











When I think about Michigan State University Public Health, three words come to mind; community, collaboration, and change. All our research, teaching, interventions, and health delivery engage our communities as crucial partners. This collaboration allows for improved health outcomes and sustainable change in the communities we serve.
Emphasizing the reduction of health disparities and promoting health equity solutions, faculty have been awarded over $115 million in externally sponsored grants. Funding success is the direct result of a strong relationship among community advocates.

CEPH ACCREDITED EDUCATION: We are educating the next generation of public health professionals. Over the past 14 years, our online Master of Public Health (MPH) and Graduate Certificate program has educated more than 700 Spartan alumni working in meaningful careers.

In 2022, our application for accreditation to the Council on Education for Public Health was approved. Thanks to our community partners, alumni, students, faculty, and staff that have been involved in our accreditation journey. We could not have gotten this far without your input.
In Spartan Spirit, Wayne R. McCullough, PhD Michigan State University Interim Division of Public Health Director Master of Public Health Director





MSU is advancing the public’s health through practice-infused instruction, research, and community partnerships that promote the attainment of health equity for all citizens.
“...the MPH is one of the first online programs in the country, and the degree continues to provide opportunity to people in the state and around the country,” said Aron Sousa, MD, dean, College of Human Medicine.




Like the Master of Public Health (MPH), this certificate is completely online. Gain competence in all of the core disciplines of public health for a fraction of the cost and time commitment.

This certificate is designed to provide students with a basis for understanding the breadth and scope of public health.
The core courses are also required of students who are pursuing a Master of Public Health degree. If you decide to pursue an MPH, credits from the Graduate Certificate do apply.
Core


Kendra works for Trinity Health IHA Medical Group as a Clinical Support Assistant where she supports patients daily. As the COVID-19 pandemic disproportionately impacted Black Americans and shed a light on the importance of public health, Kendra knew she had to act. Her commitment to creating lasting change in society led her to pursue her Master of Public Health degree. READ MORE

“Being an MSU Spartan means making an impact.
To hold the Spartan name, I realize it means that I am paying it forward.” Kendra Shannon, Student Advisory Board



“I strive to endorse my leadership skills to promote health among the Hispanic/Latinx community. As an individual of Mexican-American background, I want to create great opportunities within my community.”
Viviana Quintino-Zavala, MPH Student
Viviana Quintino-Zavala works as a Nurse Technician at Trinity Health Saint Mary’s Hospital in Grand Rapids, Michigan, working in inpatient services. She recently completed her practicum experience at the Kent County Health Department, where she worked closely with the Hispanic/Latinx community on a community-based participatory research project. Her desire to promote health equity in underserved communities inspired her to pursue a career in public health.
STUDENT VIEW

Donovan Dennis is a dual enrolled medical student at Michigan State pursuing his MD and MPH simultaneously. Studying public health reinforced his decision to apply for medical school in hopes of becoming a physician. Inspired by the work of advocates and public health professionals in Flint during the water crisis, he sought out MSU’s unique MD and MPH programs. Connecting with community members and fellow students and professors fuels his motivation for becoming a future doctor.


“To me, public health naturally compliments medicine. As such, public health, prevention and equity will be the lens through which I study and apply medicine to my daily practice.”
Donovan Dennis, MPH Student
“Applied research has always been my passion. One focus of my work is zoonotic infections—infections that can be transmitted from animals to humans. There are nearly 70 million dogs and more than 150 million cats in the U.S., two companion animals that can easily continue transmission of zoonotic infections. We can’t control something like this without studying it. Only then can we interfere and break the cycle.”



 Darline K. El Reda, MPH Interim Associate Director
Darline K. El Reda, MPH Interim Associate Director
The cost of health care in the United States continues to increase year over year, and most recent figures estimate that the total cost of health care (public and private expenditures) as a percent of our gross domestic product (GDP) is approximately 17%.
The U.S. is the highest in the World in terms of GDP spending on healthcare, but this spending has not correlated with a higher ranking in health quality or outcomes. For example, based on findings from the most recent, Global Burden of Disease Study, the US has poorer rates of “amenable mortality,” as measured by the Healthcare Access Quality (HAQ) Index. Amenable mortality is a measure of the rates of deaths considered preventable by “timely and effective care.” The US ranks last among comparable countries on the HAQ index, with a score of 88.7.
“This means that our healthcare delivery system should be actively focused on doing the right things, for all the right patients, at the right time, in order to achieve optimal population health.”


 Robert Wahl, Assistant Professor
Robert Wahl, Assistant Professor
Air pollutant exposures are associated with adverse birth outcomes and worsening symptoms of asthma, heart disease, and other chronic diseases.
Detroit air quality improved steadily over the last 20 years. However, American Lung Association ranked Detroit in the top five percent of all the cities they measured in annual particle matter (PM) pollution, so there is more work to do. Southwest Detroit suffers from higher levels of air pollution, and this pollution affects the entire city. Sources include a heavy concentration of vehicles, an oil refinery, a steel mill, a wastewater treatment plant, two power plants (one coalfired, one gas-fired), three heavily-trafficked highways, and a six-lane bridge to Canada.
How can Michiganders track local forecasted air quality? Robert Wahl explains how.



“I’m all about connections, community and systems—how we interact with the world and how it affects us. I became a huge advocate and champion for public health.”

“Being comfortable in the uncomfortable is a key takeaway... This lesson has guided me throughout the pandemic and served me throughout my public health career.”
Holly Campbell Spartan in Public Health, 2011
“It allowed me to enjoy the journey, to absorb more of what I was learning. I was able to create an independent study to meet my unique learning needs.”
Noel Pingatore Spartan in Public Health, 2020
“I want to help make lasting change to help individuals and communities overcome some of those barriers that are in place—or even break them down entirely.”

“I really want to encourage people to consider more interdisciplinary approaches, and I think the public health piece complements so many different areas of study.”

Rebecca Stone Spartan in Public Health, 2012

Bryan O. Buckley Spartan in Public Health, 2012
Tamara Jordan Spartan in Public Health, 2021

“I went into the job hunt with a very diverse set of experiences and skills. MSU’s MPH program provides opportunities for you to research new topics, develop new skills, and explore the day-to-day of other career paths.”


“Take advantage of MSU’s network of connections. That’s something that the MSU MPH program does really well - anything you need help with, there’s a person within the network that can help you.”
“Nothing can compare to the convenience of having an online curriculum while also receiving high-quality public health education. I was able to continue my work in Central and South America, all while completing my MPH at MSU.”


“There are so many directions one can go in public health. If you are interested in pursuing public health, seek out local coalitions in your area and get involved.”
“What drew me to pursue public health was its focus on prevention—through monitoring, preparing, and promotion.”
Dr. Esch is the inaugural Pediatric Public Health Initiative inaugural Alice Hamilton Scholar. Her research interests include medical education, early adversity prevention, and maternal infant health, all with the lens of health equity. She has received national and local grant funding to support programs and research relating to these interests. Dr. Esch is collaboratively working to establish a multidisciplinary pediatric prenatal clinic at Hurley Children’s clinic, to decrease maternal infant health disparities. Dr. Esch has a strong interest in advocacy and policy. She is a board member of the Michigan Chapter of the American Academy of Pediatrics, a member of the Governmental Affairs and Advocacy committee, and a co-founder of the Health Equity Workgroup. Additionally, she has an interest in writing and advocacy, with two published opinion pieces, one on gun violence prevention and the other on COVID-19 vaccination for children.


Dr. Tayler is the second Pediatric Public Health Initiative Alice Hamilton Scholar. Her research interests include asthma management, tobacco and vaping, health literacy, gender affirming care, improving access to sexual health care, and substance abuse treatment. She is interested in medical education and the cross section between improved resiliency and wellness particularly during residency and how this affects patient outcomes. Dr. Tayler has experience in advocacy and legislative policy work while living in New York which she hopes to extend in Michigan. Her previous work pertained to removing the religious exemption for vaccines for NY public schools, banning of flavored tobacco product sales to those under the age of 21, and improvements transparency of public policy during the COVID19 pandemic. She is a member of the Michigan Chapter of the American Academy of Pediatrics and a board member of the Governmental Affairs and Advocacy committee.
 Katlin Harwood-Schelb, BA
Katlin Harwood-Schelb, BA
Harwood-Schelb graduated woth a bachelor of arts in psychology and has a passion for creating healthy environments for individuals in underserved communities. She has been working toward making better learning surroundings for children during her experiences working in Genesee County elementary schools and as a research assistant in the Pediatric Public Health Initiative. Her research aspirations include the effects of Adverse Childhood Events on children’s mental health, the effectiveness of music therapy, and determining changes in discriminatory policies in resource allocation. “I plan to gain experience and knowledge to help many communities facing adversities.”

Patterson graduated with a bachelor of science in health sciences and has been working toward her goal of becoming an obstetrician and gynecologist. She plans to apply for the dual MPH/DO program at MSU. Patterson has volunteered for many Flint organizations including Carriage Town Ministries, YWCA of Greater Flint, and Boys and Girls Club. She recently finished a community garden project with Flint Urban Health and Safety Corps with the intent of lowering crime rates through environmental design. “I love the Flint community. I see a lot of creativity in the city, I see changemakers, and people that band together to make changes - and you can see the impact of your work in the community as well.


The Charles Stewart Mott Foundation has granted $25 million to expand the Michigan State University College of Human Medicine’s public health presence in Flint. The grant will create an endowed fund to increase public health faculty, academic research and community health collaborations.
“Expanding MSU’s public health program in Flint is a great thing for the community, and it also will yield important lessons for our state and nation as we struggle with both emergent and chronic health challenges,” said Ridgway White, president and CEO of the Mott Foundation. “MSU’s work in Flint is a wonderful example of what can happen when scientists, residents and community advocates work together to improve health.”
The new grant to MSU will build upon Mott’s initial support for the college’s presence in Flint. Between 2011 and 2013, Mott granted $12 million to MSU for the college’s expansion and relocation of its public health program from East Lansing to Flint, as well as $7.7 million to the Foundation for the Uptown Reinvestment Corporation to support renovation of the former Flint Journal building to house the program.
Pictured above: Dean Aron Sousa, Flint community health advocate E. Yvonne Lewis, Director Wayne McCullough. Pictured left: President and CEO of the Charles Stewart Mott Foundation, Ridgway White.



Emphasizing health disparities and health equity solutions, MSU faculty are leading community based public health research partnerships with the Flint community.
Research efforts focus on improving health in the areas of health disparities, chronic disease, and behavioral health.

From 2014 – 2022, public health researchers have been awarded over $115 million in externally sponsored grants for community research.
Funding success is the result of a strong relationship among community advocates. Partners in the community help fuel the efforts with resources and a shared commitment to improving lives.
Pictured: Bishop Bernadel Jefferson (above), a Flint community leader, and Wayne McCullough (far right), interim director, MSU Public Health.
The MSU Division of Public health was established in March 2015 with the support of the Flint community, Hurley Medical Center, McLaren Flint, Ascension Genesys Hospital, and the Charles Stewart Mott Foundation.

















Dr. Hanna-Attisha , C. S. Mott Endowed Professor of Public Health, is the founding director of the Pediatric Public Health Initiative, an innovative partnership of MSU and Hurley Children’s Hospital in Flint, Michigan. A pediatrician, scientist, activist and author, HannaAttisha was named one of Time magazine’s 100 Most Influential People in the World and recognized as one of USA Today’s Women of the Century for her role in uncovering the Flint water crisis and leading recovery efforts. She has testified multiple times before the U.S. Congress, lectures at dozens of colleges and universities, and frequently contributes to national media outlets championing the cause of children. An accomplished academic and an inspiring change maker, she is the author of the widely acclaimed and New York Times 100 most notable book, What the Eyes Don’t See: A Story of Crisis, Resistance, and Hope in an American City .






Dr. Saxe-Custack is a registered dietitian and serves as the Nutrition Director for the Pediatric Public Health Initiative, a joint effort between Michigan State University and Hurley Children’s Hospital, to address the impact of Flint’s lead exposure on children. Dr. Saxe-Custack is dedicated to the evaluation and expansion of nutrition programs for children and families living in Flint, with a particular focus on improving access to fresh foods. Her work examines the impact of an innovative fruit and vegetable prescription program for pediatric patients. She works with community partners on an experiential nutrition and cooking program for Flint children called Flint Kids Cook.


Flint Kids Cook is a free, healthy cooking program for youth cre ated by a team of registered dieticians, public health professionals and chefs. Grounded in social cognitive theory, Flint Kids Cook is designed to improve self-efficacy for healthy cooking through interactive nutrition and food preparation activities. Flint Families Cook is a 5-week virtual cooking class offered to the whole family.

Nearly 400 children have participated in Flint Kids Cook and Flint Families Cook



Similar to medical prescriptions, fresh fruit and vegetable prescriptions are ordered by pediatricians and given to patients ages 0 to 18 during office visits. Vendors treat prescriptions ($15 each) as vouchers that may redeemed for fresh produce.
+85,400 prescriptions for fresh fruits and vegetables have been distributed in Flint, MI
From practice to policy: U.S. Farm Bill national adoption of produce prescription program in 2018


Dr. Jones is a T-32 trained perinatal epidemiologist, faculty member in the Michigan State University Division of Public Health, and Director of the Flint Registry. With a career focused on applying epidemiologic methods to establish cohorts for evaluating racial disparities in health, she has over 20 years of experience on research teams centered on maternal and child health projects. Dr. Jones leads the dynamic Flint Registry staff in collaboration with broad community-based partners. As the Director of the Flint Registry, she strives to elevate the voices of the Flint community in the way that the Flint Registry is designed, implemented, and shared with others. A lifelong resident of Genesee County, she is inspired by the resiliency and spirit of the Flint community. With over 20,000 enrollees who have received over 30,000 referrals to health and development services, the Flint Registry is playing a critical role in Flint’s recovery from the water crisis.


The Flint Registry is a resource to see how the people of Flint are doing and provide support for those impacted by the water crisis. After completing a sur vey, individuals are referred to services that promote health and development such as education, health and nutrition programs. Support, especially for children, includes referral to Genesee Health System Neurodevelopment Center of Excellence – a new, no-cost child development assessment center.
The Flint Registry is modeled after other public health registries like the World Trade Center Disaster Registry. The Flint Registry is for anyone who was exposed to lead-contaminated water because they worked, lived, went to school, or daycare identified as an address on the Flint water system from April 25, 2014 – October 15, 2015, including children who were prenatally exposed. The Flint Registry is for all ages.


people enrolled
to services
Dr. O’Connell is a developmental-behavioral pediatrician practicing at Hurley Children’s Clinic in Flint, Michigan. She is a founding member of the Pediatric Public Health Initiative of Flint and committed to community-driven research. She has clinical expertise in the evaluation of the motor, cognitive, language, and social-emotional domains of development in children from infancy through adolescence, as well as the assessment and treatment of child behavioral problems.
Clinically, Dr. O’Connell works closely with the Genesee Health System

Center to identify children with autism and connect them with needed resources. Her autism-related research focuses on medical education and health
systems.

Dr. Shipp is a registered dietitian nutritionist. She is engaged in several research projects with the overarching goal of improving maternal and child health equity, specifically breastfeeding related disparities. Her research interests also spans diet and nutrition-related health disparities impacting vulnerable populations, food access and food choice in underserved areas, and community nutrition.
Dr. Shipp recently completed an NIH funded postdoctoral fellowship funded through Environmental Influences and Child Health Outcomes, ECHO program, 2020-2022. Under her supplement she received training at MSU, focused on perinatal epidemiology and design of intervention studies. She is passionate about reducing breastfeeding disparities, especially within the African American community.
Dr. Shipp served as the chair of the statewide breastfeeding coalition (2019-2022) and continues to serve as a board member with Michigan Breastfeeding Network to support breastfeeding families within Michigan.


Dr. Finegood is a developmental scientist whose research investigates how early life experience and psychological stress influence health and human development. His research is rooted in and intersects the science of child development and developmental psychology, health psychology, and public health and seeks to identify biopsychosocial factors that contribute to risk and resilience among young people exposed to social adversities and environmental stressors.
A primary focus of this work is to study connections between life experience and the development of biological systems that regulate mental and physical health processes – the broader goal of which is to better understand and address stress-related disparities in health that may begin in the early years of life. His work has been published in leading scientific journals and edited volumes.

Dr. Finegood recently completed a postdoctoral research fellowship at Northwestern University where his research was funded, in part, by the National Heart, Lung, and Blood Institute/National Institutes of Health.

Dr. Wahl is an environmental epidemiologist with research interests focusing on asthma surveillance, air pollutants’ effects on asthma and adverse birth outcomes, and the health effects of climate change. He is a Co-PI on a federal Housing and Urban Development grant looking at using portable air filtration devices to reduce indoor exposure to lead dust in contaminated homes. He has extensive experience in grant authoring and management, serving as the PI on four cooperative agreements funded by the Centers for Disease Control and Prevention and one funded by the Environmental Protection Agency. He previously managed the Chronic Disease Epidemiology and Surveillance and Program Evaluation Sections at the Michigan Department of Health and Human Services where he collaborated on a home-based environmental intervention and education program for families of children with asthma. He teaches in the MPH program where he introduces students to “real world” connections between research and policy implications. Courses taught include Epidemiology and Public Health and Study Design and Research Methods for Public Health Practice.

Bob Wahl, DVM Served as PI on six federal grants over 19 years with total funding of nearly $8M

Dr. Johnson is the first C. S. Mott Endowed Professor of Public Health at Michigan State University. She is a licensed clinical psychologist who conducts policy-relevant implementation and effectiveness trials of mental health and substance use interventions for vulnerable populations, including perinatal women and individuals involved in the criminal legal system. Her policy goals include reducing incarceration rates, better funding for community mental health, and increasing structural supports for maternal health equity (e.g., coverage of needed health services, a living wage, and affordable childcare). Dr. Johnson is committed to participatory research, leadership, and governance processes to promote equity, expand impact, empower the traditionally unempowered, and elevate their perspectives and contributions to solutions.



MSU, Henry Ford Health, Brown University to establish new center with $15M NIH grant
The new suicide prevention research center, also known as the National Center for Health and Justice Integration for Suicide Prevention, is an innovative program funded by a $15 million grant from the National Institutes of Mental Health.

The goal is to build information bridges between health care organizations and criminal-legal systems to identify individuals at risk for suicide and connect them to care.
“One of the main problems in suicide prevention is finding people at risk for suicide who are not well-connected to health care. It turns out that many such individuals are in contact with the justice system, including police, courts and local jails. The challenge with connecting individuals in jail with community services is that it is resource-intensive and difficult to do at scale. Our approach solves both problems,” Johnson said.
READ MORE
+3000 individuals in pretrial jail detention provided with suicide assessment and triage
1st evidence-based suicide prevention intervention for the 10+ million individuals passing through pretrial jail detention each year
1st evidence-based treatment for major depression in any incarcerated population
and
Intervention for
(P50 MH127512)
(U01 MH106660)
prevention; R01 MH118680)
(R01 MH130948)
Multilevel Intervention for


(MIRACLE; R01 MD016003)
Mechanisms of Stepping

collaboration; R01 MH118680)

neonatal death; R01 HD110471)


Women’s

Dr. Hailemariam is a Mental Health Epidemiologist, a researcher and advocate for equitable mental health care globally. Her research interests include mental health care for underserved populations in low-resource settings including within high-income countries. Her research focuses on developing lay provider or peer provider-delivered mental health interventions to improve access to mental health services, improve functioning and reduce mental health symptoms. Her research is guided by understanding barriers to mental health care that are disproportionately experienced by underserved populations including perinatal women, rural residents, and justice-involved individuals in low-resource settings.

Developing peer-provider-delivered behavioral health interventions:
• Peer Navigation for Individuals with Serious Mental Illness Leaving Jail (R34 MH118402)
• MOSAIC (MOthers’ AdvocateS In the Community) for Perinatal Women with Experience of Intimate Partner Violence (R34 MH127061)
Both studies are currently recruiting.

Dr. McCoy White is an acacemic research specialist coordinating community-partnered anti-racism interventions. She supports Flint community members on Dr. Jennifer Johnson’s and Dr. Steve Ondersma’s teams. She works on the Maternal Health Multilevel Intervention for Racial Equity (MIRACLE) study, an NIH-funded multilevel intervention study on African American maternal morbidity and mortality in Genesee and Kent Counties.
Dr. McCoy White facilitates testing of vaccine promotion content in ongoing implementation contexts. She is developing a series of computer-delivered messages, videos, and micro-interventions designed to promote vaccination of pregnant patients for COVID-19, and newborn infants following CDC and AAP guidelines.

Using a community-level intervention expands access to and acceptability of enhanced prenatal and postnatal care services for African American women. This project raises awareness of potentially life-threatening warning signs during and after pregnancy.

Research to Reduce Disparities in Disease

Dr. McCullough is the interim Director of the Division of Public Health and Director of the Master Public Health Program. He is responsible for curricular changes and faculty hiring in response to the evolving public health environment. He led the successful application process for the Council on Education in Public Health accreditation. His research interests include:
• The identification and resolution of health and health delivery disparities for underserved populations
•
research findings into experienced community benefits
• How communications can help advance underserved communities and population health

Dr. McCullough is co-investigator on the Research to Reduce Disparities in Disease NIH grant, which trains students to conduct mentored research through their medical education. He conducts research on men’s health issues—especially those of Black men—centered on mental health, depression, diabetes, and cardiovascular diseases.

Dr. Ondersma is a clinical psychologist. His research is focused on the promotion of maternal and child health and healthy birth outcomes using high-reach technologydelivered brief interventions. His primary interest is in population-level interventions promoting maternal and child health in underserved communities, particularly via technology-based brief interventions promoting behavioral health and connection with services in the perinatal period. He co-chairs the Neonatal Opioid Withdrawal Syndrome subgroup of the NIH’s Environmental Influences on Child Health Outcomes initiative and has led multiple NIH and CDC studies focusing on the development, validation, and implementation of novel screening techniques and electronic/mobile (mHealth) interventions in healthcare settings. He is also the developer of the Computerized Intervention Authoring System, an NIH-funded, noncommercial research resource allowing the development of sophisticated digital interventions without coding.


The Appathon events brings commu nity partners, university teams, and video producers together to develop digital interventions to promote health equity.


Modeled after hackathons, these events involve separate teams coming together for a combination of hard work and fun over 2-3 days. On the final day a panel of judges—also drawn from the lo cal community—reviews each team’s work and declares a winner, with prizes all around. Importantly, the Appathons take advantage of unique software developed at MSU to allow anyone to develop sophisticated digital interventions without coding (see more at www.cias.app). This gives community members the ability to directly develop, edit, and customize app content.
Michigan State University hosted the first Appathon in 2022. This session focused on promoting COVID-19 vaccinations during pregnancy and led to two unique interventions. This first Appathon made it clear that this novel approach met a need in the community for the ability to directly produce technology to help meet health equity goals.
Future Appathons are already being planned and will follow the lead of community partners in topic selection.

Dr. Key is a classically trained Health Disparities Researcher. He is an expert in building equitable relationships between community and academic partners for health research and elevating community-identified health priorities to the research enterprise. Dr. Key utilizes Community-engaged Research (CEnR) approaches to research with a focus on marginalized populations across the lifespan. He has worked on national, regional, and local levels throughout his career to translate the resources of government, research partnerships, and foundations into practical support. He is Past Chair of the Community Based Public Health Caucus of the American Public Health Association. Dr. Key is the Founder of the Community Ethics Review Board, a component of the Community Based Organization Partners (CBOP) where community members conduct ethical reviews of proposed research projects to ensure that no harm is done on a community level and to assess mutu al benefit. Dr. Key is a 2016 Fellow of the Robert Wood Johnson Foundation Culture of Health Leaders Program and serves on the national landscape as a Health Equity Scholar. In 2020, he au thored a resolution Declaring Racism as a Public Health Crisis and has spearheaded initiatives locally and regionally, and nationally.



Presenting at the 150th APHA, 2022.
The Flint Public Health Youth Academy FPHYA is designed to provide early en gagement and career exploration for Flint area youth, with a specific focused on underrepresented minorities. Since 2019, FPHYA youth have conducted annual Health Messaging Campaigns (COVID-19, Mental Health, and Environmental Health) with the emphasis on designing health messages “for youth by youth”!
+2,000 have participated in the online virtual talk show, “A Youth Perspective” and the annual Youth Summer Camp

“For the past three decades we have not seen a significant decrease in health disparities. To continue to conduct traditional research as is, will not yield the reduction of health disparities across health indicators. It is time to equitably engage the communities we are trying to impact in the planning, design, and all phases of the research process.”
Dr. Lucas, C. S. Mott Endowed Professor of Public Health, is a social and health psychologist. His research considers the psychosocial causes of racial health disparities. He is mainly focused on stress and preventive health behavior pathways, such as cancer screening. His research especially considers psychological justice - the causes and resulting health and social consequences of perceiving injustice for individuals and communities. His research focuses on understanding stress reactivity responses to injustice to promoting better uptake of colorectal cancer screening. Dr. Lucas is also leading an NIH Serological Sciences Network for COVID-19 (SeroNet) funded project aimed at communicating effectively about the value of COVID-19 antibody testing and better understanding why COVID-19 causes a disproportionate number of African Americans to suffer severe cases and deaths.




In partnership with the Flint Com munity Based Organizations and Partners (CBOP), the research team produced video tutorials about the potential value of anti body testing in the fight against COVID-19. The study also collects saliva samples from willing study participants. In partnership with the Environmental Health, Microbi ology, and Immunology Lab (EHMIL) at Johns Hopkins University, saliva samples are then analyzed to measure the presence of SARSCoV-2 antibodies.


National Network for COVID and Adult Vaccine Equity (NNICE), a CDC-funded project to build the evidence base of effective interventions to improve vaccine access and uptake and reduce racial disparities in vaccination coverage for African Americans and Latino adults. The NNICE partners with eight organizations across Michigan, Maryland, Illinois, and North Carolina to support a total of 48 different projects. The project anticipates reaching over 195,000 individuals through eight promising intervention strategies to increase adult vaccination.





Her most recent project is the development of a Health Equity Report Card (HERC) for Flint and Genesee County. The HERC addresses a need for disaggregated health outcome and health disparity data that is accessible and understandable.
Additional research interests include the elimination of health disparities through community-engaged research, and normalizing data disaggregation to identify disparities.
Dr. Uphold is a previous Fellow with the NSF-funded Advancing Research Impact in Society initiative where her project focused on understanding researcher dissemination-as-usual. This work identified the barriers and facilitators that academic researchers face when sharing their research findings with non-academic audiences. It also fueled her interest in reducing the research-to-practice gap through audience-centered methods of message distribution.
Dissemination and implementation science could improve the use of evidence-based practices within community-based settings. However, there are preexisting barriers to effective dissemination which includes:

Bringing a local context to a global pandemic:
weeks of the Flint Community Webinar on Coronavirus +11,000 views live and +16,000 views on YouTube
Dr. Sadler is an urban geographer with expertise in environmental science, GIS, food systems planning, and land use policy in legacy cities. In 2018, he was awarded a Bloomberg Fellowship to study at the Johns Hopkins Bloomberg School of Public Health. His research interests include integrating urban planning and public health topics related to neighborhood/built environmental effects on health. Recently, this has revolved around uncovering elements of structural racism in the housing environment and determinants of urban development that exacerbate racial and socioeconomic inequality. Methodologically, Dr. Sadler combines spatial analysis and communitybased participatory research approaches to address challenges in the urban environment. Throughout his work, the overarching goal is to strengthen the understanding between the built environment and health behaviors/ outcomes with the objective of shaping land use policy to build healthier cities.

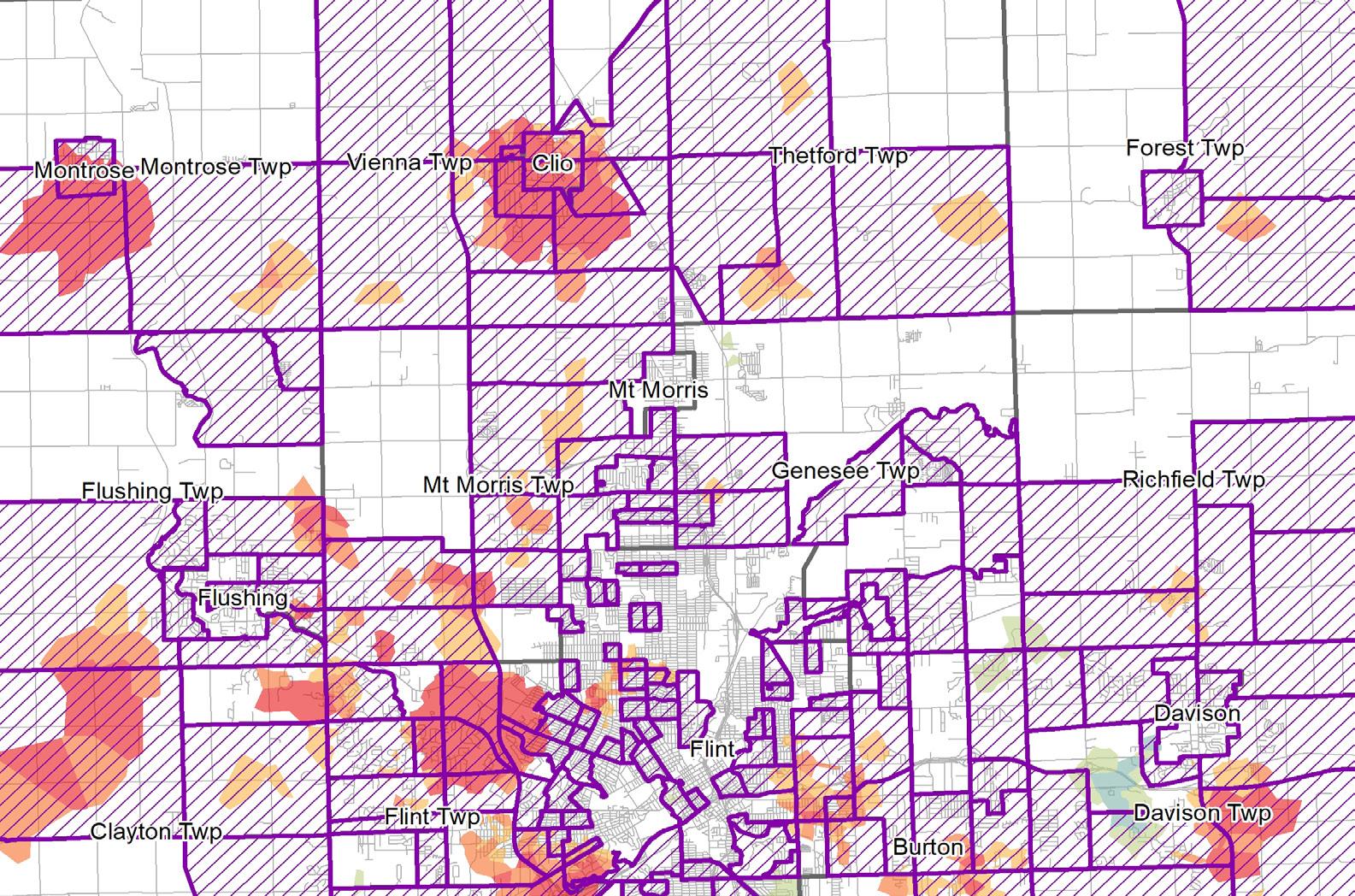

Dr. Sadler’s work is highly multidisciplinary. He collaborates with a range of psychologists, physicians, epidemiologists, biostatisticians, and geographers to explore linkages between health and the built environment. Dr. Sadler is always on the lookout for understudied linkages to the built environment—and any reason to make a map. Some of the topics he has worked to adress include local food systems, urban agriculture, access to healthy food, crime, urban disorder, blight elimination, residential segregation, and active travel.
Sprawl and fragmentation are correlated to economic stagnation and decline; driving poorer health outcomes
Urban decline is closely connected to poor mental health outcomes
“Urban planning approaches that recognize and address these underlying determinants are essential for building a more equitable society. Overlooking them created the conditions that caused the Flint Water Crisis, and this practice continues to exacerbate disadvantage for individuals— typically minoritized populations— who live in such communities.”
Dr. Smart is an epidemiologist and director of the College of Human Medicine Leadership in Medicine for the Underserved certificate program. She also serves the African Studies Center, the Institute for Global Health, and the Master of Public Health Program. She is co-director of the Research to Reduce Disparities in Disease (R2D2) program, an NIHfunded, clinical research training program. Dr. Smart has led and designed experiential education abroad programs in Uganda, South Africa, Belize, and the United States. She does alcohol policy evaluation and monitoring work in Uganda, providing the evidence needed to inform policy interventions, enforcement strategies, and campaigns for compliance uptake. She is co-investigator in the Methodology Core of the Flint Center for Health Equity Solutions. In 2020, she was named a Michigan Center for Urban African American Aging Research scientist.
+150 students and faculty participated in her global public health topics courses abroad
In 2022, despite the impact of COVID-19, Dr. Smart helped students design and complete public health and medical electives in Rwanda, Ghana, Eretria, Costa Rica, Belize, Malawi, and Nigeria


Dr. Clements is a quantitative sociologist by training with an additional specialization in environmental science and policy. He has worked in the fields of environmental chemistry, environmental project management and engineering, grant writing and management, and undergraduate and graduate medical education. His recent research focuses on health outcomes and disparities in people with diabetes and multiple chronic conditions. He is currently working to shed light on how COVID-19 influenced the course of disease for people with diabetes, focusing on disparities in outcomes that are related to race and combinations of chronic disease, as well as how rural experiences shape disease progression and access to care. He is also interested in how political and religious ideology inform attitudes about science, and while some of his early work focused on environmental issues, he is expanding this to explore how these ideologies affect attitudes about health care, and medical science. He regularly teaches the following courses in the MPH program: HM 802 (Introduction to Biostatistics), HM 807 (Practical Application and Critical Thinking Synthesis in Public Health), and HM 878 (Applied Biostatistics).


Dr. Shah (Champine) is an applied developmental psychologist who partners with communities in designing, implementing, and evaluating programs for children and families exposed to potentially traumatic events. She conducts this research in collaboration with colleagues from the Yale School of Medicine and the Child Health and Development Institute of Connecticut. She assisted in evaluating the Pottstown Trauma-Informed Community Connection, a community-led initiative that aimed to improve recognition of, and response to, signs of childhood trauma among diverse stakeholders. Dr. Shah’s overall goals are to use theory-predicated and community-engaged research to inform programs, policies, and practices that promote thriving. In addition to teaching HM 805 (Social and Behavioral Aspects of Public Health) and HM 853 (Public Health Program and Intervention Evaluation) in the MPH program, Dr. Shah is the lead facilitator of a free, external-facing course “Promoting Public Health in Michigan in the Face of COVID-19,” which aims to strengthen the MPH program’s ties to local communities and enhance understanding of public health and why it is important in the fight against the pandemic and beyond.




The Michigan State University Division of Public Health is excited to announce posting new faculty positions at its campus in Flint, Michigan. Over the coming years, we’ll be hiring up to 18 new faculty at all levels, made possible, in part, from a $25 million grant from the Charles Stewart Mott Foundation. We seek to immediately start receiving applications at careers.msu.edu, job number 814157. Come see us at the APHA annual conference in Boston at booth #1325. Learn more about pursuing your public health passions on a highly successful research and instructional team. Emphasizing health disparities and health equity solutions, MSU faculty have been awarded over $115 million in externally sponsored grants for community research. Funding success is the result of a strong relationship among community advocates. Partners in the community help fuel the efforts with resources and a shared commit ment to improving lives.
View open positions at careers.msu.edu.











