
87 minute read
tCMs In aCtIon
MetroDoctors Doctors
THE JOURNAL OF THE TWIN CITIES MEDICAL SOCIETY
Advertisement
Physician Co-editor Peter J. Dehnel, MD Physician Co-editor Thomas E. Kottke, MD Physician Co-editor Robert R. Neal, Jr., MD Physician Co-editor Marvin S. Segal, MD Physician Co-editor Richard R. Sturgeon, MD Medical Student Co-editor Zineb Alfath Medical Student Co-editor James Pathoulas Managing Editor Nancy K. Bauer
Production Manager Sheila A. Hatcher Advertising Representative Betsy Pierre Cover Design by Annie Krapek
MetroDoctors (ISSN 1526-4262) is published bi-monthly by the Twin Cities Medical Society, Broadway Place West, 1300 Godward Street NE, Suite 2000, Minneapolis, MN 55413. Periodical postage paid at St. Paul, Minnesota. Postmaster: Send address changes to MetroDoctors, Twin Cities Medical Society, 1300 Godward Street NE, Broadway Place West, Suite 2000, Minneapolis, MN 55413.
To promote its objectives and services, the Twin Cities Medical Society prints information in MetroDoctors regarding activities and interests of the society. Responsibility is not assumed for opinions expressed or implied in signed articles, and because of the freedom given to contributors, opinions may not necessarily reflect the official position of TCMS.
Send letters and other materials for consideration to MetroDoctors, Twin Cities Medical Society, Broadway Place West, 1300 Godward Street NE, Suite 2000, Minneapolis, MN 55413. E-mail: nbauer@metrodoctors.com.
For advertising rates and space reservations, contact: Betsy Pierre phone: (763) 295-5420 e-mail: betsy@pierreproductions.com
MetroDoctors reserves the right to reject any article or advertising copy not in accordance with editorial policy. Advertisements published in MetroDoctors do not imply endorsement or sponsorship by TCMS.
Non-members may subscribe to MetroDoctors at a cost of $15 per year or $3 per issue, if extra copies are available. For subscription information, contact Nancy Bauer at (612) 623-2893.
TCMS Officers
President: Ryan Greiner, MD President-Elect: Sarah Traxler, MD Secretary: Andrea Hillerud, MD Treasurer: Rupa Polam Austria, MD Past President: Thomas E. Kottke, MD At-large: Matthew A. Hunt, MD
TCMS Executive Staff
Ruth Parriott, MSW, MPH, CEO (612) 362-3799; rparriott@metrodoctors.com
Nancy K. Bauer, Associate Director, and Managing Editor, MetroDoctors (612) 623-2893; nbauer@metrodoctors.com
Kerry Hjelmgren, Executive Director, Honoring Choices Minnesota (612) 362-3704; khjelmgren@metrodoctors.com
Lynn Betzold, Program Coordinator, Honoring Choices Minnesota (612) 362-3703; lbetzold@metrodoctors.com
Annie Krapek, MPH, Senior Project Manager (612) 362-3715; akrapek@metrodoctors.com
Amber Kerrigan, Program Coordinator (612) 362-3706; akerrigan@metrodoctors.com
Kate Feuling Porter, MPH, Program Manager (612) 362-3724; kfeuling@metrodoctors.com
Nov/Dec Index to Advertisers
COPIC .................................................................21
Crutchfield Dermatology..................................... Inside Front Cover
Deaf and Hard of Hearing Services............... 2
Lakeview Clinic .................................................27
MagMutual........................Outside Back Cover
MedCraft .............................................................13
MedPro Group..................................................... 9
M Health Fairview............................................27
North Memorial ................................................24
Physicians Wellness Collaborative................21
PNC Bank .............................Inside Back Cover
Schuster Clinic...................................................23
Do your patients have trouble using the phone due to a hearing loss, speech or physical disability?

The Telephone Equipment Distribution Program offers easier ways to use the phone. Phone: 800-657-3663 Email: dhs.dhhsd@state.mn.us Web: mn.gov/deaf-hard-of-hearing

The Telephone Equipment Distribution Program is funded through the Department of Commerce – Telecommunications Access Minnesota (TAM) and administered by the Minnesota Department of Human Services.
Recognizing Our Local COVID-19 Heroes
Without doubt, the phrases, “then everything changed forever,” or “the new normal” have been overused, but I don’t believe that’s the case with COVID-19. When writing this column in late September, the headline on the Star Tribune shouted, “State’s COVID-19 spread now rated ‘uncontrolled.’” By mid-October, Minnesota reported over 106,000 cases of COVID-19 and more than 2,100 deaths. Despite the United States having only 4% of the world’s population, it has 20% of the world’s deaths from COVID-19. This is despite having the most resources, the best medical technology, and both the NIH and CDC. The lack of Federal leadership and political posturing closer to home was not helpful. However, Twin Cities doctors are not bystanders. They are fighting COVID-19 in novel ways, and we’ve collected a few of their stories; here’s a sneak peek. Dr. Nathan Chomilo, provides clinical care in the Northwest suburbs and stepped up as Medical Director for the Minnesota Department of Human Services. Our Colleague Interview foretells of even greater things to come from him. Unable to buy a disposable gown, Dr. Kevin Wang, at the University of Minnesota, organized a team to design and produce one. By mid-June they had produced 30,000. COVID-19 didn’t stop FUHN’s (Federally Qualified Health Center Urban Health Network) hypertension control program. They transitioned more than 80% of appointments to virtual care. Dr. William Walsh, a facial and plastic surgeon at Hennepin Healthcare, is championing a new model of housing so that patients don’t need to go back to the street. He attributes his success to collegial relationships created with individuals who have lived the experience of homelessness. An epidemic of measles was a real threat if childhood immunization programs were disrupted by COVID-19. Children’s Minnesota created a solution outside the exam room. We’ve all seen the massive lines of cars waiting for food. North Memorial Health is doing better than that, taking
By Thomas E. Kottke, MD Member, MetroDoctors Editorial Board to the streets with its Food as Medicine Program they launched this past July. Nearly every day the newspaper has an article about a healthcare worker who is stressed and distressed by COVID-19. Dr. Anand Shah describes how a group of physicians at HealthPartners has created an extensive menu of online psychological support tools. Over nearly 20 years, the Angel Foundation in Mendota Heights has provided more than $10 million in emergency financial assistance grants to 30,000 patients. When COVID-19 hit, they launched a new program, Angel in Action. One of your patients might be eligible. While the near record number of tropical storms coming out of the Atlantic and the fires in the West may dominate the national news, we in Minnesota are also feeling the effects of climate change. What can one person do? Read the Minnesota Declaration on Climate Change and Health, and then sign up for Xcel Energy’s Windsource® renewable energy program. It costs just a few dollars per month to dump coal power. A group of St. Olaf College students asked their classmates, “Do you care about advance care planning?” You might not have expected the answer. I know for sure that our choice of this issue’s Luminary will surprise you—medical students! And, it will give you hope for the future. As soon as COVID-19 disrupted their hospital rotations University of Minnesota medical students organized themselves into MN Covidsitters. They serve anyone in health care, not just doctors and nurses, and to date have babysat for over 250 families, tended to 38 furry friends and run over 160 errands. By the time you read this issue of MetroDoctors, Minnesota will be preparing for long winter nights and the second wave of COVID-19. We at MetroDoctors hope that the vignettes in this issue bring you light and joy.

Final Thoughts on Passing the Baton…

RyaN GREiNER, MD
I never could have imagined what the last two years were going to be like when I accepted the nomination for President of the Twin Cities Medical Society. So much has changed during that time and that change continues at a pace that our profession has not experienced for generations. At times it seems the challenges we face are extraordinary, improbable and devastating. With the cultural unrest, environmental stress, income inequality, psychological trauma, economic insolvency and political inadequacy we might wonder how we got here and how we will get out of it. What will come next? What challenges are around the corner? Do we have the perseverance to manage it all? The limit of physician resilience has been and continues to be tested. It’s not just about COVID. It’s about life. It’s about the fact that our work is challenging, stressful, emotional and high stakes. It’s all these things in addition to living in an evolving world of complexity where the innate need for connection and relationship is becoming more and more difficult to maintain. And yet our communities, our patients, our families, see us as part of the foundational bedrock of normalcy, health and prosperity. Our responsibility remains extraordinary, yet our basis will always remain human, with the same inadequacies, challenges, struggles, aspirations and dreams that all people share. The physician community must continue to grow closer, more integrated and more aligned. We need to regain our collective voice in our work, our communities, our politics and our futures. We need to revisit our connections to each other, expand them and foster their growth. We need to remain organized and deliberate, lest we lose our collective ethos to ordinary and uninspired. Passion must always remain our foundation, and care for the person our mission. Passing the baton of the presidency to Dr. Sarah Traxler inaugurates a physician who works on the frontlines of advocating for the rights of women. She is passionate, has foresight and integrity and is an advocacy leader. As I look back on the past two years I am humbled to have worked with the incredible professionals at the medical society to advance the cause of physician well-being. The story is still being written, our story, one that we can chose to write together or allow to be written for us. Let’s not lose sight of our responsibility for our futures and embrace the opportunities that are yet to come. Our future is bright and hopeful. It’s full of opportunity, excitement and adventure. There is joy and celebration every day and at every moment. It is these moments that invite our attention and appreciation. Those moments where we provide comfort to a dying patient. Those moments where we eradicate the cancer from the body of a person and restore their aspirations, hopes and dreams for the future. Those moments where we bring new life into the world and ignite the hopes and dreams of new parents. Life is certainly full of pain, suffering and disappointment, but it also full of unimaginably profound connection, joy and happiness. Thank you for joining your colleagues at TCMS on this ongoing journey and thank you for supporting us in the work that we do.
RUTh PaRRiOTT, MSW, MPh, CEO
Groundbreaking Oncologist Receives Award
The TCMS Foundation Board of Directors has had the distinct honor of selecting and awarding the Charles Bolles Bolles-Rogers Award to a “physician of excellence” since 1952. Nominated by his peers at the University of Minnesota, Daniel J. Weisdorf, MD was chosen as the 2020 recipient.

in September. All 30 fellows logged into Zoom, equipped with snacks and visual tools delivered to their homes. As fellows displayed thought bubbles with their wishes for the program, the word “community” was chosen most frequently.

As a hematologist-oncologist, Dr. Weisdorf is internationally known for his research on small cell transplantation with a focus on graft versus host disease, with over 700 manuscripts published on this topic. In 2013, as Chief of the Division of Hematology, Oncology and Transplantation at the University of Minnesota, he brought these specialties together under one division—a remarkable undertaking that continues as the only combined division within the department of medicine in the country yet today.
Medical Student Advocacy Comes Alive (Virtually)
An essential ingredient of TCMS’s medical student advocacy fellowship is connection: with mentors, with each other, with other professionals in coalitions seeking change. If there were any doubt that connection could be established despite the need for social distancing, it was quickly dispelled at the kick-off workshop The training session utilized the analogy of the fertile community soil necessary for the seeds of change to grow, and how advocates can nourish and support that soil. Live commentary was provided by Ricardo Levins Morales, a renowned social justice activist and artist who brings the soil analogy to life in his paintings. His words of encouragement and challenge to achieve health equity were as inspiring as his artwork.
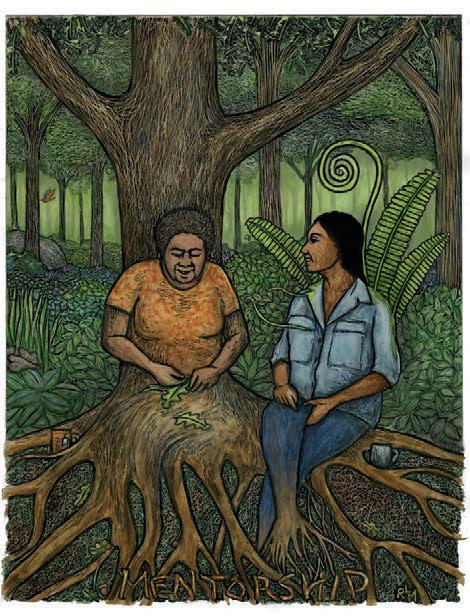
“Mentorship” by Ricardo Levins Morales— rlmartstudio.com.

TCMS will share as much as possible from the medical students and their mentors as their commitment to justice within medicine develops more fully over the school year.
Advance Care Planning
Knowing your voice is heard when making decisions about health care is important. Advance Care Planning is the process of preparing for a time when you may not be able to make your own medical decisions. The best time to make these decisions is when you are able to make your own choices.
Health Care Agent
Discussing and sharing your wishes with your loved ones, health care team and health care agent is important. A health care agent makes health care decisions based on your wishes if you are unable to communicate.
Health Care Directive
By writing a Health Care Directive, you can make your voice heard so your wishes are followed. A Health Care Directive is a written plan outlining your values and priorities for your future medical treatment.
Advance Care Planning Information: COVID-19
Your individual health care goals, values, and preferences matter greatly if you experience severe or life-threatening illness from COVID-19. People of any age with underlying medical conditions and people over age 65 have a higher risk of developing life-threatening illness with COVID-19. Complications from this virus could render you unable to make medical decisions for yourself. Due to your specific risk factors, you may have COVID-19-specific preferences you wish to convey. Your loved ones and health care team need to know who will make medical decisions for you and how you want to be cared for if you become critically ill. This guide is intended to help you address COVID-19 as a part of your advance care planning process.The most important predictors of survival are age and pre-existing conditions.To help you determine your risk level, visit: https://www.nhpco.org/wpcontent/uploads/COVID-19-Shared-Decision-Making-Tool.pdf.
Make or Update Your Advance Care Plan for COVID-19
1) Choose and ask a trusted adult to make medical decisions for you in the event that you become unable to communicate(this person is your health care agent).
2) Consider potential options for treatment, care, and support if you were to contract
COVID-19:
Hospitalization
Would you prefer to receive care in a hospital or at home? If you prefer to receive care in the hospital, do you wish to receive intensive care and CPR (cardiopulmonary resuscitation) as attempts to prolong your life? If you prefer to receive care at home, do you wish for skilled symptom management focused on comfort?
Oxygen Support
If recommended by your health care team, would you accept oxygen support? Oxygen treatment involves inhaling oxygen through a tube in your nose or mask over your mouth.
Mechanical Ventilation
Lungfailure is the main cause of deathfrom COVID-19. If you become critically ill, aspecialized team will determine if you are eligible for a ventilator, if one is available. Aventilator is amachine that pushes a mixture of air and oxygen in and out of your lungs to breathe for you. The machine connects to a tube that goes through your mouthand down your windpipe at the back of your throat. Inserting this tube down yourwindpipe is called intubation. When the tube is in place, you cannot talk orswallow. You will receive medicine to help stay calm while the tube is in place. Being on a ventilator requires care in the Intensive Care Unit (ICU) at the hospital. Early studies suggest that individuals placed on a ventilator for COVID-19 will likely require lengthy mechanical ventilation, and the risk of deathincreases the longer individuals areon a ventilator. If the ventilator does notimprove your condition or your condition worsens, you will be assessed to see whether the ventilator can still help you. It may be decided that the ventilator will no longer help you, so the breathing machine may be stopped. You will be kept comfortable during this process, and the focus of your care will be managing your symptoms and providingcomfort.If you have concerns aboutventilator use based on your current health, contact your health care provider.
Medications
Medications are used to provide sedation while on a ventilator or to provide symptom management. These symptoms may include: pain, shortness of breath, anxiety, nausea, and others. If you have concerns about specific medications used for treatment, talk with your health care provider and share with your health care agent.
Honoring Choices and COVID-19
The Honoring Choices program continues to meet the increased demand for advance care planning guidance, particularly with decisions related to COVID-19 acute care. It is notable that 31% of directives downloaded from the website are in languages other than English, a resource even more vital with the disparities revealed by the pandemic. Please see bit.ly/ HCMcovid-19 for the newly updated COVID-19 guide for advance care planning.
Colleague Interview: A Conversation with Nathan T. Chomilo, MD
Dr. Nathan T. Chomilo is Medical Director for the State of Minnesota’s Medicaid and MinnesotaCare programs and practices as a General Pediatrician and an Internal Medicine Hospitalist with Park Nicollet Health Services/HealthPartners. He received his medical degree from the University of Minnesota Medical School; completed a combined residency in Internal Medicine and Pediatrics at the University of Minnesota and was the Pediatric Chief Resident at the University of Minnesota Children's Hospital. His advocacy work has included the impact early childhood intervention and healthcare access have on the long-term prospects of our children and how physicians and health systems can address racial and health equity. He is a member of the American Academy of Pediatrics Council on Early Childhood and the Section on Minority Health, Equity & Inclusion where he is currently the interim chair of the policy and advocacy workgroup, is one of the Early Childhood Champions for the MN Chapter of the AAP where he also serves on the board of directors, is an Adjunct Assistant Professor of Pediatrics at the University of Minnesota Medical School, helped start the organization Minnesota Doctors for Health Equity (MDHEQ), was formerly appointed to the Minnesota Governor’s Early Learning Council and previously served as the Medical Director of Reach Out and Read Minnesota. He is on the board of the Institute for Clinical Systems Improvement (ICSI) and the steering committee of the Minnesota Perinatal Quality Collaborative. He received the 2018 Medical Champion Achievement Award from Reach Out and Read National, and the City of Minneapolis Department of Civil Rights recognized him as a 2019 History Maker at Home recipient. did not receive clear communication delivered with cultural
You’ve been an advocate for youth literacy. Why do you believe that youth literacy should be a developmental benchmark?
It is estimated that only about 10-20% of what impacts someone’s health happens within the walls of a doctor’s clinic or hospital. Most of the remaining drivers of health are what have previously been called social determinants. However, these are not pre-determined factors. They are drivers of health based on how we have structured opportunity within our society. They include factors like housing, nutrition, access to employment, interaction with the criminal justice system and education. To me, literacy is a core social driver of health given that it impacts access to so many of the other social drivers. A child’s early literacy skills lay the foundation for how they will do in school, their potential for graduation, which impacts their ability to get a job with fair wages and benefits like health insurance, access to of environmental racism. We also know that health literacy, not only the ability to read and write, but one’s understanding of and ability to navigate the healthcare system, has a significant impact on one’s health. We know that if someone struggles to understand how to stay healthy or how to manage a chronic disease, if they
loans and home ownership and ability to mitigate the impacts humility, then they are at an increased risk of a number of complications like medication mistakes, increased hospitalizations, more missed appointments and overall poor health. In fact, one study of Medicare-aged adults found that patients with limited health literacy had an overall adjusted hazard ratio for all-cause mortality similar to that of an individual with diabetes. In other words, the impact on one’s health of having limited health literacy is on the same magnitude as having a diagnosis of diabetes. So, we can see that literacy is a significant social driver of health that has an impact throughout one’s life.
Early literacy: What first actions beyond Reach Out and Read efforts are available to address this disparity?
Reach Out and Read is one component of an ideal early childhood ecosystem. In the first three years of life, children need safe, stable
and nurturing relationships the most; therefore, we should be advocating for policies that help provide stable housing, nutrition and economic support for families. Issues like paid family and medical leave, paid sick leave, universal childcare and extension of maternal healthcare benefits all impact the early childhood ecosystem. As clinicians and service providers we should be aware of several early childhood resources for families and know how to connect families to nurse home visiting, WIC/SNAP, Help Me Grow, housing assistance, Early Head Start and Head Start, for example. The main impact from Reach Out and Read isn’t the book; it’s the parenting support and guidance. We must support the parents and caregivers of our youngest children in order for those children to reach their full potential.
How has healthcare access in Minnesota for nonCOVID conditions been impacted by the pandemic?
We know the initial shelter-in-place mandates and suspension of elective procedures did impact access for many patients. In particular, access to dental cleaning and care has taken a hit as well as immunization rates for children, particularly those older than two. Since our gradual reopening we have seen some recovery in those numbers but we remain concerned, particularly about our immunization rates which, according to a Minnesota American Academy of Pediatrics survey in July, still showed a decrease in immunizations for young children of around 35% and a decline in immunizations for teenagers of 45%. The biggest beneficial impact on access we have seen is expansion of telehealth. Federal and state flexibility in telehealth regulations have allowed many different types of healthcare services to be delivered via telephone or video. This has really been a welcome change for many providers and patients even as payers continue to sort out what things can and should look like after COVID-19. I have heard from our Federally Qualified Health Centers, Tribal Nations and our rural county providers alike that the increase in access provided by telehealth has decreased no-show rates and even helped with some of the social isolation patients have experienced during the Stay at Home and Stay Safe orders.
Are economic and racial disparities/inequities in access or treatment more evident during the pandemic?
Yes. Data from the Centers for Medicare and Medicaid Services clearly show that among those on Medicare who are also on Medicaid (low-income folks over the age of 65, or with special needs) have higher rates of COVID-19 infections and hospitalizations. When the data is broken down by race, we see even higher rates among Black and Hispanic Americans than among white Americans. In Minnesota, we see similar numbers. Although the raw number of deaths appear to be mostly white Minnesotans, if we take a deeper look at the age-adjusted rates of hospitalizations and deaths, Black, Hispanic, Asian and Indigenous Minnesotans are disproportionately impacted by COVID-19. When it comes to telehealth, I share concerns about a relative lack of access to communities who lack English language proficiency as well as those who cannot afford a smart phone, who do not have the internet access necessary to participate in video visits or who have difficulties navigating the technology required for video visits.
How do COVID and non-COVID care experiences differ between the metropolitan Twin Cities and other more rural areas of MN during the pandemic?
From what I hear from our colleagues outside of the Twin Cities metro area, there has been a largely positive response to expansion of telemedicine for non-COVID care. Instead of having to drive hours for a 15- or 30-minute clinic appointment, their patients and community members are able to get many of their needs met remotely. Regarding COVID care, testing has been an uneven issue like it has been in other parts of the metro and across the country. There are communities that have been hit harder because they are home to facilities such as meatpacking plants with outbreaks. There are certainly similarities seen throughout Minnesota related to consistent access to testing and basic healthcare coverage. Where there are gaps, we are more susceptible to outbreaks.
What measures do DHS and you take to address the above areas of potential concern?
Regarding the pandemic response, the Minnesota Department of Human Services has taken a number of steps to help Minnesotans currently served or newly a part of Minnesota’s Medicaid and MinnesotaCare programs. During the national public health crisis, no one is being unenrolled or losing their coverage unless they move out of state, request an end of coverage, or pass away. Enrollees do not have to pay anything out of pocket for COVID-19 testing and treatment. In addition, there is access to free COVID-19 testing for many uninsured Minnesotans over the age of 18. To support social distancing we’ve greatly expanded access to telemedicine, including telephone calls, removing the limit on the number of telemedicine visits one can receive in a week, removing the requirement of a first visit with a provider needing to be done face-to-face and expanding the types of providers that can deliver their services via telemedicine to include things like substance use disorder treatment and rehabilitative therapies. Those who receive home and community-based services can have their initial assessments done via phone or video visit. Case management visits also can be handled remotely. And we’ve extended the length of prescriptions for many drugs to allow patients to get a 90-day supply of their maintenance medications. This helps avoid frequent trips for patients, promotes social distancing and decreases the burden on providers.
Colleague Interview (Continued from page 7)
Maternal-child health disparity: What early doable specific actions do you envision being possible and also effective? Accountability and outcome management of these steps?
Minnesota’s Medicaid program has been piloting a community-led intervention to help address the troubling maternal and infant health disparities seen in African American and American Indian communities in Minnesota. The integrative care for high-risk pregnancy program (ICHRP) pilot began five years ago and helps identify expectant mothers with increased risk in the Twin Cities African American population as well as expectant mothers who currently struggle with substance use disorder in the American Indian population. The pilot program has demonstrated that it is possible to improve care and decrease disparities. We are looking to bring this model to scale so that all African American and American Indian mothers served by Minnesota’s healthcare programs can have access to this model of care. We are also looking at expanding postpartum Medicaid coverage to mothers from 60 days to 12 months and continuing to evaluate how we can support doula care and other paraprofessional care. We are evaluating how well we are meeting mothers’ needs and asking whether we are helping to rebuild trust. How are we impacting access to culturally relevant and reaffirming care? By decreasing disparities in access to care and care delivery, we aim to see the rate of low birth weight babies born to African American and American Indian mothers decline and the numbers of mothers going full term and surviving the perinatal period increase. Ideally, this program will also help address the biases we have as clinicians, biases that are the result of living in and training in a healthcare system that is historically structured by racist policies and socializes us, often negatively, around race. It is both these qualitative and quantitative outcomes that will start to turn the overall tide from these deep-seated racial inequities that drive the disparities we see in maternal/child health and elsewhere.
Please comment on the public health information that is available/provided to identify and advise those with high risk conditions like obesity.
This is a good question for the Minnesota Department of Health. I would refer you to their website: https://www.health.state.mn.us/ diseases/coronavirus/.
Of existing Medicaid eligible services, which are underutilized? Are there underlying causes of this underutilization?
There isn’t a specific measure we have currently to look at underutilization. Depending on what service you look at, you could come up with different results. Certain services like pre/postnatal visits, participation in Child and Teen Checkup visits are certainly underutilized. The reasons behind this are likely related to barriers we see elsewhere in access to care like lack of transportation, economic instability and housing insecurity. Likewise, we know that the need for mental and behavioral health services exceeds the current utilization rates of those services, and that underutilization is driven primarily by lack of access to appropriate care and stigma. There are currently some services that have low utilization, but it is unclear if it is under-utilization or the demand is just low. We think about services like community health workers, doulas, community paramedics and EMTs. We know from the literature that services like doulas and community health workers have been shown to help decrease disparities and so it would reason that if we could increase awareness and access to services, we could move the needle to some degree.
What question(s) didn’t we ask that you’d like the readers to learn about?
I think structural racism is the main driver of inequity and so when we are talking about addressing health equity, we are really talking about addressing structural racism and racial equity. There have been a number of cities and counties that have declared racism a public health crisis in the last year, most since George Floyd’s torture and murder. They all have at least one common recommendation and that is the application of a racial equity assessment to policy and decision-making processes. This requires us to first look and see if there is racial inequity underlying the issue we are trying to solve. If we do not know if there is or isn’t, then the next step is to look at the data or gather data to determine if that is the case. Next, we are asked to think about what are some of the underlying structural causes of that racial inequity. How will the policy or action we are considering potentially improve or worsen racial inequities and what are possible unintended consequences of the decision(s) we are proposing? Lastly, and important to highlight because it is where I feel many organizations fail: How are we specifically addressing accountability? In my policy work I liken this to how every decision has a fiscal note. If someone were to propose a policy and had not addressed the impact on the budget, that proposal would be a non-starter. We need the same expectation and level of attention to racial equity. If proposals have not taken racial equity into consideration, they should be non-starters. And so if you look at this across all of the decisions governments and large organizations make, you can see how we can start to address structural racism and not only dismantle it but help undo the harm it has caused over generations.
You protect them. We protect you.
PEACE OF MIND EXPERTISE

CHOICE
PEACE OF MIND • A Berkshire Hathaway company • Pure consent provision gives you control to refuse to settle a claim • Unsurpassed financial strength ratings of A++ (A.M. Best) and AA+ (Standard & Poor’s)
EXPERTISE • 90% national trial win rate; 80% of claims closed without payment • 400,000+ claims handled since 1899 • Advisory Boards of experienced healthcare professionals who review claims and offer insights
CHOICE
Unique insurance solutions across the entire spectrum of healthcare
Claims-made, Occurrence, and Convert to Occurrence® coverage options give you flexibility
Comprehensive coverage in all 50 states and D.C.
THE MEDPRO GROUP DIFFERENCE
FOR MORE INFORMATION, CONTACT YOUR LOCAL BROKER OR CALL OUR MINNESOTA BASED OFFICE AT 651.735.7655.
A.M. Best rating as of 6/16/2020. Standard & Poor’s rating as of 9/25/2019. All data is MedPro Group data; claims data range is 2009-2018 unless otherwise indicated. MedPro Group is the marketing name used to refer to the insurance operations of The Medical Protective Company, Princeton Insurance Company, PLICO, Inc. and MedPro RRG Risk Retention Group. All insurance products are administered by MedPro Group and underwritten by these and other Berkshire Hathaway affiliates, including National Fire & Marine Insurance Company. Product availability is based upon business and/or regulatory approval and may differ among companies. © 2020 MedPro Group Inc. All Rights Reserved.

PROUD TO SUPPORT MINNESOTA HEALTHCARE PROVIDERS — TODAY, AND LONG INTO THE FUTURE.
Gown Design and Manufacturing During the COVID-19 Pandemic:
The Origins and Narrative of the “Gown for U” Project
In March of 2020, during the initial acceleration of the number of COVID-19 cases in the United States, demand for personal protective equipment (PPE) increased significantly worldwide due to COVID-19 outbreaks in other countries. Additionally, China, which is the largest manufacturer of PPE, had significant disruptions in PPE manufacturing. Domestically, hospital-bound PPE was being intercepted and redirected by federal government agencies. These factors contributed to an unreliable PPE supply chain for hospitals in the United States and PPE shortages that were widely reported. Hospital efforts to adapt to the PPE shortage ranged from reusing N95 masks to using garbage bags as a substitute for isolation gowns to care for patients infected with the SARS-CoV-2 virus. On a community level, widespread efforts were assembled to make face masks, N95 masks and face shields. The University of Minnesota itself had efforts geared towards designing new in-house N95 masks, cleaning techniques for N95 mask reuse, designing a box to minimize exposure to aerosolized airway secretions from patients during intubation and developing mechanically automated bag ventilation for intubated patients. During this time, the University of Minnesota Department of Anesthesiology had meetings two to three times a week to give updates on the hospital system operations during the pandemic, departmental

policies, and the general status of the PPE supply within the hospital system. At the end of March, the hospital reported potential future shortages of disposable gowns within the Fairview system due to PPE supply chain issues. Upon hearing this news, I reached out to propose working on and designing disposable gowns. A few weeks later, Fairview did not receive an expected shipment of disposable isolation gowns. A week later, the hospital reported about a day’s worth of disposable gowns available, with plans to reuse the disposable gowns to extend the supply. The gown shortage problem was now very real and on our doorstep. I ventured to see if there could be any way to design a gown that was simple enough to be produced easily and quickly on the University campus. The initial gown design I had in mind was based on the gowns that were used in the hospital. Patterns would be cut from a plastic sheet, with edges heat-sealed to form seams that would create the torso and sleeves for the gown. On April 16, I contacted Stephen Saliterman from the Department of Biomedical Engineering. I had known Dr. Saliterman from the previous year when we were involved in advising a group of senior biomedical engineering students for a capstone engineering project. The project involved heat-sealing thick plastic sheets to create air bladders for a mattress system prototype to assist with optimizing the positioning of patients for intubation. Because of our previous work together, he was the obvious person to approach for the gown project. The next day, Dr. Saliterman and I had our first virtual meeting, along with a group of biomedical engineering students, to discuss the gown supply problem within the hospital system and to discuss the feasibility of manufacturing plastic gowns on campus. One of the questions asked during the meeting was how many gowns would be needed per day. According to Fairview operations staff, approximately 15,000 gowns are used per day. This number would require a large scale manufacturing facility to meet demand, with a possible need for additional manufacturing facilities. Additional biomedical engineering faculty and students, along with several engineers from 3M joined for a second virtual meeting that evening to assist with the scope of the project, and the gown project was officially launched. The gown design project was divided into teams. The design team was tasked

with determining specifications on how the gowns would be made so the gown could be worn securely with adequate protection for the wearer, but also easily removed. The schematic program SOLIDWORKS was used to specify how the plastic was cut, what holes were punched and which edges were heat-sealed. Another team was involved with FDA requirement research and FDA paperwork submission for the use of the gown design in the healthcare setting. Due to the gown being a level 1 isolation gown, however, the FDA did not require any paperwork submission because premarket notification was not required. As a result, the FDA team was folded into the materials and manufacturing team. This team was tasked to find sources (suppliers) of the plastic sheeting for the gown, and also to identify and work with converters—companies that would convert the plastic sheeting into gowns. During the whole design and manufacturing process, Lindsey Griffin, Elizabeth Bye and Lindsey Strange from the School of Design gave insight to the manufacturing processes that would refine the gown design to facilitate fabrication. The Institute of Engineering in Medicine and the Bakken Medical Device Center within the University of Minnesota were also involved with providing additional resources and assistance in finding sources for plastic sheeting and gown converters. In the midst of Minnesota’s stay-at-home order, several prototypes of the gown were made over multiple virtual meetings and limited in-person contact due to social distancing guidelines. Some prototype testing was done at Fairview to assist with further refinement of the gown design. Price quotes were obtained by the materials and manufacturing team, in addition to some price negotiations on behalf of the Fairview system. Ultimately, Polar Plastics (Oakdale, MN) was identified as the primary source of plastic sheeting for the gowns, and Red Fox Innovations (Arden Hills, MN) selected as the primary converter to create the gowns. Additional converters were also identified within the Twin Cities to assist with supplemental gown manufacturing as needed. On May 1, purchase orders for materials and gown manufacturing were placed with future purchasing decisions to be done by the Fairview Health System. In two weeks, the gown project was completed. The final design of the gown consists of 2 mil FDA-certified polyethylene film with blue tinting with an antistatic coating added during the manufacturing process. The schematic for the gown has an open license for use, which can be downloaded at bit.ly/gown-for-u. As of mid-June, approximately 30,000 gowns had been purchased by the Fairview Health System and manufactured by Red Fox Innovations. The many people who were involved in this large, multidisciplinary project were invaluable in their contributions to the design, to the identification of materials and manufacturing infrastructure, and to the manufacturing of the gowns to supplement the local PPE shortage in the spring of 2020. If PPE shortages manifest again with increases in COVID-19 cases in the future, I hope that our efforts and gown design can be used again locally and by other cities and institutions to obtain essential gowns in an expedited fashion.

Kevin Wang, MD is an assistant professor of Anesthesiology at the University of Minnesota. He has an undergraduate degree in electrical engineering and a Masters Degree in Biomedical Engineering. His medical training was at the University of Cincinnati and the University of Minnesota. He has interests in developing engineering applications and solutions in medicine. E-mail: kxwang@umn.edu.
FUHN Clinics Respond to Rapidly Evolving Times
The Federally Qualified Health Center Urban Health Network (FUHN) was founded in 2012 and operates in Minnesota as a virtual Integrated Health Partnership (IHP) and nationally as a Health Center Controlled Network (HCCN). FUHN was the first FQHC-only safety net Medicaid Accountable Care Organization in the nation. FUHN is comprised of 10 member organizations which are Federally Qualified Health Centers (FQHC) or FQHC look-alikes: • AXIS Medical Center • Community University Health Care
Center (CUHCC) • Indian Health Board of Minneapolis • Minnesota Community Care • Native American Community
Clinic • Neighborhood HealthSource • Open Cities Health Center • People’s Center Clinics & Services • Southside Community Health
Services • United Family Medicine In 2019, FUHN clinics served over 114,000 of some of the Twin Cities’ most vulnerable patients. Roughly 91% represent diverse populations, 95% have incomes below 200% of the federal poverty level and 41% are best served in a language other than English. Approximately 47% are on Medicaid and 31% are uninsured. Caring for our most vulnerable community members presents unique challenges in the best of times, but during a global pandemic these challenges are only magnified. As the COVID-19 pandemic expanded to Minnesota in the middle of March,

our clinics became immediately aware of the need to transform how they delivered care to their patients. Additionally, our clinics would need to develop a plan to test patients for COVID-19. Many of our clinics had tested the waters of telehealth in various ways, but no clinic had developed a plan for widespread implementation of telehealth services across the full spectrum of healthcare needs. As each clinic had separate EHRs and workflows it seemed as though they would have to do this work individually. As members of FUHN, however, there was an infrastructure in place via our Clinical Quality Improvement Committee (CQIC) which met monthly to discuss clinical quality and chronic disease management. FUHN clinics added more frequent meetings during this time, now meeting three times per week for 30 minutes. These meetings provided time to ask questions, share best practices, and communicate the frequent updates coming from the Minnesota Department of Health (MDH) and Centers for Disease Control (CDC). Utilizing FUHN staff to collect and disseminate information to the clinics allowed the clinics to focus on operational implementation. During the earliest part of the pandemic response FUHN clinics transitioned around 80%-90% of their appointments to virtual appointments. Clinics adapted with various models of care. Sometimes the patient was in the clinic and the provider was at home, sometimes the providers were in clinic and patient at home and sometimes both were remote from the clinic. Some clinics began to offer driveup outdoor lab-only appointments with telehealth visits to discuss the results. Other clinics moved their patient support groups and group visits to the virtual setting. During this time, it became clear that clinics would need to provide durable medical equipment to their patients for telehealth visits to be effective. FUHN reached out to payers to see if they’d want to support chronic disease management via telehealth. UCare quickly replied and asked how they could help. Reliable thermometers, blood pressure cuffs and scales would support patients as they navigated managing their health while physically disconnected from their clinics. To that end, UCare supplied 2,000 blood pressure cuffs, 8,000 batteries, 2,000 thermometers and 50 scales for FUHN to distribute to the member clinics. Fortuitously, FUHN was working with MDH and Institute for Clinical Systems Improvement (ICSI) on a CDC grant to improve hypertension outcomes. Through that grant, while the equipment was on order, a toolkit was assembled for the deployment of the cuffs, thermometers and scales. In that toolkit, FUHN provided a workflow template and patient
education resources to the clinics. After receiving the equipment each clinic quickly developed a plan to distribute the devices to their patients. All FUHN clinics have a process in place to distribute and connect with patients after they receive their equipment. UCare providing these devices allows clinics to provide equipment to patients without barriers in a time that has only seen an increased burden for our patients. While the clinics were rapidly changing the modality of their visits, they also had to adopt protocols for COVID-19 screening and testing of their patients and the broader community. Early on, the clinics recognized that they were not only going to have to offer tests to established patients, but also test people not previously engaged with their clinics. Clinics provided outreach via paper letters and text messages to their communities and many clinics posted their sites on the Minnesota State “Find Testing Locations” website (https://mn.gov/covid19/for-minnesotans/if-sick/testing-locations/index. jsp). Several clinics offered open-air and mobile testing sites instead of or in addition to their clinic locations. Every clinic was able to provide testing, and many have partnered with each other, external agencies and community groups to expand the availability of culturally competent testing. As results came in from the testing, it became clear that there were striking disparities in who had positive tests. Minnesota Community Care (MCC), for example, provides primary care for greater St. Paul with over 50% Latinx, 15% Black, 15% Asian and 13% non-Hispanic white patients. MCC’s Lauren Graber, MD, MPH, Shawna Hedlund, MPH and Chris Singer, MN, RN wrote about their results, “Of all the Latinx patients tested at our sites for COVID 19 between midMarch and July 9th, 54% were positive, almost eight times greater than the 7% of white patients that were tested. Thirty-six percent of our Asian patients tested were positive and 12% of our Black patients. Given that we are only testing patients who have symptoms of COVID-19, we expected that our rate of positivity would be high—40% of all patients tested were positive—but the disparity between our white patients and patients of color is even more glaring than anticipated.” These disparities highlight the importance of FQHC clinics and their ability to provide culturally competent testing and care to the communities they serve. In late May, the tragic death of George Floyd and subsequent unrest disproportionately impacted FUHN clinics, patients and their communities. Just as clinics had started bringing patients back into clinic for in-person visits, several FUHN clinics had to temporarily close their doors to those visits and some had damage and equipment stolen. Despite these circumstances, the pivot to virtual visits from earlier in the pandemic allowed the clinics and patients to receive timely care. This highlights the need to continue to provide telehealth as a part of patient care in the future. Now that our clinics and patients are becoming proficient in telehealth it will remain an important part of comprehensive health care. There are many challenges that remain to be addressed as no one knows how long the pandemic will last. FUHN clinics will have to continue to innovate how they provide quality primary care services to their vulnerable patients with flu season looming. Telehealth will likely remain an important part of that picture. The work that has already been done will serve as an important template for challenges faced in the future. One thing is for certain, FUHN clinics are uniquely positioned to stand at the forefront of that work.
Nicole Kapinos, DNP, RN is the Director of Population Health/Quality Improvement at FUHN. She has over 10 years of experience in health care as a registered nurse, operations manager and clinical healthcare informaticist. Her current role blends all those experiences to provide support to FUHN clinics as they endeavor to improve population health, enhance patient experience, reduce costs and improve primary care access for the patients they serve. She holds a Bachelor of Science in Nursing from the University of Rhode Island and a Doctor of Nursing Practice in Nursing Informatics from the University of Minnesota. Ms. Kapinos can be reached at: nkapinos@fuhn.org; (952) 288-4852.
MEDICAL SPACE FOR LEASE

S M C Edina, MN


R M B Burnsville, MN
2800/2828 M B Minneapolis, MN

Leased By:
MIKE FLEETHAM (952) 7672842 MFleetham@MedCraft.com
JOLENE LUDVIGSEN (952) 8387126 JLudvigsen@MedCraft.com
Owned By:
medcraft.com/leasing
Solving homelessness should be easy: just give everyone a home. That was my simplistic view toward homelessness before I met my research colleagues with lived experience of homelessness three years ago. Since then, they have taught me that simply providing a home is not the answer to homelessness. Even delivering supportive services in addition to housing is not enough. An accepting community is essential to create stability and belonging for people to remain stably housed. Without this, many people return to the streets seeking freedom and friendship. My colleagues with lived experience of homelessness: Dewayne Parker, Freddy Toran, Junail Anderson, Rome Darring, and Sherry Shannon, have designed a new type of community for people experiencing homelessness called “Envision Community” which combines truly affordable microhousing with the secret sauce of stable housing — intentional community—where people live cooperatively and support each other. Envision Community is designed and led by people with lived experience of homelessness, while 18 collaborative organizations stand alongside Envision’s leaders with lived experience of homelessness by adding their industry-specific expertise to help make Envision a reality. My colleagues have grown into true leaders by participating in all aspects of the housing development process, making the key decisions, and possessing true expertise about homelessness, namely their personal lived experience of homelessness. The group is working to build its first community of 15-40 people living
Sherry Shannon, Freddy Toran and Dewayne Parker in front of the prototype unit.

in mircohomes around a central common house. The collaborative successfully engaged the City of Minneapolis to create a zoning ordinance that allows this new type of microhousing in Minneapolis, and the City Council unanimously approved the ordinance last year. As a result, Envision’s first community will be located somewhere in Minneapolis. While the group has been developing this new type of community for people experiencing homelessness, I have had the honor of assisting them evaluate the outcomes of their work. Specifically, Envision Community wants to rigorously study its new type of community to learn if their work creates the impact they want. Does Envision really improve the health of people experiencing homelessness? Is it cost-effective? How do social connections lead to health and housing stability? How does this community influence the surrounding neighborhood? Just as the group has changed my views toward homelessness, they have also transformed my views of effective research. While I strongly believe that thoughtful study design is essential to create quality evidence that accurately informs decision making, I am less convinced that high quality scientific work can inspire change within a grassroots community. Research seems to influence clinicians, academics and policy makers, but does traditional
research really change the thoughts and actions of people experiencing homelessness? I have learned from my colleagues with lived experience of homelessness that if research is to be meaningful for people in the homeless community, who is seated at the table when designing a study is just as important as the study design itself.
Unique Approach to Research
Traditional homelessness research is performed by researchers and other professionals who have never experienced homelessness. This traditional research seeks the input of people with lived experience of homelessness viewing those individuals as sources of data, but people with lived experience of homelessness are rarely viewed as potential researchers and scientists. In fact, the research process itself—forming a research question, making hypotheses, designing and analyzing a study—is usually carried out by researchers or other professionals, excluding the true experts on homelessness: people with lived experience of homelessness. Equity in research is as much about the process as it is about the product it creates. That is why Envision Community will measure success using Community Based Participatory Research (CBPR), where residents and other people with lived experience of homelessness are the researchers themselves, taking part in all aspects of research. Most importantly, people with lived experience of homelessness—rather than traditional research scientists—will be setting the research agenda and providing the lens for understanding the results.
Advantages of this Approach
Research is the process of uncovering the truth. When asked how they know something is true, people with lived experience of homelessness often respond that they need to see it for themselves or hear about it from a trusted friend to know it is true. Qualitative research methods especially resonate with members of the homeless community where stories and personal experiences are among the most trusted forms of information. Stories and other data gathered by members of their community creates trust in the research process

and makes the results more credible in the eyes of the homeless community. Another strong advantage of research led by members of the homeless community is their ability to share the results with their community. Envision’s leaders report their work at homelessness advocacy groups like Freedom from the Streets and Street Voices of Change, reaching hundreds of people with current or past personal experiences of homelessness. This provides an opportunity to validate (or invalidate) the results of the research through the feedback the group gives, and equally important, it gives those groups the chance to consider how to use the results to better their community. Research has the potential to cause unintended harms for a community by negatively impacting resources, opportunities, policies or perceptions of people experiencing homelessness. Our research is less likely to create those unintended harms when it is led by people experiencing homelessness and validated by large groups of people from the homeless community.
Building Our Research Capacity
Before Envision is built, we are developing the skills necessary to work as an effective research team to perform formal outcomes research. The University of Minnesota’s Center for Urban and Regional Affairs (CURA) generously funded Envision’s first program evaluation to learn our community’s response to Envision’s fully built prototype microhousing unit. This research will help us understand what a broad group of people experiencing homelessness think about Envision’s microhousing. The co-created evaluation plan will produce the metrics we need to measure the unit’s success and identify how well our prototype works socially, environmentally and operationally. During the evaluation, we will formulate research questions, generate hypotheses, design research methods, submit our plan to the Internal Review Board (IRB), gather data, analyze the results, and report our findings.
Our Long-Term Goal
Although we are focused on building a ready-to-use process to evaluate and continuously improve Envision’s first microhousing community, over the long term, the group intends to carry these skills far beyond Envision. First, we seek to perform our own research about broader issues of homelessness. We want to be known for authentic research grounded in the lived experience of the homeless community, maintaining constant awareness that research outcomes have real consequences for people experiencing homelessness. Second, we hope to become a valuable resource for any project in our community, seeking to research issues or design solutions that address issues people experiencing homelessness face. Finally, we hope to become a model for other homeless communities around the country to organize and lead research in their community that advances equity for people experiencing homelessness.
William E. Walsh, MD is a practicing Facial Plastic and Reconstructive Surgeon with Hennepin Healthcare and the University of Minnesota. He is also a research fellow with the Minnesota Design Center in the College of Design at the University of Minnesota where he researches homelessness, housing and health equity. His primary research collaboration is with people experiencing homelessness. Together they research and design grassroots solutions to address homelessness and improve health. Emails to Dr. Walsh can be sent to wwalsh@umn.edu.
Reinventing Health Care: Children’s Minnesota Responds to COVID-19
As the COVID-19 pandemic upends the norms of daily life, it has become imperative that health care reinvent itself to meet community health needs. While safety concerns were rampant among the general population, especially in a healthcare setting, the pediatric population has presented particular challenges. When the pandemic began, Children’s Minnesota saw a precipitous drop in well child visits, as well as other specialty care services. To live out our mission to be every family’s essential partner in raising healthier kids and to respond to the rapidly changing environment, Children’s Minnesota has worked deftly to meet the needs of its patients and families. Thanks to the tireless work of leaders, nurses, physicians and other healthcare professionals, the organization has managed to change trajectory and has seen patient volumes begin to stabilize in many service lines, with immunizations back up to almost 90% year-to-date as of August 2020 compared to the same time last year. Along with extensively enhancing safety and sanitization measures, key initiatives have included innovating the primary and specialty care experience as well as pivoting the approach to clinical education.
Drive-Up Care for Immunizations
Children’s Minnesota implemented safety measures in parallel with innovative new models of care. Among key initiatives implemented by Children’s Minnesota is Drive-Up Care. The Drive-Up Care program offers families the opportunity to follow the American Academy of Pediatrics guidelines for immunizations without entering the clinic. While clinics and hospitals have taken extra precautions to enhance safety measures, the model assuages parents’ fears of acquiring or spreading an infectious disease during a pandemic. To access the program, the family calls their clinic to make a drive-up appointment. Upon arrival for their visit, the family notifies the clinic of their arrival. A nurse comes to their car with the necessary protective equipment and follows sterile techniques and standard process to administer the child’s necessary care. The parent or guardian then receives aftercare instructions. This model is also used to administer injectable birth control, and Children’s Minnesota clinics plan to add A1C testing for patients with diabetes. The concept and implementation of Children’s Minnesota Drive-Up Care was completed within weeks of COVID-19’s spread into the state. Vaccination rates among Children’s Minnesota patients

had dropped 46% in April 2020 compared to April 2019. Each month since has been an improvement, and by August vaccination rates were almost back to normal levels.
Innovating the Virtual Experience
Furthermore, Children’s Minnesota worked with urgency to ramp up its virtual care offerings. Prior to the pandemic, approximately one hundred virtual visits would take place each month through the Children’s Minnesota healthcare system. This climbed to more than 6,000 per month in April and May. From March to July 2020, more than 20,000 virtual care services have taken place. Children’s Minnesota was able to quickly upgrade its technical and payment systems to make this come to fruition, easing the concern of families needing medical care but worried about exposure to COVID-19. Healthcare professionals
that had never used virtual care models were quickly trained in, partially through support of ‘super users’ who had already adopted the practice. Virtual visits have also increased access to the Children’s Minnesota healthcare system, allowing families outside of the Twin Cities to access the highest quality care. In primary care and ENT, Children’s Minnesota is piloting a home device kit, TytoCare, that would support diagnosis for virtual patients. The kit includes a tongue depressor, infrared thermometer, otoscope, stethoscope and a touch screen device, all of which will be connected remotely to a clinician and support families in managing chronic conditions and diagnosing common illnesses. A similar model will also be piloted to support physician-to-physician collaborations, allowing Children’s Minnesota clinicians more real-time data and analytics to better partner with healthcare systems outside of the Twin Cities. In our specialty care departments, it was important to find virtual solutions with some of our most medically fragile patients with complex needs and equipment. Within 10 days of COVID-19 reaching Minnesota, our specialty care pivoted to virtual services and homecare for specialty care patients. Patients were able to get COVID-19 testing, bloodwork and labs, all administered through homecare. Throughout the Children’s Minnesota system, innovative change has been a constant since the COVID-19 pandemic. The fetal cardiology team has implemented new virtual services to support babies that needed monitoring. Remote hand-held dopplers were given to parents that allowed families to monitor their newborn’s fetal heart rate from the convenience of their home. The clinical team was then able to collect that data and virtually support families. The dopplers also allowed some diagnostics to take place at home. In rehabilitation services, occupational therapy and physical therapy, Children’s Minnesota has also found unexpected success through virtual services. Through virtual care, therapists have been able to enter a patient’s home and understand firsthand challenges that would not have been as apparent in the clinic. Virtual sessions have also empowered patients and caregivers to take on a more hands-on approach to their therapy since therapists are not physically present during a session.
Pivoting Clinical Education
Children’s Minnesota is committed to providing education and resources to clinicians — to both our professional staff and members of the community and region. When the pandemic reached Minnesota, the organization quickly pivoted and prioritized creating and sharing resources broadly. The COVID-19 clinician toolkit, co-authored with Children’s Health Network and published in April 2020, is frequently updated with clinical guidelines, literature reviews and upcoming COVID-19 focused events. Previously, Children’s Minnesota’s weekly Grand Rounds was only available in an in-person format but is now available live, online each week. It is also recorded and housed in an online library. We’ve seen increased attendance compared to our in-person format, with an average of 250 attendees each week, and will continue with the online format beyond the pandemic. Additionally, Children’s Minnesota created a new pediatric podcast, Talking Pediatrics, with many episodes focused on COVID-19, and designed to be condensed and easy to consume.
Looking Toward the Future
While the pandemic has brought unexpected challenges in all sectors, it has also pushed health care in a new and more innovative direction. We have learned to be flexible in these times of continued uncertain change and have, as a result, been able to meet our patients’ needs in new ways. The pandemic will forever impact the way healthcare workers and patients approach medical needs. As we move forward, and even in the eventual post-pandemic world, Children’s Minnesota will continue to reflect on these lessons and approach each new challenge with creative twenty-first century solutions. We will continue to innovate and forge new partnerships that will allow us to truly be every family’s essential partner in raising healthier children.
Author: Razaan Byrne, MD, is a primary care pediatrician at Children’s Minnesota, who sees patients in the Minneapolis Primary Care Clinic. She is also a continuity clinic preceptor for pediatric residents from the University of Minnesota. She can be reached at: Razaan.Byrne@childrensmn. org. For detailed Drive-Up Care workflows for implementation at your clinics, please reach out to pamela.chawla@ childrensmn.org.
Food as Medicine Program Promotes Healthier Food, Healthier Lives
Food insecurity is of growing concern in many of our communities today. For those unfamiliar with the term, food insecurity is the disruption of food intake or eating patterns because of lack of money and other resources. In plainer terms, individuals or families that are “food insecure” lack access to healthy foods, enough so that their ability to live healthy lives overall is greatly reduced. While food insecurity can occur based on many factors, like income, employment status, disability and race or ethnicity (according to the U.S. Department of Agriculture Black and Hispanic households, for example, are twice as likely to experience food insecurity), the sudden impact of the pandemic has dramatically reduced access to healthy foods for many people in the United States. According to a recent brief from Feeding America, Minnesota is facing the second highest percent increase (+60%) in food insecurity rates in the nation. Another report compiled by Second Harvest Heartland and management firm McKinsey & Company reported what authors call a “hunger crisis” that will affect more than 700,000 Minnesotans in 2020.
North Memorial Health Addresses Food Insecurity in our Communities
While hunger is the most understood outcome, the health impacts of food insecurity can be lasting, even lifelong. As part of our commitment to the health of the community, North Memorial Health has been working to combat food insecurity in our North Minneapolis communities and
Peter Tanghe, MD Nicky Mack, RN
other areas for some time. For example, we’re an anchor partner for several innovative programs such as North Market, which opened in 2017 to offer affordable and healthy food to North Minneapolis residents. North Collaborative Care and North Memorial Health have been recognized by partner Second Harvest Heartland for introducing an innovative, sustainable approach to hunger relief directly into our clinics. In addition, North Memorial Health community paramedics have been with Community Emergency Assistance Programs (CEAP) and MATTER, a Minnesota-based nonprofit, to deliver MATTER Box meal kits to community residents in need. With the onset of COVID-19, however, we’ve seen a marked decrease in access to healthy food, particularly for individuals with chronic conditions, who are often at much greater risk of serious illness from the virus. With the outbreak of COVID-19, representatives from North Memorial Health including our care coordination team, primary care and community paramedic teams began working with our partners at Pillsbury
United Communities and Blue Cross and Blue Shield of Minnesota to create sustainable ways to deliver healthier foods to people who need it—those who would be at greater risk if they left their house. The goal of ensuring that our most vulnerable customers could receive healthy foods in a convenient and safe manner, has become increasingly more critical. This sense of urgency, combined with North Memorial Health and its partners dedication to our communities, resulted in the launch of a new Food as Medicine pilot program in July 2020.
About the Food as Medicine Program
The new Food as Medicine program provides personalized weekly grocery packages to vulnerable customers from the North Memorial Health Clinic –Camden who have chronic health conditions and are at a higher risk for COVID-19. Packages are delivered by North Memorial Health community paramedic team members, who can also assess participants’ wellness. North Market, a program of Pillsbury United Communities that serves as a full-service grocery store, partnered with Blue Cross and North Memorial Health to develop and fulfill the program. While our care teams witnessed a higher risk of food insecurity across many of our communities, our North Memorial Health Clinic provided an excellent hub for the pilot program. The Camden neighborhood is near North Memorial Health Hospital, with access to community paramedics based nearby. While the needs across North Minneapolis are acute, the
Camden community, in particular, has suffered the impacts of not only COVID-19, but also the recent civil unrest which has closed many neighborhood stores. For the pilot program, participants were selected by North Memorial Health care coordinators who identified the customers at higher risk from COVID-19 due to chronic conditions like hypertension or diabetes, and many of whom live alone and are at a greater risk of isolation. North Memorial Health care coordinators contacted them to offer enrollment in the Food as Medicine pilot program, with each group of 10 people participating for a total of 12 weeks. As mentioned earlier, the Food as Medicine program is based on weekly delivery of grocery items and some personal care items, selected from a menu designed by North Memorial Health care coordinators—in partnership with North Market—to provide a healthy variety of foods from each food group. Much like any other grocery delivery service, customers select groceries from this list each week, and great care is taken to accommodate specific preferences or requirements. Unlike food shelf programs or other delivery programs, those enrolled in the Food as Medicine program are not limited to receive only shelf-stable, pantry items. Instead, each week they may choose two items from each of the four food groups, including fresh produce, dairy and fresh meats. Greater choice, along with safer access to healthier foods, is an important component in the program’s success, providing people not only with proper nutrition but also with the ability to select meals that meet their own individual preferences and needs.
The North Market Advantage
Another plus of having the Food as Medicine program serve the Camden community is the North Market. North Market is a unique enterprise including a full-service grocery store and North Memorial Health’s Wellness Resource Center staffed with dietitians and community health workers (provided by Pillsbury United Communities).* North Market provides fresh, good food at affordable prices to families and individuals who might otherwise have limited choices. All Food as Medicine deliveries originate at North Market, where food packages are created and personalized based on each individual’s weekly choices. With the help of North Memorial Health care coordinators, each menu item is aligned with the essential foods that support the needs of their chronic conditions. Once prepared, our community paramedics make weekly deliveries right to each individual home.
The Role of Community Paramedics
For many individuals, COVID-19 has increased the isolation they may have already been experiencing due to chronic illness. Seven North Memorial Health community paramedics play an important role in the Food as Medicine program, providing not only meal delivery but important health checks on a monthly basis. Through the course of the program, members of our community paramedic team have often built strong personal bonds with participating customers. North Memorial Health care coordinators report several instances where the team has recognized and alleviated smaller concerns that could have turned into greater health problems. Whether it was a suspected case of COVID-19 or an increase in blood pressure, community paramedics have been quick to spot these concerns during weekly visits, perform the necessary health assessments and arrange for the appropriate resources. In one specific incident, a community paramedic noticed that one of her customers was experiencing a significant increase in anxiety. Upon further investigation she discovered that the individual had been unable to take their hypertension medication and she quickly arranged a telemedicine visit to resolve the problem. Left unchecked, this issue could have resulted in a serious health incident. Instead, based on her experience and trusting relationship with this customer, the problem was eliminated by a resourceful and caring North Memorial Health team member.
The Future of Food as Medicine
Implemented as a pilot program, Blue Cross and Blue Shield of Minnesota and North Memorial Health are measuring the success of the Food as Medicine program by conducting weekly satisfaction surveys with participants as well as providing monthly health monitoring. Already it’s clear that many needs of residents enrolled are being met by the pilot program, and that it addresses not only basic food insecurity, but also lessens the impacts of isolation. Anecdotally, North Memorial Health care coordinators, community paramedics and family practice physicians report that even after only 12 weeks, participants are experiencing better physical and emotional health. The Food as Medicine program remains in pilot stage but it’s clear that the program is squarely addressing many barriers to eating healthier foods.
Peter Tanghe, MD, is an EMS physician at North Memorial Health Hospital and Maple Grove Hospital. He is also the Medical Director for North Memorial Health Ambulance and Air Care. He has dual board certifications in Emergency Medicine and EMS. Dr. Tanghe also serves as the chairperson of the Minnesota Ambulance Association’s Community Paramedic Advisory Committee.
Nicky Mack, RN is Program Manager for North Memorial Clinic’s Community Care Management department. She is a member of the American Nursing Association, American Academy of Ambulatory Care Nurses and volunteer for the Arthritis Foundation. Nicky is a two time winner of the March of Dimes Nurse of the Year Award. She enjoys working with her team to find creative ways to provide exceptional customer service and help customers achieve their best health.
*At the time this article went to print, the Wellness Resource Center remained closed due to COVID-19 restrictions.
References: • Feeding America (2020. May 19) The Impact of the Coronavirus on Local Food Insecurity. FeedingAmerica.org. • Coleman-Jensen, A., et al. (2019). Household Food Security in the United States in 2018. U.S. Department of Agriculture Economic Research Service. Available online at: https://www.ers.usda.gov/webdocs/publications/94849/err-270.pdf?v=963.1.
The COVID-19 Pandemic has Changed our World in an Unprecedented Way
Physicians enter the field of medicine with a sense of purpose as they hope to influence the lives of others in a compassionate and caring manner. Although our ultimate goals remained the same, during the initial phase of the pandemic, the guidelines provided by the MDH and CDC drastically changed how we provided care to our patients. This change led to the displacement of physicians, care teams and colleagues from their home clinic sites, resulting in disconnection with patients. Our community faced further disruption as some physicians were either furloughed or began working virtually. The shortage of Personal Protective Equipment, a lack of prior knowledge or science related to the effects of COVID-19, and the unavailability of evidence-based treatment guidelines produced additional burden. This in turn led to confusion, stress and burnout among physicians. Physicians are still faced with uncertainty as the evidence continues to evolve and guidelines change for providing effective and safe care to patients. We are still navigating the challenges of maintaining the safety of ourselves and our loved ones as well as the economic implications of working in a new model of practicing medicine. HealthPartners addressed these challenges head-on, rapidly establishing a virtual visit platform to continue to provide high quality care during the pandemic. This measure has allowed physicians to continue to do what they love the most—connect with their patients! Patients have been highly receptive to virtual care and are very thankful to have the opportunity to connect with their clinicians and care teams. As clinicians and care teams realign with their purpose, we have been able to create a sense of normalcy amongst a chaotic state. This was an unprecedented time for all caregivers, and as we addressed the needs of our patients, we had to make sure we didn’t neglect another important group—ourselves. For many of us, the pace of work and the stress that accompanied it were unlike any situation we had ever encountered. HealthPartners physicians

with our “Be Well” team created a website to provide resources for maintaining clinician health and wellbeing. The website offers a wide range of tools, which are broadly divided in three main categories. These include strategies involving immediate support from our behavioral health team, evidence-based tools to manage stress and burnout, and the opportunity to share, connect and celebrate each other. Resources include information for childcare, eldercare and pet care, videos, and podcasts including Make it Ok, Depression and Social Distancing, and employee assistance resources, among many others. The website offers coaching, counseling, immediate access for behavioral health needs and spiritual care. Physicians have also uploaded short videos on the topics of meditation, Heartmath, MBSR, Self-compassion and Gratitude to manage stress, thoughts and emotions in order to feel calm, rested and centered during this pandemic. The website has another important function: it gives us a place to recognize each other. It offers opportunity to celebrate and share individual talents, offer gratitude and publicly appreciate colleagues. In addition, groups within the organization have participated in Zoom meetings to stay connected and to maintain our community in a socially and physically distanced environment. We also looked outside traditional approaches. HealthPartners physicians co-created the “Brave New Medicine Program” in collaboration with behavior and innovation experts from Brave New Workshop Improv Theater. Our goal is to utilize tools extracted from improvisation to transform patient interactions and boost resilience. Personally, it seems as though the unpredictability of this pandemic appears a certainty for now. It has been interesting, and at times difficult, as a leader to focus on keeping ourselves and patients safe while simultaneously delivering timely and evidence-based care. Although challenging, I found it vital to understand the truths of colleagues, staff and patients, and allay fears in order to positively impact our community.
The past few months, more than ever, have mandated time for reflection and introspection. The harsh reality of the pandemic has manifested in my personal life as I have lost loved ones and fear not being able to see my family back in India. I have taken this time to truly appreciate my role as a physician, leader, colleague, parent, spouse, son and a distant member of an extended family during the pandemic. I have focused on being present, continued to express gratitude, and spent time with my family. I have found joy in exercising at home and spending more time with nature through hikes in our beautiful Minnesota State Parks. A few moments of box breathing or meditative apps have been my saviors in being mindful during my conversations with patients, colleagues and my family. Despite all of the challenges, we have innovated and been very dynamic in embracing changes—more than I have ever seen or experienced in my 20 years of practice. We are determined to steer our path through and past this pandemic as a community with our innovation, creativity, resiliency and determination. In a few months, I’m confident we will all look back on our journey, admiring the treacherous terrain we successfully navigated together.

Anand K. Shah, MD, FAAFP, Family Physician at HealthPartners Brooklyn Center Clinic, Regional Medical Director, HealthPartners Primary Care. He can be reached at: Anand.k.shah@healthpartners. com.
Angel Foundation Combats COVID-19 with Extra Hope for Cancer Patients and Families
When we flipped the calendar to January 2020, we had little to no idea what was in store for the world. Everyone’s life has been impacted by COVID-19 in myriad ways, and especially so for those with a cancer diagnosis. Mendota Heights-based Angel Foundation is well aware of this struggle, as its mission is to bring financial support to local adults living with cancer through its Emergency Financial Assistance (EFA) grants, which help pay for rent, utilities, gas and food. The nonprofit also provides programming for children and adults. Since its founding in 2001, Angel Foundation has provided more than $10 million in emergency financial assistance grants to over 30,000 patients. A significant number of Twin Cities adults were already struggling with a cancer diagnosis when they lost their income due to COVD-19. These combined challenges put these patients in dire straits, and it was then that Angel Foundation saw a huge increase in the number of requests for assistance. To meet this unprecedented need, the Angel in Action (AiA) fund was created specifically for cancer patients impacted by the coronavirus outbreak. Modeled after the EFA program, Angel in Action Emergency Fund awarded $500 to each grantee and patients had 30 days to use the grant. Patients who qualified for the AiA grant could also receive an EFA grant in the same calendar year, for additional help. To qualify for AiA, recipients had to be at least 18 years old, in active treatment for cancer, including hospice and palliative care, and live in or be treated in the seven-county metro area. As you can imagine, the AiA fund provided a beacon of hope for many families. Here are a few examples of families who came to Angel Foundation this past spring for help and hope: • One grantee had been in active cancer treatment and was an in-demand piano player who had a full year of venues booked at the beginning of 2020. One by one, they were all canceled due to COVID. On top of that, his partner lost his income as a graphic designer and bartender, leaving the couple with zero income. He saw an
Angel Foundation billboard on the way to visit his parents and called immediately for help. • Another was diagnosed with breast cancer and had undergone chemo and surgery and was just starting radiation treatments when she lost her job due to COVID-19. • When a third grantee’s husband was diagnosed with cancer, she became the sole provider. And when her job put her at a higher risk of contracting coronavirus, she had to leave her position to prevent possibly exposing her immune-compromised husband who has a history of COPD. The AiA fund was available from March 24 through May 31, 2020. Here

are the final stats and a breakdown of who was helped:
Overview
• 202 Angel in Action applications received • 200 Angel in Action applications approved • $100,000 awarded
COVID-19 Primary Hardship
• 80% cited ability to work and their own and/or family member’s job or income loss due to COVID-19. • 20% indicated increased household costs — groceries, transportation, medical supplies, home care. • 8% were additionally impacted by
Hope Lodge closure and/or unexpected housing needs. • A handful also experienced postponement of their surgery—this affected other aspects of their life including ability to work.
Characteristics
Gender: • 60% female • 40% male
Age: • 51 average age
Race/Culture (of the 70% that identified): • 55% Caucasian • 28% African American • 12% Hispanic • 5% Other
30 different cancer types reported. Primary cancer types: • 27% breast cancer • 11% lung cancer • 7% leukemia
Counties of residence: • 70 Hennepin • 40 Ramsey • 21 Washington • 18 Dakota • 17 Anoka • 4 Carver • 3 Scott • 20 other counties represented
Distributions (Note that participant may receive more than one type of assistance)
• 62% requested grocery gift cards • 43% requested fuel gift cards • 40% requested rent/mortgage assistance • Small percentage also requested assistance with utility bills Angel Foundation raised the extra grant money a few different ways: a challenge matching gift from Dr. Mark and Margie Sborov; JNBA Financial Advisors, and individual donors. In addition to the AiA grant, the Angel Foundation had to change the structure of its very popular Camp Angel summer program. COVID-19 meant that approximately 200 kids could not unite in person for the camp, a silly and serious multi-day event for kids who have been impacted by a parent or caregiver’s cancer diagnosis. In its place, Angel Foundation rebranded the event to a virtual format with Camp Angel in a Box. Kids were given a big box full of typical camp supplies, curriculum of activities and a schedule. Kids were able to participate from the safety and security of their own homes via Zoom calls and independent activities. Angel Foundation received lots of happy feedback from families who appreciated the camp reboot and had lots of fun watching their kids participate in the creative activities. There have been countless heroes who have stepped forward during this year’s pandemic to raise spirits and show a commitment to their communities. Angel Foundation is grateful they were able to continue to support and serve cancer patients in meaningful ways.
Jennifer Kielas is Director of Financial Services, Angel Foundation. Jennifer has been with the Angel Foundation since 2012 and oversees the Emergency Financial Assistance and Financial Cancer Care programs. Her background also includes stints in law enforcement and the for-profit sector. Jen has a Master of Arts degree in Organizational Development from the University of Minnesota and lives with her husband and two teenagers in Eagan. Office: (612) 627-9000 ext. 502. Email: jkielas@mnangel.org.




est. 1978

Climate Change and COVID-19: Navigating the Twindemic
You may recall from Greek mythology the horrific decision Odysseus faced as he approached the Strait of Messina between Sicily and Calabria: should he pass by the six-headed sea monster Skylla on the Calabrian side and lose only a few sailors, or risk the loss of his entire ship in Charybdis, a whirlpool off the coast of Sicily? When the COVID-19 pandemic erupted in China in December 2019, public health leaders were forced to shift their attention from Charybdis —climate change, an existential threat to our species—to the more immediate peril posed by COVID-19. When I joined the Minnesota-based nonprofit organization, “Health Professionals for a Healthy Climate” (HPHC) in January 2015, my motive was personal. For the sake of my four grandchildren, I wanted to do whatever I could to help educate other health professionals about the momentous threat of climate change to human health. (For more information visit: www.hpforhc.org/.) Because of my professional background, four decades on the faculty of the University of Minnesota as an infectious diseases specialist, I immediately understood the role of climate change in fostering vector-borne infections, e.g., global warming and increased moisture favor the expansion of mosquitoes and ticks and thereby the pathogens that they carry. My physician colleagues in HPHC, Bruce Snyder and Mike Menzel, quickly brought me up to speed on the protean health consequences of climate change. Like a majority of the 140+ infections that have emerged in the past 50 years, it appears that COVID-19 is zoonotic, started in this case when a coronavirus (SARS-CoV-2) jumped from a bat in a wildlife market in China into a human. Like the wildfires ravaging California it has spread rapidly around the world, including Minnesota. As of early October the total number of cases passed 106,000 and deaths stood at over 2,100. Suffice it to say there are many parallels between the COVID-19 pandemic and climate change. Both are rooted in human disregard for each other as well as for other animals and our environment. And successful navigation of both, like sailing through the Strait of Messina, requires leadership of Odyssean proportions. Odysseus actually navigated a fleet of ships with a crew of 600 heroes, metaphorically akin to the large number of highly dedicated healthcare personnel battling COVID-19. At the helm, within our state we are fortunate to have Health Commissioner Jan Malcolm and Governor Tim Walz. And backing them, as well as many public leaders around the world, is Mike Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy. They are all guided by the same map—Science. And the really good news is that the crew includes many young, bright and energetic sailors who, I believe, will get us through these troubling waters.
BIMONTHLY 5
7.Complete Mailing Address of Known Office of Publication (Not printer) (Street, city, county, state, and ZIP+4 ®) 1300 GODWARD ST NE STE 2000 MINNEAPOLIS, MN 55413-1552
8.Complete Mailing Address of Headquarters or General Business Office of Publisher (Not printer) 1300 GODWARD ST NE STE 2000 MINNEAPOLIS, MN 55413-1552 $15.00
Contact Person NANCY BAUER
Telephone (Include area code) (612) 623-2893
9.Full Names and Complete Mailing Addresses of Publisher, Editor, and Managing Editor (Do not leave blank) Publisher (Name and complete mailing address) TWIN CITIES MEDICAL SOCIETY 1300 GODWARD ST NE STE 2000, MINNEAPOLIS, MN 55413
Editor (Name and complete mailing address)
NANCY BAUER 1300 GODWARD ST NE STE 2000, MINNEAPOLIS, MN 55413
Managing Editor (Name and complete mailing address)
NANCY BAUER 1300 GODWARD ST NE STE 2000, MINNEAPOLIS, MN 55413
10.Owner (Do not leave blank. If the publication is owned by a corporation, give the name and address of the corporation immediately followed by the names and addresses of all stockholders owning or holding 1 percent or more of the total amount of stock. If not owned by a corporation, give the names and addresses of the individual owners. If owned by a partnership or other unincorporated firm, give its name and address as well as those of each individual owner. If the publication is published by a nonprofit organization, give its name and address.)
Full Name Complete Mailing Address
TWIN CITIES MEDICAL SOCIETY 1300 GODWARD ST NE STE 2000, MINNEAPOLIS, MN 55413
11.Known Bondholders, Mortgagees, and Other Security Holders Owning or Holding 1 Percent or More of Total Amount of Bonds, Mortgages, or
Other Securities. If none, check box None
Full Name Complete Mailing Address
(For completion by nonprofit organizations authorized to mail at nonprofit rates) (Check one) The purpose, function, and nonprofit status of this organization and the exempt status for federal income tax purposes:
Has Not Changed During Preceding 12 Months
Has Changed During Preceding 12 Months (Publisher must submit explanation of change with this statement)
PS Form 3526, July 2014 [Page 1 of 4 (see instructions page 4)]13. Publication Title METRODOCTORS
PSN: 7530-01-000-9931
PRIVACY NOTICE: See our privacy policy on www.usps.com. 14. Issue Date for Circulation Data Below
09/01/2020
15. Extent and Nature of Circulation
Average No. Copies Each Issue During Preceding 12 Months No. Copies of Single Issue Published Nearest to Filing Date
a. Total Number of Copies (Net press run)
b. Paid
Circulation (By Mail and
Outside the Mail) (1) Mailed Outside-County Paid Subscriptions Stated on PS Form 3541 (Include paid distribution above nominal rate, advertiser’s proof copies, and exchange copies)
(2) Mailed In-County Paid Subscriptions Stated on PS Form 3541 (Include paid distribution above nominal rate, advertiser’s proof copies, and exchange copies)
(3) Paid Distribution Outside the Mails Including Sales Through Dealers and Carriers, Street Vendors, Counter Sales, and Other Paid Distribution Outside USPS®
(4) Paid Distribution by Other Classes of Mail Through the USPS (e.g., First-Class Mail®)
[Sum of 15b (1), (2), (3), and (4)]
d. Free or
Nominal
Rate
Distribution (By Mail and
Outside the Mail) (1) Free or Nominal Rate Outside-County Copies included on PS Form 3541
(2) Free or Nominal Rate In-County Copies Included on PS Form 3541
(3) Free or Nominal Rate Copies Mailed at Other Classes Through the USPS (e.g., First-Class Mail)
(4) Free or Nominal Rate Distribution Outside the Mail (Carriers or other means)
e. Total Free or Nominal Rate Distribution (Sum of 15d (1), (2), (3) and (4)) 1001
2486
0
0
3487
0
0
70
30
100 931
2331
0
0
3262
0
0
70
30
100
f. Total Distribution (Sum of 15c and 15e) 3587 3362
g. Copies not Distributed (See Instructions to Publishers #4 (page #3)) 68 138
h. Total (Sum of 15f and g) 3655 3500
i. Percent Paid (15c divided by 15f times 100) 97.21% 97.03% Statement of Ownership, Management, and Circulation * If you are claiming electronic copies, go to line 16 on page 3. If you are not claiming electronic copies, skip to line 17 on page 3. (All Periodicals Publications Except Requester Publications) 16. Electronic Copy Circulation
Average No. Copies Each Issue During Preceding 12 Months No. Copies of Single Issue Published Nearest to Filing Date
a. Paid Electronic Copies 0 0
b. Total Paid Print Copies (Line 15c) + Paid Electronic Copies (Line 16a) 3487 3262
d. Percent Paid (Both Print & Electronic Copies) (16b divided by 16c 100) 3587
97.21% 3362
I certify that 50% of all my distributed copies (electronic and print) are paid above a nominal price.
17. Publication of Statement of Ownership PS Form 3526, July 2014 (Page 2 of 4)
If the publication is a general publication, publication of this statement is required. Will be printed
in the ________________________ issue of this publication. 11/1/20
18. Signature and Title of Editor, Publisher, Business Manager, or Owner Publication not required.
Date
09/24/2020
I certify that all information furnished on this form is true and complete. I understand that anyone who furnishes false or misleading information on this form or who omits material or information requested on the form may be subject to criminal sanctions (including fines and imprisonment) and/or civil sanctions (including civil penalties).
Advance Care Planning Conversations and College Students
It’s never too early to begin the process of advance care planning (ACP), which includes having conversations about desires for end-of-life (EOL) care. But, do young adults recognize the importance of ACP and having conversations about EOL care? To explore this question, we (six undergraduate students and a professor of social work at St. Olaf College) partnered with Honoring Choices Minnesota, a state-wide ACP initiative led by the Twin Cities Medical Society. Our findings suggest that providers should engage college students in ACP and offer support, prompts and guidance for having conversations about EOL care.
Context
While prior research on healthy young adults and ACP conversations is limited, it does suggest that millennials are willing to have conversations about death, with 54% of surveyed college students having a previous conversation about EOL.1 These conversations have demonstrated benefits, including sharing of advance directives with friends and family,2 empowerment through sense of agency,3 avoiding unwanted medical interventions,3,4 and alleviating burden on family and friends to make medical decisions.3,4 Still, young adults face barriers to having ACP and EOL conversations. Some barriers include: the conversation can be viewed as culturally taboo within American society;5 the conversation can prompt challenging emotions from all participants;2,3 and, the belief that death only happens to those who are elderly.7 In this context of limited research and practice9 on EOL and ACP conversations in healthy young adults, we completed our exploratory project.
By Mary S. Carlsen, Zipi Diamond, Shannon holder and Christopher Prokosch
Exploratory Methods
Due to survey fatigue on campus, and a short academic term, our study was exploratory and did not use formal, validated data collection methods. We simply wanted to get some sense of students’ willingness to discuss EOL, therefore, we gathered students’ perspectives on ACP and EOL conversations using sticky notes. We offered sticky notes to the general student population (N = 2905) in popular campus locations, including the campus center and a heavily trafficked hallway. Respondents anonymously placed the notes in a box or on the wall. We also offered sticky notes to students in a classroom course, Frontiers in Aging (FiA), which included a unit on EOL care. Sticky note data from the general student population was separated from FiA data. Students were asked to answer any or all of the following questions: 1a. Have you ever had a conversation about the end of life with friends or family? 1b. If you’ve had a conversation, with whom, when and how? 1c. If not, what are some reasons you haven’t had a conversation about the end of life? 2a. Do you want to initiate a conversation about the end of life with friends or family? 2b. If so, what would help you initiate a conversation? In total, we collected 559 sticky note responses to the questions. We coded responses to questions 1a. and 2a. “yes” or “no.” Responses to the remaining questions were qualitatively coded for themes and subthemes.
Exploratory Findings
Student engagement in ACP and EOL conversations A majority of student responses indicated that students have had a conversation with either family or friends about the end of life (85% of responses collected in popular campus locations and 64% of responses from students in the Frontiers in Aging course). Compared to previous research, our exploration showed a greater percentage of young adults who have had ACP conversations; past research demonstrates that less than 30% of the general adult population has discussed death,8 and about 54% of millennials have had a conversation about death.1 We found that ACP and EOL conversations typically occurred with family members. Students most commonly had conversations for the following three reasons: experiencing personal death (e.g. of a family member), planning logistics following death (e.g. passing on monetary and material objects), and expressing EOL care preferences and decisions (e.g. nursing homes and palliative care). Barriers to ACP and EOL conversations Twenty two of the 559 responses indicated that students had not had a conversation about EOL, with 15 responses sharing potential barriers which included perceptions of being too young to discuss death, the conversation not being relevant, or having no personal experience with death. For example, one student shared “I haven’t lost any family members or people close to me, so it’s kind of an unspoken topic.” The barrier of being too young to discuss death supports previous research findings.7
ACP and EOL conversation desires A large majority of responses (83.9%) indicated a desire to have conversations about EOL care with family and/or friends. Many student responses (41%) indicated the desire for prompts and guidelines in order to facilitate ACP conversations. One student wrote “I wish that an outsider prompt would spark that conversation so I don’t have to bring it up myself.”
Many responses (33%) also discussed the importance of social environment when considering having an ACP or EOL conversation. For example, responses shared that creating a supportive environment to have the conversation may be helpful: “[forewarning] a friend so they seriously think about it prior to the conversation. Then sit down with predetermined goals and questions.” These findings support previous research indicating that ACP and EOL conversations may be emotional.2,3 While recognizing these challenges, students who engaged with our exploratory project desired support in facilitating ACP and EOL care conversations.
Limitations
This exploration had several limitations due to our non-traditional data collection format. We quantified sticky note responses and thus cannot conclude the number of total respondents or respondent demographics. Additionally, our survey questions did not specifically inquire as to why some students may not be interested in having ACP conversations. Lastly, student engagement was entirely voluntary, so findings likely reflect selection bias; students with more interest in the topic were probably more willing to write a note.
Conclusion
At St. Olaf College, students are having conversations about ACP. They are interested in preparing for their own and others’ EOL care and recognize the importance of ACP. While previous research suggests that ACP conversations are seen as taboo, our exploratory study did not find that this was a barrier for our students interested in having ACP conversations. Still, some students shared their belief that ACP conversations were not necessary because they were too young to think about death. However, students who did want to have these conversations expressed that prompts, guidelines and supportive environments would be helpful. Our findings suggest that providers should consider the importance of engaging young adults and college students in ACP and EOL conversations and offer prompts, guidelines and tips for creating a supportive environment to have these conversations. Our results also emphasize the need for more rigorous research with young adults about EOL conversations. Future studies could explore the effectiveness of various prompts and guidelines that providers can use to engage young adults in conversations about death.
Young Adults Talk About Death, a video about our experience as college students conducting this research and considering the importance of ACP, is available on the Honoring Choices Minnesota website. The site features a rich set of resources, including conversation starters. (bit.ly/ YoungAdultsTalkAboutDeath.) Acknowledgements: Mari Quanbeck, Kali Weiss and Natalie Wussler contributed to the design and implementation of the study.
Mary S. Carlsen, Professor of Social Work and Family Studies, St. Olaf College. Zipi Diamond, 2020, BA Sociology/ Anthropology. Shannon Holder, 2019, BA Chemistry. Christopher Prokosch, 2019, BA Chemistry. References available upon request.
PRACTICE WHERE
BREAKTHROUGHS HAPPEN EVERY DAY
M Health Fairview is the newly expanded collaboration among the University of Minnesota, University of Minnesota Physicians, and Fairview Health Services. Help us transform healthcare by joining our more than 5,000 physicians and providers across 10 hospitals, 60 primary clinics, and 100+ specialties.
Visit: Fairview.org/careers Email: recruit1@fairview.org Call: 800-842-6469
TTY 612-672-7300 EEO/AA Employer
Career oPPortunItIes
Lakeview Clinic has what you are looking for! Join an independent, physicianowned group of 50 providers in the SW Metro. Be a part of a collaborative work environment in a primary care group of family physicians, internists, pediatricians, general surgeons and OB/GYNs. • 4-day work week with 32 contact hours achieving excellent work/life balance

• Excellent compensation with a 2-year partnership track to earn in the top 10% in the state
• Outstanding benefits including 100% paid family health insurance and dental insurance, 401K and profit sharing
• We have 4 sites in the southwest metro:
Chaska, Waconia, Norwood, and Watertown

Due to retirements and growth, we are currently looking for: ◦ Internal Medicine
CONTACT: administration@lakeviewclinic.com PHONE: 952-442-4461 ext. 7215 WEB: www.lakeviewclinic.com
of Twin Cities Medicine
By Regina Martínez, MP h UMN MD Candidate 2021 MD h Epidemiologist
Minnesota CovidSitters
Many of us were on clinical rotations when the COVID-19 pandemic hit. Overnight, we were pulled out of the hospital. Dozens of our classmates met over zoom to discuss ways to help our colleagues on the frontlines. We realized that despite not being able to care for patients, we could still support our healthcare family in non-traditional roles. MN CovidSitters came to life within a two-day span after an overwhelming, yet inspiring, amount of collaboration, determination and grit. Throughout the past six months, we have babysat for 250+ healthcare worker families in the Twin Cities, pet-sat 38 furry friends, and run over 160 errands free of cost. We have 30 sister CovidSitters organizations in the US. Additionally, more than 100 other individuals and groups have reached out for help with similar projects. As our project launched, we shared our plans with students in Canada, the UK and even Sudan. Everyone was looking for a way to repurpose their skills and maximize their support for healthcare workers. Importantly, we appreciate that health care is so much more than doctors and nurses—environmental and dining services staff, interpreter services, social workers, public health workers all keep the heart of health care beating. Our mission is to serve them all. Using the streamlined processes facilitated by Clinician Nexus, we pair healthcare worker families with volunteers. We have diverse representation of the student body on our board and in our volunteer workforce —undergraduates, graduate students and professional students contribute their skill set to develop and improve our programs. In many ways, CovidSitters is a real-time learning lab where we put our education to use as we navigate all the uncertainty this pandemic brings. Most importantly, our lifeblood consists of hundreds of volunteers enrolled in local colleges. They are the true heroes on the “second lines” of the COVID-19 battlefields. We are also excited to announce that this July we became a 501c3 nonprofit organization and in August we began offering adult respite care services to care for seniors and adults with disabilities. We recognize that not everyone can participate as volunteers, and that engagement with relief efforts looks different for every person. Our sustainability relies on the generosity of the community. Of course, our priority is the health and safety of our volunteers. Our risk mitigation team is led by MD candidates
An inside look into one of the PR Team's meetings as they plan for new adult respite care services and a fundraising campaign.

with previous public health backgrounds and is informed by the most up-to-date guidelines offered by state and federal expertise. Healthcare workers and volunteers are placed in “pods” of 2-3 students to minimize exposures and all participating parties agree to report any symptoms or potential exposures. To date we have not had any confirmed cases of COVID-19 impacting our families or volunteers, and any suspected exposures were managed and tracked. We extend our sincerest gratitude for everything that our healthcare families have done for our community over the past six months. We are proud to serve our teachers, healers and friends, and expect to remain a source of support for the duration of the pandemic. We also acknowledge that while the pandemic has hit us all, it has hit us in different ways. We are especially grateful to our BIPOC healthcare workers who have had to walk through so many layers of tragedy. We are here for you. We stand with you. We support you. We are here to learn from you. As children go back to school—online or in person, it is important for all of us to remember that we all have a stake in raising the next generation. It’s a task that is impossible to accomplish without the full support of a community. In many ways, CovidSitters is a direct reflection of all the support and love our communities have offered us in times of need. Your continued support as volunteers, donors, mentors and cheerleaders keeps us going. Please feel free to use our services, volunteer, or donate at: https://www.mncovidsitters.org/.

