5 minute read
BREAKING RULES, SAVES TIME!
Improved Patient Safety and Experience
In Mental Health settings everyday items, such as phone chargers, can be used as a risk item for self harm or harm of others and can result in blanket restrictions. More rules impact on staff time, with less therapeutic activities which leads to reduced patient engagement and safety. Blanket restrictions and rules imposed upon patients can lead to frustrations and agitation and can escalate to incidents of restrictive practice such as increased medication, physical restraint and/or the use of seclusion.
Advertisement






The mission was to focus on allowing patients to have their phone chargers once risk assessed as safe to do so. Our project aimed to reduce blanket rules by 10% which would lead to a less restrictive, safe and kind environment for the benefit of all and the recovery of the patients.
By allowing patients to have their phone chargers in their rooms, once risk assessed, we have saved on average 404 hours (over 9 months) which equates to 808 x 30 minute interventions with patients. The ward has seen a reduction in complaints directed at night time restrictions due to the implementation of ‘mutual expectations’ overnight and an evening reflection group. The Patient Safety Climate Survey was repeated and has shown improvements in quality of interactions and sense of safety for the patients. There has been a 20% increase in patient’s confidence in staff to deal with difficult situations on the ward and a 25% increase in patients feeling involved in the planning of their care.
45 Minutes Per Shift Charging Devices
PATIENT SAFETY CLIMATE SURVEY results comparison and quotes

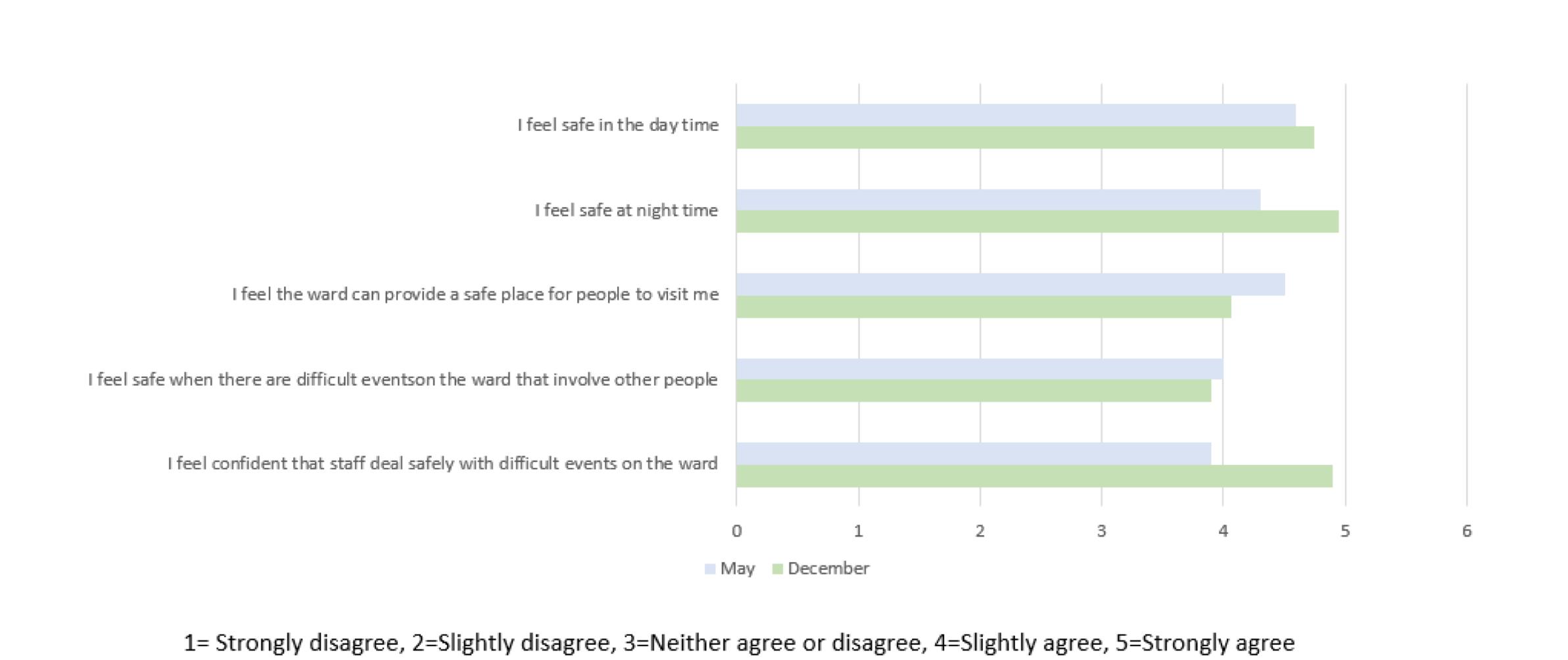
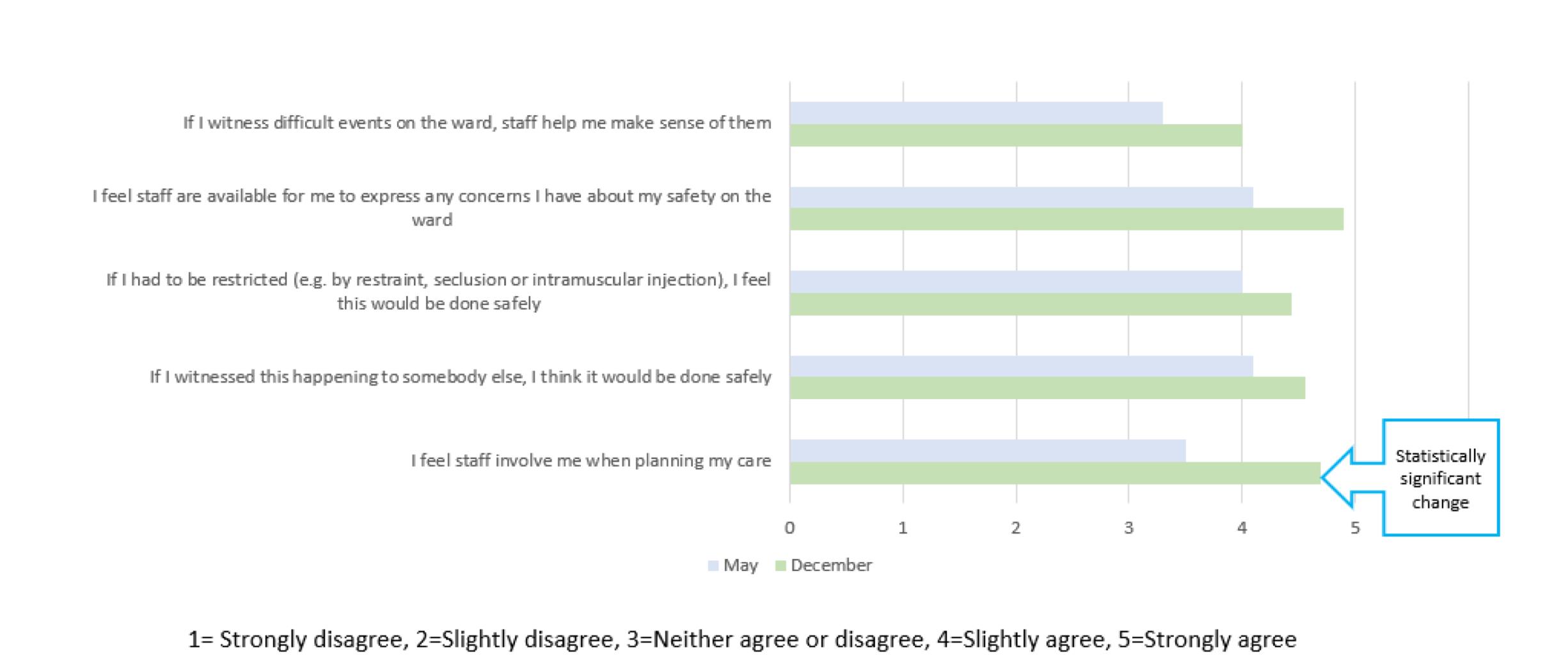
Patient Safety Climate Survey from Royal College of Psychiatry* completed by peer worker with 10 patients, and results shared with the team which led to rich, open conversation about restrictive practice on the ward.
Quality Improvement observation of staff activity was used to define the time taken on tasks related to blanket rules. Review of these tasks undertaken, and the benefit reviewed and solutions found. New practices implemented and restrictions reviewed. This has then been repeated after 6 months and results reviewed again. Changes discussed in both team meetings and ward workshops with lived experience workers involvement. Also in daily morning meetings and weekly community meetings with current patients on the ward.
Individualised risk assessments to allow patients to have their chargers
Over 9 months 404 hours saved which is
808 Therapeutic Interventions

Underpinning this project, we have worked strenuously to forge relationships and a sense of shared community between our ward staff and our service users, applying a model known as ‘Safewards’.


“My stay overall was excellent… The staff were awesome. I was never bored at any point and I believe my stay on the ward was hugely beneficial. Thanks to all the staff for their professionalism and caring nature”.
* rrp-safety-climate-survey.pdf (rcpsych.ac.uk)
We have been working as part of a national programme to look at reducing restrictive practice in mental health settings and the results of our work are being shared nationally.


By Aiknaath Jain, Heather Lund, Constantinos Parisinos, Hanna Milan
ARE PATIENTS BEING CONSENTED PROPERLY FOR ESWL? HOW CAN WE IMPROVE THE ESWL CONSENTING PROCESS?
This Audit was triggered after over 70% of patients undergoing a new highly beneficial, but risky, procedure felt t hey were not fully informed of the procedure prior to it occurring.
In one instance, someone was admitted to hospital, sedated, placed on the procedure table and withdrew.
Informed consent as a fundamental component of the medical treatment process and forms an essential aspect of one of the core pillars of medical ethics : Autonomy Indeed, the GMC writes : ‘Consent is a fundamental legal and ethical principle … Serious harm can result if patients are not listened to, or if they are not given the information they need - and time and support to understand it
To understand, evaluate and improve the consent process patients undertake before undergoing Extracorporeal shock wave lithotripsy for pancreatic duct stones.
ESWL for pancreatic stones
ESWL is a novel form of medical therapy where high energy shockwaves are delivered to the patient's abdomen to break-up pancreatic stones The procedure carries risks of pancreatitis, significant pain, pancreatic hematoma and internal organ injury
Method
We interviewed all the individuals who underwent ESWL at a major London hospital prior to their procedure in a 3-month period (n=7). We then fed this back to the medical team, adapted the consenting process in clinics and created a patient information leaflet that is being ratified and disseminated. We then garnered further survey feedback from previous patients and new patients undertaking the procedure (n=12).
Pre-intervention
100% of the patients felt as if the consenting process could be improved. The majority felt as if they did not have enough information, time or space to make an informed decision about undertaking ESWL prior to the procedure. 40% felt as if they would have not undertaken the procedure had they known the potential risks. 3 Interventions were generated
Pre-procedure telephone call explaining the procedure to the patient.
Pre-procedure clinic space to discuss the procedure if available
I did not think this procedure was so painful… had I known it.. I definitely would have waited to have it. ..I wish I’d known that I was going to be admitted for more than a day so I could have sorted home care.
Due to my condition I could not lie on my front… nobody told me this so I couldn’t have the procedure.. I spent nearly 2 full days in hospital for NO reason
.A patient information leaflet in which the patient can read about the procedure.

The patient information leaflet was really informative and the junior doctors who explained the procedure made me feel at ease prior to undertaking it. I had plenty of time to think about my options.
Discussion
Cycle 2

Post Intervention
100% of patients undergoing ESWL after the introduction of a pre-procedure phone call, clinic space and a patient information leaflet, felt as if they were adequately consented for the procedure No preventable cancellations occurred following this.
The patient information leaflet was reviewed by patients and adapted to be more patient friendly The leaflet is in the final stages of ratification before trust wide distribution



The next series of junior doctors on the rotation were given an induction on the process so they felt confident explaining the procedure
Consent is a fundamental component of medical ethics and without proper consent patients are at risk of being seriously harmed We found that patients undergoing this procedure did not fully understand the procedure before undertaking it, did not have enough time to evaluate the risks of the procedure and as a result a patient felt harmed unnecessarily and one abandoned the procedure minutes before it occurring Through simple measures such as allocating a specific clinic space for the consenting process and introducing a patient information leaflet, we have ensured that all patients undergoing this procedure in the future, have the time and space to feel adequately consented
Take Home Messages
All procedures- even ones considered low risk need a proper consent process that needs to be timely, relevant and adjusted to a patients needs.
Simple measures like clear times for consenting- preadmission clinic, clerking, and WR are effective at creating a certain and efficient space.
Patient information leaflets can be a fantastic source of information patients can refer to in their times of need and should be utilized!