
5 minute read
SKIN PROTECTORS BY DERMASAVER


pressure care
Managing Heel Pressure And How To Relieve It
Understanding Heel Pressure
Heel pressure has the potential to result in severe skin injuries behind the heel. If not effectively managed, it can escalate into further ulceration. This is particularly observed in individuals with compromised skin integrity or those who are immobile and confined to extended periods of bed rest. The vulnerability of the area behind the heel stems from the presence of a distinctive ridge on the heel bone, known as the Calcaneus, which protrudes at the back. Additionally, the skin covering this region is thin and lacks substantial cushioning, such as muscle or fat, that typically shields the bone from direct skin contact.
Heel pressure occurs when individuals lie down, causing the rear of the heel to make contact with the surface of the bed. The weight of the leg applies pressure to the back of the heel, an area with limited padding or resistance to pressure. Even slight movement of the heel against the bed leads to shear stress on the skin, resulting in redness and inflammation.

Heel pressure-related concerns are prevalent across various groups. Prolonged bed rest is a common scenario in which heel pressure can manifest. The protective skin in this region is thin, with minimal soft tissue in the form of tendons or muscles safeguarding the underlying bone. When individuals experience compromised skin integrity and are largely immobile, they spend extended periods in bed. Considering their resting position, the heels are in direct contact with the bed’s surface. The slightest movements during this time contribute to ongoing shear pressure on the bedding, potentially causing pressure injuries within a matter of hours. This could manifest as a reddish blemish, similar to the experience of developing a blister from new shoes, or progress to a burst blister and eventually transform into an ulcer.
Symptoms and Underlying Causes
As previously mentioned, initial signs of pressure may present as discolouration on the heel, characterised by shades of red, purple, or blue. This discolouration is akin to a bruise, resulting from blood accumulation at the skin’s surface. It’s also probable that fluid will accumulate within the skin, resembling a blister. Once the skin breaks, the person becomes susceptible to infection or tissue necrosis.
There are several known factors that increase a patient’s risk of developing a heel pressure ulcer, including: c Inadequate/malnutrition - Poor vitamin intake and absorption from food can lead to thinning of the skin and therefore decreased blood flow. c Advancing Age - Elderly people who spend an increased amount of time in bed can lead to shear and pressure in areas of poor skin integrity. c Abnormalities of circulation - This may be due to vascular issues where blood flow is limited to the extremities and a lack of red blood cells to an injury will delay healing. This is also common in patients with diabetes. c Sensory deficiency - For example, people with diabetes who may experience nerve damage are at increased risk of pressure sores. Nerve damage causing loss of sensation is called Diabetic Neuropathy. c Immobility - May be caused by paralysis, stroke or severe illness. Fractures of the bones in the legs may also lead to immobility for a period of time. Common fractures to occur are the neck of the femur (NOF) fractures also known as a broken hip c Major surgery - Heart, lung and some orthopaedic surgeries restrict mobility and hence increase time in bed. Long periods of time laying in bed increase chances of pressure sores. c Multiple health problems (comorbidities) - Particularly coronary or respiratory can lead to long term bed rest. Long periods laying in bed increases the chances of pressure sores. c Dehydration - Hydration is vital for maintaining skin integrity and wound healing. Adequate fluid intake is necessary to support blood flow to wounded tissues and to prevent additional breakdown of the skin.

Treatment & Prevention
Offloading is described as lifting or pushing an area of high pressure away from the cause of the pressure. To offload is to distribute the load to other areas which are not susceptible to pressure areas. Both the calf and foot can help with the offloading. Heel pressure is redistributed to both the calf, a soft muscle belly which can change shape to fit a supportive device as well as the foot.
Explore Heel Up Heel Lifter range for short term or longterm pressure offloading of the heel.
Developed in collaboration with leading wound care nurses, Levabo Heel Up ® range are the perfect solution for preventing pressure ulcers. They are single-patient use which are ergonomically designed to provide good stability and support. The Heel Up range is suitable for hospitals, aged care and home care and are available in range of sizes, with an inflation device included in each box.


More about Heel Up heel lifters c Heel Up is a single-patient product but can be used for the same user over a longer period. It can be wiped with a damp cloth, alcohol or other suitable disinfectant. Both ensures high hygiene. c Heel Up heel lifters are not inflated upon delivery and therefore take up very little space. This makes it easy to keep in storage and bring them to the user. c Supplied in clean, sealed flat pack including inflating device. c Heel Up is inflated using the supplied inflator tube or with one of Levabo’s other pumps. An adapter is also included to adjust the air pressure. c Skin friendly for sensitive skin: Tested and approved according to irritation and hypersensitivity test, ISO 10993-10:2010. The product is also CE approved.

Who benefits from a Heel Up heel lifter?
The target group for a heel lifter is people who have or are at risk of developing pressure ulcers, especially people with reduced mobility and bedridden people.


Risk groups typically include people who are: c overweight c underweight c older c critically ill c palliative c spinal cord injured
Heel Up ® has some important features that provide a number of advantages
Drainage of heat
Drainage of moisture
Lightweight
No drop foot
Malleolus
Heel
Achillies
As people get older their skin begins to change. Aged care workers have been accustomed to dealing with these changes to elderly people’s skin by moisturising and protecting the limb from the environment. This process has worked quite well in the past - but there has always been a concern with the type of elastic bandages used to keep the moisture in - this is where Protect-a-Limb® steps in.
This exciting product has been designed to take the bumps and bruises out of life due to its durability, high comfort level, easy application, and soft to touch and feel against the skin - not to mention, it’s extremely cost effective - making it a must in every aged care facility.
Protect-a-Limb® is an Australian made healthcare product designed and tested in Australian conditions. It has been engineered to ensure the person requiring the garment remains cool in summer and warm in winter - a necessity in our harsh Australian climate.
The “cool in summer and warm in winter” element of Protect-aLimb® is achieved by the unique Coolmax ® System. Coolmax®, which is a registered trademark of INVISTA, is a channelled synthetic fibre on the inner of Protect-a-Limb ®, surrounded by cotton on the outer surface which is slightly retentive.
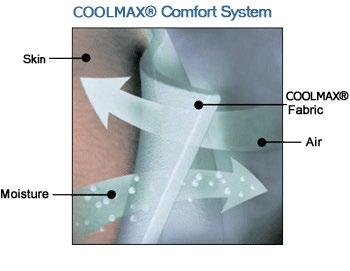

Coolmax®:
• Dries faster than other fabrics
• Is cost effective - saving time in application
• Gives protection against friction to vulnerable limbs
• Aids in patient comfort
• Wicks away moisture and prevents maceration
• Is hygienic - can be washed as easily as a pair of socks
• Has sealed ends to prevent fraying







