FP
MISSOURI FAMILY PHYSICIAN
VOLUME 42, ISSUE 3

MISSOURI FAMILY PHYSICIAN
VOLUME 42, ISSUE 3
aExample cutoff from Abbott Laboratories; adult ALP ranges are lab specific and may vary.
References: 1. Bishop N, et al. Arch Dis Child. 2016;101(6):514-515. 2. Alkaline phosphatase [package insert]. Abbott Park, IL: Abbott Laboratories; 2007. 3. Offiah AC, et al. Pediatr Radiol. 2019;49(1):3-22.
4. Colantonio DA, et al. Clin Chem. 2012;58(5):854-868.
Colantonio DA, et al. Clin Chem. 2012;58(5):854-868.
Alkaline Phosphatase (ALP) may not be flagged if your laboratory does not use
LOW Alkaline Phosphatase (ALP) may not be flagged if your laboratory does not use age- and sex-adjusted reference intervals in children when testing ALP activity1
reference intervals in children when testing ALP activity1

and sex-adjusted ALP reference ranges, U/L2,3
0-14d15d-<1y1-<10y10-<13y13-<15y15-<17y17-<19y 0-14d15d-<1y1-<10y10-<13y13-<15y15-<17y17-<19y Adults
0-14d15d-<1y1-<10y10-<13y13-<15y15-<17y17-<19y 0-14d15d-<1y1-<10y10-<13y13-<15y15-<17y17-<19y Adults
NOTE: Graph adapted from the Canadian Laboratory Initiative on Pediatric Reference Intervals (CALIPER) project. 2 Caliper samples from 1072 male and 1116 female participants (newborn to 18 years) were used to calculate age- and sex-specific reference intervals. No variation in ALP based on ethnic differences was observed. Reference intervals shown were established on the Abbott ARCHITECT c8000 analyzer. a Adult interval provided by the Abbott ARCHITECT ALP product information sheet is for females >15 and males >20 years of age. For younger ages, Abbott does not provide lower limits of normal. 3
NOTE: Graph adapted from the Canadian Laboratory Initiative on Pediatric Reference Intervals (CALIPER) project. 2 Caliper samples from 1072 male and 1116 female participants (newborn to 18 years) were used to calculate age- and sex-specific reference intervals. No variation in ALP based on ethnic differences was observed. Reference intervals shown were established on the Abbott ARCHITECT c8000 analyzer. a Adult interval provided by the Abbott ARCHITECT ALP product information sheet is for females >15 and males >20 years of age. For younger ages, Abbott does not provide lower limits of normal. 3
LOW Alkaline Phosphatase (ALP) is hallmark of Hypophosphatasia.1
LOW Alkaline Phosphatase (ALP) is hallmark of Hypophosphatasia.1
BOARD CHAIR John Burroughs, MD (Kansas City)
PRESIDENT Kara Mayes, MD, FAAFP (St. Louis)
PRESIDENT-ELECT Afsheen Patel, MD (Kansas City)
VICE-PRESIDENT Natalie Long, MD (Columbia)
SECRETARY/TREASURER Lisa Mayes, DO (Macon)
DISTRICT 1 DIRECTOR Arihant Jain, MD (Cameron)
ALTERNATE Vacant
DISTRICT 2 DIRECTOR Vacant
ALTERNATE Eric Lesh, DO (Kirksville)
DISTRICT 3 DIRECTOR Dawn Davis, MD (St. Louis) DIRECTOR Lauren Wilfling, MD (St. Louis)
ALTERNATE Christian Verry, MD (St. Louis)
DISTRICT 4 DIRECTOR Jennifer Scheer, MD, FAAFP (Gerald)
ALTERNATE Jennifer Allen, MD (Hermann)
DISTRICT 5 DIRECTOR Amanda Shipp, MD (Versailles)
ALTERNATE Misty Todd, MD (Sedalia)
DISTRICT 6 DIRECTOR David Pulliam, DO, FAAFP (Higginsville)
ALTERNATE Justin Cramer, MD, FAAFP (Marshall)
DISTRICT 7 DIRECTOR Beth Rosemergey, DO, FAAFP (Kansas City) DIRECTOR Jacob Shepherd, MD, FAAFP (Lee’s Summit)
ALTERNATE Ed Kraemer, MD (Lee’s Summit)
DISTRICT 8 DIRECTOR Andi Selby, DO (Branson)
ALTERNATE Barbara Miller, MD (Neosho)
DISTRICT 9 DIRECTOR Douglas Crase, MD (Licking)
ALTERNATE Vacant
DISTRICT 10 DIRECTOR Gordon Jones, MD (Sikeston)
ALTERNATE Jenny Eichhorn, MD (Jackson)
DIRECTOR AT LARGE Wael Mourad, MD (Jefferson City) Krishna Syamala, MD (St. Louis)
Wesley Goodrich, DO, MPH, UMKC
Kelly Dougherty, MD, Mercy (Alternate)
Karstan Luchini, KCU Joplin
Abby Crede, UMKC (Alternate)
Kate Lichtenberg, DO, MPH, FAAFP, Delegate
Peter Koopman, MD, FAAFP, Delegate
Sarah Cole, DO, FAAFP, Alternate Delegate
Jamie Ulbrich, MD, FAAFP, Alternate Delegate
MAFP STAFF
EXECUTIVE DIRECTOR Kathy Pabst, MBA, CAE
ASSISTANT EXECUTIVE DIRECTOR Bill Plank, CAE
MEMBER COMMUNICATIONS AND ENGAGEMENT Brittany Bussey
The information contained in Missouri Family Physician is for informational purposes only. The Missouri Academy of Family Physicians assumes no liability or responsibility for any inaccurate, delayed, or incomplete information, nor for any actions taken in reliance thereon. The information contained has been provided by the individual/organization stated. The opinions expressed in each article are the opinions of its author(s) and do not necessarily reflect the opinion of MAFP. Therefore, Missouri Family Physician carries no respsonsibility for the opinion expressed thereon.
Missouri Academy of Family Physicians, 722 West High Street Jefferson City, MO 65101 • p. 573.635.0830 • f. 573.635.0148
Website: mo-afp.org • Email: office@mo-afp.org
Obstetrics and Gynecology
Updated Legislation Provides Further Protections for Breastfeeding Patients
Strategies to Address Stigma on People with Opioid Use Disorder During Pregnancy
AAFP Women’s Reproductive Health Project Advisory Group
Many Missourians Confused About the Legality of Birth Control
Cardiovascular Disease: A Hidden Threat to Maternal Health
Conference Prepares Residents and Students for Success
Missouri Family Physician Advocates Visit Capitol Hill
Todd Shaffer, MD, MBA, FAAFP, DABFM, Candidate for AAFP President-Elect
The Importance of Family Medicine in Missouri
July 20
Virtual Type 2 Diabetes ECHO
https://PeerView.com/865/T2D-ECHO
August 10 & 24
Virtual Type 2 Diabetes ECHO
https://PeerView.com/865/T2D-ECHO
October 20-22
Physician Wellness Seminar
Margaritaville at Lake of the Ozarks
https://www.maops.org/general/custom.asp?page=wellnessseminar
November 10-11
31st Annual Fall Conference & Annual Meeting
Big Cedar Lodge, Ridgedale, MO
https://www.mo-afp.org/cme-events/afc/
November 12
MAFP Commission and Board of Directors Meetings
Big Cedar Lodge, Ridgedale, MO
Welcome to the 2023 Missouri Family Physician Obstetrics and Gynecology issue! Our Member Services Commission and amazing MAFP team has once again done an amazing job in sowing and reaping a collection of articles covering a diverse set of women’s health issues. I hope you are looking forward to this issue as much as I am.
The topics for the Missouri Family Physician are set more than a year in advance of publication, so it is really quite remarkable how timely this issue is in our state and country. Women’s health has come to the forefront of discussion in America which is an opportunity to address the challenges we face in providing OB/GYN care to our communities. Legislation is being introduced and passed in various states regarding pre-natal care, pregnancy termination, post-partum care, and birth control. Unfortunately, access to health care has not improved for women in Missouri over the past 10 years with maternal morbidity and mortality rates higher than the US average. The article from the Missouri Department of Health and Senior Services (page 12), provides a state of maternal care in Missouri with supporting data. With that in mind, it is imperative that we, as family physicians, provide compassionate, thoughtful, and comprehensive care for women (as well as children and men) in our practices. Up to date education helps us strive for that goal.
This issue on Obstetrics and Gynecology also causes me to reflect on the wonders of the

plasticity of a career in family medicine. I have come to the acceptance (begrudgingly) that I have been in practice for many more years than what I have in front of me. As I have aged and grown, so has my practice. As a young-pup doctor fresh out of residency, my patient base reflected my life at the time. Just as our home was filling with children, so was my practice. We naturally attract patients who we resonate with, and we resonate with those who face the same issues in life that we do. As my family aged, so did my office practice. I gradually saw less newborns, less young children, and, as a male physician, less female patients. As my work increased in nursing homes and hospice, my patient base aged considerably. But that made it even more important to keep up with evidence-based, current care in those topics that I saw less of in my practice (and my life!). So, I will be diving into the articles in this issue. Keeping informed helps keep our practices more welcoming, more vibrant, and more accurate (just to show my age, yes, I still use oxford commas and two spaces after a period).
I hope you enjoy this issue of the Missouri Family Physician Once again, thank you for all that you do for our patients, our communities, and our state. Reach out to our wonderful MAFP team for any concerns or assistance. They really are amazing. Take care of yourselves, and we hope to see you this November at our final conference at Big Cedar. Register on the back cover!
Mission Statement:
The Missouri Academy of Family Physicians is dedicated to optimizing the health of the patients, families and communities of Missouri by supporting family physicians in providing patient care, advocacy, education and research.
WOMEN’S HEALTH HAS COME TO THE FOREFRONT OF DISCUSSION IN AMERICA WHICH IS AN OPPORTUNITY TO ADDRESS THE CHALLENGES WE FACE IN PROVIDING OB/GYN CARE TO OUR COMMUNITIES



 Angie Whitesell, MD, FAAFP Mercy Clinic – Lockwood, MO
Casey Fogarty, MS4 University of Missouri – Columbia
Emily Schaff, MS4 University of Missouri – Columbia
Angie Whitesell, MD, FAAFP Mercy Clinic – Lockwood, MO
Casey Fogarty, MS4 University of Missouri – Columbia
Emily Schaff, MS4 University of Missouri – Columbia
Though the advantages of feeding with breast milk are well documented in medical literature, legal support for breastfeeding persons is relatively new. The Fair Labor Standards Act (FLSA) was first passed in 1938, establishing an hourly minimum wage, maximum hours per workweek, and minimum working age2 . National policy did not discuss nursing parents until 2010, when the Patient Protection and Affordable Care Act (ACA) amended the FLSA to require employers of more than 50 employees to provide a designated time and location, other than a bathroom, for expression of breast milk for one year following a child’s birth8. The ACA also required insurance policies created after August 1, 2012 to provide coverage for equipment rental, counseling, and prenatal and postnatal lactation support8
The ACA made considerable strides in the promotion of breastfeeding, but clear gaps still emerged in coverage. There were two major problems with gaining coverage for all people. “Grandfathered” insurance plans existing before the passage of the ACA were exempt from these requirements. Secondly, the FLSA did not cover all workers. In addition to excluding significant portions of the population, legislation did not define the equipment to be rented and counseling supports, leaving these details up to the interpretation of individual states3 .
State laws across the country vary regarding breastfeeding, and prior to the ACA, they were the primary form of legal protection for lactating persons. Like many other states, Missouri has specific legislation exempting breastfeeding from public indecency laws5. Breast and bottle feeding assistance and training were made requirements of postpartum care by H.B. 1069 in 19967. H. B. 1320, effective in August 2014, allows any nursing mother to be excused from jury duty upon request with a completed written statement from a physician4
The most recent update to Missouri legislation was in August 2021, when the state legislature passed a new bill requiring public school districts to “provide accommodations for lactating employees, teachers, and students to express breast milk, breastfeed a child, or address other needs relating to breastfeeding.” It also established a minimum of 3 opportunities throughout the school day to be offered for these activities and laid out requirements for the accommodations to include ventilation, a door that may be locked, a work surface and chair, conveniently placed electrical outlets, and be located in close proximity to a refrigerator for breast milk and sink with running water.
The requirements went into effect July 1, 2022. Missouri does not have an existing policy specifying protected locations or time for breastfeeding workers in other fields of employment.
The gaps in state and national coverage have been improved through the passage of the national PUMP for Nursing Mothers Act, a bill that had significant bipartisan support in both the U.S. House and Senate. This new legislation introduces further protections for breastfeeding persons including the coverage of nearly 9 million more individuals, the clarification that pumping time be paid if employees are not fully relieved from duty, and the opportunity to seek monetary remedies if employers fail to comply with these policies10
Prior to passing this bill, nearly 1 in 4 breastfeeding persons were without federal protections for pumping during their workday10 This bill expands coverage to include nurses, teachers, farmworkers, and eventually railway workers. The bill further clarifies that these protections apply to all breastfeeding individuals, regardless of gender. In addition, employers of all sizes are now required to follow legislation with the exception of providing break space in circumstances of “undue hardship”. This circumstance is extremely rare but provides leniency for employers who would experience significant difficulty or expense from providing this service.
The PUMP for Nursing Mother Act was implemented in several stages. The first, requiring sufficient lactation facilities and break time, went into effect on December 29, 2022. The second, which expanded provisions to allow for monetary compensation for employees if employers failed to comply with requirements, went into effect on April 28, 2023. There is a 3-year delay in implementation for certain rail careers and motorcoach employees. Current legislation notably still does not apply to pilots or flight attendants due to significant industry pushback.
Missouri currently provides resources to employers in the form of the Breastfeeding Friendly Worksite Program that can aid in adherence to this new legislation. The program works to help businesses become nursing friendly workspaces by identifying and setting up a suitable private room for feeding, scheduling appropriate breaks for nursing employees, and reviewing written policies9. Businesses can then be evaluated on their level of support and awarded gold, silver, or bronze awards for their efforts which are tracked in a complete list of Breastfeeding Friendly Businesses9
Clinicians should educate lactating patients concerned about returning to work of this new legislation as it may increase adherence and, if necessary, provide resources for employers to help with adhering to these new laws.
References on page 30.
Prior to passing this bill, nearly 1 in 4 breastfeeding persons were without federal protections for pumping during their workday
 Kento Sonoda, MD, FASAM, AAHIVS Department of Family and Community Medicine Saint Louis University School of Medicine
Angela Patel, M4 Saint Louis University School of Medicine
Kento Sonoda, MD, FASAM, AAHIVS Department of Family and Community Medicine Saint Louis University School of Medicine
Angela Patel, M4 Saint Louis University School of Medicine
More than 5 million people are living with opioid use disorder in the United States.1 Of pregnant people in the country, 6.6% reported prescription opioid use during pregnancy, and 21.2% of these pregnant people reported misuse.2 Opioid use disorder during pregnancy has several maternal and fetal health risks including fatal overdose, intrauterine growth restriction, preterm birth, low birth weight, intrauterine fetal demise, and neonatal abstinence syndrome (NAS).3 Between 2010 and 2017, the estimated rate of NAS and maternal opioid-related diagnoses significantly increased from 4.0 to 7.3 and 3.5 to 8.2 per 1,000 birth hospitalizations, respectively.4 Notably, only 11% of patients with opioid use disorder received any treatment in the past year.1 Family physicians can play an essential role in bridging the treatment gap by providing integrated prenatal care and treatment for opioid use disorder.
Many people still struggle to seek care for their substance use disorder despite the significant growth and advancement of treatment. Only 6.3% of people aged 12 or older with opioid use disorder or alcohol use disorder received any treatment in the past year.1 Stigma around substance use disorder is one of the key factors deterring people from seeking medical care.5 Therefore, it is an urgent task for all healthcare professionals to address the stigma around substance use and the true tolls of addiction in order to close the gap in care.6
Pregnant people with a substance use disorder suffer from additional stigma as their substance use disorder can negatively impact their fetus in utero, often leading to punitive measures.7-9 The following section will introduce practical strategies to mitigate the stigma around opioid use disorder in pregnancy.
• Use non-stigmatized language
• Ensure the psychological safety
and unique qualities of every individual. For instance, one can say “a person with opioid use disorder” instead of “an addict.” As patients interact with all staff members at your clinic, it is important to ensure that everyone is on the same page regarding appropriate language. You can find more information on the website entitled “Words Matter – Terms to Use and Avoid When Talking About Addiction,” from National Institute on Drug Abuse.11
2. Ensure psychological safety
People with opioid use disorder may have had traumatic encounters with the healthcare system. Therefore, it is vital for our clinic to create a welcoming and psychologically safe environment where they can disclose what they are struggling with and feel respected in the process. By creating a psychologically safe space, the door remains open for them to return to your clinic whenever they are ready to re-engage, even if they miss a followup visit. To ensure psychological safety, family physicians and all staff members should talk in a non-judgmental way and work to understand obstacles that may not be under their control (i.e., transportation and financial barriers), emotions (i.e., shame and guilt), and negative cultural attitudes (i.e., stigma).
3. Set the appropriate goal
Healthcare workers tend to set their immediate goal as abstinence. However, it may not be a reasonable or attainable goal for patients with opioid use disorder. Setting realistic shortand long-term goals with your patients through a harm reduction approach is critically important. For those who inject drugs every day, abstinence may be far from where they are and can be a challenging goal in the short term. Family physicians should approach their patients using shared decision making and traumainformed care. In that way, patients will feel understood and respected in their treatment for opioid use disorder in pregnancy.
4. Understand addiction
It is a common misunderstanding that people with opioid use disorder use the drugs to become euphoric or take pleasure. It may be true in some situations, but it is not always the case. Some patients with opioid use disorder continue to take drugs to feel “normal” and to avoid withdrawal symptoms like nausea, vomiting, diarrhea, and muscle aches (Figure 1). A proper understanding of addiction will improve how family physicians communicate with a person with opioid use disorder during pregnancy.
• Set the appropriate goal
• Understand addiction
• Apply biopsychosocial model
Words matter. Stigmatized language used in medical records can influence how clinicians treat their patients.10 All healthcare professionals should use person-centered, medically accurate terminology to describe people with opioid use disorder. Personcentered language refers to choosing words that honor the dignity
5. Apply a biopsychosocial model

Addiction treatment requires not only biological care but also psychological and social care. A multidisciplinary team approach is needed and supported by the American Society of Addiction Medicine (ASAM) to comprehensively approach complicated needs in care.12 An interdisciplinary team approach can effectively address opioid use disorder and common co-occurring conditions including depression, anxiety, and chronic pain.13-15 In addition, the integrated care reduces the transportation burden, and pregnant people with opioid use disorder have the potential to thrive in their trusted healthcare setting.
References on page 30.


Over the past year, I had the opportunity to represent Missouri on the AAFP’s Women’s Reproductive Health Project Advisory Group (PAG). I was joined by four other family physicians from Connecticut, New York, North Carolina, and South Dakota, representing states with vastly different legal climates after Roe v. Wade was overturned in 2022. In short, we were tasked with helping family physicians seeking to provide comprehensive reproductive healthcare while navigating a changing landscape.
We met virtually throughout the year, discussing changes we were seeing in our states. These ranged from patients and their concerns to resident recruitment, training, and retention issues. We have noticed a workforce shift as well, as obstetriciangynecologists transition to states with fewer legal limitations on a physician’s ability to provide care to their patients. With this comes an even greater need for family medicine physicians to fill gaps in care left by subspecialists leaving a region.
Through this PAG, we have been able to direct feedback to the AAFP from our experiences. The AAFP has launched an updated website entitled Center for Women’s Health, which is housed within the AAFP site which also includes women’s health resources. This can be found at https://www.aafp. org/family-physician/patient-care/care-resources/ womens-health/women-s-health-resources. html#reprohealth, or by scanning the QR code.
Serving on this PAG gave me the opportunity to meet with physicians practicing in different states, see how others are adapting to ongoing changes in how we deliver care, and fully realize the importance of advocacy for our patients and our practices.
Scan for more info and resources.
 Andi Selby, DO Branson, MO
Andi Selby, DO Branson, MO

There is considerable confusion about the legality of birth control in Missouri and many are worried about future access, according to a new survey (https://mfhc.org/newsevents/press-releases.html/ article/2023/06/20/manymissourians-confusedabout-the-legality-of-birthcontrol) of state residents.
• One in four (25%) Missourians do not believe or do not know that birth control pills the most used form of contraception in the U.S. are legal in the state.
• More than half (53%) do not believe or do not know that emergency contraception is legal.
• Four in 10 (40%) do not believe or do not know that IUDs are legal.
• 65% incorrectly believe or do not know that it is legal for minors to get birth control.
In addition, many in Missouri are concerned about the future availability of birth control. Fully half of survey respondents (50%) including 44% of Republicans, 48% of Independents, and 66% of Democrats are concerned that elected officials in Missouri will enact laws that restrict people from getting the birth control method they want.
The survey of 1,000 Missouri residents aged 18-35 was conducted this year between April 27 and May 3 by AYTM, an independent research organization as part of the Missouri-based The Right Time initiative. Through this effort, health centers across the state are improving access to contraception by providing free or low-cost birth control in 34 locations. The Right Time provides training, assistance, and funding to expand access to the full range of contraceptive methods. The initiative is focused on offering patients same-day access to all methods of birth control and has resources that make it easier for people in Missouri, including those who are uninsured or underinsured, to receive quality contraceptive services.

Several other themes emerged from the survey of Missouri residents. They include:
Support for access to all methods of contraception remains strong. Despite the confusion about the legality of birth control and concern about future access, an overwhelming majority (84%) of those in Missouri including 82% of Republicans, 90% of Democrats, and 85% of Independents support people aged 18-35 having access to all methods of birth control.
Missourians want the state legislature to act on birth control. About seven in 10 survey respondents (72%) including 74% of Republicans, 72% of Democrats, and 73% of Independents think the Missouri State Legislature should pass policies that make birth control more affordable and accessible. However, fully half (50%) of respondents—including 44% of Republicans, 66% of Democrats, and 48% of Independents— are concerned that elected officials in Missouri will enact laws that restrict people getting a birth control method they want. Moreover, more believe that elected officials in Missouri are not supportive of birth control (36%) than those who believe legislators are supportive (26%).
Confusion and conflation surrounds emergency contraception. Although six in 10 say they are knowledgeable about emergency contraception pills, more than half (54%) either do not know or do not believe that emergency contraception pills are different from the abortion pill.
Access to birth control remains a challenge for many. One in four (25%) respondents overall—and 37% of Hispanic respondents— report cost or insurance has made it hard for them to get the method of birth control they want to use. In addition, more Missourians say they do not know how to get birth control online (48%) than those that say they are aware of online ordering (39%).
The Right Time initiative is improving information about, and access to, quality contraceptive services by reducing costs and improving access and knowledge. TheRightTime.org provides residents of Missouri with access to free and low-cost birth control, trustworthy information on contraceptive methods, and video testimonials about services and birth control. The Right Time is an initiative of Missouri Foundation for Health and is led by Missouri Family Health Council, Inc.


The issue of maternal mortality (MM) continues to be a persistent public health concern in the state of Missouri. From 2017-2020, the pregnancy-related mortality ratio in Missouri was 30 deaths per 100,000 live births. The ratio of MM in the United States overall is three-to-four times higher than many other high income nations, and continues to increase. From 2017-2020, Missouri’s Pregnancy Associated Mortality Review (PAMR) board, the state’s maternal mortality review committee, determined that cardiovascular disease was the leading cause of pregnancy-related death in the state (32%), followed by mental health conditions, including substance use disorder (31%). During this time period, cardiovascular disease was the third leading cause of death (9%) for Missouri’s childbearing age population (females aged 15-44), after accidental injuries, and cancer.
Studies have found that there are concerns with the quality of death certificate data regarding the cause of death information. The PAMR board is a multidisciplinary committee that performs comprehensive reviews of pregnancy-associated deaths, deaths to a Missouri resident during pregnancy up to one year postpartum regardless of cause. The board uses data gathered from medical records, vital records, social media histories, and other sources.
Karen Harbert, MPH
 Lead Maternal-Child Health Epidemiologist MO Dept. of Health and Senior Services
Lead Maternal-Child Health Epidemiologist MO Dept. of Health and Senior Services
The board determines if a death was pregnancy-related, meaning that it was from a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiological effects of pregnancy; or if it was pregnancy-associated, but not related. Cases where the relatedness could not be determined are counted as associated, not related in this analysis. As part of the case review process, the PAMR board evaluates the underlying cause of death for pregnancy-related deaths. This evaluation provides an opportunity to look at the times the board disagreed with the data entered on the death certificate and what they determined was the actual underlying cause in order to illuminate possible areas of concern.
From 2017-2020, the PAMR board evaluated 270 cases of pregnancy-associated death. Eighty-seven of these were determined to be pregnancy-related. After determining pregnancy-relatedness, the board assigns an underlying cause of death per the Pregnancy Mortality Surveillance System (PMSS). The board determined that 28 pregnancy-related deaths were due to cardiovascular disease. The greatest proportion of pregnancy-related death due to cardiovascular disease occurred beyond six weeks postpartum (46%, Figure 1).
Additionally, the board evaluates if they agree with the cause of death as listed on the death certificate. The PAMR board disagreed with the underlying cause of
Ashlie Otto, RN Public Nurse Specialist MO Dept. of Health and Senior Servicesdeath provided on the death certificate in 23% of pregnancyrelated deaths. In 60% of the cases where the board disagreed with the listed underlying cause of death, they determined that cardiovascular disease was the actual underlying cause. For half of these cases, the cause of death was recorded by a physician (50%). Cardiovascular disease in this analysis is a composite of cardiomyopathy, hypertensive disorders associated with pregnancy, and other cardiovascular conditions.
For comparison, from 2017-2020, there were 5,328 deaths to Missouri resident women of childbearing age (15-44). Cardiovascular disease comprised 9% of these deaths overall. However, cardiovascular disease comprised 32% of all pregnancy-

related deaths during this time. Despite the limits of a small sample size, these differences, combined with how often the underlying cause of death was determined to be cardiovascular disease when the board disagreed with the listed cause, supports the hypothesis that cardiovascular disease may be under reported within the childbearing age population and largely unrecognized. One factor limiting the ability of medical certifiers to make an accurate ascertainment of a cause of death is a lack of autopsy. An autopsy was available for only 37% of cases where the board disagreed with the underlying cause of death. When looking at the childbearing age population, autopsies were available for 34% of all cases and 32% of cases of known cardiovascular disease. Without access to this level of data to guide determinations, medical certifiers risk missing causes that may not be immediately obvious at the time of death, including cardiovascular disease.
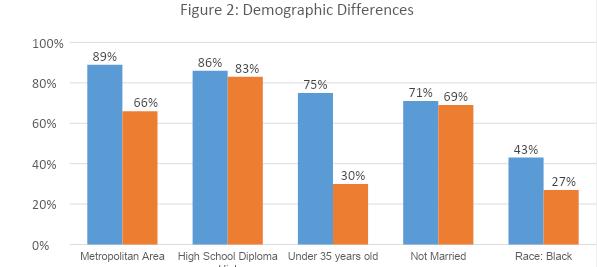
Comparing the population of pregnancy-related cardiovascular disease deaths with the childbearing age population that died from cardiovascular disease revealed a number of demographic
differences (Figure 2). A greater percentage of pregnancy-related deaths from cardiovascular disease resided in metropolitan counties (89%) than their counterparts from the childbearing age population (66%). Those with a high school diploma or higher education made up the majority of cardiovascular deaths for both pregnancy-related (86%) and childbearing age populations (83%). The percentage of the pregnancy-related cardiovascular death population that was under 35 years old was more than double (75%) the proportion in the childbearing age population (30%). The majority of these deaths in the pregnancy-related population (71%) and the childbearing age populations (69%) were not married. Lastly, Non-Hispanic Black women are overrepresented in the pregnancy-related population (43%) compared with the childbearing age population (27%).
There is a limitation to these findings as the pregnancy-related population that died due to cardiovascular disease is admittedly small. As such, these findings should be used to direct further investigation regarding cardiovascular disease risk in pregnancy, as well as the quality of death certificate data overall. This would help to determine which, if any, of the differences between groups is attributable solely to the effects of pregnancy. Additionally, looking at these population differences highlights target areas to expand awareness of cardiovascular disease during pregnancy.
However, based on the demographic discrepancies and the finding that cardiovascular disease was determined to be the most frequently misreported cause of death by the PAMR board, these findings may act as a warning sign that deaths due to cardiovascular disease may be underreported within the childbearing age population. Given that most pregnancy-related cardiovascular deaths occur more than six weeks postpartum, the PAMR board has consistently stated that it is imperative that women of childbearing age are asked if they have been pregnant within the last year to assess their cardiovascular risks and treatment paths. To this end, the board recommended that “All health care providers should utilize the cardiovascular disease assessment in pregnancy and postpartum toolkit and obtain further education regarding screening, referral, and treatment of cardiovascular disorders associated with pregnancy (i.e. peripartum cardiomyopathy, hypertensive disorders of pregnancy, etc.” in order to prevent such deaths in the future.
Congratulations to Laynie Verbick from South Holt R-1 Elementary School in Oregon, MO. Laynie won first place in the Family Health Foundation Tar Wars poster contest. Susan Lentz presented the Tar Wars materials and fun exercises before the students drew their vision of living a health, tobaccofree lifestyle on a poster.

The scope of the PAMR review process is all deaths to Missouri residents who had a pregnancy within the year prior to their death. While the generalizability of these findings is limited by a small population, the data indicates that cardiovascular disease in the childbearing age population may be under reported as the underlying cause of death. This finding warrants further investigation regarding how the underlying causes of death are determined and reported to evaluate the extent to which cardiovascular disease affects this population. Increased awareness by medical certifiers of the prominence of cardiovascular disease in pregnant and postpartum women may also improve case recognition. Supplementing these findings with additional data from the childbearing age population may highlight some key areas to begin looking for ways to better capture this information and identify prevention opportunities.
Interventions to reduce pregnancy-associated deaths are developed based on specific causes of death. If the cause of death recorded on the death certificate is inaccurate, this creates ripple effects that influence funding, research, and case identification. Interventions will fail if they are directed at the wrong cause. Therefore, it is critical for public health agencies to work with medical certifiers to ensure that the true causes of death are accurately reported in order to maximize the opportunity to prevent similar deaths in the future.
References on page 30.



As a leader in vertebral body tethering (VBT), we’re proud to offer an FDA-approved fusionless spine surgery that allows kids to maintain their spinal anatomy and range of motion. For kids whose idiopathic scoliosis can’t be managed with bracing, VBT offers:
• An early treatment option for scoliosis
• A less invasive, less limiting alternative to spinal fusion

• For most, a one-time surgery that naturally adjusts as kids grow
• The ability to avoid any sort of fusion in the spine
Daniel G. Hoernschemeyer, MD, is a board-certified pediatric orthopaedic specialist, chief of pediatric orthopaedic surgery and member of the Pediatric Orthopaedic Society of North America. As a pioneer in VBT procedures, Dr. Hoernschemeyer has been performing VBT surgeries for the past 10 years and is actively teaching the next generation of pediatric spine physicians.
Daniel G. Hoernschemeyer, MD, is a board-certified pediatric orthopaedic specialist, chief of pediatric orthopaedic surgery and member of the Pediatric Orthopaedic Society of North America. As a pioneer in VBT procedures, Dr. Hoernschemeyer has been performing VBT surgeries for the past 10 years and is actively teaching the next generation of pediatric spine physicians.
Daniel G. Hoernschemeyer, MD, is a board-certified pediatric orthopaedic specialist, chief of pediatric orthopaedic surgery and member of the Pediatric Orthopaedic Society of North America. As a pioneer in VBT procedures, Dr. Hoernschemeyer has been performing VBT surgeries for the past 10 years and is actively teaching the next generation of pediatric spine physicians.
To learn more or to refer a patient, call (573) 884-6132 or visit muhealth.org/vbt-for-docs.
To learn more or to refer a patient, call (573) 884-6132 or visit muhealth.org/vbt-for-docs
To learn more or to refer a patient, call (573) 884-6132 or visit muhealth.org/vbt-for-docs.








The MAFP and the Family Health Foundation of Missouri (FHFM) hosted the Transition to Practice conference for family medicine residents and students again this year. Held on June 9-10 at Courtyard by Marriott, Jefferson City, this conference included hands-on procedures and sessions to help medical students choose family medicine and current residents become better family physicians.

Following lunch on Friday, the conference started with a warm welcome from MAFP President-Elect Afsheen Patel, MD and an opening session from John Paulson, DO, PhD, FAAFP, on the Joy of Discomfort: The Benefit of Doing Hard Things. As a former Board Chair of MAFP and Department Chair of Primary Care at Kansas City University, Dr. Paulson shared his life experience of overcoming adversity and how difficult life experiences benefit us all and improve patient care.
Breakout sessions for residents and students targeted specific areas of interest to them. Students gained insights and were able to ask questions in an informal setting with residency directors Sarah Cole, DO, FAAFP, Mercy Family Medicine Residency, St. Louis, and Lawrence Gibbs, MD, MSEd, FAAFP, HCA Healthcare Kansas City. Residents took advantage of the beautiful weather to sit around a table outside with Ryan McDaniels, JD, Newman, Comley, & Ruth PC to discuss how to protect themselves and key components to consider when negotiating their employment contracts.
Following the breakout sessions, the group boarded a bus funded by the AAFP Foundation’s Family Medicine Chapter


Alliance to make the short trip to the Missouri State Capitol. While at the Capitol, MAFP Governmental Consultants Randy Scherr and Brian Bernskoetter provided a personal tour of the building. They were even able to get on the House and Senate Floors! Dr. Sarah Cole and MAFP Executive Director Kathy Pabst led a discussion on effective advocacy, what to expect when attending a hearing, and shared firsthand experiences of testimony. After the Capitol tour, the group participated in a brief tour of the 187-year-old decommissioned Missouri State Penitentiary. The tour guide provided insight on life in prison, social determinants of health, and a history of the human condition in Missouri. The evening concluded with dinner at a local landmark, Arris Pizza Palace, in the shadow of the Capitol.

Sunday morning started with a presentation from Andi Selby, DO, FAAFP, on Finance Basics for Physicians. Dr. Selby provided personal stories of money management, guidance on resources to consider as physicians start earning money, and insight on how to find trustworthy advisors.
Dr. Paulson and Amanda Shipp, MD, shared their experience with the AAFP Leading Physician Wellness program. Titled “If Only I Knew Then What I Know Now”, they provided concrete advice on personal wellness as these physicians began their careers.
Jack Wells, MD, FAAFP; Brea Lombardo, MD, IBCLC; and Josh Smothers, MD from University of Missouri Family & Community Medicine led an interactive practice workshop on common dermatological procedures. Students and residents were able to practice shave biopsy, punch biopsy, and suturing.

Thank you very much!
This was my first conference. I had a great experience, and everyone was very kind and welcoming.
The conference wrapped up with a light and relaxing Missouri Mingle reception. Eight exhibitors promoted their residency program or health facility to the attendees. This was an opportunity to meet with and learn more about residency and employment options in Missouri.


Attendees shared how they appreciated the opportunity to learn more about family medicine, network, and gain skills to help them in their careers.


“Thank you for the wonderful opportunity you allowed us all to have. It was my first conference and I’m glad it was with the MAFP - everyone was extremely welcoming, helpful, kind and willing to share knowledge. I wasn’t sure about what to expect or even how to approach people, admittedly, I was nervous about attending but none of that was even a concern once I arrived - it all felt like we were old friends. What a great experience and I can’t wait to see everyone again.”
“Thank you for a great Transition Conference! It was a great time of networking and learning, and I truly believe that this conference continues to get better every year since I’ve been attending it. You both do so much for the field of Family Medicine, and your support for the students and residents in our field is spectacular. Thank you both for all you do, and I look forward to continuing working with the MAFP in any capacity I can as I go through my residency and my career.”
Financial support for this program is provided by the AAFP Family Medicine Chapter Alliance which is funded by members like you! Help programs like this continue to support family medicine by giving to the FMPC. Select “Chapter Grants” when making your gift online at https://www.aafpfoundation.org/donate.html. Thank you.

This conference would not have been a success without our sponsors – The Family Health Foundation of Missouri (www.moafp.org/foundation) and Missouri Health Professional Placement Services (https://www.mhpps.org/).

Find Your Next Great Hires
• PLACE your job in front of our highly qualified members.

• SEARCH our resume database of qualified candidates.
• MANAGE jobs and applicant activity right on our site.
• LIMIT applicants only to those who are qualified.
• FILL your jobs more quickly with great talent.
Keep Your Career on the Move
• POST a resume or anonymous career profile that leads employers to you.
• SEARCH and apply to hundreds of new jobs on the spot by using robust filters.

• SET UP efficient job alerts to deliver the latest jobs right to your inbox.
• ACCESS career resources, job searching tips and tools.
Thank you so much! I’m so glad I took the time to come. I learned so much and met wonderful people so willing to help my journey. I hope to pay it back in the same way some day.


Missouri was well represented at this year’s AAFP Family Medicine Advocacy Summit in Washington, DC. We joined nearly 300 family physicians, residents, and medical students to meet with policymakers to discuss urgent health care issues affecting patients and practices. This included ensuring adequate Medicare physician payment, strengthening the primary care workforce, and easing the administrative burden too many physicians face.
The two-day meeting focusing on “Advocacy 365” prepared new, as well as experienced, advocates to share their stories with our elected US legislators and their staff. The theme of the conference, “Change Starts Here,” was the focal point in our communications about the changes that need to be made to make the health care system more efficient, effective, and equitable. Rachel Levine, MD, US Assistant Secretary of Health, was the keynote speaker. Attendees learned tactics for advocating for the specialty, then lobbied directly with members of Congress to influence the public policies affecting patients and practices.
MAFP Executive Director, Kathy Pabst, MBA, CAE, co-presented a breakout session on recruiting future advocates with Rick Madden, MD, New Mexico AFP. The session addressed our efforts in meeting with our members, residents and students and encouraging their involvement in advocacy. The MAFP annual advocacy survey was highlighted as a method to encourage
members to share their opinions and shape MAFP policy. And lastly, an idea that was generated from last year’s strategic planning session, the MAFP created an advocacy syllabus in collaboration with Mercy Family Medicine Residency and Lincoln University. This syllabus is a template to teach and lead students and residents about the impact of advocacy, legislation, and public policy in the health care industry.
Sarah Cole, DO, FAAFP, MAFP past president, was impressed by the number of physicians in training who attended this year’s summit - over 100 medical students and residents! Missouri’s own delegation included one medical student and three residents! “These physicians in training brought passion and eloquence to the forefront as they communicated with their congressional leaders and their aides. The future is bright with this next generation!” Dr. Cole appreciated the leaders willingness to consider bipartisan support with health policy issues. “MAFP members cover the spectrum of political ideology, which speaks to
the fact that health care affects us all. Whether it was urging CMS to finalize rules that allow legislation to proceed that would reduce administrative burden for physicians or supporting legislative efforts to stabilize graduate medical education in primary care, the MAFP delegation spoke expertly and our congressional leaders listened with open minds. I strongly encourage any MAFP member who’s not previously attended to consider doing so!”
“As family physicians, we really are all experts at the issues facing our country regarding healthcare. We experience the struggles of our colleagues and our patients daily. Getting to work towards solutions for some of these concerns feels like making a difference on a much grander scale than day-to-day patient care,” said Kara Mayes, MD, MAFP President. She noted that it is also refreshing to remember that many of the concerns of family physicians are truly bipartisan issues so that our country can work towards a solution that helps everyone. As an added benefit, I was able to spend time with the other family physicians who were there to represent Missouri.
This was Dr. Afsheen Patel’s first year attending Family Medicine Advocacy Summit in Washington, DC. “This year we advocated for three main issues: advancing residency slots, step therapy and prior authorization, and ensuring financial stability for Medicare reimbursement. We heard from several important speakers and received an encouraging response. As a full-time practicing physician, I shared my experience with my fellow colleagues. They were grateful that we have a voice and keep fighting for primary care. My hope is to see more of you in the following years to fight for what we do best, provide exceptional care.”
Arihant Jain, MAFP District 1 Director also attended the conference for the first time. Dr. Jain has attended the Missouri Advocacy Day, but “advocating at the US Capitol is altogether a different experience. Missouri delegates advocated to advance primary care as the bedrock of our health care system at the federal level. Members of Congress are very receptive to our problems, solutions, and share similar concerns facing primary care physicians.” He initially felt nervous about the daunting task of going to the US Capitol, but after listening and learning from conference speakers, other experienced attendees, and our own group of Missouri physicians, it alleviated all the anxiety and actually turned out to be a fun experience.”
MAFP’s resident delegate at the conference, Megan Landis, MD, Mercy Family Medicine Residency, shared that it was “a truly remarkable introduction to healthcare advocacy work at the federal level. I look forward to growing with and expanding upon the experiences I had during these three days in Washington D.C. throughout my career as a primary care physician in Missouri. I am incredibly grateful for all that the MO AFP chapter does for us on a daily basis and cannot thank them enough for giving me the opportunity to attend FMAS this year.”
Wesley Goodrich, DO, MPH, University Health Kansas City Family Medicine Residency, had the privilege of attending as well and advocating for primary care with legislators and their aids. “During my graduate studies in public health, I learned that if you wanted to enact lasting cultural change, you had to do it at the legislative level. Family physicians who tirelessly care for their patients have taken up advocating for the greatest patient outcomes and for improved quality outcomes by promoting primary and preventative care. What a gift it is to be able to share both our experience as physicians, as well as the experiences of our patients, with our nation’s leaders to improve our healthcare system and best support our colleagues and communities!”
It’s never too late to contact your legislator. You can contact your legislator at https://www.votervoice.net/AAFP/Address to become a healthcare policy resource!



As the son of a funeral director, coroner, and ambulance driver in a small midwestern town, Todd Shaffer, MD, MBA, FAAFP, DABFM, grew up seeing death and dying in the funeral home. Going with his dad to pick up residents who had passed from natural and unnatural deaths, he saw firsthand how far too many rural Americans lose their lives due to poor medical care access. He saw way too many die that should not have, whether it be from lack of basic care, to dying in a mechanical accident on farms, or accidents on the rural highways. He witnessed the true effect it had on families and communities when people were taken far before their time.
This is the spark that ignited his interest in medicine. Dr. Shaffer completed his medical degree from the University of Missouri-Columbia School of Medicine. He was accepted into the University of Missouri-Kansas City Family Medicine Residency Program (UMKC-FMR) where he joined his brother and sister-in-law who also were in the same family medicine residency program. UMKC-FMR is an innovative learning program in a community hospital where only family medicine residents are trained for all aspects of family medicine with a special focus on health equity and social determinants of health. Residents learn how to provide full-spectrum care for the poorest populations in the Midwest including inner city, suburban poor, and socioeconomically disadvantaged rural communities.
Todd’s interest was to become a fullscope rural family doctor and perform obstetrics and c-sections. However, his direction changed when he found passion for teaching other students and residents. He made the decision to devote his career to training family medicine residents so he can have a greater impact on the most vulnerable of society.
He went on to become UMKC-FMR’s residency program director for 15 years. During his tenure, he created a dual residency MBA leadership program with

a local university. The MBA program was integrated into the residency program and became the first dual program approved by both the ACGME and the ABFM. Under his leadership, UMKC-FMR program went on to add 2 residents per year, and then added fellowships in geriatrics, family medicine obstetric surgery, and sports medicine. He authored and received a PCRE expansion grant from HRSA of nearly $2 million to expand the residency program by another 2 residents per year in a rural hub and spoke system. This grant successfully supported 10 rural grant residents who are all practicing rural family medicine. Nine of the rural grant residents practice in rural Missouri. The UMKC-FMR’s 14-14-14 program received national accolades for its full spectrum training which prepares graduates for any clinical practice type. His legacy continues as he has trained over 400 residents, nearly 75 fellows, and thousands of medical students who have rotated through their residency program and department.
Todd saw the need for national changes and was elected to the AFMRD board. He served on that board for 7 years, including serving as its president. He ran on the idea of creating a shared curriculum that all residency programs could utilize, especially in small rural programs with fewer faculty to teach all the aspects of family medicine didactics and learning scenarios. This project became known as the family medicine residency curriculum resource project. Its wiki-based shared advancements continue to be used to this day in most family medicine residency programs across the country.
His passion for women’s health has led him through most of his career delivering well over 2,000 babies and leading a regional dysplasia clinic where he has performed over 18,000 colposcopies and over 25 loop LEEP procedures. He has taught the ALSO program since it was first offered in 1993. He is a recognized ALSO leader and still participates in its reverse classroom didactics and workshops which
trains the majority of family medicine residents across the country.
Todd has been serving in his private clinic for over 30 years and continues to mentor and provide home visits for his patients. He has been traveling to his state capitol for over 25 years advocating for better healthcare for all Missourians. He serves as a voice for the indigent and rural patients who are his passion. He has travelled to Washington, DC to meet with the national leadership for the past 15 years and has attended the National Conference for Family Medicine Residents and Students every year for the past 30 years.
He continues his teaching passion by developing innovative teaching methods for the next generation of family doctors. He leads the procedure and POCUS curriculum in his residency program and has taken graduate courses in simulation leadership education through UMKC. He teaches students and residents to learn by mastery in many procedures and handson evaluations of patients. Hence his moniker of #FMXSCOPE—Family Medicine eXtending Scope, for the current and future generations to widen the services and care offered to their patients no matter what town or community they live in.
He has been practicing his entire career in the only safety net hospital system in the middle part of the country. He strives for equity in health care for the less fortunate and very diverse population he cares for by being actively involved in and impacting local, state, and national policy and programs. He cares for the poorest of the poor in rural and urban Kansas City all the while mentoring and training the next generation of medical students and residents to improve health care for all, regardless of their ability to pay. The passion he developed from an early age of seeing healthcare inequality has driven his entire career to not only make a difference day to day, but to effect change for the future of all family medicine physicians, residents, and students whom he has touched on so many different levels.
Family physicians are residency-trained, primary care specialists dedicated to treating the whole person. With a focus on prevention, primary care, and overall care coordination, family physicians provide a wide variety of clinical services, and, when necessary, refer their patients to a specialist, while continuing to advocate for that patient’s care.
Family physicians are residency-trained, primary care specialists dedicated to treating the whole person. With a focus on prevention, primary care, and overall care coordination, family physicians provide a wide variety of clinical services, and, when necessary, refer their patients to a specialist, while continuing to advocate for that patient’s care.
Family physicians are residency-trained, primary care specialists dedicated to treating the whole person. With a focus on prevention, primary care, and overall care coordination, family physicians provide a wide variety of clinical services, and, when necessary, refer their patients to a specialist, while continuing to advocate for that patient’s care.
Family physicians are residency-trained, primary care specialists dedicated to treating the whole person. With a focus on prevention, primary care, and overall care coordination, family physicians provide a wide variety of clinical services, and, when necessary, refer their patients to a specialist, while continuing to advocate for that patient’s care.




Family
More Americans depend on family physicians than on any other medical specialty. AAFP members are the main source of primary health care for the Medicare population and see a large proportion of new Medicaid beneficiaries.1
More Americans depend on family physicians than on any other medical specialty. AAFP members are the main source of primary health care for the Medicare population and see a large proportion of new Medicaid beneficiaries.1
More Americans depend on family physicians than on any other medical specialty. AAFP members are the main source of primary health care for the Medicare population and see a large proportion of new Medicaid beneficiaries.1
More Americans depend on family physicians than on any other medical specialty. AAFP members are the main source of primary health care for the Medicare population and see a large proportion of new Medicaid beneficiaries.1


The MAFP delegates to this year’s AAFP Annual Chapter Leadership Forum (ACLF) and the National Conference of Constituency Leaders (NCCL) learned about wellbeing to address the challenges we are experiencing as physicians, chapters, and individuals. The leadership conference opened with a town hall session hosted by a panel including Shawn Martin, AAFP EVP; Tochi Iroku-Malize, MD, MPH, MBA, AAFP President; Steven Furr, MD, AAFP PresidentElect; and Sterling Ransone, MD, AAFP Board Chair. Questions from members focused on physician well-being, administrative burden, and physician protection for providing comprehensive health care.
The MAFP Executive Commission, along with the MAFP team, attended the ACLF. Important sessions addressed member engagement and experiences, exceptional board governance, physician leadership, communications, and diversity/equity/inclusion work. Learning from experts and colleagues ensures we continue to meet the needs of our members, stay abreast of best practices, and collaborate with other chapters and members to promote family medicine. It is an inspiring opportunity to be a resource and learn from other chapter staff.
“This year was another exciting year at ACLF,” shared Afsheen Patel, MD, MAFP President Elect. “It is always a great opportunity to network with peers from different states around the nation. It is also fascinating to see how far we have come as an organization at AAFP and staying ahead of issues that face us every day. This year, we also acknowledged AI and its role in family medicine and the opportunities and challenges we have with its integration into our practices.”
NCCL elected new AAFP board members and new alternate delegates to the Congress of Delegates. The member constituency alternate delegates represent the following constituency groups: new physicians, women; minorities; international medical graduates; and LGBTQ+ physicians or physicians who support LGBTQ issues. The constituencies also developed resolutions for the AAFP Congress of Delegates to consider during their October meeting in Chicago. Resolutions acted upon include numerous diversity, equity and inclusiveness-related issues, reproductive services, genderaffirming care, gun violence, racism, and mental health.
Missouri delegates at the NCCL were:
Women – Misty Todd, MD, Sedalia
IMG – Kento Sonoda, MD, St. Louis
LGBTQ – Andi Selby, DO, Branson
Minority – Stacy Jefferson, MD, St. Louis
New Physician – Nicholas LeFevre, MD, Columbia
proudly presents to the
Missouri Academy of Family Physicians
Second Place -Large Chapters
Highest Percent Retention New Physicians 2022
The Missouri chapter was recognized for our retention of new physicians in 2022. We were 2nd out of 55 chapters and received a certificate to commemorate our efforts.
Corey Feist, JD, MBA, president and co-founder of the Dr. Lorna Breen Heroes’ Foundation, was the keynote speaker and offered family medicine leaders steps to improve well-being on the system level by eliminating the stigma of mental health issues and seeking help.
A little over three years ago, at the height of the first wave of the pandemic, Corey lost his sister-in-law, Lorna Breen, MD, by suicide because she worried that she would lose her physician’s license as a result of her receiving mental health care. The foundation’s mission is to change the systemic laws and regulations regarding the disclosure of mental health care on license applications/renewals. Through the formation of the Dr. Lorna Breen Heroes’ Foundation, their goal is to work on reducing physician burnout, improving well-being, and ensuring that when a physician seeks mental health treatment, it is viewed as a sign of strength, not weakness. His story is not the first of its kind, but through the foundation’s efforts, they strive for it to be the last.

Our NCCL delegates offered some words of wisdom about their experience, involvement, and hope for the future of family medicine.
Kento Sonoda, MD, FASAM, AAHIVS, St. Louis, represented the IMG constituency at the NCCL. “I was deeply inspired by the passion and energy that permeated the conference. Advocating and testifying alongside like-minded individuals from different states was a truly enriching experience. Additionally, I had the opportunity to learn about resolution writing and served on the Education Reference Committee. I am immensely grateful to MAFP for providing me with this wonderful opportunity.”
“The most striking thing I noticed about this conference was overall acceptance and positivity permeating the halls. This was a great space to learn more about the legislative process and how to advocate for our specialty and our patients,” said Andi Selby, DO, LGBTQ+ delegate from Branson. “I served on a Reference Committee which gave me an insider’s experience of what happens to resolutions once submitted. I came away from this conference with more knowledge, confidence, and hope for our future…and a few new friends.”
Misty Todd, MD, Cole Camp, Women’s Delegate, was invigorated to be surrounded by other family physicians from around the country advocating for many of the same things she does daily. “It was great to have some first-hand perspectives of the reality of daily practice and access to patient care hurdles that our colleagues encounter. I sincerely appreciated learning about the process and being able to see how the AAFP truly does care about what is important to its constituents by allowing such a large influence in the process from physicians with their boots on the ground every day.”
As the New Physician delegate, Nicholas LeFevre, MD, Columbia, enjoyed meeting motivated physicians from around the country. He helped draft and testified on resolutions including
one working to improve family medicine elective opportunities for under-represented minorities and another surrounding naloxone in airline emergency kits. “Particularly impactful was a plenary session on mental health among physicians and physicians in training. I also participated in a training for physicians on how to speak more effectively with the media. The Missouri delegation was a diverse and fun group.”
Want to represent Missouri at the 2024 conference? Email Kathy Pabst at kpabst@mo-afp.org and let her know. We will select next year’s delegates in February 2024.

an alcohol-free Pregnancy is the best choice for your baby.
alcohol-free
an alcohol-free Pregnancy is the best choice for your baby.
What we know:
What we
• There’s no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
• All types of alcohol are equally harmful, including all wines and beer.
What we know:
What we know:
• There’s no
• All types of
• Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman
• There’s no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
• There’s no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
• Alcohol can
What can happen:
• All types of alcohol are equally harmful, including all wines and beer.
• All types of alcohol are equally harmful, including all wines and beer.
What can
• Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant.
• Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant.
• Drinking alcohol behavioral
What can happen:
• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders
What can happen:
What you
What you can do:
• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
• FASDs are
What we know:
• FASDs are completely preventable if a woman does not drink alcohol during pregnancy.
What you can do:
• There’s no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
What you can do:
• For more information, visit www.cdc.gov/fasd or call 800–CDC–INFO.
• FASDs are completely preventable if a woman does not drink alcohol during pregnancy.
• All types of alcohol are equally harmful, including all wines and beer.
• FASDs are completely preventable if a woman does not drink alcohol during pregnancy.
What we know:
• Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant.
• For more information, visit www.cdc.gov/fasd or call 800–CDC–INFO.
• For more information, visit www.cdc.gov/fasd or call 800–CDC–INFO.
What we know:
What can happen:
• There’s no known safe amount of alcohol use during pregnancy or while trying to
• There’s no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
• All types of alcohol are equally harmful, including all wines and beer.
• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
• All types of alcohol are equally harmful, including all wines and beer.
• Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant.
What you can do:
• FASDs are completely preventable if a woman does not drink alcohol during pregnancy.
• Alcohol can cause problems for a developing baby throughout pregnancy, including
What can happen:
• For more information, visit www.cdc.gov/fasd or call 800–CDC–INFO.
• For more information, When

What can happen:
• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
What you can do:
When a pregnant woman drinks alcohol, so does her baby. Why take the risk?
When a pregnant woman drinks alcohol, so does her baby. Why take the risk?
When a pregnant woman drinks alcohol, so does her baby. Why take
• FASDs are completely preventable if a woman does not drink alcohol during pregnancy.


• Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of behavioral and intellectual disabilities. These disabilities are known as fetal alcohol
• For more information, visit www.cdc.gov/fasd or call 800–CDC–INFO
What you can do:

an
Pregnancy is the best choice for your
an alcohol-free Pregnancy is the best choice for your baby.
The AAFP State Legislative Conference was the perfect opportunity to join members and chapter staff to discuss strengthening family medicine in our states. With many members already attending the leadership conference in May, it was a perfect transition to focus on advocacy engagement at the state level. MAFP advocacy commission co-chair Keith Ratcliff, MD, FAAFP, and Kara Mayes, MD, MAFP President, attended along with Kathy Pabst, MBA, CAE, MAFP Executive Director and Bill Plank, CAE, MAFP Assistant Executive Director. Since this conference was during the last week of the Missouri legislative session, our governmental consultants were unable to attend as they were representing you at the capitol.
This conference is always a great opportunity to learn from other chapters about their legislative successes and challenges. Best practices for increasing advocacy engagement, along with healthcare consolidation, social issues messaging, physician wellness, and roundtable discussions comprised the full day of engagement among colleagues.
We were given the opportunity to share our successes during a breakout session on “Strengthening the Pathway to More Family Physicians.” Kathy Pabst co-presented this session with Ashley Bentley, Manager, AAFP Workforce Development and Student Initiatives, and we shared initiatives that AAFP and MAFP are working on to increase and strengthen the primary care workforce.


Thanks to your support and funding, the Family Health Foundation of Missouri was able to award scholarships to the top graduating medical students entering a Missouri family medicine residency. The following recipients were awarded a certificate and $500 scholarship:

Alexander James Marx, DO, Kansas City University
Brittney Marshall, MD, University of Missouri Columbia
Noah Brown, MD, University of Missouri Kansas City
Tessa Tolen, DO, A.T. Still University, Kirksville
Tessa Tolen reached out and thanked both the MAFP and the Family Health Foundation of Missouri for the honor of being selected. “I look forward to practicing in Missouri after I complete my Family Medicine Residency at CoxHealth in Springfield and appreciate the scholarship award!”
Congratulations on a job well done!
Dear Family Health Foundation of Missouri,
Thank you very much for choosing me as the recipient of the 2023 Scholarship Award as the Outstanding Graduate of the University of Missouri-Kansas City Entering family Medicine!
It is truly an honor to have been chosen for this award, and the scholarship portion of this will lift a lot of burden as I relocate & prepare to begin my residency. Family Medicine has been my passion since coming into medical school, and I am ecstatic to get to begin my journey in our incredible field at Mercy Hospital in St. Louis for
my residency! Throughout my medical school career, the support of the Family Health Foundation has been very noticeable & appreciated. From covering student registration & lodging at conferences to sponsoring the Transition to Practice conference to sponsoring the summer externship program to sponsoring this scholarship, your support for students is palpable and incredibly impactful.
Thank you again, for your generosity & choosing me as the recipient for this award. Thank you!
Noah Brown Brittney Marshall, MD, University of Missouri ColumbiaThe Kansas City Chapter of the MAFP held its annual meeting and officer installation on February 27, 2023. Outgoing President Jay Patel, DO, installed Rachel Hailey, MD, as President; Peter Lazarz, MD, as Vice President; and Chelsie Cain, DO as Secretary/Treasurer.



UMKC medical students, Hannah Esker and Audrey Yu, gave a report on the research project they presented at the STFM meeting this year on “Population Health Management Education: New Curriculum to Equip Students for the Future of Value-Based Care.”
As the new officers assumed the helm of the Kansas City Chapter, they began looking to the future and held a strategic planning session in April. Kathy Pabst, MBA, CAE, MAFP Executive Director, and Bill Plank, CAE, Assistant Executive Director, guided their discussions for plans from the present to the future. Their vision of the chapter is in good hands with their board of directors led by Rachel Hailey, MD, and Jim Kelley, their Executive Director. Prior planning included a membership survey to capture the reasons for being a member, current feelings and perspective about the chapter, and to identify future opportunities. As a culmination of the survey results and 3 hours of discussion during the strategic planning session, it was agreed that they will focus on:
• Participating in community events
• Creating well-defined board member expectations
• Developing the image of KCAFP

• Providing student support
As with any strategic plan, the work is only beginning as the board looks at the next steps to grow and support its membership in the Kansas City area.

www.OpioidResponseNetwork.org
Opioids and stimulants have created an unprecedented health crisis. So we created an unprecedented response.
The Opioid Response Network works directly with communities, healthcare systems, and individuals to provide the resources, knowledge and connections required to turn the tide.
There is no cost. We are here to help with your prevention, treatment, recovery and harm reduction efforts, all tailored for your needs.
Funding for this initiative was made possible (in part) by grant no. 1H79TI085588 from SAMHSA. The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.


The AAFP Foundation Family Medicine Leads program recently named Kelly Dougherty, MD, as a 2023 Family Medicine Leads (FM Leads) Emerging Leader Institute (ELI) Scholar.
Dougherty, a PGY-2 at Mercy Family Medicine Residency in St. Louis, received a scholarship to attend the AAFP National Conference of Family Medicine and Students and will participate in the 8th class of the FM Leads ELI.

Family Medicine Leads, the AAFP Foundation Education Signature Program, focuses on the future of the family medicine specialty by supporting efforts to fill the workforce pathway with the best and the brightest as well as developing more and better trained family medicine leaders.
Congratulations, Dr. Dougherty!
Grant Hoekzema, MD, FAAFP, was recently selected to serve as a director on the American Board of Family Medicine (ABFM). The mission of the ABFM is to improve the health of the public through certification, training standards, research, leadership development, and collaboration. Dr. Hoekzema’s education, experience, and commitment to family medicine checks off every aspect of their mission statement.
Grant is focused on ensuring family physicians practice at the full scope of their education and training. His service in family medicine leadership roles is the foundation for his service as a board member on the ABFM. He has served on the Association of Family Medicine Residency Directors Board of Directors, Council of Academic Family Medicine Board of Directors, and the Accreditation Council for Graduate Medical Education as a review committee member, and as the board chair. The culmination of this service aligns with his efforts to transform family medicine and our health system through engagement in local, state, and national family medicine organizations.
Dr. Hoekzema is chair of the Mercy Hospital, Department of Family Medicine, in St. Louis and is committed to training the next generation of family physicians and ensuring the residents receive the oversight to become top family physicians in their communities.
Dr. Kento Sonoda was selected for Honorable Mention as part of the Society of Teachers of Family Medicine 2023 Research Paper of the Year Award. His research paper was titled “HIV Care by Early-Career Family Physicians.”

“I see patients with HIV and substance use disorder on a regular basis,” said Dr. Sonoda, who practices at both a primary care clinic and an addiction-based care center in St. Louis. “The more family physicians who can provide integrated care including behavioral health, addiction and HIV treatment, the better off these patients will be.”
Congratulations, Dr. Sonoda!
The Family Health Foundation of Missouri (FHFM) supports medical students and family medicine residents’ leadership development through participation in national and state conferences. We need your help to support these programs. The FHFM is again hosting a silent auction that will be held virtually and in conjunction with the Annual Fall Conference in November. With a goal of raising $7,000 to support the next generation of family physicians, we need you to donate an item that will be recognized in signage and printed materials for the Annual Fall Conference, in an issue of the Missouri Family Physician, and on the MAFP website. The deadline to submit a donation form is October 28. All donations can be received through November 7th unless prior arrangements are made to be delivered at the conference.
Need a donation idea? Here are some items to consider, but not limited to art, athletic tickets and gear, celebrity or team-autographed items, performance tickets (theater, music, etc.), restaurant certificates, subscriptions, theme baskets, trips, and weekends (lake houses, resorts, condos, houseboats, etc.), unique experiences and travel.

Questions? Contact Bill Plank, Assistant Executive Director, at bplank@mo-afp.org or (573) 635-0830.
Learn more about the FHFM by visiting https://www.mo-afp.org/foundation/.
pages 6-7
1. Brief Breastfeeding State Laws. (2021, August 26). National Conference of State Legislatures. Retrieved May 14, 2023, from https://www.ncsl. org/health/breastfeeding-state-laws
2. Grossman, J. (1978, June). Fair Labor Standards Act of 1938: Maximum Struggle for a Minimum Wage. U.S. Department of Labor. Retrieved May 14, 2023, from https://www.dol.gov/general/aboutdol/history/ flsa1938
3. Hawkins, S. S. (n.d.). Breastfeeding and the Affordable Care Act. Pediatr Clin North Am. PubMed Central. 10.1016/j.pcl.2015.05.002
4. Laws | Breastfeeding. (n.d.). Missouri Department of Health and Senior Services. Retrieved May 14, 2023, from https://health.mo.gov/ living/families/wic/breastfeeding/resourcesdata/laws/
5. 191.918. Breast-feeding in public permitted not sexual conduct, public indecency, or obscenity — no municipal ordinances to prohibit or restrict. (2022, February 23). Revisor of Missouri. Retrieved May 14, 2023, from https://revisor.mo.gov/main/OneSection.aspx?sectio n=191.918&bid=9697&hl=breast%u2044feeding
6. 160.995. Lactation accommodations, written policy, contents, requirements model policy rulemaking authority. Revisor of Missouri. Retrieved May 14, 2023, from https://revisor.mo.gov/main/ OneSection.aspx?section=160.995&bid=49893&hl=lactation%u2044
7. 376.1210. Maternity benefits, minimum hospital stays, exceptions notice of benefits, contents attending physician defined rulemaking. (2022, February 23). Revisor of Missouri. Retrieved May 14, 2023, from https://revisor.mo.gov/main/OneSection.aspx?sectio n=376.1210&bid=20936&hl=breast%u2044education
8. Wage and Hour Division of the U.S. Department of Labor. (n.d.). Section 7(r) of the Fair Labor Standards Act – Break Time for Nursing Mothers Provision. U.S. Department of Labor. Retrieved May 14, 2023, from https://www.dol.gov/agencies/whd/nursing-mothers/law
9. Missouri Department of Health and Senior Services. (n.d.). Breastfeeding Worksite Initiatives | Breastfeeding | Health & Senior Services. Missouri Department of Health and Senior Services. Retrieved May 15, 2023, from https://health.mo.gov/living/families/ wic/breastfeeding/worksiteinitiatives/
10. A Better Balance, American Civil Liberties Union, National WIC Association, Center for WorkLife Law,, MomsRising, & U.S. Breastfeeding Committee. (n.d.). The PUMP Act Explained. U.S. Breastfeeding Committee. Retrieved May 15, 2023, from https:// www.usbreastfeeding.org/the-pump-act-explained.html
pages 8-9
1. Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health. Centers for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Last Accessed May 4, 2023. https://www.samhsa.gov/data/sites/default/files/reports/ rpt39443/2021NSDUHFFRRev010323.pdf
2. Ko JY, D’Angelo DV, Haight SC, et al. Vital Sign: Prescription Opioid Pain Reliever Use During Pregnancy – 34 U.S. Jurisdictions, 2019. MMWR Morb Mortal Wkly Rep 2020;69:897-903.
3. Harter K. Opioid use disorder in pregnancy. Ment Health Clin. 2019;9(6):359-372.
4. Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses in the US, 20102017. JAMA. 2021;325(2):146-155.
5. Kennedy-Hendricks A et al. Social Stigma Toward Persons With
Prescription Opioid Use Disorder: Associations With Public Support for Punitive and Public Health–Oriented Policies. Psychiatr. Serv. 68, 462–469 (2017).
6. Volkow ND. Stigma and the Toll of Addiction. N Engl J Med. 2020;382(14):1289-1290.
7. Schiff DM, Stoltman JJK, Nielsen TC, et al. Assessing Stigma Towards Substance Use in Pregnancy: A Randomized Study Testing the Impact of Stigmatizing Language and Type of Opioid Use on Attitudes Toward Mothers With Opioid Use Disorder. J Addict Med. 2022;16(1):77-83.
8. Terplan M, Kennedy-Hendricks A, Chisolm MS. Prenatal substance use: Exploring assumptions of maternal unfitness. Subst Abuse 2015;9(Suppl 2):1–4
9. Crawford AD, McGlothen-Bell K, Recto P, et al. Stigmatization of Pregnant Individuals with Opioid Use Disorder. Women’s Health Rep (New Rochelle). 2022;3(1):172-179.
10. P Goddu A, O’Conor KJ, Lanzkron S, et al. Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record [published correction appears in J Gen Intern Med. 2019 Jan;34(1):164]. J Gen Intern Med. 2018;33(5):685-691.
11. National Institute on Drug Abuse. Words Matter – Terms to Use and Avoid When Talking About Addiction. Accessed May 4, 2023. https://nida.nih.gov/nidamed-medical-health-professionals/healthprofessions-education/words-matter-terms-to-use-avoid-whentalking-about-addiction
12. American Society of Addiction Medicine. Public Policy Statement on the Addiction Medicine Physician Participation in and Leadership of Multidisciplinary Care Teams. Adopted on January 20, 2016. Accessed May 4, 2023. https://www.asam.org/docs/default-source/publicpolicy-statements/multidisciplinary-care-teams-final-jan-2016. pdf?sfvrsn=14d670c2_0
13. Campbell CI, Saxon AJ, Boudreau DM, et al. Primary Care Opioid Use Disorders treatment (PROUD) trial protocol: a pragmatic, clusterrandomized implementation trial in primary care for opioid use disorder treatment. Addict Sci Clin Pract. 2021;16(1):9.
14. Brackett CD, Duncan M, Wagner JF, Fineberg L, Kraft S. Multidisciplinary treatment of opioid use disorder in primary care using the collaborative care model. Subst Abus. 2022;43(1):240-244.
15. Sokol RG, Pines R, Chew A. Multidisciplinary Approach for Managing Complex Pain and Addiction in Primary Care: A Qualitative Study. Ann Fam Med. 2021;19(3):224-231.
Cardiovascular Disease: A Hidden Threat to Maternal Health pages 12-14
1. Gunja MZ, Gumas ED, Williams RD. The U.S. Maternal Mortality Crisis Continues to Worsen: An International Comparison. To the Point (blog). December 2022. https://www.commonwealthfund. org/blog/2022/us-maternal-mortality-crisis-continues-worseninternational-comparison#:~:text=New%20international%20 data%20show%20the,most%20other%20high%2Dincome%20 countries. Accessed December 21, 2022.
2. Missouri Department of Health and Senior Services (DHSS), Bureau of Vital Statistics. Death File, 2017-2020.
3. Alipour, J, Payandeh A. Common Errors in Reporting Cause-of-Death Statement of Death Certificates: A Systematic Review and MetaAnalysis. Journal of Forensic and Legal Medicine. 2021;82:102220. doi:10.1016/j.jflm.2021.102220
4. Hameed A, Foster E, Main e, Khandelwal A, Lawton E. Cardiovascular Disease Assessment in Pregnant and Postpartum Women. November 30, 2017. Accessed June 29, 2023. https://www.cmqcc.org/ resource/3371/download.
Will you be conferred at the Fellow Convocation? (During Saturday Luncheon)
If yes, please deduct $50 from your total. One guest allowed (complimentary)
Will you be conferred at the Fellow Convocation? (During Saturday Luncheon)
□ I will be conferred □ I will bring a guest
If yes, please deduct $50 from your total. One guest allowed (complimentary)
-$50 $ EARLY BIRD DISCOUNT (until 10/09/2023) -$50* $
FHFM Donation (Tax Deductible) Tax ID 43-1480324 OPTIONAL $



FHFM MD DO Other: FAAFP
-$50 $ EARLY BIRD DISCOUNT (until 10/09/2023) -$50* $ Registration Name: AAFP ID#: Address: City: State: Zip: Phone: Fax: Email:


Deductible) Tax ID 43-1480324
LODGING INFORMATION GROUP CODE: 61X2HJ MORE INFO: WWW.MO-AFP.ORG/CME-EVENTS/AFC/

$
CME sessions, meals, breaks, and electronic syllabus included in registration fee. Exhibit hall functions for registrants only. By registering, I authorize MAFP to use photographs of me with or without my name for any lawful purpose, including print or online marketing.
Missouri Academy of Family Physicians
722 West High Street Jefferson City, MO 65101
