4 minute read
Activities
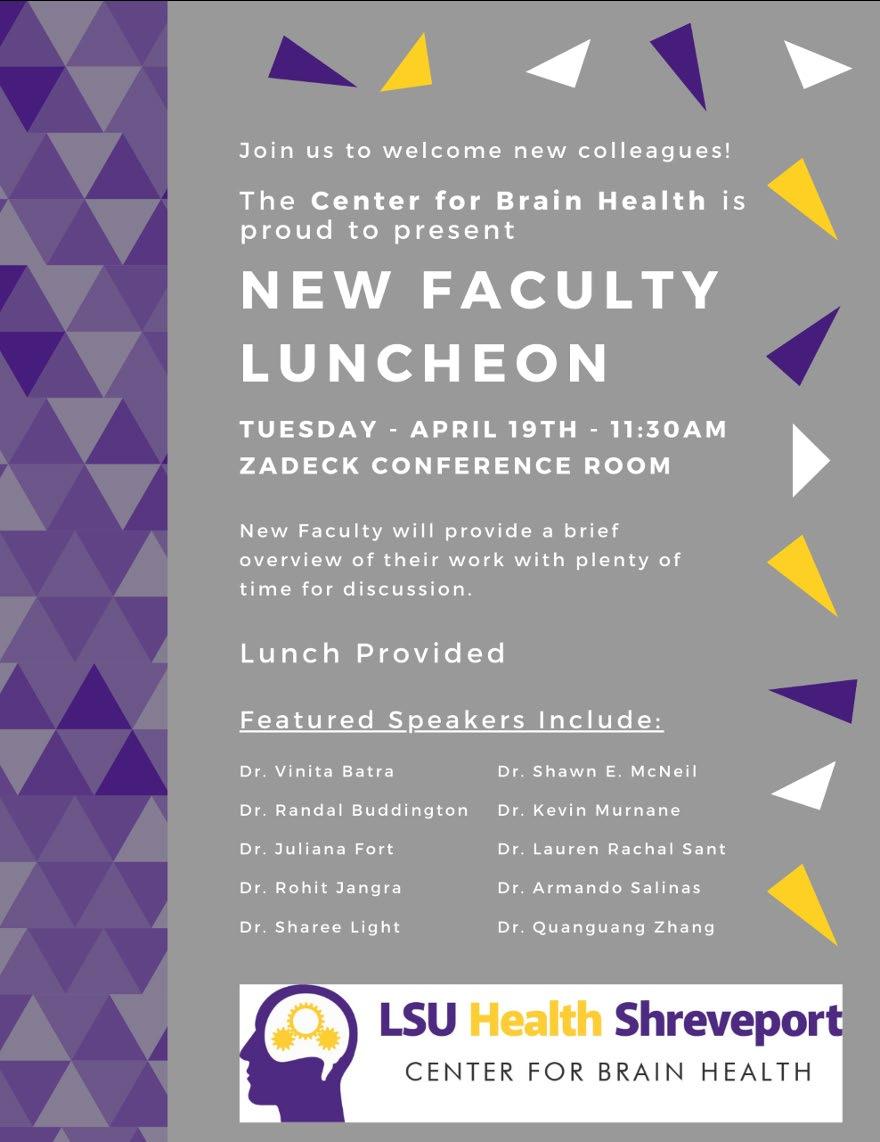
New Faculty Luncheon 2022 Lecture Series
Jun Li, PhD Associate Professor Director of Basic Stroke Research Department of Neurology University of Texas - Houston “Stroke Induced Respiratory Disorder and Cognitive Decline: Influence of Sex and Age”
Advertisement
Srdjan Joksimovic, PharmD, PhD Penn Research Associate Department of Neurology Children’s Hospital of Philadelphia & University of Pennsylvania “T-Typle Calcium Channel in the Subiculum: A New Player in Hippocampal Memory Processing”
Stephen J. Crocker, PhD Associate Professor Department of Neuroscience University of Connecticut School of Medicine “How Aging Impacts Glial Cell Functions and Diseases of the Central Nervous System”
Xiangming Zha, PhD Associate Professor Division of Pharmacology and Pharmaceutical Sciences School of Pharmacy University of Missouri – Kansas City “Brain Acid Signaling and Neuroprotection”
ACTIVITIES
Technology’s Role and Evolution in Neuro-rehab
The concept of “meeting patients where they are” transcends medicine. The idea itself is one of the reasons that compelled many of us to join the medical profession; a field that continues to inspire us all. The transcendence of this concept can be observed in a variety of patients we see as part of the Center for Brain Health’s neurorehabilitation program. Each of these patients has a unique set of rehabilitation needs, and technology can help meet those needs regardless of where patients are on the recovery continuum.
Over time, technology has enabled healthcare professionals to better meet and help their patients make measurable progress. From the minute a patient enters an episode of care to their home discharge, patients move forward with a feeling of confidence that they will meet their personal goals. Advances have been made in technology that allow therapists to meet patients at the very beginning of their rehabilitation journey and assist them throughout the recovery process to achieve better outcomes in a shorter amount of time.
The effect of technology was never more evident than with a recent young patient who needed access to technological advances, and care that was outside the norm in order to get him back to the daily activities of an active boy. Initially, BW was a normal six-year-oldy boy, running and playing like everyone his age until he was diagnosed with Perthese Disease (PD) in November 2019. PD is a disorder of the hip that leads to weakening of the bone and can result in multiple fractures or complete collapse of the femoral head. BW was placed on a nonweight bearing protocol for his right leg in August of 2020 awaiting his first surgery to repair the problem. He required two extensive surgeries over the next 15 months

ACTIVITIES
by specialists in Dallas, Texas, which required him to be non-weight bearing on his right leg for a total of 18 months. He was finally given the green light to start partial weight bearing in December of 2021, with the medical clearance for full weight bearing activities in March of 2022. But because he was so young when all this started, he really didn’t have good working motor memory of what normal walking felt like. He started physical therapy in December 2021, but his family sought our input in June 2022 to assist with his full recovery.
BW walked on his toes on his right leg and had a noticeable limp. However, his legs were the same length and he had normal strength in the muscles of his legs. There was not a structural or functional reason he walked with these impairments. We decided to simply start back with providing him with the normal experience of what normal walking feels like and to assist his muscles to fire when they are supposed to by using our available technology for him to “re-learn” how to walk and run normally. We were able to use our BioNess Neuroprosthetic technology to fire the muscles of his leg in the normal sequence of walking to “re-train” his brain how to do this simple activity. We also used our Vector Gait -n-Safety system to provide body weight support to allow him to walk longer distances and to start to learn the pattern of running before he was ready to run over ground. His surgeon was ecstatic that BW had this technology available to him and was more than pleased with his recovery on subsequent visits back to Dallas for check-ups. We are happy to say BW is back starting the 3rd grade running, swimming, and playing like all kids his age should be able to do.
This was a perfect example of “meeting a patient where they are” and challenging them to progress to where they want to be. We pursued the most aggressive approach possible, while still ensuring BW’s safety, and technology allowed us to assess his limits more easily, while also maximizing his therapy time with appropriate, yet challenging activities that were very important to him and his family.









