

Sign-in Management




FINALLY, ONE SIMPLE SYSTEM DESIGNED FOR AGED CARE

STAFF
VISITORS
RESIDENTS
CONTRACTORS
Integrate LoopSafe with your existing systems to deliver a fast, efficient and safer sign-in process for everyone coming on site.


LoopSafe creates one seamless flow of information with:



















roster and payroll
access control

resident management
visitor management
contractor management
The automated syncing across all systems gives real-time, validated data and removes the risk and cost of manual entry.























< Click to learn more >
03 9381 7897 www.loopsafe.net







































Welcome
Welcome to 2023’s first edition of Aged Care Australia, the digital resource guide that provides up-to-date industry reports of importance to the aged care and aged services sectors.
Leading industry advocates supporting the Royal Commission into Aged Care Quality and Safety recommendations continue to urge legislation reforms to ensure the Government responds to the needs of older Australians.
Organisations and individualise have provided feedback to the Senate Standing Committee on Community Affairs on the Aged Care Amendment (Implementing Care Reform) Bill 2022 [Provisions].
In welcoming the Bill as “good start” to achieving its purpose, the Australian Physiotherapy Association (APA) finds the measures do not provide certainty about ongoing access to allied health care, nor does it recognise the importance of ongoing multidisciplinary care planning and team-based quality healthcare.
The Royal Commission into Aged Care Quality and Safety identified allied health, such as physiotherapy, critical to maintaining and improving mobility and independence of older people as the allied health section in this issue of Aged Care Australia demonstrates.
In this issue of Aged Care Australia, you will also find relevant and valuable content on issues that are not only from the vanguard of aged care services in Australia, comprising reports from leading aged care associations on many issues information about products and services essential to the decision makers responsible for the financial management of aged care facilities and hospitals.
Across the new digital platform, Aged Care Australia reaches nursing homes, retirement villages, hospitals and relevant industry bodies across Australia with unlimited audience across digital and social media platforms.
We hope you enjoy this issue of Aged Care Australia and wish to extend our appreciation to all our supporters, particularly the valued contributions from aged care sector associations and organisations.
As we progress through 2023, we wish you a productive and rewarding year ahead.
ARK MediaPublisher
Managing Editor: Sue Guilfoyle
National Sales Manager: Renwick Horder
Advertising Sales: Daemen Bray, Deborah Holliday, Dennis Andrews, Merran Fox, Olivia Thomas, Paul Baird
Advertising Production: Rohit Panjwani
Design Team: Andrew Crabb, Dujon Kie, Lucas Palma @agedcareau























Are you giving your clients a voice?
Margaret Crothers has been advocating for older people for more than 15 years.
The advice she has for providers who want to improve their delivery of high quality, personcentre aged care is refreshingly simple.

“Older people want to be heard,” she says. “They want someone to listen to them and to respond to their concerns.

“Basically, people come to advocacy services when that’s not happening.”
The relationship between advocates and service providers has traditionally been seen as adversarial, but Ms Crothers, advocacy and regional services manager for Senior Rights Service, NSW, believes the two jobs are actually interdependent.
“By working as a team, advocates and service providers can resolve issues before they become complaints,” she says.
“As an advocate that’s the outcome we are looking for. And I’m sure service providers are on exactly the same page.
“Neither of us want to be dealing with issues; we want to be dealing with happy, contented people.”
Utilising the advocates’ and aged care workers’ complementary skillsets makes good business sense.
It also enables service providers to meet their legal responsibilities, under the Charter of Aged Care Rights, including the right of older people:
• to safe and high-quality services
• to be treated with dignity and respect
• to be informed about their care and services in a way they understand
• to have control over, and make choices about, their care and personal and social life
• to be listened to and understood.
And under the Aged Care Quality Standards, including:
• consumer dignity and choice
• ongoing assessment and planning
• personal and clinical care
• services and supports.
As OPAN National Older Persons Reference Group member Val Fell puts it, “It’s an older persons’ human right to ask questions, to be involved in their own well-being.”
Advocates are independent of both government and aged care services. They offer information and support to the older person to ensure their voice is heard.
“Advocates help older people understand the guidelines, what they are entitled to,” Ms Crothers says.
“We give them the power – and sometimes the words – to talk to their aged care provider.”

OPAN’s member organisations delivered more than 27,000 cases of information and advocacy support in 2021–22 – a 17 per cent increase on the previous year.
Issues around Home Care Packages accounted for 49 per cent of those cases; residential care made up 39 per cent of the overall tally.
“Quality of home care and residential care, fees and charges, communication … the issues don’t change from year to year,” Ms Crothers says.
“What makes the difference is how well we listen.”
Older people can be reluctant to speak up for a variety of reasons: some are concerned about reprisals, some don’t want to be seen as troublemakers, some are simply unaware of the alternative options available to them.
“As advocates, it’s our job is to encourage people to raise issues, to make them feel like they are being listened to and that there will be an outcome,” Ms Crothers says.

“That they are not just talking to a brick wall.”
Aged care staff, who are often the first to identify an issue, can play a key role in the provision of information and support.
“They can refer a person to us, or they can be the advocate themselves,” Ms Crothers says.
As well as individual advocacy support for older people, OPAN member organisations offer free, face-to-face information and education sessions – in the community and in residential aged care – for older people, their families and representatives.
This enables advocates to speak to older people receiving aged care services about their rights.
It also allows the local advocate to become a familiar face and to establish a trusted relationship with those clients.
“The three most important things we can do together,” Ms Crothers says, “is listen, understand, and then help.”
Case study
The manager of a residential aged care home called OPAN of which Senior Rights Service is a member, because she could see one of her clients was unhappy.
An advocate organised for a translator to visit Maria*, who was from a culturally and linguistically diverse background, so that she could express her wishes in her own language. Maria said she had no issue with the service she was being offered – she simply didn’t want to live in residential care.
With the support of the manager, the advocate was able to organise in-home care for Maria, which enabled her to live with her daughter.
*Names have been changed to protect the person’s identity.
Case study
Jack*, an aged care resident, was suffering regular bouts of gastroenteritis. His favourite meal was barbecue chicken, which he bought from a nearby shop.
One of Jack’s support workers noticed he was storing the chicken on the bench in his room and eating it slowly over the course of the week. After clearing it with her manager, she said to Jack: “How about we sit down and have a meal at the barbecue chook shop together. And you bring back maybe one serve?
“That way you can have a walk and eat your chicken without getting sick.”
Jack told the provider he would be equally satisfied with the new arrangement.
*Names have been changed to protect the person’s identity.
The Older Persons Advocacy Network (OPAN) offers education and information sessions for older people, their friends, family and representatives.
These free education sessions can be tailored to a specific audience and can be delivered online or face-to face by a member of our national advocacy team.
More information here: [https://opan.org.au/education/ education-for-community/]
OPAN’s free Talk To Us First, Aged Care Advocacy online training supports the professional development of nurses, aged care workers and volunteers and carers.
This training will help you to understand:
• the benefits of aged care advocacy by showing examples of advocacy at work
• the rights of older people and their representatives
• how the Older Persons Advocacy Network (OPAN) can help you to better support older people.
More information here [https://opan.org.au/ education/education-for-professionals]
Being #ReadyToListen
Strategies to prevent sexual assault and better support victim/survivors and sexual rights and responsibilities for people living in aged care

The #ReadyToListen project is the first of its kind in Australia. With an estimated 50 sexual assaults taking place in residential aged care in Australia every week, it aims to build the skills and capacity of service providers to better respond to – and prevent – sexual assault in residential aged care.
Being #ReadyToListen is about understanding the risk of sexual assault, knowing the indicators, believing those who disclose, acknowledging impacts, providing support and taking proactive steps to protect residents. It’s also about recognising and respecting the sexual rights of older people.
We know that service providers are finding themselves facing complex situations in this area, and recognise that there hasn’t previously been information, education or resources available to help guide policy and practice.
#ReadyToListen aims to change that and empower service providers. It’s about facilitating leadership and putting systems and processes in place, so staff know what to do.
At the heart of the #ReadyToListen project is a MAP (myths, facts and practical strategies) and the Charter of Sexual Rights and Responsibilities in Residential Aged Care.
The MAP outlines 10 ways in which service providers can improve their responses to – and prevent – sexual assault.
1. Understanding sexual assault definitions and prevalence
2. Promoting sexual rights
3. Assessing the indicators of sexual assault
4. Identifying the impacts of sexual assault
5. Complying with reporting requirements
6. Providing immediate safety and support
7. Practicing open disclosure
8. Providing trauma informed aged care services
9. Recognising and reducing resident vulnerability
10. Protection, prevention and service improvement.
It’s difficult to prevent sexual assault until we understand sexual rights and responsibilities. In our ageist world, older people are often not expected to be sexual, and as a result their sexual rights are often overlooked.
The sexual rights of older people are complex. They include both the right to engage in consensual intimacy and sexual activity; and the right to be safe from sexual assault. The Charter of Sexual Rights and Responsibilities in Residential Aged Care has been developed to promote sexual rights, particularly the right to be free from sexual assault.
Residents’ sexual rights and responsibilities
1. The right to engage in sexual activity: you have the right to engage in lawful sexual activity in the privacy of your own room without fear of judgement or restriction by staff, if all participants have consented and the activity does not involve the harassment of staff.
2. The right to sexual consent: you have the right to information about sexual consent, including the right to refuse participation in sexual activity without your consent.
3. The right to continue existing sexual relationships: you have the right to continue existing sexual relationships, including those relationships that were formed prior to your admission (contingent on Right No 1 above).
4. The right to form new sexual relationships: you have the right to form new relationships and the right to express your sexuality (including the right to have sex) in a new relationship (contingent on Right No 1 above)
5. The right to change the way you express your sexuality: you have the right to change the way you express your sexuality, including the right to change relationship patterns and gender expression/identity (contingent on Right No 1 above)
6. The right to sexual privacy: you have the right to sexual privacy; this includes privacy of information and physical privacy for sexual activities (contingent on Right No 1 above)
7. The right to be free from sexual assault: you have the right to be free from sexual assault, including any sexual activities or conduct you do not consent to.
8. The responsibility to respect other residents: you have the responsibility to ensure you do not infringe on the rights or safety of other residents in the expression of your sexuality.
9. The responsibility to respect staff: you must respect the rights of staff to work in a safe environment. Any kind of violence, harassment or abuse towards staff or others is not acceptable.
This Charter gives aged care facilities some criteria to help balance residents’ sexual rights and responsibilities and their responsibilities.
• Is it sexual activity?
• Have all participants consented?
• Does the activity infringe on the rights of other residents?
• Does the activity involve harassment of staff?
• Is the resident’s right to privacy respected?
• Can the resident participate in sexual activity without fear of judgement by staff?
• Can the resident participate in sexual activity without restriction by staff? (if all the other criteria are met)?
Here is an example of how the criteria can be applied. Maria is a widow who met Barry after she moved into an aged care home. They are in love. They hold hands in the dining room and some nights they have sex in Barry’s room. They both have capacity to provide sexual consent. Maria’s children want them separated. Barry’s children are pleased to see their dad is so happy.

1. Sexual consent – they both have capacity to consent.
2. The right to privacy – Maria and Barry’s sexual relationship is not discussed with their children because the residents can provide sexual consent.
3. Without fear of judgement – At a team meeting, staff were told of the relationship and reminded of the residents’ sexual rights and staff were encouraged to discuss any concerns they had.
4. Without restriction by staff – A staff education session was facilitated to update staff on how to support Maria and Barry.
It’s important to note that there is a shift around Australia to affirmative consent. It’s not just the absence of objection or silence.
“If older women don’t say no - that doesn’t mean yes”, Theresa Flavin, Dementia Advocate.
Consent must be given with knowledge of what’s occurring, in rationality or in keeping with a person’s character, and with free agreement. It’s important to remember that the resident is always the decision maker, if they have capacity to make decisions. If they do not have capacity to make decisions, then consent cannot be given.
#ReadytoListen in Home Care
Older people also experience sexual assault in their own homes. Home care and community services are on the front line in older people’s homes every day and may be one of their key supports.
#ReadyToListen learnings can extend to the home care environment. It’s still about leadership and having policies in place.
A #ReadyToListen webinar for home care providers and staff is available to assist with reducing and preventing sexual assault against older women in their own homes, available at www.adalaw.com.au.
Strategies provided within the available #ReadyToListen webinar to assist in responding to survivors include:
• Listening and giving the older person permission to speak
• Building a relationship and trust
• Giving choices – leaving is not the only option
• Understanding local support services – building relationships with police, family or sexual violence services for secondary consultation and referrals.
The #ReadyToListen project is led by the Older Persons Advocacy Network (OPAN), in partnership with Celebrate Ageing and the Older Women’s Network NSW. Dr Catherine Barrett, Director of Celebrate Ageing is leading the project.
Find #ReadyToListen resources and the Charter of Sexual Rights and Responsibilities in Residential Aged Care at www.opan.org.au.
ADA Australia is the Queensland member of the Older Persons Advocacy Network providing advocacy support to people in aged care to uphold their rights. To contact ADA Australia or an aged care advocacy service in your State or Territory, you can phone 1800 700 600.
All information is this article is taken from #ReadyToListen resources and webinars available at www.opan.org.au.
Glaucoma Australia patient support program proven to reduce anxiety
One of the most impactful ways Glaucoma Australia influences the eye health of Australian’s is via their innovative patient support program which empowers individuals to understand their disease and make informed decisions to maintain their quality of life.

The program that has been proven to reduce anxiety among people diagnosed with glacuoma1 has helped thousands of people like Lei Malaband, a 54-year-old mother of four who was first diagnosed with glaucoma at 41.
Lei was completely shocked when she was first diagnosed with the incurable condition 13 years ago.
“I had worn glasses for a long time but driving at night was proving more difficult. Testing with my ophthalmologist would reveal a loss of peripheral vision, with the diagnosis of open angle glaucoma that requires nightly medication and adapting my lifestyle to keep my glaucoma stable,” Lei explains.
“I turned to a support group on Facebook, which I found through Glaucoma Australia, for key support because my friends didn’t really understand it. People think of it as an old person’s disease. But unfortunately, it doesn’t discern.
“My view is that everyone’s glaucoma journey is going to be different, so don’t be frightened to ask questions and most importantly, try not to be scared, even though it can be very overwhelming. I am still the youngest in the waiting room, and I was just over 40 when I was first diagnosed. My advice to all is get your eyes tested regularly. Don’t put it off. Better still, make it part of your yearly check-ups.”
The program not only provides emotional support to help manage anxiety associated with a glaucoma diagnosis, but it also plays a facilitation role within each person’s circle of care, to maximise rates of appointment and treatment adherence.
Glaucoma Australia CEO Richard Wylie says, “We’re incredibly proud of the results from our annual patient impact survey which show patients who are supported by Glaucoma Australia do much better than those who don’t have access to our program.
“Our goal is to help eye health professionals ‘extend their care’ beyond the practice, thereby maximising long-term adherence and treatment outcomes,” adds Richard.
Glaucoma Australia’s most recent Patient Impact Measurement Survey1 which was conducted in July 2022 confirmed the program’s effectiveness:
• 20 per cent of patients surveyed said they always or frequently feel anxious in relation to their glaucoma compared to 44 per cent of patients when they first join the Patient Support Program.

• 60 per cent of patients surveyed rated their knowledge of glaucoma and how it is treated as above average or excellent compared to 34 per cent of patients when they first join the program.
• 87.5 per cent of patients supported by Glaucoma Australia said they adhered to their eye drop regimen compared to 50 per cent of unsupported patients after six months and 37 per cent after three years.2
• 91 per cent of patients surveyed said they always attend their recommended glaucoma appointments.
Patient entering the program have access to a variety of resources but it is the one-to-one support provided by qualified Orthoptist Educators that is most popular with those feeling anxious in relation to their glaucoma.
John, who was diagnosed with glaucoma 11 years ago and suffers from anxiety, first reached out to Glaucoma Australia in 2019 and has done so on several occasions since; usually before or after his glaucoma appointments with both his optometrist and ophthalmologist.
Glaucoma Australia’s patient educators were delighted with the outcome of John’s most recent interaction with the team via email.
“I would like to sincerely thank you for your kind and understanding response to my anxiety episode re upcoming ophthalmologist appointment and fears of the future of my eyesight. I really like your suggestion of visiting my local optometrist three months after visiting the eye specialist. I think that would go a long way to
reducing some of my anxiety. I will arrange to speak to the optometrist and explain the situation. You manage a wonderful service through Glaucoma Australia and I really appreciate your help, to combat my generalised anxiety in relation to glaucoma.”
Glaucoma Australia senior orthoptist educator Sapna Nand says, “I encourage all eye health professionals to refer their glaucoma patients to Glaucoma Australia so we can provide them with ongoing support and education as an adjunct to the care provided by their ophthalmologist and optometrist.
“Our clinical educators are here to provide the extra time and counselling that is not possible in a busy day to day clinic,” adds Sapna.
Health professionals can refer their patients to Glaucoma Australia via:
Oculo
Web: glaucoma.org.au/refer
Email: glaucoma@glaucoma.org.au
Phone: 1800 500 880
Mail: Patient Referral Brochure
Print: Join Our Community Poster glaucoma.org.au
Go-to resource for meaningful consultation with people impacted by dementia
“You cannot feel what it is like inside our minds. Without us, you only have half the story,” person living with dementia.

In late 2022 Dementia Australia launched Half the Story, a free guide co-authored by people impacted by dementia for organisations to engage in meaningful consultation with people living with dementia, their families and carers.

It contains information, tips, and strategies for community groups, service providers, businesses or other organisations that want to consult in a meaningful way with people living with dementia, families and carers.
It will help you set up your consultation process, refine your approach and increase participation and engagement.
What is meaningful consultation?
Meaningful consultation describes activities where the primary aim is to seek out, affirm and ratify the voice of people living with dementia, families and carers.
You may see this type of activity described as engagement, advocacy, involvement, or participation.
In many ways, meaningful consultation, especially with people living with dementia, is still an emerging methodology.
Meaningful consultation is necessary to understand the full story.
Expect that meaningful consultation will require you to work differently. Most of these changes are simple. Others require time, resources and commitment.
Why meaningful consultation matters
People living with dementia, families and carers have important things to say about life with the condition, their hopes for the future and areas where better support is needed. Through consultation, you can identify opportunities for improvement and develop solutions together.
Meaningful consultation respects the dignity and human rights of people living with dementia and recognises knowledge and skills. It amplifies their voices and involves people in decisions that will affect their lives.
Meaningful consultation can dispel myths and misconceptions about dementia. It ensures your project is ethical and meets the needs of people living with dementia, families and carers.
Participating in meaningful consultation is empowering for people living with dementia, families and carers. It is an opportunity to become a community champion, create positive change and break down discrimination.
Ensuring people impacted by dementia have a say in the decisions that impact them
People living with dementia, families and carers should be a part of any decision-making process that will impact the lives of people affected by the condition. This can range from daily care and treatment decisions, to national or international policy and service design.
Projects that need meaningful consultation include:
• scoping, feasibility or needs analyses
• developing new services or programs
• reviewing existing services or programs
• setting strategic goals, aims or plans
• applying for funding or grants
• end user or accessibility testing
• creating resources about dementia
• wanting to understand the lived experience
• community developments like a dementia-friendly community.
Additionally, it is important to highlight that as of 1 December 2022 all new aged care providers, and all existing providers from 1 December 2023 are required to offer to establish a consumer advisory body at least once every 12-months*. Aged care service providers must also establish a quality care advisory body to support and inform the governing body in adherence to the dates listed above. Dementia Australia urges any aged care providers who are required to follow the new regulations to engage in meaningful consultation.
The numerous benefits of meaningful consultation
People living with dementia, their families and carers become involved in consultation and advocating for people impacted by dementia because they want the best possible outcomes for Australians affected by the condition. They offer unique insights and ideas that will add value and conviction to your project.
People living with dementia, families and carers are experts in the lived experience and can identify shortfalls, gaps or unmet needs. They can bring new ideas and perspectives and can advise on feasibility and efficacy. People with lived experience can help you reach your target market and come from a broad range of professional backgrounds.

COMMON FAQ ABOUT MEANINGFUL CONSULTATION AND DEMENTIA
When is the right time to consult?
It is always best to consult as early as feasible, ideally in the planning stages of your project.
You should also conduct regular consultation throughout your project. This will ensure you continue to reflect the needs and preferences of people living with dementia, their families and carers. It also reduces the risk of getting negative feedback during the user-testing, implementation or evaluation stages.
Are you required to pay those who you consult with?
Respect and appreciation for an individuals’ contribution and expertise is essential to meaningful consultation. Honorariums and sitting fees are ways of acknowledging their time and expertise.
Asking someone to participate without payment can unintentionally reinforce an unequal power dynamic and make them feel secondary to the decision-making process.
For face-to-face consultations (such as committees or focus groups), an hourly or daily sitting fee is appropriate. When hosting a large group consultation, or when a sitting fee might affect a participants’ support payment, an honorarium of a gift card, voucher, or other acknowledgement might be preferable.
Not everyone feels comfortable accepting money for consultation. If someone declines, donating the sitting fee to charity or research is an alternative.
The Victorian State Government offers guidance on remuneration rates for advisory-type committees (Type C meetings). Other governments and peak bodies refer to the recommendations of the Remuneration Tribunal for offices not-specified.
Video conferences or document reviews also warrant an honorarium or sitting fee. Sitting fees should be paid on top of reimbursements for travel and other expenses.
Do I need to make any special accommodations when consulting with people living with dementia?
Dementia is more than memory change. It can change the way a person sees, understands or responds to the world around them. Some of these changes include difficulties with vision, depth perception, and defining objects and space, disorientation in time and place, difficulty with speech or reading and more.
There are things you can do to make the consultation process more accessible to people living with dementia.
Dementia accessibility involves modifying the physical environment to lessen the impact dementia has on the person.
Dementia accessibility supports independence, personhood and a sense of wellbeing. It also enables a person living with dementia to participate in consultation with confidence and in safety. Family members and carers can have their own accessibility requirements.
Half the Story lists a number of things which can be done to ensure your consultation process is accessible to people living with dementia including how to best design printed documents, environmental audits and considerations for travel and accommodation.
Where can I learn more about meaningful consultation and Half the Story?
Download Half the Story for free at: dementiafriendly.org.au
*(this requirement does not apply to state or territory approved providers or authorities or to local government authorities).
Read more in Dementia Australia’s website: dementia.org.au

Senior Australians contribute a wealth of talent and experience to our community, but ageing is not without its challenges. After the age of 65, some people will experience mental health challenges for the first time and not know how or where to find support. Isolation, grief, changing circumstances and concern about their independence are compounding risk factors.
Staying Connected highlights the importance of connection and how making time for a chat can mean so much to a friend or loved one.
One of those featured in the book is Gus Gleeson, 79. Gus’ wife had lived with dementia for five years before she passed away. The couple were married for 55 years and shared two children, four grandchildren and three great grandchildren.
Gus has subsequently experienced grief and loneliness, but has found comfort in connecting with others in his community including a weekly men’s coffee group started by Greg Smith, 42, who is an R U OK? Community Ambassador. “Most of the guys are on their own or live on their own, so are in similar situations,” said Gus. “We talk about all sorts and even share stories about learning new domestic chores since our wives have passed away. A lot of people don’t like talking about it, I think it’s a male thing.
“The coffee group is so important to me. I genuinely look forward to going and Greg is such a great bloke,” said Gus. “He puts so much thought into the groups, which is probably why we all keep showing up. It’s important that we continue to go – to keep social and to keep connected. If you can’t go, you feel like you miss out on something and if you don’t turn up, they’ll ring to see if you’re OK.”
Research has found people engaged with the R U OK? campaign are up to six times more likely to reach out to someone who might be troubled1. Which is why R U OK? is working to build awareness and engagement with those aged 65 and older to build capacity amongst seniors to look out for each other.

The Staying Connected activity book is just one of the free resources available from the
R U OK? ‘Your Natter Matters’ campaign, which tailors the R U OK? message to this audience. ‘Your Natter Matters’ aims to increase confidence levels and reinforce the value of simply asking, ‘are you OK?’ and lending a listening ear.
For R U OK? Community Ambassador Greg, forming meaningful friendships with men from the coffee group has been as valuable. Greg has been a full-time career for his mum Lyn for more than ten years.

“Being a carer is very rewarding, but it can take a toll,” said Greg. “It took me a while to realise I was so focused on Mum’s needs and looking after her, that I wasn’t doing things for myself and because of that my mental health took a hit. I noticed other blokes in similar situations to me, so I thought if I do something for myself, I could also do something for them.
“Being around these blokes, knowing what they have been through, and having them around as support gives me hope for whatever challenges I face,” explained Greg. “Spending time with older people helps you understand life a little more. And they have cracker stories. It’s really great to see the friendships that have formed over the years.”
The signs it’s time for an R U OK? conversation can be subtle. There might be changes in verbal or non-verbal
behaviour. Someone might tell you they’re having difficulty filling their days or they might be withdrawing from social situations.
“A meaningful ‘natter’ can positively impact feelings of self-worth and self-esteem and make a big difference to someone who might be struggling with life,” says Katherine Newton, R U OK? CEO. “R U OK? wants to empower our seniors and the broader community to stay connected with the seniors in their world.”
The health promotion message aims to increase levels of peer and social support for Australians aged 65+ and features both printed and digital resources that focus on when and how to have an R U OK? conversation that could change, or even save a life.
Footnote
How we can use gaming to support positive ageing
(and support our relationships with our pets, too)

Margaret, 63, loves playing online Scrabble everyday with her sister who lives interstate. The online game allows a playful way to keep in constant contact when geographically distant.
Tom, 70, discovered the joy of Wordle and sharing his daily outcomes with friends. Penelope, 67, gets online to play Roblox games with her grandchildren who are living interstate.
These are just a few examples of the many ways older adults are gaming across Australia.
During the pandemic lockdowns, games were not only spaces for everyday creativity and informal literacy, but a way to socialise and keep fit – both mentally and physically. So much so that, in 2020, the World Health Organisation acknowledged the communicative and social power of games for wellbeing.
Even though the typical gamer is middle-aged woman, ageist stereotypes about gamers continue to circulate, reflecting broader inherent ageisms embedded within Australian culture.
Maybe we could turn this problem on its head. Perhaps we could use games to empower ageing and ageing well, creating bridges between the generations – and even improve our relationships with animals while we’re at it.
Ageing well
Older adults are one of the most divergent cohort of technology users, from “silver surfer” innovators to those who have little experience or confidence.

Victoria’s Ageing Well Report lists eight attributes to ageing well: positivity, purpose, respect, socially connection, keeping up in a changing world, financial/ personal security, health autonomy and mobility.
Many of these attributes can be addressed through games and play. In our study into mobile game practices in Australian homes, we found numerous ways in which games offer intergenerational ways for socialising, connection and creativity.
Word games like Scrabble and Wordle have been deployed to add playful, social dimensions to people’s lives: older adult siblings playing online everyday, or grandparents playing with grandchildren interstate.
Game apps like Pokémon Go have been used to motivate older adults to exercise and socialise.
In countries as varied as Japan and Spain, the power of Pokémon Go has enhanced various dimensions of everyday life – from getting mobile and discovering local neighbourhoods to playing together cooperatively to win tournaments.
Game genres such as “social justice” and “games for change” have been deployed to address complex issues such as elder abuse in new ways by providing safe spaces to enhance empathy and reshape perceptions.
In our research, we accompanied and interviewed older adult players in Badalona, Spain about their use of Pokémon Go.
On the streets of Badalona, chasing Pokémons was clearly about intergenerational play and sociality. The game was such a success in older adult rehabilitation by making exercise fun and social that social workers started to prescribe it as part of their health plans.
There is a growing body of research into games for intergenerational connection. But the role of games to enhance our relationships with animals has been overlooked – despite the fact animals play an essential role in our contemporary relationships.
Our best friend
Australians love their animals: one in three prefer animals to humans.
Despite this reality, animal companions are not acknowledged in Australia’s aged care plans. This means many older adults can be disenfranchised by the system.
For many older adults, animal companions are crucial to their social and physical wellbeing.
Digital games like Stray see the player take on the role of a stray cat. These types of games can enhance our empathy for animals, but there is a missed opportunity in relation to the human-animal bonds for ageing well.
The human-animal kinship is a space ready for gameplay which could enrich the possibility of ageing well.
During the pandemic lockdowns, Melbourne’s Cherished Pet Foundation trialled different techniques to support their community – including the use of games.
Pet Playing for Placemaking (co-designed by Jacob Sheahan) invited older pet owners and local community members to partner up and compete in treasure-hunt style gameplay.
Older pet owners, limited in mobility and vulnerable to the virus, completed digital puzzles which reveal locations where their play partner (typically a volunteer or neighbour) can walk their pet and discover more challenges that lead to other places.
Participants reported they found the game a fun way to connect with their neighbourhood and their community – and it kept their pets happy, too.
The beauty of game play
Ageing well is about positive and empowering pathways for ageing across emotional, physical and mental domains.
This can take many forms: social connection, respectful relationships, regular exercise and mobility.
Games can play an active role in empowering ageing, enriching social and intergenerational connection, mobility and health.
While the pandemic has laid bare barriers to ageing well, it has also created opportunities. Maybe we all need to play more with ageing well?
Author: Larissa Hjorth, Professor of Mobile Media and Games., RMIT UniversityThis article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ how-we-can-use-gaming-to-support-positive-ageing-and-support-ourrelationships-with-our-pets-too-186554
Storytelling allows elders to transfer values and meaning to younger generations
If you spent time over the holidays with elderly relatives or friends, you may have heard many of the same stories repeated — perhaps stories you’d heard over the years, or even over the past few hours.

Repeated storytelling can sometimes be unnerving for friends and families, raising concerns about a loved one’s potential cognitive decline, memory loss or perhaps even the onset of dementia.

Our research at Queen’s University suggests there is another way to think about repeated storytelling that makes it easier to listen and engage with the stories. We interviewed 20 middle-aged adults who felt they had heard the same stories over and over from their aging parent. We asked them to tell us those stories and we recorded and transcribed them.
We used a narrative inquiry approach to discover that repeated storytelling is a key method for elders to communicate what they believe to be important to their children and loved ones. Narrative inquiry uses the text of stories as research data to explore how people create meaning in their lives.
Transmitting values
Based on nearly 200 collected stories, we found that there are approximately 10 stories that older parents repeatedly tell to their adult children.
The hypothesis was that repeated storytelling was about inter-generational transmission of values. By exploring the themes of those repeated stories, we could uncover the meaning and messages elders were communicating to their loved ones.
The ultimate purpose was to offer a new and more constructive way of thinking about stories that we’ve heard many times before, and that can be otherwise perceived as alarming.
Here’s what we have learned:
1. There are typically just 10 stories that people tell repeatedly. While 10 is not a magic number, it does seem to be about the right number to capture the stories that are told over and over. Interviewees felt that a set of approximately 10 allowed them to do justice to their parent’s stories.
2. Among our interviewees, a significant number of their parents’ stories – 87 per cent — took place when they were in their teens or twenties. A person’s second and third decades are a time when they make many of the decisions that shape the rest of their lives; a time when values are consolidated and the adult identity is formed
3. What’s important about the 10 stories is not the factual details, but the lesson that was learned, or the value that was reinforced — values like loyalty toward friends, putting family first, maintaining a sense of humour even in hard times, getting an education, speaking up against injustice, and doing what’s right.
4. Key themes in the stories reflected the significant events and prevailing values of the early to mid-20th century. Many of the stories revolved around the war, and both domestic and overseas experiences that were formative. Many of our interviewees heard stories about immigrating to Canada, starting out with very little, seeking a better life and working hard. Stories often reflected a more formal time when it was important to uphold standards, make a good impression, know one’s place and adhere to the rules.
5. The stories elders tell appear to be curated for the individual receiving them. They would be different if told to another child, a spouse or a friend.
Tips for listening
Our research offers some tips for listening to stories from elders:
• Focus on just 10 stories. It can make the listening seem less overwhelming.
• Write them down. Writing challenges us to get the story straight.
• Notice your loved one’s role in the story, as the message is often contained in that role.
• Be attentive to feelings, sensations, tension and discomfort. These can be signals or clues to the meaning of a story.
• Finally, remember these stories are for you — selected and told in the context of your relationship with your loved one. As such, they are a gift from a loved one who is running out of time.
The importance of receiving stories
Storytelling is an essential human process and a universal experience associated with aging. Neuroscientists suggest that storytelling has practical survival value for individuals and communities, as well as social and psychological benefits.
It may be as powerful as medication or therapy for overcoming depression among elders. Storytelling becomes especially important when people become aware of their mortality — when they are ill, suffering or facing death.
People don’t necessarily tell the same stories over and over again because they’re losing cognitive function, but because the stories are important, and they feel we need to know them. Telling stories repeatedly isn’t about forgetfulness or dementia. It’s an effort to share what’s important.
Our hope is that by better understanding elderly storytelling, caregivers may be able to listen in a different way to those repeated stories and understand the messages they contain. Those 10 stories can help us to know our loved one at a deeper level and assist our parent or grandparent with an important developmental task of old age.
This research offers a constructive way for caregivers to hear the repeated stories told by their aging parents, and to offer their loved one the gift of knowing they have been seen and heard.
Author: Mary Ann McColl, Professor, School of Rehabilitation Therapy, Queen's University, OntarioThis article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ storytelling-allows-elders-to-transfer-values-and-meaning-to-youngergenerations-197766
RIOT ART & CRAFT YOUR CREATIVE OUTLET


At Riot Art & Craft, we are committed to empowering your creative endeavours. As Australia's largest art and craft supplies retailer, we have been serving the artistic community for more than four decades. Our extensive range of products caters to the needs of both novice and seasoned artists, and includes painting supplies, sculpting equipment, needlework kits and more! With us, you'll find everything you require to ignite your imagination and unleash your artistic potential.
We have a no minimum order requirement. We understand that each business has different needs, and we want to make it easy for you to order the products you require, without any restrictions.
We offer priority dispatch. We know how important it is for you to receive your orders in a timely manner, and that's why we prioritize dispatching your orders as soon as possible.
We pride ourselves on our dedicated customer service support. Our team is always available to assist you with any queries or concerns you may have. We strive to provide you with exceptional customer service and ensure that you have a hassle-free experience when dealing with us.
We offer thousands of products to choose from. Our extensive range includes a vast array of products across various categories such as art supplies, resin, modelling and casting, kids craft kits, craft basics and so much more!
Finally, we offer the lowest prices in the market. Our pricing is highly competitive, and we work hard to ensure that our customers get the best deals possible. We believe that everyone should have access to affordable and highquality products, and that’s why we offer the lowest prices without compromising on quality.
At RIOT, we are committed to providing you with exceptional service and quality products. Contact us today to see how we can assist you to help spread the creativity!
Contact Details Genie Stah
P: 0460336213
E: genie@riot.com.au
W: wholesale.riot.com.au
Social Media Links: facebook.com/riotartandcraft instagram.com/riotartandcraft/ youtube.com/c/RiotArtCraft/videos pinterest.com.au/riotartandcraft/
The BrainTrainerPlus is a recreative portal designed to stimulate cognitive activities and memories for the aged through the power of games.
This revolutionary designed console and software unit for the Aged primarily aims to dust off the blanket of boredom that can persist in aged care facilities while enabling and entertaining the minds of the elderly.

A lifetime of travel, history, people and one’s personal general knowledge should never be forgotten. Residents are able to use the console independently alleviating high demand interaction by staff and positively inspiring independent interactions between residents.

EXPERIENCE THE JOY!
Take your residents on a trip down memory lane with one of our highly sought after, interactive, hatching programs. Fully resourced with information on how to run the program and a few extra activities for your residents online, our program is delivered right to your door, no mess, no fuss, just a whole lot of enjoyment. Diversional Therapists and Lifestyle Co-ordinators love the way our program encourages their residents to participate and to communicate with each other around the brooding pen. We service the Sunshine Coast; Toowoomba; Brisbane, the Gold Coast & Tweed Districts; Sydney; Newcastle & the Central Coast; Greater Melbourne; Geelong and Adelaide.
BOOK ONLINE TODAY and let your residents experience the joy and therapy that animals can provide.


www.hennypennyhatching.com.au


The BrainTrainerPlus features:

• Easy to use touch-screen console.

• Assorted quizzes, games and puzzles.
• Can be played independently, 1:1 or in groups.
• Can be personalized with a Life Story album.
• Eliminates boredom and creates smiles.
• Increases communication and encourages interaction.
• Does not require Wi-Fi for playing.
To arrange for a free trial at your facility, get in touch with us today!
info@braintrainerplus.com.au
www.btplus.com.au
Kick up your heels – ballroom dancing offers benefits to the aging brain and could help stave off dementia

The big idea
Social ballroom dancing can improve cognitive functions and reduce brain atrophy in older adults who are at increased risk for Alzheimer’s disease and other forms of dementia. That’s the key finding of my team’s recently published study in the Journal of Aging and Physical Activity.
In our study, we enrolled 25 adults over 65 years of age in either six months of twice-weekly ballroom dancing classes or six months of twice-weekly treadmill walking classes. None of them were engaged in formal dancing or other exercise programs.
The overall goal was to see how each experience affected cognitive function and brain health.
While none of the study volunteers had a dementia diagnosis, all performed a bit lower than expected on at least one of our dementia screening tests. We found that older adults that completed six months of social dancing and those that completed six months of treadmill walking improved their executive functioning –an umbrella term for planning, reasoning and processing tasks that require attention.
Dancing, however, generated significantly greater improvements than treadmill walking on one measure of executive function and on processing speed, which is the time it takes to respond to or process information. Compared with walking, dancing was also associated with reduced brain atrophy in the hippocampus – a brain region that is key to memory functioning and is particularly affected by Alzheimer’s disease. Researchers
also know that this part of our brain can undergo neurogenesis – or grow new neurons – in response to aerobic exercise. Research shows those who regularly dance with a partner have a more positive outlook on life. While several previous studies suggest that dancing has beneficial effects on cognitive function in older adults, only a few studies have compared it directly with traditional exercises. Our study is the first to observe both better cognitive function and improved brain health following dancing than walking in older adults at risk for dementia. We think that social dancing may be more beneficial than walking because it is physically, socially and cognitively demanding – and therefore strengthens a wide network of brain regions.
While dancing, you’re not only using brain regions that are important for physical movement. You’re also relying on brain regions that are important for interacting and adapting to the movements of your dancing partner, as well as those necessary for learning new dance steps or remembering those you’ve learned already.
understanding of the indirect effects of COVID-19 –particularly those that increase dementia risk, such as social isolation – is urgently needed. In my view, early intervention is critical to prevent dementia from becoming the next pandemic. Social dancing could be a particularly timely way to overcome the adverse cognitive and brain effects associated with isolation and fewer social interactions during the pandemic.
What still isn’t known
Traditional aerobic exercise interventions such as treadmill-walking or running have been shown to lead to modest but reliable improvements in cognition –particularly in executive function.
My team’s study builds on that research and provides preliminary evidence that not all exercise is equal when it comes to brain health. Yet our sample size was quite small, and larger studies are needed to confirm these initial findings. Additional studies are also needed to determine the optimal length, frequency and intensity of dancing classes that may result in positive changes.
Why it matters
Nearly six million older adults in the U.S. and 55 million worldwide have Alzheimer’s disease or a related dementia, yet there is no cure. Sadly, the efficacy and ethics surrounding recently developed drug treatments are still under debate. The good news is that older adults can potentially lower their risk for dementia through lifestyle interventions, even later in life. These include reducing social isolation and physical inactivity. Social ballroom dancing targets both isolation and inactivity. In these later stages of the COVID-19 pandemic, a better
Author Helena Blumen Associate Professor of Medicine and Neurology, Albert Einstein College of MedicineThis article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ kick-up-your-heels-ballroom-dancing-offers-benefits-to-the-aging-brainand-could-help-stave-off-dementia-194969
Transcord provides a door to door shared community transport service for a range of activities and appointments across the Gold Coast region from Ormeau to Tweed Heads.
Transcord supports social inclusion and offers transport to participate in Social Day Trips and 1/2 Day Trips to varied locations around the South East QLD and Northern NSW as well as shared transport going to:

• Visit family and friends
• Library, bingo, senior citizen groups, etc
• The movies, shopping centres, parks, theatres, expos
• RSL Clubs, bowls clubs, casino, and sports clubs
• Hospital, medical and dental appointments.
Lifestyle interventions like social ballroom dancing are a promising, non-invasive and cost-effective path toward staving off dementia as we – eventually – leave the COVID-19 pandemic behind. www.transcord.com.au
Attending the ATSA Independent Living Expo: A Guide for Those Involved in Aged Care
The ATSA Independent Living Expo is a key event for those involved in the aged care sector. Held only every two years, this expo provides a platform for industry professionals to come together, exchange ideas, and learn about the latest innovations and developments in the field. Whether you're a care worker, administrator, or business owner, attending the ATSA Independent Living Expo is a valuable opportunity to stay upto-date with the latest trends and advancements in independent and daily living products.
The seminar program, which is free to attend, has a number of international guests, many returning to Australia for the first time since borders have reopened, and some presenting at ATSA for the first time. The program will have new panel sessions as well as the return of the popular adaptive clothing fashion show that was launched in Brisbane last year at all three events in 2023. The presentations are always well attended and are a drawcard for the event.
Here are some tips for getting the most out of your experience at the ATSA Independent Living Expo:

• Pre-register: Register before you get to the show, and you will receive a voucher for a free coffee or tea. If you have an accessible parking permit/ badge permit you will receive free parking too.
• Plan ahead: Before you attend the expo, take some time to research the exhibitors, speakers, and sessions that will be taking place. This will help you make the most of your time at the event and ensure you don't miss any opportunities to learn or network.
• Network with other attendees: One of the key benefits of attending the ATSA Independent Living Expo is the opportunity to network with other professionals in the aged care sector. Take advantage of this by introducing yourself to other attendees and exchanging contact details.
• Attend sessions and workshops: The ATSA Independent Living Expo features a range of sessions and workshops that are designed to help attendees learn more about different aspects of aged care
and daily living needs. From educational sessions on specific topics to hands-on workshops, there is something for everyone. Be sure to attend the sessions and workshops that are most relevant to your role or area of interest.
• Visit exhibitor stands: The expo floor is filled with exhibitor stands representing companies and organisations supporting the aged care sector. Take the time to visit to learn more about their products and services, and to discuss your needs and requirements with the representatives.

• Take notes: With so much information to take in, it can be helpful to take notes during the sessions and workshops you attend. This will help you retain the information and refer back to it later on.
Attending the ATSA Independent Living Expo is a valuable experience for those involved in the aged care sector. By taking advantage of the opportunities to learn, network, and connect with other professionals, you can gain valuable insights and knowledge that will help you in your role. So why not make the most of this opportunity and register for the ATSA Independent Living Expo today!
Attendee feedback
‘Thanks for an absolutely fabulous two days. As a consumer I learnt lots and now have some great new pieces of assistive technology on order.’
‘So glad I made the trip to attend. I found it to be an invaluable experience. I am almost certain I will be back to attend many more expos in the future. Thank you again to all involved in making these expos happen.’ ‘It was terrific and so nice to get our community together.’
‘Loved it all as usual. Good variety of stands. EASY to navigate in a 3-wheel (small) electric scooter’ ‘Was definitely worthwhile to gain knowledge about new independent and daily living products.’
‘Thank you for continuing to provide this expo, I thoroughly enjoy attending. I also enjoy attending the information sessions and find them relevant and informative.’
‘Always look forward going to ATSA – wealth of info, products, education and networking. It was a great event! Loved every minute I was there.’
Save the dates and register early
ATSA Independent Living Expo Melbourne- 24-25 May 2023
ATSA Independent Living Expo Perth – 31 May – 1 June 2023
ATSA Independent Living Expo Canberra - 7-8 November 2023


Your Facility Before
X Medication Incidents.
X Missed Medications.
X Unqualified staff dispensing medications.
X Constantly chasing doctors for paper scripts.
X Delays getting medications from Pharmacy.
X Frustrated Staff, Doctors and Management.

X No control over second check person.
X No tracking of patch placement.
X PRN outcomes not recorded.
X Incorrect dose calculations.
X Poor Nurse retention.
X Always training agency staff and tracking issues and difficulties.
X Unhappy residents and families
We hold the Answer
Your Facilty After MediSphere
Administer and document medications. The right resident receives the right dose at the right time. No errors, no misses, no problems.
Control who administers medication and second checks with access managed at facility level.
Avatar for patch placement, PRN outcome reminders. Test results recorded and automated sliding scale dosage calculations - less human error.
eScripts frees Doctors to spend more time with residents.
Pharmacy receive scripts instantly and medication dispensed the same dayreduce delay in residents’ treatment.
Greater communication between pharmacy and facility.
Reporting requirements at your fingertips.
Happy families knowing their loved ones are well cared for. Stay up to date via the Family Portal.
Improved staff retention, less stress on care staff.


Award winning EMM solution, combining realtime prescribing, dispensing, reporting and administration.
GOLD WINNER
MediSphere can help your Facility call 1800 003 938.
Error rate of less than 1 in 1,000,000

Blisters or Sachets
Flexibility. Choose either blisters or Sachets, or a mix of both.
99.99% accuracy, packing over 3.6 million pills per week with accuracy rates improving year on year.
Over 20 years experience servicing 400+ facilities and growing
TGA licensed packing facilities producing Blister Cards and Sachets.
Scalability with packing facilities located in all states on the east coast, providing timely, efficient service to both city and country areas.
A better and safer experience for residents and facilities managing complex medications.
Growth potential for your DAA business through daily deliveries and disaster management.
MPS PAK
Innovative packing solutions, enabling facilities and pharmacies to focus on and connect with their residents and customers.
Connect with MPS PAK today, call 1800 003 938

Australia’s largest range of leisure and recreational activity resources
Looking to provide your clients with the latest and best quality activity resources? We have you covered.
Wisdom Activities was established in 1999 as an aged care activities retail shop. Today, we remain 100 per cent Australian owned and operated, selling products both nationwide and around the world. Our main goal is to provide Recreational Therapists and activities staff with evidence-based products to ensure best practice and improved client outcomes.

With almost 700 products, we have Australia’s largest range of leisure and lifestyle resources that have been selected and tested by degree-qualified Recreational, Diversional Therapists and Occupational Therapists to cater for seniors and those living with disabilities within residential, hospital and community settings.
We sell activity resources that are designed to support, challenge, and enhance the cognitive, spiritual, emotional, physical, social, and cultural wellbeing of your residents, as well as specialist Dementia resources to assist with non-Pharmacological approaches to care.
From motion sensor pets and child representation dolls, music resources, quiz and discussion material, table games and physical activities, as well as specialised resources for people living with visual, cognitive, or physical impairments, our range is constantly growing with new products being added each month to ensure that we are keeping up with the latest products available globally.
If you can’t find what you are looking for, please call us and speak to one of our friendly staff members who can assist you in finding the perfect resources to meet your activity needs. Want to speak to a specialist? We have degree-qualified Diversional and Recreational Therapists on hand to answer any questions you may have about our products.
Placing orders is quick and easy. We are an online shop, so you can place orders 24 hours a day, seven days a week, with orders being shipped daily Monday to Saturday. You can place orders online, through email or over the phone. We cater to all orders from small one-off purchases to large specialised new residence commissions. We highly value our customers

and are happy to offer 30-day credit accounts to approved returning customers. Just have your accounts or purchasing team contact us to set up your account.
We look forward to hearing from you and helping you provide the best quality leisure and lifestyle programs to your clients.
To find our more contact us on 1300 301 319, wisdom@wisdomactivities.com.au or visit us on www.wisdomactivities.com.au

Wisdom Activities specialises in providing for aged care facilities, day centres for the aged, retirement villages, nursing homes, hostels, home assistance, mental health and dementia services for elderly and older seniors. Some items on our website may also be suitable for community health organisations regardless of age. If you need assistance navigating the website or have a special request please call in. We enjoy hearing from you.

1300 301 319


wisdom@wisdomactivities.com.au

www.wisdomactivities.com.au



Prioritisation of safety initiatives
There is a concept often shared by health and aged care colleagues which describes staff ‘working to the top of their scope’. This concept embodies the ability of staff to think outside of just completing a ‘task’ to tick a job off a list. When staff work to the top of their scope they are required to use their knowledge, skills and experience to provide some robust critique to the therapeutic interventions they are carrying out and hence by default are always considering whether the solutions they are providing for the resident are the most appropriate given the circumstances.
Clinical governance provides an important framework for managers to foster and develop clinical leadership across all levels of the organisation. Such a framework is able to set expectations around best practice, assist with the analysis of what clinical interventions work best with different residents in different situations and to easily report on outcomes. An electronic clinical governance framework goes one step further providing real time analysis and vivid transparency as to the level of staff intervention and involvement in clinical care. Whether the determined solutions are directed at an individual resident or the care home as a whole, visibility provides managers with peace of mind and encourages critical thinking across the staff base regardless of role. Managers need to know if their staff interactions are benefitting or hindering the resident and whether they
are solving the right problem in the right way at the right time with the right resources.
Clinical governance requires the analysis of a range of quality indicator data – in aged care this encompasses falls, infections, wounds and continence interventions to name a few. This provides a perfect vehicle for managers to drive professional development initiatives across their workforce to raise the clinical bar. Hence a sound clinical governance framework assists managers with identifying whether staff are working to the top of their scope and if not identifies areas for improvement and further action.
Assigning a clinical ‘champion’ responsible for wounds, infections, continence and falls prevention is an excellent way to get buy in from the staff working at the coal face. The champion doesn’t have to be a manager or indeed even a registered nurse. Some of the best champions in the aged care sector have been caregivers working to the top of their scope. They have been able to bridge the often perceived divide between their care worker colleagues and management and have provided salient suggestions and real world solutions completely tailored to the individual residents they know so well.
Around the world Governments have committed to setting standards in benchmarking quality healthcare. Regulatory bodies play a vital role in setting the healthcare standards health agencies are required to meet and exceed. In the UK

(CQC), Australia (Accreditation) and NZ (Certification) Standards provide the owners and managers of aged care facilities with a bar under which they are deemed to fall short. Pre the standards revolution at the turn of the century, aged care was very task driven, mistakes were seen as inevitable and when they were made care providers often omitted to learn from their mistakes. Globalisation, commitment from Government bodies to research and benchmark best practice, and the combined knowledge of first world healthcare providers to constantly manage risk and improve services has meant that sound clinical governance is now well embedded in aged care culture and our daily work.
CONTACT:
E: admin@leecare.com.au
P: 03 9339-6888
www.leecare.com.au

Follow us: www.linkedin.com/company/leecare-solutions
www.facebook.com/LeecareSolutions
www.instagram.com/leecare_solutions
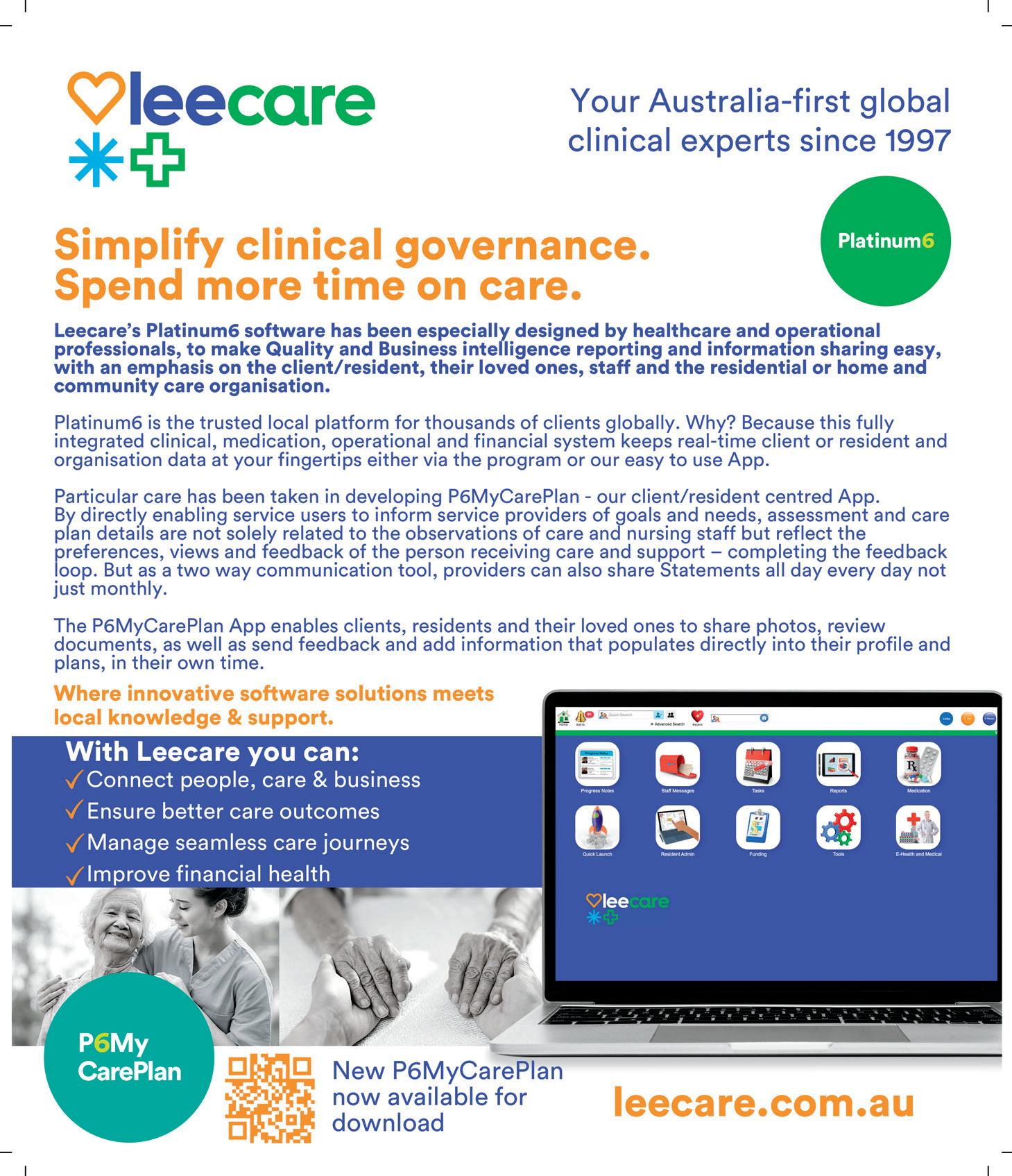
Clinical governance
Clinical governance is a relatively new concept that originated out of the NHS late last century in response to a number of significant and avoidable clinical events. It was originally defined by Gabriel Scully and Liam Donaldson in 1998 as:

“a system through which healthcare organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care, creating an environment in which excellence in clinical care will flourish.”
A sound clinical governance structure should always have the resident or patient at the centre of decision making. The safety and wellbeing of the healthcare consumer is paramount to the clinical governance process working. It is not enough to just determine what clinical intervention needs to be administered to circumvent an adverse event from happening to an individual. With the exception of providing lifesaving emergency care (and even then best practice would dictate some form of advance planning and consent), services must be person-centred, meaning the resident and/or their family must be party to all healthcare decisions that affect them.
Healthcare providers often need to carefully manage conflicting priorities with regard to managing risks and providing interventions. What may be a realistic mainstream intervention on the part of the care home may be viewed as completely unrealistic from the perspective of the individual receiving the therapeutic intervention or care.
Clinical governance lends itself easily to an electronic program which enables staff to have high visibility of the health of a range of different quality indicators at the push of a button. Most electronic programs provide at least one real time dashboard which prevents managers from having to delve into a myriad of folders and pore over excel spreadsheets to derive data. With the advent of artificial intelligence there is now even less excuse for governors of care to not be able to identify and closely manage clinical risk.
An electronic program can easily cut and slice which indicator information can be seen by which health/care discipline so the data is always relevant to the workers
scope. For instance kitchen staff need to see a real time change to someone’s texture modified diet but will not likely be remotely interested in the continence related risk to a resident.
Being able to see real time data on a dashboard or via a report means managers can circumvent worrying trends and intervene before a resident experiences an adverse clinical event and becomes very unwell. An electronic program will provide protection for junior staff when issues need to be escalated. An alerts dashboard will ensure transparency as the accountability to take action is shifted to more senior members of staff. Furthermore a Key Performance Indicator dashboard will enable managers to see a full month to month data set for comparisons.


An electronic clinical governance program that regularly pre-empts or prevents major adverse events from occurring will no doubt result in significant productivity and cost savings. In a sector that will always be challenged by lack of funding and a lack of skilled resource, clinical governance by its very nature has the ability to enhance operational efficiency and effectiveness which is a vital component of probity.
For care staff this might be reflected in more opportunities to work to the top of their scope where staff can be supported to be more self-aware of the quality of their interactions and more innovative in their care solutions. For quality assurance managers the ability to review quality indicator reports in real time and escalate concerns or provide immediate responses to staff is incredibly reassuring. For operational managers such a programme might be seen in their ability to be more collaborative and instructive, guiding their staff through professional development opportunities to reduce duplication and waste, reduce emotional distress for staff, raise the quality bar and ensure high levels of quality care at all levels of the organisation.
Clinical governance is the conductor of an orchestra that collects relevant data, contextualises it, analyses
it and then derives interventional plans to assign accountabilities to specific individuals and teams to improve clinical performance and effectiveness. Through this process a feedback loop is then able to determine and inform training requirements for staff. Mandatory clinical training is most effective when provided within the context of the quality indicators being measured. Understanding the knowledge and process gaps identified through clinical governance will mean training can be effectively tailored to meet any knowledge and process deficits. A cultural shift to drive staff engagement and commitment at both an individual and care home wide level is much more likely to occur when staff understand the ultimate goal they are aspiring to achieve and where there is transparency and a safe environment to feedback where staff are falling down in their attainment.
If nothing else a clinical governance programme will assist with identifying what the actual problem is you need to solve, whether the accountability for change sits at an individual, a team or a care home level and most importantly whether the CEO has effectively communicated the vision and provided the right leadership to create a culture where clinical safety is a priority for every member of staff.
Author: Petrina Turner-BennyFor more information contact:
Email: petrina.t@leecare.co.uk
Phone: +44 7732 7753 85
Website: www.leecare.co.uk
Could ‘virtual nurses’ be the answer to aged care staffing woes? Dream on
Former Health Department Chief Martin Bowles has reportedly proposed “virtual nurses” could help address the shortage of nurses in aged care.
This might involve remote, possibly artificial intelligence-assisted, virtual care, rather than physical nurse presence, to assist nursing homes to meet new legislative requirements to have a registered nurse present 24/7.
There are clear opportunities for technological innovations to improve the care, health, and wellbeing of older people. However, substitution of face-to-face nursing and human interaction with remote care is not the answer.
This seriously risks perpetuating the status quo where many older people suffer from isolation, neglect and lack
of human engagement. Eroding requirements to properly staff nursing homes with registered nurses could make it even harder to attract and keep staff.
What are ‘virtual nurses’?
“Robot nurses” already exist in some contexts, helping to move patients, take vital signs (such as blood pressure), carry medicines and laundry, and even engage with patients.
However, “virtual nursing” likely refers to more familiar technology where a real nurse provides a limited range of care via telehealth (by phone and/or video).

While some might appreciate when robots can assist with certain tasks, much of what nurses do cannot and should not be performed remotely (or by robots).
Indeed, older people, their loved ones, and staff are calling out for more physically present staff and more time to care and interact, not virtual interfaces and remote consultations.
The benefits of technology in health care are unquestionable and many innovations have improved care for older people. Artificial intelligence shows promise in helping prevent and detect falls, and socially
assistive robots such as PARO (a baby harp seal), have been shown to reduce stress, anxiety and antipsychotic use in people with dementia.
Technology should not, however, be introduced at the expense of care quality or supporting and sustaining a suitably sized and skilled aged care workforce. We still need to adequately staff nursing homes to provide safe, dignified care.
We need adequate staffing


The Royal Commission into Aged Care Quality and Safety heard a vast quantity of evidence regarding insufficient staffing, particularly of nurses who have the education and skills to deliver high quality clinical and personal care.

This expertise is why nurses cannot be replaced with remote care, and why the Commission recommended 24/7 registered nurse presence; this has now been legislated.
More than half of Australian aged care residents live in nursing homes with unacceptably low levels of staffing and around 20 per cent do not have a registered nurse onsite overnight.
Insufficient staffing results in workers not having time to interact with residents meaningfully and compassionately and also contributes to avoidable hospitalisations, worse quality care and outcomes, and poor working conditions for staff.
As social beings, human interaction is fundamental to health, wellbeing, and best practice care. This is particularly true for older people in nursing homes who are less able to engage with others and is especially vital for those living with mobility challenges and dementia.
Partly due to nurse low staffing levels, loneliness, isolation and mental ill health are widespread in aged care and have become more common due to pandemic related restrictions on visitors and staff.
Care experiences are shaped by human interaction and contact; the touch of a hand, a smile, eye contact, and being able to take the time to genuinely listen.
These actions are central to how nurses and other staff build effective and meaningful relationships with residents.
Seeking to replace human contact with virtual interfaces seems both inconsistent with the Royal Commission’s findings and possibly cruel.

Personal interactions also help staff, as the Royal Commission highlighted:

Knowing those they care for helps care staff to understand how someone would like to be cared for and what is important to them. It helps staff to care – and to care in a way that reinforces that person’s sense of self and maintains their dignity. This type of person-centred care takes time.
Rather than circumventing reforms to ensure more nurses provide face-to-face care in nursing homes, we need to address the range of challenges contributing to widespread and tenacious workforce shortages.
There are clear challenges for growing and retaining a sufficiently sized and skilled aged care workforce. However, government reforms, such as better pay, mandated care time, and greater accountability and transparency regarding the use of funds all work together to make aged care a feasible and attractive sector to work in.
This is one where staff are supported to provide the high quality and safe aged care all Australians deserve and where older people receive best practice, human care.
Author: Micah DJ
Peters Senior Research Fellow / Director - Australian Nursing and Midwifery Federation (ANMF) National Policy Research Unit (Federal Office), University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation. com/could-virtual-nurses-be-the-answer-to-aged-care-staffing-woesdream-on-188215

JnS Robotics: Bringing Innovative Robotics Solutions to Aged Care with Pudubot, Bellabot, Kettybot, Holabot, Swiftbot, Puductor2, SC50, and CC1
JnS Robotics is a leading importer and distributor of innovative robotics solutions that are designed to enhance the quality of care provided to elderly residents in aged care facilities. Among their offerings are delivery robots, disinfection robots, and commercial floor cleaning robots. Let's take a closer look at each of these robots and their unique names.

Delivery Robots:
Pudubot, Bellabot, Kettybot, Holabot, and Swiftbot
JnS Robotics' delivery robots are designed to address the challenge of timely and efficient delivery of medication and other essential items to residents in aged care facilities. These robots are fully autonomous and can navigate through complex environments to deliver items directly to residents' rooms. JnS Robotics offers five different delivery robots with unique names: Pudubot, Bellabot, Kettybot, Holabot, and Swiftbot. These robots can carry up to 10kg of weight per tray, making them suitable for a variety of delivery tasks.
Disinfection Robot: Puductor2
JnS Robotics' disinfection robot, Puductor2, is designed to effectively kill germs and viruses on surfaces and in the air. This robot uses a combination of UV-C light and spraying disinfectant to provide a thorough and effective disinfection process. Puductor2 is fully autonomous and can navigate through complex environments to disinfect areas that are difficult to reach manually. With its advanced sensors and cameras, Puductor2 is a reliable and efficient solution for maintaining a clean and hygienic environment in aged care facilities.
Commercial Floor Cleaning Robots: SC50 and CC1
JnS Robotics' commercial floor cleaning robots are designed to provide a reliable and efficient solution for keeping floors clean and hygienic in aged care facilities. The SC50 and CC1 robots use advanced sensors and algorithms to autonomously navigate through the facility and clean floors without the need for human intervention. The SC50 is designed for larger areas and can clean up to 3,000 square meters, while the CC1 is designed for smaller areas and can clean up to 1,000 square meters. With their unique capabilities, the SC50 and CC1 are an ideal solution for maintaining a safe and healthy environment in aged care facilities.
JnS Robotics is at the forefront of bringing innovative robotics solutions to aged care facilities. Their delivery robots, disinfection robot, and commercial floor cleaning robots are designed to enhance the quality of care provided
to elderly residents while also making the work of staff easier and more efficient. With their unique names, Pudubot, Bellabot, Kettybot, Holabot, Swiftbot, Puductor2, SC50, and CC1, JnS Robotics is helping to revolutionize the way aged care facilities operate. By embracing robotics solutions, aged care facilities can ensure that residents receive the care and support they need, while also maintaining a safe and healthy environment.
The simple solution is almost always the best - Okkam’s Razor
It is not easy to keep things simple in the complex world of aged care. Especially in the current climate. In the midst of large-scale changes, one easy digital check-in process for staff, visitors and contractors can be a step closer to a simpler and better world.
When traditional visitor books, staff sign-in sheets or contractor logbooks are replaced with different digital systems, the result is an array of disconnected systems and extra work to manually update them.
Siloed systems are rarely the best solution for anyonevisitors, staff or the business.
However, adopting one effective sign-in system that can ‘talk’ to other systems can help create a smoother and more efficient solution.
Discover what a simpler and better approach to digital sign-in for staff, visitors, residents and contractors can deliver for your aged care facility.

• 1. Increased Productivity
One of the most significant benefits of digitising the check-in process is improved efficiency. Traditional paperbased check-in methods are time-consuming, error-prone and a greater risk to spreading contagions than you might think as paper passes from hand to hand. In contrast digital check-in allows staff, visitors and contractors to sign-in quickly, accurately and with touchless options.
According to a study conducted by the Australian Institute of Health and Welfare (AIHW), digitising the check-in process in aged care can reduce check-in times by up to 60%.
The LoopSafe sign-in system takes productivity benefits even further. LoopSafe ‘talks’ to other systems such as rostering, payroll, clinical management and contractor management systems - automatically syncing verified check-in data and saving hours of manual data processing time.
• 2. Improved Compliance
Aged care needs to keep up with a shifting raft of entry requirements for staff, visitors and contractors. A digitised check-in process can help ensure that processes are compliant for everyone as well as provide audit evidence and reports with just a few clicks.
A good solution allows aged care providers to take control of their processes, make changes easily and quickly roll them out to every check-in point.
The best solution should simplify the sign-in processes even further. LoopSafe can verify documents held in other systems without the time consuming, inconvenience of visitors or contractors entering the same information each time they visit. The LoopSafe system also alerts staff of failed entry attempts via SMS, email, or a connected Nurse Call system – ensuring a consistent, compliant entry process even after hours.
•
3. Accuracy
Paper-based check-in methods can be prone to errors, particularly when it comes to recording the time and date of check-in. Digital check-in systems, on the other hand, use accurate and reliable digital clocks and eliminate approximations and errors.
Good digital systems also verify the identity of the person checking-in. A digital system that collects sign-in data but needs staff to manually check for accuracy, follow up incomplete sign-in records or upload to another system are prone to human error, inefficient and a poor use of valuable, skilled staff time.
LoopSafe offers the simple and best check-in solution with face ID technology verifying users and automatically sharing accurate check-in data with other connected systems. No human errors. No wasted time. No time delays.

•
4. Enhanced Security
Responsibility for the well-being of vulnerable individuals means security is a top priority for aged care facilities. By digitizing the check-in process, facilities can enhance security and reduce risk of unauthorized access with features such as biometric authentication, real-time tracking and the ability to flag or block individuals with restricted visiting rights.
A good digital check-in system can also provide detailed audit trails, allowing facilities to quickly track and trace or generate evidence for an incident.
When LoopSafe is used as the single check-in solution, staff have real time information about who is on the premises which can also be accessed from their mobile devices – invaluable during an emergency. LoopSafe can also provide an additional layer of security by connecting with an access control system, or directly to a door lock, and using face ID to activate access cards for verified owners – or triggering a door to open.
•
A digital check-in process can improve emergency management and reduce health and safety risk entering aged care communities.
As a minimum a check-in system should provide realtime information about who is on the premises. In the event of an emergency, staff can quickly and easily create a real-time emergency evacuation report of everyone on the premises.
LoopSafe automated more than 2 million check-ins in 2022 and alerted staff to 100K+ high risk attempted entries. Additional to emergency management features, LoopSafe can be customised to include identity and temperature checks*, document validation and screening questions all in one simple check in process. Identifying risks and raising alerts in real time to protect the health and security of staff and residents.
Simplifying your digital sign-in solution can deliver significant benefits to your staff, visitors, residents and business operations. LoopSafe is an Australian technology company, expert in designing the best, simple sign-in solution for aged care.
Technology tackling the global issue of adherence
Most older Australians take medication every day to manage their health and improve their quality of life. However, remembering to take medications on time can be a challenge. The World Health Organisation states that adherence to chronic medications is only ~50 per cent1, which means medications are only taken correctly 50 per cent of the time.
There are many factors that can contribute to non-adherence including confusion on when to take the medication, with or without food, and how long to continue the therapy. Some may have anxiety on taking too many medications, especially with the potential side effects relating to some medications. Some patients may simply forget or not fully understand the importance of their medication for managing their health condition.
MedAdvisor was developed in 2012 from a genuine need of co-founder, Josh Swinnerton, as he watched his mum struggle with managing the medication prescribed to treat her arthritis and Parkinson's disease. Keeping track of 10 medications was very difficult given their complicated

dosing regimens and different administration methods. It was also inconvenient for her to visit and wait at the pharmacy multiple times a month given her limited mobility. There had to be an easier way for his mum not only take her medications correctly but also be able to reorder her scripts conveniently from the pharmacy.
More than ten years later, the free MedAdvisor App connects over two million Australians to their local pharmacy to provide them with an automatic list of their medications. Smart reminders notify a patient when it’s time to take their medications, when it’s time to fill recurring scripts and when to see the doctor for a new script. The convenient ordering function allows patients to skip the queue at the pharmacy or request for their medication to be delivered.
If an older person is being cared for by another family member or guardian, MedAdvisor has a feature called Carer Mode which allows multiple family members to be managed under one account. The carer can manage and order scripts on behalf of the patient from near or far, providing peace of mind for carers and for those
managing their own medications, allowing the whole family to stay healthy and in control with a pharmacy at their fingertips.
As a result of using the app, MedAdvisor has shown to improve medication adherence by up to 20 per cent, which allows more patients to achieve better health outcomes from their prescribed treatments.

Source: 1.World Health Organization. Adherence to long-term therapies: evidence for action. https://apps.who.int/iris/bitstream/ handle/10665/42682/9241545992.pdf. Accessed 11/2/22.
To learn more about how MedAdvisor can improve, and support patients stay in control of their medication management, visit here: https://hubs.ly/Q01BWDsk0
See article
s







T 40MG ) O R D E R
(4) O R D E R
Add NDSS or diabetes product TrackandorderJane'sbloodglucose strips,syringes,penneedlesandmore








My non-prescription meds and vitamins
3 ABC Vitamin A 5000
DAYS LEFT
3 ABC Vitamin A 5000

DAYS LEFT


O R D E R
O R D E R
LEFT 3 ABCAMOL INHALER 100MCG ABChaler(Sample) 4 Repeats left DAYS LEFT 3 ORDER ABCHEAD TABLET 200MG ABCCofen(Sample) 0Repeatsleft ABCSTATIN TABLE ABCheart(Sample) O R D E R
Repeats left A D D
4 Repeats left O R D E R
28 ABCAMOL INHALER 100MCG ABChaler(Sample) MENU A D D
Add non-prescription meds, vitamins and supplements Starttrackingnon-prescriptionmedsand vitaminsandreceiveimportantreminders.

Staying Connected Saves Lives!
In a world where cars can drive themselves and identities can be verified with a retina scan, it seems almost inconceivable that people are still struggling to use their mobile phones indoors – especially considering the expanding global market for smart buildings, which is expected to reach more than $37 billion by 2023 according to the Globe Newswire.
Ironically, new buildings continue to be plagued by poor signal propagation, because of the very same features that brand them eco-friendly and attract potential occupants: low-emissivity (Low-E) glass, galvanised steel, metal roofs, and concrete walls are but a few common culprits. In the case of older properties whose designs simply did not take mobile coverage into consideration, building materials such as stone, concrete, and brick are notorious signal blockers, especially in densely populated urban areas.
We depend on our Public Safety Agencies to protect the Australian community, and they do it every day. Around the country over 550,000 women and men work selflessly to uphold and protect our Australian way of life. Communication is critical to that work. Smart, strong, and fast systems enable better decisions that save lives. Over 2 million triple zero (000) calls are made every year in Australia. Each one of those calls triggers a complex systematic response underpinned by missioncritical grade radio communications. Put simply, these communications systems have been built not to fail. 1
“If someone is injured or suffers a medical episode in the basement carpark of a building and can’t call 000 because there was no mobile phone signal, the body corporate managing the building could be sued.”
If someone is in distress and unable to place an outgoing call, first responders will not be aware there is an emergency that requires their response. For this reason, the Safer Buildings Coalition defines three pillars of in-building safety communications:
• Mobile 000 calls must get out with location accuracy.
• Mobile Mass Notifications must get in.
• First Responder communications must work.
If a building cannot deliver these basic characteristics, the environment puts the occupants and the property itself at risk.
Anyone who has ever tried to place a call from an elevator is not surprised that indoor coverage can be much worse than outdoor coverage. And the deeper into a building you go, the worse the signal typically gets. Penetrating walls is difficult for a mobile signal, though some of the RF spectrum blocks that the Australian mobile network operators have licenced are better for this task than others. Low band (longer wavelengths) spectrum tends to be much better at penetrating concrete and brick than high band (shorter wavelength) spectrum, such as 5G.
The Federal government is making a significant investment to improve wireless network coverage in rural areas, the Government has committed $380 million to the Mobile Black Spot Program to invest in telecommunications infrastructure to improve mobile coverage and competition across Australia. However, poor wireless coverage can be experienced in big cities as well. The networks were originally designed to work well in a “mobile” environment – namely outdoors while in moving vehicles or walking. As indoor usage has grown, the networks have densified, and greater efforts have been made to provide a signal strong enough to penetrate buildings. Providing high-quality indoor coverage is much more difficult.
Understanding which buildings fall short of providing adequate service can assist local governments in working with building owners and mobile operators to make needed improvements.
In Australia, there is no building code, regulation or legislation that mandates In-Building Coverage (IBC) to support operational communications.
For building owners, the benefits of providing reliable high-speed wireless coverage are clear: apart from the OH&S liability associated with poor IBC, there is increased tenant retention and recruitment rates, increased workforce productivity, and more attractive
property for visitors. Many building owners and operators believe having a strong indoor wireless network increases the value of their buildings by as much as 28%, according to CommScope.

Residential Care Village now Connected
A leading health care provider of residential aged care in metropolitan Sydney, Central Coast, Southern Highlands and Mid-North Coast reached out recently to commission our team to provide a mobile enhancement solution for a recently completed Retirement Village in Woy Woy NSW. Management had realised that the mobile service throughout the new complex was unsatisfactory and needed to be upgraded to keep the residents connected.
Our Solution
An In-Building Coverage solution was implemented; installing a clustered Cel-Fi system to boost the cellular signal throughout the building. The solution covered Telstra, Optus and Vodafone mobile networks to ensure residents could stay connected in the retirement village.
Our Outcome
The solution was an impressive outcome by the improved boost in carrier signal throughout the complex. Allowing staff, residents and visitors a better experience in staying connected no matter where they were within the village.
For more information on In-Building Coverage solutions talk to our Solutions Managers today on 1300 769 378, email sales@powertec.com. au or visit www.powertec.com.au


Real-time equipment tracking for a better resident experience
In the words of John Zammit – Property Services Partner at Maroba aged care, “If there are things we can do that can give our residents and their families comfort and peace of mind knowing that we can quickly deal with an emergency, then we try to do them. That means things like implementing Spotto equipment and asset tracking so that staff don’t need to go searching for the lifter they need — because they’ll know exactly where the nearest one is in the time it takes to type the name in Spotto. These are game changers for our residents, and our staff alike”
To hear John speak about how they never want to leave a resident in distress after a fall hammers home the most tangible benefit of asset visibility in aged care.
Maroba, a facility of 160 residents spread over four large buildings near the centre of Newcastle New South Wales, has consistently adapted and innovated to provide the best care they can, embracing technologies that make sense all the while being acutely aware that cost of new forward-thinking tools is a concern.
When Viv Allenson, Maroba’s much awarded CEO, learned about Spotto’s elegant and cost-effective solution for asset visibility she was enthused to just give it a go. Alongside the ability to respond to emergencies, Spotto would allow Maroba’s staff to spend more time on the core part of the organisation — resident comfort and care — and substantially less time wasted on searching for equipment. And with the ongoing challenges of staffing since COVID, every moment wasted can mean a resident not receiving care. With Spotto installed on every workstation around the four buildings, and on staff mobiles there’s never the need to send out search parties.
Spotto provides businesses like Maroba with fast, easy to use equipment search capabilities with minimal hardware requirements. If you know how to search with Google, then you already know how to locate equipment with Spotto. Maroba has set up a Spotto shortcut on all of their PCs and staff can run Spotto on their mobile devices whenever they want, and since it doesn’t cost any more to run Spotto on any device, they’re encouraged to use it as much as they need to.
Here’s how Spotto works Spotto is straightforward to set up and has been designed with non-technical folks top of mind. To start, staff can tag any piece of vital equipment with a small Bluetooth tracking tag, then install a matchbox-sized Spotto beacon reader into each zone where tracking is required. Beacon readers are on the lookout for Bluetooth signals from equipment tracking tags and show staff exactly where items are, or where they were last seen. Hot items like oxygen trolleys, Sarah steadies and WoWs are a great match for equipment tracking.
Staff and patients aren’t the only ones benefiting from real-time asset visibility. John highlights, “Spotto’s made maintenance visits from our suppliers more streamlined
too. They can go straight to the equipment they’re tasked with without having to locate it by sight around all four buildings. When there are several bits of equipment — that search can take quite a while and we end up bearing the added cost of that visit.”
John puts it very simply, “Now that we can offer these services without breaking the bank, why wouldn’t we? Our residents deserve the best care we can provide and Spotto is another of those technologies that helps us do just that.”
A radically low-cost system
A few years ago real time tracking systems were out of the price range of Aged Care facilities but Spotto’s lightweight approach and use of cloud computing has meant that businesses like Maroba can tailor the solution to their needs without relying on external services and expensive specialists.

Spotto has been engineered in regional New South Wales and is trusted by NSW Health to improve response time,

decrease operational inefficiency, and provide more patient care thanks to reclaimed time.
Electro-com, Australia’s leading specialist distributor of tracking hardware and sensor technologies is Spotto’s preferred partner specialising in supporting the Aged Care sector.
Website: spotto.io/aged-care
For info call Lynda Flanigan of Electro-Com: 1300 130 806



Aged Care Amendment Bill is a first step but more needed to ensure quality care
The Federal Government’s Aged Care Amendment Bill is a welcome first step in over-due sector reform, but more is required to meet the complex healthcare needs of older people.
The Federal Government’s Aged Care Amendment Bill is a welcome first step in overdue sector reform, but more is required to meet the complex healthcare needs of older people.
A clear action plan on allied health provision in aged care must be developed to meet the needs of residents and the recommendations of the Royal Commission into Aged Care Quality and Safety.
This plan should form part of larger legislative efforts to ensure access to the required multidisciplinary aged care workforce into the future.
Effective multidisciplinary teams, inclusive of allied health professionals, care staff, nurses and, where possible, GPs, are critical for comprehensive aged-care assessments and tailored service delivery.
Comprehensive assessment, planning and care delivered by a multidisciplinary team is vital to aged care residents and proven to maintain mobility, balance and quality of life.
The introduction of 24/7 registered nurses goes some way to addressing current system deficits.
However, uncertainty about the ongoing provision of allied health under the new funding model, the Australian National Aged Care Classification (AN-ACC), could result in fewer physiotherapists in the aged care workforce.

At the height of an aged care workforce crisis with understaffing commonplace across the sector, a diminishing allied health workforce will put further pressure on the overburdened care and nursing workforce and serve to undermine the goals of this Bill.
The Australian Physiotherapy Association (APA) is committed to improving, retaining and growing the physiotherapy aged care workforce and delivering safe and high-quality care to older Australians. We look forward to working with the Commonwealth on future reform to ensure access to high-quality, needs-based healthcare for all older Australians.
To view the APA’s submission to the Senate Standing Committee on Community Affairs inquiry on the Aged Care Amendment (Implementing Care Reform) Bill 2022 [Provisions] go to:
australian.physio/sites/default/files/ submission-2022-08/APA_ Senate_Inquiry_Aged_ Care_Amendment_%28Implementing_Care_ Reform%29_Bill_2022.pdf
Multidisciplinary Teams the key to unlocking Access to Primary Care

Allied Health Professions Australia (AHPA) welcomes the release of the Strengthening Medicare Taskforce Report today and supports the commitment of the Albanese Government to reform the primary care system, of which allied health is key.
Recognising the value of multidisciplinary primary care is long overdue. AHPA Chair and Taskforce member Antony Nicholas said “We encourage reforms that strengthen multidisciplinary team care and support funding mechanisms that allow allied health professionals to work to their full scope. However we caution that reform without an implementation roadmap and a commitment to engaging with the allied health sector will ultimately result in more of the same.”
AHPA is particularly concerned with the recommendation to increase investment in the Workforce Incentive Program (WIP). AHPA CEO Bronwyn Morris-Donovan says, “There is no evidence that the employment of allied health professionals under the WIP has improved access to multidisciplinary care.”
“The allied health sector has opposed the WIP since its inception - it undermines the entire employment model of private allied health. The Government is taking a general practice incentive payment and calling it a win for multidisciplinary team care. It is a not a win for consumers or allied health. It shows there is still no real understanding of how to build a system that genuinely puts consumers at the centre.”
While AHPA strongly supports greater investment into PHNs to strengthen their capacity to commission allied
health services, it should not be seen as a mechanism to ‘supplement general practice teams.’ We must move on from the notion that general practice is the only setting where primary care takes place.
There are thousands of allied health professionals working in the community in small private practices. The idea that bundling services under one roof is the antidote to fragmented care is fanciful. Coordinated care requires all parts of the primary health care system to work as a team, supported by appropriate resources, including connected digital technologies.
Although we welcome recommendations to modernise the My Health Record (MHR), allied health must be given access to, and considered in the development of all digital development.
Morris-Donovan said, “We must not forget that allied health professionals cannot contribute critical health information into the MHR, or choose suitable clinical information systems (CIS) that are interoperable with MHR.
“If Minister Butler is serious about improving continuity, quality and safety in health care, then bringing allied health into the digital ecosystem must urgently be addressed. “As it stands, the Strengthening Medicare Taskforce digital recommendations offer no reassurance that allied health will be prioritised.”
Additionally, while AHPA is supportive of recommendations to 'fast-track' the supply and distribution of the health workforce, we caution how this can be achieved. “There is no consistent collection and integration of allied health workforce data. This means the Government cannot confirm vital information about allied health professionals and their roles, resulting in fragmented, inconsistent approaches to workforce and service planning,” says AHPA Chair Antony Nicholas.
“The impact of this is poor access to essential allied health services, especially for people in rural and remote areas and people with chronic conditions.”
Changes in funding and infrastructure to Australia’s health systems that allow for consumer-centered primary care and equity of access to all Australians needs to happen now.
Allied Health Professions Australia is committed to working with the Australian Government to deliver the Taskforce recommendations. The impact of these recommendations is far-reaching for the health of all Australians. A clear implementation plan is the next step to reform.
Podiatrists hotfooting away from sector - issues for aged care and rural health
When we talk about the healthcare distribution in the bush versus the cities, we rarely consider access to podiatry services. Now a national study of Australian podiatrists between 2017 and 2020 reveals almost a quarter of the podiatrists surveyed are likely to leave clinical practise or the entire field within five years. Equal access to podiatry services is essential as poorer foot health outcomes, such as higher amputation rates, have also been identified in people outside of cities.
This predicted loss of podiatrists nationally is alarming because demand for podiatry services is forecast to increase until the 2050s due to the increasing burden of chronic disease and an ageing population, particularly in regional, rural and remote locations where there is an increasingly higher prevalence of chronic illness.
In a study published in the Journal of Foot and Ankle Research, PhD student Anna Couch, Associate Professor Cylie Williams and Professor Terry Haines from the Monash University School of Primary and Allied Health Care, surveyed 1129 podiatrists nationally from 2017 to 2020. They found that podiatrists from a rural background (30 per cent) were more likely to work rurally, while podiatrists who undertook a regional/rural placement during their undergraduate education were more likely to work in a metropolitan location.
Importantly, the study found that 26 per cent podiatrists indicated they were planning to leave direct patient care within five years because they were:
• unsatisfied with working conditions
• unsatisfied with opportunities to use their abilities
• perceived less personal accomplishment
• perceived less job satisfaction
Twenty-one per cent of podiatrists indicated that they were planning to leave podiatry work entirely within five years because they were less satisfied with opportunities to use their abilities; had a poor support network from other podiatrists; had less job satisfaction and did not have access to paid annual leave.
Approximately six per cent of the Australian podiatry workforce are located in outer regional or remote settings, with an estimated 16 podiatrists per 100,000 in major cities and six to 10 podiatrists per 100,000 in outer regional or remote settings.

According to Ms Couch, the findings suggest an emphasis on ensuring podiatry students from cities who undertake rural placements need further encouragement to stay once they graduate. “In Australia, people living in rural and remote areas experience higher rates of illness, hospitalisation and death when compared to other Australians, yet
these are the areas where there are greater shortages of health workers, and this is true for podiatrists as well,” she said.
“To retain podiatrists, it is important to ensure access to leave, professional support, and appropriate physical working conditions.”
Associate Professor Williams added that podiatrists play a fundamental role in the provision of health care in different settings including acute hospitals, sub-acute rehabilitation services, community health services, aged care, private practice and with participants of the National Disability Insurance Scheme.
“General practitioners increasingly rely on podiatrists for the management of people with foot problems. Chronic disease management plan funding through Medicare, in collaboration with general practitioners, has been effective in increasing access for people to podiatry services,” she said.
“Retaining podiatrists in the profession is critically important for optimising rural workforce supply, the development of strong relationships with people who have foot health needs and enhancing health outcomes within all communities.”
People living with dementia deserve timely access to physiotherapy
The Australian Physiotherapy Association (APA) and Dementia Australia are calling for timely and ongoing access to appropriately funded physiotherapy for people living with dementia.
Through a joint statement Physiotherapy and Dementia launched today, the health peak bodies united to draw attention to the critical importance of maintaining physical health, and its impact on improving mental health and wellbeing of people living with dementia.
Dementia Advocate Phil Hazell was diagnosed with younger onset dementia at 55 years old. Now 63 years of age, he has regularly visited a physiotherapist since his diagnosis to assist with the varying symptoms of dementia.
“My balance and knee joint pain were two major factors affecting my ability to do basic things, like walking up and down stairs, which significantly affected my day-to-day life,” Phil said. “One of my biggest motivators for seeing a physiotherapist was to help manage that pain and prevent another fall. I now feel more confident using stairs and I am better at judging distance one step to the next.
“I have also not fallen since last seeing the physiotherapist, so I encourage anyone living with dementia that needs help with pain management and mobility, to talk to your health care provider about physiotherapy.”
The position statement explores the early intervention measures available through physiotherapy in assessing, treating and achieving positive outcomes.
APA National President Scott Willis said that in many cases access to physiotherapy is not offered in a timely manner to people living with dementia.
“Too often the physical health of people living with dementia is neglected, as the focus traditionally has tended to be on cognition,” Mr Willis said. “Physiotherapy improves physical health and plays a significant role in improving mental health and mood.
“Physiotherapists can work individually or as part of a comprehensive, inter-disciplinary team to support the physical and cognitive needs of people living with dementia, including to help diagnose pain and other symptoms for those who with communication difficulties.” Dementia Australia COO Anthony Boffa said dementia is the second leading cause of death of Australians1 with an estimated 487,500 Australians living with dementia in 20222.
“Maintaining your independence is something everyone deserves and improving access to physical rehabilitative services is critical for those living with dementia,” said Mr Boffa. “Dementia Australia affirms the rights of people living with dementia to receive timely and ongoing access to physiotherapy services and the need for appropriate funding to support those services.”
Research has shown that physiotherapy can help improve the quality of life and independence of older Australians, including those living with dementia, by:

• improving motor skills such as gait and balance
• reducing frailty
• reducing the number of falls and fractures
• slowing cognitive decline
• improving cognition, agitation, mood3. The joint statement is available for download at Dementia Australia’s and the APA’s website.
Dementia is the second leading cause of death in Australia4. In 2022, there are an estimated 487,500 Australians living with dementia. Without a medical breakthrough, the number of people with dementia is expected to increase to almost 1.1 million by 20585. Dementia is a life-limiting condition that can have a significant impact on all aspects of a person’s physical or mental health. People living with dementia in Australia need comprehensive health care, including allied health services, but access to these services is limited.
1. Australian Bureau of Statistics (2020) Causes of Death, Australia, 2019 (cat. No. 3303.0)
2. Dementia Australia (2018) Dementia Prevalence Data 2018-2058, commissioned research undertaken by NATSEM, University of Canberra
3. ‘Physiotherapy and Dementia’ position statement, 2022 https:// australian.physio/sites/default/files/DEMENTIA_AND_PHYSIO_A4_F.pdf
4. Australian Bureau of Statistics (2020) Causes of Death, Australia, 2019 (cat. No. 3303.0)
5. Dementia Australia (2018) Dementia Prevalence Data 2018-2058, commissioned research undertaken by NATSEM, University of Canberra







































































































































































Alzheimer’s:
Blood
biomarker may help identify the disease ten years before symptoms start
Though Alzheimer’s disease affects more than 55 million people worldwide, there’s still no cure for the condition – and treatment options are limited.

While recent advancements in the field have led to the development of two medications which may delay the progression of the disease, their benefits are debated. Not to mention that in most clinical trials looking at the effectiveness of these drugs, treatment only begins after symptoms arise. This means damage from the disease has already taken place.
It’s thought that if treatment is started earlier – before symptoms begin – this may prevent the damage from happening. But the problem is the clinical symptoms that doctors look for to diagnose a patient with Alzheimer’s disease only appear after neurodegeneration has taken place.
Our recent study argues for using a different biomarker than those currently used to diagnose Alzheimer’s. We found that this biomarker, which can be detected in a person’s blood, may allow the disease to be discovered up to ten years before symptoms start. This provides a window of opportunity for early treatment intervention.
Blood protein
Our study was performed using data from Swedish families who had a form of Alzheimer’s disease caused by genetic mutations. While autosomal dominant Alzheimer’s disease (ADAD) has similar symptoms to sporadic Alzheimer’s disease (the most common form of Alzheimer’s, which is a combination of genetic, lifestyle and environmental factors), symptoms happen much earlier – typically in a person’s 40s or 50s.
Since the mutation is inherited, if a parent has ADAD their child will have a 50 per cent chance of inheriting the mutation. Although less than one per cent of all people
with Alzheimer’s disease have this form, research studies in these families provide valuable information on how Alzheimer’s disease progresses in general.
Our study looked at 75 people from three different families who all had a history of ADAD. Participants provided 164 blood samples in total, all collected between 1994 and 2018. The levels for four different blood-based biomarkers with known links to Alzheimer’s disease were analysed. We also performed other tests to look for signs of the disease, such as MRI imaging and cognitive tests.

Our main finding was that levels of one particular protein, called GFAP, increased before other known disease-associated blood-based biomarkers analysed in the study. This increase had already begun ten years prior to the first noticeable signs of Alzheimer’s disease.
GFAP is a protein released by the brain’s astrocytes –specialised cells that take part in the brain’s immune system, among other functions. While we know that GFAP is involved in the brain’s immune system processes, we don’t know its exact function. In studies on other forms of Alzheimer’s disease, GFAP has been suggested to mirror the activity of brain inflammation. It’s also associated with the presence of amyloid plaques – a hallmark of Alzheimer’s disease.
Our results are in line with other recent studies on genetic forms of Alzheimer’s, which have shown higher GFAP levels before disease onset.
Research has also shown that GFAP levels are higher in people with preclinical Alzheimer’s disease without a genetic cause, who have other signs of Alzheimer’s pathology (such as amyloid plaques) but aren’t yet
exhibiting symptoms. This suggests that our findings may also apply to the more common, sporadic forms of Alzheimer’s disease.
The results of our study are also important for supporting our general understanding of Alzheimer’s disease – particularly the early disease processes in the brain. Together with other recent findings, it’s clear that further investigation is needed to understand more about GFAP and its function in the brain – including in the progression of Alzheimer’s disease.
Perhaps future treatments for Alzheimer’s disease will be more successful if they seek to target both the brain’s astrocytes and other common hallmarks of Alzheimer’s disease – such as the accumulation of the beta-amyloid in the brain.
Authors Caroline GraffProfessor of
Charlotte
Genetic Dementia Research, Karolinska Institutet JohanssonPhD researcher, Neuropathology of Alzheimer's, Karolinska Institutet
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ alzheimers-blood-biomarker-may-help-identify-the-disease-ten-yearsbefore-symptoms-start-197745
The practical and aesthetic advantages of blinds and awnings for aged care residence

Blinds and awnings have many practical advantages for aged care residences that include providing much needed insulation, light control and privacy. These widely used window solutions not only improve the function of a building by delivering protection from the elements, but they enhance the interior and exterior appearance by adding an element of style.
Blinds and awnings prevent the sun’s harsh light entering through windows, which helps to keep temperatures inside the building cooler and provides comfort to the occupants of the internal space. It also helps to and protect the furniture, flooring and artwork from heat and sunlight damage.
Blinds and awnings can add a level of sophistication and enhance both the function and appearance of a residential care homes.
Blinds come in a wide range of styles including roller blinds, aluminium and timber blinds, vertical blinds, and Roman blinds. They are available in a variety of materials from timber, aluminium, and in material that are sheer, blackout or patterned. This wide range of choices in colour and texture make it easier to complement or contrast the existing interior design.
Awnings are also available in a range of materials, including metal, timber, and composite, and they too can be customised to fit any window shape or size.

Blinds can provide a great focal point in a room, and this serves to create interest and may function as a recognisable wayfinding point. In a residential aged care home with a predominately neutral colour scheme, a pop of colour can help specific spaces become more readily identifiable by the elderly residents.
Blinds and awnings both provide incredible control over light and temperature. This is particularly important in rooms that receive strong sunlight where heat and glare need to be minimised to protect the occupants as well as the furnishings. Blinds and awnings can be adjusted to control the amount of light that enters a room when the sun is streaming in or when more light is needed.
Another advantage of this ease of adjustment is that it effortlessly provides instant privacy in areas such as bedrooms and bathrooms.
Blinds and awnings provide a level of insulation and help to reduce energy costs by preventing heat from escaping through the windows. This is especially important for elderly residents in colder climates.
The aesthetics of blinds and awnings add architectural interest as well as interior design emphasis. Any architectural or interior design style can be catered to, from traditional or rustic looks to ultra-modern contemporary styles.
Awnings can also enhance the residence’s curb appeal by creating a striking impact or even just by visually unifying a number of exterior elements.
Blinds and awnings are a very popular window treatment in the harsh climate of Australia, and they are extremely beneficial additions to residential care homes to shield and safeguard the occupants, save energy and protect the building’s interior and enhance its appearance.
ALL PRODUCTS ARE GENUINE PATENTED TO ENSURE THE HIGHEST QUALITY POSSIBLE
Zipscreens - 50% off RRP
Shutters - 60% off RRP

Curtains - 60% off RRP

Straight Drop Blinds - 50% off RRP
Folding Arm Awnings - 50% off RRP

Roller Blinds - 60% off RRP


Vertical Blinds - 60% off RRP

ONE OF THE FASTEST LEAD TIMES IN THE INDUSTRY

Confusion, financial pressure, discomfort: Older people can struggle with sustainable living, despite its obvious benefits
Improving the sustainability of Australia’s housing stock is crucial to meeting national emissions reduction goals. But for older adults, such changes can bring both benefits and challenges.

My recent research examined the literature on environmental sustainability measures at residences for older adults. These included private homes, retirement villages and nursing homes.
I found that while sustainability measures can bring multiple benefits to older people, they also bring challenges. For example, people living in sustainable dwellings may use less energy and water which leads to lower bills. But older people may suffer cognitive decline and struggle to use sustainable technology devices.
The full effects of environmentally sustainable features must be better understood if we’re to provide seniors with high-quality residential environments.
Sustainability and ageing: A complex mix
Forecasts suggest that by 2056, 22 per cent of Australians – or 8.7 million people – will be aged 65 or older. Highquality residential environments are important to maintaining the welfare of these people as they age.

Environmental sustainability is playing an ever greater role in residential development across the board, including retirement villages. And previous research suggests most retirement village residents want to lead more sustainable lifestyles.
As climate change worsens, the dwellings of older adults should allow them to adapt to these changing conditions. The reduced ability of elderly people to regulate their body temperature means global warming is a profound threat to this group.
Improving the sustainability of a residential environment may include:
• reducing waste
• using low carbon or recycled building materials
• solar passive design
• efficient heating and cooling
• using renewable ene rgy such as rooftop solar.
Some residential projects for the elderly already include environmental sustainability. A case study of a not-for-
profit retirement village in South Australia revealed practices such as innovative floor plans, thermally efficient building materials, good window orientation and a water harvesting system.
And my previous research found a range of sustainability features at eight private and not-for-profit retirement villages in Queensland.
However, while many retirement village developers prioritise “social sustainability” features such as care provision and social interaction, environmental sustainability is largely ignored.
On the plus side
The benefits of environmentally sustainable features in in older adults’ residential environment include:
• reduced resource consumption: sustainable dwellings usually require less water and energy use, which lowers living costs. This is especially important for older adults who often have reduced financial capacity after retirement. Older people also use energy more intensively than other groups because they have fewer household members, greater heating requirements and spend more time at home.
• reduced health risks: environmentally sustainable measures can lead to healthier indoor environments. For example, good ventilation and high-quality air conditioning often lead to improved indoor air quality and more comfortable ambient temperatures.
• alleviated environmental challenges: many older people want their homes to be more environmentally friendly. Doing their bit to alleviate global problems such as greenhouse gas emissions can provide them with peace of mind.
The potential downsides
The challenges of environmentally sustainable home features for older adults include:
• financial pressure: the income of many older adults is substantially reduced after retirement. This can conflict with the high initial investment of developing an sustainable housing and the cost of replacing
existing systems with sustainable ones.
• reducing energy consumption: in some cases, sustainability measures can involve tolerating slightly higher or cooler temperatures. For example, moving from a gas-heating system to a more sustainable type may delay the arrival of heat in a room and leave older people uncomfortable for a short time. This may conflict with older people’s increased sensitivity to ambient temperatures.
• confusion and complexity: Older adults can have reduced cognitive capabilities affecting memory and information processing speed. As a result they may struggle to use sustainable technologies such as smart thermostats. Research has suggested ways of overcoming this, such as better recognising the diversity of older adults to achieve a better “persontechnology fit”.
Next steps
Older adults have unique needs which their homes must satisfy, even when sustainability features are being adopted.
Ageing should be seen as a dynamic process with physical, psychological and social dimensions. And the complex interrelationships of ageing, environmental sustainability and the residential environment also need to be recognised.
Best practices and lessons learned in creating sustainable living environments for older adults should be shared.
Finally, developers making sustainability decisions should consult other stakeholders. These include contractors, occupational therapists, researchers and most importantly, older adults themselves.
Author Xin HuLecturer, School of Architecture and Built Environment, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ confusion-financial-pressure-discomfort-older-people-can-struggle-withsustainable-living-despite-its-obvious-benefits-174535
Revamp your ageing care facility with monitored emergency lighting

We know that keeping your staff and patients safe is important to you. Elumen provides a fully compliant emergency lighting management system called EMIoT so that you can rest assured your facility is meeting the latest fire safety standards. Quick to install and easy to maintain, all our emergency fittings test themselves unobtrusively so that you never have to worry about scheduling tests again.
Emergency lighting is a crucial safety feature that is used in buildings to provide lighting in the event of a power outage or other emergency situation. It is designed to either provide temporary lighting until power is restored, or guide people to the nearest exit in an emergency situation. Aged care facilities are required to schedule an electrician to test and maintain their emergency lighting every 6 months. This can be time consuming, expensive and disruptive to staff and patients.
Harnessing the latest technology in wireless mesh networking, Elumen’s EMIoT system eliminates the need to schedule and conduct manual tests. All EMIoT fittings will automatically run a rigorous set of fire safety
compliant tests before uploading the results to our cloud service. This minimises the time electrical contractors need to spend onsite and reduces disturbance to staff and patients. Download test results and annual compliance certifications from anywhere, anytime. As a contractor friendly system, all Elumen products can also be manually drop tested by any licensed electrician so you’re never locked in to EMIoT. Save time, money and eliminate human error by choosing Elumen’s wireless monitoring system.
The EMIoT network and testing system uses a low-power mesh network technology, providing reliable wireless communications and testing functionality throughout the entire building. The mesh aspect of the network refers to the ability of the devices to communicate not only with a central hub or gateway, but also with each other, creating a network that can cover a large area and reliably support a large number of devices. All communications to the cloud are transmitted through our standalone gateway so we don’t require access to any existing IT infrastructure and you don’t need to maintain any onsite servers. Get started today with no cabling, test switches or additional hardware required.
Designed in Australia by a dedicated team of engineers, Elumen doesn’t compromise on quality. Elumen was established in 2011 and has continued to lead innovation and promote sustainability in the emergency lighting industry. In partnership with clients such as Bupa Aged Care, Sydney Olympic Park Showground, JLL, CBRE, Lend Lease and hundreds of buildings across Australia, Elumen has built a reputation for reliability, care and trust. All Elumen networking fittings include a premium 5 year replacement warranty and a dedicated service team to help you set up and manage your facility.
Get a free quote for your building today and learn how much you could save.
Phone number: 1300 927 533
Email address: info@wbstech.com.au
Website URL: https://elumen.com.au/







Thirst things first: Dehydration

Now that the weather is starting to warm up, it’s more important than ever to stay hydrated. Dehydration is common in the elderly for a number of reasons including:

• Decreased ability to recognise thirst
• Forgetting to drink
• Increased urination
• Reduced ability to self hydrate
• Lower body water content
• Difficulty swallowing
Dehydration can lead to serious complications and require hospitalisation. This can have a negative impact on health as well as quality of life. It is therefore important to recognise the signs of dehydration in the elderly and know how to address them.
WHAT TO MONITOR
Toileting
Have you noticed a change in your residents’ toileting? Are they going less frequently? Are their continence pads dryer than usual? These could be signs that they are dehydrated. When we are dehydrated, our body will conserve water by producing less urine. This results in a smaller volume of more concentrated (and stronger smelling!) urine. Once hydrated, our body will do the opposite. Noticing these changes can give you clues about a resident’s hydration status.
Skin
Skin can tell us a lot about hydration. If it appears dry or fails to return to normal after being gently pressed/ pinched then your resident may be dehydrated. Follow up by observing how their mouth and lips look. Dry, cracked lips and saliva that appears sticky and thick all
point to dehydration. Even a small sip of fluid can help return the mouth to its normal condition, which has the added bonus of making it easier to eat and chew.
Energy levels
It’s no secret that dehydration can increase levels of fatigue. This can cause a resident to sleep more which further drives dehydration. If you notice that a resident is participating less in activities, dehydration could be a possible factor.
Behaviour
Surprisingly, dehydration can cause changes to behaviour in the elderly. Do they seem less alert than usual? Are they complaining of a headache or dizziness? In some cases, dehydration can even cause delirium – a sudden and serious change in brain function resulting in significant confusion. Suspected delirium should be treated as a medical emergency.
Vital signs
Dehydration can cause a number of changes to the vital signs including an increase in heart rate and breathing, and a decrease in blood pressure. This occurs because dehydration can decrease the total volume of blood in your body, which means your body has to work harder! In severe cases, this can require hospitalisation and rehydration through a drip.
WHAT TO DO
Offer fluids
Offering regular drinks throughout the day is a good way to meet your residents’ fluid requirements. A variety of hot and cold drinks should be offered with every meal and snack, and be readily available at all times. Having
a variety of different drinks will keep things interesting for the residents, as well as increase the likelihood that they will finish it.
Offer snacks
It’s easy to forget that food also contributes to our fluid intake for the day. Foods such as yoghurt, custard, ice cream, jelly, fruits, and vegetables all have a high water content. Offering these foods regularly not only helps to keep your residents hydrated but also helps them meet their nutrition requirements.
Prompt and encourage
Never underestimate the power of encouragement! Elderly people often forget to drink or forget that they have one on their table. Just a simple reminder can make a big difference. Try different prompts, such as asking the resident if they’re enjoying their drink or if they would like another one. Ensuring drinks are within reaching distance can also significantly improve intake.
If you are concerned about your residents’ nutrition and hydration, send a referral through to your Plena Healthcare dietitian.
Bega creating great food for better nutrition in Aged Care

A cup of tea and a biscuit might be a standard morning or afternoon tea for many people; however, for older people, providing more nutrition can have a very significant impact on their health in aged care. Whilst a cup of tea and a biscuit might be comforting, it is far from the most nutritious of snacks and, for some, can get boring.
As we age, our appetite decreases but our nutrient requirements increase, so every mouthful of food counts and is critical to delivering optimal nutrition. At Bega Group we can help deliver more nutrition in every meal and snack through our range of nutritious dairy and juice products.
Recent research conducted in 60 aged care facilities across Victoria has proven just how beneficial increasing dairy foods in the diets of aged care residents can be1 Led by Dr. Sandra Illiuano, senior research fellow in the Department of Medicine at the University of Melbourne, the research involved a two-year trial in 60 Victorian aged-care facilities, including 7,195 residents.
It was the first of its kind to test the effects of providing additional calcium and protein by simply increasing dairy intakes from around 2.5 serves of dairy per day to recommended levels of greater than 3 serves of dairy per day. Dr. Illiuano’s team worked with each aged-care facility to adjust recipes and meal plans and put more milk, yogurt and cheese into as many meals and recipes
as possible. From swapping a cup of tea for flavoured milk, to adding yogurt and custard to desserts.
The results were astounding, achieving a 33 per cent reduction in all fractures, a 46 per cent reduction in hip fractures, and an 11 per cent reduction in falls – achieved simply by adding more dairy foods to the diet.1
The impact of this research is multi-fold. First and foremost, the potential to improve the quality of life of people in aged care when they are falling less and breaking less bones. However, the benefits will also be seen by carers and facility management alike with less injuries and ill health to manage.
The prevalence of malnutrition in aged care has been estimated to be as high as 50 per cent 2, and whilst dairy plays a key role in optimising muscle and bone health, fortification of food and drink with calorie-rich ingredients is a quintessential strategy to prevent weight loss and frailty of aged care residents. Fortification can be done with the addition of staple ingredients such as milk powder, cheese, sour cream, butter, custard and cream to meals and snacks.3
At Bega Group we want to help people in aged care eat more nutritious dairy foods for the sake of their health, quality of life and deliciousness of their diet. Dairy Farmers Fresh Cooking Cream, the new addition to the Bega Foodservice portfolio, is a key ingredient in the
kitchen to help health and aged care outlets provide high quality, fortified recipes. Developed and tested in conjunction with an accredited foodservice industry chef, the new Dairy Farmers Fresh Cooking Cream is ideal for high heat cooking in commercial kitchen environments.
Benefits of Dairy Farmers Fresh Cooking Cream:
• Proudly Australian owned and made
• Full cream taste profile, with fresh aroma and silky mouthfeel
• Ideal viscosity for sauteing, reducing, pan-frying, baking, freezing, and whipping

• Heats quickly to high temperatures, without burning or splitting
• 18% fat content
• Available in a 2L bottle
1. Effect of dietary sources of calcium and protein on hip fractures and falls in older adults in residential care: cluster randomised controlled trial (bmj.com)
2. https://dietitiansaustralia.org.au/sites/default/files/2021-12/202012PositionStatement-Malnutrition_in_Aged_Care.pdf
3. Bartl R, Bunney C. Best Practice Food and Nutrition Manual for Aged Care Homes Edition 2.2. Gosford: Central Coast Local Health District; 2015.
For more information please contact us on 1800 000 570 or visit our website www.begafoodservice.com.au

The majority of aged care homes are spending more on food
Spending on food for older people living in residential aged care has continued to increase with three quarters of aged care providers spending more than $10 a day on food per resident in aged care homes.
Aged & Community Care Providers Association (ACCPA) CEO Tom Symondson said the second Food and Nutrition Report 2021-22 released by the Department of Health and Aged Care shows a growing number of aged care providers are using creative and innovative practices to enhance residents’ experience with food in aged care.
“Good quality food and nutrition are vital to the health and wellbeing of older Australians. It is also essential for their daily enjoyment of life, as noted by the Royal Commission into Aged Care Quality and Safety,” Mr Symondson said.
“The importance of food quality in aged care has been further recognised with the introduction of a dedicated food and nutrition standard as part of the proposed new Aged Care Quality Indicators for age care which are currently being reviewed with sector consultation.

“This second Food and Nutrition Report shows that the majority of residential aged care providers are doing the right thing by providing nutritious food for their residents.
Managing your Food Safety Training
We specialise in design and delivery of nationally accredited Food Safety Training throughout Australia. Whether you are after basic food handlers qualification (Food Safety Level 1) or the full Food Safety Supervisor for your team, CFT can deliver accredited training to your group online or in a face to face class.

use of digital technology to support meal choice and on measuring mealtime experiences.
“Too often food in aged care gets a bad rap – unfairly so. Food and nutrition is a complex area for older people in residential care who will have different needs based on their health, personal preferences, and cultural background.
“We look forward to assessing the data contained in
Your one stop shop for all your Commercial Kitchen Equipment needs

Federal Hospitality Equipment is the importer of a very large, exclusive and professional range of commercial kitchen & catering equipment which enables us to offer our customers unsurpassed value and quality. We have a history of more than 50 years servicing the commercial catering, baking and food industries. We are an Australian owned and operated company with offices, showrooms and warehouses around the country including New Zealand.
A great aged care facility provides quality healthcare and support for the elderly which includes providing nutritious & high-quality meals to their residents. Outstanding and compliant facilities are crucial to meeting Australia’s Aged Care Quality Standards.
Aged care kitchens are an essential part of each facility & we are here to assist you build, expand, replace & consult by orchestrating & executing your kitchen requirements with you, and with Australasia’s largest range of commercial kitchen equipment, we are your one-stop shop when it comes to this.
Our range of Fagor Professional cooking ranges & combi ovens are designed around functionality & reliability making them perfect for your commercial kitchen.
Setting up a café within your facility? Then we have the perfect Espresso machine & industry leading Cake & Food Displays to help attract customers. Plus, so much more, our extensive range of equipment goes from A to Z, you name it, we have it! This makes purchasing & coordinating with us a smooth & easy process, like it should be. Why create unnecessary work & hassle for yourself when you can deal with the one company who has it all?
Whether it’s your main kitchen, staff kitchen or guest café, we have everything you need to build a safe, reliable, attractive & value for money concept.
Stock availability is rarely an issue & spare parts are in abundance, so if you need something rather quickly or yesterday (in most cases), you can rest assured that we are the right company to facilitate those demands because this is what we do. We also offer custom solutions as we know too well that ‘one size fits all’ isn’t really the case.
Our accomplished service team will assist you with any service scheduling & regular preventative maintenance, to help maintain and prolong the life span of the equipment you purchase. We assist with delivery, installation & provide product training with ongoing support. Our team are friendly, driven individuals who endeavour to provide solutions for our customers.
We have supplied thousands of businesses across the country with the equipment they need to run a smooth & successful operation. The other beauty of dealing with us is that you will be assigned your own industry professional who will be your point of contact from start to finish & throughout. Our team are highly professional, industry trained & very friendly. So be sure to contact us for any of your project or equipment requirements, no matter how big or small. We assure you of our very best attention.
Phone: 0427 296 539
Website: foodequipment.com.au
Youtube: @federalhospitalityequipment
Linkedin: /federal-hospitality-equipment

New Retigo Vision Blue makes aged care cooking easy, ergonomic, and nutritious
Food equipment leader J.L.Lennard is introducing a new combi oven to make aged care cooking simple and energy-efficient, whilst retaining maximum vitamins, nutrients and flavours.

The new Vision Blue is the most advanced in the Retigo range of combi ovens, and is able to be controlled via an intuitive and reactive touch screen that operates even with greasy hands or through gloves.
The range features six models with varying capacities that can create from 30 to 900 meals per day, so suit a broad range of aged care facilities from smaller homes to those with a large number of residents.
“The Retigo Vision Blue is highly flexible and customisable to each chef’s needs. It’s quite capable of making breakfast, lunch, and dinner, and can cook multiple different meals at the same time, even if they have varying cooking times,” says J.L.Lennard product specialist, Darren Cooper.
The Australian Royal Commission into Aged Care Quality and Safety highlighted the importance of food nutrition to the overall wellbeing of senior Australians. As a result, the Government introduced new measures and funding to increase the quality and nutrition of food in aged care facilities.
“A major advantage of the Retigo Vision Blue is that its fine mist steam prevents raining in the cook chamber, which would pool on food and crush delicate items,” explains Cooper.
"Instead, the advanced Retigo Vision steam generation system ensures great colour, taste, and consistency of prepared meals, while retaining maximum vitamins and nutrients,” he said.
Energy-efficient
The Retigo Vision Blue’s unique steam generator utilises pre-heated water injected into a centrifuge at the back of the fan to generate a fine steam mist with accurate control, saving up to 30% water consumption compared to alternative ovens used in the aged care sector.
Additionally, the oven is insulated with triple glazed door to lower heat transmission, which results in a cooler workplace and lower energy consumption. The Retigo’s unique automatic cleaning system provides optimum cleanliness while minimising water consumption, and saving money on detergents.
Ergonomic
The Retigo Vision Blue features a crosswise tray orientation for better visual control and more ergonomic removal of pans and trays.
“Everything about these ovens has been designed for a smooth and comfortable kitchen experience. The handle shape, for example, makes sure the door is easy to use and maintain. It even uses silver ions woven into the handle to reduce bacteria and minimises hygiene risks,” says Cooper.
Service Support
Retigo is represented by J.L.Lennard Australia-wide,
which means these new ovens will have the full service and backing of the family-owned J.L.Lennard company, which has 144 years of history, and prides itself on exceptional customer service.
“Not only are these machines manufactured to the highest quality and hygiene standards, but J.L.Lennard has a nationwide network of service technicians, along with spare parts, to ensure all equipment it supplies continues to operate in peak condition,” says Cooper.
About J.L.Lennard
Founded in 1879, J.L.Lennard is a family-owned fully Australasian company that distributes many of the world's leading processing and packaging machines for the food, packaging and pharmaceutical industries; food equipment for fast food outlets, restaurants, supermarkets and hotels. The J.L.Lennard name has a long history in both Australia and New Zealand, where the company established an office in 1899.
Sales, Service and Spare Parts
1800 777 440 • www.jllennard.com.au
Sydney • Melbourne • Brisbane
Adelaide • Perth • Auckland
■ Retains maximum vitamins, nutrients, and flavours
■ Cook multiple meals at once with an intuitive touchscreen display

■ Energy-efficient – saves water and energy
■ Outstanding ROI – payback typically achieved in 3 years

Staffing remains a significant challenge in the kitchen
Aged care kitchens play a critical role in ensuring the health and well-being of elderly residents. However, they face several challenges in ensuring the provision of quality meals that meet the diverse nutritional needs of the aged care population. One of the most significant challenges is staffing.
In Australia, aged care kitchens, face several staffing challenges, including recruitment and retention difficulties, skills shortages, and staff burnout. The shortage of skilled workers in the industry at present makes it challenging to find and retain staff members with the necessary skills and experience to manage the complex and demanding environment of aged care kitchens.

The demanding nature of the job, including long hours, physically demanding work, and exposure to high-stress situations, contributes to staff burnout. The high turnover rate and difficulty in filling vacant positions create significant challenges for aged care providers, who must maintain quality services while ensuring the safety and well-being of their residents.
To address these staffing challenges, aged care providers must implement effective strategies that attract and retain highly skilled staff members. This could include investing in staff training and development programs, providing flexible work arrangements, offering competitive compensation and benefits packages, and ensuring that the kitchen is best equipped to handle the rigour and demands needed in today’s push to deliver nutritious and delicious meals to residents.
It is more important than ever to ensure that aged care facilities are equipped with the latest technology to help streamline kitchen operations and provide the highest quality of care to residents. That's where Robot Coupe comes in - with its French made machines helping transform aged care kitchens across Australia into a culinary wonderland that is highly efficient, safe, hygienic and happy.
“Skilled labour and labour in general is one of the current challenges we have in our kitchens. The Robot Coupe Vegetable Preparation Machine absolutely reduces our prep time. Whether I’m slicing 10kg of carrots or banging out coleslaw for 150 residents, I can’t imagine doing it without it.”
Nathan Griffiths Estia HealthRobot Coupe machines are designed with precision and attention to detail, ensuring that your staff can prepare
meals quickly and accurately. The machines can chop, slice, grate, mix, blend, and puree ingredients with ease, making it possible to create a wide variety of dishes that cater to the unique dietary needs of each resident.

But preparing meals that meet the dietary needs of aged care residents isn't always straightforward. That's where IDDSI comes in. IDDSI stands for the International Dysphagia Diet Standardisation Initiative. It is a global initiative that aims to improve the safety and enjoyment of eating and drinking for individuals with dysphagia (difficulty swallowing). The IDDSI framework provides standardized terminology and definitions for food textures and drink thicknesses, making it easier for aged care facilities to provide meals that are safe and enjoyable for their residents.
By using Robot Coupe equipment to prepare meals that meet the IDDSI standards, aged care facilities in Australia can ensure that their residents are receiving nutritious, tasty meals that are safe to eat. This not only improves the quality of life for residents, but it also reduces the risk of choking and aspiration, which are significant concerns for individuals with dysphagia.
Another one of the biggest advantages of Robot Coupe machines is their versatility. With a range of attachments and accessories available, you can customize your machine to suit your specific needs and create a truly customized kitchen experience. Their powerful motors and sharp blades ensure consistent and uniform results every time, saving time and reducing waste.
With simple controls and intuitive design, even those with limited experience in the kitchen can quickly learn to operate them. This makes them ideal for aged care facilities where staff turnover can be high.
At Robot Coupe, we understand the importance of quality in aged care kitchens. That's why we see ourselves as #THEsolution with our machines designed to meet the highest standards of performance and reliability, ensuring that your kitchen runs smoothly day in and day out. Our machines are also backed by a comprehensive warranty and ongoing customer support, so you can rest assured that you'll always have access to the help and guidance you need.
Contact Robot Coupe
E: info@robotcoupe.com.au
T: 02 9478 0300 www.robotcoupe.com.au
Follow Us: www.linkedin.com/company/robot-coupe-official www.facebook.com/RobotCoupeOfficial/ www.instagram.com/robotcoupe_official www.youtube.com/@RobotCoupeOfficialChannel
providing solutions to the Care sector

Four ways seniors can stay youthful and healthy


Retaining a youthful way of life physically and mentally can be quite a challenging task for many aging adults.
Physical and mental exhaustion both contribute to seniors losing their vivacity and enthusiasm that they used to have in their younger years. Just because the odds are stacked against them does not mean that aging adults have to resort to a sedentary lifestyle where they are confined to their beds, couches, and chairs, with little or no recreational activity and social interaction.
As long as a individual has the mindset and determination to continue making life as enjoyable as possible, he or she will more likely to be successful despite the age and the health conditions that come along with it. After all, it’s not how old you are, but rather how old you feel. As far as aging adults are concerned, here are four simple ways in which they can feel young again:
1. HEALTHY DIET
Adopting a healthy diet will allow seniors to stay far away from mental and physical disorders. With age, it’s always good to alter your diet to maintain an optimal level of health. The ideal diet for an aging adult should consist of cooked fruits, vegetables, yogurt, nuts, and small portions of white meat protein or beans. Regular meals consisting of these foods will keep them supplied with sufficient energy and allow them to gain the physical strength required to participate in their favourite indoor and outdoor activities. Unhealthy eating habits also reduces the risk of anxiety disorders and untimely mood swings.
2. KEEPING AN ACTIVE MIND
One of the reasons why seniors feel old is because they lose the excitement and ambition that comes with learning something new and discovering something fascinating. Since most seniors stay detached from the workplace and academic facilities, it becomes difficult to come across new sources of learning. Visiting the public library or participating in a book club can solve this problem. There is no end to learning, and the sooner seniors realise this, the faster they will develop the desire to engage in learning activities. In addition, joining a book club or a library enables a way to get outdoors from the monotony and boredom of retirement life.
3. PHYSICAL EXERCISE
The benefits of physical exercise cannot be stressed enough, especially in the case of seniors. Exercising keeps the body rejuvenated and the mind refreshed. It prevents seniors from being inflicted with a number of different diseases. Heavy workout sessions are not recommended for aging adults. Rather, light exercises such as brisk walking, slow dancing, and stretching (in the form of yoga, perhaps) can help them rise above the physical restraints and limitations that accompany old age.
4. BEING SOCIAL
Surrounding yourself with people of similar ages and backgrounds is one of the easiest ways to make oneself feel youthful. It’s important for seniors to refrain isolation within the four walls of their house as they are simply asking mental and physical illnesses to set in. The more they communicate and socialise, the easier it will be for them to tackle the hardships of aging.
The saying goes “age is only a number”. We like to think of age as a perception of who we are. The key to remember is there is more to gain from life and give back to it. Having this positive attitude will help maintain a youthful outlook.
The Importance of Nutrition: Supporting the Transition from Hospital to Home
There is no denying that a healthy diet is vital to our overall health. Particularly after a hospital stay, proper nutrition is incredibly important during the healing process and can often be a key factor in preventing patients and our loved ones from returning to the hospital in the future.
Many patients experience nutrition deterioration throughout their hospital stay – even those whose nutritional status is adequate upon admission. Malnutrition is a debilitating and highly prevalent condition in the acute hospital setting. Local and international studies have reported malnutrition rates in hospital patients to be approximately 35 per cent, with 30-55 per cent of patients entering acute hospitals being at risk of malnutrition.1
What is malnutrition and its consequences?
Malnutrition is a broad term that can be used to describe any imbalance in nutrition; whether that’s considered over-nutrition, often seen in many developing countries, or under-nutrition, common in developing countries.
Malnutrition is also common in hospitals and residential care facilities even in developed countries, often due to a deficiency in dietary intake, increased requirements associated with a disease state, or from complications of an underlying illness such as poor absorption and excessive nutrient losses.
Malnutrition is associated with negative outcomes for patients, including higher infection and complication rates, increased muscle loss, impaired wound healing, longer length of hospital stays, and increased morbidity and mortality.
Not surprisingly, studies have shown that malnourished adult inpatients have a higher likelihood of hospital readmissions within 30 days than those who are well-nourished.2

Malnutrition has often been referred to as the “skeleton in the hospital closet” as it is often overlooked, undiagnosed and untreated. Most of the adverse effects on patients and the healthcare system can be prevented or improved through nutrition care – care that is essential during hospital stays to improve short-term treatment outcomes.
However, research has revealed that it is just as important, as part of effective discharge planning, to provide support, including meal support to patients who need them. Supporting patients with easy and convenient access to ready-made meal solutions can significantly impact both short-term recovery results and the long-term health of patients.
Supporting the transition from hospital to home Individuals’ nutritional needs don’t stop once they’re discharged from the hospital. In fact, adequate food intake is critical for promoting continued recovery and independence at home. It is especially key for patients suffering from a chronic condition that puts them at risk for malnutrition. Patients with chronic conditions like obesity, diabetes, or heart disease may require a low sugar, fat, sodium, or cholesterol diet.
Older adults who have been discharged from hospital do not always have guidance and follow-up on how to get proper nutrition. Even if the patient doesn’t come home with a special diet, it’s especially important to pay attention to nutrition at this time. With the right nutrition, healing, rehabilitation, and recovery can happen faster, decreasing the chance of readmission to hospital.
Providing patients with ready-made meal solutions post discharge to support their transition from hospital to home are equally important to individuals who cannot prepare meals for themselves, whose caregivers don’t know how to fulfill their nutritional needs, and for those who are food insecure. Furthermore, many times a newly discharged patient returns home to an empty refrigerator and empty cupboards, consequentially having no healthy food to help the body regenerate after the hospital stay.
Studies have shown that the convenience of ready-made, home-delivered meals can increase both diet quality and nutrient intake.3 This offers significant advantages to both the patient and the health service in terms of improved nutritional outcomes and decreased hospital readmissions.
The Good Meal Company
At The Good Meal Company, we provide ready-made meal solutions and customer service support, designed to help hospitals, community care and NDIS providers, nursing and allied health teams provide their patients and clients with expedited nutrition support at the start of their recovery, when time is of the essence, to support healing and reduce hospital readmissions.
Under the Good Meal Company brand, SPC Care manufactures and delivers a comprehensive range of over 80 pre-prepared meals. These meals are designed to support the nutritional needs of patients and cater to the diverse cultural cuisine preferences. We understand that everyone is different, so we provide a range of meals designed to meet the needs of consumers with special dietary requirements such as gluten free, vegan, vegetarian, dairy free, low GI, and texture modified (level 5 - minced and moist). Carefully developed, our meals are hand prepared and snap frozen to lock in their nutrition and flavour. All meals are manufactured at our state-of-the-art production facility in Sydney.
How to order?
1. Jump online (www.goodmeal.com.au), browse and select your meals. Add 10+ meals to your cart for the week ahead and receive free delivery. No long-term contract is required.
2. Order and pay. Check out online or simply call our friendly team (1800 155 255) to place your order.
3. Meals delivered. The delicious meals will be delivered direct to the home or nominated address on the date and time most suitable for you.
The Good Meal Company provides a dedicated range of pre-prepared, snap frozen meals to healthcare institutions and individuals being cared for at home. Meals are delivered to the patients’ home or nominated address to help them stay healthy throughout their recovery. Delivery is available throughout most states and territories in Australia.
References:
1. Barker LA, Gout BS, Crowe TC. Hospital Malnutrition: Prevalence, Identification and Impact on Patients and the Healthcare System. Int J Environ Res Public Health. 2011 Feb; 8(2): 514–527.
2. Lengfelder L, Mahlke S, Moore L, Zhang X et al. Prevalence and impact of malnutrition on length of stay, readmission, and discharge destination. JPEN. 2022 Aug; 46(6): 1335-1342.
3. Zhu H, An R. Impact of home-delivered meal programs on diet and nutrition among older adults: A review. Nutr Health. 2013 Apr; 22(2): 89-103.
For information on the comprehensive range of ready-made meals available, please visit www.goodmeal.com.au or contact Sarah Donnelly (National Account Manager) on 0490 904 258 for more information.

The Diabetes Kitchen
The Diabetes Kitchen delivers healthy, delicious, nutritionally balanced meals for people living with diabetes all around Australia.
The Diabetes Kitchen’s mission is to make healthy eating easy and accessible for people with diabetes, to help them manage their condition through good nutrition.
Australian owned and operated, The Diabetes Kitchen has been delivering meals since 2014.
Founded by a nutritionist who also manages type 1 diabetes, and an advisory board of dietitians and diabetes educators, The Diabetes Kitchen is adamant about delivering quality meals to help make mealtimes much easier.
A variety of single meals, breakfasts, lunches, desserts, snacks are available with weekly or fortnightly meal plans. Each serving has no added sugars, is carbohydrate controlled and low in saturated fats and salt.
The nutritional value of each meal is clearly indicated with colour coded labels for carbohydrates, sugars, and calories to help make mealtime choices very easy.
About the meals
The meals are pressure-cooked in single serve pouches to lock in maximum nutrition. This cooking method allows the meals to be conveniently stored in the pantry rather than in a fridge or freezer, which makes them ideal for people with limited fridge or freezer space.

Meals are simply reheated in the microwave or stove top for about 90 seconds.
Each meal meets strict nutritional criteria to ensure a healthy and balanced meal that taste delicious every single time.
The Diabetes Kitchen ensures that each meal:
• provides an average of 300 calories per serve
• contains no added sugar at all
• ranges between 4g–40g carbohydrate per serve
• ranges between 0g–6.3g saturated fat per serve
• provides at least three serves of vegetables/legumes
• is free from artificial colours or flavours.
At a generous 350gm per serve they are ideal for one person, and with the addition of steamed vegetables or basmati rice, they make a very tasty and healthy smaller meal for two people.

All meals are designed by a nutritionist in conjunction with a food technologist. The ingredients are sourced from local Australian suppliers and the preparation takes place in a state-of-the-art HACCP approved kitchen facility.
Pressure cooked casseroles, hot pots and curries are available and the meat and vegetables in the delicious and extremely nutritious liquid are cut small to make them ideal for people who have difficulty chewing or swallowing large pieces of food.
With gluten free, lactose free and vegetarian options, there is something to suit most people.
Aged care and diabetes
An estimated 33 per cent of adults aged 65 or older have diabetes. In 2020, the prevalence of diabetes increased with age with almost one in five Australians aged 80–84 living with diabetes – almost 30 times as high as for those aged under 40.
The figures are likely to underestimate the true prevalence of diabetes in the Australian population. This is because they are based on people who have received a formal medical diagnosis of diabetes. However, Australian studies have shown that many people are living with undiagnosed type 2 diabetes.
Providing nutritious meals for seniors in aged care facilities can be a challenge. The Diabetes Kitchen’s team of diabetes experts has spent years developing a range of meals that meet the specific needs of seniors, managing diabetes.
We believe that the quality of the food we eat directly affects our health and well-being. This is especially true for seniors, who may be more vulnerable to health issues due to their age and other medical conditions. By providing healthy meals to seniors in aged care facilities, we believe this makes a positive impact on their health and overall quality of life.
Meals are easy to store, and they have a long shelf life of 12 months. This makes them a convenient option for busy aged care facilities. Meals are simply reheated in the microwave or on the stovetop and served.
There are no contracts required, and The Diabetes Kitchen offers a discount based on volume for meals provided to aged care facilities.
Seniors living at home receive a five per cent discount when ordering which can be done by phone or website.
The Diabetes Kitchen also works with plan managers and can invoice them directly for their participant’s meals.
The Diabetes Kitchen’s website features a blog with helpful tips and advice on managing diabetes, as well as a Facebook forum where customers can connect and share their experiences.
The Diabetes Kitchen is NDIS approved which means NDIS participants pay for ingredients only (approximately $2.50), and NDIS pays the balance.

The Diabetes Kitchen offers excellent, super convenient options for people living at home, or in an aged care facility, who are managing diabetes, and still want to enjoy healthy, delicious meals without the hassle of cooking and meal planning.
For more information:
www.thediabeteskitchen.com.au

Phone: 1300 79 89 08
Email: info@diabetesmealsonline.com.au
THE DIABETES KITCHEN

delivering nutritionist-designed, carb controlled ready-meals Australia wide.


Hot Pots, Casseroles and Curries

Breakfast, lunch & dinners
Meal plans, desserts and snacks
Pressure cooked in the pouch for maximum nutrition. Store in pantry and reheat microwave/stove top.
Convenient, delicious and healthy.
Minimum 3 servings of veg in each, no artificial colours or flavours
Mitsubishi Electric comfort solutions









» Our range of advanced HVAC & Air Treatment products are designed to keep your valued residents comfortable all year round.
» With advance central control options, you can manage your indoor comfort and energy consumption throughout your facility.







Outdoor Cooling Solutions: Improve Aged Care Center Comfort with a Youmist System

Is your aged care centre struggling to provide a comfortable outdoor space for your residents and staff during Australia's scorching summers? Look no further! Youmist is your one-stop solution for designing, supplying, and installing high-pressure misting systems to transform your outdoor areas into cool, refreshing havens.
Benefits of High-Pressure Misting Systems for Aged Care Centres:


Enhanced Comfort and Pest Control: High-pressure misting systems create a comfortable outdoor environment for your residents and staff to enjoy while also helping to prevent flies and insects from invading the space. The fine mist evaporates quickly, reducing ambient temperatures by up to 10°C without soaking the surrounding areas. This allows your residents to relax, socialize and participate in outdoor activities without discomfort or the annoyance of pests.
Improved Health and Well-being: Studies have shown that spending time outdoors can significantly improve the mental and physical well-being of aged care residents. Our misting systems enable your residents to spend more time outside, helping to reduce feelings of isolation and improve their overall quality of life. By providing a comfortable outdoor space, you can encourage social interaction, physical activity, and mental stimulation, all crucial for the well-being of your residents.
Increase Property Value and Aesthetic Appeal: Installing a high-pressure misting system not only makes your facility more comfortable but also adds value to your property. A well-designed, efficient outdoor cooling system is an attractive feature for potential residents and their families, setting your aged care centre apart from the competition. Additionally, the misting system adds a touch of elegance to your outdoor spaces, enhancing their visual appeal.
Energy Efficiency: Our high-pressure misting systems are designed to consume minimal energy, ensuring that your facility remains environmentally friendly and costeffective. In addition, our systems are low maintenance, ensuring hassle-free operation and longevity.
Why Choose Youmist?


Expertise: With years of experience in the industry, Youmist is a leading provider of high-pressure misting systems across Australia. Our skilled professionals ensure that each project is customised to meet the unique requirements of aged care centres. We pride ourselves on delivering reliable and efficient cooling solutions for a wide range of facilities.
Comprehensive Solutions : At Youmist, we take care of everything from the initial consultation and design to the supply and installation of the misting system. This end-to-end service means that you can focus on providing excellent care for your residents while we handle the cooling solutions. Our commitment to customer satisfaction ensures a seamless experience throughout the entire process.
Advanced Technology: Youmist utilizes state-of-the-art technology in designing and installing misting systems. Our high-pressure pumps, nozzles, and other components ensure the finest mist particles for rapid evaporation and maximum cooling efficiency. We stay ahead of industry trends and continuously improve our products and services to deliver the best solutions for your facility.
Customisation and Scalability: At Youmist, we understand that each aged care facility is unique. Our team works closely with you to design a misting system that fits your specific needs, ensuring that your outdoor spaces are cooled efficiently and effectively. Our systems are scalable, allowing you to expand or modify the setup as your facility grows or its needs.
Safety and Compliance: Safety is our top priority at Youmist. All our misting systems are designed and installed in compliance with Australian safety standards, giving you peace of mind that your residents and staff are protected.
Don’t let the heat compromise the comfort and wellbeing of your aged care residents. Trust Youmist to deliver a high-quality, energy-efficient misting system tailored to your facility's needs. Get in touch with our expert team today to discuss how we can help you create an inviting outdoor space that your residents will love.

How A Youmist System Keeps You Cool

The secret to our outdoor comfort lies in the science behind evaporative cooling. A youmist system usually consists of a series of tubing and nozzles placed around the perimeter of an outdoor space.


A high-pressure pump is connected to the water source, which increases the water pressure by up to 15x its normal flow rate. By increasing the water pressure above 1000 psi, the water molecules are atomized, pushing the smallest possible droplets through the nozzles.


As the water droplets are introduced to the hot outside air, they flash evaporate. The process of evaporation requires a source of energy: in this case, the hot air molecules. When the air molecules disburse energy to evaporate the water droplets they begin to cool.
This process is repeated for each droplet and, as the misting system continues to spray, the surrounding air can be cooled by more than 10 degrees Celsius.
Providing homes, businesses and outdoor play areas with an innovative misting system to dramatically decrease room temperatures!
Even mild COVID raises the chance of heart attack and stroke. What to know about the risks ahead
A concerning report recently published in Nature Medicine suggests even a mild case of COVID can increase the long-term risks of serious cardiovascular diseases such as stroke, heart attack and heart failure. The study highlights our limited understanding of the full consequences of COVID infection and the long-term impact of the COVID pandemic.

Australia has now reported more than 10 million cases of acute COVID infection and more than 14,000 deaths, with at least 600 million more people infected worldwide.

The immediate effects of COVID infection on the heart have been well documented, with myocarditis (inflammation of the heart muscle) an infrequent but potentially lethal complication. But myocarditis only occurs in about 40 people per million infected.
The big concern raised by this fresh study is that medium- to long-term harms on the body’s blood vessel network (the vascular system) may be much more common than that. And it could drive a new pandemic of cardiovascular disease over the coming years.
What they found
The study, led by researchers at Washington University, showed a heightened risk of future cardiovascular events among people who have recovered from COVID.
The authors analysed the health records of around 150,000 US veterans, who are often studied because they are a well-documented group within a discrete health-care system. They compared the rates of cardiovascular disease in veterans who’d experienced a COVID infection against uninfected control groups that included some 10 million people.
Between 30 days and a year after recovery from COVID, survivors were 52 per cent more likely to have a stroke, 63 per cent more likely to have a heart attack, and 72 per cent more likely to develop heart failure. This means that over one year, for every 1,000 people who had COVID, there would be five extra strokes, three
extra heart attacks and 12 extra cases of heart failure. There was also evidence of an increased risk of serious blood clots on the lungs.
While these numbers might sound small to some, when scaled to 600 million COVID infections worldwide, the implications are enormous.
One particularly concerning finding was that while those with more severe acute COVID infections had the highest risk of a cardiovascular events over the following year, even those with a mild infection were at increased risk. And that risk was not restricted to those who’d had heart health problems before – it could affect anyone.
Necessary cautions
The study was large and had many strengths. But the findings must be reviewed with a degree of caution. It was an observational study (in which researchers draw inferences from what they see in a population, rather than control variables for an experimental study). So, we can’t be certain the increased risk of heart disease or stroke was definitely caused by the COVID infection. The people infected with COVID were not identical to the people who were uninfected.
That said, the researchers made statistical adjustments and could not identify another explanation for the large increases in risks seen.
It is also likely some people with asymptomatic COVID infection were accidentally included in the control groups. However, the effect of this would have been to underestimate the risks of COVID infection on cardiovascular risk.
And of course, US veterans are a very particular set of individuals (mostly older, male and white). Even if the effects of COVID on cardiovascular risk are real for them, there must be some uncertainty about whether the same effects would be seen in other populations.
COVID and hearts
The clear, but low, risk of heart disease at the time of COVID infection also provides support for a connection between COVID infection and medium- to long-term heart disease.
Even before the COVID pandemic there was a wellestablished link between the inflammation caused by infection and the risk of heart attack.
A heart attack occurs when an artery supplying blood to the heart is blocked and the heart muscle is starved of oxygen. This usually happens when rupture of a fatty plaque in the artery causes a blood clot to form. This process is driven by inflammation in the tissues and thickening of the blood, both of which can occur with COVID, and both of which can persist long after the initial infection has resolved.
These data remind us once again of the importance of limiting the spread of the SARS-CoV-2 virus. The best way to reduce COVID-related risks is to prevent COVID infection and reduce the severity of infection. We must maintain high vaccination rates and support infection control measures such as mask wearing in high-risk situations. Ever stronger evidence of the long-term effects of COVID redoubles the importance of these efforts.
Future problems
We rightly feared the respiratory complications of COVID throughout 2020 and 2021 but only now are we appreciating the full impact of the pandemic across other body systems.
Doctors will need to view COVID infection as a new long-term risk factor for cardiovascular disease in much the same way that many other chronic inflammatory conditions such as rheumatoid arthritis are viewed now. We should advocate for fair access to heart disease prevention and treatment in all Australians, particularly those at highest risk such as First Nations people. And most importantly, as patients, we must prioritise our own heart health.
And we’ll need to remain vigilant for the effects of new strains. Over the decades to come we’ll need to plan for the enduring effects of COVID.
Authors Clare Arnott Co-Director of Global Chronic and Complex Diseases, George Institute for Global Health NealBruce
Executive
Jamie
Director,George Institute Australia, George Institute for Global Health
ChamLecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ even-mild-covid-raises-the-chance-of-heart-attack-and-stroke-what-toknow-about-the-risks-ahead-190552
Older people who get lost sometimes sadly lose their lives, but those with dementia are more likely to survive
Being lost in an unfamiliar place is an unsettling feeling most of us have experienced. It requires cognitive and physical skills, and potentially other resources, to find our way and safely arrive at our destination.

This is why up to 60 per cent of people with dementia will experience becoming lost during the course of living with the disease.
We’ve conducted a study of search and rescue incidents in the United States, and found people over the age of 65 years who go missing will experience (sometimes fatal) harm more than we expected. However, the results for older people with dementia were surprising and counterintuitive.
What we know about older people and becoming lost
Older people (those over 65) are more vulnerable to becoming lost. Age-related declines in physical and cognitive function impact our ability to navigate and endure the environment, and seek assistance.
Becoming lost is very distressing for both the lost person and for their loved ones. People with dementia are at increased risk of becoming lost due to memory problems, loss of judgement, and reduced visual-perceptual ability (they might forget landmarks, become confused about direction, or not recognise places). Frailty and increased risk of disease as we age mean the risk of sustaining an injury, possibly a fatal injury, increases for older people.
What our study found
Our study examined incident reports of older people who became lost in the US, and had the matter reported to police or directly to a search and rescue team. We looked at 1703 incidents that required a search-andrescue operation to locate the person. We used US data because it was more extensive and detailed than what we have in Australia.
Of the 1703 cases, 208 (12 per cent) were found dead. This was more than we expected, but exact numbers of deaths are hard to predict, since some people will also die due to injury after being found, and some are found quickly before the police are called.
We found death was more likely in situations where there were water-related activities (such as boating and fishing), cold weather conditions (drizzle, rain, snow), and among males. And for those who didn’t survive, they were more likely to be found in water or wetlands compared to the people found alive.
Importantly, for those who didn’t survive, the time taken to notify search and rescue teams was three times longer. The search time was six times longer. Interestingly, people with dementia were more likely to be found alive than those without dementia.
Why were people with dementia more likely to survive?
While it seems a counterintuitive finding, the explanation for why those with dementia fared better may be in our approach to care, and the rescue methods applied for older people with dementia.
Caregivers for people with dementia may be using technological tracking devices or locking doors more regularly to prevent the older person with dementia from leaving their home.
It’s also plausible the greater concerns for the safety and wellbeing of people with dementia may be an impetus for caregivers to notify search and rescue teams earlier, compared to when a person without dementia is noticed missing.
Alternatively, it may also reflect the strategies employed by search and rescue teams. Searches for lost people with dementia are often prioritised and given the highest urgency by search and rescue teams.
This focus on people with dementia may overlook other older people in need of interventions. We may not feel the same level of urgency, or even recognise there’s real risk of harm to people without dementia.
What do the findings mean?
This study, while focused on the US, would likely be transferable to countries with similar search and rescue authorities, climates, and terrain. Certainly, countries such as Australia, New Zealand and the US can learn from each other and are known to share search and rescue information with the aim to improve search efforts.

It’s a stark reminder we need to focus on all older people, and not limit our focus to one population group. If a loved one is noticed missing, it’s important to contact police early. The longer a person is missing, the greater their risk of death.
For people with dementia, families should consider the use of personal tracking devices such as GPS smart watches or tags. This intervention can help locate the person quickly, and also respects their right to freedom of movement.
Often, people are found within close proximity of the place they were last seen, and so searching in places nearby may be effective. Finally, understand the dangers of waterrelated activities. This danger extends to all older people with and without dementia. Ensuring the family knows when and where an older person is visiting the water, and wearing tracking devices may just save a life.
Authors Marta Woolford PhD Candidate and Research Officer at the Department of Forensic Medicine, Monash University Joseph Ibrahim Professor, Health Law and Ageing Research Unit, Department of Forensic Medicine, Monash UniversityThis article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ older-people-who-get-lost-sometimes-sadly-lose-their-lives-but-thosewith-dementia-are-more-likely-to-survive-192938
The dreaded ‘D’ word: The search for a cure to prevent or delay dementia
If there’s one dreaded word uttered by doctors to rival “cancer”, it’s “dementia”. Patients the world over fear its impacts – the lack of independence; the higher likelihood of ending up in a nursing home. As with cancer, there’s currently no “cure” for dementia.

But the prognosis isn’t entirely bleak. It’s now becoming more apparent we may be able to prevent or delay the onset of dementia symptoms by living more healthily in our earlier years.
An often forgotten and more pressing need is how do we care for people living with dementia? Doing so will require investment both now and into the future.
Meanwhile, a large section of the scientific community is squarely focused on the search for effective treatments. Millions of dollars have been invested over the past three decades in search of a “holy grail”. This, despite the reality that dementia is a complex condition, an enigma to researchers.
For two important reasons, dementia cannot be “fixed” quickly and with great effectiveness – like a heart attack or angina is with a stent, or like some cancers can be with surgery. First, it’s a cumulative condition with multiple causes that impact on the brain at various times during a person’s lifespan. Second, dementia creeps up on a person, with changes in the brain beginning decades before a person actually starts to show symptoms.
For most people, there’s not a single cause behind their dementia symptoms, at least for the commonly
seen progressive loss of memory and other functions in older age. In fact, some of the most comprehensive autopsy studies conducted in large populations find the majority of people dying with dementia show a variety of different types of brain changes, probably occurring over a few decades.
Not only is there a build-up of proteins in the brain called amyloid and tau that are traditionally regarded as markers of Alzheimer’s disease, but also changes seen in other conditions such as Parkinson’s disease, and importantly, evidence of damage from poor cardiovascular health such as strokes.
There are several things people and governments can do to drive down symptoms of dementia and “flatten the curve” of dementia in whole populations. People are more likely to show symptoms of dementia during life if they have a combination of these brain changes rather than just one of them, suggesting that a little of each may add up over time.
Many of these brain changes occur silently and at various times during a person’s lifespan, and at varying rates in different people. There comes a point when the brain’s ability to function well becomes compromised, and this is when the first symptoms occur.
This is why there’s no one “thing” we can blame for causing dementia, and why it’s so hard to find that silver bullet to stop dementia – particularly at older ages.
Even benefits of the handful of medications developed for dementia are, at best, very small and debatable. They’re also not easily available for a large section of the global community.
The prescription of the newest, and most hotly-contested medication for people with early dementia requires a highly specialised brain scan not available to the majority of people in high-income countries, let alone for those in middle and low-income countries.
How can we reduce the burden
A logical question that follows is, what can be done about reducing the burden of dementia?
The answer is in fact, quite a lot.
There are several things people and governments can do to drive down symptoms of dementia and “flatten the curve” of dementia in whole populations.

For the general public, this means promotion of healthy diets and physical activity. For people with risk factors such as high blood pressure, diabetes, heart rhythm abnormalities, and high cholesterol, good management of cardiovascular health is required.
In high-income populations, there’s evidence of a reducing incidence of new cases, most likely due to the benefits of improvements in lifestyle and cardiovascular health over the past three decades.
Education, health literacy is key
The challenge is translating this to middle and low-income countries with larger, more diverse populations where the burden of dementia is fast increasing. Education and health literacy is a key element of protection against dementia, a measure that requires investment.
But the elephant in the room is the serious lack of investment to support people already living with dementia. Removing the stigma related to dementia, and improving environments, access to care, connectedness to communities, and health services should be supported by investment, research effort and actions equal to, if not greater than, the resources directed towards the finding of a magic cure.
Author Velandai Srikanth Professor, Peninsula Clinical School, Director, National Centre for Healthy AgeingThis article was first published in Monash Lens. Read the original article here: lens.monash.edu/@medicine-health/2022/01/19/1384262/ the-search-for-a-cure-to-prevent-or-delay-dementia
How can we meet the needs of older adults with epilepsy?
Older age is now the most common time to develop epilepsy in highincome settings, and an evidence review led by a Monash research team has highlighted that older adults are at risk of new-onset seizures due to age-related changes.

The research paper is published in Epilepsia journal, and the first author Dr Loretta Piccenna is from Monash University’s Department of Neuroscience.
Dr Piccenna says the findings highlight that epilepsy's "treatment pardigm" needs to be extended, with more emphasis on older people.Developing epilepsy at this stage of life has substantial impacts on patients’ lives, she says.
For example, they can lose confidence, suffer side-effects from treatment, lose a driving licence or independence, and in some cases might even need to move into residential care for care and support.
“We need to provide an evidence-based and personalised, integrated model of care, making changes when older adults transition from well-functioning to poorfunctioning, to focus on long-term patient-centred outcomes such as quality of life,” Dr Piccenna says. “In particular, a challenge is when older adults have a first seizure and develop epilepsy in residential aged care where there are unclear protocols, or no protocols.
“Without specialised epileptologists in residential aged care, chaos or lack of knowledge leads to inappropriate levels of management when trained staff with treatment plans can prevent emergency transportation to a hospital.”
Closer integration sorely needed
The special report found that a closer integration between primary and secondary care with multidisciplinary experts working together is a much-needed approach to improve care.
But it can be confusing to know which health professionals – GPs, geriatricians or neurologists – should be managing
these patients. Rationalising the number of specialists an older person sees without compromising the expert care needed therefore becomes a conundrum.
Researchers searched the literature to map out the types of studies published over five years. These were clinical studies (other than randomised controlled trials), narrative reviews, systematic reviews and/or metaanalyses, and randomised controlled trials.
Evidence from systematic reviews didn’t reveal any existing medications as being more effective in controlling seizures over any others.
There’s a lack of studies for the newer-generation antiseizure medications, in particular appropriate dosing regarding comorbid health conditions and sensitivity to adverse effects. Currently, the “ideal” anti-seizure medication doesn’t exist.
Taking a global approach
The International League Against Epilepsy (ILAE) is a professional association for healthcare professionals and scientists with a focus on epilepsy. To help global efforts in the area, committees, task forces and commissions have been developed.
Its Epilepsy in the Elderly Task Force of the Medical Therapies Commission has an overall goal to examine this topic and recommend how the ILAE can help move forward, with a global or international perspective.

Dr Rebecca O’Dwyer and Dr Ilo Leppik, expert epileptologists from the US, and part of the task force reporting to the commission, also contributed to the special report.
In Australia, Professor Patrick Kwan, the corresponding author of the paper, a member of the ILAE task force, and
researcher in Monash’s Department of Neuroscience, says older adults with epilepsy are a distinct group.
“They require a concerted effort across disciplines for optimal care,” he says.
The next steps to take
Several recommendations were identified by the members of the task force in this special report for the ILAE to take on board.
We’d like to highlight two particular areas of focus –prioritising high-level evidence research and supporting funding for older adults with epilepsy, and an innovative optimal treatment approach that’s specialised, holistic, and patient-centred.
We want to promote a greater focus on building the evidence with rigorous clinical trials.
We believe these clinical trials should use greater distinction in the participant demographics and numbers of older adult participants, and participants in residential aged care and community cohorts.
A greater continuum of care through the integration of primary and secondary care is the desired model of care, one that moves beyond seizure control to long-term patient-centred outcomes.
Author Loretta Piccenna Research Manager, Department of NeuroscienceThis article was first published in Monash Lens. Read the original article here: lens.monash.edu/@medicine-health/2022/12/15/1385352/ how-can-we-meet-the-needs-of-older-adults-with-epilepsy
The question of conscientious objection in the voluntary assisted dying debate
Voluntary assisted dying (VAD) has been legal in countries such as Switzerland and the Netherlands for more than a decade.

In Australia, aside from a brief introduction by the Northern Territory in 1995 that was quickly overruled by conflicting federal legislation, VAD remained illegal in every Australian jurisdiction until 2017.
In 2017, Victoria took the lead, enacting the Voluntary Assisted Dying Act 2017 (Vic). In 2019, Western Australia followed suit, and in 2021 VAD became legal in Tasmania, South Australia and Queensland.
On 19 May 2022, the NSW Parliament passed the Voluntary Assisted Dying Bill. In doing so, NSW became the final Australian state to legalise VAD.
In his second reading speech, Alex Greenwich (the MP who introduced the bill) noted that:
“The bill will create a safe framework for people who are in the final stages of a terminal illness, and who are experiencing cruel suffering that cannot be relieved by treatment or palliative care, to be provided with the choice to die peacefully, with dignity and surrounded by loved ones.”
As this statement suggests, VAD legislation is also sometimes referred to as dying with dignity legislation, because it enables an unwell person to choose the time and place of their death.
VAD has been described as involving “a physician prescribing medication to a patient with the explicit intention of causing premature death”.
Accordingly, across the country, self-administration is the predominant mechanism by which VAD is carried out. Physician-administered VAD is rare, and only occurs where a patient is unable to self-administer.
Attitudes to VAD among health professionals
VAD is a polarising issue in the healthcare sector; it’s literally about life and death, and elicits passionate and emotional responses in both the medical community and the general community.
Some people regard VAD as a human right, inherent in fundamental rights such as the right to dignity, autonomy and self-determination.
Others express concern that a doctor’s key ethical commitment is to do no harm, and on this basis doctors should not play a role in hastening a person’s death. They also worry about whether the safeguards in place are adequate to prevent undue influence or coercion.
A high proportion of the Australian population supports VAD. For example, a “recent survey carried out by the NSW Council on the Ageing found that 72 per cent of people over 50 in NSW were in favour of legalising voluntary assisted dying”. That said, many health professionals remain uncomfortable participating in VAD.

All Australian states allow a health professional with a conscientious objection to refrain from participating in VAD. As in all other states, the NSW law will allow a health practitioner to refuse to participate in VAD.
This is similar to abortion legislation, which across Australia also includes provision for conscientious objection.
States’ laws not all the same It’s worth noting that while all Australian states allow for conscientious objection, the laws between the states are framed slightly differently.
For example, both Victoria and Tasmania allow an unmitigated form of conscientious objection, with no requirement to provide information to a patient who raises the question of VAD; Western Australia requires the provision of an information booklet; and Queensland requires doctors to direct the patient to someone without a conscientious objection.
Attitudes towards VAD among health professionals aren’t binary, but rather tend to sit on a spectrum. Unfortunately, there’s a lack of accurate, comprehensive data capturing the rates of conscientious objection to VAD among health professionals in Australia.
However, the research that has been conducted suggests rates of conscientious objection to VAD are reasonably high among the cohort of medical practitioners whose patients are most likely to seek access.
For example, in a survey conducted by the Medical Oncology Group of Australia, out of the 362 respondents, 47 per cent disagreed with voluntary assisted dying. Similarly, in a survey of the Australian and New Zealand Society for Geriatric Medicine, out of the 226 respondents, 53 per cent opposed VAD.
There’s a range of reasons why practitioners object to participating in VAD. Interestingly, unlike in the abortion context, it seems the majority of health professionals who object to VAD do so for “reasons that could be regarded as secular, humanist or professional” rather than for religious reasons.
The way forward for VAD legislation
There’s a global trend towards the legalisation of VAD. For example, the past decade has seen the legalisation of VAD in Canada and New Zealand, two countries culturally similar to Australia.
It seems, therefore, that VAD is here to stay, but that– as has occurred in the context of the decriminalisation of abortion – there’s likely to be some tinkering with the legislation in the different jurisdictions.
In time, we may see greater harmonisation between states. Further, it seems that it’s only a matter of time until the federal government repeals its own legislation that prevents the territories from legalising VAD.
A society is measured by how it treats its most vulnerable, such as those who are sick and approaching the end of their lives – “I'm not interested in whether you've stood with the great; I'm interested in whether you've sat with the broken”.
Whether a person does or doesn’t support VAD, I think we can all agree that treating people with respect and dignity at the end of their lives is of paramount importance.
As a society, we need to strike an appropriate balance between respecting the right to freedom of conscience, and securing the rights of individual patients to dignity, privacy and autonomy.
This isn’t an easy conversation, but it’s one we must have.
Author: Ronli Sifris, Senior Lecturer, Faculty of Law, Deputy Director, Castan Centre for Human Rights LawThis article was first published in Monash Lens. Read the original article here: lens.monash.edu/@politics-society/2022/05/20/1384719/the-questionof-conscientious-objection-in-the-voluntary-assisted-dying-debate
The Benefits of Memorialisation & Prepaying a Memorial
Anyone who has experienced the grief of losing a loved one understands there are poignant moments when you yearn to be in their presence once again. Having a special place where you can relive cherished memories helps bridge the voyage between life and death. As we age, it is natural that we start to think about where our ideal resting place might be when our own time comes.
Why Prearrange Your Memorial?
Prepaying your memorial can give peace of mind to those you leave behind. When you make your wishes clear in advance, you may avoid confusion later at an emotional time. Arranging your memorial also provides a tangible place for friends and family to reflect upon the impact you made on their lives. Here are some insights and steps you can take to create a lasting tribute to a life well-lived.
The Importance of Memorialisation
Physical memorials are a permanent record of individual lives and are as much for the living as for the deceased. Just as in life, in death, it is important to consider the thoughts and feelings of your loved ones. Acknowledging that future generations may wonder about their place in history is also something to think about. An actual marker in a beautiful, serene location that friends and family can visit regularly helps heal the loss and preserve memories and traditions.
Things to Consider
Your memorial should be a harmonious place for loved ones to reflect on the moments you shared together - a sanctuary where they can laugh and cry or hold a one-sided conversation without embarrassment, knowing their dignity will be respected. It may be a place where they can commemorate birthdays and anniversaries. Some memorials may honour war heroes, often uniting the descendants of those who risked their lives to defend their nation. Other memorials reflect the personal religion or culture of the deceased. Choosing the location where you would like to rest for eternity is an important decision that requires thought and deliberation.
Practical Concerns
Organising your memorial yourself ensures that your specific
instructions will be carried out and relieves loved ones of the burden of having to make critical decisions at a stressful time. Would you like to be buried in a coffin? Or would you prefer to be cremated? While scattering your ashes in a significant area such as a park or bushland may sound romantic, in the future, your special place could develop into a shopping centre or become off-limits in a private housing estate. Arranging to have your memorial in an enduring place of remembrance guarantees that your loved ones will always have a haven where they can celebrate your life.
Prepurchasing your memorial is also prudent financially and helps your family by locking in current pricing and avoiding inflation. Since you are investing money to cover costs for an uncertain date in the future, it is critical that you choose a trusted sanctuary that will be maintained in perpetuity.
lnvoCare Memorial Parks and
Gardens
InvoCare operates 15 cemeteries and crematoria in New South Wales and Queensland. Each property managed by InvoCare Memorial Parks and Gardens is an oasis of serenity, rich with natural beauty and landscaped grounds maintained by a caring staff. Many locations have deep historical and cultural connections to the communities they serve, with bonds that stretch back to the 1920s. InvoCare is dedicated to preserving the distinct essence of each individual and provides a wide assortment of memorials that reflect your personal values and traditions, whether it be a simple lawn plot, a living rose garden or an estate that can accommodate your entire family.
lnvoCare Memorial Parks and Gardens strives to ensure that your loved ones will always have a welcoming place for reflection that offers comfort, beauty and serenity. Take a moment to reserve your memorial so you can rest in peace.
Courtesy of Invocare


We shall remember: The many reasons for a funeral
Since time began, all cultures have created rituals to honour their dead – they know we have an intrinsic need to acknowledge what the person meant to those left behind, and the value and healing offered in being able to say goodbye, even in the simplest form.
Today, however, with our fast-paced lifestyles it can be difficult to grieve well. We feel like we must “be strong” for others, whether it be our family members, co-workers, or even strangers, and we live in a world that encourages us to hide our pain and appear like we’ve “got it all together.”
Our minds rebel against the idea of anyone seeing how deeply affected we are, how not okay we feel inside, but as I have come to know, expressing our grief is the first step on the road to healing.
Love and grief are two sides of the same coin. One does not – and cannot – exist without the other. People
sometimes say that grief is the price we pay for the joy of having loved. It is predicated on our capacity to give and receive love, and if we allow ourselves the grace that comes with love, we must allow ourselves the grace that is required to mourn.
What should be remembered however, is that when someone dies, the farewell process is not for them, it’s about them. Family members and friends must acknowledge and honour their memories before they can move forward in their grief, and the funeral is often the first step for everyone who knew, loved and was connected to that person.
One of the purposes of a funeral is to help those left behind accept the reality of the death. In order to heal and grieve, we must first accept what has happened. And at a healing and meaningful funeral, mourners have the chance to confront reality and begin processing their grief. The funeral is not the end of the grief journey – it is the beginning of accepting a new reality – one without the loved one.
Researchers and psychologists are very clear in their message about funerals and grief – funerals underpin a necessary part of grieving. A funeral provides a safe and appropriate place to show and share one’s feelings with others.
The reality is this – you cannot avoid grief just because you don’t want to experience it, or you don’t want others to see you upset. As human beings, we need to grieve. Farewells of any sort are legitimately an emotional time, so why shouldn't we be upset when we are never going to see each other again? A meaningful funeral can help us say: Thank you. I love you. I'm lonely without you. I’ll always remember you. You meant a lot to me.
And one of the most important aspects of preparing for a meaningful funeral is selecting the right funeral director.
Funeral directors have always been deeply valued and esteemed members of their communities, and while the important work they perform can sometimes be

“Grieving doesn’t make you imperfect. It makes you human” – Sarah Dessen
misunderstood, feared, or even overlooked — that does not mean it’s insignificant.
While providing a vital service, the role is not an easy one. The job can be physically and mentally taxing. Death doesn’t work office hours, and there is often little room for downtime. That means less personal time, less family time. To be a funeral director is to be selfless.
Funeral directors often see the worst. They help mothers and fathers who have lost a child. They work with siblings that have laid a parent to rest and comfort a community in shock over an unexpected death or suicide. They mourn with every family.
But they also see the best. They bear witness to the depth of love and emotion daily, bring comfort and reassurance to grieving families and even help to provide a modicum of closure.
At this time, people want more than personalisation and more than tradition, people want understanding and guidance. Losing a loved one is a difficult process, and the funeral director serves both as a steward of the living, guiding them through the array of choices and decisions, as well as being the coordinator of the final services of the deceased.

Providing insight, comfort, and compassion, the funeral director is a master of both modernity and tradition, painstakingly setting each little detail for a service because each detail matters. They are storytellers in what will be a person’s final chapter.
They understand that by putting our thoughts and feelings into action, we begin the journey toward healing.
By recalling and sharing details about our relationship with a loved one, we help ourselves transition. We begin the process of moving our relationship with the one who has died to one of memory rather than presence.
Preparing or listening to a eulogy, viewing the tribute video (if there is one), finding solace in the songs or readings chosen, as well as finding support in the gathering of friends and family following the service can help immensely with the grieving process. Not only does this celebrate the life of the deceased, but it also allows attendees to discuss memories associated with that person.
At a funeral, we can share our memories, give voice to our feelings, and find support in others. When a funeral includes a visitation or a gathering, mourners also have the opportunity to come together and offer a listening ear and a caring hug.
Sometimes, the most important part of having a funeral service is the companionship it provides to those who need it most. Funerals are a venue for people to express their pain and sadness at the loss of someone in their lives. Being able to communicate and share that grief with others can be powerful for the healing process. Not only can funeral attendees share and acknowledge their feelings with the people around them, they also provide a safe and accepting space for people to outwardly express these strong emotions.
Without a funeral, people often don’t know if it’s alright to contact you or to bring up the subject of what’s happened. The funeral is seen as the ‘right’ time and the ‘right’ place to approach you and to offer their support to you. Friends have a need to reach out to those grieving
and say: I'm here for you. Having this kind of support is vital in the weeks and months after the funeral when the reality of the loss really starts to sink in, and we must adapt to a life without someone who mattered to us.
The final purpose of a funeral is transcendence. This happens in two ways. First, the funeral helps us find a new self-identity. Funerals help us publicly mark a change in status. For example, someone who has lost their spouse goes from someone who is married to someone who is single. A funeral allows everyone to publicly acknowledge this change and begin offering the mourner support in their new status. Second, funerals often make us review our own lives and how we might want to spend our remaining days.
“People who take the time and make the effort to create meaningful funeral arrangements when someone loved dies often end up making new arrangements in their own lives. They remember and reconnect with what is most meaningful to them in life. They strengthen bonds with family members and friends… [and] emerge changed, more authentic and purposeful. The best funerals remind us how we should live” –
Dr. WolfeltThese purposes are not necessarily distinct steps and may happen in any order, but they are intertwined. The funeral experience as a whole is like a rite of passage. We emerge transformed, with a new identity, a new relationship with our lost loved one, and a new relationship with our community.
What do I say when someone is grieving?
When a person is grieving it can be hard to know what to say. The empathy we feel may urge us to want to ‘take away’ a person’s suffering or distract them from painful feelings. We might feel uncomfortable with tears or worry that we have caused unnecessary upset.
Despite this, bereaved people need to feel that their loss has been acknowledged and that the deceased person will not be forgotten.
As we age, we are more likely to experience loss. Without someone to talk to about personal doubts and fears, older adults can feel anxious, isolated or lonely. You may hear an older adult say something like “People don’t visit me anymore” or “I don’t want to sound sad and miserable all the time”.

The importance of listening
Feeling heard and understood is one of the greatest gifts you can give a grieving person.
Remember to:
• Focus all your attention on the grieving person.
• Make appropriate eye contact whilst considering cultural norms.
• Don’t interrupt; this is their time.
• Withhold advice.
• Ask gentle questions or paraphrase to clarify that you have understood.
• Give cues that show you understand such as smiling or leaning in.
• Focus on the quality of listening rather than the time spent together.
How to talk to someone who is grieving
Don’t fear saying or doing the wrong thing.
• Acknowledge the loss. It is ok to use the D words (Death, Dying, Deceased).
• Let the person know you are sorry for their loss and you care.
• Talk about the death and what happened with curiosity rather than enquiry.
• Used the deceased person’s name, if appropriate
• Ask them how they feel and listen to the answer.
• Validate and normalise any feelings that arise.
• Let them know that it is okay to show any emotion that comes up.
• Be genuine. If you’re not sure what to say then simply admit it and say, “I’m not sure what to say, but want you to know I care”.
• Be okay with silence and use body language to show you are there.
• Offer support or ask what you can do to help.
What not to say
• Statements that begin with, “At least…”, ‘you should’ or ‘you will’.
• Platitudes like “It’s part of God’s plan”, “Look at what you have to be thankful for” or “He’s in a better place now”.
• Avoid telling the person not to cry; crying can be helpful and part of the grieving process.
• Don’t rush grief by saying things like, “This is behind you now, it’s time to get on with your life”.
Download the Australian Centre for Grief and Bereavement’s MyGrief App or www.aged.grief.org. au for immediate information about how to receive bereavement support or how to support someone who is grieving.
Contact the Australian Centre for Grief and Bereavement Aged Care support service on 1800 222 200 to arrange to speak with a Specialist Bereavement Counsellor about telephone or online bereavement counselling.
National Hotline 1800 222 200 www.aged.grief.org.au
New collaboration targets better bone health and ageing
The World Health Organization (WHO) and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) today signed an agreement to develop a strategic roadmap on bone health and ageing and advocate for a public health strategy to prevent fractures among older people.
As part of the agreement, WHO and ESCEO will collaborate to:
• develop global estimates on fracture and osteoporosis;
• review evidence-based interventions to prevent fractures;
• create an economic model for an investment case in fracture prevention and care;
from the International Osteoporosis Foundation (IOF) and the WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Ageing at the University of Liège, Belgium, which was previously designated by WHO as a technical partner for osteoporosis and musculoskeletal ageing.
“This agreement is an important step to improving the health and well-being of older people by putting in place the right public health strategy, policies and services to protect and prevent fractures in older people so they can continue to do the activities they enjoy,” said Dr Anshu Banerjee. “We look forward to working closely with ESCEO to advance progress in bone health and ageing.”
The agreement includes the development of a public health strategy and action plan to prevent fractures among older people as well as to improve the coverage of health services for fractures which are critical for achieving the triple billion targets of WHO’s Thirteen General Programme of Work (GPW13).
• provide guidance to countries on strengthening national health information systems by integrating osteoporosis and fractures in routine data monitoring; and
• provide guidance to countries on using data to design evidence-informed policies and programmes to reduce the risk of fractures in older people.

“ESCEO is fully convinced that this partnership with WHO will improve the prevention and management of osteoporosis at local, regional and national levels and will result in a greater quality of life for osteoporotic patients,” said Dr Jean-Yves Reginster, President of ESCEO.
WHO will establish a Bone Health Expert Working Group to advance the five-year workplan with support
About ESCEO
The European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) is a not-for-profit organization, dedicated to a close interaction between clinical scientists dealing with bone, joint and muscle disorders, pharmaceutical industry developing new compounds in this field, regulators responsible for the registration of such drugs and health policy makers, to integrate the management of Osteoporosis, Osteoarthritis and Sarcopenia within the comprehensive perspective of health resources utilization.
A serious risk for the elderly as TB set to overtake COVID-19 as leading infectious killer globally
As tuberculosis deaths continue rising for the first time in more than a decade, there are calls for global leaders to increase investment for prevention, treatment and vaccines.

This year the World Tuberculosis Day highlights the entirely achievable proposition of ending TB globally by 2030 with sufficient investment.
Tuberculosis, once called consumption, was the world’s biggest infectious killer before the arrival of Covid-19, with 1.5 million people dying from the disease each year. About 1.6 million people died from TB in 2021 - claiming 4,300 lives a day, including the lives of 600 children.
Experts are predicting TB will once again become the world’s biggest infectious disease killer. This week, The Global Fund’s executive director said tuberculosis will likely kill more people in low and middle income countries in 2023 than COVID-19.
To end tuberculosis by 2030, major technological breakthroughs, including a new vaccine, must be introduced by 2025.
The only vaccination for TB is more than a century old, and is less effective on adults, who account for the bulk of disease burden.
Australia’s role
Results International (Australia) CEO Negaya Chorley said, “Tuberculosis is a prolific infectious disease that devastates the most vulnerable, including in our own backyard.

“Just this month, a TB outbreak was reported in the APY Lands. Our neighbour PNG sees thousands of people die annually,” Ms Chorley said.
“The progress we were making in reducing TB cases and deaths over the years has been derailed by the COVID-19 pandemic, as TB infections have gone undetected and unmanaged. Now, for the first time in more than a decade, TB deaths are on the rise.
“TB could soon reclaim the title of leading cause of death worldwide from a single infectious agent. Yet, the disease is entirely preventable and curable.
“The same global concerted momentum to tackle COVID-19 must be applied to ending TB. We need to
use all the tools in the toolbox including scaling up prevention, treatment and cure.
“An effective new vaccine would save millions of lives and help fight antimicrobial resistance, while also offering a substantial return on investment.
“Australia must play a greater role in ending TB. Given the Asia Pacific region is home to the majority of TB cases, and the cutting edge scientific research that takes place in universities and institutes across the country, we are well placed to lead the charge in addressing TB.
“If COVID has taught us anything, it’s that we have the scientific capability and know how to tackle infectious diseases including TB - we just need the will.
“This September, world leaders will gather in New York for the UN High-Level Meeting on TB. We are calling on the Australian Government to encourage world leaders to set ambitious targets to eliminate TB and back it up with adequate financing.
“If we don’t increase our efforts and investment in TB, the cost in terms of human lives will be immense.”
A word on TB prevention from the World Health Organization (WHO) Tuberculosis (TB) infection is extremely common: an estimated one-quarter of the world’s population is infected. People with TB infection risk developing TB disease and this risk depends on multiple factors, the most important being the state of their immune system.
TB preventive treatment stops TB infection from progressing to disease in those who are infected and can protect both the individual and the community from TB. WHO develops guidelines and operational handbooks to accelerate increased treatment coverage in countries. Tools such as the Prevent TB platform support national health systems to strengthen their strategic information.
In addition, WHO supports countries to prevent TB infections through guidance and implementation of infection prevention and control measures.
These measures are critical in situations where the risk of TB transmission is high, such as health-care facilities, congregate settings and TB-affected households.
WHO also promotes preventive action through early screening and treatment for active TB, by addressing co-morbidities and health risks as well as social determinants of the disease, and by promoting access to universal health care.
Additionally, WHO advises and guides the TB vaccine development activities of the global research community through scientific consensus-building, guidance on vaccine evaluation, and assessment of the evidence base for policy recommendations.
Key facts and figures:
• The latest statistics show about 1.6 million people died from TB globally in 2021.
• TB treatment saved 74 million lives globally between 2000 and 2021.
• Just US$120 million was spent on TB vaccine research and development in 2021. This is a small fraction of the global spend on COVID-19 vaccines.
• Every US$1 invested in vaccine interventions will return US$7 in health and economic benefits over 25 years.
• Maintaining current funding levels will see an additional 43 million people falling ill and 6.6 million die from TB by 2030. There will be US$1 trillion in economic losses as a result of TB morbidity and mortality.
• The targets for 2030 are a 90 per cent reduction in the number of TB deaths and an 80 per cent reduction in the TB incidence rate.
• Annual research funding must increase fivefold from US$1 billion to US$5 billion dollars to reach the 2023-30 Global Plan funding targets.
Laundry trolleys providing a cleaner, safer facility for staff and residents

For years trolleys have been a staple in aged care laundry for providing ease of transport of linen and personal clothing between the residents’ rooms to the laundry and back to the residents’ rooms again.
We have all felt the impact of the pandemic during the last couple of years, and now more than ever it’s important to have appropriate and reliable trolleys in place to assist staff to move soiled and clean laundry throughout the facility in the safest way possible.
The first part of the process is the collection of soiled laundry from the residents’ rooms. Soiled laundry should always be placed into the designated skip bag so that when it comes time to launder, it can be done exactly the way it should be without being mixed up with laundry that requires a different laundering process.


Laundry Solutions Australia provides a wide variety of bag and lid colours for easy designation, as well as skip bins in single, double, and triple. Depending on the size of the facility the correct collection trolley size will allow staff to collect as much soiled linen as possible, avoiding multiple trips to the same areas.
Once soiled laundry has been collected it should be processed as early as possible, holding it for too long in
its soiled state undermines the wash effectiveness and increases the chances of cross infection. By pre-sorting during the collection, means that staff don’t have to sort through soiled laundry during the processing stage.

Staff should always be wearing the appropriate PPE when processing soiled laundry including gloves, apron, mask, and eyewear. It is imperative that everything possible is done to protect residents as well as staff.
Soluseam bags are great way to handle heavily soiled, foul and infectious laundry so staff do not need to handle the potentially infectious laundry. They simply place the soluseam bag in the washer and the seam of the bag will open up when the washer fills with water.
Once the washing has gone through the appropriate wash cycles, clean wet laundry can be moved from the washer directly to the dryer via a portable folding table. These portable folding tables will stop laundry staff from having to pick up any wet laundry in their hands. Likewise, once the drying is complete, dry laundry can be moved directly onto a portable folding table where it can be folded and placed into a linen distribution trolley ready to be redistributed to the facility residents.
By having all the appropriate trolley equipment, aged care facilities can ensure that their staff are always able
to ensure best practices when it comes to minimising risk of infection. While this is the biggest benefit, it is not the only one. Having all the correct trolley products allows staff to work in the most efficient manner from start to finish of the laundering process.
Laundry Solutions Australia designs and manufactures a wide range of aged care specific laundry trolleys and accessories right here in Australia for our customers large and small.

We also provide free consulting on all aspects of aged care laundry processes to our customers.
Phone: 1300 666 289
Email: info@laundrysolutions.com.au
Website: www.laundrysolutions.com.au/ trolleysandaccessories/

AUSTRALIAN MADE TROLLEYS SUPPORTING AUSTRALIAN AGED CARE

Laundry Solutions Australia manufactures and distributes trolleys to hundreds of customers every year and we understand that ensuring your laundry collection and distribution should be of the highest standards and are an essential activity in every aged care facility. With proper linen management using the correct equipment the facility can have greater confidence that standards are being met and infection control is at a minimum.
The following steps are a guide and should be undertaken with the right equipment to maintain a healthy, clean and safe environment for all residents and laundry staff alike.
Collection & Processing
• Pre-sort laundry items into their designated skip bag to avoid double handling and having to sort through soiled laundry. Single, double and triple collection trolleys will allow for varying degrees of designation

• Launder linen as soon as possible
• Always use appropriate PPE and washing of hands
• Using Soluseam bags for heavily soiled items means not having to handle potentially infections laundry

Washing & Drying
• Linen in Soluseam bags can go directly into the washer
• Clean wet laundry should be moved straight onto a portable folding table from the washer

• From the portable folding table linen can be pushed straight into the dryer, once dry it can be removed the same way (onto a dry folding table)

Distribution
• Fold and hang personals straight onto the personals trolley to minimise handling
• The use of appropriate linen and distribution trolleys is key to an effective distribution system

• Always wash hands prior to distribution of linen to residents
View our products here
Phone: 1300 666 289
Email: info@laundrysolutions.com.au

Website: www.laundrysolutions.com.au/trolleysandaccessories

The importance of oral health in aged care
Malnutrition, social isolation and declining general health are some of the serious impacts of not maintaining a healthy mouth – and this is never more so than with older Australians in aged care.

Concerning data from the Australian Oral Health Survey found:
• 32 per cent of those aged 55-74 years and 25 per cent of those aged 75+ years have untreated tooth decay,

• 51 per cent of those aged 55-74 years and 69 per cent of those aged 75+ years have gum disease,
• where the gum disease wasn’t treated, it resulted in complete tooth loss for 20 per cent of those aged 75+ years,

• 22 per cent of those aged 55-74 years and 46 per cent of those aged 75+ years have an inadequate dentition (less than 21 teeth).
"What this data shows is that many older Australians don’t have the oral health they should have," said Dr Stephen Liew, Australian Dental Association (ADA) Vice President, "and if they’re one of the nation’s 190,000 aged care residents, the lack of oral care in residential homes is a key factor."
Addressing and preventing these problems requires careful daily attention to oral hygiene, as well as regular reviews by a dentist.
Dr Mark Hutton president of the ADA writes in Australian Ageing Agenda,1 “Many older people enter aged care with poor oral health for several reasons. They may only go to the dentist when in pain, or they have reduced manual dexterity from arthritis making brushing and flossing challenging, or perhaps dementia is a contributory factor and they’re not aware brushing is a necessity.
“Add to this the many complex health conditions older people suffer and associated medications that can result in reduced saliva flow, increasing the risk of dental caries and gum disease.”

The ADA’s royal commission submission recommended setting up the ‘seniors dental benefits schedule’, a national funding model to make dentistry accessible to older Australians in both the public and private sectors. The royal commissioners agreed and included it in their set of recommendations.
Also, the ADA advocates fixing the broken system with further measures such as the Certificate III Aged Care qualification incorporating oral care as one of its core units of study for workers in that sector, and for GPs to include oral health in their assessments for seniors aged over 75.
Staff shortages in aged care and low pay are further compounding the issue of achieving appropriate oral care for aged care residents.
Dr Mark Hutton says, “It remains to be seen if the royal commission recommendations to ensure there are enough nursing staff and personal care workers for appropriate care, given there is already a national shortage of nurses and aged care workers are notoriously underpaid.

There’s much to do to improve the oral care of aged care residents but with the new Labor Government working with peak health bodies like the ADA as well as significant changes to funding models, staffing levels and training, those much needed improvements could well be within our sights.”
ACHIEVE THE HEALTH YOUR GUMS DESERVE
CHLOROFLUOR is the must have product for vulnerable gums.



Available in a Gel, Mouth Rinse or Toothpaste, Clorofluor strengthens gums and tooth enamel, helps prevent tooth decay, reduces the growth of dental plaque, helps clear persistent bad breath, helps relieve denture sores, sterilises the mouth after oral surgery and reduces the growth of dental plaque and odour on all orthodontic appliances.
Keeping Australian mouths healthy for over 30 years.

Candida Auris: A fungus with attitude
In the face of the global COVID-19 pandemic it is easy to understand that we have seen a significant shift in both awareness and practical application of improved infection prevention and control practices. The pandemic has driven advances in all aspects of disease prevention from the basics of hand hygiene and surface cleaning and disinfection, to social distancing and acceleration of vaccine development and production.
However, there are still many other bacteria, virus’ and fungi that need to be eliminated to best protect patients, healthcare staff and the wider population. If we focus just on COVID-19 and things such as disinfectant contact times and efficacy only for COVID-19, we risk not suitably managing these other pathogens, which will lead to increased adverse health outcomes and morbidity.
Candida auris (C.auris) is a fungus from the same group of germs that cause thrush (Candida albicans) or serious blood stream infections in immune-compromised patients (C. glabrata, C. parapsilosis, C. krusei and C. tropicalis). Unlike most of the other candida species which live in the gastrointestinal tract, this fungus is also commonly found living on the skin. It is much more resistant than other fungi to commonly used treatments and over 90 percent of C.auris cases to date have been resistant to Fluconazole, the standard treatment for Candida infections.
Multi-resistant C.auris has only emerged relatively recently; it was first identified in Japan and South Korea in 2009 but had spread to six continents by 2017. C.auris is of particular interest to clinicians, infectious disease experts and infection prevention and control (IPC) professionals due to the following characteristics of the fungus:
• It’s a pathogen – it causes disease
• It’s of risk to all types of patients
• It’s often mis-classified in laboratory diagnostic tests
• There are few treatment options
• It spreads easily in the environment
• It’s resilient to environmental disinfection

Healthcare facility outbreaks
As with many other antimicrobial resistant pathogens, C. auris has been implicated in many hospital outbreaks around the world. A large outbreak lasting over 12 months between 2015 and 2016 in a London cardiothoracic intensive care unit resulted in 50 cases. Contact with an environment contaminated with C. auris was found to be a significant source of infection with the fungus.

Disinfection of a contaminated environment
Removing C.auris from environments is a challenge due to the ease which it spreads and its resistance to common cleaning agents. The environment can remain contaminated for weeks. Subsequently many guidelines for the management of these infections, advise daily and terminal or discharge cleaning with a strong environmental disinfectant such as a sporicidal disinfectant.
As with all environmental disinfection options, success will be easier if the area is regularly cleaned so that surface biofilm is not allowed to build up. Importantly as with other pathogens ensuring suitable contact time exposure to the disinfectant and sporicidal agent is essential in effective outcomes and pathogen reduction.
Summary
Infection prevention and control measures
C.auris cases should be taken very seriously in all healthcare facilities and strict measures put in place to prevent spread to other patients.
These measures are similar to other important IPC practices for multidrug resistant organisms and include the following key actions:
1. Notify local IPC and infectious diseases experts
2. Place patient in single room with contact and isolation precautions
3. For symptomatic disease, begin treatment, with guidance from an infectious disease specialist (treatment of asymptomatic colonization is not recommended)
4. Contact tracing and screening to determine local transmission
5. Focus on environmental disinfection
Multi-drug resistant Candida auris is an important pathogen which demands attention and action when identified in the healthcare setting. As well as implementing common IPC measures, disinfection of a potentially contaminated environment must be a priority. Always follow requisite guidelines for managing this pathogen and ensure contact times are enforced, noting that for any disinfectant or sporicidal agent the contact times against different pathogens may vary.
References:
Schelenz, Silke, et al. "First hospital outbreak of the globally emerging Candida auris in a European hospital." Antimicrobial Resistance & Infection Control 5.1 (2016): 35.
Schwartz, Smith & TC Dingle. “Something wicked this way comes: What health care providers need to know about Candida auris”. Can Commun Dis Rep (2018);44(11):271–6.
Phone: 02 82 073 133
Email: enquiries@reynardhealth.com.au
Website: reynardhealth.com.au

Biodegradable Premier detergent & disinfectant wipes. Stay one wipe ahead of germs.
The world’s first high efficacy 100% biodegradable wipe.
Reduce a single hospital’s plastic waste by 4.2 tonnes per annum* with a simple switch to Reynard Biodegradable premier detergent & disinfectant wipes. That’s the weight of two adult rhinos in plastic waste saved from landfill each year.

The most widely used wipe in Australian hospitals today, our optimised formula is proven to kill at least 99.999% of pathogens, bacteria, viruses and fungi after just 60 seconds and is effective against SARSCOV 1 and 2 in just 30 seconds. Providing a single step, environmentally friendly solution to cleaning and disinfecting surfaces and equipment. AUSTL337692.
The cloth that is a cut above.


This 100% biodegradable cloth is made from a specially developed bamboo substrate that boasts superior formula retention and impressive strength. The cloth’s highly effective traction picks up dirt where competitor cloths simply push it around the surface. Combined with unparalleled device and material compatibility, you won’t need to compromise on quality while being environmentally conscious

Technology Saving You Hours on Messy, Smelly, Manual Labour
While most washer disinfectors only clean bedpans, this top-of-the-line machine cleans and disinfects buckets, carpet tiles, kidney bowls, bottles, vases, floor cleaning discs, overshoes, floor tiles, wash bowls and suction bottles – making it the standard by which others are judged.
Dealing with human waste is an unenviable but unavoidable part of the aged care industry. Yet while bedpans are shredded by a macerator or thoroughly cleaned with a washer disinfector, most other items are left as a smelly, messy COVID hazard.
For instance, what happens if someone vomits on a carpet tile? How do you clean a suction bottle after it’s used to clear the airways of blood, saliva, vomit or other secretions? And after you mop up a patient’s vomit on the floor, how do you clean the infectious human waste in the bucket? In most cases, it gets hosed off with some detergent in the sink and is reused again. But, that doesn’t disinfect it and consequentially puts everyone at risk of infections we’d all rather not think about.
At ward level, all reusable items should be treated as infectious and need to be made safe. However, this is rarely the case.
Many aged care services now have washer disinfectors at their premises and most do a thorough job of cleaning bedpans. However, when it comes to disinfecting everything else, they’re extremely limited. There is a better way.

Imagine having a device that handles almost every ward cleaning task quickly, easily and hygienically – automatically
flushing, washing and disinfecting every item that carries human waste.
A device that uses additional option holders and baskets, enabling you to correctly position and easily load various items from carpet squares to suction jars and medicine pots.
A device that also pre-washes instruments prior to CSSD, eliminating exposures caused by manual handling.
A device that not only does the job of two traditional machines, but improves and enhances staff productivity, electricity and water costs, and infection control practices, AND saves space.
Sounds like a dream, doesn’t it?
Thanks to Rhima, it’s now a dream come true.
The Deko 190 washer disinfector not only allows you to disinfect bedpans in patient care units without the need to empty them beforehand (reducing the risk of contamination), it’s the only machine that uses large droplet technology and provides the mechanical scrubbing action to empty, flush, clean and thermally disinfect human waste containers intended for reuse.
What’s more, it washes, cleans and disinfects itself after every seven minute cycle.
Instead of cleaning bedpans in the morning and evening, leaving the machine sitting idle the rest of the day, wash everything in the same device and get 10x more usage from it. It’s like a full time employee who cleans and disinfects everything for you – all day long! Nothing else compares.
Take a macerator, for example. While they might have a low capital cost, the running and environmental expenses are exorbitant.
Based on five users per day and $2.50 per patient, a 25 bed ward would carry a cost of approximately $22,812 per year.
If you carry that over 10 wards, with 250 patients per ward, over a five year period, the macerator would cost over $1,140,000 – not taking into account heavy patients that may flatten a papier-mâché bedpan.
Therefore you’ll need a plastic cup holder to hold the bed pan, which itself needs to be washed and disinfected, meaning you need a washer disinfector in any case.

The other downside to a macerator is that papier-mâché bedpans can leak, and machines often get blocked leading to toxic splashback.
What’s more, the waste produced can block sanitary sewage disposal pipes and cause wastewater overflow, leading to costly fines from local providers for blockage and damage of external sewage pipes.
You may save a little water (although, this is arguable considering you need a significant amount of water to grind up the papier-mâché and flush it down the sink), yet a 450 bed aged care home using a macerator easily adds up to 21 tons per year of extra waste to the environment.
Plus, even though the macerating machine itself is compact, the additional space required to store large boxes of disposable bedpans not only decreases the available workspace but also makes for a difficult and unpleasant work environment.

From protecting the environment to its space and money saving advantages, the Deko 190 is a cleaning workhorse that will ward off infections and save your team hours of unhygienic, messy and smelly work.
What’s more, the Deko 190 is:
• Easier to operate than a domestic washing machine, as pre-emptying or rinsing is not required, and a choice of five different wash programs allows you to specifically tailor it for individual washing and disinfection needs.
• Easy to service and maintain, as all electrical components are located under the top plate, meaning standard maintenance can be carried out from the front without removing the machine. Any information, advice, personnel training and service calls are attended to with the utmost dedication and urgency, and spare part availability is guaranteed for a minimum of 10 years after date of shipment.
• Requires minimal space, needing only 600 mm x 630 mm of floor space. Connections to water, electricity and drains are provided with all the necessary safety features.
If you would like to have more information about this exciting product, please visit https://www.rhima.com.au/ product/deko-190-ix-washer-disinfector/ and download the information pack.
You will immediately be sent a free-of-charge overview of exactly what puts this machine in a league of its own, and a step-by-step checklist on how to structure your team’s day to use this unbeatable machine to maximise your team’s cleaning workload by 10x – and keep your wards infections free.
Like a chef’s Combi oven, soon you won’t be able to live without it.
30 years ago, chef’s had barely heard of a Combi oven. And yet, today they’d be lost without them –and for good reason!
Just as the Combi changed the rules for restaurants, the Deko 190 is setting the standard within the aged care industry by which all other washer disinfectors will be judged.
Phone Number: 1300 347 944
Email Address: sales@rhima.com.au

Website: www.rhima.com.au
Youtube: www.youtube.com/@rhimaclean
Facebook: www.facebook.com/rhimaaustralia/
Linkedin: www.linkedin.com/company/ rhima-australia-pty-ltd/
Policy shift helps audiologists tackle hearing care inequities
Changes to Medicare are widening access to hearing care.


Whether they work in consulting rooms, soundproof booths, makeshift community health clinics or other settings, Australia’s audiologists play integral roles in diagnosing, treating and preventing hearing and vestibular disorders among thousands of people.

But there is a key issue: not everyone gets to experience equal and affordable access to hearing care. Fortunately, policies are shifting to help audiologists tackle these inequities. As of 1 March 2023, there are fundamental changes to the Medicare Benefits Schedule, which governs which healthcare services are rebated by the Government’s Medicare insurance scheme.
The only way that Australians used to be able to claim a Medicare rebate for a paid hearing assessment was to get a referral from an ear, nose and throat (ENT) specialist or a neurologist. Now, the rebated referral pathway has expanded significantly.
“You can now claim a Medicare rebate for a hearing service after being referred by any medical practitioner, whether they’re a paediatrician or a GP, just like you would for an eye examination. It’s going to make a huge difference.”
Nicole Bowden is the Principal Audiologist and Manager of Victorian Hearing, an independent chain with 10 clinics across the sprawling Greater Melbourne area. Approachable, confident and friendly, she exudes a sense of calming reassurance that you’d hope for in a healthcare professional.

Like many other audiologists, she believes the Medicare changes will break down financial barriers that may have prevented someone from booking a hearing test.
“People often enquire if there is any Medicare rebate for hearing tests. When there isn’t, it’s often a deterrent for them to book an appointment. But now there are more rebates available,” Nicole says.
“There will also be benefits from the health professional side. Now that audiology is Medicare rebatable, medical practitioners will be more likely to refer to us for services.”
Providers joining forces to improve people’s lives Highlighting inequities to hearing health access and further integrating ear and hearing care within primary healthcare are important initiatives of World Hearing Day 2023, with its theme ‘Ear and hearing care for all! Let’s make it a reality’.
Nina Quinn, an Audiology Australia Accredited Audiologist and the CEO of Neurosensory, one of Australia’s largest multistate, comprehensive hearing care providers, headquartered in Brisbane, says the Medicare changes will naturally encourage other healthcare providers to work more closely with audiologists, leading to better patient outcomes.
“I think there is an emerging opportunity here to build new relationships in the healthcare system,” explains Nina.
“First of all, we’ve got a new level of access for Australians in regional and remote areas, where there may be no neurologists or ENTs, which will encourage audiologists and other healthcare professionals, like GPs, to work closer together.
“Secondly, there’s a real opportunity now for audiologists to help other professionals get the job done to treat
patients. We can help them exclude sinister pathology and help them understand if there are any acute conditions that need a further referral.”
Driven by her personal and family history of hearing loss, Nina is highly passionate about broadening access to hearing care for larger cohorts of people, to help them more easily interact with the world around them.
While the Medicare changes represent a more fundamental opening of access, Nina is also hopeful that there will in the future be changes to the Hearing Services Program (HSP), a Government initiative offering free or subsidised hearing assessments and hearing aids to eligible Australians aged 0-26, 65 and older, or belonging to other demographics.
“I would like to see the HSP expand to include Australians aged 27 to 64. It’s a cohort where access to hearing care is largely self-funded, and robust economic modelling indicates that expanding access to this cohort, and investing in their hearing rehabilitation, will have enormous community and social benefit,” Nina says.
“There shouldn’t be any discrimination on who can access hearing care based on age, economic means or location. ‘Ear and hearing care for all’ means no one should miss out. No one should be left behind on this fundamental access to such an important sense.”
The vital work of audiologists in creating a sound future
An ageing population means that audiologists will become more important in the healthcare system as hearing and vestibular (balance-related) disorders become more common.
About 3.6 million people have some form of hearing loss in Australia, with this number expected to more than double to 7.8 million in 2060, according to the Department of Health and Aged Care. Hearing loss can often be linked to tinnitus – a condition where someone has the lived experience of ‘hearing’ ringing, buzzing or whooshing with no external source – and increase the risk of falls, isolation, anxiety and depression.
Luckily, getting a hearing assessment is usually easy for the patient in question. And for both the patient and the audiologist treating them, the results can be both personal and powerful, explains Nicole. “There’s a lot of joy when you make such a vital difference to someone’s ability to hear. As a paediatric specialist my youngest client was an eight-week-old baby. I remember crying with the parents as I turned on the hearing aids and we saw their child begin to hear well for the first time."
For more information about Audiology Australia go to: audiology.asn.au
World Hearing Day 2023
This year's World Hearing Day theme is 'Ear and hearing care for all! Let's make it a reality'.

The theme invites audiologists, patients, and others in the hearing health space to campaign to policy makers for the integration of ear and hearing care within primary healthcare.
This integration will make it easier, cheaper and quicker for you to access audiology and other hearing services to better manage your hearing health.
How integrated care benefits you
An integrated healthcare system is a crucial step towards achieving better hearing health outcomes for everyone.
In this system, your healthcare providers will work closer together, sharing their knowledge more readily to treat your hearing holistically across different stages of your life, supported by government policies. You can expect each of your healthcare providers to have an increased familiarity with ear and hearing health. This will fast-track how long it will take for you to receive a diagnosis and treatment for your hearing loss or hearing condition.
Current developments in Australia
New policy changes are making it possible for you to access hearing care services easier, at a cheaper cost, and to link with different health professionals all committed to your ear and hearing care.
The changes both acknowledge audiologists as integral partners in the healthcare system and the pivotal role audiologists play in preventing, assessing, treating and rehabilitating someone with a hearing or balance disorder.
Quicker referral times
From 1 March 2023, the Government is legislating changes to the Medicare Benefits Schedule (MBS), including widening the scope to allow any medical practitioner to refer a patient to an audiologist.

This reduces the number of referrals you need to receive audiological assessments and treatment, saving you both time and money. The changes are particularly beneficial for people in regional and remote areas and Aboriginal and Torres Strait Islander communities, who do not have frequent access to healthcare services.
More subsidised appointments for young people
Other changes to the MBS include allowing more young people with complex neurological disorders, such as a child or young person with autism, to access allied health services at a subsidised cost.
The changes increase the number of allied health assessments or treatments covered by Medicare from four to eight services, and increase the age limit of eligible patients from 13 to 25 years of age.
Free interpreting services
If you are from a culturally and linguistically diverse background, or know someone who is, you can now access a free interpreter at select locations around Australia when you book to see an audiologist.
The changes to the Government's Free Interpreting Service allow an interpreter to join you by phone, video call or even in-person during your audiology appointment. The interpreter can assist your audiologist to accurately convey information and reduce any confusion.
The service includes access to interpreters in 150 languages, including Mandarin, Hindi, Spanish, Vietnamese and Thai.
Top three frequently asked questions about hearing
1. What is World Hearing Day?
Held annually on 3 March, World Hearing Day is a global awareness campaign led by the World Health Organization (WHO) to highlight the importance and value of hearing healthcare and the need to protect hearing throughout the course of our lives.
2. How do we hear?
Our ears work with our brain using a delicate system to transport sound waves through the outer, middle, and inner ear and process and transform sound signals into the things we hear.
Sound waves travel down our ear canal where they are vibrated through the ear drum. The sound is then conducted by the smallest bones in the body 'the hammer, anvil and stirrup' into the cochlea in the inner ear where tiny hairs perfectly tuned to specific pitches transform the sound into signals that are sent along the hearing nerve to our brain.
Our brain then helps us process and understand these signals as the things we hear.
3. What does an audiologist do?
Audiologists are highly skilled and trained hearing health professionals who provide advice, treatment, education, and interventions for people with hearing,
communication, and balance problems. They can work closely with other health professions and in a wide variety of health and education settings.
Audiologists:
• conduct diagnostic hearing and balance assessments
• develop and implement personalised rehabilitation and treatment programs, including working holistically with a broader health team to manage hearing health needs
• provide counselling and rehabilitation for clients with tinnitus to help them adjust to the condition and improve their quality of life
• prescribe, fit, and program hearing aids, implants and assistive listening technology systems
• work with educators in schools and classrooms to maximise listening environments and support for children with hearing needs
• design, implement and supervise hearing health programs such as newborn screening programs.
Lots of ‘breakthroughs’, still no cure. Do the new dementia drugs bring us any closer?
We often hear about “dementia breakthroughs” in the news – new genes being discovered, new blood tests being developed, new drugs being tested.
However, there remains no effective or accessible cure for dementia. This is of great frustration to people living with dementia, and their carers and loved ones.
Two new “breakthrough” drugs have been in the news. While they may not bring much relief to those living with the disease today, we are learning more about dementia, and getting closer to a treatment.
A bit about dementia
Dementia is an umbrella term to describe a group of conditions characterised by a loss of brain function. This includes the ability to remember, plan and make decisions.

In Australia, dementia is the second leading cause of death. For women it’s the leading cause of death. Older age is the greatest risk factor for dementia. But dementia is not an inevitable or normal consequence of ageing.
Up to 70 per cent of all dementia is attributed to Alzheimer’s disease. Other types of dementia include vascular dementia, frontotemporal dementia, and Lewy body disease. Because Alzheimer’s is the most common form of dementia, most “dementia breakthroughs” often refer to “breakthroughs” in Alzheimer’s.
Searching for treatments
Alzheimer’s disease takes a long time to develop, up to 30 years or more. For a long time, scientists had only a limited understanding of the disease. To develop the right drugs, it’s crucial to have the right tools to be able to understand how the disease progresses.
Over the past 20 years, breakthroughs in brain imaging, brain fluid analysis and, more recently, blood tests, have enabled us to measure key Alzheimer’s proteins – amyloid and tau – in living people. This has allowed scientists to understand how these proteins develop over time.
We have also been able to clarify which risk factors – age, sex, genetics, environment, lifestyle – contribute to the development of cognitive decline and Alzheimer’s. This provides important insights into who and what to target.
Studies now suggest Alzheimer’s begins with the buildup of amyloid in the brain. As amyloid builds up, tau then begins to develop. Researchers think it’s this tau buildup that leads to brain cell death and cognitive decline. Some scientists refer to amyloid as the “trigger”, as once the trigger has been pulled, the “bullet” (tau) is on its way.
Stopping the buildup of amyloid, or removing it,
became a key strategy in attempts to develop drugs for Alzheimer’s.
Two new drugs
Two drugs that have received a lot of attention in recent weeks are aducanumab (marketed as Aduhelm) and lecanemab. Both drugs showed substantial reduction in amyloid in the brain. But whether this reduction in amyloid resulted in a meaningful benefit in memory and thinking is less clear.
In two aducanumab trials, patients did not show any meaningful benefit. But six months later, the drug maker Biogen released and subsequently published new data reporting participants on the highest dose had 22 per cent slower cognitive decline compared to participants on a placebo.
The Food and Drug Administration in the United States granted accelerated approval for aducanumab as it thought the drug would improve or slow Alzheimer’s symptoms.
Recently, drug companies Eisai and Biogen announced the results of a lecanemab trial. Around 1,800 participants with early Alzhemier’s were given the drug or a placebo over 18 months. They found a reduction in brain amyloid
and tau levels in those taking the drug when compared to participants taking a placebo.
Importantly, lecanemab resulted in a 27 per cent slower decline in memory and thinking ability. This was also accompanied by greater quality of life, as reported by participants and their caregivers.
This translates to roughly a six-month benefit in memory and thinking ability. This is not much. In addition, questions have been raised about whether the drug may be less effective for people with higher risk of developing Alzhemier’s, including those with certain genes, women, and culturally and linguistically diverse populations.
There are also substantial side effects that accompany both drugs. Of most concern are brain swelling and small brain bleeds as detected on brain scans. These were observed in 21-40 per cent of participants. The risk of these side effects will need to be an important discussion between patients, their families and their doctors.
Another consideration is the cost. The price of lecanemab has not yet been announced, but aducanumab costs US$28,200 (A$42,000) per patient per year. Additional costs for brain scanning will also be required to monitor side effects. This makes it inaccessible to most people to purchase privately.




It also has consequences for the availability of the drug to be considered under Australia’s Pharmaceutical Benefits Scheme (PBS). Around 150,000 people with


mild Alzhemier’s would currently be eligible for aducanumab if it were available. If all of these people received the drug, PBS expenditure would increase by 50 per cent.
Companies that develop drugs must provide evidence of their effectiveness to the government health authorities in each country in which they intend to make it available. The governing body in Australia is the Therapeutic Goods Administration. This process has not yet been completed for either drug in Australia.

So why all the breakthroughs, and still no cure?
Since Alois Alzheimer first described an “unusual disease of the cerebral cortex” in 1906, we have learned a lot about the disease and its progression.
But we still have a long way to go. Because Alzheimer’s symptoms take decades to develop, studying and tracking brain and cognitive changes from early in the disease has been difficult. Beyond amyloid and tau, a range of other biological, genetic, lifestyle, and environmental factors can also contribute to Alzheimer’s disease.
It’s unlikely any single one of these factors alone can fully explain why someone develops the disease. It’s likely the disease manifests when several of these risk factors coalesce. For example, someone with a genetic predisposition may be more likely to develop the disease in the face of poor cardiovascular health. Disentangling the contribution of these risk factors can be challenging. This is why large numbers of people are often required to participate in research.
Given the prevalence of the disease in the community, every advance is seen as newsworthy. And from a scientific point of view, they are. However these findings, or “breakthroughs,” have not been enough to offer relief to people living with Alzheimer’s or their families, for whom life gets harder every day. Their hopes are dashed when reported “breakthroughs” still haven’t translated into a cure or an effective treatment.

We now have multiple drugs that show some effect in slowing memory deterioration, but the effects are small. Outcomes of more drug trials will be announced in the coming years. While these advances may not come fast enough to help people living with the disease now, they’re an important incursion in the war against this devastating disease. They show we’re getting closer.

If you are interested in learning how to reduce your dementia risk by changing health behaviours, please join us at the BetterBrains Trial, www.betterbrains.org.au. We are actively recruiting Australians aged 40-70 with a family history of dementia.

Authors
Yen Ying Lim
Associate Professor, Monash University

Emily Rosenich
Postdoctoral Research Fellow (Neuropsychology), Monash University

An
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ lots-of-breakthroughs-still-no-cure-do-the-new-dementia-drugs-bring-usany-closer-195095 Hands-free

Differentiate your business by making client outcomes the star of your show
In an ever-evolving healthcare ecosystem, technology is at the heart of progress. The healthcare industry especially seeks innovative solutions to achieve better outcomes for people in their care - Lumary has delivered that with their specialist next generation software designed by experts in the field. Taking an expert-led approach to design means providers can now offer an even greater level of service.
Purpose-built care management software is designed to help healthcare providers streamline their operations, improve communication, and deliver better outcomes for their clients. Whether you’re operating in the aged care, disability or allied health industries, with Lumary’s next generation software, providers can manage all their client information, schedules, and billing in one place.
One of the significant benefits of operating with an all-in-one software solution is that it enables providers to manage their workforce more effectively, run their business more smoothly, whilst meeting the care needs of their clients. With features like efficient rostering, travel and transport tracking, providers can ensure that their employees are always in the right place at the right time. As a result, clients receive the care they need, when they need it - and employees can work more efficiently!
Another powerful advantage of Lumary's purpose-built software is that it is designed with and for healthcare
specialists. Providers and their staff can access the software from any device with an internet connection, making it easy to stay up-to-date with their clients' needs and operate in real-time. With a user-friendly interface, Lumary's care management software is easy to navigate, where providers can quickly find the necessary information they need about their clients to deliver high-quality care.
With the healthcare industry continuing to innovate, Lumary's next generation software is designed to support providers to maintain compliance and scale as the industry does. Designed for niche healthcare markets, Lumary eases the regulatory burden that healthcare providers face, including maintaining compliance across a wide range of governed rules. With features like audit trails, secure messaging and document control, Lumary's software ensures that providers can maintain accurate records, making client privacy a priority.
Lumary's software is also designed to help providers collaborate more effectively. Integrated communication and messaging tools help providers to work together seamlessly whilst at the same time increasing engagement with clients, allowing them to receive coordinated care. And, the workforce can work more productively!
As the Australian healthcare market continues to advance, Lumary’s next generation software is designed to support providers as they seek to differentiate themselves in-market and increase productivity. As providers expand
their operations, they need software that can keep up with their needs. Lumary’s care management software is scalable. From onboarding new clients and employees, to expanding service delivery, Lumary's software can adapt to meet the needs of the growing provider.

Whether you're a healthcare provider working in the aged and home care, disability, or allied health industries, Lumary is here to help you as a tech partner. For a software solution that can help you differentiate your business by putting people first, Lumary's next generation software is the perfect choice.
To find out how Lumary’s range of care management software can help you to improve client outcomes, book a consultation today. www.lumary.com
enquires@lumary.com.au linkedin.com/company/lumaryau instagram.com/lumary_au/ facebook.com/LumaryAU youtube.com/@lumary8738/featured
Using big data to find the best health care for older Australians
Big data is giving us a whole picture of Australia’s ageing pathways for the first time. Professor Maria Inacio is working with this data from the Registry of Senior Australians. She aims to find the best aged care and health care services for older Australians.

Big data is giving us a whole picture of Australia’s ageing pathways for the first time. Combining data to improve health care for older Australians
Professor Inacio is Director of the Registry of Senior Australians (ROSA) at the South Australian Health and Medical Research Institute. Professor Inacio helped set up ROSA in 2017. The registry combines health care and aged care data from around Australia. This combined data gives a whole picture of Australia’s ageing pathways for the first time.
“I’m a technical person. I love the challenge of working with data to learn new things,” Professor Inacio says, “I’m passionate about how we can use this information to improve care for older people.”
Evidence on aged care quality and safety
In the past, Professor Inacio used data from ROSA to give evidence to the Royal Commission into Aged Care Quality and Safety. “Our data influenced the Royal Commission’s recommendations. It helped drive reforms to aged care,” Professor Inacio recalls.
“For example, our data showed that when older people entered aged care facilities they received more psychotropic drugs. That evidence supported a recommendation to reduce the use of psychotropic drugs in aged care facilities.
“Since the Royal Commission, there has been better quality and safety monitoring and a better data strategy to evaluate aged care quality,” Professor Inacio says.
Finding the best health care for older Australians
Professor Inacio is now leading the first comprehensive nation-wide evaluation of older people’s use of primary health care and the effectiveness of this care in aged care settings.
Older people have more frailty, falls, chronic conditions and co-existing diseases. This means they have a high risk of emergency department presentations and hospital admissions.
These events often have poor health results including decline in function and quality of life. “Better primary health care could improve older people’s health and wellbeing,” Professor Inacio says.
“We want to find out how much primary health care older people get. We also want to know how care changes when people enter aged care facilities.”
Which health care services are best?
“93 per cent of people in aged care facilities visit a GP about 25 times a year,” Professor Inacio reports.
“But we don’t know the results of these visits or if they meet older people’s needs.
To answer that question, Professor Inacio is examining the relationship of primary health care services with:
• hospitalisations
• subsequent health encounters
• the length of stay at home or in residential care.
“I want to be able to find the services or best combination of services that an older person can get to do the best
they can. So, it’s better for them, better for the system and less expensive,” Professor Inacio explains.
The positive effect of preventive health care
In early results, Professor Inacio found there are three health care pathways for older people in aged care facilities. They have different mortality results:
• Older people who have preventive or multidisciplinary health care have the lowest mortality. This includes:
• ohealth assessments
• chronic disease management plans or multidisciplinary care plans
• medication reviews
• allied health services
• People who see a GP a few times a year and receive minimal other services have mid-level mortality. Professor Inacio says this is likely due to them having less health issues.
• People who see a GP frequently, including urgent, after-hours consultations have the highest mortality. Professor Inacio says this may be because they have declining health, but it also may be because their health care is not well managed. She is trying to work through this question now.
“It is reassuring to know that preventive health care can have a positive impact. We need to give people in aged care the best quality of life and the best experience they can have,” Professor Inacio concludes.
How much preventive health care do lder people get?
But Professor Inacio’s study shows that older people do not get as much preventive health care as they should.
“They should have chronic disease management plans and a health assessment and medication review every year. They should get more mental health and allied health services. “This may be enough to keep older people healthy with a stable level of functional capacity and prevent cognitive decline.
“But only about half of the people who are eligible for chronic disease management plans get them. The use of other services is even lower. This doesn’t change much or gets worse once they enter aged care settings, which is unfortunate.”
Professor Inacio’s research indicates more coordinated and comprehensive primary health care could improve the health of older people. This could translate into lower risk of hospitalisations and other health events. “This approach could also make immense cost savings,” Professor Inacio notes.
A community of stakeholders
Stakeholders who deliver primary health care to older people in aged care settings guide Professor Inacio’s research.
“That community will also help put our findings into practice,” said Professor Inacio.
Professor Inacio project “Using Big Data to Create Evidence-based Primary Health Care Service Delivery and Policy for the Australian Aged Care Sector—A Nationwide Study” received a $1.435 million grant from the MRFF. In 2021 the MRFF contributed to supporting ROSA with a grant of $2 million.

The future of positive ageing… Embrace it with Prolox!


Skin health matters. At Prolox, our formulators and skin experts work round the clock in providing out of the box smart solutions for both routine and prophylactic care.
Stratum corneum is located in the outermost layer of the skin and is the most important part of the skin barrier. It is composed of corneocytes surrounded by lipid matrix in equimolar quantity of cholesterol, fatty acids and ceramides.

The stratum corneum has the ability to prevent excess loss of fluids and electrolytes, and is mediated by the organization of the extracellular lipids into a series of parallel lamellar membranes which in addition to regulating permeability function also confer key protective functions of the epidermis. During aging, the following structures and functions of the skin barrier are changed or disturbed: (1) skin barrier structure, (2) permeability barrier function, (3) epidermal calcium gradient, (4) epidermal lipid synthesis and SC lipid processing, (5) cytokine production and response after insults, (6) SC acidity, (7) SC hydration, and (8) antimicrobial barrier.
Reductions in production of the epidermal lipids, are evident in the aged epidermis. Because formation of a competent epidermal permeability barrier requires an approximately equal molar ratio of cholesterol, free fatty acids and ceramides which are synthesized by epidermal keratinocytes, deficiencies in any of these lipids can result in a defective epidermal permeability barrier.
Moreover, levels of structural proteins for the epidermal permeability barrier, including filaggrin, loricrin and other late cornified envelope proteins, markedly decline in aged skin in comparison to young skin. Deficiencies in these proteins can result in a defective permeability barrier. Prior studies have shown that the aged stratum corneum displays a >30% reduction in total lipid content in comparison to young stratum corneum, due to reduced epidermal lipid synthesis, particularly in cholesterol synthesis, both under basal conditions and after barrier disruption
The mechanisms underlying reduced stratum corneum hydration in the aged skin can be ascribed to the reduced content of natural humectants in the skin.
1. Lipid content decreases in the stratum corneum of aged skin (ceramides exhibit waterholding properties)
2. Aged epidermis exhibits reduced levels of filaggrin and its metabolites, including transurocanic acid and pyrrolidone carboxylic acid, which are natural moisturizers in the skin.
3. Both sebum and glycerol contents are reduced in aged versus young skin

4. Finally, levels of aquaporin 3 decrease in aged versus young epidermis reduction in stratum corneum hydration. Aquaporin 3 deficiency-induced reduction in stratum corneum hydration is likely due to decreased glycerol content in the stratum corneum
Moreover, the skin barrier is assaulted in daily life by hot water, mechanical trauma, occupation related chemicals, tape stripping, detergents and solvents which depletes the skin of its lipids. Skin diseases are associated with barrier abnormalities and the geriatric patient may be suffering from them, also the skin is subject to barrier related defects in relation to the age of the individual. The impairment of water permeability function is responsible for Moisture Associated Skin Damage (MASD) which may also be aggravated by Medical Adhesive Related Skin injuries (MARSI). Also, MARSI can itself lead to impairment of skin permeability leading to barrier damage.
The skin barrier is governed by:


(A.) Non physiological lipids and (B.) Physiological lipids. The two class of lipids with their contrasting characteristics dictate the clinical situation where they are useful when formulated in the right proportions. The principles of barrier repair rests on three characteristics
1. Physiological lipids i.e. ceramides, cholesterol and free fatty acids in the correct ratios to correct the biochemical abnormalities and the deficient ingredient is used to correct the disorder in which it is deficient.


2. Non physiological lipids like petrolatum, beeswax restore function only transiently. They do not differentiate between the type of barrier abnormality achieving the same degree of repair in all cases.
Each of the three physiological lipids is required individually for barrier permeability. It has been seen that a formulation using the deficient lipid and other lipids in the ratio of 3:1:1 will accelerate barrier repair e.g. for aged skin it will be cholesterol 3: FFA 1: ceramides 1. However, using the lipids in equimolar ratio will lead to slower repair compared to when it is used in the optimal ratio. A recent study demonstrated that topical applications of an emollient containing stratum corneum lipids not only improved epidermal permeability barrier, stratum corneum hydration and skin surface pH, but also lowered circulating levels of proinflammatory cytokines in aged humans. Other natural ingredients, such as petrolatum, glycerol, coconut oil and sunflower oil, can also improve stratum corneum hydration and epidermal permeability barrier.
Barrier recovery can be further accelerated by increasing the proportion of any one of the three key lipids to a 3:1:1 ratio. The table below shows effect of physiological lipid mixtures on barrier recovery in the young versus the aged human skin.
Synergistic
How are we addressing the care and relief of ageing, fragile, sensitive &


compromised skin?
Imagine a skincare system that addresses all the concerns with ageing, fragile, sensitive and compromised skin from cleansing, moisturizing and protecting the skin, that will leave your skin feeling calm, restored and healthy again. The products have been designed using the right mix of physiological and non-physiological lipids in the right ratio with the aim to help reduce flares of existing diseases and to impart the right sensorial experience and to increase compliance by the age group. Prolox is an efficacious skin health brand that uses a unique and customized Oat Lipid Matrix. Using the optimal ratios of cholesterols, fatty acids and ceramides, known to assist in the care, relief and restoration of fragile, sensitive and comprised skin.
Formulated and tested by Dermatologists, Prolox preparation adheres to strict dermatological principles and practices using potent, efficacious ingredients. It has plant-based ingredients that are used for protection and nourishment of the skin, by acting as an antioxidant, soother, hydrator and calmative. The products are all formulated to have skin friendly pH 5.5 Prolox is also devoid of Parabens, Phthalates, Formaldehyde, Diethynolamine, Triclosan, BHT, BHA, Methyl isothiazolinone, artificial dyes & synthetic colours
3. Dressings which could be vapor permeable which allows metabolic repair to continue or non-permeable which shuts down metabolic repair process of the under lying epidermis. Find
Lipids are critical components of healthy skin. As our skin ages, the lipid content diminishes leading to imbalances in the lipid matrix in the skin, causing increased loss of moisture leading to dryness, fragility and sensitivity.PROLOX has optimal levels of cholesterol, fatty acids and ceramides, that work synergistically to enhance the lipid matrix, restore the skin barrier for protection from external elements and lock in moisture. Other plant-based ingredients are used for protection and nourishment of the skin, by acting as an antioxidant, soother and hydrator.
ENHANCING SKIN HYDRATION & PROTECTION
Formulated for rapid restoration of the barrier functions of the skin

Swedish Oat Lipid Oil and other plant-based ingredients for protection and nourishment of the skin



Skin friendly pH 5.5
NEW PRODUCTS
For stockist enquiries or to participate in a product trial offer, please email info@prolox.com.au



To order online, complete the order form on our website
Caring for Fragile, Sensitive and Compromised Skin


Lipids are critical components of healthy skin. As our skin ages, it leads to imbalances in the lipid matrix in the skin, causing increased loss of moisture leading to dryness, fragility and sensitivity. PROLOX has optimal levels of cholesterol, fatty acids and ceramides, that enhance the lipid matrix to restore the skin barrier for protection from external elements and locking in moisture.


www.prolox.com.au
Synergistic

AQUACEL® Ag+ Extra™ in a four year old wound


Clinical Case Background:
Mr PA is a 65 year old male with a history of IV drug use. He has suffered from bilateral venous leg ulcers for four years. Treatment has included advanced wound dressings and compression therapy. The wounds initially healed after one year of treatment but following a fall, both legs re-ulcerated and have not subsequently healed despite three times weekly redressing at the vascular clinic of a large tertiary hospital.




Methods:
On 25 July 2022 his right leg was selected to evaluate a new Convatec product: AQUACEL® Ag+ Extra™. This was used in combination with compression therapy and AQUACEL® Foam as a secondary dressing.
Week 0
The contralateral limb was treated with a ‘bioburden reducing’ primary dressing and superabsorber secondary dressing.
Results:
After just two weeks of treatment with AQUACEL® Ag+ Extra™ the wound had markedly improved.
Week 2
At week five it had reduced in size by more than 50%. The periwound tissue looked less macerated compared to the contralateral limb which was treated with different products, changed at the same frequency.

Conclusion:
It is known that biofilm is present in 78% of hard to heal wounds1 Biofilm is resistant to conventional treatments such as antibiotics and topical antimicrobials. The unique combination of MORE THAN SILVER™ technology in AQUACEL® Ag+ Extra™ ensures that biofilms lifted so that the silver can get to work, killing bacteria within the wound.
Week 5
CONTRALATERAL LIMB – NON-CONVATEC DRESSINGS
Week 8
Advance healing with AQUACEL® Ag+ Extra™ Dressings
WHY WAIT? YOU HAVE THE POWER TO DISRUPT AND DESTROY BIOFILM NOW!
3 2 1
Three wound healing barriers: Exudate, infection and biofilm
Prevents
biofilm formation & reformation
Up to 7 days wear time
Two powerful technologies: NEW Ag+ Technology
Revolutionary technology destroys biofilm and kills infection-causing bacteria.*
Hydrofiber® Technology
Proven technology that absorbs and retains excess exudate to help create an ideal healing environment.*

One wound healing solution:
Using our breakthrough MORE THAN SILVER™ technology – which contains ionic silver together with a surfactant (BEC) and a metal chelating agent (EDTA), our dressing delivers superior*, anti-biofilm performance compared to other silver dressings.
Effective under compression*
Soft, gentle, conformable and highly absorbent*
Can be pre-moistened
Easy to apply and remove
1800 339 412 www.convatec.com.au

To learn more about AQUACEL® Ag+ or to arrange a visit from your Convatec representative, please call New Zealand 0800 441 763 www.convatec.co.nz

The problems with set-and-forget medication in aged care
Up to 250,000 hospital admissions each year in Australia are linked to problems with medications.
As we age and our health begins to suffer, the simple solution would seem to be to take medications to address our ailments. But that can quickly lead to a bathroom cabinet full of medications and unintended adverse health consequences.
The reasons for how overprescribing occurs, and why multiple medications can cause problems are complex, but the underlying problem isn’t going away anytime soon.
Many developed nations have high and increasing rates of people with multiple chronic health conditions requiring ongoing medication. Data from the United States National Health and Nutrition Examination Survey suggests more than 90% of people aged 65 years and older have two or more health conditions. On the other side of the Pacific, the Australian Institute of Health and Welfare estimates half of all Australians aged 65 years and older have two or more chronic health conditions.
Not only does each condition typically result in a medication being prescribed to treat it, clinical practice guidelines used by health professionals increasingly

advocate combining different medications for the best therapeutic result.
Unsurprisingly, this has led to people taking multiple medications each day, a phenomenon known as “polypharmacy”, which can be defined as the concurrent use of five or more medications in the community setting, or nine or more medications in the residential aged care setting.
This may be necessary to best manage chronic health conditions, but it’s not without inherent – and sometimes hidden – risks. For the most part, prescribing multiple medications has been driven by results of randomised controlled trials demonstrating the benefits of medication treatments.
However, participants in these trials have often been younger and healthier than the average person prescribed these medications in practice.
The benefits and risks of medications prescribed to frail older people with multiple chronic health conditions may be different to benefits and risks among the randomised controlled trial participants.
Polypharmacy and complex medication regimens can be baffling to patients and increase the workload for carers, often those least able to manage their medications.
Research by Australia’s NPS MedicineWise, for example, suggests that two-thirds of Australians aged 75 years or older use five or more conventional or complementary medications each day. With multiple daily dosing, different medication formulations – some as tablets, inhalers, or patches – and special instructions for medication administration, such as take half a tablet on an empty stomach before meals, it’s easy to see why up to one-third of residents of aged care facilities have their medications administered on five or more occasions each day.
Unravelling the problem
While this all might seem to be worth if it means keeping patients well, the irony is that neither polypharmacy nor complex medication regimens necessarily lead to good health results for patients.
Polypharmacy increases the risk of drug-drug interactions and adverse drug events, while complex regimens can increase the risk of medication administration errors,
particularly in people with dementia, who are frail, or who may have difficulty self-managing their own medications.
It’s difficult to over-emphasise the scale of the problem. The Pharmaceutical Society of Australia (PSA) estimates that up to 250,000 hospital admissions each year in Australia are due to problems with medications. Work is underway to address it.
The World Health Organisation made “Medication without Harm” the topic of its Third Global Patient Safety Challenge, and in 2019, quality use of medicine and medicine safety was declared an Australian National Health Priority Area. Healthcare professionals around the world are also recognising that not all polypharmacy and medication regimen complexity is necessary.
It may be possible to discontinue or “deprescribe” medications that are no longer consistent with a person’s goal of care. Regular medication reviews performed by pharmacists and general medical practitioners can help identify unnecessary or inappropriate medications for which the benefits no longer outweigh the risks. In Australia, however, government-funded, collaborative medication reviews remain under-utilised both in the community and in residential aged care settings.
Simplifying a person’s medication regimen can also be achieved through strategies that do not necessarily mean changing the therapeutic intent.
In some cases, for example, it’s possible to reduce the number of daily administration times by administering different medications at the same time each day, or by
prescribing combination products that include two or more active ingredients in the same tablet or capsule.
In other cases, it’s possible to use long-acting formulations dosed once per day instead of using multiple short-acting products requiring multiple daily dosing.
Moves to improve medication safety
There have been a number of recent practice and policy developments to improve medication safety.
Australia’s National Aged Care Mandatory Quality Indicator Program has included a polypharmacy indicator (nine or more regular medications) since July 2021, and public-sector residential aged care services in the Australian state of Victoria now monitor the proportion of residents with more than four daily medication administration times.
If used proactively to provide feedback to clinicians, this data can help inform and evaluate improvements.
Better use of digital health applications, specifying the intended treatment duration on prescriptions, and including information on treatment discontinuation in drug information resources for prescribers could also help.
Advances in the availability of anonymised electronic health record data for research can help address evidence-practice gaps arising from under-representation of older people and those with multiple chronic health conditions in randomised controlled trials of specific medications.
Down the drain is into the water. We can do better than that.
Given the significant amount of evidence to show harm done to the environment, animals and humans when drugs are incorrectly disposed - too often down the drain - it's understandable why there are numerous drug waste disposal procedures required by law. For example, legislation states that opioids must be segregated from other waste at the point of disposal. Which is why using sharps is a big NO NO.

But we don't need laws to know that doing the right thing is a good thing. That’s why we offer a simple, compliant, cost effective, solution to help you dispose of your unused drugs. Developed by Drug Waste International, our Drug Waste Bins meet multiple legal and audit requirements with an easy, quick way to render drugs as ‘unidentifiable and unusable’ at the point of disposal, all of which helps make the world in which we live, a cleaner, healthier, and happier place. One audit, and you could be down the drain.
To claim your free trial or to find out how our Drug Waste Bins are being used by hospitals, clinics, and pharmacies, including cost/ benefits studies and testimonials, please don't hesitate to contact 1800 306 075 to discuss how you can ensure compliance, save money, and help keep your organisations safe and the waters of Australia clean.


Good news! For a limited time we are offering a free trial!
Research using routinely collected hospital and dispensing data is also a promising area for improving safe and effective medication use. This research will form the basis of more nuanced treatment recommendations that will better serve the needs of those most vulnerable to being harmed by medication.
Author:
Simon Bell, Professor, Centre for Medicine Use and Safety
Originally published under Creative Commons by 360info™. https:// newshub.360info.org/login?next=https%3A%2F%2Fnewshub.360info. org%2F
This article was published in Monash Lens under Creative Commons by 360info™: monash.edu/@medicine-health/2022/02/07/1384339/ the-problems-with-set-and-forget-medication-in-aged-care
JD Healthcare Group has established itself as a trusted provider of healthcare solutions
With over 20 years of experience in supplying products and training to clinical and support staff in hospitals across Australia, JD Healthcare has established itself as a trusted provider of healthcare solutions. In March 2020, we merged with two of our primary distributors to form JD Healthcare Group (JDHG), which has since become a leading player in the Australian healthcare market. In September 2022, we further expanded our operations with the launch of our Aged Care Division.
At JDHG, we are guided by our vision of "Looking after people, caring for people." We are dedicated to bringing our knowledge, expertise, and service reputation to the Australian Aged Care market, alongside the most costeffective and trusted products available. We believe that a safe working environment, with the most appropriate equipment and training, is essential for achieving the best outcomes for both residents and caregivers.
JDHG is committed to helping aged care providers maintain the highest standards of care and quality. In line with the National Aged Care Mandatory Quality Indicator Program, we are well-positioned to provide solutions and partner with providers to achieve compliance with 2 of the 5 quality indicators within the 7 Aged Care Quality Standards. Our specialized products and staff training are designed to support providers in pressure injury prevention and treatment, wound care, infection control, continence care, and facility evacuation during emergency situations.
Our Lift/Shift/Place program is at the heart of our Aged Care Division, and it engages us as a supplier of products and training to our customers in relation to manual handling tasks, such as resident repositioning in bed, resident fall retrieval, and fall prevention. We believe that proper training in manual handling can significantly reduce the risk of injuries to both residents and caregivers, and we are committed to providing the most effective solutions to support the aged care industry.

Thank you for considering JDHG as your partner in aged care. We are dedicated to providing the best care for your residents and ensuring the safety of your caregivers, and we look forward to working with you in the near future.
Best regards,
Rod Bowlden Business Unit Manager JDHG Aged Care Division
COMPREHENSIVE PRESSURE RELIEF
The Turn All™ System transforms a standard bed into an automated lateral turning patient support surface



Fits On Most Beds
Designed to be positioned under a static or dynamic mattress, on a standard bed, with or without electric profiling

Consistent and Controlled Turning
Automatically rolls user into a side-lying position, gently and quietly, reducing the need for manual handling intervention from care givers



Side Support Function
Reduces the risk of skin shear, while increasing the patient’s feeling of security, by slightly raising the edge of the mattress on the side they are being gradually and gently rolled towards


SCAN TO CONNECT WITH A PRODUCT SPECIALIST

JD Healthcare Group seeks out the best and most innovative medical devices available from around the world to ensure maximum staff safety and optimum patient outcomes

LIFTING HAS NEVER BEEN EASIER
The Raizer II Lifting Chair is the new and improved truly single-handed solution to lifting someone who has fallen with ease and dignity.


Faster, stronger, and more stable than traditional inflatable lifting cushions, the Raizer II Lifting Chair is an ideal solution for transferring someone who has fallen to a sitting or standing position


Easy to Assemble
4 identical legs and 2 identical back rests ensure correct assembly every time
Cleaning Friendly
Sleek surfaces make it possible to disinfect more easily
Remote Control
Purpose built storage cavity for remote, moulded to the side of seat casing

Emergency stop button is more intuitive
Adjustable Seatbelt


Independently adjustable seatbelt placed on the back rest ensures improved upper body stability when lifting fallen person.


SCAN TO BOOK A FREE TRIAL

JD Healthcare Group seeks out the best and most innovative medical devices available from around the world to ensure maximum staff safety and optimum patient outcomes





Medicine safety a major concern in Australian aged care
Nearly all older Australians in residential aged care facilities are at risk of ‘suboptimal prescribing’ of medicines, including under-prescribing, over-prescribing and high-risk prescribing, according to a new study from The University of Western Australia (UWA).

"The findings indicate that many people in aged care are at risk from medicines-related harm and that the prevalence and magnitude of the use of multiple medicines look to have increased in the past decade," said Dr Amy Page, WA Centre for Health and Ageing at UWA.
Professor Christopher Etherton-Beer and Dr Amy Page, from the WA Centre for Health and Ageing at UWA, led research published in Archives of Gerontology and Geriatrics on Polypharmacy and medicine regimens in older adults in residential aged care.1
The review, which examined the prevalence of suboptimal prescribing, comes in the wake of the Royal Commission into Aged Care Quality and Safety 2021 which found that quality use of medicines and medicine safety was important for the wellbeing of Australians in aged care.
“In our study, which used data from across 17 Australian aged care facilities from residents who were 65 years or older, we found that suboptimal prescribing affected 302 of 303 residents,” Dr Page said.
“Older people with multiple chronic conditions have potential to benefit from quality use of medicines but are at high risk of experiencing medicine related harm if prescribing is suboptimal.
“There are times when taking multiple medicines may be unsafe and the number of medicines, or the combination of medicines used, may increase the risk of poor health outcomes.”
The research found that most residents (92 per cent) were exposed to polyphamarcy, the use of multiple medicines, and were prescribed an average of between 14 and 15 medicines a day and at least one instance of potential under-prescribing was identified in 86 per cent of residents.
At least one instance of high-risk prescribing was identified in 81 per cent of residents and most participants (85 per cent) had highly complex regimens.
“The findings indicate that many people in aged care are at risk from medicines-related harm and that
the prevalence and magnitude of the use of multiple medicines look to have increased in the past decade,” Dr Page said.
“Our research also reveals the significant burden that the complexity of medicines is placing on not only residents at aged care facilities but also staff.”
Medicine safety became a policy priority in many countries when the World Health Organisation launched its Medication Without Harm initiative in 2017, which aimed to reduce medicine-related harm by 50 per cent within five years.
In Australia, the quality use of medicine and medicine safety became the newest National Health Priority Area.
FOOTNOTES:
‘Respite care’ can give carers a much-needed break, but many find accessing it difficult
To seek “respite” is to look for a break from strenuous effort to recharge and regroup. In the context of aged care, subsidised respite care provides temporary support to older people, which gives their carers a brief relief or “respite” from their caring responsibilities.

Carers look after a family member or friend who is frail or has a disability, mental illness, substance dependency, chronic condition, dementia, terminal or serious illness. Having access to respite services is crucial, as only one in five carers of an older person reports they can easily organise a friend or family member to help them out.
Access to respite can also improve a carer’s well-being, enable them to continue in their caring role, and postpone the need for an older person to move into permanent residential care.
However, in a recent survey, only 30.6 per cent of carers reported accessing respite in the previous year, and just over half of those who did were satisfied with it.
What is respite care?
Respite care is a support service for older people designed to give their carers a short-term break from their caring responsibilities. It can be planned or used in an emergency, such as when a carer falls ill.
In Australia, respite occurs in a variety of settings. The more formal residential respite occurs when an older person stays temporarily in an aged-care home. However, there is also a range of community-based respite services. These include “day stays” in local community clubs, overnight stays in dedicated “respite cottages”, as well as options for care workers to provide support in people’s own homes.
In 2020–21, 67,775 people received residential respite care, and 46,527 received community-based respite care.
While this may seem like a lot, it is small compared with the 428,500 people who are the primary carer for a person aged 65 years or older. And formal respite services accounted for just 3.2 per cent of all government expenditure on aged care.
Why don’t people use it?
Carers consistently report accessing respite care is difficult. The obstacles they face include:
• not enough residential respite care beds
• residential aged care facilities that do not routinely offer respite care
• respite providers that can’t support people with dementia and high care needs
• respite care that is not close to home
• assessment delays that mean carers can’t access respite when they need it.
The royal commission heard evidence respite care can be risky for the care recipient due to poor communication in the transition process. For example, health and medical information about care recipients tends to be stored across multiple systems, some of them paper-based. This leaves scope for errors when care recipients move into a new care system.
Potential providers of respite care also face financial disincentives to offer short stays. The cost of the admission process is relatively high, so providing residential respite care for less than two weeks may not be financially viable.

A lack of appropriate respite care has significant consequences for both carers and the family or friends they look after. As one carer told the royal commission:
“I have asked whether or not Betty can get respite care in Broome but I’m told that it is full. One time I had to go for a funeral out in the desert and I had to take Betty with me because I could not get her into respite care and I couldn’t leave her with other family. We drove over 1,000km to the funeral. Betty got sick and needed antibiotics. Having more access to respite care would make a difference, a big difference to me.”
What needs to change?
From 1 October [2022], funding for residential respite care [changed] to better align with the funding provided for permanent residents. This aims to remove the financial disincentives for providers and improve respite availability in existing aged care homes.
But given the strong preference for respite in smaller cottage settings, further resources could be directed to expanding the availability of community respite. The royal commission noted that, while these services exist, they are limited, particularly in regional areas.
Improving the uptake of respite care will require more active and personal support for carers so they have the skills and confidence to organise respite care.
The previous government committed extra funding for the Carer Gateway program to streamline access to respite care and provide more face-to-face support for people looking for local services.
Perhaps most importantly, respite care needs to be understood as a service for the carer as much as for the older person they care for. We need to understand carers’ needs so we can design and match services for them.
Authors:
Nicole Sutton, Senior Lecturer in Accounting, University of Technology
Sydney
Deborah Parker, Professor of Nursing Aged Care (Dementia), University of Technology Sydney
Gillian McAllister, Senior Research Analyst, Centre for Business and Social Innovation, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ respite-care-can-give-carers-a-much-needed-break-but-many-findaccessing-it-difficult-183976
Fixing Australia’s home-based aged care system
We know the system of home-based aged care isn’t working well – it lacks integration, is mostly labour-driven and susceptible to workforce challenges, and uses limited technology that could benefit older people and the staff working to help them.

Currently, there are more than 50,000 Australians on a waiting list for a home-care package. These people are frequently isolated, and are generally frail and grappling with a few health conditions.
They not only require help for personal care and home maintenance, but also a system of wellness checks and monitoring, to avoid premature hospitalisation or a move to residential aged care.

Support is mostly provided by family or close friends, if they’re lucky enough to have them nearby, but many require assistance from local council or government support programs, and those with the greatest need often require the Commonwealth-assisted Home Care Packages program.
Although there’s been an increase in funding for the Home Care Packages since the release of the report by the Royal Commission into Aged Care Quality and Safety, there are waiting times of up to 12 months for people to access them.
That’s a year when there’s a high chance of them ending up in hospital, rapidly moving into aged care, or even dying.
While the provision of sufficient home-care packages is being negotiated and delivered, we need to consider smarter ways of bridging the gap for people who are at risk.
There can be innovation in this area that capitalises on existing health support technology, such as personal alarm monitoring systems, that can help us integrate health and care responses for an older person’s needs, to ensure their safety and independence.
Our research at the National Centre for Healthy Ageing, based in the Frankston-Mornington Peninsula area,
looks at these technologies, including the MePACS. The system, housed within Peninsula Health in Victoria, has serviced more than 50,000 clients nationally for more than 30 years.
Two-thirds of people using MePACS are more than 80 years old and live with multiple chronic health conditions.
When the person requires assistance (fallen, feeling unwell, etc), they activate their alarm, triggering immediate call-back via the device to determine what assistance is needed – family or friends, emergency services or ambulance – and provides a daily check to ensure social connection and their wellbeing.
The research showed that this simple service led to a 30 per cent reduction in ambulance callouts, with annual cost savings of $1.5 million to ambulance services alone, as well as benefits in reduced hospitalisation costs, and quality of life for the individual.
Identifying those most at risk
The data from more than a decade of MePACS has allowed us to identify those most at risk of hospitalisation or admission to residential aged care via their patterns of personal alarm use, so we can predict need, and target our support systems to those who need it and when.
Soon, we hope to develop ways to match the caller with other services they may need – a GP, a physio, a nurse, or just even a friendly ear for social connection – and then help them navigate to these services, something many people grapple with.
This could be another cost-effective way to bridge the gap for people waiting for an aged care package, until they actually receive the package.
Of course, this isn’t a panacea for all who want to thrive at home, and some people will still require hospitalisation or a move to a residential aged care facility, but it keeps them safe while they’re on that waiting list.
There are many innovations that can bridge the gap for better support and care for older Australians in their home.
As we well know, the ageing of populations is inevitable –and the innovations are there for the testing. It just takes a forward-thinking government to invest in research and implementation of such new models, not only because they can be cost-effective, but because they have the ageing person’s needs at heart.
Author: Velandai Srikanth, Professor, Peninsula Clinical School, Director, National Centre for Healthy AgeingThis article was first published in Monash Lens. Read the original article here: lens.monash.edu/@medicine-health/2022/09/30/1384995/ fixing-australias-home-based-aged-care-system
Can pets help cure loneliness?
New research plans to find out.
There’s no doubt loneliness and social isolation are a problem for many people. A 2017 Relationships Australia survey found more than one-third (34 per cent) often felt isolated, and a further 43 per cent felt isolated some of the time.
There’s also little doubt that most of us enjoy the companionship of animals. But little research has been conducted on the benefits of the social interaction that dogs, cats, rabbits, birds and other pets provide.
My dog was a case in point when I had Greek neighbours who didn’t speak much English, and I spoke no Greek.
We didn’t share many words, but regularly interacted through my much-loved pet, Murphy, who helped facilitate contact between us and enjoyed visiting my neighbours when I was at work.
Language barriers were broken and a friendship formed.
The power of pets
More schools, universities, workplaces and care services are recognising the benefits of these simple but special interactions.
Some schools use dogs to combat student stress, and some aged care facilities have pets interact with residents. We know those involved enjoy this interaction, but just how beneficial is it?

Our project aims to find out.
Through the Living Labs Program of the National Centre for Healthy Ageing (NCHA), it will investigate whether bonding with animals can reduce loneliness and social isolation in at-risk groups.
It’s one of 13 NCHA Living Labs projects that have secured combined funding of $4.77 million in the program’s third round of grants. Round three projects

aim to empower people to optimise their health, while improving healthcare systems.
Our Monash University School of Primary and Allied Health Care pilot project will explore the benefits of regular interaction with others centred on a shared interest in animals.
Helping those at risk
Research has told us loneliness and isolation stem from a reduced sense of belonging and a lack of social connections. These risk factors increase as we age.
Members of excluded groups or minorities, such as international students or refugees and recent migrants, are also at higher risk due to a lack of social interactions or networks.
At its worst, loneliness and social isolation can lead to detrimental effects on physical health, increased incidence of depression, and suicide.
Our study will explore the way pets and the humananimal bond may reduce this sense of loneliness and social isolation in these groups. It will build upon my research over the past six years on the impact of humananimal interactions.
Keeping people connected
My previous studies examined the effectiveness of animal-assisted activity programs to facilitate conversations with community members. Using pet dogs as catalysts to social connection, they highlighted the potential for animal programs to encourage human interactions.
We found that regular conversations with others is an important way of staying connected, which in turn can improve physical and mental health and wellbeing.
The new project will focus on the potential benefits of animals as a social conduit for older people, and those from migrant and refugee backgrounds.
Although aged care settings have incorporated animals to relieve residents’ loneliness and isolation, there’s been little objective study of pets’ impact in aged care, and none into the impact of animal activities in refugee and migrant groups.

We now want to understand whether a shared interest in animals, explored in various ways, can help reduce feelings of loneliness and isolation.
Uniting pets and people
From May 2023, my team and I will enrol volunteers in the Pets and People (PaPs) Program, a low-cost animal-assisted activity group intervention proposed for aged care settings, also ensuring migrant and refugee communities are included.
Up to four partner aged care facilities across Melbourne and Queensland will host a PaPs group, with about 36 participants from the three target groups. Allied health students across Monash and James Cook universities will help implement the program.
The results will inform national approaches to tackling loneliness and isolation for our ageing population. This
is more important than ever as we start to emerge from the COVID-19 pandemic, which led to isolation for many, and compounded the isolation already felt by some.
COVID-19 restrictions showed how isolating loneliness can be, especially for at-risk groups such as residents in locked-down nursing homes, and recent migrants, refugees and international students who could not host or visit friends and family.
The way forward
The ultimate aim of this new program is to use pets to support social connection and healthy ageing.
We look forward to seeing the results of this important research, which we hope will confirm the critical role pets can play in avoiding loneliness.
This could lead to culturally appropriateness, possibly national in scale, at most if not all aged care facilities, and through groups working with migrants and refugees.
We hope this program can provide similar benefits to those shown on the ABC show Older People’s Home for Teenagers, which paired teenagers with older adults. Pets have the potential to be a key facilitator of interactions and could be particularly helpful on the first meeting when everyone is getting to know each other.
We don’t need research to tell us that a cute pet is the perfect ice-breaker for all age groups.
About the National Centre for Healthy Ageing
The National Centre for Healthy Ageing is a federally funded partnership between Monash University and Peninsula Health. The goal of the NCHA is to deliver national solutions for major challenges in healthy ageing through excellence in translational research.
Working with key partners across Monash University, Peninsula Health and other organisations, the NCHA conducts a wide range of research projects that look to improve the way Australians can age well and thrive in their communities, access care and support when required, and test innovative systems and models of health and social care for some of the most complex problems that impact on healthy ageing.
The key NCHA research programs fall under the Living Labs program. Running since 2020, it incorporates four projects in round one, three projects in round two, and 13 projects in round three.
These projects unite end-users and health consumers with the best researchers and clinical leaders in the field, along with community organisations, peak bodies, and industry partners to co-design and translate our research.
This open innovation approach ensures nationally scalable solutions that can be efficiently integrated into existing systems and practices, maximising impact for the people we’re trying to help.
Author: Em Bould, Senior Research Fellow, Occupational Therapy, Monash UniversityThis article was first published in Monash Lens. Read the original article here: lens.monash.edu/2022/11/14/1385253/ can-pets-help-cure-loneliness-new-research-plans-to-find-out?utm_ campaign=MLENS_UMC&utm_source=Lens_newsletter&utm_ medium=email&utm_content=lens_edm_bttn1
Physiotherapy fundamental to sustainable aged care
A new report on the future of Australian aged care highlights the need for better access to preventative and restorative healthcare services such as physiotherapy.

The Sustainability of the Aged Care Sector: Discussion Paper from the University of Technology Sydney (UTS) outlines significant funding issues and mounting supply and demand-side pressures in the sector.
The report warns of substantial consequences that will result without a multi-layered, strategic response from government.
The APA welcomes the report and its emphasis on preventative and restorative healthcare as a means to promote sector sustainability. Physiotherapy care is a substantial and presently under-tapped resource in this space.
“We have an ageing population that is increasing demand for aged care services and residential facilities, current arrangements are fraught and far from future proof,” APA National President Scott Willis said.
“Preventative, ongoing and rehabilitative physiotherapy care enables older people to stay healthier and independent for longer. Greater access to these services can reduce pressure on acute services and reduce the demand for residential facilities.”


The 84-page report advances four strategic approaches to government including, “improving the effectiveness of aged care services”.
Under this banner, the research team stress the critical role of restorative and transition care programs that reduce and defer the need for more highly subsidised services, reduce caregiver burden and minimise applications for permanent residential care when older people have been hospitalised.
“In the case of people with dementia, restorative care can avoid or postpone the need to access residential aged care,” the report states.
“Reducing the rate of growth of demand for subsidised aged care services” is another strategic approach. The findings centre the need for beneficial health interventions that “promote wellbeing earlier in life,” “help people cope with frailty and chronic disease while remaining at home” and “reduce dependency in older age”.
This approach places emphasis on beneficial health interventions including improving access to primary and allied health. Physiotherapy care has proven preventative health benefits and value to offer for falls prevention and mobility in both home-based and residential aged care.
“Lifelong access to physiotherapy maintains health and sets people up for a better ageing process, avoiding chronic disease progression,” Mr. Willis said.
The researchers also document the need for more timely and transparent assessment of older people’s needs and
that assessment should be conducted by a workforce that is “resourced, qualified, attuned to the diversity of individuals’ needs and backgrounds, and independent of aged care providers.”
“Improved assessment processes may better support older people to access restorative and transition care programs,” the report found.
“Appropriate and regularly reviewed clinical assessments backed by adequate, targeted funding applied consistently across home and residential care will support high-quality care regardless of setting,” Mr. Willis.
The Sustainability of the Aged Care Sector: Discussion Paper was commissioned by the Australian Aged Care Collaboration with input from Council on the Ageing Australia and National Seniors Australia. The report can be found on the University of Technology Sydney’s websit: https:// opus.lib.uts.edu.au/bitstream/10453/158194/2/UARC_Sustainability%20 Discussion%20Paper.pdf
Rehabilitation Services essential for 2021

On The Go Rehabilitation Services is a mobile service that delivers therapies including physiotherapy, exercise physiology, occupational therapy, dietetics, speech therapy, podiatry and massage in the comfort of the clients home or in their preferred locations.
If we have learnt anything from 2020 it's the importance of remaining healthy and independent. In the midst of the pandemic the services provided by On The Go Rehabilitation Services were considered an essential service, to help keep people out of hospital through falls prevention and rehabilitation. Exercise was one of the few things that we could do - and were encouraged to do - during the toughest period of restrictions.
Wanting to remain independent for as long as possible is instinctual and most seniors simply desire to continue doing the things they love to do. We don’t want to have to rely on others. The longer we are able to remain independent, the better for our health, both physically and mentally.
By providing holistic home treatments On The Go Rehabilitation Services is able to focus its approach on each person’s individual needs. The treatment programs are done in collaboration with the patients and their carers. Our patients are our family. We are here for them to help them achieve their goals and live their best possible life as independent as they can. This belief is held by every On The Go Rehabilitation Services team member across numerous allied health disciplines.
“The motivation that drives On The Go Rehab is the memory of my gran,” says Ms Thompson. “She passed away at the ripe young age of 101. She lived at home alone, could cook up a storm and was able to drive her car with no assistance. She was, and still is, my inspiration. She taught me many things but most importantly she instilled in us the importance of looking after each other.”
The therapists that work with us are driven by the same treatment ethos; focusing on the patient and their goals. We can assist with a range of conditions, including but not limited to; fall prevention, stroke rehabilitation,

diabetes management, weight control/management, speech disorders, general fitness, orthopedic rehabilitation, disabilities, neurological conditions, chronic disease and general mobility.
On The Go Rehabilitation Services is NIDS registered and DVA, Medicare and home care package approved. Private Health rebates are also available.
For more information:
Email: info@onthegorehab.com.au
Website: www.onthegorehab.com.au
Could Hydro energy power your retirement income? We hope so
Wary of risking your savings on the share market? Then Snowy Hydro 2.0 should be for you. We reckon it’s safer and builds a better Australia.
National Seniors Australia believes the Federal Government should open up the Snowy Hydro 2.0 scheme to seniors and mum and dad investors looking for stable government-backed returns.
That’s a key priority of National Seniors’ Federal Budget submission, which calls on the government to issue Snowy Hydro 2.0 Green Bonds and open up nation building opportunities for older Australians.
About the Snowy Hydro Project Snowy Hydro 2.0 is a significant infrastructure project to enhance and extend the energy generation capacity of the existing Snowy Hydro scheme.
It will use a series of pipes to pump water back up the mountain to supply energy to the grid.
The project will fill some of the growing need for energy storage required to meet demand in peak times. Initial estimates show a healthy investment return of 8eight per cent.
National Seniors believes the Snowy Hydro 2.0 project provides an exciting opportunity to help stabilise energy prices and support environmental sustainability for future generations.

Most of all, the green bonds would help fill an investment gap for seniors who are forced to rely on the share market to generate income above the inflation rate.
Creating a better future for everyone
National Seniors research shows that the average 80-year-old does not want to play the stock market, has little or no superannuation and seeks security in bank deposits, partly because they are backed by a government guarantee.
The green bonds would be backed by government and could potentially offer a higher return on investment than a bank deposit.
Many older Australians want to make a contribution to future generations, and ensure the environment
is protected and improved for their children and grandchildren.
In the National Seniors Social Survey, 74.3 per cent of respondents believe that climate change is occurring while 58.6 per cent want action, event if it increases living costs.
We will continue to consult with our members to develop a campaign that helps older Australians protect the environment for future generations.
For more information go to National Seniors Australia: nationalseniors.com.au
How to choose a legal decision-maker as you get older
“It’s my life and I’ll do what I want,” sang Eric Burdon of The Animals to the babyboomer generation. Unfortunately, that’s not always the case. As we get older, sometimes we’re no longer capable of making our own decisions. Diseases that affect the brain such as dementia, stroke and head injury can impair cognition and thinking.

Some people may choose to appoint a medical treatment decision-maker or an enduring power of attorney to make certain decisions on their behalf. Alternatively, a legal tribunal or court may appoint a guardian or trustee to help guide decisions about healthcare, finances, accommodation and lifestyle.

Who is the right person to take on this important role? Is it the family member or partner who knows you best? Or someone with time and energy? Perhaps someone who understands the services you need – such as a nurse, accountant or real estate agent?
The role of a decision-making representative has changed significantly in recent years, shifting from a paternalistic approach to a more person-centred focus. Our research looks at the differences between these approaches, and how subconscious bias can influence decision-making.
Taking care
These days, guardianship has moved from deciding what’s deemed to be in the individual’s “best interests” to what best reflects their “will and preferences”.
While previously, decisions were made for the person by their guardian or representative, new laws require representatives to enact the person’s “will and preferences”. That is, to make decisions with them.
This is an important difference. The newer model gives the represented person more autonomy over personal, financial and other decisions. It recognises that even though a person may struggle with aspects of decisionmaking, they should not be excluded from decisions about how they live their life.
This fundamental shift was earlier adopted by the United Nations in the Convention on the Rights of Persons with Disability, to which Australia is a signatory.
Challenging in real-world situations
The will and preferences framework may sound simple, but it can be challenging in practice, when concepts of empowerment are tricky to define and the will of someone with cognitive difficulties is hard to discern.
Representatives bring their own biases, perceptions and lived experience to the role of supporting another person to make decisions. This subjectivity is a natural and an inherent part of decision-making. The representative faces the challenge of setting aside their own opinion and, instead, stepping into the shoes of the represented person to give effect to what they want.
A mismatch between the age, gender, ethnicity, religion or socioeconomic status of the representative and the represented person can exacerbate this challenge.
An older able-bodied female, who is deeply religious and from a middle-to-high-income background might find it difficult to represent a young man with a disability who is an atheist and from a working-class background. Now, imagine a scenario where the young man expresses a desire to go bungy-jumping or parachuting, despite previously showing a fear of heights. What’s his representative to do?
Older people and women generally have a lower appetite for risk, as do those who have a faith and with a high socio-economic status.
A heightened perception of danger or a feeling the activity is frivolous may lead to the representative reframing the situation with their subconscious bias. They may fail to respect the younger person’s will and preferences.
Understanding what might shape a representative’s approach to decision-making is essential. Especially when decisions involve health or living arrangements.
THREE THINGS TO LOOK FOR WHEN SELECTING A LEGAL DECISION-MAKING REPRESENTATIVE
1. Deep understanding
An intimate understanding of your situation is crucial. An ideal representative is someone who actively listens and has a holistic view of your circumstances. This may come from discussions with you and your loved ones. The representative must be careful your views are not outweighed by those of family or friends who are often more vocal. They should have a deep sense of who you are as an individual.
2. Self-awareness
The person you choose should be able to describe their personal views and values, and understand how their perspective may influence their decisions. This is vital to mitigate the effects of pre-existing bias. They should be able to reflect on their own lived experiences, to understand how their history shapes their approach to decision-making. They should be able to assess whether what you would do is the same as what they think you should do, and why.
3. Effective documentation
A record of conversations between the representative and represented person often helps to illuminate a person’s will and preferences. Writing or recording compels us to commit to an idea and explain what we mean. It helps to clarify what is intended far better than a one-time conversation that may be remembered differently by participants.
Further research is needed to better match representatives with represented persons. Improved tools are needed to identify the role of bias in decisionmaking, and evaluate whether the represented person’s wills and preferences are being respected.
Authors:
Joseph Ibrahim, Head, Health Law and Ageing Research Unit, Department of Forensic Medicine
Amelia Grossi, Research Assistant, Victorian Institute of Forensic Medicine
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ how-to-choose-a-legal-decision-maker-as-you-get-older-3-things-toconsider-177631
Simple steps to make planning for Aged Care easier

Need to move to residential aged care but don’t know where to start? With over 25 years’ experience as a financial planner, Derek Armstrong, CEO of Aged Care Financial Advisors, has seen families struggle through the maze of personal and financial decisions to be made.
“It can be daunting,” says Derek, “but early planning and good advice can minimise the stress for you and your family.”
When individuals start investigating the ins and outs of aged care services, they discover it’s not a simple process. There is a lot of information. There are a lot of choices to be made. There is a lot of fine print that impacts how you arrange your affairs as well as fear, worry and overwhelm for families concerned about making a rushed and costly mistake.
“Our number one piece of advice for families is to plan early,” says Derek. “The best way to kick off the planning process is to hold a family meeting to make some shared decisions.”
At this meeting, Derek recommends:
• Discussing options and preferences for aged care
• Exploring each person’s concerns
• Deciding who in the family needs to be involved in any planning
“Frank and open discussion is the first step to an effective decision-making process.”
The next thing to consider is the type of care that is needed - in your home or in a residential service. To help you decide which option is best, a free assessment can be arranged by an aged care assessment team or service (ACAT/ ACAS).
“You will need to have ACAT/ACAS approval before you can access government subsidised services.” Derek adds.
When residential care is needed, it is important to think about what’s essential to you in deciding where to live. Making a list that includes specifics about location, amenities and your health care needs is a sensible next step.
“These essentials will help you develop a short list of potential services you might like to contact or visit,” says Derek. “Don’t forget to first check what fees will be asked for accommodation to ensure it is affordable for you.”
“Understanding the costs involved is another really important piece of the puzzle that worries families,” Derek continues. “Residential care costs are divided into contributions towards accommodation, care and additional services.”
How much you pay may depend on:
• The service you choose
• Your assessable assets
• Your assessable income
The total payable can be hard to calculate without good advice.
“The first cost in the equation to understand is the accommodation payment. This is a contribution toward the cost of the land, buildings, and maintenance. You can choose to pay a lump sum (RADS) or a daily payment (DAPS) or a combination,” notes Derek.
Refundable accommodation deposits (RADS) are paid as a lump sum. The amount you pay is fully refunded when you leave unless you ask for other fees to be deducted from the RAD or you have outstanding fees when you leave. Repayment is guaranteed by the Federal Government if paid to an accredited aged care service.
Daily accommodation payments (DAPS) are like paying ‘rent’ or interest on any unpaid RAD.
“You will also be asked to contribute toward the cost for your daily care through a fixed fee.”
This fee can be calculated in one of two ways. Either:
• Basic daily fee at a rate of 85 per cent of the basic single age pension.
• Means-tested fee is payable if you have income and assets over specified thresholds. This amount is limited by an annual cap and a lifetime cap.
“An aged care financial adviser can explain the fees and calculate an estimate of what you may be asked to pay,” says Derek.
Depending on your assets and income, concessions on accommodation payments may be available. “There are a few things to consider here. While you can be assessed by Centerlink and approved for concessions before you accept a place, I cannot stress the importance of accessing your financial options before taking this step.”
“Completing a comprehensive review of your financial situation will ensure you can create sufficient cashflow and maximise your estate. Another really important step we would recommend is booking in some time with a certified, aged care financial advisor. They are across all the specific details and can explain how different options affect how you fund your aged care plan,” says Derek.
Key Financial Decisions to consider before moving to residential care:
• What should you do with your family home?
• Is it best to pay a RAD or DAP for accommodation?
• How is your Centerlink / Veterans Affairs’ pension affected and can this be improved?
• What are the best investment options for any surplus money?
• How to manage any taxation implications?
• What are the implications to your estate?
As part of the process, a qualified aged care financial adviser will develop an appropriate strategy to help you make key financial decisions. This will include advice on how to structure assets to pay for accommodation, as well as create sufficient cashflow. This may also include strategies to minimize fees or maximise Centerlink or Veterans Affairs benefits.
“When you start the planning process early – you give yourself the best opportunity to get the aged care and lifestyle you want. And the secondary benefit is when the time comes to make the move to residential care, it is stress free for you and your family,” reassured Derek.
To make an appointment, call our team on 1300 554 393.
Transitioning to aged care can be challenging for the whole family. There


are many decisions to make and the options can be confusing.
Aged Care Financial Advisors (ACFA) have the industry knowledge and understanding of the complex financial issues surrounding aged care to support individuals and families navigate through the system. We listen to your needs, answer your questions and provide comprehensive information. Get the peace of mind you deserve. Let us guide you in your Aged Care journey and help you choose an option that best suits your unique circumstances.
Our fixed fee service includes:
4 Strategy options
4 Education and support
4 Assistance with Government agency paperwork
At ACFA, our inclusive and proactive approach can show you how best to afford your preferred Aged Care service or facility and look after your family.

Budgie battle at B'nai B'rith
Retirement village operators should monitor the progress of a matter before the New South Wales Civil and Administrative Tribunal (NCAT) to understand the extent to which NCAT may find that Village Rules are unjust, oppressive or harsh.
The Appeal Panel of the NCAT commenced 2023 with a decision about a resident keeping budgies contrary to the Village Rules at B'nai B'rith, a Jewish retirement village in Rose Bay.

Whilst the budgies will be blissfully ignorant of it, the decision calls into question the enforceability of Village Rules which are clearly communicated to residents prior to entering into and consistent with Village Contracts.
Retirement village resident fails in initial NCAT proceedings seeking to modify the operation of a village rule concerning pets
Mr Kary entered into a Village Contract in 2018 to reside at Princess Gardens Retirement Village at Rose Bay. Clause 26 of the Village Contract stated "apart from (fish which you keep in your premises) you must not keep or allow any pets or other animals in your premises… (which include) but are not limited to birds, cats, dogs, and any other companion animal."
The Village Contract also contained Village Rules which included at Rule 5: No dogs or cats allowed. You may keep fish in your premises at any time, without the need to let us know or get our consent. For safety of other residents, no other
animals (including birds, cats, or dogs) are to be kept in your premises or brought onto common areas at any time. In the initial Tribunal proceedings, Mr Kary sought an order under Section 54(2)(b) of the Retirement Villages Act 1999 (Act) modifying the operation of Rule 5 to enable him to keep a maximum of two budgerigars on certain conditions, including that he must keep the birds in their cage.
Under Section 54(1) of the Act: The operator of a retirement village or a resident of the village may, at any time, apply to NCAT for an order in relation to either or both of the following--
(a) a dispute concerning the legal validity of a village rule in force in the village,
(b) a village rule in force in the village that the operator or resident considers to be unjust, unconscionable, harsh or oppressive.
Under Section 54(2) of the Act, NCAT may make an order:
(a) setting aside the village rule concerned, or
(b) modifying the operation of the rule in its application to a resident or to some or all of the residents of the village, or
(c) upholding the rule.
The initial Tribunal proceedings were decided in favour of the Operator because the Tribunal Member held Mr Kary did not have reasonable grounds to believe that Rule 5 was unjust, oppressive or harsh.
In Paragraph 74 of the initial determination of the Tribunal, the Member held "In considering whether the belief held by the applicant is reasonably held, it is necessary to consider the relationship in contract between the applicant and the respondent (that the resident was a non-registered interest holder) and the basis upon which the applicant is entitled to believe that the terms of the contract he signed in 2018 have now become harsh or oppressive…It could not be said that the (Village) Rules inhibit unreasonably the right to enjoy the occupation of the Village which (Mr Kary) expected in 2018."
The initial decision essentially turned on the fact that as an unregistered interest holder (with rights similar to a
tenant) who signed a Village Contract clearly prohibiting the keeping of birds, Mr Kary could not reasonably consider that it was unjust, oppressive or harsh for him to be prohibited from keeping birds.
The initial Tribunal Member never considered whether or not Rule 5 was unjust, oppressive or harsh because they determined that Mr Kary did not have reasonable grounds to believe it was. Retirement village resident successfully appeals, Appeal Panel sends matter back for reconsideration
The Appeal Panel allowed the appeal because Section 54 of the Act does not require a resident to have reasonable grounds for their belief that a village rule is unjust, oppressive or harsh.
As long as the resident considers that the village rule is unjust, oppressive or harsh, the resident has the right to commence proceedings. The Appeal Panel held "the resident did assert that the Rule was unjust, and/or that it was oppressive or harsh, as it applied to him.
There were questions of fact in the application of (section 54 of the Act) to the case before the Tribunal, which were simply not answered by the Tribunal Member, or dealt with adequately, or at all, in his Reasons. These were errors on questions of law. The Tribunal Member did not consider whether Village Rule 5 was, in fact, unjust. The Tribunal Member may have considered whether, or not, a belief was reasonably held by the resident that the Rule as it applied to him, was harsh or oppressive, but this was the wrong question."
The Appeal Panel sent the matter back to NCAT's Consumer and Commercial Division for a differently constituted Tribunal to reconsider Mr Kary's application.
Considerations for retirement village operators in light of the successful appeal Retirement village operators should be mindful that as long as a resident considers that a village rule is unjust, oppressive or harsh, the resident has the right to seek orders setting aside or modifying the application of the rule to them.

When residents raise concerns about Village Rules, operators should look beyond the language of the rules and village contract and consider whether or not the rule applies generally, or to the particular resident in a way that is unjust, oppressive or hash.
Author: Nicola Arvidson, Special Counsel, Colin Biggers & PaisleyThis is commentary published by Colin Biggers & Paisley for general information purposes only. This should not be relied on as specific advice. You should seek your own legal and other advice for any question, or for any specific situation or proposal, before making any final decision. The content also is subject to change. A person listed may not be admitted as a lawyer in all States and Territories. © Colin Biggers & Paisley, Australia 2023.

Staying Ahead of the Curve: Ensuring Compliance with Aged Care Reforms - Tips for Success
Aged care is a challenging field that requires quality-focused compliance to ensure the safety and well-being of older Australians. With various changes happening simultaneously, it can be overwhelming to keep up with everything. However, complying with the reforms is crucial. So is providing person-centred and safe care.
The last six months have seen many changes, including financial and reporting, and the introduction of the Code of Conduct across the sector.
Star Ratings and changes to National Quality Indicators for Residential Care.
Home Care has had the Serious Incident Response Scheme (SIRS) commence, caps on administrative charges and a ban on exit fees, along with the requirement to follow pricing transparency requirements, updating profiles on My Aged Care and developing a new pricing schedule!
Reporting of Care Minutes and 24/7 RN care will also be mandated for most of the Residential Care market and Home Care will have further significant changes to its service model, moving towards a total reform in 2024.
And to round it all out, the Aged Care Quality Standards review has been released, and pilot testing for the revised standards is now underway.
Many of these changes aim to improve transparency and partnerships with older people and support more effective person-centred care. However, these are just the start, you and your team need to take a proactive approach to address reforms as they roll out.
But as a care provider, how do you manage this without waking up each morning with a sense of dread and throwing your hands up in the air?
1. Identify and prioritise time for implementing the reforms – the Aged Care Quality and Safety Commission and the Department of Health and Aged Care publish helpful information. After deciding which reforms apply to your organisation, work out which of your policies, procedures, and other documents need to be updated, and identify any other gaps that require attention.
2. Establish a team to share the load and assign tasks to competent individuals who can update policies, forms, and your training plan. If you don't already have a Quality Care Advisory Body (QCAB), this new team can potentially form the basis of your new advisory body.
3. Document issues and improvements against your plan for continuous improvement. Record case studies demonstrating your compliance, or how you addressed gaps, implemented positive changes, or mitigated risk.
4. Regularly check in on your team's progress in implementing the reforms and remember to celebrate achievements along the way.
5. Continue reviewing and refining your policies, procedures, documents, and training as the reforms are introduced. You don’t need an expensive automated platform to do this – you can use an Excel document Management Map or Compliance Register. If you want to know how - book a free 30-minute consultation here: https://cdcs.com.au/book-a-call-with-cdcs/
6. Don't go it alone. Reach out to your peers in the industry, network with other providers, and share experiences, ideas, and solutions to common challenges. By connecting with others, you can learn from their experiences, get feedback on your approaches, and gain new insights into managing the reforms in your organisation.
7. Seek external help from trusted and reliable sources that are up to date on the reforms and understand your service context, challenges, and goals.
The CDCS team has developed a range of videos on our YouTube channel, ‘Aged Care Answers’ that covers many of these reforms and can support your team in understanding how to apply the changes. They are in plain English, bite-sized and conversational – so great for busy staff and those from a culturally or linguistically diverse background (CALD).
And, if you're struggling to keep up with the changes, don't stress. As a trusted compliance specialist long-time panelist and supplier to the Department of Health and
Aged Care and the Quality Safety Commission, CDCS can partner with your care team to ease the burden.
If you need help keeping up with the changes, consider reaching out to CDCS for 1:1 mentoring, tailored consulting support, or up-to-date policies and procedures, documents, and staff training resources that are easily customised to suit your organisation’s needs. Take the load off your shoulders and let us do the heavy lifting, freeing you up to focus on care. We’re committed to supporting providers navigating the changing landscape of aged care, ensuring you remain compliant and equipped to provide consistent, quality, and sustainable care.
Compliance can be daunting in the face of high workforce turnover and time constraints; this can be especially difficult for small teams. However, achieving compliance is within your reach with the right approach, resources, and support.

CDCS is committed to assisting providers with compliance and helping embed a culture of quality care. If you want access to Industry experts with a proven track record, reach out to us, we’re happy to have a conversation.
culturallydirectedcaresolutions.com


Affordable, Stress-Free Compliance
Accessible, clear and up-to-date resources to help you: Plus
Apply Policies & Procedures that all your team can understandResidential and Home care included

Capture and monitor compliance through a range of Registers, Forms and Audit tools
Give your Care Team the resources they need to assess, plan and provide quality care with confidence

Understand and manage your Governance and Regulatory requirements with Reporting Templates & up to date Guides
Educate your team with relevant Aged Care Toolbox Talks & other Training tools
Keep up to date with reform requirements through fortnightly online training - live and replay
cdcs.com.au

For more information scan the QR code or email: info@cdcs.com.au

Become an approved aged care provider and expand your aged care business

As the aged population is growing in Australia, the need for a range of care, accommodation, hospitality, and other services is undeniable. To address this growth, the Government has rolled out a $23.9-billion-dollar scheme to this sector 2020–21 with a further increase to $27.1 billion in 2023–24 that can open new windows for the businesses that offer quality aged care service to more than four million elderly Australians.
The Government subsidises approved providers under the Aged Care Act, making them more affordable and accessible to eligible care recipients.
So, as the cost of your services is subsidised to make the help your client needs more affordable, you will have more potential clients compared to the Non-governmentfunded services, which will charge their clients the full cost to access their services.
As an approved aged care provider, you can offer any of the following services according to your approved scope of services:
• Home care services: provide a range of services that help elderly people live independently within their homes. The Home Care Package (HCP) is suitable for those with greater or more complex care needs who need many cares and support services on an ongoing basis beyond the Commonwealth Home Support Programme (CHSP). There are four levels of care that can be assigned to the senior people, from basic assistance to high-level care.
• Residential care services: provide a range of care, accommodation, hospitality and services, using a residential facility (nursing home) for older people who are unable to continue living independently within their own homes.
• Flexible care services: provide a range of care and services for a period of time that may be delivered in a home care setting, a residential care setting, or a combination of both. Flexible care acknowledges that the needs of aged care consumers may require a different care approach than those provided through the residential care and home care services. It includes Short Term Restorative Care Programme (STRC), Multi-Purpose Services (MPS) Program, Transition Care Program, and National Aboriginal and Torres Strait Islander Flexible Aged Care (NATSIFAC) Program.
If you have found this process very complex and timeconsuming, if you are too busy with your day-to-day operation, if you are unfamiliar with the My Aged Care registration application process and get stuck in many web pages and other resources, if you do not know where to start or how to find the relevant information in one place, and if you want to get this process done correctly, you are at the right place now.
At ISO Consulting Services, we support you to make the confusing and stressful registration process easy and hassle-free. We save your time and money by providing you with all the documents required to meet the Aged Care Quality Standards. Using our services listed below, you can rest assured that you complete the lengthy and frustrating registration process successfully through our GUARANTEED services (T&C applied).
Silver Package
• Extensive Frequently Asked Questions (FAQ)
• Aged Care Documents Package including policies and procedures, forms and other templates, handbooks and other documents.
• Your access to additional services through our business alliances for all you need, including business registration, business finance, accounting and taxation, marketing, IT support, website development, insurance and more at a DISCOUNTED fee
• Ongoing assistance with your questions on the documents and clarifying them
• Our Silver Package
Gold Package Supplementaries
• Help you complete and submit the application form to the Aged Care Quality and Safety Commission
• Help you deal with the Aged Care quality assessor and facilitate the assessment process
To have a FREE consultation session with our experienced and knowledgeable team, please get in touch with us
• Melbourne Office: 03 9190 8986
Melbourne@isoconsultingservices.com.au
• Sydney Office: 02 8935 9472
Sydney@isoconsultingservices.com.au
• Brisbane Office: 07 3726 9590
Brisbane@isoconsultingservices.com.au
• Peth Office: 08 6165 8864
Perth@isoconsultingservices.com.au
ISO Consulting Services
An Australian consultancy firm A successfully servicing Health Care compliance schemes such as NDIS and Aged Care, helping companies start a new business, improve their management systems, enhance their productivity and efficiency and maintain a Safe & Healthy work environment and last but not the least, achieve the relevant registration and approval through a hassle-free process and the lowest cost.


We offer our professional consulting services in all states as we are familiar with both the Commonwealth and state legislation.



What we offer?
• Provide the required documentations
• Answer all questions during the implementation
• Assist you with completing the application form
• Assist you with addressing the assessor’s comments and findings


Job burnout is a serious health issue
Across all industries, burnout is becoming an increasingly prevalent and serious health issue. Amplified by the exhaustion and stress of working through the COVID-19 pandemic, burnout has affected many of us, from stretched-thin essential workers to those navigating the new territory of working from home and juggling homeschooling.

Burnout extends beyond simply being exhausted by work. It’s defined as a syndrome conceptualised as resulting from chronic workplace stress that has not been successfully managed, and has been included in the World Health Organization’s 11th Revision of the International Classification of Diseases (ICD-11) as an ‘occupational phenomenon’.
It is important to note that burnout is related to work specifically – not other areas of life. It has not yet been classed as a medical condition, distinguishing it from diagnosable disorders such as depression and anxiety. Hence, if the indications of burnout are recognised and the issues addressed, then burnout will resolve.

How do you know if you are suffering burnout?
There are three tell-tale signs:
• feeling depleted of energy or exhausted
• experiencing an increased mental distance from one’s job, or feeling negative or cynical about one’s job
• reduced professional efficacy – feeling incompetent and inept at work
Understanding the risks
Long-term exposure to stress can lead to burnout, and certain occupations are at greater risk. These include police and emergency service workers, teachers, healthcare workers, and legal professionals. However, anyone can be susceptible to burnout if they experience a high workload or stressful work environment for an extended period of time.
Some common risk factors include having limited support at work, being overloaded, experiencing role conflict/ ambiguity, having low work satisfaction, lack of supportive supervision, and being younger or less experienced.
In order to counter such risk factors, workers should endeavour to boost those things that help protect their mental wellbeing.
How can I protect myself?
• Look after yourself by getting plenty of rest, regular exercise, and eating regular, well-balanced meals.
• Minimise your intake of alcohol, caffeine, nicotine or other drugs
• Make time for relaxation
• Try to schedule at least one enjoyable activity each day
• Spend time with people you care about
• Seek peer support at work
• Recognise your limits and maintain strong boundaries at work
• Seek professional support if you feel you need it
How can I support my employees’ wellbeing?
Organisations can do a lot to help prevent burnout in their employees, including providing effective leadership, a supportive team environment, realistic workloads, evidence-informed workplace policies, and access to useful resources and training.
Phoenix Australia can support a wide variety of organisations to minimise employee burnout and its impacts by providing best practice advice on service development and policy. There has been increasing interest from organisations aware of the importance of supporting the psychological health and wellbeing of their workforces.
In 2019, a training program was specifically designed and delivered for Court Services Victoria for 100 professionals working within the Children’s Court Family Division. Training was delivered in Melbourne and regional centres. The training provided a framework
for wellbeing and resilience to help workers look after themselves and decrease their risk of suffering burnout. Participants explored the elements in their own work and life situations that support wellbeing, considered how to address any risk factors and boost protective factors, and then developed an individualised self-care plan.
Judge Amanda Chambers, President of the Children’s Court of Victoria, said that she was pleased to see the training sessions “focus on how to cultivate and maintain resilience and self-care. Peer support is crucial to wellbeing for many of us, but so too should we seek professional and guided assistance when needed.”
For employees and employers alike, the good news is that burnout is manageable and preventable. With considered interventions both at an individual and organisational level, workers can be supported to prevent or overcome burnout, feel healthy and enjoy their work again.
For more information go to: www.phoenixaustralia.org/consultation-services
What makes a great footpath?
The answer is key to our happiness and wellbeing as we age.

As people age, they often become less confident about walking. Fear of falling can limit the activity of older people, leading them to become isolated.

So what, exactly, makes for a great footpath to walk on?
My colleagues and I explored this question in a recent paper. We used an evidence-based tool to measure the walkability of urban roads – assessing not just the footpath itself, but the features around it.
The results can help urban designers make our cities more walkable, especially for older people.
What makes a footpath ‘walkable’?
Only about 42 per cent of people in Sydney and Melbourne live in neighbourhoods with above-average walkability. This compares poorly with people in Lisbon (99.2 per cent), São Paulo (97 per cent) and Hong Kong (96 per cent).
Generally, features that determine whether a footpath is walkable fall into one of two categories.
Neighbourhood-level features refer to a neighbourhood’s general environment, such as:
• how well connected streets are to each other. Do they offer a variety of available routes for daily trips?
• how densely dwellings are built and how amenities are distributed. Are there parks, train stations, cafes or shops within walking distance?
Footpath-level features refer to the safety, comfort and attractiveness of a footpath, such as:
• obstacles such as tree roots and short poles

• the width of the path
• convenience of crossing facilities
• green belts (such as grass and shrubs) and fences that separate pedestrians from traffic lanes
• areas of shade
• street furniture
• bicycles travelling along the path
• vehicles parked on the path
• noise from cars and other sources
• diversity of streetscapes such as building facades, trees and grasslands.
Previous studies on walkability have mixed these two levels of features. But our research separated them, to help urban designers identify which features are most important and which should be improved.
We focused on neighbourhood walkability for senior citizens. By 2050, one in six people in the world will be aged over age 65 – almost double the number in 2015. Australian census data paints a similar picture.
Research shows older adults who perceive their neighbourhood as walkable are happier and more satisfied with life, and less lonely.
Walkable cities help senior citizens – especially those with physical restrictions – be more physically active, and promotes stronger and more regular social connections.
So it’s particularly important to identify how to make our streets more appealing for this age group.
What we found
Our research focused on the city of Shenzhen in China. Over the past 40 years, Shenzhen has grown into a megacity, and urban planners have historically prioritised the needs of motorised traffic over pedestrians and cyclists.
Among the methods involved in our study, we asked 256 senior citizens to rate footpath features to help us understand how much each one affects their walking.
Respondents told us bikes on footpaths and vehicles parked on footpaths were the biggest factors in reducing walkability. They reported that cars parked on footpaths made the space too crowded and increased the risk of being injured by bikes travelling on the footpath.
Convenient crossing facilities were rated as the second most important feature of footpath walkability. This includes formal crossings – such as zebra crossings and underpasses – as well as informal crossings such as quiet streets.
We employed two auditors to quantify how well each feature appears in 11 sample footpaths. The results showed that the way researchers quantify the quality of a footpath can differ to the views of senior citizens.
For example, we measured the quality of a green belt based on the ratio of the length of the belt to the length of the footpath. But for the pedestrians we spoke to, no matter how wide a green belt is, it’s effective as long as it separates them from traffic lanes.
We need walkable neighbourhoods, too Our research shows what makes a good footpath, but neighbourhood walkability is also important. If people don’t have destinations to walk to, or streets are not well connected, then they will be deterred from walking even if the footpath is good quality.
And we must remember, people experience footpaths differently. An able younger adult may consider a footpath walkable when a senior citizen or a younger child struggles to navigate it.
Every citizen has an equal right to use and enjoy public space – and footpath design should reflect this.
Author: Fatemeh Aminpour, Associate Lecturer, School of Built Environment, UNSW SydneyThis article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ what-makes-a-great-footpath-the-answer-is-key-to-our-happiness-andwellbeing-as-we-age-191537
Safeguarding residents and medical staff with face recognition technologies
Aged care facilities depend on a secure environment to provide optimal care to residents, and safe working conditions for medical staff.
Face recognition solutions can automate many security measures, mainly by scanning faces of visitors, comparing them to watch lists and instantly alerting security staff to known offenders.
The software can also verify authorized staff to enter specific facilities and high-risk areas, and authenticate residents during registration and entrance processes.
Aged care homes need to guarantee that only authorized staff and registered visitors are allowed to enter the living areas. A face check can support efficient access control.
Residents’ differing levels of cognitive ability influences their mobility. Some can leave the premises, wander in the grounds, whilst others have to remain inside or only leave when accompanied. Face recognition technologies can monitor access rights to certain areas, and alert to an unattended person wandering off or leaving the building.
Residents often lose or borrow their keys, access cards and fobs, or don’t have the mobility to use them. Facial recognition offers an easier, more hygienic way of accessing floors and rooms.
In addition, facial analysis technology can detect and alert to persons not wearing a required protective face mask.
Cognitec’s FaceVACS-VideoScan solution delivers intelligent technology with industry-leading match speed, sending watch list alerts and visitor notifications within seconds. Surpassing traditional video surveillance systems, the technology detects and extracts people’s faces in live video streams or video footage, and constantly compares them to each other and to images in databases.
Besides instant alerting to known persons, the software uses anonymous facial analysis to count individuals, generate demographical information, track people movement in time and space, detect frequent visitors and crowds, and much more.
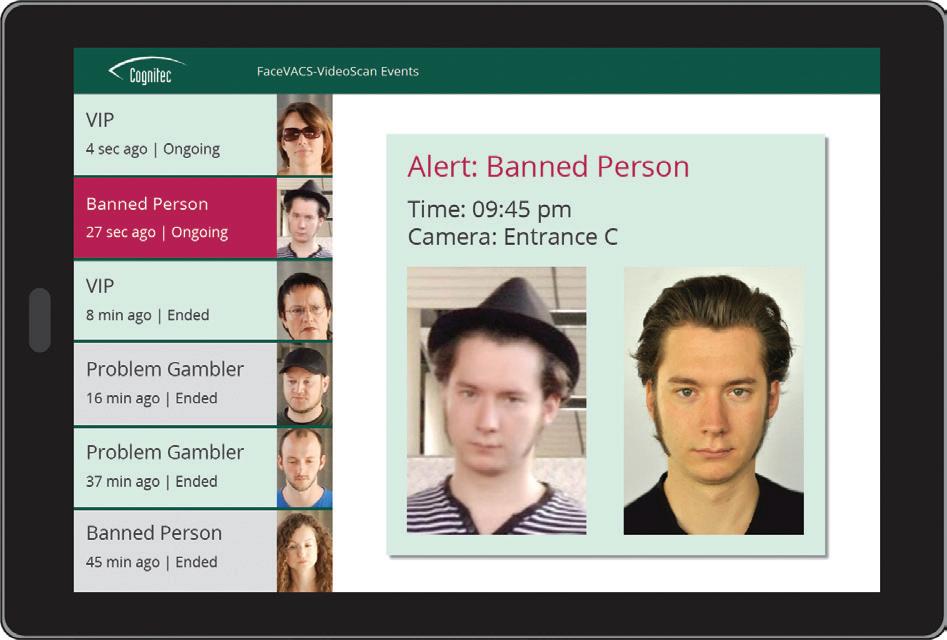
Cognitec is the only company worldwide that has worked exclusively on face recognition technology since its inception in 2002. The company’s innovative products deliver industry-leading face matching accuracy, and are supported by an Australian expert team located in Sydney. The German technology is used extensively by both the Australian government and commercial enterprises.
Let’s work together on your face recognition project!
Troublemaker? Banned? Staff? Resident?
Face recognition solutions scan faces of visitors, compare them to watch lists and instantly alert security staff to known persons.
The software can verify authorized staff to enter specific facilities and high-risk areas, and authenticate residents and visitors during registration and entrance processes.

How can face recognition benefit your facility?
Let’s start the conversation: sales@cognitec.com
Most experienced. Highly trusted. Since 2002.
Be Connected and make online safety a priority
The eSafety Commissioner is encouraging everyone to support older relatives and friends by taking the time to check their device settings and reinforce the importance of online safety, with help from Be Connected.

“Technology and electronic devices can help open up a wide and wonderful new world for older Australians – from facilitating video calls and connection on social media, to introducing new hobbies like listening to podcasts or playing online games,” eSafety Commissioner Julie Inman Grant said.
“Access to services and social connection through digital technology and the internet is empowering. However, we know that it can also be overwhelming to an older person who may not feel confident online and doesn’t know what to look for when setting up a new device or signing up for a digital service.
“Even those of us who use technology on a daily basis can find it challenging to create strong passwords and review privacy settings across our devices and accounts. For those older Australians who haven’t had as much exposure to the online world, this can be an even more intimidating process full of confusing tech jargon. “Make it your New Year’s resolution to improve the digital skills of those around you by taking time to share the importance of online safety.”
The Be Connected initiative provides a wide range of self-paced courses to help improve online safety and security settings, including how to spot scams and create strong passwords, an introduction to smart homes, and resources on getting started with laptops, desktops, tablets and mobile phones. The courses include easyto-follow instructions with short videos and summary sheets to download and use as helpful reference tools.
Keep these online safety tips front of mind to start 2023 securely, by making the most of the security features available on devices and building good habits to keep you and your loved ones safe online:
• Make your passwords strong and unique, and set up multi-factor authentication on accounts.
• Don’t share more information than you need to: when signing up for online services or registering an account, remember that you can choose to skip fields marked as optional.
• Adjust your privacy settings on social media platforms to help protect your personal information and be mindful about how much information is in the photos or videos you share.
• Be aware of scams: there are many online, email and phone scams out there, so it’s important to stay vigilant. Remember, if something looks too good to be true, it probably is.
“No matter our age or digital skill level, we all need to be careful about the amount of personal information we disclose online, especially as technology evolves and new devices have the potential to collect extensive location and biometric information including fingerprint logins,” Ms Inman Grant said.
“In connecting our loved ones through new devices and online services, we need to make sure devices and accounts are set up securely, so we don’t unintentionally open them up to scams and other vulnerabilities. “Be Connected provides everything you need to learn on how to set up devices, prioritise secure passwords and enjoy what the online world has to offer.”
A range of Be Connected resources
Find a wide range of Be Connected resources to improve your online skills, including resources for families, friends, peers and local community organisations, to help older Australians learn about the benefits of being online: www.beconnected.esafety.gov.au

About Be Connected
Be Connected is an Australian Government initiative implemented in partnership by the Department of Social Services, the eSafety Commissioner and Good Things Foundation Australia, committed to improving the online confidence, skills and safety of older Australians.
About eSafety
The eSafety Commissioner is Australia’s independent regulator for online safety. Our purpose is to help safeguard all Australians from online harms and to promote safer, more positive online experiences.
eSafety acts as a
safety
net for Australians who report cyberbullying, serious online abuse or image-based abuse. We can also investigate and remove seriously harmful illegal and restricted content including online child sexual exploitation material.
For more information visit eSafety.gov.au.
Complaints, missing persons, assaults –contracting outside workers in aged care increases problems
Aged care homes struggling to meet staffing needs are increasingly relying on externally contracted care workers to make up shortfalls.
However, our new study, shows homes that rely more heavily on externally contracted care staff provide significantly worse quality of care.
With the government convening a national jobs and skills summit next week, much attention is focused on addressing current staff shortages across the economy. Legislation has just been passed to increase the numbers of workers in aged care homes, and our research indicates workers’ employment conditions are
critical to ensuring higher quality of care is provided to senior Australians.
‘Agency’ staff across the sector
Within the residential aged care sector, approximately 9 per cent of all the registered nurses, enrolled nurses and personal care workers are external contractors. Employed by third-party labour hire agencies, these “agency” staff work across different aged care homes on a temporary basis.

This sort of employment arrangement can help homes deal with short-term fluctuations in demand and staffing shortfalls. So it’s not surprising that as shortages have become more acute, this workforce strategy has become more commonplace.
In particular, as homes have struggled to maintain sufficient staff during the COVID pandemic, the use of agency staff has increased across the sector.
As agency staff tend to work intermittently, there are concerns they lack familiarity with individual residents and their unique needs. This can be disruptive and distressing for residents and their families and undermine the continuity of their care.
Also, as agency staff frequently work across different homes, they tend to be less efficient and require more supervision. This can increase workload pressures, stress and turnover of permanent workers.
The relationship between staffing and quality care
Our study of 1,709 aged care homes over five years investigated the relationship between the quality of care provided by aged care homes and their reliance on agency contract care staff.

We found the use of agency staff was relatively common, with the majority of homes using agency care staff at some point.
More importantly, we found homes that rely more heavily on agency staff have worse quality of care. Specifically, they have higher rates of workforce-related complaints to the regulator, occurrences of missing residents, reportable assaults, preventable hospitalisations and instances of non-compliance with accreditation standards.
While this is the first such study in Australia, these results align with international evidence. One striking similarity is how sensitive care quality is to even tiny increments of agency staffing. We found that even if just 5 per cent of care time is delivered by agency staff, homes deliver significantly poorer quality outcomes.
But we’re in the middle of a workforce crisis
Our findings suggest one way to improve quality of care is for homes to reduce their reliance on contract care staff. This could involve efforts to improve the recruitment, retention and rostering of permanent nurses and care workers.
However, in the current context, this might be easier said than done. With the industry in the midst of a massive workforce crisis, homes may have no choice but to continue to rely on agency workers.
In such cases, homes should adopt strategies to mitigate the potential for bad outcomes. For example, they might improve residents’ continuity of care by drawing from a pool of regular agency workers and investing in better orientation and shift handover processes.
In terms of policy, much of the recent reform agenda has focused improving staffing numbers and skills in aged care, through funding for training programs, mandatory care minutes, 24/7 registered nurses and addressing workers pay.
Another of Labor’s election promises was to implement a recommendation from the Royal Commission to require aged care providers to preference direct employment over using contracted “agency” workers. This issue is now being investigated by the Productivity Commission, which will hand its report down next month.
No quick fixes
Simply putting limits on agency staff is unlikely to work in the current context. Imposing caps may result in homes providing less total care to residents.
Rather, the widespread use of agency across the sector reflects a need to understand and address its root causes. As will be discussed next week at the jobs summit, staffing shortages are not isolated to aged care but widespread across the economy.
Policymakers also will have to be mindful of the impact of other reforms in play. For instance, the use of contractors may well increase as providers attempt to increase staffing levels to meet incoming mandatory minimum standards, while managing the demands and disruptions of COVID outbreaks.
Despite these challenges our research highlights the importance of finding ways to sustainably curb the use of contract staff so as to deliver the quality of care all senior Australians deserve.
Authors:
Nicole Sutton, Senior Lecturer in Accounting, University of Technology
Sydney
Nelson Ma, Senior Lecturer, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ complaints-missing-persons-assaults-contracting-outside-workers-in-agedcare-increases-problems-188745
Tailored Recruitment Solutions for the Health & Community services
Is your business having trouble attracting quality permanent sta�? or do you have gaps in your daily PCA, FSA and nursing needs?
Labour care is one of Australia’s leading providers in specialist sta�ng solutions for the Aged Care sector



Our end-to-end business model and systems ensure that we successfully recruit and manage a workforce tailored to your needs.
We service all areas of VIC, NSW, WA, SA and QLD including regional and remote.
Give us a call on 1800 549 668 today to discuss your needs with our friendly sta�.
Innovative training solutions for the aged care industry
The aged care industry is changing. Over the last two years, the industry has adapted to new reforms, faced a nationwide workforce shortage and pivoted to work through the COVID-19 pandemic.
VERTO recognises the challenges the workforce is encountering and the increased pressure on the aged care sector when it comes to quality training and education. To recognise the importance of this, VERTO has developed the following resources for training and supporting workers in the industry:
• Aged Care Toolbox Talk Kits
• Mental Health Awareness Workshops
• Accredited Training.
VERTO’s Toolbox Talk Kits and eLearning packages provide a clear and concise suite of resources that meet Aged Care Quality Standards. The resources are informative and easy to understand and can be delivered in short, manageable timeframes, minimising the impact on day-to-day operations.

These resources are designed for residential aged care and community in-home care to promote active participation.
VERTO maintains the integrity of the Toolbox Talk Kits by producing and updating resources when appropriate.
A new Aged Care Quality Standards Kit will be available soon after the standards are released in 2024 and will be offered at a reduced rate to existing clients.

VERTO regularly receives positive feedback from our clients about the Aged Care Toolbox Talk Kits, with staff adopting whole-of-organisation practices based on their learning, from the carer level through to management.
Our clients also enjoy the benefits of updated and ongoing changes with VERTO’s support and maintenance of the resources.
“Our staff love the Toolbox Talk Kit, especially the senior registered nurses. Thank you for developing the amazing toolbox education kit,” Executive Director of Nursing at Thompson Health Care, Melissa Yan, said.
Mental Health Awareness Workshops
As part of VERTO’s commitment to improving aged care education, we offer a non-accredited Mental Health Awareness Workshop.
The intention of this workshop is to promote mental health awareness amongst all aged care workers. According to findings in the Australian Government’s Royal Commission into Aged Care Quality and Safety, when older people transition to permanent care, it can signify a greater need for psychological support to help
them and their families work through this major life change.
VERTO’s workshop looks at how staff can support aged care residents emotionally, as well as recognise the challenging behavioural and psychological symptoms associated with dementia.
The workshop is designed for health workers who work in residential aged care facilities and community in-home care. It aims to give participants a greater insight into the complexities of mental health awareness and working with the elderly by firstly ‘looking within’.
Looking within makes us think about our own actions and inner thoughts – introspection – and practice selfacceptance. Only then can we separate our own needs to that of the person in front of us, who needs care and attention.
The workshop is designed to facilitate group discussion on each of the following topics:
• Mental health conditions
• Behavioural and psychological symptoms of dementia (BPSD) management and awareness
• BPSD intervention
• Self-care and wellbeing
We then address how these directly relate to the consumers of aged care: the residents in aged care facilities and the users of community in-home care services.
Accredited Training
As a Registered Training Organisation, VERTO has a 40-year history of providing training. We are committed to producing market-leading, compliant resources for Certificate III and Certificate IV in Individual Support with a specific stream for ageing.

VERTO draws on the expertise of clinical consultants and dedicated writers to assist in developing resources which focus on person-centred care and mental health. Each unit also includes additional complimentary content relating the unit directly to the Aged Care Quality Standards and their requirements.
Our experience in this sector and qualified clinical staff give us a leading edge in the quality of work we produce and the training we provide.
VERTO has established long and beneficial working relationships with clients and is proud to help with bespoke training needs.
If you think VERTO could assist your organisation, please reach out to us on 1300 483 786 or email dbooth@verto.org.au.
Aged Care Toolbox Talk kit benefits:
Whole organisation training with person-centred approach
Assessment ready staff with a deeper understanding of the Aged Care Quality and Safety Commission (ACQSC) Standards and requirements
Updates and additional resources provided under support agreement.
VERTO also offers:

Aged Care Mental Health Awareness Workshop
Accredited Certificate III and IV in Individual Support
(Ageing)
training resources that include content mapped to ACQSC Standards and requirements.


Since the successful launch of the Aged Care Toolbox Talk kit in 2022, it is proving popular in both residential and home care settings Providers are seeing the benefits of being able to focus on one topic in a short, sharp face-to-face session, and are able to reach all staff for a “whole organisation” approach

VERTO has also developed a Mental Health Awareness Workshop to assist workers in aged care by giving them a greater insight into the complexities of mental health awareness and working with the elderly


VERTO’s production of resources involves a team of dedicated writers and industry specialists armed with a focus on person-centred care and mental health Our accredited resources also include additional complimentary content relating the unit directly to the Aged Care Quality Standards and their requirements.
Our staff love the Toolbox Talk Kit, especially our senior registered nurses Thank you VERTO for developing this amazing toolbox education kit MELISSA YAN Director of Nursing at Thompson Health Care
For more information visit verto.org.au or scan the QR code.

A SENSE OF COMMUNITY
By Helen ChryssidesAs most of us are heading off to bed, a new world is opening up for registered nurse Glenda George, on night shift in an aged care facility.
She recently completed a five-week locum placement in the small town of Kojonup, in Western Australia’s Wheatbelt, for Australian Government-funded Rural Locum Assistance Program (Rural LAP).
An experienced remote and rural practitioner, Glenda enjoys the lifestyle this work provides. ‘It gives me both independence and flexibility. I can choose the times I’m available and then pack up and go to a new and unique environment.’ The application process and straightforward transfer from her home 70 kilometres out of Sydney to her placement location was coordinated by Rural LAP.
‘I flew directly to Perth, picked up the hire car and drove some four hours to Kojonup. It was a smooth and easy transition, both there and back.’
It’s an ideal career for Glenda, whose husband is a fly-in, fly-out (FIFO) worker in mining.
She says her work gives her a sense of purpose. ‘I want to make a difference in a rural or remote setting where the isolation may make recruitment difficult. Many potential applicants don’t like having limited cafes and restaurants, and being away from family and friends.
‘I am at ease in my own company and appreciate looking at beautiful landscapes, such as the magnificent sunrise at Kojonup.
The town appreciates and respects their locum staff and includes us in community events.’
What makes Glenda’s work fulfilling is the contact with extraordinary individuals.
‘I love getting to know the life stories of the residents, as they have incredible skills and life experience. One wheat farmer also drove road trains full of grain hurtling down the highway. And the women are resilient with a “can do” attitude. You’ll see them flying light aircraft over properties and, if a tractor breaks down, they’re up on it, sorting out the mechanics.’
Working in the rural and remote sector has shown Glenda first-hand the geographical and socio-economic challenges faced by those living there. ‘It’s certainly an eye opener seeing what people face on a daily basis.’
Glenda’s community spirit extends beyond her work. She’s been a volunteer firefighter for rural New South Wales since 2004. ‘We run into fires while the public runs away from them.

‘We’re well-trained but fire has its own mind and can be catastrophic. You can lose your life.’ Yet she wants to help, especially after a fire almost destroyed her own property and many people came to fight it. ‘These days I also have a program training young Aboriginal women [to be firefighters].’
With qualifications in remote health nursing and mental health, Glenda can also carry out depression and cognition assessments alongside basic care interventions. ‘I care for some of the most vulnerable Australians at the end of their lives, in palliative care.’
She’s worked in aged care facilities throughout New South Wales for other organisations and, while she admits aged care can be hard work, the rewards outweigh the challenges.
With a shortage of nurses Australia-wide, there are opportunities to join Glenda, and others like her, and make a difference.
Rural LAP National Manager, Jessica Andrew, says ‘We’re focused on ensuring continuity of care and clinical leadership in locations that have difficulty hiring. We work with fantastic, hardworking locums and lovely clients.’
Ciara O’Regan, Manager of Springhaven Lodge where Glenda worked, can vouch for that.
‘Rural LAP provides a valuable service. It’s very much needed and Glenda was wonderful, absolutely wonderful. She was keen and experienced, respectful and flexible.
Rural LAP is a locum assistance program for health and aged care services across rural and remote Australia. The Australian Governmentfunded program supports eligible aged care workers, nurses, midwives, obstetricians, anaesthetists, and allied health professionals that undertake continuing professional development or go on personal leave by providing a seamless start-to-finish locum service.
Since the pandemic and the impact of workforce shortages nationwide, the program has seen a significant increase in locum requests across rural and remote Australia. In March 2022, the Australian Government expanded Rural LAP to include eligible rural and remote aged care services.
Established in June 2011 under the Australian Government’s rural workforce capacity agenda, the program has helped thousands of health professionals take a much needed and welldeserved break.
$800* PER DAY PLUS LOADING AS APPLICABLE

Get paid to explore our beautiful countryside or the vast and rustic Australian Outback as an aged care locum nurse.

As a Rural LAP locum you will receive:
• an hourly rate as determined by State and Territory Government approved schedule(s)
• superannuation as determined by Federal Government regulations
• $150 per working day incentive allowance* (inclusive of superannuation)
• $100 per day travel allowance*
• travel and accommodation arranged and paid for by us.
*Subject to terms and conditions as outlined during the Rural LAP placement process.
Territories free to make their own voluntary assisted dying laws, in landmark decision
Here’s what happens next.

Voluntary assisted dying will soon be an option for the Australian Capital Territory and Northern Territory, now the Senate has just passed a landmark bill.
The passing of the Restoring Territory Rights Bill 2022 removes the key legal barrier for the ACT and NT to introduce their own voluntary assisted dying legislation, should they wish to do so.
This could see the territories join all six Australian states, which already have voluntary assisted dying legislation.
After extensive consultation, the ACT will introduce its voluntary assisted dying legislation, with debate expected in late 2023 or early 2024. The NT government has stated it has no plans to follow suit, at least during this parliamentary term.

The territories once led reform
Although the territories are now the only Australian jurisdictions without voluntary assisted dying laws, they once led reform in this area.
The ACT was the first Australian jurisdiction to attempt to legalise assisted dying, although its 1993 Voluntary and Natural Death Bill failed to pass.
Shortly after, in 1995, the NT parliament passed the Rights of the Terminally Ill Act – the first operational voluntary assisted dying law, not only in Australia, but in the world.
However, it was the passing of this law that prompted the Commonwealth to remove the territories’ power to legislate in this field.
In 1997, the NT’s act was overturned by the Commonwealth parliament through the Euthanasia Laws Act, introduced by then Liberal backbencher Kevin
Andrews. This act also aimed to prevent the territories passing such laws in the future.
The Commonwealth was only able to do this for the territories – not the states – because the Constitution gives the Commonwealth unlimited power to make laws “for the government of any territory”.
Nine previous bills aiming to restore territory rights on this issue have been introduced into the Commonwealth parliament, but all had failed, until now.
The ACT and NT can learn from the states
If the ACT and NT choose to legalise voluntary assisted dying, they must consider the evidence and data from states where voluntary assisted dying is operational. There is also an opportunity to select the best aspects from each state law.
For instance, for all states except Queensland, for a person to access voluntary assisted dying, they must be expected to die within six months (within 12 months for neurodegenerative conditions).
Given challenges with delays in getting through the system, the 12-month period adopted by Queensland, or not imposing a specific time limit until death, may allow more time for terminally ill people to navigate access.
Similarly, all states require a person to live in the state for 12 months before requesting assistance to die. Now voluntary assisted dying is lawful throughout most of Australia, there is little need for this requirement.
The territories may choose to impose minimum legal obligations for how healthcare and aged care facilities who do not participate in voluntary assisted dying handle such requests. This is the case in Queensland, South Australia and New South Wales.
The territories also may wish to allow eligible people to choose how the medication is administered – they can take it themselves or a health professional can administer it. This choice is permitted in NSW, whereas other states make self-administration the default method.
What now for the rest of Australia?
Of the six states with voluntary assisted dying laws, those in Victoria, Western Australia and Tasmania are already operational.
Queensland’s laws started on 1 January 2023, with SA following on 31 January. NSW, the final state to pass its laws, will start on 28 November.
Should the territories propose their own legislation, we’d anticipate wide consultation and debate.
With territories now permitted to decide this matter for themselves, there is a real prospect for them to have access to voluntary assisted dying in the foreseeable future.
Katherine Waller, Project Coordinator, Australian Centre for Health Law Research, Queensland University of Technology, coauthoredthis article.
Authors:
Ben White, Professor of End-of-Life Law and Regulation, Australian Centre for Health Law Research, Queensland University of Technology
Katrine Del Villar, Postdoctoral research fellow, Queensland University of Technology
Lindy Willmott, Professor of Law, Australian Centre for Health Law Research, Queensland University of Technology, Queensland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/ territories-free-to-make-their-own-voluntary-assisted-dying-laws-inlandmark-decision-heres-what-happens-next-195291
Tonnes of COVID-19 health care waste expose urgent need to improve waste management systems
Tens of thousands of tonnes of extra medical waste from the response to the COVID-19 pandemic has put tremendous strain on health care waste management systems around the world, threatening human and environmental health and exposing a dire need to improve waste management practices, according to a new WHO report.

The WHO Global analysis of health care waste in the context of COVID-19: status, impacts and recommendations bases its estimates on the approximately 87,000 tonnes of personal protective equipment (PPE) that was procured between March 2020- November 2021 and shipped to support countries’ urgent COVID-19 response needs through a joint UN emergency initiative. Most of this equipment is expected to have ended up as waste.
The authors note that this just provides an initial indication of the scale of the COVID-19 waste problem. It does not take into account any of the COVID-19 commodities procured outside of the initiative, nor waste generated by the public like disposable medical masks.
They point out that over 140 million test kits, with a potential to generate 2,600 tonnes of non-infectious waste (mainly plastic) and 731,000 litres of chemical waste (equivalent to one-third of an Olympic-size swimming pool) have been shipped, while over eight billion doses of vaccine have been administered globally producing 144,000 tonnes of additional waste in the form of syringes, needles, and safety boxes.
As the UN and countries grappled with the immediate task of securing and quality-assuring supplies of PPE, less attention and resources were devoted to the safe and sustainable management of COVID-19 related health care waste.
“It is absolutely vital to provide health workers with the right PPE, “said Dr Michael Ryan, Executive Director, WHO Health Emergencies Programme. “But it is also vital to ensure that it can be used safely without impacting on the surrounding environment.”
This means having effective management systems in place, including guidance for health workers on what to do with PPE and health commodities after they have been used.
Today, 30 per cent of healthcare facilities (60 per cent in the least developed countries) are not equipped to handle existing waste loads, let alone the additional COVID-19 load. This potentially exposes health workers to needle stick injuries, burns and pathogenic microorganisms, while also impacting communities living near poorly managed landfills and waste disposal sites through contaminated air from burning waste, poor water quality or disease carrying pests.
“COVID-19 has forced the world to reckon with the gaps and neglected aspects of the waste stream and how we produce, use and discard of our health care resources, from cradle to grave,” said Dr Maria Neira, Director, Environment, Climate Change and Health at WHO.
“Significant change at all levels, from the global to the hospital floor, in how we manage the health care waste stream is a basic requirement of climate-smart health care systems, which many countries committed to at the recent UN Climate Change Conference, and, of course, a healthy recovery from COVID-19 and preparedness for other health emergencies in the future.”
The report lays out a set of recommendations for integrating better, safer, and more environmentally sustainable waste practices into the current COVID-19 response and future pandemic preparedness efforts and highlights stories from countries and organizations that have put into practice in the spirit of “building back better”.
Recommendations include using eco-friendly packaging and shipping, safe and reusable PPE (e.g., gloves and medical masks), recyclable or biodegradable materials; investment in non-burn waste treatment technologies, such as autoclaves; reverse logistics to support centralized treatment and investments in the recycling sector to ensure materials, like plastics, can have a second life.
The COVID-19 waste challenge and increasing urgency to address environmental sustainability offer
an opportunity to strengthen systems to safely and sustainably reduce and manage health care waste. This can be through strong national policies and regulations, regular monitoring and reporting and increased accountability, behaviour change support and workforce development, and increased budgets and financing.
“A systemic change in how health care manages its waste would include greater and systematic scrutiny and better procurement practices,” said Dr Anne Woolridge, Chair of the Health Care Waste Working Group, International Solid Waste Association (ISWA).
“There is growing appreciation that health investments must consider environmental and climate implications, as well as a greater awareness of co-benefits of action. For example, safe and rational use of PPE will not only reduce environmental harm from waste, it will also save money, reduce potential supply shortages and further support infection prevention by changing behaviours.”
The analysis comes at a time when the health sector is under increasing pressure to reduce its carbon footprint and minimise the amount of waste being sent to landfill — in part because of the great concern about the proliferation of plastic waste and its impacts on water, food systems and human and ecosystem health.

MED-X: LEADING SUSTAINABLE CHANGE IN MEDICAL WASTE MANAGEMENT


Traditionally, the medical waste industry has not been associated with sustainability. Legislative treatment requirements focusing on patient care and health, has seen medical waste compliantly handled and disposed of in the safest manner for the community. Med-X Healthcare Solutions, a specialist clinical waste and hygiene solutions service provider was founded in 2017 and has already made significant inroads into providing circular economy solutions for the industry.
Med-X’s growth accelerated in early 2020 when it was recognised by Australia’s healthcare, and specifically the aged care sector, as a rising star in reliable medical waste management amid increasing cases of the COVID-19 virus. The volume and rate of highly infectious clinical waste generated by healthcare facilities, surpassed the capacity of other medical waste vendors to manage. This became a high priority challenge for the aged care sector, with emergency assistance required. Med-X was called upon to assist in servicing aged care facilities in order to meet the increased demand.
Van Karas, General Manager of Med-X and Shred-X recalled the company’s quick response and assistance in infectious waste collection during this difficult time, “While they may not be frontline healthcare staff, our Med-X service personnel faced equally daunting situations, putting the health and safety of others before their own. Correct handling of highly infectious waste requires adherence to strict procedures and processing protocols. It’s not glamorous work but it is essential, and we are extremely proud of our team who stepped up in a time of crisis.”
However, delivering reliable clinical waste management during the pandemic and beyond, is not the only way Med-X is making its mark in the industry. The company is also becoming known for its sustainable and innovative approach to waste transformation initiatives. In an Australian first, Med-X has developed a 100% recyclable single-use sharps container system,

aptly named SharpCYCLE™ which is revolutionising the sharps container market.
The recovery of single-use sharps containers has been pioneered through Med-X’s investment in innovative contactless process technology whereby collected single-use containers are robotically decanted, separated from their contents, granulated and blow moulded into reusable products such as sanitary waste containers, plant pots and paint pails. Med-X has partnered with local Australian recyclers and plastic moulding companies to utilise extruded plastic pellets generated by the SharpCYCLE™ process in the manufacture of other recycled plastic products, creating a true circular economy.
Through the ground-breaking SharpCYCLE™ recycling system, the clinical waste segment represented by single
use sharps containers will be almost fully recoverable and diverted from landfill. “It is estimated that this recovery system will reduce sharps container landfill volumes by over 28%. This percentage will certainly grow as the market moves to the single-use container system now that there is a sustainable, recycled alternative”, Van Karas described. “Although there are good reasons to use single-use virgin plastic in sterile environments, the issue unfortunately until now has been the disposal methods both of which negatively impact our environment: incineration adding greenhouse emissions and/or landfill, contaminating our ground and water.”
Investment in sustainable technologies such as SharpCYCLE™ comes as little surprise to those who know that Med-X and sister-company Shred-X are subsidiaries of Freightways Limited, a publicly listed New Zealand company with a strong commitment to carbon reduction and waste transformation. Shred-X was born of the paper recovery industry over 20 years ago, so the company’s roots are firmly planted in sustainability and remain its mission today.
Staying true to its heritage, Med-X continues to ensure ethical disposal and wherever possible divert treated waste from landfill, finding innovative ways to transform waste into new products. From rethinking eco-friendly procedures and landfill diversion opportunities within the industry, Med-X already recycle medical equipment. The treated and shredded product is recovered by local recyclers, leading to a reduction in disposal costs and landfill volumes.
Furthermore, Med-X is proud to be the collection partner in Project ‘Divert’ - a trial lead by incontinence products manufacturer Essity to divert this waste stream from landfill. The pilot is based at the Med-X treatment facility in Sale, Victoria and is an industry collaboration using Earth Systems’ patented pyrolysis technology to process used incontinence pads and nappies into Biochar. According to research, half the landfill waste from Australia’s aged care facilities is made up of used incontinence products, so Project Divert is Australia's first large scale trial to find an alternative to landfill.
Partnerships in these waste transformation initiatives and the launch of the SharpCYCLE™ system are aligned to Med-X’s Company’s Vision and Mission of Preserving Tomorrow, Today for a Sustainable Future.
Med-X Healthcare Solutions – Be Smart, Be Safe, Be Healthy





How are you managing waste at your Aged Care facility?



Our skilled contractors will assist you with the collection of a range of waste streams, including medical waste comprising of clinical and related waste, cytotoxic, pharmaceutical, anatomical, and sharps waste. Meanwhile, the team at Wasteflex will ensure that our solutions are reliable, scalable, and appropriate for your business requirements.
Why choose us?
Wasteflex is the largest private buyer and dedicated manager of waste services in Australia
Our solutions will simplify your waste management processes
Immediate Cost Savings
Rapid, Flexible, and Reliable Service
Wasteflex will provide timely, detailed, and meaningful reporting
Directory

Face recognition solutions






scan faces of visitors, compare them to watch lists and instantly alert security staff to known persons.





The software can verify authorized staff to enter specific facilities and high-risk areas, and authenticate residents and visitors during registration and entrance processes.

Let’s talk about a plan for your facility: sales@cognitec.com



Albany Creek Memorial Park | Allambe Memorial Park | Broulee Memorial Gardens

| Castlebrook Memorial Park Forest Lawn Memorial Park | Great Southern Memorial Park

| Lake Macquarie Memorial Park | Lakeside Memorial Park Mt. Thompson Memorial Park | Newcastle Memorial Park | Northern Suburbs Memorial Garden | Pinegrove Memorial Park Rookwood Memorial Gardens | Toowoomba Garden of Remembrance | Tweed Heads Memorial Gardens


Using our consulting services, you can rest assured that you complete the lengthy and frustrating registration process successfully through our GUARANTEED services (T&C applied).
Melbourne Office - 03 9190 8986




Melbourne@isoconsultingservices.com.au
Sydney Office - 02 8935 9472




Sydney@isoconsultingservices.com.au
Brisbane Office - 07 3726 9590

Brisbane@isoconsultingservices.com.au
Peth Office - 08 6165 8864









Perth@isoconsultingservices.com.au






































































Leecare Solutions Pty Ltd

03 9339 6888 admin@leecare.com.au
www.leecare.com.au
www.facebook.com/leecaresolutions
www.instagram.com/leecare_solutions
LoopSafe Technology

Page 34, 35
On The Go Rehabilitation Services 0429 115 211 info@onthegorehab.com.au www.onthegorehab.com.au www.facebook.com/pages/On-The-GoRehabilitation/136197893104276 twitter.com/OnTheGoRehab
Robot-Coupe 02 9478 0300 info@robotcoupe.com.au
www.robot-coupe.com/australia/en_AU
www.facebook.com/RobotCoupeOfficial/ www.instagram.com/robotcoupe_official/ fr.linkedin.com/company/robot-coupe-official
Page IBC,134
Powertec

Page 70, 71
03 9381 7897 info@loopsafe.net www.loopsafe.net www.linkedin.com/company/looplearn/ Page IFC, 41
1300 769 378 sales@powertec.com.au www.powertec.com.au/ www.facebook.com/powertec.telecom/ www.linkedin.com/company/powertecwirelesstechnology
Page 44, 45
Rural LAP (02) 6108 3510 enquiries@rurallap.com.au
www.rurallap.com.au/
www.facebook.com/pages/Nursing-Allied-Health-RuralLocum-Scheme/146065388792849 www.linkedin.com/company/rurallap/

Page 158, 159
Lumary enquiries@lumary.com.au www.lumary.com/ www.facebook.com/LumaryAU/ www.instagram.com/lumary_au/ www.linkedin.com/company/lumaryau/ Page 3, 52, 53, 113
Med-X Pty Ltd
1300 116 339
Contact@med-XSolutions.com.au Med-xsolutions.com.au
www.linkedin.com/company/med-x-pty-ltd/ www.facebook.com/MedXAustralia
MedAdvisor International Pty Ltd
Page 164, 165
Professional Dentist Supplies Pty Ltd +61 (3) 9761-6615 sales@profdent.com.au www.profdent.com.au/
Page 101 Reynard Health Supplies (Aus) Pty Ltd 02 82 073 133 Enquiries@reynardhealth.com.au www.Reynardhealth.com.au
www.facebook.com/Reynard-Health-Supplies-Australia www.linkedin.com/company/reynard-health-suppliesaustralia
Page 102, 103
SPC Care
1800 805 168 customercare@spc.com.au www.spc.com.au

www.facebook.com/SPCAustralia/ twitter.com/spcaustralia?lang=en www.instagram.com/spcaustralia/
1300 125 343 support@medadvisor.com.au www.mymedadvisor.com/ www.facebook.com/MedAdvisorAustralia www.linkedin.com/company/medadvisor-international-ptyltd/
Page 42, 43
Mitsubishi Electric Australia Pty Ltd
1300 280 625 www.mitsubishielectric.com.au
Page 76
MPS Hold Co. Pty Ltd
1800 003 938 hello@mpsconnect.com.au www.mpsconnect.com.au au.linkedin.com/company/mps---australia
Page 28, 29, 30, 31
Rhima Australia Pty. Ltd 1300 347 944 www.rhima.com.au/ www.facebook.com/rhimaaustralia/ www.linkedin.com/company/rhima-australia-pty-ltd/ www.youtube.com/user/rhimaclean
Page 104, 105
Telstra
Riot Creativity Pty Ltd (03) 8400 4887 support@riot.com.au

www.facebook.com/riotartandcraft www.instagram.com/riotartandcraft/ www.youtube.com/c/RiotArtCraft/videos
Page 7, 22
The Diabetes Kitchen 1300 79 89 08 www.diabetesmealsonline.com.au/ info@diabetesmealsonline.com.au www.facebook.com/DiabetesMealsOn www.instagram.com/diabetesmealsdelivered

Transcord Community Transport Organisation Inc
Ph: (07) 5539 3733 info@transcord.com.au www.transcord.com.au
Valiryo Oceania +61 0416214588
salesaus@valiryo.com www.valiryo.com/
Verto Ltd

1300 483 786 info@verto.org.au www.verto.org.au/ www.facebook.com/VertoAu www.instagram.com/vertoau/ Page 156, 157
Wasteflex
1300 927 833 customerservice@wasteflex.com.au www.wasteflex.com.au/
WBS Technology
1300 927 533 info@wbstech.com.au www.elumen.com.au/
Page 166
Page 60, 61
Willira Pty Ltd 03 5782 1378 info@williraheating.com.au www.williraheatingandcooling.com.au/ Page 77
Wisdom Activities


1300 301 319 wisdom@wisdomactivities.com.au www.wisdomactivities.com.au/ www.facebook.com/wisdomactivities/ Page 32, 33
YouMist
1300 006 478 info@youmist.com.au www.youmist.com.au/ www.instagram.com/youmistaus/ www.facebook.com/youmistaus
Page 78, 79

















