

PG. 16-18



PG. 16-18
“Many patients are not aware that the risk of cardiovascular disease is high with lupus.”

Time has a way of slipping by unnoticed, and as I reflect on my own journey, I realize that I have been closely involved with the Lupus Foundation for over 42 years. It’s a cause that has been near and dear to my heart for decades. For the past 16 years, we’ve carried the powerful message, “Have a Heart for Lupus,” especially throughout the month of February. But what does this phrase truly mean, and why has it become such a vital part of our mission?
At its core, the expression “Have a Heart for Lupus” is a call for empathy, kindness, and understanding. Historically, the heart has been seen as the center of all human emotions. A symbol of love, compassion, and warmth. Over the years, this belief has blossomed into countless idiomatic expressions in various cultures, using the heart as a metaphor for the emotional center of our being. It’s a universal symbol of human connection, and it encourages us to act with tenderness and care for one another.
As we embarked on the creation of the first-ever Statewide Lupus Needs Assessment, we reached out to individuals who have lived with lupus, as well as their caregivers. We conducted seven focus groups to gather their insights, and what emerged from these conversations was both enlightening and humbling. One of the most significant lessons we learned from these brave individuals was their overwhelming need for empathy as they navigated their journey with lupus.
Lupus, as many who live with it will tell you, is not always visible to the outside world. The symptoms can be invisible, often leaving those affected looking healthy on the surface while they silently endure a storm of internal battles. This makes the disease particularly challenging to explain and even harder to understand. As someone who has closely witnessed the struggles of lupus patients, it deeply concerns me that so many people still fail to grasp the full scope of what it means to live with lupus. It’s not enough to simply feel sorry for someone who has lupus; what they need - what we all need - is understanding. True empathy that goes beyond mere sympathy. They need compassion, they need to be seen, and they need their challenges to be acknowledged. This is where the heart comes into play. The idiom “have a heart” has long been associated with love, kindness, and positive emotions. It’s a call to action, urging us to show mercy, to extend kindness, and to offer support

where it is needed most. And for those living with lupus, this support is crucial. By “having a heart” for lupus, we are fostering an environment of acceptance, understanding, and love. This is the very essence of our campaigns: to raise awareness about lupus and its far-reaching effects and to inspire a culture of empathy that can help combat the isolation that so many lupus patients feel.
Despite its prevalence, lupus remains one of the most misunderstood chronic diseases. In Ohio alone, more than 60,000 individuals are living with lupus, often without the understanding or support they desperately need. They can feel isolated, misunderstood, and at times, invisible in a world that doesn’t fully comprehend their struggle. This is why our message is so important: “Have a Heart for Lupus” is not just a campaign; it is a movement. It is a reminder that showing empathy is one of the simplest yet most powerful ways we can support those living with this challenging disease.
If you know someone with lupus, I urge you to reach out. Extend a hand, offer a listening ear, and show that you care. In the face of a disease that often leaves individuals feeling alone and misunderstood, your compassion can make all the difference. Support, empathy, and kindness are invaluable gifts that we can give to those who need them most. We can spread awareness, foster understanding, and ensure that no one has to walk this journey alone, together. Let’s “Have a Heart for Lupus”, and in doing so, let’s make the world a little brighter for those who need it most.

Suzanne Tierney President & CEO
Lupus Foundation of America, Greater Ohio Chapter
Pg. 1-2 Letter from Suzanne
Pg. 4-5 Patient Navigator Corner: Feb 2025
Pg. 6-9 Patient Story: Patricia M. Lyons
Pg. 10-13 Research and News
Pg. 14-15 Upcoming Walk to End Lupus Now®
Pg. 16-18 Lupus and the Heart by Heba Wassif, MD, MPH, FACC
Pg. 19-21 Heart Healthy Tips for People With Lupus
Pg. 22 Blog & Podcast
Pg. 23-24 Get Involved & Ways to Give
Pg. 25-27 Love as Medicine
Pg. 28-29 Could You Have Lupus?
Pg. 30 Staff Page
2527 1921 Heart Healthy Tips For People With Lupus Love as Medicine 6-9 Patient Story: Patricia M. Lyons 1618 Lupus and the Heart By Heba Wassif, MD, MPH, FACC




The Patient Navigator program is funded in part by an earmark from the State of Ohio and managed by the Ohio Department of Health.
Welcome back to the Patient Navigator Corner! Whether you are a lupus warrior or caregiver who is new to the chapter or if you have been with us for years, you are the heart of everything we do! ��
As our mission statement says: “The Lupus Foundation of America, Greater Ohio Chapter is dedicated to improving the quality of life for all people affected by lupus through programs of research, education, support, and advocacy.” All of us at the LFA, GOC work hard to fulfill our mission. Patient navigators do this by providing education and information and connecting lupians and caregivers to our services. Some of these services include:
Twice a year, patient navigators call and/or email all lupus patients, to check in and see how you are doing. If you have questions about lupus or have specific needs that can be benefitted by the chapter’s services, the patient navigators will provide information and assistance by phone, email, or mail. If we do not have information or cannot provide a service, then we research other agencies and organizations that may be able to help.
We produce a variety of educational programs. Our New Patient Education class meets virtually on the
third Wednesday of every month. This is a basic “lupus 101” class. Anyone interested, including caregivers and those who have been diagnosed for years, may attend. The class covers what lupus is, what causes lupus, who develops the disease, how it is diagnosed and treated, and how to manage it. It also introduces our chapter and services. Use this link to register: bit.ly/3Pd880v
We also produce several educational summits throughout the year. These in-person and virtual conferences are wonderful opportunities to learn from lupus experts on a variety of topics. Watch for details on our next virtual summit on March 22, 2025. Tentative topics include Making Medications Work, Musculoskeletal System and Pain Management, and Reducing Flares in Lupus.
We have an archive of video recordings of past summits. To search and view past summits, please visit our youtube page: https://bit.ly/4g9v2j5
Lupians and caregivers often feel alone in their lupus experience and do not have the opportunity to share their feelings and challenges with other lupians. Our support groups are a great way to connect with others, learn more about lupus, and share how to manage life with the disease. Patient navigators can recommend the groups
that meet in-person nearest to you and/or call in or virtual support groups. (By the way, many of our patient navigators are support group facilitators too!) To view our support groups, check out our Upcoming Events calendar: bit. ly/3NfLK5i
Research has shown that non-medical factors, such as socioeconomic status and geographic locations can affect health and health outcomes. These factors are called social determinants of health, and lupus patients may have barriers to caring for their lupus. In order to address these potential barriers to care, we have received grant funding from the State of Ohio to provide assistance for out-of-pocket healthcare expenses, food assistance, transportation to healthcare appointments, and mental health counseling in partnership with Signature Health. Patient navigators provide details of these programs and distribute a needs assessment form, which must be completed for eligibility.
Our physician directory is a great resource for those who are looking for a physician to diagnose and treat lupus. The directory lists physicians in Ohio who have told us that they treat lupus patients and want to be included in our directory. It does not include all physicians in the state who treat
lupus, nor do we recommend specific physicians; but it is a good starting point.
There are many different ways patient navigators provide assistance and to help lupus patients and caregivers - the heart of everything we do! Please contact the office at 1 (888) NO-LUPUS, (888) 665-8787, (440) 717-0183 or email us at info@lupusgreaterohio.org. You may also contact your regional patient navigator directly. We’d love to hear from you!
President & CEO - Suzanne Tierney Suzanne@LupusGreaterOhio. org
Lead Patient Navigator & Outreach CoordinatorRita Piccin, BS, ND, RN Rita@LupusGreaterOhio.org
Greater Cleveland - Halli Martin Halli@LupusGreaterOhio.org
Northwest Ohio - Aaron Meller, PTA Aaron@LupusGreaterOhio.org
Northeast Ohio - Brenda Angle and Renee Lyons Brenda@LupusGreaterOhio.org Renee@LupusGreaterOhio.org
Eastern Ohio - Lisa Breiding Lisa@LupusGreaterOhio.org
Western Ohio - Mike Vollmar, LSW, and Justina Patterson Mike@LupusGreaterOhio.org Justina@LupusGreaterOhio.org
Central Ohio - Samantha Sebestinas
Samantha@LupusGreaterOhio. org
Southwest Ohio - Allison Fedon and Nikki Roberts Allison@LupusGreaterOhio.org Nikki@LupusGreaterOhio.org
Southeast Ohio
Info@LupusGreaterOhio.org
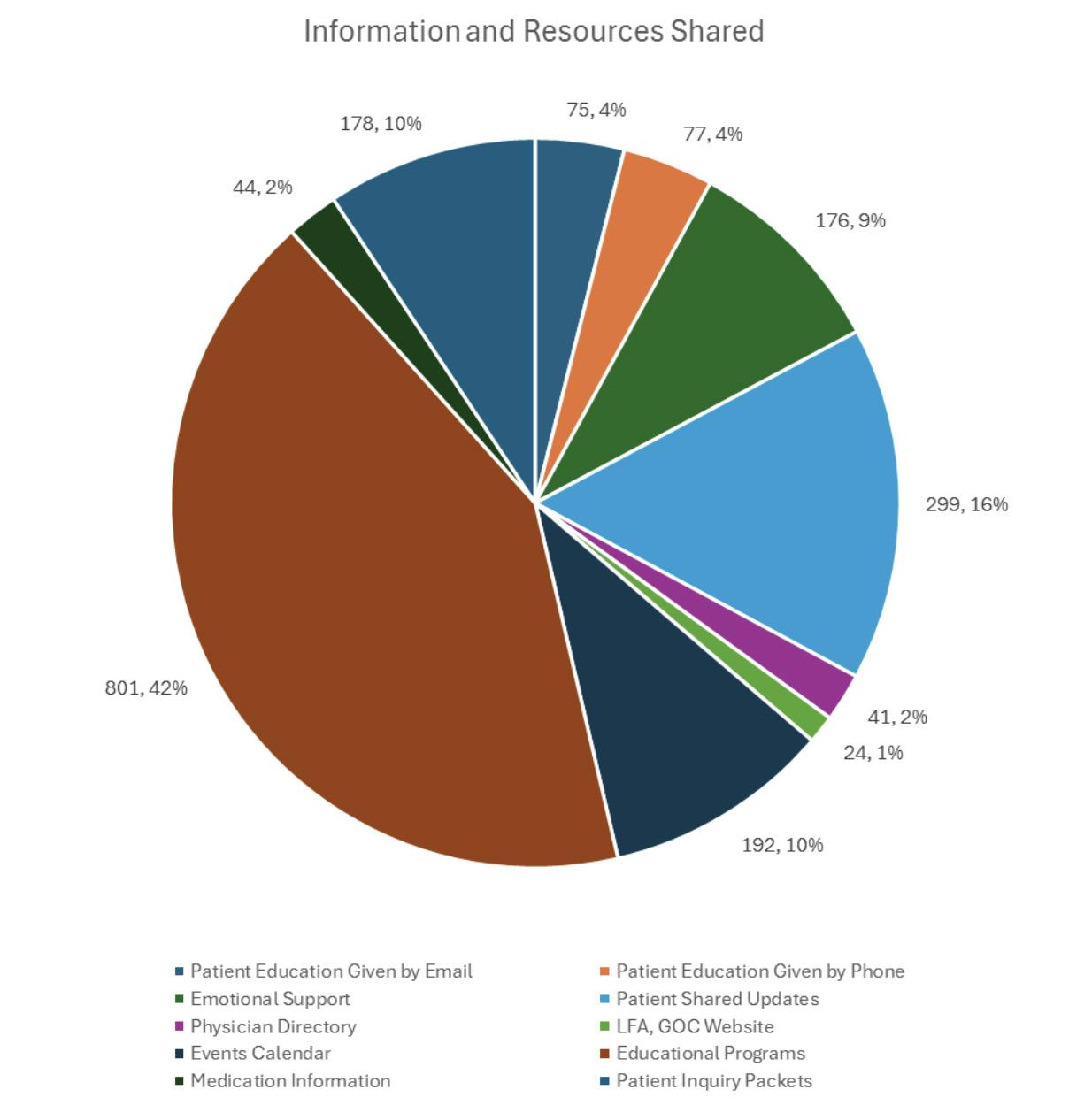
Correction to Patient Navigator Corner, November, 2024, Issue 19, page 4 - due to a technical issue, the “Information and Resources Shared” graph showed incorrect information. The issue has been resolved and the following graph displays the corrected information:

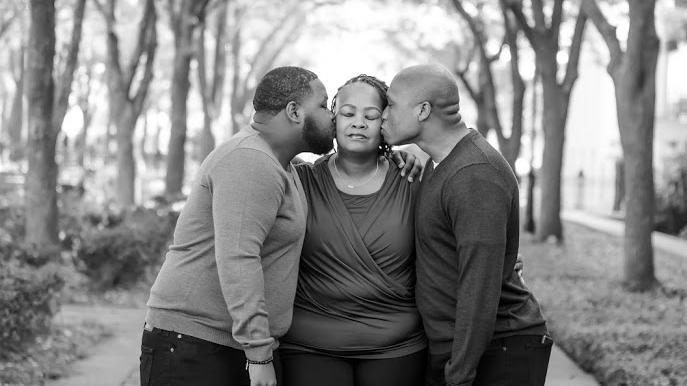
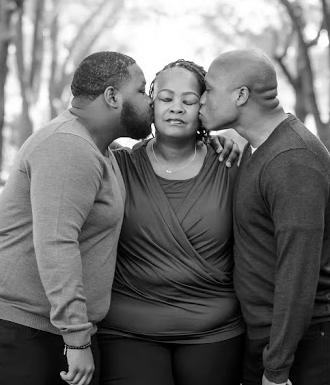
My name is Patricia M. Lyons, and I want to take a moment to share with you the struggles and triumphs that I experienced living with Systemic Lupus Erythematosus (SLE). Although it has been a difficult journey, I am blessed to have a great support system and with my resilience, I continue to conquer each day with determination. As a Black woman, I remember a time when I never had to take a pill for my daily health regimen. Considering that I am a part of a community where most of my Black female friends and family members were on medications for various health issues, I was proud that I was not one of them. Well, that unexpectedly changed....
I was diagnosed with SLE in October 2010. I had no idea what was happening as I had been ill for a little over a month. At the time, I was living in Florida, far away from most of my family in Ohio. It was my two sons and I and my oldest son had just graduated high school in June 2010 and was heading off to college in August. I was feeling “weird”, and I knew that something was wrong. My face was constantly burning across
my nose, which got worse when I would sweat, and my chest hurt when I took a deep breath, and at times, it felt like I was gasping for air. I remember my brother telling me that my face was red but that was not new to me as my face was always red.... but he said, “no, it’s redder than it’s ever been”. Shortly after, I returned home to Florida. I was having trouble laying down to sleep and eventually, went to my primary physician and she immedi-
By: Patricia M. Lyons
ately admitted me into the hospital and ran an EKG test. After five (5) long and stressful days of tests after tests, I was told that I had SLE. I remember crying myself to sleep that night, and many nights after.
One of the most difficult aspects of living with SLE is first and foremost, accepting your fate because it was a new normal for me. Learning about this chronic autoimmune disease meant that I had to accept

the unexpected and learn how to manage the unpredictability of flare-ups and not feeling well. This took both a mental and physical toll on me. There were days when I felt like I could not explain what was wrong as I was fighting an invisible and unknown battle. The amount of pain and fatigue that I felt was insufferable and the weight of carrying this chronic illness often made me feel alone. I was faced with many challenges, such as joint pain, fatigue, and skin rashes and on top of that, I had to be a mother to my two sons. I would be exhausted by the end of the day, which oftentimes became overwhelming. I eventually thought it would be best to move back home to Ohio where I had a larger support system.
Upon moving back to Ohio, I learned about The Lupus Foundation of America, Greater Ohio Chapter. There, I met other lupus patients and advocates, and I learned how to better manage my SLE. I learned how to obtain patient assistance for medication costs, attend monthly patient

meetings, and attend various events, such as the Cleveland Walk to End Lupus Now®. I actively participated in lupus awareness events and support groups, where I shared my feelings, experiences, offered advice, and connected with others who understood what I was going through. I even traveled to our state capital in Columbus, Ohio to advocate to our senators for lupus support and research funding. Being a part of the Lupus Foundation really helped me to come to grips with my diagnosis and reminded me that I could still live a happy life. I began living every day to the fullest by accomplishing as much as I could,

learning all I could about SLE, and not letting the threat of the bad days steal my joy. I have learned to pace myself, listen to my body, while continuing to advocate for myself.
On another note, living alone is an absolute bummer! My oldest son is a member of the United States Coast Guard so, he lives far away and although my younger son lives close, one of the hardest aspects of my daily life is the burden of self-care as a single person. Managing lupus requires a great deal of responsibility, and I must stay on top of it. Flare-ups are very unpredictable and it’s difficult to care for myself when I don’t feel well nor have a partner or close family member in the household with me to help. I often must rely on my own strength and determination to get through these tough times. The emotional toll of having to manage everything alone can be just as exhausting as the physical; however, I continue to push forward. I am learning how to reach out more - to my son, other family members, and friends when I need help. The journey is never easy, but I will continue fighting because I am not defined by my diagnosis. I will continue to move forward and advocate for myself because I have lupus – lupus does not have me!
As a young child, I vividly remember feeling that death loomed over us when my mother shared her lupus diagnosis with my brother and me. Watching my mother navigate this chronic illness has been both inspiring and heart-wrenching. Growing up with a mother who has lupus presents unique challenges that reshape family dynamics and personal growth.
To this day, the daily challenges we endure manifest in multiple ways: unpredictable flare-ups that disrupt family routines; bearing witness to her physical pain while feeling helpless; additional household responsibilities becoming necessary from an early age; facing healthcare system biases against Black patients; and the constant struggle to balance personal responsibilities with caregiving duties.
In the Black community, mothers traditionally serve as the family’s foundation. The intersection of racial health disparities and chronic illness compounds the difficulty of watching my mother navigate these cultural expectations while managing lupus. Not only is this expected from the mother, but it also expected from the son to be the man of the house if there is no other male present. This cultural context creates additional pressure on both my mother as the patient, and myself as the caregiver. Our traditional roles and expectations must be continuously negotiated and redefined.

Despite these challenges and expectations, the experience has yielded significant positive outcomes. From the development of strong empathy, early acquisition of essential life skills, strengthening of mother-son bonds through shared adversity, and a deeper appreciation for health and resilience,
these outcomes have shaped my character and worldview in profound ways. It always makes me question not only how I treat others, but also how I treat myself. In the same token, the experience creates a complex emotional landscape characterized by guilt over pursuing personal goals. While
“Watching my mother navigate this chronic illness has been both inspiring and heart-wrenching.”
my mother needs support, there’s persistent concern for her health, and the constant challenge of providing emotional support while processing personal feelings. This duality of roles—being both a son and a caregiver—creates a unique psychological burden that only a select few can fully grasp.
This journey of lupus illuminates the significance of patience, the power of family bonds, and the necessity of self-care while caring for others. It represents an ongoing process of balancing love, duty, and personal development, teaching valuable lessons about resilience and adaptation in the face of chronic illness. My mother is a strong woman who beats lupus each day she wakes up. I only hope and pray to emulate that same strength.

Long-term use of glucocorticoids (GCs) for the treatment of lupus is very common, however, it has also been associated with side effects like high blood pressure, diabetes, infection, and osteoporosis. A new study found that low or absent disease activity, hydroxychloroquine (HCQ) use, and gradual reduction of GC dosing can minimize flare risk and support the successful discontinuation of GCs in individuals with systemic lupus erythematosus (SLE).
In this multi-center, retrospective study, a cohort of 324 people with active SLE receiving GCs as part of
their treatment plan were analyzed. A special focus was given to 220 people within the cohort who discontinued GC use. Researchers found that their risk of disease flare lowered when GC treatment was suspended when their disease was in remission. Their risk further reduced with each additional month their disease activity remained low, and total and severe flares were prevented in those taking HCQ. Overall, the combination of disease remission, HCQ use, and slow GC tapering reduced the likelihood of severe flare activity by as much as 50 times compared to participants who continued GC therapy.
While discontinuing GCs can reduce damage and improve outcomes, close monitoring is required to prevent relapses. Talk to your doctor before making any changes to your treatment plan.
Learn more about medications used to treat lupus: https://bit.ly/4heXOQw

The Phase 1 GALLOP study evaluating investigational therapy, CB-010, for treatment of lupus nephritis (LN) has officially started. This open label, multicenter study will assess a single infusion of CB010 in adults with LN, including those with extrarenal lupus (ERL, when LN symptoms affect other parts of the body). The researchers will provide updates as the study advances.
CB-010 is a CAR-T cell therapy designed to target CD19, a protein on B cells that contributes to autoantibody production and lupus disease activity. To make
CAR-T cells, scientists create or engineer new cells called chimeric antigen receptors (CARs), and then introduce T-cells into them. CB-010 targets CD19, a protein found on the surface of B cells and produces autoantibodies and uses a person’s own immune T-cells. CB-010 also features a unique modification that removes the PD-1 protein, which helps boost its performance in targeting lupus-affected cells. Additionally, the GALLOP study includes a partial human leukocyte antigen (HLA) matching process, which could improve how well the treatment works. The U.S. Food and Drug Administration (FDA) has
granted CB-010 Fast Track designation, recognizing its potential as an innovative treatment for lupus that is difficult to manage.
Continue to follow the Lupus Foundation of America for updates on lupus drug developments and clinical trials.
Learn more about treatments being studied for lupus:
https://bit.ly/4gZNRX6



In a new study published in Lupus Science & Medicine, researchers reviewed randomized clinical trials (RCTs) to assess therapies for initial management of lupus nephritis (LN), focusing on their design with study populations and outcomes, examining the results and identifying gaps that should be addressed in the future.
Researchers reviewed 61 RCTs published between January 2000 to February 2024 which included 124 treatment groups and involved 7,058 study participants. Each RCT group was evaluated separately and was categorized
based on treatment regimen, to include mycophenolic acid analogues, mycophenolate mofetil (MMF), cyclophosphamide (CYC), calcineurin inhibitors (CNI), belimumab (Benlysta), B-cell depleting therapies, and other biologic treatments. Nearly 90% of all RCT participants were female. Asian was the most represented race (55.2%), followed by White (28.4%), while Black (7.2%) and other racial groups (9.2%) were under-represented.
The study emphasizes the importance and need for greater diversity and inclusion of under-rep -
resented populations in clinical trials, particularly Black individuals, who are more severely impacted by lupus nephritis. It also underscores the importance of using consistent and standardized study designs.
Learn more about participating in clinical trials: https://bit.ly/3WxWEYk

Neutropenia, a condition characterized by low neutrophil levels, is common in individuals with systemic lupus erythematosus (SLE) and can lead to severe infections. A new study investigates the role of Krüppel-like factor 2 (KLF2, a protein coding gene involved in a variety of regulatory pathways and plays a role in controlling inflammation) in regulating neutrophil apoptosis (cell death) and its connection to disease activity in people with SLE.
The study included 155 participants: 68 with SLE, 57 disease controls (29 with rheumatoid arthritis; 26 with Sjogren’s Syndrome), and
30 healthy controls. Researchers collected blood samples from each study participant, separated neutrophils, , and analyzed their rates of apoptosis.. They found that people with SLE had blood neutrophil counts that were significantly reduced, which was inversely linked to the SLE disease severity. The findings suggest that KLF2 in neutrophils may be closely related to the development and progression of SLE. The correlation between KLF2 and neutrophil apoptosis suggests that the decline of KLF2 levels may lead to neutropenia in people with SLE.
This is the first study to show that
KLF2 can regulate the apoptosis of neutrophils. Further research is needed to provide insights into the detailed mechanisms leading to the occurrence and development of SLE. Additionally, this study highlights the potential of KLF2 in autoimmunity and as a therapeutic target.
Learn more about lupus and inflammation:
https://bit.ly/42hAU6C



OH - 05/03/2025
OH - 05/03/2025


By Dr. Heba Wassif, MD, MPH, FACC

When Grace walked into my office after her heart attack at age 45, she was concerned as she was not a smoker, with no history of diabetes or hypertension. She considered her family history, but both her parents were alive and well. We talked about her experience and what it meant to her life choices and ability to move on. I noticed that she had been experiencing joint pains and hair shedding for some time, which she downplayed as being due to her responsibilities towards her family and her daughter. I recommended that she be seen by a rheumatologist. She was diagnosed with lupus and for me it all made sense. Although Grace

may not have had the traditional risk factors, her body had been subjected to inflammation from lupus. This was likely the main driving force behind her heart attack.
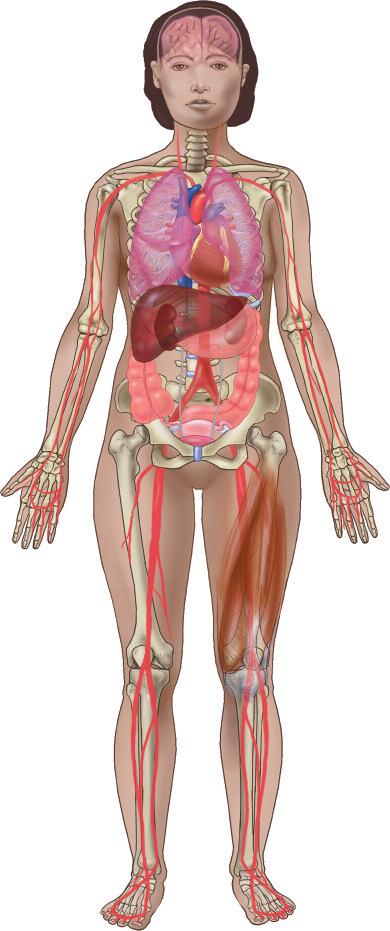
A 13th-century physician named Rogerius Frugardi is credited with using the term “lupus” to describe the facial lesions associated with the disease. Lupus, an autoimmune disorder, is often known as “the great imitator” because it can resemble and mimic many other diseases and conditions. The number of new cases is difficult to assess, but it is estimated at 16,000 every year in the United States. There are approximately 1.5 mil-
lion people living with lupus in the United States, mostly women. Not all women are affected in the same way. African American, Hispanic, Asian American and Native American/Pacific Islander women are disproportionately affected compared to other populations, with increased morbidity and mortality. Lupus occurs in black people 2-3 times more frequently than in nonblack people, with higher rates of hypertension and lupus nephritis. Black patients have a higher risk of developing cardiovascular disease at a young age, 19 times higher than non-blacks in the first 12 years after diagnosis. This can partially be explained by the disease
Heba Wassif, MD, MPH, FACC is a clinical cardiologist , Director of CardioRheumatology Director and Inpatient Clinical Cardiology in the Tomsich Family Department of Cardiovascular Medicine, Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute. She is also faculty at the Cleveland Clinic Lerner College of Medicine and participates in resident and fellow education. She is core faculty for internal medicine residency and cardiology fellowship programs. She is also a member of ACC cardiorheumatology work group and an active member of ACC. Dr. Wassif sees patients at Cleveland Clinic Main Campus.
severity and higher prevalence of risk factors.
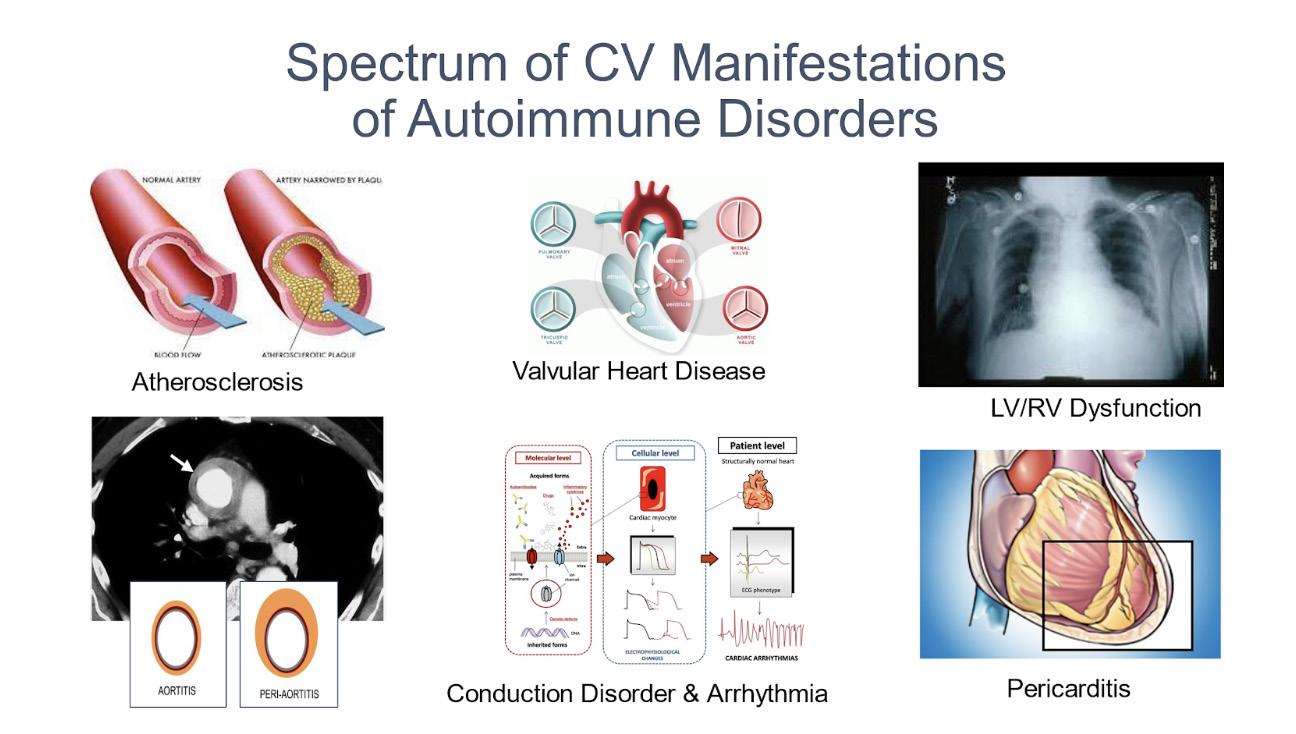
Many patients are not aware that the risk of cardiovascular disease is high with lupus. In recent years, we have come to know that atherosclerosis (the underlying process leading to heart attacks) is related to inflammation. In the presence of autoimmune conditions such as lupus, some of these pathways are accentuated in addition to other non-mutual pathways. A patient with systemic lupus erythematosus (SLE) has three times the risk of cardiovascular disease compared to a person without lupus. The concept of “accelerated atherosclerosis” is critical when treating a patient with the disease. Multiple traditional cardiovascular risk assessment tools such as the Framingham risk score consistently underestimate the risk in lupus patients. There are attempts to develop risk scores that would determine the risk more accurately, but none are currently recommended.
Lupus’ cardiovascular risk is not limited only to the blood vessels of the heart (coronary arteries) but can affect any part of the heart including the heart muscle, valves, and the outer lining of heart. Inflammation of the heart muscle is rare but what is more common is heart failure. It is estimated that up to 10% of lupus patients suffer from some form of heart failure. In many of these conditions, the underlying case is hypertension or coronary artery disease. The lining around the heart muscle called the pericardium is affected in over 50% of lupus patients, but most of these cases of valve disease are asymptomatic.
The next logical question for a lupus patient is how to mitigate the risk of cardiovascular events. As health care providers, we need to discuss general lifestyle with all our patients including patients with lupus who tend to be younger. In patients with lupus, lower levels of blood pressure are associated with lower rates of
cardiovascular events with a goal <130/80 mmHg. Higher levels of total cholesterol and low-density lipoprotein cholesterol have been associated with a higher risk of MI and stroke in SLE. There is some evidence that patients with SLE treated with lipid-lowering agents have a significantly lower risk of coronary artery disease during follow-up (mean 8.4 years) than those not treated. Moreover, shortor long-duration statin use are both associated with a lower risk of stroke. However, the diagnosis of SLE is not the only criterion for prescribing lipid-lowering treatment for primary cardiovascular prevention.
Controlling lupus symptoms not only affects your quality of life, but is also a key component in reducing cardiovascular risk. Hydroxychloroquine, a medication commonly used for the treatment of lupus, has been suggested to reduce cardiovascular risk, although this information may be biased as patients only on hydroxychloro -

quine usually have low disease activity. By contrast, steroids increase risk and most providers and society guidelines would recommend the lowest possible corticosteroid dose to minimize risks of cardiovascular harm.
Calcification is an early risk identifier of atherosclerotic plaque burden and is a hallmark sign of advanced atherosclerosis. You may have heard of the coronary calcium score (CAC) that is used as an additional tool for risk. Individuals living with lupus tend to have
higher calcium scores, making this a useful screening tool for coronary artery disease even in younger patients. There are caveats, as atherosclerosis is sometimes associated with non-calcified plaques. Novel methods for assessing coronary inflammation by CT imaging are emerging, for example, the peri-coronary fat attenuation index. These may find an important role in detecting early coronary artery disease in the future.
Your routine visits to your rheumatologist associated with good his-
tory and physical exam is the first step in determining your risk and further imaging with the coronary calcium score or a cardiac echo. This would assist your rheumatologist to determine if cardiology referral is needed. The emerging field of cardio-rheumatology highlights the collaboration between cardiologists and rheumatologists in managing patients with lupus and cardiovascular diseases. Stay healthy and in touch with your doctor.
References: Lupus facts and statistics. Lupus Foundation of America. https://www.lupus.org/resources/lupus-facts-and-statistics
Mortality and causes of death in systemic lupus erythematosus over the last decade: Data from a large population-based study. Zen, Margherita, et al. European Journal of Internal Medicine 2023:112,45 - 51. https://www.researchgate.net/publication/368407651_Mortality_and_causes_of_death_in_systemic_lupus_erythematosus_over_the_ last_decade_Data_from_a_large_population-based_study
Patients with SLE have higher risk of cardiovascular events and mortality in comparison with controls with the same levels of traditional risk factors and intima-media measures, which is related to accumulated disease damage and antiphospholipid syndrome: a case–control study over 10 years. Ajeganova, Sofia, et al. Lupus Science & Medicine 2021;8:e000454. https://lupus.bmj.com/content/8/1/e000454
Computed tomography (CT) calcium scoring in primary prevention of acute coronary syndrome and future cardiac events in patients with systemic lupus erythematosus. Wu, Michael, et al. PMC - PubMed Central (PMC). Cureus. 2023 Oct 16;15(10):e47157. https://pmc.ncbi.nlm.nih.gov/articles/PMC10653626/

People with lupus are at higher risk of developing cardiovascular problems, including heart disease. Lupus can increase the risk of heart disease in several ways. Chronic inflammation, a hallmark of lupus, contributes to the development of atherosclerosis (plaque buildup in the arteries), which can lead to heart attacks and strokes. Additionally, some medications used to treat lupus, such as corticosteroids, can increase blood pressure and cholesterol levels, further raising the risk of cardiovascular complications. People with lupus are also more likely to have other conditions, such as high blood pressure, diabetes, and kidney disease, which can contribute to poor heart health.
Given these increased risks, it is crucial for individuals with lupus
to take proactive steps to protect their heart. A combination of healthy lifestyle choices, regular monitoring, and collaboration with healthcare providers can make a significant difference.
Eating a balanced diet is one of the most effective ways to promote heart health. For those with lupus, focusing on anti-inflammatory foods can also help manage the disease itself. Consider the following dietary guidelines:
• Eat plenty of fruits and vegetables: These foods are rich in antioxidants, vitamins, and fiber, all of which support heart health and help fight inflammation. Aim for a variety of colors on your plate to ensure you’re getting a wide range of nutrients.
• Choose whole grains: Foods like brown rice, quinoa, and oats provide fiber, which can help lower cholesterol, and control blood sugar levels. Whole grains are also linked to a lower risk of cardiovascular disease.
• Include healthy fats: Omega-3 fatty acids, found in fatty fish like salmon and mackerel, flaxseeds, and walnuts, can reduce inflammation and improve heart health. It’s also important to replace saturated and trans fats, commonly found in processed foods, with healthier fats like olive oil and avocado.
• Limit salt intake: Excessive sodium can raise blood pressure, which is already a concern for many people with lupus. Reducing salt intake can help keep
blood pressure levels in check. Opt for herbs and spices to season food instead.
• Moderate protein intake: While protein is an essential part of the diet, people with lupus should be mindful of their kidney function. It’s essential to consult with a healthcare provider or dietitian to determine an appropriate amount of protein.
2.
Exercise is crucial for managing both lupus and heart health. Physical activity can help improve circulation, reduce inflammation, and manage weight, all of which reduce the strain on the heart. Regular exercise also helps manage other risk factors, such as high cholesterol, high blood pressure, and diabetes.
However, it is important for people with lupus to find a level of activity that is suitable for their condition. For those with joint pain or fatigue, low-impact exercises like swimming, walking, yoga, and cycling can be great options. Be sure to listen to your body and avoid overexertion. Consulting a healthcare provider or a physical therapist can help develop an exercise routine that is safe and effective.
3.
Chronic stress can elevate blood pressure and lead to other negative health outcomes, including heart disease. Living with lupus itself can be stressful, so finding ways to manage stress is crucial for both physical and mental health. Effective stress management techniques include:
• Mindfulness and meditation: These practices can help calm the mind and reduce stress, improving overall well-being.
Even a few minutes of deep breathing can make a significant difference.
• Adequate rest: Proper sleep is essential for managing stress and supporting heart health. Establishing a regular sleep routine and creating a calming bedtime environment can improve the quality of sleep.
• Support network: Connecting with others who understand your experience, whether through lupus support groups or close friends and family, can help you navigate the emotional
challenges of the disease.
4.
It’s essential to regularly monitor your heart health and keep track of any risk factors that could contribute to heart disease. People with lupus should have their blood pressure, cholesterol levels, and blood sugar checked regularly. Keeping these numbers within a healthy range can prevent the development of cardiovascular issues.
If you have high blood pressure,

high cholesterol, or diabetes, working with your doctor to develop a treatment plan is essential. Lifestyle changes, along with any necessary medications, can help keep these risk factors under control.
5. Medications and Medical Management
People with lupus often take medications like corticosteroids, which can increase the risk of heart disease by raising blood pressure and cholesterol levels. It’s important to discuss any concerns about medications with your healthcare provider. They may adjust dosages or recommend alternatives to minimize the risk to your heart.
In some cases, additional medications may be needed to control blood pressure, cholesterol, or other heart disease risk factors. Regular check-ups with a healthcare provider can help ensure that both lupus and heart health are being effectively managed.
For people with lupus, protecting heart health is crucial in managing the disease and reducing the risk of complications. Adopting a heart-healthy diet, exercising regularly, managing stress, and monitoring risk factors can significantly improve quality of life and long-term outcomes. By working closely with healthcare providers
and making informed lifestyle choices, individuals with lupus can reduce their risk of cardiovascular problems and improve their overall health.
Disclaimer:
The information provided in this article is for general informational and educational purposes only and is not a substitute for your physician’s advice. Please consult your physician regarding your personal medical situation.



If you would like to share your story, or have a topic you think would benefit lupus patients, contact our show’s producer Alex by email: Alex@lupusgreaterohio.org
Check out our channel: @lupusgreateroh
Episode 42 - Roberta & Jessie - Mother and Daughter Fighting Together
Roberta and Jessie sat down with Suzanne just after the Cleveland Walk To End Lupus Now.® This mother/daughter duo have an amazing story that we thought was fitting to share during the holiday season.
Episode 43 - From NY to NEO - Meet The Newest Member of the LFA, GOC
Join us for this winter break edition of My Lupus Living Room as we get to know Chris, the newest member of the LFA,GOC Team! Chris is our events assistant. He moved from Long Island, New York, to help us with educational programs, our walks, and everything in between!
Our blog, Lupus Night Light, is a place where we share stories and practical advice from patients that they have learned along their lupus journeys. You will find stories of triumph, hardship, and everything in between. It is meant to be a cathartic journey for both the contributors and readers alike.

Stay up-to-date on everything we’re doing by joining our mailing list. You will receive a monthly newsletter, support group reminders, Walk to End Lupus Now® updates, research news, and more. Sign up now: lupusgreaterohio.org/stay-informed
Text “NOLUPUS” to 833-4490800, complete your contact information, and be sure to opt in to receive important lupus updates directly to your mobile device.
Join us on our social media platforms to stay connected: lupusgreaterohio.org/stay-informed/ get-social
Instagram.com/lupusgreaterOH
Facebook.com/lupusgreaterOH
Twitter.com/lupusgreaterOH
One-year: $25 Lifetime: $200 lupusgreaterohio.org/get-involved
Do you have an idea to support the mission? Give us a call at the office to discuss and plan your own fundraising activity to benefit the LFA, GOC. Here are a few examples of virtual events that people have coordinated in the past: Pampered Chef Party, Online Auction, Charity Video Game Tournament.
If you are interested in hosting a third-party event, reach out to us for our official guidelines and an application.
Each year, the National Lupus Advocacy Summit brings together the lupus community to pursue a collective vision of a world without lupus. In addition, we help to ensure
there is a cohesive voice heard in Washington, D.C. that ensures the lupus agenda is at the forefront of the legislature. This year’s National Lupus Advocacy Summit will take place May 4-6, 2025 in Washington, DC. If you are interested in participating, please visit lupus.org for more information.
We invite you to register to be a lupus advocate in Ohio. Our current initiative is to keep lupus in the state budget for the new biennium. Much of the educational and support programming produced by the LFA, GOC over the past two years has been a direct result of the funding provided by the state of Ohio and the Ohio Department of Health. It is imperative that we let Ohio’s leadership know the importance of keeping lupus in the public health agenda. lupusgreaterohio.org/ get-involved/advocate
Traditional
• Checks
Please make checks payable to the Lupus Foundation of America, Greater Ohio Chapter, and mail them directly to:
12930 Chippewa Road, Brecksville, Ohio 44141.
• Credit Card + PayPal
Fill out the online donation form or call the office.
• Facebook Fundraisers
• Instagram Stories
In Honor of
• Memorial Donation
• Tribute Donation
Your Job
• Employer Matching Gift Program
Ask your employer if they match charitable contributions made by their employees.
• Combined Federal Campaign CFC #51890
• Stock or Other Securities
• Life Income Plans Pooled Income Fund Charitable Remainder Trusts
• Creating Healthier Communities CHC #9963
• United Way Campaigns
Other
• Donatestuff.com
Schedule a donation pickup of your gently used goods and pick the LFA, GOC as your charity.
• Leave a Bequest
You can include the LFA, GOC in your will to support the mission beyond your lifetime.
• Give the Gift of Life Insurance
Name the LFA, GOC as a sole or partial beneficiary.
For more information on ways to give, please visit: lupusgreaterohio.org/get-involved/ donate or call our office at 1 (888) NO-LUPUS.
By: Adrienne Rice-Fernandez

It is often said that love is the best medicine. This is evident through a mother’s care in the earliest stages of life. Who do we turn to when we aren’t feeling well? For most of us, it is our mom. For others, it may be a romantic partner, a friend, or relative. Love impacts every aspect of our lives. It helps establish relationships and meaningful connections. But most important, it brings fulfillment.
As lupus patients, we know what needs to be done to prolong life and stay healthy. Reduce stress, quit smoking, avoid sun exposure, exercise, eat healthy, and get plenty of sleep. The list goes on!
But have we considered that love and our social relationships have a positive impact on our health?
It is becoming more evident that love has many health benefits. It reduces stress and anxiety, lowers
blood pressure, makes us more resilient, and increases life expectancy. Love is also reported to lower pain levels, which is key for lupus patients.
Studies have consistently shown that those with stronger social relationships (romantic or otherwise) have longer survival. A study by the American Heart Association reports that social isolation is linked to a 29% increased risk of heart disease and a 32% higher risk of stroke1. The benefits of living longer have even been linked to our relationships with companion animals. A meta-analysis published in Circulation: Cardiovascular Quality & Outcomes reported a 24% decreased risk of mortality (all causes) among dog owners2.
Another benefit of strong relationships is better recovery after surgery and other health proce -
dures. Caretakers and healthcare providers consistently report these findings. Experts attribute this to lower stress levels combined with better care.
An intriguing correlation is the connection between love and lower pain levels. A CDC study of more than 127,000 adults revealed that married people are less likely to have headaches and back pain3
Committed relationships are associated with lower instances of recurring back pain and headaches4.
Other research revealed similar results. It stands to reason that this would not just apply to married couples, but to other relationships as well, though more studies are needed.
As lupus patients, we are at increased risk of depression and
anxiety disorders. As it is, love is also known to reduce depression. According to the US Department of Health and Human Services, getting married and staying married reduces depression in both men and women5.
Love is also known to lower blood pressure and induce better sleep. The health benefits attributed to love are clearly established.
A disease like lupus is complex and requires a lot of support. This does not mean that you need to go out and sign up for a dating app right now! But it does mean that forming a good network of support around us is critical. This network extends to your community, church, senior center, friends, family, and more. Building loving relationships, whether platonic or romantic, has been proven to increase longevity and improve
health outcomes. This is wellestablished in medical literature.
One of the challenges faced by lupus patients is fostering relationships while managing chronic illness. As lupus patients we know that relationships take work. There is nurturing involved. How can we do this when we barely have the energy to take care of ourselves?
The most important thing is to ensure that your network of friends and loved ones understands that you have lupus. They need to be educated as to what lupus is and how it can impact you on a daily basis. The Lupus Foundation of America, Greater Ohio Chapter offers a New Patient Education class each month (sign up by going to LupusGreaterOhio.org) which is not only for new patients, but caregivers as well.
Another great place to find empathy and camaraderie is at Lupus Foundation of America, Greater Ohio Chapter support groups. Support groups are open discussions, led by a trained facilitator where patients are surrounded by people who understand because they too are living with lupus. For more information visit lupusgreaterohio. org/find-resources/find-support/.
The second thing is to pay close attention to your illness. What time of day is hardest for you? Do you start losing energy as the day goes on? Or is it harder for you to get out of bed and get going. Most lupus patients have a pattern. So, if you are setting up lunch with friends, or planning a romantic date, make sure it’s a time that you are more likely to be successful.
Another thing to pay attention to is how your body reacts to changes


in weather. Is your illness worse in January every year? Or do the summer storms trigger your pain? Is the sun your friend or your enemy? It’s best to consider these questions when planning an outing. A picnic in August may not work for lupus patients!
During flares, practice self-love. Ensure that you are still communicating with friends and family but take the time to rest. Make sure you are getting enough fluids, practice gentle exercise (under the care of a doctor), take your medicine as prescribed, stay out of the sun, eat right, and meditate.
And last, be gentle with yourself. If you feel frustrated because your body isn’t behaving, remind yourself that flares don’t last forever. Give yourself time to heal, then make all those plans with loved ones. Loved ones and true friends will always be there for you,
through the good and the bad.
Love is the bedrock of life. We form so many different loving relationships during our lifetime and they can and do impact us in many ways, especially our health. As supported by many research studies and real-life evidence, love is another tool in our arsenal of defenses against lupus. So, make sure you take the time to surround yourself with healthy and loving relationships that lift and sustain you.
References:
1. American Heart Association. (2022, August 4). Effects of Objective and Perceived Social Isolation on Cardiovascular and Brain Health: A Scientific Statement from the American Heart Association. https://www.ahajournals.org/doi/full/10.1161/ JAHA.122.026493.
2. Circulation: Cardiovascular Quality
& Outcomes. (2020, October 20). Does Dog Ownership Really Prolong Survival? A Revised Meta-Analysis and Reappraisal of the Evidence. https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.120.006907.
3. CDC National Center for Health Statistics. (nd). Marital Status and Health: United States, 1999-2002. https://www.cdc.gov/nchs/pressroom/04facts/marriedadults.html.
4. Virginia Commonwealth University. (2013, June 5). The Relationship between Marital Status and Psychological Resilience in Chronic Pain. https:// onlinelibrary.wiley.com/doi/ epdf/10.1155/2013/928473.
5. Robert G. Wood, Brian Goesling, and Sarah Avellar of Mathematica Policy Research, Inc. under contract to ASPE. (2007, June 30). The Effects of Marriage on Health: A Synthesis of Recent Research Evidence. https://aspe.hhs.gov/reports/effects-marriage-health-synthesis-recent-research-evidence-research-brief.
Lupus is a chronic autoimmune disease that causes inflammation in various parts of the body. The disease can range from mild to life-threatening. Ninety percent of those diagnosed with lupus are females between ages 15 and 44, but lupus also occurs in men, older people, and children. Lupus can be very hard to diagnose because symptoms vary from person to person, can come and go, and can mimic symptoms of other illnesses. is important to know the symptoms of lupus and to know if you are at risk for this disease. Here is a simple test to help you. Read each question and answer it in terms of your current AND past health.
Have you had a seizure or convulsion?
Have you had unexplained confusion that lasted more than an hour?
Have you had unexplained fever higher than 100º F/38º C for more than a few days that was not due to infection?
Heart
Have you felt chest pain while taking deep breaths?
Have you had a stroke or heart attack?
Have you been told you have protein in your urine?
Have you had swelling in your legs and ankles on both sides at the same time?
Blood
Have you been told you have anemia, low white cell count, or low platelet count?
Have your fingers and/or toes become pale or red or blue, or felt numb or painful?
Have you had blood clotting problems or a miscarriage?
If you have had any symptoms like these, especially if you have had several, talk to your doctor about lupus. Early diagnosis and proper medical care are the best ways to manage lupus.
Please turn over this page for more information.
Have you had sores in your mouth or nose that lasted more than five days?
Have you developed irritation or dryness in your eyes or mouth for more than a few weeks?
Have you had unexplained weight loss or abdominal pain or tenderness when your belly is touched?
Have you had stiff, tender, and swollen joints that feel worse in the morning?
Have you had extreme fatigue and weakness for days or weeks at a time, even after plenty of sleep?
Has your skin broken out after being in the sun, but it’s not a sunburn?
Have you had redness or rash across your nose and cheeks in the shape of a butterfly?
Have you had sores on your skin that would not heal?
Have you had sudden, unexplained hair loss?
Let's Talk About It Webinar Series
Living with Lupus Magazine
Lupus Night Light Blog
My Lupus Living Room Podcast
Patient Navigator Program
Educational Summits & Classes
Support Groups
Local State Advocacy Use this QR code to access program & educational resources.

The Lupus Foundation of America is the only national force devoted to solving the mystery of lupus, one of the world’s cruelest and devastating diseases, while giving caring support to those who suffer from its brutal impact. Through a comprehensive program of research, education, and advocacy, we lead the fight to improve the quality of life for all people affected by lupus. Contact the LFA or a chapter that serves your area to find out how you can become involved in our mission and how we can help you.
Suzanne Tierney, CEO/President Suzanne@lupusgreaterohio.org

Kathy Holmes Finance Manager
Kathy@lupusgreaterohio.org
I was diagnosed with lupus in 1989 and joined the Lupus Foundation of America, Greater Cleveland Chapter the same year. I have been able to grow with the organization, as it became the LFA, GOC. Knowing how important it was to have somewhere to turn when I was first diagnosed is what motivates me to do all I can to help our chapter continue in our mission. Being in remission for the past 20 years has enabled me to take an active part in the growth of our chapter.

Mackenna Willis Creative Design Manager
Mackenna@lupusgreaterohio.org
I’m the marketing manager and creative developer when it comes to strategizing new ideas for Lupus awareness. As a graduate from Bowling Green State University with a BFA in graphic design, I’ve always envisioned utilizing my skills to make a difference. My enthusiasm to help others through design has always been a passion of mine and having the opportunity to share and grow with the LFA, GOC team has been nothing but inspiring.
I have spent the last 30 years dedicated to the lupus patients in Ohio. The goal is to provide a better quality of life until a cause or cure for lupus is found. My passion is providing programs to empower those affected by lupus so that they will have a better journey with lupus through education and emotional support. Lupus does not have to be a lonely, miserable, and misunderstood illness. My goal is to provide my chapter with the tools and resources to provide such services to all those in the state of Ohio.
Rita O. Piccin, BS, ND, RN Lead Patient Navigator /Outreach Coordinator
Rita@lupusgreaterohio.org

chapter continue to grow and help lupus patients for years to come.
I am a caring, collaborative, and resourceful nursing professional with over 30 years of experience in a variety of roles. I have a BS in Biology and French from John Carroll University and a Doctor of Nursing degree from Frances Payne Bolton School of Nursing at Case Western Reserve University. I am passionate about giving effective and empathetic customer service and education to patients, caregivers, families, colleagues and community organizations. I am honored to be a part of the LFA,GOC and dedicated to providing education, support, and resources to lupus warriors.

Community Outreach Coordinator
Aletha@lupusgreaterohio.org
two wonderful sons, they are the reason I fight lupus daily. I share my story everyday hoping that it might help or encourage someone else on their journey. I try to leave lupus patients with these thoughts and that is keep your environment positive in all aspects and do what you can

Chris Milazzo Event Assistant
Chris@lupusgreaterohio.org
Helping others has always been one of my greatest passions. After graduating from SUNY Oneonta with a degree in Media Studies, I knew I wanted to use my degree to do good. Being able to work for the LFA, GOC has been one of the most rewarding experiences in my career so far. It brings a smile on my face knowing that the work I do is able to help the lupus community of Ohio, and I hope to continue being a helping hand for the community.
www.lupusgreaterohio.org
THANK YOU FOR READING OHIO’S LUPUS MAGAZINE! FOR THE MOST UP-TO-DATE INFORMATION FROM THE WORLD OF LUPUS, PLEASE VISIT US AT WWW.LUPUSGREATEROHIO.ORG
THE FUNDING FOR THIS CAMPAIGN IS FROM AN EARMARK FROM THE STATE OF OHIO AND MANAGED BY THE OHIO DEPARTMENT OF HEALTH.
EMAIL INFO@LUPUSGREATEROHIO.ORG WITH ANY QUESTIONS OR CONCERNS.
GET IN TOUCH!
Lupus Foundation of America, Greater Ohio Chapter 12930 Chippewa Road, Brecksville, OH, 44141
Phone: (440) 717-0183 Toll-free: 1 (888) NO-LUPUS FOLLOW OUR SOCIAL MEDIA @lupusgreaterOH