
17 minute read
Retinal pharmacology has come a long way from the discovery of anti-VEGFs, but it doesn’t sit on its laurels... the quest to innovate continues
Innovations in Retinal Pharmacology
by Joanna Lee
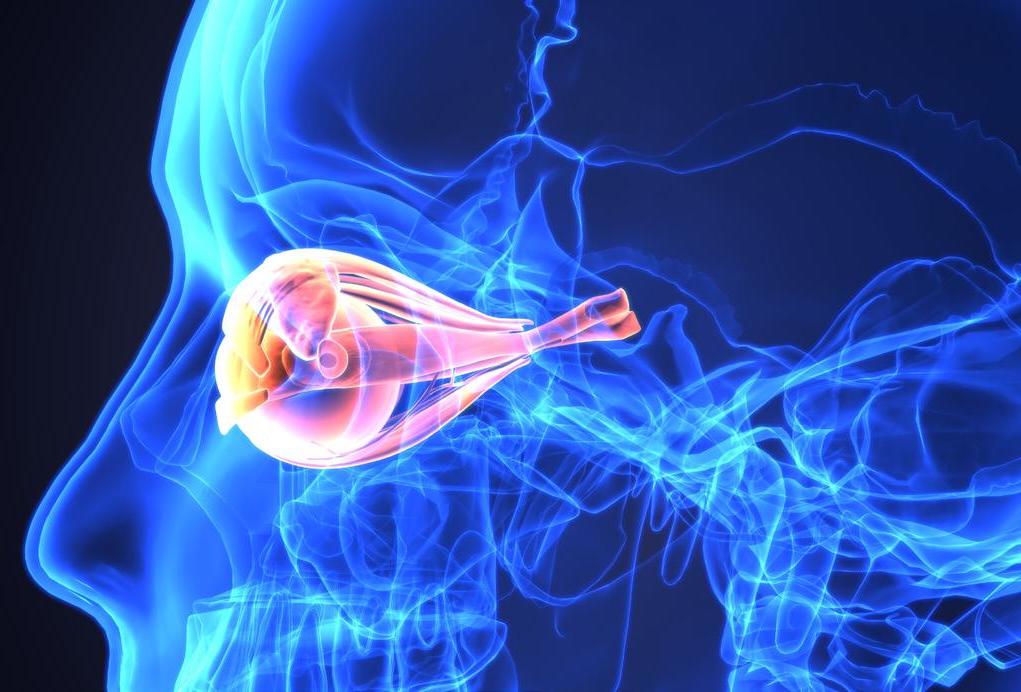
Retinal pharmacology has come a long way ever since anti-VEGF drugs came onto the scene 15 years ago. Today, new delivery methods are being developed as the quest for more effective medicine continues.
A“nuanced approach” to assessing fluid is important,” Dr. Srinivas Sadda of the Doheny Eye Institute in Los Angeles, California (USA) said during his presentation on fluid management in neovascular age-related macular degeneration (nAMD) at the 37 th World Ophthalmology Congres (WOC2020 Virtual®).
Review of literature
Clinical trial data over the decades have shown that uncontrolled exudation in nAMD is bad for vision. He cited previously published studies like CATT 1 , IVAN 2 and PIER 3 , among others, which demonstrated how intraretinal fluid, subretinal fluid and sub-RPE fluid, their absence or presence thereof, in exudative-based treatment approach influenced the visual outcome. For instance, the PIER study indicated that patients who had no residual fluid tend to have better visual outcomes compared to those who had fluid. However, the HARBOR study, of which Dr. Sadda is a part of, showed that eyes with residual sub-retinal fluid only at 12 and 24 months experienced the greatest baseline characteristic visual acuity (BCVA) improvement. This led to his hypothesis that perhaps some residual SRF may be tolerated in the short-term. However, controlling exudation, in Dr. Srinivas’ estimation is still the key to achieving optimal visual outcomes in nAMD patients.
Drug delivery devices
Providing an overview of retinal pharmacology, Dr. William Mieler of the The University of Illinois College of Medicine in Chicago (USA) noted that intravitreal injections (i.e. anti-VEGFs) and the use of sustained-release solid implant intravitreal devices are currently the most common methods used. However, the need for less invasive, safer and more effective drug delivery methods continues to drive innovation. Latest developments include microneedles, a micrometer-sized needle and injector which can deliver drug into suprachoroidal space (SC). There’s also the microcannula with (or without) light illumination for SC drug delivery as well as a microcatheter with potentials for stem cell delivery and delivery of corticosteroid. Other new delivery systems on the block include the encapsulated cell technology (ECT) where cells genetically have been modified to produce a desired agent that are encapsulated in a semi-permeable hollow fiber membrane. It is retrievable when implanted in the vitreous. Another interesting drug delivery system is the Ophthalmic MicroPump™ (Replenish, Pasadena, California, USA) that delivers continuous drugs to the anterior and posterior segments, among other innovations. Dr. Mieler’s presentation’s co-author, Dr. Jennifer Kang-Mieler of the Illinois Institute of Technology in Chicago (USA) has invented the microspherethermo-responsive hydrogel drug delivery system (U.S. patents pending) which uses a biodegradeable thermo-responsive hydrogel in the in-vitro release.
Molecules and substances of note
In another exciting development, Kyoto University’s Dr. Hanako Ikeda’s team found that VCP (valocin containing protein) ATPase inhibitors known as KUS121, KUS187 is shown to reduce death [Editor’s Note: KUS stands for ‘Kyoto University Substance’, developed by Prof. Kakizuka at the university.]
KUS, a small-molecule compound, showed neuroprotective effects on the ganglion cells/photoreceptors in animal models of ocular diseases. These compounds show promising new avenues for glaucoma or retinal degeneration treatment using neuroprotective agents. The research team tested it on a small sample of patients with central vein artery occlusion (CRAO) in humans. The results demonstrated that KUS could prevent retinal ganglion cell (RGC) loss and improved visual acuity. Further tests after these two phases of study will be done in a larger scale in the future, Dr. Ikeda said.
The chair of this session, Dr. Taiji Sakamoto from Kagoshima University in Japan, said: “So far, there’s been no drug to increase VA in CRAO so we’re looking forward to Phase 3 of this study.”
The role of imaging
Further, Dr. Seung-Young Yu from Kyung Hee University in South Korea shared
Cont. from Page 4 >> The signs of progression of KC include thinning of the cornea more than ten microns per year, and increase of the curvature of the cornea more than one diopter per year. For patients under age 30 with unstable cornea, surgeons may stabilize the cornea by corneal collagen cross linking (CXL), and wait three to six months before conducting cataract surgery. Prof. Elmassry also warned that toric IOLs do not have good results in irregular cornea. His take home message: “Provide a complete explanation to the patient, carry out all preoperative investigations, protect the cornea, and allow enough time for the compromised cornea to heal.”
Management of cataract with uveitis
There should be no uveitis activity in a cataract patient for at least three months before surgery, said Prof. Hatem Ammar of Sohag University, Egypt. Cataract is a common complication from uveitis. It occurs in 50% of patients with anterior and intermediate uveitis, and 83% of juvenile idiopathic arthritis. Phacoantigenic uveitis is an absolute indication for cataract extraction, he noted. For pediatric patients, the risk of amblyopia needs to be considered when cataract surgery is delayed. “Managing patients’ expectations with regards to visual prognosis is paramount,” said Prof. Ammar. Surgery could be more complicated and longer due to abnormal anatomy and there is a possibility of significant postoperative inflammation. Cataract surgery success is critically related to careful control of perioperative inflammation. While the condition requires delicate surgical maneuvers, well-controlled perioperative inflammation will produce excellent results in cataract with uveitis.
Cont. from Page 6 >>

a yellow glow. Dr. Basu reminded the audience that posterior segment uveitis is commonly infectious compared to anterior segment.
Third, laboratory investigations could also indicate infection with evidence of infection versus evidence of the immune response (ocular fluids, biopsy, blood, radiology).
Lastly, response to treatment like antimicrobial therapy could be observed to determine the type of infection present. Also, Prof. Zierhut invited those interested to learn more about uveitis to engage with the International Uveitis Study Group. “If you are a little more familiar with uveitis, you’ll start to love it,” he said.

Cont. from Page 9 >>
findings from her study, titled Treatment Interval of Anti-VEGF: Imaging Analysis. The study’s purpose was to evaluate the efficacy of intravitreal aflibercept for neovascular membrane, pigment epithelial detachment secondary to type 1 choroidal neovasculaization (CNV). The study found that fixed dosing of aflibercept improved both visual and anatomical outcomes in patients with nAMD for the first year of treatment. The fixed dosing also induced a “comparable decrease in pigment epithelial detachment (PED) volume, size of CNV and vessel density of the neovascular membrane at all follow-up visits.” It also recorded vessel density reduction which was significantly related to anatomical activity reflected on the OCT. This was shown to be significantly higher in patients who had improvements in BCVA compared with patients without any progress in their BCVA.
PDT versus anti-VEGFs in PCV
Finally, Dr. Joo Yong Lee of the University of Ulsan in South Korea, shared about polypoidal choroidal vasculopathy (PCV), focusing on studies involving its treatment using photodynamic therapy (PDT), anti-VEGF agents. PCV, as many know, is more prevalent in Asians compared with Caucasians. Clinical trials reviewed in this presentation included the PLANET study and Everest II, comparing the two, and more recently the DRAGON study. 4 His conclusion was that both monotherapy with anti-VEGF agents and combination therapy with antiVEGF agents or PDT can achieve visual improvement and reduction in disease activity.
References:
1
2
3
4 Maguire MG, Ying G-S, Jaffe GJ, et al. (CATT Research Group). Single-Nucleotide Polymorphisms Associated With Age-Related Macular Degeneration and Lesion Phenotypes in the Comparison of Age-Related Macular Degeneration Treatments Trials. JAMA Ophthalmol. 2016;134(6):674-681 Dakin HA, Wordsworth S, Rogers CA, et al. (IVAN Study Investigators). Cost-effectiveness of Ranibizumab and Bevacizumab for AgeRelated Macular Degeneration: 2-year Findings From the IVAN Randomised Trial. BMJ Open. 2014;4(7):e005094. Abraham P, Yue H, Wilson L. Randomized, Double-Masked, Sham-Controlled Trial of Ranibizumab for Neovascular Age-Related Macular Degeneration: PIER Study Year 2. Am J Ophthalmol. 2010;150(3):315-324.e1. Chen S-N, Cheng CK, Yeung L, et al. One-year real-world outcomes of ranibizumab 0.5 mg treatment in Taiwanese patients with polypoidal choroidal vasculopathy: a subgroup analysis of the REAL study. Int J Ophthalmol. 2018; 11(11): 1802–1808.
WOC2020 Virtual® was great but we can’t wait to return to physical conferences.
See you at WOC in Melbourne 2022!
APAO 2019 Bangkok, Thailand



APAO 2019 Bangkok, Thailand

AAO 2019, San Francisco, Calif., USA


DOSCON 2019 New Delhi, India
ASRS 2019 Chicago, Ill., USA ARVO 2019 Vancouver, Canada


APVRS 2019 Shanghai, China


New Insights into Glaucoma Genetics
by Hazlin Hassan
While glaucoma is a leading cause of blindness for people over 60 years old, blindness from glaucoma can often be prevented with early treatment. And with new insights in glaucoma genetics today, this could alter the way the disease is diagnosed and treated in the future. Speakers discussed how genetics can affect one’s glaucoma risks during a session on the final day of the 37 th World Ophthalmology Congress (WOC2020 Virtual®).
Family is thicker than water
Primary angle closure glaucoma (PACG) is an important cause of glaucoma worldwide, especially in Asia, where it reportedly affects more than 20 million people. Researchers have discovered that siblings are at risk of angle closure.
“In Singaporean Chinese, the sibling recurrence risk for having narrow angles is 49%. If one has PACG, there is almost a 50% chance that the sibling has narrow angles,” Prof. Tin Aung, from the Singapore National Eye Center, Singapore, explained to delegates.
The sibling relative risk is 7.6, so if one has PACG, a sibling has almost 8x greater risk of narrow angles compared to the general population. There were also similar findings in South Indians, where there is a family history of predisposing risk factors.
The prevalence of angle closure among first degree relatives of subjects with ACG was higher than the general population. Caucasians had 1-12% higher risk than the general population while Inuits had 3.5 times greater risk of
developing the disorder compared with the general population.
Sample collections were taken from around the world for a PACG Genomewide association study (GWAS). However, genes identified from GWAS only explain less than 10% of the genetic basis of ACG and cannot explain racial differences in ACG prevalence as there is currently a small number of non-Asians in GWAS so far.
Genetics and glaucoma care: now and into the future
Genetic testing can be useful for patients with early-onset disease, said Prof. Janey Wiggs of Harvard Medical School, United States. It helps to inform genetic counseling, and can identify people at risk, allowing for early treatment. “Some early onset glaucoma genes are emerging as targets for novel therapies,” she said. Genetic testing for early-onset glaucoma targets patients or their family members with disease onset before age 40.
Adult onset glaucoma is inherited as a ‘complex’ trait. Polygenic risk scores can identify people at high genetic risk for POAG to improve surveillance and treatment, and potential for screening, she said. In the future, more work is needed to know more about early onset glaucoma, to identify new genes and disease-causing mutations, she concluded.
Links between POAG and Alzheimer’s disease
Recent work by the International Glaucoma Genetics Consortium (IGGC) has shown that POAG and Alzheimer’s disease (AD), the most common cause of dementia, share joint heritability of 0.14 using LD score, said Prof. Michael Hauser of Duke University, United States.
This means that the two disorders share 14% of the genetic variants that increase risk of disease. While there has long been debate of possible links between AD and POAG, this is the first concrete evidence that both diseases show the same mechanism of neuronal cell death.
Recent studies have shown joint heritability between AD and POAG in Caucasian populations. As researchers discover shared underlying mechanisms connecting diseases, there is potential to come up with new ways in which to better treat patients suffering from these diseases.
New Insights into Diabetic Retinopathy
by Brooke Herron
Innovation is the name of the game when it comes to improving (or developing new) methods for screening, diagnosing and treating patients with diabetic retinopathy (DR).
Technology like artificial intelligence (AI) has entered our vernacular — although perhaps not our personal practice yet — and new developments in medical treatments and drug delivery devices are of keen interest for their longer lasting agents and durability.
These topics and more were covered during the New Insights into Diabetic Retinopathy session on the final day of the 37 th World Ophthalmology Congress (WOC2020 Virtual®).
Developments in screening and diagnosis
Over the past few years, new developments have risen to the surface for patients with diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR). These can be separated into several categories, according to Dr. Chaitra Jayadev from Narayana Nethralaya Eye Institute in India.
These include newer diagnostics, pharmacological treatments (both systemic and ocular), new surgical techniques and novel drug delivery systems.
Regarding newer diagnostics and automated screening, Dr. Jayadev said: “AI, as we know, is the next big thing that’s going to happen, not only in screening, but also in deciding which patient is going to need an earlier followup,” she explained, adding that ultra widefield imaging has also been helpful as a screening tool, as are imaging modalities like optical coherence tomography angiography (OCTA), sweptsource OCT (SS-OCT), enhanced depth imaging OCT (EDI-OCT) and adaptive optics (AO). Gavin Herbert Eye Institute at University of California Irvine, USA. He says he uses OCTA daily: “The images are fantastic, but I don’t always let them guide my treatment. In fact, I rarely do.” So, what is the best imaging modality for DR patients?
“OCTA is a novel and promising technique for non-invasive, non-dye based imaging of the retinal and choroidal circulation, but due to numerous limitations and artifacts, fluorescein angiography (FA) is still the gold standard for DR,” concluded Prof. Dr. Kuppermann.
Developments in treatment
Anti–vascular endothelial growth factor (anti-VEGF) therapy has replaced laser photocoagulation as the mainstay treatment for DME, said Dr. Jayadev.
And now, we have some additional data about these agents thanks to the Protocol T Extension. This study looked at the five year outcomes of bevacizumab, aflibercept and ranibizumab in order to answer the question: What happens after Protocol T patients were released from the structured study and into standard clinical care?

Dr. Jennifer Sun from the Joslin Diabetes Center at Harvard Medical School, USA, presented the results. It was found that after leaving the study, 95% of patients received retinal care and 68% received at least one intravitreal injection. They reported that on average, patients demonstrated visual acuity gains from baseline, but mean VA worsened between years 2 and 5. She also noted there was no change to central subfield thickness from years 2 to 5.
“These results differ from prior clinical trials in DME that have demonstrated better maintenance of visual gains. Protocol T clearly demonstrated much better maintenance than what we saw in this extension study,” said Dr. Sun. “This suggests the need for strategies to improve long-term visual outcomes in clinical care among eyes with DME.”
Stepping away from anti-VEGFs and advocating for vitrectomy in DME was Dr. Stratos Gotzaridis from My Retina Athens Eye Center in Greece. “The current treatments we have for DME are suboptimal. They have a short duration, they’re time consuming, they’re extremely expensive (even with regimens using bevacizumab), and they’re not completely risk free.”
Therefore, he prefers pars plana vitrectomy (PPV), which he said reduces or resolves DME in a large percentage of patients. “The sight-threatening complications of PPV are low or equal to an extended series of anti-VEGF injections,” he explained, adding that PPV also costs less and has more durable edema-resolving results.
Looking Through Therapeutic Contact Lenses
by Joanna Lee
Therapeutic contacts lenses seem to be at the cusp of a new edge with its indications for dry eyes and even for stem cell regeneration. Read on to get beyond its surface of innovations.
The bandage contact lenses
The first therapeutic or bandage contact lenses were approved for use in the United States in the 1970s. They were effective at pain management for keratopathy and surface defects. Fast forward to today, therapeutic contact lenses (TCL) are used to manage ocular surface diseases, particularly to improve epithelialization, for mechanical protection, structural support and most recently, as a means to deliver medication.
Prof. Christina Grupcheva of Medical University of Varna in Bulgaria introduced the background of therapeutic lenses, current developments and its use in general, sliding into an easy introduction to these lenses also known as bandage lenses.
Soft hydrogels were used in the past. But today, silicone hydrogel lenses are the gold standard. There are also scleral and semi-scleral lenses, cellulose lenses and biodegradable lenses. She said it’s important for lenses to be an optimal fit for the patient as well as having a wellselected diameter. These two parameters are vital for minimal mechanical impact on the ocular surface. TCL should have sufficient oxygen and stable water content. Ideally, it should have an inert structure and slow-release capability for medicines. Today, we have diagnostic lenses that are much better than disposable lenses but the new frontier belongs to TCLs with “nanotechnologies, programmed materials, and microelectronic opportunities”.
Contact lenses for dry eyes

Since dry eye was identified to increase one’s chances of dropping out of wearing contact lenses, Dr. Oliver Woo from Australia, spoke about using scleral lenses and soft contact lenses for dry eyes in his presentation titled Latest Contact Lenses Technology Can Solve My Dry Eye Problem. In speaking about scleral lenses he showed a case study example where a patient experienced all of her corneal staining and filaments resolved with daily scleral lens use. For soft contact lenses, he brought up Johnson & Johnson’s tear-infused designed Acuvue contact lenses and likens its hydrating Hydraluxe™ canal technology. Another interesting innovation is the SmarTears™ Technology (developed by Alcon) where phospholipids in the eyes are drawn out of the lens from the wearer’s tear film once he or she wears the contact lens. This technology combined with water Gradient technology gives birth to Dailies Total1® lenses. Dr. Woo summarized his segment saying advanced contact lens designs (scleral lenses) can be “primary therapy to restore ocular surface physiology back to homeostasis” besides giving patients quality of life, confidence and enjoyment.
Stem cell-carrying contact lenses
The next speaker, Prof. Sorcha Ni Dhubhghaill who is based in Antwerp University Hospital in Belgium, painted a unique and ironic situation in her presentation titled Contact Lens Carriers – Stem Cells where contact lenses which can cause limbus stem cell deficiency (LSCD) are also able to treat LSCD.
Using en vivo cultivated limbal epithelial stem cells (CLET), you can make the stem cells grow again through composite graft from the other eye. Prof. Dhubhghaill cited an Australian-based group of researchers who successfully carried out a study on using contact lenses for LSCD. 1
The next step was to introduce a xenofree 2 expansion (stem cells cultivation without using animal products). “The idea is you can avoid any possibility of disease from an animal source migrating to a human. And that in a time of COVID-19 seems to be extremely relevant,” she said.
“Using a lens as a carrier is really a simple and elegant way to avoid a lot of the surgical missteps of handling a composite graft. The cell layer can be placed exactly where you want it on the stroma and the most exciting part of this is it will likely reach the commercial markets soon,” she concluded.
Contact lens innovation beyond 2020
Lastly, Dr. John Gelles of the Cornea and Laser Eye Institute in New Jersey (USA) delved into current and future contact lens innovation. The innovations are a heady mix of surface-based lens designs, higher order aberration (HOA) correcting optics, drug-releasing lenses, wearable displays, photonics and combined extended reality lenses. One of the most impressive innovations he showed from his clinic is the impressionbased “EyePrint Prosthetics” lens for keratoconic patients. Impression based lenses also require less lenses to finalize than diagnostic lenses.
References:
1 Di Girolamo N, Bosch M, Zamora K, et al. A Contact Lens-Based Technique for Expansion and Transplantation of Autologous Epithelial Progenitors for Ocular Surface Reconstruction. Transplantation. 2009;87(10):1571-1578
2 Bobba S,Chow S, Watscon S, Di Girolamo N. Clinical Outcomes of Xeno-Free Expansion and Transplantation of Autologous Ocular Surface Epithelial Stem Cells via Contact Lens Delivery: A Prospective Case Series. Stem Cell Res Ther. 2015;6(1):23.



