John A. Moran Eye Center | University of Utah Health
FOCUS

Remembering John A. Moran: A Lasting Legacy
RESEARCH
Crandall Center Glaucoma
Initiatives in Action





RESEARCH
Meet Moran’s Pioneering Neuroscientists

Official Publication of the John A. Moran Eye Center University of Utah Health, Salt Lake City, Utah 84132
John A. Moran Eye Center
65 Mario Capecchi Drive
Salt Lake City, Utah 84132
801-581-2352
CO-EDITORS
Anna Cekola, Communications Editor
Elizabeth Neff, Director, PR, Communications, Marketing
EXTERNAL RELATIONS TEAM/CONTRIBUTORS
Natalie Lam, Administrative Assistant
Tawnja S. Martin, Development Officer
Brett Prettyman, Corporations & Foundations Development Editor
Heidi G. Reid, Director of Development
Lynn Ward, Executive Director, External Relations
CONSULTANTS
Virginia Rainey, Writer/Editor
Catherine Reese Newton, Copy Editor
Madison Hanna, Writer
Julia Lyon, Writer
PHOTOGRAPHY
Michael Schoenfeld, Major Portrait
Photography
Matthew Hepworth
Kristan Jacobsen
Laura Kinser
Austin Miller
Scott Peterson
Anna Pocaro
COVER
Mike
GRAPHIC
Spatafore Design
PRINTING
Sun Print Solutions,
MORAN EYE CENTER FOCUS 2024

Support Program for Those with Low Vision


A special thanks to the many hard-working Moran Eye Center employees, management, health care workers, physicians, patients, and researchers who generously contributed their time and talent to make this publication possible.
Re search work highlighted in this publication was supported by an Unrestricted Research Grant from Research to Prevent Blindness, New York, New York, to the Department of Ophthalmology & Visual Sciences, University of Utah.
©️ 2024 John A. Moran Eye Center. All rights reserved. The Moran Eye Center does not assume responsibility for any representation therein, nor the quality or deliverability of the product. Reproductions of articles or photographs, in whole or in part, contained herein are prohibited without the publisher’s express written consent, unless otherwise stated.
Message from the Chair

The passing of John A. Moran has given me pause to reflect on the legacy he’s left behind.
John was a man of great intelligence with a work ethic that made the impossible possible—for his dreams and those of others. I was lucky to have him as a friend and even luckier that he shared my vision for an eye center that really could change the world. It is a privilege to be surrounded by people who are always looking forward.
We dedicate this edition of FOCUS to John, and we are proud to share developments that are getting us closer to his goal of curing blindness.
The Alan S. Crandall Center for Glaucoma Innovation, led by Iqbal Ike K. Ahmed, MD, FRCSC, is an excellent example of thinking big. This effort is ramping up with new hires as we build a dream team to attack this disease on all fronts. We recently welcomed Zachary W. Davis, PhD, as a key part of an effort to develop new disease models. We’ve also got new projects on deck, including a collaboration with Frans Vinberg, PhD, that would allow him to study glaucoma using functioning postmortem retinal cells.
Additionally, Crandall Center Associate Director David Krizaj, PhD, is in the final stretch of experiments for a new glaucoma therapy.
In this edition, don’t miss getting to know Kristine Marcroft, the first Moran Eye Center patient to test our new gene therapy for age-related macular degeneration (AMD). She is an amazing person and an example of why Gregory S. Hageman, PhD, and I embarked on a journey to cure AMD nearly 15 years ago.

Randall J Olson, MD, and John A. Moran share the stage at a gala in 2006 celebrating the opening of the present 210,000-square-foot eye center building.
In cutting-edge clinical research, Moran Vice Chair for Clinical and Basic Science Research Paul S. Bernstein, MD, PhD, is collaborating to build a surgical robot that will assist in retinal surgeries. This is the trickiest part of the eye for a surgeon to reach, and robotic devices hold great promise for optimizing outcomes for our patients.
Of course, John’s rich legacy can be seen each day in the quality of patient care and education programs (both ranked among the nation’s Top 10) and in the dedication of our outreach team to increasing access to care.
The future is coming, and we’re helping build it.
Sincerely,

Randall J Olson, MD
Distinguished Professor and Chair, Department of Ophthalmology and Visual Sciences, University of Utah
The Cumming Presidential Endowed Chair CEO, John A. Moran Eye Center Director, University of Utah Vision Institute
2023-2024
Moran Advisory Council
TONI BLOOMBERG
La Jolla, California
WILLIAM “BILL” CHILD
Salt Lake City, Utah
THOMAS “TIM” DEE III
Salt Lake City, Utah
We are saddened to acknowledge the 2023 passing of council member John E. Warnock, PhD. He was a dear friend of the Moran Eye Center, and he is missed.
CHRISTENA HUNTSMAN DURHAM
Salt Lake City, Utah
SPENCER F. ECCLES
Salt Lake City, Utah
CHRISTINE A. FAIRCLOUGH
Salt Lake City, Utah
WAYNE A. IMBRESCIA
John A. Moran Eye Center
CLAUDIA S. LUTTRELL
Salt Lake City, Utah
RANDALL J OLSON, MD
John A. Moran Eye Center
LYNN WARD
John A. Moran Eye Center
NORM A. ZABRISKIE, MD
John A. Moran Eye Center

A Generous Philanthropist — a Dream to Restore Vision IN MEMORIAM: John A. Moran
John A. Moran often shared a simple mantra: “You won’t be remembered for how much money you made; you will be remembered for what you did with it.”
Upon his passing on September 23, 2023, at the age of 91, Moran was recognized not only as a business leader whose success exemplified the American Dream, but also as a man who heeded his own words.
Moran dedicated much of the wealth he earned during his finance career to worthy nonprofit organizations nationwide. At the University of Utah, his beloved alma mater, he left a beacon of hope bearing his name: the John A. Moran Eye Center.
Moran wanted the center to provide compassionate care and make breakthroughs in research to improve the treatment of blinding eye diseases.
“It is my hope that the research and the work that’s being done here will prevent diseases of the eye that cause blindness, and God willing, restore sight to people who have lost their vision,” said Moran in tearful remarks at a news conference opening the current Moran Eye Center building.
Today, the center he championed is ranked among the 10 best in the nation for its care, education, and research and is known for its outreach to increase access to eye care in Utah and around the world.
“John’s death leaves a huge hole in our hearts,” says Moran Eye Center CEO Randall J Olson, MD.
“He was a true friend with a desire to help others, and his dedication to our vision to provide hope, understanding, and treatment deeply motivated me and everyone at Moran to strive for excellence. We share our condolences with the Moran family, we honor John’s extraordinary life, and we are thankful to be a part of his legacy.”
Moran was born in Los Angeles on March 22, 1932, and his family moved to Salt Lake City in 1941. His father, who did not attend college, stressed the importance of an education. After high school, Moran enrolled at the University of Utah and worked as a city flag boy for the Salt Lake City road crew, rewinding signal wire at Hill Air Force Base, and as a waiter to pay his tuition.
He was a member of the Sigma Nu fraternity at the U. Moran’s father passed away from cancer shortly before his son earned a banking and finance degree in 1954.
After graduation, Moran spent three years in the U.S. Navy and served as an intelligence officer on the staff of the Commander in Chief of the U.S. Navy’s Pacific fleet from 1955 to 1958.
He then began his finance career at investment banking firm Blyth & Company Inc.

In 1967, Moran joined Dyson-Kissner Corp., a private holding company with a portfolio of companies, including businesses engaged in manufacturing, retailing, distribution, financial services, and real estate development. When he became a partner, the company was renamed Dyson-Kissner-Moran Corp. Moran served as its president and CEO before retiring in 1998.
A major contributor and fund-raiser for the Republican Party, Moran served as chairman of the Republican National Finance Committee from 1993 to 1995. He then became finance chairman of the Dole for President Campaign and co-chaired the Republican Leadership Council of Washington, D.C. He also co-chaired John McCain’s National Finance Committee.
At the University of Utah, Moran held an honorary Doctorate of Law and served on the school’s National Advisory Council, where he met Olson.
W hile Moran had no vision issue himself or in his family, he was deeply moved by his mother’s teachings and Olson’s dedication to restoring sight.
Moran wrote: “When Dr. Olson told me about his dream to carry out research that might someday restore vision to the blind, it brought to my mind stories from the Bible that my mother had read to me as a child.
“As a little boy, I was particularly touched by the story of the blind beggar, the power of faith, and the miraculous restoration of his sight. One of the reasons the Moran Eye Center exists is because my mother planted within me a belief in miracles.
“The story of the blind man transcends one man and his dream and hope for vision. It reminds us that, as individuals, we must never give up hope that we can accomplish things that were previously considered impossible. That irresistible sense of hope that exists in each of us can be felt in this new building, in the hearts of those who will be caring for patients, and in those who are working to advance the science of human sight.”
A gift from Moran established the first center building. He also contributed to opening the current Moran Eye Center building in 2006. Moran was instrumental in designing the five-story center, which has a wall of glass windows that allow patients to see



amazing views of the Salt Lake Valley after receiving sight-restoring surgeries and treatment.
Moran’s legacy at the University of Utah extends beyond vision. He was a passionate supporter of many areas on campus, including the L.S. Skaggs Jr. Pharmacy Research Building, Department of Biomedical Engineering, and Huntsman Cancer Institute.
Throughout his lifetime, Moran served as director, trustee, and member at numerous organizations, companies, and institutions. He was a trustee of New York’s Metropolitan Museum of Art, where he financed the John A. and Carole O. Moran Gallery for later Roman art and sarcophagi, and of the George and Barbara Bush Endowment for Innovation Cancer Research at the University of Texas MD Anderson Cancer Center. Moran was a director of the United Nations Association and the Foreign Policy Association.
In 2008, the Woodrow Wilson International Center selected Moran for its Outstanding Corporate Citizenship Award. In 2012, Moran received the prestigious Horatio Alger Award, which celebrates values including “personal initiative and perseverance, leadership and commitment to excellence, belief
in the free-enterprise system and the importance of higher education, community service, and the vision and determination to achieve a better future.”
In an interview accepting the Horatio Alger award, Moran humbly shared his philosophy on success: “It’s not the money,” he said. “Success is being satisfied with what you’ve accomplished, comfortable with yourself in terms of what you’re doing. That’s all I am. No better, no worse than anybody else.”
Moran is survived by his wife, Carole; daughters, Kellie, Marisa, and Elizabeth; five grandchildren; and three great-grandchildren.

“I
don’t want my children, grandchildren, or anyone else to have to deal with this.”
— Kristine Marcroft, the first Utah patient to test a new gene therapy for AMD developed at the Moran Eye Center.

Coming Full Circle
Moran age-related macular degeneration patient becomes the first to test its new gene therapy in Utah.
Kristine Marcroft has so many good memories of times with her dad.
She recalls how they wrangled sheep on their ranch in central Utah, found the best fishing spots, and toured scenic back roads. Her dad, Kristine says, was a voracious reader who taught her to pursue knowledge, to be her own person, and most of all to enjoy life.
It was difficult to see him lose his eyesight in his golden years. Marcroft watched as her father and uncle, a physician, were blinded by the same disease: age-related macular degeneration (AMD).
Then, at the age of 60, Marcroft began her own struggle with AMD as it began to take away her central vision. She knew it was time to retire from a longtime career working at the Salt Lake County Jail when she couldn’t see documents clearly, even using a magnifying glass.
W hen Marcroft heard patients were needed to test a new gene therapy for AMD developed at the Moran Eye Center’s Sharon Eccles Steele Center for Translational Medicine (SCTM), she thought about the risks. But she didn’t hesitate to volunteer.
“I don’t want my children, grandchildren, or anyone else to have to deal with this,” says Marcroft, now 70. “It was a no-brainer, and I am going blind in that eye anyway.”
In June 2023, Marcroft joined patients in Texas and Boston participating in a study to evaluate the safety of the new therapy. She made history as the first patient to receive the therapy at Moran.
Marcroft comes every few weeks for testing. She undergoes visual testing with an eye chart, extensive imaging of her eyes, and a dilated eye exam to inspect her retina.
Led by Gregory S. Hageman, PhD, SCTM researchers were the first to fully explain the genetics of a disease that can feel inescapable for some families. Genetic mutations on chromosomes 1 and 10 account for 90 percent of a person’s risk of developing AMD. Marcroft has chromosome 1 disease, the most common form. The SCTM therapy was injected into her eye.
A second testing phase will begin in 2024 to evaluate how effective the therapy is at preserving vision. The hope: one day, a single injection can be given to people at high risk for AMD or in the early stages of the disease to stop it from progressing or maybe even prevent it.
The SCTM isn’t stopping there. Its researchers have multiple therapies in their pipeline— including one for people with chromosome-10-driven AMD.
How the Therapy Works at the Cellular Level
A surgeon injects a protective gene into cells in the eye to provide protection against AMD.





Research Boost
Scientists awarded $3.8 million for leading-edge age-related macular degeneration work.
Backed by $3.8 million in new federal funding, internationally renowned clinicianscientists Monika Fleckenstein, MD, and Steffen Schmitz-Valckenberg, MD, are forging new ground in age-related macular degeneration (AMD) research.
The two National Eye Institute (NEI) grants will span five years.
The first grant supports a study of patients with so-called “dry” AMD who experience abnormal blood vessel growth in the eye without the ruptures and leakage experienced by patients with “wet” AMD. Fleckenstein and Schmitz-Valckenberg want to know if this type of vessel growth is the body’s attempt to preserve vision by getting more nutrition to degenerating cells in the back of the eye. A second grant funds research seeking ways to use imaging to more accurately detect and monitor the onset of dry late-stage AMD, which patients can have without experiencing symptoms. In theory, therapies administered in this stage of the disease could save a large portion of patients from progressive vision loss.
Fleckenstein and her team will examine patients in clinical studies. SchmitzValckenberg, who directs the Utah Retinal Reading Center at Moran, will analyze highresolution retinal imaging and functional tests.
Schmitz-Valckenberg and Fleckenstein are key members of Moran’s Sharon Eccles Steele Center for Translational Medicine. The NEI grants are “The Impact of Non-Exudative Type 1 Macular Neovascularization on AMD Progression” and “Progression of Early Atrophic Lesions in AMD.”


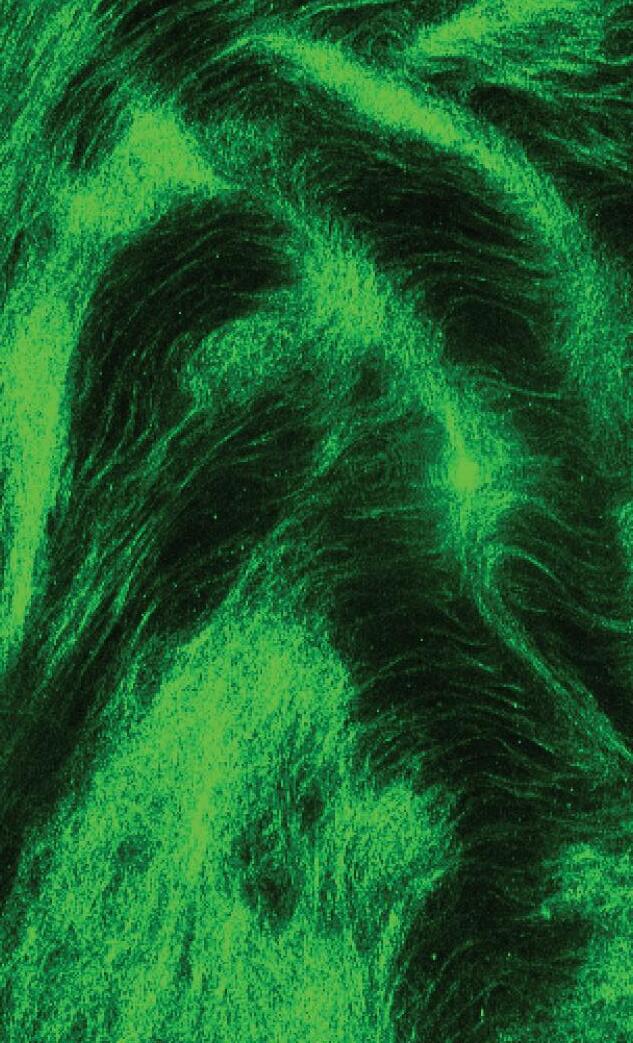
An image of human vitreous, shown after dissection and incubation in saline, from the laboratory of Eileen Hwang, MD, PhD.
New Federal Funding
Additional Moran researchers received significant National Eye Institute funding in 2023 that will provide a better understanding of blinding eye diseases and conditions.
Paul S. Bernstein, MD, PhD
$1,575,896 through 2027
“Elucidating the Role of Very-long-chain Polyunsaturated Fatty Acids in Retinal Health and Disease”
Bernstein will examine the role of fatty acids found in the eye’s retina. Insights could guide the development of new therapies that use a synthetic version of fatty acids to treat age-related macular degeneration.
Eileen S. Hwang, MD, PhD
$951,220 through 2028
“Cellular, Molecular and Physical Mechanisms of Vitreous Structural Heterogeneity Underlying Posterior Vitreous Detachment”
Hwang will study age-related changes in the vitreous, or gel that fills the eye, which can cause blinding retinal detachments. Understanding this process could help identify a way to prevent retinal detachments in high-risk patients.
David Krizaj, PhD
$1,925,000 through 2028
“Molecular Mechanisms of Mechanotransduction in the Aqueous Outflow Pathway”
Krizaj will study pressure-sensing cells in the eyes. Insights could lead to new treatments for the high intraocular pressures and optic nerve death associated with glaucoma.
Frans Vinberg, PhD
$1,924,792 through 2028
“Functional Plasticity in Retinal Degenerative Disease”
Vinberg will study how neurons in the retina change during aging or disease. A better understanding of this can lead to the development of new therapies with better outcomes.
Jun Yang, PhD
$1,876,576 through 2027
“Disease Mechanism of Usher Syndrome 2”
Yang will study Usher syndrome, a rare disease that combines blindness from retinitis pigmentosa with hearing loss. The findings will provide insights into the disease in hopes of developing a cure.
The Future of Eye Surgery
A Moran lab and campus robotics colleagues are developing a new device with the potential to transform eye surgery.
Spaces in the back of the eye below the retina measure just fractions of a millimeter—a tight spot for talented surgeons with steady hands to access even under the best of circumstances.
If a sedated patient snores or moves slightly, surgery can become even more challenging.
A new robotic eye surgery device developed by Moran’s Paul S. Bernstein, MD, PhD, and the University of Utah Magnetic & Medical Robotics Laboratory aims to transform retinal surgery by increasing precision and safety.
“Robotic surgery is the future, allowing us to go past the limits of what humans can do,” says Bernstein, a retinal specialist and scientist. “This device, in particular, is important as many new therapies, including gene therapies for retinal diseases like age-related macular degeneration, must be delivered by subretinal injections into this minute space in the eye.”
During eye surgery, patients are typically under some level of sedation but not general anesthesia. They may snore or make sudden movements, which can increase the risk of injury to the patient’s retina, a delicate layer of light-sensing tissue essential for vision.
The noninvasive device consists of a helmet-like structure worn by the patient. A small robot is attached to the structure, which moves with the patient. A surgeon controls the robot by using a joystick device that filters out any hand tremors.
Experiments have shown the device to be highly successful at preventing complications due to patient movement, says Ja ke Abbott, PhD, director of the robotics lab.
“We think of our robots as tools for surgeons,” he says.
Researchers have been testing the device on animal eyeballs resting on swim goggles worn by human volunteers. This allows them to evaluate the precision of the device under realistic conditions.
“This patient-motion aspect has been neglected in a lot of other research,” says Nick Posselli, a graduate student in mechanical engineering who has worked with Abbott to develop the device over the past seven years.
Since only a small number of surgeons are qualified to perform subretinal injections, the device could increase the number of surgeons who can perform them.
“Retinal surgery is a technically difficult surgery and takes a while to master, so for people in the earlier stages of their career, having robotic assistance can ma ke it safer and more effective,” Bernstein says.
Bernstein praised the cross-disciplinary collaboration with University of Utah engineers. The group anticipates publishing new results in the near future.
“The next step,” he says, “is to refine the system that’s working well on these models so we can take it to the next stage, which is human use.”


Glaucoma Innovation in Action
The Alan S. Crandall Center for Glaucoma Innovation, led by
Iqbal Ike K. Ahmed, MD, FRCSC, was created to lead the field in four high-impact initiatives. Catch up on the latest below.
Surgical & Medical Therapeutics: Precision Medicine
Glaucoma provides a perfect example of why tailoring therapies and treatments to individual needs is widely viewed as the future of medicine.
“Precision medicine can make all the difference in glaucoma patients because the disease is so different for each person in terms of how fast it progresses and fluctuations in intraocular pressure,” explains Ahmed, an internationally renowned surgeon who consults on device development for more than 50 companies.
In September 2023, Ahmed began the first in-human clinical study of the Calibreye System developed by Myra Vision. After placing it in the eye, physicians can adjust
this next-generation drainage device to decrease or increase drainage without additional surgery as a patient’s treatment needs change.
Since glaucoma progresses differently for each person, testing throughout one patient’s lifetime generates thousands of data points about intraocular pressure, corneal thickness, and rates of optic nerve deterioration. Researcher and glaucoma specialist Brian C. Stagg, MD, has developed an analytic system to help physicians sort through the data to decide on the best treatments and timing for follow-up testing.
“My goal is to allow glaucoma doctors to assess the data more quickly and adapt it to their patients’ needs,” says Stagg. “It is personalized medicine at the point of care.”
Translational Research: Genetics Study
Thirty years after others told him there was nothing to be done for a leading cause of blindness among people 55 and older, initiative Director Gregory S. Hageman, PhD, and his team have changed our understanding of age-related macular degeneration, clarified its genetics, and developed a new therapy for its most prevalent form.
Now, Hageman is launching a large-scale study into glaucoma. A new partnership with a major pharmaceutical company will study thousands of proteins associated with the disease.
“Glaucoma is a complex disease that emerges as a consequence of the aging process, systemic factors, and genetic makeup, although the data on a major role for genetics is extremely weak,” says Hageman. “Our studies are designed to develop a rich understanding of glaucoma to discover gene-directed pathways to identify and develop new therapies.”
Neuroprotection-Based Therapies: Expanding Team
Crandall Center Associate Director David Krizaj, PhD, and research collaborators from the University of Utah Department of Chemistry and College of Pharmacy are in the final stretch of experiments for a powerful new therapy to lower pressure associated with glaucoma and prevent optic nerve cells from dying—a function known as neuroprotection. Backed by a venture capital funder, he is conducting clinical studies as the last step before applying to the FDA to test in humans.
The initiative grew in January as neuroscience researcher Zachary Davis, PhD, joined the Moran Eye Center. Working with Alessandra Angelucci, MD, PhD, his lab is assisting in Crandall Center efforts to develop glaucoma disease models and techniques for studying the impact of glaucoma on visual perception in the brain.
Another Moran collaborator, Frans Vinberg, PhD, plans to conduct testing on functioning human photoreceptor cells to study signaling when the cells are exposed to pressure.
Global Care: Physician Training in Africa
Glaucoma is severe in Africa, where an estimated 4% of the population over the age of 40 has the disease.
Moran’s Global Outreach Division has begun training three physicians in Mwanza, Tanzania, to detect glaucoma earlier and employ treatment options, including surgery, to preserve vision.
Initiative Director Craig J. Chaya, MD, who also serves as senior medical director of the Global Outreach Division, traveled with Moran Global Fellow Shawn Gulati, MD, MPH, to Tanzania in 2023 to establish a glaucoma fellowship training program. There, they are training Drs. Nuru Mwambola, James Shimba, and Frank Sandi. The division also has hosted medical professionals from Tanzania at Moran and started remote surgical mentorship training sessions.
“In low-resource countries, the focus has been on cataracts, and we have had great success in expanding access to that type of care,” says Chaya. “Now many people are looking to treat glaucoma because the disease is so prevalent.”




Microscopy and color labeling of retinal ganglion cells (RGCs), the cells that form the optic nerve and are damaged by glaucoma. Courtesy of Krizaj Laboratory members Monika Lakk, PhD, and Chris Rudzitis.
MEET MORAN’S RENOWNED BRAIN SCIENTISTS Q&A
Surprisingly little is known about the brain and its disorders. Moran Eye Center researchers Alessandra Angelucci, MD, PhD, and Behrad Noudoost, MD, PhD, are studying visual neurons to change that. Here they discuss their pioneering vision research, funded in part by the National Institutes of Health Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.
What are the main questions your research is trying to answer?
Alessandra Angelucci, MD, PhD

Angelucci: Specialized nerve cells called neurons carry messages in the brain. Neurons work together in teams, creating circuits that help us process certain kinds of information; for example, one circuit allows us to recognize individual faces. My lab studies these circuits, especially in the visual cortex region of the brain responsible for producing vision.
The visual cortex works a bit like building blocks. It builds visual information, bit by bit, starting in the lower centers with the recognition of simple features of objects, such as their contour, color, and shape, and ending in higher centers with the recognition of complex object features and whole objects such as faces. Our goal is to learn not only how individual areas of the brain communicate aspects of vision, such as shape and color, but also how it merges that information into a single scene. We believe this information merge helps us literally distinguish the forest from the trees.
Noudoost: My lab focuses on understanding selective attention and working memory. How does the brain focus attention on one particular aspect of a visual scene?
We record and study communication between individual neurons to better understand communication between different areas of the brain responsible for processing aspects of a visual scene, such as color, motion, and shape. We also work to identify what can affect communication between neurons. For example, we have shown dopamine levels impact the brain’s attentional capacity or how much information it can process at once.
Q A A Q A &
What is most innovative about your research?
Angelucci: I always want to find the most useful technology to answer the questions I want to ask. If that technology doesn’t exist in my lab, we develop it. Over the past 10 years, we’ve developed a new technology that allows us to fill neurons with a fluorescent protein and reveal the shape and roadmap of a brain circuit. This is enabling us to build a diagram of the brain by specific cell types.
Our focus on what scientists call feedback — the exchange of information from higher to lower centers in the brain— also makes our lab unique.
Noudoost: Since the brain has about 10 billion neurons and more than trillions of connections, identifying these communicating neurons can feel a little like trying to find a needle in a haystack. Fortunately, recent technological developments have given us the ability to identify which neurons are active and to study what and when they are communicating.
Our methods allow us to trace connectivity between neurons with a remarkable level of precision and to characterize their response and function to different stimuli. This allows our lab to understand the sequence of events that happen in the brain when someone pays attention to something they see.
How do you hope your research will help patients?
Angelucci: If we know how these circuits process vision, we’ll also find clues about what may be happening when someone can’t see.
In collaboration with Dr. Steve Blair in Electrical and Computer Engineering, we are building on the work of University of Utah Professor Richard A. Normann, PhD, to develop the next generation of a visual prosthesis for people who have gone blind. The prosthesis stimulates neurons using light to create a form of artificial vision.
Noudoost: The brain is constantly selecting which aspect of information to focus on, but in disorders such as ADHD, autism, Parkinson’s disease, and schizophrenia, it is unable to prioritize what is important. Knowing what usually occurs, we can shed light on what may not be happening for these patients. We hope our work is ultimately useful in finding future treatments for disorders related to attention impairment. & &

Behrad Noudoost, MD, PhD

The Utah Electrode Array, much smaller than a penny, is a tiny device implanted in the brain.

Artificial Vision Advances
The Moran | Cortivis Prosthesis, which uses the Utah Electrode Array, has now been tested on three individuals with blindness.
Scientists from Spain’s Miguel Hernandez University and the Moran Eye Center have now used an experimental prosthesis hardwired into the visual regions of the brain to safely provide a form of artificial vision to three individuals with blindness.
Spanish neuroscientist Eduardo Fernández, MD, PhD, and Utah’s Richard A. Normann, PhD, in 2021 published results of experiments with the prosthesis conducted with a 60-yearold woman. The prosthesis, which uses the Utah Electrode Array (UEA) developed by Normann to stimulate neurons in the brain’s visual cortex, enabled the woman to identify lines, shapes, and simple letters evoked by different patterns of stimulation.
Speaking at a symposium held at the Moran Eye Center in September 2023, Fernández announced he had achieved similar results in two additional study participants.
His latest experiments have gone one step further to test if the prosthesis can provide a form of vision useful for the blind. In one video shown to the audience, a man wears the prosthesis while independently navigating a sidewalk and around people. In another, he avoids objects while walking on a treadmill in front of a virtual reality video screen.
“This provides a ‘proof of concept,’ and the stage is now set for more work in this area and for developing engineering technologies to transform this prototype into a clinical system,” says Normann, Distinguished Emeritus Professor of Bioengineering and Ophthalmology and Visual Sciences.
An adjunct professor at the Moran Eye Center, Fernández says he is preparing to recruit a fourth patient.
“We’re still only at the beginning of possibilities this prosthesis might provide,” he says.
How Does It Work?
Just 4 mm by 4 mm, one UEA is implanted into the brain of a study participant, who then works with researchers for six months to test the prosthesis before it is removed.
Participants wear eyeglasses equipped with a miniature video camera; specialized software encodes the visual data collected by the camera and sends it to the UEA. The array then stimulates neurons to produce phosphenes, perceived as white points of light, to create an image.
Normann and colleague Gregory Clark, PhD, first used a variant of the UEA in amputees to evaluate its safety and efficacy. The UEA allowed the amputees to control artificial limbs simply with their desire to move a finger or hand. The experiments in Spain were the first to implant the UEA into the visual cortex of blind human volunteers.
The research has used one UEA, but in the future, Fernández would like to implant several UEAs into the visual cortex to produce a more complicated form of artificial vision. Earlier published research conducted by Normann indicates between seven and 10 arrays in the visual cortex, working together, could produce more detailed images.



Frody Volgger is back to riding his motorcycle after requiring emergency medical treatment for an eye stroke.


Frody Volgger, left, talks with the ophthalmologists who treated his eye stroke, Theresa Long, MD, center, and Ayesha Patil, MD, during a follow-up visit at Moran.
‘Time Is Vision’
Quick action by Moran’s ophthalmic hospitalist helps prevent blindness in eye stroke patient.
On a summer afternoon in 2023, as Frody Volgger neared the end of a motorcycle ride on Utah’s scenic Monte Cristo Loop, he suddenly lost vision in his right eye. He gestured to his riding partner and pulled to the side of the road.
“I thought I had something in my eye,” Volgger, 72, says. “I took my glasses and helmet off, closed my good eye, and saw only darkness and a few stars. There was no warning, no pain. I just couldn’t see a thing.”
He considered going home to change clothes and get his car before heading to the emergency room at University of Utah Hospital, but instead, he rode straight there. That decision made a world of difference.
Based on Volgger’s complaint of sudden vision loss in one eye, the emergency department (ED) triage nurse and neurology team called a possible “brain attack,” which alerted the hospital’s stroke team as well as Moran’s ophthalmic hospitalist, Theresa Long, MD, and her consulting resident that day, Ayesha Patil, MD.
“We were nearby and able to drop everything and head right to the ED,” says Long. “Neurologists say ‘time is brain’ regarding stroke and the promptness needed to respond. We say ‘time is vision’ when it comes to sudden vision loss and the need to respond.”
Long and Patil met Volgger—motorcycle gear and all—as he received a CT scan. They walked him back to the ED, dilated his eyes, quickly performed a range of tests, and evaluated radiographic images that indicated Volgger had experienced a retinal artery occlusion (RAO), also known as an eye stroke.
Once Long diagnosed RAO, the team promptly followed the protocol to prepare and inject Volgger with a “clot-busting” medication.
“The arteries that lead to the brain are like an interstate highway,” says Long. “Fortunately for Frody, the blockage in his artery took the first exit ‘off the interstate’ and headed to his eye rather than further up to his brain. The sudden vision loss was a warning sign, a possible precursor to a stroke. Because everyone acted so quickly and administered appropriate medicine within an hour of arrival, we saved about 30% of normal vision in that eye. This is a big deal—these patients are usually permanently blind in the affected eye. We also admitted him to the hospital for monitoring and treatment to prevent another stroke.”
Volgger says he’s “incredibly grateful and amazed” at how everybody responded. “I’m back on my motorcycle—feeling good and very lucky.”
What You Need to Know About Retinal Artery Occlusion
Retinal artery occlusion (RAO) is a type of stroke marked by a loss of blood supply in the retina, the light-sensitive layers of nerve tissue at the back of the eye. Since the eye is an extension of the brain, loss of blood supply and oxygen for a short period leads to severe and irreversible complications and permanent vision loss.
Doctors consider RAO a medical emergency and a possible warning sign for an impending brain stroke.
S ymptoms
Sudden onset of painless, dramatic vision loss and loss of side vision in one eye could indicate RAO.
Take Action
Anyone who experiences sudden vision loss should call 911 and get to an emergency room as soon as possible.
Risk Factors
RAO risk factors include obesity, high blood pressure, smoking, high cholesterol, diabetes, and atrial fibrillation.
Treatment
A “clot-busting” treatment is most effective when given within 3 hours, but no longer than 4 1/2 hours after the onset of symptoms.
What People with Low Vision Want You to Know
Lisa Ord, LCSW, PhD, director of Moran’s Patient Support Program, shares 10 things to consider when approaching someone who looks like they may need assistance:
Introduce yourself.
Ask questions and ask before assisting.
Ask before offering an arm or elbow.
If you’re unsure about the person’s needs, ask for clarification.
Be aware of making assumptions. For example, a person with visual impairment standing on a corner might appear to be lost when, in fact, they are listening to the traffic patterns.
Be yourself, and don’t worry about using terms like “look” and “see.”
Always ask before approaching working guide dogs.
Accept “no” as an answer if someone declines your help.
If they want your assistance, be as descriptive as possible when orienting someone to a space, food selections, or other options.
Remember that people are more than their low vision.
‘In My Corner’
Moran’s Patient Support Program helps AMD patients get back to doing what they love.
Four years ago, Barbara LaCoste began seeing blurry spots in her central line of vision. During an eye exam at the Moran Eye Center, the 78-year-old received a diagnosis that was all too familiar to her and her family: age-related macular degeneration (AMD).
The disease is a leading cause of blindness for people age 55 and older, and LaCoste says she probably inherited it from her mother, who was completely blind when she passed away in 1996.
Today, LaCoste is legally blind and can no longer drive. But she often thinks of her mother and is grateful for modern treatment options allowing her to cope with the sight-robbing disease.
“I wish my mother could have taken advantage of the treatment options that have helped me today,” says LaCoste, who at one time received regular injections to treat blood vessel leaks caused by her form of the disease.
Another part of LaCoste’s care plan is Moran’s Patient Support Program, which assists people with low vision. The term “low vision” refers to vision loss that can’t be corrected by surgical or medical treatments or eyeglasses. It may result in blind spots, blurry sight, loss of central or peripheral vision, or trouble with depth perception.
LaCoste has attended informational vision loss seminars and support groups through the program, directed by Lisa Ord, PhD, LCSW. Last year, the program gifted her a pair of magnifiers and another reading device with a screen. LaCoste says the tools have helped her continue to live independently with her husband, who has Alzheimer’s disease.
“Dr. Ord is such a sweet person, and I’m so glad she’s in my corner,” says LaCoste. “She has not only provided me with resources and emotional support, but the 2x/4x/10x magnifiers help me with everyday tasks like reading our mail or prescription bottles.”
LaCoste was also a patient of Robert M. Christiansen, MD, FACS, who runs a clinic that gives patients with low vision strategies to improve functional ability, such as customized lighting inside the home.
“I’m so grateful for Moran because I have been able to continue doing the things I enjoyed before vision loss, like cooking and baking; it’s the little things in life that are the most precious,” says LaCoste. “Sit down and do nothing? That’s not for me; I choose life.”
About the Patient Support Program

The program offers professionally moderated support groups and vision rehabilitation services to help patients, families, and caregivers find ways to understand, accept, and move past the limitations of vision loss. Scan the QR code at left or visit moraneye.link/patient-support for more information or to make an appointment.
“It’s important to treat people with low vision as you would treat anyone else. Keep in mind that low vision does not mean low ability, and that will go a long way.”
— Lisa Ord, LCSW, PhD, director of Moran’s Patient Support Program

Barbara LaCoste reads with a magnifier device supplied by the Patient Support Program.
Nishika Reddy, MD, right, and a patient discuss a new treatment option for extreme dry eye available at the Moran Eye Center.

What Causes Dry Eye
When a person blinks, a protective layer called the tear film spreads across the surface of the eyes to provide protection and nourishment.
When one or more of the three layers of the tear film are out of balance, it can trigger the cycle of disruptive dry eye.
New Hope for Extreme Dry Eye
Three new treatments are among the options available for this complex condition that affects millions.
Dry eye disease affects almost 20 million people in the U.S. yet remains notoriously misdiagnosed and undertreated.
That is, in part, because dry eye is a complex condition with a range of potential causes and symptoms, explains Moran ophthalmologist Nishika Reddy, MD.
“It can manifest if your tear gland doesn’t make enough tears. It can also happen if tears don’t contain enough oil, which causes them to evaporate too quickly. For some people, the condition causes mild irritation and redness. For others, it can bring on blurry vision and eye pain that can disrupt everyday life,” Reddy says. “Fortunately, we have access to some highly effective new treatments for patients experiencing that kind of disruption.”
Reddy, a corneal specialist, uses her expertise to diagnose patients, consider underlying causes, and guide them through their options.
“Often what’s successful is a variety of ongoing treatments,” she says. “Unfortunately, right now, most health insurers do not cover the newest treatments, but for some patients, it’s worth the out-of-pocket expense.”
Latest FDA-Approved Options for Dry Eye
T EARCARE
On the extreme side of dry eye, Reddy treats patients with meibomian gland dysfunction (MGD), a condition caused by the dysfunction of a few dozen tiny eyelid glands that help make the oil layer of tears. This layer, one of three that keep the eye surface from drying out too quickly, is critical. When the meibomian glands get clogged, less oil reaches the eye surface, and tears dry out too quickly.
“Not all patients with dry eye have MGD, so they need a good exam to make sure that’s the condition. Often, it’s patients with significant symptoms who have not had good results with over-the-counter treatments such as artificial tears, warm compresses, and eyelid scrubs,” says Reddy.
“In these cases, I may recommend TearCare—a painless procedure where we place a noninvasive, comfortable device on both eyelids for 15 minutes to gently warm the meibomian glands. While the device is doing its work, the patient can just relax. Then, while the glands are nice and warm, I come in and express, or ‘clean out,’ the glands.”
Patients need to repeat the procedure in three months, and Reddy cautions the treatment does not negate the need for drops or other medications.
M IEB O
Excessive tear evaporation can trigger a chronic cycle of inflammation and friction, damaging the ocular surface and disrupting the intricate balance among the many layers of the eye’s surface. For some people, that includes a chronic stinging sensation, a feeling that something foreign is in the eye, or other irritations.
“Studies have shown that Miebo, a prescription eye drop that directly targets excessive tear evaporation instead of tear formation, is highly effective,” Reddy says. “The solution, called perfluorohexyloctane, is designed to mimic a key natural function where meibomian glands produce a lipidrich secretion that forms the tear film lipid layer and helps to maintain a healthy ocular surface.”
T YRVAYA
Tyrvaya (Varenicline solution) offers another option for patients whose eyes don’t make enough tears. It’s a nasal spray that kick-starts your body to produce its own natural tears.
“Tyrvaya works by activating glands and cells connected to a nerve inside your nose that is part of the pathway for controlling tear film production,” explains Reddy. “In some cases, it can help relieve symptoms for people who haven’t had success with other therapies.”
Caring for Our Communit y
A look back at Global Outreach Division initiatives last year to provide free or low-cost eye exams, surgeries, and eyeglasses to those in need in Utah and the Navajo Nation. Moran Eye Center outreach work is funded solely by donors.

50 COMMUNITY CLINICS Child Eye Exams Adult Eye Exams New Eyeglasses Surgeries 655 1,411 1,053 367 LOCAL
July 2022—June 2023
moraneye.link/local-outreach-video.




Outreach volunteers provided 110 eye exams and 110 pairs of eyeglasses at Salt Lake City’s 2023 Project Homeless Connect.




Operation Sight Program
A single father of two, Joey was working as a brickmason when he began losing his eyesight to cataracts.
As his vision began to fail, he quickly realized he was increasingly in dangerous situations at work and while driving but had no way to afford surgery.
“It’s tough being a single dad,” Joey said. “You don’t want the kids to worry. But I don’t have health insurance. I can’t afford it.”
Joey was relieved to hear about Moran’s Operation Sight program. Funded solely by generous donors, Operation Sight provides sight-restoring cataract surgery to people who could not otherwise afford it.
Including Joey and other patients from a Saturday surgery day held in June 2023, the program restored vision to more than 100 people in fiscal year 2023.
“I’m so relieved,” said Joey after surgery. “I don’t know what people who can’t access this program do.”

Rachel G. Simpson, MD, middle, stands with her first residency class as Moran’s new vice-chair of education.
Growing a Top 10 Residency Program
Enhancing hands-on surgical training and the interactive classroom experience is a top goal for Moran’s new vice-chair of education.
Among other qualities, the Moran Eye Center’s residency education program is known for superb training that provides more surgical experience than the national average and a hands-on curriculum that goes beyond traditional didactic teaching.
Newly appointed Vice-Chair of Education Rachel G. Simpson, MD, aims to build on that reputation.
“We have some exciting new initiatives in the works, and we’re looking forward to even more positive growth,” says Simpson.
Team Approach to New Curriculum
Former Moran resident Katherine Hu, MD, has joined the faculty and is now the surgical curriculum lead for the Program Evaluation Committee (PEC). Hu was part of the Moran Ophthalmology Learning Experience Committee, headed by Simpson, which rolled out a new, interactive curriculum in 2020.
Hu’s surgical curriculum team is revamping the four-year comprehensive surgical curriculum, including suturing, strabismus procedures, and cornea and cataract surgeries. The new curriculum will advance in complexity year by year.
“The goal is to be more intentional, providing enhanced mentorship with lots of hands-on learning,” says Simpson. “The curriculum will build on skills through all four years of residency, so the first-year residents are getting basic suturing lessons while the more experienced chief residents are getting more complex cataract surgery lessons. We will also emphasize surgical video reviews, one of the teaching legacies left by Moran’s late Alan Crandall, MD.”
Theresa Long, MD, director of Ophthalmology Consult Services, also serves on the PEC. Now in her second year as the institution’s first academic hospitalist, Long works one-on-one with residents, assessing and managing clinically complex, hospitalized patients experiencing a range of conditions.
“We’ll also be welcoming additional, nationally regarded adjunct faculty to assist with the educational programs soon,” says Simpson. “Each will be focused on a specific critical aspect of training, including clinical care, community outreach, and research.”
ARCS: Supporting Student Physician-Scientists
The Achievement Rewards for College Scientists (ARCS) Foundation of Utah is supporting two incoming Moran Eye Center residents with research scholarships for 2024-2025.
ARCS awarded $15,000 each to the honorees to pursue research during residency, hoping they will choose careers that continue their scientific investigations. Moran matches the award for the following two years of residency, providing a total of $45,000.
Nadim Azar, MD, received the Might Family Foundation Award in memory of Bertrand T. Might; Chase Paulson, MD, received the Mark and Kathie Miller Award in honor of Moran CEO Randall J Olson, MD.
Azar graduated with high distinction from the American University of Beirut with a bachelor of science in biology in 2017; he earned his medical degree from the American University in 2021. He then completed a postdoctoral research fellowship at Duke Eye Center.
At Duke, he focused on research in ocular immunology, including the therapeutic and preventive potential of peptides. His clinical research has focused on applying artificial intelligence in ophthalmology and pioneering innovative methodologies for detecting dry eye disease.
As a Moran resident, Azar plans to expand his research. Paulson completed his bachelor of science at Brigham Young University while playing collegiate lacrosse. He earned his medical degree from the University of Utah.
Under the mentorship of Moran’s Barbara Wirostko, MD, he has worked on projects and publications in the field of pseudoexfoliation syndrome and glaucoma. Working with Moran’s Global Outreach Division, he has conducted research in Guatemala and has studied these conditions across Utah, including the Navajo Nation.
At Moran, he plans to utilize unique database resources and conduct research to optimize high-quality care locally, regionally, and globally.

Moran offers one of the nation’s top educational programs, providing excellent didactic training and extensive surgical experience. A 2023 survey by physician website Doximity placed Moran’s residency program at No. 6 in the U.S. and No. 1 in the West.
FOR 4 SPOTS IN 2023
PRACTICING in 45 U.S. states, the District of Columbia, Puerto Rico, and 2 countries
FELLOWSHIP PROGRAM 2023-2024












IN A TYPICAL THREE-YEAR period, one Moran resident, on average, performs about 740 SURGERIES & PROCEDURES.
300 MORE THAN ARE CATARACT SURGERIES
86 IS THE NATIONAL REQUIREMENT
PUBLICATION S BY MORAN RESIDENTS IN 2023
CURRICULUM DETAILS
Scan for more information about our Education Program.

RESIDENCY PROGRAM 2023-2024












INTERNS 2023-2024







An Inspiring Night for Sight
The biannual gala supports the Global Outreach Division’s work to solve the worldwide problem of preventable blindness.
“See the need, be the change.”
Donors took the Moran Eye Center motto to heart at the Night for Sight 2023 gala, donating more than $650,000 and surpassing a fundraising goal for outreach care.
More than 500 guests attended the November 11 event at the Grand America Hotel in Salt Lake City, with proceeds benefiting the Moran Global Outreach Division’s work to end curable blindness by increasing access to eye care in Utah and worldwide.
“I am profoundly grateful to our sponsors, donors, committee and board members, colleagues, patients, and friends for seeing the need and generously rising to be the change,” said Moran CEO Randall J Olson, MD.

The evening’s program included an online and live auction and a remembrance of the late John A. Moran, with members of his family in attendance.
In another highlight of the evening, Olson named Mark and Kathie Miller the John A. Moran Eye Center Global Ambassadors for 2023, honoring them for their years of volunteer service and support of outreach initiatives. Mark Miller has donated his time and resources to fly Moran volunteer surgeons to the Navajo Nation through the Angel Flight nonprofit organization. Kathie Miller serves on Moran’s Global Vision Board.
Kathie and Mark Miller were honored as the John A. Moran Eye Center Global Ambassadors for 2023.
Members of the late John A. Moran’s family in attendance were grandchildren John Sullivan and Danielle Charlot, at left, and daughter Marisa Moran, second from right. Also pictured: Randall J Olson, MD, center, and Paul Jones.




Video Feature
Scan or visit moraneye.link/NFSVideo to watch “Be the Change: Moran Eye Center Utah Outreach.”


Photo Gallery
Scan or visit moraneye.link/nfs-photogallery to see more photos from the Night for Sight 2023 gala.

Event Program
Scan or visit moraneye.link/nfs-program to read the event program and learn more about our outreach division, supporters, and more.




HIGHLIGHTS Awards & Honors




Jeff Pettey, MD, MBA, received Real World Ophthalmology’s 2023 RWO Humanism in Ophthalmology Award, recognizing exceptional standards of care, compassion, and sensitivity in patient interactions. Pettey, Moran’s vice-chair of clinical affairs, will also receive the Intraocular Implant and Refractive Society, India (IIRSI) Gold Medal in 2024, honoring his contributions to the field of ophthalmology.
Afua Asare, OD, PhD, and Eileen Hwang, MD, PhD, were selected for Early Career Development Awards from the Intermountain Foundation at Primary Children’s Hospital. Asare, whose research focuses on pediatric vision health, will use the grant to fund her work to improve vision screening practices in pediatric primary care clinics. Hwang, a surgeonscientist, focuses her research on the vitreous, the transparent gel that fills the back of the eye between the lens and retina.

The grant will fund her continuing studies into Stickler syndrome, an inherited cause of retinal detachments in children.
Silke Becker, PhD, a faculty member in the Vinberg Laboratory, received a University of Utah Research Incentive Seed Grant. Sponsored by the University of Utah Research Foundation, the grant program supports investigators in collecting preliminary data in new, innovative research areas that will be leveraged for extramural grant applications. Becker studies retinal degenerative diseases, including diabetic retinopathy. Also, in 2023, Becker received a grant from Diabetes Research Connection, which pairs donors with early-career scientists to foster research to prevent and cure type 1 diabetes.
Two graduate research assistants in the lab of Paul S. Bernstein, MD, PhD, received special recognition in 2023. Emmanuel Kofi Addo, OD, received an Inclusive Excellence Award from the University of Utah College of Health. The award recognizes faculty, staff, and students who have exemplified the values of respect and equity and demonstrated diversity and inclusion in extraordinary ways. Addo was also one of three College of Health students awarded a scholarship at the NAACP Salt Lake Branch Annual Dr. Martin Luther King Jr. Commemoration. Pharmacology student Amaka Nwagbo received a University of Utah Graduate Research Fellowship Award, which provides the opportunity for full-time research during the fellow’s academic year.
HIGHLIGHTS
Awards & Honors
POWER LIST
The Ophthalmologist magazine named four Moran leaders in care and research to its 2023 Power List of the 100 most influential people in ophthalmology worldwide.






Iqbal Ike K. Ahmed, MD, FRCSC, director of the Alan S. Crandall Center for Glaucoma Innovation, was ranked No. 4. Ahmed is recognized as one of the world’s top surgeons for complex eye conditions and known for his research in the field of microinvasive glaucoma surgery. He divides his clinical practice between Canada and the Moran Eye Center.
The magazine also recognized Randall J Olson, MD, Moran CEO and chair of the Department of Ophthalmology and Visual Sciences; Liliana Werner, MD, PhD, co-director of the Intermountain Ocular Research Center and vice-chair of Equity, Diversity, and Inclusion at Moran; and Nick Mamalis, MD, co-director of the Intermountain Ocular Research Center and director of Moran’s Ophthalmic Pathology Lab.
Steffen Schmitz-Valckenberg, MD, was honored with the 2024 Macula Society Young Investigator Award and Lecture. The award recognizes individuals under age 50 whose work promises notable advances in the clinical treatment of eye disorders. A clinician and scientist, Schmitz-Valckenberg specializes in treating retinal diseases, including age-related macular degeneration. He is a world-renowned expert in highresolution retinal imaging and directs Moran’s Utah Retinal Reading Center.
Brian C. Stagg, MD, received the highest ranking out of nearly 2,000 submitted abstracts for personalized recommendation frequencies of visual field testing for patients with primary open-angle glaucoma at the 2023 American Glaucoma Society annual meeting. He presented his research and represented the American Glaucoma Society at the 2023 World Glaucoma Congress in Rome. A glaucoma specialist and public health researcher, Stagg has used informatics to simplify and streamline decision-making for physicians.
HIGHLIGHTS Awards & Honors
Gregory S. Hageman, PhD, received a Lifetime Achievement Award at the University of Utah’s 2023 Innovation Awards celebration. The award recognizes U researchers working to translate their research into technologies that benefit the public. Hageman, executive director of Moran’s Sharon Eccles Steele Center for Translational Medicine, has led his field in understanding the genetics of age-related macular degeneration and developing new therapies for the disease.
Nick Mamalis, MD, and Liliana Werner, MD, PhD, co-directors of the Moranbased Intermountain Ocular Research Center, received video, poster, and best-paper-of-session awards at the 41st American Society of Cataract and Refractive Surgery (ASCRS) meeting. The video, “The key to clarity: The open/expanded-bag IOL concept,” also received top honors at the Brazilian Society of Cataract and Refractive Surgery annual meeting. Additional honors for Werner in 2023 included delivering the Richard P. Kratz Lecture at the 35th Congress of German Ophthalmic Surgery and the 67th Snell Memorial Lecture at the Rochester Ophthalmology Conference.


Moran’s neuro-ophthalmology team and collaborators received numerous honors at the 2023 North American Neuro-Ophthalmology Society (NANOS) meeting. Meagan Seay, OD, received the Merit Award, and Nancy Lombardo, librarian emerita at the Spencer S. Eccles Health Sciences Library, received the Tom Carlow Distinguished Service Award for their work on the Neuro-Ophthalmology Virtual Education Library (NOVEL) project. Neuro-ophthalmology fellow Carolyne Riehle, DO, won Best Presentation by a Fellow, and U of U medical student Merrick Reynolds received the J. Lawton Smith Award for the paper in the Journal of Neuro-Ophthalmology receiving the most views in 2022. Co-authors included Moran faculty members Bradley J. Katz, MD, PhD, Kathleen B. Digre, MD, and Judith E.A. Warner, MD.

HIGHLIGHTS Awards & Honors
NEW
ENDOWED CHAIRS
Three Moran Eye Center faculty scholars were awarded endowed chairs in 2023 and honored in events that also recognized chair donors. “As the University’s primary means of recognizing academic distinction, endowed chairs and professorships promote excellence and enable the university to attract, retain, and honor distinguished faculty members,” says Randall J Olson, MD, Moran CEO, distinguished professor and chair of the Department of Ophthalmology and Visual Sciences, and holder of the Cumming Presidential Endowed Chair. “We are grateful to all of the donors who, across generations, make the Moran Eye Center the object of their lasting and generous philanthropy.”
T HE NEW CHAIR HOLDERS ARE:
Iqbal Ike K. Ahmed, MD, FRCS
—Jack R. and Hazel M. Robertson Presidential Endowed Chair Ahmed, a surgeon-scientist known for innovation, directs Moran’s Alan S. Crandall Center for Glaucoma Innovation. In this position, he spearheads efforts to develop better diagnostics, safer and more effective therapies and surgical devices, a deeper understanding of glaucoma and its genetics, and expanded access to care.

Nick Mamalis, MD
—Calvin S. and JeNeal N. Hatch Presidential Endowed Chair Mamalis is a surgeon-scientist who directs Moran’s Ophthalmic Pathology Laboratory and co-directs the Intermountain Ocular Research Center. An expert on intraocular lenses used to replace the eye’s natural lens during cataract and other surgeries, Mamalis has also helped hospitals nationwide protect patients from a rare but potentially sight-threatening condition known as Toxic Anterior Segment Syndrome.
Liliana Werner, MD, PhD
—Ralph and Mary Tuck Presidential Endowed Chair Werner co-directs the Intermountain Ocular Research Center and serves as vice-chair of Equity, Diversity, and Inclusion at Moran. Her research focuses on ophthalmic implantable biodevices, particularly intraocular lens design, materials, and complications. Among her honors, she was the first woman to receive the American Academy of Ophthalmology’s prestigious Charles D. Kelman Award and Lecture.


HIGHLIGHTS Events

Diversity Day at Moran
The Moran Eye Center’s Second Annual Diversity Day Robert H. Hales, MD, Memorial Endowed Lectureship highlighted a national mentorship program to boost the number of underrepresented medical students in ophthalmology residency programs.
Keith D. Carter, MD, chair of the University of Iowa Department of Ophthalmology and Visual Sciences and former president of the American Academy of Ophthalmology, delivered the endowed lecture, “Working Toward Diversity in Ophthalmology.”
Bench to Bedside Competition
A device that helps patients keep a steady gaze during eye surgery took the Grand Prize Runner-Up award at the 2023 Bench to Bedside competition presented by the Center for Medical Innovation at University of Utah Health. Named the OcuGuide, the invention is the brainchild of Joanna Gorka, a medical student, aspiring ophthalmologist, and mentee of Moran ophthalmologist Austin S. Nakatsuka, MD.


Translational Research Day
Moran’s annual Translational Research Day focused on the center’s current breakthroughs.
The National Eye Institute’s Kapil Bharti, PhD, delivered the keynote address, “Translating RPE Biology in Disease Treatment Using Stem Cells.”
The annual conference, co-chaired by Bryan W. Jones, PhD, and Leah Owen, MD, PhD, included presentations from several Moran faculty members on a variety of ophthalmic research topics.
HIGHLIGHTS Events

Department of Defense Presentations
Moran Eye Center CEO Randall J Olson, MD, and University of Utah Health CEO Michael L. Good, MD, welcomed Department of Defense (DOD) dignitaries to a day in September of research tours and presentations at Moran, Huntsman Cancer Institute, Huntsman Mental Health Institute, and the campus orthopedic surgery lab of Dustin L. Williams, PhD.
Moran researchers Paul S. Bernstein, MD, PhD, Moussa Zouache, PhD, David Krizaj, PhD, and Frans Vinberg, PhD, were among those participating. DOD officials included The Honorable Lester Martinez-Lopez, MD, assistant secretary of defense for Health Affairs, and Eugene Smith Jr., DHA, FACHE, executive officer to the assistant secretary of defense.
Robert Charles, chief, medical research collaborations, U.S. Army Medical Research and Development Command, presented “Collaborative Research with Defense Health Agency Laboratories and Hospitals.”
Uveitis Fellows Forum
The Moran Eye Center in January 2024 hosted the 15th Annual Uveitis Fellows Forum, presented by the American Uveitis Society. Co-chaired by Moran’s Albert T. Vitale, MD, and Marissa Larochelle, MD, the event served as a robust career planning and mentoring conference. It included a session moderated by Moran’s Caroline Craven, MD, of case presentations by uveitis fellows from institutions around the U.S. and a lively discussion of these cases by a roster of distinguished faculty physicians.
Interventional Glaucoma Consortium
The 2023 Interventional Glaucoma Consortium returned to Salt Lake City in 2023, bringing together top thought leaders in the field and offering a dedicated program for glaucoma fellows in partnership with Moran.
Program chairs and keynote speakers included Moran’s Ike Ahmed, MD, FRCSC, and Rachel G. Simpson, MD. Moran faculty member Craig J. Chaya, MD, presented “Going Global with Interventional Glaucoma,” and Brian C. Stagg, MD, presented “Glaucoma Informatics.”
The consortium promotes a proactive approach to patient care.





William Barlow, MD
Professor; Jack R. and Hazel M.
SPECIALTIES
• Glaucoma
• Complex Cataract Surgery
• Lens Implant Complications
Associate Professor
SPECIALTIES
• Comprehensive Ophthalmology
• Cataract Surgery
• Refractive Surgery
CEO of the John A. Moran Eye Center
Randall J Olson, MD
Distinguished Professor and Chair, Department of Ophthalmology and Visual Sciences
The Cumming Presidential Endowed Chair Director, University of Utah Vision Institute
SPECIALTIES

• Cataract Services
• External Eye Diseases


J.
Professor; Val A. and Edith D. Green Presidential Endowed Chair
SPECIALTIES
• Vitreoretinal Diseases and Surgery
• Retinal Biochemistry-Nutrition
• Inherited Retinal Diseases
• Macular Degeneration
Associate Professor; Medical Director, Moran Global Outreach Division; John E. and Marva M. Warnock Presidential Endowed Chair
SPECIALTIES
• Cataract Surgery
• Glaucoma
• Anterior Segment Surgery




Adjunct Associate Professor; Associate Editor of morancore.utah.edu
SPECIALTY
• Glaucoma
Caroline M. Craven, MD
Assistant Professor SPECIALTIES
• Ocular Oncology
• Uveitis and Ocular Immunology
• Vitreoretinal Diseases
Associate Professor SPECIALTY
• Neuro-Ophthalmology


B.
Distinguished Professor of Neurology and Ophthalmology; Chair, Clinical Ophthalmology Resource for Education (Moran CORE) Committee; Senior Editor, morancore. utah.edu
SPECIALTY
• Neuro-Ophthalmology




Associate Professor
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
• Complicated Adult and Child Strabismus
• Craniofacial Disorders

Assistant Professor SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)

Robert C. Kersten, MD, FACS, FASOPRS
Professor; Division Chief of Oculoplastics
SPECIALTIES
• Oculoplastics and Facial Plastic Surgery
• Pediatric and Adult Eyelid, Eye Socket, Tear Duct Abnormalities
Professor
SPECIALTIES
• Treatment and Management of AMD
• Degenerative Retinal Diseases

Assistant Professor SPECIALTIES
• Adult and Pediatric Retina Diseases and Surgery

Associate Professor
SPECIALTIES
• Oculoplastic and Facial Plastic Surgery
• Pediatric and Adult Eyelid, Eye Socket, Tear Duct Abnormalities
Assistant Professor; Director of Ocular Oncology
SPECIALTIES
• Vitreoretinal Diseases and Surgery
• Ocular Oncology

Associate Professor; Director of Medical Student Education for the Department of Ophthalmology; Editor of morancore.utah.edu
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
Professor SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
• Complicated Pediatric and Adult Strabismus
• Pediatric Outreach

J.
Professor SPECIALTIES
• Cataract Services
• Neuro-Ophthalmology
• Comprehensive Ophthalmology


Associate Professor
SPECIALTIES
• Uveitis and Ocular Immunology
• Comprehensive Ophthalmology
• Cataract Surgery
Associate Professor; Medical Director of Utah Lions Eye Bank; Vice Chair of Faculty Affairs
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)
• Ocular Surface Disease




Assistant Professor; Director of Ophthalmology Consult Services
SPECIALTIES
• Cataract Surgery
• Comprehensive Ophthalmology
• Ophthalmic Hospitalist Services

S.
Assistant Professor
SPECIALTIES
MD
• Anterior Segment and Complex Cataract Surgery
• Medical and Surgical Glaucoma
• Comprehensive Ophthalmology

Associate Professor
SPECIALTIES
• Comprehensive Ophthalmology
• Ocular Surface Disease
Professor; Director of the Ophthalmic Pathology Laboratory; Calvin S. and JeNeal N. Hatch Presidential Endowed Chair
SPECIALTIES
• Cataract Services
• Ophthalmic Pathology
• Comprehensive Ophthalmology

Pettey, MD,
Associate Professor; Dr. Ezekiel R. and Edna Wattis Dumke Endowed Chair; Vice-Chair of Clinical Affairs
SPECIALTIES
• Anterior Segment and Complex Cataract Surgery
• Comprehensive Ophthalmology

Brian T. Rose, MD
Adjunct Associate Professor
SPECIALTY
• Comprehensive Ophthalmology
Adjunct Associate Professor SPECIALTIES
• Oculoplastic and Facial Plastic Surgery
Professor; Director, Cornea and Refractive Division; Associate Medical Director, Utah Lions Eye Bank; Director, Cornea Fellowship Program
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)
Meet Our Physicians

Scan for a video playlist to learn more about the care our physicians provide.

Steffen Schmitz-Valckenberg, MD
Professor; Jon M. Huntsman Presidential Chair at the University of Utah
SPECIALTY
• Macular and Vitreoretinal Diseases and Surgery




Assistant Professor; Chair of Visual Electrophysiology
SPECIALTIES
• Neuro-Ophthalmology
• Visual Electrophysiology

Adjunct Associate Professor SPECIALTY
• Comprehensive Ophthalmology
Associate Professor; Director of the Uveitis Fellowship Program
SPECIALTIES
• Retinal Diseases and Surgery
• Uveitis and Ocular Immunology
Assistant Professor; Vice Chair of Education
SPECIALTIES
• Glaucoma
• Cataract Surgery
• Anterior Segment Surgery



Professor; Director of the Uveitis Division
SPECIALTIES
• Uveitis and Ocular Immunology
• Vitreoretinal Diseases
Professor; Chief of NeuroOphthalmology; Vice-Chair of Quality and Value
SPECIALTY
• Neuro-Ophthalmology

Professor; Director of Vitreoretinal Diseases and
• Retinal Diseases and Surgery
Assistant Professor SPECIALTIES
• Glaucoma
• Comprehensive Ophthalmology
• Cataract Services
• Geriatric Ophthalmology

Assistant Professor; Associate Program Director of Education
S PECIALTIES
• Neuro-Ophthalmology
• Pediatric Ophthalmology
• Adult and Child Strabismus


Adjunct Professor; Adjunct Professor Biomedical Engineering
SPECIALTY
• Glaucoma
Associate Professor; Chief, Division of Pediatric Ophthalmology
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
Meet Our Physicians

Scan for a video playlist to learn more about the care our physicians provide.


Professor; Glaucoma Division Chief; Glaucoma Fellowship Director
SPECIALTIES
• Glaucoma Services
• Cataract Services
Associate Professor
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)
OTHER SPECIALTIES




Medical Director of Anesthesia Services at Moran
SPECIALTY
• General Anesthesiology
Patient Support Program Specialist
SPECIALTY
• Vision Rehabilitation
Director, Ophthalmic Ultrasound Department
SPECIALTIES
• Ophthalmic Ultrasound
• Comprehensive Ophthalmology
Director, Patient Support Program
SPECIALTIES
• Psychosocial and Functional Issues Related to Vision Loss

Deepika Bagga, OD, provides a full range of optometry services, with special interest in contact lenses and dry eye management.
John A. Moran Eye Center
Midvalley Health Center

Brandon J. Dahl, OD, FAAO, specializes in comprehensive optometry, pediatrics, disease management with special emphasis on anterior segment disease, and contact lenses.
Farmington Health Center

David Meyer, OD, FAAO, is the Director of Contact Lens Services, specializing in fitting lenses for keratoconus, post-surgical corneas, pediatrics, irregular or high astigmatism, and eye trauma. He also provides comprehensive eye care for glasses and soft contacts.
John A. Moran Eye Center
Midvalley Health Center

Shandi M. Beckwith, OD, provides a full range of optometry services for adults and children, with special interests in myopia management and contact lenses.
Farmington Health Center
Redwood Health Center
South Jordan Health Center

Timothy L. Gibbons, OD, is the Director of the Optometry Division, specializing in comprehensive eye care with special interest in contact lenses, pediatrics, and glaucoma.
Redwood Health Center Stansbury Health Center

Edward R. Nicholls, OD, provides comprehensive eye care services, with special interest in contacts, ocular pathology, myopia control, pediatrics, and those with special needs.
Westridge Health Center

Robert H. Corry, OD, provides a full range of optometry services for adults and children, with a special interest in ocular pathology, contact lenses, and dry eye management.
South Jordan Health Center

Gabriel A. Hulewsky, OD, provides comprehensive optometry services, with special interest in contact lenses, dry eye management, and sports vision.
Midvalley Health Center Parkway Health Center

Dix H. Pettey, OD, MS, specializes in fitting contact lenses for keratoconus, pediatrics, post-surgical, and eyes with severe or irregular astigmatism. He also provides comprehensive eye care for glasses and soft contacts.
John A. Moran Eye Center
Midvalley Health Center

Ryan Coyle, OD, provides a full range of optometry services, with an emphasis on primary care, contact lenses, and the diagnosis and treatment of ocular diseases.
Redstone Health Center

Mark A. McKay, OD, specializes in full-scope optometric care, including adult and pediatric care, contact lenses, and anterior segment eye disease.
John A. Moran Eye Center Redwood Health Center

Iqbal Ike K. Ahmed, MD, FRCSC
Professor; Director, Alan S.Crandall Center for Glaucoma Innovation; Jack R. and Hazel M. Robertson Presidential Endowed Chair
SPECIALTIES
Glaucoma, Cataract, and Lens
Implant Surgical Therapeutics; Novel Device and Surgical Technique Development

Research Assistant Professor
SPECIALTIES
Retinal Electrophysiology; Retinal Degenerative Diseases; Diabetic Retinopathy; Photoreceptor Physiology

Research Assistant Professor
SPECIALTY
Cortical Mechanisms of Visual Perception

Alessandra Angelucci, MD, PhD
Professor; Mary H. Boesche Endowed Professor of Ophthalmology and Visual Sciences
SPECIALTIES
Visual Cerebral Cortex Structure and Function; Development of Novel Technologies

Paul S. Bernstein, MD, PhD
Professor and Vice-Chair for Clinical and Basic Science
Research; Val A. and Edith D. Green Presidential Endowed Chair
SPECIALTIES
Nutritional Biochemistry; Macular and Inherited Retinal Degeneration; Fluorescence Lifetime Imaging Ophthalmoscopy

Professor
SPECIALTIES
AMD, Degenerative Retinal Diseases; High-Resolution Imaging; Identification of Prognostic Biomarkers for Disease Progression; Validation of Clinical Endpoints for Interventional Trials

Research Assistant Professor
SPECIALTIES
Pediatric Vision Health; Health Services and Systems Research; Health Equity and Disparities; Cost Effectiveness Analysis; Implementation Science

Research Assistant Professor SPECIALTIES
Visual Cerebral Cortex Structure and Function

Professor
SPECIALTIES
Membrane Protein Transport in Photoreceptors for Inherited Retinal Disease; Photoreceptor Biochemistry; Molecular Cell Biology

Research Professor (Emeritus) SPECIALTY Electrophysiology

Research Associate Professor
SPECIALTY
Retinal Cell and Molecular Biology

John A. Moran Presidential Endowed Chair; Executive Director, Sharon Eccles Steele Center for Translational Medicine
SPECIALTIES
Genetics and Assessment of Pathways Involved in AMD Etiology; AMD Target Identification and Therapeutic Development
MORAN EYE CENTER Research Team 2023-2024

Assistant Professor
SPECIALTIES
Vitreous; Collagen; Extracellular Matrix; Aging; Protein Aggregation

David Krizaj, PhD
Professor; Deputy Director of Research; John Frederick Carter Endowed Professor of Ophthalmology and Visual Sciences
SPECIALTIES
Glaucoma and Intraocular Pressure Regulation; Photoreceptor Signaling; Calcium Regulation in Neuropathological Disorders

Assistant Professor
SPECIALTIES
Glaucoma; Conventional Outflow Physiology; Extracellular Vesicles; Extracellular Matrix; Biomedical Engineering Microfluidics; Eye Perfusions

Associate Professor; Direc tor, Marclab for Connectomics
SPECIALTIES
Retinal Degeneration Disorders; Retinal Neurotransmission and Neurocircuitry; Metabolomics

Binxing Li, PhD
Research Assistant Professor
SPECIALTIES
Biochemistry and Biophysics of Macular Carotenoids; Mouse Models of Retinal Disease; Raman Imaging of Nutrients in the Retina

Research Assistant Professor; Assistant Professor, Electrical and Computer Engineering
SPECIALTIES
Computational Neuroscience; Neural Mechanisms of Visuospatial Perception

Professor
SPECIALTIES
Photophobia (abnormal light sensitivity); Migraine and its Effects on Visual Quality of Life; Ischemic Optic Neuropathy

Professor; Co-Director, Intermountain Ocular Research Center; Calvin S. and JeNeal N. Hatch Presidential Endowed Chair
SPECIALTIES
Ocular Pathology; Comprehensive Ophthalmology; Intraocular Lens Research; Postoperative Inflammation

Professor (Emeritus); Distinguished Professor of Bioengineering, University of Utah; Doctor Honoris Causa, Universidad Miguel Hernandez de Elche, Spain
SPECIALTIES
Artificial Vision/Neural Prosthetics

Professor (Emerita); Doctor Honoris Causa, Universidad Miguel Hernandez de Elche, Spain; Editor, webvision.med.utah.edu
SPECIALTY
Retinal Anatomy

E.
Distinguished Professor (Emeritus)
SPECIALTIES
Retinal Neurotransmission and Networks; Retinal Degenerations; Metabolomics

Associate Professor
SPECIALTIES
Cognitive Neuroscience; Prefrontal Modulation of the Visual Cortex
MORAN EYE CENTER Research Team 2023-2024




Steffen Schmitz-Valckenberg, MD
Associate Professor; Dr. Ezekiel R. and Edna Wattis Dumke Endowed Chair
SPECIALTIES
Phacoemulsification Platform
Efficacy and Efficiency; Ophthalmology Training Methods and Outcomes

Assistant Professor SPECIALTIES
Clinical Decision Support in Glaucoma; Personalized Medicine; Health Informatics; Population Health

Professor SPECIALTIES
Pathogenetic Mechanisms of Retinal Degeneration; Cell Biology of Photoreceptors
Assistant Professor
S PECIALTIES
Neuroscience; Microscopy (Electron, Fluorescence, Confocal, Bright-field); Data Science; Connectomics

Ning Tian, PhD
Professor; Adjunct Professor, Neurobiology SPECIALTIES
Retinal Neurobiology; Synaptic Plasticity
Assistant Professor SPECIALTIES
Retinal and Central Visual Processing; Mechanisms of Light Adaptation; Retinal Computations; Retinal Diseases; Comparative Biology of Vision

Associate Professor SPECIALTIES
Retinal Neurobiology; Bioengineering; Mechanisms of Light Signaling and Plasticity in the Retina; Retinal Disease

Research Assistant Professor
SPECIALTIES
Retinal Degeneration Diseases; Neuroscience; Gene Therapy

Assistant Professor SPECIALTIES
AMD; Genetics of Eye Disease; Computational Biology; Engineering Ophthalmology; Drug Development
Professor; Jon M. Huntsman Presidential Chair; Director, Utah Retinal Reading Center, uread.org
SPECIALTIES
AMD; Retinal Imaging; Structural-Functional Correlation

Professor; Co-Director, Intermountain Ocular Research Center; Ralph and Mary Tuck Presidential Endowed Chair; ViceChair for Equity, Diversity, and Inclusion
SPECIALTIES
Ocular Biodevices Research; Different Intraocular Lens Designs; Materials and Surface Modifications; Interactions between Ocular Implants and Ocular Tissues
MORAN EYE CENTER ADJUNCT RESEARCH TEAM
Paul Bressloff, PhD
Brittany Coats, PhD
Karen Curtin, PhD, MStat
Michael Deans, PhD
Jungkyu Kim, PhD
Kristen Kwan, PhD
Jon Rainier, PhD
Jason Shepherd, PhD
Monica Vetter, PhD
Catherine Bowes Rickman, PhD
Victor Chong, MD
Carter Cornwall, PhD
Margaret DeAngelis, PhD
Adam Dubis, PhD
Eugene de Juan, MD
Eduardo Fernandez, MD, PhD
Werner Gellermann, PhD
Mary Elizabeth Hartnett, MD
Wen Fan Hu, MD, PhD
Ariana Levin, MD
Li Jiang, MD, PhD
Anat Loewenstein, MD
P hilip Luthert, MBBS, FRCP, FRCPath, FRCOphth
Jordi Monés, MD, PhD
Debra Schaumberg, ScD, OD, MPH
Matthew B. Schlenker, MD
Arsham Sheybani, MD
William Daniel Stamer, PhD
Omer Trivizki, MD
Larry A. Wheeler, PhD
Barry Willardson, PhD
Lloyd Williams, MD, PhD
ADJUNCT VOLUNTEER OPHTHALMOLOGISTS 2023-2024
Adjunct volunteer faculty collaborate on research projects, participate in clinical studies, attend teaching opportunities, and assist on our outreach medical missions.
Jason Ahee, MD
St. George, Utah
Arwa Alsamarae, MD
Santa Rosa, California
Lisa Arbisser, MD Sarasota, Florida
Nicholas Behunin, MD St. George, Utah
John Berdahl, MD Sioux Falls, South Dakota
Ashlie Bernhisel, MD Rochester, Minnesota
Ronnie Bhola, MBBS St. Augustine, Trinidad
Kristin O. Bretz, MD Salt Lake City, Utah
Eric Brinton, MD Salt Lake City, Utah
Gregory Brinton, MD Murray, Utah
Michael Burrow, MD Salt Lake City, Utah
Joseph Chen, MD Ventura, California
Robert J. Cionni, MD Salt Lake City, Utah
Richard P. Corey, MD Provo, Utah
David A. Crandall, MD West Bloomfield, Michigan
Sonya Dhar, MD New York, New York
Jane Durcan, MD Salt Lake City, Utah
Jayson David Edwards, MD St. George, Utah
David Faber, MD Salt Lake City, Utah
Sophia Fang, MD Tigard, Oregon
William J. Fishkind, MD Tucson, Arizona
Nicole R. Fram, MD Los Angeles, California
Roger C. Furlong, MD Butte, Montana
Mitchell J. Goff, MD Salt Lake City, Utah
Shawn Gulati, MD Chicago, Illinois
Reeta Gurung, MD Kathmandu, Nepal
Anna Gushchin, MD Hines, Illinois
Arezu Haghighi, MD Ventura, California
Tara Hahn, MD Houston, Texas
Bradley Hansen, MD Idaho Falls, Idaho
Matheson A. Harris, MD Salt Lake City, Utah
James G. Howard, MD Murray, Utah
Todd Jackson, MD Las Vegas, Nevada
Zachary Joos, MD Renton, Washington
Khizer Khaderi, MD Sacramento, California
Victoria Knudsen, MD Murray, Utah
Elliott Kulakowski, MD Park City, Utah
Robert C. Kwun, MD Murray, Utah
David P. Lewis, MD Brigham City, Utah
Susan MacDonald, MD Concord, Massachusetts
Jay J. Meyer, MD Auckland, New Zealand
Majid Moshirfar, MD Draper, Utah
Valliammai Muthappan, MD Sewickley, Pennsylvania
William Myers, MD Chicago, Illinois
Anastasia Neufeld, MD Vancouver, British Columbia, Canada
Tom Oberg, MD Salt Lake City, Utah
Hreem Patel, MD Stickley, Illinois
Rachel Patel, MD Sacramento, California
David B. Petersen, MD Salt Lake City, Utah
Marcos Reyes, MD St. George, Utah
Trent Richards, MD Layton, Utah
Christopher Ricks, MD Provo, Utah
Sanduk Ruit, MD Kathmandu, Nepal
Derek J. Sakata, MD Salt Lake City, Utah
Joshua Schliesser, MD St. George, Utah
Loren S. Seery, MD Kennewick, Washington
Barry S. Seibel, MD Los Angeles, California
D. Snow Slade, MD St. George, Utah
Robert E. Smith, MD West Valley City, Utah
R. Doyle Stulting, MD, PhD Atlanta, Georgia
Russell Swan, MD Bozeman, Montana
Scott O. Sykes, MD Ogden, Utah
Geoff Tabin, MD Palo Alto, California
Robert L. Treft, MD Layton, Utah
James Tweeten, MD Boise, Idaho
Albert Ungricht, MD
Salt Lake City, Utah
Jeremy Valentine, MD Bangor, Maine
Aaron N. Waite, MD Lehi, Utah
Gary Wallace, MD
Idaho Falls, Idaho
Matthew S. Ward, MD Provo, Utah
Charles H. Weber, MD Oregon City, Oregon
Eric Weinlander, MD Madison, Wisconsin
Robert C. Welch, MD Twin Falls, Idaho
John Welling, MD Medford, Oregon
Brice J. Williams, MD, PhD Ogden, Utah
Darcy Wolsey, MD, MPH Salt Lake City, Utah
Gilbert C. Wong, MD West Jordan, Utah
DonRaphael Wynn, MD Boise, Idaho
Zachary J. Zavodni, MD
Salt Lake City, Utah
The following individuals and organizations contributed to the Moran Eye Center between January 1, 2023-December 31, 2023.
DONORS
GIFTS OF $1,000,000 AND ABOVE
David W. Bernolfo
Dick and Timmy Burton Foundation
Olson-Huntsman Vision Foundation
Perceive Biotherapeutics
GIFTS OF $100,000 AND ABOVE
Cumming Foundation
Thomas R. and Susan C. Hodgson
Judelson Family Foundation
Gabe L. Newell
Ruth and Randall J Olson, MD
Sylvia Prahl-Brodbeck
Research to Prevent Blindness
Sharon Steele-McGee
GIFTS OF $50,000 AND ABOVE
Val A. Browning Foundation
William H. and Patricia W. Child
Crocker Catalyst Foundation
Thomas and Candace Dee Family Foundation
David Kelby Johnson Memorial Foundation
The Mark and Kathie Miller Foundation
gifts of $25,000 and above
Iqbal Ike K. Ahmed, MD, FRCSC, and Ruby Alvi, MD
Kurt Bestor
The Jeffrey and Helen Cardon Foundation
Bill* and Barbara Chrisman
Eileen Crawford and Alan Jones
George S. and Dolores Doré Eccles Foundation
Willard L. Eccles Charitable Foundation
Christine A. and Fred W. Fairclough
Grandeur Peak Global Advisors
William B. Hale*
Thomas C. Praggastis and Michelle Dumke Praggastis
Edward H. Skinner
Mikel and Janel Trapp
Carlene and Jay Williams
gifts of $10,000 and above
Anonymous
David G. and Marie P. Anderson
ASCRS Foundation
William and Sara Barrett
Joe Bernolfo
Burningham Foundation
Andrea S. Dumke-Manship and Michael A. Manship
Jane and Stuart Engs
Joan and Tim Fenton Family Foundation
Joan B. and John H.* Firmage
John H. and Carol W. Firmage
Teri and Dean Flanders Foundation
The Firmage Group, Inc.
The Firmco Group
Chris Gandy
Margaret D. Hicks
Carol O. Holding
Stephen and Lynda Jacobsen Foundation
G. Frank and Pamela M. Joklik
Lindsey Fairclough Little and Jon Little
James M. and Alison Luckman
Dr. Nick and Mercy Mamalis
Dr. Tina Mamalis and Dr. Shawn Purnell
John M. Martin
Thomas O. and Diane J. Might
Marisa Moran
Dave and Donna Newberry
The Olch Family Trust
Gilman* and Margaret D. Ordway
George and Cynthia Strike Petrow
Reagan Outdoor Advertising
The Semnani Family Foundation
Rod Semnani
Jonathan P. and Elizabeth M. Slager
James M. Steele and Linda Wolcott-Steele
Sun Print Solutions
Haru Toimoto
James W. and Jeanne J. Welch
Duff M. and Lori Willey
Lisa and Bill Wirthlin
Terry L. Wright
gifts of $5,000 and above
Anonymous
Byron B. and Deborah K. Barkley
Ann P. Bernstein and Paul S. Bernstein, MD, PhD
Rodney H. & Carolyn Hansen Brady Foundation
Julie T. Crandall
Tony and Joyce G. Crandall
Robert W. and Carol N. Culver
Errol P. EerNisse and Sonja Chesley EerNisse
Tom and Lynn Fey Family Foundation
Cecelia H. Foxley, PhD
Linda L. Francis
Drue B. Huish
Katie and Griffin J. Jardine, MD
John W. and Helen B. Jarman Family Foundation
Kay W. Lipman
William and Suzelle McCullough
Charles H. McLeskey, MD, and Nanci S. McLeskey, DNP
Vicki Bettilyon Merchant
The June Morris and Frendt Family Foundation
Karl and Joan M. Mosch
Pegah N. and Majid Moshirfar, MD
George and Pauline Mulligan
San Diego Eyelid Specialists
Steffen Schmitz-Valckenberg, MD, and Monika Fleckenstein, MD
Meagan D. Seay, DO
Susan O. Taylor
John Cramer Terrill
Gretchen and Michael P. Teske, MD
Albert T. Vitale, MD, and Patricia A. Vitale, MD
Warde Foundation
James R. and Linda R. Wilson
gifts of $1,000 and above
Anonymous
George M. and Tracy J. Ahn
Barry J. and Cathy F. Angstman
Patrice M. Arent and David M. Mock
Wendell Arrington, MD, PhD
Eugene W. Banks
Bonnie Barry
William F. and Victoria F. Bennion
Scott and Elaine Bergeson
Margaret D. and Peter W. Billings
Barry and Denise Blackett
Gary and Anne Borman
Michael and Patricia Brill
Cadenza Family Dentistry
John Cahill
Camp Chef
Blaine L. Carlton and Marilyn Bushman-Carlton
Robert S. Carter Foundation, Inc.
Irene G. Casper and Ruth A. Morey
Danielle Charlot
Val E. and Steve L. Chin
Karen R. and John J. Chipman, MD
Ben Chortkoff, MD, and Susan Chortkoff, MD
Howard and Betty Clark
Jeff and Jane Cobabe
Daniel M. Cook
Richard L. and Janice M. Corbin
Traci O’Very Covey
Ronald W. Crouch and Elizabeth A. Nielson
Current Fish and Oyster
Allison A. and Michael E. Daun, MD
Jim and Susan C. Deacon
Deerfield Ranch Winery
Kevin W. Deesing
Dry Creek Charities
Tracy J. Eilers
Jack M. and Marianne Ferraro
The Fletcher Jones Foundation
David and Karen Flood
John Foley, MD, and Dorene K. Sambado
Richard K. Frerichs and Jean Zancanella
Pamela Fullerton
Ernest and Judith Getto
Robert M. Graham
Elizabeth Gray
Sivaraman Guruswamy and Vasantha Sivaraman
R.Craig and Gloria H. Hansen
Julia A. Hardy
Julie K. and Ryan Harmon
Carolyn S. and Robert O. Hoffman, MD
Jerry S. and Claudia F. Howells
Katherine Hu, MD
Hullinger Family Foundation
Theodore M. and Charlotte G. Jacobsen
Jim S. and Jeanne M. Jardine
Rodney John Adell Johnson*
Donald C. Johnson
Jeffrey E. Jones
Karen and Douglas K. Kelsey, MD, PhD
Rick and Beth Kent
Lisa G. and David B. Kieda
Judd P. and Lori R. King
Kate Lahey and Michael J. Lahey, MD
Christine Lake and Heber S. Jacobsen
Frank and Barbara Layden
S.Whitfield and Christina Lee
The Robert B. Lence Family
Chris and Susan E. Lockwood
Kimberly G. and W. Scott Lohner, MD
Alice and Jared Lynch
Paul and Ruth Lyon Family Foundation
Milo S. and Karen J. Marsden
Ted A. McKay
Valerie A. and Mark D. Mifflin, MD
Roy F. Miller
Moschetti Family
Viet Tan Nguyen
Donald E. Nickelson
Van B. and Maude E. Norman
Ruth L. Novak
O.C. Tanner Company
Suzanne E. Oelman
C.James Olson
Sarah Olson
Nancy A. and Randy A. Parker
Bonnie D. and James L. Parkin, MD*
Andrew Pendleton
Chris and Lisa A. Peterson
Gretchen and Jeff Pettey, MD, MBA
Tanya Polzer
Brent Price
David P. and Suzanne J. Razor
Ronald Reaveley Family
Red Butte Lions Club
Barbi Reed
Daniel and Lynette E. Reichert
Arnold and Mary Richer
Edward N. Robinson
Gary W. Rodgers and Chris Filtz
Gerald Rolfe
Karen O. and Stephen C. Roney
John and Patricia Rosenwald
Derek Sakata, MD, and Cindy Sumarauw, DDS
Scheels All Sports
Rachel G. Simpson, MD
Mimi and Cory Sinclair
Britney and Tyler S. Snell
Snowbird Ski and Summer Resort
Stephen and Marji Bailey Sofro
Kent P. and Dana L. Strazza
Stephen D. and Sonnie S. Swindle
Lary J. and Judy W. Talbot
Virginia S. and Verl H. Talbot, MD
Allan and Frances Tessler
Daniel M. Thomas
I.Ray Thomason, MD
Candy Turnbull
Susan Bollinger Tybur and Jim Tybur
Stephen and Ingrid Tyler
University of Utah Advancement
University of Utah Department of Athletics
University of Utah Football US Foods
Sravanthi Vegunta, MD
Tod Wadsworth
Matthew J. and Lynn W. Ward
Judith E.A. Warner, MD
Thomas and Melissa Wheatly
Larry Allen Wheeler, PhD
Andre and Brenda L. Williams
Loren and Jane Yager
W.Craig and Jan L. Zwick
William J. Zwiebel, MD
gifts of $100 and above
Anonymous
Hans G. Ahrens
Anne Davis Alexander
John C. and Sheryl L. Allen
JoAnne Ambrose
Carol A. and James A. Anderson, PhD
DeAnn R. Anderson
Lissa C. Anderson
Milton M. and Emily Diane Anderson
Brent and Cheri Andrus
Ronald I. Apfelbaum, MD, and Kathleen A. Murray, MD
Seamus Appel
Asart Design
Pamela J. Atkinson
Ekhlas A. Attia
Robert K. Avery, PhD, and C. Frances Gillmor
Ann Crandall Bagley
Ballet West
Margaret D. and Bryce G. Barker, MD
Larry R. and DeAnn Barrigar
Barbara E. Bean, MD, and James R. Haisley
David W. Becker Jr. MD, JD
John E. Bendixen
Richard and Ronni Bergman
Erin Westenskow Berrett
Sarah A. Berry
Sheila M. Bilbrey
Beverly Blair
Bonnie Blanchard
Christie and BJ Blaser
Jonathan D. and Stephanie Anne Bletzacker
Blue Halo
BMW of Murray
Arlyn R. and Norma Bodily
Sheri A. and O’Dell M. Bodily
Jon Boney
William J. and Heather F. Bonn
Peter and Billie Borgerding
Gary and Herlinda B. Bowen
Alan C. and Ann Bradshaw
Dennis and Kathy Brandon
Richard T. and Sharon Bretzing
Steven M. and Joan M. Brinton
Merle Y. Broadbent
Tim W. and Marlise P. Brough
Barbara and Lewis J. Brown, MD
Susan J. Brown
Judge James Bucci
Doris V. Buckholtz
Jean Buhl
Ann and Darryl Butt, PhD
Cactus & Tropicals
Jules Campbell
Linda J. Campbell
Robin C. Campbell and
Marion R. Riley
Charlie Cardon
George Cardon-Bystry
Randall C. Carlisle
John K. and Shirley A. Carmack
Levi and Marcie Carrigan
Tyler D. Carson
Jason E. Castor
Jean Chang
Becky Chapman
Kathleen Chatelain
The Cheesecake Factory
Jimmy Chen, PhD, and Ling-Ling Leu
Chick-fil-A
Qing Chong
Karen Christensen
Kurt P. and Deborah Christiansen
James A. and Margaretha Church
David M. and Carol A. Cise
Kara Clapp, PhD
Sherman and Susan Clow
Kristen Merinda Cobabe, MSW
Susan Coble
Cohenour Family Trust
Chris Conabee
Marian A. Connelly-Jones and Gary Jones
Rebecca and Vernon Cooley, MD
Wade and Judy Coon
Craig Cooper and Suzanne A. Harris Cooper
Sandra Lee Corp
Bernadette M. Coughenour
Cranky’s Bike Shop
Caroline M. Craven, MD
Dorothy Cromer
Everett P. and Mary Kay Davis
Wayne Day
Monika M. and H. James de St. Germain
Linda P. and Nathan C. Dean, MD
Kyle L. Dearden
Nancy DeCamp
Carl Dennison
Carolyn Bartlett Deru
Richard S. and Janet DeWolfe
Kathleen B. Digre, MD, and Michael W. Varner, MD
Discovery Gateway Children’s Museum of Utah
Huyen T. Do
Vivian Dowsett Interiors
Dream Inn
Jauna and Gregory Dupratt
Lois M. Dutson
Ecobabe
Edison House
John S. Edwards
Peter M. and Bonnie H. Edwards
Karen Ehresman
Maureen C. Ellis
Eugene F. and Joan R. Erbin
Erin Evans
Shirley Evans
Every Blooming Thing
Dennis D. and Carma B. Ewing
Fat Cats
Daniel S. and Carri Fergusson
Theresa Ferraro
Tyler Firmage
Fish Tech Outfitters
Carole E. Fishburn
Russ Fjeldsted*
Kristen M. Fletcher and Dan McPhun
Robert D. Folker
Jennifer J. and Mark C. Foote, MD
Scott and Petria H. Fossel
Elaine T. and Frank W. Fox, PhD
Todd and Michelle France
Luella B. Freed
Gloria Freedman
B. J. and Brian Fullmer
D.Jay Gamble
The Garden Store
Gregory and Jannis Gardner
K.Gary and Linda S. Garff
Martin I. and Sheila G. Gelman
Rebekah Gensure, MD, PhD
Jennifer George
Tyler Gillespie
William A. and Claudia M. Gislason
Stephen V. Goddard
Lawrence K. Goldsmith
Steve and Merrilee Gottfredson
The Grand America Hotel
Green Drake Outdoors, Dustin Carlson
Kay B. Greene
Jean Groce
Nancy O. Groce
Bernard I. Grosser, MD, and Karen J. McArthur
Kathleen Gubler
Kirsty Ann Gunther
Duane L. Haas
Margaret L. Haas
Jill L. and Gregory S. Hageman, PhD
Jon and Karen J. Hale
Mark R. and Julie K. Hale
Steven T. and Julie Halvorson
Ronald C. Hamblen and Kristine Janson
Miles and Siena Hansen
Francis Hanson
Gareld D. and Betty Jo Hanson
Joan M. and Francis V. Hanson, PhD
Franz Hardin
Joann Hardin
Brad D. Hardy and Jolie A. Coleman
Harper Nail Salon
Deborah Y. Harrison
Patricia Harte
Robert Hartleben
Douglas Hattery
James V. and Gail Hawkins
Susan D. Heath and William R. Tanner
James A. and Arlene M. Helfand
Nicole L. Herman
Deon T. Hilger
Hires Big H
Raymond Hollowell
Vaughn Howard
Nancy C. and Dennis C. Hughes, MD
Samuel and Sandra Hunter
Hunt’s Trading Post
I.J. & Jeanne Wagner Jewish Community Center
ilLumin8skin
Albert Imesch
Harry F. and Marjorie Immerman
Kathleen A. Isaac
JAM Collective and Vasque Footwear
Roy and Eileen G. Jenkins
Martha Lewis Jennings
Linda H. and Leland D. Jensen
Peter E. Jensen, MD
Amy A. and Matthew Johnson
James and Lauren Jolly
Paul Jones
Robert Jones
W.Stanley Jones and M. Gay Taylor-Jones
Judy O’s Floral
Kamas Valley Lions Club Service Project
Brad, Tracey, Sam, Jonah, and Zev Katz
Kurt and Joette M. Katzer
Robert C. Kersten, MD, FACS, FASOPRS
Lloyd Kianfar
Paul and Geraldine Kilpatrick
Cornelia Kincanon
Laura Kinser Studios
Julia J. Kleinschmidt, PhD
Koloa Landing Resort
Barbara Brittain Korous
Bob and Marilyn Kukachka
Melinda Kurnath
Heather L. Labrum
Frank B. and Denise A. Ladenburg
Roger O. and Sue Ladle
Lagoon Corporation
Stephen and Natalie Lam
Loris Largo-Rhodes
Jean M. Larsen, PhD
Shane Larson and Genevieve Christianson
LC Hess Construction
Barbara and Melvin D. Leibsla
Lawrence J. Leigh, PhD, and Wendy Foster Leigh
Judy Levine
Liberty Heights Fresh
Herb Lichtenstein and Barbara E. Highlander Lichtenstein
Light Walk at Tracy Aviary
Amy Lin, MD
Edward G. Lind
Theresa Long, MD
Loveland Living Planet Aquarium
Janet M. Luke
Holly Lund
Kenneth M. Lund
David L. and Marilyn J. Maher
Myroslava Maksymtsiv
Peter Mandros
Collette Marthia
Peter F. Martin
Tawnja Stout Martin
Dustin Matinkhah
Kurt Matzen
Willard Z. Maughan, MD, and Rona Lee W. Maughan, PhD
Therese M. Mayes
John McClain
Robert A. and LeeAnne McConnell
Lori L. McCoy
Marcie and Wade McEntire
Philip and Susan L. McLaughlin
Michael McNamara
Juan E. and Esther R. Medina
Marvin A. and Renee B. Melville
Lloyd R. and Marjorie R. Merrill
Sheri and David A. Meyer, OD
Suzanne H. Mihalopoulos
Ann Marguerite and Kenneth G. Miller
Frances J. Miller Fund
Larry H. Miller Megaplex Theatres
Loretta Miller
Betsy J. Minden
Kerry C. and David B. Miner, MD
MINI of Murray
Minky Couture
Risa Moffitt
Mubarik Mohamad, MD
Momentum Indoor Climbing Gym
Sean Mooney
Casey E., Daysha, and Elle Moore
Moran Eye Center Optical Shop
Moran Eye Center’s Leadership Team
Edward B. Moreton
Mary and Tony W. Morgan, MD
Paula F. and Michael V. Morris
Gary and Lisa Mulcock
Derek and Gina A. Murdock
Maral Namdari
Natural History Museum of Utah
Kent O. and Deanna Naylor
Ron and Anna M. Naylor
Gary W. and Roslyn S. Nelson
Julie Kristl and Richard E. Nelson
Jeanette Nice
Deanna Nielsen
Teresa Nielsen
Brent T. Nilsen
Vincent and Elizabeth Novack
Jim and Sandra C. O’Hearn
Mark and Robin O’Rourke
Joan J. Odd
Aaron Oliver
Erica Oliver and Kylie Wack
Stephen L. and Barbara F. Olsen
Anthony P. and Millie A. Olson
Emily E. and Patrick R. Olson, MD
Julie and Jeffery E. Olson, PhD
Lisa M. Ord, PhD
Orvis
Erma J. Oten
Lacy Page
Brent Palfreyman
Ian and Tammi Parish
Park City Culinary Institute
Anne J. and Dennis L. Parker, PhD
Wells S. and Jennifer L. Parker
Sangita Patel
Aurelia L. and Jordan C. Pederson, PhD
Madison Perchik
Ronald J. Petersen
Bessie M. Peterson
Elaine Peterson
Lynn and Gary G. Peterson, PhD
Nedra A. Peterson
Wade Peterson
Jax Hayes and Kathryn H. Pettey
PETZL USA
Tamara Phillips
Warren S. Phillips
The Pie Pizzeria
Lyddia and Robert D. Pierce
Virginia N. Pinder
Pintura Fine Art Imaging and Framing
Roy W. and Elizabeth E. Simmons
Pioneer Memorial Theatre
Howard and Sharon Poch
Ashley Polski, MD
Donald R. and Joyce M. Polster
Lillian Pontacolone
Mike and Deborah A. Poor
Brett Prettyman
Charlotte and Patrick H. Price
John and Marcia P. Price Family Foundation
Kandace O. and Keith A. Prisbrey, PhD
Scott E. and Karin U. Pynes
Diana L. Ramirez
Thomas U. and Karma Ramsey
V. Raman and Elizabeth D. Rao
Red Butte Garden and Arboretum
Nishika Reddy, MD
Jerry B. and Barbara G. Reese
Jeffery A. and Heidi G. Reid
Ronald L. Rencher
Burt T. Richards
Jo Richardson
Helene H. Richer
Merrill K. and CoDele C. Ridd
Debra J. Rodriguez
Janie L. Rogers
Tonya Rogers
Lorena and Thomas D. Rosenberg, MD
Francis X. and Georgina Rossbach
Duane and Judy D. Rupp
Alene M. Russon
RX Sight
Patricia Sanchez
Joseph and Ann S. Sasich
Lara M. Schenk
Steve Schmidt
Susan B. Schulman
Jeff Scott
Kellie and Weston Seiler
Duane and Christine C. Seppi
David K. and Patricia L. Sias
Sherman Simmons
Susan M. Skankey
Vicki A. Slotte
Richard and Jenny M. Smartt
Gerald C. and Stacey F. Smith
Rosanne Smith
Gay Snider
Still SLC, Julie Nielsen, DNP, FNP-C
David and Londa Stout
Weston P. Stringham
Cathleen Stutzman
Dean G. and Cathleen M. Stutzman
Sundance Catalog
Edward S. and Lu Matheson Sweeney
Carlyn S. Sweet
Thomas C. and Marsha Swegle
Jean Tabin, MD
Temple Grounds Coffee Company
Laura Thomas
Sally B.L. Thompson, MD
Toni Thompson
Ning Tian, PhD, and Ping Wang
Timmy Grips, Tim Johnson
Torrent Cycle
Sylvia D. Torti, PhD
Tracy Aviary
Stephen Trimble and Joanne C. Slotnik
Alice M. Tsosie
V. Randall and Susan F. Turpin
Stephen and Ingrid Tyler
University of Utah College of Pharmacy
Utah Museum of Fine Arts
Utah Olympic Park
Utah Symphony | Utah Opera
Utah Division of Wildlife
Utah Trout Unlimited
Utah’s Hogle Zoo
V Chocolates
L. Craig and Margaret B. Vernon
Theresa Vonier
Laurene Walker
Verdon R. and Laurene S. Walker
Cynthia A. and Gary W. Wallace, MD
Kelsey Warburton
Garda L. Wardle
Wallace J. and Maysie E. Watts
Charles H. Weber, MD, and Lana S. Weber, MD
Elaine B. Weis
Liliana Werner, MD, PhD
Western Rivers Flyfisher
Lisa Weston
Bart L. Wheelwright
David C. and Gloria H. Whipp
Abby Whiting
John D. and Diane B. Whittaker
Steven D. and Deidre Whittaker
Coach Kyle Whittingham
Pauline Wiessner, PhD
Janet C. and H. James Williams, MD
Stephen P. and Nancy Z. Williams
Willow Creek Country Club
David J. Wilson
Barbara M. Wirostko, MD, and Joseph Morelli, MD
Albert Woodmansee
Hope H. Worner
Phillip A. and Judy V. Yeates
Louise M. and Norm A. Zabriskie, MD
Vera S. Zaccardi
David R. and Susan Zangrilli
IN HONOR OF
Those in whose honor gifts were made to the Moran Eye Center from January 1, 2023- December 31, 2023.
JoAnne Ambrose
David R. Bachman
Karen S. Bachman
Heidi Bailiff
Paul S. Bernstein, MD, PhD
Colleen H. Bowman
Doreen Bromfield
Craig J. Chaya, MD
Ben S. Chortkoff, MD
Susan Chortkoff, MD
Caroline M. Craven, MD
Joseph D’Agnillo
Kathleen B. Digre, MD
David Dries, MD
External Relations Team at the John A. Moran Eye Center
Christine Fairclough
Monika Fleckenstein, MD
Jason Groce
Eric Hansen, MD
Rachael Jacoby, MD
Griffin Jardine, MD
Gracie Jones
Robert C. Kersten, MD, FACS, FASOPRS
Marissa Larochelle, MD
Amy Lin, MD
Lions Club Member #182189 Park City Lions
Kay Winston Lipman
Lindsey Fairclough Little
Maureen K. Lundergan, MD
Nick Mamalis, MD
David Meyer, OD, FAAO
Mark D. Mifflin, MD
Kathie Miller
Majid Moshirfar, MD
My 3rd Transplant
Austin Nakatsuka, MD
Randall J Olson, MD
Our 48th Wedding Anniversary
Bhupendra Patel, MD
Dix H. Pettey, OD, MS, Best of State!
Jeff Pettey, MD, MBA
Ashley Polski, MD
Heidi G. Reid
Rachelle Rupp
Akbar Shakoor, MD
Rachel G. Simpson, MD
St. George Lions Club
Brian C. Stagg, MD
Mano Swartz, MD
Norm Zabriskie, MD
Brian E. Zaugg, MD
IN MEMORY OF
Those in whose memory gifts were made to the Moran Eye Center from January 1, 2023-December 31, 2023.
Martha S. Ahrens
Lynn Arent
Marvin L. Arent
Thomas Arquette
Barnie P. Babbitt
Elizabeth Beck-Thomason
Rourke H. Bowman
William J. Buhl
Lyman Buhler
Neal P. Busk
Carol A. Butterfield
F. Burton Cassity
Bianca Coppa
Ruth H. Craig
Alan S. Crandall, MD
Donald C. Crawford
Margaret Crawford
Yuriko Dennison
Edmund W. Dumke
Elwin J. Duston
Joseph K. Everton
Bruce Robert Fishburn
J. R. Fisher
Susan Bracken Ford
William Arthur Francis
Suzanne F. Goldsmith
Larry Dean Hale
Jamie
Yoshie Kondo Kishimoto
WM. M. Kleinschmidt
Hazel Lohman
Jack Lohman
Jo Ann Miller Mahoney Butler
Margaret W. Martinez
Paul R. Martinez
Helen Torgerson Mehrens
Gerald E. Millard
Jean Holt Miller
John A. Moran
Katherine Tingey Morton
J. Bill Moschetti
Steven J. Nichols
Jerry S. Nielsen
Marilyn Noorda
Darcy Rollins-Peterson
Darlene M. Phillips
Maurine Pixton
Randall “Randy” Smith Taylor
Richard J. Tillery
Richard Dean Tomlin
Richard M. Walker
William A. Worner
Paul J. Zabolotney
PLANNED GIFTS
Those who have planned gifts in place to the Moran Eye Center as of December 31, 2023.
Anonymous
Joanne Ambrose
Neal R. Anderson
David R. and Karen S. Bachman
Bonnie Barry
Joseph E. Bernolfo
Elmen D. Bloedel
Toni F. Bloomberg
Irene G. Casper and Ruth A. Morey
Donald A. Cathcart
Richard and Susan Coe
Thomas D. and Candace C. Dee
Carol M. Fay
Daniel G. Forman, CVM
Elaine T. and Frank W. Fox, PhD
Bernard I Grosser, MD, and
Karen J. McArthur
Cliff Hammer
Joseph L. Hatch, MD
Jerry S. and Claudia F. Howells
Curtis C. and Lynne P. Kennedy
Tim and Wendy A. Lacy
Charles H. McLeskey, MD, and Nanci S. McLeskey, DPN
John A. Moran*
Ruth and Randall J Olson, MD
Sylvia Prahl-Brodbeck*
Linda Stauss Rankin, PhD
Don B. Reddish*
Ken and Holly Reynolds
Janet M. Schaap
Edward H. Skinner
Daniel Soulia
Sharon Steele-McGee
Susan O. Taylor
Alice G. Telford
Mary E. Thompson
Haru Toimoto
The Moran Eye Center is grateful for the contributions made to support our mission and goals. We have made every effort to ensure that this January 1, 2023-December 31, 2023, Donor Report is as accurate as possible. Should you find an error or wish to change your listing, please contact us at 801-585-9700.
*Deceased

2023-2024
Best Hospitals for Ophthalmology No. 10 Nationwide 2023

Residency Education No. 6 Nationwide No. 1 in the West
The John A. Moran Eye Center at the University of Utah is the largest ophthalmology clinical care and research facility in the Mountain West, with more than 60 faculty members, 10 satellite clinics, and 20 research laboratories and centers.
Physicians provide comprehensive care in all ophthalmic subspecialties, making Moran a major referral center for complex cases. Services include:
Cataracts
Cornea & External Eye Disease
Electrophysiology
Emergency Care
Glaucoma
LASIK and Vision Correction
Surgery
Neuro-Ophthalmology
Oculoplastic and Facial
Plastic Surgery
Ocular Oncology
Optometry
Patient Support Program for Patients with Vision Loss
Pediatric Ophthalmology
Pediatric Retina
Retinal Diseases
Strabismus
Ultrasound
Uveitis




















