
4 minute read
Building a Successful Healthcare System Infrastructure
In planning for healthcare Rahman A. Parker systems in urban areas public Program Deployment health and private healthcare SME providers are addressing Booz Allen Hamilton a growing heterogenous demographic, multiplicity of languages, cultural practices, and ingrained health attitudes and practices. These challenges are then complicated by uncertainty driven by the politics of government support and subsidization of the system. Planning for urban healthcare systems is then much more than simply property acquisition, project planning and management, and a quick transition to operations and maintenance. Any plan will have to consider that patients in the urban environment must be considered up front as stakeholders in every aspect of the planning cycle. Urban healthcare systems must plan beyond the curative cycle and include institutional outreach that encourage patient-stakeholders to become active in their own wellness.
Urban health systems must respond to rapid demographic, social and disease transition while also contending with a plurality of providers and a need to stimulate a multisectoral response to address the wider determinants of health.
Rapid urbanization presents challenges to traditional conceptualization of health systems. Conceptualization of urban health system must consider multisector responses, engagement with a plurality of providers, the role of local governments and engagement of urban residents, particularly the poor. Data and evidence, and technological advances in e-health, can provide the glue to hold together this complex urban health system. (Elsey, Agyegong, Hugue, et. al., 2019) Functional healthcare systems are built on the basic principle of service. The golden rule. We are a nation of laborers, innovators, and optimistic entrepreneurs. Our spirit of ingenuity is one of the distinct features that help us reach patient care goals. With that in mind, it is important to examine the effects of a healthcare system on an urban population. Well planned, implemented and managed urban healthcare systems have community appeal. Systems built to service the whole person, oriented towards cultural and social sensitivity provides
urban communities with a 360-degree health and wellness impact. Comprehensive healthcare systems not only guarantee access to affordable healthcare they so desperately need, urban, fullscope healthcare by their very nature educate communities as to the importance of health maintenance and wellness habits.
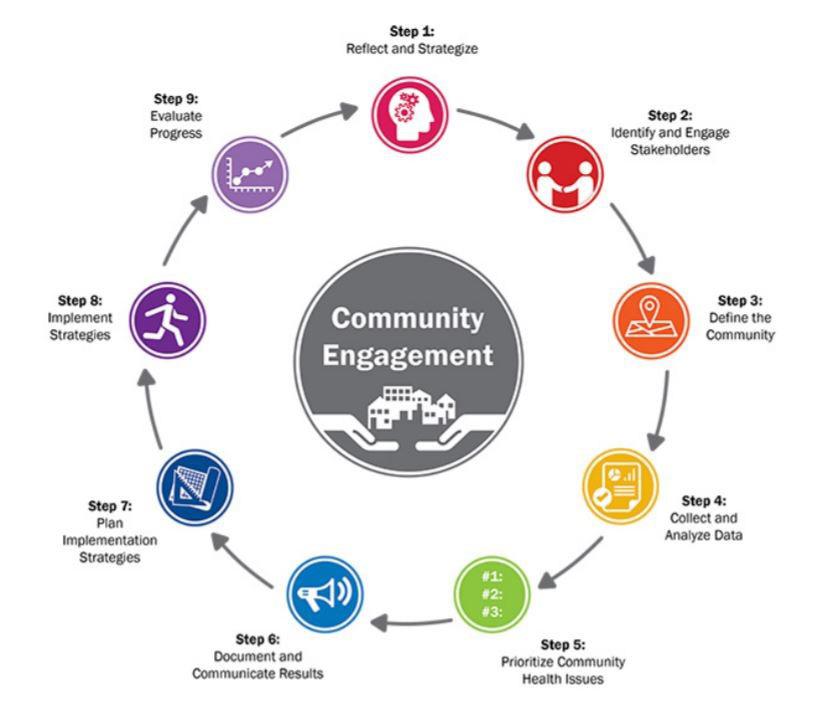
Following a 360-degree methodology and including community concern and input the University of Maryland Medical Center conducted a healthcare assessment centered on city of Baltimore. “To complete a comprehensive assessment of the needs of the community, the Association for Community Health Improvement’s (ACHI) 9-step Community Health Assessment Process was utilized as an organizing methodology. The UMMC Community Health Improvement Team (CHI Team) served as the lead team to conduct the Community Health Needs Assessment (CHNA) with input from other University of Maryland Medical System Baltimore City-based hospitals, community leaders, the academic community, the public, health experts, and the Baltimore City Health Department.” (UMMC, 2018) UMMC used a 9-step process (see Figure 1) to complete the community needs assessment. In 2018 UMMC and for the first time all of the hospitals and healthcare centers in Baltimore collaborated in key data collection strategies to complete a joint community needs assessment. (UMMC, 2018)
The Next Step – Infrastructure and Services Maintenance
More often than not urban institutions falter once transitioned to operations and maintenance and suffer from infrastructure “slippage”. Slippage, for the purpose of this proposal, is defined as an unplanned gap in services causing deviation from complete health coverage. We are wise to examine the infrastructure “slippage” found in other Urban Healthcare Systems worldwide; such as the systems in Ghana, and Canada’s Health System (Health Canada); to help understand how to design a proper community-based care system that can heal an urban area.
One method that will address the issue of slippage with focusing on smaller patient populations and customizing unique healthcare plans and programs to those in need with a four-phase (logic model) approach to infrastructure development.
First: identify specific communities of patients and their diseases. With this approach, those affected by diabetes can go to diabetes clinics specialized to deliver quality care with health education focused on prevention and maintenance of a balanced food diet. Second: build the healthcare clinics. The clinics can be built to provide specific levels of customized care for identified patients and their diseases. Each clinic will address the unique healthcare needs of the community. Third: staff the healthcare clinic infrastructure with a mix of paid and volunteer physicians, nurses and allied health services employees with a Direct Employment Vehicle (DEV) to cycle in prospective employees. Healthcare Systems designers should partner in institutions to ensure their graduates receive employment after receiving degrees or licensures.
Fourth: replicate these clinics to the identified populations. These clinics can be managed by a Healthcare Systems Infrastructure team or company like the teams I have created at local, state, and federal government levels. This type of quality care delivery to an infrastructure with inherent slippage can help reduce general service/treatment waiting times that come with an inherently unorganized Healthcare System. I believe that with strategic partnerships and great focus on quality care and proper infrastructure development, we can place a fundamentally sound healthcare system in our Urban areas and create a method of healthcare delivery to show as a first rate example for global public healthcare.
References:
Rethinking health systems in the context of urbanization: challenges from four rapidly urbanizing low-income and middle-income countries, 2019)
Community Health Needs Assessment & Implementation Plan, Executive Summary FY2019-FY2021, 201










