







































t’s evident that we’re all living through a time that will be noted by history: Beyond the current political and humanitarian events, the impacts of the COVID-19 pandemic will certainly be recorded for posterity (for better or worse). Will we know more about our mistakes once this is largely behind us? Or has our ability to communicate via social media created platforms for misinformation that are too numerous to combat?
Thankfully, when we take a look back at the history of posterior segment surgery, we don’t have to battle this type of misinformation. Rather, we find studies, data and expert insight on how the practice has evolved — from ancient times to now. From Hippocrates’ first theories on the retina … to today, where we have innovative imaging and instrumentation to operate on it, we’ve certainly come a long way. In this issue’s cover story (page 16), this topic is covered in depth to showcase how surgical techniques and instruments have grown to allow surgeons to operate in the safest (and most effective) manner possible.
And although it’s interesting to review the roots of retina from a historical perspective, the more recent “history” of ophthalmology is perhaps even more crucial to saving sight. After all, it wasn’t that long ago that anti-VEGF became a firstline treatment for progressive diseases like age-related macular degeneration and diabetic retinopathy. Today, these intravitreal agents are used worldwide and have been proven to slow the progression of these sight-threatening conditions. Further, new molecules are being developed to fill the gap in current treatments: To decrease treatment burden, to develop more efficient regimens, and to increase durability are among some of the top targets. (For more on this, check out the story on page 10.)
These therapies have been revolutionary, indeed. But we’d also be remiss if we didn’t include imaging. Without the ability to view the posterior segment, we would lose the critical ability to diagnose and manage posterior segment disease — not to mention operate. These days, we can not only view the posterior segment, we can see all the way to the periphery with widefield imaging, which can be vital to catching retinal pathologies (see page 14).
As treatments and imaging systems have evolved, so have the surgical techniques that accompany them. Smaller instruments make smaller incisions — leading to less inflammation and better outcomes. Devices, like vitrectomy systems, have also improved to make this relatively common surgery safer than ever before. In ophthalmology, we are indeed fortunate to have such a wide network of surgeons, experts and industry partners to continue to propel the practice forward and to serve the ultimate goal: To prevent blindness and save sight.
Ophthalmology is experiencing a growth spurt, indeed. At PIE, we’re proud to be a small part of that: To stand out, report the latest news and help share the important updates in the field. We hope you enjoy “The History Issue” of PIE magazine.
Editor PIE, CAKE & COOKIE magazines
Arunodaya Charitable Trust (ACT)
Prof. Gemmy Cheung, MBBS, FRCOphth (UK), FAMS, MCI, is currently a professor at Duke-NUS Medical School, National University of Singapore, and head of the Medical Retina Department at Singapore National Eye Center (SNEC). Her research focuses on retinal diseases, including age-related macular degeneration (AMD), polypoidal choroidal vasculopathy (PCV) and myopic macular degeneration, as well as risk factors for these conditions that may be unique to Asian populations. Prof. Cheung has more than 200 peer-reviewed publications and serves on the editorial boards of several journals, including the American Journal of Ophthalmology, Retina and Eye.

gemmy.cheung.c.m@singhealth.com.sg
Asean Ophthalmology Society
Asia-Pacific Academy of Ophthalmology
Asia-Pacific Vitreo-retina Society
Prof. Mark Gillies, MBBS, PhD, FRANZCO, presently holds a number of positions including: director of research and director of the Macula Research Group for the Save Sight Institute; foundation fellow for the Sydney Medical School; professor in the Department of Clinical Ophthalmology at the University of Sydney; head of the Medical Retina Unit at the Sydney Eye Hospital; deputy chair for the Ophthalmic Research Institute of Australia; and director of Eye Associates in Sydney. Prof. Gillies has served as a principal investigator or associate investigator in more than 70 clinical trials, and his research regarding macular degeneration and drug safety and efficacy has been published in 188 journals. He has also received a number of grants to study treatments for age-related macular degeneration, retinal disease and Muller cell dysfunction — among other treatments and studies. Prof. Gillies is a dedicated and multi-awarded researcher.

mark.gillies@sydney.edu.au
Prof. Dr. Vishali Gupta, MD, is an accomplished vitreo-retina and uvea expert of international repute. She currently works as a professor of ophthalmology at Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. Throughout her career, she has completed original work in the fields of intraocular tuberculosis, optical coherence tomography, diabetic retinopathy and fungal endophthalmitis. In addition, she is actively studying vitreoretinal and uveitis diseases. Prof. Gupta also holds a U.S. patent for the development of multiplex PCR for uveitis. In addition, she is a sought-after speaker and has delivered more than 870 invited lectures and conducted sev eral instruction courses at various international and national meetings. She has more than 200 publications in peer-reviewed journals; has edited five books and contributed 72 book chapters in textbooks. She is the secretary of the International Uveitis Study Group, and member of the AAO, Club Jules Gonin and the Macula Society. She is currently the president of the Uveitis Society of India. Prof. Gupta has received several awards for her work, including the first JN Pahwa award from the Vitreo-Retinal Society of India (VRSI), the first NA Rao Award from the Uveitis Society of India, and the first NA Rao award from All India Ophthalmological Society (AIOS).

vishalisara@yahoo.co.in
Ophthalmology Innovation Summit
Orbis International


Retinawesome Retina & Vitreous International

Russian Ophthalmology Society (ROS)



Vitreo-Retinal SocietyIndia

Young Ophthalmologists Society of India ( YOSI )




+ Ultra-Widefield of view up to 200˚

+ Rich in details from center to periphery + Imaging through media opacities
iCare’s unique combination of sharpness and TrueColor offers now even wider view on the retina from 120° with a single shot, up to 200° with Mosaic functionality, helping to detect subtle signs of pathologies further in the periphery.*

Discover the new Ultra-Widefield view of
Insert
bevacizumab, ranibizumab, aflibercept and brolucizumab.
Pegaptanib sodium was the first intravitreal anti-VEGF treatment developed for nAMD. It is a pegylated oligoribonucleotide (aptamer) that binds with high specificity and affinity to VEGF 165, sequestering and therefore preventing VEGF 165 from activating its receptor. It is no longer recommended for treating exudative AMD as it is less effective compared to other anti-VEGF drugs.

Ranibizumab is a fully humanized monoclonal antibody fragment that binds to multiple isoforms of VEGF-A. It was originally approved for treating nAMD. The efficacy and safety of fixed regimens of ranibizumab have been evaluated in various trials, including ANCHOR, MARINA, PIER and EXCITE.
Aflibercept is a fusion protein (115 kDa) comprising the second Ig domain of human VEGFR1, the third Ig domain of human VEGFR2, and the Fc region of a human IgG1.
Brolucizumab is a low molecular weight, single-chain antibody fragment that targets all forms of VEGF-A with high affinity. Initially developed for the treatment of nAMD, it is currently in pivotal studies for diabetic macular edema and macular edema, secondary to retinal vein occlusion.
Age-related macular degeneration (AMD) remains one of the most prevalent eye problems among the elderly worldwide. With an overall prevalence of 8.7%, it is projected to affect 288 million by 2040.1

To medical retina specialist Dr. Kelvin Teo Yi Chong from the Singapore National Eye Centre, treating neovascular AMD (nAMD) is commonplace. “I see about two to three new cases per week in my practice. In Singapore, the incidence of late AMD is about 0.5%,” he said.
Neovascular AMD is a type of late
AMD characterized by choroidal neovascularization with intraretinal or subretinal leakage, hemorrhage and retinal pigment epithelial (RPE) detachment. Despite therapeutic advances in the management of nAMD, none of the currently used treatments cures the disease or reverses its course.2
Nevertheless, the introduction of vascular endothelial growth factor inhibitors — known as anti-VEGF — have brought forth significant advancement in nAMD treatment. This has altered the prognosis from blindness to a significant chance (about 30%)3 of visual acuity improvement, at least during the first two years of treatment.4-6
Some of the more common antiVEGF agents include pegaptanib,
Bevacizumab, a humanized monoclonal antibody that inhibits VEGF-A, was originally developed as a medication for use in combination with existing metastatic colorectal cancer chemotherapy regimens. Intravitreal injections of bevacizumab are used widely as an off-label treatment for nAMD. According to the currently available evidence, bevacizumab may be considered as a reasonable and affordable alternative to ranibizumab in patients with nAMD.
Although anti-VEGF therapy has become the standard treatment for nAMD, many patients do not respond adequately to it, or experience a slow loss of efficacy after repeated administration over
time. Resistance can occur at any time during the course of therapy. Besides this, patients also require repeated and frequent injections, resulting in the inconvenience of numerous hospital visits.
Hence, in real clinical practice, patients usually received fewer anti-VEGF injections and achieved worse visual outcomes than patients in clinical trials who receive frequent therapy according to a fixed regimen.
According to Dr. Teo, the prognosis in patients treated with anti-VEGF is variable. “I suspect, like in most practices, patients generally have a better prognosis if they are willing to adhere to treatments. Many other factors also play a part, such as starting vision and how late is the presentation of the disease. Generally, proper counseling on treatment and management are the key for good outcomes,” he said.
“In Singapore’s public healthcare system, off-label use of bevacizumab is currently the most affordable antiVEGF treatment, with its cost almost fully covered by the national insurance equivalent. This is by far the most commonly used anti-VEGF agent in my practice. On-label ranibizumab and aflibercept are less common due to the cost. Unfortunately, cost does play a huge part in the decision making process for my patients as these treatments are ongoing and may continue for years.
Choice of treatment is often decided after consultation with the patient and his or her family members.”
New strategies have been proposed for treating nAMD, which include a multitargeted approach and molecules such as designed ankyrin repeat protein (or DARPin).
The AVENUE7 and STAIRWAY8 trials found faricimab, the first bispecific antibody targeting both Ang2 and VEGF-A, to be non-inferior to ranibizumab in treating nAMD. Phase 3 studies with faricimab are ongoing.
Meanwhile, OPT-302, a VEGF-C/D trap molecule, has been devised to be used in conjunction with existing standard-of-care anti-VEGF-A therapies. A phase 1/2a study that included 51 nAMD patients showed that OPT-302 was non-inferior as both monotherapy and in combination with ranibizumab.9 Additionally, a phase 2b 24-week study, conducted on 366 nAMD patients showed that combined therapy (OPT-302 + ranibizumab) provided a statistically significant improvement in visual function compared to 0.5mg ranibizumab alone.10
Meanwhile, DARPin molecules (such as abicipar pegol) offer potential therapeutic advantages over antibodies or antibody
1. Wong WL, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health. 2014;2:e106–e116.
2. Ricci F, et al. Neovascular Age-Related Macular Degeneration: Therapeutic Management and NewUpcoming Approaches. Int J Mol Sci. 2020;21(21):8242.
3. Jager RD, Mieler WF, Miller JW. Age-Related Macular Degeneration. N. Engl. J. Med. 2008;358:2606–2617.
4. Rosenfeld PJ, et al. Ranibizumab for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006;355:1419–1431.
5. Brown DM, et al. Ranibizumab versus Verteporfin for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006;355:1432–1444.
6. Kaiser PK., Blodi BA, Shapiro H, Acharya NR. Angiographic and Optical Coherence Tomographic Results of the MARINA Study of Ranibizumab in Neovascular Age-Related Macular Degeneration. Ophthalmology. 2007;114:1868–1875.
7. Patel SS, et al. Anti-VEGF/anti–angiopoietin-2 bispecific antibody faricimab (RG7716) in neovascular AMD. In Proceedings of the Retina Society 43rd Annual Scientific Meeting, San Francisco, CA, USA, 12–15 September 2018.
8. Khanani AM. Simultaneous inhibition of ang-2 and VEGF with faricimab in neovascular AMD: STAIRWAY phase 2 results. In Proceedings of the American Academy of Ophthalmology Retina Subspecialty Day, Chicago, IL, USA, 26–27 October 2018.
9. Dugel PU, et al. Phase 1 Study of OPT-302 Inhibition of Vascular Endothelial Growth Factors C and D for Neovascular Age-Related Macular Degeneration. Ophthalmol. Retin. 2020, 4, 250–263.
10. Opthea. Opthea Meets Primary Endpoint in Phase 2b Study of OPT-302 inWet AMD. Available at: https:// www.opthea.com/wp-content/uploads/2019/08/Opthea-Limited-Opthea-Results-of-Wet-AMD-ClinicalTrial-10001623-070819_V2.pdf
fragments, by providing high affinity, stability and high molar concentration. However, this drug was not approved by the FDA for the treatment of nAMD as the rate of intraocular inflammation observed following administration of 2mg/0.05 mL resulted in an unfavorable benefit-risk ratio.
Although there have been new and promising developments in AMD treatment, the need for long-lasting treatments and robust predictors of optimal retreatment intervals for true personalized treatment regimens remain unmet.

“Current AMD treatments are revolutionary. They work well and have addressed the impact of blindness due to nAMD over the last decade, giving a new lease of life in many patients. Nevertheless, much can be improved in terms of longer durability and efficacy. Hopefully, in the future, there will be durable treatments which are more accessible, with bio markers that can precisely predict response and optimal retreatment needs,” Dr. Teo said.
Assistant Professor Kelvin Teo , MBBS, MMed(Ophth), is a medical retina specialist consultant at the Singapore National Eye Centre (SNEC), one of the largest tertiary eye hospitals in Asia. Concurrently, he is the head of the clinical trials platform in the Singapore Eye Research Institute (SERI), one of the largest eye research institutes in Asia, and the deputy clinical director of the SNEC ocular Reading Centre (SORC). Dr. Teo has published more than 70 scientific publications in high impact ophthalmology journals in clinical research and ocular imaging of AMD. He has received >SGD$1M in grant funding as principal Investigator. His expertise, coupled with his roles in clinical trials platform and reading centre, gives him the unique experience of understanding the entire spectrum of clinical research and real world management of AMD.
kelvin.teo.y.c@singhealth.com.sg
achieves and maintains clinically meaningful long-term vision gains in nAMD patients. But how do these outcomes translate into the real world?

“We’ve all faced the challenge of the efficacy gap. We see these results in pivotal clinical trials and we are disappointed when, in our clinical practice, we can’t achieve those results,” began Dr. Varun Chaudhary, Hamilton Regional Eye Institute, McMaster University, Canada.
“I think that many of us look for pragmatic, easy-to-replicate clinical trials, where we can replicate the treatment protocol in our own practice effectively, reduce the efficacy gap and improve patients’ outcomes,” he said, adding that ALTAIR is one such study.
Today, there are more medical options than ever before to treat conditions like neovascular agerelated macular degeneration (nAMD) and diabetic macular edema (DME). Much of this is thanks to anti-vascular endothelial growth factor (anti-VEGF) agents which have proven efficacious and safe to slow the progression of these vision-threatening conditions.
Although we know these intravitreal agents work, frequent visits are burdensome for patients, their caregivers and physicians — and therefore, a more practical (and proactive) approach is needed to maintain vision and prevent disease progression. Thus, during the Virtual Congress on Controversies in Ophthalmology (COPHy Global 2021), this important topic was covered during an industry-sponsored symposium — and we have all the can’t-miss insights below...
We are now relatively familiar with the Treat & Extend approach for patients with nAMD, began Professor Paolo Lanzetta, University of Udine, Italy. Aflibercept (2 mg) is approved in Europe and elsewhere for use in a Treat & Extend (T&E) regimen with the option to extend treatment intervals starting in the first year of treatment.
“With aflibercept, after the 3 initial monthly doses, the next administration is usually given after 8 weeks. Then, based on the physician’s assessment of functional and morphological outcomes, the treatment interval can be maintained at 8 weeks or it can be extended by 2-4 week increments up to 16 weeks.”

Importantly, this extension can be performed in the first year of treatment and is more than a compromise between PRN and fixed dosing resulting in a minimum number of injections while delivering optimal vision outcomes for the patient, he continued.
Prof. Lanzetta then shared some T&E treatment algorithms. For example, if the patient outcome worsens, the interval should be decreased to the previous stable interval. Following this approach will minimize treatment burden and fluid fluctuation.
“Today, we know that Treat & Extend has many advantages over fixed or PRN approaches,” said Prof. Lanzetta. And there is evidence — both in clinical trials and clinical practice — to attest that this regimen works.
In a clinical trial setting, proactive, individualized T&E with aflibercept
In implementing treatment regimens from clinical trials, Dr. Chaudhary said that he prefers T&E regimens that can be applied in a busy clinic effectively. “Practical T&E studies such as ALTAIR are very important in my clinical practice because they have allowed me to get positive outcomes and reduce the efficacy gap between what the clinical trials demonstrated and what I can achieve in my clinic.”
Fluid was another key topic discussed during the symposium. Importantly, emerging evidence suggests that, depending on its location, fluid can have different impacts on patient vision.
Dr. Chaudhary said that he looks at fluid from a patient perspective: “We need to remember that for patients, there is only one outcome that matters — and that’s visual acuity. So, looking at OCT in its totality — whether it’s wet or dry — may not be the best surrogate outcome measure. What may make more sense is to look at fluid compartments.”
For example, some stable subretinal fluid (SRF), in the absence of intraretinal fluid (and with stable vision), may be tolerated by either maintaining the treatment interval or carefully extending treatment interval.1-3
Dr. Chaudhary continued that this
doesn’t necessarily mean that clinicians should change their practice based on data from studies like VIEW, ARIES, ALTAIR and CATT. While we shouldn’t change clinical practice based on such post hoc analyses alone, there is a RCT examining exactly this question: FLUID.
In fact, FLUID4 found that meaningful vision gains can be achieved when tolerating residual SRF in nAMD patients.
The trial participants were randomized to receive ranibizumab 0.5 mg monthly until either complete resolution of SRF and IRF (intensive arm: SRF intolerant) or resolution of all IRF only (relaxed arm: SRF tolerant except for SRF >200 μm at the foveal center) before extending treatment intervals. According to the authors, “significantly more participants in the intensive group never extended beyond 4-week treatment intervals (13.5%) than in the relaxed group (2.8%; p=0.003). Further, significantly more participants in the relaxed group extended to — and maintained — 12week treatment intervals (29.6%) than the intensive group (15.0%; P = 0.005). In addition, the BCVA outcomes in both groups are the same.”
“All these data suggest that aggressively chasing subretinal fluid in nAMD may not be necessary if the fluid is stable and less than 200 microns,” he explained.
Choosing an anti-VEGF agent is one of the first things clinicians must consider before embarking on a treatment course for DME patients. Thankfully, there is data that can help guide this process: Protocol T* is currently the only head-to-head RCT that compares the efficacy of aflibercept, ranibizumab and bevacizumab in DME. Results from this study were shared by Dr. John Kitchens, Retina Associates of Kentucky, USA.
In case you missed it, Protocol T was a 2-year study (with a one-time followup, 5 years after the study started) involving 660 adults diagnosed with center-involving DME on OCT with vision ranging from 20/32 to 20/320.
“When we look at year 1, what we can
see is that patients in the first 6 months were treated really aggressively,” said Dr. Kitchens. “Over 90% of patients in the Protocol T study received the planned 6 initial injections. That speaks to the fact that we do see continued improvement in patients’ visual acuity beyond injection 3.”
He then shared data from a real-world study by Moorfields Eye Hospital (United Kingdom) which showed that twothirds of patients receiving aflibercept presented with baseline VA <69 letters. Across studies from clinical practice, approximately two-thirds of patients with DME typically present with baseline BCVA <69 letters (worse than 20/40), said Dr. Kitchens.
“In the Moorfields study, we saw unprecedented visual acuity gains of almost 3 lines,” he said, adding that importantly, patients in this study received 5 initial monthly loading doses.
“We can see that there was a difference between these different treatment modalities: Patients treated with aflibercept gained close to 4 lines of VA; patients treated with ranibizumab gained almost 3 lines of VA; and the patients treated with bevacizumab gained just over 2 lines of VA — and this was carried out not just in year 1 but in year 2.”
Dr. Kitchens continued: “There’s a significant area under the curve, where during those 2 years if the lower VA cohort patient is receiving any other agent than aflibercept, they’re leaving vision on the table in many instances. We want the best vision for our patients, not only at the end of the day, but during the entirety of their treatment course.”
Notably, real-world evidence from the Fight Retinal Blindness Study! (FRB!) has shown that patients with baseline VA <69 letters had significantly greater VA gains with aflibercept than with ranibizumab over 12 months. Additionally, in clinical practice, aflibercept delivers clinically meaningful vision gains that are maintained in
patients with baseline VA ≥ 69 letters, he continued, sharing that this is based on real world data from APOLLON, Moorfields and FRB!.
“Really, it’s these data from Protocol T and from these supporting studies that have led multiple different societies to recommend that if a patient has 20/50 or worse VA, they are better served receiving aflibercept as their treatment of choice.”
This symposium was bursting with more pertinent information than we can include here — such as the finer points of aflibercept’s molecular properties. What we can take away, however, is that aflibercept is proving to be a gold standard when it comes to managing patients with DME and nAMD. Further, proactive treatment regimens like T&E provide a practical approach for both patients and physicians by lowering the treatment burden, with no compromise on visual gains.
* In Protocol T, the dose of ranibizumab tested was 0.3 mg (US-approved dosage), whereas the ex-US dosage of ranibizumab is 0.5 mg. The treatment regimen tested in Protocol T was not the label regimen for either aflibercept or ranibizumab. Bevacizumab has no marketing authorization for intravitreal use. For prescribing information for aflibercept solution for injection, please consult local guidance.
1. Schmidt-Erfurth U, Waldstein SM. A paradigm shift in imaging biomarkers in neovascular agerelated macular degeneration. Prog Retin Eye Res. 2016;50:1–24.
2. Jaffe GJ, et al. Macular Morphology and Visual Acuity in Year Five of the Comparison of Agerelated Macular Degeneration Treatments Trials. Ophthalmology. 2019;126(2):252–260.
3. Singer M, et al. Association of Early Anatomic Response with Visual Function in Neovascular Age-Related Macular Degeneration. Ophthalmology. 2021;S0161-6420(21)00369-9.
4. Guymer RH, Markey CM, McAllister IL, et al.; FLUID Investigators. Tolerating Subretinal Fluid in Neovascular Age-Related Macular Degeneration Treated with Ranibizumab Using a Treat-andExtend Regimen: FLUID Study 24-Month Results. Ophthalmology 2019;126(5):723–734.
This publication, produced on behalf of Bayer Consumer Care AG, summarizes presentations and discussions from the satellite symposium organized and funded by Bayer and held during the COPHy 2021 Virtual Congress, August 20-21, 2021. The views of faculty speakers do not necessarily reflect the opinion of Bayer. Medical writing assistance was provided by PIE Magazine (authored by Brooke Herron) and was funded by Bayer. Prescribing Information for aflibercept solution for injection (EYLEA®, Bayer AG) can be found on www. Ophthalmology.Bayer.com. September 2021 - PP-EYL-ALL-0878-1
The success rate for conventional macular hole (MH) surgery is good — but it’s not great. Complex MH’s are associated with higher chances for surgical failure. This includes chronic, large macular holes (full-thickness, >400 µm diameter); MH-associated retinal detachment; prior failed surgical closure; highly myopic eyes; as well as post-traumatic or inflammatory etiology.
Meanwhile, the poor surgical success of wide MHs may be due to various factors, including the need for wide ILM peel or flap dislocation and excessive intraoperative manipulation of the macular hole edges.1
In recent years, there has been tremendous interest in using human amniotic membrane (hAM) allografts in the management of retinal disease. So, how exactly do they work? These hAM allografts serve as a scaffold for glial cell growth and migration, thereby facilitating re-epithelialization and, at the same time, reducing inflammation and scarring by inhibiting TGF-β signal transduction.2
Clinical studies have demonstrated improved outcomes following the use of human amniotic membrane patches in the closure of recurrent macular holes,3 retinal breaks,3 and high-myopic macular holes associated with retinal detachment.4
There are two types of commercial hAM graft products available for medical use: cryopreserved and dehydrated amniotic membranes. They differ in morphology
by Olewale Salamiand structure due to differences in processing. However, both cryopreserved hAM and dehydrated hAM are feasible alternative grafts for either persistent or recurrent macular holes, as shown in a preliminary case series that demonstrated similar anatomical and functional outcomes.5
According to Dr. Harvey Uy, medical director at Peregrine Eye and Laser Institute in Makati City, Philippines, cryopreserved MH have been more extensively reported by several surgeons. “They are thicker and readily visible in the vitreous cavity on the retinal surface, which facilitates manipulation and insertion into the MH to form a plug,” he explained.

So, how can surgeons determine the optimal graft type in each case? Dr. Uy noted: “Sizing is an important consideration — the cryopreserved AM plug should be large enough to contact the MH edges to facilitate the migration of cells into the hole to enable closure. Overly large hAM discs may override the edges resulting in AM folds that may retard the closure process.
Cryopreserved AM may be cut using retinal scissors while inside the vitreous cavity, or they may be punched out using biopsy punches of various sizes.”
Dr. Uy also shared insights into the intraoperative technique:
“Cryopreserved AM are thick, therefore larger gauge trocars (e.g., 23-gauge) are needed to facilitate trans-scleral insertion into the vitreous cavity,” he shared.
Recently, Dr. Uy and colleagues explored the potential of utilizing dehydrated hAMs to patch macular holes. “Cryopreserved AM has been out of production in the Philippines,
and we were prompted to investigate dehydrated AM patches (AmnioTek, ISP Surgical, Bangkok, Thailand) as a substitute for cryopreserved AM,” said Dr. Uy.
In a series of four eyes with complicated MH, they tested the hypothesis that the dehydrated hAM graft will provide a scaffold that facilitates glial cell migration over the surrounding retinal tissue to close the macular hole.

Dr. Uy said: “After complete pars plana vitrectomy and fluid air exchange, a 2mm, brilliant blue-stained patch was applied onto the MH, followed by gas or silicone oil tamponade.” On the postoperative outcomes, Dr. Uy noted that “postoperative OCT demonstrated that the hAM remained in place in all eyes. The amniotic membrane disappeared in all eyes at the 1-month visit leaving a completely closed MH. No adverse events were observed.”
This small case series suggests that hAM patching may be a helpful adjunct in the management of complex MH.
Dr. Uy explained some of the advantages of the dehydrated graft, which may have played a role in the positive results seen in patients. He said: “The dehydrated graft is readily available and differs from cryopreserved AM in several ways: It is thinner, so easier to handle; semitransparent and can be stored at room temperature.”
He also shared important surgical tips. “Our current technique is to trim the AM using Wescott scissors to a size slightly larger than the MH diameter to ensure complete overlap; stain with brilliant blue dye; and insert through a 25-gauge trocar using 27-gauge retinal forceps. Then we place the AM on the fluid-air interphase and position it over the macular hole using a soft tip cannula to cover it completely. Finally, we complete the fluid-air exchange and apply a tamponade agent (SF6 or silicone oil).
“Our success rate for complex MH closure using dehydrated amniotic membrane patching is about 80%. We encourage patients to strictly assume face-down positioning for two days postoperatively,” continued Dr. Uy.
How can surgeons achieve a high surgical success rate like that of Dr. Uy and his team? “Case selection, atraumatic handling of the AM on the retinal surface, and appropriate sizing will help optimize procedural success rates,” concluded Dr. Uy.

1. Caporossi T, Tartaro R, Bacherini D, et al. Applications of the Amniotic Membrane in Vitreoretinal Surgery. J Clin Med. 2020; 9:2675.
2. Liu J, Sheha H, Fu Y, et al. Update on amniotic membrane transplantation. Expert Rev Ophthalmol. 2010;5(5):645–661.
3. Rizzo S, Caporossi T, Tartaro R, et al. A Human Amniotic Membrane Plug to Promote Retinal Breaks Repair and Recurrent Macular Hole Closure. Retina 2019;39:S95–S103.
4. Caporossi T, Tartaro R, Angelis L De, et al. A human amniotic membrane plug to repair retinal detachment associated with large macular tear. Acta Ophthalmol 2019;97:821–823.
5 Huang YH, Tsai DC, Wang LC, et al. Comparison between Cryopreserved and Dehydrated Human Amniotic Membrane Graft in Treating Challenging Cases with Macular Hole and Macular Hole Retinal Detachment. J Ophthalmol; 2020. Epub ahead of print.
Dr. Harvey S. Uy is a clinical associate professor of ophthalmology at the University of the Philippines, and medical director at the Peregrine Eye and Laser Institute in Makati, Philippines. He completed his fellowships at St. Luke’s Medical Center (Philippines) and the Massachusetts Eye and Ear Infirmary (USA). Dr. Uy is a pioneer in femtosecond cataract surgery, accommodation restoration by lens softening, modular intraocular lenses and intravitreal drugs. He has published over 30 peer-reviewed articles and is on the editorial board of the American Journal of Ophthalmology Case Reports. He is a former president of the Philippine Academy of Ophthalmology (PAO) and current council member of the APVRS.
harveyuy@gmail.com
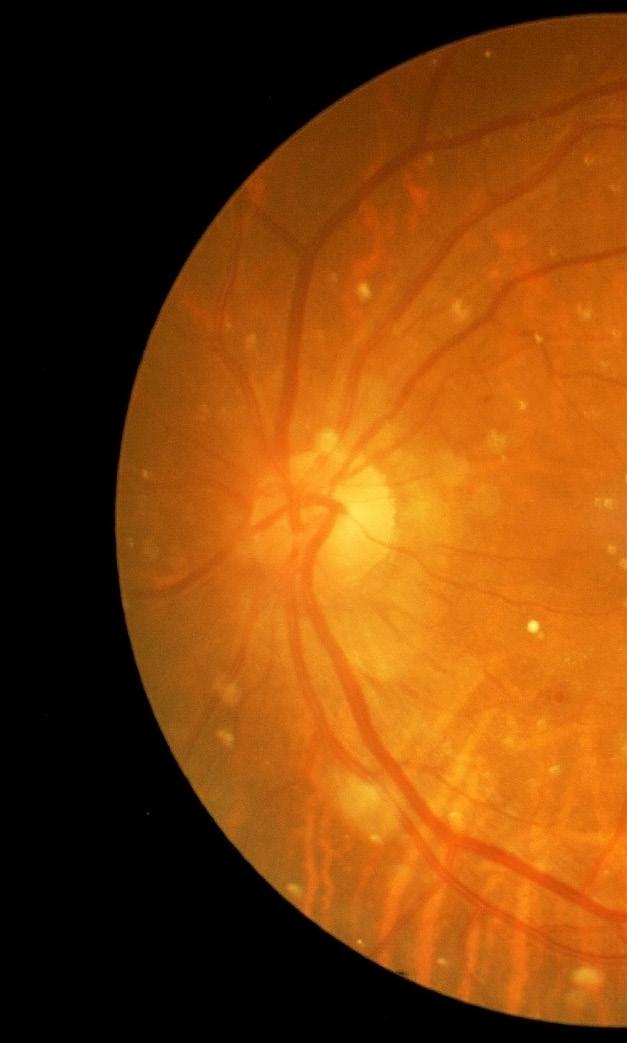
Often, the damage done by retinal pathologies is irreversible. As such, it’s crucial to detect and diagnose posterior segment diseases as early as possible. A growing body of research shows that the peripheral retina can contain disease pathologies — and now, thanks to ultra-widefield imaging, clinicians can now see these important “edges” in order to better diagnose — and even manage and treat — sightthreatening retinal conditions.

While all imaging is “good,” all platforms are certainly not equal. For example, standard field imaging devices are not good enough to reveal the early signs of different pathologies. This is because they are limited to imaging
only a small portion of the retina — and unfortunately, we’re learning that in some cases, the most pertinent details lie outside of those boundaries. Further, if left unnoticed, disease progression can occur. However, earlier diagnosis of retinal diseases is now more feasible thanks to the new iCare EIDON UltraWidefield Module. By providing a wider image of the retina than ever before, the device allows for the discovery of more information involving the signs of pathologies in the periphery.
The iCare EIDON Ultra-Widefield Module enables clinicians to capture 120 degree images of the retina in a single shot (and even up to 200 degrees with the Mosaic functionality), making it an
indispensable tool. In addition, iCare EIDON TrueColor Confocal Technology can also be applied to the UltraWidefield Module. This makes it easier to diagnose and monitor retinal diseases, such as diabetic retinopathy, where lesions can occur in the periphery.
In fact, a clinical study found that the iCare EIDON provides more balanced color images with a wider richness of color content compared to conventional flash fundus cameras. Further, the overall higher chromaticity of iCare EIDON may provide advantages in terms of discriminative power and diagnostic accuracy.

Confocal imaging is the standard in excellent image quality — and iCare EIDON offers the
best of this technology. To take retinal diagnostics to the next level, it guarantees heightened image sharpness, better optical resolution, finer details and greater contrast. Plus, it is the first TrueColor Confocal device that combines the best features of scanning laser ophthalmoscopy (SLO) systems with those of standard fundus imaging, resulting in a winning combination that sets a new performance standard in retinal imaging. Clearly (pun intended), this combination of vital technologies makes it the perfect retinal imaging system with TrueColor and Ultra-Widefield views in multiple modalities.
It is also more advanced when compared to conventional fundus photography. This is because it blocks the backscattered light of structures from the outside of the retina focal plane.
The iCare EIDON also preserves image quality — even in the case of media opacities, including cataract — and can work with pupils as small as 2.5 mm without the need for dilation – thus benefiting pediatric patients. Combined with its easy-to-use interface and patient-friendly features, the iCare EIDON is a valuable and efficient tool in any clinical setting.

Applying the iCare EIDON TrueColor
Confocal Technology to Ultra-Widefield imaging is particularly crucial as it helps to improve the detection, analysis and monitoring of pathologies that could arise in the retinal periphery. These features help to preserve sharpness and fine details even in the periphery, facilitating improved and early diagnosis.
iCare EIDON uses white light LED to provide TrueColor imaging with no distortion and superior color fidelity. Using white light LED, the retina appears as it looks when directly observed, as the entire visible spectrum is present in the
captured image. Thus, it produces crisp and sharp widefield images representing the actual appearance of the retina in multiple imaging modalities.
The added advantage of ultra-widefield imaging is that it is available in all photo modalities: color, infrared, auto fluorescence (AF) and fundus fluorescein angiography (FFA).
AF enables the assessment of the retinal pigment epithelial (RPE) layer integrity while fluorescein angiography images and videos enable the clinician to observe and monitor retinal blood flow details.
The FFA mode allows users to take 120 degree videos for a realistic and dynamic view of the retinal vasculature and circulation mechanisms that may be missed with static flash photography.
No other product in the market allows a wide field conjugated with such sharp images.
The iCare EIDON is easy to use and
requires minimal staff training, which can help reduce examination time and improve patient workflow — which helps clinicians make better use of their valuable time. In fact, all iCare EIDON Family models are user-friendly as they are fully automated, which allows the operator to focus on the patient during the exam. And patients benefit, too: With its ergonomic, motorized chin rest, soft flash, and no need for dilation, the iCare EIDON ensures enhanced comfort for patients.
In addition, the iCare EIDON multi-touch tablet makes magnification and review easy. The remote viewer feature allows for effortless remote data review and any computer or laptop on the same local area network (LAN) can remotely review iCare EIDON images, as data access and detailed analysis are available on multiple review stations.
All of these features come together in the iCare EIDON Ultra-Widefield Module with TrueColor Confocal Technology — and for clinicians who manage patients with retinal disease, it’s one tool that is invaluable for preserving patient’s vision and preventing unnecessary disease progression. For more information, visit www.icare-world.com/uwfl
We all have our weaknesses and this article is going to (rather unexpectedly, it must be said) start with a story about one. Your writer has a peanut allergy: It’s relatively minor considering he can be in the presence of them and not immediately run into problems, but still strong enough to make him jumpy with new food and obsessively check menus. On this occasion, he was meeting a friend for lunch — some vegan dim sum (which as a carnivore he was already suspicious of) — and ordered some tofu dumplings with spicy sauce.
He asked about the presence of nuts in English, his friend did the same in the local language, and was reassured there were none. Turns out, there were, and a pleasant afternoon turned into
an impromptu trip to the hospital. A few hours later after having his body pumped full of steroids, antihistamines and a number of the drugs he couldn’t pronounce, he left feeling woozy, craving sugar with a wallet some $10 or so lighter (the benefits of being European).
The point is, we all have our weaknesses and in our writer’s case, peanuts are certainly one of them, but perhaps what’s more important is how medicine has changed to treat said weaknesses over the years. A relatively mild reaction to peanuts in 2021 is far easier to deal with than it would have been 200 years ago — and as he also has asthma, your correspondent is especially glad he wasn’t alive 2,000 years ago. The leaps and bounds medical science has made in treatment over the centuries
by Andrew Sweeneyare remarkable, and indeed the last 100 years in particular, witnessed incredible progress in posterior segment treatment.
We can point to the Greek physician Hippocrates as being the most likely candidate to indicate the posterior segment. Based on the findings of Alcmaeon of Croton, Hippocrates points to it comprising three layers: 1) a thick outer layer, 2) a thinner middle layer which may protrude like a bladder when injured and 3) an inner layer which is thinnest and very prone to damage. His work would be expanded on by fellow Greek Herophilus, whose surviving

fragments show his understanding of the eye to include the lens (a drop-like body named crystalloids), and a large empty space (locus vacuus) containing humour, likely representing the anterior chamber.1
It wouldn’t be until the golden age of ophthalmology in the 19th century — and the invention of the ophthalmoscope by German physician Hermann von Helmholtz, which allowed doctors to fully examine the inner eye — that posterior segment treatment became fully differentiated.1
Now, we live in an era of constant technological advancements (not just in ophthalmology), and progress can come at breakneck speed. We thought: “Well, we know a pretty good deal about the posterior segment, but who knows better than an ophthalmologist?” So, we reached out to some of the posterior segment’s rockstar doctors to ask them about their history working in the field, and how much it has changed.
“I started as an ophthalmologist around 25 years back … and as you would expect, a lot has indeed changed in the field of the posterior segment. From diagnostics and imaging, to surgical
decision-making and instrumentation, almost everything has changed for the better,” said Dr. Manish Nagpal, a vitreoretinal specialist and director at the Retina Foundation in Ahmedabad, India.
“When I started out, macular hole was considered to be an untreatable condition, however, today one can achieve an almost 95% success rate with surgery for the same condition. Vitreomacular traction is also diagnosed and understood better due to improved imaging, and therefore can be operated as indicated with more accuracy,” said Dr. Nagpal.
A macular hole is a small break in the macula and can cause distorted central vision and blurring. The condition is usually caused by shrinking vitreous due to aging, and as it pulls away from the retinal surface, vision begins to degrade. Natural fluid fills the area where the vitreous has contracted and some patients experience no issues during this process. However, if the vitreous is firmly attached to the retina when it pulls away, it can tear the retina and create a macular hole.2
Macular hole is a relatively common condition and for years it was thought to be untreatable because of missing tissue and photoreceptor degeneration. Initial attempts to treat the condition involved the use of laser photocoagulation; however, it would be the advent of keyhole surgery and improved imaging techniques that would allow this common, yet destructive, disease to be fully treated.3
Now, many retinal surgeons are able to treat macular hole via macular hole surgery, a form of keyhole surgery performed under a microscope. In this process, the vitreous jelly is removed and the inner limiting membrane peeled away, allowing a temporary gas bubble to be pressed into the hole flat to help it seal. The use of this technique resulted in remarkable improvement in patient outcomes, and nowadays, most patients who present less than six months from symptoms onset report a full recovery.
“This was a condition where the patient was certain to lose their central vision with time; today, we can save that vision,” Dr. Nagpal said.
And it’s not just keyhole macular surgery that is being used to cure this one-time vision killer. According to Dr. Hudson Nakamura, a retinal specialist at the Brazilian Center for Eye Surgery in Goiania, Brazil. He points to the use of the internal limiting membrane (ILM) technique as being a great discovery in macular hole treatment.
“ILM peeling for macular hole is fast on the way to becoming the tested and established procedure in the field. That’s just one example besides the comparative results involving the use of this technique from combined procedures such as scleral buckling surgery and vitrectomy,” Dr. Nakamura said.
“Also, with the development of minimally invasive vitreoretinal surgery, surface diseases became a lot better understood. This is because when smaller instrumentation took over for larger gauges, we could manage better and have greater outcomes with surgeries involving macular holes,” he added.

While speaking with Media MICE, Dr. Nakamura was keen to stress the importance of the improvement in gauges in vitreoretinal surgery, which allows for exponentially smaller incisions to be made in the ocular surface. He described that when he started out, the 20-Gauge was used for vitrectomies, and for some procedures a 19-Gauge was used to extract intraocular foreign bodies (IOFBs). The picture he describes today through his experience as a clinician is markedly different, with much more choice now available.
“In 2000 I started my practice with minimally invasive vitreoretinal surgery (MIVS) and it was great to see that from the development of the smaller gauge instruments,” Dr. Nakamura said.
“This began with the 23-Gauge, which was first developed for vitrectomy by Peyman back in 1990 for biopsy purposes; then the 25-Gauge variant for transconjunctival vitrectomy was used back in 2002, by Fuji et al. Subsequently, Eckart developed the
23-Gauge transconjunctival vitrectomy as an alternative to the 25-Gauge system, followed by the development of 27-Gauge by Oshima,” he said.

Retinitis pigmentosa (RP) is another condition that has exemplified the recent rapid advances in posterior segment treatment, said Dr. Nakamura. This condition is usually a single gene disorder, while diabetic retinopathy has a multifactorial (also known as polygenic or complex) etiology. The prevalence of RP is estimated 1 in 4000 in western populations. However, in South Indian populations aged 40 years or above, it has an estimated prevalence of approximately 1 in 930 in urban areas and 1 in 372 in rural locations.4
Many researchers have looked for ways to prevent or slow the visual loss or disability caused by RP, but this drive has been limited by the poor understanding of the pathological or molecular events of the condition. At present, gene therapy and cell transplantation experiments are our best hope in stopping RP, something that Dr. Nakamura was keen to point out.
He highlighted the development of the Argus II (Second Sight Medical Products, Inc., California, USA), a retinal prosthetic system designed to provide useful vision to blind individuals severely impacted by RP. The device is placed at the back of the eye and includes external accessories such as glasses with a built-in camera and a small portable processing unit that captures and processes video signals to be sent to the implant.
“It really is an interesting sector, genetic therapy, and it is becoming more popular in tandem with the development of implants like the Argus II as well,’’ Dr. Nakamura said.
While they may have differed on the posterior segment conditions they wanted to cover, both doctors were keen to emphasize the importance of one aspect in particular: improving technology. They emphasized that ophthalmology (in general) and the posterior segment (specifically) are witnessing better patient outcomes thanks to innovative surgical and treatment techniques. Dr. Nakamura, in particular, drew attention to more than just minimally invasive vitreoretinal surgery, he also pointed out a wide array of improvements in surgery.
“Surgeries are a lot faster these days thanks to high cutting rates and new illumination devices, which make it easier to see the retina during surgery. This has made it possible to carry out bimanual vitrectomies involving safer aspiration and duty cycles, all of which is new,” Dr. Nakamura said.
“Good laser tips appeared in the process. Of course, better intraocular liquids and gases are used intraoperatively today, as well as products to stain the vitreous and membranes,” he added.
These sentiments were echoed by Dr. Nagpal, who pointed out that vitrectomy machines have undergone a remarkable transformation from a surgical point of view. For a procedure that was primarily used as a last resort due to safety concerns, he said that as of today, vitrectomy has evolved to become one of the safest ways to tackle a lot of conditions. However, he would emphasize that of all the various aspects in the posterior segment to undergo change, it’s imaging that is the most remarkable.
“Technology has remarkably changed almost every aspect of the diagnosis to management process for various conditions. The imaging systems have become superb with high-class resolution and easy reproduction, as well as storage for fundus cameras and scanning laser ophthalmology-based units. Optical coherence tomography (OCT) totally changed the way we look at the macula,” said Dr. Nagpal.
“Earlier macular findings had to be made via a subjective examination by a specialist. Today, OCT can objectively pick up even the slightest change in contour, thickness, hole, cells, fluid, etc., and can accurately guide us to the diagnosis, as well as follow-up of treatment. Fluorescein angiography evolved further on digital platforms with better quality and peripheral examination capability (as did ICG angiography). Now we have OCT angiography (OCTA), where one can noninvasively look at vasculature without injecting a dye,” he said.
Naturally, however, the work never ends — and while your writer may very well feel glad that he lives in a

time where his peanut allergy attack could be treated quickly, he does wish that it could be cured entirely. So the search for innovation, new treatments, technologies and cures in posterior segment ophthalmology must go on, ensuring that patient outcomes become better and better. This was a sentiment shared by Dr. Nakamura, who pointed out that while everything had changed, nothing has changed either — as the key purpose of research remains the same.
“What hasn’t changed — what will not change — is the interest to seek for more possibilities and treatments, and the interest to give the patient the better approach, equipment and prognosis,” concluded Dr. Nakamura.
1. Sim PY. The History of Ophthalmology. The American Academy of Ophthalmology. Available at https:// eyewiki.aao.org/History_of_Ophthalmology. Accessed on August 23, 2021.
2. Macular Hole. National Eye Institute. Available at https://www.nei.nih.gov/learn-about-eye-health/eyeconditions-and-diseases/macular-hole. Accessed on August 23, 2021.
3. Bhavsar AR, Gomez J, Kelly NE, Wendel R. Macular hole surgery: A review of past, present and latest treatments for macular hole. Expert Rev. Ophthalmol. 2014;9(5):443-453.
4. Natarajan S. Decoding Retinitis Pigmentosa. Indian J Ophthalmol. 2013; 61(3):91-94.
Dr. Hudson Nakamura is a medical specialist in ophthalmology and specializes in retina and vitreous. He completed a fellowship in vitreoretinal diseases in Canada at the University of Toronto, and another retinal fellowship in his hometown, Goiânia, Brazil, at the Brazilian Center for Eye Surgery. He completed his medical studies at the School of Medicine at the Federal University of Goiás – UFG, and was a resident at the Base Hospital of the Federal District in Brasília. He is currently a professor at the Department of Retina and Vitreous Course of Medical Residency in Ophthalmology at the Bank of Goias Eye Foundation. He is the founder of the Retinawesome meeting, which brings together retinal specialists and vitreoretinal surgeons around the world for discussions on many subjects in retina and retinal surgery. In addition, he is also a member of the Brazilian Council of Ophthalmology.
hudson.nakamura@gmail.com
Dr. Manish Nagpal is a vitreoretinal consultant at Retina Foundation, Ahmedabad, since 1999.


After completing his ophthalmology training at the
M&J institute of Ophthalmology, Ahmedabad in 1996, he further went on to accomplish the FRCS (Ed) at U.K. in 1997. He is a recipient of the prestigious Distinguished Service Award of APAO in 2007. He has a keen interest in making surgical videos and has received the Rhett Buckler award for best video at the annual meeting of ASRS (6 times) 2009 in New York; 2010 in Vancouver; 2011 in Boston; followed by Las Vegas in 2012, Toronto in 2013 and Seattle in 2020. He received the best video award at the film festival held at the 25th APAO meet held at Beijing, China in 2010 and the Best of Show at the annual AAO meeting held at New Orleans in October 2013. At the annual All India Congress (AIOS) he won the best paper in retina four times, including the S. Natarajan award in 2008 and the C.S. Reshmi award for the best video presentation in 2012. He was also the recipient of the IIRSI special gold medal in 2012, as well as the Young Achievers award from BOA in 2012. He has numerous peer reviewed articles to his credit, along with numerous chapters in various international books. He is a regular reviewer with ophthalmology journals such as Retina, American Journal of Ophthalmology (AJO), EYE, European Journal of Ophthalmology and IJO.
drmanishnagpal@yahoo.com
Don’t you just love first times, challenges, experiences and the unknown? In fact, “firsts” are often exhilarating — particularly when outcomes are not guaranteed. While there is no crystal ball in life, when decisions are based on science however, you can be comfortable that the information is solid and evidence-based.
Due to the accelerating global circumstances, it seems like a “sure thing” that our lives will change evermore in the coming months, or even years. Remember not too long ago — before the COVID-19 pandemic — when going to work, the doctor, shopping or even on a date, happened in the physical form? Times have changed and are ever-evolving to a world of working online, remote learning, cloud storage and relying heavily on technology. The encouraging upside of this is that this changing reality is also extremely
efficient in its production of results and transmission of information. Cloud technology is predominant in our lives, providing the “at our fingertips” data required for reliable and life-changing information transportation.
So, fasten your seatbelts and let’s look at an ophthalmic example of the above in action. Pilot TV programs are a chance to trial what may or may not work with a target audience, this applies likewise to pilot studies. In this instance, the target audience and physicians involved suggest the pilot study of daily selfimaging with patient-operated home optical coherence tomography (OCT) is a clear winner.
Introducing Israel-based Notal Vision
Inc., a diagnostic services company that operates the Notal Vision Diagnostic Clinic, a medical provider with a proven platform for engaging patients and AI-enabled analyses of high-volume personalized health data. This extends disease management from the clinic to the home to improve vision outcomes, reduce treatment burden, and improve health economics.
The company recently conducted its first longitudinal pilot study on its Notal Home OCT, a daily, in-house selfimaging for neovascular age-related macular degeneration (nAMD) patients. This patient-operated home OCT is not only convenient for nAMD patients, but also provides quick and accurate results to retina
specialists via the cloud. And let’s face it, in this current climate the whole world needs not only efficiency, but a way to continue protecting vulnerable patients during an ever-changing environment.
Notal Home OCT uses a quick, noninvasive technique via a range of light that takes a rapid scan of the eye within just minutes. The whole process is so convenient for the user, it is not classified as being a chore — but rather an effortless part of everyday life.
The pilot study’s results have been published* and detail the number of successfully completed OCT tests by four individuals aged approximately 73 years. Let’s check out the solid preparation that led to the results of this super pilot study...
The study was led by Prof. Anat Loewenstein, director of the Department of Ophthalmology at Tel Aviv Medical Center (Ichilov) in Tel Aviv, Israel. Conducted in Israel, the pilot study
followed four patients undergoing routine anti-VEGF therapy for nAMD in one or both eyes for up to three months. Out of 240 self-imaging attempts 87.9% were successful — and importinaly, of these 97.6% had satisfactory image quality. Further, for fluid presence, the Notal OCT Analyzer (NOA) agreed with human grading in 94.7% of cases.
They found that participants could perform daily self-imaging at home and generate macular cube scans of satisfactory quality — and automated quantitative OCT analysis achieved high agreement with human grading. Further, daily self-imaging with automated OCT analysis permitted detailed characterization of the dynamics of fluid exudation and revealed wide variation between eyes. Not only do home OCT telemedicine systems represent an alternative paradigm of disease monitoring, they may allow highly personalized retreatment decisions, with fewer unnecessary injections and clinic visits.
Fewer unnecessary injections and visits to the doctor is sounding very convenient and resourceful for all involved, leaving more time to live life. The OCT analyzer performs automated analysis of the OCT scans and generates a report to the physician when a specified change in the disease movement is detected. Doctors are provided with 24/7 access to all scans and can request their patient attend the clinic or office for further
evaluation or treatment should it be deemed necessary.
Notal Vision CEO Dr. Kester Nahen said: “We thank the investigators for their pioneering efforts and laying the foundation for a new paradigm in patient management,” he shared, adding that the device successful demonstrates all elements required for a home OCT monitoring system, including intraretinal fluid and subretinal fluid volume trajectories from NOA segmentation from both the patient’s right and left eye.
“Retinal fluid exposure described by the area under the curve between treatments (syringe) differs significantly between eyes, despite similar fluid volumes measured on the day of office treatment visits illustrating the medical insights gained from daily OCT imaging at home,” continued Dr. Nahen.
“Longitudinal home-based study has allowed us to embark on several ongoing larger scale trials with pharmaceutical companies that are using our investigational home monitoring service,” he concluded.
This data shows that exciting times for the Notal Vision Inc. and its Home OCT certainly lie ahead. It has all the potential to support existing and future developments in the treatment and management of retinal disease. What an extremely perfect and rewarding landing for this pilot study!
Acalling that is close to the heart of Dato’ Dr. Haslina Binti Mohd Ali is the prevention of blindness in Malaysia. And now, her years of dedication and service in providing vitreoretinal care has rightly earned the honor of being the 2021 recipient of the Asia-Pacific Academy of Ophthalmology (APAO) “Outstanding Service in Prevention of Blindness Award.”
Dr. Haslina is the only vitreoretinal surgeon in the North Malaysia states of Kedah and Perlis. She has been instrumental in not only treating patients in Hospital Sultanah Bahiyah Alor Star in Alor Setar, but has also collaborated with hospitals around Malaysia.
She graduated from the National University of Malaysia (UKM) in 1989 and obtained her master’s in
Ophthalmology in UKM In 1999. She then completed her fellowship in Vitreoretina at the Royal Liverpool University Hospital in the United Kingdom from January 2004 to April 2005.
When she started providing vitreoretinal services at the new turnkey Hospital Sultanah Bahiyah, she served patients from four states in the Northern Peninsula. With the presence of younger vitreoretinal surgeons in the state of Perak in 2011 and in Penang in mid-2014, she began focusing on serving these two states, which have a population of more than two million. Since then, she has remained the sole vitreoretinal surgeon in these two states.

“Two days per week, we run two vitreoretinal clinic rooms, one

preoperative clinic room and one antiVEGF clinic room,” said Dr. Haslina. “Before the COVID pandemic, we used to have between 80-130 patients per day and clinic [hours] used to stretch regularly up to 7:30 or 8 p.m.. We try to do as much as possible each day.”
She also examines patients in the emergency clinic room on her clinic days. The waiting time for a vitreoretina; clinic is more than two months, but at times patients that need early intervention will be seen as soon as possible.
For the affable and down-to-earth Dr. Haslina, her interest in vitreoretina
started during her post-graduate years.
“My professor in vitreoretina was very encouraging and allowed us to do many things. Our head of ophthalmology services was also a VR surgeon and she made the path easier for me. I developed an interest in vitreoretina before I was a specialist.”
The longer Dr. Haslina worked as a VR-surgeon, the more she realized that there are so many needs. Diabetic retinopathy (DR) is a main eye disease encountered by vitreoretinal specialists. Thus, she said that there were active collaborations with the state’s Health Department, family medicine specialists, endocrinologists, and also feto-maternal subspecialists (obstetricians) to screen for DR.
“Many patients lost their sight due to vitreoretinal problems and diabetes. And many of them were young. So I thought what I was doing must be correct,” she says.
She recalls that when she was a fellow in Liverpool, she had two patients with very bad diabetic retinopathy. One was a young woman in her early 20’s and the other was a Pakistani woman who could not speak English well. Seeing and treating these patients for 1.5 years gave her the conviction to battle blindness.
“When I returned home, I wanted to give myself 10 years to try to decrease significant blindness. But 16 years later, I know I have failed,” she said. “I am seeing patients much younger coming in with really bad diabetic eye disease. The conditions are difficult and complicated and many of them are depressed because they can’t see.
“Unfortunately a substantial number of patients come late, and they expect miracles. I have tried to do as much as possible. Any one time I would have easily more than 250 patients waiting for surgeries and during COVID, it has increased,” said Dr. Haslina, adding that seeing her patients suffer can make her feel depressed.
No doubt, the COVID-19 pandemic has made things much harder for both doctors and the patients: “I was constantly worried that patients could not come to the hospital and that we
were missing out on urgent cases,” said Dr. Haslina. “Many surgeries had to be postponed. The waiting list spiked from 300 to 700 cases. Surgeries requiring general anesthesia could not be performed and we could only operate until 6 p.m.”
Throughout the years, Dr. Haslina and her team have been providing vitreoretinal care in other parts of Malaysia. One of her more unforgettable postings was working at Hospital Umum Sarawak from early 2018 to February 2020, which was halted due to the pandemic. She and her team worked there every four months in 2018 and then once every three months from 2019-2020. The monthly visits were rotated between Dr. Haslina and two VR surgeons from the states of Kelantan and Penang.
Another stint that gave her great satisfaction was providing ophthalmology services in Langkawi, an island in the state with a population of about 100,000.
“Together, with my doctors in the ophthalmology department, we traveled to Langkawi by ferry once a month. My initial excitement turned to a nightmare when extreme weather caused me to have severe motion sickness,” she recalled.

But that didn’t deter Dr. Haslina from carrying out her duty. The team started conducting cataract surgeries at the then new Hospital Langkawi and further increased their services by visiting the hospital for three days every three
weeks.
“We screened students for refractive errors and adults for cataract for three consecutive years. The high volume of cataract surgeries that were performed there at a regular interval managed to decrease waiting time for cataract surgery, from 10 months to six weeks after each exercise,” she said.
Dr. Haslina and her team also have outreach programs and work together with NGOs.
“We liaise closely with Rotary Club of Langkawi and they provided intraocular lenses for the poor there. The last high volume cataract surgeries were done last year in April as a shared project with the Ministry of Education. More than 80 patients were operated on.
“Our team also works closely with Yayasan Sultanah Bahiyah. The foundation provided a bus complete with equipment and instruments for mobile eye screenings for the Kedah state in 2017 — plus full-time staff who have been trained to capture and interpret fundus photos,” she said.
Dr. Haslina has also initiated a series of courses conducted by World Sight Foundation based in the U.K. This includes courses on orthoptics, ocular oncology and neuro-ophthalmology that were conducted in a few states in Peninsular Malaysia.
One area of work that brings her much joy and satisfaction is teaching medical officers (MO) in the master’s programs, and also servicing the MOs.
“I like teaching. To be able to teach and
motivate the younger generation is very gratifying, especially when you see them as specialists now.
“We seniors regularly emphasize to our young doctors to treat and speak to patients well, to work from our hearts, and to empathize. As head of the department, I used to interview candidates before they joined us to emphasize that hard work was expected of them and that ophthalmology is not a relaxing posting,” she explained.
“They knew what they were getting into. We had excellent MOs who joined the master’s program and are currently providing service to other hospitals. Nowadays, there are many young doctors who come to us as a transit before they get their actual postings. Most stay with us for less than eight months. But we continue to impart what we can.
“The young doctors who worked with us would remember what the seniors imparted on them. My advice to them is: Work with all your heart. So whatever they do, they will continue to spread to their juniors,” she said.
Dr. Haslina will receive the APAO Outstanding Service in Prevention of Blindness Award in September 2021.
“I don’t know what I did to deserve this,” she said humbly. “But I guess when you have passion for your job, this is a bonus and a gift from God.”
After serving the government sector for 31 years, Dr. Haslina decided to opt for early retirement in June this year.
“I’m not retired from ophthalmology and vitreoretinal services, but just retiring from government service,” she clarifiesd “I still go to the hospital twice a week to do surgeries. And twice a week I go to an eye center in Sungai Petani and do vitreoretinal work as well.
“I have been doing the same thing for so long, I believe there is a time when you need to have a change,” she shared.
Dr. Haslina is blessed to have a supportive husband who is her best friend, and three daughters aged 23, 25 and 27. Her eldest daughter is pursuing early childhood education and her second daughter is studying medicine. Her youngest is an architecture student.
She admits it’s difficult to balance her career with her family. She has been dedicating a lot of time for work, as surgeries can stretch into the night. Plus, she could be on-call during weekends. “I am lucky that I have a very supportive husband and very forgiving children and they know that I love them,” she quipped.
Dr. Haslina was an active member in the government’s committee of Prevention
of Blindness. In recent years, she has taken a step back to let younger ophthalmologists helm the committee. She hopes that they will continue to be active in the prevention of blindness.
“In Malaysia, we need more general ophthalmologists, but we also don’t have enough subspecialists. We definitely are in need of more VR surgeons. There are only 13 of us in the government sector, but a bit more in private practice,” she said.

Dr. Haslina has always loved her job. And to her, learning is a continual process.
“I can never imagine not working. The ability to continue to learn new things and to make progress gives me inspiration and keeps me going,” she concluded.
Dato’ Dr Haslina Mohd Ali is a consultant ophthalmologist and vitreoretina subspecialist based in Hospital Sultanah Bahiyah Kedah, a state in the Northern Peninsular of Malaysia. She started working at Hospital Alor Setar (state general hospital) as a general ophthalmologist in 1999 and subsequently pursued the vitreoretinal subspecialty at Royal Liverpool University Hospital in 2004. She has been providing vitreoretinal (VR) services since she returned, and remains the sole VR surgeon in Kedah and Perlis. She was head of the Ophthalmology Department at Hospital Sultanah Bahiyah from 2013 until 2020. She provided VR services in Sarawak for two years, a large state in East Malaysia, in rotation with two other VR surgeons, before the post was filled in July 2020, by one of her fellows. She also collaborated with an NGO Yayasan Sultanah Bahiyah for mobile screening in the state of Kedah. She was also previously a member of the National Prevention of Blindness and Cataract Outreach Committee. She has trained fellows in vitreoretina and postgraduate students, many of whom are now working all over the country. Dr Haslina is the recipient of the 2021 Asia-Pacific Academy of Ophthalmology (APAO) Outstanding Service of Prevention of Blindness Award.

haslina.eye@gmail.com




For some people, marketing comes naturally. Garnering positive attention, networking with strangers and generally putting oneself and one’s business out there is just easy for a lucky few.
For most of us others, getting good at marketing often takes concerted effort, a bit of luck and a willingness to bounce back from missteps. Perhaps most importantly, it takes conscious analysis to improve marketing skills based on observations and experimentation. It’s as much of a science as it is an art, and we can engage our trusty ol’ left brain to help us make crucial decisions.
To help our CAKE & PIE Expo (C&PE 2021) attendees up their marketing game, Media MICE put on a marketing seminar at said event. You’ll get the benefit of the seminar here as a reader, too, as there are some valuable nuggets of insight about how to stand out from

the crowd. Just as an example, this writer has taken it upon himself to challenge the “pearls of wisdom” cliché with “nuggets of insight” simply because it’s different.
So, let’s take a look at what our three speakers at the presentation had to say — because we all might learn something here. Our first speaker was Nikki Hafezi, from the Elza Institute in Zurich, Switzerland. She was followed by Dr. Kristie Nguyen, our dear friend and optometrist in Orlando, Florida. Finally, none other than our very own CEO and publisher Matt Young stepped in to share his story, and just how bananas it’s been.
Mrs. Hafezi’s presentation focused on questions clinicians can ask themselves to help improve their business. As any
independent practitioner knows, you have to wear multiple hats as a business owner — not only do you have to be an expert in eye care, but you also need to be an expert in marketing. You can look at it as exhausting or exhilarating depending on your mood on a given day.

Nikki began with a good analogy — analyzing threats in the form of mosquitoes, tigers and dragons. Mosquitoes are the annoying, daily problems that pop up that you can target and neutralize. Doing so takes time, but still has to be done. Tigers are your competitors — you have to keep an eye on them at all times, since they would love to eat you given the opportunity. Dragons are the unforeseen, major events that can pose existential risks to your business. Think COVID-19.
When considering how to improve your marketing, Mrs. Hafezi suggests a deep dive into your business plan
and personal desires. Who are your customers? Are you focusing only on business-to-customer relations, when business-to-business could help you? What are your desired outcomes, or what does success look like? Who are your competitors, and what do they want? What makes you stand out, and what do you offer that’s unique?
The way to identify what makes you special is what your competitors see as a threat. Focus on those aspects of your company and you’ll have a clear value of what you’re offering. Identify your weaknesses and hire people who are better than you at those specific areas — and note that human resources may be frustrating, but a good HR department is worth its weight in gold.
Finally, consider what happens to your company if and when you’re not there anymore. Continuity and predictability are crucial to a company’s stability and success, so having succession lined up and training future leaders will help your company weather any storm.
Both Dr. Kristie Nguyen and our notDr. Matt Young have had a similar experience with getting noticed. Namely, taking physical steps to stand out has been a crucial part of the success of each person, but in notably different ways. The message remains similar, though.
attention to herself, she pointed out. Her older brother was the attention-getter of the family, and she was content to be quietly successful in the background, both in her personal and professional life.
Attending a marketing session gave her the idea to change her outward appearance, so she radically changed her hair color. That seemed to be the trick — in the two years since, she’s exploded onto the digital scene with some 30,000 followers on LinkedIn and a massive presence online. As it turns out, a simple trick like changing her hair color helped her stand out and made her not only feel more confident about herself — it made potential clients, patients and business partners feel more comfortable talking to her as well.
Matt’s story follows a roughly similar trajectory, though with a lot more trial and error involved. For years, he was a standard suit-wearing fella — even shopping at the same suit shop that President Joe Biden shopped at in Delaware. If you’re going for the same outfits a president is, you’re probably dressing a bit conservatively.
The thing is, no one noticed someone in a boring old suit at a conference. Despite years of writing experience, no one knew who the heck Matt was. So, he tried some gimmicks.
First came the gadgets — Google Glass to start, which did indeed attract some attention. But as Google Glass’s star faded, this option wasn’t really … well,
So, what to do? PIE Magazine’s first edition was out, and we needed attention. Time to grab life by the bananas.
Matt had the strawberries to get suits made with all sorts of fruit print — bananas, pineapples, watermelons, oranges and so on. Unsurprisingly, a suit like that does stand out in a blandly colored ophthalmic conference, where safety in color is the order of the day. The trick worked, people noticed, and PIE flew in people’s faces as 3,000 magazines were snatched up in a few hours. The rest is history.
That is to say, there’s a lot more history, but we’re running out of page space.
What’s the takeaway here? It’s simple: Life is colorful. People like life, and pay attention to it. Color draws attention because we’re biologically designed to notice it.

There’s more than just that, of course. Embracing a colorful life — physically and metaphorically — is ultimately more rewarding than camouflaging oneself in a sea of drab colors. When you stand out, you get noticed. And when you get noticed, you’re doing marketing right.
See? We ended up back at the beginning. Combine your analytical side with your colorful side and you’ll end up being who you’re meant to be. That nugget of insight goes for practices, too. Happy marketing, everyone
The CAKE & PIE EXPO (C&PE) 2021 was held from June 18 to 19. Reporting for this story took place during the event. You can still watch the full video of this marketing symposium on Media MICE YouTube Channel .
Strabismus in adults is often associated with childhood development or as a comorbidity, but in rare cases can be caused by retina detachment surgery. Is there a way to avoid this complication?

In the medical field, there are a number of conditions and entities that have a scientific name that is less commonly known amongst the lay community. For example, the web between your thumb and forefinger is called the purlicue (and is pronounced just like “curlicue”). The small, triangular pink bump on the inside corner of each eye is called the caruncula. Paresthesia is that tingling sensation when your foot falls asleep.
So too is strabismus known by another term, one that has been the bane of kids in the schoolyard subjected to bullying, for a long time: strabismos. It is a common condition and the term comes from the ancient Greek strabismus, meaning “to squint.” Many of us will remember that kid in junior school, or maybe we were that kid, with the eye patch, but that was actually used to treat amblyopia or “lazy eye,” and in fact, strabismus is a different kettle of fish.
Strabismus occurs when your eyes are

not lined up properly and they point in different directions. One eye may look straight ahead while the other eye turns in, out, up or down, and the misalignment can shift from one eye to the other. The most obvious symptom of the condition is where one of the patient’s eyes looks in a different direction to the other one.
It is more common among children and can be caused by a number of conditions including cerebral palsy, Down syndrome and hydrocephalus, and while it can affect vision it is often treatable by either wearing special glasses or via surgery in more severe cases. Patient
outcomes in childhood strabismus are usually good especially if treatment is performed quickly on the presentation of symptoms.1
In adults, however, it can be more severe, especially if their childhood strabismus was untreated as this can lead to permanent double vision. When it occurs later in life, it is usually caused by ocular trauma including accidents or damage during surgery; it can also be caused by a number of other conditions including diabetes, thyroid disease, Myasthenia gravis, brain tumors or stroke. Surgery is the most common treatment and often involves more than one surgery to treat the condition.2
Now while the aforementioned causes of strabismus in adulthood are among the most common, there are of course rarer reasons — ones which make for an interesting article to sink your proverbial teeth into. Retinal detachment, which involves the separation of retinal cells from the layer of blood vessels that provides oxygen and nourishment to the eye, does not in itself usually cause strabismus. However, in rare
cases it can also occur following retinal detachment surgery, leading to a group of researchers from Atlanta, Georgia (USA) and Bucheon, South Korea, to investigate the issue.

The published paper, Effect of Scleral Buckle Removal on Strabismus Surgery Outcomes After Retinal Detachment Repair, 3 investigated the effect of scleral buckle removal on outcomes of strabismus surgery in patients with a prior history of retinal detachment surgery. Scleral buckling has been considered to be an effective means to reattach the retina for over 50 years, but it has also been associated with the development of strabismus. Removing the scleral buckle can resolve the strabismus issue, but may, of course, result in the retina becoming detached again.
The researchers, therefore, reviewed the medical records of 18 patients who underwent strabismus surgery
following a scleral buckling procedure at one institution. The effect of multiple variables on outcomes like gender, age, surgeon, number of strabismus surgeries, adjustable suture use, previous pars plana vitrectomy, preoperative best-corrected visual acuity, and time of surgery were considered to eliminate any anomalies in data recording. The Fisher’s exact test and Mann-Whitney test were used and outcomes were considered successful if there was ≤10 prism diopter (PD) residual horizontal and/or ≤4 PD residual vertical deviation.
The researchers found that strabismus surgery coupled with scleral buckle removal was associated with a higher rate of success at 62.5%, with success without buckle removal at 10.0% (p=0.04). In fact, despite concerns about detachment, none occurred after scleral buckle removal in any of the 18 patients. Noting that recent studies have uncovered post-scleral buckling retinal detachment rates of a maximum of 8%, they also found that removing the scleral buckling element either before or during strabismus surgery was associated with improved ocular alignment.3
1. Strabismus in Children. The American Academy of Ophthalmology. Available at https://www.aao. org/eye-health/diseases/strabismus-in-children. Accessed on Wednesday, August 4, 2021.
2. Strabismus in Adults. The American Academy of Ophthalmology. Available at https://www.aao. org/eye-health/diseases/what-is-strabismus. Accessed on Wednesday, August 4, 2021.
3. Chang JH, Hutchinson A, Zhang M, Lambert SR. Effect of Scleral Buckle Removal on Strabismus Surgery Outcomes After Retinal Detachment Repair. Strabismus. 2013;21(4):235-241.


Teams from Japan, China and India tested their surgical mettle and battled it out during the second episode of “Repair that Retina,” the world’s first competition-webinar for eyecare professionals. Organized by Alcon (Geneva, Switzerland), the competition was judged by renowned vitreoretinal specialists Dr. David Chow from Canada, Dr. Kourous Rezaei from the United States, and a mystery judge.
by Tan Sher LynnDuring the basic surgery round, Dr. Hemanth Murthy from Team India presented a video on bimanual surgery. To begin, he entered the cleavage plane by redefining the secondary membrane. As he started clearing the secondary membrane, he saw a dense and broadbase addition at the macula. “That’s the time when I switch over to bimanual
surgery. I used the scissors and the forceps for the bimanual surgery, because the scissors provide an elegant tool to safely dissect the membrane from the retina.
“As you can see, there are major vessels that are adherent to this membrane. The scissors dissection is a good way to separate these vessels from the fibrovascular tissue. By doing so, I’m able to save major blood vessels and prevent bleeding, which is very important in diabetic TRD (tractional retinal detachment) surgeries,” said Dr. Murthy.
Once he was able to dissect the membrane, he cleared it off using a cutter before doing an ILM (internal limiting membrane) peel, endolaser
treatment, followed by a fluid exchange. All the major vessels were intact and there were no tears.
“A preoperative OCT (optical coherence tomography) can help you decide which cases need bimanual surgery. If you see a densely adherent membrane at the retina, this should alert you to the possibility of a bimanual surgery,” he suggested.

During the complex surgery round, Dr. Xiaorong Li from Team China presented a case involving a 50-year-old woman with high myopia. Suprachoroidal hemorrhage occurred during surgery. The posterior chamber pressure increased, while the anterior chamber was shallow. The vitreous cavity was filled with blood. He tried to remove the blood as much as possible. Silicone oil was also injected into the eye and removed in order to drain the blood. This was repeated eight times. One month after the surgery, OCT images showed that the suprachoroidal hemorrhage was totally absorbed.
Residential judge Dr. David Chow commented that he would first check the blood pressure of the patient if he were to perform vitrectomy on a high myope.
He also noticed that in the video, the trocar cannula was used to stabilize the contact lens holder on the eye. “The
trocar cannula is made for internal clearance of a certain length, and by putting it through the wing of the contact lens holder then through the sclera, I would be worried whether the cannula has a higher risk of going suprachoroidal in its location. So, if the cannula goes suprachoroidal in a high myope with high blood pressure, those are risk factors for a choroidal hemorrhage,” he commented.
Summing it up, residential judge Dr. Kourous Rezaei said: “The key is to pay attention to where the choroidal hemorrhage is coming from. You need to pay attention to the IOP, maybe use perfluorocarbon as the mystery judge pointed out, or make sure the eye is pressurized. Get things done quickly and get out of the eye. You don’t want to mess around too much. Generally, it’s not a great idea to drain it as it may cause more bleeding.”
Meanwhile, Dr. Mihori Kita from Team Japan shared a case of proliferative vitreoretinopathy (PVR) with severe corneal opacity, for which she decided to perform endoscopicguided vitrectomy with a 25-gauge endoscope. This was opposed to the temporary keratoprosthesis followed by keratoplasty, as this option can possibly cause corneal graft failure. A few months later, after silicone oil removal, the
patient was referred to the corneal surgeon for cornea transplantation.
The mystery judge commented that he would prefer to do the keratoprosthesis instead of the endoscopic-guided vitrectomy as it offers better visualization, which would lead to better outcomes.
Dr. Chow said that the mystery judge’s comments resonated with him, as in his experience he had been limited by the visualization of the endoscope. Nevertheless, he applauded the fact that Dr. Kita’s video provided a clear visualization of the vitreous. “You can see that when she was pulling up those membranes and the vitreous was lit up and was visualized way better than what we normally see with a microscope or NGENUITY. So, even though the resolution is not great, the technology itself may allow us to visualize the vitreous membrane and PVR membrane better as what we saw in her video,” he concluded.
The second episode of Repair that Retina was held on 14 August 2021. Reporting for this story took place during the event. A version of this article was first published in piemagazine.org on August 19, 2021.

