
6 minute read
Governor Reynolds' COVID-19 Vaccine
Forums that bring together likeminded practitioners, who may even be competitors, to create a sharing of ideas for the good of patients.
I recently spoke with one of the Flip the Pharmacy coaches: “Flip the Pharmacy focuses on promoting medication synchronization and utilizing an appointment-based model to manage pharmacy workflow and give the pharmacist time to focus on their patient's overall healthcare picture...there is a focus on developing advanced roles for non-pharmacist staff and improving bidirectional communication with prescribers.”
Embrace the change but keep in mind, there can be a very fine line between Progress and Progression! Make sure the changes you embrace are truly progress not just a progression of useless data collection that is not utilized, drop down boxes that are stale and create robotic, unhelpful documentation, safety checks that end up creating unsafe workflows, etc.
So many times over my career as a pharmacist, a supervisor, a clinical coordinator, a director, a transitional care coordinator, I have told co-workers, staff, and patients: “Change is good, Change is our friend – keep telling yourself that and embrace it!” ■
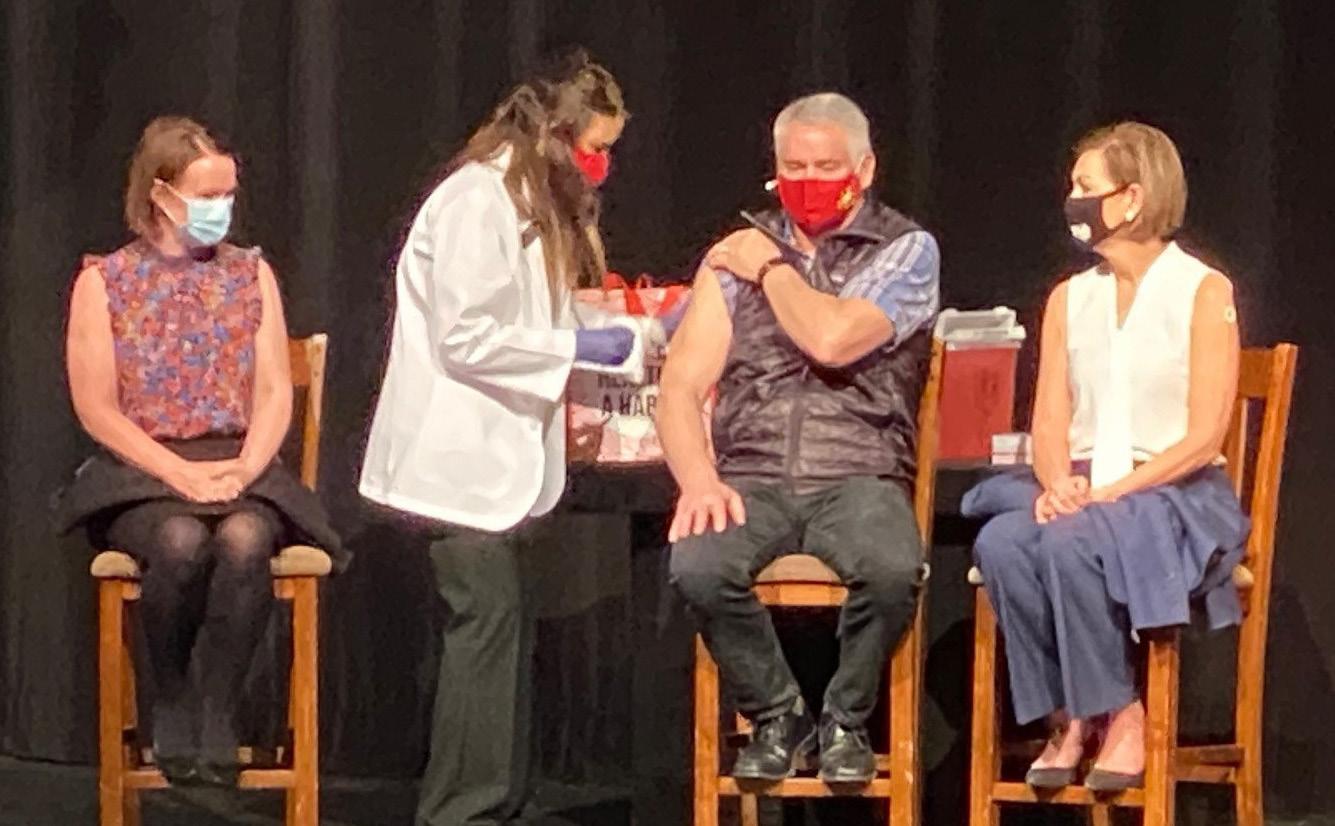
Pictured left to right: Iowa DHS Director Kelly Garcia, Jane Allen, Kevin Reynolds, Governor Kim Reynolds
IPA MEMBER ADMINISTERS COVID-19 VACCINE TO GOVERNOR REYNOLDS
On Wednesday, March 3, Governor Kim Reynolds and Iowa Department of Human Services (DHS) Director Kelly Garcia received the Johnson & Johnson (Janssen) COVID-19 vaccine during a weekly press conference.
“Is she done? Wow, OK,” said Governor Reynolds after receiving her vaccine. The pharmacist who administered the quick and painless shot was IPA member Jane Allen of Ankeny.
Jane Allen, PharmD, MBA, is an active member of the Iowa Pharmacy Association and a pharmacist at Hy-Vee. When asked about the opportunity, Jane stated, “It was an honor for me and a great moment for Hy-Vee.”
IPA is proud of the massive efforts made by pharmacists, student pharmacists, and pharmacy technicians to vaccinate patients across the state of Iowa, whether hosting large vaccine clinics, scheduling daily appointments, or standing-by ready for the opportunity. The association continues to advocate on behalf of our members with the overarching goal of collaborating with the entire public health team to vaccinate as many Iowans as safely and efficiently as possible.
IPA has been sharing the great coverage our members have received by media outlets throughout the pandemic. Watch for these continued posts on our social media with the hashtag #MembersInTheMedia.
Additional photos of the press conference are available on the Des Moines Register website.
The Supreme Court of the United States on Dec. 10, 2020 issued a unanimous decision in Rutledge v. PCMA, No. 18-540, holding that a federal law, the Employee Retirement Income Security Act of 1974 (ERISA), does not prevent states from enacting laws regulating the abusive payment practices of pharmacy benefit managers, the controversial middlemen that manage prescription drug benefits for health insurers, Medicare Part D drug plans, and large employers.
The 8-0 decision (Justice Barrett did not participate) is a resounding victory for patients and community pharmacies, which have been fighting for years to regulate PBMs. The Pharmaceutical Care Management Association, the lobbying arm of the PBM industry, had argued that ERISA preempts Act 900, an Arkansas law that includes rate regulation and enforcement provisions to ensure that PBMs compensate pharmacists fairly for the medications they dispense to patients.
In her opinion for the Court, Justice Sotomayor explained that nothing in ERISA prevents states from enacting laws that regulate the rates that PBMs pay pharmacies: “Act 900 is merely a form of cost regulation. It requires PBMs to reimburse pharmacies for prescription drugs at a rate equal to or higher than the pharmacy’s acquisition cost. PBMs may well pass those increased costs on to plans . . . . But ‘cost uniformity was almost certainly not an object of [ERISA] pre-emption.’” Op. at 6.
The Court also rejected PCMA’s arguments that Act 900’s enforcement mechanisms were impermissible because they affect how PBMs administer benefits on behalf of ERISA plans. As Justice Sotomayor explained, Act 900’s enforcement mechanisms “do not require [ERISA] plan administrators to structure their benefit plans in any particular manner, nor do they lead to anything more than potential operational inefficiencies” for PBMs. Op. at 7-8. Moreover, if Arkansas’s enforcement mechanisms were deemed preempted, the state would have no way to ensure “compliance with Act 900’s cost regulation.” Op. at 8 n.3.
The Supreme Court’s decision is the culmination of a years-long effort led by the Arkansas Pharmacists Association and the National Community Pharmacists Association to hold PBMs accountable for their abusive practices, which have needlessly restricted patient access to life-saving medications and added billions of dollars annually in unnecessary costs that are ultimately borne by hard-working Americans.
APA helped secure passage of the Arkansas law that the Supreme Court reviewed, and APA and NCPA provided support to the state throughout the litigation — at the trial court, the intermediate appellate court, and then the Supreme Court. APA and NCPA also filed an amici curiae (“friends of the Court”) brief — along with the American Pharmacists Association, the National Alliance of State Pharmacy Associations, and all state pharmacist associations — educating the Court on abusive PBM practices. APA and NCPA were joined by a diverse coalition of other amici curiae filing their own briefs defending Arkansas’s law, including the United States government, forty-five other states, the American Medical Association, and the AARP.
For all these reasons, it is no surprise that nearly every state — red and blue — has enacted laws regulating PBMs. It is also why the federal government and nearly every state — from Texas to California — argued in defense of Arkansas’ law in the Supreme Court.
PBMs are middlemen who have secretly put their own interests and record-breaking profits above the patients and plans that they are supposed to serve. The Supreme Court just cleared the way for state laws like Arkansas to police PBMs’ abusive behavior and protect patient access to affordable medications. This is a historic victory for pharmacists and their patients.
You Need a CQI Program
Mistakes happen. Risky processes become normalized and your operations can shift slightly with staffing changes, new products, and new procedures.
The APMS Patient Safety Organization (PSO) provides Pharmacy Quality Commitment+ (PQC+) Compounding, a confidential, highly secure, continuous quality improvement program. Track and analyze how, when, and where the risk in your workflow occurs so you can reduce Rx corrections and operational costs.
Our program includes:
1 Pharmacy Quality Commitment+

A web-based reporting portal to collect patient safety events Tools to chart, graph, and analyze data Expert advice, tips, and safe practices Resources to help you meet accreditation and quality improvement requirements Support to build a just culture of safety QA Continuing Education and training opportunities
2 APMS PSO Services
Patient Safety Organizations (PSOs) provide a safe space for members to conduct patient safety work. When you partner with our PSO for your Quality Improvement activities, the collection of quality assurance data and patient safety work is in Customer Service a protected environment. We are passionate about medication safety in community pharmacy and are here to walk you through the entire process. Our customer service team has years of experience in pharmacy and is excited to help.
Let' s chat! (866)365-7472 info@medicationsafety.org







