The Career and Education Resource for the Minority Nursing Professional • FALL 2013
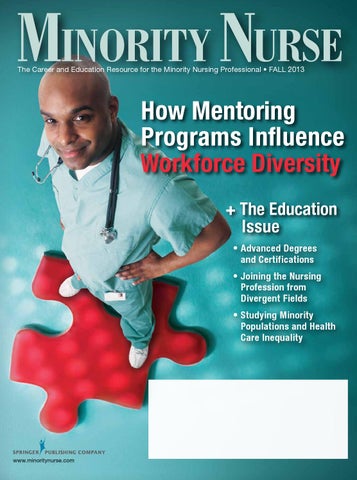
How Mentoring Programs Influence Workforce Diversity + The Education Issue •A dvanced Degrees and Certifications • J oining the Nursing Profession from Divergent Fields •S tudying Minority Populations and Health Care Inequality
www.minoritynurse.com
Handbook of
MINORITY AGING EDITED BY
KEITH WHITFIELD, PhD TAMARA BAKER, PhD
T
his text provides up-to-date, multidisciplinary, and comprehensive information about aging among diverse racial and ethnic populations in the United States. It is the only book to focus on paramount public health issues as they relate to older minority Americans, and addresses social, behavioral, and biological concerns for this population. The text distills the most important advances in the science of minority aging and incorporates the evidence of scholars in gerontology, anthropology, psychology, public health, sociology, social work, biology, medicine, and nursing. July 2013 · 592 pp · Softcover · 978-0-8261-0963-7
Key Features: • Offers “one-stop shopping” regarding the development of a substantial knowledge base about minority aging • Provides current, comprehensive information about minority aging through a multidisciplinary lens • Includes recent progressive research pertaining to the social, cultural, psychological and health needs of elderly minority adults in the US • Integrates information from scholars in gerontology, anthropology, psychology, public health, sociology, social work, biology, medicine, and nursing
Don’t Miss Another Issue of
Minority Nurse! America’s most respected publication for practicing minority nurses and nursing students is now available by individual subscription! Minority Nurse is a must-read! Each issue comes to you packed with in-depth articles on hot topics in nursing, minority health issues, and profiles of outstanding minority nurse role models. Plus, advance your career with pages full of professional resources.
YES! I want a personal subscription to Minority Nurse magazine! Please send my one-year (4 issues) subscription for $19.95 to:
Payment Information (please check one payment option)
Name __________________________________
Credit Card #_________________________________ Expiration Date _____________
Address_________________________________
Verification # ________________ (last three digits on back of card)
_______________________________________
Name as it Appears on Card ________________________________________________
City ____________________________________
Cardholder Billing Address (only if different than subscription destination address)
State ______________ ZIP ________________
Name ________________________________________________________________
Phone __________________________________
Address_______________________________________________________________
Fax ____________________________________
City______________________________ State _______ ZIP ____________________
E-mail __________________________________
Signature of Cardholder___________________________ Date____________________
q My check for $19.95 is enclosed (please make check payable to Springer Publishing Company) q Please charge $19.95 to my credit card (appears as a charge from Springer Publishing Company) Credit Card Type (please check one):
q MasterCard
q VISA
(required)
e Sav Off SuE r IS 70% E PE rICE Th VEr P Co
Order personal or institutional subscriptions at
www.minoritynurse.com/subscriptions Fax or mail this completed form to: Circulation Dept., c/o Springer Publishing, 11 West 42nd Street, 15th Floor, New York, NY 10036 Phone: 212-431-4370 · Fax: 212-941-7842
Table of Contents
In Every Issue
Cover Story
3
Editor’s Notebook
4
Vital Signs
9
Making Rounds
Diversity
48
In the Spotlight
By Christine Hinz
49
Highlights from the Blog
Discover how mentoring can give you the necessary leg-up in
56
Index of Advertisers
fine-tuning your skills and broadening your career options
Academic Forum 37 An American Journey: From Constipation to Colorectal Cancer By Ed James, MD An overview of common colorectal conditions Americans face and the role a healthy diet can play in preventing them 38 Keeping Back Pain at Bay By Terah Shelton Harris Find out how to avoid back pain despite long shifts and heavy lifting
10 How Mentoring Programs Influence Workforce
Features 19 Studying Disparities: How Nursing Schools Cover Minority Populations and Health Care Inequality By Margarette Burnette An examination of how nursing schools report on racial disparities and the best practices they teach to address them
24 Advanced Degrees and Certifications: What
Second Opinion
You Need to Succeed
40 Honesty and Ethics in Nursing By Jebra Turner Recognize the public’s trust in nurses and embrace your role as a patient advocate
By Pam Chwedyk
42 Technology in the Workplace: How You Can Prepare By Nikki Yeager Don’t let technology put you on the wrong side of the digital divide
Degrees of Success 44
Growing the Numbers of Diverse Nursing Faculty By Robin Farmer The advantages of diverse academic role models
46 Racial Disparities of Nursing Educators and Students By Eliss Cucchiara The correlation between culturally competent care and diverse nursing faculty
2
Minority Nurse | FALL 2013
Learn more about the benefits of pursuing higher education and the credentials that will open the door to rewarding advanced practice careers and leadership roles
32 New to Nursing: Joining the Profession from Divergent Fields By Leigh Page Considering a career change? Find out how others made the switch and what motivated them to make the leap
Editor’s Notebook:
CORPORATE HEADQUARTERS/ EDITORIAL OFFICE
Inspiration is Key
W
hat made you want to pursue an education in nursing? The most common reply I see to this question is “I want to help people,” which may be true enough, but go beneath the surface and you will most likely find that there was someone in your life who inspired you to help others first. Maybe a hospice nurse eased your mother’s passing, or a boss recognized your leadership qualities and took you under her wing. Be it a nurse, a family member, or a coworker, a mentor comes in many forms. And a random act of kindness may be all it takes for inspiration to strike. In our cover story, Christine Hinz highlights the importance of mentorship and the positive influence it has on diversifying the workplace. On a similar note, Eliss Cucchiara and Robin Farmer discuss the racial disparities of nursing educators and the steps we can take to recruit more minorities into nursing. The benefits of having diverse faculty are twofold: it will broaden your knowledge on delivering culturally competent health care to a diverse nation; and it will encourage others to follow suit. In turn, this will help eliminate racial health disparities. In Margarette Burnette’s article, she investigates how nursing schools are covering minority populations and health care inequality in our country. There is a reason inequality exists—and nurses are in a powerful position to do something about it. According to the most recent Gallup Poll on honesty and ethics in professions, nursing is once again the most trusted profession. Jebra Turner explores the reasoning behind this and gives you tips for upholding that hard-earned trust. Trustworthy or not, everyone needs a little guidance now and then. A mentor’s knowledge can be invaluable whether you are just graduating from college, considering a career change, or contemplating retirement. It’s never too late for a career shift, as Leigh Page’s article on second-career nurses demonstrates. And once you have made the decision, Pam Chwedyk will equip you with the knowledge to determine which degrees you need on your nursing journey. Finally, check out our latest In the Spotlight column (and our blog at www. minoritynurse.com/blog) for a little dose of inspiration. Wherever your journey may take you, learn to inspire others, and let them inspire you. After all, inspiration is contagious. — Megan Larkin
11 West 42nd Street, 15th Floor New York, NY 10036 212-431-4370 n Fax: 212-941-7842
SPRINGER PUBLISHING COMPANY
President & CEO Theodore Nardin Vice President & CFO Jeffrey Meltzer
MINORITY NURSE MAGAZINE Publisher James Costello Editor-in-Chief Megan Larkin
Creative Director Mimi Flow
Circulation Latoya Butterfield
Production Manager Diana Osborne Digital Media Manager Joey Stern Minority Nurse National Sales Manager Peter Fuhrman 609-890-2190 n Fax: 609-890-2108 pfuhrman@springerpub.com Minority Nurse Editorial Advisory Board Jose Alejandro, PhD, RN-BC, MBA, CCM, FACHE President National Association of Hispanic Nurses Teresita Bushey, MA, APR-BC Assistant Professor, School of Nursing The College of St. Scholastica Wallena Gould, CRNA, MSN Founder and Chair Diversity in Nurse Anesthesia Mentorship Program Constance Smith Hendricks, PhD, RN, FAAN Professor Auburn University School of Nursing Ed James, MD Founder and President Heal2BFree, LLC Sandra Millon-Underwood, PhD, RN, FAAN Professor University of Wisconsin, Milwaukee, College of Nursing
Minority Nurse (ISSN: 1076-7223) is published four times per year by Springer Publishing Company, LLC, New York. Articles and columns published in Minority Nurse represent the viewpoints of the authors and not necessarily those of the editorial staff. The publisher is not responsible for unsolicited manuscripts or other materials. This publication is designed to provide accurate information in regard to its subject matter. It is distributed with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice or other expert assistance is required, the services of a competent professional person should be sought. The publisher does not control and is not responsible for the content of advertising material in this publication, nor for the recruitment or employment practices of the employers placing advertisements herein. Throughout this issue we use trademarked names. Instead of using a trademark symbol with each occurrence, we state that we are using the names in an editorial fashion to the benefit of the trademark owner, with no intention of infringement of the trademark.
Tri Pham, PhD, RN, AOCNP-BC, ANP-BC Nurse Practitioner The University of Texas-MD Anderson Cancer Center Ronnie Ursin, DNP, MBA, RN, NEA-BC Parliamentarian National Black Nurses Association
Subscription Rates: One year print subscription USA and Canada: Individuals, $19.95/year; Institutions, $35/year. Visit www. minoritynurse.com to subscribe. Change of Address: To ensure delivery we must receive notification of your address change at least eight weeks prior to publication. Address all subscription inquiries to Springer Publishing Company, LLC, 11 West 42nd Street, 15th Floor, New York, New York 10036-8002 or e-mail subscriptions@springerpub.com.
For editorial inquiries and submissions:
Claims: Claims for missing issues will be serviced pending availability of issues for three months only from the cover date (six months for issues sent out of the U.S.). Single copy prices will be charged for replacement issues after that time.
For subscription inquiries and address changes:
Minority Nurse ® is a registered trademark of Springer Publishing Company, LLC.
editor@minoritynurse.com admin@minoritynurse.com
© Copyright 2013 Springer Publishing Company, LLC. All rights reserved. Reproduction, distribution, or translation without express written permission is strictly prohibited.
www.minoritynurse.com
Minority Nurse Magazine
3
@MinorityNurse
Vital Signs
High Job Satisfaction among Public Health Nurses, But Many State Health Departments Struggle to Fill Vacancies Public health nurses play an essential role in improving the population’s health and delivering essential health services to communities, but the public health nursing workforce is facing significant challenges. More than two in five state health departments report having “a great deal of difficulty” hiring nurses, and nearly 40% of state and local health departments report having insufficient resources to fill vacant nurse positions.
T
hose are among the findings of a report released by the Robert Wood Johnson Foundation (RWJF), which provides the first comprehensive assessment of the size, composition, educational background, experience, retirement intention, job function, and job satisfaction
4
Minority Nurse | FALL 2013
of nurses who work for state and local health departments. Enumeration and Characterization of the Public Health Nurse Workforce: Findings of the 2012 Public Health Nurse Workforce Surveys, produced by the University of Michigan Center of Excellence in Public Health Workforce Studies and funded
by RWJF, collected data from state and local public health departments and surveyed public health nurses themselves. It finds that public health nurses report concerns about job stability, compensation, and career growth in light of budget-tightening at many state and local health departments. Yet these nurses also report very high levels of job satisfaction and that they feel they are making a difference in their communities—factors that could bolster recruitment efforts. “Capturing this data about public health nurses, who represent the largest profes-
sional sector of the public health workforce, gives us a clearer picture of the challenges before us,” said Pamela G. Russo, MD, MPH, RWJF senior program officer. “It should be a high priority to address gaps and take steps to strengthen the public health nursing workforce. As health reform is implemented, and as public health agencies are transforming to a more population-health-oriented role in promoting health and protecting communities, public health nurses will need additional training to keep pace with the changes. The size, makeup, and preparation of
Vital Signs the public health nursing workforce greatly affect the ability of agencies to protect and improve the health of people in their jurisdictions.” The new report offers a snapshot of the current public health nurse workforce— estimated at 34,521 full-time equivalent RNs—and highlights the need for ongoing systematic monitoring in order to: inform competency, compliance, and credentialing efforts; permit better alignment of academic resources with workforce needs; and allow for better understanding of the relationship between workforce infrastructure and population health outcomes.
Among its findings: • Nearly two in five respondents to the survey (39%) report that their highest nursing degree is a diploma/associate’s degree. Just 10 states require public health nurses to have BSN degrees. • Providing clinical services is part of the work done by RNs in state and local health departments, but these nurses assume a wide variety of roles, including health promotion, disease surveillance, community health assessment, policy development, and more. • The public health nursing workforce does not reflect the diversity of the communities it serves. Just 4% of public health nurses self-identify as Hispanic/Latino and 95% of those in leadership positions self-identify as white. • The public health nurse workforce is aging; however, most RNs do not intend to retire within the next five years. • Recruitment and hiring of RNs into public health nurses positions can be challenging,
particularly for state health departments. • Lack of promotion opportunities is a concern to both health departments and RNs. • Public health nurses report extremely high levels of job satisfaction, despite reporting high levels of dissatisfaction with salaries.
Recommendations in the report, created by the project’s advisory committee, include: • Develop feasible opportunities for additional education and training for public health nurses. • Improve the pipeline and intensify recruitment so public health nurses in health departments reflect the racial and ethnic composition of the communities they serve. Determine how changes in the functions of public health departments, due to health care reform and the transformation of public health agencies’ work, may affect the education public health nurses need. • Identify options to address concerns about recruitment, compensation, and promotion opportunities. • Conduct follow-up studies to monitor size, composition, capacity, and functions of the public health nurse workforce over time, to help ensure this workforce is well-prepared to meet emerging needs. “The nation depends on a strong public health nursing workforce, and these surveys identify clear challenges that federal, state, and local policymakers, health agencies, and academic and philanthropic leaders can address,” said Matthew L. Boulton, MD, MPH, director of the Center of Excellence in Public Health Workforce Studies and associ-
ate professor at the University of Michigan School of Public Health (UMSPH). “We shouldn’t overlook the importance of positive findings related to job satisfaction,” added Angela J. Beck, PhD, MPH, the Center’s associate director and research assistant professor at UMSPH. “With 85% of public health nurses reporting job satisfaction and 90% reporting that they feel they make a difference in the health of their communities, we have a strong foundation to build on.” Several earlier national studies have attempted to count public health nurses in specific settings, but until now there has been little data collected on the characteristics of the public health nursing workforce as a whole. This limitation has made it difficult to determine the most strategic and sustainable approaches to
www.minoritynurse.com
providing training that will increase the skills and impact of this essential workforce. For this report, RWJF commissioned both organizationaland individual-level public health nurse workforce surveys, conducted by the University of Michigan Center of Excellence in Public Health Workforce Studies, to address these gaps in knowledge. A public health nursing research agenda, established in 2010 by a collaborative working group of leaders in public health nursing, emphasized developing a better understanding of how metrics related to public health nursing impact population health. The recent Enumeration and Characterization of the Public Health Nurse Workforce report provides baseline data that can further this research agenda. For more information, visit www.rwjf.org.
Minority Nurse Magazine
5
@MinorityNurse
Vital Signs
Healthy Life Expectancies at Age 65 Highest in Hawaii, Lowest in Mississippi Residents of the South regardless of race, and blacks throughout the United States, have lower healthy life expectancy at age 65, according to a recent report in the Morbidity and Mortality Weekly Report released by the Centers for Disease Control and Prevention (CDC). Healthy life expectancy (HLE) is a population health measure that estimates expected years of life in good health for people at a given age.
T
he CDC used 20072009 data from the National Vital Statistics Systems, US Census Bureau, and Behavioral Risk Factor Surveillance System to calculate HLEs by sex and race for each of the 50 states and Washington, DC, for all people aged 65 years. “Where you live in the United States shouldn’t determine how long and how healthy you live—but it does, far more than
6
Minority Nurse | FALL 2013
it should,” said CDC Director Tom Frieden, MD, MPH. “Not only do people in certain states and African Americans live shorter lives, they also live a greater proportion of their last years in poor health. It will be important moving forward to support prevention programs that make it easier for people to be healthy no matter where they live.” For all adults at 65, the highest HLE was observed in
Hawaii (16.2 years) and the lowest was in Mississippi (10.8 years). By race, HLE estimates for whites were lowest among Southern states. For blacks, HLE was comparatively low throughout the United States, except in Nevada and New Mexico. HLE was greater for females than for males in all states, with the difference ranging from 0.7 years in Louisiana to 3.1 years in North Dakota and South Dakota.
Other findings: • HLE was greater for whites than for blacks in all states and Washington, DC, that had sufficient data, except Nevada and New Mexico. • HLE for males at age 65 years varied between a low of 10.1 years in Mississippi and a high of 15.0 years in Hawaii.
• HLE for females at age 65 years varied between a low of 11.4 years in Mississippi and a high of 17.3 years in Hawaii. HLE estimates can predict future health service needs, evaluate health programs, and identify trends and inequalities. Furthermore, examining HLE as a percent of life expectancy can reveal populations that might be enduring illness or disability for years. Public health officials, health care providers, and policymakers can use HLE to monitor and understand the health status of a population. For the full report, please visit www.cdc.gov/mmwr.
Vital Signs
Women’s Height Linked to Cancer Risk The taller a postmenopausal woman is, the greater her risk for developing cancer, according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
H
eight was linked to cancers of the breast, colon, endometrium, kidney, ovary, rectum, and thyroid, as well as to multiple myeloma and melanoma, and these associations did not change even after adjusting for factors known to influence these cancers, in this study of 20,928 postmenopausal women, identified from a large cohort of 144,701 women recruited to the Women’s Health Initiative (WHI). “We were surprised at the number of cancer sites that were positively associated with
height. In this data set, more cancers are associated with height than were associated with body mass index,” said Geoffrey Kabat, PhD, senior epidemiologist in the Department of Epidemiology and Population Health at Albert Einstein College of Medicine of Yeshiva University in New York. “Ultimately, cancer is a result of processes having to do with growth, so it makes sense that hormones or other growth factors that influence height may also influence cancer risk.” Some genetic variations as-
sociated with height are also linked to cancer risk, and more studies are needed to better understand how these heightrelated genetic variations predispose some men and women to cancer, according to the study’s authors. Kabat and colleagues used data from the WHI, a large, multicenter study that recruited postmenopausal women between the ages 50 and 79, between 1993 and 1998. At study entry, the women answered questions about physical activity, and their height and weight were measured.
www.minoritynurse.com
The researchers identified 20,928 women who had been diagnosed with one or more invasive cancers during the follow-up of 12 years. To study the effect of height, they accounted for many factors influencing cancers, including age, weight, education, smoking habits, alcohol consumption, and hormone therapy. They found that for every 10-centimeter (3.94 inches) increase in height, there was a 13% increase in risk of developing any cancer. Among specific cancers, there was a 13% to 17% increase in the risk of getting melanoma and cancers of the breast, ovary, endometrium, and colon. There was a 23% to 29% increase in the risk of developing cancers of the kidney, rectum, thyroid, and blood. Of the 19 cancers studied, none showed a negative association with height. Because the ability to screen for certain cancers could have influenced the results, the researchers added the participants’ mammography, Pap, and colorectal cancer screening histories to the analyses and found the results remained unchanged. “Although it is not a modifiable risk factor, the association of height with a number of cancer sites suggests that exposures in early life, including nutrition, play a role in influencing a person’s risk of cancer,” said Kabat. “There is currently a great deal of interest in early-life events that influence health in adulthood. Our study fits with this area.”
Minority Nurse Magazine
7
@MinorityNurse
Vital Signs
Redefining Cancer: New Recommendations Could Reduce Unnecessary Treatments, but Improved Diagnostic Testing Still Required New cancer recommendations made by a National Cancer Institute (NCI) working group could reduce unnecessary treatment by eliminating the fear factor linked with some early-stage cancers. However, there is a need for diagnostic tests that can recognize whether these early conditions could become life-threatening, states an analyst with research and consulting firm GlobalData.
T
he NCI scientists recommended that words like cancer, neoplasia, and carcinoma should
8
Minority Nurse | FALL 2013
be removed from premalignant conditions in order to reduce the incidences of over diagnosis and to prevent patients from
undergoing irrelevant surgery, radiation, or drug treatment. “The implementation of this recommendation will
help make patients and physicians more comfortable with refraining from unnecessarily treating benign disease,” says Cheryl S. Gradziel, PhD, oncology analyst with GlobalData. “The term cancer and its synonyms are alarming, which leads patients to strongly believe that premalignant conditions such as ductal carcinoma in situ or high-grade prostatic intraepithelial neoplasia should be treated aggressively, when this is often not the case.” As people become more aware and screening for many common cancers increases, more tumors are being treated at early stages. But, those screenings have resulted in more frequent diagnoses of abnormalities that would never become life-threatening, which is what the NCI is trying to minimize by redefining the terms surrounding cancer. In order to reduce the excessive treatment of low-risk diagnoses, GlobalData’s analyst argues for the importance of investing in tests that could determine early on if a condition will become malignant or not. “There is ample market opportunity for such tests, and their approval and subsequent adoption will have the greatest impact towards reducing the overdiagnosis and overtreatment of cancers in the US,” says Gradziel.
Making Rounds
October 4-6
International Society of Nurses in Genetics Silver Anniversary Conference: 25 Years of Leadership in Genetic Nursing DoubleTree Hotel Bethesda, Maryland Info: 412-344-1414 E-mail: isonghq@msn.com Website: www.isong.org/ISONG_annual_conference.php
11-14
23-26
8-10
The Transcultural Nursing Society
National Organization for Associate Degree Nursing
39th Annual Conference: Transcultural Nursing: Relationships for Health Locally, Nationally and Internationally Hotel Albuquerque at Old Town Albuquerque, New Mexico Info: 888-432-5470 E-mail: staff@tcns.org Website: www.tcns.org
2013 Annual Conference Peppermill Resort Spa & Casino Reno, Nevada Info: 877-966-6236 E-mail: noadn@dancyamc.com Website: www.noadn.org
8-11
American Association of Nurse Life Care Planners 13th Annual Conference Loews Philadelphia Hotel Philadelphia, Pennsylvania Info: 801-274-1184 Website: www.aanlcp.org/conference
November
Society of Urologic Nurses and Associates
2-6
44th Annual Conference Hyatt Regency Chicago, Illinois Info: 888-827-7862 E-mail: suna@ajj.com Website: http://event.suna.org
141st Annual Meeting and Exposition Boston Convention and Exhibition Center Boston, Massachusetts Info: 202-777-2478 E-mail: annualmeeting@apha.org Website: www.apha.org/meetings/AnnualMeeting
17-19
American Academy of Nursing
American Public Health Association
7-9
40th Anniversary of the Academy’s Transforming Health Care: Driving Policy Conference Hyatt Regency on Capitol Hill Washington, District Of Columbia Info: 202-777-1170 E-mail: info@AANnet.org Website: www.aannet.org/2013conference
Association for Medical Education and Research in Substance Abuse
23-25
8-9
The American Assembly for Men in Nursing 38th Annual Conference: Men in Nursing: Guided by the Past, Based in the Present, and Unfolding Our Future Hilton Newark Airport Elizabeth, New Jersey Info: 205-956-0146 E-mail: aamn@aamn.org Website: http://aamn.org/conference.shtml
37th Annual Conference DoubleTree Hotel Bethesda, Maryland Info: 401-243-8460 E-mail: doreen@amersa.org Website: www.amersa.org
Sigma Theta Tau International Honor Society of Nursing 42nd Biennial Convention JW Marriott Indianapolis Indianapolis, Indiana Info: 888-634-7575 E-mail: convention@stti.org Website: www.nursingsociety.org
December 2-4
OMICS Group
Aging and Society 2013 Interdisciplinary Conference University Center Chicago Chicago, Illinois Info: 217-328-0405 E-mail: support@agingandsociety.com Website: http://agingandsociety.com/theconference
www.minoritynurse.com
16-20
International Conference on Nursing & Emergency Medicine Hampton Inn Tropicana Las Vegas, Nevada Info: 800-216-6499 E-mail: nursing2013@omicsonline.net Website: www.omicsgroup.com/conferences/ nursing-emergency-medicine-2013
Minority Nurse Magazine
9
@MinorityNurse
How Mentoring Progra Inuence Workforce Diversity
10
Minority Nurse | FALL 2013
grams
BY CHRISTINE HINZ Karen Bankston, PhD, MSN, FACHE, didn’t have management in her career sights when she started as a fledgling emergency room nurse in 1976 at thenSouthside Hospital in Youngtown, Ohio. She wasn’t thinking much beyond giving the best care possible to patients with traumatic injuries and acute health issues.
Y
et Bankston’s chief nursing officer, Ruth Eldridge, MSN, RN, had a different idea. She saw enough leadership potential in her young nurse to offer herself as a mentor. Bankston admits that she didn’t even know what the term meant back then. But with Eldridge’s counseling persistence, her career took a rewarding trajectory, eventually leading to her present position as associate dean for clinical practice, partnership, and community engagement at the University of Cincinnati’s College of Nursing. It’s from that perch that Bankston now offers similar counsel to nurses-in-training. As faculty advisor for AMBITION—Advising Minorities By Inspiring and Transforming Them Into Outstanding Nurses—she wants to impart the same wisdom that her now retired mentor did to her years ago. “I’ve always been grateful to Ruth. If she hadn’t taken that step and said to me, ‘I’m going to help guide you because I see that you can do some great things,’ I might have had a totally different career than the one I’m enjoying today.”
A Place at the Table Perhaps you’ve had a similar experience. Someone spotted you as a diamond in the rough, a professional gem ready to be mined and polished. Or maybe you were the one searching for a seasoned colleague to help you buff your skills, build your portfolio, or strategize your next move. In either case, you’ve likely reaped the benefits in forging relationships with people who have your back and your best interests at heart. But in the bigger universe, how does mentoring actually help diversify the nursing workforce? What role does it play in answering the calls of the National Academies’ Institute of Medicine (IOM) and other nursing organizations for increasing diversity and giving an ever-changing patient population culturally competent care? Mentoring can have widespread implications beyond boosting individual careers. By giving minority nurses and nurse practitioners a necessary leg-up in broadening their options and fine-tuning their skills, mentoring changes the face of one organization and the makeup of the entire field. By encouraging persons of color to join, grow, succeed, and stay in the profession, it expands diversity, one person at a time. More specifically, developing a mentoring relationship exposes you to jobs you’ve never heard of—and to people who’ve never heard of you. It shows you that others have done what you’ve only thought of doing in passing. Now that you know their www.minoritynurse.com
Minority Nurse Magazine
@MinorityNurse
11
path, however, you can accomplish those goals too! Finally, by tapping people you respect for their wisdom, you ready yourself as an effective participant at any leadership table. In doing so, you’ll bring diversity to the highest decision-making levels of the profession’s ladder, not just those lower rungs. As Commander James Dickens, DNP, NP, FAANP, US Public Health Services, Office of Minority Health, Dallas-based Region VI, observes: “Nurses always talk about having a place at the table, but I think it’s more important than just that. You also need to have a fundamental understanding of what occurs…of what roles you and your colleagues bring to the team. Sometimes you may be the only nurse or nurse practitioner sitting there, so it’s important to understand the expectations.”
An Invitation into the Fold Yet you can’t diversify the leadership table if you’re not in the profession in the first place. Although mentoring is an essential technique for helping nurses and nurse practitioners of color enter the job market and capitalize on their skills, it’s also an effective tool in attracting promising young men and women into the field initially. By encouraging ethnically and racially diverse students to take the academic plunge, mentors play a critical role in expanding the nursing universe at the earliest possible juncture. They’re key for steering mentees as they navigate the rigors of training programs that are both new and challenging. They’re a sounding board when the educational waters get murky or rough. But their primary role, be-
12
Minority Nurse | FALL 2013
yond helping fledgling nurses graduate with flying colors, is to make sure persons of diversity understand that they have a place in the profession and are capable of the work. “People sometimes have the perception that they can’t succeed at nursing, especially if they’re part of a racial minority or from a different culture or lower socio-economic
background,” says Willa Hill Fuller, RN, executive director of the Orlando-based Florida Nurses Association and a veteran mentor and mentee. “They didn’t have a mom like my mother who just never let me think that I couldn’t do something. Mentors can help eliminate those kinds of attitudes, so their mentees can realize their potential.”
Growing up disadvantaged, Gordon Gillespie, PhD, RN, a Robert Wood Johnson Foundation Nurse Faculty Scholar and assistant professor at the University of Cincinnati’s College of Nursing, had no aspirations to be a nurse. Like many men, he initially bought into the gender biases surrounding the profession, stereotypes that can stifle that initial interest and
prevent retention. But Gillespie had a major supporter in his mother-in-law, herself an RN. She not only saw his potential,
having a one-on-one relationship with a single mentor was the perfect situation,” he says. “But now I realize that a pack-
“We want them to be able to go out and broadcast to the world, ‘Here I am. I’m proud of what I do.’”
Formalizing Tasks
By helping mentees fine-tune their business savvy and sharpen their political senses, mentors are critical assets in broadening choices beyond direct patient care. They facilitate diversity not only by helping nurses boost their competencies in areas never addressed in nursing school, but also by steering them to new options for their expertise. but eventually, with the help of other nurses, convinced him that nursing fit him to a “T.” “As I look back, it’s almost a miracle that I graduated from college, let alone became a PhD,” he says. “But someone looked at me and said, ‘I have faith in you. I believe in you. I will challenge you.’ That’s where mentorship is really essential. It can keep students in a program until graduation so we have that diverse workforce.” Today, Gillespie is both a mentor and mentee. As part of a scholarship program designed to single out the next generation of academic leaders, he’s put together a team of role models to facilitate his own growth beyond the doctorate and the experience he’s already amassed. For Gillespie, that includes two campus colleagues—one a nurse and the other from a different discipline—to help him deal specifically with being a good researcher, teacher, and fellow professional within his program. A third mentor, separate from both nursing and Cincinnati, serves as his external “safeguard.” She offers a broader perspective on a given situation from her spot in Baltimore. “I used to believe that
age of mentors is excellent. It’s going from good to great.” The model has worked so well for Gillespie that he uses it as a guide in mentoring his own students, particularly the young men he meets as the faculty advisor for the College of Nursing’s MENtorship program. With the ultimate goals of enrollment and retention to graduation and beyond, MENtorship was initiated to help male nursing students not only recognize the possibilities of a career in a caring profession, but also to deal with the real-life issues of choosing one dominated by women. In doing so, the discussion between mentors and mentees—upper classmen for lower classmen, and licensed nurses for seniors—often centers on dispelling gender myths and dealing with the challenges of caring for the opposite sex. Gillespie’s mission is to turn out male nurses who are not only potential leaders, but also content enough in their own skin to stick with the profession. “Our goal is to give these young men the support they need so they’re very comfortable with who they are as men in nursing,” Gillespie says.
To be effective, should mentoring occur vis-à-vis a formal structure or can you connect successfully in other “organic” ways? Truth is, whether you come together in the framework of a program or by linking with people whose substance and style you admire, you can have a very successful relationship. That is, as long as you’re on the same page in terms of goals, expectations, and even practicalities. There are times, however, when a formal construct not only cements mentoring as an important part of a nurse’s professional life and training, but also serves as a significant tool for bringing and keeping more persons of color into the fold. For instance, in 2008, the Robert Wood Johnson Foundation (RWJF) joined with the American Association of Colleges of Nursing (AACN) to launch the RWJF Careers in Nursing Scholarship Program, an effort to alleviate the nation’s nursing shortage by dramatically expanding the pipeline of students from minority backgrounds via accelerated nursing programs. Since its inception, RWJF has awarded some 2,700 $10,000 scholarships, through grantee schools of nursing, to entry-level nursing students coming into the field from other careers. Preference is given to awardees from underrepresented groups or disadvantaged backgrounds. To achieve that success, however, program officials knew early on that they had to establish consistency in
www.minoritynurse.com
how their grantees—nursing programs throughout the country—not only defined mentoring, but how they would be implementing it. Out of the concerns that people don’t confuse mentoring with academic counseling came a toolkit (www.NewCareersinNursing.org) to guide grantees in setting up a program. “If organizations can formalize their mentoring efforts, I think the odds are much better that they’ll see success,” says Vernell P. DeWitty, PhD, RN, program deputy director. “But even if they don’t have the resources we provide our grantees, as long as they have a good understanding of what mentoring should look like and how it should be approached, I think it can work.” Likewise, for the past six years Marquette University’s College of Nursing has used Project BEYOND (Building Ethnic Youth Opportunities for Nursing Diversity), an effort funded by the Federal Health Resources and Services Administration, to increase the number of minority BSN students admitted to and graduating from its nursing program. Mentoring is one aspect of an agenda that also includes tutoring, structured leadership programming, and peer-to-peer support. In terms of connecting, both mentors and mentees come together in what’s called the “World Café,” a meet-and-greet event conducted much like speed dating. Mentees spend five minutes with each licensed RN to share information and measure the chemistry. Before formalizing any relationship, however, they spell out their three top choices from which program directors make the
Minority Nurse Magazine
13
@MinorityNurse
final match. From there, it’s a matter of meeting initially to firm up the details, which must include at least two face-to-face meetings per semester. Most mentoring pairs, however, are regularly in touch throughout their collaboration. Since the goal is academic success, Project BEYOND features a separate specialist who also oversees a small cadre of upper grads or graduate assistants who peer tutor younger students. “We find that peer mentoring can be very effective because the relationship with another student is often easier to establish than with a faculty member or nurse,” says Juanita Terrie Garcia, MEd, RN, Project BEYOND coordinator. “Mentees have a level of confidence that they’ll benefit from their mentors because they’ve just gone through something similar. It’s fresh.” Since the inception of Project BEYOND, Marquette nursing officials have witnessed an increase in minority enrollment from 12% to 18% with retention rates of 96% to 100%. That’s translated into more than 30 underrepresented minority students successfully graduating, with seven enrolling in graduate programs. Project staff members believe they’re making progress because they’ve taken a “holistic” approach to raise not only academic skills, but self-confidence as well. “One of the most significant factors affecting the success of minority students is their level of confidence,” says Gloria Rhone, MSN, RN, Project BEYOND’s academic support coordinator. “They have to deal with all sorts of stereotypes about their ability to perform whether they’re appli-
14
Minority Nurse | FALL 2013
cable or not. So having somebody there to motivate them, encourage them, and just be a good listener can help build that self-esteem.”
Opening Doors, Expanding Opportunities By connecting with supportive and insightful individuals, minority students can indeed bolster their initial skills so they’re ready to be successful, working members of the profession. Yet establishing mentoring relationships after you’ve finally entered the workplace as a licensed practitioner can be just as fruitful as connecting with role models in training. Mentoring throughout your working years not only secures your personal long-term success, but also introduces your talent, perspective, and vision to the organization. By assisting new (or seasoned) nurses in plotting their career paths and fine-tuning their skills, mentors help mentees take their ambitions to the next fulfilling level. Whether you connect formally or informally, working with a mentor is a way to network with colleagues, demonstrate your abilities, and grow into jobs that fit your ambitions and long-term plans. From promotions to PhDs, mentoring brings a bevy of people into the job force, priming them for the next move. But for starters, it bridges the inevitable gap between education and practice so there can be no doubt that a new face on the block will be a valuable asset. Once they come on board at Minneapolis-based Fairview Health Services, for instance, new graduates, along with nurses new to an acute care
setting, undergo a variety of steps to ensure their initial success and long-term tenure. Beyond orientation and a preceptor to help them navigate the hospital and their unit, they’re also part of a year-long
“It shows that you care about them…that you’re not just throwing them out there. Instead, you’re giving them a safe place to ask questions, especially when they’re overwhelmed and need to reach out.”
To broaden her perspective, DeWitty has tapped people from fields other than nursing throughout her career. The variety, she says, “not only gives you a different perspective but also helps you become a much more rounded professional.” nursing residency program, an added layer of training and support. It’s then that they buddy with a mentor—usually a nurse manager or other nurse leader—to master the nuances of Fairview’s unique workplace. They may also join the system’s diversity circle, a separate mentoring effort that brings minority professionals together to broaden their networking reach in meeting leaders of color. Although diversity is part and parcel of every endeavor, the circle puts real faces to the concept that you can grow within the organization. Indeed, later on when they’re ready to take on more responsibilities, they’ll have access to developmental programs available to every promising nurse. But initially, the focus is on grappling with the challenges of picking up the pace and seeing greater numbers of patients than they did in training. It’s about learning how to be in command of their new environment—and comfortable enough to commit for the long haul. “It’s important to connect people with people,” says Laura D. Beeth, Fairview’s systems director, talent acquisition.
In terms of diversity, Fairview’s residency program is far from the organization’s only attempt to broaden its nursing corps. Officials have established a veritable roadmap of pipeline programs to lure minority persons into the medical field, whatever their ultimate career choice. From support for two Minneapolis health career-focused high schools to individual scholarships and summer internships, Fairview has instituted opportunities at every step of the training continuum to find, attract, and fund potential nurses of color. Much of the activity begins with the hospital’s awardwinning SCRUBS Camps, an annual opportunity for minority teens, among other high schoolers, to live and breathe what it’s like to work in medical careers. So named for the attire of the attendees, SCRUBS is an intense three- to five-day college campus tutorial involving a largely hands-on agenda. Participants network with faculty members who, if only for a short time, mentor them on their choices. Although her introduction to Fairview didn’t involve summer camp, Marion Lee, RN, BA, MSN, has benefited in
other ways from her relationship with the health system and her colleagues. Besides a $10,000 sponsorship to finish her nursing education (via an accelerated master’s degree), Lee has reaped many rewards from the preceptors and mentors she’s encountered as both a student and newly minted professional. The people surrounding her have been instrumental, for instance, in helping her sharpen her skill sets, especially in approaching patients, interacting with their families, and managing her time doing both. But the biggest advice she’s received may involve just being sensitive to other cultures. Even though Lee is Mexican by birth, she has to keep in mind that patients from other areas of the world don’t always appreciate her Latino warmth.
“We’re very touchy, feely people,” Lee says. “We love to hug and touch. Sometimes patients look so lonely that I just want
ground. Whether filling a forprofit or not-for-profit position, nurses and nurse practitioners are sought-after commodities
Mentoring is critical at every step in a minority nurse’s professional journey—to soar academically as a student, to transition into the workplace as a novice, and to plot the best career path as an experienced pro. to hold their hands. But I have to step back and realize that I can’t do that. I have to remember that there are boundaries.”
Testing New Waters Like Lee, you may have discovered your niche at the bedside. But not every nurse will find caring for patients his or her forte. Fortunately, in today’s market there are other ways to use your skills and unique back-
in all sorts of places that need their clinical expertise and patient perspectives. So how can mentoring ensure that minority nursing professionals have options beyond traditional health care jobs? By helping mentees finetune their business savvy and sharpen their political senses, mentors are critical assets in broadening choices beyond direct patient care. They facilitate
www.minoritynurse.com
diversity not only by helping nurses boost their competencies in areas never addressed in nursing school, but also by steering them to new options for their expertise. As Elizabeth Allee, BSN, clinical trial project manager for Indianapolis-based Eli Lilly and Company, observes: “Mentoring in a corporate environment is extremely, extremely important. In a hospital, a nurse is a nurse, even though every area is different. But when you come into a company, your knowledge and training can be used across multiple departments. You need a mentor to help you leverage your expertise so someone will look at you and say, ‘This person would be a great fit for our team!’” Allee credits the right people for giving her the right advice at the right time as she’s transi-
Minority Nurse Magazine
15
@MinorityNurse
tioned from her first Lilly job in global patient safety to her current role overseeing global clinical trials for various therapeutic teams. Ten mentors along the way have helped her navigate the politics of the organization and readied her for the next step. Today, she’s returning the favor by marshaling advice for 12 fellow employees, many of whom are nurses of color. She’s also a founding leader of the Lilly Nursing Forum, a ground zero effort for promoting both patient-centered community initiatives and nursing professionals. Even though there’s no formalized mentoring structure within the forum, the networking that occurs exposes nurses to opportunities not always obvious in a behemoth corporation. Allee, for instance, just returned from a six-month assignment in China, a stint that wasn’t on her career radar until she learned of it through her forum contacts. Among their activities this year, forum participants are keying into Lilly’s corporate initiative, “Fit for Life,” by focusing on career as one of several wellness areas. As part of that agenda, Allee predicts an increased emphasis on mentoring, not only as a strategy to help individual nurses realize their potential within the company, but also to help the company retain its nursing talent. When Dorothy Jackson, RN, MS, came to Lilly in 2006, she brought along 20 years of diverse experience in surgical, coronary care, ICU, and community health nursing. As a former clinical research coordinator for an outside cardiology group, her past experience fit nicely into her first job, a contract employee on Lilly’s cardiovascular research team.
16
Minority Nurse | FALL 2013
Today, Jackson serves as a global lead for case management, meaning she provides safety collection oversight for Lilly’s endocrine clinical drug trials. She’s also a Lilly Nursing Forum leader, a position suggested initially by her friend and current mentor, Liz Allee.
Jackson had worked with two previous mentoring colleagues before tapping her former department co-worker to help her identify her next professional steps. Together, the two are focused on fine-tuning her career development plan so the path she chooses fits her strengths and skills. Besides offering advice and networking contacts, Allee has encouraged her mentee at every turn to chase new pursuits in broadening herself and upping her profile. When the nursing forum started, for instance, she
urged Jackson to join, even though her mentee was hesitant of the time commitment. Allee persevered, however. Today, they’re collaborating not just on Jackson’s future, but also in creating educational outreach projects using a variety of forum nurses. It’s a natural fit
Jackson. “She kept saying, ‘You’d be good at this. You do community service all the time. You have a good outlook on nursing. Let’s do this together.’ I think an important part of being a good mentor is simply looking at a person and saying, ‘You’d be a great fit.’”
“As I look back, it’s almost a miracle that I graduated from college, let alone became a PhD,” Gillespie says. “But someone looked at me and said, ‘I have faith in you. I believe in you. I will challenge you.’ That’s where mentorship is really essential. It can keep students in a program until graduation so we have that diverse workforce.” for Jackson, who does health training and diabetes education in her community. “Liz made me take a second look at something I probably would have passed on,” says
Good Mentors Worth Gold What makes for good mentoring? There’s no one-size-fits-all formula in selecting people to emulate or tap for their advice. But here are some factors that
you may want to think about as you make your choices.
Numbers and variety count. Mentoring doesn’t have to be one-stop shopping. Putting together a team of people who can work with you on a variety of fronts can help you address issues beyond even nursing.
Numbers Make Mentoring Imperative
T
here are many reasons to encourage diversity, not the least of which is to alleviate the well-established health disparities experienced by minority communities either lacking access to quality care or the cultural incentive to get it.
Research consistently shows that patients experience improved outcomes when their caretakers share their cultural story or worldview. They respond positively in terms of navigating both the health system and their own medical issues when someone of the same background is helping them on that journey. “You can take culturally and linguistically appropriate classes,” says Dickens. “But studies still show repeatedly that if a nurse or nurse practitioner looks like the patient and is someone that patient can relate to, his or her outcomes will be better.” Yet configuring a nursing corps with an adequate mix of African Americans, Latinos, Asians, American Indians, and Alaskan Natives to match those needs remains a daunting challenge, given the current state of nursing and projections for the future. The US Bureau of Labor Statistics, for instance, suggests that more than a million new and replacement registered nurses will be needed by 2020. The profession is soon to lag, regardless of its makeup. Furthermore, although minority groups comprise more than one-third (37%) of the populace, according to 2012 US Census Bureau data, the numbers of racially and ethnically diverse health professionals to care for them are hardly adequate today. A bevy of studies compiled over the past decade by both government and private entities demonstrate that although minorities have made strides in the health professions, they’re still an underrepresented nursing class when compared to the patients they serve. They embody less than 17% of the registered nurse (RN) workforce, according to 2008 National Sample Survey of Registered Nurses data compiled by HRSA, the US Health Resources and Services Administration. Those numbers reflect an RN population comprised mostly of Asians (5.8%) and African Americans (5.4%) with fewer Hispanics (3.6%), American Indian/Alaskan Natives (0.3%), and multi-racial nurses (1.7%). Although the number of men has climbed steadily since 1980, they still only comprise 6.2% of the workforce.
One of the best mentors DeWitty had as a young unit head nurse, for instance, was her hospital director. He gave her the opportunity to sit in on meetings and afterwards ask any questions about the deliberations. By delving into the details of such conversations, she had a better understanding of how things worked. To broaden her perspective, DeWitty has tapped people from fields other than nursing throughout her career. The variety, she says, “not only gives you a different perspective but
In terms of where they’re headed educationally, the statistics represent further evidence of the task ahead. In its 2012-2013 Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing report, for instance, the AACN noted that minority nursing students represent 28.3% of entry-level baccalaureate programs, 29.3% of master’s programs, and 27.7% of research-focused doctoral programs. At the same time, men comprised 11% of BSN students, 10% of MSN students, and 7.9% of students in research-focused and 10% of students in practice-focused PhD programs. The AACN 2011 annual survey data also reveals a full-time nursing school faculty that is only 11.8% minority and only 5.1% male. Supported by similar findings from a cache of other major nursing organizations, the IOM made nursing diversity the focus of its 2010 landmark report, The Future of Nursing: Leading Change, Advancing Health. In calling for a greater emphasis on a nursing workforce that’s better able to interact with and provide culturally competent care to a wide swath of patients, the authors offered many recommendations, particularly in the area of education. They urged systemic changes to both increase the recruitment of undergraduate students from all backgrounds and ready an expanded crop of graduate-level minorities prepared to be faculty, scientists, and researchers. In so doing, IOM’s authors identified mentoring, particularly in nursing education, as one tool among many to woo more qualified candidates who will help counter any training and workplace shortages.
www.minoritynurse.com
Minority Nurse Magazine
@MinorityNurse
17
also helps you become a much more rounded professional.”
Think culture and beyond. Don’t limit yourself to nurses who share your race or ethnicity. Even though it’s important to find examples of people within your own community who’ve excelled at what you want to do, it’s just as important to match your needs with the best resources available. The first mentor who made such a difference in Bankston’s life, for instance, was Caucasian. Likewise, it was expected that DeWitty would pair with African American nurse mentors during her PhD program. But she had lived and worked most of her life in a culturally diverse environment, so she looked for a role model mix. “Similarities in ethnicities are important,” she says. “But you should go deeper to see if two people are operating on the same wavelength and are really the best match.”
Reach beyond your environment. Nowhere is it written that you have to limit your choices to those directly surrounding you. A good mentor can be as close as the next office or as far away as a distant land. Just as long as you have a structure in place for connecting with someone efficiently, you can make those long distance collaborations work nicely. For instance, Dickens, who usually confines his advice as a mentor to mastersdegree hospital administration nurses stateside, also mentors a chief nursing officer at an American hospital in Saipan. He’s helping her traverse the concerns of being isolated geographically in a hospital that needs help with its CMS (Centers for Medicare and Medicaid Services) status when she’s not
18
Minority Nurse | FALL 2013
necessarily being prepared for the job. Be flexible. If you’re the mentee, don’t be afraid to ask for a referral or to end the relationship when you’ve gone beyond what this person can offer you. If you’re the mentor, be ready to suggest another nurse or professional who has the right contacts and advice if that’s not you. Dickens, for instance, doesn’t hesitate to push people along or connect them with new sources. “It’s extremely fluid,” he says. “Some of my mentees have outgrown me because their career trajectory has set them in another direction. I understand that. I say, ‘Look, I want to keep you in my back pocket. I’ll never go away. I’ll always be available to you.’”
A Final Note Whether you’re starting your career or just moving into the next phase, seeking the counsel of wise and diverse colleagues can make the difference between success and failure. Mentoring is critical at every step in a minority nurse’s professional journey—to soar academically as a student, to transition into the workplace as a novice, and
to plot the best career path as an experienced pro. It can provide nurses of color the kind of insight and edge that helps them succeed personally as they bring needed diversity to their patients, colleagues, and the profession at large. Bankston, for instance, has benefited immensely from her mentor’s early and frequent message: To be taken seriously, especially in a world fraught with biases, she’d need to be at the top of her game. Whether that meant polishing her skills, dusting off her professional demeanor, or adding another credential to a growing resume, Bankston responded by listening, learning, and doing. When Eldridge pointed out, for instance, that Bankston’s hand movements were a distraction when she presented, she practiced diligently in front of the mirror to employ them effectively. Likewise, when her mentor suggested that an advanced degree would be paramount in the roles she envisioned for her young charge, she started thinking PhD. Today, Bankston counts stints as both a hospital chief nursing officer and chief ex-
ecutive officer among the titles she’s earned since her mentor first spotted those leadership qualities. As the faculty advisor for AMBITION, a peer-topeer tutoring group, she wants young minority nursing students not just to have the right skills to behave admirably in the workplace, but to master the rigors of nursing school so they can get their foot in the door. By pairing upper classmen with freshmen who need to overcome any hurdles, AMBITION alleviates the isolation that Bankston herself felt in nursing school 40 years ago. It also keeps a new generation of minority nurses committed to a profession they, in turn, will diversify. “As minority nurses, we need people in our lives who’ve already navigated the waters,” says Bankston. “Finding mentors who are both trustworthy and honest can help us recognize the potential missteps and even push us when we think that we just can’t do anymore. They’re very important in our career journey.” Christine Hinz is a freelance writer based in Milwaukee, Wisconsin.
Studying Disparities How Nursing Schools Cover Minority Populations and Health Care Inequality BY MARGARETTE BURNETTE About 30% of Hispanic Americans and 20% of African Americans don’t have a usual source of health care, but less than 16% of white Americans lack a source.
F
or women who have had an abnormal screening mammogram, the length of time before a follow-up test is conducted is twice as long in Asian American, Hispanic, and black women than it is in white women. It’s no secret that there are racial and ethnic disparities in health care. These statistics, which come from the Agency for Healthcare Research and
Quality’s Medical Expenditure Panel Survey, highlight a major concern in the field of medicine. Not all patients receive the same level of high quality treatment—or in some cases, receive treatment at all. This concern is important within nursing schools, because they are tasked with making sure our country’s future nurses fully understand racial disparities and what can be done to address them, says
Mary Green, PhD, MN, RN, interim chair of the Dillard University School of Nursing in New Orleans. Schools must show the latest research and best practices to the next generation of nurses, and take them into communities so they can see firsthand the effects of health inequality, argues Green. “Nurses need to get the broadest experiences they can.”
Learning in the Community Many nursing schools have mandatory community health courses that expose students to inequalities among groups of
www.minoritynurse.com
people. Nursing students learn about the statistical differences in health care outcomes, and along with that, many of these institutions require nursing students to meet the people behind the statistics. For example, at the University of Alabama-Birmingham (UAB) School of Nursing, undergraduate students, along with faculty, go into communities in the greater Birmingham area that have historically had less access to health care, says Linda Moneyham, PhD, RN, FAAN, senior associate dean for academic affairs at UAB. There, nursing students learn
Minority Nurse Magazine
@MinorityNurse
19
This concern is important within nursing schools, because they are tasked with making sure our country’s future nurses fully understand racial disparities and what can be done to address them, says Mary Green, PhD, MN, RN, interim chair of the Dillard University School of Nursing in New Orleans.
how to master their clinical work while partnering with neighbor representatives who are interested in improving the community’s health, she adds. “These tend to be communities that are lower income, have high minority populations, and have a lot of health needs,” she says. “In fact, Alabama is often the epicenter for some of the major health problems the country faces.” Moneyham explains that Alabama ranks near the top for prevalence of heart disease, obesity, and HIV—and minorities are disproportionately affected. “We have to focus on these populations because they are the populations nursing students are going to be caring for,” says Moneyham. At the University of Washington School of Nursing in Seattle, there is a similar ap-
20
Minority Nurse | FALL 2013
proach. “We have for years had a required course on community health nursing that addresses health disparities and inequities,” says C. June Strickland, PhD, RN, associate professor, psychosocial and community health nursing, at the school. “It’s [often] the very first course that students take when they come into our program to study,” she says. “Essentially, it focuses on health disparities, equities, and social justice.” “In addition, we have clinical sites in multicultural environments that include American Indian, African American, Latino, and Asian populations,” explains Strickland. “When faculty members take students to those clinical sites, they get a cultural immersion and opportunity to understand some of the issues people
are facing. For instance, with Native people, some of what we experience is the impact of colonialization that continues on in our community.” The School of Nursing also attracts other students that plan to work in related fields, such as social work, public
health, and psychology, says Strickland. “I teach a core course in assessment and that course also draws students from all over campus, because certainly these issues come up [in those disciplines].” There are also graduate level courses that dig deeper into
That course looks at health status around the world, and it certainly looks at disparities in the US,” says Ward. “We also have another course called Community Connection. Our masters students in the leadership program take this course where pairs of students work with community agencies,” she continues. Examples of these agencies include the Sacramento Unified School District and the local food bank’s parent-child program to provide support for parents with a variety of special needs. “Students come face to face with the issues that community agencies are working on, which includes the health effects of disparities of all kinds,” says Ward. For example, one pair of students working with the county health department looked at soft drink vending machines in certain schools. School districts that are strapped for funds— and often in minority neighborhoods—can get money by having vending machines for soft drinks in their schools, Ward explains. “But on the other hand, if you have vending machines in schools that deliver sugary drinks, you’re
“If you have people who have lower income, less education, and who live in communities that are less friendly to activity [and exercise], their health by definition is going to be less,” explains Hines-Martin. problems associated with inequalities. Deborah Ward, PhD, RN, FAAN, is associate dean for academics at the Betty Irene School of Nursing at the University of California-Davis in Sacramento. “We have a course in health status that all of our masters and PhD students take.
contributing to the obesity epidemic that places students at all kinds of risk.” Students who are obese are at great risk for many health problems, such as diabetes, says Ward. So the nursing students learned how school pupils in minority neighbor-
hoods are exposed to factors that contribute to the obesity epidemic.
this is something that can directly help reduce the inequalities that have historically ex-
“Going into the community gives a more accurate picture of the racial and ethnic disparities that exist,” says Green. In this particular course, nursing students wanted to address the question of whether or not it was good for a cashstrapped school system to get immediate money from vending machines, or if it was better to ban the vending machines and have students ingest fewer sugary drinks. “The students did a sophisticated analysis of the cost and benefits to the community in having soda machines in the school,” says Ward. “Armed with that kind of data, you can come back to your community as a nurse leader and demonstrate the long-term advantages of not having soda machines in a school.” The students learned how to work at system-level changes that are going to help communities make decisions about important health issues in their community, Ward adds.
Filling in Gaps With upcoming changes in health care laws, there are going to be thousands of people from different communities who are going to be seeking health care services they might not have sought in the past, says Moneyham. In many areas, especially rural areas, nurse practitioners will be called on to help fill in the gap between patients requiring care and available physicians, Moneyham explains. Nursing schools are teaching their students that
isted in those communities, she adds. In addition, nursing students will be called on to share information about programs that help disadvantaged patients. For example, there are pharmaceutical companies that may supply medication for patients for minimal charge, particularly if the shelf life of the medicine is short. “Sometimes they’ll distribute those to poorer patients,” says Moneyham, and a nurse can be the link between that patient and the pharmaceutical company.
Avoiding Stereotypes In order to give quality care to people who are from different cultures and ethnicities, all nurses, including minority nurses, need to learn to overcome misconceptions and even prejudices they may have about the patients they serve, says Moneyham. “For example, one stereotype is that if someone is overweight or they have health problems, they don’t care about themselves, and you can’t help those people because if they wanted to lose weight they could.” But the nursing school helps students understand that there are often external affairs that affect a person’s health, and health professionals should understand what those factors are in order to effectively help a patient, she says. “We provide the experiences to nursing stu-
dents to help them walk in the [patient’s] shoes, and try to understand their perspective about their weight problem and their challenges.” The methods used when approaching people should be appropriate and respectful. If nurses don’t understand someone’s situation, any recommendation will likely not be effective, says Moneyham. She conducts focus groups with women who may be classified as obese, and she finds that many may not see themselves as overweight. Students learn that in these cases, giving lectures on losing weight likely won’t work. “What we need to focus on are things that help these women feel healthier, such as getting enough exercise or watching the types of food they eat,” she argues. “We have to work where the person is ready to work.” Even then, minority nursing students should learn that individual actions are only a small piece of what impacts health, argues Vicki HinesMartin, PhD, CNS, RN, FAAN, director of the office of health disparities and community engagement at the University of Louisville School of Nursing. In fact, students are often surprised to learn that social factors outside of a person’s con-
care, and health outcomes are all influenced by things that are not specifically health-related, says Hines-Martin. Those determinants include economic status, education, and even access to transportation. “If you have people who have lower income, less education, and who live in communities that are less friendly to activity [and exercise], their health by definition is going to be less,” explains Hines-Martin. “Increasingly, students at both the undergraduate and graduate levels are expected to think critically about the context from which a person comes. And as a result of that, faculty are changing where they do their work clinically, how they do their classroom teaching, and the examples they use to help a nursing student make better decisions about the populations they work with,” says Hines-Martin. “Not only do we need to teach our nurses what they should be doing directly with the patient, we also need to put them into the context of where that patient comes from. Then we realistically adjust, adapt, or support that person’s ability to maintain whatever wellness they can,” she continues. At Dillard, nursing students learn to address disparities and
Understanding disparities can occur with one-onone teaching, but diversity initiatives should also occur on an administrative, school-wide level, says Strickland. trol have a very large influence on their health. These “social determinants of health,” as outlined by the World Health Organization, identify that a person’s health status, access to
www.minoritynurse.com
overcome their own prejudices by looking at case studies, says Green. She gives the following example of a case study: Let’s say we have JM, who is a 47-year-old African American
Minority Nurse Magazine
21
@MinorityNurse
male who is currently homeless, jobless, and suffers from schizophrenia, uncontrolled diabetes, and hypertension. Because of the behavior attributed to his mental illness, he may be in and out of jail and perceived as a threat to the community. As nurses, what do we do? Green explains that nursing students learn how to deal with urgent problems, such as the uncontrolled diabetes, as well as seek out other resources, such as helping to locate a case manager who could help JM access mental services that may be available. These case studies are then followed up by actually visiting similar neighborhoods. “Going into the community gives a more accurate picture of the racial and ethnic disparities that exist,” says Green.
School Diversity Understanding disparities can occur with one-on-one teaching, but diversity initiatives should also occur on an administrative, school-wide level, says Strickland. This means having a nursing school that reflects and celebrates racial and ethnic diversity in addition to teaching it. “It’s important to have systems and structures in place that support these behaviors.” Strickland states that the University of Washington has a diversity council and an office of minority affairs that’s very active. “There is also a diversity council within our School of Nursing, and some of the activities have included working with faculty to design an evaluation so faculty can evaluate how effectively they’re addressing disparities and diversity in their course content,” she says. Strickland
22
Minority Nurse | FALL 2013
adds that the school recently voted to include diversity in their promotion and tenure documentation for faculty. At UC-Davis, Ward says the first area where the school practices the goal of cultural inclusiveness is with its faculty and staff. “We like to think of what we’re doing as a multifaceted approach,” she says. “This means cultural inclusiveness, teaching cultural approaches to care, and working with all of our communities to improve care and health.”
At the UAB School of Nursing, Moneyham says that more than 26% of students are minorities. “This is high compared to the national average,” she explains. “A lot of that has to do with where we sit in the Deep South region of the United States.” Moneyham adds that cultural diversity in nursing schools is good because nurses are able to accurately reflect the communities they serve. When nursing schools cover minority populations and
health care inequality effectively, they produce nurses who are more competent at addressing those inequalities. This in turn produces better nurses who are more likely to take a leadership role in helping eliminate disparities, says Hines-Martin. “It is a strategy of engaged scholarship, engaged teaching, and engaged research that has evolved.” Margarette Burnette is a freelance writer based in Georgia.
Only those who care for others know what it’s really like to care for others. That’s why AARP created a community with experts and other caregivers to help us better care for ourselves and for the ones we love.
aarp.org/caregiving or call 1-877-333-5885
Advanced Degrees What You Need to Succeed Advanced education and specialty certifications can help minority nurses take their careers—and their ability to improve health outcomes—to a whole new level. BY PAM CHWEDYK
24
Minority Nurse | FALL 2013
s and Certifications Carmen Paniagua has so many educational and professional credentials after her name that she practically needs an oversized business card to fit them all. In addition to being an RN, she is an ANP (Adult Nurse Practitioner), a board-certified ACNP (Acute Care Nurse Practitioner) and AGACNP (Adult-Gerontology Acute Care Nurse Practitioner), an APNG-BC (Advanced Practice Nurse in Genetics), and a FAANP (Fellow of the American Academy of Nurse Practitioners). She’s also a CPC (Certified Procedural Coder) and a CMI (Certified Medical Interpreter), and she holds MSN and EdD (Doctor of Education) degrees.
“S
ome people probably look at my CV and think this is just a lot of ‘alphabet soup,’” says Paniagua, a faculty member at the University of Arkansas for Medical Sciences College of Medicine in Little Rock. “But advanced degrees and certifications are more than just a collection of letters. They’re the evidence and recognition of your competence and clinical expertise. They enable nurses to take pride in the accomplishment of advanced practice knowledge and to demonstrate their specialty expertise to both employers and patients.” Jose Alejandro, president of the National Association of Hispanic Nurses and corporate director of case management at Cornerstone Healthcare Group in Dallas, agrees that it’s what those abbreviations really stand for that counts. “You can have all the de-
grees and certifications you want, but it’s the tools you learn from having them that’s the biggest benefit,” says Alejandro, an RN-BC (Registered Nurse-Board Certified), CCM (Certified Case Manager), FACHE (Fellow of the American College of Healthcare Executives), and a MBA who recently earned his PhD. “They give you additional skills and what I call your ‘chops.’ That’s primarily what has enabled me to move up in my career, because I can accomplish things based on more than just having experience.”
to nurse practitioner, nurse anesthetist, nurse executive, and more. Furthermore, the Institute of Medicine’s (IOM’s)
landmark 2010 report The Future of Nursing: Leading Change, Advancing Health calls for all nurses to “achieve higher levels of education and training” and “attain competency in specific content areas” in order to respond more effectively in today’s rapidly evolving health care environment. But the IOM report also underscores an even more persuasive reason. Advanced degrees and certifications—or more precisely, the specialized
Opening Doors There are many compelling reasons for minority nurses to pursue graduate education and specialty nursing certifications. Acquiring these credentials opens the door to a wide new horizon of rewarding advanced practice careers and leadership roles—from nursing professor and nurse scientist
www.minoritynurse.com
Minority Nurse Magazine
25
@MinorityNurse
knowledge and skills nurses gain from them—are linked to improved patient outcomes and better nurse-led interventions for eliminating minority health disparities. “This is a wonderful time
patients will be members of medically underserved minority populations. The other issue is that there’s a shortage of primary care physicians. So there’s a tremendous need to increase the number of cul-
“But advanced degrees and certifications are more than just a collection of letters. They’re the evidence and recognition of your competence and clinical expertise. They enable nurses to take pride in the accomplishment of advanced practice knowledge and to demonstrate their specialty expertise to both employers and patients.”
for all nurses, and particularly nurses of color, to seriously look at graduate education, because of the millions of uninsured and underinsured people who will now be coming into the health care system as a result of the Affordable Care Act,” says Kem Louie, PhD, RN, PMHCNS-BC, APN, CNE, FAAN, professor and director of the graduate nursing program at William Paterson University in Wayne, New Jersey. “Many of these new
26
Minority Nurse | FALL 2013
turally competent advanced practice nurses who can meet these patients’ primary health care needs.” Of course, it’s also hard to ignore the “what’s in it for me?” benefits. Becoming certified in an in-demand specialty—for example, emergency nursing, perioperative nursing, critical care, or pediatrics—increases your value to employers. Plus, it’s no secret that many advanced practice (APRN) specialties that require a master’s
degree and board certification—such as Certified Registered Nurse Anesthetist (CRNA) and Certified Nurse-Midwife (CNM)—pay substantially higher salaries than the typical staff RN position (see sidebar). In fact, according to the most recent (2008) Health Resources and Services Administration (HRSA) National Sample Survey of Registered Nurses, RNs with graduate degrees earn an average of at least $20,000 more per year than nurses with lower education levels. But it’s not just about the money, argues Henry Talley V, PhD, CRNA, MSN, MS, director of the nurse anesthesia program at Michigan State University College of Nursing in East Lansing and treasurer of the American Association of Nurse Anesthetists. “Advanced degrees and specialty certifications do increase your earning powers,” he says. “But they also increase your ability to make change happen in health care. They make you an expert in your particular field, and they put nurses on an equal footing with other health professionals.”
Breaking Down Barriers Minority enrollments in graduate nursing programs have nearly doubled over the past decade, according to the American Association of Colleges of Nursing (AACN). Yet racial, ethnic, and gender minority nurses continue to be underrepresented among the ranks of APRNs and certified RNs—primarily because they’re still underrepresented in the nursing population as a whole. Fortunately, numerous nursing organizations, from AACN to the American Board of Nursing Specialties, are recognizing the need to identify and remove barriers that may prevent nurses from diverse backgrounds from earning the advanced credentials they need to succeed. Traditionally, one of the biggest challenges in going back to school—for majority and minority nurses alike—is finding the funds to pay for it. And thanks to the current economy, with its skyrocketing tuition rates and burgeoning student loan debt, figuring out how to afford graduate school can be a trickier task than ever. Then there’s the cost of certification examinations, which in some cases can range from about $300–$400 to as high as $725 for the CRNA exam. But even though finances can be a formidable obstacle, they’re not an insurmountable one. “What I have personally observed is that our potential minority nursing students are much more hesitant to take out loans and incur debt than majority students,” says Courtney Lyder, ND, ScD(Hon), GNP, FAAN, dean and professor at UCLA School of Nursing. “And what I tell them is: Nurses make good
salaries. Compared with other academic disciplines, the compensation in nursing makes it one of the few professions in which you can actually pay off student debt in a timely manner.” “One of the benefits of coming to graduate school now is that there are still scholarships and federal financial assistance
programs available,” adds Louie, who is also the founding president of the Asian American/Pacific Islander Nurses Association. She cites HRSA programs like the National Health Service Corps, which provides scholarships for nurse practitioner and nursemidwife students in return for a commitment to practice in a
Recognizing the Value Growth in Minority Enrollments in Graduate Nursing Programs, 2002–2011 MASTER’S DEGREE PROGRAMS Race/Ethnicity*
2002 2005 2008 2011
Non-Hispanic White
61.3%
78.0%
76.0%
73.4%
Black/African American
7.0%
10.7%
11.9%
12.6%
Hispanic/Latino
3.2% 4.7% 4.9% 5.1%
Asian/Pacific Islander
3.7%
5.9%
6.7%
7.0%
American Indian/Alaskan Native 0.5%
0.7%
0.6%
0.7%
Two or More Races
N/A
N/A
N/A
1.13%
Total Minority Enrollment
14.4%
22.0%
24.0%
26.6%
DOCTORAL PROGRAMS (RESEARCH-FOCUSED) Race/Ethnicity*
2002 2005 2008 2011
Non-Hispanic White
71.6% 81.6% 77.9% 75.3%
Black/African American
6.8%
Hispanic/Latino
2.0% 3.3% 4.0% 4.7%
Asian/Pacific Islander
3.6% 4.5% 5.9% 5.9%
9.9%
10.9%
11.9%
American Indian/Alaskan Native 0.5%
0.7%
1.3%
1.4%
Two or More Races
N/A
N/A
N/A
0.85%
Total Minority Enrollment
12.9%
18.4%
22.1%
24.7%
*Percentages may not total to 100 due to rounding. Source: American Association of Colleges of Nursing
www.minoritynurse.com
Minority Nurse Magazine
27
@MinorityNurse
medically underserved area for at least two years after graduation, and the Nurse Faculty Loan Program, which forgives 85% of student loan debt for RNs who complete a graduate degree at a participating school and agree to serve as full-time nursing faculty. Talley and his wife, a Clinical Nurse Specialist (CNS), recently conducted research examining some of the other factors that impede minority nurses from pursuing advanced degrees in general and nurse anesthesia degrees in particular. Lack of knowledge about APRN and specialty nursing career paths is another big barrier, he says.
“There are still people of color out there who have just not had the exposure to these career options,” Talley explains. “Nursing specialties have to get the message out to them about these opportunities and what the requirements are. Nurses need to know early on that they will want an advanced degree, because the key to opening that door will be how well they do in their undergraduate studies. Otherwise, they’ll find out about advanced practice specialties later in their BSN programs and decide ‘I want to do that’ when their GPAs will not support it.” But Alejandro believes that
Power Earning Highest-Paying Nursing Specialty Certifications and Advanced Practice Careers Specialty
Average Annual Earnings
Certified Registered Nurse Anesthetist
$154,221
Nurse Practitioner
$85,025
Certified Nurse-Midwife
$82,111
Nurse Consultant
$76,473
Informatics Nurse
$75,242
Clinical Nurse Specialist
$72,856
Management/Administration
$72,006 to $96,735
Source: The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses (US Department of Health and Human Services, Health Resources and Services Administration, September 2010)
28
Minority Nurse | FALL 2013
perhaps the hardest hurdle for minority nurses to clear is the surprisingly common “fear factor.”
es. “Is it pediatrics, geriatrics, psych/mental health, administration, nurse-midwifery, nurse anesthesia? Once you’ve fig-
“Advanced degrees and specialty certifications do increase your earning powers,” Talley says. “But they also increase your ability to make change happen in health care. They make you an expert in your particular field, and they put nurses on an equal footing with other health professionals.” “It’s the fear of failure, fear of the unknown, fear of whatever,” he says. “I tell all the students I mentor: ‘The very first barrier you have to overcome in pursuing any advanced education or any certification is removing that fear.’ In my case, once I was over that fear, I was able to ask questions. If I didn’t understand something in a particular class, I went ahead and asked classmates who understood it a little better.”
Starting the Journey So you’ve decided it’s the right time to return to school, earn an advanced degree, and chart your course toward a fulfilling specialty nursing career. Congratulations! But where do you start? How do you choose which graduate program to apply to? And what type of degree should you go after? Is a terminal master’s enough or will you need a doctorate? Lyder, who made history by becoming the first male minority dean of a school of nursing in the United States, as well as the first African American dean at UCLA, says it all boils down to answering one basic question: What do you want to do? “Find your bliss,” he advis-
ured that out, the next step is to identify schools in your community that may have those programs. Then, contact those schools and schedule a time to talk with the admissions counselors—and I don’t mean an e-mail—to see if this is something you really want to pursue. Also, try to find an opportunity to shadow someone who’s in that role. Identify that CRNA or that psychiatric nurse practitioner and say, ‘Can I shadow you for a day to get a sense of whether this is what I want to do?’” Getting over the fear of speaking directly with admissions officers or the graduate program director to get the facts you need to make wellinformed decisions about a school is key, Louie emphasizes. “You have to tell yourself, ‘Just pick up the phone,’” she says. “Graduate programs in nursing are competitive and some of them can be very daunting. But I find that I have to invite students to talk to me, to ask me, ‘What support services are available? Tell me about the admission requirements. Help me through the application process.’” As for what kind of advanced degree to get, once again it all depends on your goals.
“Some nurses are confused about advancing their education. They think they all have to be PhDs,” says Paniagua. “Well, if you’d like to be a nurse researcher, then a PhD is fine, because it’s primarily a research-focused doctorate. But then there are other avenues. You can get a doctorate in nursing practice (DNP), which is a professional practice degree, or you can get an EdD, which is an education-focused doctorate. So if you’re planning to have a career in academia, you should pursue either an EdD or a PhD. If you’re planning to practice or to work in the clinical setting, you should
Above all, the most important thing to consider when shopping around for a graduate program is finding one that’s the right fit for your specific needs—both academic and personal. “You need to make sure that your value system is in sync with the mission and vision of the institution,” Lyder says. “For example, here at UCLA we are a research-intensive school of nursing. Our professors infuse research and evidence-based practice into every course, every lecture, everything they do. If that’s not the type of learning environment you want, then this
But Alejandro believes that perhaps the hardest hurdle for minority nurses to clear is the surprisingly common “fear factor.”
get your DNP. Or you can just get a master’s degree [in your specialty area of interest, such as an MBA or an MSN in nursing informatics].”
isn’t going to be a good match for you.” Louie recommends investigating different program formats to find options that will
accommodate what she calls “your life needs.” For instance, if you have to keep working at your job while going to school, or you have young children or other family obligations, the traditional fulltime, brick-and-mortar campus model may not work for you. “You need to know that there are online programs, there are blended online/oncampus programs, there are part-time and weekend programs,” she says. Another alternative worth exploring is the accelerated (fast track) format. These programs include RN-to-MSN— also known as a Master’s Entry Program in Nursing (MEPN)— which bypasses the traditional BSN degree, and BSN-to-PhD, which bypasses the master’s. Their greatest advantage is that they enable nurses to earn graduate degrees more quickly and earlier in their careers. However, because the accelerated time frame makes the academic workload extremely intensive, these programs aren’t for everybody.
www.minoritynurse.com
Taking the Plunge Achieving the advanced degrees and certifications that will boost your career to a higher level can be an arduous process. But all the nurse leaders interviewed for this article agree that the rewards are worth it. In fact, with the right preparation, the right program, and strong support networks (family, friends, faith, colleagues, mentors, and minority nursing associations), it might just be easier than you think. Talley offers this advice: “Don’t be afraid to take the plunge. I think sometimes we [minority nurses] doubt ourselves, and there’s no reason to. Believe in yourself, have faith in yourself, and don’t let anyone interfere with your dreams.” Pam Chwedyk is a freelance health care writer based in Chicago. She is a former editor of Minority Nurse.
Minority Nurse Magazine
@MinorityNurse
29
The Take Pride Campaign The country is changing, with one-third of the population representing a historical “minority.” In this increasingly diverse world, you can confidently say your workplace actively fosters diversity, inclusiveness, and cooperation. For these reasons and others, you’re proud to be a part of it—and we want to hear from you. Minority Nurse is looking for nominations for health care’s diversity MVPs, from the magnet hospitals to nursing schools to local hospice care centers. Nurses can nominate their workplaces based on the facility’s efforts to improve and maintain inclusiveness and diversity. Think about what makes for a diverse institution. What does a “commitment to diversity” mean? And what does it mean to you? At Minority Nurse, it’s not just about a visible variety of skin tones seen in the halls. It’s . . . • Faculty and staff recruitment and retention efforts aimed at underrepresented populations • Collaborative hiring practices • Diversity initiatives and accessible organizations on site • Cultural competency training and resources, such as diverse foods, translators, etc. • Partnerships with other diversity organizations • And so much more When hiring groups devoted to minority recruitment and retention not only exist, but are consistently used, it shows a commitment to diversity. When hospital administrators take the time to include their nursing staff in development, they exhibit a commitment to diversity. And you, in taking the time to recognize your workplace for its commendable practices and diverse work environment, are showing a commitment to diversity as well. It’s not necessarily a numbers game—we don’t require applicants to produce statistics or quotas, though you are welcome to do so if you wish. We’re simply looking for readers who take pride in their workplaces’ commitment to diversity. A PDF of the Take Pride Campaign application is also available on our website, www.minoritynurse.com. Applications must be received before July 1, 2014. We will then reach out to our nominees to determine our winners! Questions? Let us know by e-mailing editor@minoritynurse.com.
30
Minority Nurse | FALL 2013
MINORITY NURSE
2014 Take Pride Campaign Application Application Form (Please print clearly. All fields required. The 250–500-word nomination can be attached separately.)
Your name __________________________________________________________________________________________ Your place of employment (must be a health care facility or institution employing nurses*) _______________________ ____________________________________________________________________________________________________ Location of facility___________________________________________________________________________________ How long have you worked at/for this facility? _________________________________________________________ Preferred e-mail _____________________________________________________________________________________ Preferred phone number _____________________________________________________________________________ In 250–500 words describe why you are nominating this facility—what makes it a model of diversity and inclusivity? __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ * All nominees must be health care–related workplaces that employ nurses, such as hospitals, nursing schools, nursing homes, hospice facilities, etc. Those work environments falling into nontraditional territories will be considered according to the discretion of the editors, staff members, and advisors of Minority Nurse. www.minoritynurse.com
Minority Nurse Magazine
31
@MinorityNurse
New to Nursing Joining the Profession from Divergent Fields BY LEIGH PAGE
32
Minority Nurse | FALL 2013
Two years ago, Evelyn Javier was working in a research lab in Maryland and was unhappy with her career. “I liked the job, but it did not fulfill my purpose,” she says. “I felt like there was more I could do.”
W
hat she really wanted to do, she decided, was to help people. In 2011, she quit her lab job and entered nursing school in New Jersey. Javier, now age 29, just received her RN degree and is about to launch her new career. Many young minorities,
who worked for a few years in low-paying jobs and then became more serious about their careers. Raines, who authored the 2011 study “What Attracts Second Degree Students to a Career in Nursing?” in OJIN: The Online Journal of Issues in Nursing, says nursing tends to be something these second-
These career-changers—usually in their mid-20s— are attracted by the opportunity to help others, get out of an office setting, and interact with many different people. after making false starts in other fields, discover that a career in nursing is actually the best fit for them. These career-changers—usually in their mid-20s—are attracted by the opportunity to help others, get out of an office setting, and interact with many different people. They also like the wide variety of nursing jobs they can choose from. Nurse educators say these more seasoned students are generally more intense, get higher grades, and have a clearer idea of their career goals than their younger counterparts. After trying out something else, “they know what they want,” says Deborah A. Raines, PhD, RN, ANEF, a professor of nursing at the University at Buffalo School of Nursing. Though Javier had good grades, Raines says some latecomers to nursing were initially poor students
careerists always wanted to do, but they were sidetracked into careers like teaching, business, or marketing for a few years. These students often bring skills from the previous jobs. Javier, for instance, says she brought a knowledge of aseptic techniques and teamwork skills from her lab job.
A Career Change From the Heart While traditional nursing students often cite salary and job security as key reasons for going into nursing, Raines says career-changers tend to have “intrinsic” motivations— reasons that come from the heart. “They really want to help other people,” she adds. Javier switched to nursing after she took a career aptitude test, showing the field was her real calling. “I realized I wanted to go back into the community,” she says. “I
www.minoritynurse.com
wanted to be the person providing the extra care for those in need.” As with many second-career nurses, Javier already had a college degree and could shorten her nursing education. Since she had already taken all the science courses she’d need for a bachelor’s in nursing degree, she was able to jump right into clinical training at the Muhlenberg School of Nursing in Plainfield, New Jersey. To help support herself as well as decide whether she wanted to be in clinical care, she took a job as a patient care technician at the same hospital where she was training. “I wanted to see if the hospital environment was right for me,” Javier says. It turned out to be a good fit. Having just earned her degree, Javier now plans to work for about a year and start a bridge program for a master’s in nursing degree next spring. Ultimately, she wants to be a nurse practitioner specializing in family health with an emphasis on women’s health. And as a member of the New Jersey Chapter of the National Association of Hispanic Nurses (NAHN), she wants to focus on helping Hispanic patients. “I’m concerned about the cultural and language barriers that Hispanics face,” she explains.
Overcoming Family Expectations Raines says second-career nurses often have to overcome family expectations about another line of work. “They were
Minority Nurse Magazine
@MinorityNurse
33
directed a certain way by their parents, and then they found out that nursing was what they really wanted to do,” she says. She recalls a second-career student from Haiti whose parents insisted that she should work at a law firm. The student did so for a while, but “she always wanted to be a nurse,”
in biology. But she didn’t like it and instead considered a career as a science teacher or in public health. Her career path took another turn when, as an undergraduate, she began working for a program to help boost minority participation in certain health care professions,
do research. Every discipline needs a nurse because we are the gatekeepers.” After graduating college in 2003, Curry briefly considered taking another minority recruitment job at the University of California in Los Angeles, but instead she enrolled in the University of Michigan’s
terest revolves around how parents with teenagers communicate about sex. Raines says many second careerists are “very focused about where they want to go.” She recalls a nursing student who came from a human resources job. “She wanted a nursing job in a certain unit, with a certain number of beds,” she recalls.
Helping Others
says Raines. She earned her nursing degree, worked for a year as an emergency medical technician, and then went back to graduate school. She is now in a doctoral program. Jade Curry, an African American nurse, also had to overcome the expectations of some family members who thought she should be a doctor. To see if she’d like it, she even worked in a dermatology office for a year and attended a mini-medical school at the University of Michigan, where she majored
34
Minority Nurse | FALL 2013
including nursing. She became a strong proponent of the profession. “There are so many things you can do with a nursing degree,” says Curry. “You can go into
School of Nursing. “Basically, I recruited myself,” she says. After earning a nursing degree in 2006, Curry received a master’s of science in nursing degree from the University of
Vaneta Condon, PhD, RN, served as director of the Pipeline to Registered Nursing program at Loma Linda University in California, which recruits underrepresented minorities into nursing. She says about 30% of the students already had a college degree in areas such as science, business, and teaching, and some already held jobs before they switched to nursing. “The biggest reason they give for going into nursing is wanting to spend more time helping people,” she says. Since they already had some life experiences, “they start off as better nurses. They can adapt more readily to a nursing program and working with other people.” Helping people has been the life work of Suleima RosarioDiaz, RN, who has been a minister in the American Baptist Church in New Jersey for many years. A few years ago, she decided to get a nursing
“There are so many things you can do with a nursing degree,” says Curry. teaching or practicing. You can work in multiple settings, like the ER or the ICU. You can get into a specialty like pediatrics or oncology. Or you can
Pennsylvania in 2009. Now married with a one-year-old son, she is a nursing PhD candidate and is working at a teen health center. Her research in-
degree with the goal of performing health care missionary work in other countries. Rosario-Diaz entered an accelerated nursing program at
the University of Medicine and Dentistry of New Jersey. Now age 30 and married, she works as an admissions and discharge nurse at Palisades Hospital in Edgewater, New Jersey, and is working on a master’s degree. She is still a minister as well as vice president of the New Jersey Chapter of NAHN. “Being a minister helps me to be a better nurse, to show love to people,” she says. “I want to be a calming presence.” Rosario-Diaz wants to combine her therapeutic education with pastoral counseling. “A lot of religious folks do chaplaincy work in the hospital, but that does not interest me,” she explains. “I want to be handson, to be a presence when you are in pain. I am task-oriented, so it’s a great fit.”
Other Experiences Minorities have entered nursing from all kinds of walks of life. From the loss of a loved
one to an unfulfilling job, inspiration can strike just about anywhere—and the smallest trigger can ignite that spark to become a nurse. Here are four examples to encourage you to make the leap:
nurse and then enrolled in the Accelerated Second Degree in Nursing Program at the Elms College School of Nursing. Combining Passions. For nine years, Randi Simpkins taught fifth and sixth grades
knowledge that I, myself, had not attained my own goals of academic accomplishment.” She “stumbled upon the opportunities in nursing” and enrolled in the Duke University School of Nursing in January 2012.
While traditional nursing students often cite salary and job security as key reasons for going into nursing, Raines says career-changers tend to have “intrinsic” motivations—reasons that come from the heart.
When Christine Hernandez’s mother was dying of cancer, a hospice nurse came into their home to care for her and sparked Hernandez’s interest in nursing.3 “She was amazing,” Hernandez told RN Builder.com. “It wasn’t just my mother she was helping but all of us. She was a strength that we just couldn’t have done without.” A few years later, Hernandez worked as a nanny for a dual-physician couple. They encouraged her to get an RN degree, so she enrolled in an RN program at Salt Lake Community College in Utah. Her goal is to work in pediatrics, oncology, or hospice.
Encouraged by Others.
Losing a Loved One. Chrispina Chitemerere was a schoolteacher in Zimbabwe before immigrating to the United States.1 She got a teaching job but didn’t like the work, she said in the May 2013 issue of the Elms News. Chitemerere said she found a new calling while taking care of her mother, who was dying of cancer. She became a licensed practical
in elementary school.2 “While I absolutely love the field of education, I knew that there was more for me to learn,” she wrote in an essay that won a Robert Wood Johnson Foundation New Careers in Nursing scholarship last year. “Daily I encouraged my students to pursue excellence and reach beyond their limits. Upon reflection, I was forced to ac-
www.minoritynurse.com
Minority Nurse Magazine
35
@MinorityNurse
Divine Intervention. In India, Binny Varghese earned a bachelor’s degree in human genetics and worked as a researcher in the biosciences.4 But as a child, “I gained a passion to serve others,” he told the Kansas City Nursing News in 2012. After immigrating to the United States for an arranged marriage with an Indian American woman, he decided that nursing was his real calling and entered an accelerated nursing program at MidAmerica Nazarene University in Olathe, Kansas. “When God wants you to do something better, he shows you the way,” he told the paper. Leigh Page is a Chicago-based freelance writer specializing in health care topics.
References 1. Elms College. From Africa to Chicopee, Two Students Earn Second Degree in Nursing. Elms News. May 15, 2013. www.elms.
edu/elms-news/from-africa-tochicopee-two-students-earn-second-degrees-in-nursing.xml. 2. Randi Simpkins. “I believe this about nursing...” essay. Robert Wood Johnson Foundation New Careers in Nursing. August 2012.
www.newcareersinnursing.org/ scholars/essay-contest/winners/ randi-simpkins. 3. G. Jones. Nursing Student Interview with Christine Hernandez. RN Builder. April 11, 2013. www.
rnbuilder.com/blog/education/ nursing-student-interview-withchristine-hernandez. 4. Nursing is second career for MNU student. Kansas City Nursing News. 2012. prewww.kccom-
munitynews.com/kc-nursingnews/30992401/detail.html.
A Man’s Guide to a Nursing Career Chad O’Lynn, RN, PhD
$30.00 | October, 2012 232 pp | Softcover ISBN: 9780826106858
11 West 42nd Street, 15th Floor, New York 10036 | P: 212 431 4370
36
Minority Nurse | FALL 2013
Academic Forum
An American Journey: From Constipation to Colorectal Cancer BY ED JAMES, MD
In my work as a radiologist, every day I see a whole lot of poop, well, actually images of poop. One of the most common emergency room patient complaints is abdominal pain and, too often, particularly in children, the cause is simply constipation. This is evident on imaging studies, and I believe this is a symptom of a much larger problem, our Standard American Diet, which is generally very high in animal-based foods and processed foods, and quite low in plant-based whole foods (e.g., fruits, leafy vegetables, and whole grains).
U
nfortunately, constipation is just the beginning for many of these youngsters. Here are just a few of the problems they are likely to encounter later in life without significant dietary changes: Hemorrhoids. These are vascular structures in the anal canal that help with stool control. They become pathological when swollen. They are composed of arterio-venous channels and connective tissue. Internal hemorrhoids usually present with painless rectal bleeding, whereas external hemorrhoids may be asymptomatic or, if thrombosed, may cause significant pain and swelling related to the anus region. Factors that increase intra-abdominal pressure (e.g., chronic constipation) contribute to hemorrhoids.
Diverticulosis/Diverticulitis. Diverticulosis refers to diverticula in the colon, which are outpocketings of the colonic mucosa and submucosal, through weaknesses of muscle layers in
the colon wall. These are more common in the sigmoid colon, which is a common place for increased pressure (e.g., chronic constipation) and are uncommon before the age of 40. Diverticulosis often results in painless rectal bleeding. Diverticulitis results when one of these diverticula becomes inflamed, may cause pain and fever, and can be complicated by abscesses, which occasionally require drainage procedures or surgery. Colorectal Cancer. Cancer is an uncontrolled cell growth, which in this case occurs in the colon or rectum. Symptoms of colorectal cancer typically include rectal bleeding and anemia, which are sometimes associated with weight loss, pain, and changes in bowel habits. Results of The China Study showed that high fiber intake (e.g., plant-based whole foods) was consistently associated with lower rates of cancers of the rectum and colon.1,2 Constipation and hemorrhoids used to be personal is-
sues for me. However, since adopting a whole food, plantbased diet, neither has been a problem and I sincerely doubt they ever will be. I consider myself fortunate that I did not progress to diverticulitis or colorectal cancer before making my dietary changes. It is noteworthy that recent studies seem to suggest that the environment within our colon may be a predictor of our risk of many chronic diseases. A chronic failure to expeditiously eliminate waste/toxins through our bowel seems to have reverberating consequences throughout our body. Furthermore, it has been my anecdotal observation over the last 15 years as a practicing radiologist that adults in whom I diagnose constipation on imaging studies are much more likely to have cancers (e.g., breast, prostate, and colorectal) and visible atherosclerotic disease. Yet, relatively few dollars are spent on research and education related to the benefits of a plant-based diet to promote colon health. Instead, like other cancers—including breast and prostate—most expenditure in the United States is toward screenings for early detection and implementing treatment regimens following diagnosis. Why do we not place more value on nutritional prevention in our US health system? Why do we generally prefer only to diagnose/screen and to treat? As health care professionals, we can and should educate our patients and encourage them with regard to plant-based foods as the most comprehensive and effective way to prevent the diseases that result in most American deaths. By starting with our children, we can give them each an opportunity
www.minoritynurse.com
for a healthier, longer, and more productive life, free of many chronic diseases. Dr. Ed James is an editorial advisory board member of Minority Nurse and the founder and president of Heal2BFree, LLC (http://
heal2bfree.com) References 1. Li JY, Liu BQ, Li GY, et al. Atlas of cancer mortality in the People’s Republic of China. An aid for cancer control and research. Int J Epidemiol. 1981 Jun;10(2):127-33. 2. Junshi C, Campbell TC, Junyao L, Peto R, eds. Diet, Life-style and Mortality in China: A Study of the Characteristics of 65 Chinese Counties. Oxford, UK; Ithaca, NY; Beijing, PRC: Oxford University Press; Cornell University Press; Peoples’s Medical Publishing House; 1990.
Minority Nurse Magazine
37
@MinorityNurse
Academic Forum
Keeping Back Pain at Bay BY TERAH SHELTON HARRIS
Nurses are at a greater risk of back pain than many other occupations. According to a study by the University of Alberta’s faculty of rehabilitation medicine, 65% of orthopedic nurses and 58% of ICU nurses develop debilitating lower back pain at some point in their careers. Due to the nature of the job, it isn’t hard to see why. Nurses often work with poor posture (repetitively leaning and bending over bedridden patients, lifting and transferring heavy and slumped patients), so it’s no surprise that they have the greatest incidence of back pain.
T
odd Sinett, a chiropractor and author of The Truth about Back Pain, says back pain sends more patients to the doctor than every other condition except the common cold and is the leading cause of job disability in people under 45. “Nurses often suffer from back pain more than other professions because they are susceptible to many triggers that can cause back pain,” he says. “Standing for long hours, reaching over patients, and doing heavy lifting are all contributing factors to structural
38
Minority Nurse | FALL 2013
causes of back pain.” He adds that back pain affects all ages and demographic groups, so all nurses, not just minority nurses, are equally at risk of getting lower back pain.
Work-Related Factors Michael Ho, a chiropractor and acupuncturist, adds that nurses’ high stress levels often causes chronic muscle fatigue and strain, which can lead to the eventual hardening of muscles, loss of range of motion, and early degeneration of the lower back structure.
“The subluxation of spinal joints over time causes premature degeneration of the facet joints and spinal disc,” he says. “Over time, degeneration of the disc causes herniation and irritation of spinal nerves. This, with the combination of tight muscles, joint restrictions, disc herniation, and nerve impingement can cause local back pain as well as radiating hip and leg pain.” Poor dietary practices are the most overlooked causes of back pain, Sinett adds. Nurses tend to have long shifts that can make eating right difficult.
Diets filled with caffeine and sugar elevate the body’s cortisol levels. Elevated cortisol levels often raise the inflammatory factors in the body, which can result in back pain. “We are what we eat, so make sure that you are eating good, healthy, wholesome foods,” he says. “Plan ahead and make healthier eating choices [and] your back will thank you.”
Avoid Back Pain During Long Shifts Even though back pain is quite common, it doesn’t make it normal. Sadly, some
Academic Forum nurses have resigned themselves to living with some level of discomfort. But they don’t have to. David Simpson, a chiropractor and owner of Gotham Healing Arts, believes a few simple changes such as proper posture and body usage may prevent nurses from sustaining injuries. He recommends the following tips for nurses: Don’t slouch. The lower back or lumbar spine joints
hour squeezes most of the water out of this spongy tissue; quicker if you slouch. Without the water, your joints become brittle and susceptible to wear and tear. Lift with your legs. “In spite of this advice, most lift improperly,” says Simpson. “Most people bend their knees first, but only for about 30 degrees, then they involve their back, and they start to bend at the waist, especially if the object
Sadly, some nurses have resigned themselves to living with some level of discomfort. But they don’t have to.
are like moist sponges, he says. Healthy joints contain a lot of fluid, and sitting for an
is not directly under them.” Ideally, the back should never round like that of a low-
humped camel. This body position puts pressure on the spinal joints, which leads to damage over time and will eventually turn into pain at some point in your life, he adds. Erect, good posture. At best it is a bad habit, but there are practical biomechanical reasons for standing up straight, Simpson says. Proper standing helps you keep your normal spinal curves, reduces the compressive forces on those joints, and reduces the likelihood of painful episodes of back pain. Sinett says stretching is one of the best back-pain-relieving exercises and suggests nurses stretch at least for 3 sets at 12 petitions each day. “Stand up straight, raise both arms above your head, and gently lean back approximately 35 degrees,” he says. “Extending
www.minoritynurse.com
the spine will counteract the forward hunch that nurses do by sitting in front of the computer and being hunched over patients.” Overall, Ho stresses the importance of nurses taking care of themselves first. He recommends all nurses exercise, rest, and eat properly every day, and more importantly, get the treatment they need to relieve any minor problems in their back before it gets more severe and becomes more chronic in nature. “It’s important to remember that it’s better to get rid of a mild back problem before it becomes a serious degenerative problem that can lead to disability,” he says. Terah Shelton Harris is a freelance writer based in Alabama.
Minority Nurse Magazine
39
@MinorityNurse
Second Opinion
Honesty and Ethics in Nursing BY JEBRA TURNER
The latest Gallup Poll of Honesty/Ethics in Professions says the most trusted profession (for an astounding 13 out of the last 14 years) is—drumroll, please—nursing. When random Americans were asked to “please tell me how you would rate the honesty and ethical standards of people in these different fields,” more than 85% gave nurses “high” or “very high” marks.
T
his year’s rating is the highest since 1999 when the profession was first included in the poll. The one year nurses didn’t top the list? It was 2001, after the terrorist attacks of 9/11, when firefighters were included for the first and only time and scored higher. Gallup conducts the telephone survey in late November each year. Health care professions dominated the top five most trusted groups: pharmacists came in next at 75%, medical doctors rated 70% (tied with the oddballs in this cohort— engineers), and dentists earned 62%. The lowest rankings go to car salespeople (8%) and, sadly, members of Congress (10%). What is it that makes nurses so trustworthy? There are as many theories as respondents.
therapists, say? Not likely. The Gallup data suggest that women—on the whole and on average—are seen as more trustworthy than men. So would male nurses earn the same trust ranking as female nurses? Most likely. But can nurses count on garnering trust automatically? Definitely not. In the end, trust is personal. Some minority nurses especially feel that they must battle for respect. Here are a few ways to enjoy high regard in this very special profession—one that for many nurses is more of a “calling” than an occupation.
Embrace your role as a caregiver and patient advocate. “One reason for trust is that nurses have what I call the home-court advantage,” says Ramón Lavandero, RN, MA,
fessionals. In the hospital, it’s 24/7; even with home care, nurses still have more patient and family contact than anyone else.” Lavandero says another factor is that above all else, nurses keep their patients’ needs in mind. “They see nurses going
Strong communication skills become even more important when there is perceived bias, such as a patient who believes a minority nurse may be less competent or have a substandard education. Some say intimacy. After all, we stand naked—both literally and metaphorically—before nurses. But would the ratings be similar for massage
40
Minority Nurse | FALL 2013
MSN, FAAN, senior director of the American Association of Critical-Care Nurses. “They’re with patients and their families more than any other pro-
to bat for them when there are rules or systems in a health care setting that aren’t effective.” For example, it doesn’t serve end-of-life patients, he
says, when hospital regulations don’t allow visits from a lifelong pet.
Turn up the volume with stellar communication skills. “One of the things I learned as a man and a nurse and as a native Puerto Rican is that if I was comfortable in a situation, the patient was comfortable,” says Lavandero. “Ninety-nine percent of my experience was without problem, and that includes the year I worked in a labor and delivery unit.” Strong communication skills become even more important when there is perceived bias, such as a patient who believes a minority nurse may be less competent or have a substan-
Second Opinion dard education. “That’s when your communication needs to shine,” he says, “perhaps by addressing the unasked question with a comment like ‘Did you know, when I was a student at Columbia University …’” A skilled communicator learns that direct confronta-
The future can be brighter, though, if nurses realize the public’s trust in nurses is “sacred” and “hard won.” tion is only one way to address barriers such as mistrust, he adds. Nurses must communicate with many parties besides patients, including families, administration, and other health care staff members. It’s not easy to speak to (and on behalf of) multiple constituencies, especially when a nurse isn’t familiar with a patient’s desires, circumstances, or cultural background. “That’s why we need to learn all we can about a patient and have to determine how to be honest without creating or introducing more difficulties,” says Lavandero.
Recognize that ethical issues are a cornerstone of nursing. “Nurses are also trusted because their Code of Ethics is grounded in fairness and respect for all people,” says Cynda Hylton Rushton, RN, PhD, FAAN, the Anne and George L. Bunting professor of clinical ethics at Johns Hopkins University in Baltimore. Ethical training is part of every nursing school curriculum, and a code of ethics guides all nurses as they care for patients, she says. This is not a profession that only pays lip
service to a moral ideal. Some common ethical questions that nurses must consider, according to Rushton, are: “How do we balance what patients or families want with what’s available? (Often there are limits.) Also, how do we balance quality care with safety and efficiency?” One element of quality care is relationships, she says, but the “health care system is relationally depleted” and devalues relationships in favor of efficiency. Also, our American society and health care system “would like to pretend that death is optional,” she explains. “There is such fear and despair around aging, illness, disability, and death. Sometimes we feel that we’re doing things that are harmful or disrespectful to patients. That’s not what we’re called to do as nurses.” Nurses are often at the center of trying to navigate a broken system that causes them much distress, she adds. Moral distress is a term Rushton uses to describe when a nurse knows the moral thing to do, but feels powerless to act on it. It’s paramount that nurses become knowledgeable about ethical issues and effective ways to address quandaries, she says. The future can be brighter, though, if nurses realize the public’s trust in nurses is “sacred” and “hard won.” She implores nurses to “make sure, first of all, that we’re deserving of it. And second of all, uphold that trust.” Jebra Turner is a freelance health and business writer based in
NURSING OPPORTUNITIES The University of Connecticut Health Center is a leading healthcare, educational and research facility offering challenging nursing positions in all specialty patient care areas as well as Case Management, Nursing Informatics, and Outpatient Services. We are an equal opportunity employer with a strong commitment to diversity and provide: • Competitive Benefits
• Competitive Salaries
• Upward Mobility
• Excellent Training
Department of Human Resources 16 Munson Road Farmington, CT 06034-4035
860.679.2426 phone 860.679.1051 fax
For a complete listing of all open jobs visit our website:
www.uchc.edu Affirmative Action /Equal Opportunity Employer
KNOW BETTER CARE
You care for patients. Who cares for you?
J AC K S O N V I L L E
NOW HIRING MOTIVATED AND DEDICATED RNS
University of Florida Health Jacksonville is an academic health center that provides a wide range of health care services on an inpatient and outpatient basis. We offer a fast-paced environment on the leading edge of the latest treatments and technologies.
Portland, Oregon. She frequently contributes to the Minority Nurse magazine and website. Visit her
Apply today at 1-800-889-8920 or UFHealthJax.org/nursing.
online at www.jebra.com.
UF Health Jacksonville is an equal opportunity employer.
www.minoritynurse.com
Minority Nurse Magazine
@MinorityNurse
41
Second Opinion
Technology in the Workplace: How You Can Prepare BY NIKKI YEAGER
Most of us have heard the term “digital divide,” and many of us are familiar with the move towards electronic health records (EHRs) in the workplace. However, very few hospitals or medical offices are discussing the reallife implications of those two facts merging in hospitals and medical offices across the country where nurses who have limited computer experience are suddenly being asked to do electronic charting.
A
ccording to the US Census Bureau, only 56.9% of black and 58.3% of Hispanic households had internet access in their home, compared to 76.2% of all non-Hispanic white households, in 2011. This means minority households are currently falling on the wrong side of the digital divide. That being said, 26.8% of the nursing students in baccalaureate
42
Minority Nurse | FALL 2013
programs from 2010-2011 were minorities, according to the American Association of Colleges of Nursing, which means we have a significant percentage of nurses who will be entering the workplace with the potential of having limited computer experience. In the past, that wouldn’t have been a problem, considering most medical offices used paper charts and filing systems.
However, with the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009, medical offices and hospitals are being strongly encouraged to adopt EHRs as quickly as possible. According to the HITECH Act, medical offices that do not use an EHR in a “meaningful way” by 2015 will start to incur penalties, beginning with a cut of 1% to Medicare funding in 2015 and increasing to 3% in 2017. After that point, medical offices may also be subject to additional financial penalties. What does that mean for today’s nurses? Based on government reports, 72% of office-based physicians used electronic medical records (EMRs) or EHRs in 2012. In
Massachusetts, that number goes as high as 89.2%. In order to qualify for funding and avoid penalties, offices must have met “meaningful use” objectives in 2012, including electronically tracking all orders, vital signs, medication allergies, medications taken, patient demographics, and smoking status. Any of those items sound familiar? The same things nurses have been entering on paper charts for decades are now being entered electronically. In short, this means if you haven’t already begun using an EHR or EMR on the job, you will probably see one soon. And if you’re just starting out, the chance of finding a nursing position without needing to use one on a daily basis is dwindling
Second Opinion incredibly fast. For some, that could mean using a piece of hardware or technology for the first time. But the transition doesn’t need to be scary. So, how exactly can you prepare for the change?
If for any reason you cannot attend a session the first time around, don’t hesitate to ask for additional training or inquire about what tutorials and materials might be available for you to review. There are
In short, this means if you haven’t already begun using an EHR or EMR on the job, you will probably see one soon. First of all, it’s important to understand that the EHR/EMR industry comes with support— and lots of it. If you’re currently at a job that’s implementing an EHR system like Cerner, Epic, or Allscripts, and you haven’t already done so, ask for training. Almost all EHR companies offer comprehensive training during the implementation process, and it’s expected that staff will attend those sessions.
entire support and training departments within each of the large EHR companies. Those departments are available to make your transition easier, so don’t be afraid to use the resources made available to you. For the thousands of nursing students who will be entering a largely electronic workplace, what other preparations can be made? Many nursing instructors have decided to face
201 Careers in Nursing Joyce Fitzpatrick, PhD, MBA, RN, FAAN; Emerson E. Ea, DNP, APRN-BC, CEN
$20.00 | August, 2012 312 pp | Softcover ISBN: 9780826133823
the issue head on. By providing nursing students with access to an academic EHR in the classroom, instructors can help make the transition easier for students when entering the workforce. After all, nurses have enough to worry about during their first week in the field. Computer programs like EHR Tutor, based in Parma, Ohio, can be purchased by nursing schools and used as a daily teaching tool in the classroom. For example, when discussing vitals or medications, students can look at charts done for electronic patients and analyze that data. Students can also chart information themselves, just as they would on paper, which can then be submitted to the instructor for grading. Schools with access to iPads or laptops are also allowing students to use programs like EHR Tutor during
Fast Facts for the Student Nurse
clinical rotations to chart real information under fake patient names. That way, by the time students are on their own, using EHRs will be just as comfortable as pen and paper. EHRs and EMRs are here to stay. For some nurses, that may present a tremendous challenge. However, there are many tools available to nurses who may be feeling a bit overwhelmed. By using those resources (like using academic EHRs in the classroom and asking for additional training in your workplace), we can ensure that our nurses and future nurses make the transition to EHRs as painlessly as possible. That way, our nurses can spend more time focusing on the important things—the patients. Nikki Yeager is a freelance writer and software trainer based in New York City.
The New Nurse Educator Mastering Academe
Nursing Student Success in a Nutshell
Deborah Dolan Hunt, PhD, RN
$50.00 | October, 2012 304 pp | Softcover ISBN: 9780826106414
Susan Stabler-Haas, MSN, RN, CS, LMFT
$30.00 | May, 2012 200 pp | Softcover ISBN: 9780826193247 WWW.SPRINGERPUB.COM/NURSING
www.minoritynurse.com
Minority Nurse Magazine
43
@MinorityNurse
Degrees of Success
Growing the Numbers of Diverse Nursing Faculty BY ROBIN FARMER
A chance encounter with a professor at the University of Colorado Denver changed the trajectory of Anissa Buhring’s career, transforming her dream of teaching into a goal with a deadline.
Anissa Buhring, CNS, RN
I
t was a summer day in 2003 when she decided to learn more about the university’s doctoral programs, recalls Buhring, CNS, RN, a clinical education specialist at East Morgan County Hospital in Brush, Colorado. Buhring, who is Latina, had always wanted to earn her PhD and teach. “[But] those were jobs that people outside of my ethnic background held. Even though that was a dream of mine...there was nobody else like me that I came across,” she notes. But that summer day, she briefly met Dr. Ruby Martinez and walked away inspired. “She doesn’t realize what a huge influence she had on me that day. At that moment, I realized [my goal] was possible and that there was someone else like me that had done it. She told me that I needed to do it and I could do it. She gave me her card, and I never ran into her until years later as part of the National Association of His-
44
Minority Nurse | FALL 2013
Carolina G. Huerta, EdD, RN, FAAN
panic Nurses. And now she’s my mentor,” says Buhring, a 2012 recipient of the Johnson & Johnson/American Association of Colleges of Nursing (AACN) Minority Nurse Faculty Scholars program and a PhD candidate at the University of Colorado Denver. Buhring’s memorable experience illustrates the power of diverse academic role models, which most nursing schools and programs across the country lack. According to 2011 data from AACN’s annual survey, only 11.8% of full-time nursing school faculty come from minority backgrounds, and only 5.1% are male. “I believe that when students do not see faculty that look like them, they feel that it may be impossible to attain high-level career goals,” says Carolina G. Huerta, EdD, RN, FAAN, chair of the nursing department at the University of Texas-Pan American (UTPA), where 85% of the faculty is minority. “Stu-
dents who do not see faculty that look like them may not approach faculty for clarification on academic material for fear that they will not be understood. All of the literature supports the importance of role models that look like and can relate to the students culturally.” In 1992, when Huerta became chair, she decided the program would grow its own diverse faculty to better serve the majority-Hispanic student enrollment. Today, out of 27 nursing faculty, four are nonHispanic white; six are Asian; one is mixed Hispanic; and 17 are Hispanic. There is one male, although that may change since 20% to 25% of students in the nursing programs (BSN and MSN) are male. Located 12 miles from the Texas-Mexico border, “our university is located in an area that is poor and medically underserved, and many do not find it a desirable place to seek employment,” says Huerta. Not many people apply for faculty
from UTPA. Seventeen of the 27 faculty employed received their MSN through UTPA or through a UTPA cooperative program. Seven faculty members have either finished or are at the dissertation phase of their PhD/ DNP. “I believe that the ‘grow your own’ philosophy has been extended by my giving them the time to complete doctoral work. The program coordinators and I have done as much as possible to accommodate their work schedule so that it does not conflict with their doctoral study,” says Huerta, who is “unaware of another program like ours.” Culturally competent mentoring, more scholarship money, and better faculty salaries will increase diversity in nursing education, says Huerta, who was named by AACN and the Robert Wood Johnson Foundation (RWJF) as the National Advisory Committee chair for RWJF’s New Careers in Nursing (NCIN) program. The program provides scholarships to secondcareer college-educated minor-
Buhring’s memorable experience illustrates the power of diverse academic role models, which most nursing schools and programs across the country lack. positions or employment from outside the area. There are few jobs for spouses or significant others, and the proximity to the Mexican border is not a selling point. Many of the nursing faculty were born and raised in the community or are longtime residents. Many graduated
ity or disadvantaged individuals pursuing a career in nursing by enrolling in accelerated BSN and/or MSN programs. The NCIN program has supported over 125 schools and awarded $35,170,000 in scholarships to 3,517 entry-level nursing students in the United States since it started in 2008.
Degrees of Success
RN_Generic-3.4 x 4.5_HFSC 7/22/13 11:46 AM Page 1
Special Careers begin in a Special Place.
As the only long-term acute-care hospital in the nation serving adults and children, Hospital for Special Care is nationally recognized for advanced care and rehabilitation in the highly specialized areas of pulmonary care, acquiredbrain injury, medically-complex pediatrics, neuromuscular care, congestive heart failure, and spinal cord injury. We are a 228-bed, Joint Commission and CARF-accredited, state-of-the-art facility with our main campus located in New Britain, CT and a satellite campus in Hartford, CT.
Nursing Opportunities For a complete listing of all open positions, visit our web site at www.hfsc.org To apply, please submit your resume to: Employee Development Services Hospital for Special Care 2150 Corbin Avenue, New Britain, CT 06053 E-mail: jobs@hfsc.org FAX #: (860) 827-4848 AA/EOE M/F/D/V
“I think that a program such as this that focuses specifically on preparing nursing educators could be a success,” says Huerta. More scholarships would make a difference, especially if no major strings are attached such as having to work for X number of years in an underserved area, she says. Boosting faculty salaries would also make nursing education a more appealing career. “We need to infuse money into campaigns that highlight minority and diverse nurses making a difference, especially in nursing education. I know that Johnson and Johnson has done this and they have been success-
ful. We need more of this.” One of five recipients selected for the Johnson & Johnson/ AACN Minority Nurse Faculty Scholars program last year, Buhring agrees more opportunities are needed to develop a pipeline for minority educators. She pitches in as a mentor for middle and high school students as well as first-generation college students. Buhring looks forward to the impact she will have as an educator. “I want to pass that flame to others,” she says. “Whether it’s for nursing or just knowing it’s possible as a Latino to go to college.”
Help
InSPirE Better Health
At Carilion Clinic, our nurses inspire better health for our patients and our communities through comprehensive, compassionate care. We offer numerous opportunities for professional development, competitive pay and relocation assistance. Take advantage of all that southwest Virginia has to offer including stunning mountain and lake views, four-season climate, excellent schools and nationally recognized colleges and universities including the Virginia Tech Carilion School of Medicine and Research Institute. Visit CarilionClinic.org for details. Carilion Clinic is an Equal Employment Opportunity/Affirmative Action Employer.
Robin Farmer is a freelance writer based in Virginia.
www.minoritynurse.com
Minority Nurse Magazine
45
@MinorityNurse
Degrees of Success
Racial Disparities of Nursing Educators and Students BY ELISS CUCCHIARA
Due to the shortage of nurses in the workforce, many nursing schools are making an effort to increase their enrollment of students. Although there is an effort to increase the enrollment of nursing students, there are still racial disparities within the nursing student population—and this disparity correlates to the racial disparity of nursing educators.1 Without a diverse population of nursing educators, minority students are often made to feel invalidated in various situations, particularly in relating to professors culturally and receiving appropriate advice on cultural and ethnic relations in the workforce.
A
ccording to the National League for Nursing’s Annual Survey of Schools of Nursing, only 12% of the nursing student population in a baccalaureate program in 2012 was African American. That number dwindles for other minority groups: 8% were Asian or Pacific Islander; 1% were American Indian or Alaskan Native; 6% were Hispanic; and 6% were “other.” When you compare that to the fact that only 12.6% of nursing educators are minorities and only 6.2% are male, then you realize there is a dire need for diversity within nursing school institutions to correlate with the student population.2 In addition to the academic stressors that all nursing students have to face, minority nursing students have other challenges. Those challenges include having limited access to moral and emotional support, inadequate academic advising, low professional socialization, and little to no mentoring. Due to these fac-
46
Minority Nurse | FALL 2013
tors, minority students have to overcome additional barriers that may impede on their academic success. Minority students also often feel the encumbering emotions that are attributed to isolation and discrimination. Isolation is often felt by minorities in professional settings, and it is heightened in various pro-
by a nursing school admission counselor, “They don’t want your kind.” Discrimination of a minority nursing student is often felt in the classroom as
Additionally, too often minority students feel as though they’re going through a hazing process in school in order to be placed on the same level as their white peers.
fessional schools.3 As a result of limited minority nursing peers and nursing educators, minority nursing students often feel as though they’re not supported. Veronica, an African American woman who recently matriculated from a nursing school in the southeastern part of the United States, noted experiencing the disheartening emotion of racism when she was told
well as in the clinical setting. Minority students feel the burden of being discriminated against by patients who don’t wish to work with the student due to the color of the student’s skin. Additionally, too often minority students feel as though they’re going through a hazing process in school in order to be placed on the same level as their white peers.3 Men continue to be highly
underrepresented in the field of nursing, and their presence is even smaller in the classroom. Being a double minority comes with added hardships at times, and it may explain why many minority males do not choose to go into the field of nursing. Manuel Romo is a thirdsemester nursing student at Northern Arizona University’s Tucson campus. He is the president of the Student Nursing Association and one of the few Hispanic male students. When asked about his perception of his role as a double minority in the nursing program, he verbalized, “As I have seen, nursing is predominately white females, which in turn is probably a reason why there are mostly Anglo female instructors. I believe that more needs to be done to attract instructors from various di-
Degrees of Success verse backgrounds in order to attract more minority groups to enter the nursing field.” The US Census Bureau predicts that minority ethnic groups will be the majority by the year 2043. With the change in our society will also come a change in the patient populations; they, too, will be predominately minority ethnic groups. The nursing profession will need to be able
to be culturally sensitive and diverse in order to provide adequate clinical care. The fundamental change of the nursing profession starts at the level of the nursing students, and it’s imperative that nursing schools acknowledge this and begin to welcome an environment that represents diversity in its faculty. Currently, the National Sample Survey’s data notes that mi-
nority RNs are more likely than white RNs to obtain baccalaureate degrees and other terminal degrees in nursing.2 The reasoning for this isn’t fully understood beyond the recognition of knowing an advanced terminal degree brings about more career opportunities and the opportunity to have leadership and education roles—roles that seem to be absent in nursing institutions.
The methods for recruiting and retaining minority nurse educators aren’t a one-sizefits-all solution. Every school is different and unique in its own way, but the methods can’t wait too long. It’s about time that nursing institutions implement a reliable and realistic plan to promote diversity within their faculty and within their students. As nurses, we’re committed to being lifelong learners for the advancement of our patients and ourselves. Cultural competence is a key factor in relating to one another, and if it’s not cultivated in the classroom, then we as nurses are bound to face problems beyond. Eliss Cucchiara is a second degree nursing student at Northern Arizona University. She will obtain her bachelor’s of science degree in nursing in the fall of 2014. References 1. National League for Nursing. 2010 NLN Nurse Educator Shortage Fact Sheet. February 2010.
www.nln.org/governmentaffairs/pdf/nursefacultyshortage. pdf 2. American Association of Colleges of Nursing. Enhancing Diversity in the Workforce. Fact Sheet. Last updated April 17, 2013. www.aacn.nche.edu/ media-relations/fact-sheets/ enhancing-diversity 3. Loftin C, Newman SD, Dumas BP, Gilden G, Bond ML. Perceived Barriers to Success for Minority Nursing Students: An Integrative Review. ISRN Nurs. 2012;806543.
www.minoritynurse.com
Minority Nurse Magazine
47
@MinorityNurse
MINORITYNURSE.COM In the Spotlight
Newsletter
Marsha D. Thomas, RN NOMINATED BY REV. STEVEN K. WHEELER, MSN, RN
M
arsha D. Thomas, RN, is a servant leader and an innovator. She has accomplished much in her lifetime: she was the first Upward Bound student at the University of Cincinnati/Xavier University; she was the first African American parish nurse in the city of Cincinnati; she received a grant from the Susan G. Komen Foundation to develop a faithbased play on breast cancer; and she is the current president of the Black Nurses Association of Greater Cincinnati. Marsha has created strong, positive programs to bring in disadvantaged students and take them through the nursing program to graduation. She has recruited nursing leaders
from diverse backgrounds that will lay a strong foundation for future nurses within the Black Nurses Association. Thomas, along with Rev. Steven K. Wheeler, MSN, RN, will institute a citywide graduation celebration for any/all minority students who graduated from any nursing school in 2013. Marsha is a very passionate person, and she is constantly challenging the community to change health outcomes for the disadvantaged. She is the project manager for her church at a clinic that is currently under construction in Benin, West Africa, to help women and children. Marsha has three grown children and three grandchildren. She is truly a bright light in a very dark world.
What makes Marsha even more remarkable is that she has been diagnosed with multiple sclerosis and has been undergoing radiation treatment as well. But she has not allowed her disability to stand in the way of her service to others. At the community graduation celebration of nurses, you could witness firsthand the handiwork of this great lady. One graduating nurse had flunked out of several schools, and this student was about ready to throw in the towel on her dreams. Someone recommended that she go and speak with Marsha Thomas. After speaking with Marsha, this student was connected with tutors and received the necessary help to make it through the program.
Marsha held on to this student all the way through the nursing program, and that night everyone witnessed the success story that Ms. Thomas helped to orchestrate. Might I add that this young lady had one eye. Marsha had the student focus on her ability and not her disability. As a result of Marsha’s dedication to the field of nursing and to humanity, Impact Christian Ministries has designed an award to be given away on a yearly basis in honor of this beautiful young lady. The award will be given to an outstanding individual nurse. Attached to the award will be $1,000 and an award that will be designed by local artist Jon Carter. Nomination forms will go out around the country so that this living legend will not be forgotten but emulated for generations to come. The first annual “Citywide Graduation Celebration” can be seen at www.ConsciousMediaProductionsTV.com. Is there a nurse in your life who inspires you? Nominate him or her to be featured in our new “In the Spotlight” series by sending an e-mail to editor@minoritynurse. com. Or visit our blog at www. minoritynurse.com/blog to learn about outstanding nurses across the country making a difference.
48
Minority Nurse | FALL 2013
MINORITYNURSE.COM Highlights from the Blog
Newsletter How to Tackle Nurse-on-Nurse Bullying It’s common knowledge that bullies are mean, manipulative, and moody. But do you know what to do when the bully is your boss? Bullies exist in every workplace; but when nurses harass other nurses, their harmful behavior can also affect patient care and safety.
Should You Relocate? Three Things to Consider Have you ever dreamed of living in another region? Have you often wondered if your location is a career roadblock? Relocating for your career or for a desired lifestyle change is sometimes the best move for nurses and one that is frequently available to nurses specifically. Nursing skills are needed in all areas, and a move can not only bring a career boost, but much needed personal change as well.
Start Now to Improve Your Organization’s Climate Any nurse knows a well-run unit has excellent staffing and dedicated workers, but such a cohesive environment also has something not so easily defined. What can you do if you don’t feel supported by your organization or if, as a supervisor, you would like to see your unit operating more effectively?
Social Media Profile May Win or Lose You Jobs Looking for a job? Before applying for a new position, examine your social media profile. Employers are increasingly searching social media sites to look for potential hires with a professional image and good qualifications. Anything less, and you may be rejected on the spot.
To read more, visit www.minoritynurse.com/blog.
www.minoritynurse.com
Minority Nurse Magazine
49
@MinorityNurse
MINORITY NURSE SCHOLARSHIP PROGRAM Sponsored by the National Coalition of Ethnic Minority Nurse Associations (NCEMNA) and Minority Nurse Magazine Nurses will always be valuable members of any health care team, regardless of their educational backgrounds. Yet, the baccalaureate and master’s degrees in nursing may offer the most professional opportunities. That’s why Minority Nurse has teamed up with NCEMNA to co-sponsor an annual scholarship to help outstanding nurses from under-represented groups complete their studies toward a Bachelor or Master of Science in Nursing. To date, we have awarded scholarships to more than 40 students, honoring their commitment to the profession, academic excellence, and community service. We are currently accepting applications for our 15th annual scholarship competition, consisting of two $1,000 awards and one $3,000 award. Scholarships will be paid in summer 2014 for the fall 2014 academic term. Questions? E-mail editor@minoritynurse.com or visit www.minoritynurse.com/scholarship/minority-nursemagazine-scholarship-program
MINORITY NURSE 15th Annual Scholarship Program
Application Form (Please print clearly) Name ______________________________________________________________________________________________ Address ____________________________________________________________________________________________ City/State/ZIP Code _________________________________________________________________________________ Phone _______________________________ E-mail________________________________________________________ Nursing school ______________________________________________________________________________________ Expected date of graduation _________________________________________________________________________ Gender: ❏ Male
❏ Female
Ethnic background: ❏ African American ❏ Hispanic/Latino ❏ Asian/Pacific Islander ❏ American Indian/Alaskan Native ❏ Filipino ❏ Other______________ Please list any nursing associations (student, minority, or otherwise) to which you belong: __________________________________________________________________________________________________________ __________________________________________________________________________________________________________
Who Is Eligible (Please read carefully. Applications that do not meet the eligibility criteria will be disqualified.) To apply for this scholarship, students must meet all four of the following criteria: Be a minority in the nursing profession Be enrolled (as of September 2014) in either the third or fourth year of an accredited BSN program in the United States OR an accelerated program leading to a BSN degree (such as RN-to-BSN or BA-to-BSN) OR an accelerated master’s entry program in nursing for students with bachelor’s degrees in fields other than nursing (such as BA-to-MSN). Graduate students who already have a bachelor’s degree in nursing are not eligible. Have a 3.0 GPA or better (on a 4.0 scale) Be a U.S. citizen or permanent resident How to Apply (Please read carefully. Applications that do not include the required documentation will be disqualified.) Complete and return this form along with all three of the following documents: Transcript or other proof of GPA Letter of recommendation from a faculty member outlining academic achievement A brief (250-word) written statement summarizing your academic and personal accomplishments, community service, and goals for your future nursing career Important: An English translation must be provided for any documentation that is not in English. Minority Nurse will award one $3,000 scholarship and two $1,000 scholarships in 2014. Selections will be made by NCEMNA. Scholarships will be paid in summer 2014. Minority Nurse reserves the right to verify community service and financial need.
Deadline for application: February 1, 2014 Return application form and documentation to: Minority Nurse Magazine Scholarship, Springer Publishing Company, 11 W. 42nd Street, 15th Floor, New York, NY 10036
Academic Opportunities
A
s you are probably aware, the demand for nurses continues to skyrocket. What you may not know is that there’s also a critical need for nurses with advanced degrees, as hospitals turn to nurses to fill more administrative and leadership roles. Nursing schools around the country are jumping at the chance to fill this void by offering flexible Master of Science in Nursing and Doctor of Nursing Practice programs, and you’ll find many great examples in the following pages. There truly has never been a better time to pursue an advanced nursing degree. Be sure to secure your spot in the program— and your financial aid—by applying early.
52
Minority Nurse | FALL 2013
Academic Opportunities
Applications now open! The Betty Irene Moore School of Nursing at UC Davis — a new nursing school with a vision to advance health and ignite leadership through innovative education, transformative research and bold system change. Current graduate degree programs:
Doctor of Philosophy Master of Health Services — Physician Assistant Master of Science — Leadership Master of Science — Nurse Practitioner Admission is competitive and space is limited! nursing.ucdavis.edu
Bet t Y Irene moore sCHooL oF nursIn g Scan this code to learn more
The University of North Carolina at Chapel Hill
Distance Education from the Birthplace of Nurse-Midwifery and Family Nursing in America
Now Offers the Doctor of Nursing Practice Degree A tradition of excellence leads to careers of excellence. Come be a part of something great….
BSN to DNP Pathway n
Become a... • Nurse-Midwife • Family Nurse Practitioner • Women’s Health Care Nurse Practitioner
Health Care Systems
Complete your coursework and clinical work in your own community
Administration Informatics l Outcomes Management l l
n
Advanced Practice
Adult-Gerontology NP Family NP l Pediatric NP (primary care) l Psychiatric Mental Health NP l l
MSN to DNP Pathway Health Care Systems n Advanced Practice n
Distance education options: • Doctor of Nursing Practice (DNP) - new in • Post-Master’s Doctor of Nursing Practice (DNP) • Master of Science in Nursing (MSN) • Bridge Option for ADNs • Post-Master’s Certificates
www.frontier.edu/mn www.minoritynurse.com
Minority Nurse Magazine
@MinorityNurse
53
Academic Opportunities
Take the next step to advancing your
education and career.
School of Nursing ENROLL NOW
www.nursing.pitt.edu 1-888-747-0794 Ranked 7th among schools of nursing in U.S. News & World Reports 2011 America’s Best Graduate Schools.
Discover Johns Hopkins doctoral nursing education The Doctor of Philosophy (PhD) for research leaders. Advance the science of nursing and healthcare. The Doctor of Nursing Practice (DNP) for clinical leaders. Advance the practice of nursing and improve health outcomes. Choose your path at the Johns Hopkins University School of Nursing—a place where exceptional people discover possibilities that forever change their lives and the world.
www.nursing.jhu.edu/doctoral
5 2 5 N . Wo l fe S t.
54
Baltimore,MD 21205
Minority Nurse | FALL 2013
410.955.7548
Faculty Opportunities
NURSING FACULTY POSITIONS
T
he world needs more nurses. With that comes the need for experienced, dedicated nursing faculty to train them.
There is a true shortage of nursing educators—particularly minority nursing professors, who comprise a small percentage of nursing faculty overall. The American Association of Colleges of Nursing says the scarcity of professors may actually be stunting the growth of nursing programs. To counter this, nursing schools are improving the pay for nursing school faculty to increase their numbers, especially those who hold a doctorate. This section of Minority Nurse is dedicated to open faculty positions from nursing schools all over the country. Requirements vary, but all are sure to lead to exciting, rewarding careers in nursing education and research.
The University of Wisconsin – Eau Claire, College of Nursing and Health Sciences is seeking applicants for full-time tenure track faculty positions beginning in either January or August 2014. Positions are available in Eau Claire where excellent opportunities for research, leadership, clinical practice and professional development are available. The Department of Nursing offers CCNEaccredited BSN, MSN, and DNP programs, and a statewide collaborative BSN completion program. Expertise is preferred in the following areas: Advanced Practice with Adult, Gerontological, and/or Family Nurse Practitioner Certification and prescriptive authority, and Mental/Behavioral Health nursing. Applicants from other specialties are encouraged to apply. Qualifications include a master’s degree in nursing and doctorate or substantial progress toward a doctorate. Applicants must have RN licensure in the US and be eligible for RN licensure in Wisconsin, with WI RN license required by the start of the contract period. For a complete list of requirements and full position description, please refer to the following website: http://www.uwec.edu/Employment/NursingFacultyF-648.htm. For questions and information, contact: Mary Canales, PhD, RN Chair of Search and Screen Committee College of Nursing and Health Sciences University of Wisconsin – Eau Claire 105 Garfield Avenue Eau Claire, WI 54702-4004 Phone: 715-836-5737 Email: canalemk@uwec.edu Please submit letter of application, official transcripts, curriculum vita, and contact information for three references online at http://www.uwec.edu/Employment/NursingFacultyF-648.htm. Please submit PDF documents. Only applications submitted through UW Career site will be accepted. UWEC is an EOE/AA employer http://www.uwec.edu
Global Disaster Nursing MSN, DNP, & PhD Post-Master’s Certificate
Preparing nurse leaders for practice, policy, and scholarship Competency-based curriculum combines classroom learning, simulation exercises, and fieldwork for exceptional hands-on training opportunities and global perspective.
Coursework in: * Natural & Man-Made Disasters * Public Health Emergencies * Humanitarian Relief * Domestic & International Response * Crisis Management & Leadership
Now Accepting Applications Distance Learning Available
Speraw
For more information: CONgrad@utk.edu (865) 974-7553 http://nursing.utk.edu
Speraw
www.minoritynurse.com
Minority Nurse Magazine
@MinorityNurse
55
Faculty Opportunities
Faculty Diversity Success and Support at the University of Pennsylvania School of Nursing The importance of diversity to nursing science is incalculable. In an era of increasing health disparities and lack of access to quality healthcare, it is crucial to have diverse faculty conducting research, educating future nurse leaders, and shaping practice to improve health worldwide. Success Penn Nursing is one of the world’s premier research institutions in nursing, influencing practice, policy, and education. • Penn Nursing faculty consistently receive more research funding from the National Institutes of Health than any other private nursing school. • Many Master’s programs are ranked first in the country. • The Center for Health Equity Research, directed by Dr. Loretta Sweet Jemmott, and the Center for Global Women’s Health, directed by Dr. Lynn Sommers, are international leaders in evidence-based efforts to eradicate health inequities and disparities across the lifespan. Support Penn Nursing is committed to a diverse faculty and student body supported by: • A dedicated Office of Diversity and Cultural Affairs • A long history of outreach programs and curricular initiatives on cultural competence • Stellar faculty conducting community-based participatory research to improve the health status of marginalized and underserved populations • The Penn Nursing Faculty Mentorship Program which offers guidance and counsel for faculty at all stages of their careers • An Office of Nursing Research fully supporting faculty through every stage of the grant process. Penn Nursing faculty are internationally renowned researchers and policy leaders who create new knowledge that is reflected in cutting-edge teaching and refreshes evidence-based practice. For faculty opportunities at Penn Nursing, see www.nursing.upenn.edu/positions To learn more about Penn Nursing’s commitment to diversity, see www.nursing.upenn.edu/diversity The University of Pennsylvania is an equal opportunity employer. Minorities, males, veterans, and individuals with disabilities are encouraged to apply.
Index of Advertisers ADVERTISER . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . PAGE #
Johns Hopkins University . . . . . . . . . . . . . . . . . . . . . . . . 54
AARP. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23
University at Buffalo . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53
Carilion Clinic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45
University of California, Davis. . . . . . . . . . . . . . . . . . . . . 53
Hospital for Special Care . . . . . . . . . . . . . . . . . . . . . . . . 45
University of Nevada. . . . . . . . . . . . . . . . . . . . . . . . . . . . 54
Springer Publishing Company . . . . . . . . . . . . . . C2, 36, 43
University of North Carolina . . . . . . . . . . . . . . . . . . . . . . 53
UNCF. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C4
University of Pittsburgh . . . . . . . . . . . . . . . . . . . . . . . . . 54
University of Connecticut Health Center. . . . . . . . . . . . . 41
FACULTY OPPORTUNITIES . . . . . . . . . . . . . . . . . . . . . . . PAGE #
University of Florida Health Jacksonville . . . . . . . . . . . . 41
University of Pennsylvania . . . . . . . . . . . . . . . . . . . . . . . 56
ACADEMIC OPPORTUNITIES . . . . . . . . . . . . . . . . . . . . . PAGE #
University of Tennessee . . . . . . . . . . . . . . . . . . . . . . . . . 55
Frontier Nursing University. . . . . . . . . . . . . . . . . . . . . . . 53
University of Wisconsin. . . . . . . . . . . . . . . . . . . . . . . . . . 55
Oakland University . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
56
Minority Nurse | FALL 2013
THE MAGAZINE IS JUST THE BEGINNING...
Minoritynurse .coM YOUR GO-TO SOURCE FOR NURSING NEWS ON THE WEB. WHAT ELSE WILL YOU FIND ON MINORITYNURSE.COM? JOB POSTINGS ACADEMIC AND EMPLOYER PROFILES SCHOLARSHIPS
Hundreds of national listings, updated regularly. Explore schools of nursing, hospitals, and other health care facilities. Almost 15,000 scholarship opportunities, worth $52 million.
IT’S NEVER TOO EARLY TO INVEST IN A GOOD THING.
Introducing Better FuturesTM —a whole new kind of investment with a greater return than money. When you invest, it helps kids go to college. Because a mind is a terrible thing to waste but a wonderful thing to invest in.TM ©2013 UNCF
Invest in Better Futures at UNCF.ORG/INVEST