












































We use a term around Media MICE called “visit a printer.”
It dates back to 2009 where I went around Singapore visiting multiple printers, whereby I was “trained” to understand the printing aspect of publishing.

Although I learned journalism in school and in the work environment, up until 2009 I only understood the writing and editing portion. The entire production side to publishing was foreign to me.
And so I set about learning the other half of the profession in a foreign country with foreign printers in sometimes what seemed like a foreign language: “Singlish.”
I don’t recall any single printer that explained the process particularly well. But after visiting half a dozen or more, I had enough of an idea to create a publication. A4 size, opening to A3, check. 180 gsm, check. To complicate things, my first publications would have to be produced overnight, set to the printer at 9 pm, delivered at 9 am the next day to a conference venue. This was to happen several days in a row, to produce what we call “show dailies” in the industry.
Later on, as the team grew, we would visit printers in Malaysia, Hong Kong, Australia, China, India and beyond, always learning something new.
Throughout the process, something became apparent. While my education in journalism provided basic building blocks to the business I had chosen to develop, there would be times I’d have to learn and leap in order to develop the business in new areas.
This learning stage, we eventually called “visit a printer.” Based on what we had learned, it was then up to us if we wanted to leap or not.
2020 set the stage for a major leap. With
physical conference after conference cancelled, and no major digital conference providing any semblance of replacement in Asia-Pacific, we decided we might be able to pull off a major digital conference and exhibition in AsiaPacific.
We set about visiting “printers” so to speak, but in this case, we met with digital conference and exhibition vendors.

The complexities were enormous. With printers, the task was to imbibe as much information as possible. But with digital exhibition vendors, oftentimes we were bringing up points that were particularly relevant in the field of ophthalmology that they hadn’t considered before. Would ophthalmologists appreciate using game-like avatars to circulate around a digital exhibition hall? What would the average Internet speed be for our eye care visitors? Would they gravitate to the virtual exhibition hall from scientific sessions?
Of particular concern, we had organized a fairly well promoted “birthday party” for our 10-year anniversary two years prior in Bangkok at the Asia-Pacific Academy of Ophthalmology exhibition center, where we were the official media partner. I recall about 20 people came.
It was going to be a big risk to our solid publishing reputation if we were to fail at organizing an entire show. Healio had succeeded with Hawaiian Eye. Bryn Mawr had succeeded with Millennial Eye. But would we, in Asia-Pacific during virtual times?
Fortunately, the answer was a resounding yes.
The CAKE & PIE Expo (C&PE) was launched June 18-19, 2021. Nearly 2,000 people registered for the live days. 3,000+ views of the 24 sessions and 2 parallel tracks occurred. Hundreds of people visited individual exhibition booths. And for the most part – no small miracle – it ran on schedule. And it’s still on demand until July 19 at expo. mediamice.com for free, upon log-in.
Of all the various possibilities of what could have gone wrong, nothing major did. We had two leftover gallons of petrol to show for it, as they were hanging
out nearby our generator on the office roof, should a blackout have occurred. (Gloria, our Chief Editor, had another 2 gallons reserved at her home office over in southern Philippines … on day 2 of our expo, her town was on a 12-hour scheduled power blackout.)
In our profession, the word “education” often is used almost haphazardly, and usually has to do with that which happens in universities, during conference lectures, or even potentially through “enduring education” programs run by ophthalmic media.
But the next time you feel the need to learn something outside your comfort zone in order to make a business leap, remember it doesn’t take an Oxford degree to learn in life. Sometimes all it takes is visiting a printer.
 CEO & Publisher Media MICE, PIE, CAKE and COOKIE magazines.
CEO & Publisher Media MICE, PIE, CAKE and COOKIE magazines.
We would like to invite you to join our panel of experts as they explore the latest evidence and share their insights through informative patient case presentations and discussions.
Retinal disease today: Optimizing proactive patient care through evidence-based insights










Saturday, August 21, 2021 | 19:00–20:00 (SGT) | 13:00-14:00 (CEST)
“Achieving optimal outcomes for patients with retinal diseases, such as nAMD and DME, remains the goal of treatment. As clinicians we should understand the fundamentals for achieving optimal outcomes by considering all aspects of proactive patient care and through sharing of knowledge and practical guidance.”


Symposium Chair: Professor Paolo Lanzetta University of Udine, Italy

To register to attend the congress, click here.
Learn more about Bayer by visiting our online channels:
Prof. Gemmy Cheung, MBBS, FRCOphth (UK), FAMS, MCI, is currently a professor at Duke-NUS Medical School, National University of Singapore, and head of the Medical Retina Department at Singapore National Eye Center (SNEC). Her research focuses on retinal diseases, including age-related macular degeneration (AMD), polypoidal choroidal vasculopathy (PCV) and myopic macular degeneration, as well as risk factors for these conditions that may be unique to Asian populations. Prof. Cheung has more than 200 peer-reviewed publications and serves on the editorial boards of several journals, including the American Journal of Ophthalmology, Retina and Eye.

gemmy.cheung.c.m@singhealth.com.sg


Prof. Mark Gillies, MBBS, PhD, FRANZCO, presently holds a number of positions including: director of research and director of the Macula Research Group for the Save Sight Institute; foundation fellow for the Sydney Medical School; professor in the Department of Clinical Ophthalmology at the University of Sydney; head of the Medical Retina Unit at the Sydney Eye Hospital; deputy chair for the Ophthalmic Research Institute of Australia; and director of Eye Associates in Sydney. Prof. Gillies has served as a principal investigator or associate investigator in more than 70 clinical trials, and his research regarding macular degeneration and drug safety and efficacy has been published in 188 journals. He has also received a number of grants to study treatments for age-related macular degeneration, retinal disease and Muller cell dysfunction — among other treatments and studies. Prof. Gillies is a dedicated and multi-awarded researcher.

mark.gillies@sydney.edu.au
Prof. Dr. Vishali Gupta, MD, is an accomplished vitreo-retina and uvea expert of international repute. She currently works as a professor of ophthalmology at Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. Throughout her career, she has completed original work in the fields of intraocular tuberculosis, optical coherence tomography, diabetic retinopathy and fungal endophthalmitis. In addition, she is actively studying vitreoretinal and uveitis diseases. Prof. Gupta also holds a U.S. patent for the development of multiplex PCR for uveitis. In addition, she is a sought-after speaker and has delivered more than 870 invited lectures and conducted sev eral instruction courses at various international and national meetings. She has more than 200 publications in peer-reviewed journals; has edited five books and contributed 72 book chapters in textbooks. She is the secretary of the International Uveitis Study Group, and member of the AAO, Club Jules Gonin and the Macula Society. She is currently the president of the Uveitis Society of India. Prof. Gupta has received several awards for her work, including the first JN Pahwa award from the Vitreo-Retinal Society of India (VRSI), the first NA Rao Award from the Uveitis Society of India, and the first NA Rao award from All India Ophthalmological Society (AIOS).

vishalisara@yahoo.co.in









Expanding
+ Ultra-Widefield of view up to 200˚

+ Rich in details from center to periphery + Imaging through media opacities
iCare’s unique combination of sharpness and TrueColor offers now even wider view on the retina from 120° with a single shot, up to 200° with Mosaic functionality, helping to detect subtle signs of pathologies further in the periphery.*
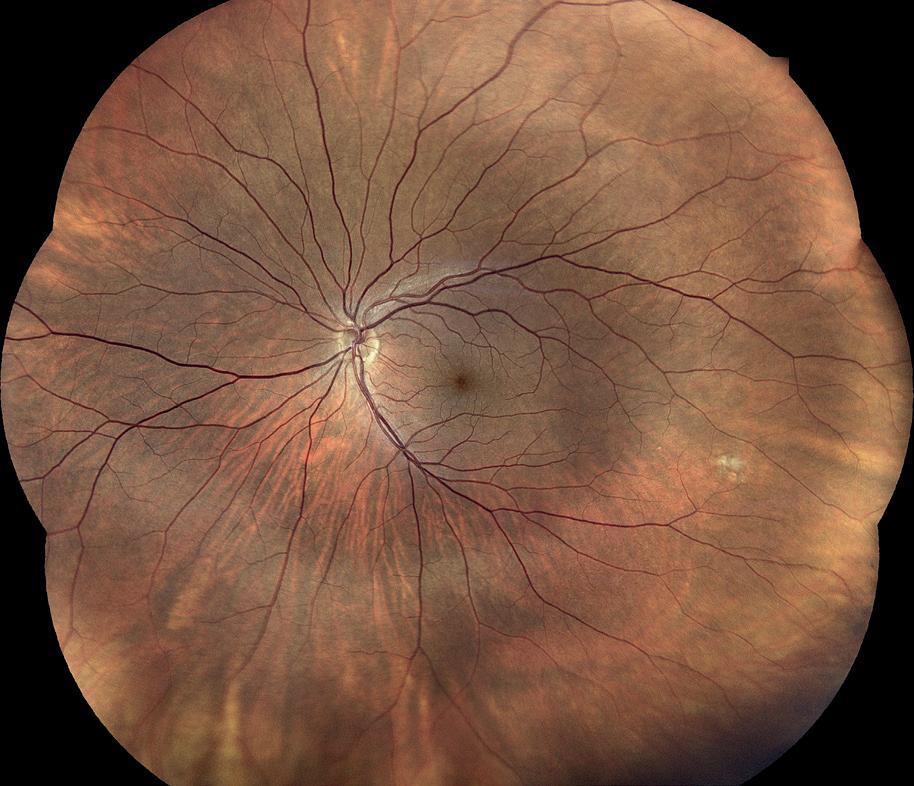
Discover the new Ultra-Widefield view of
Insert
For quite some time now, frequent intravitreal anti-VEGF injections to manage neovascular age-related macular degeneration (nAMD), diabetic macular edema (DME) and retinal vein occlusion (RVO) have been associated with a high treatment burden. Such reports from real-world data is steering the need for sustained-release (SR) antiVEGF drug delivery systems.

One of the many groups of investigators to address this is David Lutz, senior biological research scientist at AbbVie (Illinois, USA), and colleagues. The team compared the duration of effect
of a single intravitreal injection (IVI) of a sustained-release (SR) formulation of Abicipar pegol (Abicipar SR, Allergan, Dublin, Ireland), a novel investigational DARPin therapy, with a bolus dose of aflibercept in a rabbit model with persistent retinal vascular leak (PRVL).
New Zealand red rabbits previously injected in vitro with DL-2-aminoadipic acid (0.8mg; OD) to induce PRVL were injected in vitro with 50μL of either
Abicipar SR (500μg drug load; n=8) or aflibercept (700μg bolus; n=7). Results showed that a single IVI of Abicipar SR completely inhibited retinal leak in all eyes of the PRVL model for 22 weeks. Comparatively, the aflibercept treatment only completely inhibited retinal leak in all eyes for 10 weeks. The duration of effect of Abicipar SR was at least twice as long compared to aflibercept, providing 14 additional weeks of activity. Complete retinal leak suppression persisted in 71.4% and 42.9% of Abicipar SR-treated eyes at weeks 24 and 26, respectively. Both Abicipar SR and aflibercept were well tolerated with no intraocular inflammation observed.
Animal models currently available do not replicate clinically relevant aspects of AMD, despite being needed to test drugs in development to treat AMD. As such, Lakshmi Rajagopalan of AbbVie (North Chicago, Illinois, USA) and colleagues, did a study to compare the visual deficits in 1) non-human primates (NHPs) with blue light-induced macular damage, 2) a cohort of patients with AMD and 3) a cohort of age-matched healthy individuals, using similar imaging and vision psychophysics testing systems. This was to establish structural and functional correlates between the two species so that greater confidence in drug testing and predicting clinical efficacy can be achieved.
For the NHP model, eight cynomolgus monkeys were unilaterally irradiated (study eye, SE) with blue light centered on the macula (8mm diameter) for 20 to 30 min; while the contralateral eye (non-study eye, NSE) remained naïve. For the human study, 10 AMD patients with simplified Age-Related Eye Disease Study (AREDS) scores of 3 or 4, and eight age-matched controls were enrolled. Both NHP and human subjects were evaluated with fundus autofluorescence (FAF) and optical coherence tomography (OCT) to quantify retinal pigment epithelium (RPE) disruption and outer nuclear layer (ONL) thickness.
Results showed that in NHPs, the lesion was diffuse (late stage AMD; GA); while in humans it was multifocal (early stage AMD). In NHPs, mean log contrast sensitivity (CS) was 1.27 ± 0.06 (NSE) and 0.73 ± 0.08 (SE). Peak reduction was 0.68 log units at 6 cpd (cycles per

degree). In the human study, mean log CS in the control subjects was 1.34 ± 0.07; while in AMD patients it was 1.28 ± 0.06. Peak reduction was 0.16 log units at 3 cpd. A reduction in CS, as well as disruption of the RPE/photoreceptor outer segment complex/layer, was found in both NHP and human subjects. The reduction in CS was correlated with the severity of the damage. This study demonstrated that vision psychophysics can be used as a valuable tool in evaluating disease models and efficacy prior to clinical study initiation.
Geographic atrophy (GA), an advanced form of AMD, currently lacks an approved therapy to prevent or slow its progression. Lori-Ann Christie, senior director of biology at DTx Pharma (California, USA), and colleagues, investigated the cytoprotective effects of brimonidine, a potential agent for the treatment of GA, in an induced pluripotent stem cell (iPSC)-derived RPE model of AMD. iPSCs were derived from CD34+ cells isolated from peripheral blood samples of individual donors and differentiated into RPE. Cell viability was assessed using immunohistochemistry for propidium iodide after 24hour exposure to a broad range of brimonidine (3nM to 30μM).
The authors observed that pretreatment of iPSC-RPE cells with brimonidine prevented CC-HS-induced transepithelial resistance reduction and deposition of lipid droplets, as well as partial restoration of cyclic adenosine monophosphate (cAMP) and intracellular calcium levels in CC-HSchallenged iPSC-RPE cells treated with 3nM brimonidine. These data suggest that brimonidine has cytoprotective properties and preserves key functional RPE characteristics, restoring homeostatic mechanisms in cells challenged by an AMD-like insult.
A substantial proportion of diabetic macular edema (DME) patients show limited responsiveness to intravitreal anti-VEGF therapy. These patients show significant retinal edema and
vision impairment, despite evidence that intravitreal anti-VEGF therapy markedly reduces elevated VEGF levels in the vitreous. This suggests that other molecules may be involved in DME pathogenesis.
To investigate this, Matthew Mason, senior biological research scientist at AbbVie (North Chicago, Illinois, USA) and colleagues, compared known and putative permeability associated markers in the aqueous humor samples of 108 healthy nondiabetic control subjects at cataract surgery, non-proliferative diabetic retinopathy (NPDR) with absence of DME, and NPDR with DME. Of the 47 protein markers surveyed in DME subject samples, 13 were significantly upregulated when compared to control or NPDR following age-corrected univariate ANCOVA (analysis of covariance) with Dunnett’s correction for multiple comparisons.
Upregulated factors included angiopoietin 2, angiostatin, endothelin 1, hepatocyte growth factor, placental growth factor 1, stem cell factor, soluble epidermal growth factor receptor, soluble hepatocyte growth factor receptor, soluble urokinase plasminogen activator surface receptor, and thrombospondin 2 (p values < 0.001). Platelet-derived growth factor B dimer (PDGF AB/BB) was downregulated compared to CTL (p< 0.01). The study identifies several angiogenic factors in the aqueous humor that are strongly associated with DME, prompting further investigation as prospective biomarkers for disease progression and modification.

It is thus necessary to mitigate immunogenic responses in order to effectively test the pharmacodynamics and pharmacokinetics of new biologics. Lisa Hernandez-Denlinger, biological research scientist at AbbVie (North Chicago, Illinois, USA) and colleagues, investigated the methotrexate (MTX)induced immune tolerance in a rabbit model with persistent retinal vascular leak (PRVL).
PRVL rabbit models were treated with immunosuppressive drugs methylprednisolone acetate (DepoMedrol®; 10mg/kg intramuscular [IM], single dose) or MTX (5mg/kg IM or 30mg/kg subcutaneous [SC] dosed daily for 14 or 24 days, respectively). They found that the incidence of moderatesevere ocular inflammation was eliminated in MTX-treated rabbits, which coincided with significantly reduced systemic anti-drug antibody (ADA) titer levels compared to phosphate buffer saline (PBS) treated controls.
The Association for Research in Vision and Ophthalmology (ARVO 2021) annual meeting was held virtually on May 1-7, 2021. Reporting for this story took place during the event.
Histologic evaluation determined that 4/10 eyes of PBS-treated rabbits showed substantial lymphoplasmacytic infiltrate following IVT administration of the biologic while eyes of MTX-treated rabbits did not. The authors concluded that a course of MTX can dramatically reduce unwanted ADA formation after IVT injection of an experimental biologic, as well as intraocular inflammation. With this, animal attrition can be avoided, which allows for better deployment of rabbit models used to study IVT biologics.
Immunogenicity can complicate preclinical testing of biologics.
It is no secret that high intraocular pressure (IOP) can wreak havoc on the mechanics of healthy eye functioning. Axonal damage can occur, as well as disruption of nutrient delivery, which eventually leads to cell death of retinal ganglion cells and vision loss. Despite our best efforts to achieve pressure control, some glaucoma patients with reduced or normal IOP still experience optic nerve damage and vision loss.
Within our diagnostic arsenal, we rely on pressure checks, dilated exams and visual field tests to assess structure and function and guide our management decisions. Even though optical coherence tomography (OCT) does not provide insight into visual function, it is widely used to evaluate neural loss in our glaucoma patients. A quick and non-invasive OCT delivers quantitative and reproducible measurements across several glaucoma-affected structures, including the retinal nerve fiber layer (RNFL). So, now you have all these OCT measurements, what do they mean?
Can OCT be the “Magic 8-ball” in predicting functional deterioration in glaucomatous eyes? The thought is that, even in glaucoma suspect eyes, OCT may detect early structural changes and damage before these changes result in detectable visual field defects. For those already well into their


glaucoma journey, advancing neural tissue loss observed on OCT, may be predictive of disease progression and outcomes.
As with so many ophthalmic conditions, the key to better outcomes and vision loss prevention lies in our ability to detect and intervene at earlier stages — and in glaucoma, OCT may be that key.
Although we have seen early studies that investigated whether OCT measurements are predictive of future functional deterioration, which they seem to be, their findings were reported in hazard ratios. From a research perspective, a hazard ratio is based on sound statistical methodology. Translating a reported hazard ratio into how we approach our daily clinic patients is a very different story. Ideally, we could look at a patient’s OCT thickness measurements over time and be able to give that patient some idea as to how and when they may experience visual field changes in the future.
Swarup S. Swaminathan, MD, assistant professor of clinical ophthalmology at Bascom Palmer Eye Institute at the University of Miami Miller School of Medicine agreed: “For a given RNFL thinning, the risk of SAP [standard automated perimetry] deterioration may be 2 or 3 times higher than a certain baseline, but remain relatively small in magnitude. Hazard ratios are relative measures which do not help a clinician decide whether a specific rate of change on OCT actually carries a risk of fast visual field progression for an individual patient.” Dr. Swaminathan and colleagues recently published their work in the American Journal of Ophthalmology, “Rapid initial OCT RNFL thinning is predictive of faster visual field loss during extended
follow-up in glaucoma.”* Their study investigated the relationship between the extent of RNFL thinning seen during an initial period of follow-up in their glaucoma patients and the magnitude of visual field loss over an extended follow-up period.
Dr. Swaminathan and colleagues assessed 1150 eyes of 839 patients from the Duke Glaucoma Registry. The rate of RNFL loss was based on global RNFL thickness values of the patient’s first five OCTs, and categorized as fast, moderate or slow progressors based on ≤-2µm/year, -2 to -1µm/ year and ≥-1µm/year, respectively. The corresponding rates of visual field loss were assessed using SAP mean deviation across the entire follow-up period.
The group had hypothesized that, “fast initial RNFL progression would be associated with fast visual field progression, justifying the rationale for and providing guidance to the use of longitudinal OCT results in assisting clinical decision-making in glaucoma.”
So, what did their results show? As expected, rapid initial RNFL thinning was predictive of concurrent and subsequent rates of visual field decline over the follow-up period,
which extended to nearly more than 6 years. More specifically, 66% of eyes were categorized as slow, 29% moderate and 5% fast progressors, and the corresponding rates of RNFL thinning were -0.36µm/year, -1.34µm/ year, and -2.87µm/year respectively. The rates of RNFL were statistically significantly associated with rates of SAP MD loss in all groups, a -0.16 dB/y loss for the slow group, -0.32dB/y for moderate and -0.71dB/y for the fast group. Additionally, in a multivariable model, age, OCT progressor group and concurrent SAP rate were all significantly associated with overall rate of SAP MD loss.
Dr. Swaminathan describes how these findings solidify OCT in glaucoma management strategy. “These results provide further evidence to support a common clinical practice in glaucoma management, namely altering glaucoma treatment based on changes in OCT RNFL alone.” He added: “Clinicians are correct in their belief that those with rapid changes on OCT will ultimately exhibit rapid progression on visual field testing.”
Noting the immediate applicability of these findings to our daily practice, Felipe Medeiros, MD, PhD, professor of ophthalmology at Duke University School of Medicine, and senior author on the paper shared his impression: “These results have important implications for the use of OCT in clinical practice, as well as for validating OCT as a potential biomarker to be used in clinical trials.”
These results support what our instincts have been telling us all along, but to have actual rates and values from more than 1100 eyes, justifies the belief that
observed RNFL thinning on OCT will likely be accompanied by concurrent or future rapid visual field loss. The clinical implications are tremendously valuable. “Those patients classified as fast progressors by OCT may be at higher risk for developing subsequent functional disability. In addition, this finding may be used to identify eyes at risk for fast visual field progression when designing clinical trials in glaucoma,” he concluded.

Swarup S. Swaminathan , MD is a board-certified ophthalmologist focused on caring for patients with cataracts or glaucoma. A magna cum laude graduate of the Harvard-MIT Health Sciences and Technology program at Harvard Medical School, Dr. Swaminathan completed his residency at the Bascom Palmer Eye Institute. He subsequently completed a fellowship in glaucoma at the Duke Eye Center, where he was mentored by Drs. Leon Herndon, Sanjay Asrani and Felipe Medeiros. Dr. Swaminathan is eager to work with his patients to identify optimal medical, laser or surgical options to treat their glaucoma, including the use of traditional surgeries as well as minimally invasive glaucoma surgeries (MIGS). Dr. Swaminathan has received multiple accolades, including the Barry M. Goldwater Scholarship for his research in protein biochemistry, the Howard Hughes Medical Institute Medical Research Fellowship to study trabecular meshwork dysfunction in glaucoma, and the Heed Ophthalmic Foundation Fellowship, awarded to young ophthalmologists with a strong dedication to ophthalmic research. With a keen interest in imaging research in glaucoma, Dr. Swaminathan is eager to assist ophthalmologists in improving their ability to diagnose glaucoma and identify patients at high-risk for vision loss.
sswaminathan@med.miami.edu



o be fair, the Media MICE team is hardly traveling anywhere right now (though your correspondent recently received his vaccine, so here’s hoping that will change soon) but do please come in, settle down, and join us on this expedition into the rare and remarkable world of posterior segment practice.
Editor’s Note (and a bit of inside information): Your current writer has something of a reputation within the editorial team. Up until remarkably recently, I was incredibly squeamish about eyes. But since joining the funkiest ophthalmology team around, I have become fascinated by the weird and rare. Whether it be ocular syphilis or unusual forms of childhood glaucoma — if it’s strange, odd or even a bit terrifying, it lands on my desk.
And to be honest, I love it, becoming enamored with the strange cases of ophthalmology has been remarkably cathartic. Before I could not even look at someone inserting a contact lens into their eye, I can now devour research papers about ocular tumors, gangrene and all other sorts of disease. But it is not all distanced scientific curiosity — in fact, for the first condition in this article, it’s personal.


Tuberculosis (TB) is still one of the most common diseases today and it’s endemic
in many parts of the world. At any point in time, up to two billion people (that’s around one-third of the planet’s total population) are affected by the disease, but most of them will not present the stereotypical symptom of a persistent cough with bloody phlegm. Most people carry the virus as a latent condition, which may or may not develop into the active form at a later date … and I was one of them.
The difference between active and latent TB was not something I was unaware of when I was diagnosed, and perhaps mercifully, I was unaware of ocular TB too. While 80% of patients with active TB are affected primarily in the lungs, the remaining 20% may be affected in other organs, including the eye. Indeed, ocular tuberculosis is usually not associated with clinical evidence of pulmonary tuberculosis, as up to 60% of extrapulmonary tuberculosis patients may not have pulmonary disease.¹
consultant of vitreoretinal and refractive surgery at Pink City Eye & Retina Center (Jaipur, India), once treated a 28-year-old woman who presented with progressive loss of vision in her right eye. Best corrected visual acuity (BCVA) was 20/800 in the right eye and 20/20 in the left eye; the anterior segment was unremarkable; and a fundus examination of the right eye revealed a large globular convex elevation of the retina, with a yellowish mass lesion underneath.
“A vitreous biopsy was planned and performed, with the specimen being processed for cytology and a patented multiplex PCR test, the latter of which revealed mycobacterium TB DNA. Systemic anti-tuberculosis treatment (ATT) was promptly initiated and systemic steroids were added after a week. While steroids were tapered over six weeks, ATT was continued for nine months,” Dr. Kothari shared.
Step right up folks, and prepare to peer into the perfectly petrifying world of ophthalmic oddities. Hold on to your hats, your glasses — and even your contact lenses — because you’re in for a spectacle. Truly, you will be shocked to the core by the marvelous and malign medical mysteries that permeate this particular specialty. I will be your guide on this journey into the jungle of healthcare horrors and disturbing diseases … but have no fear, because nothing can harm you while you’re in the very capable hands of the Media MICE traveling show.
inflammation. No evidence of tuberculosis was found in the chest or the brain and in the absence of any indirect evidence, the definitive diagnosis and successful treatment rested solely on the invasive vitreous biopsy sample,” explained Dr. Kothari.
“In this case, the lesions in both eyes showed remarkable resolution over time with a temporal scar in the right eye and barely noticeable pigmentary alterations in the left eye. Visual acuity was restored to 20/20 in the right eye,” he added.
Imagine if you visited a zoo that advertised itself as playing home to a Siberian Tiger, truly a mighty and rare beast that by some miracle was available for you to see. Upon entering the tent full of excitement to see this mighty feline of legend, you end up finding yourself staring at a Scottish wildcat. Sure, they are pretty cool and rare in their own way, but they’re not the greatest tiger species on earth.
In this analogy the delightful Scottish wildcat represents macular hole (MH). This is a rare, though not Siberian Tiger rare, condition that affects the retina and occurs when the nerve cells of the macula become separated from each other and pull away

Symptoms of MH include a decrease in the ability to see fine details, a change in vision that makes a person feel like he or she is looking through dense fog or thick, wavy glass, and the appearance of a dark spot across the middle of the field of view.²
MH is wildcat rare, and traumatic MH is a veritable Siberian Tiger. This is a very rare complication of a blunt or an open injury of the globe and can lead to permanent loss of vision. Patients usually tend to be younger and a significant percentage of cases result from sporting injuries, but there are even less common causes.³
Dr. Alay S. Banker is the director of Banker’s Retina Clinic and Laser Centre (Ahmedabad, India), and as a retina specialist has seen some remarkable cases. Of all of these, perhaps the most shocking is an incredibly rare occurrence of MH caused by accidental exposure to a dermatological laser. The patient involved, a 25-year-old woman, was a skincare professional self-administering a dermatological laser.
“The patient was skin bleaching using a SPECTRA cosmetic laser machine with a 1,064nm wavelength. She was not wearing any protection for her eyes, and while she was adjusting the laser probe
it slipped. She heard a “pop” sound and saw a bright flash, followed immediately by floaters and blurred vision in the right eye,” Dr. Banker said.
“The laser injury resulted in the endothermal destruction of the retinal layers causing a macular hole. This usually causes loss of central vision, along with micropsia and metamorphopsia. We diagnosed the issue via clinical macular examination and optical coherence tomography,” he said.
“One should always wear protective eye wear while using lasers, and one must be aware of the potential damage they can cause to the eyes,” he added.

Our last ocular oddity is usually only encountered in a few countries — in particular, Turkey. According to Dr. Koushik Tripathy, a vitreoretinal and uvea consultant at ASG Eye Hospital in Kolkata, India, Behçet’s disease (BD) is a chronic, multisystemic disease characterized by recurrent inflammatory episodes involving various organs and tissues, recurrent oral ulcers, recurrent scrotal and genital ulcers or scarring, vasculitis, and skin lesions including pseudofolliculitis, erythema nodosum, acneiform nodules, and lastly papulopustular lesions. That is all pretty horrific, but the disease of course, has an ocular component (Behçet’s uveitis) which is characterized by bilateral recurrent non-granulomatous panuveitis and occlusive retinal vasculitis, sometimes combined with vitritis, with patches of retinitis also being common.
“BD typically affects countries falling on the historic Silk Road for trading and appears in countries like Turkey (which has the highest rates), as well as Iran, Saudi Arabia, Iraq, Israel and Japan,” said Dr. Tripathy.
“We do not know why it is so prevalent in Turkey, but one possible explanation is genetic susceptibility thanks to the HLA B51 gene. However, environmental factors may be more crucial as there is a low prevalence of BD in Turks residing in Germany. Also, BD is associated with a lower socioeconomic status and a higher unemployment rate,” he said.
When you compare the prevalence rate of BD between Turkey and the United States, a remarkable disparity is clear, with rates of 80 to 370 per 100,000 in Turkey compared to 5.2 per 100,000 in the U.S. However, despite its relative rarity in the U.S., more American patients reported substantial morbidity related to their disease compared with Turkey.⁴
Regardless of a patient’s geographic location or comorbidities, clinicians can struggle to diagnose BD because no pathognomonic laboratory test currently exists, according to Dr. Mirta Avila Santos, executive director of the American Behcet’s Disease Association in Rochester, Michigan.

“In the United States, women are more often affected; however, it is more common among men in other countries. Clinicians must be aware of the signs and symptoms of BD, particularly of recurrent oral ulcers, and must continue to follow patients closely to arrive at a definitive diagnosis,” Dr. Avila Santos said.

“Better randomized control clinical trials and biomarkers, as well as natural history studies will help accelerate pathways to better diagnostics and treatment,” she added.
Remember dear reader, to step right up next time the PIE magazine carnival comes to town to regale you with all that is rare and remarkable in the world of the retina. We’re sure the next time our crazy carnival comes to your town, we’ll have the real Siberian tiger cases for you to sink your claws and teeth into. In the meantime, please, please remember: Wear goggles if you are using lasers...
References:
1. Shakarchi FI. Ocular Tuberculosis: Current Perspectives. Clin Ophthalmol. 2015;9:2223-7.
2.
Dr. Abhishek Kothari is the director and chief consultant in vitreoretinal and refractive surgery at Pink City Eye & Retina Center in Jaipur, India. He received his medical degree from Coimbatore Medical College and completed his ophthalmology residency at S.M.S. Medical College, Jaipur. He has considerable experience in cataract, refractive and retinal surgery, and has particular interests in research into advanced diagnostics, ocular infectious diseases and newer therapeutics.



dr.a.kothari@gmail.com
Dr. Alay S. Banker is the director of the eponymous Banker’s Retina Clinic and Laser Centre in Ahmedabad, India. He held a vitreoretinal fellowship at the Medical Research Foundation, in Madras, India, and was previously a clinical instructor and fellow at the Department of Diseases of the Retina and Vitreous, Uvea and Inflammation of Eye at the University of California, San Diego. He received the International Ophthalmologist Education Award by the American Academy of Ophthalmology in January 2009.
alay.banker@gmail.com
Dr. Koushik Tripathy is a vitreoretinal and uvea consultant at ASG Eye Hospital in Kolkata, India. He received his medical degree with a specialization in ophthalmology from the All India Institute of Medical Sciences in New Delhi. The author of a number of research papers covering various areas of ophthalmology, Dr. Tripathy holds particular interests in Behçet Disease, retinal diseases, and macular degeneration.
koushiktripathy@gmail.com
Dr. Mirta Avila Santos is the executive director at the American Behcet’s Disease Association. She received her medical degree from the Pontificia Universidad Católica Madre y Maestra (Mother and Teacher Pontifical Catholic University) located in Santiago de los Caballeros, the Dominican Republic. She has considerable experience of working in non-profit organization management and the medical sector.
mavilasantos@behcets.com
Macular Hole. The Cleveland Clinic. Available at https://my.clevelandclinic.org/health/diseases/14208macular-hole. Accessed on Wednesday, June 2, 2021. 3. Fiortenzis M, Seitz B, Viestenz A. Traumatic Macular Hole. Klin Monbl Augenheilkd. 10.1055/a-0608-4780. 4 Sibley C, Yazici Y, Tascilar K, et al. Behçet Syndrome Manifestations and Activity in the United States versus Turkey — A Cross-sectional Cohort Comparison. J Rheumatol. 2014;41(7):1379-84.As the name suggests, rare diseases are uncommon — but that doesn’t mean they’re not encountered. According to a 2019 study¹:
1 10 people are affected by rare diseases
350M
1 2 patients diagnosed with a rare disease is a child people suffer from a rare disease globally
8 10 rare diseases are caused by a faulty gene
8yrs
is the average time it takes for rare disease patients to receive an accurate diagnosis
95% of the rare diseases lack an FDA approved treatment
Tears tinged with blood usually signal another underlying problem.
There are different forms of the disease, but all are fatal — doctors are still working on a treatment
There’s no cure, but promising treatments like bionic eyes are in development.
Stargardt disease can go undetected until adolescence or adulthood, when blurry or distorted vision develops.
Extremely rare in in in
25 100,000 12 100,000 6 100,000
There’s not yet a treatment, but gene therapies and stem cell therapies may alleviate or cure this condition in the future.
People of Asian descent are most likely to develop this condition. There is not yet a cure or treatment
1.5 100,000 in
This syndrome causes various eye problems including a thin iris and an off-center pupil — and in some cases, extra holes in the iris can give the appearance of multiple pupils. In other cases, the cornea is affected.
4 100,000 <1 100,000
in in
In the United States, a disease is considered “rare” if it affects less than 200,000 people.
Here are some of the less common pathologies treated by ophthalmologists.²
 by Brooke Herron
by Brooke Herron
While the COVID-19 pandemic has reinforced the importance of remote monitoring and telemedicine for progressive ophthalmic diseases, the technology — and need — has existed for quite some time.
This is especially true for conditions that impact sight and have no cure, like age-related macular degeneration (AMD), which is a leading cause of visual impairment and severe vision loss in industrialized countries. In its advanced stages, AMD comes in two forms: wet and dry, both of which lead to vision loss. Wet AMD will develop in 10 to 15 percent of people with intermediate AMD and often the progression from dry to wet is not caught until vision loss has already occurred.¹
Because baseline vision is a strong determinant of long-term vision, early detection of wet AMD can be crucial to achieving favorable therapeutic outcomes. Further, a recent cost-utility analysis reported that early treatment was 138 to 149 percent more costeffective than late treatment² — and this, combined with better outcomes, cements the need for early detection.
The standard of care for AMD
monitoring includes routine office visits and using an Amsler grid. However, the grid does not always provide early detection — meaning, when distortion is noticed on the grid, vision may have already been lost. In fact, wet AMD may be present for 6 to 12 months before detection and treatment.³ And although the Amsler grid has long been used for home monitoring, its efficacy can be compromised by patients’ perception of distortions and compliance. In fact, no well-designed clinical trial has shown that the Amsler grid is effective in detecting wet AMD in patients with good visual acuity (VA).²
And of course now, during a global pandemic, routine office visits are no longer an option for many people — either out of fear of contracting COVID-19 or due to office closures and other regulations. This is precisely where home monitoring can have a big impact.
In fact, a recent large-scale data analysis of 3.2 million tests, titled RealWorld Performance of a Self-Operated Home Monitoring System for Early Detection of Neovascular Age-Related Macular Degeneration² found that
remote monitoring using the ForeseeHome (Notal Vision, Manassas, Virginia, USA) provided significant benefits by helping to detect wet AMD earlier and with better visual acuity. This has been found to have a positive impact on long-term anti-VEGF treatment visual outcomes.
This retrospective analysis from the Notal Vision Diagnostic Clinic, the medical provider of the ForeseeHome remote monitoring program, included 306 eyes that converted to wet AMD between October 2009 and September 2018. Of the 306 eyes with confirmed disease progression, 211 (69%) were identified following the at-home system alert, and the remaining 95 (31%) were identified during a routine or a symptom-driven visit.
The authors found that functional vision (of 20/40 or better) at conversion was maintained in 81% of patients in the
real-world ForeseeHome cohort compared to only 34% in the IRIS® Registry real-world data using standard of care. This is a substantial difference and clearly illustrates the benefits of home monitoring.
Dr. Allen C. Ho was the study’s principal author. He said: “This real-world data analysis confirms that the use of ForeseeHome provides a significant benefit to patients as a means of increasing the early detection of wet AMD when vision is
“Earlier detection of wet AMD with this FDA-cleared device is a strong predictor of better vision over time with current anti-VEGF therapy. ForeseeHome can be a useful strategy to monitor at-risk intermediate AMD and help protect vision. The era of at-home digital monitoring of medical conditions including AMD continues to
evolve and improve for patient benefit,” continued Dr. Ho, who is also director of Retina Research of Wills Eye Hospital and professor of ophthalmology at the Kimmel School of Medicine at Thomas Jefferson University in Philadelphia, Pennsylvania, USA.
This was echoed by another study author, Dr. Jeffrey Heier, who serves as director of the Vitreoretinal Service and director of Retina Research at Ophthalmic Consultants of Boston (Massachusetts, USA): “Artificialintelligence enabled home monitoring between office visits could be extremely helpful in early detection of conversion and the ForeseeHome program is a meaningful complement to the at-risk dry AMD patient’s care plan.”
The authors added that in today’s climate, the ability to detect AMD conversion — while limiting potential exposure to COVID-19 — certainly adds even more value. “It may drive physicians, patients, and their families to request access, gain benefit from the expected performance, and drive a large-scale improvement in the quality of life of this growing population,” concluded Dr. Ho and authors.
The Notal Vision Diagnostic Clinic includes patient engagement, If you just saved some vision, you’d dance too.
compliance monitoring and alert generation services; ForeseeHome is part of this comprehensive monitoring program by Notal Vision.
To use the device, patients do a short, daily test on the device. Results are automatically transmitted to the Diagnostic Clinic and when a statistically significant change in visual distortion is detected, the referring physician is alerted to determine the best course of action.
“The newly published real-world data shows that the performance of the ForeseeHome program resembles the findings from the randomized controlled AREDS2-HOME study, which ultimately led to Medicare coverage,” said Kester Nahen, PhD, CEO of Notal Vision.

“The Notal Vision Diagnostic Clinic is proud to partner with physicians by providing complementary care for their patients.”
References:
1. Waugh N, Loveman E, Colquitt J, et al. Treatments for dry age-related macular degeneration and Stargardt disease: a systematic review. Southampton (UK): NIHR Journals Library; 2018 May. (Health Technology Assessment, No. 22.27.) Chapter 1, Introduction to age-related macular degeneration. Available from: https://www.ncbi.nlm.nih.gov/books/ NBK500483/.
2. Ho AC, Heier JS, Holekamp NM, et al. Real-World Performance of a Self-Operated Home Monitoring System for Early Detection of Neovascular Age-Related Macular Degeneration. J Clin Med. 2021;10(7):1355.
3. Ho AC, Albini TA, Brown DM, Boyer DS, Regillo CD, Heier JS. The potential importance of detection of neovascular age-related macular degeneration when visual acuity is relatively good. JAMA Ophthalmol. 2017;135(3):268-273.
A version of this article was first published in piemagazine.org on May 5, 2021.

Highlights from OIS Digital Innovation Showcase
by Chris HigginsonHistorically, acquisitions and mergers have been fairly small compared with other deals happening in Silicon Valley. But now, “mega deals” — or deals over $100 million — are becoming common as gigantic tech companies merge with healthcare intuitions and providers.
Dr. Ranya Habash, from the Bascom Palmer Eye Institute (Miami, Florida, USA), opened the recently held OIS Digital Innovation Showcase by going over the four biggest trends in the digital health sphere, happening right now:
• Mergers, acquisitions, SPACS (special purpose acquisition companies) which help start-ups go public faster, and mega deals
• On-demand healthcare
• Data management
• Consumer empowerment
The COVID-19 pandemic has encouraged the growth of on-demand healthcare. Patients are both more willing and more able to engage in telehealth, with a larger number of patients seeing more doctors online. In the future, not just consultations, but basic tests will be done at home, allowing more flexibility for both doctor and patient.
Patients want control of their healthcare data, but there is also the potential to share data among healthcare professionals. In the future, doctors may be able to look at all aspects of a patient’s health, from exercise to diet and lifestyle, in order to recognize diseases as they emerge.
Consumer empowerment is currently on the rise, as huge numbers of people are using wearable tech every day and providing that information to their doctor, along with potential diagnoses and questions they’ve found online.
Carl Zeiss Meditec’s President of Ophthalmic Devices and Head of Digital Business Unit, Euan S. Thomson, PhD, joined this OIS event’s fireside chat with Dr. Tanya Habash to discuss his insights on the rise of telemedicine.
Needless to say, COVID-19 gave telemedicine a huge boost, but it has continued to grow, even as restrictions were later lifted and life returned to normal (or the “new normal”) in many parts of the world. However, due to the number of tests and imaging that are a part of any ophthalmology consultation, it will always require more in person meetings than other branches of medicine.
According to Dr. Euan S. Thomson, artificial Intelligence (AI) will grow and increase in importance in ophthalmology due to the high number of images that need interpretation. AI has the potential to be able to look for changes a person might miss; easily compare changes over time; and, using patients’ information from the cloud, look for disease patterns in data that their doctor isn’t specialized in — such as cardiac tests or brain function.
The Internet of Things (IoT), meaning patients’ increased use of wearable tech that can monitor their health, will also grow in importance. IoT can enable
“holistic management of the patient,” allowing professionals to monitor a patient’s overall lifestyle, which has a huge impact on patient health. Consistent observation means chronic diseases such as diabetic retinopathy, and even myopia, can be constantly monitored, rather than relying on occasional examinations by a specialist.
In 2020, the ZEISS Group (Jena, Germany) partnered with Microsoft Corporation (Washington, USA)* to expand the digital healthcare marketplace and to build a platform that’s both secure and accessible, so patients can upload more of their healthcare data into the cloud, without needing to worry about data security. The idea is that all of a patient’s data — from doctor’s diagnosis, to x-rays, ophthalmological images and wearable data — will be stored in one “connected cloud environment” and accessed by the professionals who need it, along with the patients themselves.
This means that by having all the data in one place and by giving access to professionals who wouldn’t normally see some parts of it, insights can be generated that couldn’t be generated any other way. In addition, once it [data] is anonymized, it can be pooled with data from people all over the world, making it a lot easier for researchers to get hold of large amounts of data they wouldn’t have been able to see before.
The OIS Digital Innovation Showcase was held on 20 May 2021. Reporting for this story took place during the event.
Dr. Thomson’s hope for the future is that the digital healthcare space includes more of the data that surrounds a patient and gets better at bringing in long-term data, as well as including their patients’ lifestyle, to see what effect that has on their health. This jump in data quantity should mean that doctors get better at understanding disease cycles and allow them to manage diseases in a more holistic way. The future lies in large scale collaborations and data-sharing, with a broad view of what constitutes medical data, activities such diet, sleep, stress, etc., as we know these things influence our health, but we haven’t been able to quantify the effect until now.



Ophthalmic science got a shoutout in a fascinating, if very human-interest story-driven, Netflix documentary dubbed Unnatural Selection. We love it when ophthalmology goes mainstream, and this was a great example of the cutting-edge of ophthalmic science.
It wasn’t just ophthalmic science, of course — the documentary was all about gene therapy, gene editing, and “biohacking,” the movement that has seen CRISPR/Cas9 labs move into basements, garages and spare rooms. The democratization of gene editing terrifies some — and thrills many others.
We’re at the beginning of a revolution in gene therapy, and genetic eye disorders will hopefully be a thing of the past once we collectively move forward.
Part of the documentary focuses on a boy named Jackson, who has inherited faulty RPE65 genes from his parents. The condition inexorably leads to blindness, which is especially poignant because Jackson dreams of being an astronaut. Unfortunately, astronauts
need 20/20 vision, which Jackson does not have. As of the documentary, he can detect light and that’s about it.
But a new gene therapy drug on the market can potentially fix these faulty genes and restore sight. Let’s dive into the good stuff.
Luxturna (voretigene neparvovec-ryzl) is a gene therapy injection developed by Spark Therapeutics (Philadelphia, Pennsylvania, USA). Rather than gene editing, it relies on an innocuous virus to inject a healthy version of the RPE65 gene into the eye, which changes the DNA replicating in the eye. It can work as fast as a few weeks, and may hail a new era of ophthalmic gene therapy. It promises to restore vision, though not necessarily perfectly. But if you’re nearly blind, any improvement in vision is a win.

Luxturna was approved by the FDA in 2017, the same year that the first gene therapy of any kind was approved. Nearly a decade of research went into
by Sam McCommonthe development of the drug, and we struggle to imagine the man-hours of labor involved.
Despite the enormous amount of time in trials, there was a relatively small cohort of patients tested in phase 3 — 41, to be specific. Finding patients who have the RPE65 defect may be plenty of a chore in itself, and then finding ones willing to undergo clinical trials narrows the field even further.
But for those with the faulty RPE65 gene, even a shot in the dark is better than guaranteed blindness. Add in the fact that it is indeed FDA approved, and what reasonable person wouldn’t do just about anything to give their loved one the chance to see?

Of course, nothing this miraculous could happen in the current U.S. environment without some sort of catch. And there’s more than one, but we’ll start with the biggest one: the cost.
Luxturna costs a mind-boggling $850,000 for a one-time treatment, or $425,000 per eye. Since the vast majority of people don’t have $850,000 in cash sitting in their bank account, this price can represent an insurmountable challenge.
As was shown in the documentary, and completely unsurprisingly, insurance companies are reluctant to want to cough up that much money. In Jackson’s case, his insurance company wouldn’t pay for genetic testing, so the viewer is left to assume his parents had to pay for it out of their own pocket.
Spark Therapeutics is trying to help families afford such an astronomical sum by introducing different pricing programs, like outcome-based treatment, installment payments, and more. But the problem remains: This treatment is exorbitantly expensive.
The documentary cites philanthropic medical advances, like how Jonas Salk refused to patent his polio vaccine or the discoverers of insulin sold their patent for $1. That sort of humanitarian thinking didn’t take place here. Now, of course, you can’t expect a company to spend years developing a treatment and then expect to do them for free — a for-profit company can still make a lifechanging treatment and doesn’t have to be a charity.
But much of the money for the research behind Luxturna was taxpayer-funded through the National Institute of Health (NIH) and the European Commission. The treatment received orphan status,
meaning it likely would not have been commercially viable without government assistance.
To have a treatment granted orphan status and then turn around and charge nearly a million dollars certainly raises eyebrows, and has certainly drawn at least some ire from activist and watchdog groups. As one man in the documentary lamented, “They could just lower the price.”
When asked “How much is your vision worth?” most people will say something along the lines of “everything.” Perhaps that’s why the price is so high — companies know that parents will sell their house and maybe even a kidney if their doomed-to-be-blind child has a chance of seeing.
As PIE magazine recently reported, there’s a high potential for ocular complications involving gene therapy treatments. In the phase 3 trial of voretigene neparvovec, 27 of the 41 patients experienced complications — a rate of 66%. That’s quite a high number, and would make anyone take pause.

As Dr. Steven Tsang of Columbia University pointed out, the majority of the complications in gene therapy treatment come from the method of application. Luxturna requires a subretinal injection and retinal detachment — something that certainly spooked Jackson, though not enough for him to steer clear of the treatment.
The most common adverse effects in the phase 3 trial were conjunctival hyperemia (22%), cataract (20%), increased intraocular pressure (15%) and retinal tear (10%).* These are all treatable conditions, but they should still be taken into account for anyone considering the treatment.
The tagline that accompanies the documentary’s intro goes, “All technology is inherently about changing away from what is natural.”
While that may seem an accepted fact
on the surface, considering it a bit more closely leads to some questions. First, it assumes that humans are separate from nature, and technology is “artificial” or somehow itself not part of the natural world. Second, it implies that gene therapy is unnatural.
The first assumption only works if you see humankind and its efforts as somehow removed or separate from nature. Where do we draw the line? Is man-made fire natural? Stone tools? Iron tools? Space flight? Gene therapy? Is new technology somehow unnatural despite the fact that it was created by humans, who are ourselves a product of nature?
Second, our species has been practicing gene therapy for tens of thousands of years via selective breeding — gene therapy is just a new way to do it. Are Chihuahuas or seedless watermelons natural? Are Norman Borlaug’s worldchanging advances in agricultural science unnatural?
We’ve got to stop here before we go too far down the philosophical rabbit hole, but these are questions worth addressing. Unnatural Selection does a good job of raising questions in the audience, and we think it’s worth a watch. Gene therapy is something that we’re just at the dawn of, and it’s good to have at least a crash course on it.
Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet. 2017;390(10097):849-860. Erratum in: Lancet. 2017;390(10097):848.
Unnatural Selection is a documentary series available on Netflix.by Nikki Hafezi, MAS IP ETHZ
This story is a continuation of CEO Nikki Hafezi’s professional journey and successes. Read Part 1 in PIE 17
EMAGine is where I pulled together all of my eclectic experiences: practical, educational, networking, private, public and governmental. It was an opportunity to demonstrate my understanding of what I’ve learned in these past 15 years.
The story started in 2011 when my husband, Farhad, was the director of the University Eye Clinic in Geneva. One of Farhad’s biggest clinical and research interests is corneal cross-linking (CXL). CXL is used to treat corneas that have been weakened thanks to ectasias like keratoconus. CXL involves saturating the cornea in riboflavin and then irradiating it with UV light, which causes a photochemical reaction that strengthens the cornea and arrests these diseases (and sterilizes the cornea to boot, so much that it can be used to treat infectious keratitis).
However, back then, mercury vapor UV lamps were big, expensive, and generated a lot of heat. Farhad’s MDPhD student at the time, Olivier Richoz, came to him with the latest generation of 9 mW LEDs, saying that, “Look, these are so small, they fit on the tip of a Goldmann tonometer head — here’s one I glued on earlier.” My husband’s thought was: If you can do that, then they can be used at the slit lamp! The next day, Olivier came back with a lot of wiring and batteries, and they irradiated the first corneas in a Petri dish just to show that these small LEDs were powerful enough to do the job just as well as the old — and hideously expensive — mercury vapor UV lamps.
Taking CXL out of the operating theatre and into the office had the potential to be huge: Slit lamps are everywhere — even in the most rural of locations in the poorest of countries — so, if there is someone examining eyes somewhere, it’s going to be with a slit lamp. Taking a

procedure out of the operating theatre reduces costs, and a small, portable CXL that can be used anywhere there’s a slit lamp opens up the whole world to CXL, not just major population centers with operating theatres. And that was the birth of the C-Eye device, and shortly thereafter, EMAGine was founded in 2013. We thought we wanted a quick exit strategy: to show proof of concept, then license the technology, or sell the company structure to a larger entity.
However, something we didn’t anticipate happened in July 2014, when the European Commission issued the “borderline classification” recommendation. This change meant that the European Commission was recommending to its member states that riboflavin should no longer be classified as a medical device. This decision was a game-changer in the industry. This new directive meant that EMAGine couldn’t apply for a CE mark for riboflavin. EMAGine’s business plan was not simply a cross-linking device that worked at the slit lamp (C-Eye) but the riboflavin consumable as well. In other words, EMAGine’s business model wouldn’t be interesting if riboflavin was not part of the product portfolio. Although we had a strong patent on crossing-linking at the slit lamp, we needed the approval to sell riboflavin to increase the value of the product portfolio — and ultimately, the company.
We took the risk and decided to continue developing the C-Eye while finding a solution for the riboflavin problem. We called upon our network of contacts, secured funding for the continuation of development, and achieved the goal of developing the C-Eye into a bona fide medical device. CSO Italia was one of the critical partners that allowed us
to achieve this major milestone. CSO Italia has extensive experience with medical UV light source research and development, as well as the capabilities and know-how to manufacture the device, which made them the most logical partner. Together, we debuted the C-Eye at ESCRS in September 2019, and Farhad performed the first CXL at the slit lamp using the C-Eye device in the Summer of 2020.

If I had to summarize, I would use eight building blocks as the foundation to structure a medtech company in ophthalmology.
These building blocks are:
Intellectual property.
The monopoly created by our CXL at the slit lamp patent enabled an immediate market barrier to entry. This barrier enables a window to EMAGine to enter the international market despite its limited resources.

Corporate set-up.
When explaining entrepreneurship, most people ignore these unsexy but critical administrative procedures. Put quite simply, you need knowledgeable and experienced people handling legal documents for the establishment and management of your company. Critical agreements include the shareholders’, manufacturing, distributor, etc.
Research and development, informed by the regulatory environment.
Your market and the legislation that surrounds it, are moving targets. And, the future of your product pipeline depends on this block.
Establishing a manufacturing/supply chain.
The manufacturer and suppliers are central to the success of the product, so you need to make sure you’re confident with their ability to produce and deliver the quality product(s) you need.
Establishing a distribution network/know who your customers are and how to get to them .
Most medical device sales (and service) go through distributors. Especially for lean start-up companies, the key to sales success is to choose the right distributors. Constant attention, communication and trust are imperative when working with them. As a result,
good distributors will be an extension of the quality service and products that you want the end user to have.
National regulations/ national regulatory approval for the final product.

Regulatory affairs, put quite simply, is difficult and requires a lot of time to feel rewarding. It is challenging work and different in every market. Extreme organization, close communication with our manufacturer and patience are essential to be successful. The longawaited reward is the clearance to sell your product line in the nation.
Operations/fulfillment.
Stock sitting in warehouses consumes money, as well as creates a risk with pending expiration dates. So, you need to optimize not only your manufacturing process, but also market research and sales forecasting in order to minimize your exposure to these costs. This continual process requires constant attention to the market, sales and understanding of future events.
Sales and marketing
This building block might be selfevident, but if your customer base isn’t aware of your product, or why they should consider buying it, then you’re going to struggle. Marketing drives sales, and in addition to traditional marketing efforts, work with your distributor to get the message out there: they know your customers better than anyone, so equip them with the best !
We created these blocks in an incredibly lean manner that we later used to build the foundation of EMAGine. We achieved all of what we have now by knowing who our audience was at each stage of the game … investors, consultants, manufacturers, distributors, regulatory bodies, or most importantly, the doctors and patients who will use and be treated by C-Eye. We worked with each and every one of them; we shared our story and goals; and we remained flexible and open to constructive feedback to help shape EMAGine through the years.
Most of the battle is as simple as this: you need (1) to be prepared for surprises, (2) to know the market, (3) to identify what makes your company the envy of your competitors, (4) to know when you need professional help, and (5) to be extremely organized. No one can know everything, so building a good team and knowing when to ask for help, can ultimately decide the fate of your company.
I had to rely on the experiences and education that I had in my previous jobs to be able to fulfill all of these roles because frankly, we bootstrapped the company with our own money for most of our journey. This brings us to the present day, where C-Eye is now a commercialized product in 60 countries.
07-C-Eye-at-the-Slit-Lamp
Nikki Hafezi is partner of GroupAdvance (Management) Consulting GmbH, Zug, Switzerland; managing director and board member of EMAGine AG, Zug, Switzerland; head of Strategy, Business Development and Licensing, The ELZA Institute, Zurich, Switzerland; and co-founder and managing partner of the Light for Sight Foundation, Zurich, Switzerland.
nhafezi@groupadvance.com
Overall, women are 12% more likely to have vision loss than men, reported the panel led by Dr. Lucia Silva (Guatemala), Dr. Angela Fernandez (Colombia), Dr. Keith Carter (USA) and Prof. Dr. Ciku Mathenge (Rwanda). There is no simple, single reason for this, rather it stems from multiple different causes.
Firstly, women more often suffer from the diseases that cause blindness than men. Sometimes this is due to cultural gender roles, such as childcare, which results in women being more likely to contract disease from children. Poor eye health can also be due to biological and hormonal factors, sometimes linked to pregnancy or menopause. A further factor is that life
expectancy, all over the world, is higher for women than for men and diseases such as cataract, glaucoma and presbyopia all increase in likelihood as people age.

Potentially the largest issue is getting women access to available services. Women are less likely to be prioritized by the community, resulting in a fear of the unknown and a feeling they are not worthy of treatment. Older women especially are the most likely to suffer from blindness but are also often the least prioritized members of the community, meaning they are forced to suffer poor visual health when treatment is available and close at hand. In many countries women have only limited influence over decision making, both at a community and national level, meaning their needs are not prioritized. Women are less likely to be able to travel independently than men, sometimes because they require an escort to move around outside the home or potentially because they need to organize alternative childcare when they leave.
Women are less likely to be literate and educated enough to understand
by Chris Higginsonwhat is happening and to know that their illness can be treated — the highest levels of blindness are found in the areas with the highest levels of illiteracy. Finally, there is the issue of financial independence — women are less likely to have access to their own finances and are less likely to have their health prioritized if a family or community is poor.
The “Second Generation Gender Bias” is at the root of a lot of current disparities, emphasized Dr. Rosa Balcells (Chile) during the second part of the panel discussion on gender inequalities in the workplace. This bias applies to practices that appear neutral initially, but discriminate against a particular gender because they reflect the values of the gender that created the setting. This is in contrast to first generation bias, which is deliberate and intentional exclusion.
A study* published in the United Kingdom, interviewed a variety of medical students in order to find out what their perceptions of
femininity were in the workplace. It found three areas that need to be addressed. Firstly, there is a cultural bias that sees femininity as a form of weakness and automatically questions a woman’s competence and commitment following motherhood, as well as women’s physical strength and intelligence. Secondly, there is the organizational culture that assumes all doctors are men and all nurses are female, restricting career opportunities for women. These factors result in women having less access to leadership positions, fewer podium opportunities, a lack of work recognition and a pay gap between their male colleagues.
Dr. Nancy Al Raqqad (Jordan) spoke about how women are forced to perform to exactly the same standards and capabilities as men, even when those exact standards are not necessary for the job but are in place simply because of the numerical superiority of men. Although there is already a bias within the workplace, Dr. Al Raqqad believes the COVID era will make things worse — when schools close and there is a lack of childcare and social support, pressure will start to rise and women will be expected to withdraw from work and return to the home.
Dr. Al Raqqad believes the problem stems from two different places.
Some issues arise from women –she believes women suffer from imposters’ syndrome, that there is a lack of mentoring and support and, most importantly, women accept the way things are. Also, there are men, work and community related issues — there are current preconceptions and the issue that many women accept them; men’s fear that if more women compete then they may outperform them; and a culture of bullying and intimidation to keep women in the household and out the workplace.
Dr. Julia Haller (USA) presented on the discussion of how things are at the moment for women in medicine. Women have improved in their salary negotiation, which previously has been seen as part of the reason for the pay gap, but the women who are getting better salaries are now being labeled as bullies or pushy. Sadly, a huge number of female doctors are suffering from sexual harassment in the workplace with up to 75% saying they have been sexually harassed at work, something that needs to change.
Women also tend to gravitate towards
academia. However, the vast majority of women faculty are either at the instructor or assistant professor level, with only 25% of full professors being women. In terms of paper authorship, things are improving, but there is still a marked shortfall in the number of women in the first and last authorship positions, with all journals reporting a lower number of female authors.
To improve the situation, Dr. Haller believes women should work on their knowledge, skills and expectations; improve mentorship and guidance; network; pursue leadership training and carve out leadership roles in whatever area of influence they find themselves in.
The Cybersight webinar series on Women Leaders in Eye Health was held on May 8 and May 22. Reporting for this story took place during the event.
Ophthalmology Innovation Summit (OIS) Israel never disappoints. Held virtually for two years in a row now, this showcases innovation at its most sophisticated level. From ophthalmic tech to medical and surgical innovations, the world needs to know what Israel is doing right in this arena.
This particular exhibition of Israeli innovation began with a case study focused on artificial intelligence (AI) and remote diagnostics, led by Notal Vision CEO, Kester Nahen, PhD.

Notal Vision, Inc. (Tel Aviv, Israel) makes several products at the forefront of diagnostic medicine. The Notal
Home OCT is a remote diagnostic monitoring device for patients with sight-threatening intra- and subretinal fluid. It is designed to allow constant monitoring of sight based on daily patient self-imaging done at home, rather than making a patient wait for imaging until they see a physician.
Currently, patients may suffer from an acute onset of a disease between physician visits, but with the Home OCT device, patients are able to test themselves daily in their own homes. It is an easy to use, patient-oriented device that takes less than one minute to use per eye.
Once it has scanned the retina it uploads the image to the cloud, where it is analyzed by AI and any changes
that meet a physician-selected threshold are reported to the prescriber. Daily examinations mean fluid is tracked over time to enable individualized remote patient monitoring and alerts. Physicians have 24/7 access to the data and receive a monthly interactive surveillance report to manage the patient.
The Home OCT has had excellent results in clinical trials and Notal Vision is aiming to get FDA clearance in Q2 of 2022.
Co-Founder & CEO of AEYE Health, Zack Dvey-Aharon, PhD, gave a presentation about how AEYE Health is combining

top quality AI with new innovations in retinal screening — effectively making diagnostic screening available everywhere.

AEYE Health (New York, USA) has produced the Aurora AEYE, a handheld camera with an integrated diagnostic AI. This is the first ever handheld diagnostic bundle that makes screening for more-than-mild diabetic retinopathy quicker, easier and more accessible. A primary-care physician, endocrinologist or pharmacist takes an image of the patient’s retina using the handheld scanner, the on-board AI scans the image, and then only those with suspicious findings are referred to an ophthalmologist. In a study released in May 2021, when screening for diabatic retinopathy with the Aurora AEYE, physicians are able to achieve 92.7% sensitivity and 95.3% specificity –incredibly high numbers, especially for a handheld device.
AEYE Health also has the Broad Screening Service, the broadest screening solution on market by far. It can scan a single image per eye for 12 different indicators: diabetic retinopathy, occlusions, glaucoma, DME, hypertensive retinopathy, papilledema, AMD, hypertension, cardiovascular risk, cancer indicators and dementia (alpha). Being able to look for all 12 indicators from a single image makes the Broad Screening Service the most comprehensive screening solution on the market.
Ron Schneider, MD, CEO and cofounder of Beyeonics (Haifa, Israel) gave an overview of the Beyeonics One visualization system, a digital augmented reality exoscope for ophthalmic surgery. The company began by developing headmounted displays for aviation, and then adapted and integrated that technology into the medical field.
Beyeonics One is a full visualization system for anterior and posterior segment surgery. It is composed of a high-resolution stereoscopic camera head displayed with a resolution more than eight times better than 4k and
zero latency (<20 msec), which can be transmitted to up to three headwearable devices as well as a 3D TV and touch screen for other staff. Because the image is displayed on a headset rather than making the surgeon bend down to see into a microscope, the surgeon is able to sit comfortably and normally in surgery whilst looking into a 3D immersive display, with virtual screens and can control all system functions using intuitive head gestures, diagnostics and real-time data overlaid seamlessly on the visual field.
Nahum Ferera, CEO and co-founder of EyeYon Medical (Ness Siona, Israel) discussed the EndoArt. There are approximately 12.7 million people with corneal edema waiting to receive corneal transplant, but the reality is that there are not enough donor corneas and the surgery is complex and expensive. This means that only 200,000 operations are performed every year, fewer than 1 in 60 of what is required.
Therefore, EyeYon has developed the EndoArt – a synthetic implant that treats the root cause of the corneal edema, leaving the cornea intact. Instead of removing the old cornea and replacing the donor tissue, a polymer film is attached to the posterior corneal surface, thereby resolving the source of the problem. It is minimally invasive procedure that can be performed by any anterior segment physician
They have so far operated on 22 patients, all of whom have shown a reduction in corneal thickness, a decrease in pain and improvement in eyesight.
Miki Olshansky, co-Founder and CEO of Elgan Pharma (Nazareth, Israel) spoke about how her company focuses on rare conditions in neonates such as retinopathy of prematurity (ROP), which effects 70-90% of very young premature babies, and for which there is no approved treatment for preventing or curing. The solution is ELGN-EYE, an infant targeted, local nano-emulsion
therapy in the form of eye-drops with a high penetration profile, that promotes normal retinal blood vessel development and reduces oxidative stress, toxicity and inflammation. It has completed phase 1 trials and phase 2 is ongoing and Elgan Pharma believes there is a market of up to 53,000 patients a year.
Elad Kedar, CEO of Orasis Pharmaceuticals (Herzliya, Israel) spoke about how his company is developing eye drops to treat the 1.8 billion people worldwide who suffer from presbyopia and currently wear glasses. Using eye drops to effect pupil modulation without affecting distance vision or night vision is extremely difficult. However, by using a low concentration of pilocarpine with a proprietary multi-faceted vehicle, Orasis Pharmaceuticals was able to strike the perfect balance.
In phase 2b studies they were able to achieve excellent improvements, with 47% of subjects achieving a ≥3-line improvement versus baseline, only mild and temporary adverse events and, importantly, no negative impact on distance and night vision.
Yariv Baron, co-founder and CEO of Blink Energy (California, USA) spoke about how his company is developing a new way of charging the latest generation of ocular and intraocular devices such as Google’s Physio sensors and Sensimed’s Smart contact lens, which currently need to be charged externally, often with bulky systems.
The BlinkIt is a “smart eyelid patch” that charges the lens and communicates with the outside world. Every time the patient blinks it charges their smart contact lenses with an ultra-thin, ergonomically designed patch that slides within the epicanthal fold. Not only does it charge the smart contact lens with every blink, but it can also communicate with the lens and then pass on information to and from the outside world.
Almog Aley-Raz, CEO and VP R&D of Corneat Vision (Raanana, Israel) spoke about the CorNeat KPro, which is a reliable synthetic substitute for the human cornea that can restore sight to corneal blind patients with a simple operation and follow up. Rather than trying to integrate with the native cornea, the CorNeat KPro is connected via a nanofiber skirt placed under the conjunctiva. This area is rich with blood vessels and heals easily and, once implanted, the lens gives vision with a wide field of view that is equivalent, or even better than the original quality of sight.
Nir Israeli, CEO and co-founder of Sanoculis (Kiryat Ono, Israel) talked about its MIMS procedure, a stent-less, simple and fast way to perform glaucoma surgery. Using a single-use sterile tool and a multi-use external machine, a tiny sclerocorneal drainage channel is drilled and removed from the eye. This reduces intraocular pressure as the intraocular surplus fluid is allowed to drain from the anterior chamber into the subconjunctival space. The procedure is minimally invasive, takes only around two minutes and is simpler and faster than existing methods. It has efficacy similar to trabeculectomy with fewer side effects — and 97% of patients did not require anti-glaucoma medication afterwards.
Moshe Weinstein, CEO of Everads Therapy (Tel Aviv, Israel) spoke about the Everads suprachoroidal tissue separator, which opens a channel to the choroid, allowing the surgeon to inject into the suprachoroidal space. This method has a proven ability to quickly reach the back of the eye and macula and can deliver large volumes (up to 200 μl) of viscous material and large particles.
This technique has several advantages, but the most important are that it allows the targeting of the choroid and retinal tissues with posterior and circumferential spread, it is an effective way of reaching the posterior pole and macula, and it does not interfere with the visual axis.
Ariel Weinstein, CEO of Ophthalmic Sciences (Tel Aviv, Israel) spoke about their intraocular pressure monitor. IOP fluctuates throughout the day, but by using their new headset patients can easily check their IOP at home with just a two minute test. The test does not require physical contact with the eye and is unaffected by corneal thickness. The results are uploaded to the cloud where they can be accessed by the patient’s physician. It allows detection of cataract and corneal edema, central/ branch vascular occlusions, ocular motor disorder and early exophthalmia.
Aryeh Batt, CEO of Precise Bio (North Carolina, USA) spoke about how they are 3D printing, cell by cell, tissues and organs for transplant. By printing on a cellular scale, they can mimic natural tissue, copying the exact anatomical structure. Because the structure of the cornea is so well understood and is relatively simple, it is fairly easy to 3D print.
Precise Bio has had great success at the pre-clinical study stage and anticipates reaching the clinic in 2022.

Ran Yam, CEO and co-founder of NovaSight (Washington, USA)
spoke about CureSight, their treatment for amblyopia, which affects 200 million children. The standard treatment, an eye patch, has only 40% compliance. Instead of an eye patch, the patient watches any streamed content on the CureSight device, which tracks eye movement as they watch. The device then blurs the center of vision of the strong eye, forcing the brain to use the weak eye more and encourages the improvement of binocular vision and 3D perception.
Daria Lemann Blumenthal, CEO of BELKIN Laser (Yavne, Israel) spoke about their new treatment for glaucoma. It’s an automated treatment that can be completed in seconds, simply and easily. Glaucoma affects over 100 million people worldwide, but the number of ophthalmologists who can help them is nowhere near high enough, especially in Asia. The current treatment, eye drops, has low adherence.
Belkin’s Direct SLT is an entirely automated procedure that locates the exact treatment area and directs laser beams precisely to that area through the limbus. Clinical trials showed a 22% reduction of IOP at 6 months and the amount of medication was reduced from 1.6 to 0.4 at 6 months. It is even effective on both open-angle and angle closure glaucoma.
After the company showcase, a panel of four leaders in the field gathered to discuss what companies can expect from investors and strategic partners, as well as the state of innovation in Israel. The panelists were Begoña Carreño, PhD, Global BD&L head of ophthalmology from Novartis; Colin Francou, managing director from Théa Open Innovation; Yaacov Michlin, CEO from Biolight Life Sciences; Prabhu Velusami, MD, New Venture & Transactions Lead for Vision Ophthalmology at Johnson & Johnson Innovation Center.
Prabhu Velusami and Begoña Carreño began by discussing if it was ever too early to approach investors and strategic partners and suggested that as long as a company has a coherent way of treating an unmet clinical need, it was never too early. Approaching strategic partners early on can be great for new start-ups, large companies with a lot of experience can be fantastic assets because they can advise, give feedback and offer course correction to companies that are still establishing themselves, potentially saving them from going down the wrong path early on.
Begoña Carreño spoke about working in Israel, where there is a huge amount of ophthalmological innovation, especially for such a small country. In her view, Israel is impressive because, rather than relying on consultants, Israeli start-ups display a high level of interdisciplinary collaboration, with engineers, clinicians and pre-clinical scientists all working together in a seamless team. Colin Francou was particularly impressed by the high levels of inter-connectivity between companies, even in very different parts of the ophthalmic field, which allows people to share ideas and a high level of cross-fertilization between diverse companies.
Prabhu Velusami said that, in his experience, Israeli innovators are exceptionally entrepreneurial — they ask how interesting science can be commercialized and made compelling
from the very early stages. In addition, the funding environment in Israel is very conducive to innovation, including a government that is very supportive, and with excellent leverage mechanisms for early stage funding and startups. Yaacov Michlin spoke about the government support of Israeli startups, where $200 million dollars are invested yearly into the biomedical field, with grants available all throughout a company’s growth cycle. In addition, the government encourages large multi-national companies like Johnson & Johnson to invest in Israel in order to increase innovation and keep growing companies in the country one they are established.
The panel moved on to what they felt were the biggest unmet needs in ophthalmology at the moment and where their companies are looking to invest in the next few years. Prabhu Velusami spoke about how Johnson & Johnson believes there is still a great unmet need in the pharmacological sphere for treatments for retinal diseases such as wet and dry AMD and diabetic retinopathy; they are also looking into neuro-protection for glaucoma and ways for make gene therapy more effective and less immunogenetic.
Regarding contact lenses, J&J are looking for improvements in comfort, new optical designs and designs that address presbyopia. However, looking to the future he believes the biggest unmet need will be myopia, which requires a toolkit of approaches from drops to spectacles and will come to dominate ophthalmological treatment innovation in the next few years.
Begoña Carreño agreed with, and reiterated, many of Prabhu Velusami’s points, adding that she believes the world is heading for an epidemic of myopia, especially high myopia — which is going to be the greatest issue in ophthalmology in around five years’ time. She also wanted to emphasize that anyone who believes they have found a solution to an unmet clinical need should approach Novartis, as they are always
looking for start-ups with the ability to treat problems that are currently untreatable.
Yaacov Michlin is excited about the potential of AI to diagnose diseases like diabetic retinopathy. If patients can be allowed to take a new generation of sophisticated tools home with them in order to do daily monitoring, we can diagnose and monitor diseases in their early stages. This combination of at home-testing and AI has the ability to deal with many of the diseases which cause vision loss, and the technology should be with us in the next two or three years.
The panel then moved onto the effect of the COVID-19 pandemic on the industry. Colin Francou said that, with the exception of a few clinical trials, it did not affect his company’s running very much. However, they will be looking more to their digital strategy, which they shall now look to invest in more. Prabhu Velusami agreed, saying he believes there will be a permanent change in attitudes due to COVID-19 and that J&J will be prioritizing innovative technologies that avoid patients having to meet physicians face to face, such as remote monitoring, diagnosis, treatment and telerefraction.
The 2021 OIS Israel Innovation Showcase was held on June 10. Reporting for this story took place during the event. A version of this article was first published in piemagazine.org on June 15, 2021.
If you have no idea what that headline is all about … then where were you? June 18 and 19 happened, the world’s funky ophthalmology expo went LIVE and in case you missed it (we hope you didn’t…) start by reading the summarized highlights of the show dailies, CAKE & PIE POST…
The CAKE & PIE Revolution has Begun and it’s Bananas!
Do not adjust your television set, computer monitor or smartphone … normal programming will not resume — and welcome to the colorful world of Media MICE. The revolution has begun, comrades: banana costumes will

become mandatory ophthalmic daily wear and everyone has to try Media MICE CEO Matt Young’s cooking (at least once). The CAKE & PIE Expo (C&PE) 2021 has arrived, and the ophthalmic conference arena will never be the same again.
So, glory to the revolution and welcome one and all to the Expo’s first day, featuring the absolute best and brightest
by Andrew Sweeneyin our awesome industry. The entire Media MICE team has labored in the foundries and factories to mine for nuggets of creative genius (or insanity, it’s all a matter of perspective) for you all to enjoy. You will find all your usual favorites, including the auditorium’s superlative symposiums (on two tracks) and positively perfect exhibitor booths — with a dash of our very own quirky take on things.
Log-in to the virtual lobby to take stock of the menagerie of the medically mesmerizing exhibits, starting with

a cheeky little offering you’ll find at the bottom right of your screen called Humorous Scientific Posters. [Editor’s Note: You may or may not take these posters seriously, they’re of the humorous kind after all.] Featuring some of the (ahem) leading and totally backed up by, well, research, this isn’t something you’ll want to miss. It even features a reference to my favorite medical malady, syphilis [Editor’s note: Oh god, no not again…]
But that’s not all! No, no, no. We have far more, including previous copies of CAKE, PIE and COOKIE magazines for you to peruse and download; our awesome Show Dallies – CAKE & PIE POST – made possible by our friends at OCULUS, Allergan, Quantel Medical; Media MICE TV; and much, much more. Make sure you check all of these cool functions out, and swing by our social media pages (i.e. LinkedIn and Facebook) to really spread the love. We’re all very sensitive people, after all.
Of course, the main events of the show on Day One, the brightest stars in the sky as it were, were the scientific sessions. With a veritable cosmic
smorgasbord of content on offer, beginning with a discussion on What’s Cooking in Cataract? and ending with tasty retina recipes from the Special Session: Retinawesome. There was also a smattering of COVID-19’s effect on clinics, a pinch of posterior segment insights, and a heavy drizzling of the very best cutting-edge innovation in ophthalmology.
We also want to draw your attention to the debut of the Subthreshold Ophthalmic Laser Society (SOLS) which officially launched at C&PE: Welcome to the madness! They have fully joined the revolution, and we hope you will too.
We’ve Gone Bananas: Russian Irises, Myopia on Motorbikes and Retinal Oopsies

Everybody that felt a little bit bananas at the first ever CAKE & PIE Expo, please say “Aye”. “Aye”. Is it just me? I don’t think so. Well, that’s just the way we like it. And we have to say we’re pretty happy with how the first-ever CAKE &PIE Expo
turned out. We got to bring together some of our favorite ophthalmologists from around the world, and also make some new friends from emerging societies and new markets.
From starting the day with cool cataracts, to ending the day with a marvelous masterclass in managing myopia, Day 2 of the Expo had it all. We set up a video vault to keep you completely engrossed with reams of content about all aspects of ophthalmology, perfect for those locked down or looking for some light viewing before bed. The exhibition hall was bursting with virtual booths, and we hope you dropped by to say hello to the Media MICE team. (We locked a couple team members in there and frankly, we forgot the login information to get them back out, so they’re probably getting lonely and hungry at this point.)
As you’ve probably noticed by now though, Media MICE likes to get noticed and our outlandish costumes and quirky character is definitely a marketing strategy and a pretty cool one at that. Marketing yourself and your company in ophthalmology is crucial to getting ahead, which was what our very own CEO Matt Young talked about when he hosted the Expo’s Marketing Session: Get Noticed Now, covering all aspects of marketing that people working in our field should know about. The featured guests include Nikki Hafezi, managing director and board member of EMAGine AG (Zug, Switzerland); head of Strategy, Business Development and Licensing at The ELZA Institute (Zurich, Switzerland); and co-founder and managing partner of the Light for Sight Foundation (Zurich, Switzerland), as well as optometrist, social media influencer and brand ambassador Dr. Kristie Nguyen. For now you can watch the recording of this lively session at Media MICE’s YouTube Channel
Now the Media MICE team has a lot of hidden talents, even if they cannot successfully extricate themselves from a virtual booth. Your current writer sadly doesn’t have any superhuman abilities (besides his ability to tell any single malt whiskey apart by smell alone), but he can speak Russian. Therefore he
was very excited to attend the Russian Ophthalmology Society (ROS) Presents Reconstructive Surgery and More! while perusing through the day’s events. Russia’s ophthalmology expertise is extraordinary, and it was awesome to welcome the ROS to attend our Expo, so we hope you were able to drop by their booth in the exhibition hall!

A particular highlight of this symposium was the first presentation by Dr. Marina Shanturova of the S. Fyodorov Eye Microsurgery Federal State Institute (Irkutsk, Russia). She focused on the perils of damage to the iris, including diaphragmatic dysfunction, double vision and reduced visual acuity, and provided some fascinating insight into the history of Russian contributions to iridoplasty development. She recommended localizing iris defects, identifying the presence of synechiae, and monitoring changes in the actual structure of the iris.
One of the last events of the day was ORBIS Singapore Session: The Myopia Epidemic in Asia Pacific, and you’ll know from our recent content just how much of an issue short-sightedness is in the region. It’s an emerging epidemic of staggering proportions, and it was

awesome to see some of the brightest minds in myopia management coming together to share their experiences and ideas about what can be done to tackle this disease. It was also pretty cool to see our CEO Matt Young change in a phone booth from his banana suit in the marketing session to his “candyland ‘’ suit in an Orbis-supported session. As for which is the superocular costume – well, we’re still scratching our heads at that – and that a phone booth even exists in 2021.
Dr. Nathan Congdon, a professor at the Queen’s University Belfast in Northern Ireland, spoke about how glasses are a first line of defence against myopia, and that providing free glasses can help to slow visual decline if administered early. He described how India has a national policy of free vision screening in children, which highlights the country’s correct strategy of focusing on prevention. He also pointed to a study called STABLE in which young myopia motorbike drivers are provided with free glasses to reduce road injuries and deaths in Vietnam, and if successful, will lead to tougher vision requirements for licensure.
A special shoutout to our friends at the Vitreo Retina Society of India (VRSI) who held their own in a session titled, When Retinal Disasters Happen, and More, which covered some fascinating aspects of retinal treatment. We already wrote a specific review about this event (which you can find on page 8), so make sure you give it a read and watch the session.
The same goes for all the participants of both sessions entitled Get Smart: On Education & Attitudes in Ophthalmology, which offered some fascinating perspectives on ophthalmic treatment. We learned that chocolate could have a role in glaucoma treatment, and consumed some brutal yet highly informative reports on ocular trauma in South Africa. These sessions are not to be missed, you can find them on Track 1 of Saturday’s streams.
Thank you for your participation!
So kudos to all for attending what we’re hoping will become the global premiere event in ophthalmological awesomeness, where everyone can come together to trade the latest news about everything, from cataracts to macular edema, and where everyone will be compelled to wear a banana suit costume. Remember, the revolution will be available on our social media channels, so make sure you keep following our Facebook and LinkedIn accounts for the latest news on all things eyeballs. In the meantime, it’s been marvelous friends, and thank you for coming.
Over 8 million people have vision loss due to neovascular age-related macular degeneration (nAMD)1. Regular, long-term anti-vascular endothelial growth factor (VEGF) treatment can stabilise disease, leading to visual gains that can be maintained with continuing treatment. However, up to 50% of patients with nAMD stop anti-VEGF treatment by 24 months, and up to 42% of patients do so due to the perception that treatment is not helpful or not required2


The nAMD Barometer Leadership Coalition is an international group of experts in the field of retinal disease, vision care and ageing, convened to develop evidence-based solutions for optimal management of nAMD, with the aim of improving patient adherence and persistence to anti-VEGF treatment.
Develop interventions to shape clinical practice and treatment regimens, and drive behaviour change that supports a patient’s need to remain adherent and persistent
Advocate to peers and relevant stakeholders the benefits of clinic optimisation and modification of treatment regimens, and the importance of timely and relevant patient education
Encourage the community to assess practice outcomes and the benefits of implementing recommended interventions in clinical practice

The Leadership Coalition is conducting a series of evidence-generation initiatives to help understand why non-adherence and non-persistence to anti-VEGF therapy occurs, which will help design interventions to support changes in behaviour and optimise treatment:
• Systematic literature review to identify risk factors associated with non-adherence and non-persistence –now published in Ophthalmology2
• Standardisation of definitions of ‘non-adherence’ and ‘non-persistence’ to enable consistency and alignment in future data collection – now published in JAMA Ophthalmology3
• In-depth semi-structured interviews with patients to identify modifiable and non-modifiable risk factors to increased patient (non-) adherence and persistence
• Multi-country, comprehensive, market research survey of patients, healthcare professionals and allied health staff to quantify trends and perspectives, cultural differences, and healthcare systems
The efforts of the nAMD Barometer community aim to uncover meaningful and practical interventions to inform future practice and policy, with the collective goal of improving the lives and livelihoods of the patients we
References:
1. Adelson J, et al. Lancet Glob Health. 2021;9:e144–e160. Accessed via the IAPB Vision Atlas (https://www.iapb.org/learn/vision-atlas);
2. Okada M, et al. Ophthalmology. 2021;128:234–247;
3. Okada M, et al. JAMA Ophthalmol. 2021 online.
