11 minute read
How D’You Know?
Analysis with a child requires flexibility, responding to where the child is mentally, physically & emotionally on any given day.
By Bri Lange & A. Bergquist
Advertisement
The very first thing I do when a child [i.e. kid] comes to see me at the clinic, is establish a bond with the parent or caregiver, making sure that the child sees this. Kids are always looking to their parents for guidance, asking “Is this okay?”. If you are not bonding with the parent, you are unlikely to bond with the child. Once I’ve made a connection with the parent, I will then get on the child’s level, look them in the eye, and talk about what the visit will look like for them. I talk with them like I would an adult, but in understandable language. A trick I use to build rapport with a child is to look to their shoes or outfit, and comment on something they are wearing. Do they have animals or a character on their clothes that I could comment on before entering their space? Bonding with the child sets the foundation for how the rest of the interaction will go. Another technique I use to initiate contact with the patient, is to invite the child into my space, rather than entering their space. This gives the child a sense of autonomy and a sense of safety, to be allowed to choose to be assessed.

When I do my analysis, I verbalize everything I’m doing, what I’m looking for, and what I find. I’ll say, “I’m looking to see that there is equal muscle tension from side to side. Oh look, this side has more tension. Can you feel that [presses on paraspinal muscles]?”. Without verbalizing, parents and kids will often have no idea what you are doing. I will regularly talk with the parent to ask questions like, “How has [child’s name] been sleeping?”, but I will always come back to making eye contact and talking with the child, because maintaining that connection with them is “super” important.
My analysis differs, depending on the age. For infants, I would have the child face up on a pediatric pillow to start. For toddlers, they are establishing their autonomy and often choose not to follow instruction, so my analysis will happen while they are playing
with a toy (Are they balanced, how is their rotation, is their walking symmetrical, are their toes pointed in?) and for older kids who respond to instruction (>4 y.o.), I will ask them to go face-up or face-down on the table. If a child is not responding to my instruction, a trick I use is to have the child lay on their parent and usually the child feels comfortable enough to do that. One time I used this technique with a young girl who I just could not keep still at all, and when she went face up on Mom, she
was a complete “noodle” for my assessment. So, use the parents!
Toys are also helpful. I have finger puppets that I use to help me assess cervical range of motion. I have the child follow my finger puppets left, right, up, down. It’s all about making it fun for kids! Unlike analysis with adults which can be relatively consistent and structured from visit to visit, the analysis with a child requires flexibility from visit to visit, responding to where the child is mentally, physically & emotionally on any given day. A useful technique to help build a sense of safety is to have the child palpate a toy or Mom or Dad before working with the child. I would say, “oh, can you help me palpate your stuffy?”, and then go through the motions. “Oh, can you use this ‘clicky’ toy to adjust Mom? Now that we did that, could we use this on you today too?”. Once the child sees that Mom is okay with it, then the child is usually more receptive. Also, kids love helping, so giving them a role to play helps them feel a part of the process.
When I assess kids, I’m not so focussed on posture, so much as I
am on function. Are they balanced in their movements? Can they bend equally from side to side, are they using both feet. I’ll toss them a ball and see if they can catch the ball. If they can’t, I’ll see how they pick it up. I’ll also ask a child that is walking already, to show me how they crawl. Demonstrating how they crawl can give me information about their pelvis that I might not gather from their walking. Symmetry is hugely important in kids. This kind of analysis will happen at every visit.
I have a strong philosophy and believe that we should adjust kids, or anyone for that matter, in a state where they are comfortable. So, I will never adjust a screaming, crying, or complaining child. Kids have full body autonomy, and I want to be congruent with their wishes. Some days, I’ll put my hands on a child’s neck, and they will say, “No, I don’t like that!” and I will just say, “Okay, we’re not doing that today”. It can be tricky though, because sometimes the child doesn’t want to be touched in an area of the spine, say the atlas, because palpation in the area is tender and might be related to a subluxation. So, you have to figure out when it’s a subluxation, or when its just that they don’t want your hands near them. Sometimes the parents will say that they will help and “hold them down”, but that’s not what this is about for me, so I don’t push it. It’s not life or death, I would just check again the next week. Sometimes the hardest part about working with kids is about reading the signals and knowing when to stop.
When it comes to finding subluxation in kids, a general rule of thumb is that things should feel “squishy”. If you are finding restriction, or a tightness, that is a good indication the area needs attention. With kids, palpation is the most important technique for finding subluxation. I use visualization, take history, do leg checks when the child is weight bearing, but palpation is the most valuable information for finding subluxation. With atlas, I will slide off of the mastoids and feel for symmetry, motion lateral to medial on one side, then the other. With atlas, you should feel the contact side move in and the opposite TPs separate. Sometime when an atlas is subluxated, it will feel like a tight ball of muscle sticking out. I would correct atlas adjustments with light sustained contact, maybe a light vibration, until you feel there is “ease” in the system. With lower cervicals, the line of correction is P-A, but still sustained contact. Sometimes I will do leg check for cervical syndrome as an added


piece of information. With kids, I prioritize atlas and pelvis. These two areas give the biggest bangfor-your-buck.
When checking pelvis, I will do a heel-to-buttock check to point me in a direction. If I get a positive [uneven leg restriction], I would be looking for a posterior segment, either S1, S2, S3, S4 on the side of greater leg restriction. The sacrum is not fused in kids, so I will palpate and feel for any posteriority at any one of these segments. I use these two fingers [index and chiro index] and apply pressure I-S, P-A across each segment, and as before, it should feel “squishy”. If not, then the area needs attention. With infants, I will squeeze the bum cheeks, and the butt-crack will point to the side of sacrum that is anterior-inferior [Bri: “Austin, can you maybe use a better word for ‘butt-crack’? *laughing*; Austin: “Sure I can” *laughing*]. Always ask for permission from the parents to do this test, because you are literally pulling the back of the infants pants down and squeezing their bum cheeks together to look for a deviation of their [intergluteal cleft] or [bum-crease]. The crease will “fall” into the A-I side. With this finding, you can choose to hold the sacrotuberous ligament on the A-I side, and/ or look for an adjustment of a posterior segment contralateral to the A-I side. When doing this test, make sure that the infant’s legs are even, because having one leg in front of the other can affect the outcome of the test.
To check ilium, I want to rock the ilium [grabs the air like she is holding an ilium in each hand] forwards and backwards, outwards and inwards feeling for symmetry in motion and resistance. One important thing to note is how far apart the PSIS’s are. In kids, they should be about 1-2 inches apart. If they are wider apart, there may be bilateral EX iliums. I had a child with severe toeing-in and their PSIS’s were really far apart. I used a [spring loaded instrument] to bring the iliums back inwards and it totally helped their toeing-in. I was so pumped!
After checking the iliums, I’ll use these two fingers again [index and chiro index], and palpate I-S, P-A up the lumbars and thoracics, again looking for a lack of “squishiness”. If I find something, I will do sustained contact (especially with infants), or put a little knife edge over a finger and add some vibration, or [spring loaded instrument] over my finger.
Do you adjust everything you find?
No, I don’t adjust everything I find. In kids, thoracic and lumbar subluxations are less common, especially lumbar subluxations. Like we talked about earlier, I prioritize atlas and pelvis. I always check full spine, but I get a sense of what the primary subluxations are based on all the information I gather during the interaction, and I address those subluxations. Sometimes I will adjust thoracics, but I always focus on atlas and pelvis. Overall, I find that less is more when adjusting kids. §
POLICY
Lifelines is the official quarterly magazine of the LifeWest student body, and is funded by Student Council. Any articles published herein do not necessarily reflect the opinions or beliefs of Life Chiropractic College West.
EDITOR/DESIGNER/PHOTOS
Dr. Austin Bergquist, PhD
FACULTY ADVISOR
Dani Lorta, MA
PRINTING Michael Poss
CONTACT
abergquist@college.lifewest.edu
ARTICLE SUBMISSION
Would you like to write for Lifelines magazine? We look for chiropractic articles that inspire & challange. Email CONTACT for more information.
PHOTOGRAPHIC SUBMISSIONS
Do you have amazing chiropractic photos that you would like showcased in Lifelines magazine? By sending your photos, you agree that you have the right to distribute the image, and maintain that all people depicted agree to have their image published. Email CONTACT for more information.
CREDITS
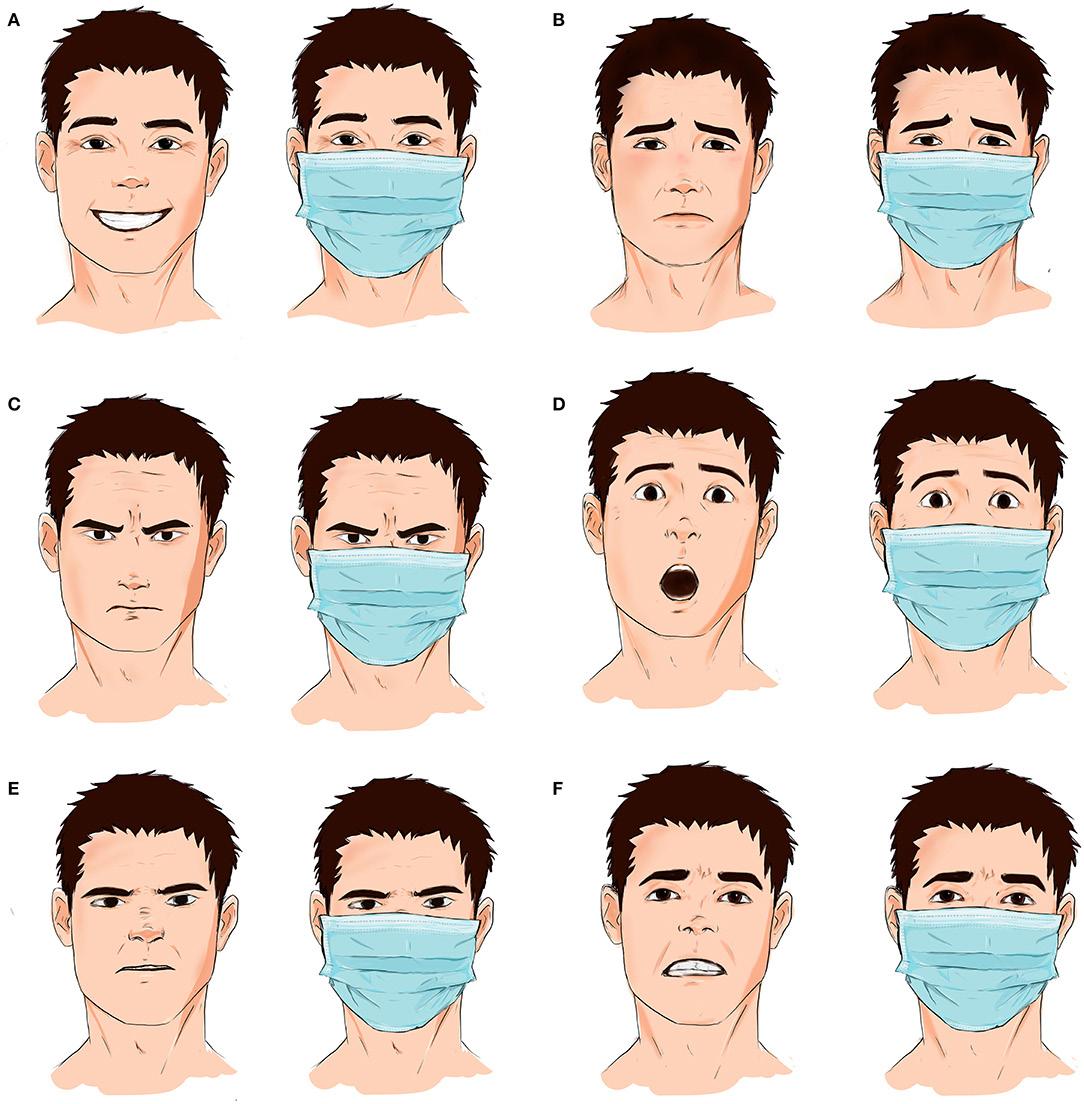
COVER Nolan Halverson; 2-3 EDITOR’S LETTER 2: Yosemite National Park, Dr. Austin Bergquist; 3: Julia Rose; Emma Harbage, Maddy Duncan; Simran Chawla; 4-5 MEET OUR PEOPLE Simran Chawla; Alexis Griffith; Nolan Halverson; Bri Lange; Sara Parsons; Meagan Stachnik; 6-7 CONTENTS 08 Alexis Griffith; 10 Fruit & Veg/PixaBay; 12 LifeWest.edu; 14 BJ Palmer/Lifewest.edu; 16 Simran Chawla; 18 Bri Lange; 8-9 WHY RESEARCH? Alexis Griffith 10-11 BUDGET EATS IN THE BAY Food plate/canadafoodguide.ca; Meagan Stachnik 12-13 25001 INDUSTRIAL BLVD. Pressure Cooker/PixaBay 14-15 ALL ELSE FOLLOWS Football Field/PixaBay 16-17 WHAT’S YOUR STORY? Simran Chawla 18-21 HOW D’YOU KNOW? Bri Lange on the shore; KIDS/PixaBay; Bri Lange with Spine; Child on Carpet/PixaBay; 22-23 CREDITS Masked Emotions/Mheildy et al (2020) Effect of Face masks on interpersonal communication. Frontiers in Public Health. BACK COVER “Doctored” Gaze of Mona Lisa/PixaBay
(A) Happiness is usually perceived when the corners of the lips rise upward. With face masks, happiness can be caught on the face by focusing on the wrinkles at the edge of the eyes. (B) Sadness involves movement of the eyebrows, the nasolabial folds, and the corners of the lips; however, the last two are masked by face masks. (C) Facial expression of anger emphasizes the downward and central movement of eyebrows, the glaring eyes, and narrowing of the corners of the lips, with the latter getting covered by face masks. (D) Expressions of surprise and shock are usually formed of elevated eyebrows and a raised upper lip; only the latter is covered by protective masks. (E) Nose wrinkling and raising of the upper lip convey feelings of disgust; however, face masks cover both expressions. (F) Feelings of guilt are usually portrayed by slightly upping eyebrows together and stretching the mouth, with the latter getting covered with a face mask.

The eye, the window of the soul, is the chief means whereby the understanding can most fully and abundantly appreciate the infinite works of nature; and the ear is second. - Leonardo Da Vinci