2 minute read
Optimising and improving the management of patients with abnormal liver function tests in primary care
Background
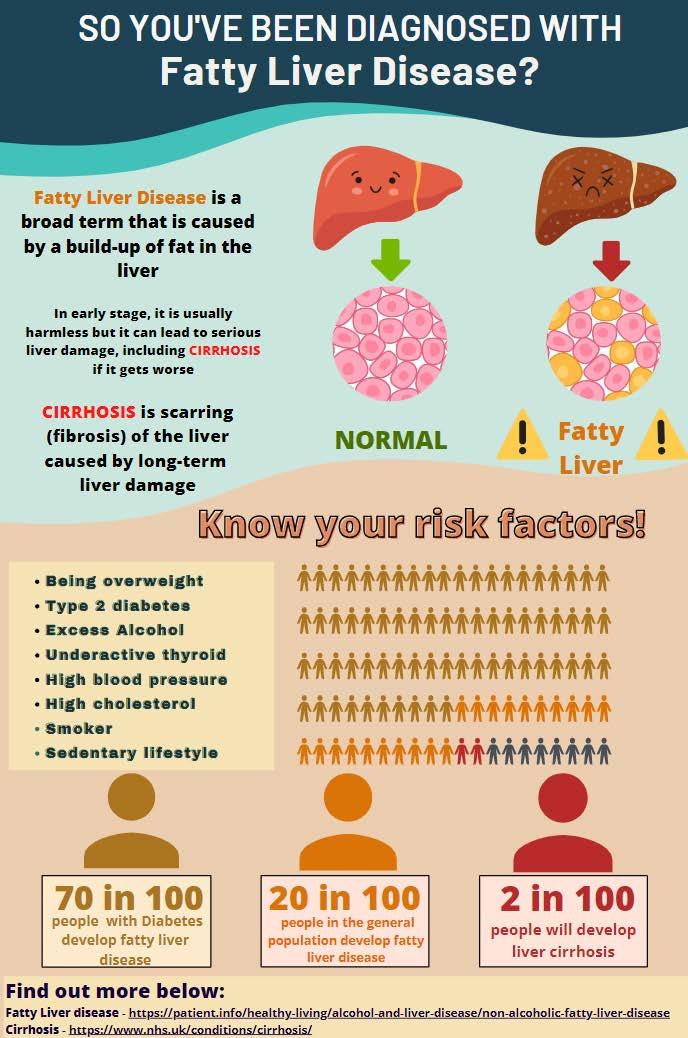
Fattyliverdisease is oneof thecommonestcauses of abnormalliverblood tests(LFTs) and canlead to livercirrhosis in 1-3% ofpatients. Patientsandcliniciansareoftenfalselyreassuredthat itis leading to poor management.
Advertisement
In our analysis, ~30 % of patientswhohadabnormalLFTsare inappropriatelymanaged.
Only1 in 5 patients in our analysishaveariskstratification(FIB4) performed to assesstheirrisk of cirrhosis(NICEguideline). Based onour predictivemodelling atour GP practice, we estimatedthat only1 in 10 patientshaveaconfirmeddiagnosisoffattyliver and there is 170 undiagnosedfattyliverdiseases in patientswithderangedLFTs at our practice.

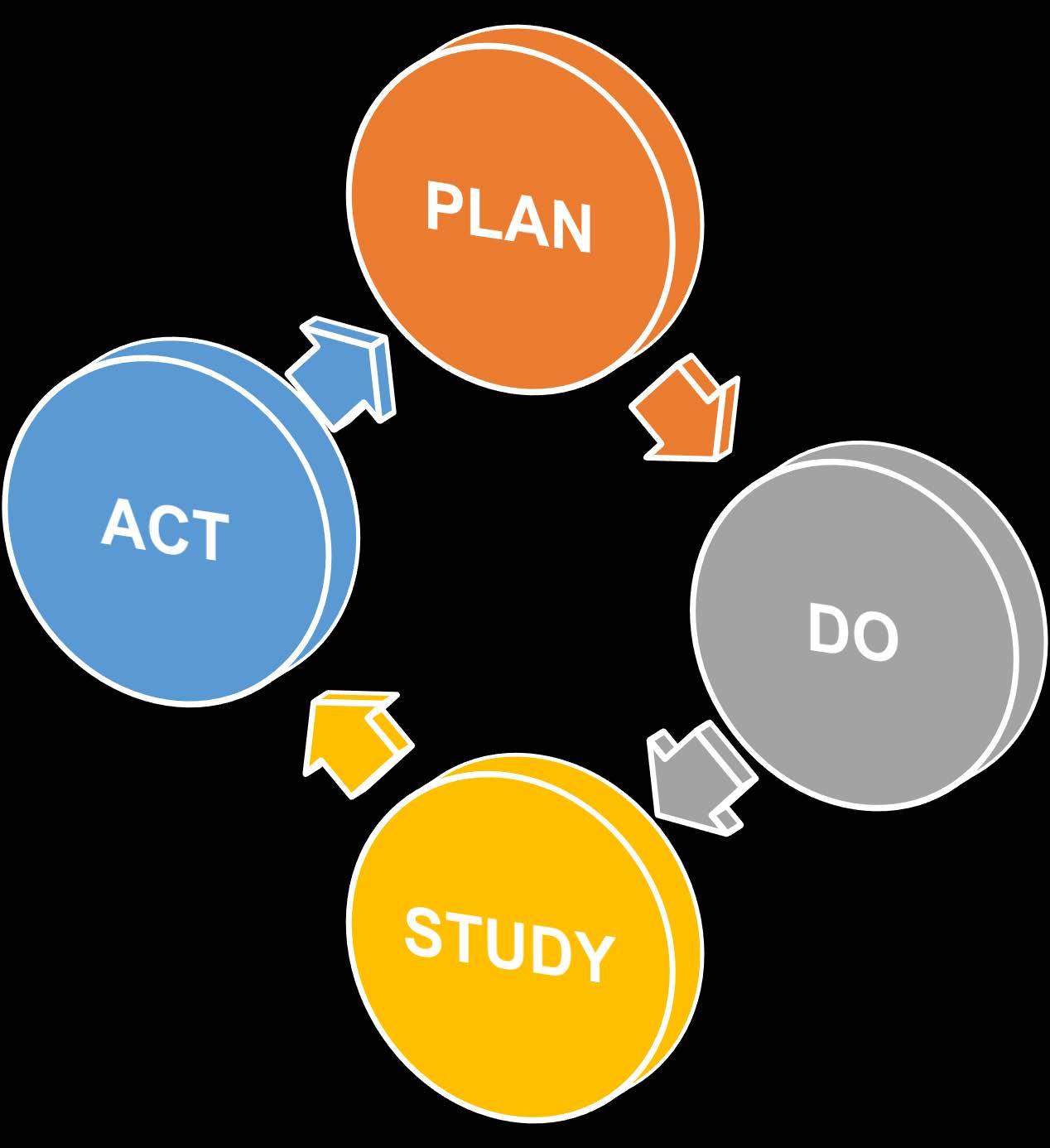
PDSA Cycle/ Intervention



Our project focused on 3 separate workstreams and 5 interventions, each with their own PDSA cycle:
Refining interventions based on feedback:
Improving patient leaflet

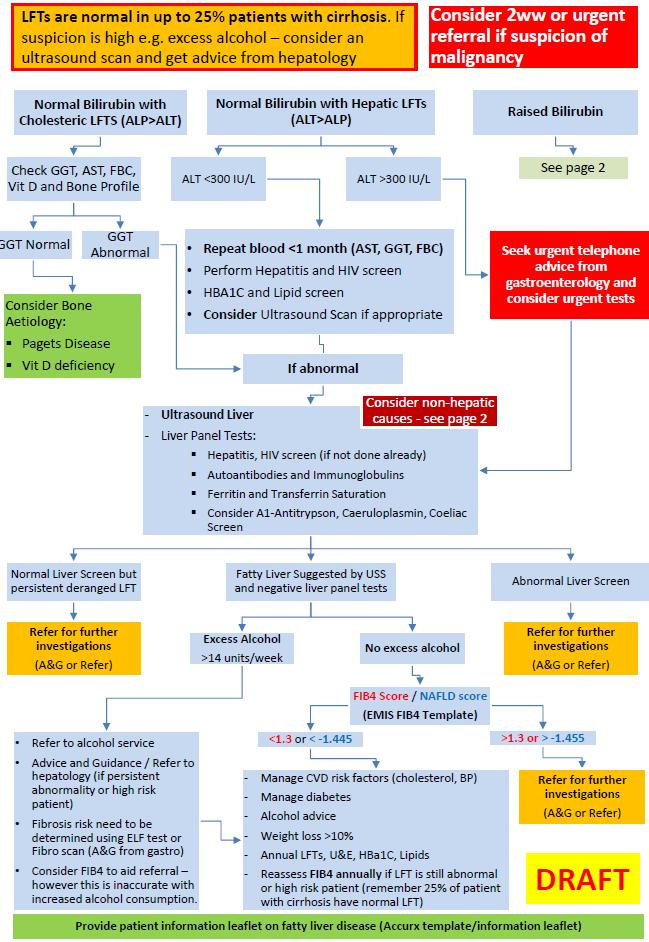
Adjustment to local guideline
Manual to Automating FIB 4 calculator
Ad-hoc teaching sessions
Step by Step guide
Stakeholder engagement
Interventions
B.Improve the management of
Work streams / Aims
A. disease
B. Improve the management of deranged LFTs
C. Implement interventions in the early stages of NAFLD to prevent liver fibrosis
Re-call Clinic: Our recall clinic identified high-risk patients and all patients were appropriately managed with ~10% of the patients being referred to hepatology
All patient had repeat blood requested via call or text message
Risk (FIB4) Analysis The number of patients who had risk stratification (FIB4) score coded on EMIS increased by 2x after the introduction of our integrated FIB4 calculator

All patients were informed about management, complication and monitoring.


2patients were REFERRED to hepatology due to high risk of cirrhosis
C.Implement interventions in the early stages of NAFLD to prevent liver fibrosis
5.Re-call clinic
PCN teaching - Learnings, interventions and teaching sessions were shared with 9 GP practices across 3 PCN groups and we received overwhelmingly positive feedback from all the stakeholders
"Really helpful presentations."
"Could you have this installed (FIB4 calculator) in our EMIS?"
9 GP practices across 3 PCNs
"This is excellent work. Well done!"
"I scored her using your template!"
AbnormalLFTsare not wellmanaged in primarycare due to multiplefactors lack of time,awareness and localguidelines. After our rootcauseanalysis, we identifiedkeychangeswhichlead to improvedoutcomes:
Explainingcomplications (3xincrease)
Performingriskstratification (2xincrease)
Increasedreferral and identification of high-riskpatients
The toolkit(composedof an automatedFIB-4calculator,patient leaflet, and aconciseguideline) we had implementedwaswellreceivedacrossthree PCNs
Marie Jasim, 1
Bridget McManamon, 1
Benjamin Stone, 1
Rebecca Spiby 1
1 Torbay and South Devon NHS Trust
100% felt the workload was now more manageable
‘[great] result… I'm honestly delighted”
Improving patient safety, on-call working experience and junior doctor wellbeing through improved weekend phlebotomy provision: A Quality Improvement Project BACKGROUND
“Much better service now”
Methods
>50% increase in number of weekend phlebotomists ‘[it’s] definitely improved and made the weekend shift a much easier experience’
- Existing limited weekend phlebotomy service was incompatible with the number of patients requiring blood tests, which was impacting safe discharge and urgent out-of-hours care
-Junior doctors were therefore required to spend significant amounts of time taking blood.
Serious concerns raised:
Unmanageable workloads for the on-call doctor team, who were already working at full capacity. Patients were not being bled in a timely fashion to enable safe and effective care
Discharge planning was being compromised
- A working group of junior doctors and hospital representatives was formed (phlebotomists, laboratory staff, operations managers).
- A mixed-methods online survey collecting quantitative and qualitative data was circulated to all junior doctors.
-Data analysis identified the extent of the issue, and trends for targeted improvements.

- A business proposal secured funding to trial an increase in number of weekend phlebotomists by >50%, and an increase of 2.5 to 4 working hours per phlebotomist.
- A follow-up online survey identified whether implemented changes had a demonstrable effect, and areas for further improvement.










