AfricanAmericans and San Diego Medicine

BLACK HISTORY MONTH




FEBRUARY 2024
Publication of SDCMS
Official
DR. EDGAR CANADA
DR. LATISA CARSON

For more than 40 years, the Cooperative of American Physicians, Inc. (CAP) has delivered financially secure medical malpractice coverage options and practice solutions to help California physicians realize professional and personal success. Find out what makes CAP different. www.CAPphysicians.com 800-356-5672 MD@CAPphysicians.com Medical professional liability coverage is provided to CAP members through the Mutual Protection Trust (MPT), an unincorporated interindemnity arrangement organized under Section 1280.7 of the California Insurance Code. STAY AHEAD OF THE CRITICAL HR CHALLENGES IMPACTING MEDICAL PRACTICES Scan the QR code to download your free guide now! www.CAPphysicians.com/HRnow CAP’s free guide, Addressing Critical Human Resources Challenges in the Medical Practice, offers tips and guidance to help you: • Improve the interview process • Foster an environment of employee engagement • Reduce the chances of an employment-related lawsuit
Stay current on state and federal laws • And more!
•
Editor: James Santiago Grisolia, MD
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; William T-C Tseng, MD; Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
OFFICERS
President: Nicholas (dr. Nick) J. Yphantides, MD, MPH
President–Elect: Steve H. Koh, MD
Secretary: Preeti S. Mehta, MD
Treasurer: Maria T. Carriedo-Ceniceros, MD
Immediate Past President: Toluwalase (Lase) A. Ajayi, MD
GEOGRAPHIC DIRECTORS
East County #1: Catherine A. Uchino, MD
Hillcrest #1: Kyle P. Edmonds, MD
Hillcrest #2: Stephen R. Hayden, MD (Delegation Chair)
Kearny Mesa #1: Anthony E. Magit, MD, MPH
Kearny Mesa #2: Dustin H. Wailes, MD
La Jolla #1: Karrar H. Ali, DO, MPH (Board Representative to the Executive Committee)
La Jolla #2: David E.J. Bazzo, MD, FAAFP
La Jolla #3: Sonia L. Ramamoorthy, MD, FACS, FASCRS
North County #1: Arlene J. Morales, MD
North County #2: Christopher M. Bergeron, MD, FACS
North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Latisa S. Carson, MD
AT–LARGE
DIRECTORS
#1: Rakesh R. Patel, MD, FAAFP, MBA (Board Representative to the Executive Committee) #2: Kelly C. Motadel, MD, MPH #3: Irineo (Reno) D. Tiangco, MD #4: Miranda R. Sonneborn, MD #5: Daniel Klaristenfeld, MD
#6: Alexander K. Quick, MD #7: Karl E. Steinberg, MD, FAAFP #8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Young Physician: Emily A. Nagler, MD
Resident: Alexandra O. Kursinskis, MD
Retired Physician: Mitsuo Tomita, MD
Medical Student: Jesse Garcia
CMA OFFICERS AND TRUSTEES
Immediate Past President: Robert E. Wailes, MD
Trustee: William T–C Tseng, MD, MPH
Trustee: Sergio R. Flores, MD
Trustee: Timothy A. Murphy, MD
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Albert Ray, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Kyle P. Edmonds, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
At–Large: David E.J. Bazzo, MD, FAAFP
At–Large: Sergio R. Flores, MD
At–Large Alternate: Bing Pao, MD
CMA DELEGATES
District I: Steven L.W. Chen, MD, FACS, MBA
District I: Franklin M. Martin, MD, FACS
District I: Eric L. Rafla-Yuan, MD
District I: Ran Regev, MD
District I: Kosala Samarasinghe, MD
District I: Thomas J. Savides, MD
District I: James H. Schultz, MD, MBA, FAAFP, FAWM, DiMM
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
District I: Randy J. Young, MD
RFS Delegate: David J. Savage, MD
Opinions expressed by authors are their own and not necessarily those of SanDiegoPhysician or SDCMS. SanDiegoPhysicianreserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request. Acceptance of advertising in SanDiegoPhysicianin no way constitutes approval or endorsement by SDCMS of products or services advertised. SanDiegoPhysicianand SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org. SanDiegoPhysicianis published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]
FEATURES
4 Freedom House Ambulance Service: America’s First Paramedics By Edgar D. Canada, MD
6
Obesity and Black Women
By Latisa S. Carson, MD,
FACOG, DABOM
8
Women and Minorities Bear the Brunt of Medical Misdiagnosis
By Liz Szabo
DEPARTMENTS
2 Briefly Noted: Physician Wellness • Advocacy • Prior Authorization
10 Disease-Modifying Medications for the Treatment of Alzheimer’s Disease By Michael Lobatz, MD


14
What is Tianeptine and Why Is It in Demand?
By Rachael Robertson
16
HHS Expands Access to Methadone, Buprenorphine
By Shannon Firth
17
The Aging Vitruvian Man and the Modern Practice of Medicine
By Daniel J. Bressler, MD, FACP
18
Thriving in ‘A Time Like This’
By Helane Fronek, MD, FACP, FASVLM, FAMWA
19
Dementia Predicted 10 Years Before Diagnosis
By Judy George
20 Classifieds
SAN DIEGOPHYSICIAN.ORG 1
10
VOLUME 111, NUMBER 2
Contents
FEBRUARY 8
PHYSICIAN WELLNESS
The Creation of San Diego County Physicians’ Chamber Orchestra
Musically Inclined Physicians Sought By David
M. Steinhorn, MD, FAAP
“Science and art create from the same source.” —Theodore Billroth
PHYSICIANS LIKELY HAVE THE GREATEST participation in music than any other professional group. Doctors and medical people seem to have a special connection to music as represented in Billroth’s quote above, which reflected his special friendship to Brahms. Billroth was an accomplished pianist and violinist during his days in Switzerland long before he was called to Vienna as chief of surgery. The association between music and health goes back to the dawn of humankind and is found still in the use of percussive instruments, drums, rattles, and chanting in indigenous healing rituals. Both music and healing involve an intimate human connection not found in most professions. Perhaps the work ethic, commitment and tenacity needed to achieve success in music provides the foundational skills for attention to detail and dedication that lead to success in medical professions.
There are currently 38 medical orchestras in the United States, with the majority located east of the Mississippi. In California until last year, Los Angeles was home to the 70-yearold LA Doctors Symphony Orchestra, which morphed into the Orchestra Nova LA in 2023 as a result of changes among physician musi-
CMA Physician Stands with Legislators in Support of Proposition
ON JAN. 16, ANNA YAP, MD, A Sacramento emergency medicine physician, represented CMA’s nearly 50,000 members at a press conference in support of Proposition 1, which will appear on the March 2024 ballot and aims to expand mental health and addiction services for Californians.
Dr. Yap said Prop 1 will create thousands of inpatient and outpatient resources. That’s
cians. The lone medical orchestra in California is presently at Stanford. Elsewhere, the World Doctors Orchestra was formed in 2008 and currently involves 1,800 physician musicians from 60 countries, having performed more than 40 concerts worldwide and raising nearly 2 million Euros for medical charity. With the above as background, a new initiative underway in San Diego County aims to create a San Diego Physicians Chamber Orchestra. By way of announcement, this short report serves to begin the process of recruiting interested physician musicians or medical and nursing school faculty who are accomplished instrumental musicians. Rehearsals will take place every two weeks at a central location currently under negotiation. As a chamber orchestra, the initial membership will be 24 to 30 members with pairs of winds, percussion, keyboard, and the balance strings. Interested readers should let their medical musician friends know about this new opportunity and may contact Dr. Steinhorn at sdmedicalorchestra@gmail.com with any questions. Interested musicians should include a brief description of their musical background including instrument, self-rated playing level, and contact information.
why the California Medical Association — representing nearly 50,000 physicians across California — is proud to support Proposition 1.”
Dr. Yap, a former CMA Trustee who currently serves on numerous CMA councils and committees, was joined at the press conference by legislative and community leaders, including Senator Susan Eggman, Assemblymember Jacqui Irwin, Assembly Majority Leader and Vice Chair of Legislative Women’s Caucus Cecilia AguiarCurry, and other healthcare organization representatives in support of Proposition 1.
2 FEBRUARY 2024
ADVOCACY
Feds Finalize Significant Prior Authorization Reform Regulation
By CMA Staff

THE CENTERS FOR MEDICARE and Medicaid Services (CMS) recently finalized comprehensive prior authorization reform regulations. These meaningful reforms apply to Medicare Advantage plans, state Medicaid and Children’s Health Insurance Program (CHIP) fee-for-service programs, Medicaid and CHIP managed care plans, and Qualified Health Plan issuers on the federally facilitated Exchanges (FFE).
These regulations reflect the bipartisan legislation supported by the California Medical Association (CMA) and authored by California physician Congressman Ami Bera, MD and others — HR 3173/S 3108 “Improving Seniors’ Timely Access to Care Act” that unanimously passed the U.S. House of Representatives in September 2022 with more than 375 bipartisan House and Senate cosponsors.
The final rule requires electronic prior authorization processes, shortens the time frames to respond to prior authorization requests, requires the public reporting of certain prior authorization metrics, and establishes policies to make the prior authorization process more efficient and transparent.
The rule will require impacted payers (not including QHPs on the FFE) to send prior authorization decisions within 72 hours for urgent requests and seven calendar days for standard requests. For some payers, this new timeframe for standard requests cuts current decision time frames in half. The rule also requires payers to include a specific reason for denying a prior authorization request, which will help facilitate resubmission of the request or an appeal when needed.
These operational or process-related prior authorization policies are being finalized with a compliance date starting Jan. 1, 2026, and the initial set of metrics must be reported by March 31, 2026.
Other highlights of the final rule include:
• Allows payers to exempt physicians with a history of high prior authorization approval rates.
• Mandates appropriate and public clinical evidence to substantiate prior authorization decisions.
• Requires plans to establish Utilization Management Committees with physicians.
• Increases public transparency of approvals, denials, overturned decisions, and response times.
CMS estimates that efficiencies introduced through these policies will save physician practices and hospitals more than $15 billion over a 10-year period.
CMA will be working with the American Medical Association on federal legislation to achieve our remaining prior authorization goal — real-time decisions. CMA also continues to support state-level legislation to reform prior authorization process to ensure that patients receive the care they need — when they need it.

SAN DIEGOPHYSICIAN.ORG 3 (858) 569-0300 www.soundoffcomputing.com TRUST A COMMON SENSE APPROACH TO INFORMATION TECHNOLOGY Trust us to be your Technology Business Advisor HARDWARE SOFTWARE NETWORKS EMR IMPLEMENTATION SECURITY SUPPORT MAINTENANCE Endorsed by PRIOR AUTHORIZATION
Freedom House Ambulance Service: America’s First Paramedics
By Edgar D. Canada, MD
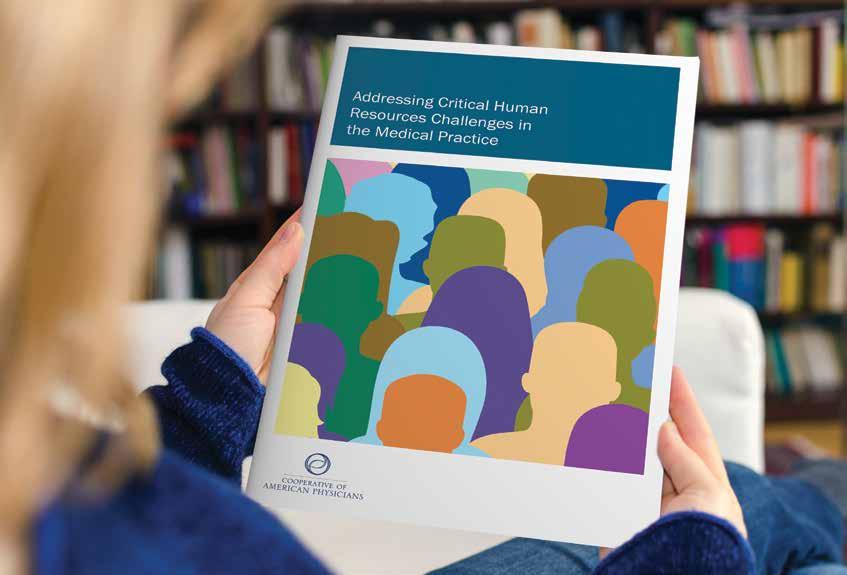
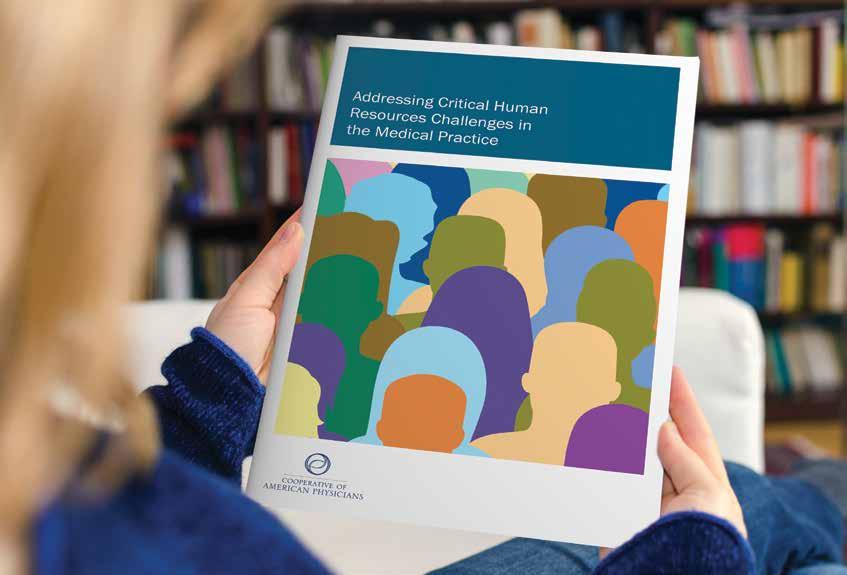
IN A STORY REMINISCENT OF THE ONE TOLD IN
the 2016 book by Margot Lee Shetterly, Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space Race that later became the basis for the 2017 movie Hidden Figures, medicine has a somewhat similar but probably less known story — as told in the 2022 book by Kevin Hazzard, American Sirens: The Incredible Story of the Black Men Who Became America’s First Paramedics.
“In 1968, twenty-four Black men led a revolution in emergency medicine. This is the extraordinary story of the birth of the paramedic and the people who forever changed how we save lives.”1 This book chronicles the innovation that created the emergency medical services system in use across the United States that most of us take for granted.
In the late 1960s if you needed to be transported urgently to the hospital, in most communities you would either be transported by funeral workers in a hearse or policemen in a paddy wagon. Most times, no one would be with you in the back of the vehicle and no treatment would be delivered en route to the hospital. There were no guidelines for acceptable treatment and no standards for training of the personnel providing care. Their goal was simply to get you to the hospital as quickly as possible, often referred to as swoop and scoop. Sometimes patients were lucky and well served by this intervention; but with no treatment, often patients arrived at the hospital only to be pronounced dead.
All of this was about to change. Surprisingly, this innovation took place in the Hill District of Pittsburgh, a predominantly Black neighborhood. “It was known by many names: Little Harlem, Little Haiti, and the crossroads of the world.”2 From the 1930s to the 1950s, the Hill District was a thriving area of the city for Black residents offering music, art, culture, and business opportunities. In the 1960s, with a declining economy and poor implementation of urban renewal compounded by civil unrest, life was bleak for the residents of the Hill District. This is not the neighborhood where one would expect to witness a transformation in the method of providing out-of-hospital care. A neighborhood association
known as Freedom House Enterprises was founded in 1967 and dedicated to promoting business and employment opportunities in the Hill District. Initially, its vans and drivers delivered fresh fruit and vegetables to residents of the Hill District owing to a lack of grocery stores providing such items in this neighborhood. It was thought that expanding the services to include transporting patients to and from their medical appointments would be quite useful and beneficial for the community.
Discussion and meetings of James McCoy Jr. from Freedom House Enterprises with Philip Hallen, president of the Maurice Falk Medical Fund and Dr. Peter Safar3-5, founding chair of the department of anesthesiology and critical care medicine at the Presbyterian University Hospital (now part of University of Pittsburgh Medical Center) led to the creation of Freedom House Ambulance Service. Laypersons from the neighborhood (all Black men) would be recruited to train in a program designed by Dr. Safar. At the beginning, Freedom House Ambulance Service only operated in the Hill District, but as time progressed, they operated citywide. “More than 50 Freedom House paramedics and dispatchers handled more than 45,000 emergency calls over their eightyear history.”4
In 1975 the City of Pittsburgh created its own ambulance service and did not renew the contract for Freedom House Ambulance Service. A few of the Freedom House Ambulance Service paramedics transitioned to the new service but were required to perform additional training and testing to continue. The new ambulance service operated by the city consisted of a mostly white staff. One would have to be naïve or indifferent to not note that this was racism, plain and simple.
Kevin Hazzard’s book details this incredible story in a well-documented and referenced manner. His book tells this story through the lives of three individuals intertwined with the overall story of the Freedom House Ambulance Service: John Moon, a Freedom House paramedic; Dr. Peter Safar, the anesthesiologist/innovator who changed prehospital medical care; and Nancy Carol, the first medical director of Freedom House Ambulance Service. It is well worth a read
4 FEBRUARY 2024
AFRICAN-AMERICANS AND MEDICINE
and truly a story that more people should know about. A hint at what awaits the reader can be found in a National Public Radio interview by Dave Davies6 .
Endnotes
1. Kevin Hazzard, American Sirens: The Incredible Story of the Black Men Who Became America’s First Paramedics (New York: Hachette Books, 2022), jacket cover.
2. “The Rich History of Pittsburgh’s Hill District,” Shop Pittsburgh Beautiful, August 7, 2017, https://www.pittsburghbeautiful.com/2017/08/07/the-rich-history-of-pittsburghshill-district/ (accessed January 14, 2024).
3. Jose Ramirez, “Peter Safar, ‘The Father of C.P.R.’Is Dead at 79,” New York Times, August 6, 2003, https://www.nytimes. com/2003/08/06/us/peter-safar-the-father-of-cpr-is-deadat-79.html (accessed January 14, 2024).
4. “Profiles in Diversity – Peter Safar, MD,” Department of Anesthesiology and Perioperative Medicine, University of Pittsburgh, February 1, 2011, https://www.anesthesiology. pitt.edu/news/profiles-diversity-peter-safar-md (accessed January 14, 2024).
5. Jeanne Lenzer, “Peter Josef Safar: The Father of Cardiopulmonary Resuscitation,” British Medical Journal 327(7415): 624, September 13, 2003, https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC194106/pdf/bmj32700624.pdf (accessed January 15, 2024).
6. Kevin Hazzard, “How a Black Neighborhood Association in Pittsburgh Helped Shape Emergency Medicine,” Interview by Dave Davies, Fresh Air, NPR, December 19, 2022, https:// www.npr.org/2022/12/19/1144150485/how-a-black-neighborhood-association-in-pittsburgh-helped-shape-emergencymedici (accessed January 14, 2024).

Dr. Canada is a recently retired pediatric anesthesiologist and former member of Anesthesia Service Medical Group. His 46-year clinical experience was mostly in San Diego County. He served as a naval medical officer, past president of the San Diego County Medical Society, past president of the San Diego Society of Anesthesiologists, past president of the California Society of Anesthesiologists, and chief of staff at Rady Children’s Hospital San Diego.









SAN DIEGOPHYSICIAN.ORG 5
PLACE YOUR AD HERE Contact Jennifer Rohr 858.437.3476 Jennifer.Rohr@SDCMS.org FEBRUARY2020 Official Publication of SDCMS Celebrating 150 Y Artificial Intelligence and Medicine THE DEBATE Official Publication of SDCMS Celebrating 150 How to BUILD DIABETES Reversing the Risks DEMENTIA Reducing the Burden GUN SAFETY Engaging Patients BREAST CANCER Preventing Deaths NOVEMBER/DECEMBER2019 PREVENTION

Obesity and Black Women
By Latisa S. Carson, MD, FACOG, DABOM
IN 2010, I DECIDED TO START TAKING COURSES in obesity medicine to educate myself on the pathophysiology of obesity and the medical management of weight loss. My postpartum and perimenopause/menopause patients were struggling with weight gain and associated morbidities.
I realized that I had little medical knowledge of obesity and I was not adequately trained in medical school or residency on the diagnosis, management, or treatment of obesity. I could not give my patients tools for weight loss, nutrition, exercise, or prescription of pharmacotherapy. When I began the journey, I did not know that it would eventually lead to me moving my practice after dedicating 16 years of community service in National City to the Eastlake area in Chula Vista in 2018, joining 3,370 board-certified physicians in obesity medicine in 2019, studying functional medicine, and retiring from the practice of obstetrics in 2022 to expand my medical weight-loss practice.
Since it is Black History Month, I would like to focus on treatment of Black women with obesity. How can we take population-based treatment of obesity and individualize it for the treatment of obesity in Black women? Addressing obesity in Black women as a personalized treatment plan is important.
6 FEBRUARY 2024
AFRICAN-AMERICANS AND MEDICINE
The prevalence of obesity is high and 70% of Black women are overweight or obese.
Obesity is associated with more than 236 diseases. Obesity is the root cause of death in all ages and all causes from hypertension, diabetes, stroke, and heart disease. For many Black women, obesity commonly begins during pregnancy. Black women will gain 40% more weight during pregnancy than white women and retain their postpartum weight. Failure to lose this weight in the postpartum period may begin weight stacking with subsequent pregnancies.
The Obesity Society has a great resource, which lists the more than 70 contributing factors to energy storage. The calories in/calories out and/or telling the patient to eat less and move more is obsolete when the clinician is educated on the complexity of triggers and contributing factors to obesity. Obesity is a hormonal dysregulation and has nothing to do with willpower. Once physicians are educated on the pathophysiology of obesity, this will help eliminate weight bias approaches to patient care management.
Our most common determinant of obesity is the body mass index. Black people have more lean muscle mass. Black women also have higher fat percentage that is subcutaneous and may be distributed in the belly and hips. Leptins and adiponectin are also higher among Black people who have obesity. BMI overestimates obesity with traditional BMI thresholds in Black women.
The “Health at Every Size Movement” led by Dr. Sabrina Strings, PhD, believes BMI should be eliminated in the evaluation of Black women. Obesity scientists believe that the BMI should be modified for Black women as a population-based tool to a BMI of 31–33, if obesity co-morbidities such as hypertension, dyslipidemia, diabetes, or two or more risk factors for obesity are absent. An independent measure of waist circumference, a measure of hip circumference, and a body composition calculation of body fat percentage are also additional special considerations in obesity diagnosis. A patient’s race, ethnicity, and age should also be considered.
The Pillars of Treatment developed by the Obesity Medical Association address the chronic disease of obesity, assessment and evaluation, nutrition, physical activity, behavior modification, medication, and surgery. Racial disparities, systemic racism, and social determinants of health for Black patients exist at every pillar. Nutrition may be jeopardized secondary to living in a food desert, where foods are highly palatable but calorie dense and nutritionally deficient. Socioeconomic status may play a role in lack of physical activity challenged by neighborhood safety, crime-prone areas, and lack of access to parks and gyms. Chronic psychologic stress and those experiencing systemic racism are 60% more likely to develop obesity.
Clinicians are less likely to address obesity in Black patients unless they also have cardiovascular disease. Clinicians may not realize their own weight bias and implicit bias when delivering healthcare and counseling. The role of community and social support influences the success of weight loss.
While counseling patients on lifestyle, assess your bias and
avoid assumptions. A patient’s “happy weight” is individualized and is related to a cultural perception of beauty. The “body confidence” and “body positivity” movement within the Black community can be discordant with health standards. In certain parts of the African diaspora, curves and additional weight are celebrated and are associated with the cultural perception of beauty, good health, and wealth.
The literature has shown that Black patients are less likely to be referred for medical or surgical treatment of obesity. There has been limited Black patient representation in pharmacological studies due to lack of recruitment and the mistrust of the Black community of the healthcare system. Black people have different responses to the medication and tend to have less pharmacologic weight loss. Weight bias in healthcare affects access, prescribing, insurance coverage, and the shortage of availability of subcutaneous pharmacotherapy.
Bariatric surgery referrals are lower for Black patients. Black patients tend to have higher complication rates and less weight loss at one year. But there are not any significant differences in remission of diabetes with insulin dependence, diabetes with insulin dependence, or hyperlipidemia. Metabolic health is improved, despite the differences in surgical outcome.
The Black Women’s Health Study is the largest ongoing health study from Boston University, started in 2003. The study summarizes the predictors of good overall health and good mental health in areas that clinicians may be able to positively influence; brisk walking, having no major health conditions, lower BMI, never smoking, and eating healthy portions of fruits, vegetables, lean meats, and nuts. Social determinants of health included fewer caregiver responsibilities, fewer experiences of everyday racism and discrimination, being single, being a college graduate, and an income of $100,000 or more.
Healthy weight may be different for Black women when adjusting for body composition and waist circumference. A “happy weight” by cultural standards, weight goals, and higher medical thresholds may be different, and clinicians need to use shared decision making for weight and health goals. We should normalize treatment equity by initiating early obesity treatment in Black women.

Dr. Carson is the only AfricanAmerican female double board-certified obstetrician gynecologist and obesity medicine specialist in solo private practice in San Diego County. She provides gynecology care and gynecology surgery, along with medical weight loss care to men and women in the community. This article is adapted from “Obesity in Black Women: What Are We Missing?” by Sylvia Gonsahn-Bollie, MD.
SAN DIEGOPHYSICIAN.ORG 7
Maternal mortality for Black mothers has increased dramatically in recent years. The United States has the highest maternal mortality rate among developed countries. According to the Centers for Disease Control and Prevention, non-Hispanic Black mothers are 2.6 times as likely to die as non-Hispanic white moms. More than half of these deaths take place within a year after delivery.
Research shows that Black women with childbirth-related heart failure are typically diagnosed later than white women, said Jennifer Lewey, MD, MPH, co-director of the pregnancy and heart disease program at Penn Medicine. That can allow patients to further deteriorate, making Black women less likely to fully recover and more likely to suffer from weakened hearts for the rest of their lives.
Watkins said the diagnosis changed her life. Doctors advised her “not to have another baby, or I might need a heart transplant,” she said. Being deprived of the chance to have another child, she said, “was devastating.”
Racial and gender disparities are widespread.
Women and minority patients suffering from heart attacks are more likely than others to be discharged without diagnosis or treatment.
Black people with depression are more likely than others to be misdiagnosed with schizophrenia.
Minorities are less likely than whites to be diagnosed early with dementia, depriving them of the opportunities to receive treatments that work best in the early stages of the disease.
Misdiagnosis isn’t new. Doctors have used autopsy studies to estimate the percentage of patients who died with undiagnosed diseases for more than a century. Although those studies show some improvement over time, life-threatening mistakes remain all too common, despite an array of sophisticated diagnostic tools, said Hardeep Singh, MD, MPH, a professor at Baylor College of Medicine who studies ways to improve diagnosis.
“The vast majority of diagnoses can be made by getting to know the patient’s story really well, asking follow-up questions, examining the patient, and ordering basic tests,” said Dr. Singh, who is also a researcher at Houston’s Michael E. DeBakey VA Medical Center. When talking to people who’ve been misdiagnosed, “one of the things we hear over and over is, ‘The doctor didn’t listen to me.’”
Racial disparities in misdiagnosis are sometimes explained by noting that minority patients are less likely to be insured than white patients and often lack access to highquality hospitals. But the picture is more complicated, said Monika Goyal, MD, an emergency physician at Children’s National Hospital in Washington, DC, who has documented racial bias in children’s healthcare.
In a 2020 study, Dr. Goyal and her colleagues found that Black kids with appendicitis were less likely than their white peers to be correctly diagnosed, even when both groups of patients visited the same hospital.
Although few doctors deliberately discriminate against
women or minorities, Dr. Goyal said, many are biased without realizing it.
“Racial bias is baked into our culture,” Dr. Goyal explained. “It’s important for all of us to start recognizing that.”
Demanding schedules, which prevent doctors from spending as much time with patients as they’d like, can contribute to diagnostic errors, said Karen Lutfey Spencer, a professor of health and behavioral sciences at the University of Colorado-Denver. “Doctors are more likely to make biased decisions when they are busy and overworked,” Spencer said. “There are some really smart, well-intentioned providers who are getting chewed up in a system that’s very unforgiving.”
Doctors make better treatment decisions when they’re more confident of a diagnosis, Spencer explained.
In an experiment, researchers asked doctors to view videos of actors pretending to be patients with heart disease or depression, make a diagnosis, and recommend follow-up actions. Doctors felt far more certain diagnosing white men than Black patients or younger women.
“If they were less certain, they were less likely to take action, such as ordering tests,” Spencer said. “If they were less certain, they might just wait to prescribe treatment.”
It’s easy to see why doctors are more confident when diagnosing white men, Spencer said. For more than a century, medical textbooks have illustrated diseases with stereotypical images of white men. Only 4.5% of images in general medical textbooks feature patients with dark skin.
That may help explain why patients with darker complexions are less likely to receive a timely diagnosis with conditions that affect the skin, from cancer to Lyme disease, which causes a red or pink rash in the earliest stage of infection. Black patients with Lyme disease are more likely to be diagnosed with more advanced disease, which can cause arthritis and damage the heart. Black people with melanoma are about three times as likely as whites to die within five years.
The COVID-19 pandemic helped raise awareness that pulse oximeters — the fingertip devices used to measure a patient’s pulse and oxygen levels — are less accurate for people with dark skin. The devices work by shining light through the skin; their failures have delayed critical care for many Black patients.
Seven years after her misdiagnosis, Watkins is an assistant professor of social work at North Carolina Central University in Durham, where she studies the psychosocial effects experienced by Black mothers who survive severe childbirth complications.
“Sharing my story is part of my healing,” said Watkins, who speaks to medical groups to help doctors improve their care. “It has helped me reclaim power in my life, just to be able to help others.”
Liz Szabo was a senior health correspondent for Kaiser Health News, where this article first appeared.
SAN DIEGOPHYSICIAN.ORG 9
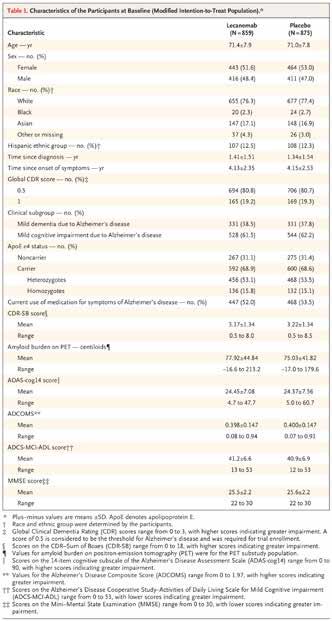
Disease-Modifying Medications for the Treatment of Alzheimer’s Disease:
The Good, the Bad, and the Ugly
By Michael Lobatz, MD
I HAVE BEEN A CLINICIAN FOR MORE THAN 40 years and have seen changes in treatment including the standard course of anticholinesterase inhibitors and memantine, none of which have worked very well. And I have had to deal with many ethical issues along the way, just as any practitioner who has to deal with issues related to dementia:
• Do you tell your patient of the diagnosis? This is one of the main complaints to physicians, that patients may not know they have dementia.
• Driving: We are in between the DMV and he patient, and we are required to report a diagnosis. Yet loss of ability to drive can cause great distress.
• What about getting consent for treatment? How do you get consent, and how do we ethically deal with getting consent from a person who does not understand?
• Genetic testing: Do we recommend it? When your patient brings you the results of their 23andMe and is concerned that it indicates APOE positivity, what do you tell them?
The Alzheimer’s Project Clinical Roundtable was created in 2014 by the County of San Diego as a realization that ADRD was a public health issue. Currently there are
between 100,000 and 130,000 community members with Alzheimer’s disease, and that estimate may be low. Factor in the average 1.5 caregivers for each individual, and you can see that dementia affects a large portion of our population. The Clinical Roundtable brought together practitioners from multiple health systems to develop guidelines for screening, evaluation, and the behavioral aspects of dementia. These guidelines have been widely disseminated both locally and across the country. And now 10 years from our start, we are seeing significant changes in the field. We are now at an inflection point.
New things are happening and the slope of change is rapidly increasing. Blood testing is coming, with the ability to look for amyloid and tau, specific for correlation with amyloid plaque deposition in the brain. We now have monoclonal antibodies (MABs) that are FDA approved — new treatments that have the potential to modify the disease for the first time. For those of us who have been in the field for a long time, to find something that makes a difference is stunning and has created huge amounts of press. This notoriety brings with it a new set of challenges for practitioners.
10 FEBRUARY 2024
ALZHEIMER’S DISEASE

Amyloid
and Tau, and What the DiseaseModifying Medications Do
We know that amyloid plaque is present in the brain long before there is any notice of cognitive dysfunction. Generally, plaque may be present for 10 years prior to any symptoms. Synaptic dysfunction and tau-mediated neuronal injury and dysfunction also are present prior to symptoms of cognitive decline, but generally later than the presence of amyloid.
There have been a number of drugs that have not done much, but the accepted theory is, let’s
treat what we know may be causing disease. Amyloid is easier to target than tau. So researchers have been able to create antibodies that actually pull the plaque out of the brain.
In 2012, bapineuzumab, the first of the MABs, failed trials due to evidence of futility at the halfway point of the study. In 2019, aducanumab reached futility analysis and failed, but came back to the FDA with new data that showed a trend toward benefit, and requested approval. This was despite a lot of skepticism about the study; the FDA Advisory Panel unanimously voted against approval, but FDA granted accelerated approval anyway. (Note: Biogen abandoned ownership rights and stopped clinical trials on Jan. 31, 2024.)
Lecanemab was approved in 2023, and donanemab is seeking approval in 2024. The MABs have shown that they do what they are supposed to do — clear plaque — but they can also create side effects, such as ARIAs (amyloid-related imaging abnormalities: either edema ARIA-E or hemorrhage ARIA-H). Most ARIA episodes are asymptomatic and can be seen on MRI. However, symptoms may occur including: headache, nausea, confusion, dizziness, and rarely stroke or seizures.
Lecanemab binds to soluble protofibrils of amyloid and clears amyloid from plaques, while donanemab binds to insoluble amyloid and clears plaques. Both antibodies slowed clinical progression, and both were associated with ARIA,
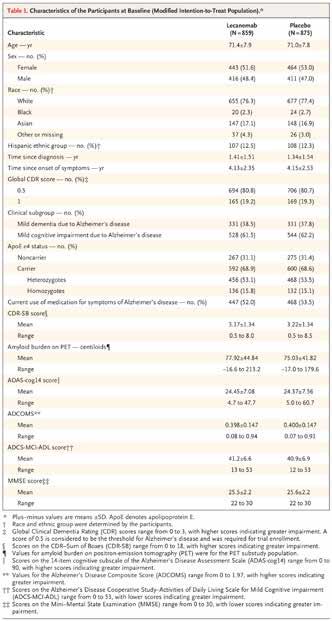
although significantly less than what was seen with aducanumab. Basically, the drugs show statistically significant slowing of disease progress compared to placebo, but there was no clinically significant change. These were 18-month studies; we can see curves are diverging, so we may see increasing benefits after 18 months. This is yet to be proven.
And the drugs have a number of exclusions and contraindications — heart issues, renal or liver functions, anything that could thin the blood. There is also the cost for the testing required to qualify, imaging, biomarkers, and then the drug itself and infusion costs, monitoring, and the physical and psychological toll on patients and care partners through the treatment process.
Profound advances in research have shown us it’s not just about the plaque. The Abeta inside the neuron is causing synapses to fail. Other researchers are also exploring the inflammation theory, and many call dementia Type 3 diabetes. How we treat AD will continue to evolve, but the recent approvals point to significant progress.
SAN DIEGOPHYSICIAN.ORG 11
ALZHEIMER’S DISEASE
What Should I Tell Patients and Families Inquiring About the Drugs?
Now that anti-amyloid therapies are available, we need to:
• Detect MCI or mild dementia
• Determine if Alzheimer’s is the cause of cognitive decline (biomarker tests performed must be used to confirm diagnosis)
• Explain risks and benefits of anti-amyloid immunotherapy
• Refer appropriate patients for consideration of therapy
Primary care providers are critical to early screening and diagnosis of dementia, including Alzheimer’s disease. The medications are appropriate only for those identified as asymptomatic or mild cognitive impairment due to Alzheimer’s disease. Patients in moderate to severe stage disease would not be appropriate. Nor are patients with other forms of dementia. If after a thorough evaluation the patient is diagnosed with probable Alzheimer’s disease, the primary care
provider would discuss reasons for diagnosis, and would inform patients and family members on a variety of topics, including the opportunities for treatment. If the patient is interested in learning more about MAB treatment, a referral to a specialist providing the treatment would be appropriate. Further testing including imaging and either blood tests or lumbar puncture would be conducted by the neurologist to determine if the patient would be most appropriate.
How Do I Assess if the Patient Is Appropriate for Referral?
The protocol developed by the Clinical Roundtable includes screening utilizing a patient exam and history inclusive of
an informant questionnaire. A full evaluation (if appropriate, would include the use of a MOCA, SLUMS, MMSE, and/ or qMCI), as well as labs and imaging are necessary prior to a conclusion and diagnosis of Alzheimer’s disease. If the patient meets the criteria of asymptomatic, early stage or mild cognitive impairment caused by Alzheimer’s disease, and the patient is interested in learning more about the MAB, a referral is appropriate. Not all patients will elect to pursue this course of treatment due to personal beliefs and their assessment of risks and benefits. Some patients may feel that slowing the disease for eight months is not worth the effort, while others may say, “Hey doc, give me everything you’ve got!” Of course, many will fall in between these two.
If the Patient Is Not a Good Candidate, What Can I Offer?
All patients and family caregivers will rely on their PCP for education and information in this journey. The traditional medications to treat some of the symptoms, such as cholinesterase inhibitors, also require education on risks and benefits, and may be helpful for a period of time. At moderate-stage dementia, memantine has been known to slow symptoms. Neither of these medications alter the disease, but may slow symptoms and delay functional decline. Healthy lifestyle changes may make the biggest difference for patients: healthy eating, physical activity, maintaining social contact, and keeping the brain active are known to enhance an individual’s overall health. These interventions are important whether the patient plans to pursue MCA treatment or not. Community resources will also greatly improve outcomes for patients and their care partners.
How Does Equity Fit in the Discussion?
The MABs were not tested broadly across the population; most study participants were white, higher educated, and with few comorbidities. Costs can be a barrier and access is likely limited to the uninsured and MediCal population. Rural areas are likely not to have infusion centers, specialists, or pharmacists — and with the shortage of specialists, many people may have delays in getting diagnosed, and therefore not have access to treatment.
For more information, links to CME webinars, resources, and after visit summary materials, see https://ChampionsforHealth.org/alzheimers.
Dr. Lobatz is a neurologist in private practice, chair of the Alzheimer’s Project Clinical Roundtable, and a longtime SDCMS member. He was accompanied in two virtual meetings by UC San Diego physicians Gabriel Leger, MD, neurologist; William Mobley, MD, neurologist; Ian Neel, MD, geriatrician; and Lindsey Yourman, MD, county chief geriatric officer. The content in this article was presented by these colleagues.
12 FEBRUARY 2024


Customized insurance solutions for members The CMA Insurance Program is administered by Lockton Affinity, LLC d/b/a Lockton Affinity Insurance Brokers LLC in California #0795478. Coverage is subject to actual policy terms and conditions. Policy benefits are the sole responsibility of the issuing insurance company. The California Medical Association will receive a royalty fee for the licensing of its name and trademarks as part of the insurance program offered to the extent permitted by applicable law. Not available in all states. Visit LocktonAffinityCMA.com to schedule a 15-minute call with Lockton Affinity’s dedicated team. Together, we will determine the policies you need to be fully protected. Info@LocktonAffinityCMA.com | (800) 278-8130 The CMA Insurance Program, administered by Lockton Affinity, offers key benefits: Using group purchasing power, CMA members get exclusive, comprehensive coverage at discounted rates. Unique coverage offerings help safeguard yourself, your loved ones, your business and your livelihood. Access to newly available Medical Malpractice insurance.
What Is Tianeptine and Why Is It in Demand?
Here’s Why This Unregulated Compound Is Known as ‘Gas Station Heroin’
By Rachael Robertson

AN UPTICK IN ADVERSE EVENTS CONNECTED TO
unregulated tianeptine products — often referred to as “gas station heroin” — along with the voluntary recall of a popular product have brought renewed attention to the atypical tricyclic antidepressant.
Earlier this week, the company that makes a product called Neptune’s Fix issued a voluntary recall of several of its products due to “undeclared tianeptine.” The move follows a warning from FDA last November urging consumers not to purchase or use Neptune’s Fix products or products with tianeptine, given reports of seizures, loss of consciousness, and death.
So what is tianeptine and why is it becoming so popular?
Daniel Lasoff, MD, emergency medicine physician and toxicologist at UC San Diego Health, told MedPage Today that the compound “has some opioid receptor activity, which is unusual for a tricyclic antidepressant.”
“We’ve had a pretty large migration away from tricyclic antidepressants as a first-line drug,” Dr. Lasoff said, noting that
selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) have taken their place.
Some tricyclic antidepressants, such as nortriptyline (Pamelor), imipramine, and amitriptyline are still commonly used, though “those drugs don’t typically have any opioid agonism,” he said.
Tianeptine was developed in the 1960s and is used in some parts of Europe, Asia, and South America to treat depression and pain. Some brand
names include Coaxil, Stablon, and Tatinol.
But in order for tianeptine to ever be used clinically here in the U.S., there would need to be solid research and clinical trials, Dr. Lasoff said.
“I don’t think it’s a particularly effective drug with a good safety profile compared to what’s already available out there,” he said.
Since tianeptine is not regulated and is easily available in powder, liquid, or capsule form at gas stations and online, its popularity has surged. According to the FDA, there were only 11 total tianeptine exposure cases at poison control centers from 2000 to 2013, but in 2020 alone there were 151 cases.
A recent report from New Jersey’s poison control center published in Morbidity & Mortality Weekly Report highlighted an “uncharacteristic spike” in patients who became critically ill after ingesting contaminated tianeptine products.
Among the 17 patients identified, 14 took products made by Neptune’s Fix, Christopher Counts, MD, of Rutgers New Jersey Medical School, and colleagues reported. Thirteen of the 17 patients were admitted to the ICU and seven required intubation. Patients reported symptoms such as tachycardia, hypotension, seizure, and cardiac arrest.
After testing six bottles of the product, the CDC found “variable composition,” and some were
14 FEBRUARY 2024 HEALTH AND CONSUMER PRODUCTS
contaminated with emerging synthetic cannabinoids, they reported.
“It’s important for members of the public and healthcare professionals to be aware that readily purchased tianeptine products might be adulterated with synthetic cannabinoid receptor agonists or other drugs and can produce severe adverse effects,” the researchers cautioned.
Dr. Lasoff also warned that people who buy and use tianeptine products “tend to develop dependency or addiction” and then doctors “see people develop withdrawal syndromes from them.”
In a 2023 narrative review of tianeptine’s pharmacology and abuse potential published in Pain and Therapy, Amber Edinoff, MD, and co-authors wrote that tianeptine can act as a full agonist at the mu-opioid receptor and “its short halflife can lead to rapid withdrawal, increasing its potential for addiction and misuse.”
Reddit has a “quitting tianeptine” forum with more than 5,200 members. Some people share stories of trying to stop using tianeptine while others post about using tianeptine to lessen dependency on other substances, like kratom.
Dr. Lasoff said he’s heard of both situations, and rather
than trading one drug for another, “the smart thing to do would be to use some sort of replacement therapy that is already approved and has good research behind it — things like buprenorphine or methadone,” which both have long half-lives. He also urged fellow doctors to talk to their patients about supplements and substances.
Last month, five members of Congress, including emergency physician Rep. Rich McCormick, MD, (R-Ga.) wrote a letter to FDA commissioner Robert Califf, MD, urging the FDA to issue guidance on tianeptine.
Specifically, they wanted the FDA to research the health effects of using and overusing tianeptine and investigate whether it should be a controlled substance.
A few days after the letter, Rep. Jimmy Panetta (D-Calif.) introduced a bill to Congress to “amend the Controlled Substances Act to provide for the scheduling of tianeptine as a schedule III substance, and for other purposes.”
Rachael Robertson is an enterprise and investigative writer for MedPage Today, where this article first appeared.









SAN DIEGOPHYSICIAN.ORG 15
FEBRUARY2020 Official Publication of SDCMS Celebrating 150 Years Artificial Intelligence and Medicine THE DEBATE MARCH2020 Official Publication of SDCMS Celebrating 150 How to BUILD DIABETES Reversing the Risks DEMENTIA Reducing the Burden GUN SAFETY Engaging Patients BREAST CANCER Preventing Deaths NOVEMBER/DECEMBER2019 Official Publication of SDCMS PREVENTION Contact Jennifer Rohr 858.437.3476 • Jennifer.Rohr@SDCMS.org PLACE YOUR AD HERE
HHS Expands Access to Methadone, Buprenorphine
Updates to 20-Year-Old Rules Allow Take-Home Methadone, Treatment Initiation via Telehealth
AS PART OF A BROADER overdose prevention strategy, the Biden administration announced changes to decades-old federal rules, which aim to simplify and expand access to addiction treatment in order to save more lives.
Specifically, the final rule, issued by HHS, makes permanent pandemic-era flexibilities that allow eligible patients with an opioid use disorder (OUD) to receive take-home methadone doses. Studies have suggested that takehome doses improve treatment adherence and reduce patients’ risk of illicit opioid use, according to a Substance Abuse and Mental Health Services Administration (SAMHSA) press release.
“At HHS, we believe there should be no wrong door for people who are seeking support and care to manage their behavioral health challenges, including when it comes to getting treatment for substance use disorder,” said HHS Deputy Secretary Andrea Palm in the press release. “The easier we make it for people to access the treatments they need, the more lives we can save.”
In addition, the administration announced that grant dollars can now be used to buy xylazine test strips, providing one more mechanism for preventing overdose deaths. Xylazine, a veterinary tranquilizer thought to be involved in a growing number of overdose deaths, is approved by the FDA for use in animals, but has not been approved for use in humans. HHS released a specific plan to address fentanyl-laced xylazine in July 2023.
The new final rule also includes the following additional provisions:
• Allows the use of telehealth to initiate treatment for an OUD and
By Shannon Firth
to reduce transportation barriers; for treatment with methadone, audio-visual telehealth is allowed, and for treatment using buprenorphine, audio-only technologies are permitted
• Allows nurse practitioners and physician assistants to order medications in opioid treatment programs, where state laws permit such a practice
• Eliminates “stringent admission criteria,” which previously restricted eligibility for treatment to those with at least a one-year history of addiction
• Increases access to “interim treatment” by enabling patients to start medications while waiting for additional services to become available
“While this rule change will help anyone needing treatment, it will be particularly impactful for those in rural areas or with low income for whom reliable transportation can be a challenge, if not impossible,” said Miriam E. Delphin-Rittmon, PhD, the HHS assistant secretary for mental health and substance use, who leads SAMHSA, in the press release.
“In short, this update will help those most in need,” she added.
Delphin-Rittmon also highlighted SAMHSA’s updated “Overdose Prevention and Response Toolkit” which was released earlier this week and provides guidance on the role of opioid overdose reversal medications, and how to respond to an overdose.
Importantly, in January 2023, the Biden administration also eliminated the X-waiver requirement for clinicians who use medications to treat
patients with substance use problems. The Biden administration aims to invest $83 billion in treatment, which is 42% more than under the Trump administration, according to a White House press release.
“Under President Biden’s leadership, we have invested more funding and broken more barriers to treatment than any previous administration,” noted Rahul Gupta, MD, MPH, director of the Office of National Drug Control Policy. “As a physician who has provided addiction treatment firsthand, I know these actions can mean the difference between life or death.”
Bobby Mukkamala, MD, chair of the American Medical Association’s Substance Use and Pain Care Task Force, hailed the final rule as a “step in the right direction in the fight against the worsening overdose epidemic.” The task force was especially pleased to see the administration’s focus on increasing equitable access to care and reducing the stigma around treatment, he said.
“Whether audio-only, video visits, or in-person appointments, physicians provide high-quality, evidence-based care for OUD, including prescribing medication that can save lives,” Dr. Mukkamala noted. “Modernizing rules and regulations for prescribing these medications continues to be of paramount importance.”
The final rule takes effect April 2, with a compliance date of October 2.
Shannon Firth has been reporting on health policy as MedPage Today’s Washington correspondent since 2014.
PUBLIC HEALTH POLICY 16 FEBRUARY 2024
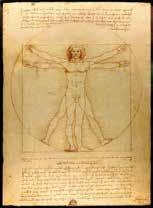
The Aging Vitruvian Man and the Modern Practice of Medicine
By Daniel J. Bressler, MD, FACP
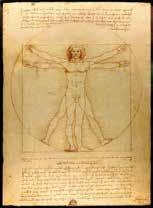
HANGING ON THE
wall behind my office desk is a poster of the famous Vitruvian Man by Leonardo DaVinci. It is sometimes explained as a diagram of human perfection. Living during the Renaissance, Leonardo sketched it in 1490 according to idealized ratios of anatomy that echoed back to Greek and Roman concepts of geometric proportion in nature, architecture, and engineering. In his own notes on the drawing, Leonardo proposed many such ratios: “The length of a man’s outstretched arms is equal to his height”; “from the elbow to the armpit is the eighth part of the human being”; and “from the bottom of the chin to the top of the head is one-eighth of the height of the person.” We know that in real human beings, the ones that come into our offices and clinics, such ratios hold true only as approximations, not hard-and-fast rules. Yet the concept of ideal values (of weight, blood pressure, hemoglobin A1C and other parameters) persists as targets for our patients and for the treatments we offer them.
Leonardo’s Vitruvian Man is young. Based on his face and musculature I’d estimate him to be between 25 and 35, the same age at which most professional athletes peak. This makes sense if one is trying to depict human perfection. Besides the ratios set out by Leonardo in his notes on the work, we might imagine a modern Vitruvian Man would have a blood pressure of 110/70, a body mass index of 25, and an average blood sugar of 80. He would be on no medications and his review of systems would be, as we say, “negative in detail.”
But what happens as VM ages? We know that his muscle mass decreases and his visceral fat increases. His testosterone declines, his lenses stiffen and opacify, his ejection fraction declines, his red blood cell mass dwindles, his prostate enlarges and his hairline recedes. His sister, The Vitruvian Woman, suffers a similar fate with some differences based on the comparatively dramatic decline in her estrogen at menopause. Her skin thins faster than her brother’s, she develops atherosclerosis less quickly and osteoporosis more quickly than he.
Normal aging (one might say that “optimal aging”), even for “The Vitruvians,” is a process of decline. This is the tragic
truth we rarely say out loud to ourselves and to others. The graph of physiologic function over time has a negative slope. The difference between the healthiest and unhealthiest of an aging cohort (your high school graduating class, for example) is simply the angle of that slope. As I tell patients to help persuade them to take steps to control their dyslipidemia or hypertension: “Success means getting your MI at age 95 rather than at age 65.” As part of our understanding of that decline, we have to be mindful that Vitruvian ideals change with age. A PSA of 4.5 is normal for an 80-year-old man but would be the sign of a problem for a 40-year-old. A cataract means something very different in an octogenarian than in a millennial. The systolic blood pressure of 110 in the 25-yearold with a supple vascular system wouldn’t be sufficient to feed the afferent arterioles of the 70-year-old diabetic.
We meet our patients where they are. Rarely do they come to us as a blank slate at the very start of their lives waiting to be instructed and guided as to lifestyle and medical therapies. They come with a host of histories: a “family history,” a “surgical history,” a “social history,” etc. They come with a set of beliefs and habits about diet, exercise, sleep, work, alcohol, and sex. When I first meet a new patient I create in my mind a starting place for our work together by imagining a Vitruvian poster of them (modified for modesty) that becomes the symbolic potential ideal for the medical journey they take under my care. Then we work together to find out how close he or she can come to that ideal using the tools of lifestyle and medical interventions. We personalize their treatment based on their biological, mental, and social idiosyncrasies. And we adapt the treatment and even the goals of treatment as they age. As they change, so too do the targets and objects of our therapies. The annual physical exam is, among other things, the updated imagining of the latest version of their Vitruvian Selves.
There is always an ideal of health toward which we can point our patients. An imaginative appreciation of the Vitruvian Man and Woman reminds us that the ideal can and must evolve as our patients age and change.
Dr. Bressler has practiced outpatient internal medicine in San Diego since 1984. He maintains privileges at Scripps Mercy Hospital, where he served as chairman of the Biomedical Ethics Committee, and at Mission Hills Post Acute Care where he served as medical director. Dr. Bressler has been a member of CMA for 35 years.
SAN DIEGOPHYSICIAN.ORG 17
THE PRACTICE OF MEDICINE
Thriving in ‘A Time Like This’
By Helane Fronek, MD, FACP, FASVLM, FAMWA

POET ROSS GAY RECALLS BEING ASKED HOW
he “can write about flowers at a time like this.” Living in a particularly dangerous, challenging, or conflictual time — “a time like this” — is what many of us are experiencing, as we are told repeatedly we live in a divided society and we feel surrounded by conflict. Yet, if we study history, we find that “times like this” with significant divisions occurred in every age. Conditions may seem worse than we have known them, but humans have encountered and overcome challenges throughout history.
Holding this larger perspective suggests we have strengths and successful coping strategies we can call on again. Conversely, focusing exclusively on what we don’t like can be problematic. It encourages us to emphasize differences, challenges, and discomfort.
Notably, it’s differences, challenges, and discomfort that help us grow. As children, if we avoided challenges we would never have learned to read. Our training and “practice” of
medicine provide ongoing challenges and uncomfortable experiences that continually help us improve our knowledge and skills. If it feels uncomfortable to acknowledge current stressors, like the divisions in society, ask yourself what strengths and strategies have been successful in meeting other uncomfortable situations in your life. Those aspects of yourself are still there, waiting to help you adapt to our current situation.
Another question is what we might gain from our current experience. Becoming curious about what people who are different have to offer is more productive than recoiling or immediately making them wrong. What do they do that I don’t do? What are the benefits of their customs or behavior? What positive role might this play in my own life? And, while there are differences, in what ways are we similar? This is a helpful strategy for living well in a multicultural society.
Gay also highlights a troubling message contained in the question: What you hate is more important than what you love.
An often-forgotten truth is that what we love gets us through tough times by illuminating a path that is hopeful, positive, connects with our values, and engages our strengths. A Sufi story describes a man who came across three bricklayers and asked them what they were doing. The first man angrily retorted, “What does it look like I’m doing? I’m putting one brick on top of the other!” The second smiled and replied, “I’m earning a living to provide food and a home for my family.” The third looked upward with a dreamy look and said, “I’m building a Temple where we will gather to worship, provide community and support each other.” When we connect our actions to our deepest values, they provide meaning and passion for the work we do.
So, as we collectively live through “a time like this,” let’s draw on our strengths to support us through yet another challenging time in life. Let’s lean into our values, bringing meaning and passion to our actions. In so doing, we may shift what seems like a perilous and uncertain time into one of growth and positive action.
Dr. Fronek is an assistant professor of clinical medicine at UC San Diego School of Medicine and a Certified Physician Development Coach, CPCC, PCC.
18 FEBRUARY 2024
PERSONAL AND PROFESSIONAL DEVELOPMENT
Dementia Predicted 10 Years Before Diagnosis
Blood Proteins Identified Those at Risk for All-Cause, Alzheimer’s, or Vascular Dementia
By Judy George
BLOOD PROTEIN PROFILES PREDICTED FUTURE
dementia in healthy adults, a large longitudinal study showed.
Blood samples from more than 50,000 people in the U.K. Biobank showed that four proteins — glial fibrillary acidic protein (GFAP), neurofilament light (NfL), growth differentiation factor-15 (GDF-15), and latent-transforming growth factor beta-binding protein 2 (LTBP2) — consistently were associated with subsequent all-cause dementia, Alzheimer’s disease, or vascular dementia over 14 years, according to Jin-Tai Yu, MD, PhD, of Fudan University in Shanghai, and co-authors.
Combining GFAP or GDF-15 with demographics led to an area under the curve (AUC) of 0.891 for all-cause dementia prediction, 0.872 for Alzheimer’s prediction, and 0.912 for vascular dementia prediction, the researchers reported in Nature Aging. Cognitive tests did not improve predictive power significantly.
People with higher GFAP levels were 2.32 times more likely to develop dementia, Dr. Yu and colleagues said. GFAP and LTBP2 were highly specific for dementia prediction, they added.
GFAP and NfL levels began changing at least 10 years before dementia diagnosis, with concentrations rising most steeply in people with all-cause dementia or Alzheimer’s.
Previous models to detect dementia risk depended largely on cerebrospinal fluid or imaging data, Dr. Yu noted. “The proteomic biomarkers are more [easy] to access and noninvasive, and they can substantially facilitate the application of large-scale population screening,” he said in a statement.
The study adds “to what we know about changes in blood that occur very early in diseases that cause dementia, which will be important for early diagnosis in the future,” wrote Tara Spires-Jones, DPhil, of the University of Edinburgh in Scotland, in a post on the U.K. Science Media Centre.
“However, it is important to note that these are still scientific research studies and that there are currently no blood tests available for routine use that can diagnose dementia with certainty,” Spires-Jones emphasized.
GFAP, a marker of astrogliosis, and NfL, a marker of axonal injury, have predicted dementia symptoms a decade before they emerged in an inherited form of Alzheimer’s disease. Plasma GFAP also has been proposed as a potential biomarker of Alzheimer’s-related pathologies.
The U.K. Biobank findings “appear robust given the knowledge we already have about GFAP being highly associated with Alzheimer’s disease and NfL not being specific for any one dementia,” Amanda Heslegrave, PhD, of University College London, posted on the Science Media Centre site. “[T]he message to take away here is that, for accurate diagnosis and differentiation between dementias, we need focused panels of biomarkers.”
Dr. Yu and colleagues used data from the prospective U.K. Biobank cohort to assess 1,463 plasma proteins. Blood samples were collected between 2006 and 2010. Baseline median age was 58. About 54% of the cohort was female and 94% was white.
The study included 52,645 participants without baseline dementia. Over a median follow-up of 14.1 years, 1,417 people were diagnosed with dementia, including 219 incident cases within 5 years, 833 within 10 years, and 584 beyond 10 years.
The researchers combined the top protein markers associated with incident dementia and demographic variables like age, sex, education, and family history to produce a predictive model for dementia risk over 10 years. They trained the model with data from two-thirds of the cohort (35,096 people) and tested its performance using data from the remaining third.
For 10-year risk, GFAP combined with demographic characteristics predicted all-cause dementia (AUC 0.872) and Alzheimer’s disease (AUC 0.847). Plasma GDF15 combined with demographic characteristics predicted 10-year incident vascular dementia with an AUC of 0.895.
Besides dementia, no significant association emerged between baseline GFAP and risks of other neurodegenerative diseases (HR 1.06, 95% CI 0.94-1.20, P>0.999), neurological disorders (HR 0.94, 95% CI 0.88-1.00, P=0.493) or mental and behavioral disorders (HR 1.05, 95% CI 0.95-1.15, P>0.999), “indicating that GFAP may be specific for dementia,” Yu and co-authors suggested.
The study had several limitations, the researchers noted. Plasma amyloid and tau-related proteins were not included in the analysis. Dementia incidence was lower than what other cohorts have reported, most likely because U.K. Biobank participants were younger at enrollment. The findings also have not been validated in an independent, external cohort.
Judy George covers neurology and neuroscience news for MedPage Today, where this article first appeared.
NEUROLOGY
SAN DIEGOPHYSICIAN.ORG 19
CLASSIFIEDS
PRACTICE ANNOUNCEMENTS
PSYCHIATRIST AVAILABLE! Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla and San Diego. Visit hylermed.com or call
619-707-1554.
VOLUNTEER OPPORTUNITIES
PHYSICIANS: HELP US HELP IMPROVE THE HEALTH
LITERACY OF OUR SAN DIEGO COUNTY COMMUNITIES by giving a brief presentation (30–45 minutes) to area children, adults, seniors, or employees on a topic that impassions you. Be a part of Champions for Health’s Live Well San Diego Speakers Bureau and help improve the health literacy of those with limited access to care. For further details on how you can get involved, please email Andrew. Gonzalez@ChampionsFH.org.
CHAMPIONS FOR HEALTH - PROJECT ACCESS SAN DIEGO: Volunteer physicians are needed in the following specialties: endocrinology, rheumatology, vascular surgery, ENT or head and neck, general surgery, GI, and gynecology. These specialists are needed in all regions of San Diego County to provide short term pro bono specialty care to adults ages 26-49 who are uninsured and not eligible for Medi-Cal. Volunteering is customized to fit your regular schedule in your office. Champions for Health is the foundation of the San Diego County Medical Society. Join hundreds of colleagues in this endeavor: Contact Evelyn. penaloza@championsfh.org or at 858-300-2779.
OPPORTUNITIES
PHYSICIAN
COUNTY OF SAN DIEGO PROBATION DEPT. MEDICAL
DIRECTOR: The Probation Medical Director plays a pivotal role in the medical management team, spearheading the Justice-Involved California Advancing and Innovating MediCal (CalAIM) program. This initiative targets individuals with a history of incarceration, who face elevated risks of harm. California’s groundbreaking approval on January 26, 2023, allows Medicaid services to be extended to aid in their transition back into society. The Medical Director’s responsibilities encompass Cal-AIM’s implementation, oversight of clinical programs, and seamless integration of services for justice-involved youth. This leadership role involves collaboration with various stakeholders, ensuring quality healthcare, behavioral support, and a successful return to the community. https://www.governmentjobs. com/careers/sdcounty/jobs/4193564/medical-directorprobation-23034008u?keywords=medical%20director&pa getype=jobOpportunitiesJobs
PART-TIME CARDIOLOGIST POSITION AVAILABLE: Cardiology office in San Marcos seeking part-time cardiologist. Please send resume to Dr. Keith Brady at uabresearchdoc@yahoo.com.
INTERNAL MEDICINE PHYSICIAN: Federally Qualified Health Center located in San Diego County has an opening for an Internal Medicine Physician. This position reports to the chief medical officer and provides the full scope of primary care services, including diagnosis, treatment, and coordination of care to its patients. The candidate should be board eligible and working toward certification in Internal Medicine. Competitive base salary, CME education, four weeks paid vacation, year one, 401K plan, no evenings and weekends. Monday through Friday, 8:00 am to 5:00 p.m. For more information or to apply, please contact Dr. Keith Brady at: uabresearchdoc@yahoo.com.
FAMILY MEDICINE/INTERNAL MEDICINE PHYSICIAN: San Diego Family Care is seeking a Family Medicine/Internal Medicine Physician (MD/DO) at its Linda Vista location to provide outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810-8700.
MEDICAL CONSULTANT (MD/DO): The County of San Diego is currently accepting applications from qualified candidates for Medical Consultant-Public Health Services. Vacancies are in the Public Health Services, Epidemiology and Immunization Services Branch (EISB) and Tuberculosis (TB) Control and Refugee Health Branch.
Salary: $183,747.20–$204,900.80 annually. An additional 10% for Board Certified Specialty and 15% for relevant sub-specialty. For job posting information visit https:// www.governmentjobs.com/careers/sdcounty?keywords= 23416202PHS.
MEDICAL DIRECTOR, FULL-TIME: FATHER JOE’S VILLAGES: Join us in ending homelessness! We are a dynamic team that runs an FQHC. The Medical Director oversees clinical aspects of the primary care, psychiatry, dental and behavioral health. This position will be a mix of clinic and
admin time and will have direct reports (Dental Director, Director of Behavioral Health, and frontline primary care/ psychiatry providers). Reports to the Chief Medical Officer, who is responsible for all aspects of the clinic. The Medical Director is a counterpart to the Clinic Director (who oversees admin staff, MA/RN team, billing, PSRs, etc.). See FJV Jobs to apply.
SEEKING MEDICAL DIRECTOR : subcontracted position: 4-8 hours per month. Responsibilities: 1. Support case conferences, refractory SUD, co‐occurring conditions, specialty populations. 2. Conduct clinical trainings on issues relevant to staff (e.g., documentation, ASAM Criteria, DSM‐5, MAT, WM, co‐occurring conditions) 3. Provide oversight and clinical supervision. 4. Refer co‐occurring conditions. 5. Lead Quality Improvement functions (e.g., Quality Improvement Projects, clinical team meetings, etc.). 6. Attend annually 5 hours of continuing medical education on addiction medicine. Required by contract with San Diego County BHS, position is for a Physician licensed by CA Medical Board or CA Osteopathic Medical Board. Contact Name: Jennifer Ratoff: e-mail: jratoff@secondchanceprogram.org, phone: 619-839-0950
PSYCHIATRIST SPECIALIST: The County of San Diego is currently accepting applications from qualified candidates. Annual Salary: $258,294.40. Note: An additional 10% is paid for Board Certification, or 15% for Board Certification that includes a subspecialty. Why choose the County? 1. Fully paid malpractice insurance; 2. 13 paid holidays; 3. 13 sick days per year; 4. Vacation: 10 days (1-4 years of service); 15 days (5-14 years of service; 20 days (15+ years); 5. Defined benefit retirement program; 6. Cafeteria-style health plan with flexible spending; 7. Wellness incentives. PsychiatristSpecialists perform professional psychiatric work involving the examination, diagnosis, and treatment of specialty forensics, children/adolescents and or geriatric patients. This is the specialty journey level class in the series that requires a fellowship or experience in child and adolescent psychiatry or forensic psychiatry. For more information visit our website at sandiegocounty.gov/hr or select this link to go directly to the Psychiatrist Specialist application.
PRIMARY CARE PHYSICIAN: Imperial Valley Family Care Medical Group is looking for Board Certified/Board Eligible Primary Care Physician for their clinics in Brawley & El Centro CA. Salaried/full time position. Please fax CV/ salary requirements to Human Resources (760) 355-7731. For details about this and other jobs please go to www. ivfcmg.com
ASSISTANT, ASSOCIATE OR FULL PROFESSOR (HS CLIN, CLIN X, ADJUNCT, IN-RESIDENCE) MED-GASTROENTEROLOGY: Faculty Position in Gastroenterology. The Department of Medicine at University of California, San Diego, Department of Medicine (http://med.ucsd.edu/) is committed to academic excellence and diversity within the faculty, staff, and student body and is actively recruiting faculty with an interest in academia in the Division of Gastroenterology. Clinical and teaching responsibilities will include general gastroenterology. The appropriate series and appointment at the Assistant, Associate or Full Professor level will be based on the candidate’s qualifications and experience. Salary is commensurate with qualifications and based on the University of California pay scales. In-Residence appointments may require candidates to be self-funded. For more information: https://apol-recruit.ucsd. edu/JPF03179 For help contact: klsantos@health.ucsd.edu
DERMATOLOGIST NEEDED: Premier dermatology practice in La Jolla seeking a part-time BC or BE dermatologist to join our team. Busy practice with significant opportunity for a motivated, entrepreneurial physician. Work with three energetic dermatologists and a highly trained staff in a positive work environment. We care about our patients and treat our staff like family. Opportunity to do medical/ surgical and cosmetic dermatology in an updated medical office with state-of-the art tools and instruments. Incentive plan will be a percentage based on production. If you are interested in finding out more information, please forward your C.V. to jmaas12@hotmail.com
INTERNAL MEDICINE PHYSICIAN: Healthcare Medical Group of La Mesa located at 7339 El Cajon Blvd is looking for a caring, compassionate, and competent physician for providing primary care services. We require well-organized and detail-oriented with excellent written and oral communication skills, and excellent interpersonal skills to provide high-quality care to our patients. We provide a competitive salary, paid time off, health insurance, 401K benefits, etc. We provide plenty of opportunities to refine your clinical competency. Our CEO Dr. Venu Prabaker, who has 30 years of teaching experience as a faculty at multiple universities including Stanford, UCSD, USC, Midwestern, Western, Samuel Merritt, Mayo, etc., will be providing teaching rounds once a week. You will also get plenty of opportunities to attend other clinical lectures at many of the 4- to 5-star restaurants in San Diego. We also have a weekly one-hour meeting for all the staff for team building and to create a “family atmosphere” to improve productivity and thereby create a win-win situation for all. Visit us at caremd.us.
RADY CHILDREN’S HOSPITAL PEDIATRICIAN POSI -
TIONS: Rady Children’s Hospital of San Diego seeking board-certified/eligible pediatricians or family practice physicians to join the Division of Emergency Medicine in the Department of Urgent Care (UC). Candidate will work at any of our six UC sites in San Diego and Riverside Counties. The position can be any amount of FTE (full-time equivalent) equal to or above 0.51 FTE. Must have an MD/DO or equivalent and must be board certified/eligible, have a California medical license or equivalent, PALS certification, and have a current DEA license. Contact Dr. Langley glangley@ rchsd.org and Dr. Mishra smishra@rchsd.org.
PER DIEM OBGYN LABORIST POSITION AVAILABLE:
IGO Medical Group is seeking a per diem laborist to cover Labor and Delivery and emergency calls at Scripps Memorial Hospital in La Jolla. 70 deliveries/month. 24-hour shifts preferred but negotiable. Please send inquiries by email to IGO@IGOMED.com.
MEDICAL CONSULTANT, SAN DIEGO COUNTY: The County of San Diego, Health and Human Services Agency’s Public Health Services is looking for a Board Certified Family Practice or Internal Medicine physician for the Epidemiology and Communicable Disease Division. Under general direction, incumbents perform a variety of duties necessary for the identification, diagnosis, and control of communicable diseases within the population. This position works closely with the medical and laboratory community, institutional settings, or hospital control practitioners. Learn more here: https://www.governmentjobs.com/careers/ sdcounty?keywords=21416207
KAISER PERMANENTE SAN DIEGO PER DIEM
PHYSIATRIST: Southern California Permanente Medical Group is an organization with strong values, which provides our physicians with the resources and support systems to ensure they can focus on practicing medicine, connecting with one another, and providing the best possible care to their patients. For consideration or to apply, visit https:// scpmgphysiciancareers.com/specialty/physical-medicinerehabilitation. For questions or additional information, please contact Michelle Johnson at 866-503-1860 or Michelle.S1.Johnson@kp.org. We are an AAP/EEO employer.
PRIMARY CARE PHYSICIAN POSITION: San Diego Family Care is seeking a Primary Care Physician (MD/ DO) at its Linda Vista location to provide direct outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care, and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@ sdfamilycare.org or call us at (858) 810- 8700.
FAMILY MEDICINE OR INTERNAL MEDICINE PHYSICIAN: TrueCare is more than just a place to work; it feels like home. Sound like a fit? We’d love to hear from you! Visit our website at www.truecare.org. Under the direction of the Chief Medical Officer and the Lead Physician, ensure the provision of effective quality medical service to the patients of the Health center. The physician is responsible for assuring clinical procedures are continually and systematically followed, patient flow is enhanced, and customer service is extended to all patients at all times.
PUBLIC HEALTH LABORATORY DIRECTOR: The County of San Diego is seeking a dynamic leader with a passion for building healthy communities. This is a unique opportunity for a qualified individual to work for a Level 3 Public Health Laboratory. The Public Health Services department, part of the County’s Health and Human Services Agency, is a local health department nationally accredited by the Public Health Accreditation Board and first of the urban health departments to be accredited. Public Health Laboratory Director-21226701UPH
NEIGHBORHOOD HEALTHCARE MD, FAMILY PRACTICE AND INTERNISTS/HOSPITALISTS: Physicians wanted, beautiful Riverside County and San Diego County- High Quality Family Practice for a private-nonprofit outpatient clinic serving the communities of Riverside County and San Diego County. Work full time schedule and receive paid family medical benefits. Malpractice coverage provided. Be part of a dynamic team voted ‘San Diego Top Docs’ by their peers. Please click the link to be directed to our website to learn more about our organization and view our careers page at www.Nhcare.org.
PHYSICIAN WANTED: Samahan Health Centers is seeking a physician for their federally qualified community health centers that emerged over forty years ago. The agency serves low-income families and individuals in the County of San Diego in two (2) strategic areas with a high density population of Filipinos/Asian and other low-income, uninsured individuals — National City (Southern San Diego County) and Mira Mesa (North Central San Diego). The physician will report to the Medical Director and provide the full scope of primary care services, including but not limited
20 FEBRUARY 2024
to diagnosis, treatment, coordination of care, preventive care and health maintenance to patients. For more information and to apply, please contact Clara Rubio at (844) 2002426 EXT 1046 or at crubio@samahanhealth.org.
PHYSICIAN POSITIONS WANTED
PART-TIME CARDIOLOGIST AVAILABLE AFTER
7/4/23: Dr. Durgadas Narla, MD, FACC is a noninvasive cardiologist looking to work 1-2 days/week or cover an office during vacation coverage in the metro San Diego area. He retired from private practice in Michigan in 2016 and has worked in a San Marcos cardiologist office for the last 5 years, through March 2023. Board certified in cardiology and internal medicine. Active CA license with DEA, ACLS, and BCLS certification. If interested, please call (586) 2060988 or email dasnarla@gmail.com
PSYCHIATRIST AVAILABLE! Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla & San Diego. Visit hylermed.com or call 619-707-1554.
PRACTICE FOR SALE
GASTROENTEROLOGY GI PRACTICE FOR SALE: Looking to expand or move? Established 25+ years Gastroenterology GI office practice for sale in beautiful San Diego County, California. 500 active strong patient relationships and referral streams. Consistent total gross income of $600,000 for the past couple years; even through the pandemic. Located in a professional medical building with professional contract staff. All records and billing managed by a professional service who can assist with insurance integration. Office, staff & equipment are move-in ready. Seller will assist Buyer to ensure a smooth transition. Being On-Call optional. Contact Ferdinand @ (858) 752-1492 or ferdinand@zybex.com
OTOLARYNGOLOGY HEAD & NECK SURGERY SOLO
PRACTICE FOR SALE: Otolaryngology Head & Neck Surgery solo practice located in the Ximed building on the Scripps Memorial Hospital La Jolla campus is for sale. The office is approximately 3,000 SF with 1 or 2 Physician Offices. It has 4 fully equipped exam rooms, an audio room, one procedure room, one conference room, one office manager room as well as in-house billing section, staff room and a bathroom. There is ample parking for staff and patients with close access to radiology and laboratory facilities. For further information please contact Christine Van Such at 858-354-1895 or email: mahdavim3@gmail.com
OFFICE SPACE / REAL ESTATE
AVAILABLE
MEDICAL OFFICE FOR SALE OR SUBLEASE: A newly remodeled and fully built-out primary care clinic in a highly visible Medical Mall on Mira Mesa Blvd. at corner of Camino Ruiz. The office is approximately 1000 sq ft with 2 fully equipped exam rooms, 1 office, 1 nurse station, spacious and welcoming waiting room, spacious reception area, and ADA accessible restroom. All the furniture and equipment are new and modern design. Ample parking. Perfect for primary care or any specialty clinic. Please contact Nox at 619-7765295 or noxwins@hotmail.com. Available immediately.
EL CAJON RENOVATED MEDICAL OFFICE AVAIL-
ABLE: Recently renovated, turn-key medical office in freestanding single-story unit available in El Cajon. Seven exam rooms, spacious waiting area with floor-to-ceiling windows, staff break room, doctor’s private office, multiple admin areas, manager’s office all in lovely, drought-resistant garden setting. Ample free patient parking with close access to freeways and Sharp Grossmont and Alvarado Hospitals. Safe and secure with round-the-clock monitored property, patrol, and cameras. Available March 1st. Call 24/7 on-call property manager Michelle at the Avocado Professional Center (619) 916-8393 or email help@avocadoprofessionalcenter.com.
OPERATING ROOM FOR RENT: State of the Art AAAASF Certified Operating Rooms for Rent at Outpatient Surgery of Sorrento. 5445 Oberlin Drive, San Diego 92121. Ideally located and newly built 5 star facility located with easy freeway access in the heart of San Diego in Sorrento Mesa. Facility includes two operating rooms and two recovery bays, waiting area, State of the Art UPC02 Laser, Endoscopic Equipment with easy parking. Ideal for cosmetic surgery. Competitive Rates. Call Cyndy for more information 858.658.0595 or email Cyndy@roydavidmd.com
PRIME LOCATION – MEDICAL BUILDING LEASE OR
OWN OPPORTUNITY IN LA MESA: Extraordinary opportunity to lease or lease-to-own a highly visible, freewayoriented medical building in La Mesa, on Interstate 8 at the 70th Street on-ramp. Immaculate 2-story, 7.5k square foot property with elevator and ample free on-site parking (45 spaces). Already built out and equipped with MRI/CAT machine. Easy access to both Alvarado and Sharp Grossmont Hospitals, SDSU, restaurants, and walking distance to 70th St Trolley Station. Perfect for owner-user or investor. Please contact Tracy Giordano [Coldwell Banker West, DRE# 02052571] for more information, (619) 987-5498.
CLASSIFIEDS
POWAY MEDICAL OFFICE SPACE FOR LEASE
2/1/2024: Fully built out, turnkey 1257 sq ft ADA-compliant suite for lease. Great location in Pomerado Medical/ Dental Building, next to Palomar Med Center Poway campus. Building restricted to medical/allied health/dental practices, currently houses ~26 suites. Ideal for small health practice as primary or satellite location. Lease includes front lobby, reception area, restrooms, large treatment area, private treatment/exam rooms. Located on second floor, elevator/stair access. Bright, natural lighting; unobstructed views of foothills. On-site parking; nearby bus service. Flexible lease terms available from 3-5 years at fair market rate. Contact Debbie Summers at debjsummers3@gmail. com (858) 382-8127.
KEARNY MESA OFFICE TO SUBLEASE/SHARE: 5643
Copley Dr., Suite 300, San Diego, CA 92111. Perfectly centrally situated within San Diego County. Equidistant to flagship hospitals of Sharp and Scripps healthcare systems. Ample free parking. Newly constructed Class A+ medical office space/medical use building. 12 exam rooms per half day available for use at fair market value rates. Basic communal medical supplies available for use (including splint/ cast materials). Injectable medications and durable medical equipment (DME) and all staff to be supplied by individual physicians’ practices. 1 large exam room doubles as a minor procedure room. Ample waiting room area. In office x-ray with additional waiting area outside of the x-ray room. Orthopedic surgery centric office space. Includes access to a kitchenette/indoor break room, exterior break room and private physician workspace. Open to other MSK physician specialties and subspecialties. Building occupancy includes specialty physicians, physical therapy/occupational therapy (2nd floor), urgent care, and 5 OR ambulatory surgery center (1st floor). For inquiries contact kdowning79@gmail.com and mgamboa@ortho1.com for more information. Available for occupancy projected as February 2024.
LA JOLLA/UTC OFFICE TO SUBLEASE OR SHARE:
Modern upscale office near Scripps Memorial, UCSD hospital, and the UTC mall. One large exam/procedure room and one regular-sized exam room. Large physician office for consults as well. Ample waiting room area. Can accommodate any specialty or Internal Medicine. Multiple days per week and full use of the office is available. If interested please email drphilipw@gmail.com
ENCINITAS MEDICAL SPACE AVAILABLE: Newly updated office space located in a medical office building. Two large exam rooms are available M-F and suitable for all types of practice, including subspecialties needing equipment space. Building consists of primary and specialist physicians, great for networking and referrals. Includes access to the break room, bathroom and reception. Large parking lot with free parking for patients. Possibility to share receptionist or bring your own. Please contact coastdocgroup@gmail.com for more information.
NORTH COUNTY MEDICAL SPACE AVAILABLE: 2023
W. Vista Way, Suite C, Vista CA 92082. Newly renovated, large office space located in an upscale medical office with ample free parking. Furnishings, decor, and atmosphere are upscale and inviting. It is a great place to build your practice, network and clientele. Just a few blocks from Tri-City Medical Center and across from the urgent care. Includes: multiple exam rooms, access to a kitchenette/break room, two bathrooms, and spacious reception area all located on the property. Wi-Fi is not included. For inquiries contact hosalkarofficeassist@gmail.com or call/text (858)740-1928.
PHYSICIAN OFFICE SPACE FOR LEASE. 1500 Sq ft.
3 exam room. Large private office. Large reception area and patient prep room. New upgraded flooring. Private entrance. Located in Rancho Bernardo in prime central location. Easy access to interstate 15. Palomar /Pomerado within 10 min. Security card access during off hours. $2,500/month. Contact: (619) 585-0476. Ask for Peg.
HILLCREST OFFICE TO SUBLEASE OR SHARE: Gorgeous office located across from Scripps Mercy hospital. Office is approximately 2000 sq. ft. with procedure/effusion room. Office is fully staffed and looking to add a new provider. We currently have Rheumatology/Pulmonary/Allergy specialists but can accommodate any specialty or Internal Medicine. Multiple days per week and full use of office is available. If interested please reach out to Melissa Coronado at Melissa@sdpulmonary.com or call (619) 819-7224.
SUBLEASE AVAILABLE: Sublease available in Del Mar off 5 freeway. Share rent. 2100 sq ft office in professional building. Utilities included. Great opportunity in a very desirable area. 858-342-3104.
CHULA VISTA MEDICAL OFFICE: Ready with 8 patient rooms, 2,000sf, excellent parking ratios, Lease $4,000/ mo. No need to spend a penny. Call Dr. Vin, 619-405-6307 vsnnk@yahoo.com
OFFICE SPACE AVAILABLE IN BANKERS HILL: Approximately 500sq feet suite available to lease, includes private bathroom. Located at beautiful Bankers Hill. For more details, please call Claudia at 619-501-4758.
OFFICE AVAILABLE IN MISSION HILLS, UPTOWN
SAN DIEGO: Close to Scripps Mercy and UCSD Hillcrest. Comfortable Arts and Crafts style home in upscale Mission Hills neighborhood. Converted and in use as medical / surgical office. Good for 1-2 practitioners with large waiting and reception area. 3 examination rooms, 2 physician offices and a small kitchen area. 1700 sq. ft. Available for full occupancy in March 2022. Contact by Dr. Balourdas at greg@thehanddoctor.com.
OFFICE SPACE IN EL CENTRO, CA TO SHARE: Office in El Centro in excellent location, close to El Centro Regional Medical Centre Hospital is seeking Doctors of any specialty to share the office space. The office is fully furnished. It consists of 8 exam rooms, nurse station, Dr. office, conference room, kitchenette and beautiful reception. If you are interested or need more information please contact Katia at 760-427-3328 or email at Feminacareo@gmail.com
OFFICE SPACE / REAL ESTATE WANTED
MEDICAL OFFICE SPACE WANTED IN HILLCREST/ BANKERS HILL AREA. Mercy Physicians Medical Group (MPMG) specialist is looking for office space near Scripps Mercy Hospital. Open to lease or share office space, full time needed. Please respond to rjvallonedpm@sbcglobal. net or 858-945-0903.
MEDICAL EQUIPMENT / FURNITURE FOR SALE
UROLOGY OFFICE CLOSING 6/2023—EQUIPMENT
AVAILABLE: Six fully furnished exam rooms including tables (2 bench, 3 power chair/table, 1 knee stirrup), rolling stools, lights, step stools, patient chairs. Waiting room chairs, tables, magazine rack. Specialty items—Shimadzu ultrasound, SciCan sterilizer, Dyonics camera with Sharp monitor, Medtronic Duet urodynamics with T-DOC catheters, Bard prostate biopsy gun with needles, Cooper Surgical urodynamics, Elmed ESU cautery, AO 4 lens microscope. RICOH MP-3054 printer with low print count. For more information contact: r.pua@cox.net.
NON-PHYSICIAN POSITIONS AVAILABLE
RESEARCH SCIENTISTS: (non-tenured, Assistant, Associate or Full level): The University of California, San Diego campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ORU/index.html are conducting an open search. Research Scientists are extramurally funded, academic researchers who develop and lead independent creative research programs similar to Ladder Rank Professors. They are expected to serve as Principal Investigators on extramural grants, generate high caliber publications and research products, engage in university and public service, continuously demonstrate independent, high quality, significant research activity and scholarly reputation. Appointments and duration vary depending on the length of the research project and availability of funding. https://apol-recruit.ucsd.edu/JPF03713/apply
PROJECT SCIENTISTS: Project Scientists (non-tenured, Assistant, Associate or Full level): The University of California, San Diego, Office of Research Affairs https://research. ucsd.edu/, in support of the campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd. edu/ORU/index.html is conducting an open search. Project Scientists are academic researchers who are expected to make significant and creative contributions to a research team, are not required to carry out independent research but will publish and carry out research or creative programs with supervision. Appointments and duration vary depending on the length of the research project and availability of funding. https://apol-recruit.ucsd.edu/JPF03262/apply
OFFICE MANAGER: 1. Hiring, Training, Managing staff on procedures/policies. Monitors continuing compliance and office statistics. Oversee stocking/maintenance of supplies, retail. Equipment/ facilities management. Daily bookkeeping, collections. 2. Ensure smooth/efficient patient flow with increasing production/collections. 3. Create a friendly environment where patients expectations are exceeded, where staff can work together as a team. 4. Ensure staff working at maximum productivity/efficiency. Salary: 60-70K depending on experience/qualifications. Benefits: healthcare reimbursement, PTO, retirement, employee discount, bonuses, commission. Contact: info@manageyourage.com
ASSISTANT PUBLIC HEALTH LAB DIRECTOR: The County of San Diego is currently accepting applications for Assistant Public Health Lab Director. The future incumbent for Assistant Public Health Lab Director will assist in managing public health laboratory personnel who perform laboratory activities for the purpose of identifying, controlling, and preventing disease in the community, as well as assist with the development and implementation of policy and procedures relating to the control and prevention of disease and other health threats. Please visit the County of San Diego website for more information and to apply online.
SAN DIEGOPHYSICIAN.ORG 21

San Diego County Medical Society 8690 Aero Drive, Suite 115-220 San Diego, CA 92123 [ Return Service Requested ] $5.95 | www. SanDiegoPhysician.org PRSRT STD U.S. POSTAGE PAID DENVER, CO PERMIT NO. 5377