
firsthealth Limited trading as Murrumbidgee Primary Health Network (ABN 15 111 520 168). Murrumbidgee Primary Health Network gratefully acknowledges the financial and other support from the Australian Government Department of Health. The Primary Health Networks Program is an Australian Government Initiative.
While the Australian Government Department of Health has contributed to the funding of this material, the information contained in it does not necessarily reflect the views of the Australian Government and is not advice that is provided, or information that is endorsed by, the Australian Government. The Australian Government is not liable in negligence or otherwise for any injury, loss or damage however arising from the use of or reliance on the information provided in this material.
Murrumbidgee Primary Health Network acknowledges the Traditional Custodians of the land in the Murrumbidgee region. We pay respect to past and present Elders of this land: the Wiradjuri, Yorta Yorta, Baraba Baraba, Wemba Wemba and Nari Nari peoples.
TABLE OF
Supporting healthcare professionals
Supporting workforce recruitment
Response, recovery and
Integration and transformation –
solutions for primary healthcare in Snowy Valleys
Transforming the health of Murrumbidgee
Our
credit to the team
report
recipients
service providers
Our region 2 Chair report 4 CEO report 5 Our board 6 Our senior leadership team 7 Snapshot of 2021-22 8 Committees and councils 10 Making a difference 12 Understanding community needs 14 Long term recovery key 16 Alternative approaches to supporting services for mental health and Alcohol and Other Drugs 18 Saving lives 20 Local solutions sought for primary health care in the after-hours period 22 Culturally safe services and workforce deliver results 24 Healthy ageing 26 Living healthily 28 One-of-a-kind palliative care 31
32 Cross team collaboration enhances general practice 34
and retention 37
resilience 38 Congratulations to our 2021 Primary Healthcare Award winners 41
one health system 42 Living well your way 44 Community-led
46
children 48
people 50 Full
52 Treasurer’s
54 Grant
56 Commissioned
57
contents
OUR region POPULATION 0.1-16.6 PERSONS /KM2 DENSITY INACTIVE 79.0 YEARS 37.4% 21.9% SMOKERS POPULATION CONSUME ALCOHOL AT RISKY LEVELS PSYCHOLOGICAL DISTRESS 246,073 122,550 MALES (49.9%) LIFE EXPECTANCY LIFE EXPECTANCY OBESE 34.9% 14.1% SMOKERS OBESE 70.2% 11.7% 20.4% 83.9 YEARS 123,532 FEMALES (50.1%) 126,124KMLAND AREA COMMUNITIES 508 BORDER WESTERN RIVERINA WA GGA WA GGA 2 | Annual Report 2021-2022
OUR priorities 2,387 TOTAL BIRTHS 51,269 (21.6%) OVER 65 YEARS 32 PUBLIC HOSPIT ALS 3 ABORIGINAL MEDICAL SERVICES GENERAL PRACTICES89 191 PRACTICE NURSES 306 GENERAL PRACTITIONERS 74.1 YRS 2,033 OVER 55 YEARS LIFE EXPECTANCY 15,408 ABORIGINAL AND TORRES STRAIT ISLANDER (5.8%) (13.2%) 252 GPs , 54 GP REGISTRARS MENTAL HEALTH ABORIGINAL AND TORRE S STRAIT ISLANDER HEALTH POPULATION HEALTH HEALTH WORKFORCE DIGITAL HEALTH AGED CARE ALCOHOL AND OTHER DRUGS Annual Report 2021-2022 | 3
Earlier this year as I was going through my personal archives I came across some old media clippings from my time as a junior doctor at the Wagga Base Hospital. One article, with accompanying photo, welcomes us as 10, fresh faced, new interns and speaks of rural general practice as interesting and varied. The second, features the same group being asked for their opinion about a financial incentive being offered for rural general practitioners. We were all in agreement then, that financial incentives alone were not the answer. Now, here I am 15 years later and not much has changed. Rural GPs have the best job in the world, one where we get to build relationships and change the lives of our patients. Yet, despite the rewarding career a rural GP presents, recruitment and retention for regional and rural general practices continues to be an issue.
As a local GP I understand the challenges facing the primary healthcare sector. The impacts on patients and all primary care clinicians arising from the hardships of the previous few years, has only exacerbated health workforce issues. And as Board Chair the industry experience of myself and fellow board directors, in delivering primary healthcare in a regional and rural setting continues to be critical in providing guidance and support for the work of Murrumbidgee Primary Health Network (MPHN). Over the past 12 months there have been a range of NSW and federal reviews, policies and reforms which will guide our future direction.
Among them Australia’s Primary Health Care 10 Year Plan 2022-2032, the Royal Commission into Aged Care Quality and Safety, the NSW Health and NSW Primary Health Networks Joint Statement – Working together to deliver personcentred healthcare.
The Joint Partnership, in particular, recognises patientcentred care requires collaboration and integration between the primary, community, hospital and social care settings. We know when we work together to get this right, health outcomes for people and communities are improved.
Over the coming years, MPHN will continue to support clinicians and primary healthcare providers to implement the range of various health reforms at a local level. Ensuring the needs and priorities of local communities are addressed remains a key focus of the Board. Critical to this success will be developing locally led and collaborative approaches with the aim to develop innovative solutions to improve health outcomes for our most at-risk population groups. Despite the perennial difficulties, there are significant opportunities ahead for primary healthcare. And I know the strength of our partners and the outstanding and unflagging commitment of the CEO and staff to deliver on the MPHN vision of well people, resilient communities will help us meet the challenges head on.
Dr Jodi Culbert


CHAIR
report 4 | Annual Report 2021-2022
What a privilege it is to be back in the CEO seat after maternity leave. When I returned in late 2021 I was pleased to see continued progress towards our vision of well people, resilient communities under the leadership of Julie Redway. I would like to formally thank Julie for her time as Acting CEO, employees who took on acting roles, and for all staff for their continued efforts in supporting the health and wellbeing of our communities.

Recently I was reflecting on my own first early experience of the health system and the challenges rural and regional communities face in accessing health services. For me, my own birth was several hours from my hometown, and some weeks early, providing challenges for my family as I received the care I needed. Yet this experience is not uncommon for many people living across our 508 communities who often experience challenges when attempting to access care close to home throughout their life.
Personal experiences are key to understanding the impact and challenges people face in accessing health care. The Health Needs Assessment 2022-2025 published in May 2022 captures qualitative stories to either support stories being illustrated through quantitative data sources or highlight emerging needs. It is not unusual for data delays, and personal stories of people’s experience accessing healthcare is critical. Equally important is working with our communities and healthcare providers to develop solutions.
In fact, Working Together is the theme of this year’s annual report. Within the pages of this Annual Report you will find stories of how MPHN has worked closely to collaborate with our various stakeholders to improve health outcomes for our communities. I’m incredibly proud of what we have achieved over this financial year. The challenges of health pandemics and natural disasters have, and will, continue to test us. But like all rural and regional communities, innovations to meet these challenges often come from the grassroots, and as an organisation we have a role in supporting community driven innovations.
As we continue to look for opportunities to collaborate, innovate and inspire, our partners are critical. From larger organisations and peak bodies, to health providers including general practice, pharmacy, allied health, aged care, and our commissioned services; and our communities through councils, Local Health Advisory Committees, and community groups. Each has a role. Each has a voice. And each has an important role in improving health outcomes of Murrumbidgee communities.
Melissa Neal

CEO
report Annual Report 2021-2022 | 5
OUR BOARD
BOARDour pauljodi alam
Jodi was a physiotherapist before returning to study and qualifying as a GP in 2011. Her interests include musculoskeletal medicine, mental health, preventative health and medical student education. Jodi is a strong advocate for the role of general practice in primary care.


Paul is the director of a livestock equipment company, with a background in project management. Paul is passionate about addressing the challenges faced in delivering effective integrated health care to our significant region. He also has broad involvement in the local business and sporting communities.



Alam is a rural GP from Finley NSW with particular interests in public health, palliative care and emergency medicine. Alam has been working as the principal GP at Finley Regional Care and GP/VMO at Finley Hospital since 2008. He is passionate about providing better health outcomes to rural remote communities in the region.

Donna is a practice nurse, working in primary healthcare, with a Masters in Gerontology. Donna has 30 years nursing experience and is proud to be a nurse leader facilitating preventive health programs to improve health outcomes for all age groups.



Peta was an Accredited Practising Dietitian, and is currently CEO of Riverina Medical and Dental Aboriginal Corporation. She has held senior health management positions in regional and remote communities across acute, primary and community settings. Peta is passionate about improving access to health and community services for those who need it most.
Kristen is the practice manager at Corowa Medical Centre, a mediumsized general practice. Kristen brings a well-rounded knowledge of the healthcare field from both a clinical and a business management perspective. Her background in administration, nursing and practice management brings a diverse perspective to all of her endeavours.
PennockHowardDr Scholtz rene
christinejacques
Jacques is a GP obstetrician in Cootamundra who’s also interested in family health and a strong voice for palliative care provision. He participates on MLHD and MPHN committees and is the principal/owner of a large general practice. He stands for equitable healthcare across all segments of society and works towards an integrated primary healthcare model.
Christine is the Director of Charles Sturt University’s Three Rivers Department of Rural Health. With more than 30 years’ experience working in rural health, Christine has diverse executive health management and leadership experience. She is passionate about the Murrumbidgee region and improving rural health outcomes.
Rene is an experienced health sector consultant, who has worked extensively with allied health, nursing and medical professionals. Formerly the CEO of South Western Sydney Primary Health Network, Rene has qualifications in physiotherapy and gerontology, and is committed to improving the health of the communities he serves.
Larsen MannMcLean peta kristendonna
Gianniotis (Treasurer)
Dr Culbert (Chair)
Dr Yoosuff
6 | Annual Report 2021-2022
melissa Redway Chief Executive Officer

Appointed as CEO in 2018, Melissa is committed to developing local partnerships and working with organisations to improve outcomes for people and communities across the Murrumbidgee. During her 20year career in the primary health and community services sector, Melissa has gained experience in governance, leadership, strategic management, human resources and industrial relations.



Executive Commissioning and Operations
Julie is responsible for leading the execution of MPHN strategies with a focus on results and outcomes for health service providers and consumers. Having started her career in medical science, Julie transitioned into the primary care environment in 1993. Julie holds a Bachelor’s in Medical Science, Masters in Health Service Management and is a graduate of the Australian Institute of Company Directors (AICD).
julie our SENIOR LEADERSHIP TEAM
andrewMills
Executive Integration and Partnerships

Narelle has more than 20 years’ experience in primary health program development and implementation with interests in quality improvement, chronic disease management, integrated care, aged care and palliative care. Narelle has an Honours Degree in Applied Science, a Graduate Certificate in Public Sector Management and is currently studying an MBA.
Senior Manager, Primary Care Engagement
Andrew has spent the last 10 years in the field of primary care engagement and has a particular interest in current and emerging digital health solutions and continual quality improvement. Andrew has experience in acute and primary health sectors in metropolitan and rural settings and holds qualifications in medical science (Pathology) and music.
Senior Manager, System Integration
Anita’s mental health career started in support work and community development, before moving into management roles. Anita’s ongoing passion is that everyone deserves access, in every meaning of the word, to the supports required to live a fulfilling and meaningful life.
Bennie (PhD)Dr
Neal jason
Senior Manager, Population Health, Planning and Data
Jason has an extensive background in public health research and expertise in epidemiology, biostatistics, and health promotion. Jason has a PhD in Behavioural Epidemiology from Deakin University. He has more than 15 years of experience in managing large-scale public health projects from conception to execution to evaluation.

janelle
AshwoodDufty jessica
Senior Manager, Commissioning
Janelle has worked for MPHN for nine years and was appointed Senior Manager Commissioning in March 2022. Interested in how minds work, Janelle completed postgraduate studies in psychology in 2013. While mental health and suicide prevention are areas of interest, Janelle also has an affinity for data and how it relates to decision making.
Senior Manager, Finance and Corporate Services
Jessica graduated from Macquarie University in 2010 and was advanced to the status of Certified Practising Accountant of CPA Australia in 2016. After working in Australia and internationally for 10 years in the retail and consumer goods industries, she now lends her skillset to the betterment of the Murrumbidgee community.

 McRaeHeap anita
narelle
McRaeHeap anita
narelle
Annual Report 2021-2022 | 7

OF 2021-22 PRIMARY HEALTHCARE PROVIDERS CPD CHILDHOOD IMMUNISATION WORKFORCE PRACTICE VISITS TOTAL PRACTICE ENGAGEMENTS snapshot “The community of practice meeting is the reason I have remained working in aged care Previous to this meeting commencing, I felt very isolated and overwhelmed. It has been a game changer and I always go away with something from every meeting.” Simone Fuller, Aged Care Services Manager, Allawah Lodge 2,529 REMOTE SUPPORT INTERACTIONS1,980 IN PERSON SUPPORT VISITS549 Events212 PRACTICE ENGAGEMENTS TO SUPPORT CHILDHOOD IMMUNISATIONS of all children in the Murrumbidgee region are fully vaccinated by the age of 5 years* of all Aboriginal and Torres Strait Islander children in the Murrumbidgee region are fully vaccinated by the age of 5 years* 236 95.7% 94.3% PEOPLE AT TENDED CPD EVENTS977 new medical practitioners to the region 21 GP Registrars trained in the region 59 University of Wollongong students completed placements5 AT TENDANCE RATe FOR IN PERSON EVENTS78% AT TENDANCE RATE FOR VIRTUAL EVENTS62% DIGITAL HEALTH OF ALL ELIGIBLE PRACTICES ENABLED TO USE EPRESCRIPTIONS100% OF ALL ELIGIBLE PHARMACIES SUPPORTED TO ACCEPT EPRESCRIPTIONS98% 44 hosted by MPHN 168 External events *Data source: Australian Institute of Health and Welfare 2018/2019 2 IN Griffith 3 in Leeton 8 | Annual Report 2021-2022


MENTAL HEALTH WAGGA GP AFTER HOURS ALLIED HEALTH Community grants CLIENTS ACCESSING2,840 OCCASIONS OF SERVIC E34,211 occasions of service supporting someone e xperiencing sucidalit y 6,321 aged 0-11 years205 aged 12-24 year s568 aged 25-65 year s1,575 aged 66 years and over492 Patient consultations4,885 Home Visits123 GPS FROM43 PRACTICES8 identify as 438 total services delivered by WARATAH, comprising5,062 FUNDING$224,52041 GRANTS PODIATRY1,396 DIABETES EDUCATION1,029 DIETETICS2,000 OTHER, INCLUDING PHYSIOTHERAPY637 OTHER ALLIED HEALTH SERVICES including COPD/Asthma education, speech pathology and foot care nurse 1,168 New clients2,088 Total clients2,404 healthpathways with190 request pages and191 resource pages in total55 page views40,013 sessions10,567 average pages per session3.8 users1,115 returning visitors90% “I never knew mental health peer support workers existed until I accessed services myself. I met two amazing peer support workers and thought, ‘Wow, one day I hope I’m well enough to do something like that’. They gave me an amazing sense of hope and recovery, just seeing somebody else navigate working in the with mental McGill, MyStep “Thank you MPHN for making these grants available - the importance of strong social connections cannot be underestimated in improving health and wellbeing,” Fran Day, Chair, Lockhart Local Advisory Committtee Annual Report 2021-2022 | 9
AND COUNCILS committees
Community Advisory Committee (CAC)
Chair: Garth Hungerford

Over the past 12 months as COVID-19 restrictions have eased somewhat, the Clinical Advisory Committee continued to provide a consumer perspective as healthcare advocates and advised MPHN on a number of fronts as it affects communities across the region. Significant impacts continue for many people with domestic and family violence, mental health, Aboriginal health, aged care and particularly a shortage of primary care clinicians and general practitioners has added to an already overwhelmed health system. These concerns have been discussed at length at CAC meetings and MPHN has responded to the committee’s representations by continuing to bolster and promote commissioned services. Further community feedback via the Health Needs Assessment and Conversations on the Couch throughout the region has been vital in helping develop new services for communities across the Murrumbidgee.
Members: Chris Blake (from July 2021), John Harper, John Moi, Julie Mecham, Lee Ncube, Margaret King, Ruth White, Stan Warren, Michael Gooden (to September 2021), Cheney Dewar (from September 2021)
Board Representatives: Peta Larsen, Kristen Mann
Clinical Councils
Border Clinical Council
Chair: Dr Marion McGee

The Border Clinical Council continues to raise local issues and provide input into the activities of MPHN across a broad range of areas. As we moved to managing COVID-19 in the community, we sought to ensure our community members and providers had access to up-to-date and clear information. Additionally, we provided feedback and input on the allocation of new mental health funding to support mental wellbeing during the continuing pandemic; improving navigation of MapMyRecovery; respiratory care pathways; new and existing service models; improving outcomes for older people at risk of regular hospital presentations; and the delivery of professional development including the provision of multidisciplinary approaches and hybrid events. Finally, we helped identify improvements to clinical council operations more broadly, and highlighted the importance of maintaining a local issue focus while simultaneously supporting networking opportunities with other councils to discuss broader system issues and reform.
Members: Jeremy Car, Laura Ross, Lourene Liebenberg, Michael Love (from July 2021), Rachel James, Simon Lloyd (from April 2022)
Board Representative: Dr Alam Yoosuff
10 | Annual Report 2021-2022
Riverina Clinical Council
Chair: DR NANG WIN

It’s been a challenging year for health professionals across the region, and collectively we’ve achieved good vaccine coverage, management of active cases and establishment of strategies to manage the effects of long COVID. Additionally, we have catered for health burdens from the pandemic in terms of physical, social and financial concerns affecting mental wellbeing. The Riverina Clinical Council has focused on priority areas of aged care, Aboriginal and Torres Strait Islander health, population health, health workforce, digital health, mental health and alcohol and other drugs. MPHN has been measuring the key performance indicators on preventable hospital admissions, cancer screening rates, childhood immunisations and mental health treatment rate in conjunction with the Department of Health. The Riverina Clinical Council has focussed on increasing efficiency and effectiveness of medical services, and improving coordination of care particularly for patients at risk of poor health outcomes.
Members: Brett Causer, Evan Feather, Lee Francis, Luke Peacock, Dr Daniel Fry Board Representative: Dr Jacob Scholtz
Wagga Wagga
Clinical Council
Chair: Dr Rachael Fikkers

It was another year of living with COVID-19 and the Wagga Wagga Clinical Council was able to provide valuable feedback regarding challenges facing primary care and potential solutions to these challenges to MPHN for incorporation into HealthPathways. The Wagga Wagga Clinical Council has been integral in providing feedback regarding the development of the Murrumbidgee Local Health District’s Improving Outcomes in Aged Care program in relation to feedback on potential issues and proposing possible solutions pertaining to primary Care. We also provided feedback on the following triennium Health Needs Assessment, the after-hours regional plan and palliative care services in the region. This year saw a collaboration with other clinical councils across the region to share ideas and information on future strategic planning. It provided the opportunity to reflect on other priority areas and discuss current and future health policy impacting primary care and PHNs.
Members: Dr Jonathan Ho, Carin Lewis, Dr Ayman Shenouda, Kimberly Aylward, Luke van der Rijt, Michael O’Reilly, Nancy Kaur, Paul Colenso, Sandra Skaf, Dr Khalil Soniwala (to August 2021), Tom Shumack Board Representative: Dr Jodi Culbert
Western Clinical Council
Chair: Dr Muhammad Shahzad Arshed

The primary focus of the Western Clinical Council in the 2021/2022 financial year has been on local issues in relation to mental health, Aboriginal and Torres Strait Islander health, paediatric health, health workforce, digital Health, aged care, alcohol and other drugs, and the optimisation of care and outcomes for people living with chronic diseases. In this period our Clinical Council is proud of our achievements. Among them include improved palliative care access especially home palliative care; improved community paediatric care service with better and quick access to a paediatrician; improved screening and optimisation of chronic obstructive pulmonary disease patients with the winter strategy program; better access to mental health services and practitioners; and better coverage and access of allied health services under WARATAH program. We have also valued the opportunity to collaborate with the region’s clinical councils about solutions to state and national health system challenges.
Members: Belinda Guest, Dr Bhupinder Kumar, Dr Khaled Bardawil, Dr Shahid Abbas, Elizabeth Dixon, Emma Kelly, Jessica Ammendolia, Karen Ingram. Leanne Baulch, Leanne Kennedy, Sandra Royal, Sean Dodd (from June 2021) Board Representative: Donna McLean
Annual Report 2021-2022 | 11
a

DIFFERENCE
“We pride ourselves on making a difference to the health and wellbeing of people living in our communities – it’s the heart of MPHN’s vision – well people, resilient communities. And just like people, our communities are unique also. There isn’t a one-sizefits-all approach to primary healthcare, and this is why we aim to ensure services are accessible as close to home as possible. Key to achieving this is understanding the health needs, and funding programs and services to meet those needs. It’s pleasing to see real life examples of how our funded services have improved the health and wellbeing of our communities that are at most at-risk of poorer health outcomes.”
this section
Understanding community needs
Long term recovery key
Julie Redway Executive Commissioning and Operations
Alternative approaches to supporting services for mental health and Alcohol and Other Drugs
Saving lives
Local solutions sought for primary care in the afterhours period
Culturally safe services and workforce deliver results

ageing
One-of-a-kind
Healthy
Living healthily
palliative care making
in
12 | Annual Report 2021-2022

Tell it Well storyteller Nic Steepe Annual Report 2021-2022 | 13
COMMUNITY NEEDS understanding
MPHN undertook a number of activities this year to continue its person centred approach of listening and responding which informed the development of the 2022 to 2025 Health Needs Assessment.
Community engagement continues to be the engine driving MPHN’s response to existing and emerging health needs and this year a range of activities provided community members, volunteers and health professionals from across the region the opportunity to authentically reflect on and share personal stories of their challenges and successes when interacting with the healthcare system.
MPHN conducted activities designed to connect and empower conversations. Participants ranged from members of local health advisory committees and community members from a range of demographic groups including harder to reach populations such as First Nations and those experiencing socio-economic disadvantage.
Conversations on the Couch gives participants the opportunity to speak in person on health matters and experiences. It’s an important cog in identifying service gaps and key issues and informs the process of commissioning effective interventions and solutions to address them.

As part of the Conversations on the Couch activity in 2022, MPHN’s Manager Planning and Reporting Toni Preuss travelled to 19 communities with populations of 1,000
people or more.
“We had 215 people attend one of the 15 Conversations on the Couch and four Yarns on the Couch opportunities and we heard housing affordability, older people moving into smaller communities and smaller towns becoming commuter towns is putting significant pressure on communities, for both housing and health.”
“Among the challenges we heard were food insecurity, awareness of services, and advocacy for those with low health literacy. However, people were quick to thank and commend their local health professionals who do so much for their communities, and those who attended a Conversation on the Couch expressed appreciation for us being there to listen to both their good and the not so good health experiences. We collected some critical data from a wide range of people, and it was always an insightful and sometimes humbling experience for staff to be involved with.”
2022 saw the introduction of ‘Yarns on the Couch’ events which were specifically provided for Aboriginal and Torres Strait Islander people to meet in a familiar location for them
14 | Annual Report 2021-2022
to discuss their health needs. Four locations were attended in Wagga Wagga, Tumut, Hay and Deniliquin and attended by 45 people.


“A major challenge for our First Nations people is around cultural awareness and respect, with many choosing to not attend treatment or seeking testing to avoid mistreatment. It’s a stark reminder of the need for better cultural understanding of local First Nations people and their needs.”
The updated Health Needs Assessment reveals insights into the health needs of the Murrumbidgee, using quantitative and qualitative data from the Australian Bureau of Statistics, the Australian Institute of Health and Welfare and MPHN’s Community Feedback Survey.
MPHN’s Senior Manager Population Health Planning and Data Dr Jason Bennie reflected on the value of strategically connecting current data from a wide range of sources with key priority areas and the needs of target population groups.
“By examining this data we can really see where our current priorities are meeting or not meeting the needs of those community members who are most at risk. One example of this is the growth in population of older people and the increase in needs for ageing related services, which will inform commissioning of aged care activity.” Dr Bennie said.
“The 2022-25 health needs assessment also clearly shows a continued need to increase ante-natal support as higherthan-average teenage birth rates persist along with lower than average life expectancy due to prominent causes of death such as heart disease and dementia.”
Another important barometer on health comes in the form of the region’s 33 Local Health Advisory Committees (LHACs).
MPHN’s Senior Manager Primary Care Engagement Andrew Heap said LHACs play a critical role in providing authentic on-the-ground feedback to inform many of MPHN’s activities.
“LHACs have the unique perspective of knowing their communities in a way that we don’t, they are across what works well and where the issues are. Our biennial LHAC forums and regular LHAC meetings are a wonderful opportunity to get real time feedback and learn where MPHN can provide support,” Mr Heap said.
“As the COVID-19 pandemic restrictions eased, a return to in person consultation with our LHACs through regular meetings and the LHAC forums was a priority and has been widely valued and embraced by all particularly with respect to the forums where we see spirited discussions, and where LHACs can share their local insights, success and highlight where they see the most need.”
THE REGION’S LOCAL HEALTH ADVISORY COMMITTEES Adelong-Batlow Barham Berrigan Boorowa Coolamon-Ganmain Cootamundra Corowa Culcairn Deniliquin Finley Griffith Gundagai Hay Henty Hillston Holbrook Jerilderie Junee Lake Cargelligo Leeton Lockhart Moulamein Murrumburrah/Harden Narrandera Temora Tocumwal Tooleybuc Tumbarumba Tumut Urana Wagga Wagga West Wyalong Young community feedback 822 9 260 HNA COMMUNITY FEEDBACK 1091 March to August 2022 people provided feedback including: completed online surveys and Aboriginal and Torres Strait Islander online surveys people attended Conversations on the Couch and Yarns on the Couch social media comments Conversations on the Couch, Temora; Yarns on the Couch, Deniliquin Annual Report 2021-2022 | 15
LONG TERM RECOVERY key
Two and a half years on from the 2019/2020 summer bushfires, the Murrumbidgee communities impacted continue to be supported through a range of MPHN initiatives and collaborations.
The March 2021 10 Years Beyond The Bushfires report into the devastating Victorian ‘Black Saturday’ fires found positive long term recovery from major disasters requires more than two years of support. The study aimed to build an understanding of longer-term recovery and the ongoing impacts of a major disaster experience, to identify where support is needed for those affected and to guide preparedness and recovery from future events.
MPHN’s bushfire recovery lead, Maja Asmus said the report highlighted the power of community strategies to strengthen resilience. “The influence of family, friends and social networks really can enhance longer term resilience and recovery, and MPHN’s approach to activities has been to support initiatives with the potential for longevity and sustainability at the local level,” Maja explains.
“Through the Bushfire Recovery Steering Committee, MPHN was able to facilitate relationships with organisations outside of health who were providing various support activities in these communities, such as councils, farming and land care organisations, and education. Together we worked collaboratively to dovetail into existing activities and coordinate recovery efforts to avoid duplication of services.”
An example of collaboration was the establishment of The Men’s Table initiative in Tumbarumba during December 2021. It was a regional and natural disaster area pilot and its success saw the beginning of another table start for Khancoban/ Corryong and more will commence in late 2022.
The Men’s Table in Tumbarumba was a welcome social opportunity for participant Andrew Rae. “After the fires we received great community support from organisations providing mental health support. None focused solely on men until The Men’s Table came. This is a safe place for men to lean on each other for support. The men are there to help each other, and that’s a big part of why they’ve come.”
Kane Stewart, another Men’s Table participant agrees adding “it’s been awesome connecting with people from all walks of life. We are all willing to listen. From the outset everyone has space and we are going to talk without judgement. These community spaces are absolutely vital.”
activities through
RECOVERY GRANTS
Young people also needed targeted support. Culcairn’s Billabong High School hosted the Tomorrow Man and Tomorrow Woman sessions, with the first receiving positive student and staff feedback. One staff member said “the session was amazing. Especially the Man Code. It was a safe space to give the boys a chance to speak about their feelings and how they are perceived in school. The session with the girls was also just as amazing. They discussed some very personal issues young girls face. Both sessions helped the cohorts see each their fellow students in a different light and relate to each other’s wellbeing”.
$275,406 supported 36
BUSHFIRE
“The Black Summer Bushfires took a devastating toll on my community and we are still feeling the effects today, two years on. The scars on our beautiful lands are still evident, but it is the scars that you can’t see, these are the ones that concern me the most. I live in the Snowy Valleys in remote southern NSW; cattle country, with farmers who have resilient DNA. They have lived through it all and nothing appears to faze them. But it does. They just don’t put their hand up for help.”
Snowy Valleys community member, Andrew Rae
16 | Annual Report 2021-2022
In June, MPHN engaged the Resilience Project to support the schools and early childhood centres in bushfire impacted communities. It’s a targeted all of school approach and the project will support teachers to embed the learning within regular lessons, provide a journal to support and guide students, and parent information sessions. Onboarding is now underway with commencement of the project expected in late 2022.
MPHN’s Bushfire Recovery Grants also provided more than $275,000 in funding for 36 activities. One of these is the Nature Fix trails which will design and install a series of nature wellness stops at targeted locations across the Snowy Valleys area. Under the leadership of the Murrumbidgee Local Health District’s Disaster Recovery clinicians the project is community designed to support healing and recovery through storytelling, while simultaneously aiding the rebuilding of local tourism. Culturally sensitive Indigenous stories will be respectfully embedded throughout the program at sites of significance.
“These all are a small snapshot of the various projects and activities being undertaken in the region’s bushfire impacted communities,” explains Maja.
“We also have funded Bushfire Service Navigator roles in the Greater Hume and Snowy Valleys councils to facilitate wellbeing support through linking community members to available services and coordinate social connectedness events like the Are you bogged, Mate? sessions in Jingellic, Adelong and Holbrook to help rural men talk about mental health and suicide. At one of the sessions, a community member shared that he had been having suicidal thoughts but had never talked to anyone about it previously. Events like these allow us to reach people that may not seek help otherwise. For this community member they were able to get the help they needed and this just shows the positive impact of dedicated funding to support disaster affected communities.”
Bushfire Recovery steering committee
Thank you to all members of the Bushfire Recovery Steering Committee for your guidance on funding and your collaboration on activities supporting the region’s bushfire impacted communities. Members of the committee represented a diverse range of organisations and communities, and included people with lived experience.
• Snowy Valleys Local Government Area
• Greater Hume Local Government Area
• New South Wales Police
• Rural Fire Service
• Rural Doctors Network
• Department of Education
• Local Land Service
• Department of Primary Industry
• Regional NSW
• NSW Farmers
• Rural Aid
• Murrumbidgee Local Health District
• Albury Wodonga Health
• Riverina Aboriginal Medical and Dental Corporation
• Resilience NSW
• National Recovery and Resilience Agency
• Lived experience community representatives

• State Emergency Service
• Rural Financial Counselling Service
Kane Stewart, The Men’s Table, Tumbarumba
Annual Report 2021-2022 | 17
to supporting services for mental health and Alcohol and Other Drugs alternative approaches
MPHN funds a range of initiatives to support mental wellness and Alcohol and Other Drug (AOD) use issues with dedicated services for young people, and mothers and families, among the offerings.
Given the limited local workforce, MPHN is supporting its mental health and Alcohol and Other Drug (AOD) service providers to utilise the wide breadth of workforce available locally.

MyStep to Mental Wellbeing is a stepped care approach to providing mental health services and operates on the premise that no matter the level of support required, people can move seamlessly throughout service options if their level of care needs change. MPHN’s Senior Manager System Integration Anita McRae said in addition to clinicians, peer support workers play a vital role supporting mental wellness.
“Peer workers have always been part of the MyStep model and they play an important role in building social confidence. Anecdotally the activities peer workers lead are showing positive results,” Anita says.
Deniliquin based MyStep peer worker Spencer McGill works with clinicians to support people living with mental illness. “Being a peer support worker means I have lived experience of mental illness as one of the qualifications for my job. Clinicians are good at doing therapy, and I’m good at knowing how it feels to access a service,” Spencer explains.
“My role is dynamic and can look very different each day depending on the person and their needs. That could be working on someone’s exercise goal, going out in the community with them to practice being in social situations or meeting with somebody at school to chat with them where they’re most comfortable,” he adds.
Anna, another peer worker in Wagga Wagga leads a fortnightly walking group with participants ranging from ages 31 to 80 years. “We walk and talk for around 45-minutes and finish with a 10-minute mindfulness body scan and cool down stretches, and when I ask at the end of each session ‘how can I run this better?’ the reaction is always – ‘100 percent nothing, we love it just the way it is’,” Anna explains.
An alternative workforce is being harnessed by Gidget Foundation with CEO Arabella Gibson saying “psychologists would typically provide our services, but recruitment to these roles has been challenging, so we recruited two mental health nurses who have successfully provided local services with great results.”
MPHN also funds dedicated mental health nurses into general practice and Riverina Medical and Dental Corporation. One clinician shared how two of his clients participated in five sessions of Written Exposure Therapy (WET), which resulted in major diminishment of trauma symptoms allowing both to be discharged much earlier than by ‘treatment as usual’. It’s another example of how alternative approaches to mental health and AOD services is providing much needed services to the Murrumbidgee community.
For young people, headspace centres in Wagga Wagga and Griffith provide valuable mental health supports. MPHN’s Portfolio Manager Maya De Mattia oversees the contract management of both saying “Wagga Wagga has provided
Spencer McGill, MyStep Peer Support Worker
18 | Annual Report 2021-2022
support to the region’s young people well above national centre averages and achieved a 90 percent client satisfaction rate, while Griffith has achieved an 88.5 percent client satisfaction rate. Youth Reference Groups at both centres are active and pivotal in guiding funding activities. And, there are now two fully trained Aboriginal Health Workers available to support young people.” Both headspace centres receive outreach AOD services to young people too.

Directions provides AOD supports more broadly across the region under the Murrumbidgee Pathways program. It involves pre and post rehabilitation support to gain employment and is available more broadly across the region. Sam* who had a dependency on methamphetamine, participated in the program and has retained his job and paid off his debt. He continues to take steps to maintain abstinence by spending more time with family and friends who support his AOD-free choices.
AOD support is also available for pregnant women and new mothers through the Women’s Wellness and Recovery program delivered by Calvary Health Care Riverina. Recently, MPHN learned about Maria* who self-referred to the program after concerns she was having with her alcohol consumption and cannabis use. Maria has managed to achieve her goal of reducing her cannabis and alcohol intake. Soon, Maria’s support team received heartening text messages from Maria as she celebrated and shared her sobriety milestones.
“When that first 25-days sober text came through, I was so proud of how well Maria was doing. Then, five days later, she celebrated with a 30-days sober message. It is really inspiring for me as a clinician to see our clients achieve their goals. I am optimistic about Maria’s future. She continues to make effective changes in her life through engagement with our program, and I know she has the skills in her toolkit to continue her sobriety and maintain a healthy relationship with her young daughter,” shared one of Maria’s clinical support workers.
1,533 13,580 total clients occasions of service including 614 occasions of service in Residential Aged Care Facilities Wagga Wagga and Griffith 1,568 5.2 757 8,201 total clients average occasions of service per client new clients total occasions of service Alcohol and other drug (AOD) support programs Mental health and alcohol and other drug (AOD) nurses 117 34 total clients for pre and post treatment total clients through headspace Griffith Wagga Wagga Tumut Gundagai Cootamundra Temora THREE SERVICES OPERATING IN 536 3,166 total clients occasions of service Women’s wellness and recovery 158 total clients 60 288 total clients total occasions of service comprising: 151 in person consultations 137 telehealth consultations “When you are experiencing any issues surrounding pregnancy and motherhood, I cannot imagine going anywhere else.” Client of Gidget Foundation Annual Report 2021-2022 | 19
LIVESsaving
The whole of region approach to suicide prevention and aftercare in the Murrumbidgee region is unique and continues to be regarded as a leading example at both the NSW and national level.
MPHN is proud to lead the Murrumbidgee Suicide Prevention and Aftercare Collaborative of like-minded organisations including service providers, first responders and local, state and federal government representatives and agencies. Together they work closely to implement activities aimed at preventing suicides or providing support to families and communities impacted by suicide events or critical incidents.
For a suicide event or critical incident, the Local Response Group (LRG), which includes MPHN, Murrumbidgee Local Health District, Wellways, NSW Police and NSW Ambulance connects to facilitate suicide prevention activities as well as implement responses in accordance with the Murrumbidgee Suicide/Critical Incident Communications and Response Protocol. This enables the delivery of coordinated and timely response to suicide events and other critical incidents; and to minimise the risk of contagion following a suicide event and other critical incidents.
MPHN’s Senior Manager System Integration Anita McRae said while LRG activity focuses on responses to events, they also work with the Collaborative to support region wide suicide prevention initiatives.
“This year, MPHN led the development of two initiatives under the Collaborative’s guidance. First is the STOP campaign which encourages community members who are at crisis point to stop, take a breath, focus on one thing at a time and to pick up the phone as part of a new suicide prevention campaign,” Anita explains.
The campaign, which was made possible with a grant from the headspace NSW Community Collaborative Grants program, features four local people one of which was Murrumbidgee Men’s Group co-founder Rhys Cummins. “When someone is having suicidal thoughts, it can be like tunnel vision. You can’t seem to focus on anything else and it can be difficult to know what to do,” Mr Cummins says.
The second initiative guided by the Collaborative was the establishment of the Wellbeing: Connect and Share series in April 2022. The webinars are designed to educate, inspire and share learnings as well as provide an opportunity for networking and connection for community groups and individuals across the Murrumbidgee region.
The first webinar’s key address was from Gotcha 4 Life’s founder Gus Worland, and according to MPHN’s Mental Health, Alcohol and Other Drugs Manager Maja Asmus the premise of the series is to provide a space for community groups to connect with each other and service providers.
“We know a whole of region approach to suicide prevention is critical, and across the Murrumbidgee service providers, first responders and government agencies are well connected. However, with a number of existing community groups and more groups being established to support specific people like veterans or bereaved parents, the Collaborative was looking to create an opportunity for these groups to connect with each other and to services around the region,” Maja explains.
While MPHN plays a critical role in both the Collaborative and LRG, it also funds Wellways to deliver suicide prevention and aftercare services including The Way Back Support Service, Peer Enhancement and the Murrumbidgee After Suicide Support Program.
For Miranda* her suicide ideation led her to being a participant of The Way Back Support Service. At the completion of the program she said her participation had been life changing.
“It doesn’t matter if you think your problems are smaller compared to someone else’s, we all deal with emotions and situations differently. Your feelings do matter. After getting the help I feel fulfilled, happy, empowered, determined and excited for what the future holds. It’s an ongoing journey but it’s comforting knowing I’m not alone.”
But for those who are feeling a little more apprehensive about accessing The Way Back Support Service, engaging with the Peer Enhancement’s Peer Care Companion is an option. Wellways Regional Manager Zoe Evans said it facilitates peer-to-peer rapport and guidance.
“One participant who was hesitant about speaking with a clinician would meet their Peer Care Companion in a local park to get to know each other and build trust. In the end, the participant was able to relax and open-up about her experiences which has led to her feeling happier and better equipped to remove herself from situations having a negative impact on her mental health.”
While The Way Back Support and Peer Enhancement services focus on supporting someone with suicide ideation, the After Suicide Support Program supports people bereaved by a suicide death. Zoe says the supports are as unique as the people and communities accessing the services.
“Irrespective of the supports provided, it’s the tools and skills learned that can have the greatest impact. For example, a participant of the After Suicide Support Program said she shared the grief and bereavement resources with a colleague experiencing intense shock, grief and regret following the sudden death of her mother,” Zoe describes.
*Not real name
20 | Annual Report 2021-2022



Wellbeing Connect and Share series STOP campaign advertisement Murrumbidgee suicide prevention and aftercare collaborative members • ACON • Catholic Schools Office • Centacare South West NSW • Dr Joe McGirr MP, State Member for Wagga Wagga • Hay Aboriginal Medical Service • headspace Griffith • headspace National • headspace NSW Community Collaborative • headspace Wagga Wagga • Griffith Aboriginal Medical Service • Griffith City Council • MPHN • Lifeline • LikeMind Wagga Wagga • Marathon Health • Mindframe • Ms Steph Cooke MP, State Member for Cootamundra • Multicultural Council – Griffith • Multicultural Council – Wagga Wagga • Murrumbidgee Local Health District • NSW Ambulance • NSW Department of Community and Justice • NSW Department of Education • NSW Police • Regional NSW • Relationships Australia • Riverina Aboriginal Medical and Dental Corporation • Riverina and Murray Joint Organisation • Riverina Murrumbidgee and Murray Alliance • Riverina Eastern Regional Organisation of Councils • The Hon. Michael McCormack MP, Federal Member for Riverina • The Hon. Sussan Ley MP, Federal Member for Farrer • Viney Morgan Aboriginal Medical Service • Wellways total clients total clients total clients occasions of service occasions of service clients in group sessions group sessions 212 54 918 5,401 919 484 37 THE Way back support service Peer Enhancement After suicide support program Annual Report 2021-2022 | 21
Local solutions sought for primary health care in theafter-hours period
In addition to the continued services of the Wagga GP After Hours Service and the Wagga Women’s Health Centre, work continued on regional approaches to after hours primary healthcare with pilot locations determined to devise tailored solutions.
For many people living in regional and rural communities, accessing primary healthcare services for urgent health concerns when their GP is closed often results in a trip to the emergency department.
After the 2020/2021 review into after hours primary care services across the region, MPHN commissioned Larter Consulting to undertake co-design activities to develop flexible and locally appropriate options for accessing primary health care services outside of regular working hours.
In March 2022 work commenced on stakeholder consultation and co-design in Griffith and Leeton, and across the catchment of Berrigan, Finley and Deniliquin. The stakeholders engaged included community members, health workforce from general practice, Aboriginal medical services, pharmacy, and aged care, as well as community based local health advisory groups and councils.
MPHN’s Executive Integration and Partnerships Narelle Mills said findings from the consultations and co-design sessions shows a one-size-fits-all approach is not always the solution.
“We need to work directly with communities to develop suitable after hours measures that take into consideration the

local workforce constraints, and what services would be used by the community. This could be anything from supporting general practices and pharmacy to provide services in the after hours period, upskilling existing workforce, to looking at commissioning telehealth services” Narelle explains.
“The best possible care option for people with urgent, nonlife threatening concerns is to see their regular GP. If the GP is not available in the after hours period, then establishing services that are linked to their regular GP is critical to ensuring continuity and coordination of care. I’m looking forward to continuing the pilot initiatives and learning how we can provide further support to other communities.”
For people living in or near to Wagga Wagga, the Wagga GP After Hours Service provides people with another option to access care. It’s a well accessed service with the 43 GPs on a rotational roster from eight Wagga Wagga clinics, undertaking 4,885 patient consultations and 123 home visits to residential aged care facilities.
Chair of Wagga GP After Hours Service Management Committee A/Prof Ayman Shenouda said the commitment from the staff is exemplary.
WHAT THEY SAID
occasions of service (individual) group sessions 755 477
“Thank you for rescuing me.” “I feel so much better after talking to you. I know what my options are.” “I’m so grateful for this service and the staff.” “It felt great to get stuff off my chest.” “That was easier than I thought it would be. You made it very comfortable.” “Thank you for everything you’ve done.” 22 | Annual Report 2021-2022
WHAT THEY SAID
“Given the challenges for medical practices in the current operating environment, the fact that all service staff, both clinical and support, continue to provide this important primary healthcare service to the community of Wagga Wagga, 365 days per year, is an amazing achievement,” A/ Prof Shenouda praises.
“This year we have seen increased consultations, and as we moved into winter, the flu season and increased COVID positive cases resulted in peak demand for the service. This coincided with increasing demand at the emergency department, and as part of the combined MPHN and MLHD winter strategy, the clinic was able to increase shifts and a broader marketing campaign undertaken to promote the various options for after hours care.”
While the Wagga Women’s Health Centre is located in Wagga, services to support women experiencing family violence is available region wide. MPHN’s Portfolio Manager Maya De Mattia said geography and COVID-19 restrictions have enabled the service to pivot to provide more telehealth services.
“The Wagga Women’s Health Centre has successfully moved to providing more telehealth services for women to be able to access individual counselling services. Access to traumainformed counselling services using both a mix of in-person and telehealth options has been a focus for both individual and group sessions. However, most importantly, women have the ability to access services after hours,” Maya explains. Participants accessing after hours services find them valuable with one client saying she could “engage in counselling on a day when I don’t have to work and can spend time after the appointment focusing on my emotional wellbeing and self care, rather than rushing back to work.” While one Sunday Yoga participant says she feels “more relaxed and helps my blood pressure”.
Maya said the positive feedback shows how the service supports the safety of women experiencing family and domestic violence. “The women accessing the various after hours services have trust in the employees and they feel respected and valued. This goes a long way to building their individual self-esteem and self-worth, and community connections, while simultaneously reducing social isolation and loneliness.”
“I visited the practice last night at 8pm with my 17-month old. I just wanted to let you know how brilliant the doctor was, I left feeling very satisfied.”
Wagga GP After Hours Service patient
Congratulations to the WGPAHS team who have contributed 10 years or more of service • A/Prof Ayman Shenouda • Dr Samiah Azab • Dr Enas Aziz • Dr Jodi Culbert • Dr Megan Elliott-Rudder • Dr Alison Gilmour • Dr Carl Henman • Dr Lee Jeffery • Dr Hanaa Mishricky • Dr Charles Oliver • Dr Joanne Osborne • Dr Enas Sedrak • Dr Marietjie van der Merwe • Julie Bailey • Jan Campbell (retired November 2021) • Sarah Larwood • Sharon Rogers (retired January 2022) KOORINGAL MEDICAL CENTRE BLAMEY STREET SURGERY MORGAN STREET HEALTHCARE CLINIC CENTRAL WAGGA MEDICAL RIVERINA FAMILY MEDICINE WAGGA WAGGA MEDICAL CENTRE GLENROCK COUNTRY PRACTICE HAMMOND HEALTH thank you Annual Report 2021-2022 | 23
Culturally safe services and workforce deliver results
MPHN supports a range of programs for First Nations people, participates in the Murrumbidgee Aboriginal Health Consortium, and facilitates cultural awareness training with the aim of improving cultural understanding and ultimately closing the health gap.
Understanding the needs of Aboriginal Torres Strait Islander people is critical to ensure services are delivered in a culturally safe and sensitive manner.
The Integrated Team Care (ITC) program is designed to improve the capacity of Aboriginal and Torres Strait Islander people to self-manage their complex chronic diseases.
While Marathon Health delivers the ITC program to First Nations people accessing mainstream general practice, this year MPHN decentralised the service delivery for AMSs to provide local autonomy through the individual services; Riverina Medical and Dental Aboriginal Medical Corporation (RivMed), Griffith Aboriginal Medical Service (GAMS), and Cummeragunja Housing and Development Aboriginal Corporation (Viney Morgan).
“The shift to three individual contracts has allowed each AMS to deliver the program to meet the needs at the local level. To ensure each consumer experience is the same regardless of the provider, MPHN established a Community of Practice in late 2021. The monthly meetings are well attended, and feedback shows sharing learnings and ideas for how to manage challenges is valued. Workforce support through initiatives like communities of practice, not only strengthens skills and capacity, but provides opportunities to further enhance client outcomes,” MPHN’s Senior Manager Commissioning Janelle Dufty explains.
One ITC client, Tracey* aged 60, was referred by her GP after a recent invasive breast cancer diagnosis. This was in addition to an existing chronic respiratory condition. Tracey was also caring fulltime for her teenage granddaughter and was feeling overwhelmed with her health and financial situation. MPHN’s Portfolio Manager Donna Jeffery said Tracey was guided and supported through a range of activities available as part of the ITC program.
“Tracey’s Care Coordinator attended GP and other specialist appointments, acted as GP-client liaison between appointments, referred her to an oncology social worker and nicotine cessation support, helped navigate My Aged Care, arranged financial support for travel and accommodation and liaised with Tracey’s GP to complete a Disability Support Pension application,” Donna describes.
Speaking about her experience, Tracey says “I am very grateful for the help. I had no idea about any of this. I didn’t know what to do. I was so scared about the stress on my granddaughter. Thank you for taking some control and asking some questions on my behalf and helping me get through. I feel stronger to deal with this now.”
Like the ITC program, Work it Out provides practical supports for First Nations people who are at risk of losing, have difficulty in gaining, employment, or are at risk of dropping out of education due to substance dependency. The program is staffed entirely by Aboriginal and Torres Strait Islander workers and delivered locally by Directions under Murrumbidgee Pathways.
“Work It Out consistently receives high client satisfaction results, and the strong rapport built between the client and support worker contributes to this, with clients reporting they feel welcomed and respected when accessing the service,” explains MPHN’s Portfolio Manager Maya De Mattia.
“Outcomes for clients are equally important. One Work It Out client who gained and now maintains fulltime employment reports his job provided him structure and purpose and has significantly improved his feelings of isolation.”
248 13,288 2,874 10,441 INTEGRATED TEAM CARE telephone consultations new referrals total consultations comprising of: in person consultations 128 137 WORK IT OUT total clients epsiodes of care Client Satisfaction Questionnaire (CSQ) results: 100% 96% of clients reported they would recommend the service to a friend of clients rated the quality of services as “Excellent” and 6% as “Good” 24 | Annual Report 2021-2022
Murrumbidgee
membership
• Aboriginal community participants
• Riverina Aboriginal Medical and Dental Corporation
• Griffith Aboriginal Medical Service
• Cummeragunja Housing and Development Aboriginal Corporation (Viney Morgan)
• Riverina Murray Regional Alliance
• Local Aboriginal Land Council representatives
• Murrumbidgee Local Health District (MLHD)
• MPHN
• Non-Government agencies delivering Aboriginal wellbeing initiatives aligned with the Aboriginal Health Consortium Plan.
Guiding MPHN’s activities to support the health, wellbeing and cultural understanding of the region’s First Nations people is the Murrumbidgee Aboriginal Health Consortium. Comprised of several organisations supporting Aboriginal people from across the region, the Consortium works with the community to coordinate actions to improve the wellbeing of the region’s First Nations people. Consortium Chair Stacey O’Hara said the holistic approach to health and wellbeing was key.
“Wellbeing in our purpose isn’t just the physical health of an individual but refers to the social, emotional and cultural wellbeing of the whole community in which each individual is able to achieve their full potential and thereby bring about the total wellbeing of their community,” Stacey says.
In April 2022 Melinda Green stood down as Consortium Chair and GAMS CEO Stacey O’Hara was elected in the role.
“I would like to thank Melinda for her contribution to the Consortium, both as Chair and member for many years.”
In her role as MPHN’s Aboriginal Health Strategy and Programs Manager, Melinda also led the implementation of cultural awareness training for MPHN staff, commissioned service providers and general practice staff. Facilitated by Coolamon Advisors Group, the training provided participants with an increased knowledge of First Nations history, culture and health, enhanced skills in working effectively with Aboriginal and Torres Strait Islander people, and strategies and resources to improve cultural safety within their organisation.
*Not real name
CULTURAL
TRAINING
Aboriginal Health Consortium core
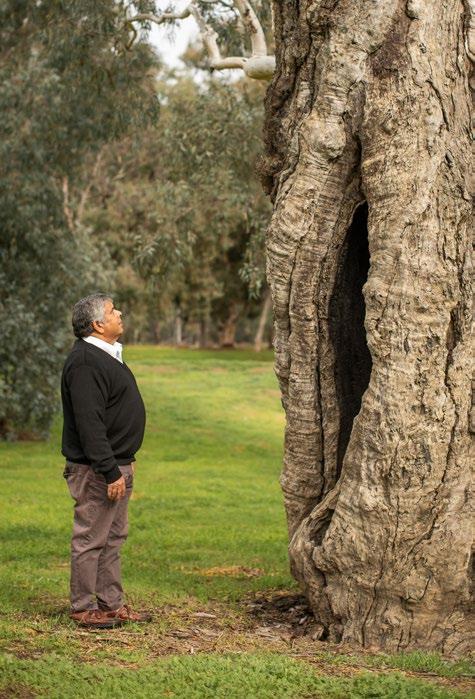
Greg Packer,
Tell it Well storyteller 136 36 57 42
AWARENESS
people undertook Cultural Awareness Training with Coolamon Advisors MPHN staff employees of MPHN’s commissioned service providers of the region’s general practice staff Annual Report 2021-2022 | 25
AGEINGhealthy
With the Royal Commission into Aged Care Quality and Safety identifying the need for significant reform within the aged care system, MPHN has continued to work collaboratively with a range of aged care stakeholders to improve health outcomes for our older communities.
A total of 20.8 percent of people living in one of the Murrumbidgee’s 508 communities are aged 65 years or more. This is higher than both the NSW and national figures which are 16.7 percent and 16.3 percent, respectively. It’s certainly top of mind for MPHN’s Senior Manager System Integration Anita McRae who oversees the organisation’s various activities designed to support healthy ageing.
“As one of the seven priority areas for PHNs nationally, supporting older Australians is a critical component of our work and in the context of the Royal Commission findings and our ageing population, MPHN is committed to working with all health professionals who support older people,” Anita explains.
MPHN’s Healthy Ageing and Palliative Care Manager Stacey Heer works closely on these projects and said the aged care sector has experienced several challenges throughout the year.
“It’s been an unprecedented and highly challenging year for the aged care sector for many reasons including COVID-19, aged care reform and significant workforce challenges. Despite the challenges, I’ve witnessed the incredible resilience, commitment and compassion of our region’s aged care workers and leaders,” Stacey says.
“The support MPHN has been able to provide to our aged care health workforce has certainly alleviated some of the pressures, and it’s had the added benefit of fostering strong relationships.”
One way these relationships have been developed is through the implementation of a regular community of practice meeting with Residential Aged Care Facilities (RACFs). One participant of these meetings has been Allawah Lodge’s, Aged Care Services Manager Simone Fuller.

“The community of practice meeting is the reason I have remained working in aged care. Previous to this meeting commencing, I felt very isolated and overwhelmed. It has been a game changer and I always go away with something from every meeting,” Simone details.
The relationships developed between MPHN and RACFs have enabled support for virtual health consultations; installing a best practice in pain management validated clinical software tool; access to in-reach mental health supports; guiding RACF after-hours action plans to help avoid unnecessary hospitalisations; providing COVID-19 updates and supporting access to personal protective equipment.
Another way MPHN has been supporting the health workforce caring for older people has been a recent partnership with Dementia Australia and MPHN’s Murrumbidgee HealthPathways program.
MPHN’s Murrumbidgee HealthPathways Manager Briohny Hart said service and referral mapping, creating new, and reviewing and updating existing HealthPathways and pages has been the focus.
26 | Annual Report 2021-2022
“Eighteen pathways or pages relating to older persons’ health have been created or updated in the last financial year to ensure clinicians have access to the most current local information about assessment and referral pathways. All new pathways are developed in collaboration with MPHN and MLHD’s aged care teams, including subject matter experts in aged care such as geriatricians, Dementia Australia, and pharmacists,” Briohny explains.
“Our goal with the localised HealthPathways is to support independent living for older community members as long as possible, and we will continue to work with clinicians to develop pathways to guide, support and assess patient care.”
Supporting older people to live well at home for longer is an aim of the Vitality Passport programs delivered by Back on Track Physiotherapy. The programs encourage an holistic approach to health and wellbeing through exercise, nutrition and cognition activities. This year Vitality in the Community expanded its geographical reach and developed additional program resources.
Back on Track Physiotherapy Director Jeremy Carr said the expansion doubled service delivery and capacity, despite limitations of COVID-19.
“All of our Vitality programs receive very positive feedback from participants, but the most telling story is in the numbers. More than 80 percent of participants report either a reversal or halt to their frailty risk. This means they are living well and improving their health outcomes,” Jeremy explains.
“The Vitality program delivered in RACFs was a little more challenging to implement with various COVID-19 lockdowns in place, however, we know this program requires clinical continuity to ensure the best conditions for participants living with dementia.”
Connect with Vitality was another initiative specifically aimed at connecting with older people to support their mental health after the impacts of COVID-19 isolation.
While the program finished in December 2021, one Connect with Vitality participant and Coleambally resident praised the program highly saying he believes “very strongly that the Vitality Passport programme should be a National Programme because it is an excellent health tool to refer to and to study.”
MPHN has also continued to contribute to the Murrumbidgee
Consortium and commenced consultation to establish a new aged care finder program.
Aged Care
Vitality in the community Vitality in RESIDENTIAL AGED CARE FACILITIES Connect with vitality Cootamundra West Wyalong Coolamon Barooga Hillston Cowra Mulwala Deniliquin Hillston Tumut Coleambally Goolgowi Cowra Griffith Coleambally Gundagai Wagga Wagga Coleambally Moama Cowra Howlong WHAT THEY SAID “The exercises are a real eye-opener for me; learning that they are meant to be done slowly and not too many at once.” “I found the sessions with the dietitian and occupational therapist very helpful.” “Now I am much more active and making sure I am eating better and adding protein to meals.” LOCATIONS LOCATIONS LOCATIONS 180 98 125 51% 10% 45%32% 71% 43% clients participants participants reversed their frailty risk reversed their frailty risk reversed their frailty risk halted their frailty risk halted their frailty risk halted their frailty risk Annual Report 2021-2022 | 27
LIVING healthily
There are many facets to healthy living. There’s addressing a specific health ailment or injury through a dedicated clinician, there’s managing chronic conditions, and then there is staying well and healthy. How effectively people stay healthy often is a result of their health literacy and their social determinants of health.
There’s no better way to promote healthy living than looking at grassroots community-led initiatives, and in April 2022 MPHN did just that by opening a new round of Murrumbidgee Community Grants for activities to strengthen social connectedness and enhance physical and mental wellbeing. A total of $224,520 was shared among 41 grant activities, including community festivals, first aid training, and wellbeing workshops and programs.
The Lockhart Local Health Advisory Committee (LHAC) received $9,920 to deliver a range of community events. Chair Fran Day says the various events will make a real difference to the community.
“Our grant will allow a range of social inclusion and participation activities suitable for all ages such as social events, student workshops, health checks, group fitness and a seniors expo. Thank you MPHN for making these grants available - the importance of strong social connections cannot be underestimated in improving health and wellbeing,” Fran says.
Equally important is being able to navigate the health system. MPHN’s Integrated Care Coordination (ICC) and Health Navigator Support Service programs do just that. Contract Administrator Melissa Billingham says “the changes these programs can make in people’s lives is really evident. Having knowledge of how and when to access services and an understanding of your health conditions is vitally important to living healthy and well.”
The ICC and Health Navigator programs are delivered by Marathon Health, with the ICC program connecting participants to the right health and social services in relation to their complex chronic conditions.
“Care coordinators work to connect participants with necessary services, coordinate and attend health appointments to support in health information translation, and support medication scheduling. This helps reduce the feeling of being overwhelmed and enables participants to better self-manage and help them to a live a more manageable and symptom-free life,” Melissa says.
It’s a program delivering results. Survey results for April – June 2022, show 90 percent of clients report improved health and wellbeing. One of these clients, Sally*, a 46-yearold woman living with her daughter in Wagga Wagga, lives with a range of musculoskeletal and neurological chronic conditions and was referred to ICC by her GP. She received help coordinating and attending medical appointments,
navigating the health system, improving health literacy and understanding, and referrals to allied health and mental health supports through enhanced primary care planning. Sally says she feel better supported with her Care Coordinator at her appointments. “I feel that having someone there to advocate for me helps to achieve positive outcomes, which wasn’t the case before.”
ICC clients can also access the Health Navigator Support Service for practical social and living support. The aim is to engage participants in community and social activities, improve self-care and lifestyle choices, and build resilience and confidence.
Wayne*, 51, required support with making social connections and domestic living. Through the program he was able to move into a group home during the week and return to his home on weekends. Wayne says “I love living with people and last night I assisted to mash the potatoes. I have never been taught or shown that before and it makes me very happy to help out in the house. I love collecting the eggs and watering the garden.”
WHAT THEY SAID
“I love living with people and last night I assisted to mash the potatoes, I have never been taught or shown that before and it makes me very happy to help out in the house. I feel like I am helping out. I love collecting the eggs and watering the garden (at the respite house).”
Wayne 28 | Annual Report 2021-2022
Similar to the Health Navigator is WARATAH’s Health Linker role which ensures patients engaged with WARATAH (Wellness And Resilience Achieved Through Allied Health) are supported more broadly in accessing health and social supports. The service is welcomed by patients and clinicians alike, as it makes accessing and navigating the health system more streamlined. Talking about her experience Julie* says her Health Linker “listens to my needs and I know that she genuinely cares and is not just ticking a box for the sake of her job.”
WARATAH services are provided to 28 different locations across the Murrumbidgee, and in a 12-month period more than 4,100 services have been delivered in podiatry, diabetes education, dietetics, and physiotherapy. Under other funded programs, MPHN has also provided more than 1,500 allied health services for respiratory education, speech pathology and foot care (nurse delivery).

In addition to funding established programs and grants, MPHN supports dedicated marketing campaigns aimed at seasonal preparedness for flu (Winter Strategy) and asthma (Asthma/Spring Thunderstorm). This year MPHN added a new television commercial to the Winter Strategy campaign to promote the various things you can do to be winter ready such a preparing a sick day action plan.
*Not real names
290 4,110 237 51 1,342 2,013 755 INTEGRATED CARE COORDINATION HEALTH NAVIGATOR new clients total occasions of service comprising:100 1,545 telephone consultations internet/other consultations total clients total services new referrals people discharged in person consultations 272 1,273 telephone consultations in person consultations Annual Report 2021-2022 | 29

30 | Annual Report 2021-2022
PALLIATIVE CARE one-of-a-kind
Improving equity in access to quality palliative care is an Australia wide challenge and one Murrumbidgee general practice is the first in Australia to implement an innovative program to better support palliative care patients.
The Hay Medical Centre, under the leadership of Dr Muhummad Arshed, is leading in evidence based primary care management of palliative care through involvement with MPHNs At Home Palliative Care project and the Palliative Care Outcomes Collaboration (PCOC).
The project focuses on enhancing local palliative care service provision and improving access to safe palliative care services in primary and community care.
With support from MPHN, Dr Muhummad Arshed has implemented PCOC into his practice processes, and said every palliative patient in his care receives a standardised palliative care assessment to ensure they receive best practice care.
“We know most expected deaths in Australia are due to chronic conditions and I realised there was a large cohort of patients who were not receiving the benefits of early identification of palliative care needs and routine palliative care assessment,” Dr Arshed explains.
“We found only certain patients with malignant conditions were having their palliative needs regularly assessed and addressed, and in response we created a new practice process to identify which of our patients with chronic conditions might have palliative care needs and therefore were likely to benefit from the PCOC program.”
For the practice to be able to easily identify at-risk patients, MPHN palliative care staff worked closely with health analytics software provider, Pen CS, and the Hay Medical Centre, to develop a filter recipe allowing the practice to produce a list of patients with a chronic condition and a likely shorter prognosis of one to two years. This list is then reviewed using the prognostic question ‘would you be surprised if this patient died in the next year?’ If the answer was no, then that patient is entered into the PCOC program.
“We are currently the only general practice in Australia who has implemented this program. Now our patients are assessed regardless of diagnosis or setting of care, which ensures their palliative care needs are identified early and addressed.”
The benefits for both community and general practice have been impressive and according to Dr Arshed, are leading to sustainable practices in quality palliative care and less complications for family and carers.
“This new process strengthens the patient and carer voice, which ensures patient centred care. The regularity of the process works to eliminate crisis, especially in out of hours periods, which is also helping to prevent emergency room presentations and hospitalisations.”
“We are also seeing some fantastic benefits within the practice as well with better use of GP time, and a focus on best use of clinical skills of our practice nurse.”
The remarkable work and results achieved by Hay Medical Centre and others across the region in response to the palliative care challenge is gratifying to MPHN’s Healthy Ageing and Palliative Care Manager Stacey Heer and her team, but Stacey knows there is more work to be done.
“We need to continue to promote having conversations about death so people are more willing to engage in this often difficult but important discussion. Community capacity around death literacy and encouraging people to engage in meaningful end of life planning, will lead to people with chronic disease being more open to having real conversations about their goals for end-of-life care.”
MPHN is supporting the roll out of the overall At Home Palliative Care Project in several general practices across the region and Stacey is passionate about its implementation.
“We must get this right. Access to palliative care should be based on need, and often this is not the case in Australia. You’re far more likely to be referred to a palliative care team if you have a cancer diagnosis and live in a metropolitan area. There are many population groups who are disadvantaged – First Nations, people who are incarcerated, LGBTIQ+ community members, and we also know accessing palliative care in aged care facilities remains a challenge,” Stacey says.
“We have worked with some remarkable local health professionals who have a tremendous attitude towards getting this right and improving palliative care processes and outcomes for their patients, and I am looking forward to continuing support our region’s practices to implement palliative care initiatives.”
Opportunities for general practices in the Murrumbidgee region to participate in the PCOC program and other At Home Palliative Care Project activities will be available throughout the rest of 2022 and 2023.
Annual Report 2021-2022 | 31
HEALTHCARE PROFESSIONALS
“Despite the ever-changing COVID-19 landscape our region’s health professionals continue to deliver quality care to their patients while also ensuring a return to more ‘business as usual’ activities. Key to supporting our primary healthcare workforce was MPHN’s capable COVID-19, Primary Care Engagement, HealthPathways, and Aged and Palliative Care teams. Nothing was too big or small and their support was welcomely received by all. In fact, collaboration, not only between MPHN’s teams, but between the Murrumbidgee Local Health District and primary health care providers has lead to many innovations and improvements across the health system. It really is inspiring, and I am looking forward to these collaborations continuing.”
Andrew Heap Senior Manager Primary Care Engagement

supporting in this section
Cross team collaboration enhances general practice

Supporting workforce recruitment and retention Response, recovery and resilience
Congratulations to our 2021 Primary Healthcare Award winners
32 | Annual Report 2021-2022

Annual Report 2021-2022 | 33
ENHANCES GENERAL PRACTICEcross team collaboration
While COVID-19 support has dominated, the team has worked collaboratively across their areas and the organisation to leverage opportunities to further support primary care across the region.
MPHN’s Primary Care Engagement team’s primary purpose is to support general practice and other primary healthcare providers by working on a range of projects and activities including COVID-19, quality improvement, digital health, Murrumbidgee HealthPathways, Continuing Professional Development (CPD), workforce recruitment and retention, seasonal planning and immunisation. It’s a large portfolio of work, and key to the team’s success has been a real focus on working across the various projects and activities within the team and across the organisation to coordinate and support primary care engagement.
Senior Manager Primary Care Engagement Andrew Heap said the team have worked hard throughout the year to support primary care providers despite the ongoing challenges of COVID-19.
“Even with the demands of supporting general practice, pharmacy and residential aged care facilities in relation to COVID-19, the team achieved more than 2,500 practice visits either in person or virtually, 236 practice engagements supporting childhood immunisations, nearly 1,000 people attended professional development opportunities, all eligible general practices and nearly all eligible pharmacies were enabled to use and accept ePrescriptions,” Andrew states.
“It’s been a big year and I am proud of the dedication and enthusiasm of the team to go above and beyond to support the health providers who diligently ensure our communities are well and safe.”
Supporting patient consultations
Key to this success has been looking for opportunities to support primary health providers with various tools to streamline patient consultations. One such tool is GoShare Healthcare, which is an intuitive online tool for health practitioners to customise and send health information to patients via email or SMS. In the Murrumbidgee region, 35 of the 89 general practices have registered to use the GoShare platform.
“General practices are able to incorporate GoShare into their routine practice workflow and the team is working to engage practitioners to utilise the platform effectively and seamlessly to support patient health literacy, knowledge and selfmanagement,” Andrew explains.
To date there have been 4,505 information bundles sent including Why you should get your flu shot this season, COVID vaccinations, COVID precautions, 45-49yr health checks, 75+yr health checks and Heart Health checks.

In addition to GoShare, Murrumbidgee HealthPathways supports clinicians with assessment, management and local referral information. MPHN’s Murrumbidgee HealthPathways Manager Briohny Hart said under the guidance of an active steering committee, almost 100 pathways and pages were developed or updated in line with key priorities this year. “This year’s focus was to ensure pathways were established or updated to further support commissioned services or
identified needs, initiatives or focus areas. For example, with the implementation of the Enhanced Paediatrics in Primary Care program, we localised child and youth health paediatric pathways, Aboriginal and Torres Strait Islander people pathways were updated to support the Integrated Team Care program, and pathways for older people were updated in relation to both dementia and aged care,” Briohny says.
“The HealthPathways team implemented state-based pathways for SafeScript and COVID-19 and this relied on Primary Care Engagement teams to support training and implementation.”
34 | Annual Report 2021-2022
Supporting digital health technologies
The digital health team worked on the Australian Digital Health Agency (ADHA) project to upgrade NASH certificates and eRequesting to electronically request pathology tests across the region, achieving 98 percent 40 percent respectively of upgrades for the region’s general practices, pharmacy and medical specialists. The team also engaged with medical specialists and community health organisations to register them for the My Health Record system.
The team also provides support in relation to ePIP (Practice Incentive Payments) compliance, telehealth and secure message delivery.
“Through our review process, we identified four general practices not receiving their ePIP and worked with Medicare, clinical software vendors, and IT support to reconnect My Health Record and assist them to continue to receive the ePIP,” explained MPHN’s Digital Health Officer Vimal Pasupathy.
Implementation of NSW Health’s SafeScript, which assists general practitioners with real-time notifications for high-risk medications to reduce doctor shopping, was also supported by the digital health team with general practice and pharmacy implementation.
•
Healthpathways
committee
Supporting quality improvement
MPHN also provides general practices an opportunity to share de-identified data, which is used to generate Quality Improvement (QI) Benchmark Reports for participating practices.
Primary Care Engagement Team leader Alison
said there has been renewed interest in quality improvement and these reports are helping practices to get back to business as usual.
“Our QI Benchmark Reports are a useful tool to guide practices with their quality improvement activities and identify opportunities to improve patient care.

The Primary Care Engagement Officers review their practices’ reports in detail to provide suggestions for improvements, such as coding to recall patients with or at risk of chronic diseases, and easy identification of overdue routine health assessments to help foster streamlined systems and processes,” Alison explains.
“The team also identifies missing health summary data to support practice accreditation requirements.”
Jansen
steering
• Dr Marietjie van der Merwe (Chair) – Senior Lead GP Clinical Editor HealthPathways • Dr Jane Goddard – GP Clinical Editor HealthPathways
Dr Jane Laloma – GP Clinical Editor HealthPathways • Dr Genevieve Thompson – GP Clinical Editor HealthPathways • Dr Elizabeth Campell – GP Clinical Editor HealthPathways • Dr. Isabel Paton (PhD) – MLHD Community Care Manager - Integrated Care & Allied Health • Andrew Heap – MPHN, Senior Manager Primary Care Engagement • Briohny Hart – MPHN, HealthPathways Manager • Olivia D’Souza – MPHN, HealthPathways Coordinator
Annual Report 2021-2022 | 35
Supporting professional development
Underpinning the practice and patient supports to general practice, pharmacy and other primary healthcare providers are regular opportunities for relevant and accredited professional development. MPHN’s CPD Coordinator Edyta Wrobel said it was important to provide training opportunities relevant to the current environment.
“Obviously with the ever-changing COVID-19 environment, promoting and supporting a range of COVID specific CPD events was important and necessary for our primary healthcare providers. However, there were other key CPD events linked to specific team activities such as GoShare,
ShareScript and the annual Immunisation Update,” Edyta explains.
“Our 2021 Immunisation Update workshop had 98 registrations and 71 attendees, consisting of practice nurses and nurse immunisers from MLHD and the Kapooka Defence base.

“Like the Immunisation Update the Antenatal Shared Care CPD event is always very well received, with workshop facilitators including a local GP obstetrician, who dedicate their time to share a wealth of knowledge to upskill local GPs in providing antenatal care for their patients.”
congratulations to
Supporting seasonal planning and immunisations

Eighteen general practices participated in the Living Well, Your Way Winter Strategy program, which included MediCoach coaching sessions. Relevant MPHN staff attended sessions to support practices with their Practice Action Plans like archiving old patient records, coding improvements, updating management processes, and recalling at-risk patients.
MPHN’s Immunisation Support Officer Kate Warren said flu vaccines were a priority for the region given last year’s virtually non-existent flu season.
“With restrictions easing and borders re-opening, this winter saw an influx of both flu and COVID, and one measure to support practices was a presentation to the Practice Manager Network about recalling vulnerable patients for flu vax using GoShare Plus,” Kate says.
“It was also critical for MPHN to support practices with the administration of flu vaccines, and also remind people to get their flu shot and to maintain good hand hygiene.”
In addition to supporting flu vaccine administration and promotion, MPHN also supported general practice in the administration of all childhood vaccines.
Dr Gracy Gouda for being awarded Murrumbidgee and ACT Supervisor of the Year at the 2021 GP Synergy Awards in December 2021.
Dr Max Graffen on his retirement September 2021 after 40 years of service to the region. Additionally, Dr Graffen served on MPHN’s Board in its various iterations for a number of years including five as Chair.
36 | Annual Report 2021-2022
SUPPORTING WORKFORCErecruitment and retention
It’s the practical assistance provided by MPHN that’s helping to meet some of the workforce challenges in primary health across the Murrumbidgee.

MPHN’s Team Leader Primary Care Engagement and Workforce Manager Alison Jansen said we offer flexible workforce assistance based on need.
“Practices can approach us directly and let us know they have a vacancy or say ‘I’ve received this CV, can you help us?’. We can assist as a start by promoting vacancies on our website, or providing advice on applicant’s CV noting medical board standard requirements have been met. Medical practitioners also directly approach MPHN specifically looking for opportunities to work in our region,” Alison explains.
“The reality is, recruitment requires a whole of family approach. Practitioners will naturally form collegial bonds, however their family don’t have a ready made network and it’s important to help foster this sense of community. If we get the recruitment right, we have a better chance at retaining our workforce”
Ensuring the doctor and family meet people in the town, connecting to Local Health Advisory Committee members, hospital managers, school and sporting clubs, sourcing accommodation for example, is vital to settling in and retaining our health professionals.
Dr Elizabeth Campbell commenced as a general practitioner at the Lake Cargelligo Family Practice in September 2021.
“Before I moved to Lake Cargelligo, I was working as a General Practitioner in Sydney, with a special interest in women’s health, reproductive health, and children’s health. Since moving to the country, I have enjoyed learning about rural medicine and am enjoying my role as Visiting Medical Officer at the local hospital. I am loving both my work and my life here,” Dr Campbell says.
“Since my arrival, the Murrumbidgee Primary Health Network has welcomed and helped to orient me about their programs, providing helpful information about local services for my patients and education and rural grant opportunities for myself. It has been great getting to know the MPHN team and making connections in the Murrumbidgee region.”
Dr Campbell was one of the 21 new medical practitioners commencing in the Murrumbidgee region during this financial year.
MPHN also offers a range of support to the education and training of medical students from the University of Wollongong while on rural placement. In this financial year, five students enjoyed their time learning and living in the Murrumbidgee.
Dr Campbell celebrates her oneyear anniversary of work at the Lake Cargelligo Family Practice with fellow GP and practice principal Dr Bardawil.
Workforce pressures in the primary healthcare sector have been exacerbated with COVID-19, but on-the-ground support from MPHN is making a difference.
Annual Report 2021-2022 | 37
RESPONSE, RECOVERYand resilience
Delta, Omicron, anti-virals, third and fourth doses, masks mandatory, lockdown, care in the community, get tested, get vaccinated, isolation, RATs, PCR – so many catchphrases from the COVID-19 landscape, but the Murrumbidgee community and health professionals navigated the changes with diligence, coordination and compassion.
As the Delta outbreak took hold across New South Wales, many people living in the Murrumbidgee region were sent back into lockdowns and quarantine in July 2021 to emerge to mask mandates. Then the Omicron outbreak in December sent us racing for Rapid Antigen Tests (RATs), and queuing for PCR tests and waiting for results. Isolation periods have changed, mask mandates have eased, and those QR checkins are a thing of the past.
The ever-changing COVID-rules and environment was challenging to navigate for the community, and general practitioners, practice staff, and other primary health professionals including pharmacy and allied health are to be commended for staying up to date with changes to vaccinations, testing and PPE requirements, and medications and care plans for COVID-19 patients, to ensure they delivered exemplary care to their patients, no matter their need.
The region’s six GP Respiratory Clinics (GPRC) were also pivotal for alleviating pressures on the health system delivering vaccines and tests. Young GPRC’s principal Dr Asitha Wickramaratne explains “the GPRC has been able to

provide thousands of vaccinations as well as being a trusted centre for testing and treatment for COVID-19 positive people. This has resulted in reduced pressure on other health services, including the local hospital.”
The implementation of a Primary Care Clinical Coordinator (PCCC) role within the Murrumbidgee Local Health District (MLHD), was also critical to navigating between primary and acute care settings and increasing confidence for caring for patients in the primary care setting. Andrew Heap, MPHN’s Senior Manager Primary Care Engagement said the role, together with a suite of information sessions has enabled the care of COVID-19 positive patients at home.
“As more and more people were contracting COVID-19 in the first part of 2022, many were being managed in the acute or hospital setting. However, this wasn’t sustainable, so we worked on a model to support transition of care to the primary care setting,” Andrew explains.
“Then anti-viral medications became available and there was much for our GPs to understand to properly care for COVID-19 patients and prescribe the medications.
Primary Care Clinical Coordinator Karen McDowell (R) meets with GP Registrar Dr Shanika Samuel
38 | Annual Report 2021-2022
Information sessions were critical to developing knowledge and understanding. Additionally, day-to-day support was provided by the PCCC role and MPHN’s COVID-19 and Primary Care Engagement teams. Soon GPs became increasingly confident in managing COVID-19 positive patients, either via telehealth or in their practices.”

Karen McDowell, a Primary Care Clinical Coordinator said confidence is high among GPs and COVID-19 diagnosis and support is just business as usual.

“The great thing for me, is watching the growth that happens. So now watching the GPs run ahead with it and we are just
a back up as opposed to the other way around. It’s that normalising of COVID,” Karen says.
additional support for treatment plans is needed the PCCC is always available. For Dr Shanika Samuel, a GP Registrar at KRS Health in Wagga Wagga, a telephone consultation with a young gentleman with an injury and a medical condition who had recently contracted COVID-19 warranted some additional guidance from the PCCC. Unfortunately, because of his age and not being immunosuppressed, the gentleman was not eligible for antiviral medication. It was at this stage Dr Samuel called Karen.
When
600,000 800,000 142 5 550 91 PERSONAL PROTECTIVE EQUIPMENT (PPE) COMMUNICATIONS AND PROMOTIONS VACCINATIONS AND TESTING RESIDENTIAL AGED CARE FACILITIES Facilities where 80-100% of residents have received three vaccination doses Approximately active COVID-19 vaccination sites across the region, including pharmacy of these are general practices General Practice Respiratory Clinics in Deniliquin, Gundagai, Tumut, Young, Wagga Wagga and Griffith of these facilities have seen 80-100% of residents receive four vaccination doses PPE packs ready for distributions; MPHN’s COVID-19 Manager Peta Anderson at Viney Morgan Aboriginal Medical Service 47 27 vaccinations have been ordered by primary care vaccination sites 128 75 6 PPE items or equipment issued to healthcare providers • 43,750 surgical masks • 11,170 P2 masks • 8,090 gowns • 12,720 gloves • 1,790 goggles • 1,790 face shields • 166 bottles of hand sanitiser • 600 pulse oximeters COVID-19 eNewsletters issued to general practice, aged care, allied health, pharmacy and LHAC distribution lists media engagements paid social media campaigns promoting testing and vaccination reaching 185,990 people and 1,135,759 impressions organic social media posts across Facebook, LinkedIn and Twitter reaching almost 142,000 people Annual Report 2021-2022 | 39
“The two of us went through the protocol again, and we both agreed that it was a grey area and didn’t fit the criteria, but we felt this patient was high risk,” Dr Samuel explains.
Together Dr Samuel and Karen were able to make a plan to care for the young man and reduce the risk of deterioration. This was achieved through daily telehealth check ins and sending him a pulse oximeter to measure oxygen levels.
“This is why I love the team that I work with. I look at the GP network, and our network, and I think we are a team of people who care about people. It’s that patient focussed care,” Karen adds.
In addition to the PCCC role to support general practitioners the Murrumbidgee HealthPathways team ensured COVID-19 HealthPathways were regularly updated and maintained.
MPHN’s COVID-19 team provided constant and consistent support by providing updated information and changes, additional PPE, and assistance in ordering vaccinations. Similar PPE support was also extended to the region’s private Residential Aged Care Facilities (RACFs). Perhaps the most challenging times came with the more frequent COVID-19 outbreaks within facilities.
“COVID outbreaks have interrupted vaccination clinics, impacted on facility workforce, PPE supplies, and day-today facility operations,” says MPHN’s COVID-19 Manager Peta Anderson. “MPHN was able to support our privately operated RACFs with the provision of PPE in special COVID-19 bundles including gloves, goggles, face shields, hand sanitiser, masks, and gowns to replenish diminishing supplies.

“We also supported wider vaccination opportunities with pop-up vaccination clinics to remote rural communities to allow everyone the opportunity to be vaccinated regardless of location. These were carefully coordinated with the
Murrumbidgee Local Health District’s mobile clinics to ensure maximum coverage.”
Peta continues saying her role in supporting the region’s primary care and aged care providers has been inspirational and a real privilege.
“Everyone has a great sense of pride in being able to support their communities to live safely with COVID-19. We have had GPs and pharmacists travel to remote and rural communities to administer vaccines. Our residential aged care facilities have provided exemplary care to their residents, but even more so during the lockdown periods when loved ones aren’t able to visit. Everyone is united under the common goal of providing the best care no matter the conditions,” Peta shares.
The hard work and dedication of the region’s primary healthcare providers was recognised with the development of a small ‘Thank-you’ campaign, comprising of video messages from MPHN staff and the community. The workforce responded too – with approximately 30 primary care providers – from general practitioners, practice nurses, allied health providers, and our commissioned service providers thanking their patients and the community for their patience. A short 15-second video was also created for use as a television commercial. All were gratefully received.
“The thank you campaign really was such a small token of the region’s deep appreciation to the primary care professionals across our region. Their dedication to serving their patients while under lots of pressure with the ever-changing COVID-19 landscape is commendable. And then, for so many providers to also contribute to a community thank you in between their usual activities, this demonstrates their commitment to keeping their patients and community safe and well,” Peta says.
THANK YOU TO THE REGION’S GPRC TEAMS
A big heartfelt thank you and congratulations to the GPs, nurses and practice staff at the region’s five GP Respiratory Clinics (GPRC) in Wagga Wagga, Deniliquin, Young, Gundagai and Griffith for your tireless work in providing the community with a central location to receive COVID-19 testing and vaccinations.
40 | Annual Report 2021-2022
to our 2021 Primary Healthcare Award winnersCongratulations
Each year MPHN recognises excellence in primary healthcare and in 2021 the awards were again impacted by the COVID-19 pandemic with presentations taking place virtually and postponed to 10 March 2022.
Despite the challenges of an evolving pandemic, a virtual awards presentation was held to acknowledge the significant contribution of the region’s primary healthcare professionals and initiatives, and four worthy recipients were recognised for their work in what was another challenging year. Outstanding Contribution to Leadership in Primary Healthcare award recipient Kylie Perry was recognised for the establishment and leadership of the Murrumbidgee Pain Hub. Ms Perry paid tribute to the people she has worked with who are dedicated to supporting patients with persistent pain.
“I am very proud of Murrumbidgee Pain Hub and the work we are doing to ensure access to contemporary research and resources for local clinicians,” Ms Perry said.
A Youth Mental Health Forum involving students and staff from 16 regional high schools took out the Promoting Healthy Living award. The initiative was led by headspace, Wagga Wagga, with Manager Shane Thomas acknowledging the young people and schools for their valued contributions to the event.

“I’d like to recognise the efforts of all involved who worked so hard to facilitate an event that is playing an important role
OUTSTANDING CONTRIBUTION TO LEADERSHIP IN PRIMARY HEALTHCARE
Winner: Kylie Perry
Finalist: Brodie Palmer
PROMOTING HEALTHY LIVING
Winner: headspace Wagga Wagga
Finalist: Sunflower House, Dr Heba Azer
in effectively bringing about change regarding mental health and wellbeing,” he said.
Recipient of the Innovation award, The Gidget Foundation, delivered a workforce initiative to improve access to mental health clinicians for Murrumbidgee families. Gidget Foundation Program Director Michaela Durrant said the program was created to maintain a high level of care for people in the region
“The Alternative Workforce Program has allowed us to better utilise the wonderful expertise and resources we have in the region to grow capacity and support more expectant and new parents in need,’ Ms Durrant said.
A unique and valued community gym won the Murrumbidgee Grant of the Year Award. Community member Rob Houghton expressed his appreciation for the recognition and thanked MPHN for the funding opportunity.
“The community has been through a lot but this space is providing life changing benefits to our growing group of members who have become a close unit who value the safety and welfare of each other and the wider community.” Mr Houghton said.
Innovation
Winner: Gidget Foundation
Murrumbidgee community grant of the year
Winner: Gogeldrie Gym
Finalist: Connecting Communities ‘Gather’ events
Annual Report 2021-2022 | 41
and
TRANSFORMATION ONE HEALTH SYSTEM
“People are often not concerned about who is delivering their healthcare or who funds the service, but they do care about how health services work together so they can experience care that is connected and seamless. It’s the premise MPHN operates by when we look at how we can support transformative and integrated health care for our communities. This year we have continued developing collaborative initiatives with our key partners and together we have been working to improve access to coordinated and integrated care pathways and innovative workforce solutions, and this is exciting for our communities.”
Narelle Mills Executive Integration and Partnerships


Living Well, Your Way Community led solutions for primary healthcare in Snowy Valleys Transforming the health of Murrumbidgee children integration
in this section
42 | Annual Report 2021-2022

Annual Report 2021-2022 | 43
LIVING WELL your way
The Living Well, Your Way initiative is the next horizon of integrated care. It aims to improve care in the community, and keep people well.
Peter*, 43, lives in a Murrumbidgee regional community. In July 2021, after presenting to the emergency department with shortness of breath, and lower leg swelling, Peter was diagnosed with heart failure. He stayed in hospital for 10 days, during which time he commenced many new medications. Peter says he ‘wasn’t told much’ about his condition and was confused about how to look after himself at home. Within a week following discharge Peter was admitted to hospital again. Peter says he manages his condition ‘blindly’ on his own and google searches things for better understanding.
Peter’s story was just one of many heard as part of consultation for the development of the Living Well, Your Way care pathway. More than 120 people from pharmacy, general practice, non-government organisations, private medical specialists, community groups, consumers and carers, and private businesses were able to contribute their thoughts on how to improve health outcomes, specifically for people with Chronic Obstructive Pulmonary Disease (COPD) and Congestive Heart Failure (CHF). Many shared stories similar to the experiences of Peter.
The Living Well, Your Way initiative is part of a collaborative commissioning approach between MPHN and the Murrumbidgee Local Health District with the aim to realign the system through a joint pathway of care and improve health outcomes.

Acting Program Director, Sue Massey said the new Living Well, Your Way pathway was designed for and by the people in the Murrumbidgee with chronic disease and their carers.
“Often people living with COPD or CHF experience siloed and expensive care, with regular travel and frequent visits to hospital. We want to help people stay healthier at home for longer and reduce the demand on emergency departments and hospital admissions by providing optimal care in the community,” Sue explains.
“Each step in the pathway has been tested and re-tested with local stakeholders, with clinical input from a clinical advisory group and validation from individual consumers.”
The co-design approach to the new Living Well, Your Way care pathway is something the Patient Centred CoCommissioning Group (PCCG) is extremely proud of, so too is the New South Wales Ministry of Health who recently endorsed its implementation.
MPHN’s Narelle Mills, Executive Integration and Partnerships, is part of the joint governance group overseeing all aspects of the initiative and said the key to the pathway development was to ensure optimal use and alignment of existing resources to the care pathway.
“A key requirement of the Living Well Pathway was to ensure we build on what already exists with the aim to streamline the care process to make it easier for both the patient, and
Ryan Williamson, Susan Massey, Caroline Holtby and Melanie Reeves
44 | Annual Report 2021-2022
their carers and clinicians to navigate the system. Importantly, working in collaboration with the MLHD with shared governance and accountability ensures a ‘joined-up’ care pathway for our communities” Narelle explains.
pathway aims to shift models of care from acute into primary, community and outpatient services and provide alternatives to admitting patients for the purpose of diagnosis or stabilisation of chronic disease. We want people to feel empowered to self-manage their health and to navigate the health care system with confidence.
“Regardless of where you live across the Murrumbidgee region, the pathway should help facilitate increasing access to services in rural and regional areas and promoting optimal care in the community.”
Over the next three years, the Living Well, Your Way care pathway will be implemented across the Murrumbidgee and Sue is excited for the future for people like Peter.
“At its heart, the pathway is a wellness model–providing alternative, home-based ways of supporting health. As a clinician, I know it’s easy to think we explain things to people, but do we really ensure they understand when they are discharged? Knowledge is power –if patients understand how to stay well and manage their health then they will be able to manage at home and have a better outcome. I am confident this new pathway is going to help clinicians manage and support their patients, and bring about improved health and wellbeing for all.”
real name
2020-25 national health reform agreement NSW FUTURE HEALTH PLAN MLHD’S STRATEGIC PLAN 2021-2026 MPHN’S STRATEGIC PLAN 2023-2027 AUSTRALIA’S PRIMARY HEALTH CARE 10 YEAR PLAN 2022-32 NSW GOVERNMENT PREMIERS PRIORITY TO REDUCE PREVENTABLE VISITS TO HOSPITAL The new Living Well, Your Way pathway is aligned with Commonwealth, state and local priorities outlined in various future plans including:
“The
*Not
S u p p o r t i n g t he patientjourneythrough care navigation Restoring function Transition to home Proactive coordinated treatment Prevention, screening and intervention Early diagnosis Optimal care in the Community There are seven steps in the pathway following patients with COPD and CHF from diagnosis through to end of life. SOME OF THE HIGHLIGHTS OF THE PATHWAY INCLUDE: • Engaging pharmacies to screen patients with chronic disease and link to general practice • Public private partnerships to implement outreach cardiology clinics with echocardiograms • Expansion of after hours primary care options • Enhanced GP led management models • Community nursing in-reach to hospitals and support for the transition home • Expansion of cardiopulmonary rehabilitation. Annual Report 2021-2022 | 45
Community led solutions
FOR PRIMARY HEALTHCARE IN SNOWY VALLEYS
From the ashes of the tragic 2019/2020 summer bushfires rose a community spirit, strength and resilience among the people living in the foothills of the snowy mountains.
Residents, community leaders and local healthcare professionals of the Snowy Valleys Local Government Area (LGA) have continued to support each other, most recently through consultation and engagement with the Collaborative Care project to address local primary healthcare needs.
One of five pilot sites across New South Wales, and the only site in the Murrumbidgee, the Collaborate Care project is focussed on exploring opportunities to connect local primary healthcare services to each other, and to those community members who require access to the services.
Project Officer for the Snowy Valley’s Collaborative Care project, and Snowy Valleys local Catherine Cusack said momentum for this project was achieved in part due to the leadership from the three partner organisations.
“I know how innovative and resilient our communities are in the Snowy Valleys. When we see a need, we are pretty good at fashioning solutions. However, healthcare does require the backing of organisations within the system to enact change. Often when you are trying to get buy in from the community for these types of activities, people look up to see what’s happening higher up in organisations and think, ‘yeah, that’s not going to happen’, but with Collaborative Care, people look up and see what collaboration is occurring and are excited about being involved,” Catherine enthuses.
“It starts at the top. MPHN, MLHD and RDN are partnering with the Snowy Valleys communities to progress this work. This level of collaboration is priceless. The project is about identifying what valuable services and supports already exist across our communities, sometimes unevenly distributed, and how we can collaborate together with the purpose of achieving better health outcomes for the whole region,” she continues.
Community interest was evident during the consultation phase of the project with more than 570 community surveys completed, and hundreds more people consulted at community events like Christmas markets, service club meetings, interagency meetings, organisation representatives, local healthcare providers including general practitioners, registered nurses and allied health professionals.
The feedback, which also included quantitative health data, was then processed through the Collaborative Care working group members to determine five key areas of focus including, Aboriginal health, health literacy, crosscommunications between health providers, allied health and welcoming new health workers. Each priority area has a project group to brainstorm and progress ideas to implementation.
“As the project officer I am privileged to see how each area’s activities are progressing. We have connected with the national Health Direct service to support a health literacy strategy; facilitating health provider forums to improve crossservice communications and networking; and while it isn’t in the remit of Collaborative Care to recruit health workforce, we are supporting health workers new to the area with a welcome pack, which have been made possible through connections with local Rotary clubs which also ensure longer term sustainability of the activity,” Catherine explains.
“The allied health group has only recently commenced and is working to make these services more accessible to people in the Snowy Valleys.
“Work with the Aboriginal health group has been inspiring. Seeing that drive and passion is really motivating. The group are creating three different videos focussing on diabetes – from the point of view of someone living positively with diabetes, a carer, and someone who has a genetic predisposition to diabetes. All people featured will be local Aboriginal people and the videos will be a terrific resource for helping curb diabetes prevalence in local Aboriginal and Torres Strait Islander people.”
For Linda Swales, Batlow community representative and Collaborative Care working group member, seeing progress on these activities makes her excited about the future of primary healthcare in the community.
“We are all unique and we all have different needs, but the one thing that this is going to fix up is that we will be more connected. The project is about trying to get this puzzle together so we are all receiving exactly what we deserve –good healthcare in our area,” she says.
Almost 600 Snowy Valleys residents have contributed to the development of project activities for a joint initiative between MPHN, Murrumbidgee Local Health District (MLHD) and Rural Doctors’ Network (RDN) known as Collaborative Care.
46 | Annual Report 2021-2022

SNOWY VALLEYS COLLABORATIVE CARE WORKING GROUP • Justyn Walker – A/RDN Program Lead, Collaborative Care • Darryn Binks – RDN Regional Manager • Cate Cross – LHAC Representative • Hansie Armour – Tumut LHAC Chair and Snowy Valleys Councillor • Sue Bulger – CEO Brungle Tumut Local Aboriginal Land Council/Indigenous Community Representative • Tahnee Bulger – Aboriginal AoD and Mental Health Worker, MLHD/Indigenous Community Representative • Dr Alam Yoosuff – Director Primary Health Care, MLHD and Finely GP • Emma Field – Director Integrated Care and Allied Health, MLHD • Carla Bailey – Director Clinical Operations- East, MLHD • Wendy Arentz – Disability Inclusion Action Reference Group Member • Narelle Mills – Executive Integration and Partnerships, MPHN • Andrew Heap – Senior Manager, Primary Care Engagement, MPHN • Chris Blake – Tumbarumba LHAC and Project Officer Resilient Towns Initiative • Linda Swales – Batlow Community Representative and Chair • Tracy Wiggins – Manager Community Services, Snowy Valleys Council Representative • Catherine Cusack – Project Officer WHAT THEY SAID “It’s very important the health providers come together and are aware of the service they provide and what they specialise in.” “I enjoyed meeting other health professionals and discussing how we can move forward to improve access to health services for the Snowy Valleys population.” Participant feedback from the Collaborative Care Health Professionals Forum held on Monday 20 June 2022 COMMUNITIES OF THE SNOWY VALLEYS TUMUT BATLOW ADELONG BRUNGLE KHANCOBAN TUMBARUMBA TALBINGO (L-R) Emily Stepasiuk, Tess Lucas, Kim Scott, Evan Feather attendees at the Health Professionals Forum Annual Report 2021-2022 | 47
Transforming the healthof Murrumbidgee children
The Enhancing Paediatrics in Primary Care (EPiPC) program is increasing the confidence of the region’s general practitioners to improve both the lives and health outcomes of their youngest patients and their families.

Among the 77 recommendations from the 2019 Henry Review of health services for children, young people and families within the NSW Health system was to increase the skills of general practitioners in managing complex behavioural problems in children and improving integration between hospital, community paediatrics and child health services.
This, coupled with the First 2000 Days Framework and the joint MPHN and Murrumbidgee Local Health District (MLHD) Maternal and Child Health Strategy for the region, has led to the implementation of the EPiPC program, jointly funded by MPHN and the MLHD.
Leading implementation is Community Paediatrician Dr Lahiru Amarasena, to enhance capability and capacity of general practitioners and their teams to identify and appropriately manage the region’s most at-risk children between the ages of 0 to 7 who are experiencing developmental and behavioural issues.
“By increasing capabilities locally around children with behaviour and developmental issues, we hope to improve the diagnostic and management journeys for children and their families across the region,” Dr Lahiru explains.
The project is being delivered across three different streams – clinical support, enhancing GP skills, confidence and capabilities, and integrated paediatric clinics – and four local practices in Wagga Wagga, Deniliquin, Hay and Gundagai applied to be part of the program pilot.
One GP who is participating in the pilot is Dr Rachel James from Deniliquin Clinic, has found the clinical support key to managing her youngest patients.
“Having someone like Dr Amarasena who is a trained community paediatrician, can really support you in those areas which you might not be hugely confident with. For example, I want the confidence to be able to support my patients with up to date and relevant information and screening tools so I can ensure there is nothing else this child, living in Deniliquin, a rural town, is missing out on compared with a child who is living in a bigger resourced setting,” Dr James remarked.
“We know any interventions put in place in those early years have a huge impact on the child’s school and home life, and into adulthood. So it’s one of the more important areas of general practice, but it can be challenging to navigate. This is where the email support really comes in.
Dr Lahiru Amarasena and Dr Marietjie Van Der Merwe with a young patient
48 | Annual Report 2021-2022
General Practitioner Dr Marietjie Van Der Merwe from Kooringal Medical Centre in Wagga Wagga, also participating in the pilot program, agrees, and believes the training and upskilling stream of the program is a critical component of the pilot success.
“Through my work with MPHN as Clinical Editor for Murrumbidgee HealthPathways, I have been working behind the scenes with Dr Amarasena to ensure localised clinical paediatric pathways are updated and available for the region’s clinicians,” Dr Van Der Merwe explains.
“These have been published to coincide with key webinars and CPD events. This means, after undertaking the session, the relevant HealthPathways can be accessed to further strengthen learning and knowledge.”
Training sessions have been very well received. MPHN’s Executive Integration and Partnerships Narelle Mills, who oversees implementation of the program, said feedback from the pilot showed an increase in confidence among general practitioners to complete screening and behavioural assessments.
“When looking at pre and post event data, we can see confidence improving across the board, and this will lead to positive outcomes for children,” Narelle shares.
“We have also expanded supports for children with the establishment of two additional initiatives that will integrate into the EPiPC model. First, an 18-month pilot for a paediatric allied health program as part WARATAH (Wellness And Resilience Achieved Through Allied Health), known as WARATAH for Kids, and second, a feasibility pilot for a paediatric psychiatry pathway to establish a telecare multidisciplinary assessment pathway for children.
“Dr Amarasena is involved in both of these activities, which are excellent examples of how MPHN is collaborating across the health sector to improve outcomes for children.”
All 89 general practices in the Murrumbidgee region have access to services under EPiPC program. The four pilot sites of the program will continue to develop an approach with a multi-disciplinary team to implement coordinated care and foster greater allied health integration.
EPiPC WORKING GROUP MEMBERS • Dr Lahiru Amarasena – Community Paediatrician, Murrumbidgee Local Health District • Nicole Myers – Manager Integrated Child and Family Wellbeing, Murrumbidgee Local Health District • Narelle Mills – Executive, Integration and Partnerships, MPHN • Maya De Mattia – Portfolio Manager, MPHN • Dr Marietjie Van Der Merwe – Kooringal Medical Centre • Dr Shahzad Arshed – Hay Medical Centre • Dr Rachel James – Deniliquin Medical Centre • Dr Maya Eamus – Gundagai Medical Centre Pilots of the Enhancing Paediatrics in Primary Care are conducted in the above four medical centres for testing and adapting prior to being made available to all practices across the
Murrumbidgee.
* Only 3 evaluations completed to date 100% 100% 33% 67% PRE workshop POST workshop Confidence in using developmental screening in the blue book Very confident 11% 25% Somewhat confident 47% 75% Not confident 42% 0% PRE workshop POST workshop Confidence in using developmental screening in the blue book Very confident 11% 20% Fairly confident 0% 60% Somewhat confident 22% 20% Slightly confident 67% 0% Not confident 0% 0% PRESCHOOL DEVELOPMENTAL SCREENING PREVENTION OF CHILDHOOD OBESITY STRONGLY AGREE Satisfied with quality of service STRONGLY AGREE Satisfied with timeliness Encounter will help reduce time to accessing services STRONGLY AGREE AGREE Annual Report 2021-2022 | 49
Full
Bushfire

OUR
credit to the team Treasurer’s report Community grant recipients
recovery grant recipients Commissioned service providerspeople in this section 50 | Annual Report 2021-2022
Melissa Neal
Chief Executive Officer

Our people are at the centre of all we can achieve as an organisation. I’m so proud of what we have accomplished in the past 12 months and I am always inspired by the ideas, enthusiasm, commitment and resilience of our people. We are now internationally accredited for quality management, our first Reconciliation Action Plan is already being implemented, we have really listened to the feedback from the 2021 Staff Engagement survey and continue to implement strategies to address these concerns, and I’ve seen the skills and capabilities grow among team members through secondments and training. I’m looking forward to seeing where the next 12 months takes us”

Annual Report 2021-2022 | 51
TO THE TEAMfull credit
ISO, EA, RAP, WHS – no acronym is too small for team MPHN! But what does all this mean?
It’s been a busy 12 months with employees helping to formalise an internationally recognised quality accreditation, negotiate a new Enterprise Agreement, refine the Reconciliation Action Plan, and implement various activities to streamline processes and upskill staff.
HR and Quality Manager Kristy Hawkins said MPHN achievements would not have been possible without the assistance of all employees.
“This year we have asked employees to participate in a range of really significant work to help improve our systems, processes, working arrangements, and our commitment to Reconciliation, and it’s been pleasing to see all staff contribute,” Ms Hawkins says.
“For example, we worked really hard to address feedback from the 2021 Staff Benchmarking survey by critically reviewing and updating delegations and processes, performance reviews, and internal meetings.”
Employee participation was critical to achieve ISO 9001 Standard: Quality Management Systems accreditation, which is an internationally benchmarked standard for organisations to meet in relation to how it manages and ensures quality in all its work.
“Every team across MPHN was involved in preparing for our accreditation, and I would like to acknowledge their efforts in preparing their documents, systems and processes in alignment with the ISO requirements,” Ms Hawkins says.
“The whole accreditation process was a great opportunity to review our quality management system and demonstrate how each employee can ensure quality across all that we do. It was great to hear the lead Auditor from SAI Global compliment us on our clear commitment to quality.”
Commitment was also evident during the negotiations for a new Enterprise Agreement (EA), which commenced in December 2021. After discussions with staff EA bargaining representatives and the union, the EA was reviewed and voted on by staff before being issued to Fair Work Commission for approval.
The new EA includes changes to time in lieu, addition of remote work arrangement provisions, amendments to Domestic and Family Violence Leave, and the addition of Cultural and Ceremonial Leave, Miscarriage or Pre-Term Birth Leave, and extra pay points in level 5 and level 6.
Toni Preuss, one of the five staff bargaining representatives, said the addition of the Cultural and Ceremonial leave was a key element of the negotiations.
“As a member of MPHN’s Reconciliation Action Plan (RAP) working group, I was pleased we were able to successfully negotiate culture and ceremonial leave. It’s a small way for MPHN to acknowledge the importance of First Nations employees engaging in their culture, and for non-Indigenous employees to gain a greater understanding and awareness of culture,” Toni explains.
Seryn named Cootamundra Electorate Woman of the Year
As part of International Women’s Day celebrations in March 2022, MPHN’s Suicide Prevention Project Officer
Seryn Adams was recognised as the 2022 Cootamundra Electorate Woman of the Year for her outstanding work in suicide prevention. The award was announced by State Member for Cootamundra Steph Cooke MP.
Seryn said it feels like an understatement to say she is honoured to receive this award.
“To be acknowledged in this way truly inspires me to continue advocating for positive change, speaking out and stepping up for those who experience mental ill health and suicidality.” Ms Adams said.
“I would also like to take this opportunity to thank my employer MPHN and my various managers for allowing me to turn my passion for suicide prevention into a career. Working with incredible colleagues to support our many communities across the Murrumbidgee gives me a great sense of purpose.”
52 | Annual Report 2021-2022
In fact, culture and ceremonial leave provisions is part of MPHN’s draft RAP, as is completing cultural awareness training, which was held throughout the year with staff, general practice staff and commissioned service providers.
RAP working group Chair, Kelly Dal Broi said cultural awareness training is a key strategy in closing the gap on Aboriginal people’s health.
“It is so important to understand how to deliver culturally safe services and practices. I’m pleased this training will continue to be offered to all MPHN staff. The more we know and understand, the better able we are to contribute to closing the health gap for our First Nations people,” Kelly says.


The first draft of the RAP vision and actions was endorsed by Board in May 2022, and will be submitted to Reconciliation Australia in late 2022 for final endorsement.
“It’s great to see some of the actions listed in the RAP draft being implemented already, and I would like to take this
opportunity to thank all the working group members for their continued effort and enthusiasm,” Kelly says.
MPHN staff are always eager to engage in internal committees including the CEO Consultative Committee and the Workplace Health and Safety (WHS) Committee.

Chair of the WHS Committee Naomi Richards said training completed by members in late 2021 highlighted the significance of keeping people safe at work.
“The training highlighted the legality around WHS and got us thinking about what other things can we do to keep our colleagues safe,” Naomi says.
Wellbeing Wednesday was also implemented to help support health and wellbeing among staff. These activities included yoga, walks, lunch get-togethers and webinars.
Other training completed by staff throughout the year included 7 Habits of Highly Effective People and Coaching and Mentoring training for our leaders.
In early 2022, two MPHN employees marked 10 years of service with MPHN in its various iterations. First, Julie Bailey who is currently a casual receptionist with the Wagga GP After Hours Service reached 10 years of service in January.
“My first role was with Wagga GP After Hours, I was then lucky enough to be employed by headspace Wagga as their Practice Manager in the Medicare Local days. Since then I’ve worked in various mental health positions for MPHN. Even though now I am not employed by MPHN in a fulltime role, I have still work at the Wagga GP After Hours. It is a role I really enjoy; I like meeting all the local doctors and assisting them to help unwell people after hours. This is such a valuable service for our area,” Julie shares.
Then in March, Finance Manager Bettina Goolagong followed.
“My first role was a maternity leave finance position and when the maternity relief was complete, I was fortunate to be able to continue working here – at one stage working three roles at once in other programs, before coming back into the Finance team. This broad scope of roles and experience is a major reason why I’ve achieved this milestone,” Bettina shares.
Reflecting on her last ten years, Bettina said “Life is so unpredictable, and we are all faced with so many challenges, especially with COVID. From what I see in and around the office, MPHN embraces the challenges and just runs with it.”
Julie and Bettina celebrate 10 years of service
Staff Christmas lunch (top left); staff consultation session (bottom left); MPHN’s Workplace Health and Safety Committee training (right)
Annual Report 2021-2022 | 53
TREASURER’S report
I am pleased to present the highlights of the 2021-22 financial report for Firsthealth Limited.
The Company’s major activity remains the conduct of the Murrumbidgee Primary Health Network (MPHN) under contract with the Australian Government Department of Health. The Company’s major activity remains the conduct of the Murrumbidgee Primary Health Network (MPHN) under contract with the Australian Government Department of Health and Aged Care. The company also received funding form other sources under separate contracts, aimed at improving access and quality of primary health care across the Murrumbidgee.
Revenue from funders increased by 16 per cent overall from the previous year to $25 million. These funds have been applied in accordance with relevant funding agreements.
As at June 30 2022, the company held an additional $10.9 million in unspent funding which will be utilised for health service provision in 2022-23. The challenges of the global pandemic continued in 2021-22 and has impacted on the ability of the MPHN as well as its commissioned service providers to fully utilise available funding. It is important to note that a significant proportion of this amount has already been committed in contracts with service providers to fund the delivery of health services. Firsthealth Limited continues to implement plans to utilise these funds in an agile and community-led manner.
Please refer to the graphics on the next page which show the sources and applications of the funding received and effectively managed by the company in deliverables to funders.
The company operates on a not-for-profit basis and is precluded from making any profit on government funded services. In 2021-22 the company made a profit of $25,733 from the management of its own members’ funds.
Full financial statements are available on the company’s website. I particularly draw your attention to Note 1 Basis of Preparation, Note 2 Summary of Significant Accounting Policies, and Note 3 Critical Accounting Estimates and Judgements.
 Paul Gianniotis
Paul Gianniotis
FULL FINANCIAL STATEMENTS

54 | Annual Report 2021-2022
$20,343,912
$2,421,468 $1,330,291
$337,519 $309,630
$83,504 $134,976
$16,171 $84,447
$25,648,080 $22,203,256
$17,028,319 $14,495,221
$4,766,925 $4,673,588
$118,091 $144,526
$530,091 $381,138
$474,513 $262,665
$371,020 $236,370
$822,292 $464,212
$1,511,096 $1,485,998
$25,622,347 $22,143,718
$25,733 $59,538
Revenue EXPENSES REVENUE EXPENSES 89% AUSTRALIAN GOVERNMENT DEPARTMENT OF HEALTH 66% CONTRACTORS 19% EMPLOYMENT COSTS 6% OTHER EXPENSES 3% SERVICE FEES 2% GRANTS 2% GP PAYMENTS 0% BOARD & COMMITTEE COSTS 1% COMMUNICATIONS 9% OTHER SOURCES 1% CLIENT FEES & SERVICES 0% INTEREST EARNED 0% OTHER INCOME SOURCE 2021-2022 2020-2021 % CHANGE AUSTRALIAN GOVERNMENT DEPARTMENT OF HEALTH $22,789,418
12% FUNDING (OTHER SOURCES)
82% CLIENT FEES AND SERVICES
9% INTEREST EARNED
-38% OTHER INCOME
-81% TOTAL
16% SOURCE 2021-2022 2020-2021 % CHANGE CONTRACTORS
17% EMPLOYMENT COSTS
2% BOARD & COMMITTEE COSTS
-18% GP PAYMENTS
39% GRANTS
81% COMMUNICATIONS
57% SERVICE FEES
77% OTHER EXPENSES
2% TOTAL
16% PROFIT (OR LOSS)
Annual Report 2021-2022 | 55
COMMUNITY GRANT RECIPIENTS
Soroptimists International Griffith
Berrigan Shire Library Service
Murrumburrah-Harden Flexible Care Services Inc.
Mate Helping Mate
Zac’s Place Inc
Griffith Aged Support Service
NSW Service for the Treatment and Rehabilitation of Torture and Trauma Survivors (STARTTS)
PEAK ABUNDANCE
Country Universities Centre Western Riverina
Leisure and Recreation Group- Cootamundra Pool and Sports Stadium
CALM Training Hotel Koorawatha Henty Respite Ltd.
Boys to the Bush Ltd
Griffith Local Health Advisory Committee
Fit for life Koraleigh - Amanda Wells Parkrun Australia LTD
Lockhart Local Health Advisory Committee
Tumbarumba Local Health Advisory Committee
Howlong Preschool
Griffith City Library
PHYSIOFAMILY
Deniliquin Local Health Advisory Committee Culcairn Local Health Advisory Group
Deniliquin Mental Health Awareness Group
Inspired Youth
Thyra Community Hub Incorporated
The Leisure Company Disability Services LTD
Pretty Pine Grounds Committee
headspace Griffith and Centacare Southwest NSW Coast & Country Community Services Ltd T/A Young Community Transport
MedicinesED and the Rotary Clubs of Boorowa, Harden and Tumut
Tumbarumba Rural Fire Brigade
Ganmain Grong Grong Matong Football Netball Club Multicultural Council of Wagga Wagga Urana Arts in partnership with Urana Incorporated Wagga Autism Support Group Inc
Courabyra Public Hall Learning Matters
Griffith Community Centre Amanda Elliott
BUSHFIRE Recovery GRANT RECIPIENTS
Tarcutta Valley Landcare Group
Franklin Public School
Tumbarumba Gym & Fitness Amanda Elliott Healing and Training Dairy Business Network Group
TUMUT ART SOCIETY INC
Village Support Services
Marty’s Music School
Save Tumbarumba Shire Inc
St. Vincent de Paul (Tumut Conference)
Batlow Men’s Shed Incorporated
Gundagai Neighbourhood Centre Community Foundation for Tumut Region
Downstream Yoga
Adelong Pastoral & Agricultural Show Society
Tumbarumba Basketball Association
Tumut Regional Family Services
Greater Hume Shire Council
Murrumbidgee Local Health District Disaster Clinicians C. Jones Training
Rural Financial Counselling Service
Tumbarumba Rural Fire Brigade Courabyra Public Hall Land Manager
Do It For Batlow Incorporated Rotary Club Tumbarumba Oasis Creative Arts Therapy Tumut Remedial Massage
56 | Annual Report 2021-2022
COMMISSIONED SERVICE PROVIDERS
Advance Care Planning Australia
Altura Learning
Amaranth Foundation
Back On Track Physiotherapy
Blamey Street Surgery
Boorowa Hospital Medical Centre & Kruger Medical Centre
Bright Agency
Business Data Enterprise
Calvary Health Care Riverina Caremonitor Pty Ltd
CBT Institute
Centacare South West NSW Charles Sturt University
Community Foundation for Tumut Region Community Options Australia Limited
Coolamon Advisors
Cootamundra Medical Centre
Corowa Medical Centre
Deniliquin Clinic
Directions Health Services Dr Taghrid Samuel Evohealth Pty Ltd
Gidget Foundation Australia Glenrock Country Practice Grand Pacific Health Greater Hume Council Griffith Aboriginal Medical Service Gundagai Medical Centre
Hammond Health Hay Medical Centre
IQVIA
J Alster & M Alster
Juntos Marketing Pty Ltd
Kooringal Medical Centre
Lakeside Medical Centre Larter Consulting Pty Ltd
Leeton Medical Centre
Leeton Medical Practice
Lockhart Medical Practice
Marathon Health MedCirc Medical Centre MediCoach
Moama Health Clinic
Murrumbidgee Local Health District
Murrumbidgee Medical & Primary Care Centre
Painchek Ltd
Positive Living Skills Procare PwC
Rao Medical Centre
Relationships Australia Riverina Medical & Dental Aboriginal Corporation
Riverina Psychology
Roth’s Corner Medical Centre
Royal Far West
Shiloh Medical Practice
Snowy Valleys Council
St George Family Medical Centre
Sunflower House Incorporated Swan Hill District Health
The Benchmarque Group Pty Ltd
The Men’s Table
The Resilience Project
The Trustee for Sana Medical Services Trust Trail Street Medical Centre
Trinity Medical Centre
Tumbarumba Medical Practice
Cummeragunja Housing and Development Aboriginal Corporation (Viney Morgan)
Wagga Wagga Medical Centre
Wagga Women’s Health Centre
Wellways Australia
Young District Medical Centre
Annual Report 2021-2022 | 57
www.mphn.org.au
Tel 02 6923 3100
Fax 02 6931 7822
1/185 Morgan Street, Wagga Wagga NSW 2650





















 McRaeHeap anita
narelle
McRaeHeap anita
narelle





















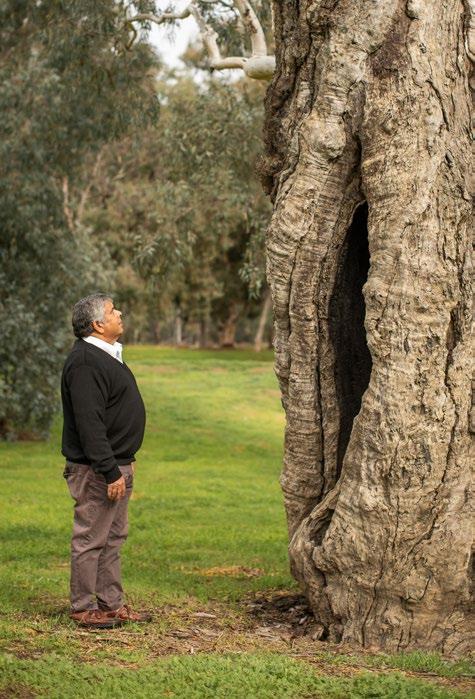




























 Paul Gianniotis
Paul Gianniotis

