7 minute read
By Woodson “Scott” Jones, MD
Graduate Medical Education:
The Physician Pipeline for Bexar County and South Texas
Advertisement
By Woodson “Scott” Jones, MD
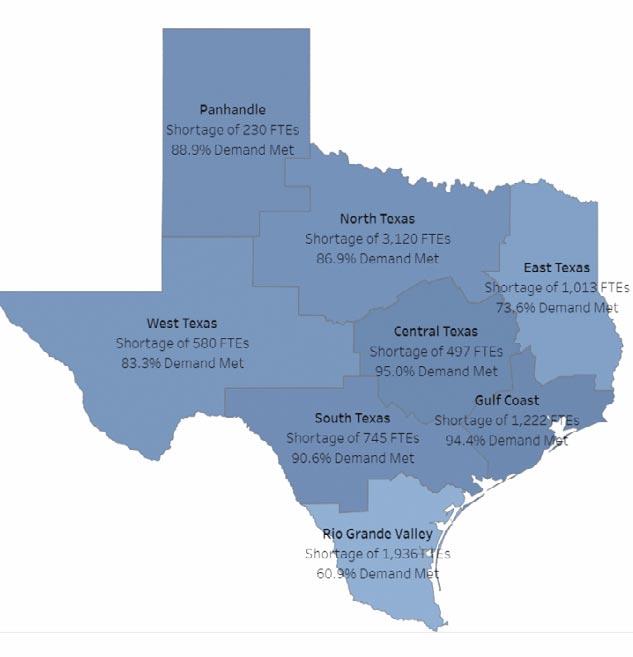
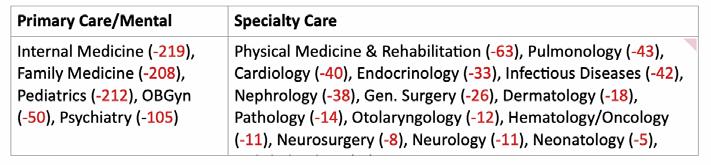
Multiple organizations have projected a growing shortage of physicians over the next decade. The Association of American Medical Colleges (AAMC) projects a national shortage of between 37,800 and 124,000 physicians by 2034.1 Further, Texas is ranked 41st of the 50 states in the number of active physicians (231) per 100,000 population.2 We have close to the most elderly physician workforces, ranked 49th of the 50 states. Given the aging Texas physician workforce and the COVID Pandemic leading to physicians choosing the leave the workforce sooner, Texas physician shortages may be greater than current projections.1 Texas Health and Human Services (HSS) project South Texas will be short 745 physicians by 2032, 10% short of the need (Figure 1).3 The Rio Grande Valley, despite the growth of the University of Texas Rio Grande Valley (UTRGV) School of Medicine GME programs, is projected to meet only 61% of the physician demand. Specialties with Texas HHS projects shortages in the Texas South Region, which includes San Antonio, are in Table 1. More granular Bexar County data also indicates physician shortages by 2026 (Table 2). Our region and county have projected physician workforce shortages in primary, specialty and subspecialty care.
UT Health San Antonio (UTHSA), with its two major partners, University Health (UH) and the South Texas Veterans Healthcare System (STVHCS), have been the central Graduate Medical Education (GME) pipeline in South Texas and the Rio Grande Valley since 1968. We currently have over 85 GME Programs and over 900 interns, residents and fellows, 55% with funding support from UH and 26% from the STVHCS. We train throughout the city with support from multiple partnerships, including the San Antonio Military Health, Methodist, Baptist and Christus Santa Rosa systems. GME truly is a city-wide collaborative effort. UTHSA was the initial sponsoring institution for the UTRGV launch of GME programs that have now grown to 19 residencies and fellowships. A review of Doximity alumni data demonstrates excellent retention to practice in the region and State (Table 3). Of UTHSA graduates from core resi-
Figure 1: Texas Physician Shortages 2030 By Region2 dency programs, 64% (3301) are located in Texas and 33% (1,716) in the San Antonio area. 36% of UTHSA faculty were trained in our residency and/or fellowship programs. UTHSA is truly the predominant source for physicians in Bexar County. In the last decade, the region has benefitted from the other institutions starting and growing GME positions. Christus Santa Rosa has had a Family Medicine Residency for many years. In partnership with the Children's Hospital of San Antonio, Baylor began a new Pediatric ResTable 1: Texas Health and Human Services South Texas Projected Shortages 20302
idency in 2012 and expanded to a few pediatric subspecialty programs. The Texas Institute for GME and Research (TIGMER) is the GME arm of the University of the Incarnate Word School of Osteopathic Medicine. They now have six accredited programs in Laredo and San Antonio. Methodist also plans to expand GME programs, beginning with an Internal Medicine program in 2023. As crucial as these expansions are for our region, the capacity to train the number and breadth of subspecialists remains a challenge. In particular, many subspecialty residencies and fellowships require a mix of both volume and complex patients, multiple other specialties and subspecialty GME programs, and research expectations with the associated teaching and research faculty typically

Table 2: Bexar County Physician found in larger teaching institutions. Shortages 2026 Even as Texas has been growing the GME pipeline, its population is growing as fast or faster and also aging. Texas has successfully brought in physicians from out of state, partly due to tort reform.4 However, the projected shortages remain despite substantive investment into starting new and growing existing medical schools and GME programs. While state formula funding to the medical schools has stagnated for Undergraduate Medical Education (UME) and GME for many years, the GME state formula funding is about a tenth of the UME funding. This challenges educational institutions that sponsor GME programs as the most significant proportion of GME funding goes to the teaching hospitals. For reasons to follow, the teaching hospitals may not have sufficient funds to support the educational institution's GME infrastructure, such as program directors, coordinators and faculty educational time. Established teaching hospitals have been constrained because the Centers for Medicare & Medicaid Services (CMS) "capped" or froze the number of positions they would pay for at the number of residents and fellow FTEs in 1996. Hospitals are not reimbursed for trainees over these "caps," limiting GME expansion by established teaching hospitals.
Source: SG2 The good news is that the State of Texas and the Federal Government have taken several steps to address the GME funding challenge. The State recognized it must keep as many of the growing number of medical students in the State as possible for GME. Texas routinely ranks in the top 2-3 states, keeping 81% - 83% of physicians who do both UME and GME in the State to practice.2 The desired ratio is 1.1 GME positions for each UME graduate. The Texas Higher Education Coordinating Board (THECB) GME Expansion Program, started in 2013, has been a significant factor in sustaining this ratio and will fund almost 1,400 GME positions each year by July 2023.5 The UTRGV and TIGMER have particularly benefited from this funding due to their fortunate timing of starting new programs that also aligned with the THECB funding priorities for primary care and mental health. However, this funding is under scrutiny for potential cuts each legislative session, mainly since the spending has grown to nearly $100 million annually.6 The other challenge is the GME expansion grants do not address the increasing needs for specialists and sub-specialists. Another GME funding initiative was expanding a Medicaid DME matching program for residents from only the State-owned teaching hospitals to include non-state owned and operated government teaching hospitals.7 Therefore, two new state-lead programs have enhanced GME funding to both the medical schools and teaching hospitals. Beginning in 2016, CMS allowed some hospitals to reclassify to a rural geographic designation, resulting in a 30% increase in their IME "cap" and a substantive increase in CMS funding for GME.8 Additionally, Congress passed landmark legislation in 2021, imple-
Table 3: UT Health San Antonio GME Alumni Practice Locations

menting processes to grow 1,000 new GME positions over five years.9 The number of positions at 200 per year for the nation was not a "landmark" but represented the first time since 1996 that Congress approved increases in the DME "cap." Unfortunately, the implementation process defined by CMS proved unfavorable for us. Finally, new hospitals and hospitals that have not had residents are another potential way to expand CMS-funded GME training positions. As UTHSA opens its Multispecialty Research Hospital, there will be a few new GME programs and positions.10 However, CMS rules limit new funding in new hospitals to only new GME programs, a challenge for UTHSA with 85 GME programs. Therefore, new CMS or State funding for expanding our outstanding, established specialty and subspecialty training has been and will likely remain a challenge.
In summary, UTHSA has had a long history of supplying a substantial portion of the workforce to Bexar County, the region, and the valley, primarily with its two major partners in University Health and the STVHCS. The expansion of GME by TIGMER, UTRGV and others is vital to the region's rapidly growing population needs for primary care. While medical school growth is welcomed, GME growth must keep pace in this region to ensure we meet the healthcare needs of our future. Continued support of the THECB GME Expansion Program, use of new CMS or other identified funding for increasing GME specialty and sub-specialty positions, and capitalizing on starting new GME programs in new hospitals in the county and region will be necessary to meet our future physician workforce needs.
References 1. Association of American Medical Colleges (AAMC) The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. https://www.aamc.org/media/54681/download?attachment 2. Association of American Medical Colleges (AAMC) State Physician Workforce Data Report. https://www.aamc.org/data-reports/workforce/report/state-physician-workforce-data-report 3. Texas Department of State Health Services Texas Workforce Supply & Demand Projections, 2019 - 2030. https://healthdata.dshs. texas.gov/dashboard/health-care-wf/wf-sup-and-demand-proj 4. Berlin J. Coming of Age: Celebrating 15 Years of Texas Tort Reform. Texas Medicine Sept 2018. https://www.texmed.org/Template.aspx?id=48427 5. The Graduate Medical Education (GME) Report: An Assessment of Opportunities for Graduates of Texas Medical Schools to Enter
Residency Programs in Texas A Report to the Texas Legislature per Texas Education Code, Section 61.0661 October 2020. https://reportcenter.highered.texas.gov/reports/legislative/grad-
uate-medical-education-report-an-assessment-of-opportunitiesfor-graduates-of-texas-medical-schools-to-enter-residency-programs-in-texas-fy2020/ 6. Price S. Texas Medicine "Medical Education: Lawmakers invest in
Texas' future." August 2021. https://www.qgdigitalpublishing. com/publication/?m=55178&i=714147&p=40&ver=html5 7. Texas Health and Human Services Supplemental Programs https://www.hhs.texas.gov/providers/medicaid-supplementalpayment-directed-payment-programs/supplemental-paymentprograms 8. Bazakas A. Declassifying the GME Reimbursement Benefits of
Rural Reclassification. January 2018. https://www.ecgmc.com/ thought-leadership/blog/declassifying-the-gme-reimbursementbenefits-of-rural-reclassification 9. Graduate Medical Education Final Rules Published for FY 2022
IPPS AAMC Jan 7. 2022. https://www.aamc.org/advocacy-policy/washington-highlights/graduate-medical-education-finalrules-published-fy-2022-ipps 10. Garcia L. Express-News Exclusive: First look at UT Health San
Antonio's $430M hospital. March 29, 2021. https://www.expressnews.com/news/local/article/Express-News-Exclusive-First-lookat-UT-Health-16059475.php
Woodson “Scott” Jones, MD is Vice Dean, GME & DIO and Professor of Pediatrics at the UT Health Long School of Medicine. He is a member and on the Board of Directors of the Bexar County Medical Society.









