

INSIDE:
Ontario’s Health811
Ontario’s Health811 has been expanded from a nurse-led telephone service to one that also provides a variety of computer and smartphone-based options, including an AI-driven symptom checker, chat and video.
Page 6
Advances in wound care
Applying digital technologies to wound care has improved the diagnosis and treatment of wounds. AI is even suggesting care paths based on data from millions of collected images.
Page 18
First Nations app
The Sq’ewlets First Nation recently celebrated the launch of the q’eyex app. The wellness app provides users with a safe space to connect with ancient teachings, and to learn from Elders and knowledge keepers.
Page 20

Humber partners on innovation with MEDITECH
MEDITECH has selected Toronto’s Humber River Health as the first collaborator in its global Expanse Innovation Partnership program.
Barb Collins, president and CEO of Humber River Health, has led the emergence of the organization as a ‘digital hospital’, and says the Humber team will extend the capabilities of the electronic health record to benefit patients in Canada and worldwide. SEE STORY ON PAGE 4.
West Montreal health region devises its own EHR
BY NORM TOLLINSKY
When the senior leadership teams at most Canadian hospitals are in the market for a new Electronic Health Record (EHR), they almost invariably opt for one of the mainstream solutions. But that wasn’t the case at CIUSSS West-Central Montreal, which includes the Jewish General Hospital (JGH). Instead, the CIUSSS and the JGH partnered with Harris Healthcare to develop a solution from scratch.
“Several years ago, when we started looking at the EHR options out there, we had a couple concerns with what was available,” said Dr. Justin Cross, the hospital’s chief digital health officer.
Foremost was the ability of an EHR system to fully support the way Quebec’s healthcare system is organized into integrated health and social service networks.
The JGH is part of the Integrated Health and Social Services University Network for West-Central Montreal (also known as CIUSSS West-Central Montreal), and serves as the network’s acute-care site. The integrated network also includes long-term care centres and rehab hospitals, community care, public health community centres, fam-
The new EHR is being developed to more easily support views of patient care across the continuum.
ily medicine clinics, mental health services, and other social services.
“Many EHRs on the market are very hospital-focused, and we wanted to build something for the continuum of care across our health network because a lot of our patients transit from one service or facility to another. It’s very important for the different members of the care team to be able to see what’s going on,” said Dr. Cross.
There were other reasons that steered the JGH toward developing a new EHR. Citing an article published by the Annals of Family Medicine in 2016, Dr. Cross highlighted the findings that for every hour of direct patient care, doctors are spending two hours in their EHR.
“Coming out of the pandemic, we have
Montreal region and Harris devise a new Electronic Health Record
seen a lot of burnout that has resulted in both doctors and nurses taking early retirement. We’re dealing with a workforce that’s tired. We have an aging population that requires more from our care teams, so we didn’t want to put in a software system that would add to their burden.
“We wanted to develop something that’s easier to use because a lot of the mainstream solutions have been out there for decades. They’ve been upgraded over the years, but the way the screens are set up and how clinicians interact with them hasn’t really changed. There are still a lot of tabs, a lot of clicking, and a lot of hunting for information. We shared our vision with Harris Healthcare and discovered that they too were interested in reimagining the EHR, so we entered into a partnership in January 2022. The teams here at CIUSSS West-Central Montreal serve as the clinical and strategic experts, and the Harris Healthcare team provides the software development expertise.”
JGH doctors, nurses and administrative staff have had numerous meetings with the
Harris teams at which they describe what they need clinically “because we don’t want to end up with software that doesn’t work for us. We want the software to support the clinical reality,” said Dr. Cross.
The end goal of this innovative project is a modern enterprise EHR called Harris Arc, which will be used not only at the Jewish General, but across the CIUSSS network to fully incorporate the clinical information architecture across the care and social services continuum.
Another goal for Harris Arc is improved data accessibility. Years ago, explained Dr. Cross, provincial government budgets were based on volume alone. Today, they also take into consideration the quality of care delivered, which means there’s financial risk associated with hospital readmissions and failure to follow standards-based care.
“So, we wanted to make sure that we have access to the data necessary for all of our quality improvement initiatives,” said Dr. Cross. “Historically, there have been challenges accessing data from EHRs that are in a proprietary format and difficult to get to. This often resulted in extra charges for a health system to access its own data.

We are making sure to follow a more modern standards-based design approach to ensure that data is available and accessible for necessary purposes.”
Dr. Cross, a primary care physician with a sub-specialty in clinical informatics, is originally from the U.S. where he worked in the U.S. Department of Health and Human Services’ Office of the National Coordinator of Health Information Technology. As a medical officer and Medical Di-

CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 29, Number 6 September 2024
Address all correspondence to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9 Canada. Telephone: (905) 709-2330. Fax: (905) 709-2258. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2024. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2024 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9. E-mail: jerryz@canhealth.com. ISSN 1486-7133
rector for Systems Safety at ONC, he worked on a wide range of issues – from interoperability and safety to best practices around implementation of electronic health records and reduction of burden associated with health IT. Dr. Cross joined the Jewish General in February 2019.
The JGH-Harris partnership celebrated their first milestone in November 2023 with the release of the EHR’s first module, the Patient Timeline.
“It’s a chronological viewer of all of a patient’s information across our healthcare network that allows a clinician to zoom in and out and pan back and forth on one screen,” said Dr. Cross. The Timeline module has incorporated and normalized many disparate data sources from the CIUSSS current software ecosystem into a standard patient data model. The Timeline is serving to unlock previously siloed data and will also serve as a historical data load for the eventual future full EHR launch.
Clinicians can see when the patient was in the ER, the hospital, in long-term care, in rehab, and can see other community encounters along the care continuum. By clicking on the various encounters, they can pull up notes, lab reports, diagnostic imaging, and other documentation.
“This is the first time in our health network that we have had a unified clinical view of a patient’s trajectory. We released it to all our clinicians in November 2023, so it’s live now and includes five years of historical data.
“We have nurses working in long-term care who are now able to see what’s happening with their patients who are in acute care and can start planning for their return. We even have home care workers out in the community who can now optimize their home visit routes and save an hour of driving if they see their patient is currently in hospital.”
The Patient Timeline module and the EHR as a whole use Microsoft Azure’s cloud environment with its full security suite. It’s compliant with Quebec’s certification process for health software.
The system is also language-agnostic; it is built to support both French and English at the individual user’s configuration settings level.
Simon Beck, vice president of Sales for Harris Healthcare, commented that the Harris development team is using FHIRbased technologies to promote interoperability and aims to link all major systems to its new Patient Timeline. “It will take feeds from all of the major systems,” said Beck. He observed that interoperability and the ability to include data from different parts of the patient journey are critical to producing the best outcomes. “Healthcare isn’t just
CONTINUED ON PAGE 8
Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Office Manager Neil Zeidenberg neilz@canhealth.com
Contributing Editors
Dianne Craig dcraigcreative@yahoo.ca
Dianne Daniel dianne.l.daniel@gmail.com
Dr. Sunny Malhotra Twitter: @drsunnymalhotra
Norm Tollinsky tollinskyn@gmail.com
Art Director
Walter Caniparoli art@canhealth.com
Art Assistant Joanne Jubas joanne@canhealth.com
Dr. Justin Cross, chief digital health officer, JGH.







Humber becomes MEDITECH’s first Expanse innovation partner
BY JERRY ZEIDENBERG
TORONTO – Humber River Health has been selected as MEDITECH’s first collaborator in its Expanse Innovation Partnership program, in which the Boston-area electronic medical records company will work with large and technologically sophisticated healthcare organizations to advance the abilities of its web-based EHR for all customers.
“We’re bringing our capabilities in technology to the program, as well as our resources as a living laboratory to improve care for patients,” said Barb Collins, president and CEO of Humber River Health, which has been a long-time user of MEDITECH.
Collins asserted the work will benefit Humber patients, and the innovations developed will also be used by MEDITECH with its customers worldwide. “We have a duty to help improve patient care for everyone,” said Collins.
Humber River Health emerged in 2015 as one of the world’s first “digital hospitals”. It was built from the ground up with many computerized systems – from automated climate controls and advanced infection management to one of the industry’s first “command centres”.
The command centre brings data from multiple systems to a centralized room, where clinicians and administrators can monitor the performance of the hospital –including patient flow, length-of-stay, and possible logjams – while watching a wall of display screens. Importantly, Humber River Health worked closely with the command centre supplier – GE HealthCare –to refine the technology.

Collins said, “We have experience working with vendors to produce technology that helps our patients.”
For its part, MEDITECH is opening up its own resources to the Innovation Partnership, contributing access to its experts and adding capabilities to Expanse, the company’s most advanced system. As part of the initiative, MEDITECH will also collaborate on dedicated Innovation projects in addition to ongoing product development.
“We’re providing a direct link to our development and product teams,” said Helen Waters, executive VP and COO with MEDITECH. “Together with Humber River Health, we’re hoping to achieve an even higher level of EHR development.”
Waters noted that about 50 percent of the company’s employees are involved in

technological innovation and development.
Working together, the hospital and the company plan to speed up the rate at which innovations can be produced, tested and delivered.
“Our focus right now is on AI, and how to use it to unburden our physicians,” said Peter Bak, Humber’s CIO. He noted that the administrative burden on physicians has become a huge problem –many studies have recently identified this as an issue afflicting physicians worldwide. Not only does it take time away from patient care, but it also robs doctors of time with their families.
“We have the data scientists and engineers who can solve this problem,” said Bak. “We have the ability to build things to unburden the physician, using AI tools like text generation and relevancy.
Symposium on monitoring radiation exposure in medical imaging
Hotel Estrimont, Quebec, Canada • September 23-25, 2024
Radiation dose monitoring plays a critical role in medical imaging to ensure patient safety and optimize healthcare outcomes. Furthermore, dose monitoring supports compliance with radiation safety guidelines and regulations, fostering a culture of accountability and continuous improvement in healthcare settings. However, the implementation of dose monitoring and analysis programs remains a distant prospect for many healthcare facilities.
The symposium will:
• provide a platform to discuss and disseminate best practices and guidelines related to radiation dose monitoring among healthcare professionals, researchers, policymakers and encourage interdisciplinary collaboration.
• highlight technological advancements and innovations in radiation monitoring tools and software.
• develop recommendations to help provincial and national authorities in adopting better practices in radiation dose monitoring Register until September 18, 2024 - 6:00 PM Symposium on Monitoring Radiation Exposure in Medical Imaging, Magog (Quebec), Canada, September 23-25, 2024
If you have any questions, please contact patricia.pare.ciussse-chus@ssss.gouv.qc.ca
When searching databases for up-todate and meaningful information about their patients, clinicians shouldn’t be overwhelmed with data; instead, they should receive information that’s most useful to them. AI can help with that.”
Bak noted with pride that MEDITECH has chosen Humber River Health – a Canadian site – as its first Innovation Partnership collaborator. He added that Fraser Health, in British Columbia, is coming on board as the second partner in the program, with Canadians continuing to lead the way.
Fraser Health is also extending the use of AI in healthcare and its role in the MEDITECH Expanse system. One of its major projects is the Digital Twin, in which a virtual copy of a hospital will be constructed, and various functions and operations can be optimized through testing in a completely virtual environment.
When improved performance or outcomes are discovered to be achievable in the Digital Twin, they can then be transferred to the real-world hospital.
At Humber River Health, Collins observed that it’s not only the technological resources of the organization that are being brought to the table. When the hospital works on all types of computerization projects, it also relies on clinicians and administrators to join the project teams.
This is what it did with the command centre, which was supplied byGE HealthCare, but Humber River Health helped to develop. The resulting innovations are now used by other GE HealthCare clients worldwide.
“We have a culture of innovation here,” said Collins.
The Expanse partnership was signed with MEDITECH in March, and the partners were set to have their first strategy meeting in the summer. The meeting involved C-suite executives along with clinicians and MEDITECH representatives.
While the hospital executives knew they wanted to focus on the physician administrative burden, the meeting was designed to further refine the scope of the work to be done.
Bak noted that Humber River Health is already involved in a MEDITECH collaborative with other Ontario hospitals using MEDITECH systems.
As part of this work, Humber River Health is testing and deploying Canada Health Infoway’s e-prescribing system, PrescribeIT. It’s the first hospital in Canada to do so.
Bak said that Humber River Health will refine the system for use in hospitals. Other hospital users will then gain access to the lessons learned so they can deploy the e-prescribing technology, too.
He asserted that with the Innovation Partnership, Humber River Health will be creating new systems of its own. The systems will be add-ons to the Expanse system, and they will be used not only at Humber River Health, but potentially by other MEDITECH hospitals in Canada and around the world.
Bak observed that the pressure to improve electronic systems and the delivery of care has been quickly growing. “The pace is a lot faster than, say, 10 years ago. By collaborating, we can move a lot more rapidly.”
Helen Waters, executive VP with MEDITECH, looks forward to developing new solutions with Humber.
MAMMOMAT B.brilliant





Meet MAMMOMAT B.brilliant, a whole new mammography system that brings you the next generation of 3D mammography.
Experience:

Only 50° Wide Angle Tomosynthesis
Excellent depth resolution and in-plane resolution
PlatinumTomo
Scanning in under 5 seconds
PlatinumComfort

For both technologists and patients




Scan to learn more or visit: siemens-healthineers.ca/ mammomat-bbrilliant








Health811 expands its range, adding AI and appointment scheduling
BY JERRY ZEIDENBERG
TORONTO – Ontario’s Health811 service, which evolved from the province’s traditional, nurse-led telephone service, Telehealth Ontario, has rapidly expanded its range of capabilities since launching in 2022. It continues to offer access to nurses via telephone, but it’s now also providing a host of computer and smartphone-based options, including chat and video.
“It’s like a busy digital highway,” said Dr. Sacha Bhatia, a cardiologist and senior vice president, Population Health and ValueBased Health Systems, at Ontario Health. He notes Health811 is getting people connected to the right resources faster than ever before, thanks to the new slate of digital resources.
“We’ve added roads that connect people to towns and cities, so to speak,” said Dr. Bhatia. There’s an increasing variety of resources and tools available, giving consumers much more choice.
Ample choice also extends to language preferences, as Health811 is fully available in English and French, both by phone and through its digital offerings, and provides on-demand translation support for its phone line in more than 150 languages.
Artificial intelligence (AI)-based technologies are quickly expanding across the health tech space, and Health811 is no exception. Now, not only can a mother concerned about her toddler’s symptoms go to Health811’s website to chat online with a nurse, but she can also use an AI symptom assessment tool to get a quick opinion. Powered by ADA Health, the evidencebased system is the world’s leading program of its kind. It can tell users whether they need medical attention immediately, if it’s safe to wait for an appointment with a primary care provider or, if appropriate,
Lhow to manage their symptoms at home.
“If you’ve got chest pain, you always go to the emergency department right away,” said Dr. Bhatia. But for problems like fevers, rashes and minor aches and pains, the symptom assessment tool could very well advise the patient to go to a walk-in clinic or wait for an appointment with their primary care provider.
Usage of the symptom assessment tool is averaging over 2,000 completed assessments each month, while, unsurprisingly, the bulk of Health811’s interactions still stem from phone calls and online chats –
Health811 response times are very fast: Ninety percent of calls and chats are answered in under 90 seconds.
on average, the service fields a combined total of around 70,000 calls and chats per month.
Impressively, anxious callers don’t have to wait long on the line before their call is answered. “There’s a high level of responsiveness,” said Michael Hillmer, assistant deputy minister with the Ministry of Health and Ministry of Long-Term Care. “Ninety percent of calls and chats are answered in under 90 seconds.”
He said ample credit should be given to Health811’s industry partners, who include Orion Health, for creating the platform solutions that tie together the various components of the service and provide fast responses.
“Our ongoing work with Ontario Health in the Health 811 initiative highlights the importance of making healthcare and health information more accessible,” said Andrea Tait, SVP patient empowerment and equity at Orion Health. “By in-
tegrating digital tools and streamlining appointment scheduling, we’re working to simplify the healthcare journey and enhance access and equity across Ontario.”
Though Health811 is intended to support non-urgent health concerns, nurses can refer people to a hospital, in the event the situation could be an emergency, or to a Ministry of Health-funded virtual urgent care centre. These virtual urgent care centres are operated by hospitals and receive guidance and support regionally through Ontario Health.
With the current combination of nurse help lines, the symptom assessment tool, chats and the option of video visits, Health811 is providing more avenues to care.
Dr. Bhatia observed that over 80 percent of the encounters at Health811 are still phone calls to nurses. “But, as people really start to understand all that Health811 offers, we’re seeing more interest in the other services and resources provided,” he asserted.
Once they’re online with Health811, those accessing the service soon see that a variety of resources are available to them – including a health services directory, medical library and connections to mental health lines, addiction services, cancer screening
information, registered dietician supports, resources for equity deserving communities and more.
“Every Ontario Health Team (OHT) has collaborated with Health811 to ensure that local services are showcased,” said Dr. Bhatia. OHTs are clusters of acute, primary and community care providers that have been organized by the Ministries of Health and Long-Term Care.
Dr. Bhatia said that while the ‘main roads’ of the Health811 are now working, the Ministry is constructing more services to add value.
Hillmer noted that Ontario has created a provincial electronic health record (EHR) that includes components such as lab results, diagnostic imaging, drugs and more. It’s accessible using a viewer, and many doctors use it extensively.

“Now that more Health811 information is being captured, we’re looking at how to add it to the provincial EHR,” said Hillmer.
On another front, to solve the problem of access to a doctor, Health811 has been working with healthcare providers to tie their booking systems to Health811.
In the future, patients will be able to see, manage, and book appointments with their healthcare providers from one convenient place. This work will be happening over the next few years. This new form of scheduling is designed to remove a serious painpoint for many patients.
“We’ve got a lot happening on the horizon,” said Dr. Bhatia. “And the plan is to keep adding value.”
A digital navigator can troubleshoot and get patients connected
ONDON, ONT. – Every day across Southwestern Ontario, about 1,000 patients of St. Joseph’s Health Care London (St. Joseph’s) and London Health Sciences Centre (LHSC) receive care without leaving their home. These patients are benefitting from the convenience and expanding options of virtual care for numerous programs and services within the two hospital organizations. For those daunted by tuning in virtually, there’s now assistance from a new kind of patient care expert. Sam Ayoko doesn’t have a healthcare background, but for the patients he works with, he plays an invaluable role in their healthcare journey with a unique specialty –improving access to virtual care.
Ayoko is a digital navigator who is passionate about helping patients and their caregivers feel more comfortable and confident preparing for their virtual care appointment at LHSC and St. Joseph’s.
Patients and their caregivers can book Ayoko, who will ensure they are ready
for their remote appointment. “Our primary role is to bridge the gap between patients and technology,” says Ayoko.
“We provide one-on-one assistance prior to their appointment, helping them set up the necessary software, troubleshoot technical issues such as audio and video problems, and ensure a smooth and seamless virtual care experience.”
Mike Drabick refers to Ayoko as “a lifesaver.” For the most part, the 65-yearold is housebound due to various health issues and relies on virtual care to participate in numerous health, wellness, educational and social programs of Third Age Outreach – a communitybased program of St. Joseph’s – as well as essential medical appointments with the respirology team at LHSC and the heart failure team at St. Joseph’s.
The digital navigator walked him through uploading and using Webex on his computer for quick and easy access to virtual care.
“Virtual care and the support I received has opened my world – to being
active and to friends through Third Age Outreach, and to healthcare I need, without leaving home,” says Drabick. “I’m fairly new to the computer and was having big problems connecting. Now I can simply push the right button and I’m in.”
While virtual care is not new, a growing number of care programs and ser-
The digital navigator can walk patients through the steps needed to get them online and ready for virtual care.
vices now offer this option and an increasing number of patients are taking advantage of these web-based appointments as a convenient and safe way to consult with their care providers. Through the Virtual Care Program of LHSC and St. Joseph’s, patients can meet with their healthcare providers using a video conferencing platform from their home, community space, or any-
where the patient can safely and securely connect.
This shift, however, has highlighted a digital divide. While many are unfazed by tuning in remotely, some patients lack the necessary skills, assurance or resources to access virtual care effectively. A key role for Ayoko is providing patient-friendly education that appeals to all ages and tech comfort levels.
In addition to technical support, he can also: help patients safely access spaces that have Wi-Fi or devices in their community; access, fill in and return online documents and forms the hospitals may require; create email addresses that may be needed for virtual care; and offer an opportunity to participate in a practice virtual care appointment.
By ensuring individuals have the knowledge and skills they need to confidently navigate virtual care, Ayoko is playing a crucial role in removing barriers to virtual care and ensuring all patients of LHSC and St. Joseph’s have access to the care they need.
Dr. Sacha Bhatia
Say hello to Auxita and say good-bye to Patient Support Program paperwork.


Auxita’s seamless interoperability into your hospital’s EHR and connectivity to speciality service providers means more












































Learn how we can help your organization. Visit auxita.com today.





































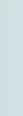
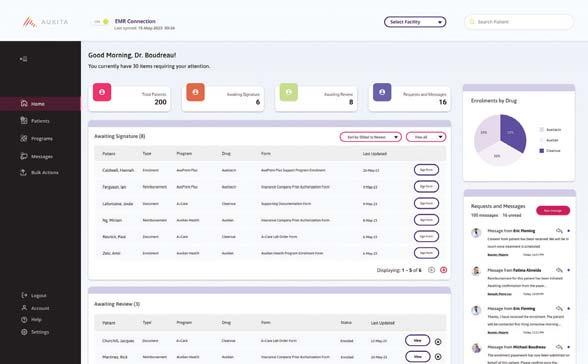
















































































Discover why hospitals across the country are using AUXITA
Seamless EHR integration: Whether it’s Epic or , Auxita is easy to use. 1 2 3 Enables optimal charting: All forms are completed and saved digitally for quick access. Less paperwork, more focus on care: reimbursement forms reduce paperwork and admin time.
Newfoundland and Labrador opts for ‘utility model’ of data storage
BY NORM TOLLINSKY
Robert Drover, director of information technology at Newfoundland and Labrador Health Services, no longer loses sleep over having to compete for capital every five years to replace the health authority’s data storage infrastructure – not since acquiring Pure Storage’s Evergreen/One storage as-a-service.
“These were battles we needed to have with everyone else looking for money from the government and, typically, information technology is the last to the dinner table when you’re competing against MRI machines,” he stated. “Everything we do in technology is so big now that we can’t operate on a capital procurement model. Every solution we’ve introduced in the last five years has had a multi-million-dollar price tag, so we had to find a way to operationalize these costs.”
With the five-year refresh point in plain view for its two storage solutions in 2020–both of which were based on spinning disk technology– Drover was determined to put an end to the battle for capital.
“A request for proposals went out and all the major players bid on it,” recalled Drover. “So did Pure Storage and when I read through their proposal, it was quite compelling. It gave us a lower total cost of ownership and the utility model that we wanted.”
Drover added, “It was a game changer not having to worry about procuring capital. I could now operationalize this expense.”
“Evergreen/One combines the flexibility of cloud storage with the security and performance of an on premise all-flash, secure sustainable infrastructure,” said Bill Bryer, Pure Storage healthcare lead for Canada. “This guaranteed, SLA-driven storage service improves how data is stored, mobilized, and protected.”
The upgrades are performed without any interruption of service. And rather than competing for scarce capital resources, the health authority pays a monthly subscription fee based on the consumption of the storage it uses.
With the Pure Storage solution, IT doesn’t have to worry about having enough storage capacity, especially with the volume
demand rate” they pay for when storage demand spikes.
“The utility model is the way of the future,” Drover predicted. “This is the way the cloud has presented itself to the industry. They operate on a utility model as well. The client pays for what they use, and they look after housing it, feeding it and maintaining it.
still happen, but it won’t get this immutable copy. What this means is it might hit us as it did before and shut us down, but we’ll only be down for however long it takes us to repoint it to the immutable copy, which is less than an hour.”
The use of solid-state drives also has an environmental benefit because Pure Storage arrays run on about the same power as

of data exploding and fluctuating due to AI and research-related demands.
“We wanted to have the storage available to us when we need it, but when we don’t need it, we don’t have to pay for it,” said Drover.
Bryer explains there’s a “committed rate” the health authority pays and an “on-
Montreal hospital devises its own EHR
given in the hospital now, it’s out in the community and in the home, too,” said Beck. “Clinicians need to see those records. Otherwise, they’ve got an incomplete record.”
Dr. Cross thinks the Harris Arc Patient Timeline could appeal to healthcare systems across Canada and elsewhere that also want a view of a patient’s trajectory of care across a network of health services along with improved usability and data accessibility, especially for jurisdictions that contain multiple clinical data source systems. Quebec’s Ministry of Health has classified the Jewish General initiative as an innovation project.
The JGH and its software development partner are targeting the launch of Harris Arc for the end of 2025. The EHR will initially be launched at the hospital itself and the medical clinics associated with it, to be followed by the long-term care facilities and rehabilitation hospitals in a second phase and the community care centres in phase three.
“We keep reminding ourselves that we have to keep the clinicians at the center of the design process, because we know that when we take care of our teams, we can ultimately deliver better care to patients, which is why we’re all here. We are proud of what we’ve accomplished so far, and we are
The new EHR, Harris Arc, will be launched in waves, in hospitals and clinics, followed by long-term care and rehab.
very focused on getting this done. We think that others will find value in it as well.”
Dr. Lawrence Rosenberg, president and CEO of CIUSSS West-Central Montreal, said that Arc is a perfect complement to “Care Everywhere”, the CIUSSS’s broad approach to patient-centred care. Its goal is to achieve the right outcomes by delivering the right care at the right time in the location that is most appropriate, safest and most convenient for healthcare users.
“Customers are looking for a service that delivers a cloud operating experience, but also has predictable costs,” noted Bryer.
With Pure’s as-a-service model, customers get the cloud operating experience, in a non-disruptive architecture backed by 10 guaranteed SLAs, including performance, capacity, availability, efficiency, and cyber recovery.
The Pure Storage proposal also solved another problem by relieving Drover’s IT team of responsibility for the care of the solution.
Recruiting IT resources is one of the health authority’s biggest challenges. “On any given day we have 30 to 40 open positions, so I can’t use my staff to be caretakers of this equipment. I need my staff to work with the doctors and nurses and everybody else to help solve the challenges they have. And who better to care for the equipment than the people who built it? We benefit from that because all of the security patches and updates are taken care of,” said Drover.
Easing the burden on IT resources is also critical as the department has its hands full with several major projects, including the adoption of an Epic EHR, a personal health record application and a virtual health solution.
Having experienced a ransomware attack in October 2021 that impacted the delivery of healthcare services, Drover is confident that the Pure Storage solution will expedite recovery in any future disruptions.
“This technology from Pure Storage gives us an immutable copy of our data,” he explained. “A ransomware attack can
a toaster, said Bryer. “That’s important when you consider that data centres currently account for about 2 percent of the world’s power consumption and, as AI kicks in, the volume of data storage increases 15 to 20 percent per year.”
Drover estimates that the all-flash arrays reduce the department’s carbon footprint by 40 percent and saves it in the range of $100,000 in electricity costs per year.
Lightning-fast data retrieval speeds are yet another benefit of Pure Storage’s Evergreen/One solution, remarked Drover. “This means that when a doctor needs an X-ray, it’s instantaneous, so the end-user experience is much better.”
“Pure Storage continues to revolutionize enterprise data storage and eliminates storage change management outages forever,” said Bryer. “Investing more than 20 percent of revenue in R&D, we believe that Pure Storage continues to be the only data storage platform future-proofed for innovation.”
Founded in 2009, Pure Storage has offices around the world, over 12,500 customers, 5,600 employees, annual revenues of US$2.8 billion (most recent full year earnings announced in February) and one of the highest net promoter scores in the industry of 82, but “is still relatively new to the game,” acknowledged Bryer.
With Pure Storage, organizations have ultimate simplicity and flexibility, saving time, money, and energy. Drover and his team are one of many customers realizing the value Pure Storage brings to their organization.








rele







Make a Tangible Difference with MEDITECH Expanse AI Solutions




anse int xp CH E
antinformation fo elev e int decisions. Th — n tssuppor
g dy seein ea e alr
MEDITE inform fo ore e m mak
advan
egrates o impr t edm
ent en docum m h or elligent platf e mak es — th eplac ot r
tremendous impact
e wh t a tim . A y ar e , that th ast e f e pilot p . Som yqualit
vider efficien o es pr improv out is v n vider bur o en pr , an oncise e c mor e epor ants r ticipar ac dous imp tremen d m , an cies
al, this solution e y r er isk a e r e th reduc d
d , an counters d linicians fin elps c e g car in echnology ed AI t anc administr omissions twic e qualit not e ar W “ dens e bur dministrativ
MEDITECH Expanse integrates advanced AI technology that supports — not replaces — the people making care decisions. The intelligent platform helps clinicians find relevant information, efficiently document encounters, and make more informed decisions to improve patient care.
e. atient car e p ov
eat y can cr e t that th gs an e-savin on tim ct tantly ost impor reduces ccidental ies e summar at ced d enhan
twice as fastmore concisereduce the risk of accidental omissionsreduces administrative burdensimproves provider efficiencies enhances patient care
Best in He enhan wor e f althcar
e atient car es p enhanc ward.”
vide Bet o o pr e t dat
Dr
Chief Medic
g our man ivin — dr ov , F
ity ty uthor th A aser Heal r fficer ation O alInform fo yeenHassanali.Amye my r r. alth. er He t tantly,
aser He Fr with aut uthorit th A al ation of c er o gen ently deplo r y is cur entation, in linical docum
g AI in its MEDITE yin g th cludin anse EHR t xp CH E our ospital c e h o assist y. se summar


Scan this code to learn more about MEDITECH’s AI solutions including Expanse search and summarization, powered by Google Health, conversational AI, and ambient listening.
c He inc n m ar o le ode t conv th,al sear luding e MEDITE or d , an sationalver ization d summar h an arc sCH’ ening ambient list y ed b wer , po
The latest on AI in healthcare: 10 trends busy leaders must know
BY ALEXANDRA T. GREENHILL, MD
Whether you have been to trying to catch up to the rapidly changing AI landscape or never really had a chance to understand the AI basics in the first place, here are the 10 key trends to know about AI in healthcare in order to be up to speed:
1. This is just the beginning of the age of AI – the only choices we have are how we respond and whether we can learn from the past. The move of AI into every aspect of our lives, including healthcare, is well underway and is simply inevitable. We need to understand how we can steer these changes to fulfill their potential with the minimum missteps and best use of funds. We also need to learn from the first wave of digitization of healthcare and its many issues – from massively overrun budgets and timelines to unintended negative impacts such as reduction of access, increased fragmentation and extensive provider burnout.
2. Canada has played a huge role in AI, but we are at risk of falling behind. Two of the “Godfathers of AI” who received the Turing Award for laying the foundations for modern AI are Canadian – Yoshua Bengio and Geoffrey Hinton. We boast as a country the highest concentration in the world of researchers in deep learning as well as the highest concentration of AI startups in the world. Launched in 2017, Canada’s national AI Strategy was the first in the world. That said, we are unfortunately not leading in the next way of applying these discoveries to real life, and this is a massive opportunity that shouldn’t be missed. One of the key strategies for success is to upskill the AI know-how of the
people in the healthcare system so they can get involved in the design, deployment, use and evaluation of these new approaches.
3. Definitions really matter – always ask what is specifically meant by “AI” in a given exchange. AI is a term applied loosely to any concept related to data and automation – from Machine Learning (ML) to Human-in-the-loop systems (HITL) to Generative AI (GenAI)/Augmented Intelligence (AuI or often just abbreviated AI) to true Artificial General Intelligence (AGI). Read the Primer for AI in Medicine for a quick guide on these core concepts, so you can better understand what is being discussed and thus avoid the fate of the duped leader from the old fable “The Emperor’s New Clothes”.
4. Regulation…it’s coming. While some jurisdictions are creating healthcare specific laws, in most cases, the first regulations of AI are voluntary and generalized. It will take some time to create healthcare specific guidance. In the meantime, it can be a challenge to decide whether to proceed and take the risk of having to change things once the regulation becomes available.
5. To AI or not AI: Do you really need to use AI for a given project? Not everything needs AI – in the current excitement, AI is being added to literally everything. The opportunity cost must be considered, as should the effort required and risks to be managed. Get in the habit of asking more questions about why AI is the right approach and what other solutions were considered.
6. The secret to unlocking AI for health is data! Unlike ChatGPT, which had the entire internet of data to train on, data is scarce in life sciences and needs to be reflec-
tive of the context the algorithm will be used in. It makes sense that it will be hard to adapt AI developed by looking at how patients with asthma do in a hospital in a major city, to then develop predictions on how patients with asthma will do in a rural community setting or at home, or if they have more than just asthma as a diagnosis. Our data in healthcare is mostly siloed, fragmented, unstandardized, blocked by data sharing obstacles and mostly also just plain missing – while over 95 percent of care happens at home, most of our accessible data sets are healthcare provider and organization-focused.

7. Don’t think “Is there bias?”, but rather “What bias is there?” Biases can come from the data used to train the models, the design of the algorithms themselves, or the ways in which they are deployed. The recognition that biases are an inherent part of AI is the first step in addressing AI related issues that otherwise may remain unnoticed.
8. The three main domains of application of AI in healthcare are to support clinical, administrative and research objectives. The applications that are likely to advance faster are domains where large data sets are available, the risk of errors is lower, there are significant needs that can’t be easily met with other methods and there are clear direct economic benefits that justify the costs and risks.
9. There is very limited evidence avail-
able for health AI’s effectiveness and safety, plus our entire model for how we generate research needs to be rethought. There aren’t many studies yet into the risks and consequences of AI systems, especially as they become more complex and integrated. In addition, our entire system of research generation and use – study, publish, disseminate – is challenged at its core by the privately owned data sets and algorithms that are in constant evolution and whose creators don’t have incentives to publicly share any evidence generated. 1 0. Lack of clarity on liability is the biggest unsolved blocker. For as long as it’s not clear who will bear the responsibility when things don’t go as planned or harm is caused, whether it’s because the AI system suggested a given approach or a human ignored the AI suggestions, this is the real rate limiting step of adoption of AI.
The next article will cover the must-read key reports and regulations that will help you get a deeper understanding of AI’s potential in health care and how to best harness it through optimizing deployments.
Dr. Alexandra T. Greenhill is CEO and Chief Medical Officer at Careteam Technologies, an award winning integrated care platform, enabling health teams to support their patients across the healthcare system. Associate Clinical Faculty, Department of Family Medicine, University of British Columbia, Canada, Coeditor “AI in Clinical Medicine” book, Wylie, 2023. Dr. Greenhill is also Chair of the Board for Physician Innovator, Board member of Halo Health and Canadian Institute for Health Information (CIHI). Views expressed are solely that of the author and are not made on behalf of these organizations.
IDS: Ontario’s most widely used solution for sharing health partner data
One of the most persistent barriers to better integrating care for patients is access to data, especially in a system that has traditionally operated in siloes. Integrated Decision Support (IDS) was developed to address these data “blind spots” through its data sharing platform and is now empowering a host of connected subscribers, including hospitals, home and community care, primary care, community health centres, community mental health, and paramedic services. Today, IDS is Ontario’s most mature and widely used collaborative solution for sharing integrated health partner data.
Through its platform, IDS offers data at a patient level across a continuum of healthcare services, giving subscribers a line of sight into the patient journey, even when they cross regional boundaries.
IDS links patient data for over 100 healthcare organizations, covering 9.8 million unique patients and over 180 million patient encounters.
IDS also integrates province-wide Statistics Canada Population Census information and the Ontario Marginalization Index, allowing population health equity
questions to be married with healthcare data utilization in a population health management approach, right to the patient level. These data are used for system planning, performance management and efficiencies, analytics, reporting, integrated care planning, outcome measurement and evaluation – all focused on improving quality of care for Ontarians.
Guided by the principle of “once-formany”, IDS is a provider-driven, collaborative community that simplifies data integration and common analytical challenges, supported by customer-focused training, education and knowledge transfer.
Harnessing data from a well-organized repository and set of tools, such as pre-built reports and dashboards, IDS helps save time for busy analysts and enables standardization and comparability of initiatives and indicators amongst subscribers.
Paired with IDS’s Tableau analytics platform, these reporting templates – developed in response to requests from the subscriber community – provide validated, ready-made reports that can be tailored to meet local needs. IDS supports care delivery organizations with a
view into their shared patients and the ability to cohort and segment populations by patient condition, patient geography, age, cost, and many more factors.
For example, IDS recently released two new Stroke Distinction Tableau reports, which provide subscribers participating in the Accreditation Canada program convenient, easy access to their or-
The data are used for system planning, performance management, analytics, evaluation and more.
ganization’s stroke distinction key quality indicator results in just one click.
The reports provide results for 13 stroke quality indicators for specific organizations and enable benchmarking with peers across nine indicators. Quarterly and annual indicator results are readily available, making monitoring and submission to Accreditation Canada effortless, and built-in flexibility allows IDS analysts to save customized versions of these reports for their organization.
What sets IDS apart: Subscribers
benefit from several features and services that set IDS apart, including timely access to data, and most notably, its unique ability to support local integration activities, such as Ontario Health Teams (OHTs), bundled care, and Integrated Care Programs.
Consultations with 37 OHTs in 2023 have resulted in new geographical-based catchments that equip IDS subscribers with the ability to easily select practical cohorts to support timely OHT-related analytics and planning efforts.
Now live on the platform, these OHT Catchments complement the Ontario Health OHT Attributed Population, allowing IDS subscribers to drill into patient-level details to discover drivers and patterns of healthcare utilization, and much more. IDS continues to add to its OHT reporting catalogue, which now includes hospital metrics for OHT Catchments, palliative care cohort monitoring, and frail seniors’ care transitions.
Subscribers also benefit from more granular collaborative Quality Improvement Plan (cQIP) measures that help evaluate the success of OHT initiatives.
Groundbreaking work with the
Alexandra T. Greenhill
UHN expands digital pathology to its partner hospitals in northern Ontario
BY SHAUNA MAZENES
It was almost two years ago, early in Dr. Klaudia Nowak’s medical career, that she received an urgent call in the middle of the night. With a patient on the operating table and the surgeons standing by, she had 30 minutes to diagnose a sample of human brain tissue. Her conclusions could alter the course of brain surgery.
“Needless to say, I was quite nervous,” Dr. Nowak, a gastrointestinal pathologist at the University Health Network, in Toronto, said of the diagnosis.
However, thanks to digital pathology, the biopsy was scanned and converted into a virtual image. Dr. Nowak sent it to a neuropathology colleague, the pair viewed it in real-time, and their diagnosis led the neurosurgery team to stop the procedure before it started.
This is just one example of the many ways digital pathology is revolutionizing patient care at UHN.
Now, UHN, the first multi-centre hospital in Canada to fully adopt digital pathology, is expanding it to 29 partner hospitals in Northern Ontario – giving these communities equitable access to enhanced laboratory medicine services.
“Digital pathology is bringing us to places we could have never even imagined five years ago,” said Dr. George Yousef, medical director of the Laboratory Medicine Program at UHN.
Pathologists, the doctors who diagnose cancers and infectious diseases, have traditionally done so by examining a biopsy on a glass slide under a microscope. In digital pathology, glass slides are converted into virtual images on a computer screen, allowing for faster, more precise diagnoses while eliminating the manual work of a microscope.
In the past, if a general pathologist needed a second opinion from a specialist they didn’t have, the glass slide would have to be shipped in the mail to the appropriate hospital for analysis. This process could take weeks, with the possibility of the slides breaking with the biopsy in it, posing serious safety risks.
Now, Dr. Yousef said, the flexibility of digital pathology can bypass geographic barriers around the world, speeding up consultation and diagnosis from weeks to days, days to hours, or even hours to minutes.
Bringing the infrastructure for digital pathology to Timmins Cluster Lab Services Program, Kenora Rainy River Regional Laboratory Program and the Sault Area Hospital – an initiative called We The North – will give more remote communities access to UHN’s specialized pathologists.
Northern expansion can also enable better metrics and data for communities that have been historically underrepresented in medical research.
The Lake of the Woods Hospital in Kenora recently began stocking new medications in their pharmacy to treat diseases that are common in the community – something Dr. Nowak said is a direct result of the high-quality, detailed pathology reports from UHN’s Laboratory Medicine Program.
“It’s amazing how we can collaborate

Dr.

UHN’s
endto-end digital pathway from patient biopsies to patient
with our northern partner sites to bring about change in the manner patients are treated,” said Dr. Nowak, who serves as the anatomical pathology director for the Kenora Rainy River Regional Laboratory Program.
Artificial intelligence also plays a key role in digital pathology, making diagnoses faster and more precise than the human eye.
“We can now use AI to significantly improve our capabilities and take patient care to the next level, something we call precision medicine,” Dr. Yousef said.
AI can help identify specific genetic disease patterns in biopsies and eventually develop algorithms to predict the best course of treatment for the patient based on their condition, he said.
Dr. Yousef adds that having access to digital files of human biopsies allows for the full engagement of a multidisciplinary
team in a patient’s treatment plan, which wasn’t previously possible in pathology. Now that everything is electronic, he said, oncologists, pathologists and surgeons can sit down together and have a complete view of everything related to the patient.
“It truly is a new era of pathology – a holistic approach to patient care,” Dr. Yousef said.
For Dr. Rumina Musani, digital pathology is more than just teamwork. For her patients, it can make the difference in a life and death situation.
“The ability for technologists to communicate immediately with pathologists can save lives as far as leukemia goes,” said Dr. Musani, a pathologist specializing in hematology at UHN.
One of the most urgent diagnoses hematologic pathologists may face is called acute promyelocytic leukemia. A patient
may be hemorrhaging all over their body and can die if they don’t start treatment immediately.
Dr. Musani remembers being a young pathologist on call and having to physically go into the hospital in the middle of the night to make that and other urgent diagnoses, trips that wasted valuable time. She adds that biopsies or blood smears aren’t always easy to read and often don’t present how they do in the textbooks.
“Not being able to access second opinions back then were very scary, high-pressure situations,” she said.
Now, being able to get a high quality second opinion in urgent cases is not only critical for safety of the patient, but for the development of a young pathologist, she said.
“Being able to consult your colleagues builds confidence,” said Dr. Musani. “Being alone creates fear.”
She adds it’s a big step for hospitals in Northern Ontario, who didn’t previously have access to specialized hematology pathologists.
“It’s really a good feeling when you’re able to find something that was missed, but to know you also helped save a patient’s life,” she said.
UHN is looking ahead to even bigger collaboration and recently signed with the Mayo Clinic to expand digital pathology into the United States. The next step is expansion in Israel and Brazil.
However, Dr. Yousef said digital pathology is a very expensive innovation that needs philanthropy to keep moving forward.
“We’re leading the way in Canada at UHN, but the idea is to create a global hub for digital pathology,” he said. “International collaboration will help build the case.”
Shauna Mazenes is a Communications Coordinator at UHN, in Toronto.

Dr. Klaudia Nowak, a gastrointestinal pathologist at UHN who also serves as the Anatomical Pathology Director for the Kenora Rainy River Regional Laboratory Program, says UHN’s “We The North” initiative is near and dear to her heart.
George Yousef, Medical Director of
Laboratory Medicine Program, said UHN is the first multicentre hospital in Canada to offer a complete
records.
Orchestration software at busy Brampton clinic results in quick improvements
ueen Square Doctors (QSD), a large and busy primary care clinic in Brampton, Ontario, partnered with CHIME Technology Inc. to address rising overhead costs and operational inefficiencies.
With support from the Innovating Digital Health Solutions (IDHS) Program, the Ontario Centre of Innovation, and the Ministry of Health, QSD implemented CHIME, an intelligent clinic orchestration platform.
Preliminary results after three months evidenced gross annual cost savings of over $160,000, roughly a 500 percent return on investment. Additional cost savings are possible as the use of the system expands and matures.
A comparison of pre- and post-implementation metrics revealed improved efficiency, staff satisfaction, and patient satisfaction. A key and surprising case study learning was to deploy the full system quickly, instead of incrementally.
“CHIME has been the biggest improvement that Queen Square has ever made,” commented Shelly Medeiros, director of operations, Queen Square Doctors.
This case study has demonstrated that CHIME can be successfully implemented in existing clinics like QSD to achieve multiple pillars of the Quadruple Aim of better care, better experience for staff and clients alike, all at lower cost. The magnitude of the savings achieved illustrate that CHIME is a scalable model that can contribute to the sustainability of the public healthcare ecosystem.
Queen Square Doctors (QSD) is a 36exam room primary care clinic located in Brampton, Ont. It hosts 19 family physicians and three registered practical nurses, along with other interdisciplinary healthcare providers, who collectively care for 30,000 patients.
Prior to this case study, these clinicians were supported by a team of four medical assistants (also known as “runners”), included within a complement of 26 administrative staff. QSD faced the same financial pressures of other clinics within primary care. In response, they have been leaders in finding and implementing solutions that reduce costs while improving care and experience.
For its part, CHIME Technology Inc. is an Ontario based company that develops and deploys a clinic orchestration platform. It was designed in collaboration with clinicians and clinic operators to address key financial and operational challenges faced by clinics like QSD. CHIME has been successfully deployed to numerous newly built clinics, but there have been few opportunities to demonstrate a meaningful improvement in an established organization.
The Innovating Digital Health Solutions (IDHS) Program was funded by the Government of Ontario and administered by the Ontario Centre of Innovation on behalf of the Ministry of Health and Ontario Health. This program supported the deployment of CHIME to QSD with the key goals noted above.
CHIME is a clinic orchestration system –deployed on a variety of tablets, screens, and

kiosks – that coordinates and automates its real-time day-to-day operation. This platform is analogous to restaurant technologies used by hosts, waiters, and kitchen staff to coordinate seating guests, taking orders, and delegating kitchen duties. The cornerstone of this platform is tracking and using the real-time status of clinicians, staff, patients, and rooms to achieve improved user journeys, as noted below.
•Patient User Journey: A patient enters the facility; checks-in via a kiosk, sits down; sees their name and wait time on a waiting room screen; is automatically assigned to a clean exam room; is informed via visual and audio cues to proceed to their assigned room.
•Medical Assistant User Journey: A medical assistant is doing admin work on a computer; a tablet pings to say a patient in room 5 needs prep; they proceed to room 5, and check into the room via a wallmounted tablet; they prep the patient in the room; they check-out of the room via the same wall-mounted tablet; the wallmounted tablet tells them there’s another patient in room 7 that needs to be weighed; the medical assistant proceeds to room 7.
•Physician User Journey: A physician sees their patient in room 3 has been prepped and proceeds there; the wallmounted tablet outside the room reminds the physician that PPE is recommended given this patient’s chief complaint; the physician checks-in via the tablet; when done, the physician uses the wall-mounted tablet to “add shots” for this patient; the wall-mounted tablet tells them their next patient is in room 9.
•Manager User Journey: A clinic manager is deciding whether there is room for another family doctor on Monday afternoons. The technology advises Monday afternoons are only running at roughly 70 percent capacity of Wednesday mornings, and concludes there is room for another family doctor to see patients on Monday.
Evaluation metrics: For the purpose of
2024 and continued uninterrupted until March 31, 2024. Use of the actual system has continued post April 1, 2024 and there are no plans to stop its use.
Financial Impact: Given the financial pressures on primary care, this evaluation metric was the single most important consideration. CHIME traditionally advertises two types of financial impact: 1. By automating tasks, staffing needs can be reduced, thereby reducing operating costs. 2. By reducing the per MD usage of exam rooms, more clinicians can see more patients from the same physical real estate.
Operating Costs: During the evaluation period, two specific roles were identified as being measurably impacted by automation.
•Runners: Previously, QSD required four runners to summon, prep, and escort every patient from the waiting room to their assigned exam room, as well as clean and turn over rooms between patients. With the implementation of CHIME, QSD reduced this role to two runners. This is because the step of summoning and escorting most patients from the waiting room to the assigned exam room was automated and two runners were now sufficient.
this case study, seven specific evaluation metrics were identified in collaboration with QSD. These metrics were identified prior to deployment of CHIME for the purpose of obtaining a suitable evaluation baseline so that a validated outcome could be measured. A summary is included below.
•Would there be a measurable financial impact? At least $160,000 annually, or a 500+ percent annual return on investment.
•Would support tasks be measurably automated? 87 percent of patients checked-in
Preliminary results evidenced gross annual cost savings of over $160,000, roughly a 500% return on investment.
via a kiosk 94 percent of patients were automatically roomed.
•Would clinic nuances be accommodated? Yes, via qualitative and anecdotal measures.
•Could internal staff be retrained and redeployed? Yes. Frequency of average patient phone wait hold times exceeding five minutes reduced from four days monthly, to zero. 12 percent increase in administrative tasks completed per week by support staff.
•What would be the staff experience? Clinic support staff perceive improvements across the board. Four out of five support staff perceive a reduction in daily stress.
•What would be the physician experience? Clinic physicians perceived benefits primarily in the areas of staying on time and overall patient flow. One out of five physicians perceived a reduction in daily stress.
•What would be the patient experience? Three out of four patients advised they were happy or very happy with the kiosk self-check in experience. Only one out of 10 were very unhappy. Four out of five patients advised they perceived the estimated wait time feature to be useful or very useful.
The evaluation period began January 1,
•Receptionists: Previously, QSD required multiple receptionists at the front desk windows to check in every patient, including asking standard questions of every patient, as well as other ordinary receptionist tasks. The exact number on duty would vary over the course of each day, based on how busy it was. With the implementation of CHIME, QSD reduced this role by approximately two full-time equivalents. This is because most patients could now check in via a kiosk.
QSD reports that in combination, these four eliminated positions cost the organization at least $160,000 per year, or an average of $40,000 per position. In comparison, QSD’s annualized cost of CHIME is roughly $30,000 per year, resulting in a 500+ percent annual return on investment. That is, for every $1 invested, the organization recouped at least $5. Notably, QSD elected to re-invest at least $80,000 of this annual $160,000 in savings by increasing the staffing in other areas of the organization. QSD therefore achieved net $80,000 in annual savings while simultaneously increasing staffing in some areas.
Increasing Capacity: Anecdotal evidence suggests the potential for increased capacity is there. For example, one highvolume physician was previously allocated three to four rooms whenever he was seeing patients. With CHIME, only two rooms needed to be allocated to him, creating potential room capacity for adding additional clinicians into the clinic. This observation is consistent with an anticipated long-term benefit of the technology, namely, increasing the capacity of the clinic by 40-60 percent, without any renovations or expansion.
The primary author of this case study is Tess Walker, an experienced primary care leader with day-to-day as well as strategic experience in her role as Director of Operations of Magenta Health, a network of primary care clinics in Toronto.
Cyber-security strategies must consider the mental health of staff
BY FLORIN SOLTAN
With cyber attacks on the rise, organizations need strict cybersecurity measures to prevent full-blown breaches from causing damage to finances, reputation, and the mental health of those involved. The impact of a ransomware attack can be debilitating and long-lasting on a company’s business and morale.
According to the Canadian Medical Association Journal, there have been at least 14 major cyber-attacks on Canadian health information systems since 2015, with serious impacts, including ransomware.
This impact was severe after the co-ordinated ransomware attacks on Bluewater Health, Chatham-Kent Health Alliance, Erie Shores HealthCare, Hôtel-Dieu Grace Healthcare and Windsor Regional Hospital, and their shared service provider, TransForm Shared Service Organization. The resulting stolen data was published online and negatively impacted operations as teams worked to restore services.
Overlooking the human factor of cyber security: While good cyber-security practices typically focus on computing devices and networks, the human factor is often overlooked. Healthcare IT security professionals are always on high alert and the fear of missing a critical threat or vulnerability can lead to stress and anxiety. From the ongoing risk of ransomware attacks to phishing emails and malware, it can feel that cyber security threats are becoming more advanced and persistent.
IT workers bear the responsibility of safeguarding sensitive patient record systems and data, critical care management systems that lives depend on. The fear of making a mistake that could compromise patient safety or privacy can weigh heavily on their minds. And the relentless pace of cybersecurity work, especially during incidents or breaches, can lead to burnout and high-pressure situations that take a toll on mental health.
Supporting the mental health of IT security professionals is crucial for their well-being and effectiveness. Flexible work schedules, backup staff, and health plans are just the beginning. Companies should also promote work-life balance, encourage employees to take breaks and disconnect from work when needed, and help workers monitor and reduce stress levels.
The importance of company-wide awareness and protection: Cyber security stress is inevitable among security professionals, and discussing burnout can be complicated. However, IT security leadership must address these workplace issues to avoid compromising team members’ wellbeing, talent retention and productivity.
One way to support IT team members is to spread the responsibility of cyber-security among all staff to proactively enhance the organization’s security posture. This can be accomplished by:
•A security-first culture backed by enforced policies and guidelines that define expected behaviours and outcomes.
•Mandatory security training to reduce vulnerabilities and emphasize ownership by teaching everyone how to respond to a perceived cyber attack.
•A disaster recovery plan that addresses safe data storage, backup, and quick recovery from a data-destructive event, assuring employees, patients, and partners that their information can and will be protected.
Remember, cybersecurity is everyone’s responsibility. By fostering a security-con-



scious culture, organizations can significantly reduce risks and protect valuable assets. By prioritizing employee well-being and implementing measures to mitigate the impact of cyber attacks, healthcare organizations can better protect their patients, customers, and critical infrastructure.



Arc Patient Timeline

Florin Soltan is a Cyber Security Product Manager at Acronym Solutions. He helps customers protect against digital threats by developing and implementing security strategies to safeguard sensitive data and infrastructure.




Transforming Healthcare Delivery





Don’t Let Blind Spots Compromise Patient Care.
Key Benefits
Unify Fragmented Patient Data
See the entire patient journey in one interface, eliminating the need to log in to separate systems.
Drive Informed Clinical Decisions
Empower clinicians with seamless, anytime access for informed collaboration, wherever they are.
Boost Operational Efficiency
Effortlessly integrate and consolidate data from legacy systems.
Improve Patient Care
Gain a comprehensive view to enhance care delivery.
Prevent Clinician Burnout
Streamline workflows and reduce the burden on healthcare professionals.
Why Choose Arc Patient Timeline?
Proven Expertise
With over 40 years in the medical so ware space, we understand the challenges physicians and clinicians face.
Transform Your Care Delivery in ree Easy Steps:
Request a Demo
Email harrisarc.health/contact-us
Receive a Customised Quote
Tailored to your unique requirements.
Gain a Clear Vision
Experience the power of our advanced healthcare data solution.
Tailored Solutions
We've partnered with healthcare providers to develop Arc Patient Timeline, addressing your specific needs.
harrisarc.health
info@harrishealthcare.com
+1 (800) 393-0278
Groundbreaking mammography imaging technology comes to Canada
Siemens Healthineers’ MAMMOMAT B.brilliant platform has received Health Canada licensing.
OAKVILLE, ONT. – Siemens Healthineers announced that MAMMO-
MAT B.brilliant, the company’s first completely redesigned mammography platform in more than a decade, has received Health Canada licensing. This innovative system with wide-angle tomosynthesis offers significant advancements in image quality, user ergonomics, and patient comfort level.
“We are excited to bring MAMMOMAT B.brilliant to Canada to offer more accurate, faster and conclusive breast cancer screenings for women to exclude the maybes,” said Peter Vidic, X-ray business line manager at Siemens Healthineers, Canada. “It’s a completely new system design that is focused entirely on the patient and the mammographer,” he added.
PlatinumTomo, the new 3D technology, will acquire the tomosynthesis volume at the unique angular range of 50° – the widest angle on the market and equal to the company’s current system, the MAMMOMAT Revelation – for a high level of depth resolution and tissue separation.
The 3D portion will feature completely new acquisition technology, with a new detector and Xray tube design based on the premium z-sharp (flying focal spot) technology found on the company’s computed tomography scanners.
The flying focal spot technology is designed to allow for continuous tube motion, while holding the focal spot size effectively stable. UltraHD reconstruction technology will provide customizable image impression as well as a new form of synthetic 2D and 3D imaging.
Enhanced patient comfort: MAMMOMAT
B.brilliant, with a scan time of around five seconds, is the fastest wide-angle tomosynthesis on the market, creating a 3D image with high-depth resolution in the shortest time possible.
It offers a 35 percent faster acquisition speed compared to other devices, making the examination more comfortable for patients. The ComfortPackage, which is standard on the system, includes an ergonomic hand grip and an optimized, stationary face shield that allows the patient to lean into the system during image acquisition for greater stability and ease of positioning.
These new features are combined with a redesigned ambient light display, personalized soft breast compression, and curved breast compres-
sion paddles. These features can not only reduce patient discomfort but also improve breast positioning and enable more consistent image quality.
Advanced ergonomics and workflow for technologists: Several new features benefit the radiologic technologist. They include a prominent display monitor that enables the technologist to clearly see patient information and work steps, regardless of where the technologist is positioned.
The automated ComfortMove ergonomic feature reduces physical strain on the technologist, who can move the tube head independently of the bucky for safe, easy patient access during positioning without bending or twisting. A laser positioning guide helps the technologist accurately position the patient’s breast. Together, these user features can significantly improve workflow.

Commitment to women’s
health: “With the licensing of the MAMMOMAT B.brilliant, Siemens Healthineers is proud to bring this next-generation mammography technology to Canada,” said Melissa Reeve, women health clinical product specialist. “Our commitment to women’s health is unwavering, and we believe in providing access to the most advanced screenings and diagnostics available.”
For more information on MAMMOMAT B.brilliant, please visit www.siemens-healthineers.com/en-ca/mammography/digitalmammography/mammomat-bbrilliant
INOVAIT funds developers of image-guided therapies that use AI
TORONTO – INOVAIT and the Government of Canada in June announced a $10.7 million investment in seven commercialization-focused R&D projects under the second round of INOVAIT’s Focus Fund program.
Founded by the Sunnybrook Research Institute and supported by the Government of Canada’s Strategic Innovation Fund, INOVAIT is Canada’s network focused on advancing imageguided therapy (IGT) through the integration of artificial intelligence, big data, and machine learning.
The INOVAIT network supports Canadian innovators who are harnessing the power of AI to improve image-guided diagnosis and therapy and to improve healthcare outcomes.
“Canada has tremendous strength in the research and development of medical imaging and AI technologies. We need to capitalize on this opportunity and leverage both these strengths to advance technologies that can improve clinical outcomes and healthcare efficiencies,” said
Kullervo Hynynen, co-executive director of INOVAIT and vice-president of research and innovation at the Sunnybrook Research Institute.
Through this iteration of the Focus Fund program, the seven selected high-potential projects will integrate machine learning capabilities into IGT technologies. Selected Focus Fund projects were evaluated based on their potential impact to innovation, healthcare, and economic development.
Focus Fund project members will invest an additional $21.3 million into these projects for a total influx of $32 million into the Canadian IGT sector. The Focus Fund contributions will help attract investments into these Canadian technology companies, create jobs for highly skilled professionals, and cement Canada’s status as a global leader in IGT and AI innovation.
One of the seven companies to receive INOVAIT funding in the latest round was Oncoustics, a Torontobased medtech startup that develops advanced AI solutions for low-cost,
non-invasive surveillance, diagnostics, and treatment monitoring of diseases with high unmet clinical need, such as asymptomatic structural liver disease. “We are thrilled to be part of the INOVAIT network as we develop our novel AI solutions to advance diagnostics and deliver precision treatments using low-cost, point-of-care ultrasound systems,”
Oncoustics is one of the innovators that will receive funding to expand its development.
said Beth Rogozinski, CEO of Oncoustics. “This pan-Canadian effort promotes the future of healthcare that leverages AI to democratize access and improve outcomes.”
Oncoustics, alongside clinical partners at University Health Network (UHN), was awarded this funding to enhance its existing OnX Liver Assessment Solution. The OnX is a software-as-a-medical-device (SaMD) so-
lution that captures and interrogates the raw RF signals from ultrasound to assess structural liver disease.
The raw sound signals provide a wealth of information that goes beyond image analysis and enables powerful clinical decision-support tools right at the point of care.
The Focus Fund-awarded project is expected to receive up to $2 million to advance Oncoustics’ OnX Liver Assessment Solution that’s appropriate for high BMI patients and can be used for monitoring treatment response.
“Oncoustics’ innovative OnX Liver Assessment Solution is poised to leverage existing imaging data to power transformative AI-driven healthcare results,” said Raphael Ronen, co-executive director of INOVAIT. “We are pleased to support high-impact projects, like Oncoustics’, to greatly improve healthcare globally and drive economic development in Canada.”
The Oncoustics solutions for ultrasound will be submitted for regulatory approval in the United States, Canada, and the European Union.
ORION HEALTH VIRTUOSO DIGITAL FRONT DOOR

Orion Health’s Digital Front Door is an omni-channel consumer engagement platform that integrates data, tools and services for end-to-end healthcare navigation and management. Making it easier for patients to navigate their care and connect with the services they need.
Discover how we’re simplifying the healthcare journey and enhancing access and equity for all. Find out more at www.orionhealth.com

Getting online appointment booking right: The jurisdictional scheduling approach
Interoperability should start with the most frequent transaction in the entire healthcare system.
BY DR. JONATHAN MARCUS AND DR. KARIM KESHAVJEE
Have you tried booking an appointment with your doctor recently?
Was it as easy as making a reservation at your favorite restaurant?
Why not? That’s what we were curious to know.
It turns out that current booking systems are fragmented. Appointments can be arranged by phone, email, portals, fax and Online Appointment Booking systems (OAB), often by multiple systems at a single location.
Communications can be lost since they can’t be tracked, patients fall through the cracks, delaying patient treatments and leading to poor outcomes. Ontario introduced OAB Standards in 2021 but it hasn’t led to widespread uptake. It took Quebec 10 years to get their system up and running, but that system is unlikely to work elsewhere.
All players, including patients, providers, organizations and government, agree on the need to break down digital silos and create better data infrastructure to bring about system transformation. This is necessary not only to provide a better, safer experience for patients and providers, but also for government and organizations to plan better, given their limited budgets.
We represent a team of researchers at the University of Toronto. After 30 years of studying digital health implementations, we came to the conclusion that the next steps towards interoperability should be directed at provider and service scheduling. Appointment bookings are the most frequent transaction in the entire healthcare system, exceeding lab tests and prescriptions by a large margin. They are also relatively simple compared to other data that we collect in the healthcare system.
The current approach for online appointment booking in Ontario is for each healthcare provider to implement a system in their own office. The systems do not talk to each other, nor do they talk to other systems.
This creates new silos that are difficult to break down. It forces everyone to start keeping a list of new websites for all the doctors they see. Maintaining databases with all the different online appointment booking systems across the province makes no sense. It increases administrative effort and slows clinics down. It’s the opposite of what was intended.
So what’s the solution?
In February 2024 our team published, Measuring and Managing Healthcare Supply and Demand in Real-Time. In it we presented a system design that aggregates all provider, location and organization schedulers within a jurisdiction into a single Jurisdictional Scheduler (JS).
Individual EMRs are linked to the JS through APIs. This includes, for example, physicians, allied health providers, labs, DI facilities, walk-in clinics, ERs, clinics, hospitals and programs.
Apps enable patients to book appointments with their doctor, their pharmacist and their specialists using a single solution. Data is available bi-directionally in real-time, just like GoogleMaps. All users contribute to and access system-wide scheduler data as well other user-identifying information, such as name of provider/location, contact info, specialty, language spoken and gender.

All users would have accounts that would be maintained by the users themselves. For providers and organizations, accounts would function as profiles that could be searched by other users.
Apps would be developed, providing users a digital front door to the JS with a consistent interface, two things sorely missing from the current piecemeal approaches. Providers could also access the JS directly from their EMRs with no need for another password.
The JS would have an adjudicator function that would apply booking rules. There would be basic rules that apply to all users such as those found in the Ontario OAB Standards.
Providers could customize their own rules such as a specialist only allowing booking if patients have a referral. A referral could be logged into the system as a digi-
The current approach for online appointment booking in Ontario is for each healthcare provider to deploy their own standalone system.
tal token. Another rule might be that a family doctor would only allow booking by patients on their roster.
Patients needing a family physician could search based on geography, preference, gender, etc. A patient with an acute problem such as a laceration could search the system for walk-in clinics and ERs and join a transparent queue. They could show up just in time, saving hours sitting in a waiting room.
Apps, as mentioned above, could be developed by vendors for users to access the jurisdictional scheduler. Apps would be interchangeable because of standardization of data and processes. This would enable competition in the digital health system like never before, driven by individual consumer choice, not procurement. Organizations and governments would have access to aggregated data to aid in planning. Ontario Health Teams (OHTs) could check the status of any component of their organizations– clinics, providers, admin, locations and programs in real-time. For example: appointment wait-times and physicians taking new patients. New providers and clinics could be added flexibly if they already had accounts in the JS. Government could view components of the sys-

tem at any point in time to measure supply, demand, access and wait-times. Data could be subdivided by region, primary care, specialties, ERs, hospitals, LTC and patients needing a primary care provider. This would enable planning without the months to years delay at present.
In April 2023, the Ontario MOH issued a ‘Digital health strategy refresh’. Among other things, it called for a digital front door, connecting all major digital and data users, building on Health811, seamless integrated care and simple digital tools for frontline providers that are not a burden. The jurisdictional scheduler concept solves all these problems elegantly in real-time.
The healthcare system is strained due to increased demand and poor efficiency. Patients are bearing the brunt; providers are burning out and quitting. Government is already paying for this – even if it can’t be measured.
We recommend the following steps.
The government should regulate:
•The building of a central repository of appointments and requests for appointments. This will enable a real-time view of supply of and demand for care. It will ensure the market can respond to market needs while ensuring standardization of appointments.
•The setting up of a user account system for patients, providers,facilities and organizations with API access. The accounts should be user managed and could be used for other systems, such as e-referrals, e-lab reqs, eprescribing, as well as a patient portal system.
The government should also incentivize:
•The building of apps by vendors that allow viewing and workingwith data by patients, providers, facilities and organizations. With standardized data, it would be easy to switch apps without migration, leading to innovation by competition not monopolies.
There’s a saying, “If you want to go fast, go alone. If you want to go far, go together.” We welcome your thoughts and ideas. Feel free to reach us at the contact info below.
Dr. Karim Keshavjee is the Program Director for the Health Informatics Program at the University of Toronto. Contact him at: karim.keshavjee@utoronto.ca. Dr. Jonathan Marcus is Adjunct Professor, IHPME, University of Toronto. Contact him at: jonathan.marcus@utoronto.ca
Dr. Jonathan Marcus
Dr. Karim Keshavjee
Unity Health Toronto prepares for Epic electronic patient record go-live
TORONTO – On November 30, 2024, Unity Health will launch its new electronic patient record (EPR) system, transforming communication and information sharing between patients, families and their care teams. Called Project Connect, this major clinical transformation project will improve the way that clinical teams deliver care and empower patients to play a more significant role in their care journey.
The new system is powered by Epic Systems and was informed by over 500 staff, physicians, patients, and patient/family partners who sit across several work groups and advisory councils. These groups are making sure the system is designed to meet the needs of Unity Health patients and teams.
Caroline Assouad, an EPR applications specialist inpatient with a background in nursing, is working with clinicians in the obstetrics departments at St. Michael’s Hospital and St. Joseph’s Health Centre to ensure their Epic module, called Stork, meets their workflows and needs prior to go-live.
“We need to build one system, so harmonization of policies, order sets and workflows across the organization is key,” said Assouad, who meets with clinical experts to review the module and then edits it to fit their specific needs. “I really enjoy the sort of problem solving that building the system requires.”
At Providence Healthcare, where most clinical and corporate processes are paper based, this project marks a major change in practices and workflows.
It’s a lot of work, said Olga Krasik, a clinical nurse educator at Providence, but it’s also really exciting. “The new EPR system will relieve nurses of more of the administrative burdens and give them more time to do what they do best – provide excellent patient care,” said Krasik.
Across Unity Health, clinicians say they’re looking forward to seamless information sharing with patients and fellow clinicians, whether they’re sharing laboratory test results, diagnostic images or medication information. The ease of information sharing also promises to improve patient safety.
“Clear, automated tracking of medication, treatments and diagnoses allows everyone on a patient’s care team to obtain the same information,” said Krasik. “It’s a great way to help us reduce the number of potential errors.”
Alina Lalani, a clinical pharmacy specialist and leader at St. Joseph’s, said that while communication and information sharing within each site will improve, the new system will also make it easier to seamlessly transfer patients between sites.
“The current practice for transfer of information is to download and share our documentation which is labor intensive and not always consistently done,” said Lalani. “Epic will allow seamless conversations between our teams across sites which will reduce our workload overall.”
Though Project Connect is a clinical transformation project, it will also transform processes for some corporate and support services teams. For instance, the Patient Transport teams at Unity Health will be able to receive transport requests on their mobile devices, eliminating the need for colleagues
to monitor a central intake email and dispatch team members upon request.
“This improvement will lead to quicker responses to patient needs and smoother overall operations,” said Punya Ross, manager of environmental, patient food and transport services at Providence. “It’ll give
us more time to focus on what’s most important – patient care.”
The decision to work with Epic Systems was made following a robust engagement and procurement process that involved over 500 staff, physicians, learners and patient and family partners, the organization said on its website. An international leader in the EPR space, Epic Systems is the chosen vendor of many premier health systems across Ontario and Canada, including SickKids Hospital, UHN, Trillium Health Partners, Mackenzie Health and The Ottawa Hospital.

Canadian Healthcare Technology magazine

White Papers
shopping.
Canadian Healthcare Technology offers the country’s leading healthcare I.T. publications. Are you getting all the news?

eMessenger newsletter
Canadian Healthcare Technology’s e-Messenger contains breaking news about important deals, installations and developments. Four blasts are sent each month, via e-mail, to over 7,000 senior managers and executives in hospitals, clinics and health regions.
Canadian Healthcare Technology’s White Papers are sent out once a month, via e-mail, to over 5,000 senior managers and executives in Canadian hospitals and health regions. The monthly blast contains summaries and links to White Papers issued by various organizations, providing cutting-edge information about topics of interest to healthcare decision-makers.
Canadian Healthcare Technology breaks the news about important projects, programs and technologies, and provides hospital executives and senior managers with an excellent source of information for improving the delivery of healthcare. It’s sent to over 5,200 readers in print format and to 6,800 opt-in subscribers as a digital edition. For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com

Canadian technological solutions at the forefront of proactive wound care
Until recently, wound care has been left to visual inspection; high-tech systems provide major improvements.
BY DIANNE DANIEL
With an estimated annual spend of $3.9 billion – and a ‘hidden’ cost of more than $12 billion in 2023, according to a recent report from Wounds Canada – wound care management in Canada is currently undergoing significant change.
The over-arching goal is to raise the standard of care, and digital innovations from Canadian companies – including Toronto start-up Mimosa Diagnostics Inc., Toronto-based Swift Medical Inc. and Abbotsford, B.C.-based Pixalere Healthcare – are helping to pave the way, replacing error-prone visual inspections and manual measurements with more consistent and reliable approaches that heal wounds faster and engage patients in their personal wound care journeys.
“The reality is we use multiple modalities –imaging and lab work – in other medicine, but this is the last remaining area where a visual inspection has been acceptable,” said Mimosa Diagnostics founder and CEO Dr. Karen Cross. “I’m not saying those decisions are wrong. It’s just that we need more information to confidently say, ‘This is what’s happening.’”
The impact of wound care on the Canadian healthcare system is huge, with one out of every two community nursing visits involving some form of wound care delivery. From bed sores and surgical wounds to diabetic foot ulcers and burns, wounds present many complex challenges that compromise healing and lead to complications.
Diabetes Canada, for example, has said that “every four hours, someone across Canada suffers a lower limb amputation due to a nonhealing or infected diabetic foot ulcer.”
Not only is there variance with measurements and visual assessments when the current standard of care remains a paper ruler, but clinicians are typically left to rely on a ‘wait and see’ approach to understand if interventions are working and wounds are healing. The issue is compounded by limited availability of certified wound care specialists, with most physicians receiving less than 10 hours of formal wound care education.
Diagnostics CTO and co-founder, said he believed it could work.
The result is Mimosa Pro, a handheld imaging platform that uses near-infrared and mid-infrared light to detect tissue oximetry and temperature while capturing a digital image, taking technology originally developed to determine burn depth and transforming it into a pocket-size device.
Referred to as multispectral imaging, the process sends multiple wavelengths of light below the top surface of the skin to look for very specific biomarkers in tissue, enabling clinicians to ‘see’ conditions that can’t be seen by the naked eye.
“The light is tuned to give you a special fingerprint,” explained Dr. Cross, noting that the Mimosa Pro is one of the first medical devices to use light detection and ranging (LiDAR) technology. “When the light returns, because of the way it returns, we know
others to improve outcomes. AI-driven insights are also provided.
After being approved by Health Canada earlier this year, the class II medical device is currently being used in a study at Hamilton Health Sciences to see if it can better identify early signs of pressure injuries, with a focus on people with darker skin pigmentation due to the technology’s ability to measure melanin.
The technology is also being implemented in clinics and hospitals in Nova Scotia through a partnership with the Nova Scotia Health Innovation Hub, and a downtown Toronto hospital is acquiring the device this fall.
Swift Medical’s Skin and Wound app was the brainchild of a group of engineers who wondered if the technology used by the Mars rover to accurately generate 3D images of moon craters could be applied to further understand deep cratering in wounds. The technology is compatible with most Apple and Android devices, and uses a biomedical sticker called HealX which is placed next to a wound to scientifically calibrate its length, width, depth and colour when an image is captured using a smartphone or tablet.
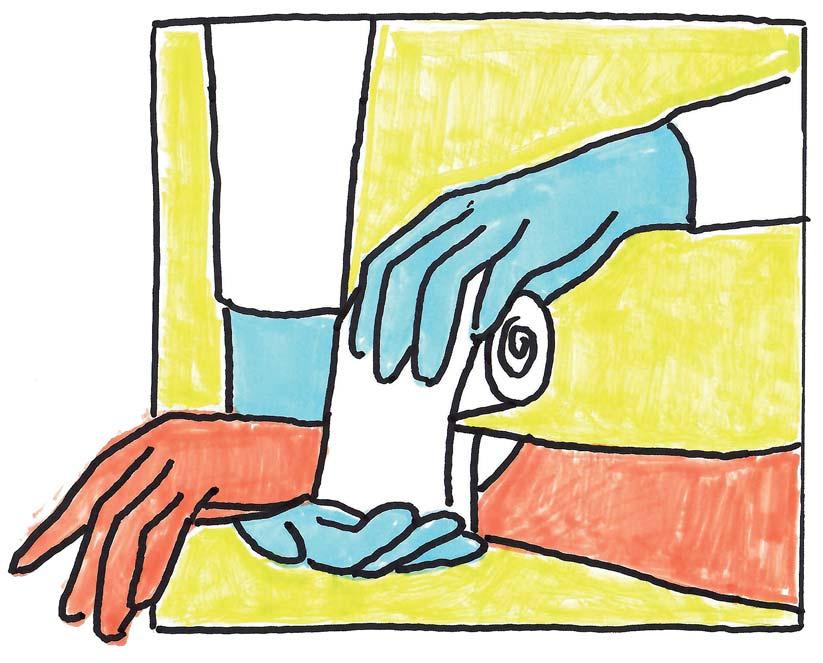
Advances in digital wound care aim to raise the bar by supporting clinicians with secure point-ofcare applications and devices that capture accurate wound measurements and other characteristics, automate the evaluation process, and extend the expertise of wound care specialists by connecting them to front line staff virtually to guide decision making.
Artificial intelligence is also being used to suggest recommended care paths based on data from millions of previously collected images, and more advanced features are in the pipeline.
As a physician treating wounds and someone who lost a family member to a mismanaged diabetic foot ulcer, Dr. Cross was determined to find a way to improve patient outcomes when she had a chance encounter with physicist General Leung in a coffee shop. She described her idea for a novel mobile device and Leung, who now serves as Mimosa
exactly what it was absorbed by which means we can precisely determine how much of this one biomarker or two biomarkers are in the tissue at a time.”
By combining a digital image with physiological data like whether or not the skin has a fever or the amounts of oxygenated and deoxygenated hemoglobin within the tissue, Mimosa Pro provides clinicians with quantitative information to help assess and treat wounds. It can also be used to monitor and keep patients in remission after a wound has healed, or to help clinicians assess the impact of an intervention at point of care.
Similar to the way standard operating procedures are applied to chest X-rays, the technology uses standard image capture to automate how images are collected, ensuring the image is taken the same way each time, regardless of who is using the device. Images are sent to a HIPAA-compliant web portal where clinicians can identify opportunities for early intervention, track patient progress and collaborate with
Once captured, images are shared with wound care certified clinicians through a secure, cloud-based platform so they can advise on treatment, type of dressing, removal of bandages and other guidelines. Dashboards provide a range of information from patient-specific evaluations to trends analysis and AI algorithms are incorporated to provide data insights gleaned from the company’s database of more than 25 million scientifically calibrated images. “Literally, in front of their eyes, they’ll see how the wound has progressed over time, they can take pictures, do measurements and other documentation,” said Swift Medical chief commercial officer Neil Sharma, sharing the testimony of a cancer patient who suffered with a post-surgical wound for five years before their caregivers started to use Swift Skin and Wound, successfully closing the sore within six months.
The technology, which is integrated into the PointClickCare electronic health record for senior care, is currently used by 21,000 clinicians at 4,800 facilities who generate 600,000 images monthly.
Swift Medical is also involved in a $9-million DIGITAL innovation project through Telewound Care Canada that aims to integrate three AI-powered technologies into the company’s wound care platform: SmartTissue which will identify wound issue types to determine if a wound is improving or deteriorating; AutoDepth, which will create a 3D model of a wound; and, Healing Index, which will track size, tissue type and clinical documentation to identify wounds at risk of not healing.
Swift Medical vice-president of clinical innova-
tion Rob Fraser calls wound care a “costly and hidden burden” within the Canadian healthcare system. As a wound care certified registered nurse, Fraser is passionate about changing the standard of care because based on his personal experience, treatment plans typically don’t change until a patient shows signs of sepsis or is clearly in need of emergency care.
“Often, the approach is ‘Let’s give it a few more weeks to see’ because they don’t have the data, they don’t have the measurements, they have poor documentation, and it’s very hard to read a narrative note and say with great confidence that a wound is getting better or worse,” explained Fraser. “If we’re not actually closing them, but just changing the dressings, wounds are going to be an ongoing and expensive issue.”
Pixalere started out in electronic wound care management two decades ago, evolving its technology as clinical needs and environments changed. From day one, clinical input was essential, helping the company to modify its app according to user needs.
Today, the cloud-based wound management system is providing 200,000 assessments per month and has expanded to South Africa and Australia. Clinicians snap pictures of wounds using a smartphone or tablet, and the AI-driven app sizes the wound for length, width and colour, comparing it to the last image. A Braden scale evaluation is also generated.
A clinical assistant module then leverages the more than 10 million images in the company’s data set to suggest recommended care paths based on changes to the wound. After implementing Pixalere, users report a 10-fold productivity gain for their nurses specialized in wound, ostomy and continence (NSWOCs), with an average wound evaluation time of 6.5 minutes.
Pixalere CEO Ken Hendsbee said it’s been interesting to see how the digital technology is engaging patients. When his company first started using wound images to advance care, he actually thought they might encounter patient resistance. As it turned out, quite the opposite happened, he said.
“It was interesting to see how patients actually got involved in their wound care to a greater degree,” said Hendsbee. “They now have the ability to view their wound equally to the nurses and specialists.”
In his role at Swift Medical, Fraser recalls visiting a Hamilton, Ontario-based diabetic wound care clinic which was open concept so patients could see each other as they sat in different bays. When a nurse using the app told a patient their wound was reduced by x percent, other patients would clap.
They were happy for each other,” he said. “Often patients rely on clinicians’ opinions. Now they have objective measurements to monitor and drive decision making … a nurse can say keep wearing the compression for your venous leg ulcer because it’s working.”
All three digital wound care platforms use connectivity to bridge the gap between centrally located wound care specialists and remote healthcare providers, but also work offline as well to ensure patients in remote areas or places with poor Internet service still benefit. They continue to advance their technologies as the Canadian
wound care market is expected to experience significant growth.
“We’re already suggesting care paths based on what users are inputting. To be able to take it to the next level, to use all of that data to do more of an individualized care path, it’s going to happen,” said Hendsbee. “It’s a little Star Trekky and leading edge, but it’s going to be very exciting within the next three to five years to
see how far we’re going to be able to go.”
Mimosa Diagnostics anticipates a future when, based on preliminary information and the technology’s ability to ‘make the invisible, visible,’ clinicians will be able to look at intact skin and apply wound care interventions before a wound surfaces.
“It’s really like catching everyone at stage four cancer, which would be absolutely unacceptable, but we just accept they have a
wound, let’s treat the wound. It’s a very reactive system,” said Dr. Cross. “We’re trying to move into being able to provide information so nurses and doctors can be proactive about wound care and can do a little bit more in prevention. Maybe there are instances where it’s not possible to prevent it, but we’ll have information where we can finally determine who’s going to heal and who’s not going to heal.”
Düsseldorf, Germany 11–14 November 2024
Montreal-based AlayaCare uses AI to help Canadians age safely at home
Canadians overwhelmingly want to remain in the comfort of their homes as they age. This preference is especially pronounced in the aftermath of the COVID-19 pandemic, with a survey indicating almost 100 per cent of Canadians over 65 want to age in place.
As labour shortages and thin profit margins strain healthcare providers in the home-care sector, technology, including generative AI, can play a critical role in ensuring aging Canadians can safely remain at home.
Alison Green founded Bien Chez Soi, a Québec home-care company, when she was just 23 years old after seeing first-hand how difficult it was for her own grandparents to navigate the public healthcare system.
“We offer home-care services that are directly related to our clients’ actual needs – we specialize in matchmaking so that the needs of a family and the needs of our employees have a long-term fit and that our caregivers, as well, are happy and well in the work environment.
In seven years, Bien Chez Soi has grown from one to 47 locations, serving 10,000 families in Quebec. Green says that a key part of the organization’s success and ability to scale is their partnership with AlayaCare, a Montréal-based global technology platform for home and community-based care.
“With AlayaCare, we’re giving our workers the tools and the technology to make sure that 99 percent of their time is spent beside the person they care for,” said Green.
AlayaCare’s mission is to empower care providers to achieve better health outcomes for their home-care clients by delivering transformative technology and data insights to focus on what really matters. This is particularly important in the face of research that shows aging people have healthier outcomes when they remain at home.
“Our population is getting older and older, and we need more help to ensure they’re safe and comfortable when they’re on their own,” said Naomi Goldapple,
AlayaCare’s senior vice president, Data and Intelligence.
All of AlayaCare’s work is ultimately aimed at enabling quality care for loved ones at home – and ensuring they can stay there.
“We know for elderly people, for example – they’re going to fall. It’s not if, but when. So how can we minimize the impact or prevent them from ending up in the hospital with a broken hip, which can too often be the beginning of the end,” said Goldapple. “Maybe it means a home-care
At Bien Chez Soi, the technology helps manage staff at their 47 locations.
“I can ensure the quality of care, do background checks, make sure there are no dropped visits, make sure that notes are being taken on a daily basis – we can track where our employees are going, when they’re at their clients’ homes,” said Green. “The AI that’s enabling this is people-first technology that allows our employees to focus on people, not process.”
Launched in 2014, AlayaCare powers

worker moves a carpet that’s a trip hazard, for example, or we can put ambient, passive technology in the home that can tell us they’re up and active and check on them if they’re not.”
The company’s platform, which includes client and family portals, lives on the Amazon Web Services (AWS) cloud. It leverages AWS’ artificial intelligence (AI) and machine learning (ML) services to create prediction models to see which clients are most at risk, and then builds that data into the workflow process.
It also helps healthcare providers automate repetitive tasks so home-care workers can spend more time caring for their clients.
seven million visits per month and is growing, with services in Canada, the United States, Australia and New Zealand via several AWS Cloud Regions.
AlayaCare is using AWS infrastructure and services to run schedule and route optimization algorithms to help schedulers quickly see the home-visit slots they need to fill. It provides them with the best employee matches based on specific criteria that satisfy caregivers and patients alike.
With AWS’s Amazon Bedrock, a fully managed service that offers a choice of high-performing foundation models through a single API, AlayaCare can prototype and experiment with different large-
language models (LLM) to connect LLMs to internal data for asking questions against your patient/employee data.
LLMs are also used to automatically extract clinical information from unstructured documents like forms and notes to give caregivers the information they need.
With seven million visits logged-on their platform every month, there’s an enormous amount of data related to those visits at AlayaCare’s fingertips, she adds.
“That anonymized and aggregated data is golden because our customers depend on us to tell them how they’re doing compared to their competitors in their states and provinces,” said Goldapple.
“We’re able to house all that data on AWS, which we use for data pipelines. We’re now in the process of moving to a more sophisticated data pipeline to offer up fast refreshes and all of the insights that our customers need, as well as being able to feed our machine learning models.”
Elizabeth Keller, Healthcare Business Development Lead at AWS Canada, says innovative, safe and secure technologies are invaluable to the healthcare industry, and a true way to advance. “The adoption of emerging technology like artificial intelligence and generative AI among Canadian organizations is less than half of the U.S., which is of concern for improved support and care for our aging population, and for our economy as a whole.”
“However, healthcare and life sciences organizations like Canadian-born healthtech AlayaCare are increasingly turning to technology as a business differentiator – especially with the explosion of generative AI. They are seeing success on a global scale, while helping address the industry’s shortage of health personnel,” Keller continued.
“Today, almost every customer and partner is exploring how to make the most of AI and generative AI. Ultimately, they see opportunities to improve acceleration and productivity, and provide a better experience for patients.”
App connects community members with Elder teachings and more
HARRISON BAY, BC – Community members and leadership in Sq’ewlets First Nation recently gathered to share a meal to celebrate the launch of the q’eyéx app. The app uses the CheckingIn platform to provide users with a confidential and safe space to connect with ancient teachings, learn from Elders and knowledge keepers and lift up the Sq’ewlets’ ways of being.
The app was developed with various funding sources, including the First Nation Health Authority’s (FNHA’s) Urban and Away From Home Funding Initiative. The initiative provides grants to support the urban and away from home population in areas of primary care, mental health and wellness, the toxic drug response and addressing racism in health and wellness.
In less than two months since its launch, 21 percent of Sq’ewlets Nation
members have signed up to use q’eyéx. Members have access to wellness services such as daily check ins, cultural programs, Elder teachings and harm reduction resources. Activities are provided in modules titled “teachings”. Since signing up users have completed 2,378 total teachings.
The development of the app and its teachings was community-led. Speakers from the FNHA Urban and Away From Home team, CheckingIn and community leadership highlighted the success of the application’s release.
“It is wonderful to see one of the initial UAH Funding Initiative grants come full circle with the launch of the q’eyéx app,” said Ruhee Mardhani, advisor, Urban and Away from Home, FNHA. “The impact the app will have by supporting future generations in staying connected to culture, no matter where they reside, is immeasurable.”
“It’s been an amazing journey develop-
ing this app with CheckingIn, said Sonya Williams, Sq’ewlets BSDW & education coordinator. “It’s such a great resource for our members both on and off reserve. I was reflecting on how it all started and can’t help feeling so proud of it all.”
In addition to its aim to heal commu-
The app provides access to wellness services, including cultural programs and harm reduction resources.
nity members, revitalize language and preserve cultural teachings, the app has created a full-time role for the community coordinator who is responsible for engaging with community and coordinating knowledge keepers, Elders, youth and the storytelling behind the teachings.
“I truly feel the impact we are making
and the importance of my role here” said Atawni Hall, community coordinator. “It has brought me so much closer to everyone in my community and I just feel proud of the work that’s been done. The work has taught me how to present myself to my community confidently and I have grown so much since starting. There is so much more to complete and I’m ready for it! Great programs ahead.”
Future plans to enhance the app and increase its use include customized swag and prizes, and the integration of additional land-based teachings in order to offer members real-time knowledge of its significance.
Learn more about the application at the q’eyéx website, or take a look at CheckingIn.co
This article was originally published on the First Nations Health Authority website, www.fnha.ca
























Clinical Education
Grow professionally with our extensive continuing education opportunities.

Register for an upcoming GE HealthCare education symposium:




BC Breast Imaging Symposium
BC Breast Imaging Symposium
As advocates for women's health, we have curated a distinguished panel of well-known experts in the field of breast care to share their insights and knowledge with you.
As advocates for women's health, we have curated a distinguished panel of well-known experts in the field of breast care to share their insights and knowledge with you.
We will have experts like Dr. Anat Kornecki, M.D, RCPSC, (London ON) and Louise C. Miller (San Diego, US) covering key aspects in breast imaging.
We will have experts like Dr. Anat Kornecki, M.D, RCPSC, (London ON) and Louise C. Miller (San Diego, US) covering key aspects in breast imaging.


Saturday October 5th |
Saturday October 5th |
8:00 am to 4:00 pm PT Symposium & Positioning workshops
8:00 am to 4:00 pm PT Symposium & Positioning workshops


The Westin Bayshore Vancouver
The Westin Bayshore Vancouver
Accredited by CAMRT


















Scan here to register now Accredited by CAMRT




Imaging Summit Saskatchewan
Imaging Summit Saskatchewan
This event is designed with an intent to provide you a holistic approach on transforming imaging with AI and digital tools to help
This event is designed with an intent to provide you a holistic approach on transforming imaging with AI and digital tools to help
We will have experts covering the latest trends on AI in medical imaging, surgical imaging, ABUS, and innovative digital solutions.
We will have experts covering the latest trends on AI in medical imaging, surgical imaging, ABUS, and innovative digital solutions.




Tuesday October 8th | 5:30 to 8:30 pm CT
Tuesday October 8th | 5:30 to 8:30 pm CT














Wednesday October 9th | 5:30 to 8:30 pm CT
Delta Hotels by Marriott Regina
Delta Hotels by Marriott Regina








Sheraton Cavalier Saskatoon










MUSE User Group Meeting
MUSE User Group Meeting
This event brings users together from across the country to collaborate, discover best practices, and gain hands-on experience in diagnostic cardiology and more. The sympoium focuses on the complete configuration of the clinical application, as well as day-to-day use of the system.
This event brings users together from across the country to collaborate, discover best practices, and gain hands-on experience in diagnostic cardiology and more. The sympoium focuses on the complete configuration of the clinical application, as well as day-to-day use of the system.
Thursday October 24th | 9:00 am to 4:00 pm PT
Thursday October 24th | 9:00 am to 4:00 pm PT
JW Marriott Parq
Vancouver
JW Marriott Parq Vancouver


















Scan here to register now
Scan here to register now


MR in the Maritimes
MR in the Maritimes






This education event is dedicated to expanding the capabilities of MR through open collaborations and insights to influence the future of imaging.
This education event is dedicated to expanding the capabilities of MR through open collaborations and insights to influence the future of imaging.
We will have experts covering varied topics such as MRI safety, perspectives from physicists and image reviews.
We will have experts covering varied topics such as MRI safety, perspectives from physicists and image reviews.


Friday October 25th | 8:00 am to 4:00 pm AT
Friday October 25th | 8:00 am to 4:00 pm AT










The Westin Nova Scotian Halifax
The Westin Nova Scotian Halifax










Building trust is a prerequisite for bringing tech to rural home-care
BY CHENNY XIA AND GINA JOHAR
When the Rural Stop Gap Project was first introduced to bring AI-enabled home health monitoring and a virtual team-based care model to Ontario’s Hastings region, the project team quickly learned that the acceptance of technology is so much more than technical literacy and its implementation.
Here’s how the project works: Gotcare brings its AI-enabled triage and health monitoring tools into residents’ homes, starting in North Hastings, Ontario. Eligible residents are then matched with a Health Ambassador, an upskilled community care provider with digital health skills, who collaborates with virtual clinicians to deliver as much care as possible in the home setting.
This project helps bridge gaps in primary care for Hastings residents who do not have a family doctor (they’re part of the 2.3 million Ontarians in this category).
It will also help divert patients occupying an alternate level of care (ALC) bed due to a lack of sufficient home and community support available, rather than keeping them in the hospital. Across Canada, approximately 15 percent of ALC beds in hospitals are filled by patients due to a lack of structural support for care within their own homes.
Technology that can help reduce the load on overburdened healthcare workers and clear up wait times? Sounds like a dream, right?
Not exactly.
We quickly learned that implementing healthcare innovation everywhere – but especially in rural communities – needs to be done with a focus toward learning how public, private and academic organizations can partner together and deliver change in these communities, rather than simply introducing a new innovation.
First off, a rural hospital network, such as Quinte Health, has to think of how its
teams and community health partners are going to participate in these new implementations. Across Canada, many healthcare workers have expressed legitimate concerns in response to AI-enabled technologies. They ask questions, such as: Is there bias in this AI? Will it hurt my patient to use this technology?
For example, one community care coordinator was skeptical of the Rural Stop Gap Project when it was first launched. She didn’t see the value right away and was quick to jump to reasons why virtual interventions wouldn’t work in rural communities.
But after a while, she came to see that the project allowed her patients to receive significantly faster access to care. One of her patients, a woman who was at risk of falls and lived alone with very little family support in a very remote part of the region, was waiting several weeks for a comprehensive home safety assessment.
A Health Ambassador visited the patient in her home, where they used satellite internet to complete a virtual care call with an occupational therapist to complete a basic safety check in the patient’s home and optimize for safe functioning, such as where furniture is arranged in her bedroom when she is getting up in the morning to reduce the risk of a fall.
We gained an advocate in this region’s rural health ecosystem from someone who others trust. That built trust from other frontline workers.
One of our learnings was that when true engagement and co-design to introduce AI tools takes place, we need to be prepared to hear what may initially feel like uncomfortable, unsupportive, or negative feedback.
Upon reflection, building trust with partners also should accept that we need to not only listen to these concerns, but accept them and solution-build together with the intent of continuously working together to find improvements.
The end-user experience (real or perceived) has to be considered to be a “truth” that needs attention and a solution.
Defensiveness, use of technical lan-
guage, or an answer for every concern can frustrate partners and we learned that meeting teams where they are at, working with them to ensure a shared understanding of the problem to solve, and taking a clinical and workflow “first” approach can help set the conditions for AI technology.
We also worked hard to personalize our patient-facing technology to their unique needs and lifestyle goals, instead of pushing a one-size-fits-all solution on to them. For example, the program provides patients with a personalized touchscreen device, where patients can use video to call a


nurse when they are experiencing an exacerbation in symptoms, receive remote queuing and prompting to promote enhanced self-management, reminders of upcoming appointments or medications, or virtually meet with their family doctor or community care coordinator.
When patients were first socialized to the concept, it evoked nervousness around their capability to adopt new technologies, so we stopped calling it a “technology,” and adapted the language of “your personal safety device.”
We showed patients how a TV remote is significantly more difficult and complicated to operate than the safety device and related it to the nurse call bell at the hospital, something they were already comfortable with operating. This helped de-escalate any fears or concerns around using the safety device.
But getting to patients’ homes first required many months of effective stakeholder engagement and change manage-
IDS Ontario’s most widely used solution for sharing data
Guelph Wellington OHT is a great example of IDS in action. Leveraging IDS to share data across providers is now enabling the OHT to segment their population by complexity of needs which, in turn, is helping inform the development of care plans tailored to patients’ specific requirements across a range of providers. This has led to better care coordination and optimal use of the OHT’s available resources. Additionally, by incorporating the Hospital-Patient One-Year Mortality Risk (HOMR) tool into IDS, the OHT can now use IDS’s integrated data to identify patients who would benefit from a palliative approach to care.
This allows the care team to proactively initiate an integrated care plan that includes all aspects of palliative
care, including advanced care planning, serious illness and symptom management conversations, etc.
Benefits are two-fold: for providers, informing them which individuals may benefit from wrap-around care, and at
One Ontario Health Team uses the application to segment their population by complexity of needs.
the system level, allowing the OHT to predict required palliative care capacity across the Guelph Wellington population and plan accordingly. The HOMR score is now available to the IDS network of subscribers via IDS’s once-for-many approach.
ment with Gina, who is the chief digital officer for Quinte Health.
She often receives generic emails and pitches from tech companies where these solutions are built with urban communities in mind. For example, many solutions assume that all patients will have access to the internet, or at least a 3G mobile connection. Unfortunately, that’s not the case in much of Hastings.
Leading change is ultimately the biggest part of a technology implementation – you can’t just add tech and stir. In today’s healthcare environment, adaptive leadership and approaches to supporting one another are essential as we all do our best to deliver the right outcomes for our patients and teams.
Technology providers must have change management capabilities embedded in their team and offer wraparound services that enable patients to adopt their innovations. In rural regions, there are other obstacles that technology providers have to address – such as internet accessibility and connectivity.
The reason that Quinte Health and Gotcare could form a partnership is because we hold mutual respect for one another, share common goals, collaborate and consult with one and have set aside the traditional mental models of how a vendor partner and public sector partner can help advance change.
This is where the importance of co-creation comes in. This truly means working with each healthcare organization in the region to find out how technology can help – not hinder, not burden and, most importantly, not create more problems.
We socialized the Rural Stop Gap Initiative with over 20 stakeholders in the region, including community leaders, various members of the Hastings Prince Edward Ontario Health Team, coordinators of other patient support programs, and Ontario Health Team members. This meant months of consultations, discussions and presentations to these stakeholders.
Through active listening, IDS will continue to expand its offering with new datasets, tools and insights of the greatest interest to its user community. For example, currently in the pilot stage are integrations with community support services and hospital ambulatory clinics – both non-traditional datasets –as well as long-term care. As more organizations join the IDS network, everricher data is being made available to improve health service delivery across the province.
By putting analytical power in the hands of its subscriber community, IDS is working to support a vision of an integrated and patient-focused system of care. Learn more about how IDS can support your organization, or reach out directly to Wendy Gerrie, director, IDS, at wgerrie@oha.com.
We then started to co-design the program. Being an innovator means being an excellent holder of space. Stakeholders cannot have an open mind if they do not feel seen and heard around their concerns. We gathered everyone in a single room together where they were free to speak their mind. It’s important to remain curious, and not get frustrated during this part of the process.
From there, we followed up with each stakeholder and hosted a co-design session with their team. We role-played different scenarios and discussed how the technology could be customized to focus on addressing their unique needs. This allowed us to figure out what worked for them, so that our program and technology could make a high degree of impact, with as little human effort as possible from their team.
Afterwards, we synthesized everything we heard from each stakeholder, and our team co-created workflows that supported referrals from the hospital discharge team, family doctors, and home and community care case managers. This also included warm hand-offs to other, more permanent programs when patients were notified that there was a spot open for them.
Chenny Xia Gina Johar
Read
Canadian Healthcare Technology, published eight times per year, is sent free of charge to managers of hospitals and clinics, and executives in nursing homes and home-care organizations. Qualified subscribers need only periodically renew their subscription information to ensure continued delivery of the magazine. Please take a minute to complete your renewal and make sure Canadian Healthcare Technology keeps coming to you – absolutely free.
ARE TWO WAYS YOU CAN SUBSCRIBE:
COMPLIMENTARY SUBSCRIPTION REQUEST
(PLEASE PRINT)
Your organization’s business or industry?
Hospital
Health region
Long-term care institution
Home care Clinic
Computer or software vendor
Telecommunications vendor
Medical
VAR or systems integrator
Education
Finance/insurance
Consulting/legal
Public relations
Other
If you are employed by a hospital, which of the following categories would best apply to you?
CEO/President/VP/Executive Director
Finance
MIS
Medical Director
Physician
Purchasing
Nursing
Pharmacy
Radiology
Pathology & Laboratory
Human resources
Health records
Public relations
Quality assurance
Other
