THE KENTUCKY PHARMACIST Vol. 11, No. 4 July/August 2016 News & Informat ion for Members of the Kentucky Pharmacists Ass ociation
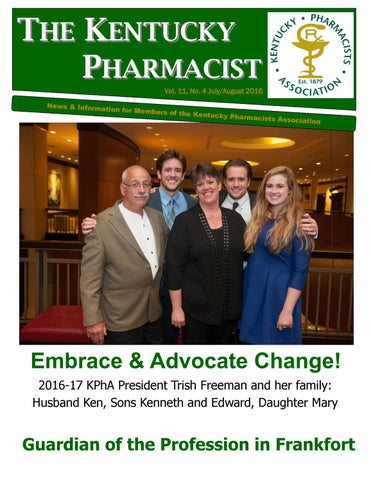
Embrace & Advocate Change! 2016-17 KPhA President Trish Freeman and her family: Husband Ken, Sons Kenneth and Edward, Daughter Mary
Guardian of the Profession in Frankfort
Table of Contents
July/August 2016 National Provider Identifiers and You August 2016 CE — TAF vs. TDF: Is There Really a Difference? August Pharmacist/Pharmacy Tech Quiz Answer Sheet KPPAC Contribution Form Report of the KPhA House of Delegates KPhA Board Strategic Planning Retreat The Campaign for Kentucky’s Pharmacy Future KPhA New and Returning Members Naloxone Atomizer Distribution Project APSC Pharmacy Law Brief Thank you Gloria Doughty Pharmacy Policy Issues Pharmacists Mutual Cardinal Health KPhA Board of Directors 50 Years Ago/Frequently Called and Contacted
Table of Contents Table of Contents— Oath— Mission Statement President’s Perspective 2016 KPhA Professional Awards From your Executive Director 2016 KPERF Golf Scramble KPhA Emergency Preparedness 138th KPhA Annual Meeting & Convention Kentucky Reportable Disease Regulation Changes 2016-17 KPhA Board Members 2016 NASPA/NMA KPhA Student Pharmacist Self Care Championship DSCSA Information July 2016 CE — The Case for Pharmacists Receiving Provider Status July Pharmacist/Pharmacy Tech Quiz Answer Sheet
2 3 4 6 8 9 10 13 14 15 16 17 26
27 28 34 35 36 37 39 40 42 43 44 45 46 48 49 50 51
Oath of a Pharmacist At this time, I vow to devote my professional life to the service of all humankind through the profession of pharmacy. I will consider the welfare of humanity and relief of human suffering my primary concerns. I will apply my knowledge, experience, and skills to the best of my ability to assure optimal drug therapy outcomes for the patients I serve. I will keep abreast of developments and maintain professional competency in my profession of pharmacy. I will embrace and advocate change in the profession of pharmacy that improves patient care. I take these vows voluntarily with the full realization of the responsibility with which I am entrusted by the public.
Kentucky Pharmacists Association The mission of the Kentucky Pharmacists Association is to promote the profession of pharmacy, enhance the practice standards of the profession, and demonstrate the value of pharmacist services within the health care system.
Editorial Office: © Copyright 2016 to the Kentucky Pharmacists Association. The Kentucky Pharmacist is the official journal of the Kentucky Pharmacists Association published bi-monthly. The Kentucky Pharmacist is distributed to KPhA members, paid through allocations of membership dues. All views expressed in articles are those of the writer, and not necessarily the official position of the Kentucky Pharmacists Association. Editor-in-Chief: Robert McFalls Managing Editor: Scott Sisco Editorial, advertising and executive offices at 96 C Michael Davenport Blvd., Frankfort, KY 40601. Phone 502.227.2303 Fax 502.227.2258. Email ssisco@kphanet.org. Website http://www.kphanet.org.
The Kentucky Pharmacy Education and Research Foundation (KPERF), established in 1980 as a non-profit subsidiary corporation of the Kentucky Pharmacists Association (KPhA), fosters educational activities and research projects in the field of pharmacy including career counseling, student assistance, post-graduate education, continuing and professional development and public health education and assistance. It is the goal of KPERF to ensure that pharmacy in Kentucky and throughout the nation may sustain the continuing need for sufficient and adequately trained pharmacists. KPERF will provide a minimum of 15 continuing pharmacy education hours. In addition, KPERF will provide at least three educational interventions through other mediums — such as webinars — to continuously improve healthcare for all. Programming will be determined by assessing the gaps between actual practice and ideal practice, with activities designed to narrow those gaps using interaction, learning assessment, and evaluation. Additionally, feedback from learners will be used to improve the overall programming designed by KPERF. 2
THE KENTUCKY PHARMACIST
President’s Perspective
July/August 2016
PRESIDENT’S PERSPECTIVE Trish Freeman KPhA President 2016-2017
our professional oath directs us to do. As Jessika Chinn, who has graciously agreed to serve as my past president representative this year, so aptly pointed out, "A football team who only plays defense is not going to win many games." How true. Thanks Jessika for that analogy. It takes a strategically prepared offense, playing in concert with a strong defense to win the final game. Let us work together this year, willingly and enthusiastically to strategically prepare our offensive “game of change” to advance the profession and improve patient care.
Second: advocate. To advocate, one must publicly support or recommend a particular cause or policy. As we proactively, and with willingness and enthusiasm, identify the changes we need to make to advance our profession and improve patient care, I challenge us, both as an organization and as individuals, to do our part to "make it happen." Adapted from The President’s Address delivered at the We must make the time to attend meetings, where our Ray Wirth Banquet during the 138th KPhA Annual Meeting plans for change are discussed and decided upon. We and Convention. must then spread the message regarding the need for Thank you for the opportunity to serve you as your presichange, our plans for change and the potential outcomes dent. The phrase that forms the basis of what will be my from the changes we are pursuing, not only to our colplatform as your president this year is taken directly from leagues within the profession, but among our elected offithe Oath of a Pharmacist. We read the oath and take its cials and the communities we serve. I truly believe it is our vows each year during this convention, and at graduation, individual and collective responsibility to do this and imand at other varied times throughout the year, but I wonplore each of us to commit to these activities during the der, sometimes, how many of us have ever really stopped next year. to contemplate the meaning of each phrase. I, personally, am optimistic about our future. As Noam Although I have always personally strived to live up to the Chomsky said, "Optimism is a strategy for making a better obligation that each vow represents, one vow, in particular, future. Because unless you believe that the future can be continues to be what drives me to do what I do each and better, you are unlikely to step up and take responsibility every day: “I will embrace and advocate changes that imfor making it so." I ask for each of you to be optimistic prove patient care.” about our future and do your part to "step up" and take responsibility for making it better, both for our patients and Let's take this phrase apart. First let's look at the word our profession. Step up and embrace our “Campaign for “embrace.” When we embrace change, we accept or supBuilding Pharmacy's Future,” which not only includes the port it willingly and enthusiastically. Change is hard, I recbuilding of our physical space, but the collective building of ognize that, but as we all know, change is inevitable. None the professional future we envision – one where pharmaof us practice today as we did 20, 10 or even five years cists are recognized and valued for the patient care serago. With this in mind, I challenge us, as an organization vices we provide. and as individuals, to be proactive in our mission to identify changes we can make that will advance our profession and Thank you for allowing me to serve as your president. I will improve patient care. Let us get out in front and play ofdo my best to lead our charge to embrace and advocate fense – promote the innovative ideas we have and not changes that advance our profession and improve patient solely rely on defensive plays to guard and protect the sta- care, and I am humbled and honored by the opportunity to tus quo – and let us do so willingly and enthusiastically as do so.
The Campaign for Kentucky’s Pharmacy Future: The Next 50 Years http://www.kphanet.org/?page=buildingcampaign 3
THE KENTUCKY PHARMACIST
2016 KPhA Professional Awards
July/August 2016
2016 KPhA Professional Awards Bowl of Hygeia Ron Poole, Central City Pictured with 2015-16 KPhA President Chris Clifton and Chair Bob Oakley
KPhA Pharmacist of the Year Joel Thornbury, Pikeville Pictured with 2015-16 KPhA President Chris Clifton
KPhA Distinguished Young Pharmacist of the Year sponsored by Pharmacists Mutual Insurance Matt Carrico, Louisville Pictured with President Clifton and Chair Oakley
Cardinal Health Generation Rx Champion Award Trish Freeman, Lexington Pictured with 2015-16 KPhA President Chris Clifton, Chair Bob Oakley and Todd Wright from Cardinal Health 4
THE KENTUCKY PHARMACIST
138th KPhA Annual Meeting & Convention
July/August 2016
KPhA Professional Promotion Award
KPhA Distinguished Service Award
Suzanne Francis, Florence
Kim Croley, Corbin
KPhA Excellence in Innovation Award sponsored by Upsher-Smith Laboratories, Inc. Christopher Harlow, Louisville Pictured with 2015-16 KPhA President Chris Clifton and Chair Bob Oakley
KPhA Meritorious Service Awards
Sen. Max Wise, Campbellsville
Rep. Jeff Greer, Brandenburg
5
THE KENTUCKY PHARMACIST
From Your Executive Director
July/August 2016 MESSAGE FROM YOUR
EXECUTIVE DIRECTOR Robert “Bob” McFalls
Kentucky is currently finalizing its proposal to implement major changes to the state’s Medicaid program. Recently, Governor Matt Bevin and the Cabinet for Health and Family Services announced plans for a new statewide transformative healthcare program entitled, Kentucky HEALTH (Helping to Engage and Achieve Long Term Health). OUR KPhA has been working to obtain information on this new plan, participated in one of the public hearings where this initiative was discussed and subsequently provided written comments. We believe this proposal represents an incredible opportunity to tap into the underutilized resource that pharmacists represent in direct alignment to Kentucky HEALTH’s design to introduce “innovative delivery system reforms targeting substance use disorder, chronic disease management and managed care to improve quality and outcomes.” Having worked with the older population for more than 25 years prior to coming to work with OUR KPhA, I certainly recognize the potential that exists to improve health outcomes.
as non-adherence. Medication non-adherence is highest among patients with chronic illnesses and results in an increased risk of side effects, adverse events, hospitalizations, disease state complications, drug-related problems or even an untimely death. This was fully illustrated by research commissioned by the National Community Pharmacists Association on medication adherence in 2013. Conducted by Langer Research Associates, the survey focused on American adults 40 and older who had been prescribed ongoing medication(s) for a chronic condition — the group that uses prescription medication most regularly and therefore is at greatest risk of non-adherence. This population represents 30 percent of all adults, with a median age of 60 and taking an average of four ongoing prescriptions. The report was less than promising. Nationally, patients with chronic medical conditions earned a troubling C+ grade in the first National Report Card on Adherence, a very weak score given the risks and costs of failing to take prescription medications as directed. And, as we know, non -adherence can threaten patients’ health individually as In submitting our recommendations, we are calling attenwell as add vast costs to the health care system. tion to the white paper issued by the National Governors Association that clearly recognizes that “The health care Similarly, the Institute of Medicine’s* 2004 report, Health system is undergoing a significant transformation in both Literacy: A Prescription to End Confusion (2004) reported the finance and delivery of health care services. States, in 90 million people have difficulty understanding, using and particular, are examining their health care systems to de- acting on health information, which leads to medication non fine policies that create efficient models of care focused on -adherence. To emphasize the gravity of this problem, improved quality and health outcomes as well as reduced studies have shown that approximately 50 percent of patients do not take their medications as prescribed and more costs. Integrating pharmacists, who represent the thirdthan one in five new prescriptions go unfilled. Direct costs largest health profession, into such systems is important for of medication non-adherence to our health care system is achieving intended goals. Pharmacists have the profesestimated at up to $290 billion annually nationally and is sional expertise to address key challenges facing the considered the largest fixable problem in health care today. health care system, including the prevalence of people As the medication experts, pharmacists have unique skills who have multiple chronic conditions and the inand training to address this problem and are among the creased use of more complex medications to manage most accessible health care providers in our local commuthose diseases” (emphasis added). nities to engage patients one-on-one in helping them unAs the profession is acutely aware, proper medication ad- derstand and manage their disease states. Quite simply, herence occurs when patients take their medications ac- this is the argument that OUR KPhA has advanced to cording to the prescribed timing, dosage, frequency and CHFS and to Medicaid — why not utilize pharmacists to directions. Any situation when patients do not take their educate and coach their patients at all levels to impact their medication according to one of these factors is referred to health and improve their outcomes? 6
THE KENTUCKY PHARMACIST
Pharmacy Time Capsules Similarly, Health Affairs reported in July on the CVS Health Research Institute’s findings from a new study that measured the impact of an insurer-supported medication reconciliation program on clinical outcomes and health care spending. The unidentified insurer and its pharmacy benefit manager, CVS, identified members at high risk for readmission. According to the study, pharmacists reconciled members’ medication, provided personalized adherence education and shared patient care plans with providers.
July/August 2016 change or intervention to their therapies.
The researchers found that risk of hospital readmission at 30 days decreased by 50 percent, reducing overall risk of hospital readmission from 22 percent to 11 percent for those in the medication reconciliation program. The health plan also saved $2 for every $1 spent on the program, for a total mean savings of $1,347 per member. The study provided evidence that “an insurer-supported program, independent of provider programs, can reduce both readResearchers analyzed hospital readmissions of more than mission rates and the costs of care.” 260 members of a national health plan who were hospital- As the state H.E.A.L.T.H. initiative leads and advances the ized during a five-month period, and they compared read- transformation of healthcare delivery throughout the Commission rates for patients enrolled in a medication reconcil- monwealth, the time for Kentucky to innovate is now by iation program upon hospital discharge to a control group. taking actions that would include pharmacists as integrated Adverse drug events contribute to up to two-thirds of 30- members of community-based health care teams. By incorday readmissions, the study noted. Most care transition porating the expertise of pharmacists to counsel and coach and medication reconciliation programs are managed by patients in the management of their chronic disease states, hospitals and other providers. One program in California, not only can patient health outcomes be improved, but the for example, found that 79 percent of patients discharged health care delivery system should simultaneously become over a six-month period required reconciliation of their more efficient and cost effective. Let’s advocate together to medication lists, and 53 percent needed some sort of make this happen here in the commonwealth.
Pharmacy Time Capsules 2016 (Third Quarter) 1991 Chicago College of Pharmacy – Midwestern University established at Downers Grove, IL 1966 FDA contracted with the National Research Council to undertake the Drug Efficacy Study Implementation (DESI) Program to determine the efficacy of products marketed prior to 1962. One of the early effects of the DESI study was the development of the Abbreviated New Drug Application (ANDA). 1941 Baxter introduces the Plasma-Vac container, providing the first means of separating plasma from whole blood and storing it for future use. 1916 The U.S. Pharmacopoeia drops whiskey and brandy from its list of drugs.
By: Dennis B. Worthen, PhD, Cincinnati, OH One of a series contributed by the American Institute of the History of Pharmacy, a unique non-profit society dedicated to assuring that the contributions of your profession endure as a part of America's history. Membership offers the satisfaction of helping continue this work on behalf of pharmacy, and brings five or more historical publications to your door each year. To learn more, check out: www.aihp.org
7
THE KENTUCKY PHARMACIST
2016 KPERF Golf Scramble
July/August 2016
2016 KPERF Golf Scramble
First Place: Brian Smith, Jeff Mills, Brian Yarberry, Matthew Casper Second Place: Leon Claywell, JT Roby, Ron Poole, Duane Parsons Last Place: Mike Burleson, Steve Hart, Chris Killmeier, Alan Daniels Longest Drive: Jeff Mills Closest to the Pin: Chris Killmeier
Special Thanks to KPERF’s Golf Scramble Hole Sponsors Ad-Venture Promotions Bingham Greenebaum Doll LLP Booneville Discount Drug The Clifton Family Corum Family Pharmacy Duncan Prescription Center Fred’s Pharmacies George Hammons, Frankie Abner & Tom Houchens
Harrod & Associates Medica Pharmacy and Wellness Center, Bardstown-Bloomfield Pharmacists Mutual Co. Insurance Poole’s Pharmacy Care Republic Bank & Trust Rite Aid
8
Rx Discount Pharmacy Sullivan University College of Pharmacy Joel Thornbury Walgreens Wayne’s Pharmacy Your Community Pharmacy Commons and St. Matthews
THE KENTUCKY PHARMACIST
KPhA Emergency Preparedness
July/August 2016
Volunteer Volunteer Volunteer It’s 2016 and pharmacist, pharmacy technician and student pharmacist recruitment is underway for the Kentucky Pharmacists Association emergency preparedness program! Pharmacy professionals play a critical part in responding to emergency events such as a natural disaster or infectious disease outbreak. You may sign up as a volunteer on the KPhA website, completing a volunteer form below or simply sending an email directly to Leah Tolliver at ltolliver@kphanet.org. Please join the emergency preparedness program and help to recruit other volunteers! We need all of you! For more information on how you can be involved in the KPhA Pharmacy Emergency Preparedness Initiative, contact Leah Tolliver, KPhA Director of Pharmacy Emergency Preparedness at 502-227-2303 or by email at ltolliver@kphanet.org.
For more resources, visit YOUR www.kphanet.org and click on Resources—Emergency Preparedness.
KPhA Pharmacy Emergency Preparedness Volunteer Form
Name: __________________
____
Status (Pharmacist, Technician, Student): ___________________
Email: ______________________________ Phone: ________________________ County: Interest in serving as a volunteer: Yes____ No ____ Interest in serving as a Volunteer District Coordinator: Yes____ No _____ You also may join the Medical Reserve Corps by following the KHELPS link on KPhA Website to register (www.kphanet.org under Resources) Please send this information to Leah Tolliver, KPhA Director of Pharmacy Emergency Preparedness via email at ltolliver@kphanet.org, fax to 502-227-2258 or mail at KPhA, 96 C Michael Davenport Blvd., Frankfort, KY 40601.
Donate online to the Kentucky Pharmacists Political Advocacy Council! Go to www.kphanet.org and click on the Advocacy tab for more information about KPPAC and the donation form.
9
THE KENTUCKY PHARMACIST
138th KPhA Annual Meeting & Convention
July/August 2016
Highlights from the 138th KPhA Annual Meeting & Convention
Join us for the 139th KPhA Annual Meeting & Convention! June 22-25, 2017 Griffin Gate Marriott Resort Lexington 10
THE KENTUCKY PHARMACIST
138th KPhA Annual Meeting & Convention
July/August 2016
11
THE KENTUCKY PHARMACIST
138th KPhA Annual Meeting & Convention
July/August 2016
KPhA Would Like to Thank Our 2016 Sponsors Event Sponsors
Annual Meeting Supporters
Aetna Better Health of KY American Pharmacy Services Corporation Cardinal Health Customers in Kentucky CareSource Foundation for a Health Kentucky Jefferson County Academy of Pharmacists KPhA District 1 Kroger Corporation—Mid-South Division Medica Pharmacy and Wellness Center, Bardstown-
Rx Systems, Inc. EPIC Pharmacy Network Kroger—Northern Kentucky Division
Sponsoring Pharmacy’s Future Alcon Cardinal Health Customers in Kentucky Matt Caricco Kim Croley Brian Fingerson GeriMed Humana
Bloomfield
Northern Kentucky Pharmacists Association Pharmacists Mutual Co. Insurance Poole’s Pharmacy Care Samford University McWhorter School of Pharmacy Sullivan University College of Pharmacy Union Springs Integrative Medicine University of Kentucky College of Pharmacy
Miami-Luken National Association of Chain Drug Stores Duane Parsons Clay Rhodes Richard & Zena Slone Tolliver Management Group WellCare of Kentucky
Government Affairs Program Support American Pharmacy Cooperative, Inc.
… and our 2016 Exhibitors Allergan Kaleo Pharma NovoNordisk American Pharmacy Kentucky Cabinet for Health & Pfizer Cooperative, Inc. Family Services (KASPER) Pharmacists Mutual Companies Kentucky Deprt. for Public Health— AmerisourceBergen Purdue Pharma Immunization American Pharmacy Services Corp. QS/1 Kentucky Pharmacy Education & Astrazeneca Rite Aid Research Foundation Avanir Pharmaceuticals Samuels Products, Inc. Kentucky Renaissance Bristol-Myers Squibb Sanofi US Pharmacy Museum Cardinal Health Silvergate Pharmaceuticals KPhA Emergency Preparedness Fred’s Pharmacy Smith Drug Company McKesson Pharmaceutical Freedom Pharmaceuticals SUCOP Student Organizations Merck GeriMed UK COP Experiential Ed/ CAPP Miami Luken HD Smith Union Springs Integrative Medicine Mylan InfiniTrak Walgreens Novarits 12
THE KENTUCKY PHARMACIST
Kentucky Reportable Diseases Regulations
July/August 2016
Kentucky Reportable Diseases regulation requires pharmacist reporting An amendment to the Kentucky reportable diseases regulation, now called "902 KAR 2:020. Reportable disease surveillance" has added new reporting requirements for pharmacists for tuberculosis (TB).
Note: There is a newer treatment regimen for latent TB infection that uses Isoniazid and Rifapentine. "Rifapentine" was not listed among the drugs in the regulation, but a pharmacist could decide to report the dispensing of Isoniazid and Rifapentine. For more information, see http://www.cdc.gov/ mmwr/preview/mmwrhtml/mm6048a3.htm? s_cid=mm6048a3_w.
Visit this site for the regulation: http://www.lrc.ky.gov/ kar/902/002/020.htm The section dealing with pharmacists is below: "Section 15. Tuberculosis. (1) A pharmacist shall give notice if two (2) or more of the following medications used for the initial treatment of active tuberculosis are dispensed to an inpatient in a health facility or to an ambulatory patient in a health facility or a pharmacy: (a) Rifampin or rifabutin; (b) Isoniazid; (c) Pyrazinamide; and (d) Ethambutol. (2) A report of tuberculosis shall be considered priority and shall be reported to the local health department serving the county in which the patient resides. (3) If the local health department cannot be reached, notification shall be given to the Kentucky Department for Public Health. (4) The report shall include: (a) Information required in Section 4(16) of this administrative regulation; and (b) Names of the medications dispensed." Visit this site for a reporting form:
UPDATE: Zika Virus subject of proposed change The Department for Public Health has filed a proposed administrative regulation to amend 902 KAR 2:020. Reportable disease surveillance. If approved, this administrative regulation will make Zika Virus Disease a permanent addition to the list of diseases that are reportable in Kentucky and will replace the emergency amendment already in effect for this purpose. The amendment classifies Zika Virus Disease notification as priority, within one (1) business day, submitted electronically, by fax or by telephone to the local health department serving the county in which the patient resides and, if submitted by phone, followed up by electronic or fax submission of a report to the local health department serving the county in which the patient resides within one (1) business day. A report submitted by fax shall be made with the EPID 200 form, which has also been revised through this proposed amendment. The proposed regulation is posted on the Kentucky Legislative website at http://www.lrc.ky.gov/ kar/902/002/020reg.htm.
Watch eNews and this publication for further updates!
https://kphanet.site-ym.com/?page=38
Are you connected to YOUR KPhA? Join us online! Facebook.com/KyPharmAssoc Facebook.com/KPhANewPractitioners @KyPharmAssoc @KPhAGrassroots
KPhA Company Page
13
THE KENTUCKY PHARMACIST
2016-17 KPhA Board Members
July/August 2016
2016-17 KPhA Board Members New board members Katherine Keeney, Louisville (SUCOP Representative); Cassy Hobbs, Louisville; Cathy Hance, Louisville; and Kevin Chen, Lexington (UKCOP Representative) accepted their duties during the House of Delegates meeting at the 138th KPhA Annual Meeting and Convention. Absent from the photo is Jeff Mills, who was reelected. 2016-17 Speaker of the House Lance Murphy also recited the oath. Amanda Jett was elected Vice Speaker for 2016-17 at the meeting.
KPhA sends email announcements weekly. If you aren’t receiving: eNews, Legislative Updates, Grassroots Alerts and other important announcements, send your email address to ssisco@kphanet.org to get on the list. 14
THE KENTUCKY PHARMACIST
Self Care Championship
2016 NASPA/ NMA KPhA Student Pharmacist Self Care Championship
July/August 2016
2016 Winners: The Legit Scripts Spencer Reed, Jordan Potter, Adam Laker, and Kevin Chen from the University of Kentucky College of Pharmacy pictured with the host, 2015-16 KPhA President Chris Clifton.
Student Pharmacists from Sullivan University College of Pharmacy and University of Kentucky College of Pharmacy formed teams to answer Jeopardy type questions about over-the-counter products and care.
Thanks to our judges, Ryan Hatfield, Lance Murphy (both past winners of the competition) and KPhA Past President Condit Steil 15
THE KENTUCKY PHARMACIST
DSCSA Compliance Tips
July/August 2016
The New Normal DSCSA Compliance Tips: Policy Matters What is my new normal? The newly enforced Food and Drug Administration’s (FDA) Drug Supply Chain and Security Act (DSCSA) requires electronic tracking and tracing of all dispensed prescription drugs and requires a process for product verification in the event of a suspect product and mandatory reporting requirements. These latest regulations bring a new way of life and create a new normal when approaching compliance as a part of your day to day business practices. The best way to document standard operating procedures related to DSCSA is to adopt and document policies. Developing your Policy and Procedure Manual for DSCSA compliance may seem like a daunting task, especially when considering all of the elements of the new law and what is required of you as a dispenser. A store policy clearly communicates to staff the standard operating procedures for any process, ensuring that all employees handle situations consistently. Adopting a policy is also an important risk management move because, if done properly, it verifies your standard business practices. Even if an employee makes mistakes, evidence of a clear policy and guidelines (which the employee may not have followed) will be helpful to lessen any potential fines or penalties. A clear policy combined with annual staff training is excellent protocol to show compliance with regulatory process requirements.
Keeping a policy up to date and easily accessible to staff will bring you real protection and peace of mind! InfiniTrak, has been following the development of these DSCSA regulations since they began in 2013. When designing a software solution, they looked at the situation from the point of view of the dispenser - and independent pharmacies like yours - and created a tool to meet your needs. For example, InfiniTrak provides its customers with a template for a track and trace policy document to be created to meet each location’s requirements. InfiniTrak is a cost-effective, easy to use software that will save you time and money, increase productivity, ensure full compliance and provide the peace of mind that comes from knowing that all of your data is at your fingertips, when you need it. Contact us today to learn more about how you can electronically create and transmit FDA and other government reports as required, all in a cloud solution. OUR KPhA has partnered with InfiniTrak to bring this resource to you. Questions regarding your store policy and your compliance plan? Contact info@infinitrak.us.
KPhA Remembers KPhA desires to honor members who are no longer with us. Please keep KPhA informed by sending this information to eramey@kphanet.org . Deceased members for each year will be honored permanently at the KPhA office. 16
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
The Case for Pharmacists Receiving Provider Status: Meeting Patients’ Needs By: Sydney M. Haubner, Pharm.D. (May 2016 graduate), Joseph L. Fink III, B.S.Pharm., J.D., University of Kentucky College of Pharmacy The authors declare no financial relationships that could be perceived as real or apparent conflicts of interest.
KPERF offers all CE articles to members online at www.kphanet.org
Universal Activity # 0143-0000-16-007-H04-P&T 1.5 Contact Hours (0.15 CEUs) The work reported here was completed in partial fulfillment of the requirements for the course GRN 786 – Independent Readings in Gerontology. Dr. Haubner completed this project and course as a portion of the requirements for the Graduate Certificate in Gerontology she earned while also pursuing the Pharm.D. degree at UK. Dr. Fink was her mentor for that course offered through the Graduate Center for Gerontology at the UK College of Public Health. Objectives: At the conclusion of this Knowledge-based article, the reader should be able to: 1. Identify professions the members of which are currently classified as “providers” for purposes of Medicare; 2. Identify the proportion of the U.S. population age 65 or older; 3. Identify whether the classification of the pharmacist as a “provider” under Medicare would be done by statute or by regulation; and 4. Identify what the phrase “practice at the top of one’s license” means. care system and upcoming changes as related to the older The United States health care system is in dire need of adult patient. It also analyzes how this patient population reform. With millions of Americans uninsured, astronomical could benefit should pharmacists be recognized as health costs and a continuously increasing national debt, some care providers. may call the state of our health care system a crisis spiral- Current Status of Our Health Care System ing out of control.1 Our country is taking strides toward Before we can better improve health care for the older adult modernization and health care reform, as reflected by the population, we must first understand the current state of Affordable Care Act. However, upcoming changes to our our health care system and how current standards impact health care system can bring about both positive and negathis population. The U.S. spent a staggering $3 trillion on tive results. health care in 2014.3 State of the art facilities and equipAlthough the quality of our health care system affects every ment in addition to the army of staff members required to member of society, the older adult population represents run a health care facility come with a hefty price tag. The the largest percentage of patients.2 Care for the average U.S. Centers for Disease Control and Prevention states older adult is complex and costly to both the patient and that 86 percent of our nation’s health care cost is due to society. This population may be uniquely impacted by the treating people with chronic diseases.4 Medicare footed repercussions of upcoming changes in our health care sys- over 20 percent of the bill, spending over $600 billion. 3 All tem. Focusing on the care of older adults is one step that told, Americans paid in excess of $330 billion in out-ofcan make a great difference in health care system costs. pocket expenses for health care. Analysts determined prePharmacists have both the knowledge and the growing scription drug spending accounted for nearly $3 billion. 3 workforce to fulfill a large number of new and necessary As the biggest spender on health care in the world, all roles for these patients. However, pharmacists are not curthese expenditures in our system have not resulted in the rently recognized by Medicare or most other payers as a outcomes one might or should expect, indicating possible primary care provider to bill for professional services. wasteful expenses.5 Non-adherence has been estimated to Should pharmacists achieve provider status under Medicost almost $300 billion.6 A 2012 study assessing the ecocare, private insurers often will follow suit. nomics of health care and medical errors estimates medical This discussion focuses on the current state of our health errors to cost $1 trillion.7 Despite the technology in place Introduction
17
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status today and the amount we spend on health care, preventable medical errors are actually the nation’s third leading cause of death, just behind heart disease and cancer. 8 This number is alarming and demands a solution. There are more than 42 million adults 65-years-old and older in the United States, representing almost 14 percent of the population. However, this relatively small percent of the population consumes more than 40 percent of prescription drugs and 35 percent of all over-the-counter medications.9,10 On average, an older adult patient takes 14 to 18 prescription medications.9 Ninety-two percent of seniors are living with at least one chronic condition, and 77 percent have at least two chronic conditions.9 Due to increased incidence of chronic diseases and resultant use of prescription medications in this population, older adults are at a higher risk of medical errors. Focusing more time and attention toward the care of this smaller percentage’s care could make a significant impact on health care cost and ultimately better improve the health care system for everyone. Not only is health care costly, the percentage of care related to appropriate and proper use of medications can make significant impact on health care cost and ultimately improve the health care system for everyone. Our health care system is currently experiencing a shortage of primary care providers. The Association of American Medical Colleges (AAMC) stated in March 2015 that the US could be short between 46,000 and 90,000 physicians overall by 2025.11 AAMC President and CEO Darrel G. Kirch, M.D., stated, “The doctor shortage is real – it’s significant – and it’s particularly serious for the kind of medical care that our aging adult population is going to need.”12 Many physicians also choose to specialize after medical school. With an increasing number of medications and ever expanding knowledge regarding disease states, there certainly is a need for specialists. However, there also appears to be a misdistribution of the current physician workforce with the percentage of physicians practicing in a primary care specialty currently at an all-time low.11 Nonetheless, the health care system cannot afford for medical schools to sacrifice quality for quantity by opening their doors to anyone who desires to be a physician. Being a physician requires a certain skill set and mental aptitude not possessed by everyone. This shortage of primary care providers affects the care our older adult population receives. Not only will an older adult patient spend more time in the waiting room, but he or she also will experience an increased waiting time between initial and follow-up appointments. A shortage of primary providers also results in rushed office visits. Studies have found that 82 percent of family physicians spend less than 20 minutes during an encounter with their patients. 13 To-
July/August 2016
day’s physician appointments are commonly scheduled at 15-minute intervals, a situation exacerbated by frequent interruptions.14,15 Care of the older population requires more time with the patient or caregiver to obtain health information and to educate or counsel about their treatment regimens. Rushed appointment times can result in a lack of continuity in a patient’s care as many seniors are under the care of multiple specialists. Older adult patients have often described their care as, “my left hand doesn’t know what the right is doing.”16 Aside from the shortage of primary care providers, practitioners often operate with “one eye on the patient, and one eye on the clock.”17 Primary care providers have to be focused on the amount of time spent with a patient due to our health care system’s broken payment model. Health care in the US largely operates under a “fee-for-service” model, meaning health care providers collect when care is provided. This payment system relies on the sick to keep the system functioning and profitable. However, this system also is backwards. The goal of health care is to keep patients well, and the payment system should reflect treatment goals. Primary care providers do not perform procedures such as biopsies or colonoscopies to generate revenue compared to their specialist counterparts, but are instead paid per visit with little extra compensation for longer visits.16 Primary care providers practicing in the office face greater financial pressure from insurers who often reimburse at lower rates and offer to increase compensation by instead proposing to send more patients.16 This is not the kind of care the older adult population needs nor is this payment model capable of producing effective results. Impending Changes in Health Care Continuously increasing health care costs have brought the need for health care modernization to the forefront. One of the biggest changes in our health care system is increased access to care provided by the Affordable Care Act (ACA), sometimes referred to as “Obamacare.” “ACA” actually refers to two pieces of federal legislation, the Patient Protection and Affordable Care Act as well as the Health Care and Education Reconciliation Act of 2010.18 The ACA ultimately seeks to expand coverage, lower health care costs, hold insurance companies accountable and enhance the quality of care for all Americans.18,19 Though the bill was met with some resistance, most disagreement with the bill was related to new taxes and individual/employer mandates versus the expansion of health care coverage. An increase in the patient population is currently taking place in the system, but this expansion is only expected to continue and grow. By mid-2015, 28.5 million Americans were still without health care. This is actually a 16.3 million de-
18
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status 20
crease from 2013. Unfortunately, flooding the health care system with additional patients will exacerbate some of the problems already present in our broken system. Our system needs providers and a payment system to care for this increased capacity. Despite the fact that providing care earlier in life can help create a healthier older adult population, our current system is not equipped to treat an increased patient population. An increased patient population will exacerbate the shortage of primary care providers. For the older adult population this could result in increased waiting times both in the office and between office visits, waiting times even longer than the current less-than-positive experience. Integrating primary care nurse practitioners and physician assistants can alleviate some of the shortage, but that likely will not totally fix the problem as the demand for these other positions remain high.21 The U.S. health care system also can expect an increase in our older adult population. Those in the “baby-boom” generation, referring to the population spike observed after World War II from 1946 to 1964, are currently between the ages of 52 and 70 years old. Many citizens referenced by this cultural term will be entering the 65 years old and older age bracket over the next decade, creating an older adult population larger than ever before in this country. The older adult population is expected to represent almost 20 percent of the population by 2050, compared to the current 14 percent.22 Meanwhile, the ratio of people ages 16–64 to those age 65 and over is projected to decline 43 percent from 2000 to 2050.22 A decline in the working population will jeopardize the services and the taxes needed to finance services older adult patients need. Improved health care and prevention have contributed to a longer life span for Americans. The average life expectancy is now 78.8 years old, compared to that of 70.8 years in 1970.23 However, this also has led to an increase in the prevalence of chronic diseases and a need for primary care providers to manage those maladies. The effect of longer life spans on the demand for health care exceeds the impact due to an increased patient population. For example, improved diabetes care has resulted in diabetics living longer lives and dying of heart failure or renal failure before succumbing to their diabetes. As treatment options continue to improve, the health care system can expect to see more diseases associated with age, such as heart failure, cancer and chronic kidney disease. At the same time our population also is becoming unhealthier, living a sedate lifestyle and consuming high sugar/high fat diets. Obesity is on the rise, with the proportion of the adult population meeting the criteria to be considered
July/August 2016
obese increasing from 14.4 percent to 29.6 percent between 1995 to 2015.24 Obesity can lead to Type 2 diabetes, high blood pressure, heart disease, stroke, cancer, breathing disorders and other serious health problems. 25 Health care costs attributed to obesity could reach almost $900 billion by 2030 should current obesity trends continue. 24 Combined with a longer life expectancy and improved medical care, more patients will potentially be taking medications indicated for chronic use for longer periods. These growing obesity and diabetes rates result in an even larger primary care provider deficit. As research continues, we can expect to see more therapeutic options available for patients. Prior to the 1990s, insulin and sulfonylureas were the only treatment options for diabetes.26 Dozens of medications have since been introduced to the US market, and there are now 11 different therapeutic classes of medications to manage hyperglycemia in diabetic patients, each with its own unique sideeffect profile.27 As therapeutic options continue to increase, determining the best option for the patient can become difficult. Increased number of therapeutic options and higher costs associated with these newer entities increases the need to monitor older adult therapy regimens for interactions, adverse effects and adherence. This is difficult for the already short supply of primary care providers to do within their 15-minute appointment window. The cost of new medications entering the market is continuously increasing. More than 50 percent of medications under development are considered specialty medications. 28,30 Specialty medications are novel therapies that require special handling and a higher education and/or monitoring. However, the most distinguishing aspect of specialty medications is the high-cost.28 The Medicare Modernization Act defined specialty medications as “pharmaceuticals costing $600 or more per month.”28,29 In 2013, the average annual price of therapy for specialty prescription drugs was 189 times higher than the average annual price of therapy for generic prescription drugs, $53,384 versus $283 respectively.31 Only 1 percent of the prescriptions dispensed are considered specialty medications, but this group of medications accounts for 32 percent of total drug spending. 27,30,31 Specialty drug spending is expected to increase by more than 16 percent annually between 2015 and 2018, comprising more than 50 percent, $235 billion, of total drug spending by 2018.31 While it is problematic to have a patient nonadherent to a $4/month medication, this becomes even more significant when the medication is $10,000/month and the effectiveness of the medication can be reduced due to non-adherence, as is the case with certain HIV and hepatitis-C medications. It is important to ensure that patients have tried and failed other treatment options while being
19
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
adherent before jumping to some of these very expensive ing professional course work in addition to the undergraduspecialty medications. ate course of studies, focusing on a rigorous curriculum including physiology, disease states, medications, how to Last, pharmacogenomics can be expected to affect health monitor therapy and interact with patients. The shortage of care services and therapeutic options for patients in the physicians could be decreased if pharmacists engaged in upcoming decade. Research has led to an increased unpatient care to their full capacity. This would save time for derstanding about our DNA and that is opening the door for physicians, improve access to care and enhance clinical a field referred to as pharmacogenomics. One reason we and economic outcomes.34 A phrase used to describe or currently have so many options within a therapeutic categodesignate pharmacists using all of their knowledge, skills ry is because we know that some individuals respond betand abilities for benefit of patients is “practicing at the top of ter to one medication than another. Researchers are disthe license.” covering that the patient’s DNA may play a pivotal role in effectiveness of certain medications. Certain genetic muta- Complex drug regimens are a costly burden to both society tions make patients more likely to experience successful and patients. These regimens also result in an increased therapeutic outcomes and other mutations have been potential for problems to arise in a patient’s care.10 Extra linked with increased incidence of adverse side effects. In attention from a pharmacist can contribute toward a dethe future, we can expect to see an increase in this field of crease in overall health care costs through medication optigenetic testing to help identify the patients who will re- mization. Research data have shown that having pharmaspond/not respond to a particular therapy and who are at cists on the health care team contributes to improvement in risk of experiencing potential adverse side effects. intermediate and final health outcomes and costeffectiveness.34 One and a half million adverse events in How a Pharmacist Can Make Positive Contributions the U.S. have been reported as being preventable and There are countless changes coming to our health care medication-related each year. A 2006 survey conducted by system, and there are a variety of ways one could address the Centers for Disease Control and Prevention’s National these upcoming changes. However, there is one profes- Center for Health Statistics found that only 47 percent of sional who can positively impact all the aspects previously medications used at home were documented in the medical discussed, and that is the pharmacist. record.34 Of the medications recorded in a patient’s chart, Pharmacists can help address the shortage of primary care 89 percent of prescription medications and 72 percent of and herbal treatments had discrepanproviders. Unlike some of these growing projections related over-the-counter 34 to patients and their use of medications, pharmacists ap- cies. Pharmacists are specially trained in obtaining medipear to be outgrowing the demand for their services. The cation history and know the correct follow-up and clarificanumber of pharmacists has more than doubled since 2001, tion questions to ask. Involving the pharmacist as part of and the trend is expected to continue.33 Pharmacists, once the health care team in both the hospital and the clinic or considered to be in short supply, now find that the supply of office setting can help to prevent these errors. professionals has quickly out stripped the demand.33 Pharmacist manpower is available to take on extra roles and continue to do so as our nation sees increased access to care. The role and livelihood of other members of health care team would not be adversely affected, as they would continue to visit with and provide patient diagnoses. Pharmacists could supplement the services of other professionals by providing follow-up appointments, either in person or by telephone.
A 2013 study found that pharmacist-provided care resulted in significant improvements in hospitalization rates, medication adherence, combined therapeutic outcomes and combined safety endpoints.34 Blue Cross/Blue Shield also found that through medication therapy management, they received a return on investment 12 to 1 when a pharmacist was involved in the care of their beneficiaries. Another study enrolling Medicare patients with multiple diseases and using many medications found that the pharmacist identified an average of 10 drug-related problems per patient, saving each patient an average of approximately $1,500 on health care costs, with a return on investment of 2.5 to 1.34 It is estimated the U.S. spends more than $290 billion each year in avoidable costs to treat adverse events from inappropriate medication use.36 Pharmacist provided services could help prevent these costs.
Training a physician requires at least 10 years when preprofessional and professional degree programs are combined with now-mandatory residency programs. Medical schools would need to train at least 3,000 more graduates a year to meet the health care needs of our nation’s growing and aging population.11 However, pharmacists also receive a doctoral level education. To obtain a Doctor of Pharmacy, a pharmacist typically spends four years pursu- Pharmacists also can help to increase medication adher20
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status ence through profile monitoring and education. With nonadherence costing almost $300 billion, including medication waste and excess care/hospitalization expenses, patient profile monitoring by pharmacists can reduce costs and help to improve outcomes.35 Only 20 percent of patients with hypertension have acceptable medication adherence, defined as taking 80 percent of their prescribed antihypertensive medications in a year.36 Medication not taken cannot treat patients. Uncontrolled disease states, such as hypertension, diabetes, elevated cholesterol and heart failure can have severe consequences that lead to high costs. Non-adherence is the result of many factors, including expense, side effects and a misunderstanding of how the medication works. For example, some medications used to treat depression can require four to six weeks to take an effect. These medications cannot be taken on an asneeded basis. Pharmacists also can prevent use of unnecessary medications. Not all patients report OTCs and dietary supplements to other providers who may not think to inquire. Seeking an over-the-counter medication for a chronic cough without realizing that the cough is an adverse effect of the ACE-inhibitor they use, can occur even in patients who have been taking the medication for years. Pharmacists have the unique skill set to address these issues should they be provided the time and compensation to meet with patients.
July/August 2016
potentially perform medication therapy management and chart reviews more frequently, make reminder phone calls regarding prescriptions not picked up and even offer compliance enhancing packaging for patients should they be able to bill for these services. They also are capable of assessing a patient’s adherence and response to a newly prescribed blood pressure medication. Pharmacists also could be involved in a patient’s clinic meetings and followup. Pharmacists also can appropriately monitor patients’ lab values related to use of their medications. Patients can check in regularly with their pharmacist in a clinic setting while opening time for the physician to see these patients annually as well as to see other patients. The same also is true for patients with diabetes and dyslipidemia. Once diagnosed and assessed by the physician, pharmacists could use their in-depth understanding of how to monitor and adjust the patient’s therapy to enhance beneficial outcomes. A study assessing the role of pharmacists in improving patient care in elderly heart failure patients found that pharmacists’ involvement through medication reconciliation and discharge counseling can decrease readmission rates. 38
Pharmacists also can monitor patients for potential pharmacogenomic interventions. As researchers learn more about the genome, testing will likely become more common practice. Through conversations with patients regarding the effectiveness of their medications, pharmacists can know Many members of society are unaware about what the full when to appropriately test patients for genetic mutations capacity of pharmacist provided patient care entails. Phar- that may affect the effectiveness of their medications. macists are trained to do more than dispense prescriptions. Pharmacy technicians should be knowledgeable about this Pharmacists receive doctoral level education, and are proposal to extend provider status to include pharmacists trained to obtain detailed medical histories especially with because they make major contributions to the overall imregard to use of medications, perform medication therapy pression the profession makes on patients and caregivers. management, counsel patients about proper use of their Because this proposal could have far reaching implications medications, monitor drug use and perform disease manfor a wide variety of practice sites it could well have very agement services and other preventive services, while positive benefits for pharmacy technicians as well as for serving as a liaison between the patient and other health pharmacists. Just as was seen when the advent of authoricare practitioners, especially, but not only, with regard to ty to immunize in the pharmacy brought a need for pharmaoptimal use of medications. Considering 89 percent of precy technicians to be aware and knowledgeable to handle scription medications are not being documented in the papatient inquiries, the same could be true for this developtient’s chart correctly, proper counseling including treatment. Just as is seen when one makes a visit to a primary ment expectations and potential side effects to watch for care physician, who certainly does not practice without suplikely do not occur within the 15 minute window allotted for portive colleagues at the practice site, there is no reason to a physician’s patient encounter.34 expect that pharmacists expanding their roles would not Pharmacists are the most accessible health care profes- also work with a collection of valued supporters at the pracsionals with thousands of people visiting a pharmacy per tice site. week. They also are skilled and knowledgeable health care Relevant Legislation professionals under-utilized in health care at a time when skillful and knowledgeable practitioners are in short supply. As outlined above, there are numerous ways the pharmaPharmacists can and are more than willing to step up to cist can make a difference in the care of older adults and in fulfill unmet needs and help manage chronic disease states many ways pharmacists already are doing these things. through the proper use of medications. Pharmacists could However, a major limitation on pharmacists dedicating the 21
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
time and work-effort toward these efforts is that pharmacists cannot bill Medicare for their services. Unlike physicians, physician assistants, nurse practitioners, psychologists, clinical social workers, certified nurse midwives and certified registered nurse anesthetists, pharmacists and their patient care services are not included in key sections of the Social Security Act. That is the federal statute that determines eligibility for being a participating provider in federal health care programs such as Medicare Part B, meaning pharmacists cannot bill Medicare for services provided to Medicare beneficiaries.38 Private insurers and other health plans frequently model Medicare with its coverages and cite this omission as a reason for lack of coverage for services of pharmacists provided to their enrollees and beneficiaries. There is a tremendous opportunity for pharmacists to render very substantial benefit to the older adult populations if recognized as health care providers under the Medicare program.35 Excluding the older adult population from beneficial pharmacy services prevents improvements to our health care system. The education and knowledge of the contemporary pharmacy practitioner often are not acknowledged; practitioners with equal or less educational background can bill Medicare for services provided to beneficiaries.
with patients. There are limited data to demonstrate the value of pharmacist-provided services to the older patient population due to a lack of documented services and claims.10 A study conducted by Perez and colleagues during 2009 established that for every dollar invested in clinical pharmacy service, $4.81 of savings resulted due to reduced costs and other return on investment.39,40
A proper payment model is necessary to ensure that these services can remain available to older adult patients through Medicare.34 One of the biggest obstacles these legislative proposals face is that few studies investigate or establish the perceived and true value of these services
medical histories and drug regimen in current use.
What can a pharmacist or pharmacy technician do to advance the cause of provider status? The most direct answer is that all can be alert for opportunities to influence legislation through communicating with federal legislators. It is especially powerful to share descriptions of incidents where substantial patient savings was the result of action and decision making by someone at the pharmacy.
A more indirect yet frequent answer lies with taking advantage of each and every opportunity to display to patients and care givers as well as to other health professionals their knowledge and skill in dealing with patients and the health issues they confront. By using all their abilities and striving to “practice at the top of the license” in order to best serve patients, pharmacists and pharmacy technicians can shape how the profession collectively, and themselves individually, are viewed. For pharmacy technicians serving on the front line of patient interaction, their demeanor, disThere are currently Federal legislative proposals, H.R. 592 cretion and sound judgment with patients will facilitate optiand S. 314, that would extend federal recognition of pharmal services and go far to enhance the overall impression macists as health care providers in the sections of Medicreated by the profession of pharmacy. care Part B through the amendment of Title XVII of the Social Security Act.35,38 H.R. 592 and S. 314 are known as the Conclusion Pharmacy and Medically Underserved Areas Enhancement Our health care system needs to improve outcomes and Act. These bills enable seniors in medically underserved cost effectiveness. Our country is spending billions of dolareas to access pharmacist patient care services which are lars more than any other country on health care goods and authorized by scope of practice definitions in state pharma- services without commensurate results. Obstacles such as cy practice acts by providing coverage under Medicare Part our payment system, provider shortage, increasing older B.34,35 In 2014, California enacted a landmark provider sta- adult and other patient populations need to be addressed. tus law, SB 493, granting pharmacists the ability to initiate Health care also is transitioning to an approach emphasizspecific treatments, administer certain medications and ing team-based care with a focus on cost-effectiveness and order laboratory tests. Nonetheless, SB 493, the California outcomes. However pharmacists have been excluded from legislation, did not address one of the key barriers – com- making maximum contributions to addressing these issues pensation.37 H.R. 592 and S. 314, the federal legislative due to their lack of provider status. Pharmacists are unique proposals, specify reimbursement parameters “equal to 80 in their specialty training related to medications and enjoy percent of the lesser of the actual charge or 85 percent of commonly being referred to as the “medication expert.” Not the fee schedule… if such services had been furnished by having a medication expert on the team does the patient a a physician.”37 disservice, especially older adult patients with complex past Editor’s Note: As of press run, all six of Kentucky’s Congressmen, including the original sponsor, Rep. Brett Guthrie, have signed on as Co-Sponsors of H.R. 592 but neither Senator has signed on to S. 314.
22
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
Highlands Today. Oct. 4, 2014. Accessed May 2, 2016. http://www.highlandstoday.com/the-role-of-pharmacists -and-the-elderly-20141004/
References
1. Health Care Facts: Why We Need Health Care Reform. Obamacare Facts. http://obamacarefacts.com/ healthcare-facts/ 11. Porter S. Significant Primary Care, Overall Physician Shortage Predicted by 2025. American Academy of 2. The Concentration of Health Care Spending: NIHCM Family Physicians. March 3, 2015. Accessed May 1, Data Brief. National Institute for Health Care Manage2016. http://www.aafp.org/news/practice-professionalment. July 2012. Accessed May 2, 2016 issues/20150303aamcwkforce.html http://www.nihcm.org/pdf/DataBrief3%20Final.pdf 12. New Physician Workforce Projections Show the Doctor 3. National Health Expenditures 2014 Highlights. Centers Shortage Remains Significant: Solution Requires for Medicare & Medicaid Services. 2015. Accessed Delivery Innovation, Team-based Care, Federal May 1, 2016. https://www.cms.gov/research-statisticsSupport. Association of American Medical Colleges. data-and-systems/statistics-trends-and-reports/ March 3, 2015. Accessed May 1, 2016. nationalhealthexpenddata/downloads/highlights.pdf https://www.aamc.org/newsroom/ 4. Chronic Disease Prevention and Health Promotion. newsreleases/426166/20150303.html Centers for Disease Control and Prevention. Updated 13. The Amount of Time Physicians Spent with Each March 15, 2016. Accessed May 1, 2016. Patient as of 2015. Statista. 2015. Accessed May 1, http://www.cdc.gov/chronicdisease/ 2016. http://www.statista.com/statistics/250219/us5. Squires D, Anderson C. U.S. Health Care from a Globphysicians-opinion-about-their-compensation/ al Perspective: Spending, Use of Services, Prices and 14. Costa C. Why Doctors Do Not Spend Enough Tine with Health in 13 Countries. The Commonwealth Fund. Oct. Patients Anymore. CheatSheet. June 15, 2015. 8, 2015. Accessed May 1, 2016. Accessed May 1, 2016. http://www.cheatsheet.com/ http://www.commonwealthfund.org/publications/issuepersonal-finance/why-doctors-do-not-spend-enoughbriefs/2015/oct/us-health-care-from-a-globaltime-with-patients-anymore.html/?a=viewall perspective 15. Sangeloty Higgins P, Shugrue N, Ruiz K, Robinson J. 6. Philipson TJ. Non-Adherence in Health Care: Are PaMedicare and Medicaid Users Speak Out about Their tients or Policy Makers Ill-informed? Forbes. May 8, Health Care: The Real, the Ideal, and How to Get 2015. Accessed May 1, 2016. http://www.forbes.com/ There. Population Health Management. 2015;18(2):123 sites/tomasphilipson/2015/05/08/non-adherence-in-30. health-care-are-patients-or-policy-makers-ill-informed/ #5dccfcf77a32 16. Rabin RC. You’re on the Clock: Doctors Rush Patients Out the Door. USA Today. April 20, 2015. Accessed 7. Andel C, Davidow S, Hollander M, Moreno D. The EcoMay 1, 2016. http://www.usatoday.com/story/news/ nomics of Health Care Quality and Medical Errors. nation/2014/04/20/doctor-visits-time-crunch-healthJournal of Health Care Finance. 2012 (Fall); 39(1):39care/7822161/ 50. Accessed May 1, 2016. http://www.wolterskluwerlb.com/health/resource-center/ 17. Sangeloty Higgins P, Shugrue N, Ruiz K, Robison, J. articles/2012/10/economics-health-care-quality-andMedicare and Medicaid Users Speak Out about Their medical-errors Health Care: the Real, the Ideal, and How to Get There. Population Health Management. 2015;18(2):123 8. McCann E. Deaths by Medical Mistakes Hit Record: -130. The Way IT is Designed Remains Part of the Problem. Healthcare IT News. July 18, 2014. Accessed May 1, 18. Affordable Care Act. Medicaid.gov. Accessed May 1, 2016. http://www.healthcareitnews.com/news/deaths2016. https://www.medicaid.gov/affordablecareact/ by-medical-mistakes-hit-records affordable-care-act.html 9. American Society of Consultant Pharmacists. ASCP Fact Sheet. Accessed May 1, 2016. https://www.ascp.com/articles/about-ascp/ascp-factsheet 10. Gardner I. The Role of Pharmacists and the Elderly.
19. The Pros and Cons of Obamacare. Obamacare Facts. Accessed May 1, 2016. http://obamacarefacts.com/ obamacare-pros-and-cons/ 20. Blumenthal D, Squires D. 2015: The Health Care Year in Review. The Commonwealth Fund Blog. Dec. 22, 23
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status 2015. Accessed May 1, 2016. http://www.commonwealthfund.org/publications/ blog/2015/dec/2015-health-care-in-review 21. Projecting the Supply and Demand for Primary Care Practitioners through 2020. Health Resources and Services Administration. November 2013. Accessed May 1, 2016. http://bhpr.hrsa.gov/healthworkforce/ supplydemand/usworkforce/primarycare/
July/August 2016
30. Medical Cost Trend: Behind the Numbers 2016 Report. PwC. 2016. http://www.pwc.com/us/en/healthindustries/behind-the-numbers/behind-the-numbers2016.html 31. Trends in Retail Prices of Specialty Prescription Drugs Widely Used by Older Americans, 2006 to 2013. AARP. November 2015. http://www.aarp.org/content/ dam/aarp/ppi/2015/rx-price-watch-specialtyprescription-drug-prices-continue-to-climb-final.pdf
22. Wiener TM, Tilly J. Population Ageing in the United States of America: Implications for Public Programmes. 32. U.S. Rx Spending Increased 13.1 Percent in 2014. International Epidemiological Association. 2002. Express Scripts. March 10, 2015. Accessed on May 2, Accessed May 1, 2016. http://ije.oxfordjournals.org/ 2016. http://lab.express-scripts.com/insights/industrycontent/31/4/776.full updates/us-rx-spending-increased-13-percent-in-2014
23. Life Expectancy at Birth, total (years). The World Bank. 33. Brown DL. A Looming Joblessness Crisis for New http://data.worldbank.org/indicator/SP.DYN.LE00.IN Pharmacy Graduates and the Implications It Holds for the Academy. Am J Pharm Educ 2013;77(5). 24. Obesity, United States. America’s Health Ranking. 2016. http://www.americashealthrankings.org/all/ 34. White CM. Pharmacists Need Recognition as Providers obesity to Enhance Patient Care. Annals of Pharmacotherapy. 2014;48(2):268-273. 25. Mayo Clinic Staff. Obesity. Mayo Clinic. June 10, 2015. Accessed May 2, 2016. http://www.mayoclinic.org/ 35. The Pursuit of Provider Status: What Pharmacists diseases-conditions/obesity/basics/ complications/conNeed to Know. American Pharmacists Association. 20014834 September 2013. 26. White Jr JR. A Brief History of the Development of Diabetes Medications. Diabetes Spectrum. 2014 (May);27(2) 82-86. http://spectrum.diabetesjournals.org/ content/27/2/82.full 27. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2014 Update: A Report from the American Heart Association. Circulation. 2014;129:e28–e292. https://www.heart.org/idc/ groups/heart-public/@wcm/@sop/@smd/documents/ downloadable/ucm_462025.pdf 28. “The Growing Cost of Specialty Pharmacy - Is it Sustainable?” American Journal of Managed Care. February 2013. Accessed May 2, 2016. http://www.ajmc.com/payer-perspectives/0213/thegrowing-cost-of-specialty-pharmacyis-it-sustainable 29. Specialty Drugs and Health Care Cost Fact Sheet. The Pew Charitable Trusts. November 2015. http://www.pewtrusts.org/en/research-and-analysis/fact -sheets/2015/11/specialty-drugs-and-health-care-costs
36. Ho MP, Bryson CL, Rumsfeld JS. Medication Adherence: Its Importance in Cardiovascular Outcomes. Circulation. June 2009. 124:3028-3035. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3068890/ 37. Kitts N, Reeve AR, Tsu L. Care Transitions in Elderly Heart Failure Patients: Current Practices and the Pharmacist’s Role. The Consultant Pharmacist. 2014 (Mar);29:179-190. 38. Harper, PC. Pharmacist Provider Status Legislation: Projections and Prospects. J Am Pharm Assoc. 2015;55:203-207. 39. Helling, DK & Johnson, SG. Defining and Advancing Ambulatory Care Pharmacy Practice: It Is Time to Lengthen Our Stride. Am J Health-System Pharm. 2014(Aug 15);71:1348-56. 40. Perez A, Doloresco F, Hoffman JM, et al. Economic evaluations of clinical pharmacy services: 2001–2005. Pharmacotherapy 2009; 29:128.
The Campaign for Kentucky’s Pharmacy Future: The Next 50 Years http://www.kphanet.org/?page=buildingcampaign 24
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
July 2016 — The Case for Pharmacists Receiving Provider Status: Meeting Patients’ Needs 1. Our country spends much more per capita on health care than other industrialized nations, and the U.S. also enjoys the best return on that investment as evidenced by improved health status reflective of that expenditure. A. True B. False 2. Which of these professions is not currently recognized in federal law as a being a “provider” within the Medicare program? A. Clinical social workers B. Certified registered nurse anesthetists C. Psychologists D. None of the above; all are currently recognized. 3. There have been no legislative proposals in Congress designed to designate pharmacists as providers under the Medicare Part B program. A. True B. False
7. Older adults have a disproportionate incidence of: A. Acute conditions. B. Chronic conditions. C. Allergic conditions. D. None of the above. 8. Older Americans are using, on average, how many prescription medications in what range? A. 5-8 medications B. 9-13 medications C. 14-18 medications D. 19-24 medications 9. A major challenge related to elders and their use of medications is what we know as “adherence”, i.e., taking the medication when it should be taken each and every time. A. True B. False
10. The phrase “practicing at the top of the license” refers to pharmacists: 4. Approximately what percent of Americans are age 65 A. Performing activities described at the outset, or top, of or older? the Pharmacy Act. A. 5 percent B. Using all of their knowledge, skills and abilities for B. 10 percent benefit of patients. C. 15 percent C. Performing pharmacy tasks very well, such as being D. 20 percent fast and accurate. D. Doing those professional activities that even pharmacy 5. Designation of professions recognized as providers interns may not perform. within the Medicare program is done by statute so that requires Congressional action, not a regulation adopted by a federal agency. A. True B. False 6. Being designated a “provider” under the Social Security Act means that members of that profession can do what? A. Initiate therapy with federal legend medications B. Authorize refills of federal legend medications C. Receive compensation for service under Medicare D. None of the above
Send potential continuing education topics to Scott Sisco at ssisco@kphanet.org 25
THE KENTUCKY PHARMACIST
July 2016 CE — Case for Pharmacists Receiving Provider Status
July/August 2016
This activity is a FREE service to members of the Kentucky Pharmacists Association. The fee for non-members is $30. Mail completed forms to: KPERF, 96 C Michael Davenport Blvd., Frankfort, KY 40601. Credit will be applied to your CPE Monitor Profile. Expiration Date: July 6, 2019 Successful Completion: Score of 80% will result in 1.5 contact hours or .15 CEUs. Participants who score less than 80% will be notified and permitted one re-examination. TECHNICIANS ANSWER SHEET. July 2016 — The Case for Pharmacists Receiving Provider Status: Meeting Patients’ Needs (1.5 contact hours) Universal Activity # 0143-0000-16-007-H04-T Name _______________________________________________KY Cert. # __________________________________ Address ______________________________________________Email_____________________________________ PLEASE CIRCLE THE APPROPRIATE ANSWERS: 1. A B 3. A B 5. A B 2. A B C D 4. A B C D 6. A B C D
7. A B C D 8. A B C D
9. A B 10. A B C D
Met my educational needs ___Yes ___No Achieve the stated objectives ___Yes ___No Posttest was appropriate ___Yes ___No Was well written ___Yes ___No Commercial bias was present ___Yes ___No Is relevant to my practice ___Yes ___No If yes, please explain on a separate sheet. Unmet Objectives:______________________________________________________________________________ I hereby certify that I completed this self-study program independently and without assistance from any other party. Signature ____________________________________________Completion Date___________________________
Personal NABP eProfile ID #_____________________________ Birthdate ____________(MM/DD) PHARMACISTS ANSWER SHEET July 2016 — The Case for Pharmacists Receiving Provider Status: Meeting Patients’ Needs (1.5 contact hours) Universal Activity # 0143-0000-16-007-H04-P Name ________________________________________________ KY Lic. # __________________________________ Address ______________________________________________Email_____________________________________ PLEASE CIRCLE THE APPROPRIATE ANSWERS: 1. A B 3. A B 5. A B 2. A B C D 4. A B C D 6. A B C D
7. A B C D 8. A B C D
9. A B 10. A B C D
Information presented in the activity: Met my educational needs ___Yes ___No Achieve the stated objectives ___Yes ___No Posttest was appropriate ___Yes ___No Was well written ___Yes ___No Commercial bias was present ___Yes ___No Is relevant to my practice ___Yes ___No If yes, please explain on a separate sheet. Unmet Objectives:______________________________________________________________________________ I hereby certify that I completed this self-study program independently and without assistance from any other party. Signature ____________________________________________Completion Date___________________________
Personal NABP eProfile ID #_____________________________ Birthdate ___________________(MM/DD) The Kentucky Pharmacy Education & Research Foundation is accredited by The Accreditation Council for Pharmacy Education as a provider of continuing Pharmacy education.
26
Quizzes submitted without NABP eProfile ID # and Birthdate cannot be accepted.
THE KENTUCKY PHARMACIST
National Provider Identifiers
July/August 2016
National Provider Identifiers and You By: Fred S. Morlan, BS, PharmD Candidate The Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandated the use of a standardized identifier to be used by health care providers, including pharmacists. To fulfill this requirement of HIPAA, the Centers for Medicare & Medicaid Services (CMS) created regulations that established the National Provider Identifier (NPI). All pharmacists are eligible for an NPI, though it is only required of pharmacists who bill on their own behalf. Currently, pharmacists are not recognized by Medicare as health care providers and thus cannot bill under Medicare Part B for coverage of services that we provide. Nationally, groups such as the American Pharmacists Association, the National Community Pharmacists Association, the National Alliance of State Pharmacy Associations and the American Society of Health System Pharmacists, have been pushing for provider status for some time now, and there is reason for optimism that their efforts may finally be leading to success. There are currently two bills in Congress – one in the House and one in the Senate – that would give pharmacists status as health care providers under the law. H.R. 592 and S.314 have garnered wide support, with over twothirds of the House and nearly one-half of the Senate cosponsoring the legislation in their respective chambers. If the bill passes, pharmacists practicing in federally designated underserved areas (which currently includes 87 of Kentucky’s 120 counties) could potentially bill for services under Medicare Part B.
How to get an NPI Pharmacists may apply for an NPI electronically at https://nppes.cms.hhs.gov/NPPES/Welcome.do. There is no cost for applying for one. This process requires the user to create a username and password, log in and then complete the application. It takes approximately 20 minutes to complete this process. It also is possible to apply for an NPI with a paper application; there is one available at https://www.cms.gov/ Medicare/CMS-Forms/CMS-Forms/downloads/ CMS10114.pdf. Regardless of the method of applying for an NPI, assistance with the application process can be received by calling the NPI Enumerator team at 1-800-465-3203 or by emailing customerservice@npienumerator.com.
As we move forward with provider status initiatives in Kentucky, pharmacists are encouraged to apply for an NPI so they are ready to implement advanced services when payment opportunities arise. According to a recent search on the NPI registry, only about 40 percent of pharmacists who practice in Kentucky currently have an NPI. Fortunately, registering for an NPI is a relatively easy and painless process. References
Recent state efforts to achieve recognition of pharmacists 1. Issue Brief: HIPAA: National Provider Identifier (NPI). as health care providers have met with success in Califor(n.d.). Retrieved July 18, 2016, from https:// nia, Oregon and Washington. In Kentucky, pharmacists www.pharmacist.com/sites/default/files/files/ recently gained statutory recognition as health care providmtm_NPI_issue_brief.pdf ers for the purpose of initiating the dispensing of naloxone, and efforts are underway to achieve provider status in Ken- 2. Pharmacists Provide Care. (n.d.). Retrieved July 18, 2016, from http://www.pharmacistsprovidecare.com/ tucky as a result of recent professional initiatives of the Kentucky Pharmacists Association and the Advancing 3. Search NPI Records. (n.d.). Retrieved July 18, 2016, Pharmacy Practice in Kentucky Coalition. from https://npiregistry.cms.hhs.gov/
27
THE KENTUCKY PHARMACIST
August 2016 CE — TAF vs. TDF
July/August 2016
TAF vs. TDF: Is There Really a Difference? By: Kelly Peddy, PharmD, MPA; Katie Petrone, PharmD; Cathy Spencer, PharmD, BCPS, AAHIVP; Sullivan University College of Pharmacy There are no financial relationships that could be perceived as real or apparent conflicts of interest. Universal Activity # 0143-0000-16-008-H02-P&T 1.5 Contact Hours (0.15 CEUs) Goal: To discuss differences in new antiretroviral therapies, with a specific focus on tenofovir alafenamide versus tenofovir disoproxil fumarate.
KPERF offers all CE articles to members online at www.kphanet.org
Objectives At the conclusion of this Knowledge-based article, the reader should be able to: 1. Identify differences between tenofovir alafenamide fumarate (TAF) and tenofovir disoproxil fumarate (TDF); 2. Discuss newly approved, TAF-containing medications for the treatment of HIV; and 3. Demonstrate understanding of appropriate use of these medications in a patient case. Introduction As antiretroviral therapies have progressed, infection with human immunodeficiency virus (HIV) has transformed from an acute, often fatal disease to a chronic disease state. Life expectancy of HIV-infected individuals who are receiving chronic antiretroviral treatment has improved drastically over the years. Life expectancy for HIV-positive men at age 20 increased from 37 to 51 years between 1996 and 2011 and for HIV-positive women at age 20 increased from 38 to 49 years between 1996 and 2011.1 As HIV-infected individuals are on antiretroviral therapy longer, newer antiretroviral therapies seek to reduce risk for long-term adverse events and resistance. Tenofovir Disoproxil Fumarate (TDF) Since its approval in 2001, tenofovir disoproxil fumarate (TDF) has been one of the “backbone” nucleoside reverse transcriptase inhibitors (NRTIs) required for antiretroviral treatment (ART) regimens, or more recently termed combined antiretroviral therapy (cART) regimens. Its active metabolite, tenofovir, was initially shown to have anti-HIV activity in 1993. However, tenofovir had poor membrane permeability and oral bioavailability, which led to investigation of prodrug agents. TDF showed improved oral bioavailability and more efficient loading of peripheral blood mononuclear cells (PBMCs) compared to parenteral tenofovir. This led to selection of TDF as the prodrug of choice for investigational research and eventually drug approval.2 HIV, TDF and Osteopenia/Osteoporosis Generally, TDF is well tolerated, but studies have revealed long-term adverse effects on bone mineral density (BMD) and renal function. TDF- and protease inhibitor (PI)containing antiretroviral regimens especially have been associated with reduced bone mineral density. The ASSERT
trial compared changes in bone mineral density between treatment naïve HIV infected individuals on efavirenz and either abacavir/lamivudine or TDF/emtricitabine.3 In this trial, investigators found that both treatment groups experienced reductions in BMD from baseline as measured by hip and spine dual x-ray absorptiometry (DXA) scans.3 However, patients receiving TDF/emtricitabine as compared to abacavir/lamivudine had significantly greater decreases in mean BMD at the total hip (-3.6 percent vs. -1.9 percent, p< 0.001) and spine (-2.4 percent vs. -1.6 percent, p= 0.036).3 Another trial, a substudy of ACTG A5202, found that TDFemtricitabine and atazanavir/ritonavir resulted in significantly greater BMD loss than TDF-emtricitabine and efavirenz.4 Both ritonavir-boosted PIs and TDF independently increase risk for BMD loss. Together, these agents seem to result in even further BMD loss.4 Prevalence of osteoporosis and low bone mineral density (BMD) is more than three times greater in HIV-positive than HIV-negative persons.5 This increased risk for osteoporosis is believed to be multifactorial, including HIV infection, traditional osteoporotic risk factors and antiretroviral therapies.6 HIV proteins can increase osteoclast activity and promote apoptosis of osteoblasts, promoting reduced BMD.6 Additionally, use of any antiretroviral regimen has been associated with reductions in BMD.7 A substudy of the SMART trial examining continuous versus intermittent ART and BMD effects found a statistically significant difference in BMD between treatment groups.7 Subjects receiving continuous ART had average hip and spine BMD decline of 0.8 percent (p< 0.001) and 0.4 percent (p=0.04), respectively, per year.7 Those receiving intermittent ART had stable or increased BMD during the first year of ART.7 During subsequent years, rates of BMD decreases between groups were similar, and no difference in incidence of osteoporosis was
28
THE KENTUCKY PHARMACIST
August 2016 CE — TAF vs. TDF
July/August 2016
7
detected (p=0.80). In summary, HIV-infected persons who are receiving ART are at higher risk for osteoporosis at baseline than HIV-negative persons. This osteoporotic risk is only magnified with use of TDF-containing ART regimens. Thus, the impetus for an antiretroviral agent with an improved side effect profile.
accumulation of tenofovir in lymphoid tissues when administered as TAF. TDF is converted to tenofovir in the plasma, which leads to increased concentrations of tenofovir in the plasma compared to TAF. It is theorized that these differences in overall tissue exposure to tenofovir could reduce the risk for adverse effects such as reduced bone mineral density and impaired renal function. Since TAF is better HIV, TDF and Renal Toxicity able to penetrate lymphoid tissues than TDF, studies have There have been many case reports of TDF-related neshown to greater accumulation of tenofovir in peripheral phrotoxicity, such as Fanconi’s syndrome and acute kidney blood mononuclear cells (PBMCs). Due to better penetrainjury. A meta-analysis of studies examining TDF-related tion into the lymphoid tissues, TAF does not require as high nephrotoxicity showed a significantly reduced creatinine of a dose as TDF in order to effectively exert its antiretroviclearance (CrCl) in patients treated with TDF as compared ral effects.2 to non-TDF antiretroviral regimens.8 The mean difference in The New Agents CrCl, calculated using the Cockcroft-Gault equation, was 8 3.92 mL/min with a 95 percent CI of 2.3-5.7 mL/min. While Genvoya® consists of cobicistat 150mg, elvitegravir this was statistically significant, it may not represent a clini- 150mg, emtricitabine 200mg and TAF 10mg. It is comparacally significant change. This meta-analysis also showed a ble to the active ingredients of Stribild®, replacing TDF with higher risk for acute renal injury associated with TDF use. TAF. It was approved Nov. 5, 2015. It is indicated as a It’s important to note that TDF-related nephrotoxicity has complete regimen for the treatment of HIV-1 infection in identified risk factors, including older age, underlying renal adults who are: 12 disease and other comorbidities and regimens containing 1. Treatment-naïve (never received treatment for HIV), or ritonavir-boosted protease inhibitors.8 Specifically, the use 2. To replace a current regimen in patients who meet the of boosted protease inhibitors in combination with TDF has following: been associated with increased risk for chronic kidney dis- virologically suppressed (HIV viral load <50 copies/mL) ease, especially if the patient has underlying risk factors for stable on a regimen for at least 6 months chronic kidney disease.9 Boosted protease inhibitors can have no known treatment failures increase overall TDF exposure and slow clearance of TDF.9 have no known resistance to any component of Genvoya® Up to 30 percent of HIV-infected patients have abnormal kidney function, and kidney disease has been associated The FDA approval of Genvoya® is largely contributed to by with progression of HIV to AIDS.10 Thus, it’s important for two Phase 3 clinical trials. Both were randomized, active patients with chronic kidney disease to receive appropriate controlled, non-inferiority trials comparing TAF and TDF. antiretroviral therapy. Per the IDSA HIV Medicine AssociaOne focused on treatment-naïve patients and the other on tion Treatment Guidelines for HIV-infected persons with treatment-experienced, virologically suppressed patients. 12 CKD, it’s recommended to avoid tenofovir in patients with a One trial included treatment-naïve patients on fixed-dose CrCl less than 60 mL/min/1.73m 2.11 Additionally, patients combinations of either elvitegravir/cobicistat/emtricitabine/ receiving tenofovir who experience a GFR decline greater than 25 percent are recommended to substitute alternative TAF (n=866) or elvitegravir/cobicistat/emtricitabine/TDF (n=867). Non-inferiority was set at a margin of 10 percent. antiretroviral agents for tenofovir.11 Ultimately, it is likely best to avoid use of TDF in patients with risk factors for ne- The regimen including TAF was found to be similar in efficacy to the TDF regimen at 96 weeks (TAF 86.6 percent vs phrotoxicity or renal impairment. TDF 85.2 percent; difference 1.5 percent; 95 percent CI, Tenofovir Alafenamide (TAF) 1.8-4.8). Mean increase in serum creatinine levels was significantly less in the TAF group (0.08 vs 0.12 mg/dL; Alternative tenofovir prodrugs have been studied as the long-term adverse effects of tenofovir disoproxil fumarate p<0.0001). Additionally, there was significantly less pro(TDF) have come to light. Tenofovir alafenamide monteinuria in the TAF group (median change -3 percent vs -20 ofumarate (TAF) is an alternative prodrug of tenofovir, percent; p<0.0001). The mean change in BMD was found which has a slightly different pharmacokinetic profile than to be significantly less in the TAF group at the spine (-1.30 TDF. TAF is converted to the active metabolite tenofovir percent vs -2.86 percent; p<0.0001) and at the hip (mean change -0.66 percent vs -2.95 percent; p<0.0001). More intracellularly by the enzyme cathepsin A. Cathepsin A is results are expected as the trial completed July 2016.13 highly expressed in lymphoid tissue, allowing for greater 29
THE KENTUCKY PHARMACIST
August 2016 CE — TAF vs. TDF
July/August 2016
Table 1. Recommended Initial Antiretroviral Regimens for Treatment-Naïve Patients
INSTI-based Regimens
PI-based Regimens
Darunavir/ritonavir + tenofovir disoproxil fumarate/emtricitabine
Dolutegravir/abacavir/lamivudine (ONLY for HLA-B*5701 negative) Dolutegravir + tenofovir disoproxil fumarate/emtricitabine Elvitegravir/cobicistat/tenofovir alafenamide/emtricitabine (ONLY if CrCl ≥ 30 mL/min) Elvitegravir/cobicistat/tenofovir disoproxil fumarate/emtricitabine (ONLY if CrCl > 70 mL/min) Raltegravir + tenofovir disoproxil fumarate/emtricitabine
INSTI = integrase inhibitor; PI = protease inhibitor; HLA-B = human leukocyte antigen-B; CrCL = creatinine clearance The other trial was open label and included patients already stable on an HIV regimen and virologically suppressed (viral load <50 copies/mL). Those patients were either switched to elvitegravir/cobicistat/emtricitabine/TAF (n=799) or remained on one of four different TDF-containing regimens (n=397). Non-inferiority was set at a margin of 12 percent. At 48 weeks virological suppression was found to be similar between groups (TAF 97 percent vs TDF 93 percent; 4.1 percent; 95 percent CI, 1.6-6.7). This trial also found renal function and hip/bone mineral density to be improved in the TAF group. Additional results are expected as the trial completes January 2017.14 Odefsey® consists of emtricitabine 200mg, rilpivirine 25mg and TAF 25mg. It is comparable to the active ingredients of Complera®, replacing TDF with TAF. It was approved March 1, 2016. It is indicated as a complete regimen for the treatment of HIV-1 infection in adults who are: 15
Truvada® for PrEP in HIV-negative patients. 17 One trial exists comparing the efficacy and safety of TAF compared to TDF with emtricitabine as a backbone in combination with a third active antiretroviral drug. Patients who were virologically suppressed (<50 copies/mL) were selected. Those patients were either switched to TAF (n=333) or remained on TDF (n=330) while continuing use of emtricitabine and a third agent as a complete regimen. Noninferiority was set at a margin of 10 percent. At 48 weeks virological suppression was similar between groups. (TAF 94 percent vs TDF 93 percent; difference 1.3 percent, 95 percent CI, -2.5-5.1). Adverse events were noted to be similar between groups at 48 weeks. More results are expected December 2016.18 Treatment Considerations: What is the Place in Therapy for TAF?
The Department for Health and Human Services (DHHS) HIV Treatment Guidelines on initial therapies for treatmentnaïve HIV-infected persons were updated in November 2015 to include the new combination medication, Genvoya® (see table 1).19 It is likely that other new combination medications containing TAF instead of TDF will be addressed in upcoming guidelines. With this update, Genvoya® represents the first single tablet regimen in the list of first line agents that can be used in patients with a creatinine clearance between 30-50mL/min. Whereas for patients with iniOdefsey® has no head-to-head trials comparing it to the tial creatinine clearance between 30-50mL/min other first alternative TDF combination. FDA-approval is largely based line regimens must be broken down and used as individual from a bioeviqualence study showing similar drug levels of agents increasing pill burden for patients. emtricitabine and TAF in Odefsey® compared to Genvoya®, as well as similar drug levels of rilpivirine between As these treatments are considered life-long therapies, 48 Odefsey® and the marketed brand of rilpivirine as a single to 96 weeks is a relatively short duration. Therefore, these agent. 16 results do not fully assess the long-term effects of TAF on renal function and bone mineral loss. Descovy® consists of emtricitabine 200mg and TAF 25mg. It is comparable to the active ingredients of Truvada®, reAdditional studies identified in ClinicalTrials.gov are looking placing TDF with TAF. It was approved April 4, 2016. It is into specific populations including patients on chronic hemoonly indicated in combination with other agents for use in dialysis, with hepatitis B virus (HBV) co-infection, with hepatreatment of HIV-1 infection in adults and adolescents. titis C virus (HCV) co-infection and in patients³ 60 years old. Descovy® is not approved for use in pre-exposure prophy- It is important to note that at the doses provided with TAF in laxis (PrEP); therefore, clinicians should continue using these combinations for the treatment of HIV-1 infection, it 1. Treatment-naïve AND HIV viral load ≤ 100,000 copies/ mL or 2. To replace a current regimen in patients who meet the following: virologically suppressed (<50 copies/mL) for at least 6 months have no known treatment failures have no known resistance to any component of Odefsey®
30
THE KENTUCKY PHARMACIST
August 2016 CE — TAF vs. TDF
July/August 2016
Table 2. General Considerations of TAF Combination Products
CrCL not recommended Complete Three-Drug Regimen Administration
Common Side Effects
Considerations
Elvitegravir/cobicistat/ emtricitabine/TAF (Genvoya®)
Rilpivirine/emtricitabine/TAF (Odefsey®)
TAF/emtricitabine (Descovy®)
<30 mL/min
<30 mL/min
<30 mL/min
Yes
Yes
No
Take with food
Take with food
Food optional
Emtricitabine/TAF may cause diarrhea, nausea, fatigue, headache Do not use in severe hepatic impairment Cobicistat increases drug interactions
Emtricitabine/TAF may cause diarrhea, nausea, fatigue, headache RPV may cause depressive disorder, insomnia Contraindicated with proton pump inhibitors due to decreased effectiveness of rilpivirine
Emtricitabine/TAF may cause diarrhea, nausea, fatigue, headache
Not indicated for use in PrEP
CrCl = creatinine clearance; TAF = tenofovir alafenamide; PrEP = pre-exposure prophylaxis has activity against HBV. However, these combinations are considerations when using TAF products. not labeled for the treatment of HBV. Additionally, the FDA References has required a black box warning to be included on each of 1. Cairns, G. Life expectancy in HIV-positive people in the the TAF products (similar to TDF products) to identify that US still lags 13 years behind HIV-negative people. discontinuation of these may result in a serious flare-up of 12, 15, 17 NAM AIDSmap website. http://www.aidsmap.com/Lifean active HBV infection. expectancy-in-HIV-positive-people-in-the-US-still-lagsSeveral additional active trials are in place to compare safe13-years-behind-HIV-negative-people/page/3040314/. ty/efficacy of TAF in other regimens/combination forms. Published Feb. 28, 2016. Accessed May 13, 2016. Currently, TAF regimens are being compared to other exist2. Ray AS, Fordyce MW, and Hitchcock MJ. Tenofovir ing first line and alternative regimens for treatment-naïve 20 alafenamide: a novel prodrug of tenofovir for the treatpatients including: ment of human immunodeficiency virus. Antiviral Res. Abacavir/dolutegravir/lamivudine (equivalent to 2016 Jan;125:63-70. Triumeq®) 3. Stellbrink HJ, Orkin C, Arribas JR, et al. Comparison of Darunavir/cobicistat + emtricitabine/tenofovir disproxil changes in bone density and turnover with abacavirfumarate (equivalent to Prezcobix® + Truvada®) lamivudine versus tenofovir-emtricitabine in HIV Efavirenz/emtricitabine/tenofovir disproxil fumarate infected adults: 48-week results from the ASSERT (equivalent to Atripla®) study. Clin Infect Dis. 2010 Oct 15;51(8):963-972. Conclusion 4. McComsey GA, Kitch D, Daar ES, et al. Bone mineral Based on the unique pharmacokinetics, TAF has the added density and fractures in antiretroviral-naïve persons benefit of reducing tenofovir exposure within the body, porandomized to receive abacavir-lamivudine or tenofovir tentially limiting adverse effects in comparison to TDF. As disoproxil fumarate-emtricitabine along with efavirenz current antiretroviral treatments are lifelong therapies, TAF or atazanavir-ritonavir: AIDS clinical trials group is expected to have reduced negative outcomes on renal A5224s, a substudy of ACTG A5202. J Infect Dis. function and BMD loss while preserving efficacy in terms of 2011;203:1791-1801. suppressing viral load. In trials thus far, it appears that TAF does have fewer negative impacts on BMD and renal func- 5. Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a metation. As always, before initiating ART, practitioners must analytic review. AIDS. 2006;20:2165-2174. evaluate other comorbidities, genotype resistance and patient preferences. Table 2 highlights some of these main 6. McComsey GA, Tebas P, Shane E, et al. Bone disease 31
THE KENTUCKY PHARMACIST
August 2016 CE â&#x20AC;&#x201D; TAF vs. TDF
July/August 2016
in HIV infection: a practical review and recommendations for HIV care providers. Clin Infect Dis. 2010; 51 (8): 937-946. 7. Grund B, Peng G, Gibert CL, et al. Continuous antiretroviral therapy decreases bone mineral density. AIDS. 2009 July 31;23(12):1519-1529. 8. Cooper RD, Wiebe N, Smith N, et al. Systematic review and meta-analysis: renal safety of tenofovir disoproxil fumarate in HIV-infected patients. Clin Infect Dis. 2010;51(5):496-505. 9. Morlat P, Vivot A, Vandehende MA, et al. Role of traditional risk factors and antiretroviral drugs in the incidence of chronic kidney disease, ANRS CO3 Aquitaine cohort, France, 2004-2012. PLoS One. 2013 Jun 12;8(6):e66223. 10. Gupta SK, Eustace JA, Winston JA, et al. Guidelines for the management of chronic kidney disease in HIVinfected patients: recommendations of the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2005;40(11):1559-1585. 11. Lucas GM, Ross MJ, Stock PG, et al. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014Nov 1;59 (9):e96-138.
alafenamide in antiretroviral regimens for virologically suppressed adults with HIV-1 infection: a randomised, active-controlled, multicentre, open-label, phase 3, non -inferiority study. Lancet Infect Dis. 2016 Jan;16(1):4352. 15. Odefsey (emtricitabine/rilpivirine/tenofovir alafenamide fumarate) [prescribing information]. Foster City, CA: Gilead Sciences Inc; March 2016. 16. Food and Drug Administration approves Gileadâ&#x20AC;&#x2122;s second TAF-based single tablet regimen Odefsey (emtricitabine, rilpivirine, tenofovir alafenamide) for the treatment of HIV-1 infection [press release]. Foster City, CA: Gilead Sciences Inc., March 1, 2016. http://www.gilead.com/news/press-releases/2016/3/usfood-and-drug-administration-approves-gileads-second -tafbased-single-tablet-regimen-odefsey-emtricitabinerilpivirine-tenofovir-alafenamide-for-the-treatment-ofhiv1-infection. Accessed May 27, 2016. 17. Descovy (emtricitabine and tenofovir alafenamide) [prescribing information]. Foster City, CA: Gilead Sciences; April 2016. 18. Gallant JE, Daar ES, Raffi F, et al. Efficacy and safety of tenofovir alafenamide versus tenofovir disoproxil fumarate given as fixed-dose combinations containing emtricitabine as backbones for treatment of HIV-1 infection in virologically suppressed adults: a randomised, double-blind, active-controlled phase 3 trial. Lancet HIV. 2016 Apr;3(4):e158-e165.
12. Genvoya (elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide) [prescribing information]. Foster City, CA: 19. Panel on Antiretroviral Guidelines for Adults and AdoGilead Sciences; March 2016. lescents. Guidelines for the use of antiretroviral agents 13. Sax PE, Wohl D, Yin MT, et al. Tenofovir alafenamide in HIV-1-infected adults and adolescents. Department versus tenofovir disoproxil fumarate, coformulated with of Health and Human Services. Available at elvitegravir, cobicistat, and emtricitabine, for initial http://aidsinfo.nih.gov/contentfiles/lvguidelines/ treatment of HIV-1 infection: two randomised, doubleAdultandAdolescentGL.pdf. Accessed May 27, 2016. blind, phase 3, non-inferiority trials. Lancet. 2015 Jun 20. ClinicalTrials.gov [Internet]. Bethesda (MD): National 27;385(9987):2606-2615. Library of Medicine (US) [cited 2016 May 27]. 14. Mills A, Arribas JR, Andrade-Villanueva J, et al. Switchhttps://clinicaltrials.gov/ct2/results? ing from tenofovir disoproxil fumarate to tenofovir term=tenofovir+alafenamide&Search=Search
Send potential continuing education topics to Scott Sisco at ssisco@kphanet.org 32
THE KENTUCKY PHARMACIST
August 2016 CE — TAF vs. TDF
July/August 2016
August 2016 — TAF vs. TDF: Is There Really a Difference? 1. How do the pharmacokinetics of tenofovir alafenamide (TAF) differ from tenofovir disoproxil fumarate (TDF)? (Objective 1) A. TAF is metabolized to tenofovir intracellularly. B. TAF has less accumulation in peripheral blood mononuclear cells (PBMCs). C. TAF results in higher plasma concentrations of tenofovir. D. TAF requires higher doses than TDF to exert similar antiretroviral effects.
5. Which of the following is an appropriate counseling point for rilpivirine/emtricitabine/tenofovir alafenamide (Odefsey®)? (Objective 2) A. Must take on an empty stomach B. Not to be used with a proton pump inhibitor C. Not to be used in treatment-naïve patients D. May be used in patients with viral load >100,000 copies/mL 6. Which the following is true for use of tenofovir alafenamide/emtricitabine (Descovy®)? (Objective 2) A. It is a complete regimen for the treatment of HIV-1 infection in adults. B. It can be taken with or without food. C. It may be used as pre-exposure prophylaxis for patients at risk of HIV-1 infection. D. It is approved for use in creatinine clearance <20mL/min.
2. Which of the following is true? (Objective 1) A. HIV-infected persons are at lower risk for osteoporosis than HIV-negative persons. B. Continuous antiretroviral (ART) therapy contributes to decreased BMD loss. C. Tenofovir disoproxil fumarate (TDF) is the only ART medication which has been linked to BMD loss. D. Tenofovir alafenamide (TAF) has lower risk for BMD loss than TDF.
7. A patient presents to the clinic to initiate antiretroviral therapy for a new diagnosis of HIV-1 infection. He would prefer a single tablet option but his creatinine clearance is 41mL/min. Which of the following would be the most appropriate choice of initial treatment based on current guidelines? (Objective 3) A. Elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide (Genvoya®) B. Rilpivirine/emtricitabine/tenofovir alafenamide (Odefsey®) C. Elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate (Stribild®) D. Tenofovir alafenamide/emtricitabine (Descovy®)
3. Which statement below is true? (Objective 1) A. TDF has not been linked to acute kidney injury and Fanconi’s syndrome. B. Use of protease inhibitors with TDF results in reduced risk for nephrotoxicity. C. Underlying risk factors for TDF-induced nephrotoxicity include older age and comorbidities. D. The CrCl cut-off for tenofovir use in patients with chronic kidney disease is 50 mL/min/1.73m2. 4. Which of the following combinations utilizes 10mg of TAF? (Objective 2) A. Tenofovir alafenamide/emtricitabine (Descovy®) B. Elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide (Genvoya®) C. Rilpivirine/emtricitabine/tenofovir alafenamide (Odefsey®)
The Kentucky Pharmacist is online! Go to www.kphanet.org, click on Communications and then on The Kentucky Pharmacist link.
Would you rather receive the journal electronically? Email ssisco@kphanet.org to be placed on the Green list for electronic delivery. Once the journal is published, you will receive an email with a link to the online version.
33
THE KENTUCKY PHARMACIST
June 2016 July/August
August 2016 CE — TAF vs. TDF
2016
This activity is a FREE service to members of the Kentucky Pharmacists Association. The fee for non-members is $30. Mail completed forms to: KPERF, 96 C Michael Davenport Blvd., Frankfort, KY 40601. Credit will be applied to your CPE Monitor Profile. Expiration Date: July 15, 2019 Successful Completion: Score of 80% will result in 1.5 contact hours or .15 CEUs. Participants who score less than 80% will be notified and permitted one re-examination. TECHNICIANS ANSWER SHEET. August 2016 — TAF vs. TDF: Is There Really a Difference? (1.5 contact hour) Universal Activity # 0143-0000-16-008-H02-T Name _______________________________________________KY Cert. # __________________________________ Address ______________________________________________Email_____________________________________ PLEASE CIRCLE THE APPROPRIATE ANSWERS: 1. A B C D 3. A B C D 5. A B C D 2. A B C D 4. A B C 6. A B C D
7. A B C D
Met my educational needs ___Yes ___No Figures and tables were useful ___Yes ___No Achieve the stated objectives ___Yes ___No Posttest was appropriate ___Yes ___No Was well written ___Yes ___No Commercial bias was present ___Yes ___No Is relevant to my practice ___Yes ___No If yes, please explain on a separate sheet. Unmet Objectives:______________________________________________________________________________ I hereby certify that I completed this self-study program independently and without assistance from any other party. Signature ____________________________________________Completion Date___________________________
Personal NABP eProfile ID #_____________________________ Birthdate ____________(MM/DD) PHARMACISTS ANSWER SHEET August 2016 — TAF vs. TDF: Is There Really a Difference? (1.5 contact hour) Universal Activity # 0143-0000-16-008-H02-P Name ________________________________________________ KY Lic. # __________________________________ Address ______________________________________________Email_____________________________________ PLEASE CIRCLE THE APPROPRIATE ANSWERS: 1. A B C D 3. A B C D 5. A B C D 2. A B C D 4. A B C 6. A B C D
7. A B C D
Information presented in the activity: Met my educational needs ___Yes ___No Figures and tables were useful ___Yes ___No Achieve the stated objectives ___Yes ___No Posttest was appropriate ___Yes ___No Was well written ___Yes ___No Commercial bias was present ___Yes ___No Is relevant to my practice ___Yes ___No If yes, please explain on a separate sheet. Unmet Objectives:______________________________________________________________________________ I hereby certify that I completed this self-study program independently and without assistance from any other party. Signature ____________________________________________Completion Date___________________________
Personal NABP eProfile ID #_____________________________ Birthdate ___________________(MM/DD) The Kentucky Pharmacy Education & Research Foundation is accredited by The Accreditation Council for Pharmacy Education as a provider of continuing Pharmacy education.
34
Quizzes submitted without NABP eProfile ID # and Birthdate will not be accepted.
THE KENTUCKY PHARMACIST
KPPAC Contribution Form
July/August 2016
Kentucky Pharmacists Political Advocacy Contribution Form Name: _________________________________ Pharmacy: ___________________________ Address: _______________________ City: ________________ State: _____ Zip: ________ Phone: ________________ Fax: __--_______________ E-Mail: __________________________________ Contribution Amount: $_________ Check ____ (make checks payable to KPPAC)
Mail to: Kentucky Pharmacists Political Advocacy Council, 96 C Michael Davenport Blvd., Frankfort, KY 40601
CONTRIBUTION LIMITS The primary, runoff primary and general elections are separate elections. The maximum contribution from a PAC to a candidate or slate of candidates is $1,000 per election.
Cash Contributions: $50 per contributor, per election. Contributions by cashierâ&#x20AC;&#x2122;s check or money order are limited to $50 per election unless the instrument identifies the payor and payee. KRS 121.150(4)
Individuals may contribute no more than $1,500 per year to all PACs in the aggregate.
Anonymous Contributions: $50 per contributor, per election, maximum total of $1,000 per election.
In-kind contributions are subject to the same limits as monetary contributions.
(This information is in accordance with KRS 121. 150)
35
THE KENTUCKY PHARMACIST
KPhA House of Delegates Report
July/August 2016
Kentucky Pharmacists Association House of Delegates Report of Action Items Marriott Downtown Louisville June 3-5, 2016 Chris Harlow, PharmD—2016 Speaker
Delegates present: 58 Total Delegates
Lance Murphy, PharmD—2016 Vice-Speaker and Chair of the Reference Committee Joey Mattingly, PharmD—Parliamentarian (Friday, June 3, 2016)
Secretary Brooke Hudspeth chaired the credentialing process. She reported that 30 Delegates were needed for a Simple Majority vote and 39 were needed for a 2/3 Majority vote.
Joe Fink, PharmD—Parliamentarian (Saturday, June 4, 2016)
The following reports were presented to the House of Delegates:
At the 2016 KPhA House of Delegates members from throughout the Commonwealth gathered to discuss, debate and make recommendations to not only shape OUR KPhA, but also to push forward OUR beloved profession.
Chair’s Report: Bob Oakley
Opening Session
Executive Director’s Report: Robert McFalls
Speaker Chris Harlow convened the Opening Session on the KPhA House of Delegates on Friday, June 3, 2016 at 7:50 a.m. Delegates were slated in accordance with the updated KPhA Bylaws, and annual reports of the association were presented.
Appreciation awards were presented to the outgoing KPhA Board members.
The Invocation was given by Duane Parsons.
Organizational Affairs—Ralph Bouvette
Lance Murphy led everyone in the Pledge of Alliance.
Public and Professional Affairs—Chad Corum
Juliana Swiney led the Oath of a Pharmacist.
Government Affairs—Richard Slone
The minutes from the June 26-28, 2015 House of Delegates minutes were presented. A motion was moved to approve the minutes and seconded. Motion carried.
Membership Engagement Committee—Trish Freeman
New Practitioner Committee—Amanda Jett
Provider Status Workgroup—Trish Freeman
Rx Therapy Management—Cathy Hanna
KPPAC—Matt Carrico
Kentucky Renaissance Pharmacy Museum—Gloria Doughty & Jaime Millard
Treasurer’s Report: Chris Palutis
Committee Reports, Affiliate Boards and Organizations were presented as follows:
From the 2015 House of Delegates, there were some ByLaw Changes in which all Pharmacists Members are now Delegates of the House. With the By-Law Changes, the need for updated Rules and Procedures are needed. Chris Harlow asked all in attendance to review the suggested changes to the Rules and Procedures as they were presented electronically before the Annual Meeting to all Members of KPhA. A motion was made and seconded to suspend House Rules. Motion carried. The motion was made to amend the Rules as presented, and seconded. After discussion, the amendment was suggested to have the Speaker of the House identify how many Student Delegates are eligible from each college of pharmacy. Have the students to sign in as delegates on a first come, first served basis and once their limit has been met, no further student delegates will be certified for that HOD Session. Motion carried.
President’s Report: Chris Clifton
Nominations were requested for Vice-Speaker; Amanda Jett was nominated. There were not additional nominations. Reference Committee Speaker Harlow appointed the Reference Committee as follows: Lance Murphy (Chair, Vice Speaker), Amanda Jett, Joey Mattingly, Chad Corum and Juliana Swiney. Speaker Harlow announced that the committee would meet Saturday morning at 7:00 a.m. in the Clubhouse Room on the second floor, and that the meeting was open to all inter-
36
THE KENTUCKY PHARMACIST
KPhA House of Delegates Report
July/August 2016
ested KPhA members. The committee’s charge was to discuss the resolutions from the Board of Directors to the House of Delegates and to provide feedback to the House in accordance with its Rules and Procedures.
policy was reviewed and recommended for adoption, archiving 1983.5 to be replaced by 2016.4 for a new record retention policy and Chair Murphy so moved: “In accordance with federal and state requirements, including but not limited to the Sarbanes Oxley Act, the Association shall maintain the following records permanently: Articles of Incorporation; Audit reports from independent audits; Determination Letter from the IRS, and correspondence relating to it; Financial Statements (year-end); Minutes of Board and HOD meetings; Real Estate deeds and records; Retirement Plan(s); and, Federal, State and Local Tax Returns, including Form 990. Other Association documents, e.g., canceled checks, invoices and routine financial records, shall be maintained for a period of seven (7) years unless required otherwise by agreement, contract or other authority.” Motion was seconded. Speaker Harlow called for the vote and ruled that the motion carried.
Closing Session The Closing Session convened on Saturday, June 4, 2016. During this session, recommendations of the Reference Committee were discussed and the vote for Vice-Speaker commenced. Invocation was led by Jessika Chinn. The report of the Credentials Committee was presented by Lance Murphy. Delegates Present: 49 Total 25 Delegates needed for a Simple Majority vote, 33 needed for a 3/4 vote, and 37 for a 2/3 Majority vote. Speaker Harlow called upon Vice Speaker Murphy, Chair of the Reference Committee, for its recommendations. Action taken by the House is also listed below with recommendation for adoption by the Reference Committee.
Proposed New Article 1.17 to be added to the Kentucky Pharmacists Association Bylaws: Article 1.17 Retired Pharmacist Members. A retired pharmacist is defined as a pharmacist who maintains his or her licensure but who has ceased to work. The Reference Committee recommended the adoption of the resolution as amended, and Chair Murphy so moved. — Motion was seconded. Speaker Harlow called for the vote and ruled that the motion carried. The Kentucky Pharmacists Association (KPhA) supports the establishment of a separate Board of Directors for the Kentucky Pharmacy Education and Research Foundation (KPERF). No final action will be taken without approval of the KPhA House of Delegates. The Reference Committee recommended the adoption of the resolution as amended, and Chair Murphy so moved. — Motion was seconded. Speaker Harlow called for the vote and ruled that the motion carried.
The election was conducted for Vice-Speaker with one nomination; Amanda Jett. A vote via paper ballots was held. Amanda Jett was officially elected and appropriately sworn in as Vice-Speaker of the House of Delegates. Installation of 2016-17 Incoming KPhA Board of Directors
Kevin Chen
Cathy Hance
Cassandra Hobbs
Katherine Keeney
Jeff Mills (unable to attend due to work conflict)
Secretary Brooke Hudspeth was installed as Secretary on Friday
The 2016 House of Delegates, once again, was a time for discussion and debate. This is when we decide the next steps of OUR KPhA and look forward to more involvement and discussion in the House as we advance OUR profession. Speak up to become involved, serve on a committee, become a delegate in the House and voice OUR stance. KPhA is YOU!
The KPhA supports the development of innovative voting practices for meetings of the House of Delegates. The Reference Committee recommended the adoption of the resolution as amended, and Chair Murphy so moved. — Motion was seconded. Speaker Harlow called for the vote and ruled that the motion carried.
The KPhA recognizes that its record retention policy needs to be updated and that a new policy is needed to replace HOD 1983.5 (Procedural Policy). The following 37
The next meeting of the KPhA House of Delegates will be at the 2016 KPhA Legislative Conference November 11, 2016 at the Capital Plaza Hotel in Frankfort. Mark your calendar now! THE KENTUCKY PHARMACIST
KPhA Board Retreat
July/August 2016
2016 KPhA Board Strategic Planning Retreat Members of the KPhA Board of Directors gathered July 15-16, 2016 at Kentucky Dam Village State Resort Park to discuss the strategic direction of the Association and update the Strategic Plan from 2012. Watch for an updated plan later this fall. Special thanks to our volunteer facilitators, Dean Cindy Stowe from SUCOP and Interim Dean Kelly Smith from UKCOP!
38
THE KENTUCKY PHARMACIST
The Campaign for Kentucky’s Pharmacy Future
July/August 2016
The Campaign for Kentucky’s Pharmacy Future: The Next 50 Years
Leave a legacy by participating in the campaign to replace OUR KPERF/KPhA Headquarters! Learn more about options for payment and levels of recognition at http://www.kphanet.org/?page=buildingcampaign or call 502-227-2303. Join the Committee of 100 and help OUR KPhA accelerate to 50 percent of our Campaign Goal!
Donors to the campaign as of August 1, 2016
Jeff Arnold Ray Bishop Fred Carrico Matt Carrico Jessika Chinn J. Leon & Margaret Claywell Chris & Katy Clifton David Dubrock Brian Fingerson Renie & Joe Fink Matt Foltz Andrew & Virginia France Trish Freeman Robert Goforth
Cynthia Gray George & Burnetta Hammons Chris Harlow JCAP Don & Vicki Kupper Phil & Julie Losch Joe Mashni Bob Oakley Chris & Consuelo Palutis Duane Parsons Richard & Zena Slone Leah Tolliver Sam Willett Mary Ann & Michael Wyant
39
THE KENTUCKY PHARMACIST
KPhA New and Returning Members
July/August 2016
KPhA Welcomes New and Renewing Members May-June 2016 Cathy Adams Pineville
Jonathan Buckman Bardstown
Kim Croley Corbin
Kasey Alford Smiths Grove
Robert Buckner Campbellsville
Robert Croley Corbin
Shannon Allen London
David Burgess Lexington
Leah DeVaughn Richmond
Brittany Antle Jamestown
Julie Burris Louisville
Jackie Dickerson-Galer Inez
Rosana Aydt Villa Hills
Holly Byrnes Louisville
James Dixon Barbourville
Danielle Ayres Nicholasville
Joseph Carroll Salyersville
Barry Eadens Bowling Green
To YOU, To YOUR Patients To YOUR Profession!
Larry Barnett South Williamson
Katherine Chase Lexington
David Edmundson Bowling Green
Aaron Gilbert Butler
Crystal Belt London
William Chauvin Elizabethtown
Harold Ellis Frankfort
Michelle Gilbert Butler
William Bentley South Shore
Jessika Chinn Beaver Dam
Ashley Eschenbach Louisville
Natasha Good London
Alexander Bessler Newport
Margaret Christopher Winchester
Jamie Ferrell Winchester
Dwaine Green The Villages, Fla.
Nick Boggess Flatwoods
Kenneth Clayton Elkton
Justin Fink Fort Wright
Melissa Greenlee Burlington
Charlotte Bowling London
Heather Clayton Elkton
Timothy Finley Florence
Larry Hadley Frankfort
David Bowman Columbia
Richard Clements Morganfield
Alan Flener Glasgow
Kelsey Hall Louisville
Terry Box Cynthiana
Virginia Clements Morganfield
Sophia Foree Sulphur
William Hall Whitesburg
Abigail Breit Louisville
Joe Coffey Somerset
Patricia Freeman Lexington
Joan Haltom Danville
Tyler Bright Lexington
Arica Collins Albany
Charles Galer Inez
Kathy Hardy Smiths Grove
Benjamin Brown Louisville
Paul Cooper Morehead
Roy Gentry Monterey, Tenn.
Kyle Harris London
Dianna Bryant Hartford
Ruth Croghan Louisville
Paula Gibson Manchester
Jonathan Hayes Prospect
40
MEMBERSHIP MATTERS:
THE KENTUCKY PHARMACIST
KPhA New and Returning Members
July/August 2016
Kevin Higgins Benton
John McFarland London
John Price Louisvillle
Katherine Spencer Louisville
Gregory Hines Bowling Green
Aaron Mcintosh Midway
Adam Robinson Brandenburg
Julie Spivey Lexington
Carolynn Horn Philpot
Lisa Miles Bardstown
Marcella Robinson Paducah
Rodney Stacey Cumberland
Tom Houchens London
Dan Minogue Louisville
Frank Romanelli Lexington
Tyler Stevens Lexington
Jan Houchens London
Judith Minogue Louisville
Barry Rose Clay City
Dan Stevenson Portsmouth, Ohio
James Howard Fountain Run
Jeffrey Moore Middlesboro
Richard Ross Louisville
Christopher Stovall London
Reymonda Howard London
Mary Murphy Louisville
Andrew Rudd Floyds Knobs, Ind.
Juliana Swiney Prospect
Mark Huffmyer Lexington
Owen Neff Centerville, Ohio
Angela Rudd Floyds Knobs, Ind.
Joanne Taheri Louisville
Bill Hurley Simpsonville
Chanin Nelson Middlesboro
Joanna Sames Shelbyville
Clint Tilford West Paducah
Karen Jackson Paducah
Brad Newcomb Paducah
Lisa Schwartz Crestview Hills
Leah Tolliver Lexington
Daniel Jones Paducah
Frank Nicks Bowling Green
Jan Scott Earlington
Brett Vickey Wilmore
Euisoon Kang Louisville
Christopher Noetzel Lexington
William Sewell Utica
Sarah Vickey Wilmore
Patricia Kinney Erlanger
Jamie Otte Florence
Elizabeth Sharp Louisville
Lenville White Louisville
Sarah Lawrence Louisville
Richard Parsons Lexington
Patricia Slone Hindman
Shirley White London
Mike Leake Danville
Megan Pendley Lexington
Justin Smith South Windsor, Conn.
Charlsie Williams Paducah
Timothy Lewis Winchester
Brookes Pickard Louisville
Marla Smoot Crittenden
Cindi Williams Hazard
Andrew Logsdon Mayfield
Aric Polston Bowling Green
Walter Soja Taylorsville
Clyde Wilson Danville
Elizabeth Lovell Lexington
Amanda Powers Boaz
Lindsey Spalding Louisville
Thomas Mason Fairfield, Ohio George McDannold Eminence
KPhA Honorary Life Members Ralph Bouvette, Leon Claywell, R. David Cobb, Gloria Doughty, Ann Amerson Mazone, Kenneth Roberts 41
THE KENTUCKY PHARMACIST
Naloxone Atomizer Distribution Project
July/August 2016
Naloxone Atomizer Distribution Project Thanks to a grant from WellCare of Kentucky, OUR Kentucky Pharmacists Association is distributing naloxone atomizers to combat opioid overdose deaths in Kentucky. The atomizers allow naloxone to be administered like a nasal spray instead of through an injection – which can be a less intimidating way to deliver the life-saving drug. The atomizers are to be provided by Kentucky Board of Pharmacy certified pharmacists free of charge to Medicaid recipients when dispensing a naloxone kit. A state law passed last year authorizing certified pharmacists to dispense naloxone via a physician-approved protocol to people who may be at risk for an opioid overdose. In order to receive a small supply of free atomizers, a pharmacy must:
Have a naloxone-certified pharmacist on staff Have an active protocol established to offer naloxone Actively dispense naloxone to at-risk Medicaid recipients
If you are interested in becoming naloxone-certified, please visit the KPhA website to access an online, Board-approved training program offered by the Kentucky Pharmacy Education and Research Foundation. (See below.) To request your supply of atomizers, contact KPhA at 502-227-2303 or email info@kphanet.org.
KPERF Naloxone Certification Training The online training program can be found at the following link on the KPhA website: http://www.kphanet.org/?page=NaloxoneCert2015 The cost of the training is $5 for KPhA members, and $10 for non-KPhA members. After successfully completing the course, credit will be applied to your CPE Monitor Profile and you will be emailed a certificate of completion. 42
THE KENTUCKY PHARMACIST
APSC
July/August 2016
43
THE KENTUCKY PHARMACIST
Pharmacy Law Brief
July/August 2016
Pharmacy Law Brief: Pharmacists Serving as Expert Witnesses Author: Peter P. Cohron, B.S.Pharm., J.D., practicing pharmacist and attorney, Henderson, Ky. Question: I’ve had a contact from an attorney out of state who knows a relative of mine about serving as an expert witness in a case. He wants me to first evaluate a bunch of background documents to then be discussed with him. He said that down the road it also may involve a deposition and even testimony at trial. What am I potentially getting myself into here? How much time might this take? What’s my role? I assume I can bill for my time and expertise, right?
Submit Questions: jfink@uky.edu Disclaimer: The information in this column is intended for educational use and to stimulate professional discussion among colleagues. It should not be construed as legal advice. There is no way such a brief discussion of an issue or topic for educational or discussion purposes can adequately and fully address the multifaceted and often complex issues that arise in the course of professional practice. It is always the best advice for a pharmacist to seek counsel from an attorney who can become thoroughly familiar with the intricacies of a specific situation, and render advice in accordance with the full information.
Response: Many pharmacists today are taking on the role of expert witness. It is another way to exercise the knowledge gained through education and experience and can be an additional source of income. I have acted as an expert in severSecond, be ready to be grilled over minute details, even by al cases. the attorney hiring you. A deposition and trial are sworn testiSome lawsuits have issues beyond what a reasonable lay mony so you want to be sure of what you are saying. And person would understand. This is often the case in medicacross-examination in a trial by the opposing attorney is, quite tion-related lawsuits. The jury would be lost listening to medi- often, a special kind of h*ll. Third, as for the time involved, cal jargon and have trouble understanding the professional the complexity of the case will determine that. Most cases I standards. So, the opposing sides bring in experts to explain have worked only required a few hours of my time, but a couthe issues at hand in an understandable manner so that the ple went well over a hundred or more. Your initial interview jurors may make an informed decision. with the hiring attorney and your first review of the records What is an expert witness? It is a pharmacist with similar ed- should clue you as to the time required. Finally, are you prepared to have another pharmacist’s career depend on your ucation, skills and experience as the pharmacist on trial. If you have similar credentials as the pharmacist in the lawsuit, opinion of how she acted? That is how it will be; your words go for it. If she is a hospital pharmacist and you practice in a will have a lot of sway with the jury. community chain pharmacy it would be best to turn it down — you are not qualified. If you have recently graduated and the pharmacist has 30 years experience, again, you are not the right expert. Similarity is the key to being an expert.
Should you bill for this? Absolutely. Someone wants to avail themselves of your services, of your pharmacist skills. Check around to see what the going rate for pharmacist experts is. If you cannot get this information, at the very least set your hourly rate at three times your pay per hour as a pharmacist. On what does the expert opine? Interestingly, the focus is not Cheap experts, attorneys will tell you, are not believed or apso much what the pharmacist being sued did or did not do. preciated as much as the more expensive ones. Instead, the expert indicates whether or not another pharmacist with similar education, skills and experience would have, If you decide to do this, remember that you are the expert. It under similar circumstances, reasonably come to the same will not only be the opposing attorney who will try to twist action or conclusion as the actual pharmacist did. “Would a your words. Even the lawyer who hires you will often want reasonable pharmacist have honored the prescription?” you to bend your words, say your statement in a different “Would a reasonable pharmacist have contacted the premanner, etc., in order to strengthen your opinion in a manner scriber before dispensing the medication?” From that, you more suited to them than you. Do not let your opinion or testiconclude that the pharmacist acted properly or not. For exmony get “evolved” away from your opinion. ample, “To a degree of reasonable medical certainty, in the Finally, take this seriously. Being an expert, as I have indicatsame situation, I would have called the prescriber just like the ed above, is a sizable responsibility. Do not do this just for pharmacist did. Therefore, I believe she acted correctly.” added income. Act in a manner that is professional and one What are you getting yourself into? First, you need to have that engenders respect and admiration, and give due considthe records you review down pat. This may take some time. eration and weight to just what results your words may bring. 44
THE KENTUCKY PHARMACIST
Thank You Gloria!
July/August 2016
Thank you Gloria! Gloria Doughty, who recently celebrated her 90th birthday, has donated a silver punch bowl set to KPhA. The set, which was originally a gift from William Curry upon Gloria’s transition from Hubbard & Curry Pharmacy in 1962, was used during the Open House in May at the new headquarters of the Association, and will be used at many future events, thanks to Mrs. Doughty’s generosity. “You are my family,” Gloria told Executive Director Bob McFalls in bestowing this much-appreciated gift to OUR KPhA.
45
THE KENTUCKY PHARMACIST
Pharmacy Policy Issues
July/August 2016
PHARMACY POLICY ISSUES: Rescheduling Hydrocodone Combination Products - One Year Later Author: Rebekah Wahking is a third professional year student at the UK College of Pharmacy. She also is completing requirements for the degree Master of Business Administration at the UK Gatton College of Business and Economics. A native of Lexington, Ky., she completed a Bachelor of Science in Psychology at UK (summa cum laude) before entering pharmacy school. Issue: Hydrocodone combination products were re-scheduled about one year ago. Sometimes difficulties and unintended consequences don’t become obvious until after such a public policy change has been implemented. What are some challenges that have surfaced as a result of this change? Discussion: One year after the rescheduling of Hydrocodone Combination Products (HCPs), there appear to be clear benefits to stronger regulation of these products. The rescheduling seems to be helping the addiction and overdose problems related to HCPs in Kentucky. On the other hand, there are some well-defined issues in pharmacy practice that are burdensome on day-to-day pharmacy operations and patient needs. Specifically, pharmacists cannot change the prescriber on a prescription for a C-II medication and the extreme limitations on partial dispensing of these medications can be problematic. This can be very challenging for the patient who is in pain. Obviously, there needs to be a balance in combating abuse issues and regulating pharmacy practice with respect to HCPs.
Have an Idea?: This column is designed to address timely and practical issues of interest to pharmacists, pharmacy interns and pharmacy technicians with the goal being to encourage thought, reflection and exchange among practitioners. Suggestions regarding topics for consideration are welcome. Please send them to jfink@uky.edu.
First, some Medicaid plans will not pay for a prescription if a medical resident or other non-covered prescriber signs the HCP prescription. Therefore, patients presenting such prescriptions must either pay out-of-pocket or choose to return to the prescriber’s office to have the prescription re-written. This is extremely time consuming for any patient and especially inconvenient for one who is dealing with severe pain. This rule is challenging for pharmacists to explain to patients. The Kentucky General Assembly already made exceptions for APRNs to authorize prescriptions for HCPs, while other narcotic C-IIs do not fall within their scope of authority. “If any substance is designated, rescheduled, or deleted as a controlled substance under federal law and notice thereof is given to the Cabinet for Health and Family Services, the Cabinet for Health and Family Services may similarly control the substance under this chapter by regulation. If hydrocodone or any drug containing hydrocodone is rescheduled to Schedule II in this manner, the prescriptive authority existing 46
on March 19, 2013, of any practitioner licensed under the laws of the Commonwealth to prescribe, dispense, or administer hydrocodone or drugs containing hydrocodone shall remain Inviolate and shall continue to exist to the same extent as if those drugs had remained classified as Schedule III controlled substances.”1 (emphasis added) Perhaps the same approach of a carve-out could be used to allow pharmacists to have latitude with these issues given the circumstances. If pharmacists were authorized to verbally clarify and minimally change an HCP prescription that might include changing the prescriber name, some of this confusion could be limited. This is compliant with the DEA since the DEA does not regulate if a prescriber can be changed on a C-II prescription. All the DEA mandates is that the “essential elements” of a prescription cannot be changed by a pharmacist after oral consultation with the prescriber. These elements are the name of the medication, strength of the medication, dosage form and quantity.2 Oddly enough, the DEA does not list the prescriber as an essential element of the prescription. In this letter, the DEA defers to the states to make the decision if a pharmacist can change the other elements of a C-II prescription. According to Kentucky Board of Pharmacy, the signature of the prescriber cannot be changed on a C-II prescription.3 With state legislative changes, HCP could be an exemption.
THE KENTUCKY PHARMACIST
July/August 2016
Pharmacy Policy Issues Furthermore, if the DEA would allow as many partial dispensings as a patient or pharmacist needs in the 60 day life of the prescription, this would eliminate some cost barriers for the patient. A partial dispensing occurs when a portion of the medication is dispensed and the rest is to be provided at a later time. Since under the current approach, the remainder must be picked up in 72 hours, or lost, many pharmacies will not dispense less than the full quantity on an HCP prescription.4 Also, patients must be able to pick up and pay for their entire prescription at once. Even though most of these products are relatively inexpensive, there are quite a few patients who cannot afford the entire cost all at once. As it stands now, it is the DEA who regulates the partial fill limitations. The DEA would need to go through the regulatory process and the Kentucky Board of Pharmacy would need to follow suit.5
little latitude when trying to help a patient in pain may be the solution when trying to find the balance. References 1. K.R.S. 218A.020(3). 2. Letter from the U.S Department of Justice Drug Enforcement Administration dated Oct. 15, 2008. Retrieved Jan. 12, 2016. http://www.deadiversion.usdoj.gov/faq/ multiple_rx_clarification_ltr_102010.pdf. 3. Kentucky Board of Pharmacy. Controlled Substances Questions. Retrieved Jan. 12, 2016. http://pharmacy.ky.gov/Pages/Controlled-SubstancesQuestions.aspx.
4. 21 C.F.R. §1306.13. Partial filling of prescriptions. These proposed policy changes are not likely to make HCPs more accessible to patients who do not have a legiti- 5. Kentucky Board of Pharmacy. Statutes and Regulations. Kentucky Pharmacy Law Book. Retrieved Dec. mate need. Rather, these would tear down some common 12, 2015. http://pharmacy.ky.gov/ barriers for pharmacists and patients. Pharmacists already statutesandregulations/Pages/default.aspx. are being expected to do more work on a daily basis. A The Kentucky Renaissance Pharmacy Museum offers several ways way to show support of the Museum, our state's leading preservation organization for pharmacy. While contributions of any size are greatly appreciated, the following levels of annual giving have been established for your consideration.
Friend of the Museum $100 Proctor Society $250 Damien Society $500 Galen Society $1,000 Name______________________________________ Specify gift amount________________________ Address ____________________________________ City____________________Zip______________ Phone H____________________W________________ Email___________________________________ Employer name_____________________________________________________for possible matching gift. Tributes in honor or memory of_____________________________________________________ Mail to: Kentucky Renaissance Pharmacy Museum, P.O.Box 910502, Lexington, KY 40591-0502 The Kentucky Renaissance Pharmacy Museum is a non-profit 501(c)(3) business entity and as such donations are tax deductible. A notice of your tax deductible contributions will be mailed to you annually.
For more information on the Kentucky Renaissance Pharmacy Museum, see www.pharmacymuseumky.org or contact Gloria Doughty at g.doughty@twc.com.
The Campaign for Kentucky’s Pharmacy Future: The Next 50 Years http://www.kphanet.org/?page=buildingcampaign 47
THE KENTUCKY PHARMACIST
July/August 2016
Pharmacists Mutual
48
THE KENTUCKY PHARMACIST
Cardinal Health
July/August 2016
49
THE KENTUCKY PHARMACIST
KPhA Board of Directors/Staff
July/August 2016
KPhA BOARD OF DIRECTORS
HOUSE OF DELEGATES
Chris Clifton, Villa Hills chrisclifton@hotmail.com
Chair
Lance Murphy, Louisville lancemurphy84@gmail.com
Trish Freeman, Lexington trish.freeman@uky.edu
President
Amanda Jett, Louisville ajett@sullivan.edu
Chris Harlow, Louisville cpharlow@gmail.com
President-Elect
KPERF ADVISORY COUNCIL
Brooke Hudspeth, Lexington brooke.hudspeth@kroger.com
Secretary
Christen S Bruening, Cincinnati, Ohio cmschenkenfelder@gmail.com
Chris Palutis, Lexington chris@candcrx.com
Treasurer
Matt Carrico, Louisville matt@boonevilledrugs.com
Jessika Chinn, Beaver Dam jessikachilton@ymail.com
Past President Representative
Vice Speaker of the House
Kim Croley, Corbin kscroley@yahoo.com Kimberly Daugherty, Louisville kdaugherty@sullivan.edu
Directors Matt Carrico, Louisville* matt@boonevilledrugs.com Kevin Chen, Lexington kevin.chen@uky.edu
Speaker of the House
Mary Thacker, Louisville mary.thacker@att.net University of Kentucky Student Representative
Chad Corum, Manchester pharmdky21@gmail.com Matt Foltz, Villa Hills mfoltz@gomedcare.com Cathy Hance, Louisville cathy@compoundcarerx.com Cassy Hobbs, Louisville cbeyerle01@gmail.com Katherine Keeney, Louisville Sullivan University KKEENE6675@my.sullivan.edu Student Representative Chris Killmeier, Louisville cdkillmeier@hotmail.com Jeff Mills, Louisville jeff.mills@nortonhealthcare.org Richard Slone, Hindman richardkslone@msn.com Sam Willett, Mayfield duncancenter@bellsouth.net * At-Large Member to Executive Committee
KPhA/KPERF HEADQUARTERS 96 C Michael Davenport Blvd., Frankfort, KY 40601 502.227.2303 (Phone) 502.227.2258 (Fax) www.kphanet.org www.facebook.com/KyPharmAssoc www.twitter.com/KyPharmAssoc www.twitter.com/KPhAGrassroots www.youtube.com/KyPharmAssoc Robert McFalls, M.Div. Executive Director rmcfalls@kphanet.org Scott Sisco, MA Director of Communications & Continuing Education ssisco@kphanet.org Angela Gibson Director of Membership & Administrative Services agibson@kphanet.org Leah Tolliver, PharmD Director of Pharmacy Emergency Preparedness ltolliver@kphanet.org Elizabeth Ramey Receptionist/Office Assistant eramey@kphanet.org
50
THE KENTUCKY PHARMACIST
50 Years Ago/Frequently Called and Contacted
July/August 2016
50 Years Ago at KPhA FROM KENTUCKY AT A GLANCE R.W. Leake, R.Ph., Danville, who underwent emergency surgery at Memorial Hospital in Richmond, Virginia, while returning from a New York vacation following the 1966 convention, has now been removed to the Ephraim McDowell Hospital in Danville, where he is recovering. R.W. has long been active in Association work and is a past President of the Kentucky Pharmaceutical Association. We all wish him an early recovery. EDITORâ&#x20AC;&#x2122;S NOTE: Mr. Leake served as KPhA President in 1963. - From The Kentucky Pharmacist, August 1966, Volume XXIX, Number 8.
Frequently Called and Contacted Kentucky Pharmacists Association 96 C Michael Davenport Blvd. Frankfort, KY 40601 (502) 227-2303 www.kphanet.org Kentucky Board of Pharmacy State Office Building Annex, Ste. 300 125 Holmes Street Frankfort, KY 40601 (502) 564-7910 www.pharmacy.ky.gov Pharmacy Technician Certification Board (PTCB) 2215 Constitution Avenue Washington, DC 20037-2985 (800) 363-8012 www.ptcb.org
Kentucky Society of Health-System Pharmacists P.O. Box 4961 Louisville, KY 40204 (502) 456-1851 x2 (502) 456-1821 (fax) www.kshp.org info@kshp.org American Pharmacists Association (APhA) 2215 Constitution Avenue NW Washington, DC 20037-2985 (800) 237-2742 www.aphanet.org
National Community Pharmacists Association (NCPA) 100 Daingerfield Road Alexandria, VA 22314 (703) 683-8200 info@ncpanet.org Drug Information Center Sullivan University College of Pharmacy 2100 Gardiner Lane Louisville, KY 40205 (502) 413-8638 www.sullivan.edu Kentucky Regional Poison Center (800) 222-1222
KPhA Government Affairs Contribution Name: _______________________________Pharmacy: _____________________________
Email: ______________________________________________________________ Address: _____________________________________________________________ City: ___________________________________________ State: _________ Zip: ____________ Phone: ________________ Fax: __--_______________ E-Mail: _____________________________ Contribution Amount: $_________ Check ____ (make checks payable to KPhA Government Affairs)
Mail to: Kentucky Pharmacists Association, 96 C Michael Davenport Blvd., Frankfort, KY 40601
51
THE KENTUCKY PHARMACIST
July/August 2016
THE
Kentucky PHARMACIST 96 C Michael Davenport Blvd. Frankfort, KY 40601
SAVE THE DATE
Show your Pharmacist Pride with a KPhA Roamey Window Cling ($5) or your own personalized Roamey ($25)! All proceeds benefit the KPhA Building Fund Available at the KPhA Online Store www.kphanet.org, click on About Tab, Online Store 52
THE KENTUCKY PHARMACIST