

Neurological Conditions
| A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content
“Each type of dystonia has its own clinical name, making diagnosis and treatment even more complex.”
Dayna Ferdinandi, Director of Fundraising and Communications, Dystonia UK Page 04

“Brain skills are not elusive but must be fostered and strengthened critically and strategically.”
Orla Galvin, Executive Director, European Federation of Neurological Associations (EFNA) Page 06


Advancing the field of stroke and brain aneurysm therapy through innovation
Incorporating physician feedback into the stroke and brain aneurysm device innovation process can more accurately address clinical needs, explains Carsten Schroeder, President and CEO of Terumo Neuro.

Can you provide an overview of the company and conditions you treat?
Our neuroendovascular business originated as MicroVention, a California-based company acquired by Terumo in 2006. We specialise in innovative stroke and aneurysm treatment devices, offering a full portfolio of ischemic and haemorrhagic stroke solutions. Alongside our commitment to best-in-class products, we are leveraging our global infrastructure to advance neuroendovascular innovation.
How has stroke and aneurysm treatment evolved over the past 15–20 years?
In the early 2000s, the primary treatment options for brain aneurysms were surgical clipping or coiling. Over the last two decades, we’ve pioneered the development of catheter-based, minimally invasive, neuroendovascular technologies that provide therapeutic advantages for neurovascular disorders. The evolution of these minimally invasive techniques has resulted in safer, more effective treatments with fewer complications.
Our braided devices offer superior visualisation and manoeuvrability in complex anatomy for aneurysms, otherwise known as a haemorrhagic stroke. Meanwhile, innovations like the SOFIA™ catheter provide safer and more efficient treatment options for ischemic stroke.
Why are physician partnerships and innovation part of your DNA?

@Mediaplanet UK & IE
Physician collaboration is central to our innovation process. We work closely with neurovascular specialists to understand the real-world challenges they face. By integrating physician feedback into our design process, we develop devices which
accurately address clinical needs. We actively partner with physicians to provide training and education, to ensure that our products and solutions are used both safely and effectively.
Can you highlight an innovative product and its impact on patient outcomes?
The SOFIA™ catheter has set the standard in ischemic stroke treatment for over 11 years. Designed for aspiration thrombectomy, it efficiently removes clots from brain arteries, restoring blood flow quickly. The SOFIA™ catheter is now recognised globally as the gold standard in aspiration catheters.
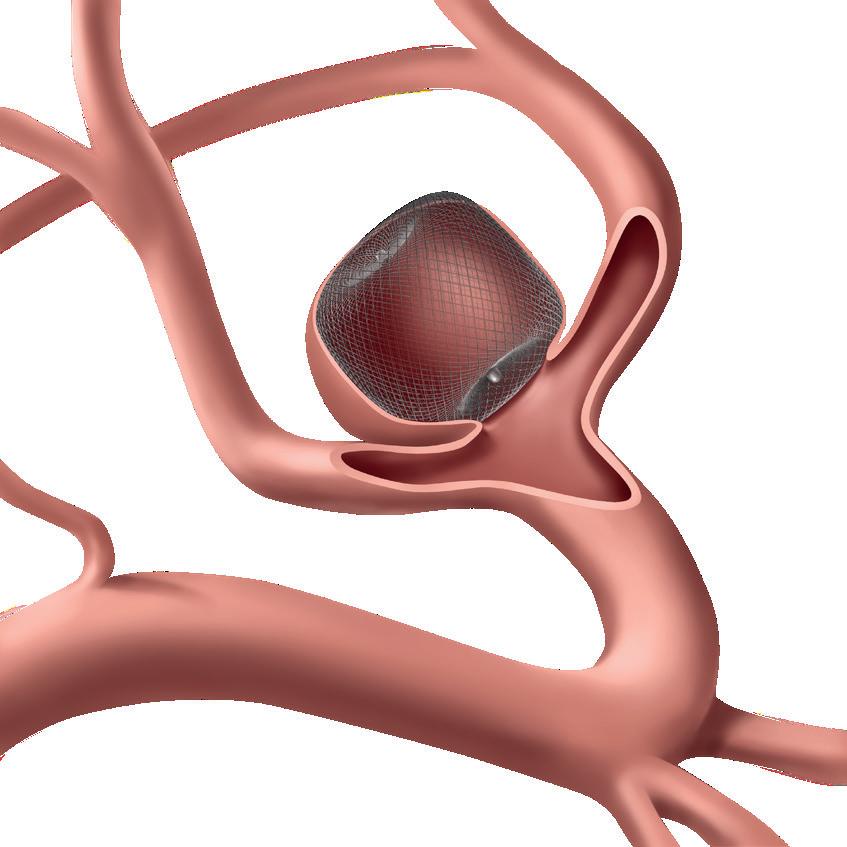
The Woven EndoBridge (WEB™) device, a novel intrasaccular implant, has simplified the treatment of intracranial and bifurcated brain aneurysms in haemorrhagic stroke care. By eliminating the need for adjunctive devices and open brain surgery, the device has a proven track record of low complication and rebleed rates.
What are the future priorities for your company in neurological health?
We are constantly evolving with our innovations. We are expanding into new areas, including middle meningeal artery embolisation and liquid embolics for chronic subdural haeomatomas. Additionally, research explores venous stenting for conditions like tinnitus and hydrocephalus treatment through endovascular approaches. In neuro-oncology, we are developing embolic solutions to improve tumour treatment. We continue to focus on generating clinical data to advance neurointervention and are open to working with external companies to develop new neuroendovascular technologies using our global infrastructure.
Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737 @MediaplanetUK Please recycle
Project Manager: Caitlin Piper caitlin.piper@mediaplanet.com Business Development Manager: Jack Adamson Managing Director : Ellie McGregor | Junior Designer: Ellen Cahill Senior Content Manager: Angelica Hackett O’Toole | Paid Media Strategist: Jonni Asfaha Social & Web Editor: Henry Phillips | All images supplied by Getty Images, unless otherwise specified
National and international collaboration to improve life after stroke
There have been major advances in the treatment of stroke. Drugs and procedures administered in the first hours following a stroke can be life-saving and life-changing.

Stroke (an interruption of the blood supply to the brain) is a devastating condition and the most common cause of death and disability in the world.
Improving life after stroke
Stroke research has tended to focus on these precious first hours, but for stroke survivors, there is a whole life after the initial stroke. This area has been traditionally underresearched; there are many unanswered questions around longer-term stroke recovery.
Professors Jesse Dawson and Terry Quinn, both doctors and researchers from the University of Glasgow, are working to improve life after stroke. They work together but focus their activities on different aspects of stroke recovery.
Reviving movement post-stroke
Prof Dawson is passionate about improving the movement and function that can be taken away by stroke. His research has used medications, robots and devices. He was part of the team that first showed how electronic nerve stimulation, alongside physical therapy, can restore strength and dexterity in stroke survivors, even years post-stroke. His research is giving hope to many people left with long-term physical issues following a stroke.
Brain health and stroke
Prof Quinn and his team have an interest in the memory, thinking, and mood problems that can follow a stroke. Although conditions like stroke, dementia and depression
are all ‘brain diseases,’ clinical practice and research have tended to treat them as separate issues.
Their research shows that the conditions are closely linked. For example, one in three stroke survivors are living with dementia, and there is a one-in-three chance that a stroke survivor will experience major depression. Having identified the overlap, potential treatments that could be useful for all three conditions are in development.
Supporting stroke recovery
Stroke recovery is too big an issue for one (or two) researchers to tackle alone. Professors Dawson and Quinn proudly partner with stroke teams across Europe and beyond. The European Stroke Organisation (ESO) is the voice of stroke clinicians and researchers across Europe. ESO is working on several issues related to life after stroke.
Action plan for Europe
Both professors play important parts in ESO; Prof Dawson is treasurer and member of the executive committee, while Prof Quinn chairs the production of clinical guidelines. Through this triple-helix of research, clinical practice and international policy, we can look forward to continuously improving life after stroke.
Source: European Federation of Neurological Associations. 2024. EFNA Survey: The Invisible Issues of Neurological Conditions.

INTERVIEW WITH Carsten Schroeder
WRITTEN BY Bethany Cooper
Time is brain: leader in stroke and brain
aneurysm medical device innovation
Global neuroendovascular innovation
leader urges, ‘Time is brain,’ developing groundbreaking ischemic stroke and brain aneurysm medical device technology deeply rooted in clinical evidence and physician collaboration.
Amplified by the American Stroke Association, the globally recognised acronym F.A.S.T. (Face drooping, Arm weakness, Slurred speech, Time to call emergency services) was created to ensure a speedy and effective response for people experiencing a stroke. While the tool is widely used to facilitate the identification of stroke symptoms, it also underscores the urgency of seeking immediate treatment. T = Time, and ‘Time is brain,’ explains Nagesh Uppuluri, Senior VP of Global Clinical and Medical Affairs at Terumo Neuro. “Millions of neurons die every minute during stroke, which could result in irreversible damage; every minute counts.”

Development of neurovascular technology
This race against time is not only
ImageprovidedbyTerumo Neuro
facilitating speedy access to primary care, but it is driving the development of quick, effective and minimally invasive devices designed to enhance treatment outcomes. Terumo Neuro is globally known for medical device innovations that redefine what is possible in neuroendovascular treatment to meaningfully advance both physician practice and patient outcomes.
“Over the last 15–20 years, we have seen a rapid rate of technological innovation within the neurovascular space. Devices used to treat aneurysm and stroke are becoming more precise, minimally invasive, less traumatic, safe and improving outcomes,” says Uppuluri. “In the past, coils were the primary method for treating brain aneurysms, but with the introduction of devices like the FRED™ X™ flow
diverter, we are now able to treat the underlying disease mechanism — not just the rupture risk.”
Terumo Neuro’s FRED™ X™ flow diverter sits within a wide portfolio of products that continue to set the standard for neuroendovascular care, including the SOFIA™ catheter and the Woven EndoBridge (WEB™) device.
Evidence-based innovation
Setting themselves apart through evidence-based innovation, Terumo Neuro is dedicated to generating the clinical data needed to bring neuroendovascular products to market. Uppuluri says: “Clinical evidence instils trust in both physicians and patients, ensuring that devices are not only safe but also effective at improving outcomes.” Working alongside clinicians to accurately address real-world clinical needs, the company’s commitment to innovation in neurovascular technology is contributing to the improvement of global patient outcomes.
“Stroke was once one of the leading causes of death and disability, but thanks to this improved technology and clinical advancements, we’re seeing a slight reduction in its burden. However, there is far more work to be done to make a significant impact, thus our continued commitment to innovation in this area,” he explains. “The clinical evidence we have today shows that many patients can live disability-free lives after stroke treatment, which is an incredible achievement that is giving people back their pre-stroke quality of life.”


INTERVIEW WITH Nagesh Uppuluri Senior Vice President, Terumo Neuro
BY Bethany Cooper

BY Stefan König CEO, Merz Therapeutics
Global partnerships and patient-centricity fuelling neurological innovation
Neurology-focused pharmaceutical company accelerates research into neurological treatments with equitable access.
Medical innovation is accelerating at an unprecedented scale.
Harnessing the full ecosystem of patients, caregivers, clinicians and payors is quickly becoming an essential component in the development of treatments that are not only effective but practical and accessible.
Ecosystem of neurological product development
Stefan König, CEO of Merz Therapeutics, discusses the importance of this for product development. “The patient is our north star, meaning our approach to innovation is always guided by the question: what does this bring to the patient?”
He cites the example of a Parkinson’s disease product, where patients often struggle with fine motor skills.
“With this in mind, we developed easy-peel packaging that allows medication to be accessed more easily,” explains König. “We develop solutions with a 360-degree approach, consulting clinician and patient advisory boards before moving into practical development while collaborating with payors to ensure broad access and quick delivery to patients.” This approach aims to centre each step of design with real patient challenges in mind.
Balancing heritage with driving innovation
Merz Therapeutics is a company of the Merz Group, a privately held, family-owned German company founded by Friedrich Merz. Grounded in more than 115 years of health and innovation expertise, the company
has evolved to become a global leader in neurological solutions and neurotoxin therapy.
“Our heritage provides a strong foundation for continued adaptation and growth,” explains König.
“We combine innovation, patient centricity, agile long-term decisionmaking and a strategic investment approach to ensure our company is future-proofed and well-positioned for sustainable growth.”
Beyond product development, they offer a number of digital health solutions, with nurse-led patient support programmes guiding patients in the management of complex neurological conditions.
The role of strategic partnerships
With an array of global partnerships, including esteemed research institutions and universities, the company continues to lead the development of patient-led solutions.
“Being a mid-sized organisation allows us to stay close to patients and better understand disease areas that may be too small for big pharma companies to address while maintaining the ability to propel neurological innovation on a global scale,” explains König.
“Our research centre in Frankfurt has over 160 research scientists from approximately 12 different nationalities. By combining in-house expertise with innovative ideas from smaller biotech companies, we help bring personalised therapies to market,” he adds. “We hope to continue partnering with clinicians, patient organisations and biotech companies to drive neurological innovation for many generations to come.”

Dystonia signs, symptoms and how to get help in the UK and beyond

Dystonia is a neurological movement disorder affecting over 100,000 people in the UK, yet so few have heard of it. We aim to change that.
What is dystonia?
Dystonia is a neurological movement disorder. However, there is so much more to this often misunderstood condition. Dystonia causes uncontrollable muscle spasms, triggered by incorrect signals from the brain. These spasms can be painful and debilitating. Dystonia is the third most common movement disorder in the UK, yet awareness remains low. It can affect any region of the body — including the eyelids, face, jaw, vocal cords, torso, limbs, hands and feet — and presents differently depending on the area affected.
Each type of dystonia has its own clinical name, making diagnosis and treatment even more complex. Sadly, long waiting times and frequent misdiagnoses mean people can go years without answers, often enduring an immense emotional toll alongside their physical symptoms.
Providing support and understanding
At Dystonia UK, we know the struggle of living with dystonia goes far beyond the physical. When you’re facing a condition so few understand, it can feel incredibly isolating. That’s why we’re dedicated to creating a community where no one feels alone.
Our nationwide support groups provide a safe space to share experiences, receive practical advice and connect with others who truly understand the challenges of dystonia. We also host community events across the UK, bringing people together in solidarity while raising awareness and offering opportunities to meet healthcare professionals and experts.
Raising awareness through creativity
Education is key to understanding dystonia. That’s why we’ve developed animations to help explain the condition in clear, engaging ways, making it easier for patients, families and professionals to grasp the complexities of dystonia. Our podcast also shares personal stories from those living with the condition, reminding listeners that they are never alone.
Join the community
On our website, explore FAQs, webinars, podcasts, animations and more. Together, we aim to build a future where no one has to ask, ‘What is dystonia?’ — because everyone will already know.

WRITTEN
WRITTEN BY Dayna Ferdinandi Director of Fundraising and Communications, Dystonia UK
WRITTEN BY Bethany Cooper
Discover cervical dystonia with key insights from the patient journey map
Cervical dystonia affects daily life in significant ways. Understanding the patient journey helps improve care, support and awareness of this condition.

Living with dystonia presents unique challenges, making it essential to understand the patient’s journey for better care and support. In collaboration with the European Reference Network for Neurological Diseases (ERN-RND) and with support from Ipsen, Dystonia Europe has developed the Cervical Dystonia Patient Journey to highlight the experiences of individuals affected by this condition.
What is cervical dystonia?
Dystonia is a movement disorder characterised by sustained or intermittent muscle contractions, leading to abnormal, often repetitive movements or postures. Cervical dystonia (CD) is the most common form of focal dystonia in adults, typically beginning between ages 30 and 50 and progressively worsening over five years. This painful condition causes involuntary neck muscle contractions, leading to the head twisting, tilting or turning uncontrollably.
The role of patient journeys
Development of the patient journey map
To develop the CDPJM, a survey was conducted with 15 individuals affected by cervical dystonia, followed by validation through an expert-patient focus group. Qualitative analysis identified five key stages of the patient journey: (1) symptom onset; (2) diagnosis and therapeutic relationship with healthcare professionals (HCPs); (3) initiation of care for cervical dystonia; (4) start of treatment; (5) living with treated cervical dystonia.
Designed from the patient’s perspective, these journeys help clinicians address care gaps effectively.
Patient journeys serve as infographic tools that visualise patients’ needs throughout their rare disease care. Designed from the patient’s perspective, these journeys help clinicians address care gaps effectively. The Cervical Dystonia Patient Journey Map (CDPJM) provides a comprehensive view of the patient experience, spanning pre-diagnosis to long-term treatment.

CWithin these stages, gaps in care and barriers to treatment were identified. The Patient Journey Map highlights critical updates needed in healthcare systems, including improved communication, accessible highquality information and clear treatment pathways.
Emphasising needs of the dystonia community
By understanding the dystonia patient journey, we can enhance early detection, improve access to specialised care and optimise treatment approaches. Our goal is to empower individuals with dystonia, equip healthcare providers with valuable insights and advocate for policies that prioritise the needs of the dystonia community.
Living with cerebral palsy and why society’s perception needs to change
Cerebral palsy (CP) is a lifelong condition affecting movement and muscle control. Despite its prevalence, it remains overlooked and misunderstood.
erebral palsy (CP) is caused by an issue with the brain that develops before, during or soon after birth. It is a condition that affects muscle control and movement. It is the most common lifelong motor disability in the world.
With numbers in the UK similar to that of people living with multiple sclerosis and Parkinson’s, CP does not receive the same attention and is only just being seen as a life-long condition. Some of the main challenges are the archaic and pejorative attitudes attached to CP.
Lack of cerebral palsy support harms adulthood
Combatting negative attitudes is difficult, even within the healthcare system. Adults with CP live on a precipice. While many of us receive extensive care as children, that support abruptly ends at 18. The narrative is often “this is as good as it gets.” This leaves individuals to navigate adulthood without the care or resources they need.
Scope’s CP Network and Online Community seek to provide that support. Without adequate care, people with CP can experience premature ageing. This can lead to experiencing an increase in pain
and a decline in mobility, which can then restrict life choices and social participation.
Disabling societal prejudices
We are far more disabled by society’s attitudes than by our condition itself. Being denied access simply because we ‘look drunk’ — judged not for who we are, but for how we move or sound. Plus, there’s the constant disbelief: ‘You can’t have CP; you look fine.’ Since when did appearance determine diagnosis? It may surprise some to learn that a large percentage of people with CP can walk unaided. Our community is diverse, with a wide range of needs, and it’s time that was properly recognised.
Growing cerebral palsy representation
Despite the challenges I witness daily in my work with Scope’s CP Network, I remain optimistic. There is a positive shift occurring within the CP community. Representation of CP is becoming more visible in mainstream media, from shows like The Traitors to Sex Education. These portrayals help dismantle misconceptions and highlight the diverse experiences of those living with CP.

WRITTEN BY Lucy Hindmarch Cerebral Palsy Specialist, Scope UK
WRITTEN BY Monika Benson Executive Director, Dystonia Europe
Stroke research has tended to focus on these precious first hours, but for stroke survivors, there is a whole life after the initial stroke.
~Professor Jesse Dawson, Treasurer of the European Stroke Organisation & Professor of Stroke Medicine, University of Glasgow
Page 02

Brain skills empowering the neurology patient community

Empowering neurology patients and caregivers to live optimally is facilitated by an understanding and harnessing of the value of a brain-positive economy.
The societal and economic impact of living with a neurological condition is vast. For those in the neurology community, the profound impact of both visible and invisible aspects of living with a neurological condition on employment and financial stability is all too familiar.
Challenges facing the neurology patient community Beyond the symptoms, individuals and families grapple with numerous challenges, including access to healthcare. EFNA’s 2022 report ‘Socioeconomic Impact of Neurological Conditions’ reports the following:
• 69% of people miss days off work
• 76% experienced a negative impact on relationships with colleagues
• 83% experienced a negative impact on their finances
• 85% experienced a negative impact on their relationship with friends
• 86% experienced a negative impact on their relationship with family
• 94% experience a negative impact on their social life
A brain-positive economy
Brain capital prioritises brain skills and brain health — both of which are increasingly valuable in our innovation and knowledge-driven, postcovid economies. With advances in the AI and technologies sector, adaptation and development of brain skills are critical to preserving human employment and regional income (Eyre et al, 2021; Cell Press; NeuroView, Building brain capital).
What do we mean by brain skills?
Brain capital can ultimately improve the quality of life of those affected.
• 99% experience a negative impact on their overall wellbeing
Brain capital opportunity
Under the umbrella of ‘brain capital’ neurology, patient advocates, patient organisations, individual patients and caregivers can advocate and influence change — not only in themselves but also to support research and innovation, access to therapeutics, services and supports.
Brain capital can ultimately improve the quality of life of those affected (patients and caregivers). This, in turn, serves as a foundation for benefits to healthcare systems and the employment sector.
Brain skills are not elusive but must be fostered and strengthened critically and strategically. Many individuals facing the challenges of living with a neurological condition are not only surviving but also striving to thrive. Necessity drives them to navigate life with brain skills such as resilience, innovation, imagination, improvisation, critical and analytical thinking, communication, curiosity, creativity, exploration, goal engagement, systems thinking, motivation and opportunity recognition.
Brain skills such as compassion, altruism, emotional intelligence, mindfulness and self-control also manifest in caregivers of individuals with a chronic neurological condition. Seize the opportunity — you own your brain capital.

WRITTEN BY Orla Galvin Executive Director, European Federation of Neurological Associations (EFNA)

Navigating life after stroke and the road to recovery
Life after a stroke is a lifelong journey. With the right care and support, survivors can rebuild their lives and regain independence.

Stroke is one of the leading causes of death and disability worldwide. Each year, nearly 1.5 million people suffer a stroke in Europe. It can be devastating and deeply affects survivors and their families. Today, more than 9 million people across Europe are living with the long-term health, social and financial impacts of stroke.
Stroke prevention and early action save lives
Fortunately, many strokes are preventable. Common risk factors like high blood pressure, smoking, obesity and lack of exercise all contribute to stroke risk. The Stroke Alliance for Europe (SAFE) recently launched StrokePrevention.org, which highlights the power of healthy lifestyle changes, regular health checks and early intervention to reduce the chances of a first or second stroke. It also outlines what governments should be doing to create healthier environments that protect brain health.
Acting quickly when a stroke happens can save lives and improve recovery. The F.A.S.T. test — Face (drooping), Arms (weakness), Speech (slurred), Time (act fast) — helps people spot the signs and seek urgent medical attention. Fast treatment in a specialist stroke unit gives people the best chance of survival and reduces the risk of long-term disability.

Stroke rehabilitation and support
For many, the effects of stroke continue long after leaving hospital. Survivors often face ongoing physical, emotional and mental health challenges. Access to rehabilitation services, peer support and strong networks are essential to recovery and rebuilding independence.
The European Life After Stroke Forum, led by SAFE, brings together healthcare professionals, researchers and stroke survivors to improve post-stroke care. Patient organisations also play a vital role, providing peer support, counselling and rehabilitation services to help reduce isolation and support mental wellbeing.
Long-term management for stroke survivors and carers
The Stroke Action Plan for Europe, developed by SAFE and the European Stroke Organisation, aims to improve prevention, care and long-term support. It aims to ensure all stroke survivors — and their carers — have access to highquality rehabilitation and ongoing support. Stroke is not just a medical emergency; it is a lifelong journey. With the right support, survivors can rebuild their futures.
WRITTEN BY
Arlene Wilkie Director General, Stroke Alliance for Europe (SAFE)
Adults with CP live on a precipice. While many of us receive extensive care as children, that support abruptly ends at 18.
Lucy
Hindmarch, Cerebral Palsy Specialist, Scope UK
Page 05

What people affected by Parkinson’s can do now to access healthcare and support

Parkinson’s is the fastest-growing neurological condition, affecting 153,000 people in the UK. With over 40 symptoms that evolve, each person’s experience is unique, and there is currently no cure.
Receiving the right care from health professionals following a diagnosis is important to ensure symptoms are well managed.
Types of Parkinson’s professionals
A Parkinson’s healthcare team comprises a variety of healthcare professionals from GPs and Parkinson’s nurses to pharmacists and specialist therapists, such as physiotherapists. Each expert will have a different role to play in helping someone with the condition manage their symptoms.
However, understanding which services could benefit you, and navigating the system can be challenging for many people. Below are three ways people with Parkinson’s and their loved ones can help manage symptoms and access healthcare.
A Parkinson’s healthcare team comprises a variety of healthcare professionals.
1. Do your research
Knowing the condition and how it affects you will help you better understand and manage your symptoms and healthcare. Whether you have Parkinson’s or support someone with the
condition, Parkinson’s UK offers a number of resources on its website and in printed guides. Find out more about who can help and what is available at parkinsons.org.uk/health-team
2. Reach out for support Parkinson’s UK offers in-person, online and helpline support for people living with Parkinson’s, their loved ones and carers. It has a team of 90 local advisers that can offer support, wherever you live in the UK. It also has a confidential helpline (0808 800 0303), which is free to call.
You can speak to an expert about which health professionals can help, the type of healthcare and support you should be getting and what to do if you’re having problems in your area.
3. Managing your condition
There are lots of things you can do to help manage your Parkinson’s — from doing regular physical activity and maintaining a healthy, well-balanced diet to joining local groups and connecting with others. Remember, no matter what stage you are at in your Parkinson’s journey, Parkinson’s UK has people and services to help you.

