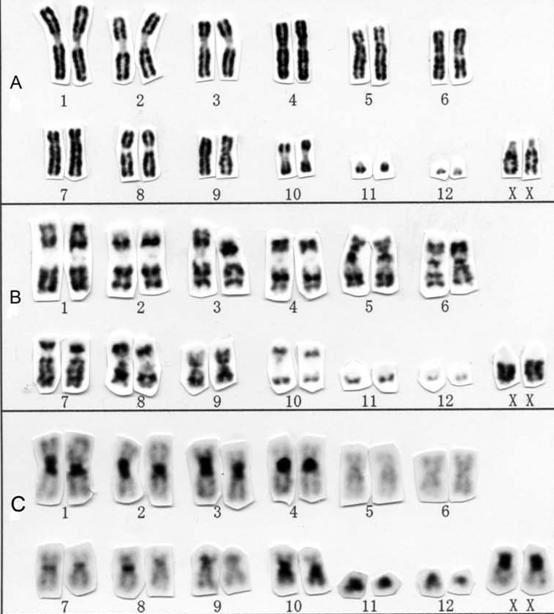
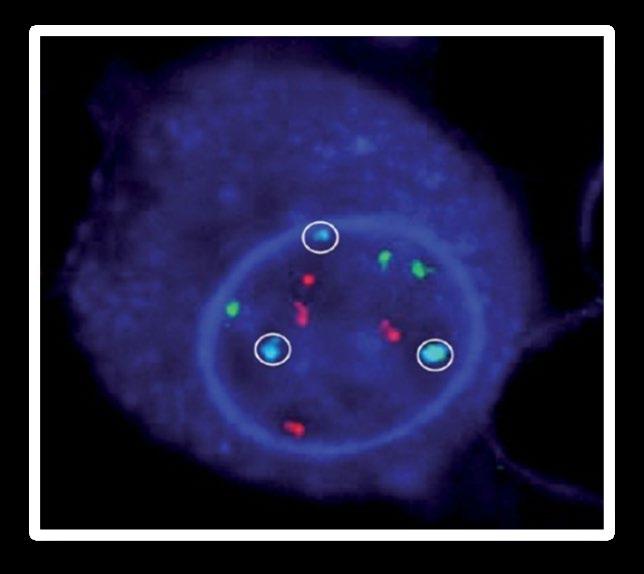

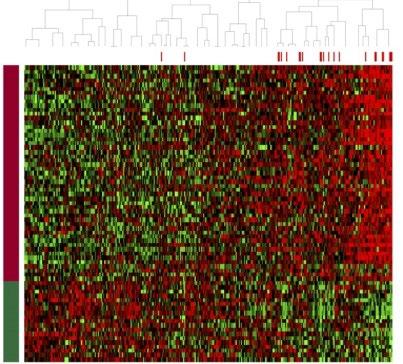
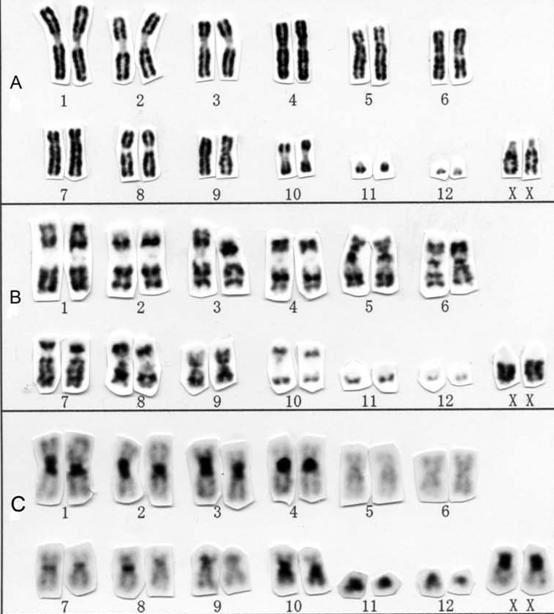
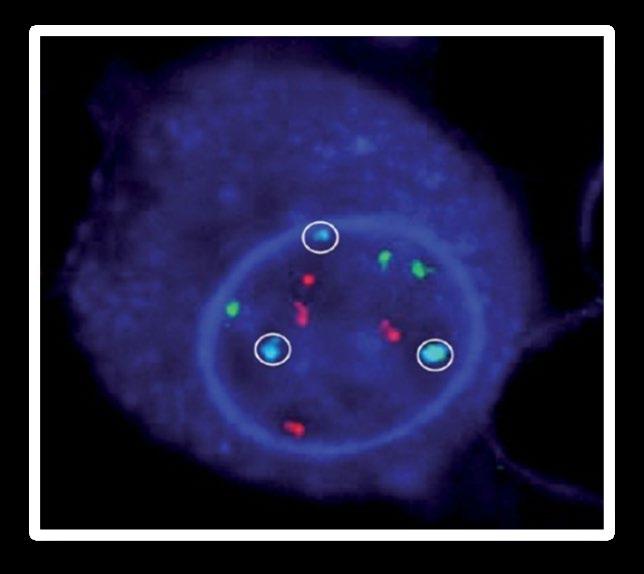
Conventional cytogenetic analysis (karyotyping) FISH (fluorescence in situ hybridization) Advances • Genetic expression profiling [GEP] • Whole-genome/ whole-exome sequencing • Plasma cell next generation sequencing DNA
Myeloma: The Importance of Genomic Testing
Staging Myeloma: FISH helps to Assign Risk in Myeloma Risk Category High Risk Standard Risk Findings on Chromosome (FISH) Analysis Results in the Bone marrow FISH: • Deletion 17th chromosome • Gain of chromosome 1q • Translocation 4 and 14 • Translocation 14 and 16 • Translocation 14 and 20 NGS: p53 mutation (on chrom 17) FISH: • Hyperdiploid: More than 1 pair of chromosomes (Trisomies) • Translocation 11 and 14 • Translocation 6 and 14 • Others • Normal *Based on the Updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) Consensus Guidelines 2013 Mikhael JR et al. Mayo Clin Proc. 2013;88:360. • Double Hit Myeloma: 2 high risk genetic abnormalities • Triple Hit Myeloma: 3 or more high risk genetic abnormalities











Stage 3 β2-microglobulin over 5.5 mg/L HIGH Lactate Dehydrogenase (LDH) High Risk Cytogenetics (FISH) Deletion 17 chromosome Translocation 4th and 14th Translocation 14th and 16th Translocation 14th and 20th AND Stage 1 β2-microglobulin under 3.6 mg/L Normal Lactate Dehydrogenase (LDH) NO High Risk Cytogenetics (FISH) AND *Based on the Updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) Consensus Guidelines 2013 Mikhael JR et al. Mayo Clin Proc. 2013;88:360. Palumbo et al. JCO September 10, 2015 vol. 33 no. 26 2863 2869 Revised International Staging System for Multiple Myeloma From International Myeloma Working Group Stage 2 Does not meet Criteria for Stage 1 or 3
Immunomodulatory Drugs ( Thalomid(Thalidomide), Revlimid(Lenalidomide Proteasome Inhibitors (Pis): Velcade(Bortezomib), Ninlaro(Ixazomib), Kyprolis(Carfilzomib) Antibodies Against Myeloma (Immunotherapy): Darzelex (Daratumumab), Sarclisa(Isatuximab), Empliciti(Elotuzumab)
IMiDs for Multiple Myeloma
How does it work?-SCIENCE!
• Direct inhibition of DNA synthesis of myeloma cells.
IMiDs for Multiple Myeloma
How does it work?-SCIENCE!
VEGF bFGF • Inhibition of blood vessel synthesis in the bone marrow.

• Direct inhibition of DNA synthesis of myeloma cells.

IMiDs for Multiple Myeloma
How does it work?-SCIENCE!
• Direct inhibition of DNA synthesis of myeloma cells.
• Inhibition of blood vessel synthesis in the bone marrow.
• Inhibition of adhesion between the myeloma and bone marrow stromal cells.
IMiDs for Multiple Myeloma
How does it work?-SCIENCE!
Direct inhibition of DNA synthesis of myeloma cells.
Inhibition of blood vessel synthesis in the bone marrow.
Inhibition of adhesion between the myeloma and bone marrow stromal cells.
Inhibition of the release of the cytokines IL-6, TNF-α, and IL-1β.



IL 6 IL 1β TNF α
•
•
•
•
IMiDs for Multiple Myeloma
How does it work?-SCIENCE!
• Direct inhibition of DNA synthesis of myeloma cells.
• Inhibition of blood vessel synthesis in the bone marrow.
• Inhibition of adhesion between the myeloma and bone marrow stromal cells.
•
Inhibition of the release of the cytokines IL-6, TNF-α, and IL-1β.
•
Activation of the body’s natural killer cells (T-cells) which attack the myeloma cells.
Rise of the IMiD Biologic Therapies
1990s, several thalidomide analogs were synthesized to increase efficacy and minimize toxicity.
2006 FDA approves Lenalidomide (Revlimid).
Revlimid is felt to be 50 to 2000 more potent than thalidomide.
Phase 2 trial 91% new myeloma achieved responses with Lenalidomide plus dexamethasone.
2013 FDA approves Pomalidomide.
Pomalyst and dexamethasone given to multi-refractory myeloma with response rates of 35 to 65%.
Combination of pomalidomide, bortezomib, and dexamethasone in relapsed MM response rates of 72%.
Iberdomide (CC-220) is the newest in the class and is now in clinical trials
CELMODs are the next class of IMiD with CC92480 drug more potent than iberdomide
Lenalidomide
N
H N O
NH2
Pomalidomide

O O
O O Thalidomide N
H N O
Blood. 2005;106:4050 4053. Blood. 2013 Jan 14. [Epub ahead of print]. Exp Hematol Oncol. 2012; 1: 27; J Clin Oncol. 2009;27(30):5008 5014.
O
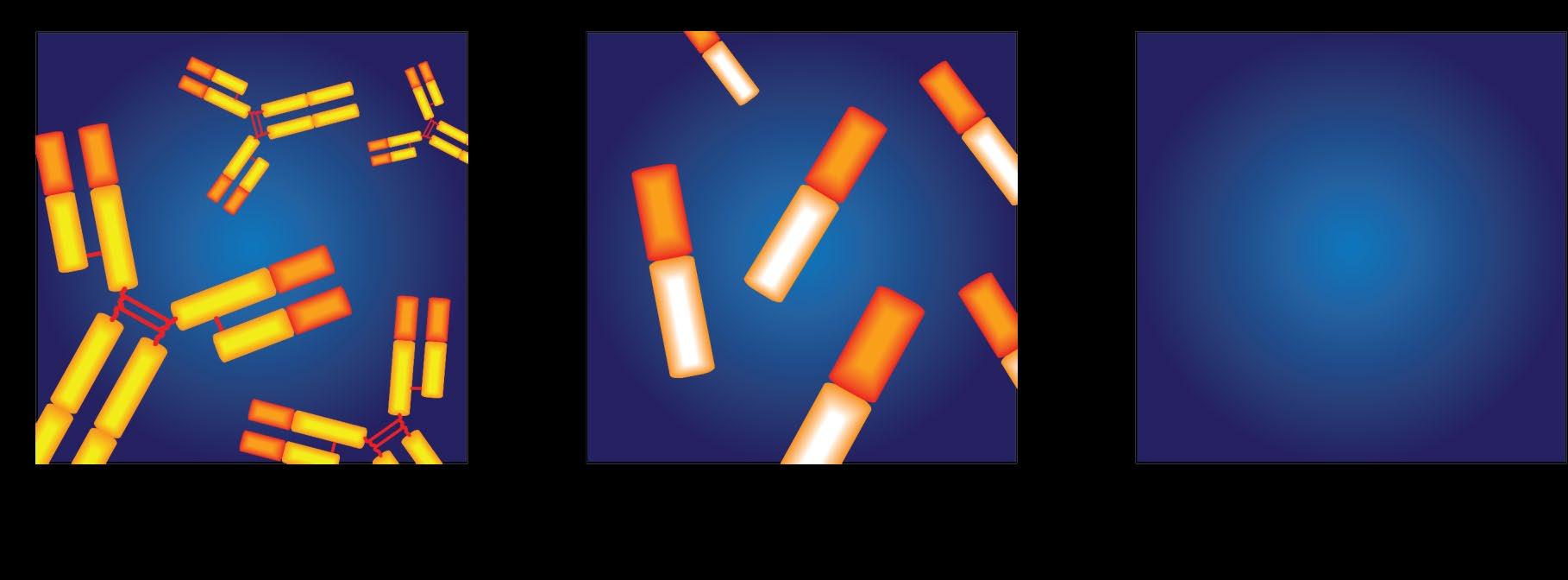
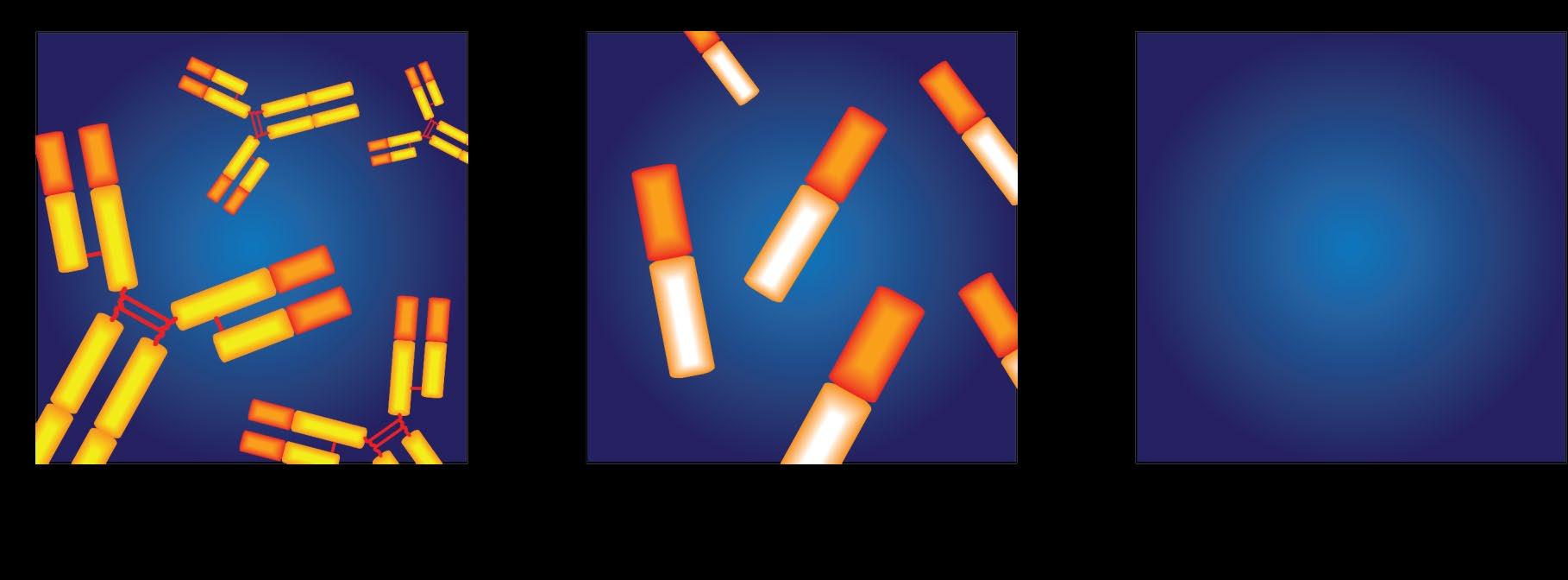
Rise of the Proteasome
Proteasome

 R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012
R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012
Rise of the Proteasome
Proteasome

R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012
Rise of the Proteasome

R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012
Rise of the Proteasome
• Bortezomib(velcade) approved by the FDA in 2003 in patients with relapsed refractory myeloma.
• Several phase 2 trials in newly diagnosed myeloma with bortezomib-dexamethasone induction.
o Responses 66% to 90%, including 15% to 21% Complete Responses!
• 2012 FDA approves Carfilzomib(Kyprolis); secondgeneration irreversible Proteasome inhibitor
• In refractory myeloma with 48% response rates. Higher in combination!
• Ixazomib (Ninlaro) is new oral boronated reversible proteasome inhibitor currently approved by the FDA in 11/2015.
Bortezomib(Velcade)
Carfilzomib(Kyprolis)

Ixazomib (Ninlaro)
R Vij et al. Br J Haem , June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012; Blood. 2014;124(7):1047–1055

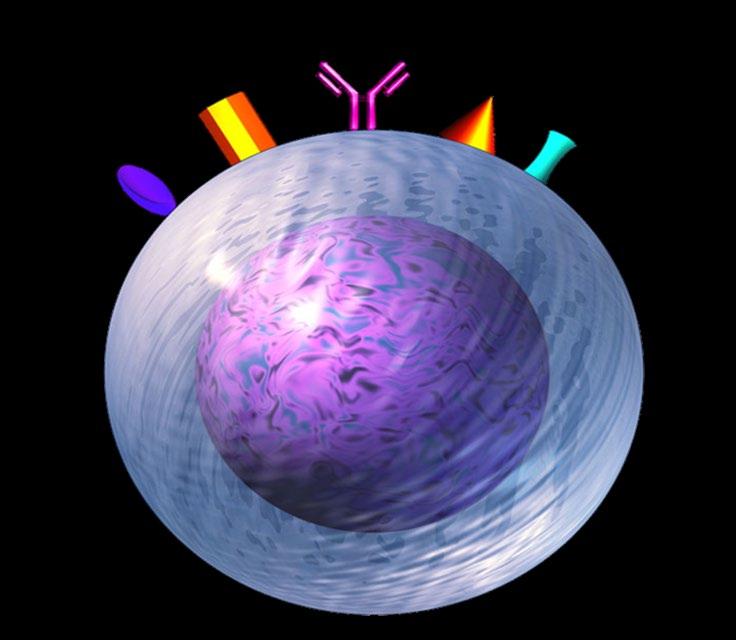










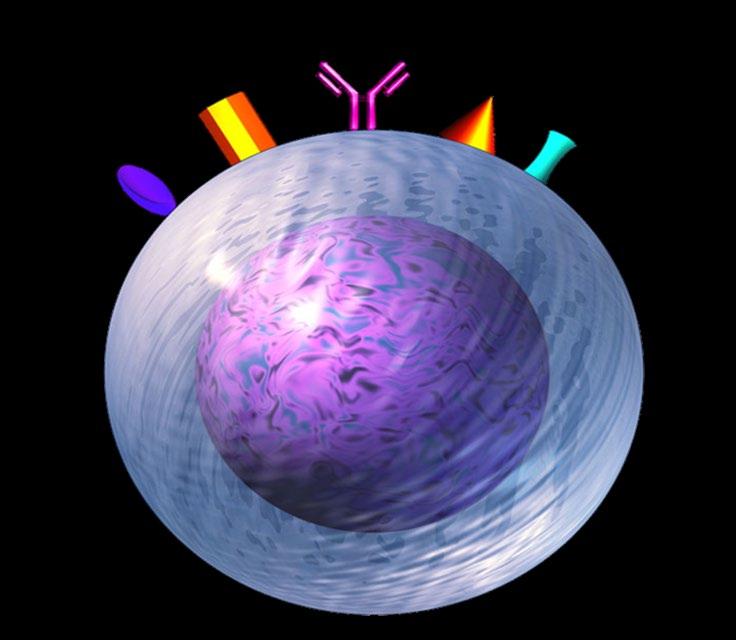
Targets on the Myeloma Cell Surface and Therapeutic Antibodies BCMA CD38 GPRC5D SLAMF7 FcRH5 Immune Therapies Belantamab Ide cel CAR T Cilta cel CAR T Teclistamab Other Bi-Specific Antibodies Other CAR-Ts Antibody Drug Elotuzumab Bi-Specific Antibodies Antibody Drug Daratumumab and Darzalex Faspro Isatuximab TAK-079 MOR202 Bi-Specific Antibodies CAR-T Bi-Specific Antibodies CAR-T













































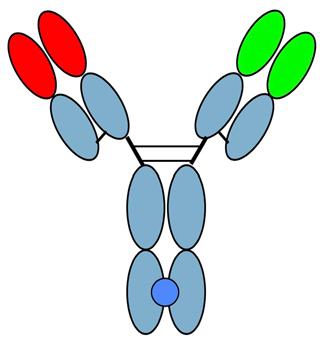
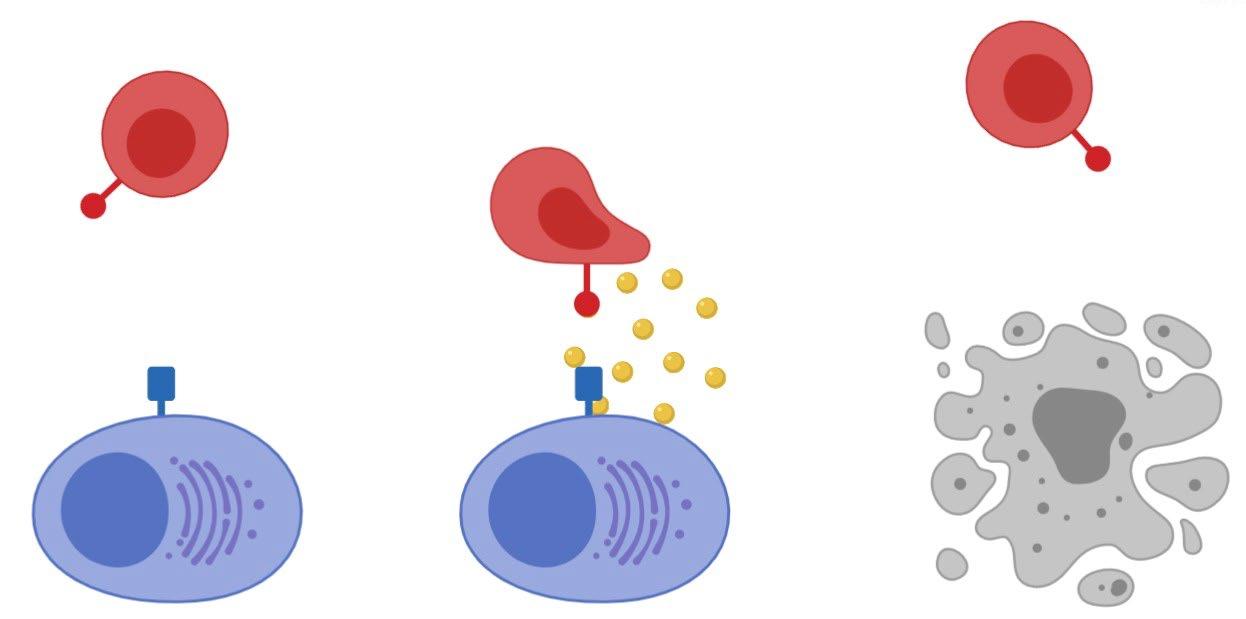
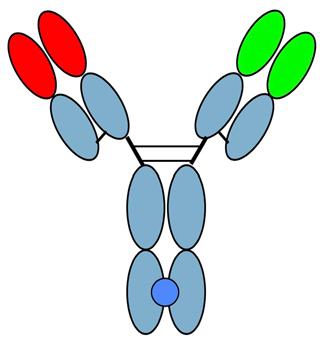
Antibody and Immune System Attack Manufactured Antibody Targeting of Myeloma Antibody Receptor Natural Killer Cell Good Guys Myeloma surface targets Manufactured Anti-Myeloma Antibody Complement Proteins Complement Protein Attack Myeloma Cells Attacking the Myeloma Cell Biology Macrophages Good Guys Increase production of cytoxic macrophages Inhibition of adhesion between the myeloma and bone marrow stromal cells
Tools of the Trade for Frontline Therapy Standard Drug Overview Class Drug Name Abbreviation Administration IMiD immunomodulatory drug Revlimid (lenalidomide) R or Rev Oral Thalomid (thalidomide) T or Thal Proteasome inhibitor Velcade (bortezomib) V or Vel or B Intravenous (IV) or subcutaneous injection (under the skin) Kyprolis (carfilzomib)* C or K or Car Ninlaro (ixazomib)* N or I Oral Chemotherapy Cytoxan (cyclophosphamide) C Oral or intravenous Alkeran or Evomela (melphalan) M or Mel Steroids Decadron (dexamethasone) Dex or D or d Oral or intravenous Prednisone P Monoclonal Antibodies Daratumumab (Darzalex) Dara Intravenous (IV) or subcutaneous injection (under the skin) *In Clinical Trials/ not FDA approved




Treatment Sequence and Regimens for Active Myeloma
Cancer
Clinical Practice
Oncology
• Revlimid • Velcade • Ninlaro • Observation • Thalidomide • Revlimid/Dara • Clinical trial • Velcade/Revlimid/Dex:(VRD) • Velcade/Thalomid/Dex:(VTD) • Velcade/Cytoxan/Dex:(CyBorD) • Darzalex/Revlimid/Dex:(DRD) • Darzalex/Velcade/Melphalan/Dex • Darzalex/Velcade/Thalidomide/Dex • Kyprolis/Revimid/Dex(KRD) • Darzalex/Velcade/Revlimid/Dex: Dara-RVD • Ninlaro/Revimid/Dex(IRD) • Clinical trials Frontline treatment Maintenance Relapsed Induction Maintenance • Stem Cell Transplant • Continue Induction • Clinical trial Consolidation Dara+Pomalyst+Dex Kyprolis+Pomalyst+Dex Cytoxan+Pomalyst+Dex Ninlaro+Pomalyst+Dex Elo+Pomalyst+Dex Elo+Thaliomide+Dex Dara+Kyprolis+Dex Kyprolis+Revlimid+Dex Elo+Revlimid+Dex Dara+Revlimid+Dex Dara+Velcade+Dex Elo+Velcade+Dex Cytoxan+Kyprolis+Thalidomide+dex 4 drug therapies of novel agents Ninlaro+Cytoxan+Dex Velcade+ Cytoxan+Dex Velcade+ Pomalyst+Dex Chemotherapy Selinexor+Dex Selinexor+Velcade Selinexor+ Dara Isatuximab(Sarclisa)+ Pomalyst+Dex Darzalex Faspro (under skin) Belantamab mafodotin (FDA approved 8/5/2020) Ide cel CAR T (FDA approved 3/26/2021) Cilta-cel CAR-T (FDA approved 2/28/2022) Teclistamab (FDA approved 10/25/2022) CLINICAL TRIALS! Rescue
National Comprehensive
Network. The NCCN
Guidelines in
Multiple Myeloma (Version 1.2020). http://www.nccn.org/.
https://www.msmart.org/mm-treatment-guidelines

Dispenzieri et al. Mayo Clin Proc 2007;82:323-341; Kumar et al. Mayo Clin Proc 2009 84:1095-1110; Mikhael et al. Mayo Clin Proc 2013;88:360 376. v18 //last reviewed June 2020
Transplant Candidate Newly Diagnosed MM Not Transplant Candidate Revlimid/Velcade/Dex (RVD) or Dara-Revlimid Dex (Dara-Rd) 9 to 12 cycles RVD-light or Dara-RD Others: D-VMP,D-VTD,RD 9 to 12 cycles High Risk Standard Risk Velcade Based Maintenance of VRD or Continued Dara-Rd Maintenance Revlimid Maintenance or Continued DaraRd Maintenance Dara-RVD x 4 cycles Other: KRD or Dara-KRD High Risk Early Auto SCT ?Tandem SCT or Dara-RVD Early Auto SCT Delayed Transplant Collect & store Continue Tx for 8m Standard Risk Revlimid Maintenance +/- Dara Revlimid Maintenance +/- Dara Velcade (PI) Based Maintenance Continued Dara-Rd Maintenance Preferred








Goals of Therapy: The Iceberg Model of Myeloma Partial response 50% reduction in M protein Very good partial response 90% reduction in M protein immunofixation positive only Complete remission No M-protein immunofixation negative Minimal Residual Dis Next Generation Molecular testing Minimal Residual Dis Flow Cytometry At diagnosis >1 Trillion Disease Burden (# of myeloma cells) Symptomatic Myeloma >1 Billion >10 Million 1 myeloma cell in 100K to 1 million normal cells
Stem Cell Transplant: Fighting Myeloma with the Left Hook!


33
N Engl J Med. 2022 Jul 14;387(2):132-147. doi: 10.1056/NEJMoa2204925 -Patients aged 18-65 yrs with symptomatic newly diagnosed MM following 1 cycle of RVD -56 sites within the United States from 2010 to 2018 Stem cell collection Induction Consolidation Maintenance Until Progression RVD cycles 2-3 (n = 357) RVD cycles 2-3 (n = 365) RVD cycles 4-8 RVD cycles 4-5 R (n = 291) R (n = 289) ASCT: Melphalan 200 mg/m2 + Stem Cell Support (n = 310) RVD +Stem Cell Transplant vs. RVD without Transplant DETERMINATION Trial of Newly Diagnosed MM: DESIGN End Points of Study and Follow -up • Primary end point: progression-free survival (time to next relapse) • Secondary end points included: • Response rates, overall survival, quality of life, and adverse events • Follow-up on participant status : median of 6 years






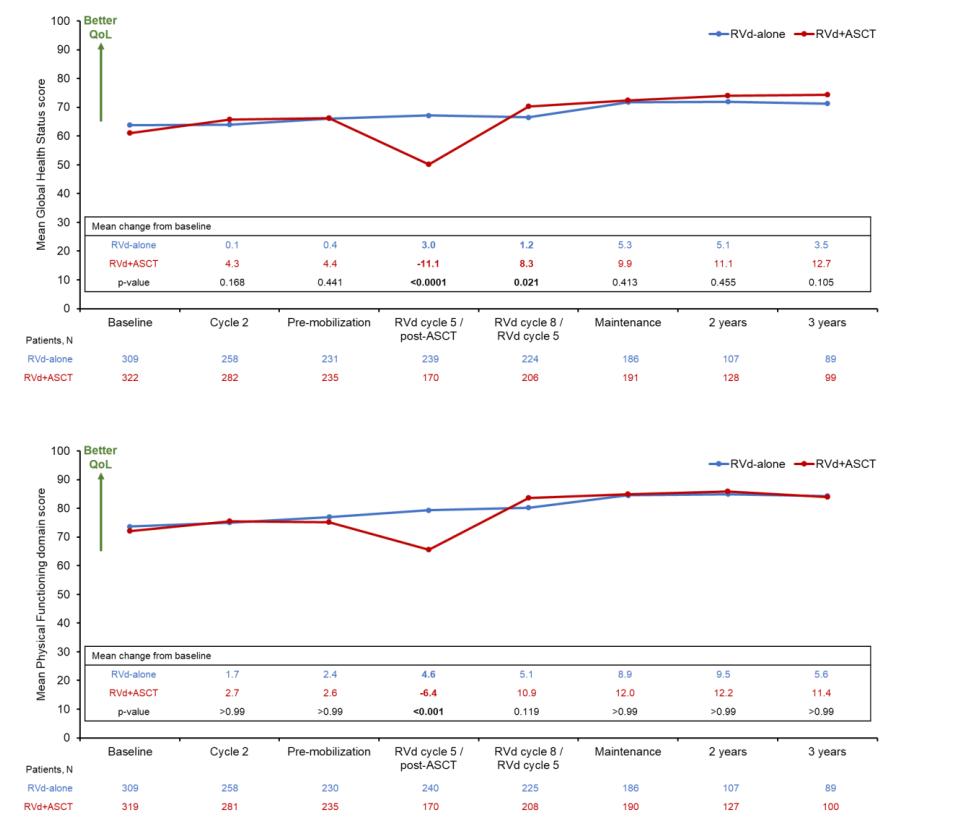
Parameter RVd- No Transplant (n = 357) RVD with Up Front Transplantation (n = 365) P Value Is it Significant? Grade 3 or 4 toxicities 78 94 YES! P<0.001 P<0.001 P<0.001 OVERALL SURVIVAL at 5 years (%) 79.2 80.7 NO Median duration of Partial Response or better, mo 38.9 54.4 YES! .003 Negative MRD 39.8 79 RVD +Stem Cell Transplant vs. RVD without Transplant DETERMINATION Trial of Newly Diagnosed MM RESULTS • At a median follow up of 76.0 months, the risk of disease progression or death was 53% higher in the RVD alone group than in the transplantation group (P<0.001) N Engl J Med. 2022 Jul 14;387(2):132-147. doi: 10.1056/NEJMoa2204925
RVD +Stem Cell Transplant vs. RVD without Transplant DETERMINATION Trial
of Newly Diagnosed MM Quality of Life
Global Health Status/QoL,
Physical Functioning
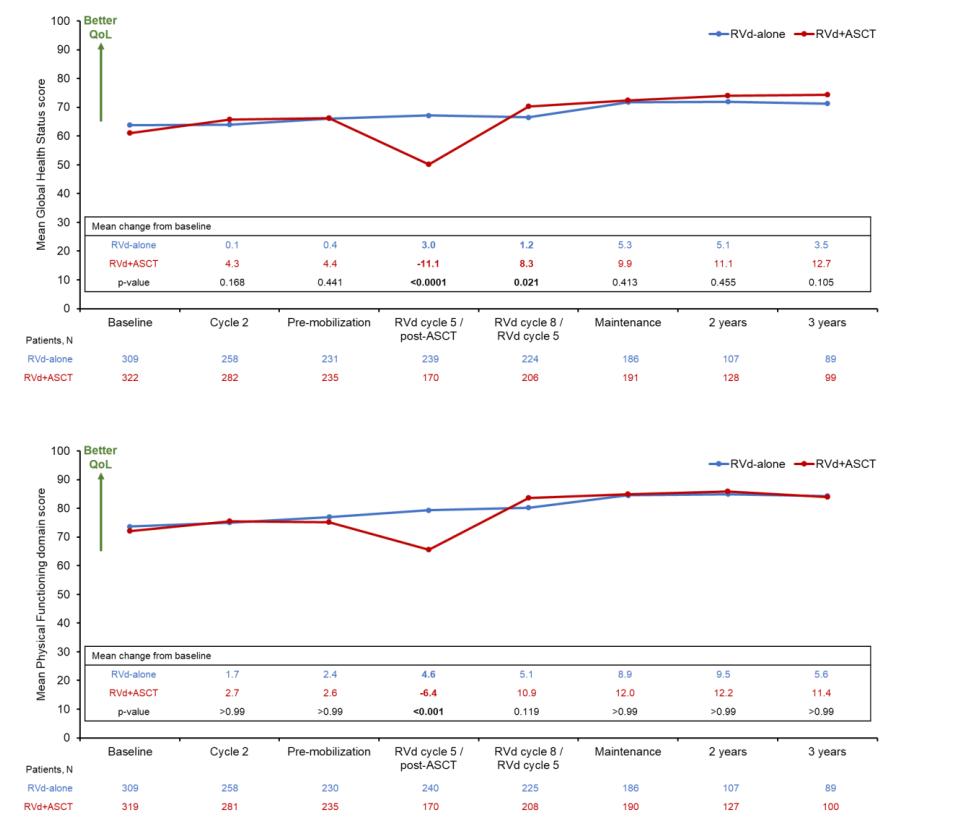
N Engl J Med. 2022 Jul 14;387(2):132-147. doi: 10.1056/NEJMoa2204925





Stadtmauer
ASH
ASCO
8506-8506 New Dx Myeloma After >2 cycles induction Tx ASCT eligible ≤ 70 yrs (N = 758) Melphalan 200 mg/m² IV Stem Cell Transplant Revlimid Maintenance 10 mg/day for 3 cycles, then 15 mg/day* (n = 257) Consolidation Velcade 1.3 mg/m² IV Days 1, 4, 8, 11 Revlimid 15 mg Days 1-15 Dexamethasone 40 mg IV Days 1, 8, 15 Four cycles (n = 254) Revlimid Maintenance 10 mg/day for 3 cycles, then 15 mg/day Second (Tandem) Stem Cell Transplant Melphalan 200 mg/m² IV Second ASCT (n = 247) Induction regimens RVD CyBorD RD VD Others What to do After Transplant? STaMINA: Phase III Study Design RESULTS • No difference in time to relapse (PFS) or Overall Survival in standard risk patients who have two transplants, consolidation RVD therapy, or just straight to maintenance after first BMT • Straight to maintenance is the easiest! • ? If high risk patients benefit from two transplants
EA, et al.
2016. Abstract LBA-1; Journal of Clinical Oncology 38, no. 15_suppl (
May 20, 2020)
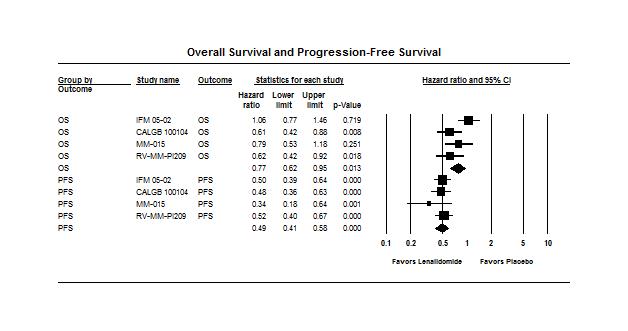
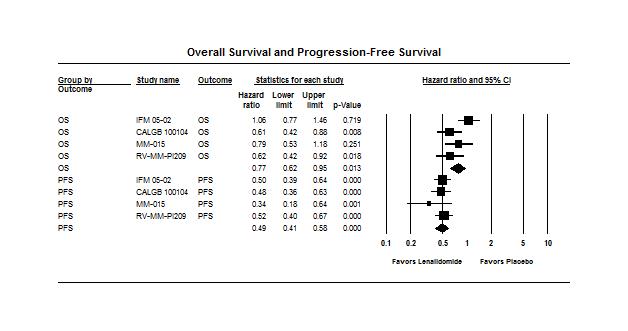
Analysis of the Maintenance Revlimid (Lenalidomide) Trials
• Data from 4 randomized trials of Revlimid (lenalidomide) maintenance vs. no maintenance – Involving a total of almost 2,000 multiple myeloma patients
• The results of the analysis showed that Revlimid maintenance therapy is associated significant improvement in progression-free survival and a modest improvement in overall survival
• Duration of maintenance is unknown

Support & Control of Bone Pain Multiple myeloma can cause weakened areas in the bone called osteolytic lesions which can compress the spinal cord or cause bone destruction. • Bone strengthening drugs: bisphosphonates (pamidronate & Zometa) or monoclonal antibodies (Xgeva) are given at diagnosis and continued for at least 2 years • Vitamin-D and Calcium supplements to help bone healing • Orthopedic support – Physical therapy, physical medicine consults, orthopedic/neuro surgery, radiation therapy, etc • Minimally invasive procedures: kyphoplasty or vertebroplasty • Use of medication to control pain • Anticonvulsants and antidepressants for treat relieve pain from nerve damage or numbness
Bone

GRIFFIN Randomized Phase II: Dara-RVD vs. RVD in Newly Diagnosed Multiple Myeloma Dara-RVD in 21-day cycles (n = 104) Transplant-eligible adults with Newly Diagnosed MM, with good performance status and kidney fxn (N = 207) Dara-RVD in 21-day cycles D: 16 mg/kg IV D1 VRd: as in induction Dara-R in 28-day cycles D: as in consolidation Q4W or Q8W R: 10 mg PO D1 21 of C7 9 and 15 mg PO D1 21 of C10 A S C T Induction: Cycles 1-4 Consolidation: Cycles 5-6† Maintenance: Cycles 7-32 Primary endpoint: CR by end of consolidation RVD in 21-day cycles (n = 103) RVD in 21-day cycles VRd: as in induction R in 28-day cycles R: 10 mg PO D1-21 of C7-9 and 15 mg PO D1-21 of C10 Randomized 1:1 Kaufman. ASH 2020. Abst.594; Voorhees PM etal. Blood. 2020 Aug 20;136(8):936 945.


Complete Response
Response
Good Partial Response
Partial Response
Patients (%) 60 0 Dara-RVD (n = 99) RVD (n = 97) ≥
≥
10.3 18.6
Response Rate
Response Rate = 99.0% End of Consolidation ≥ VGPR:
Abst#
Overall Response Rate = 99.0% End of study 83% ≥ 60% ≥ VGPR: 77% 14
Response Rate = 91.8% GRIFFIN Randomized Phase II: Dara-RVD vs. RVD in Newly Diagnosed Multiple Myeloma In the final analysis after >4 years of follow up, the addition of DARA to RVd led to a Progression Free Survival benefit favoring the Dara RVd arm with a 55% reduction in progression or death These data support use of D RVd induction/consolidation and D R maintenance as a NEW standard of care in Newly Diagnosed Myeloma
Depth of Response Stringent
(sCR) Complete
(CR) Very
(VGPR)
(PR)
CR: 42.3%
VGPR: 73.2%
Overall
= 91.8% Overall
Voorhees PM et al. Blood. 2020 Aug 20;136(8):936-945. Sborov et al. IMS Annual Meeting. 2022 Aug 26;
OAB-057
Overall
Study No. of patients Phase of study Efficacy Data Safety Data Dara-VMP vs VMP Dimopoulos MA, 2018 706 Phase III ORR = 90.9% sCR = 22.3% VGPR = 27.7% PR = 18.0% ≥VGPR = 72.9% CR+ = 45.1% Median PFS (at 27.8 months) = NR Grade 3 or 4 TEAEs = 23.7% Dara-IRD Kumar 2019 40 Phase II CR = 11% VGPR = 47% PFS = 97.5% ORR = 95% Grade ≥3 AEs = 42% Dara-RVD vs RVD followed by ASCT Voorhees 2020 D-RVD: 99 RVD: 97 Phase III ORR: DVRD=99.0% vs VRD=91.8%; 22 mo sCR: DVRD 62.6% vs RVD 45.4% MRD negativity DRVD 51.0% vs RVD 20.4% 24-mo PFS DRVD 95.8% RVD 89.8% Serious AEs were reported in 39 (39.4%) patients in the D-RVd group and 52 (51.0%) in the RVd group Dara-CVD Yimer 2018 87 NDMM (101 total) Phase II ≥VGPR = 56% CR = 9% ORR = 81% 12-month PFS = 87% OS = 99% Grade ≥3 AEs = 56% Dara-KRd Costa 2019 -------------------Landgren 2021 38 ----41 Phase II ORR = 100%; ≥VGPR = 92% after induction CR/sCR = 91% before BMT; MRD negative 65% at best response ORR = 100%; ≥VGPR = 95% after induction; PFS was 98%MRD negative 71% at 20.3 months follow-up Grade 3/4 AEs: neutropenia (n=7), infection (n=6), insomnia (n=4), hyperglycemia (n=2), rash (n=2) Isatuximab-RVD Ocio 2018 22 Phase I ORR = 93% MRD negativity = 38.5% sCR = 7.14% VGPR = 71.43% CR = 7.14% 7.5 mo PFS = 100% Grade ≥3 AEs = 46% Isatuximab-KRD for high-risk MM Abstract S204. EHA 2020 46 Phase II ORR = 100%, with PR=10%, VGPR=44% and CR=46%; 20 of 33 pts were MRD negative in ASCT eligible arm Grade 3/4 AE: neutropenia 34%, anemia10%, thrombocytopenia 14%, hypertension 12%, infection 8% Where We Are Going…4-Drug Induction for Newly Diagnosed Myeloma


It’s important to know… How to read your M-protein level IgG Kappa M-Protein M-Protein What is your MM risk/ stage What are your therapy options Know what side effects to expect so you can report them What is your response to tx Who is on your care team Obtain a second opinion Ask about clinical trials What are YOUR goals of therapy Be informed and empowered!

Survival
Multiple
Blood (ASH Annual Meeting Abstracts) 2011 118: Abstract 5070; Blood Advances, 2017 Vol1(4);p282-287. • With new biology-based medication 3 and 4 drug regimens the response rates are now >98% • We have had 32 drugs and tx indications FDA approved for myeloma 2015-2022! Myeloma is not curable…yet. But is survivable now! • With novel therapies are used at diagnosis, survival has improved dramatically ’ From 3.8 years to >8 years! ’ The 10yr relative survival rate has nearly doubled since in the past 20 years 2019 74,814 2011 2021 138,451 54,963 2004 People in the United States living or in a Remission from Multiple Myeloma
Advancements in
of
Myeloma






colecrai@msu.edu


47
Agenda After Break


11:05 AM - Relapsed Therapy and Clinical Trials
Amrita Krishnan, MD, City of Hope Comprehensive Cancer Center 11:45 AM - How to Manage Myeloma Symptoms and Side Effects

IMF REGIONAL COMMUNITY WORKSHOP – November 19, 2022
48
Sandra Rome, RN, MN, AOCN, CNS, CEDARS-SINAI
12:05
PM - Q&A with Panel
Relapsed Therapy and Clinical Trials Amrita Krishnan, MD


City of Hope Comprehensive Cancer Center

49
Approaches to Relapsed Myeloma


 Amrita Krishnan, MD FACP Director of Judy and Bernard Briskin Center for Myeloma City of Hope Cancer Center Executive Medical Director of Hematology & HCT- City of Hope Orange County
Amrita Krishnan, MD FACP Director of Judy and Bernard Briskin Center for Myeloma City of Hope Cancer Center Executive Medical Director of Hematology & HCT- City of Hope Orange County
Multiple Myeloma

Not
Time: Years!
is
One Disease! RVD+ASCT+Lenalidomide Maintenance Relapse 1 Relapse 2 Relapse 3
Disease Activity Relapse 1 Relapse 1 Relapse 2
Relapsing Nature of Multiple Myeloma: Clones Change over Time



Clone 1.1 Clone 1.2 Clone 2.1 Clone 2.2 Misc
Adapted from Dr. Brian Durie and Keats JJ, et al. Blood. 2012;120:1067 1076.
SYMPTOMATIC REFRACTORY RELAPSE RELAPSE MGUS or SMOLDERING MYELOMA ACTIVE MYELOMA M Protein g/L 2 5 10 ASYMPTOMATIC PLATEAU REMISSION Therapy Time MGUS = monoclonal gammopathy of undetermined significance



Factors in Selecting Salvage Therapy • Age/frailty • Performance status • Lifestyle/patient preferences • Drug metabolism • Compliance/adherence • Caregiver support • Renal insufficiency • Comorbidities Neuropathy − Cardiac Diabetes Low blood counts Burden • ISS/LDH • Marrow burden • Biochemical vs CRAB symptoms • Rate of progression • Extramedullary Biology • LDH elevation • Molecular − del[17p], t(4;14) • Access/trial availability • If previously treated Depth/duration − Relapse >60 d vs progression • Toxicity Myelosuppression Neuropathy VTE − Secondary cancers • Administration route • Single or combination • Cost and copays Treatment Disease Patient
Slide courtesy of A Chari.
Open-Label, Multicenter, Randomized, Active-Controlled, Phase 3 Study of DRd vs Rd in Patients With Relapsed or Refractory MM: POLLUX Key eligibility criteria • RRMM • ≥1 prior line of therapy • Prior lenalidomide exposure but not refractory • Patients with creatinine clearance ≥30 mL/min Primary end point • PFS Secondary end point • TTP • OS • ORR, VGPR, CR • MRD • Time to response • Duration of response R A N D O M I Z E DRd (n=286) Rd (n=283) 1:1 Cycles: 28 days Stratification factors • No prior lines of therapy • Daratumumab is like chocolate SS stage at study entry • Prior lenalidomide
DRd vs Rd in Pts With Relapsed or Refractory MM (POLLUX): 4 Year Follow-Up
Intent-to-treat population
48 mo PFS rate
100 80 60 40 20 0
% Surviving Without Progression 21%
HR, 0.44; 95% CI, 0.35–0.54 P<0.0001
48% D Rd Median: 45.0 mo Rd Median: 17.5 mo
One previous line of
48 mo PFS rate
This is our common regimen for first relapse
100 80 60 40 20 0
% Surviving Without Progression 24%
HR, 0.42; 95% CI, 0.31 0.58 P<0.0001
treatment 0 3 6 9 12 15 24 27 18 21 30 33 36 39 42 51 54 45 48 57 60 63 Months
54% D Rd Median: 53.3 mo Rd Median: 19.6 mo
0 3 6 9 12 15 24 27 18 21 30 33 36 39 42 51 54 45 48 57 60 63 Months
Kaufman JL et al. Blood. 2019;134: Abstract 1866.
Dara-Pd vs Pd (APOLLO): PFS; Favored Regimen
Median PFS among patients refractory to lenalidomide was 9.9 months for D-Pd and 6.5 months for Pd
Dimopoulos MA et al. Lancet Oncol. 2021;22:801.
4 6 8 10 12
14 18 16 20 22 24 26
Median follow-up Tthis is our regimen for patients progressing on Lenalidomide % Surviving Without Progression 20 40 60 80 100 0 0 2
34 Months
28 30 32 Pd median: 6.9 months 12-month PFS rate D-Pd median: 12.4 months HR, 0.63; 95% CI, 0.47–0.85; P=0.0018 36 52% 35%
Addition of DARA SC to Pd improved PFS, with a 37% reduction in the risk of progression or death.
Carfilzomib, Dexamethasone, and Daratumumab vs Carfilzomib and Dexamethasone in RRMM: Phase 3 CANDOR Study
28-day cycles until disease progression
KdD (n=312)
Carfilzomib 56 mg/m2 IV (30 min) Days 1, 2, 8, 9, 15, 16 (20 mg/m2 days 1, 2, cycle 1 only)
Dexamethasone 40 mg (20 mg for patients >75 years old) oral or IV once weekly
Key inclusion criteria:
• Relapsed or refractory multiple myeloma
• 1–3 prior lines of therapy
• Partial response or better to ≥1 line
Daratumumab 8 mg/kg IV days 1, 2, cycle 1; 16 mg/kg once weekly for remaining doses of cycle 1, 2, then every 2 weeks (cycles 3–6), then every 4 weeks
Kd (n=154)
Carfilzomib 56 mg/m2 IV (30 min)
Days 1, 2, 8, 9, 15, 16 (20 mg/m2 days 1, 2, cycle 1 only)
Dexamethasone 40 mg (20 mg for patients >75 years old) oral or IV once weekly
• Primary end
PFS • Key secondary end points: OS, ORR, safety
point:
2:1
N=466 Randomized
Updated Efficacy Results of the Phase 3 CANDOR Study
Kd
41% reduction in the risk of progression/ death and a 13.4-month improvement in median PFS with KdD versus Kd I use this young patients Aggressive Relapse
Dimopoulos MA et al. Blood. 2020;136: Abstract 2325.
0 3 6 9 12 15 18 21 24 27 30 33 36
Months From
1.0 0.8 0.6
KdD (n=312) Kd (n=154) Median treatment duration, months 18.3 9.3 Median PFS follow-up, months 27.8 27.0 Median PFS by ORCA, months 28.6 15.2 HR (KdD/Kd) (95% CI) 0.59 (0.45–0.78)
KdD
Randomization
0.4 0.2 0.0 Proportion Surviving Without Progression
Generally Consistent PFS Benefit for KdD vs Kd Across Subgroups
0.0 0.5 1.0 1.5 2.0
Dimopoulos MA et al. Blood. 2020;136: Abstract 2325.
Subgroup KdD (n=312) Kd (n=154) Hazard ratio for KdD vs Kd (95% CI) Events/ patients Median PFS, months Events/ patients Median PFS, months All randomized subjects 140/312 28.6 85/154 15.2 0.59 (0.45, 0.78) ISS stage per IXRS at screening 1 or 2 101/252 NE 68/127 15.8 0.60 (0.44, 0.81) 3 39/60 13.0 17/27 7.4 0.57 (0.32, 1.03) Age at baseline (years) ≤65 0.51 (0.35, 0.73) >65 0.73 (0.48, 1.12) Cytogenetic risk group High risk 30/48 15.6 18/26 5.6 0.49 (0.26, 0.92) Standard risk 39/107 NE 26/56 16.6 0.54 (0.32, 0.91) Unknown 71/157 28.1 41/72 15.7 0.64 (0.43, 0.94)
Kd better KdD better
IKEMA
Isatuximab + Carfilzomib and Dex vs Carfilzomib and Dex in RRMM
Stratification factors:
• Prior line 1 vs >1
• R-ISS: I or II vs III vs not classified
Isa-Kd (n=179)
• Isa: 10 mg/kg on D1, 8, 15, 22 in C1, then Q2W
• K: 20 mg/m2 D1–2; 56 mg/m2 D8–9, D15–16 C1; 56 mg/m2 D1–2, D8–9, D15–16 all subsequent cycles
• d: 20 mg D1–2, D8–9, D15–16 and D22–23 each cycle
3:2
Treatment until PD, unacceptable toxicities, or patient choice
Primary end point: PFS (IRC)
Key secondary end points: ORR, rate of ≥VGPR, MRD negativity, CR rate, OS
Median PFS control arm estimated at 19 months
Kd (n=123)

• 1–3 prior lines

• No prior therapy with carfilzomib
• Not refractory to prior anti-CD38
• K: 20 mg/m2 D1–2; 56 mg/m2 D8–9, D15–16 C1; 56 mg/m2 D1–2, D8–9, D15–16 all subsequent cycles
• d: 20 mg D1–2, D8–9, D15–16 and D22–23 each cycle
Prespecified interim analysis when 65% PFS events (103) as per IRC Other CD38 antibody choices are all good
Study: A Phase 3 Randomized, Open-Label Study of
Relapsed MM N=302 R a n d o m i z a t i o n
IKEMA Study: PFS
Proportion Surviving Without Progression
1.0 0.8 0.6 0.4 0.2 0.0 0 3 6 9 12 15 18 21 24 27
Isa-Kd: mPFS: NR (95% CI, NE–NE)
Kd: mPFS: 19.15 months (95% CI, 15.770–NE)
HR 0.531 (99% CI, 0.32–0.89) P=0.0007
Months Since Randomization
Isa-Kd showed improvement in PFS with 47% reduction of risk of progression or death vs Kd.
Moreau P et al. Lancet. 2021;397:2361.
Isa-Kd vs Kd in RRMM (IKEMA): PFS Subgroup Analyses
Isa-Kd Kd
Subgroup
Hazard ratio (95% CI) No. of events/total no.
All patients 48/179 55/123 0.531 (0.359–0.786)
Age <65 years 25/88 26/66 0.640 (0.370–1.109) ≥65 years 23/91 29/57 0.429 (0.248–0.742)
Baseline eGFR (MDRD)
≥60 mL/min/1.73 m² 32/122 38/93 0.625 (0.391–1.001) <60 mL/min/1.73 m² 10/43 10/18 0.273 (0.113–0.660)
Number of prior lines of therapy 1 18/80 19/55 0.589 (0.309–1.123) >1 30/99 36/68 0.479 (0.294–0.778)
Prior PI treatment*
Yes 22/81 20/47 0.565 (0.308–1.036) No 26/98 35/76 0.493 (0.296–0.819)
Prior IMiD treatment* Yes 22/81 29/62 0.498 (0.286–0.869) No 26/98 26/61 0.542 (0.314–0.933)
Refractory to Len Yes 23/57 25/42 0.598 (0.339–1.055) No 5/15 9/17 0.448 (0.149–1.349)
High-risk cytogenetic status Yes 17/42 15/31 0.724 (0.361–1.451) No 27/114 35/77 0.440 (0.266–0.728)
ISS staging at study entry I 20/89 24/71 0.592 (0.327–1.071) II 17/63 16/31 0.375 (0.188–0.748) III 11/26 14/20 0.650 (0.295–1.434)
Consistent treatment effect was seen for Isa-Kd across subgroups.
0 0.5 1 1.5 2
Isa-Kd better Kd better
Moreau P et al. Lancet. 2021;397:2361.

My Comments: RRMM, 1–3 Prior Lines • Targeting CD38 = Peloton; everyone’s doing it! • Combo with carfilzomib = very effective • …but what if you used dara in the 1st line? Trial Arms PFS triplet (mo) PFS doublet (mo) HR P value Apollo DPd vs Pd 12.4 6.9 0.63 0.0018 CANDOR KdD vs Kd 28.6 15.2 0.59 NA IKEMA IKd vs Kd NR 19.15 0.531 0.0007
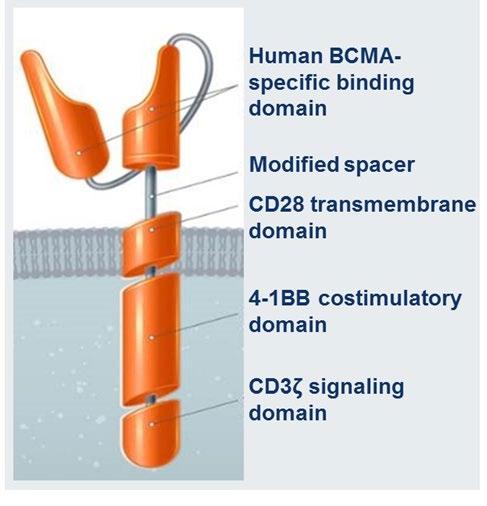
Rationale for Targeting BCMA
• BCMA is a cell surface protein expressed on late-stage B cells and plasma cells but virtually absent on naïve and memory B cells1-3
• BCMA is highly expressed on malignant plasma cells in all patients with MM3-5 • BCMA ligands, BAFF and APRIL, are detected in increased levels in the circulation of patients with MM3,5
Cho S-F et al. Front Immunol. 2018;9:1821;
Novak AJ et al. Blood. 2004;103:689;
Tai YT et al. Blood. 2014;123:3128.
3.
• BCMA is essential for the proliferation and survival of malignant plasma cells 3 Growth and survival of MM cells Activation of signaling cascades Malignant plasma cell BCMA APRIL BAFF γ-secretase sBCMA 1. Tai YT et al. Immunotherapy. 2015;7:1187; 2. Ryan MC et al. Mol Cancer Ther. 2007;6:3009;
4.
5.
Summary of Administration Considerations for
Tai YT et al. Blood. 2014;123:3128. Trudel S et al. Lancet Oncol. 2018;19:1641. Trudel S et al. Blood Cancer J. 2019;9:37.
Belantamab
mafodotin: humanized, afucosylated, IgG1 BCMA-targeted ADC that neutralizes soluble BCMA FDA-approved: For patients with R/R MM after ≥4 previous therapies including an anti−CD-38 mAb, a PI, and an IMiD Anti-BCMA antigen-binding site mAb that targets tumorspecific or tumorassociated antigens MMAF (potent cytotoxic agent) Stable linker releases payload only in target cell Enhanced ADCC Afucosylation Stable in circulation Linker MMAF (highly potent auristatin) Cytotoxic agent 2.5 mg/kg IV once every 3 wk as infusion over 30 min Dosing
steroids not required
to
or
with belantamab, but patients should be
for infusion-related reactions Counsel patients on what to expect when receiving belantamab, including the risk of ocular toxicity and the need for ophthalmic examinations prior to each dose
is only available through REMS program due to potential for ocular toxicity
Mafodotin Belantamab
Systemic
prior
initial infusion
in combination
monitored
Belantamab
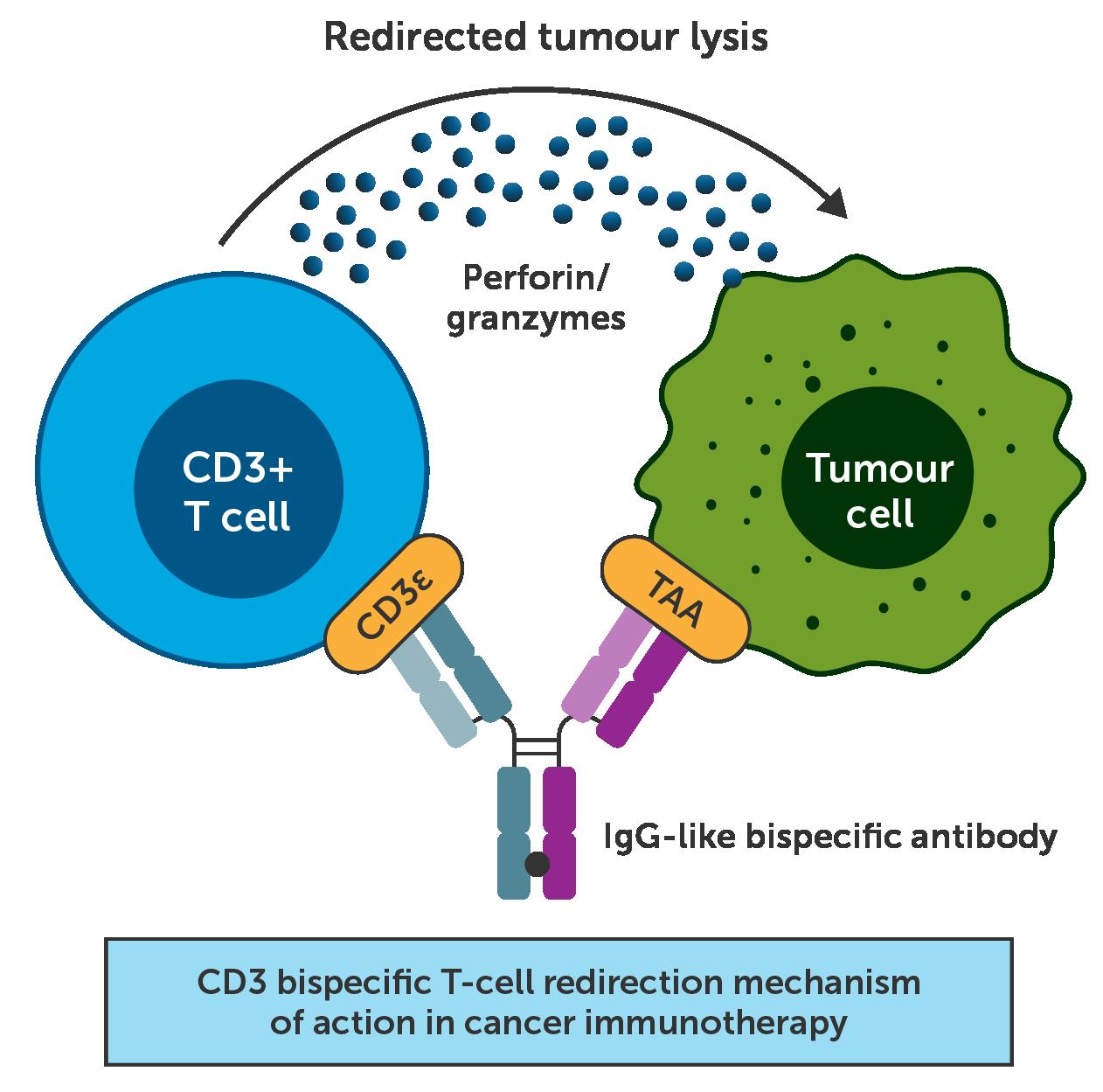
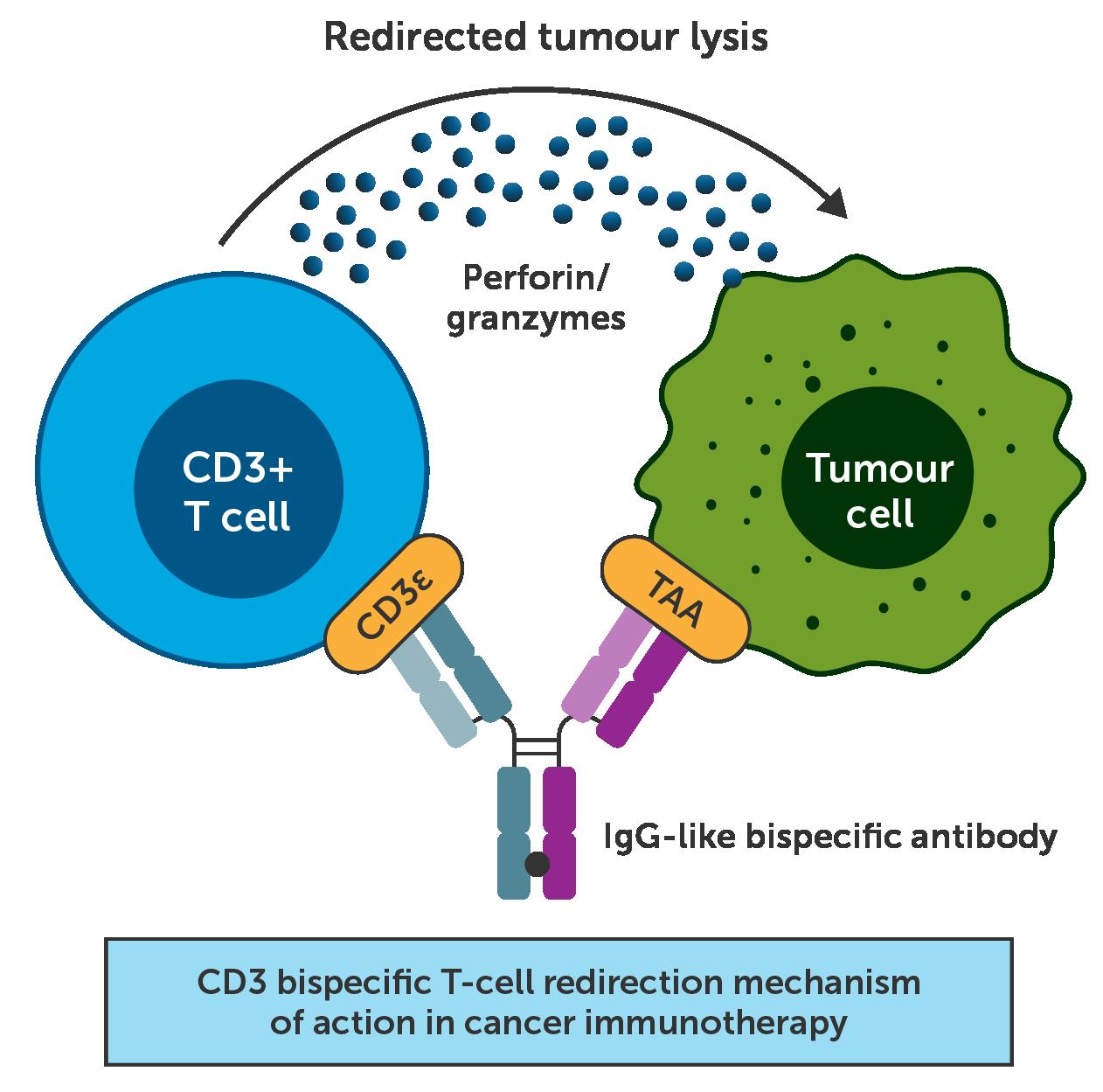
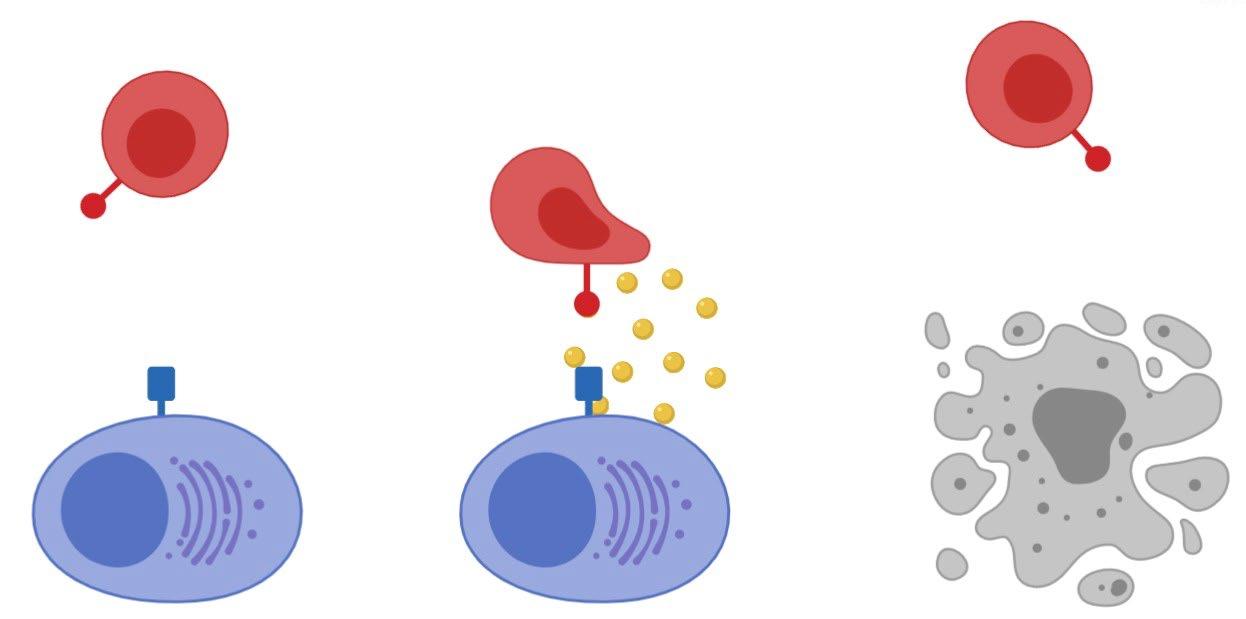
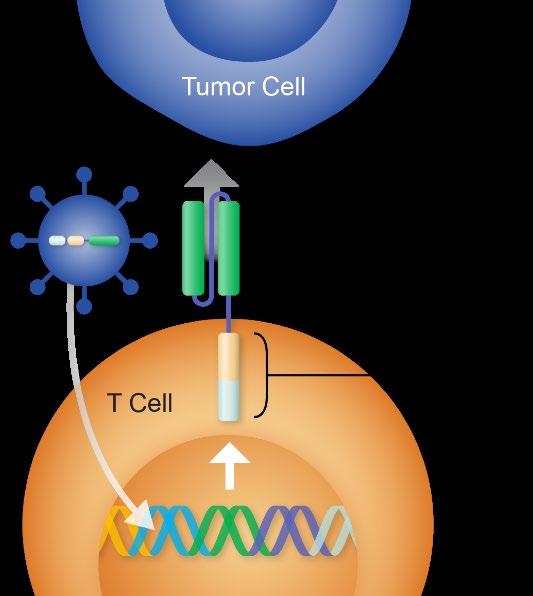
Bispecific Antibodies
Singh A, et al. 2021;124(6):1037 1048.
CITY OF HOPE
• Bispecific antibodies bind MM cell (multiple targets available) and to T lymphocyte
MajesTEC-1: Study Design
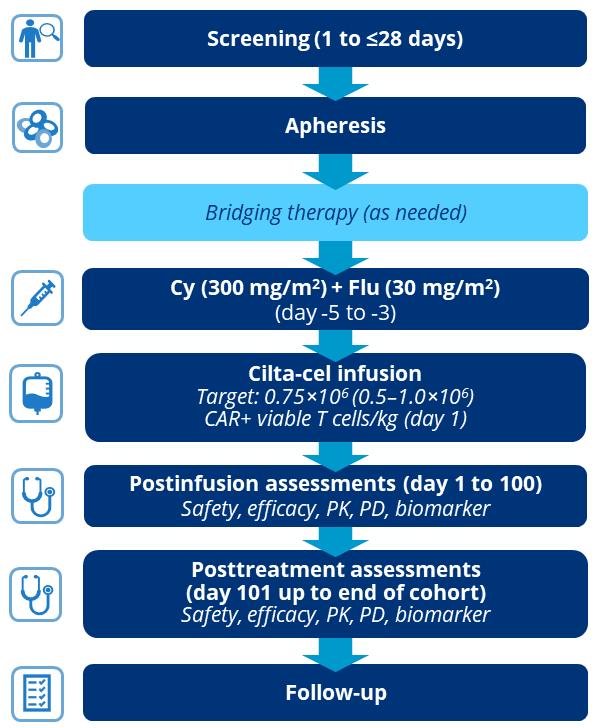
• First-in-human, phase 1/2, open-label, multicohort, multicenter, dose-escalation study evaluating teclistamab in patients with RRMM who previously received ≥3 lines of therapy (triple-class exposed)
SCREENING
Cohort A (triple-class exposed)
Key eligibility criteria

• Documented, measurable RRMM
• ≥3 PL, including prior PI, IMiD, and anti-CD38
• No prior BCMA-targeted therapy
Week 1
TREATMENT
POST TREATMENT
• Step-up doses of teclistamab SC (0.06 and 0.3 mg/kg) Cycles ≥1
• Weekly teclistamab SC 1.5 mg/kga
• Continue until progressive disease
Follow-up 2 years after last patient enrolled
• Primary endpoint: ORR
• Key secondary endpoints: DOR, ≥VGPR, ≥CR, sCR, TTR, MRD status, PFS, OS, safety, PK, immunogenicity, PROs
aSchedule change to biweekly (every other week) dosing was permitted based on response.
BCMA, B cell maturation antigen; CR, complete response; DOR, duration of response; IMiD, immunomodulatory drug; MRD, minimal residual disease; ORR, overall response rate; OS, overall survival; PFS, progression free survival; PI, proteasome inhibitor; PK, pharmacokinetics; PL, prior line; PRO, patient reported outcome; RRMM, relapsed/refractory multiple myeloma; sCR, stringent CR; SC, subcutaneous; TTR, time to response; VGPR, very good partial response
67
MajesTEC-1: Overall Response to Teclistamab
ORR of 63.0% (95% CI: 55.2–70.4) represents a substantial benefit for patients with triple-class exposed disease
• Median time to response (n=104)
• First response: 1.2 months (range: 0.2–5.5)
• Best response: 3.8 months (range: 1.1–16.8)
• MRD negativity rate at 10 5b
in the all-treated (N=165)

of
population
evaluable patients (44 of 54) were MRD negative
Almost half (46.2%) of
with
were
68
• 26.7%
patient
81.5%
MRD
•
patients
≥CR
MRD negative Analysis cutoff date: March 16, 2022. aPR or better, IRC assessed, per IMWG 2016 criteria. bAll MRD assessments were done by next generation sequencing. CR, complete response; IMWG, International Myeloma Working Group; IRC, independent review committee; MRD, minimal residual disease; ORR, overall response rate; PR, partial response; sCR, stringent complete response; VGPR, very good partial response 4.2% 19.4% 6.7% 32.7% 0 10 20 30 40 50 60 70 80 All Treated PR VGPR CR sCR ORRa ≥VGPR: 58.8% Patients (%) 63.0% (104/165) ≥CR: 39.4%
MajesTEC-1: Duration of Response
DOR
CR or better median DOR not reached (95% CI: 16.2–NE)
• Overall median DOR of 18.4 months (95% CI: 14.9–NE), and was not yet mature with data from 71 patients (68.3%) censored
Patients at risk Overall
Overall median DOR 18.4 months (95% CI: 14.9–NE)
• 12-month event-free rate:
• Overall:
Patients with CR or better:
68.5% (95% CI: 57.7–77.1) 80.1% (95% CI: 67.6–88.2)
69
•
104 101 35 17 0 Months 0 0 3 6 9 12 15 18 21 24 20 40 60 Patients (%) 80 100 0 27 65 65 89 60 74 55 28 16 7 6 2 2 0 0 CR or better
MajesTEC-1: Overall Safety Profile; watch for infections
Hematologic
Teclistamab was well tolerated; discontinuations and dose reductions were infrequent
• 2 patients (1.2%) discontinued due to AEs (grade 3 adenoviral pneumonia; grade 4 PML) • 1 patient had dose reduction at cycle 21 • The most common AEs were CRS and cytopenias • Infections occurred in 126 (76.4%) patients (grade 3/4: 44.8%) • 123 patients (74.5%) had evidence of hypogammaglobulinemiaa • There were 19 deaths due to AEs, including 12 COVID-19 deaths • 5 deaths due to teclistamab-related AEs:
70
• COVID-19 (n=2) • Pneumonia (n=1) • Hepatic failure (n=1) • PML (n=1) AEs ≥20%, n (%) Any Grade Grade 3/4
Neutropenia 117 (70.9) 106 (64.2) Anemia 86 (52.1) 61 (37.0) Thrombocytopenia 66 (40.0) 35 (21.2) Lymphopenia 57 (34.5) 54 (32.7)
Nonhematologic CRS 119 (72.1) 1 (0.6) Diarrhea 47 (28.5) 6 (3.6) Fatigue 46 (27.9) 4 (2.4) Nausea 45 (27.3) 1 (0.6) Pyrexia 45 (27.3) 1 (0.6) Injection site erythema 43 (26.1) 0 (0) Headache 39 (23.6) 1 (0.6) Arthralgia 36 (21.8) 1 (0.6) Constipation 34 (20.6) 0 (0) Cough 33 (20.0) 0 (0)
Bispecific Antibodies Clinical Trials in Multiple Myeloma future state Agent Targets Phase Clinical Trial Number Status AMG420 BCMAxCD3 I NCT03836053 Completed Pavurutamab AMG701 BCMAxCD3 I/II NCT03287908 Ongoing Alnuctamab CC93269 BCMAxCD3 I NCT03486067 Ongoing Elrantamab PF06863135 BCMAxCD3 I NCT03269136 Ongoing Linvoseltamab RGN5458 BCMAxCD3 I/II NCT03761108 Ongoing Teclistamab JNJ64007957 BCMAxCD3 Ib I NCT04108195 NCT03145181 Ongoing Ongoing TNB-383B BCMAxCD3 I NCT03933735 Ongoing Talquetamab JNJ64407564 GPRC5dxCD3 Ib I NCT04108195 NCT03399799 Ongoing Ongoing Cevostamab BFCR4350A FCRH5xCD3 I NCT03275103 Ongoing GBR1342 CD38xCD3 I/II NCT03309111 Ongoing AMG424 CD38xCD3 I NCT03445663 Closed Updated from Lancman, et al. ASH 2020.
Talquetamab: GPRC5D x CD3 Bispecific Antibody























Talquetamab includes technology licensed from GenMab. 1Smith Sci Transl Med 11(485):eaau7746. 2Verkleij HemaSphere 3(S1):230, Poster #PF556. 3Pillarisetti Blood 135(15):1232. RRMM, relapsed and/or refractory multiple myeloma

• Talquetamab is a first-in-class DuoBody® antibody that binds to both GPRC5D and CD3
• Talquetamab redirects T cells to GPRC5D-expressing myeloma cells to mediate cell killing
72 Myeloma Cell T cell GPRC5D Talquetamab CD3 Cell Death Activation
• Antitumor activity was demonstrated in primary myeloma cells and xenograft models of MM1 3 • First-in-human phase 1 study is ongoing to evaluate talquetamab in patients with RRMM (NCT03399799)
Perforin and Granzymes
Talquetamab: Overall Response Rate
73
n=2 n=3 n=4 n=3 n=1 n=3 n=5 n=2 0% 20% 40% 60% 80% 5–45 µg/kg SC n=14 135 µg/kg SC n=8 405
SC
n=13 800
SC n=11 ORRa for SC Doses PR VGPR CR sCR 69% ≥VGPR 39% 50% 14% 73%
At the RP2D of 405 µg/kg SC 69% ORR (9/13) Median 3.7 month (1.7–6.5) follow up for responders Median time to first confirmed response was 1 month (1–2) 67% (6/9) of triple class refractory patients responded 100% (2/2) of penta drug refractory patients responded aAmong response evaluable patients who had at least 1 study treatment and 1 postbaseline disease evaluation; includes unconfirmed responses. CR, complete response; ORR, overall response rate; PR, partial response; sCR, stringent complete response, VGPR, very good partial response
µg/kg
(RP2D)
µg/kg
At most active doses of 20–180 µg/kg IV and 135–800 µg/kg SC 66% ORR (33/50) ≥VGPR was 42% 67% ORR (12/18) in IV cohorts and 66% ORRa (21/32) in SC cohorts
Talquetamab: Safety Profile ;unique Taste and Nails
AEs (≥25% of Total) `
Hematologic, n (%)
Total (N=157) 3.6 mo (0.1 28.1) mF/U
405 µg/kg SC RP2D (n=19) 2.7 mo (0.1 6.5) mF/U All Grade Grade ≥3
Anemia 76 (48) 43 (27) 5 (26) 0 Neutropenia 74 (47) 48 (31) 9 (47) 8 (42)
Lymphopenia 62 (40) 57 (36) 3 (16) 3 (16)
Leukopenia 50 (32) 25 (16) 4 (21) 3 (16) Thrombocytopenia 50 (32) 20 (13) 4 (21) 1 (5)
Nonhematologic, n (%)
CRS 84 (54) 5 (3) 13 (68) 0
Dysgeusia 60 (38) NA 9 (47) NA
Fatigue 46 (29) 1 (1) 3 (16) 0
Headache 43 (27) 2 (1) 3 (16) 0
Pyrexia 42 (27) 1 (1) 2 (11) 0
Diarrhea 39 (25) 4 (3) 3 (16) 0
3 DLTs across all doses; no DLT at RP2D
Gr 4 increased lipase (7.5 µg/kg IV)
Gr 3 maculopapular rash (n=2; 135 and 800 µg/kg SC)
Dose reductions at the RP2D were less frequent and occurred later compared with the 800 µg/kg dose
Infections in 38% of patients; 16% at RP2D
8% had Gr ≥3 infections across all doses No Gr ≥3 infections at RP2D
Neurotoxicity in 9 patients (6%); 1 (5%) at RP2D
6 (6%) with IV and 3 (6%) with SC dosing 3 Gr ≥3 events with IV dosing; none with SC Gr 2 encephalopathy at RP2D (resolved)
Injection-site reactions in 18% of patients; 21% at RP2D (all events were Gr 1–2)
Skin-related AEs in 45%; 58% at RP2D (majority Gr 1–2)
Nail disordersa in 17% of patients; 21% at RP2D
No Gr 5 AEs across all doses
aIncludes nail disorders, onychomadesis and nail dystrophy. AEs, adverse events, CRS, cytokine release syndrome; DLT; dose-limiting toxicity; Gr, grade; mF/U, median follow-up; NA, not applicable
All Grade Grade ≥3
Cevostamab:
FcRH5xCD3 Bispecific Antibody



• Fc receptor-homolog 5 (FcRH5)
• Expressed on myeloma cells with near 100% prevalence1
• Expression on myeloma and plasma cells > normal B cells1
• Cevostamab
• Humanized IgG based T cell engaging bispecific antibody1
• Targets FcRH5 on myeloma cells and CD3 on T cells1
•
Fab, fragment antibody binding; Ig, immunoglobulin; RRMM, relapse/refractory multiple myeloma 1. Li et al. Cancer Cell 2017;31:383 95; 2. Cohen et al. ASCO 2020
Anti-CD3 Fab region Anti-FcRH5 Fab region T cell Synapse
Activation Apoptosis Myeloma cell
CD3 FcRH5
Ongoing Phase I dose-escalation and expansion trial (NCT03275103) is evaluating the safety and activity of cevostamab monotherapy in patients with RRMM2
Response Rate
• 51/53 pts efficacy evaluable; no response in ≤3.6/10.8mg cohorts
• ORR* in ≥3.6mg/20mg cohorts
• 53% (18/34) in all pts
• 41% (7/17) in penta-drug refractory pts
• 63% (5/8) in pts with prior anti BCMA
• Median time to first response/best response: 29.5 days (range: 21–105)/57.5 days (range: 21–272) • Response irrespective of target expression level in patients assessed to date
• MRD negativity by NGS (<10−5) detected in 6/7 evaluable pts with ≥VGPR
ORR: 53% ≥CR: 18% ≥VGPR: 32% 3.6/20mg 3.6/60mg (n=16)
ORR: 61%
(n=34)
ORR: 44%
Response rate (%) in ≥3.6/20mg cohorts 3.6/90mg 3.6/132mg (n=18)
*best response of PR, VGPR, CR or sCR by IMWG uniform response criteria 2016; BCMA, B cell maturation antigen; MRD, minimal residual disease; NGS, next generation sequencing; ORR, overall response rate; sCR, stringent CR
PR: 21% PR: 25% PR: 17% VGPR: 15% VGPR: 28% CR: 6% CR: 11% sCR: 12% sCR: 19% sCR: 6% 0 20 40 60 80 100 Rate (%) ≥3.6/20mg
N (%)
Hematologic AEs (≥15%)
Adverse Events
All Gr (N=53) All Gr 3−4 (N=53)
Platelet count decreased* 17 (32) 13 (25)
Anemia 15 (28) 10 (19) Neutropenia 9 (17) 8 (15)
Lymphocyte count decreased 8 (15) 8 (15)
Non hematologic AEs (≥15%)
Cytokine release syndrome 40 (76) 1 (2)
Hypomagnesemia 15 (28) 0
Diarrhea 15 (28) 1 (2)
Infusion related reaction 12 (23) 0

Hypokalemia 11 (21) 2 (4)
Hypophosphatemia 10 (19) 5 (9)
Nausea 10 (19) 0
Fatigue 9 (17) 2 (4)
AST increased 8 (15) 1 (2)
• Median follow-up: 8.1 months (range: 0.2–30.4)
• 28 pts with serious AEs
• Treatment-related† events (13 pts) in ≥2 pts were CRS (6 pts)
• 5 pts (9%) with AEs leading to withdrawal
• Treatment related events (2 pts) were pneumonitis (1 pt) and meningitis (1 pt)
• 7 pts (13%) with Gr 5 AE (malignant neoplasm progression, 5 pts; respiratory failure, 2 pts)
• No treatment-related Gr 5 events
• 1 pt (2%) with DLT of Gr 3 pneumonia in the 3.6/90mg cohort; MTD not reached
*platelet count decreased includes the terms thrombocytopenia and platelet count decreased; †AE considered by the investigator to be related to study treatment; AST, aspartate aminotransferase; DLT, dose limiting toxicity; Gr, Grade; MTD, maximum tolerated dose
CAR-T has entered standard of care for multiple myeloma in the

Feb 2022 Cilta-cel (CARVYKTI)
These are the first regulatory approved CAR-Ts that are not targeting CD19.
Presenter: Yi Lin, M.D.Ph.D.
U.S.
House of
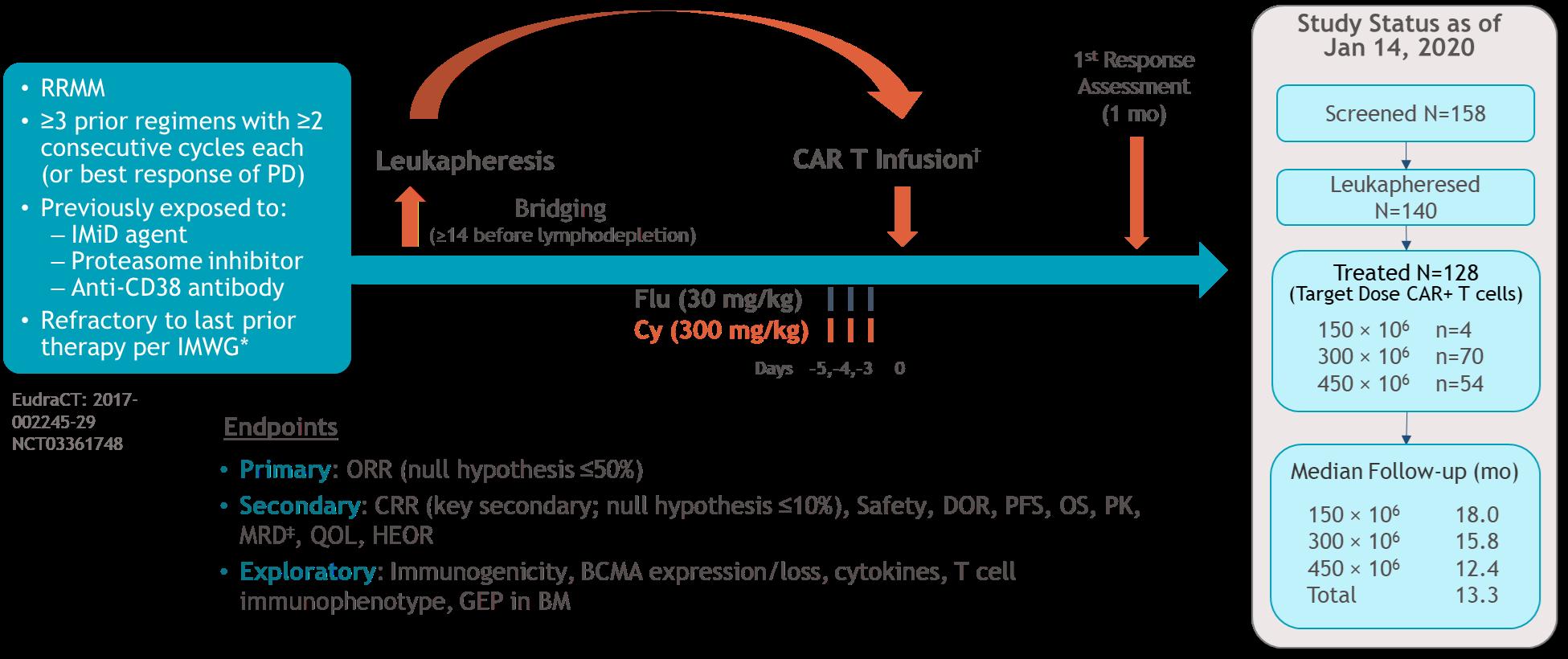
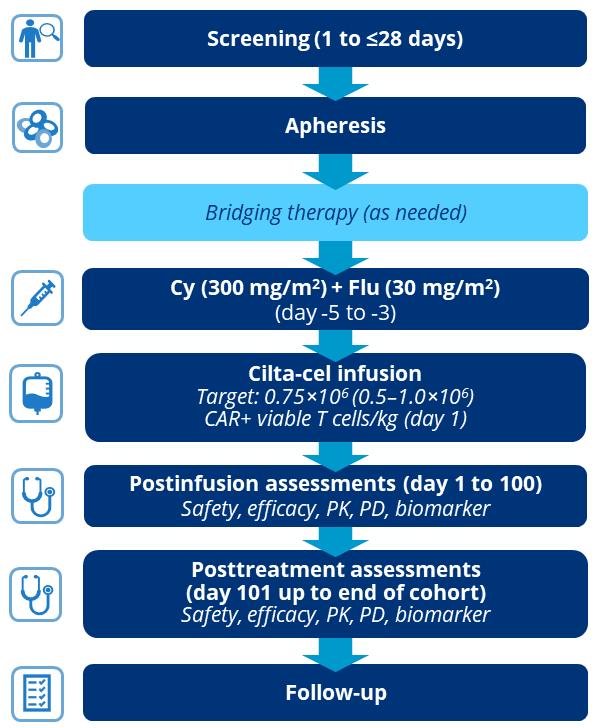
CARTITUDE-1 (phase Ib/II, n-97) JNJ-4528 (Ciltacel) 6 Bi-epitope binding to BCMA 97 92 20.1 (16.5 ICANS) @ 18 mo: 66% prog-free; DOR 21.8 m Google to the Yahoo?
ORR
CARs Trial CAR T product Med prior lines Special sauce
(%) CRS (%) Neurotox (%) Survival data Notes
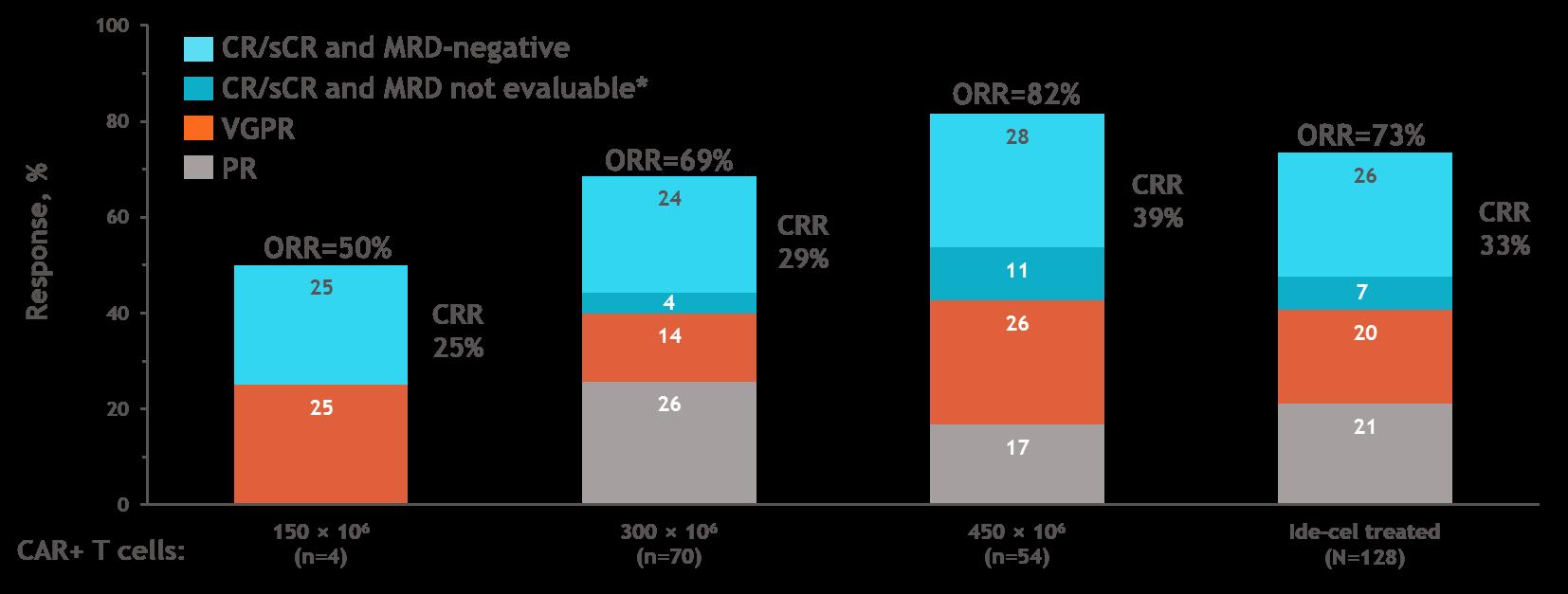
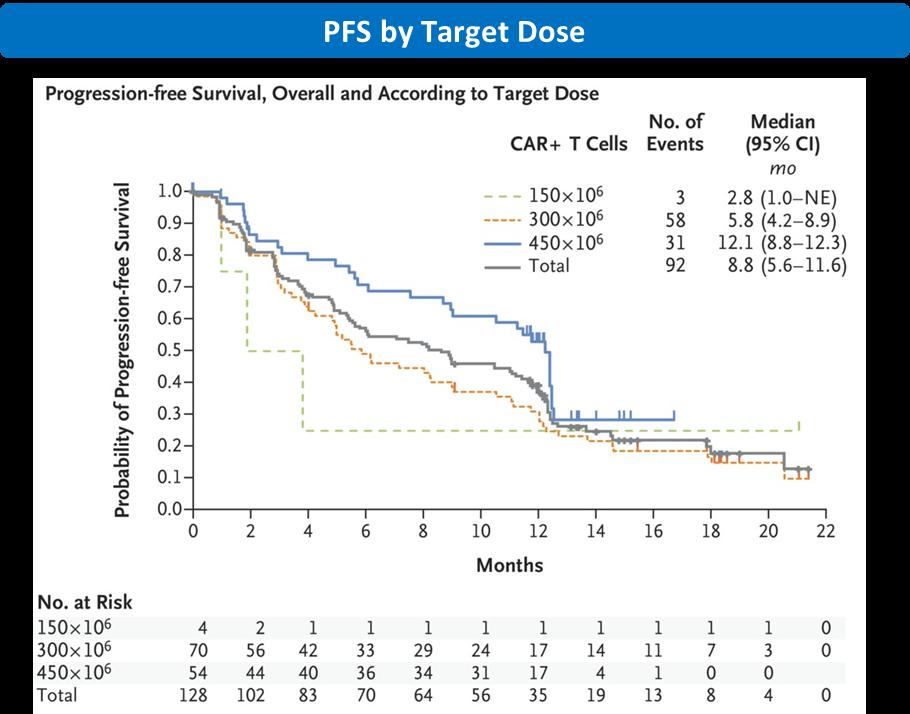
Karmma-1 (phase II, n=128) bb2121 (Ide-cel) 6 73 (82 @450 dose) 84 18 mPFS 8.8mo, 12.1 mo @450 dose OS 24.8 CAR-T Par-T in 2021!
LUMMICAR-2 (phase Ib/II, n=18–20) CT053 5 Fully human 94 (n=18) 77–83 15–17 NA PRIME (phase I/II, n=55) P-BCMA101 8 Piggy-bac system, centyrin technology 67 w/ nanoplasmid (n=6); 44–75 w/OG mfg (n=30) 17 3.8 NA CRB-402 (phase I, n-69) bb21217 6 PI3Ki culture to increase Tscm cells 68 (73 at 450 dose, 84 w/ new mfg) 70 16 mDOR 17 mo (all doses) Memory cell phenotype in DP may correlate w/ response UNIVERSAL (phase I, n=26–31) Allo-715 5 Allo CART 60–67 at 320 dose 45 0 NA Variability in LD, tx within 5 days of enrollment!! No GVH FasT CART GCO12F 5 CD19 BCMA dual CAR T, ON manufact 95 95 0 NA
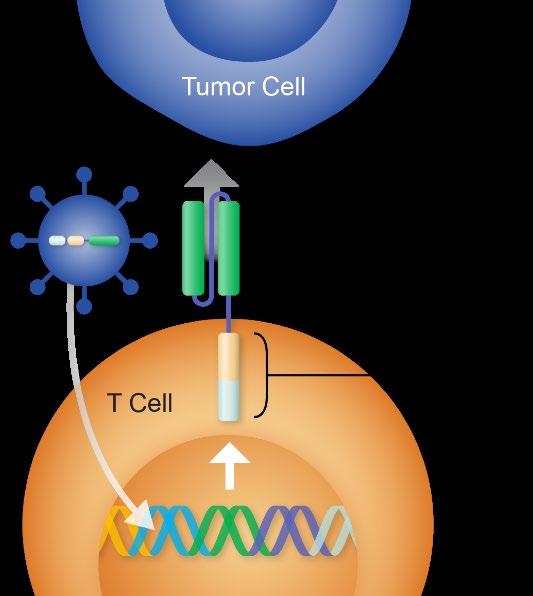






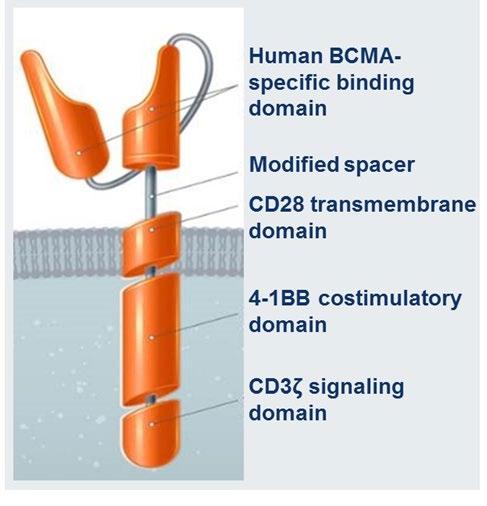
Autologous BCMA CAR-T in Pivotal Trials ide-cel CAR design SP Anti BCMA scFv CD3ζ CD8 4 1BB MND Tumor binding domain Signaling domains Linker Promoter Idecabtagene vicleucel (Ide-cel, bb2121, Abecma) VHH VHH Binding domains CD3ζ 4-1BB Ciltacabtagene autoleucel (Cilta-cel, JNJ-68284528) Orvacabtagene autoleucel (Orva-cel, JCARH125) 1. Lin Y et al ASH 2020. 2. Madduri et al, ASH 2020. 3. Mailankody et al, ASCO 2020. FDA Approved FDA Approved Study Discontinued. Next generation CAR-T in trial.
KarMMa - 1 Registration Study (Ide - cel)
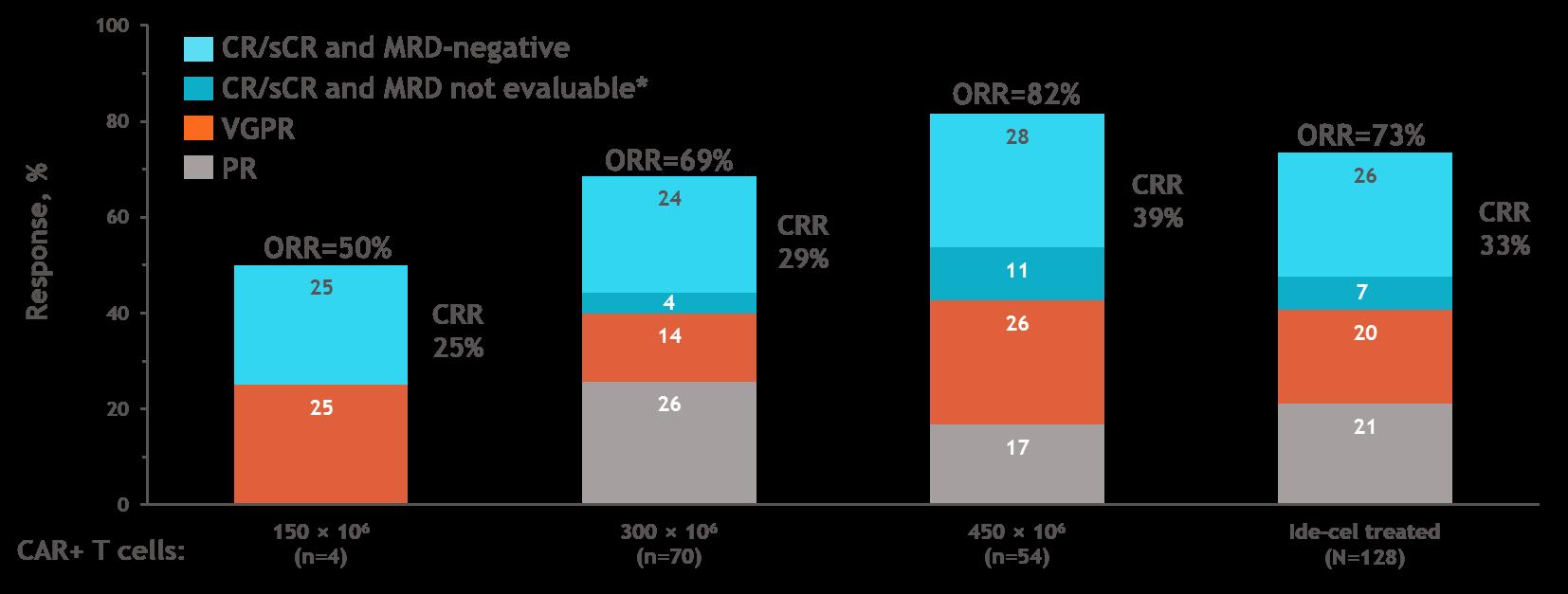
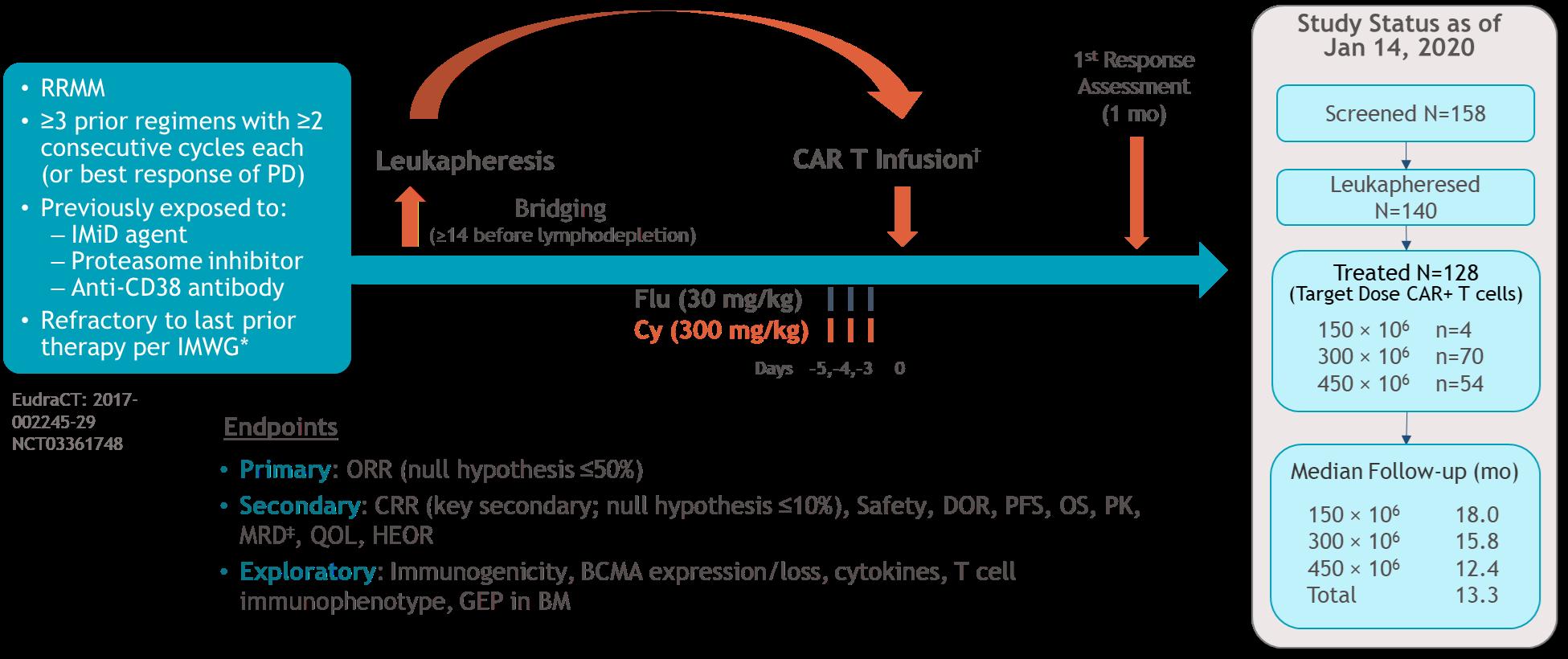
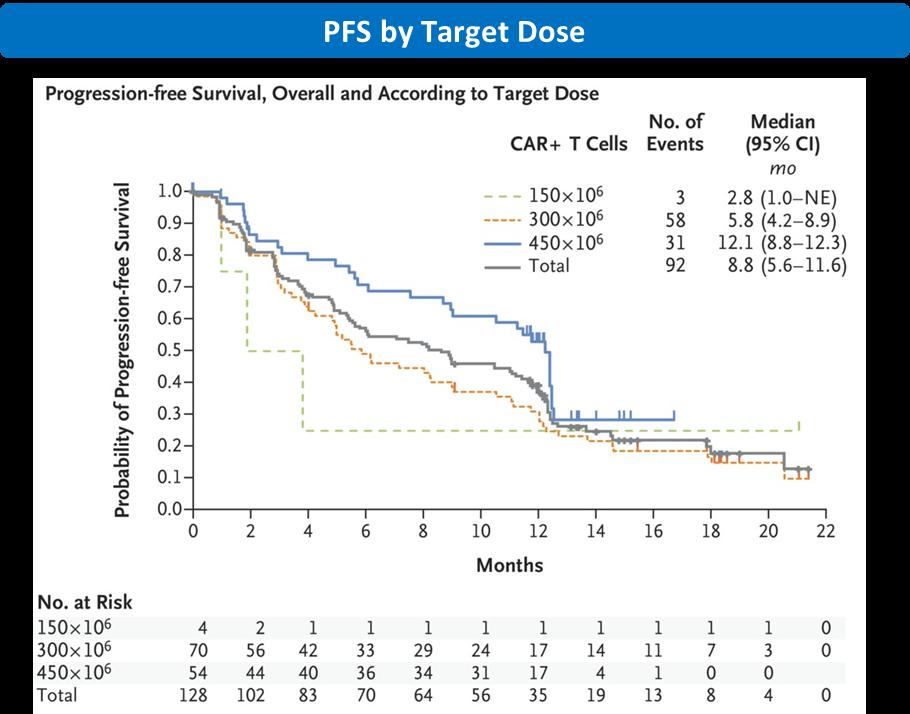
• PFS increased with higher target dose & depth of response
• median PFS was 12 mo at 450 × 106 CAR+ T cells
• median PFS was 20 mo in patients with CR/sCR Munshi NC et al. N Engl J Med 2021;384:705 716. Presenter: Yi Lin, M.D.Ph.D. Regulatory agency approved Dose
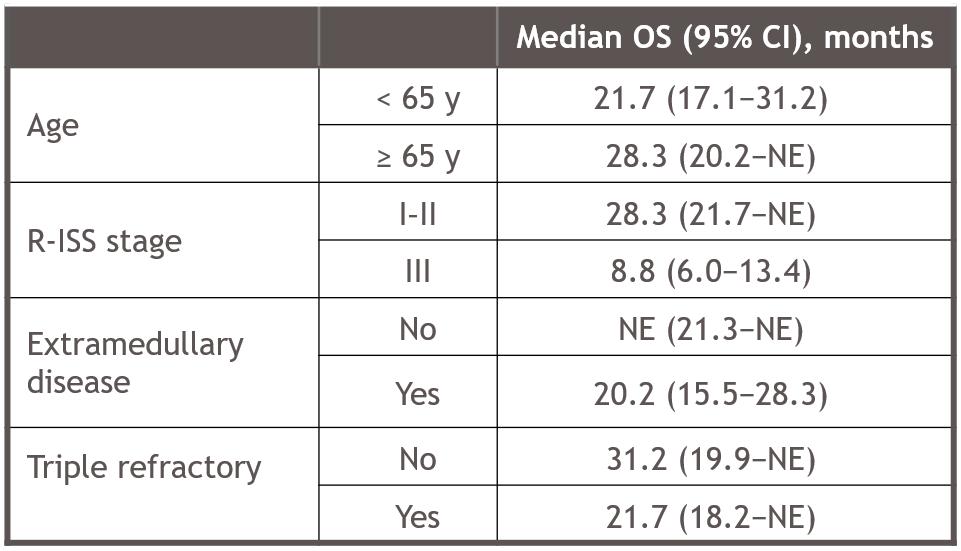
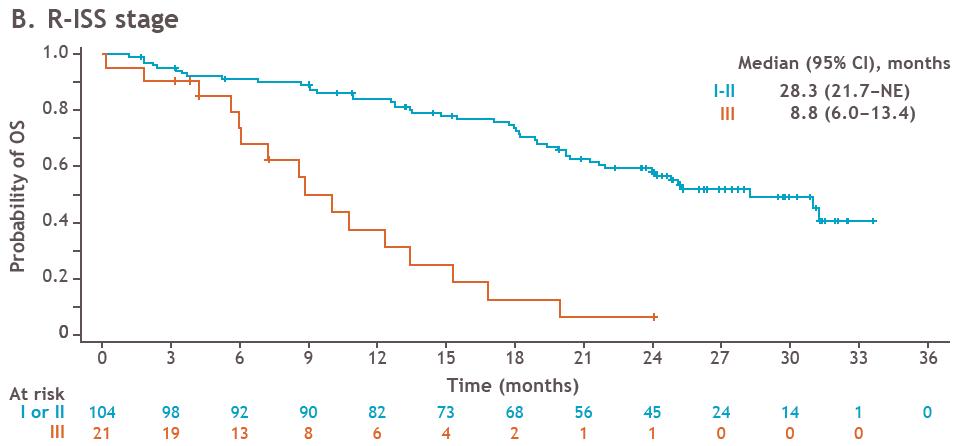
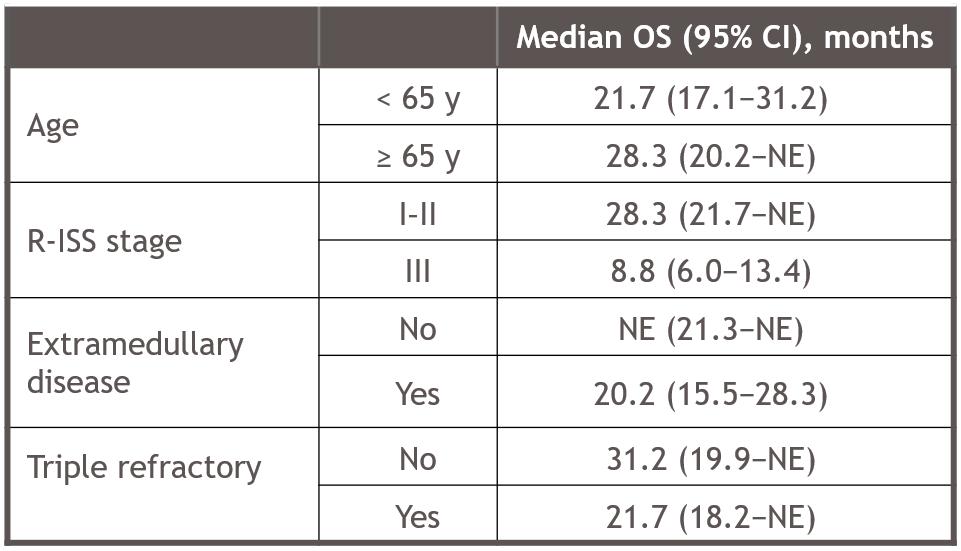
KarMMA-1 Study (Ide-cel) Long Term Follow-up
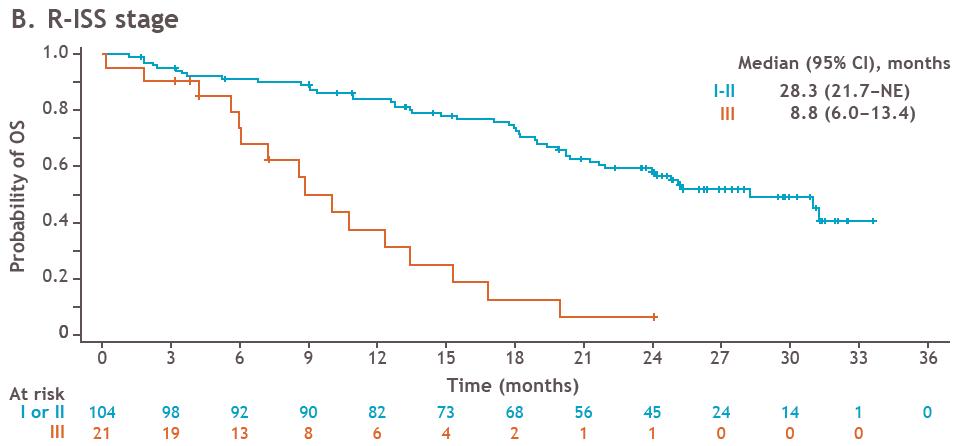
• OS is not decreased for elderly, those with extramedullary or triple refractory disease.
• OS is decreased with patients with R-ISS stage.
OS in high-risk patient subgroups
Anderson L et al. ASCO 2021. Abstr 8016.
CARTITUDE-1 Registration Study (Cilta-cel) 3.1% 12.4% 82.5% 0% 20% 40% 60% 80% 100% Patients, % ORR: 97.9% (95/97) sCR VGPR PR Best response = ≥VGPR: 94.9% Martin T et al. ASH 2021, abstr 549. • Study population • 3 or more prior lines of therapy • Triple class and CD38 mAb exposed • Median 2-YR follow-up
CARTITUDE-1 Registration Study (Cilta-cel)
Progression-Free
Martin T et al. ASH 2021, abstr 549. 80 80 78 73 71 64 61 35 19 4 1 1 2-year PFS: 71.0% (95% CI, 57.6–80.9) Median PFS not reached (95% CI, 25.2–NE) 0 sCR patients All patients sCR patients Patients (%) 100 80 60 40 20 0 0 3 6 9 12 15 18 Months 21 24 27 30 33 36
Survival Patients at risk All patients 97 95 85 77 74 67 63 36 19 4 1 1 0 2-year PFS: 60.5% (95% CI, 48.5–70.4) Median PFS not reached (95% CI, 22.8 months–NE) 100 80 60 40 Patients (%) 20 0 0 3 6 9 12 15 18 Months 21 24 27 30 33 36
Overall Survival Patients at risk All patients 97 96 91 88 85 81 78 46 23 8 2 1 0 2-year OS: 74.0% (95% CI, 61.9–82.7) Median OS not reached (95% CI, 27.2 months–NE)

Cilta-cel CARTITUDE-1 vs LocoMMotion Real World Prospective Study: PFS and OS is better with CAR-T • LocoMMotion (NCT04035226) patients with RRMM, triple class exposed treated with SOC regimens • LocoMMotion patient distribution 91% Europe, 9% US. Mateos M et al. ASH 2021, abstr 550.
BCMA CAR-T Pivotal Trials: Toxicities Ide-Cel – Phase 1 (CRB-401)1 N = 62 Ide-Cel – Phase 2 (KarMMA-1)2 N = 128 Cilta-Cel – Phase 1b/II CARTITUDE-13 N = 97 CRS, Any Gr / ≥ Gr 3 76% / 6.5% 84% / 5% 95% / 5% Onset day median (range) 2 (1 – 19) 1 (1 – 12) 7 (1 – 12) Duration, days median (range) 5 (1 – 32) 5 (1 – 63) 4 (1 – 97) ICANS, Any Gr / ≥ Gr 3 36% / 1.6% 18% / 3% 21% / 10%* Drug use Toci: 29% Steroid: 16% Toci: 52% Steroid: 15% Toci: 69% Steroid: 22% Anakinra: 19% 1. Lin Y et al ASH 2020. 2. Munshi et al ASCO 2020. 3. Madduri D ASH 2020. * Delayed onset movement and neurocognitive symptoms noted in 12.4%, 9.3% Gr3 or higher.
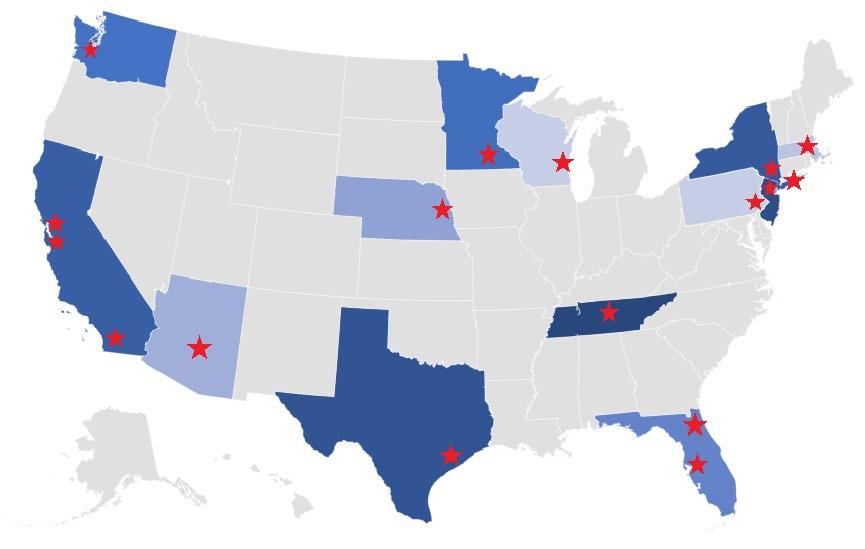
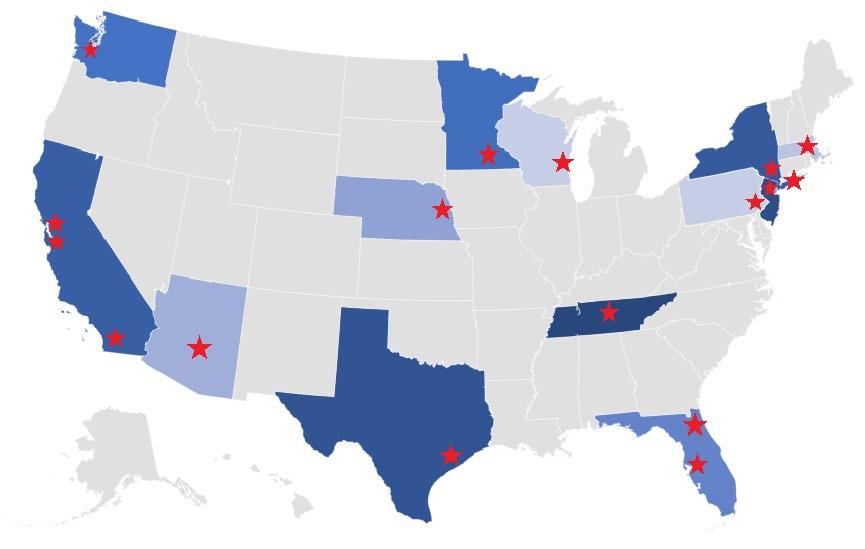
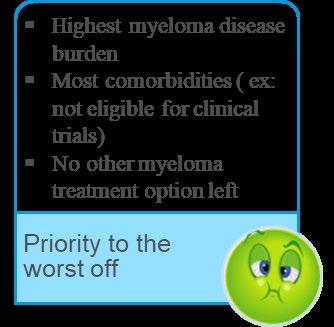
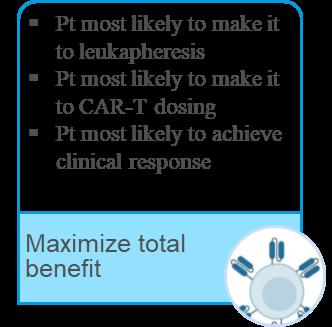
CAR-T access remain an issue Survey of 20 centers. Responses from 17 centers. Median (range) MM CAR-T infusion volume in 2021 10-50 (<5,50-100) Number of FDA approved CAR-T slots given per month 1 (0-4) Patients on wait list (FDA approved CAR-T) 20 (5-100) Duration a patient is on waiting list 6 (2-8) months Outcomes of patients on wait list FDA approved CAR-T CAR-T trial non-CAR-T trial hospice or death 25% (0%-64%) 25% (0-50%) 25% (0-50%) 25% (0%-75%) Kourelis T et al. ASCO 2022.
Challenges with commercial CAR-T slots patient selection

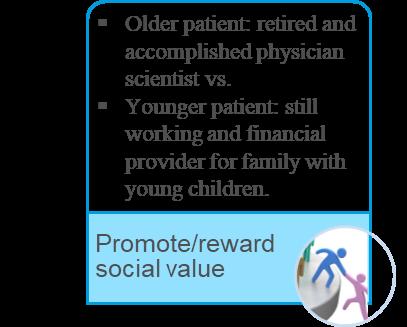
et al. ASCO 2022.
Kourelis
Conclusions
• The therapy of relapsed MM rapidly changing • Bispecifics represent a huge step forward • CART cells are here but challenges remain • INFECTION is an issue (COVID)


90
How to Manage Myeloma Symptoms and Side Effects


Sandra Rome, RN, MN, AOCN, CNS, CEDARS-SINAI

91
LIFE IS A CANVAS, YOU ARE THE ARTIST
 Sandra Rome, RN, MN, AOCN, CNS
Sandra Rome, RN, MN, AOCN, CNS
Cedars-Sinai
Medical Center
Los Angeles, California
Patient Education Slides 2022 November 19, 2022
GALLERY OF GOALS MYELOMA TREATMENT SUPPORTIVE THERAPIES • Rapid and effective disease control • Durable disease control • Minimize side effects • Allow for good quality of life • Improved overall survival • Prevent disease- and treatmentrelated side effects • Optimize symptom management • Allow for good quality of life DISCUSS GOALS AND PRIORITIES WITH YOUR HEALTHCARE TEAM 93
PREPARE FOR VISITS & CONSIDER TELEMEDICINE
Come prepared:
• Bring a list of current medications, prescribed and over the counter
• Write down your questions and concerns. Prioritize them including financial issues

• Have there been any medical or life changes since your last visit?
• Current symptoms - how have they changed (improved, worsened, stable)? Keep a symptom diary. Bring it along
• Communicate effectively: your health care team can’t help if they don’t know
• Know the “next steps”, future appointments, medication changes, refills, etc
Check with your healthcare team –Is telemedicine an option? Similar planning for “in-person” appointment PLUS:

• What is the process and what technology is needed?
• Plan your labs: are they needed in advance? Do you need an order?
• Plan your location: quiet, well-lit location with strong wi-fi is best
• Plan yourself: consider if you may need to show a body part and wear accessible clothing
• Collect recent vital signs (blood pressure, temp, heart rate) self-serve blood pressure cuff is available at many pharmacies and for purchase
IMF Telemedicine Tip Sheet. In development.
(bortezomib)
(carfilzomib)
(ixazomib)
(elotuzumab)
(Isatuximab)
(lenalidomide)
(pomalidomide)
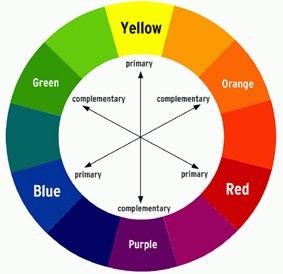
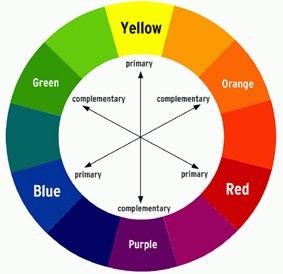
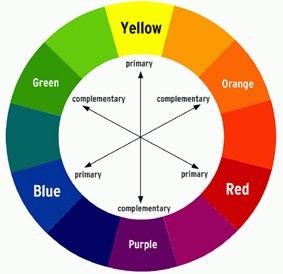
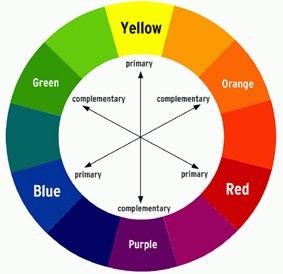
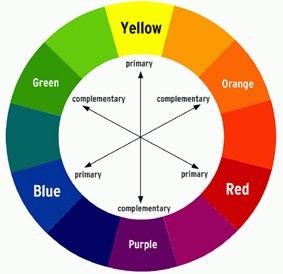
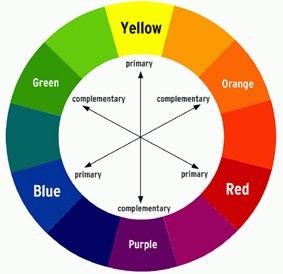
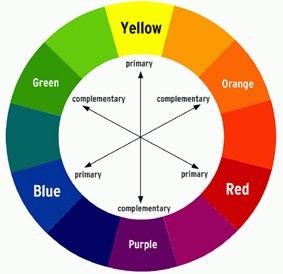
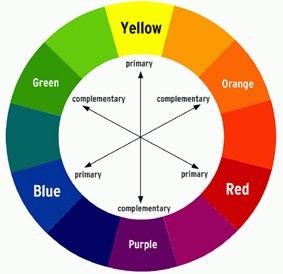
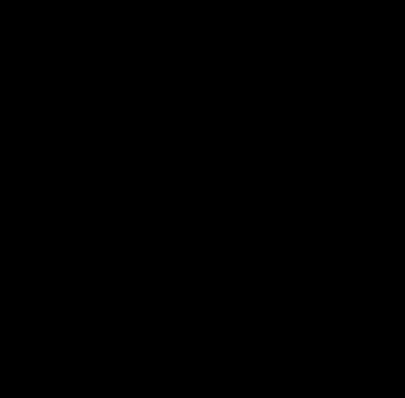
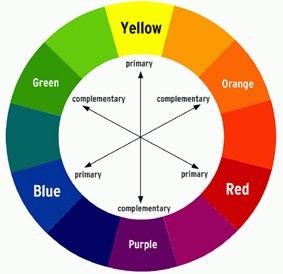
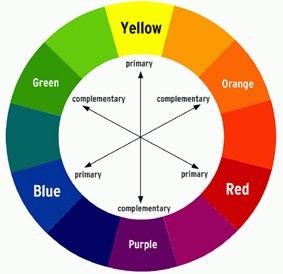
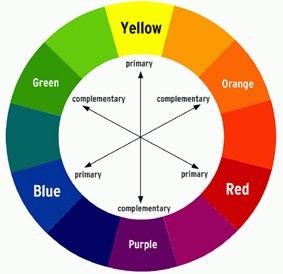
-Mibs -MAbs -Mides Steroids Alkylators ImmunoTherapy Others Cellular Therapies
Velcade® (bortezomib) Darzalex® (daratumumab) Thalomid® (thalidomide) Revlimid® (lenalidomide) Dexamethasone Prednisone Prednisolone SoluMedrol Melphalan Cyclophosphamide Melphalan + ASCT
CelMods •
•
ADCs BSAs Ex: Talquetamab Cevostamab Venclexta®
Neuropathy Carfilzomib: Cardiac Infusion reaction DVT/PE See steroid slide Myelosuppression Infusion reaction Blenrep: Keratopathy Teclistamab: CRS, neurotoxicity Myelosuppression, GI Selinexor: Low sodium Infection risk CAR
and neurotoxicity Frontline Relapse Pending FDA Approval Maintenance COLOR WHEEL OF TREATMENT OPTIONS Noted Side effects 95
Velcade®
Revlimid® (lenalidomide) Kyprolis®
Ninlaro®
Darzalex® (daratumumab) Empliciti®
Sarclissa®
Thalomid® (thalidomide) Revlimid®
Pomalyst®
Dexamethasone Prednisone Prednisolone SoluMedrol Melphalan Cyclophosphamide Bendamustine Pepaxto (melphalan flufenamide) “Melflufen” Blenrep® (Belantamab mafodotin) “Belamaf ” Teclistamab Xpovio® (Selinexor) Doxil (liposomal doxorubicin) Farydak® (panobinostat) Melphalan + ASCT CAR-T: Ide Cel Cilta Cel
Iberdomide
CC 92480
(venetoclax)
T: CRS
SHADES OF “AUTO” STEM CELL TRANSPLANT (ASCT)
Clinical Experience Data from Research Patient Preference
DECISION
Adapted from Philippe Moreau, ASH 2015
• There are no black and white answers to deciding to undergo a transplant
• Undergoing transplant is a commitment for both you and your care partner
• Understanding the process will help bring to focus elements needed to decide if/when to undergo transplant
CARE PARTNER SUPPORT
Care partner support is essential for the entire transplant and CAR T processes
• Sedated procedures; Education sessions
• Assistance with daily activities, managing medications and alerting the medical team of changes
• Continued support and assistance is often needed in the early days after returning home. Less assistance will be needed as time goes on.


Care partner can be one person or a rotation of many people.



SYMPTOMS Physical • Fatigue • Constipation • Pain • Neuropathy • Impaired Physical Functioning • Sexual Dysfunction Psychological • Depression • Anxiety • Sleep Disturbance • Decreased Cognitive Function • Decreased Role & Social Function Financial • Financial burden (80%) • Financial toxicity (43%) A meta-analysis identified the most common patient-reported symptoms and impact on QOL, and were present at all stages of the disease. Symptoms resulted from both myeloma disease and treatment, including transplant, and were in these categories: Ramsenthaler,
98
PATIENT-REPORTED
et al. 2016. https://doi.org/10.1111/ejh.12790.
How You Feel 99 Myeloma cells in excess numbers cause symptoms • Calcium elevation • Renal dysfunction • Anemia • Bone pain • Fatigue • Infection • Other symptoms Treatments for myeloma kill myeloma cells but can cause symptoms – Myelosuppression – Peripheral neuropathy – Diarrhea – Fatigue – Deep vein thrombosis – Infection (eg, shingles) – Other symptoms MYELOMA AND TREATMENTS BOTH CONTRIBUTE TO HOW YOU FEEL
Faiman B, et al. CJON. 2017;21(5)suppl:19 36. Miceli TS, et al. CJON. 2011;15(4)suppl:9 23. Dimopoulous M, et al. Leukemia. 2009;23(9):1545-56.
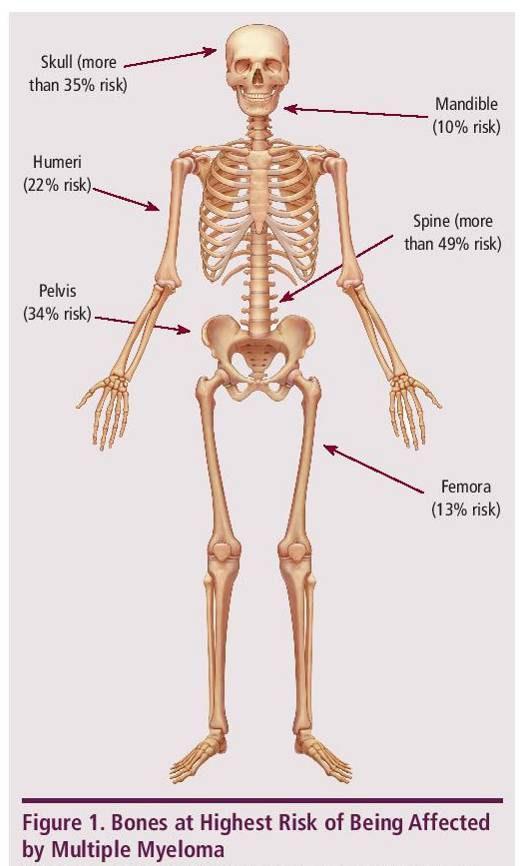
CELLS CAN CAUSE DAMAGE
MYELOMA
TO BONES
► Approximately 85% of myeloma patients develop bone disease ► Protecting bone health – Nutrition – Weight-bearing activity – Medications • Vitamin D • Calcium (if approved by doctor) • Bone strengthening agents: Zometa® (zoledronic acid), Aredia (pamidronate), or Xgeva® (denousamab) ► Report new pain to your health care provider Most myeloma patients will experience bone involvement at some point; it is important to protect your bone health This Photo by Unknown Author is licensed under CC BY SA

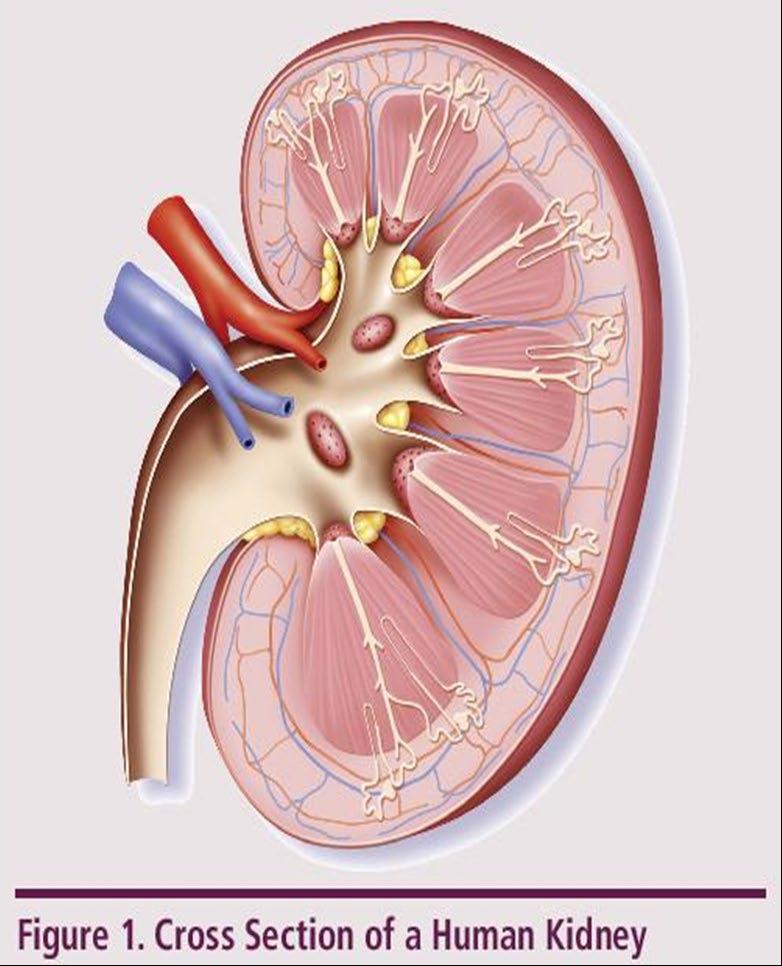
►Risk Factors – Active multiple myeloma (light chains, high calcium) – Other medical issues (ex: Diabetes, dehydration, infection) – Medications (MM treatment, antibiotics, contrast dye) ► Prevention – Drink, Drink, Drink – Avoid certain medications, when possible ► Treatment – Treatment for myeloma – Hydration – Dialysis Brigle K, et al. CJON. 2017;21(5)suppl:60 76. Faiman B, et al. CJON. 2017;21(5)suppl:19 36. Faiman B, et al. CJON. 2011;15suppl:66 76. Water glass: Cleanwateraction.org Many myeloma patients will experience kidney function problems at some point; it is important to protect your kidney function early and over time. 101
UNDERSTANDING CHANGES TO KIDNEY/RENAL FUNCTION

Steroid Side Effects • Consistent schedule (AM vs. PM) • Take with food • Stomach discomfort: Over-the-counter or prescription medications • Medications to prevent shingles, thrush, or other infections THE BRIGHT DARK SIDE
STEROIDS Steroid Synergy Steroids are a backbone and work in combination to enhance myeloma therapy Steroid Side Effects • Increase in blood sugar levels, diabetes • Weight gain, hair thinning/loss, skin rashes • Irritability, mood swings, depression • Muscle weakness, cramping • Blurred vision, cataracts • Difficulty sleeping (insomnia), fatigue • Flushing/sweating • Stomach bloating, hiccups, heartburn, ulcers, or gas • Increased risk of infections, heart disease • Increase in blood pressure, water retention Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME, Abonour R, Siegel DS, Katz M, Greipp PR, Eastern Cooperative Oncology Group (2010) Lenalidomide plus high dose dexamethasone versus lenalidomide plus low dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open label randomised controlled trial. Lancet Oncol 11(1):29 37. King T, Faiman B. Steroid Associated Side Effects: A Symptom Management Update on Multiple Myeloma Treatment
. Clin J Oncol Nurs. 2017 Apr 1;21(2):240 249. doi: 10.1188/17.CJON.240 249. PMID: 28315528. Do not stop or adjust steroid doses without discussing it with your health care provider & 102
Managing
TO

Diarrhea may be caused by medications and supplements • Laxatives, antacids with magnesium • Antibiotics, antidepressants, others • Milk thistle, aloe, cayenne, saw palmetto, ginseng • Sugar substitutes in sugar free gum Avoid caffeinated, carbonated, or heavily sugared beverages Take anti-diarrheal medication • Imodium®, Lomotil ®, or Colestid if recommended • Fiber binding agents – Metamucil®, Citrucel®, Benefiber® • Welchol ® if recommended Smith LC, et al. CJON.2008;12(3)suppl:37 52. Faiman B. CJON. 2016;20(4):E100 E105. Fluid intake can help with both diarrhea and constipation, and good for kidneys. Discuss GI issues with health care providers to identify causes and make adjustments to medications and supplements. Constipation may be caused by • Opioid pain relievers, antidepressants, heart or blood pressure medications, others • Supplements: Calcium, Iron, vitamin D (rarely), vitamin B-12 deficiency Increase fiber • Fruits, vegetables, high fiber whole grain foods • Fiber binding agents – Metamucil®, Citrucel®, Benefiber® Physical GI SYMPTOMS: PREVENTION & MANAGEMENT 103


Peripheral neuropathy: damage to nerves in extremities (hands, feet, or limbs) • Numbness • Tingling • Prickling sensations • Sensitivity to touch • Burning and/or cold sensation • Muscle weakness Prevention / management: • Bortezomib once-weekly or subcutaneous administration • Massage area with cocoa butter regularly • Supplements: • B complex vitamins (B1, B6, B12) • Folic acid, and/or amino acids but do not take on day of Velcade® (bortezomib) infusion • Safe environment: rugs, furnishings, shoes If PN worsens, your HCP may: • Change your treatment • Prescribe oral or topical pain medication • Suggest physical therapy PERIPHERAL NEUROPATHY MANAGEMENT 104 Faiman B, et al. CJON. 2017;21(5)suppl:19 36. Tariman, et al. CJON.2008;12(3)suppl:29 36. Report symptoms of peripheral neuropathy early to your health care provider; nerve damage from PN can be permanent if unaddressed Physical
PAIN PREVENTION AND MANAGEMENT
Pain can significantly compromise quality of life Sources of pain include bone disease, neuropathy and medical procedures
Management

Physical
• Prevent pain when possible • Bone strengtheners to decrease fracture risk; anti viral to prevent shingles; sedation before procedures
• Interventions depends on source of pain
• Monitor serum calcium levels • Imaging may be needed depending on type and location of pain (eg, MRI, PET-CT)
• May include medications (eg bone modifying agents), activity, surgical intervention, radiation therapy, etc • Complementary therapies (Mind-body, medication, yoga, supplements, acupuncture, etc)
Faiman B, et al. CJON. 2017;21(5)suppl:19 36.
105
Tell your health care provider about any new bone pain or chronic pain that is not adequately controlled
FATIGUE, ANXIETY & DEPRESSION
All can affect quality of life and relationships
Psychological
• Fatigue is the most common reported symptom (98.8%)
Sources include anemia, pain, reduced activity, insomnia, treatment toxicity, bone marrow suppression


• Anxiety reported in >35%
• Depression nearly 25% Financial concerns, disease progression, end-of-life, and change in social and sexual function were highlighted sources
Often, people do not share these symptoms with their provider. Talk to your provider about symptoms that are not well controlled or thoughts of self harm. Help is available.
Ramsenthaler, et al. 2016. https://doi.org/10.1111/ejh.12790. Catamero D et al. CJON. 2017; 21(5)suppl:7 18.
Physical
106



IMPORTANT WAYS TO SLOW THE SPREAD OF COVID-19 • Get a COVID-19 vaccine (and booster) as soon as you can • Wear a mask (N95 is most protective) that covers your nose and mouth • Stay 6 feet apart from others who don’t live with you • Avoid crowds and poorly ventilated indoor spaces • Test to prevent spread to others • Wash your hands often with soap and water. Use hand sanitizer if soap and water aren’t available CDC = Centers for Disease Control; FDA = Food and Drug Administration. CDC website. Understanding Variants. Accessed January 30, 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/understanding-variants.html

Manage stress • Rest, relaxation, sleep hygiene • Mental health / social engagement • Complementary therapy Maintain a healthy weight • Nutrition • Activity / exercise Preventative health care • Health screenings, vaccinations • Prevent falls, injury, infection • Stop smoking • Dental care Maintain renal health • Myeloma management • Hydration • Avoid renally-toxic medications – Dose adjust to renal function • Diabetes management Protect your bones • Nutrition, Calcium + D supplement • Weight-bearing activity / walking • Bone strengthening agents
36. Dimopoulous M, et al. Leukemia.
56.
Faiman
“An ounce of prevention is worth a pound of cure.” Benjamin Franklin 108 HEALTHFUL LIVING STRATEGIES: PREVENTION
Faiman B, et al. CJON. 2017;21(5)suppl:19
2009;23(9):1545
Brigle K, et al. CJON. 2017;21(5)suppl:60-76.
B, et al. CJON. 2017;21(5)suppl:19-36. Faiman B, et al. CJON. 2011;15suppl:66-76. Miceli TS, et al. CJON. 2011;15(4)suppl:9-23.










KNOWLEDGE IS POWER USE REPUTABLE SOURCES Download or order at myeloma.org Website: http://myeloma.org IMF InfoLine 1 800-452-CURE 9am to 4pm PST eNewsletter: Myeloma Minute IMF TV Teleconferences 109
YOU ARE NOT ALONE

Regional Community Workshop

November
Thank you for joining us today for the IMF
19, 2022
Thank you to our sponsors!








112
We want to hear from you!

Feedback Survey
At the close of the meeting a feedback survey will pop up.
This will also be emailed to you shortly after the workshop.
Please take a moment to complete this survey.
Workshop Video Replay & Slides
As follow up to today's workshop, we will have the speaker slides and a video replay available. These will be provided to you shortly after the workshop concludes.







Website: http://myeloma.org eNewsletter: Myeloma Minute IMF Webinars Videos Download or order at myeloma.org








































































 R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012
R Vij et al. Br J Haem, June 2012. ; MOREAU et al. BLOOD, AUG VOL 120(5 ); 2012

























































































 Amrita Krishnan, MD FACP Director of Judy and Bernard Briskin Center for Myeloma City of Hope Cancer Center Executive Medical Director of Hematology & HCT- City of Hope Orange County
Amrita Krishnan, MD FACP Director of Judy and Bernard Briskin Center for Myeloma City of Hope Cancer Center Executive Medical Director of Hematology & HCT- City of Hope Orange County




























 Sandra Rome, RN, MN, AOCN, CNS
Sandra Rome, RN, MN, AOCN, CNS