5 minute read
DOMESTIC VIOLENCE IN THE EMERGENCY DEPARTMENT:
MAKING IT EASER FOR CLINICIANS TO ASK (A QIP in Progress)
Introduction: Domestic violence (DV) is often a hidden crime and is globally under-reported. In a survey done by the Office for National Statistics in 2021, 5.5% of adults aged 16 to 74 years (2.3 million) had experienced domestic abuse (DA) in the past 12 months.1
Advertisement
ARE DUE TO DOMESTIC ABUSE2 12% OF ED ATTENDANCES
1 in 7 men Will experience DV in their lifetime3
2 ARE KILLED BY THEIR PARTNER EVERY WEEK4 WOMEN
1 in 4 women Will experience DV in their lifetime3
The Problem: NICE state that “People presenting to frontline staff with indicators of possible domestic violence or abuse (should be) asked about their experiences in a private discussion.”5 However, a case review of Kings College Hospital ED found that over a 3 month period 30% of those presenting having been assaulted with a head or facial injury were not asked about the perpetrator and 90% of them did not have safeguarding referrals, even when their partner was documented as the perpetrator. Furthermore, 100% of the females who had been stabbed and presented as a major trauma call (MTC) had been stabbed by their partner.
Aim: This project aims to identify barriers to asking about DV and address these through the implementation of interventions to improve the rates of screening for domestic violence in high risk patients.
Diagnostics: A survey was sent to all staff in the ED called “Staff’s views on what would make it easier to ask patients about intimate partner violence (domestic violence) in the emergency department: returning a total of 36 responses from a variety of nurses and doctors who work in the department. Their answers were used to create both a cause and effect diagram (Figure 1) and a driver diagram (Figure 2) and determine potential change ideas.
Measured outcomes : the number of domestic violence related referrals made to the ED safeguarding team.
1. Training about DV and how to ask for all ED staff – which prepares them to recognise & ask & what to do
2. Culture of asking in ED by all staff so that it is routine
DV Bitesize teaching at end of Week 5
3. DV guidelines & proforma easily accessible
4. DV proforma appropriate to time available to staff & clear about guidance
5. Ensuring staff have a private space to ask intimate questions (i.e. not curtains)
1.1 Bitesize teaching
Only 1 doctor and 6 nurses attended. There was no change in the number of referrals the week following the teaching.
1.2 Simulation teaching for junior doctors & registrars Use a survey pre and post teaching to asses confidence in asking about DV and monitor number of referrals in the subsequent weeks
2.1 Presentation to the team about the QI with summary of the earlier case review findings
2.2 “Ask for Nurse Angela” Posters to be placed in the department so that DV victims know what to say to subtly alert staff. To utilise handovers to explain what a patient is alerting you to in asking for nurse Angela.
2.3 Screening questions to be incorporated into the social history of junior doctors doing the rapid first assessment of an ambulatory patient and into the nursing triages.
2.4 Prompt to be added to MTC booklet and incorporated to electronic MTC form to remind clinicians to ask about safeguarding including DV.
2.5 Reminder about DV in the nursing handover as part of ”The Big 5” to actively screen for DV in individuals presenting secondary to assault
3.1 DV contacts made more accessible by adding them to the widely used ”Induction” app so that key contacts for the management of DV are readily available and therefore quicker to access
4.1 DV proforma review to ensure that it is easier to follow and the next steps are obvious for staff to take depending on patient’s answers.
5.1 Private space for DV discussion to be allocated
Monitor the number of referrals in subsequent weeks
Monitor the number of referrals made to the safeguarding team in the following weeks and review how many were made due to the “Ask for Nurse Angela” scheme
Monitor the number of referrals made to the safeguarding team in the following weeks
Monitor the number of referrals made to the safeguarding team in the following weeks and review how many were MTCs
Monitor the number of referrals made to the safeguarding team in the following weeks
Monitor the number of referrals made to the safeguarding team in the following weeks
Monitor the number of referrals made to the safeguarding team in the following weeks and review how many had the new DV proforma fully completed
Monitor the number of referrals made to the safeguarding team in the following weeks
Figure 5: Table of future interventions according to which secondary driver the intervention targets, “Act” reflection to be completed following each intervention.
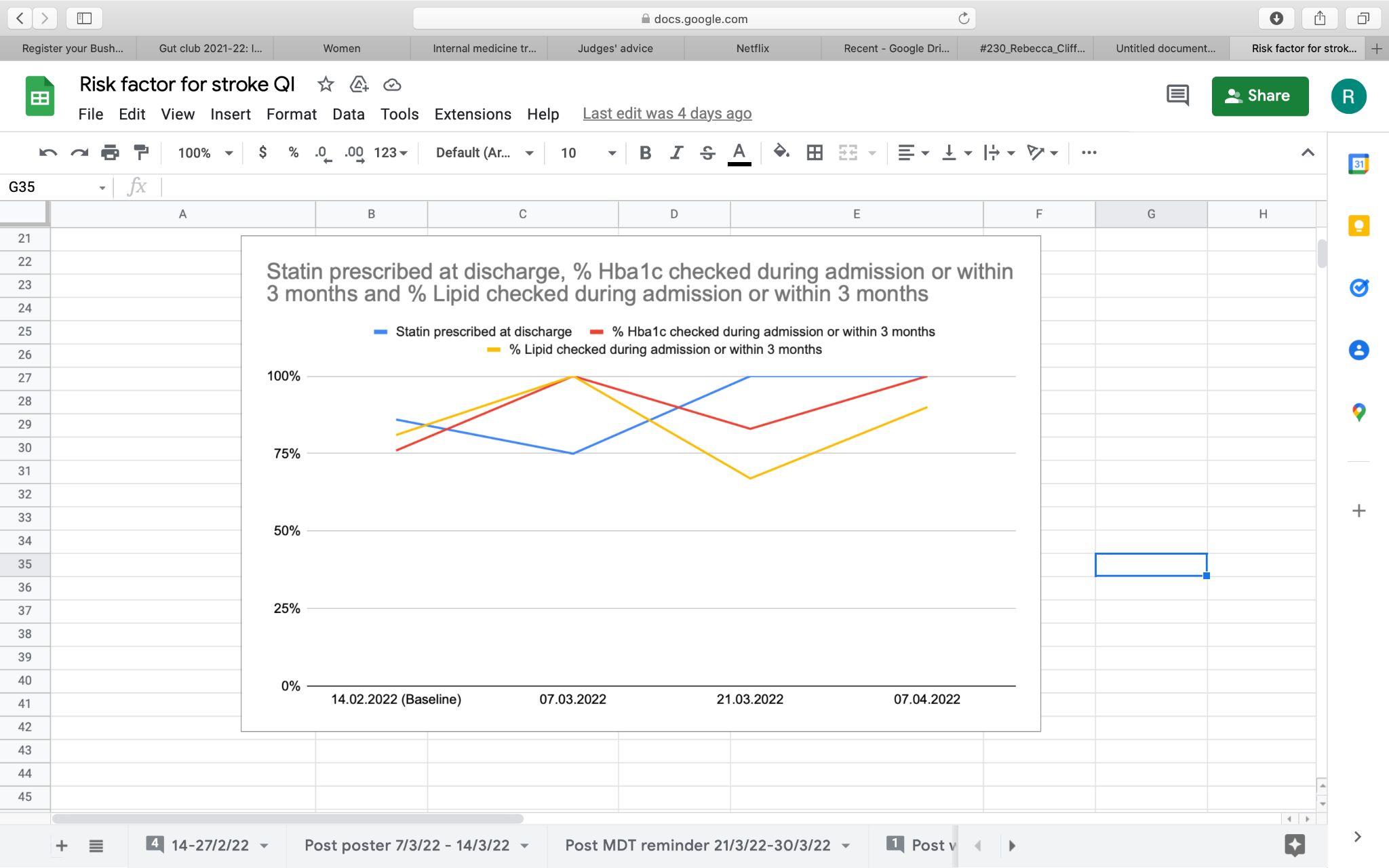
Results: A baseline measurement was done for 5 weeks, showing lots of variability in the number of DV safeguarding referrals made in the ED. PDSA 1 (figure 3) was implemented at the end of week 5, with no changes in the number of safeguarding referrals, so the teaching is to be repeated and changed to a time more suitable for both doctors and nurses. Future PDSA cycles to be implemented as above and studied with continuous reflection on interventions which make a difference.

Lessons Learnt:
• The importance of screening for DV in the emergency department
• The value of involving staff and actively asking them where the barriers to asking about DV lie
• When dealing with a large-scale departmental problem requiring cultural change, many interventions of different natures targeting different groups will need to be made. This can take time, require communication with many different teams and will require constant re-evaluation.
Improving the Quality of Trial without Catheter (TWOC) on the Elderly Care Ward
H.Sutton, T. Bobmanuel, G. Slabbert Portsmouth University Hospital NHS Trust, Portsmouth, United Kingdom

Introduction
Urethral catheterisation is a common procedure, performed predominately to monitor urine output and relieve urinary retention which may be due to a number of underlying factors.
Trial without Catheter (TWOC) is a process that involves the removal of a catheter from the bladder and the subsequent monitoring for the passage of urine. A failed TWOC has detrimental consequences to patient safety as it increases the risk of urinary tract infections, mobility of the patient is impaired and ultimately leads to prolonged admissions.

Aims
1. Assess the success rate of TWOC in the elderly care ward
2. Determine if the TWOC process is carried out in line with best practices
3. Identify any issues preventing healthcare professionals from using best practices for TWOC and the impact this has on TWOC success
Methodology
Data was collected prospectively for patients undergoing a TWOC procedure between September-December 2021. Electronic patient records and documentations were interrogated to identify the success rate of TWOCs, collecting data on various variables that could result in a failed TWOC such as regular bowel opening, baseline mobility, review of medication that can contribute to urinary retention, exclusion of possible UTI and BPH. Interventions were implemented in the form of a sticker containing check boxes for the factors that need to be considered prior to a TWOC –see Figure 1
Results
Data was collected for 12 patients and the TWOC success rate was 67% (8/12).
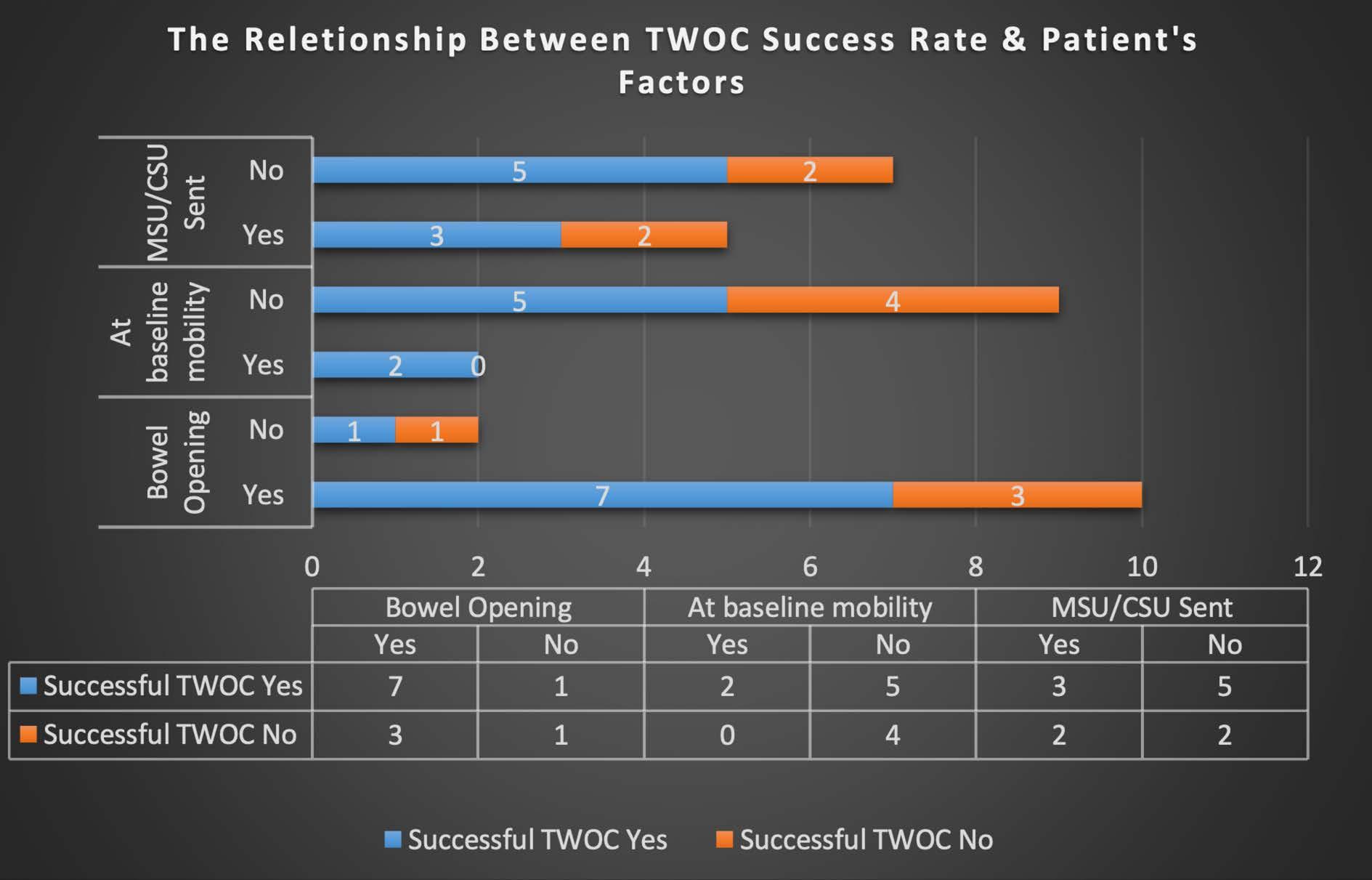
Patients at baseline mobility and who had regular bowel movements had the highest TWOC success rate with 70% of patients with regular bowel opening and 100% of patients at baseline mobility being TWOC’d successfully. However, only 2 patients were at baseline mobility due to the medical state and frailty of the patient. The full analysis of the data is demonstrated in Figure 2
The QIP revealed there was no standardization or uniformity in the TWOC process on the ward despite the success rate observed. Further cycles are essential to assess patient outcomes and improve standardisation and level of care.
Conclusion
In summary, our data revealed that there is a lack of standardization for TWOC in geriatric patients. With further cycles, we will identify if the TWOC checklists help to improve the standardization and success rate of TWOC.