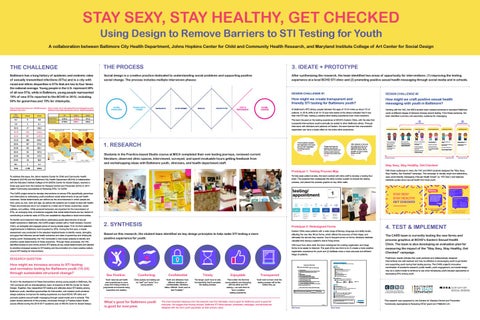
STAY SEXY, STAY HEALTHY, GET CHECKED Using Design to Remove Barriers to STI Testing for Youth A collaboration between Baltimore City Health Department, Johns Hopkins Center for Child and Community Health Research, and Maryland Institute College of Art Center for Social Design
THE CHALLENGE
THE PROCESS
3. IDEATE + PROTOTYPE
Baltimore has a long history of epidemic and endemic rates of sexually transmitted infections (STIs) and is a city with racial and ethnic disparities in STIs that are two to four times the national average. Young people in the U.S. represent 50% of all new STIs, while in Baltimore, young people represented 70% of new STIs reported to the BCHD in 2012, including 60% for gonorrhea and 70% for chlamydia.
Social design is a creative practice dedicated to understanding social problems and supporting positive social change. The process includes multiple interwoven phases:
After synthesizing the research, the team identified two areas of opportunity for interventions: (1) improving the testing experience at a local BCHD STI clinic and (2) promoting positive sexual health messaging through social media and in schools.
Rate of Gonorrhea Cases per 100,000 persons Rate of youth 10-19 with gonorrhea and chlamydia by race Baltimore City 2009 (Age-specific rate per 100,000 population) Baltimore City 2013 Age Groups
Cases
0-4
0
0.0
5-9
3
8.1
10-14
47
136.5
15-19
529
1,343.2
20-24
687
1,257.3
25-29
389
649.9
30-34 35-39
187 104
All
Black
White
Gonorrhea
1234.5
1329.8
141.5
Chlamydia
4778.9
5589.1
449.9
Rates
375.6 283.1
40-44
63
167.9
45-54
116
137.5
55-64
28
38.6
65+
4
5.4
Total
2,158
346.6
DESIGN CHALLENGE #1
DESIGN CHALLENGE #2
How might we create transparent and friendly STI testing for Baltimore youth?
How might we craft positive sexual health messaging with youth in Baltimore?
At Baltimore’s STD clinics, people between the ages of 15-24 make up about 1/3 of patients. In 2016, 65% of all 15-19 year olds tested at the clinics indicated that it was their first STI test, making a positive clinic testing experience even more important.
Working with the YAC, the MICA student team created personas to represent Baltimore youth at different stages of behavior change around testing. From these personas, the team identified a primary and secondary audience for messaging.
The team focused on the testing experience at BCHD’s Eastern Clinic, with the idea that successful interventions could eventually be scaled to other Baltimore clinics. Through interviews with clinicians and patience at Eastern, the team learned that unsuccessful registration can have a ripple effect on the entire clinic experience.
1. RESEARCH
“A lot of patients complain that registration is the worst part and after registration everything is great.” PROVIDER
Students in the Practice-based Studio course at MICA completed their own testing journeys, reviewed current literature, observed clinic spaces, interviewed, surveyed, and spent invaluable hours getting feedback from and workshopping ideas with Baltimore youth, clinicians, and health department staff.
“After waiting for an hour just to be called up to turn in my registration forms I lost all faith that I would be able to complete my visit in a timely fashion, so I left.”
“People don’t know the process, and when you don’t know the process you become anxious because you don’t know what’s next.”
2
PRIMARY AUDIENCE
Do DoNothing Nothing Danny &&Danielle Danielle Only-if-Necessary Only-if-Necessary Only-if-Necessary Owen &&Olive Olive Do Nothing DannyDanny & Danielle OwenOwen & Olive
Hesitant Hesitant Haley &&Harry Harry Hesitant HaleyHaley & Harry
• Littleknowledge knowledge STIs Little • Little •knowledge of STIsofofSTIs
• fence Onthe thefence fenceabout aboutgetting gettingtested tested • On • On the about getting tested
Never • Never been beentested testedbefore before • Never• been tested before
•only Would only gettested there • Would only get • Would get tested iftested thereif ifthere BIGmotivator motivator likeshowing showing isis a aBIG like is a BIG motivator like showing symptoms and theirpartners partners symptoms and their symptoms and their partners saying theyshould should gettested tested they get sayingsaying they should get tested
• Doesn’t have timetotoget get • Doesn’t have • Doesn’t have time totime get tested STIs forforSTIs testedtested for STIs
• Uneducated • Uneducated and andunmotivated unmotivated • Uneducated and unmotivated about about STI STItesting testing about STI testing • Not • Notreceiving receiving any anyguidance guidance • Not receiving any guidance about about STI STItesting testing about STI testing
Motivated Motivated Michelle Michelle &&Malik Malik Motivated Michelle & Malik
Healthy Healthy Henry Henry &&Heather Heather Healthy Henry & Heather
Neutral Neutral Nancy Nancy &&Nick Nick Neutral Nancy & Nick
??
• “It •never “Itcan can never neverhappen happen me” • “It can happen to me”totome” • Refuses • Refuses totoget gettested tested • Refuses to get tested
SECONDARY AUDIENCE
• Wants •to Wants toget gettested, tested, butisis • Wants get to tested, but is but unsure ofofwhere unsureunsure of where towhere go totogogo
Gets • Getstested testedregularly regularly and andforfor • Gets• tested regularly and for allallSTIs STIs all STIs
• Neutral onthe theissue issuebecause because • Neutral • Neutral on theonissue because they have not hadsex sex they have not had they have not had sex
• Doesn’t • Doesn’t have havetransportation transportation • Doesn’t have transportation
• Knowledgeable • Knowledgeable abouthealthy healthy sex, • Knowledgeable aboutabout healthy sex, sex, STIs, STIs, and andtesting testing STIs, and testing
• Feel that thisissue issuedoes doesnot not Feel that this • Feel•that this issue does not themYET YET totothem applyapply toapply them YET
• Hasdistrust distrust localclinics clinics • Has forfor local • Has distrust for local clinics
• Has • Hasdistrust distrust forfor local localclinics clinics • Has distrust for local clinics
• Isworried worried aboutfriends friendsand and • Is • Is worried about about friends and familyknowing knowing family family knowing
• Has •solid Hasasupport asolid solidsupport support system, system, but • Has a system, but but they they donot not talk talkabout about sex, sex,STIs, STIs, they do notdo talk about sex, STIs, orortesting testing or testing
• Know doforfortheir their it’sit’ssmart totodo • Know• Know it’s smart tosmart do for their health, butconcerns manyconcerns concerns but many health,health, but many prevent them fromtesting testing prevent them from prevent them from testing
Has • Hasregular regular doctor’s doctor’s check-ups check-ups • Has •regular doctor’s check-ups •support Hasa asupport support system system that thatopenly openly • Has •aHas system that openly discusses discusses sex, sex,and STIs, STIs, and andtesting testing discusses sex, STIs, testing
Likely to Get Tested
Not NotLikely Likely toGet GetTested Tested Not Likely to GettoTested
Likely Likely toto Get GetTested Tested Likely to Get Tested
Not Sexually Active Yet No NoNeed Need for forTesting Testing No Need for Testing
Stay Sexy, Stay Healthy, Get Checked Prototype 1: Testing Process Map To help ease patient anxiety, the team worked with clinic staff to develop a testing flow chart. The students then redesigned the clinic number system to include the testing process, and placed the process graphic on key clinic walls.
With these audiences in mind, the YAC and MICA students designed the “Stay Sexy, Stay Healthy, Get Checked” campaign. The campaign is visually bright and celebratory, uses youth-friendly messaging (“Sexual Health Check” vs. “STI Test,”) and features relatable quotes about sexual health from local youth.
What does sexual health mean to you?
1
STAY SEXY STAY HEALTHY GET CHECKED
“Knowing about the outcomes of your decision, keeping up with your physical sexual health and being aware of your sexual agency.
”
– DeAndrea, 16 Dundalk
#staysexystayhealthy STAY SEXY, STAY HEALTHY, GET CHECKED
#staysexystayhealthy
2. SYNTHESIS
Prototype 2: Redesigned Forms Eastern Clinic sees patients with a wide range of literacy, language and ability levels, affecting the way they fill out forms, which affects the accuracy of their triage, and ultimately the service they receive. Due to frequent errors on forms, clinicians dedicate valuable time during a patient’s visit to fixing errors.
Based on this research, the student team identified six key design principles to help make STI testing a more positive experience for youth:
With input from clinic staff, the team redesigned the existing registration and triage forms to be easier to interpret. The goal of the new form is to (1) create a more positive registration experience for youth and (2) facilitate more a more accurate and efficient triage of patients.
Tell us why you’re here so we can help you get registered (Check all that apply)
Registration Information
testing
Why are you here? [Please check all that apply]
Sex Positive
Comforting
Confidential
Timely
Enjoyable
Transparent
Youth need sexual health care experiences to move away from being punitive or judgmental and towards being supportive and positive.
Clinic spaces and testing can be “cold” and “scary” to a young person.
Youth and clinicians have different definitions of confidentiality. Clinicians follow HIPAA6. Youth want to feel “invisible.”
The longer youth have to wait, the less likely they’ll complete the testing process.
This is often the first time young patients are interacting with the clinic and STI testing— we want them to have a positive testing experience.
Youth want to know what the testing process will be like before they go.
I HAVE symptoms Painful or burning urination Discharge (draining, drip) from penis, vagina or rectum
Painful urination Discharge (draining, drip) from penis, vagina or rectum Sore/Bumps on penis, vagina, rectum or mouth Rash Vaginal itching Abdominal pain (females only) Pain in rectum, penis, testicles or vagina I am pregnant or I think I may be pregnant I am over 21 and I have not had a Pap smear (test for cervical cancer) in over 2 years I am here for a hepatitis vaccine Someone told me to come get checked out for an STD I was given a blue/yellow or /pink card I received a letter telling me one of my tests was positive Other non-STD-related reason
4. TEST & IMPLEMENT The CARS team is currently testing the new forms and process graphics at BCHD’s Eastern Sexual Health Clinic. The team is also developing an evaluation plan for measuring the impact of the “Stay Sexy, Stay Healthy, Get Checked” campaign. Preliminary results indicate that youth-centered and collaboratively designed interventions are well received and may be effective in encouraging youth to get tested and supporting youth during their testing journey. The CARS project’s innovative combination of academic research, public health, youth engagement, and social design may be a useful model to continue to use when developing youth-focused approaches to decreasing STIs among youth.
how can we help you?
CARS@ HTN Poster_FINAL_11.20.17.indd 1
Secondary Secondary Audience Audience Secondary Audience
1
Not Likely to Get Tested
RESEARCH QUESTION
To aid in the development of these interventions among young people in Baltimore, the YAC partnered with an interdisciplinary team of students at MICA’s Center for Social Design. Together, they researched STI testing and attitudes about STI testing among Baltimore youth, identified opportunities for intervention, and created youth-centered design solutions to improve the testing experience at a local BCHD STI clinic and promote positive sexual health messaging through social media and in schools. This poster shares elements of this process, conducted through a Practice-based Studio course offered during the 2016-2017 academic year at MICA’s Centr for Social Design.
2 22
PATIENT
PROVIDER
The CARS project aimed to develop interventions to reduce STIs (specifically gonorrhea and chlamydia) by addressing youth-prioritized social determinants of sexual health outcomes. Social determinants are defined as the circumstances in which people are born, grow up, live, work and age, as well as the systems put in place to deal with health. These circumstances are in turn shaped by a wider set of forces: economics, social policies, and politics. While personal behaviors are important for the transmission of STIs, an emerging body of evidence suggests that social determinants are key factors in contributing to endemic rates of STIs and racial/ethnic disparities in local communities.
How might we increase access to STI testing and normalize testing for Baltimore youth (15-24) through sustainable structural change?
11
Primary Primary Audience Audience Primary Audience
?
To address this issue, the Johns Hopkins Center for Child and Community Health Research (CCHR) and the Baltimore City Health Department (BCHD) in collaboration with the Maryland Institute College of Art (MICA) Center for Social Design, received a three-year grant from the Centers for Disease Control and Prevention (CDC) in 2014 called “Community Approaches to Reducing STIs,” or CARS.
To identify and implement interventions addressing social determinants of sexual health outcomes in Baltimore, the CARS project worked with a Youth Advisory Council (YAC), an energetic and engaged group of young people (ages 15 to 24) from selected neighborhoods in Baltimore most impacted by STIs. During the first year, a needs assessment was conducted in the selected neighborhoods to identify needs, strengths, and gaps that influence sexual health outcomes and rates of gonorrhea and chlamydia among youth. Subsequently, the YAC conducted a root cause analysis to identify and prioritize social determinants of these outcomes. Through these processes, the YAC identified access to and norms around STI testing as key social determinants and elected to prioritize increased access to STI testing and the promotion of a more positive culture around STI testing for interventions.
1
Sore/bumps on penis, vagina, rectum or mouth Rash Vaginal itching or burning Pain in rectum, penis, testicles or vagina Abdominal pain (females only) I am pregnant or think I may be pregnant I have NO symptoms I don’t have symptoms, only need a routine STD check-up My partner has an STD and asked me to come get tested: HIV
Syphilis
Chlamydia
Hepatitis (B or C)
Gonorrhea
Trichomonas
I don’t know
results I am here to collect results
I am here for results but still have symptoms
None of the above-I only need STD testing
I was given a Blue/Yellow/Pink card or received a call from the clinic to come in I received a letter telling me one of my tests was positive
If you check “None of the above” and that is not correct you will be asked to reregister and may not be seen by a clinician today. ___________ (please, initial)
other I am here for blood test only -
HIV
Hepatitis
Syphilis
I am here for 2nd / 3rd Bicillin shot (syphillis treatment) I am here for a follow-up appointment I am over 21 and not had a Pap smear (cervical cancer test) in over 3 years Other Reason: ____________________________________________________
What’s good for Baltimore youth is good for everyone.
The most important takeaway from the research was that ultimately, what is good for Baltimore youth is good for everyone. We suggest that moving forward, Baltimore STI clinic spaces, processes, messages, and services are designed with the city’s youth population as their primary users.
I understand if the information I enter is incorrect, I can be asked to re-register and may not be seen by a clinician today. Signature:
Version 8-30-13
Old Form
Date:
thank you! Baltimore City Health Department Division of Clinical Services, Sexual Health Clinic
This research was supported by the Centers for Disease Control and Prevention “Community Approaches to Reducing STDs” grant U22 PS004541-01.
New Form
11/20/17 1:23 PM