3 minute read
Government failed to plan for Covid impact
The government failed to plan for the economic shock which hit the care home sector due to the Covid-19 pandemic, a major report has found
The ‘Bailed out and burned out?’ report analyses the financial impacts of the pandemic on UK care homes for older people and their staff. The report is the result of a collaboration between Warwick Business School, University College London and think tank Centre for Health and the Public Interest, and was funded by the Economic and Social Research Council,
The study finds that although 60% of care homes for older people were at risk of insolvency in the event of a mild economic shock, the government had failed to make any contingency plans for the pandemic that hit the sector in March 2020.
Around £2.1 billion in financial support was provided by government to care homes as part of the pandemic response.
Care homes, meanwhile, suffered an 8% reduction in occupancy during the first year of the pandemic.
“Four-fifths (80%) of staff worked more hours during the pandemic than previously. And more than two in five (42%) care workers reported financial problems related to working in care homes during the pandemic.”
Report Recommendations
• Improved contingency planning for the financial effect of future pandemics and their consequences for staffing, including creating a standby emergency social care workforce
• Sustained government support for care homes coping with the lasting effect of pandemics
• Public funding for care, including emergency support during pandemics, should take account of evidence showing varying outcomes by ownership type and should seek to promote forms of provision that offer both good care and good jobs
• Government and employers should improve pay and conditions for care staff in general and especially during pandemics (including recognition payments, enhanced sick pay and overtime rates)
• Government should work with employers to promote a better understanding of how care staff experience their working lives, for example through an annual national workforce survey, and to ensure adequate personal, professional and clinical support is accessible to social care staff, particularly during a pandemic.
Four-fifths (80%) of staff worked more hours during the pandemic than previously. And more than two in five (42%) care workers reported financial problems related to working in care homes during the pandemic.
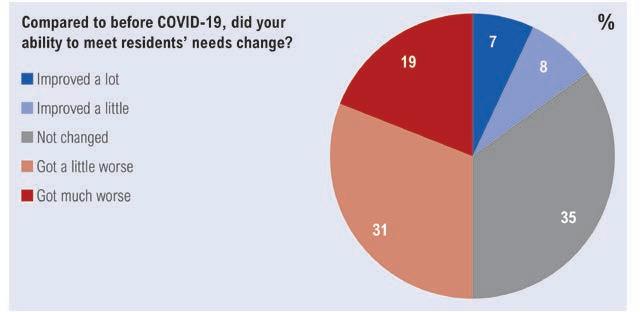
Half of care workers said their ability to meet residents’ needs worsened during the pandemic.
Staff vacancy rates almost doubled in percentage terms between April 2021 and January 2022 rising from 6% to 11%.
The report found the financial effect on staff varied by ownership type and size. Compared to not-for-profit homes, staff in homes owned by for-profit companies were more dissatisfied with their sick pay and reported higher increases in their hours and amount of work. Staff in not-for-profit care homes were also more satisfied with support from their manager than those in care homes owned by for-profit companies. Homes that were part of bigger chains fared worse in staff satisfaction with workloads, pay (including sick pay), ability to offer good care, and support from their managers and organisations cited as concerns.
Dividends from 122 out of the 460 companies assessed rose by 11% or £11.7 million on the previous year to £120 million. Insurance costs were predicted to rise by 300% as a result of the pandemic.
Marianna Fotaki, professor of business ethics at Warwick Business School and co-author of the study, said: “The decision by government to end financial support for care home companies after the peak of the pandemic had passed, even though the financial impact of the pandemic was clearly not over, has likely contributed to the current financial and operational difficulties experienced by the sector. A pandemic does not end when government says that it does.”
Professor Martin Green, chief executive of Care England, said: “This report graphically illustrates the impact that Covid has had on both staff and the sustainability of care services. What comes across is that the government's approach is very piecemeal, and whilst helpful at some points, it does not give us what we need, which is a long-term vision for social care, underpinned by the funding to make organisations sustainable, and to significantly invest in the pay, conditions and training of staff.”
Mike Padgham, chair of the Independent Care Group, said: “Whilst we got some help during the worst of Covid-19, that stopped far too quickly. Since then, the extra costs associated with the pandemic, combined with huge increases in energy and utility costs and the ongoing staffing challenges, have all pushed the sector deeper into the abyss.”
Nadra Ahmed, executive chairman of the National Care Association and chair of the Care Provider Alliance, commented: “Nothing in this report will come as a major surprise to social care providers and their dedicated workforce. Much of the monies announced did not reach the front line, although what did made a huge difference to providers enabling them to support those in their services and their workforce.
“The findings are clear that there was no plan for social care and the limited time grants did not all reach the front line. Our workforce was tireless throughout the pandemic delivering services. There was no funding available to recognise their dedication in England, whilst the other devolved nations made at least one payment to mark their contribution.
“The government’s announcement of ‘business as usual’ made little difference to the operational stance for providers, as Covid restrictions remained in place for care homes. There was no additional funding to support our workforce for time off if they contracted Covid. Precedents were set up but not sustainable for an already underfunded and fragile sector with additional pressures post Covid.”









