

BONES


FIRST AID TO THE INJURED
THE AUTHORIS E D TEXTBOOK
O F TH E
ST. JOlI N ASSOCIATION
A F O UNDATIO N O F
The Grand Prio ry of th e Mo s t Venerabl e Orde r of the Hospi ta l of St. John of Jerusalem.
FORTIETH EDITION
THIRTEENTH IMPRESSION 1957
INCLUDL G SUP?LEM E. TS : Holger ielsen Method of Artificial Respiration, Insensibility, and Civil Defence
P rice 3/6 net; P ostage ex tra
PUBLISHED BY
T HE ST. J O H N AMBU L ANCE ASSOCIATION
ST. JOHN'S GATE, CLERKE WELL, LONDON, B.C.l
COPYRIGHT
H. & S.-ll/57
PREVIOUS PUBLICATIONS
I. "Aids for Cases of Injun'es or Sudden Illness," by Shepherd
2 DlClo.
3. "Shepherd's First Aid ta che II/jured," by Bruce
4. Dicta .
5. Ditto.
6. "First Aid ta the Injured, " by Cantlie, 1st Edition
7. Di£10. 6th "
8. 9. 10. 11. 12. Duro. Dicta, by a Commutee
Ditto. " "

" " "
IMPRESSIONS OF THE 40th EDITION
1st 100.000 Copies 1950
2nd 100,000 1950
3rd 100,000 1950
4th 100 ,000 1951
5th 100,000 1952
6th 120,000 1952
7th 100,000 1952
8th .. 100,000 1955
9th 50,000 1955
10th 100,000 1956
11th 50,000 1956
12th 56,000 1957
13th 35,000 ;,
Syllabus of Instruction
List of Illustrations
Introduction Preface
I.-Outline of First Aid Il.-Structure and Functions of the Body IlI.-Dressings and Bandages . . IV.-Shock V.-Respiration VI.-The Circulation of the Blood . . VI I.-Wounds and Hremorrhage .. VlIl.-Hremorrhage from Special Regions
IX.-Fractures
X.-Injuries to Joints and Muscles
XI .-Insensi bili ty
XII.-Poisons . .
XIII.-Miscellaneous Injuries
XIV.-Preparation for Reception of Accidents
XV.-Transport of Injured Persons .. ..
SYLLABUS OF INSTRUCTION-ADULT COURSE
A course of instruction shall extend over a minimum of twelve hours, and only members of the medical profession are recognised as Insu·uctors. The Surgeon Instructor usually prefers to divide the course of instruction into six weekly lectures, each of two hours' duration, devoting the first hour to theory and the second to practical instruction in the application of dressings and bandages, treatment of hremorrhage and fractures, artificial respiration, hand-seats, and lifting and carrying injured persons on stretchers. If preferred, the Surgeon Instructor may divide the course into twelve lectures each of one hour's duration, or as convenient. If the Surgeon Instructor does not find it possible to undertake the practical part of the instruction he is permitted to entrust to a qualified layman or . woman approved by himself the practical instruction of the class, but the whole of the theoretical instruction must be given by the Surgeon Instructor.
FIRST LECTURE
Outline of First Aid
Structure and Functions of the
Body*
Dressings and Bandages
Practical Instruaion.-Dressings. Practice in use of sterilized dressings, lint, gauze and emergency dressings, and care in handling. Slings and the application of the triangular bandage to the head, chest, shoulder, elbow, hand, hip, knee, foot and stump. Ring pad.
*NoTE.-When poss!.:>ll a skeleton should be used. Too much time should not, however, be spent on instruction in anatomical and physiol o gical detai ls. Lecturers and Examiners are particularly requested to remember that it is "First Aid" that has to ue (aught and tested, and not anatomy and physiology.
SECOND LECTURE
Shock
Respiration. The, respirat?ry sys,tem. Asphyxia. respiration by Schafer s and SIlvester s methods.
Practical Instruction.-Artificial respiration.

Artificial
THIRD LECTURE
Circulation of the Blood. General description of the heart, blood-vessels and circulation.
\Vounds and Hremorrhage. Infection. Wounds. accompanied by severe hremorrhage. Direct pressure. Pressure pomts. Wounds accompanied by slight hremorrhage.
Hremorrhage from Special Regions. Hremorrhage. from an internal organ and from the mouth, nose and ear. BrUlses.
Practical Instruction .-Direct Cons.trictive Indirect pressure. Application of ordmary dressmgs and bUllt-up dressings.
FOURTH LECTURE
Fractures. Causes, types, signs, symptoms and general rules for treatment. Special fractures.
Injuries to Joints and Muscles. Dislocations, sprains and strains.
Practical Instruction.- Treatment of fractures.
FIFTH LECTURE
Insensibility. The nervous system. General rules for treatment of insensibility. Commoner and less common causes of insensibility.
Poisons. General rules for treatment of poisoning. Antidotes.
Practical Instruction.-Artificial respiration. Application of bandages and dressings.
SIXTH LECTURE*
Miscellaneous Injuries. Burns and scalds. Frost-bite. Abdominal hernia. Stings. Foreign bodies under the skin, in the eye, in the ear, in the nose, in the stomach and in the throat.
Preparation for Reception of Accidents.
Transport of Injured Persons. Hand-seats and stretcher.
Practical Instruction.-Hand-seats and stretcher
Care should be taken when women are lifting.

In Civil Defence classes the subject matter in the supplement on pages 186 (a) to 186 (d) should be included in this lecture.
LIST OF ILLUSTRATIONS
8

31 St. John (final stage-front view)
32 St. John Sling ( final stage-back view)
33 Bandage for scalp . . . .
34 Bandage for chest (front view)
35 Bandage for chest ( back view) ..
36 Bandage for shoulder
37 Bandage for elbow
38 Bandage for hand
39 Bandage for hip ..
40 Bandage for knee
41 Bandage for foot
42 -45 Bandage for stump (four
46 Ring pad. . .. ..
47. Upper respiratory tract. .
48 Upper respiratory tract ..
49 Lower respiratory tract. .
50 Terminal bronchus, bronchiole and
5 I , (Schafer's method)
52 (Schafer's method)
53 ( Schafer's method)
54 (Silvester's method)
55 respIration (Silve ster ' s method)
56 DIagrammatic illustration of the heart
57 Capillaries . .
58 Section of
59 Valves of vein (open)
60
(closed)


INTRODUCTION
The St. John Ambulance Association, a Foundation of the Grand Priory of the Most Venerable Order of the Hospital of St. John of Jerusalem, came into existence in 1877, forty-six years after the revival of the Order in England. In 1872 tentative efforts had been made to introduce an ambulance service in the Potteries.
Certificates of proficiency in First Aid after attendance at lectures and examinations were granted in 1877, and the first manual of instruction was published in r878, having been written for the Association by the late Surgeon-Major Peter Shepherd, M.B. So keenly was the work taken up, especially by miners, policemen and railwaymen, that in 1879 the Association introduced a system of re-examination for further awards.
Commencing in 1878 Centres of the Association began to be formed in some of the larger towns, and eventually on all the main line Railways, in the Post Office and in some Collieries. Centres of the A£sociation were also formed overseas, and now come under the jurisdiction of Priories and Commanderies of the Order in those Dominions in which such Establishments exist. In these Centres ambulance classes and examinations for proficiency certificates and, in many cases, Ambulance Competitions (team and individual), are held regularly and both men and women take part.
No greater tribute to the work of the St. John Ambulance Association could have been paid than the granting of the Charter to the Order of St. John in 1888 by Her Majesty Queen Victoria, primarily on account of the work done by the Association.
Since its inception over 70 years ago, Association has ,
issued owr 6 million certificates of profici.ency to and women who have qualified in First Aid. and kindred subjects Home Nursing, Hygiene and Child Welfare. The AssoclatlOn s certificates are recognised by the Home Office, the Board of Trade, Admiralty, War Office, Air 0-i?istry and other Government Departments and Local Authontles.
The experience of the earl?, rea;s shm,:,ed that many of who had received the ASSOClatlOn s Certlficates an.d exhibited a keen desire to utilise their knowledge In the of the public. Many accordingly banded III units at various places and provided ambulance statlons at Natlonal and International Exhibitions and other places where large assembled. Thus originated the St. Jolm which was formally established by the Orde: In 1887 and, III 1948, was raised to the status of a Foundatlon of the Order. The Brigade now numbers, at home and 0:rerseas, more than 186,000 members, and is uni'l ersally as a. necessary unit of civil life, ready to serve the public .on all where accidents are liable to occur. It compnses, besI.des 0 e. :uale units (Ambulance Divisions ), women:s units (Nu:smg DlvlSlons) and Cadet units and in addition prOVIdes fully tramed persons for Voluntary Aid Detachments. I?uring the .1939-45 World the Association and Brigade provlded for varIOU S Authontles a substantial number of trained personnel for serVIce at A.R.P. Casualty Clearing Stations and First Aid Posts.
In the early years of its the Association turned its attention to the manufacture and Improvement of ambulance litters and stretchers. These latter were so designed as. to fit all methods of transport, and even in those early days I.t was po ss ible for a patient to be conveyed Europe needing removal from the stretcher or suffenng from in transport. To-day the standard J Stretcher combmes a maximum of comfort to the patlent With ease of r;novement for the bearers, and adaptabi!ity for conveyance by varIOUS types of transport by land, sea or rur.
PREFACE
At the request of the Committee of the St. John Ambulance Association, we have revised the 39th Edition of its Textbook First Aid to the Injured.
In the course of the work we have examined and carefully considered many hundreds of suggestions and criticisms from the United Kingdom and all parts of the British Commonwealth and Empire, not only those received in response to the special appeal for such constructive help made when we started our task, but also many others sent to the Association during the years which have elapsed since the last general revision of the Textbook. We are much indebted to these numerous correspondents for their help.
We also wish to express our thanks to Dr. H. L. Marriott, e.B.E., for rewriting the Chapter on Poisons; to Professor B. G. Maegraith, Dean of the School of Tropical Medicine, Liverpool, for revising the section on Snake Bite which now appears as Appendix VII to the Textbook; and to the Chief Medical Officer and Chief Safety Officer of the British Electricity Authority for rewriting the section on Electric Shock.
In conclusion we desire to record our high appreciation of the care and skill with which Captain A. N. Cahusac, O.B.E., M.e., Secretary of the St. John Ambulance Association, and the Assistant Secretary, Mr. O. Horne, have edited the text during the Course of the Revision.
W. E. e. LAZENBY (Chairman).
A. C. WHITE KNOX, O.B.E., M.C., h?B., CH.B.
M. M. SCOTT, M.R.C.S., L.R.C.P.
OLIVE S. MAy, M.R.C.S., L.R.C.P.
G. STANLEY PHILLIPS, M.D., M.R.C.S., L.R.C.P,

CHAPTER I
OUTLINE OF FIRST AID
WHAT FIRST AID IS
The science of First Aid to the is based on fundamental principles of practical and a knowledge of which, in cases of accIdent Illness, enables trained persons to render such skilled assIstance. as will preserve life, promote or. prevent aggravation of the injury or condition untIl the arnval of the Doctor or during transport.
First-Aid is definitely limited to the assista,nce rendered at the time of the emergency with such as may be available. It is not intended that. the FIrst-Aider should take the place of the Doctor; . .It must be clearly understood that the re-dressing of and. other such aftertreatment are outside the scope of FIrst Ald.
The First Aider's responsibilities end as soon as aid is available; but he should stand by after his report to the Doctor in case he can be of further assIstance.
Throughout the book standard methods of treatment are given for standard conditions in or average circumstances, but the .wIlI be confronted with many variations of ,condItiOnS to which he must be prepared to adapt a,nd to which he must apply an intelligent appreCIatIOn,
FIG. I THE EIGHT-POINTED AMBULANCE CROSS

l\TECESSARY QUALIFICAnONS OF A FIRST-AlDER
In order to render the skilled required the FirstAider should be :-
(a) that he may note the causes and signs of Injury.
(b) Tactful, that he may, without thoughtless questions, learn the symptoms and history of the case, and secure the confidence of the patient and bystanders.
(c) Resourceful, that he may use to the be s t advantage whatever is at hand to prevent further damage and to assist Nature' s efforts to repair the mischief already done.
(d) Dextrous, that he may handle a patient without causing unnecessary pain, and use appliances efficiently and ne a tly.
(e) Explicit, that he may give clear instructions to the patient and /or the bystanders how best to assist him.
(f ) Discriminating, that he may decide which of several injuries should be treated first.
(g) Persevering, that he may continue his efforts, though not at first succes sful.
(h) Sympathetic, that he may give real comfort and encouragement to the suffering.
ESSENTIALS OF FIRST AID
In First Aid to the Injured it is essential :-
(a) To determine the nature of the case requiring attention so far as is necessary for intelligent and efficient
treatment-in other words, to make a sufficient diagnosis for the purposes falling within the province of the First-Aider.
(b) To decide on the character and extent of the treaUllent to be given.
(c) To apply the treatment most suited to the circumstances until medical aid is available.
The First-Aider must therefo;e cultivate a methodical, and approach to his case, taking into conthings which have a bearing on it, complete hIS diagnosIs and treatment and arrange for the immediate after-care of the patient.
APPROACH TO THE CASE
The First-Aider must always
I. Respond quickly to cans for assistance. The saving of a life may depend on promptness of action.
2. Take First Aid material if it is immediately available.
3· Study the surroundings carefully. These will exercise a most important bearing on the action to be taken and therefore require careful consideration, e.g.:
Ca) from falling buildings, moving machinery, electnc current, fire, poisonous gases and similar hazards.
(b) Weather. If the accident occurs out-of-doors the . , patIent may be treated out-of-doors if the weather is fine: if the weather is inclement, he must be removed to shelter as soon as reasonably possible.

(c) Light. It is impossible to treat a patient satisfactorily without adequate light, and the First-Aider must make provision for this during the darker hours.
Cd ) Shelter. Note houses and buildings near at hand, whether occupied or unoccupied , and whether likely to be particularly useful such as a Chemist's shop. Otherwise, temporary shelter may be secured by means of umbrella s, rugs and the like.
(e) Assistanc e. Crowds must be ta.ctfully controlled. If a Doctor is present, work under his direction. If not, ask if anyone with a knowledge of First A id is present. If neither is available, utilise bystanders to the best advantage .
(f) Mat erial avail able. If standard equipment is 110t available, the First-Aider must d epend on material at hand which will have to be improvised as required.
4. Speak encouragingly to his patient, warn him to lie still and tell him that he is in competent hands.
EXAMINATION OF A PATIENT
A patient may have more than one injury or there may be more than one patient. The First-Aider must attend to the more serious injuries first and, if bystanders are present, direct them to the treaUllent of others.
DIAGNOSIS
In deciding the nature of the case, the First-Aider must consider its history, symptoms and signs.
History. may be from the patient (if cOP c;dous) or from wltnesses and IS the story of how an accident or illness or it is information that a person IS subject to a parucular disease.
Symptom.s are the sensations of the patient, such as cold or .faintness, nausea, thirst and pain, which he can, If conscIOUS, describe. In the conscious patient who can describe his symptoms intelligently, pain IS a very helpful diagnostic point to the First-Aider, as it draws his attention to the part which is most probably in trouble and saves a great deal of time durinO' the examination of the patient.
b
Signs are any variations from the condition of the such as pallor, conge stion, swelling and deformity, which can be noted by the direct use of the senses.
Signs are the most reliable indications on which to base diagnosis, but the circumstances of each particular case will d.etermine the relative importance of history, symptoms and SIgnS.
If the patient is conscious and able to give reliable information, examine first at the points where pain or other symptoms or obvious signs indicate injury or illness. 1 hen examine him for other possible injuries.
If the patient is unconscious or cannot give reliable information :-
I. Note if breathing is present or absent. If absent, commence artificial respiration immediately.
2. Note if severe ha'morrhage is present. Examine everywhere for dampness indicating blood, especially under the patient. If pre sent, find the source and arrest the hremorrhage immediately.

3. Establish the cause of the insensibility by examining
(a) the character of the breathing;
(b) the character of the pulse (felt at the radial artery by placing three fingers along the line of the artery in front of the wrist half an inch in from the thumb side ) ;
(
c) the colour of the face ;
(d ) the head for injury and the ears, eyes, nose and mouth for blood or other signs;
(e ) the pupils of the eyes for any change from normal.
4. Make a thorough examination of the whole body for signs of injury.
In making a diagnosis, it may be necessary to remove or displace a certain amount of clothing. Do not remove more than is necessary, and replace it as quickly as possible because conserving heat in a patient's body is one of the most important factors in hi s recovery. Do not destroy clothing unneces sarily, but if further access to a part is essential, do not hesitate to cut the clothing sufficiently for tlle purpose.
Rem.oval of Clothing :-
Coat: Raise the patient a nd slip the coat over his shoulders; then remove from the sound limb first; and, if n ecessary, slit up the seam of the sleeve on the injured side.
Shirt and Vest: Slit down the front and remove as the coat.
Trousers: Pull up or down as required; or, if necessary, slit the seam on the injured side.
Boot or Shoe: Steady the ankle, undo or cut the laces, and remove carefully.
Sock: Insert two fingers between the sock and the leg, raise the edge of the sock and cut it between your fingers.
TREATMENT
If the cause of the condition is still active remove the cause; or, if this is impossible, remove the patient from the cause.
Apply such treatment as may be required for the preservation of life, promotion of recovery and the prevention of aggravation of the condition. Pay special attention to the treatment of failure of breathing, severe bleeding an d shock.
Where there is the slightest doubt as to whether a patient is dead or alive, continue treatment until the arrival of medical aid.
DISPOSAL
Arrange for the patient's removal either to his horne, to hospital or to other suitable shelter. Unless the patient is examined by a Doctor on the spot or is sent to hospital, he must in all cases be instructed by the First-Aider to see his own Doctor.
MEANS OF TRANSPORT
The patient must be conveyed home, to shelter or to hospital in the manner considered most suitable in the circumstances. A tactful message should be conveyed to the patient's horne or next-of-kin indicating in a general way what has happened and the patient's destination.
PROVISION FOR MEDICAL AID
AND THE TREATMENT OF SHOCK ARE ESSENTIAL PARTS OF FIRST AID. AS THESE TWO MAXIMS MUST BE FOLLOWED IN ALL CASES, IT WILL BE UNNECESSARY TO REFER TO THEM AGAIN EXCEPT TO EMPHASISE THEIR URGENCY.

CHAPTER
II
STRUCTURE AND FUNCTIONS OF THE BODY
In order to und er stand fully the principles of it is necessary that something should be kr:own ate structure of the body (a natomy ), and the functlons some of the more important organs and systems (p hy SIO logy ) .
THE STRUCTURE OF THE BODY THE SKELETON
The hum an body is moulded upon a bony framework (the skeleton) which serves :_
I. To give shape and firmness to the body.
To afford attachment to the mu scles.
To protect imp ortant organs, such as those m the skull, chest and abdomen.
THE SKULL
The Bones of the Skull are arranged in two groups, those of the brain case (crani um) and those of the face' d
The Boundaries of the Cranium are the vault or orne (t he rounded portion forming the top of the he ad) ; the front or brow' the back of the head, where the greates t of the b:ain is situated, and where therefore the is widest and deepest; the sides or temples. Th; f ase of the skull is hidden from view by the bones of t e . ace and of the spinal column. There are numerous operungs in the base of the skull for the passage of nerves; through the largest opening the bram and sp mal co rd are continuous.
The Bones of the Head and Face, with the exception of the lower jaw, are firmly united so that movement between them is impossible. The cavities of the nose and of the eye sockets (orbits) are formed by the bones of the cranium and of the face conjointly. The mouth cavity is formed between the upper and lower jaws; the palate being the bony roof of the mouth which separates it from the nasal cavity above.
The Lower Jaw consists of:-
(a) A horizontal portion in which are the sockets for the teeth . .
(b) Vertical portions terminating on either side at the joint between the lower jaw and the base of the skull situated immediately in front of the ear. The angle of the jaw indicates the junction of the horizontal and vertical portions.
THE BACK-BONE OR SPINE (VERTEBRAL COLUMN)
The Spine (Fig. 2) is composed of bones called vertebrre. Each consists of a body or bony mass in front, from the sides of which processes extend backwards and unite to form the spinal canal, which encloses the spinal cord (Figs. 3 and 4)·
The Vertebrre, 33 in all, are grouped into regions in each of which they are known by numbers, counting downwards :-
1. In the neck 7 cervical vertebrre. The first vertebra (atlas) forms a joint with the base of the skull, at which the nodding movement of the head takes place; the second (axis), by means of the joint between it and the atlas, permits the side-to-side movements of the head.
SKULL AND VERTEBRAL COLUMN
Showing left ribs and porti on of breast bone The right ribs are removed .
FrG . 3 .
THORACIC VERTE BRA SPINOUS PROCESS
DODY OF VERTEBRA PROCESSES. CANAL FOR SPINAL CORD.

SURFACES SUPPORTINC HEADS OF RIBS. TRANSVERSE PROCESS
SPINOUS PRO CESS.
FIG. 4
SIDE VIEW OF A THORACIC VERTEBRA
2. In the back 12 thoracic vertebrre, to which the ribs are attached.
3. In the loin 5 lumbar vertebrre.
4. The rump-bone (sacrum) consists of 5 sacral vertebrre united in adults as a solid mass.
5. The tail-bone (coccyx) consists of 4 vertebrre joined together.
Between the bodies of the vertebrre, in the upper three regions, are interposed thick pieces of gristle (cartilage), which allow of free movement to the column as a whole, and help to break the shock of any sudden force applied to the spine (for example, when falling from a height on the feet). The whole spine is strapped together by bands of strong fibrous tissue (ligaments) reaching its entire length.
THE RIBS AND BREAST-BONE
The Ribs consist of twelve pairs of curved bones extending from the thoracic vertebrre to the front of the body, and are known by numbers-first, second, etc., commencing from above. The ribs are not bony throughout their entire length, but at a short distance from the front the bony material ends and cartilage takes its place. The upper seven pairs, called the "true" ribs, are attached by their cartilages to the Breast-bone (sternum), a dagger-shaped bone with the point downwards, just above the pit of the stomach. The lower five pairs of ribs are called "false." Of these the upper three pairs are attached by cartilage to the ribs immediately above them. The last two pairs are unattached in front and are called "floating." The ribs enclose the chest and serve to protect the lungs, heart, liver, stomach. spleen, etc.
PART OF COLLAR BONE (CLAVICLE)
SHOULDER BLADE (S CAPULA)

5
FIG 6
SHOW LNG THE POSITION OF THE RADIUS AND ULNA WHEN THE THUMB IS TURNED INWARDS
(Compare Fig. 5, in which the thumb is turned outwards).

THE UPPER LIMBS
The Shoulder-bones are the collar-bone (clavicle) and the shoulder-blade (scapula).
The Collar-bone can be felt on either side beneath the skin at the lower and front part of the neck as a narrow curved rod about the thickness of a finger. Its inner end is attached to the upper part of the breast-bone, and its outer end joins with the shoulder-blade.
The Shoulder-blade lies at the upper and outer part of the back of the chest and forms joints with the collar-bone and the bone of the arm.
The Bone of the Arm (humerus) reaches from the shoulder to the elbow.
In the Forearm are two bones, one on the outer or thumb side (radius) and the other on the inner or little finger side (ulna). Both bones reach from the elbow to the wrist, and they change their relative position witl1 every turn of the hand (Figs. 5 and 6).
The Hand is composed of :-
1. The bones of the wrist (carpus), eight in number, arranged in two rows of four.
2. The framework of the palm (metacarpus)-five bones which form the knuckles and support the bones of the fingers.
3. The finger-bones (phalanges), three in each finger, and two in the thumb.
THE PELVIS AND LOWER LIMBS
The Pelvis. The large basin-like mass of bone attached to the lower part of the spine is called the pelvis and is
PELVIS NUCK OF FBMUR PATBLLA. -composed of the two innominate-bones, the sacrum and the coccyx. The innominate-bones meet at the front .in the line, only a small piece of cartilage mtervemng, but behind, the sacrum is placed between them. The pelvis supports the abdomen and its contents and provides the deep sockets for the lllp-joints. '
The Thigh-bone (femur) reaches from the hip to the knee-joint. Its shaft is stout, rounded and arched forwards .; the upper end presents a rounded head, supported on a neck which projects inwards, to fit into the socket of the innominate-bone.; the lower end broadens and enters into [he formation of the knee-joint.
The Knee-cap (patella) is a flat triangular bone lying with its base upwards in front of the knee-joint immediately beneath the skin.
The Bones of the Leg are the shin-bone (tibia) and the fibula. The tibia extends from the knee to the ankle, in both of which joints it plays an important part; its sharp edge can be felt immediately beneath the skin of the front of the leg. The fibula lies on the outer side of the tibia. I t does not enter into the formation of the knee-joint, but its lower end fonus the outer part of the ankle-joint.
The Foot is composed of:-
1. A group of seven irregular bones (tarsus) at the instep. The largest is the heel-bone, and the uppermost (the ankle-bone) forms the lower part of the ankle-joint.
2. The five long bones in front of the tarsus (metatarsus) which support the toes.
3- The toe-bones ( phalanges), two in the big toe, and three in each of the other toes.
33 JOINTS
Joints are formed by the junction of two or more bones and may be of two varieties :-
1. Immovable. The' edges of the bones forming this kind of joint are dove-tailed accurately into each other so that the joint is permanent and does not allow of any movement. Typical immovable joints are those between the bones forming the dome of the skull.

c.
A. Articular Cartilage
B. Synovial Membrane
C. Capsular Ligament
D. Synovial Fluid
FIG. 8
(Fig. 8). The ends of the bones forming this kind of Jomt are covered by cartilage and held together by of strong (ligaments) and enclosed in a bag surular strong tissue (capsule) reinforced by further ligaments. The bones are therefore held securely in position but free movement is allowed. Within the capsule is a linino(synovial membrane); its function being to secrete fluid (synovial fluid) which is always present inside these joints and acts as a lubricant.
The two common types of movable joints are :-
(a) Ball-socket joint (Fig. 9) formed by the rounded head of one bone fitting into the cup-shaped cavity formed by the other. In these joints very free movement is allowed. Examples are the shoulderand hip-joints.

35
In the knee-joint are two fiat crescentic pieces of cartilage (semi-lunar cartilages) which lie on the upper end of the . tibia, and deepen the surface for the rounded ends of the femur. In sudden wrenches of the knee, such as are met
SHOULDER- JOINT
ELBOW-JOINT
(b) Hinge joint (Fig. 10) in which the surfaces of the bones are moulded to each other in such a manner as to allow movement in one plane only, i.e., b ending (flexion) and straightening (extension). The elbow is an example of this type of joint (Figs. II and 12).
with in football and other games, or in slipping off a step, these cartilages may be displaced or torn.
THE TISSUES
The Muscles (red flesh ) of the body are classified into two groups-voluntary and involuntary.
The Voluntary Muscles are met with in limbs, the head and neck and the walls of the trunk (Flgs. 13- 18 ). They are attached to the bones either direct ;y or by st rong
 FIG. I3-MuSCLES OF THE TRUNK (Front View)
FIG. I4-MUSCLES OF THE TRUNK (Back View)
FIG. I3-MuSCLES OF THE TRUNK (Front View)
FIG. I4-MUSCLES OF THE TRUNK (Back View)
bands fibrous. tissue (tendons), and have the power of contractmg, l.e., gettmg shorter and thicker. They cause all the of the body and limbs, and are controlled by the bram, which sends messages (impulses) through the nerves of the cerebro-spinal system ( see page I59 ) to any mu.scle or gro,:!p of muscles which it wishes to call into actIon . . In this way all movements, such as walking or swallOWIng, are performed.

FIGS. 15 AND 18
MUSCLES OF THE LOWER LIMBS (Front and Back Views)
FIGS. 16 AND 17
MUSCLES OF THE UPPER LIMBS (Front and Back Views)
The Involuntary Muscles are met with in the walls of the stomach and intestines, in the air passages, and in most of the internal organs and blood-vessels; and, in a special form, in the heart. They are not under the influence of the will, but continue their work during the hours of sleep; their functions are regulated by a separate set of nerves (autonomic system, see page 161).
Connective Tissue consists of yellow elastic and white fibrous tissue intermixed in varying proportions. It is present in many parts of the body and forms a layer between the skin and underlying flesh all over the body, fat being contained benveen its meshes, often in large quantities. The chief use of the connective tissue is to bind parts together.
The Skin covers the whole of the body and protects the underlying structures. It consists of two layers, the outer or hard layer (cuticle) and the inner layer (true skin or dermis). In the latter are numerous glands which secrete sweat (consisting of water and impurities from the blood), the evaporation of which from the surface of the skin cools it and helps to regulate the temperature of the body.
THE TRUNK AND ITS CONTENTS
The Trunk is divided by a large arched muscular partition (Diaphragm) into two large cavities.
The upper cavity, the Chest (thorax), is bounded in front by the breast-bone; behind by the spine; below by the diaphragm, and is encircled by the ribs. It contains the Heart and Lungs.
The lower cavity, the Abdomen, is bounded above by the diaphragm; below by the pelvis; behind by the lumbar
FIG. 15 FIG. 16LUNG (RIGHT)

• • LUNG ( LEFT) HEART
- SPLEEN
STOMACH
TRANSVERSE • __ _ COLON
ASCENDING COLONBLADDER __
SPLEEN· ••KIDNEY·
DESCENDING •• _ COLON
- • SMALL INTESTINE - CREST OF ILEUM
URETER.
LIVER
.• AS CENDING COLON
FIG. 19
ORGANS OF THE CHEST AND ABDOMEN (Front View)
FIG. 20
ORGANS OF THE CHEST AND ABDOMEN (Back View)
vertebrre ; and in front and at the sides by muscular walls. It contains several important organs, namely, the Stomach, just below the diaphragm towards the left side; the Liver, in the upper part of the abdomen, where it is mostly covered by the right lower ribs; the Spleen, covered by the ribs at the upper part of the left side of the abdomen; the Pancreas, behind the stomach; the Intestines, which occupy the greater part of the cavity of the abdomen; the Kidneys, at the back, one at each side, in the region of the loin; and the Bladder, which lies to the front in the pelvis.
FUNCTIONS OF THE BODY
The food and fluid taken into the body provide fuel for heat and energy and new material to repair wear and tear. Food is digested in the mouth, stomach and intestines by various digestive juices secreted by various glands, thereby splitting up the foodstuff into simpJer substances which can be readily used by the body. The absorption of the food takes place in the small intestine and passes into the blood-stream via the capillaries and lymphatic vessels.
Oxygen is also necessary for the support of life. It is obtained from the air we breathe in respiration, and is absorbed into the blood-stream in the lungs.
The waste products are removed through the lungs, kidneys, skin and bowel.
The great carrier is the blood which conveys the fresh supplies of oxygen and nourishment to the cells of the body from the lungs and organs of digestion, and also the waste products to the organs of excretion. All the movements and functions of the body are regulated and controlled by the nervous system.

CHAPTER III
DRESSINGS AND BANDAGES
DRESSINGS
A dressing is a covering applied to a wound or to an injured part and may be used :-
(a) To protect a wound from further injury.
(b) To prevent or min im is e infection.
(c) To ass ist in controlling hremorrhage.
(d) To ease pain (moist dressings). .
The dressings used in First Aid are dry or mOIst.
DRY DRESSINGS
(a) Prepared Sterile The ideal for all wounds consists of a stenlised (germ-free) pIece of gauze or lint to which is sometimes stitched a pad and a roller bandage. This dressing is enclosed and sealed in a protective covering.
. .
To use a prepared sterile dressmg, loosen the protecuve covering; sterilise your finger.s if P?ssible (see 'page 94) ; remove the dressing; expose It as little as pOSSIble to the air and avoid fingering the surface of the dressing which is be applied to the wound. While the fingers are sterile, care must be taken not to handle anything which is not clean.
(b ) Gauze or Lint. If a prepared sterile dressing is not available, cover the wound with a piece of clean gauze or lint (s mooth side touching the wound).. .
To use gauze or lint, loosen the covenng and WIth clean scissors cut a piece to the size required to cover the wound adequately; take care not to touch the side which is to be applied to the wound.
Place the unused portion of the gauze or lint in a clean container.
(c) •. If a prepared sterile dressing or gauze or lint IS not unmediately available, the inside fold of a clean handkerchief or a piece of linen or clean unprinted as the inside of an. envelope, may be used but theIr use IS only temporary unul a prepared sterile dres sing or gauze or lint is available.
Dry dressings must be covered with an adequate pad of cotton wool which must extend well beyond the dressing and be kept in place with a bandage.
MOIST DRESSINGS
(a) Compress. This is used to ease pain, to lessen swelling or to control hremorrhage from an internal organ. Cold has the effect of constricting the blood-vessels and thus of reducing the quantity of blood flowing the affected area
.
To make a cold compress soak two thicknesses of linen or of a clean handkerchief in cold water, wring out the compress until it does not drip when held up and then apply it to the affected part. The compress must be left uncovered to encourage evaporation.
. Evapora.tion is accelerated and the beneficial effect thereby mcreased If one part of methylated spirit is added to three parts of water.
A compress dries rapidly and a second one should be soaking in readiness to take the place of the first as it dries.
(b) Hot Compress. This is used to ease pain. It promotes a free flow of blood and relieves congestion. E-
To make a hot compress soak three thicknesses of flannel
or of lint in very hot water, wring the compress dry, shake it and apply it to the affected part. .
As it is important to retain the heat as long as pOSSIble, the compress must be .covered witJ: a piece of jaconet, oiled silk or greaseproof paper, then. WIth pad of cotton wool of adequate size and secured m posluon by meat,ls of a bandage. The compress must be renewed as soon as It cools.
POINT

FIG. 2I-B AN DAGE SPREAD OUT
BANDAGES
Bandages form an important part of First Aid the Triangular Bandage being generally used. TrIangular bandages may be applied :- .' ..
(a ) To retain dre ss ings and splints m poslUon and to immobilise fra ctures. .
(b ) To afford support to an injured part (e.g ., spramed ankle) or in the form of a sling.
(c ) To control bleeding . .
Cd) To reduce or prevent swelling.
(
e) To assist in the lifting and carrying of a patient
(Fig.2I) are made by cutting a' piece linen or. calico, less than thirty-eight inches square, dIagonally IlltO two plec.es. A triangular bandage has three borders. The longest IS called the . "base" and the other two the "sides." There are three corners; the upper one
It is sometimes advisable to halve the size of the bandage by bringing the two ends together before foldmg it into the broad or narrow bandage. . To secure the ends of a bandage a reef knot (FIg. 25) must be used. To make a reef knot, the en.ds of (he bandage one in each hand. Cross the end III the nght d r and then over the end in the left hand thus makmg un Then cross the end now in the right hand. over then under the end in the left hand, thus making a second turn.

(opposite the base) is called the "point" and the others t..'1e "ends." The bandage may be applied :-
(a) As a whole cloth spread out to its full extent, e.g., chest bandage.
(b) As a broad bandage made by bringing the point down to the centre of base (Fig. 22). and then folding the bandage agam III the same dIrection ( Fig. 23).
(c) As a narrow bandage made by folding the broad bandage once again in the same direction (Fig . 24).
The knot must be placed where it does n?t cau.s e ?iscomfort or chafe the skin. If the bandage or lalot IS likely to be uncomfortable, a pad must be placed bervveeI1: the banda ge or knot and the body. After the reef knot IS compl.eted the ends of the bandage should be t.ucked away out of sIght. Granny knots (Fig. 26) are apt to slip and must not be used.
FIG. 22-BANDAGE ONCE FOLDED FIG. 21-BROAD BANnA FIG. 24-NARROW BANDAGEBandages may be improvised from handkerchiefs, belts, braces, ties, or any piece of linen, calico, tape, cord and the like.
SLINGS
Slings are used :-
(a) To afford support and rest to an upper limb.
(b) To prevent the weight of an upper limb pulling on or moving the chest, shoulder or neck.
ARM SLING
This supports the forearm and hand and is used in cases of fractured ribs; and in cases of wounds and injuries of the upper limbs, except when there is a fracture.
To apply an arm sling, face the patient and put one end of a spread-out triangular bandage over his shoulder on the sound side, with the point towards the injured side, pas s it round his neck so that it appears over the shoulder of the injured side, and let the other end hang down in front of the chest; carry the point behind the elbow of the injured limb, and place the forearm over the middle of the bandage so that it is at right angles to the arm; then carry the second end up to the first and tie them in the hollow just above the collar-bone; tuck the bandage in to the back of the elbow, bring the point forward and secure with two safety pins to the front of the bandage (Fig. 27).
When the bandage has been applied, the base should be at the root of the little finger nail so that all the finger nails are exposed. A bluish tinge of the finger nails indjcates that there is a dangerous constriction of the circulation in the upper limb.
The bandage should be kept as low as possible at the bac k of the neck and below the collar of a coat if worn. If there is no coat, a pad must be placed under the loop to prevent chafing.

ARM SLING
COLLAR AND CUFF SLING
This supports the wrist. To apply a collar and cuff sling, ben d the patient's elbow and lay hi.s forearm across his chest with his fingers touching his oppo1>1te shoulder. Pass a clove hitch round his wrist and tie the ends of the bandage in th e hollow just above the collar-bone.
FIG. 28
CLOVE HITCH (FIRST STAGES)

To a hitch take a narrow bandage and make a loop as m FIg. 28. Make a second loop and lay it on taI? of the first: then turn the top loop behind :he first (FIg. 29).
FIG. 29
CLOVE HITCH (FINAL STAGE)
51
ST . JOHN SLING
This keeps the hand well raised and is used in the case of a fractured collar-bone.
Place the patient's forearm across his chest so that his fingers point tow .: rds the shoulder and the centre of the palm rests on the breast-bone. Lay an open bandage over the forearm with one end over the hand and the point well beyond the elbow (Fig. 30). Steady the limb and tuck the base of the bandage well under the hand and forearm so that the lower end may be brought w.i.der the bent elbow and then upwards across the back to the uninjured shoulder where it is tied in the hollow above the collar-bone. The loose point of the bandage is then tucked well in between the forearm and bandage in front and the fold thus formed is turned backwards over the lower part of the arm and pinned (Figs. 31 and 32).
IMPROVISED SLINGS
Slings may be improvised in many simple ways, for example, by pinning the sleeve to the clothing; by turning up and pinning the lower edge of the coat; by passing the hand inside the buttoned coat or waistcoat. Scarves, ties, belts and the like may also be used as slings.
APPLICATION OF BANDAGES
(for the retention of dressings)
In practising bandaging the First Aid student is advised t o place a pad of wool or other material on the part to be b andaged to represent a dressing.
31
JOHN SLING ( FINAL STAGE) (Front View )

30
32
JOHN SLING ( FINAL STAGE) (Back View)
For the Scalp. (Fig. 33 ) . Fold a hero inwards along the base of an open bandage; stand behind the patient and p lace the open bandage on his head so that the hem lies on his forehead close down to his eyebrows, and the point hangs down at the back of his head. Gather the ends together an d carry them round the head just above the ears to the back, cross the ends over the point of the bandage low down
FIG . 33 BANDAGE FOR SCALP
n ear the nape of the neck, bring them forward round the h ead above the ears and tie them in a knot on the forehead clos e to the lower border of the bandage. Steady the patient's h ead with one hand and with the other draw the point of the bandage downwards; then turn it up and pin it to the b an dage on the top of the patient's head.
For the Forehead, Side of the Head, Eye, Cheek, and f or any part of the body that is round. The narrow or
broad bandage should be used according to the requirements of the case , the centre being placed over the dressing, and the ends carriej round the head or limb, cro ssed, and then tied in the most convenient position. Redundant bandage may be taken round the limb and tied.

FIG. 34
BANDAGE FOR CHEST (Front View)
FIG. 35 BANDAGE FOR CHEST (Bac k View )
For the Front of the Chest. (Figs. 34 and 35 ) . Stand in front of the patient and place the centre of an open bandage over the dressing with the point over his shoulder on the same side; fold a three-inch hem inwards along the base of the bandage, carry the ends round the patient's waist and tie them, leaving one end longer than the other; then di.".'\w the point over his shoulder and tie it to the longer end.
For the Back of the Chest. Stand behind the patient and proceed as for the bandage for the front of the chest.
55
For the Shoulder. (Fig. 36). Stand facing the patient's injured side and place the centre of an open bandage on his shoulder, with the point running up the side of the neck; fold a hem inwards alon g the base, carry the ends round the middle of the arm, cross and tie them on the outer side so as to secure the lower border of the bandag e. Apply an arm sling. Turn down the point of the ftrst b andage over the knot of the sling, draw it tight and pin it.
For the Elbow. (Fig . 37). FIG. 36
B end the patient's elb o w to BANDAGE FOR SHOULDER a right angle. Fold a n a rrow hem inwards along the ba se of an open bandage; lay th e point 011 the back of the arm and the middle of the base on th e b ack cf the forearm; cross the ends in front of the elbow, then round [he arm and tie above the elbow. Bring t he p oir.t down over the knot
FIG. 37-BANDAGE FOR ELBOW
and elbow and pin it. If it is inadvisable to bend the elbow a narrow or broad bandage should be used. '
For the 38). Place an open bandage over the mJury bemg uppermost-with the point away fro.m the and the base of the bandage at the wrist. Brmg the pomt under the hand to the wrist and after folding

38
BANDAGE FOR HAND
39
BANDAGE FOR HIP
a hem inwards along the base of the bandage, pass the ends the w!ist, cross them and finally tie over the point; brmg the pomt over the knot and pin it to the bandage over the hand.
For the Hip or Groin. (Fig. 39) . Stand or kneeJ facing the hip to be bandaged and tie a narrow bandage round the
57
body, with a knot on the injured side. Carry the point of an open bandage under the first bandage and turn it down over the knot. Fold a hem inwards according to the size of the patient along the base of the open bandage, carry the ends round the thigh, cross them and tie them on the outer part of the thigh so as to secure the lower border of the bandage; fix the point of the bandage with a safety pin.
40
I
For the Knee. (Fig. 40). Bend the patient's knee to a right angle. Fold a narrow hem inwards along the base of an open bandage; lay the point on his thigh the. middle of the base below his knee; cro ss the ends behind hi s knee, then round hi s thigh and tie above his knee on the front of his thigh. Bring the point down over the knot and knee and pin it. If it is inadvisable to bend the patient's knee, a narrow or broad bandage should be used.
For the Foot. (Fig. 41 ) . Place the patient's foot on the centre of an open bandage with his toes towards the point;
FIG. FIG. FIG. BANDAGE FOR KNEE FIG·4 BANDAGE FOR FOOTdraw up the point over his instep, bring the ends forward so that his heel is covered and cross them; pass the ends round the ankle, cross at back and then tie them in front. Draw the point forward and pin it to the b a ndage over the instep. For a Stump. Fold a narrow hem inwards along the base of an open bandage. Place the base of the bandage high up on the under side of the stump with the point hanging down . Draw the point up over the stump (Fig. 42) and cross th e ends in front over the point (Fig . 43). Carry the ends behind the stump, cross them again, bring them forward and tie in front (Fig. 44). Bring the po.int down over the knot and pin it (Fig·45).
A Ring Pad. This pad is used to control bleeding from a wound of the scalp when foreign bodies or broken bone are present. To make a ring pad pass one end of a narrow bandage round the fingers; then bring the other end of the bandage through the loop thus formed and continue to pass it through and through until the whole of the bandage is used and a firm ring (Fig. 46 ) is formed.

BANDAGE FOR STUMP (FOUR STAGES)
When not in use the triangular bandage should be folded narrow; the two ends should be folded to the centre, the bandage folded to the centre again and then folded in two, reducing it to a packet about in. by in.
FIG. 42 FIG. 43 FIG. 44 FIG. 45
1. NERVE SHOCK
CHAPTER IV
SHOCK
Shock is a condition of prostration of the body aflsmg from sudden exhaustion of vital activities. Shock may vary appreciably in degree according to circumstances, particularly according to the type and severity of the causative factors. As shock is a common cause of death when the patient is not killed outright, prompt and efficient First Aid treaonent is of paramount importance.
FACTORS CONCERNED IN THE PRODUCTION OF SHOCK
(a) Injury.
(b) Emotion (which may be the sole cause, or may complicate the shock produced by 'Injury').
(c) Medical emergencies (e.g., colic, perforation of an acute appendix, etc.).
The degree of shock may be aggravated by the age or constitution of the patient, e.g., old people or persons debilitated as a result of disease react more severely.
TYPES OF SHOCK
There are three types of shock and they may occur singly or in combination :-
I. Nerve. 2. Hremorrhagic.
3. Toxic.
These give rise to characteristic signs and symptoms, which may vary appreciably in degree.
Nerve Shock is of immediate onset and may vary from no more than a feeling of faintness to complete unconsciousness. It is characterised by a sudden fall of blood pressure (see page 90), so leading to insufficiency of blood in the brain.
(a) WARNING INDICATIONS
(i) Pallor of the face and lips, with beads of cold sweat appearing on the brow.
(ii) Yawning, overbreathing, or sighing respiration.
(iii) The patient may complain of a sensation of heat.
Some or all of these may be noticed before consciousness is lost, thus allowing time for preventive action to be taken.
(b) SIGNS AND SYMPTOMS OF NERVE SHOCK
(i) The face and skin are cold, pale and clammy.
(ii) The pulse is feeble. In the earlier stages it is slow, but later it becomes rapid and may be imperceptible at the wrist.
(iii) Breathi'ng is irregular.
(iv) The pupils are usually dilated.
(v) There is general weakness, resulting from loss of muscle tone.
(vi) There is a varying degree of insensibility. (See page 161). When the patient is not fully unconscious, there is giddiness with clouding of consciousness, more marked in the upright position. This phase also occurs during the onset of and recovery from complete unconsciousness.
(c) COURSE OF NERVE SHOCK
(i) The condition may pass off in a few seconds or minutes.
(ii ) Recovery may be retarded by apparent or concealed hremorrhage.
(iii) The condition may merge with that of toxic shock (and this in turn may be further complicated by hremorrhage) .
(iv) The severity of the condition may cause death.
2. HJEMORRHAGIC SHOCK
Hremorrhagic Shock is general'y preceded or accompanied by some of nerve shock.
SIGNS AND SYMPTOMS
(i) The face and skin are cold, pale and clammy. Blueness is often observed, more particularly in the lips and the finger tips.
(ii) The pulse is rapid and feeble.
(iii ) The breathing becomes shallower and, if hremorrhage is severe, air hunger (see page 107) will supervene.
(iv) The pupils may be normal in size or dilated.
(v) The patient may be apprehensive and restless, or talkative and abnormally cheerful. Unconsciousness may supervene on either state.
(vi) There is often little complaint of pain but, when this is marked, vomiting may occur.
(vii) The patient complains of intense thirst and, if fluids are taken in quantity, vomiting may result.
3. TOXIC SHOCK
Toxic Shock results from serious injuries such as crushing ; the effects of blast; fracture of large bones (e.g., femur)
or of the spine; and burns (especially of the face and abdomen ) ; and particularly when infection supervenes on these injuries. This variety of shock is due to the formation of poi sonous (toxic) substances, which gain entrance to the blood-stream, and to loss of fluid from the blood into the tissues.
SIGNS AND SYMPTOMS
(i)

(ii)
The face and skin are cold, pale and clammy, with beads of cold sweat appearing on the forehead. In more severe cases, the pallor tends to become blue, grey or even leaden. This change of colour is first apparent in the lips, lobes of the ears and finger tips. The pulse is rapid and feeble and may be imperceptible, at the wrist. A sustained pul se of 100 per minute, when due only to toxic shock, indicates a serious condition.
(iii)
The breathing is shallow and rapid and, when toxic shock is complicated by hremorrhage, air hunger may supervene.
(iv) The lips and mouth are dry, and the tongue is furred.
(v) The eyes have a glassy or vacant stare and the pupils are dilated. The longer the dilatation persists, the more serious is the patient's condition.
(vi) General weakness persists and is accompanied by sensations of faintness, giddiness, or even nausea. If the condition develops, insensibility deepens and death may ensue.
The severity of shock in any particular case depends upon the type and severity of the causative and contributory fa ctors (see Appendix II).

TREATMENT OF SHOCK
This may be dealt with under three headings :-
(a) Preventive action following warning indications.
(b) Immediate action in established cases.
(c) Subsequent action at shelter, pending arrival of medical aid.
(a) PREVENTIVE ACTION FOLLOWING WARNING INDICATIONS
(i) Remove the patient from crowds or a stuffy atmosphere.
(ii) Lay the patient on his back on a rug in a suitable place, e.g., if out-of-doors on a hot sunny day, put him in the shade.
(In the case of a threatened faint, it may often be more expedient and quicker to place the patient's head between his knees immediately and to move him later).
(iii) Raise well his lower limbs unless contra-indicated by the nature of the injuries, and undo tight clothing about his neck, chest and waist.
(iv) Give cold water in sips, or stimulate the patient, if necessary, by one of the methods described in Rule b (viii).
(b) IMMEDIATE ACTION IN ESTABLISHED CASES
(i) Arrest severe hremorrhage, if present.
(ii) Lay the patient on his back on a blanket, carefully steadying and supporting any injured part.
(iii ) Keep his head and shoulders low, turn his head to one side, and raise his lower limbs unless contra-indicated by the nature of the
(In a true faint breathing may cease momentarily, but rapidly returns when the head is lowered).
(iv) Loosen all clothing about his neck, chest and waist, and ensure a free circulation of air. In particular, remove all wet clothing.
(v ) Examine for and prevent aggravation of injuries and treat the patient.
(vi) While the pulse remains feeble, apply vigorous friction to the uninjured limbs on their inner sides towards the heart.
(vii ) Ensure that the patient is warm. Wrap him in blankets, coats and the like, not forgetting exposed surfaces such as the hands and face. Care must be taken not to impede breathing by the use of heavy coverings tucked in too tight y. Heat, in the form of hot water bottles, can then be applied outside the coverings (which will preclude the possibility of burning a patient), but with stress on "warmth" rather than "heat."
It is essential that the patient be not overheated to the point of flushing, as sweating may follow, thus increasing shock by reducing the amount of fluid in the body. Aim to preserve body heat and prevent the patient from becoming colder rather than try to warm him up too much. This is most important in cases of severe burns; when there has been hremorrhage; or when hremorrhage is still uncontrolled.
(viii) StiInulate the patient by such suitable methods as are immediate 1y available, bearing in mind that nothing must be given by the mouth when injury to an internal organ is suspected, or when the patient is unable to swallow, e.g., as in insensibility. Other-
(x)

wise,when the patient is conscious and able to swallow, he may be given strong tea or coffee with plenty of sugar, meat extracts or milk, all as hot as can be drunk, or half a teaspoonful of sal volatile in half a tumblerful of water. Alcohol is less suitable than sal volatile, and must be withheld when hremorrha g e is obvious or suspected. Ampoules of ammonia m ay be crushed in a handkerchief, or smelling salts held cautiously to the patient's nose; in each case test the strength first. Stimulation may also be effected by sprin 1ling the patient's face with cold and hot water alternatelY; by warmth applied to the pit of the stomach and over the heart; and by vi gorous friction of the limbs as described in Rule b (vi ) . , Prevent excitement and worry, and diminishapprehension, pain and re s tlessness by re-assurance and the appropriate treatment . A ci g arette is often a great comfort and a mental distraction . Never discuss a patient's condition or injuries or those of others within his hearing. Remove the patient to the nearest suitable shelter.
Those patients suffering from severe shock, and therefore in d a nger of losing their lives, must be removed to hospital on a stretcher immediately for special anti-shock treatment such as blood transfusion.
Patients suffering from the effects of crushing should likewise invariably be removed to hospital immediately, even if there are no apparent indications of shocl!; present.
SPECIAL ADDITIONAL TREATMENT IN CRUSH INJURIES OF LIMBS
(xi) In crush injuries of limbs, the severity of the injury depends upon the weight of the crushing factor, the height from which it fell, and the length of time the limb has been subjected to pressure. If the weight can be removed immediately, typical toxic shock does not usually arise . If toxic shock is suspected and no doctor is immediately available , before giving the patient stimulant treatment de scribed in Rule ( b) (viii ), he should be given as much weak alkaline solution as he i s able to take by the mouth, a suitable solution being two teaspoonfuls (one level dessertspoonful) of baking soda (bicarbonate of soda) dissolved in each pint of water. If no alkali i s available, plain water may be used. Although the object is to administer large quantitie s, the fluid should not be given so quickly as to induce nau sea. The fluid should be given , if pos sible, before the limb is released, but it is unwi se to leave the limb crushed while obtaining the alkali unl ess thi s takes only a few minutes to procure. N o te sh ould be .made of the quantity of solution or water admini s t ered.
(c ) SUBSE QUENT ACTION AT SHELT ER, PENDING ARRIVAL OF M E DI CAL AID
(i) Continue with such methods of stimulation as are possible :
(ii ) Re-examine the patient and, if necessary, modify or elaborate the treatment already given.
(iii ) Maintain careful watch on the patient's general condition.
CHAPTER V
RESPIRATION
When the lungs do not get a sufficient quantity of fresh air, they cannot perform their wor k of purifying the blood and inconsequence impure blood circulates around the body. This leads to a dangerous condition called asphyxia characterised by partial or entire cessation of breathing, which may lead to loss of consciousness and often death.

47 FIG. 48
THE UPPER RESPIRATORY TRACT
A. Pharynx D. Trachea
B. Larynx E. Gullet
C. Epiglottis (FIG. 47 Open, FIG. 48 Closed)
In order that the First-Aider may be able to deal with cases of asphyxia, he must know how and why we breathe, i.e ., the anatomy and physiology of respiration.
THE RESPIRATORY SYSTEM
This consists of the respiratory tract, the respiratory mechanism and the respiratory centre.
THE RESPIRATORY TRACT
Air enters through the nose and mouth and passes down the back of the throat (pharynx), whence the air passes into the organ of voice (larynx) . (At its upper end the larynx is protected by a flap (epiglottis), which closes over the top of the larynx while food or fluid is being swallowed and prevents its entry into the larynx (Figs. 47 and 48).) From the larynx the air passes into the windpipe (trachea). About two inches below the top of the breast-bone (sternum), the trac hea divides into a right and left air tube (bronchus). Thes e bronchi pass into the right and left lung respectively an d in the lung-substance divide into smaller tubes (bronchioles). Finally the bronchioles enter the air sacs (alveoli} of the lungs (Figs. 49 and 50) where the interchange of gases ta kes place, as explained in Chapter VI.
The lungs, which occupy the greater part of the chest (thorax), lie immediately above the diaphragm and are protected by the ribs. The lungs consist of large numbers of alveoli, venous and arterial capillaries, veins and arteries an d connective tissue. The part of the lung where the bronchus and the large arteries enter and the large veins emerge is known as the root of the lung. The lungs are l O, c:red by a membrane, the pleura, which at the root of the 1ung passes on to the chest wall which it lines.
7 1
These two layers of pleura are known as visceral (lung) pleura and parietal (wall) pleura, but they are two layers of one membrane and NOT two separate membranes.

49
THE LOWER RESPIRATORY TRACT SHOWING SECTION
FIG. 50
TERMINAL BRONCHUS, BRONCHIOLE AND ALVEOLI
A. Terminal Bronchus
B. Bronchiole
C. Alveoli
THE RESPIRATORY MECHANISM
Respiration is normally effected by the action of the diaphragm and the ribs and consists of three phasesinspiration, expiration and a pause.
On inspiration the diaphragm contracts and its domeshaped centre becomes flattened, thereby increasing the cubic capacity of the chest from above downwards. The ribs, which are normally inclined downwards and forwards, rise outwards and upwards, thereby increasing the cubic capacity of the chest from front to back. The muscles
FIG. A. Trachea C. B. Bronchus D. RIGHT LUNG IN Lung Bronchioles
responsible for this are the outer of the two layers of muscles occupying the spaces between the ribs. This would not in itself cause air to be drawn in, were it not for the elasticity of the lungs and the fact that for physical reasons the two layers of pleura (parietal and visceral) keep in close contact and thus the lungs themselves become enlarged and air is drawn into them.
In expiration the reverse process takes place owing to the relaxation of the diaphragm and of the action of the inner of the two layers of muscles occupying the spaces between the ribs.
The muscles of the abdominal wall also play a part in respiration: when the diaphragm descends they relax to allow room for the displaced abdominal organs; when the diaphragm ascends they contract.
THE RESPIRATORY CENTRE
At the base of the skull in the brain substance there is an area known as the respiratory centre which controls respiration. This centre reacts to various forms of stimulation, the most important of which from the point of view is an increase of carbon dioxide in the blood.
Anything which interferes with the respiratory processes produces asphyxia and this calls for prompt and intelligent attention if life is to be saved.
ASPHYXIA
1. CAUSES AFFECTING THE RESPIRATORY TRACT
(a) Foreign bodies in the air passages causing choking, e.g., portions of food, artificial teeth, vomited matter in the case
of an unconscious person (owing to failure of the action of the epiglottis ), tongue falling back in the case of .an unconscious person, blood collecting from a fractured Jaw, weeds (in drowning). .. .
(b) Compression of the wrndpIpe, e.g ., hangrng, strang ulation or throttling. . .
(c) Smothering, e.g., overlying an mfant, an unconSCIOUS person lying face downward on a pillow. . .
(d) Foreign fluid in the air passages as m drownmg.
(e) Foreign gases in the air passages, e.g., coal gas, motor exhaust fumes, after-damp fumes, smoke, sewer gas, ammorua.
(f) Swelling of the tissues within the throat as a result of burns, scalds, corrosives, stings (wasp or bee), or from some diseases affecting the throat.
2. CAUSES AFFECTING THE RESPIRATORY MECHANISM
(a) Pressure on or crush of the. chest from accidents in mines, quarries, sand PIts or demolitIOns, or from pressure in a crowd. .
(b) Spasm of respiratory muscles m the case of certain poisons, e.g., strychnine (s ee qh:lpter
(c) Nervous diseases causmg of t?e c:hest muscles or the diaphragm, e.g., infantile paralysIs, diphthena.
(d) Tetanus (lockjaw).
3. CAUSES AFFECTING THE RESPIRATORY CENTRE
(a) Electric shock.
(b) Stroke by lightning.
(c) Poisons such as prussic acid and strychnine (see Chapter XII).
SIGNS AND SYMPTOMS OF ASPHYXIA
Early Stages
(i) Dizziness and weakness.
(ii) Pain over the heart.
(iii) Shortness of breath and difficulty in breathing.
(iv) Rapid breathing.
(v) Rapid pulse.
(vi) Possibly irregular breathing.
(vii) Partial loss of consciousness.
These signs and symptoms may vary with the degree of asphyxia present.
Later Stages
(viii) fhe lips, nose, ears, fingers and toes are bluish-grey·
(ix) Swelling of the veins of the neck.
(x) Breathing intermittent or absent.
(xi ) Pulse slow and irregular.
(xii) Complete loss of consciousness.
GENERAL RULES FOR TREATMENT OF ASPHYXIA
1. Remove the cause if possible or the patient from the cause.
2. Ensure that there is a free passage for air.
3· Apply artificial respiration (see pages 78-85).
4. Utilise any help available to :
(a) provide warmth, e.g ., blankets, hot water bottles;
(b) provide shelter from the elements;
(c) promote circulation by vigorous friction of the inner side of the limbs towards the heart.

SPECIAL TREATMENT IN SPECIAL CASES
DROWNING .
While artificial respiration is being performed, instruct bystanders to remove wet clothing as far as practicable and wrap the patient in dry blankets or other dry clothing.
STRANGULATION
Cut and remove the band constricting the throat.
HAN GING
Do not wait for a policeman. Grasp the lower limbs and raise the body. Cut the rope and free the neck.
CHOKING
To dislodge the obstruction bend the patient's head and shoulders forward and thump his back hard between the shoulder-blades. If this is not successful, encourage vomiting by passing two fingers right to the back of the patient's throat.
SWELLING OF THE TISSUES WITHIN THE THROAT
If possible seat the patient before a fire. Ap ply hot compresses to his neck from chin to breast-bone and renew them frequently. If breathing has not ceased or when it has been restored give ice to suck or, failing ice, cold water to sip. Butter, olive oil or medicinal paraffin may also be given.
SUFFOCATION BY SMOKE
Ensure plenty of fresh air by opening or if necessary by breaking doors and windows. Protect yourself by tying a towel, handkerchief or cloth, preferab ;y wet, over your mouth and nose.
SUFFOCATION BY POISONOUS GAS
On entering any enclosed space known or susJ?ected. to contain poisonous gas of any kind, ensure a cIrculatIOn of air by opening or if necessary by breaking doors and windows. .
Hold your breath and, if the gas rur, keep low; if heavier, remain in the upnght posltlon. Remove the patient as quick ly as possible. .

500, although in a few cases there may be equipment at voltages as high as 6,600 or 11,000.
If the patient is still in contact with a live conductor before attempting to free him switch off the current if possible. If the switch cannot be found quickly the patient should be freed from contact without delay, the procedure varying as follows according to the voltage :-
In cases where ventilation is not possIble and the character of the gas is known to be deadly, a suitable gas mask must be worn.
.th
Gases lighter than air which are most commonly WI . are: Carbon monoxide (found as a result of combustIon III car exhaust vapours and in coal gas and as a result of incomplete combustion, i.e., charcoal stoves and as white-damp in coalmines). Methane or marsh gas (found as its name implies in marshes and as fire-damp in coalmines).
Gases heavier than air which are most commonly met with are: Carbon dioxide (found in the black-damp of coalmines).
Sulphuretted hydrogen (found in sewer gas).
ELECTRIC SHOCK
This is an emergency which calls for prompt and intelligent action-prompt action if the to be ; intelligent action, where the IS stIll III contact WIth a live conductor, if two casualtIes mstead of one are to be avoided. . .
Cases most likely to be encountered are III domestIc or office premises where the voltage does not exceed 250 and in factories where, in general, the voltage does not exceed
(a) For vo ltag es up to 500, take precautions against receiving an electric shock yourself in handling the patient by the use of some dry insulating material such as a pair of rubber gloves, a cap, a coat or other dry garment. Avoid direct contact with the patient's skin or any part of his clothing which may be damp, e.g., under the armpits. A dry crooked wooden stick may be useful, but an umbrella is not suitable owing to the metal ribs and in some cases the metal "stick" of the umbrella. A length of dry rope is another alternative. If possible it is also a good precaution to stand on dry insulating material such as a rubber mat, linoleum, thick carpet or rug. Where the supply to the live co nductor involved is through a flexible cable the current may be cut off by removing the plug or even breaking the ca ble by pulling on it. Do not attempt to cut the cable with a knife or scissors.
(
b) If the voltage of the supply involved is higher than 500 (and in electricity stations or on overhead lines it may be as high as 132,000 volts) it is likely that a person who has had such an electric shock will be found near the conductor rather than in contact with it. Leave the rescue in such cases if possible to a properly trained electrical man. Although there is no danger if the current is switched off, anyone not suitably trained in electrical work is unlikely to

know whether 0 :[ not a conductor is "live." In the absence of anyone trained in electrical work, if the circumstances warrant an attempt at rescue, approach with great caution keeping the greatest possible distance between yourself and any part of the electrical equipment. Do not handle the patient directly but use a long dry wooden stick or a length of dry rope, keeping as far away from him as possible. Wear rubber gloves made for electrical purposes (the household variety give little protection for voltages higher than 500) and/or rubber boots if readi lY availa ble, but above all remember that unless the current is switched off a rescue of this nature by persons with little knowledge of electricity may be a hazardous procedure.
In cases of electric shock the patient is usually unconscious and the act of breathing is wholly or partially suspended. In addition electric shock, particularly at the higher voltages, is often accompanied by burns which may be very severe.
TREATMENT IN ALL CASES OF ELECTRIC SHOCK
1. Unless the patient is breathing normally immediately commence artificial respiration.
2. Treat any burns after breathing is restored.
ARTIFICIAL RESPIRATION SCHAFER'S METHOD
Adjust the Patient's Position. At once lay the patient in a prone position (i. e ., face downwards) with hi s arms above his head and the palm s of his hands on th e ground. Turn his head to one side to keep his no se and mouth away from the ground. Do not W.1ste time in loosening clothing. A pad under the patient is not required nor need his tongue be drawn out. 79
Turning the Patient. Should the patient be lying on hi s back, turn him to the prone position as follows ;-
(i) Stoop at his side.
(ii ) Place his arms close to his body.
(iii) Cross his far leg over hi s near leg .
(iv) Protect his face with one of your hands.
(v) Grasp his clothing at the hip on the opposite side of the body and quickly and gently turn him over.
Position of Operator
(i) Face the patient' s head.
(ii) Kneel on both knees in a position just below his hip-joint (Fig .5 r ).
G . 51
ARTI F I CI AL RESPIRATION ( Schafer' S Method )
(iii) (iv )
Sit back on your heels at the patient's side in a position to allow free sway. Place your hands on the of. the patient, one. on each side of the backbone wIth WrIsts almost touchmg, with thumbs as far forward as possible without strain,

(v)
ARTIFICIAL RESPIRATION (Schafer's Method) ., and the fingers close together at the side of the and bent over the flanks in the natural hollows Just above the brim of the pelvis but clear of it, the tips of the fingers pointing to the ground (Fig. 52). Keep your elbows quite straight.
52
Application of Artificial Respiration
Mo ve m ent I
Without bending your elbows, swing slowly forward by unbending the knee s until the thighs are in an almost upright position and the shoulders vertically above the hands, so allowing the weight of your body to be communicated to the patient' s loins ( Fig. 53 ) .
53
ARTIFICI AL RESPIRATION (Scha fer ' s M e thod )
This causes the patient's abdominal organs to be compressed against the ground and up against the diaphragm .
Air is thus forced out of the lungs, t.e., expiration takes place.
The compression in movement 1 is to be effected solely by the weight of the operator's body and not by muscular effort.
Movement 2
Swing slowly back on to your heels thus relaxing the pressure.
This causes the abdominal organs to fall back and the diaphragm to drop, thus inducing inspiration.
Rhythm
The two movements, which must be carried out smoothly and rhythmically, should take five seconds (i.e., 12 times a minute), two seconds being occupied by movement 1 and three seconds by movement 2.
Changing Operators
I t may frequently be found necessary to change operators as follows:-
The relief takes up a position at the opposite side of the patient to the operator, places his hands over those of the operator without exercising any pressure and gradually falls into the rhythm of his movements. After working thus together for a few seconds the operator arrives at the "off" position (i.e., relaxation). He should carefully remove his hands whilst at the same

time the hands of the relief occupy the vacated position. The movements are thus carried on without any jerk or disturbance of rhythm .
When natural breathing begins the rate of artificial respiration must be adapted to correspond with it.
Artificial respiration must be continued perseveringly until natural breathing is restored, unless a Doctor decides that further efforts will be of no avail.
SILVESTER'S METHOD
This method is to be used only when it is impossible or inexpedient to turn the patient on to his face.
Adjust the Patient's Position.
(i) Immediately place the patient on his back on a flat surface.
(ii) Undo all his tight clothing.
(iii) Raise and support his shoulders on a cushion or folded article of clothing in such a way that his head hangs backwards.
Maintain a free entrance of air into windpipe. In order to prevent the tongue falling back and obstructing the windpipe, an assistant must grasp the tongue firmly with a handkerchief, draw it forward as far as possible and hold it there. If no assistant is available, the patient's head must be turned as far as possible to one side.
85
Application of Artificial Respiration
Movement I
Kneel just above the patient's head, place his forearms on his chest as near each other as possible, and grasp them firm'y below the elbows. Draw his arms upwards, outwards and towards you with a sweeping movement, pressing his elbows towards the ground (Fig·54)·

54
ARTIFICIAL RESPIRATION (Silvester's Method)
This causes an expansion of the cavity of the chest and thus air is drawn into the lungs, i.e., inspiration.
Movement 2
Bring his flexed arms slowly back along the same route
and press them firmly against the front and ribs of his c?est (Fig. 55). This forces air out of the lungs, i.e., expiratIon.
55
ARTIFICIAL RESPIRATIO N ( Silvester's Method )
Rhythm
These m?vemems, which must be carried out smoothly rhythmIcally, should be performed I2 times per minute, z.e., each completed cycle should take five seconds, three seconds for movement 1 and two seconds for movement 2.
When natural breathing begins, the rate of artificial respiration must be adapted to correspond with it.
Artificial respiration must be continued perseveringly until natural breathing is restored unless a Doctor decides that further efforts will be no avail.
FIG. FIG.
85 (a)
SUPPLEMENT TO CHAPTER V OF "FIRST AID TO THE INJURED"
ARTIFICIAL RESPIRATION " HOLGER NIELSEN" METHOD
Position of Patient
Lay the patient in the prone posltlon on a fiat surface. If there is a slight slope place the head low if the face is pale; high if the face is congested.
Place the patient's hands one over the other, under his forehead. If this is insufficient to keep the nose and mouth from the ground, the head must be turned slightly to one side. The nose and mouth must be unobstructed.
Turning
If the patient is lying on his back turn him to the prone position as follows. Go down on the right knee opposite the patient's head. Place the left foot on the ground out to the side.
Place the patient's arms carefully above his head and keep them there during the turn.
Grasp the patient's left upper arm and turn him over, protecting his face with the right hand. Adjust the position of the patient's hands as previously instructed.
Slap the patient smartly several times between the shoulders with the fiat of the hand. This helps the tongue
85 (b )
to fall forward and drives out any water which may have been inhaled in drowning cases .
Position of Operator
Place one knee with the inner side in line with the patient's cheek six to twelve inches from the top of the patient' s head .

B
85 (c)
Place the other foot with the heel in line with the patient's elbow.
Place the hands on the patient's back with the palms resting on the shoulder blades, the thumbs on the spine and the fingers pointing to the patient's feet. (Figs. A and B).

CIDLDREN
For children down to the age of 5 years the pressure on the shoulder blades should be considerably reduced and applied with the finger tips only. The rate should be 12 times per minute. (Figs. I and J).
The operator should be nearer the patient and after pressing on the shoulder-blades for Expiration (Movement I), should place his hands under the shoulders and raise them for Inspiration (Movement 2). He should then lower them and continue with Movement I at the standard rate of 8 t o 9 times per minute. (Fig. M).
SCHAFER-HOLGER NIELSEN METHOD OF ARTIFICIAL RESPIRATION
When two operators are available it may be found advantageous to combine the expiratory movement of Schafer's method of artificial respiration with the inspiratory movement of the Holger Nielsen method.
Application of Schafer-Holger Nielsen Method of Artificial Respiration
Adjust the patient's position as for the Holger Nielsen method.
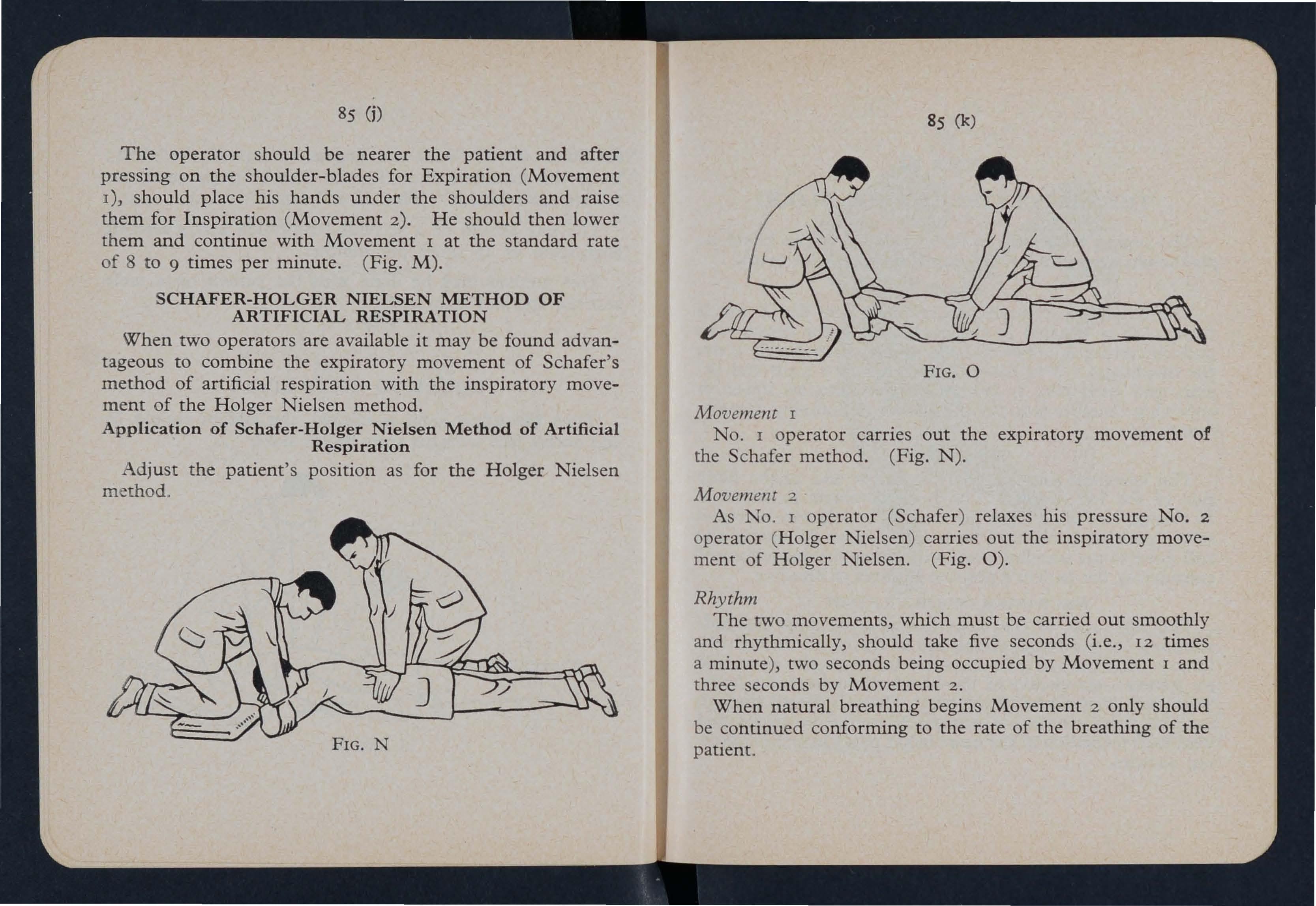
85 (k)
FIG. 0
Movement I
No. I operator carries out the expiratory movement of the Schafer method. (Fig. N).
Movement 2
As No. 1 operator ( Schafer) relaxes his pressure No. 2 ope rator (Holger Nielsen ) carries out the inspiratory movement of Holger Nielsen. (Fig. 0).
Rhythm
The two movements, which must be carried out smoothly and rhythmically, should take five seconds (i.e., 12 times a minute), two seconds being occupied by Movement 1 and th ree seconds by Movement 2.
When natural breathing begins Movement 2 only should be continued conforming to the rate of the breathing of the patient.
CHAPTER VI
THE CIRCULATION OF THE BLOOD
The organs concerned in the circulation of the blood are the heart, the arteries, the capillaries and the veins.
HEART
The heart is a muscular organ which acts like a double pump. It is situated in the chest behind the breast-bone and rib cartilages, between the lungs and immediately above the diaphragm. The heart is divided into a right and left side, and each side is further divided into an upper or collecting chamber (auricle) and a lower or pumping chamber (ventricle).
HEARTBEAT
The heartbeat may be felt just below and to the inner side of the left nipple. The heart contracts in adults at an average rate of 72 times per minute, but the rate increases as the position is changed from the lying to the sitting and still more to the standing position; hence the importance of considering the patient's position in cases of bleeding.
MECHANISM OF CIRCULATION
The right side of the heart is connected with the pulmonary (or purifying) circulation of the blood through the lungs; and the left side is connected with the systetnic (or general) circulation of the blood throughout the body. With each contraction of the heart, blood is forced through both of these circulation systems from the ventricles and with each relaxation of the heart blood pours into the collecting auricles.

56
DIAGRAMMATIC ILLUSTRATION OF THE H EA RT SHOWING THE ENTRY AND EXIT OF THE ARTERIES AND VEINS
The arrows indicate the direction of the blood flow.
R.L. Right Lung; L.L. Left Lung; LV.C. Inferior vena cava (the large vein carrYlIlg blood from the lower part of the body to the! heart); S. V.C Superior vena cava (the large vein carrying blood from the upper part of the body to the heart) ; R.A. Right Auricle; L.A. Left Auricle; R.V. Right Ventricle; L.V. Left Ventricle; P.A. Pulmonary Arteries; P.V. Pulmonary Veins j A.A. Abdominal Aorta.
88
Pulmonary Circulation. Impure blood is collected from the two large veins draining the upper and lower parts of the body into the right auricle and from this chamber passes through a valve to the right ventricle, whence it is forced by compression through the pulmonary artery to the lungs. In the lungs it gives off carbon dioxide gas and water vapour, and is purified by picking up oxygen gas from the inspired air. This process is known as the interchange of gases. After purification the blood returns to the left auricle through the four pulmonary veins.

Systemic Circulation. The pure blood from the left auricle passes through a valve to the left ventricle and from there is forced out through the aorta to the arteries and capillaries and so to all parts of the body.
89
ARTERIES, CAPILLARIES AND VEINS
These are known as the blood-vessels of the body and are the tubes in which the blood circulates.
Arteries are the strongest vessels because they have to withstand the surge of blood from each powerful heart contraction. They have an internal lining, a middle elastic
59
V ALVES OF VEIN
58
SECTION
FIG. 60
VALVES OF VEIN (Closed) and muscular coat, and an outer fibrous covering. The vessels expand with the volume of blood forced along them and return to their normal size while the heart fills up ready for the next contraction. Arteries penetrate to all parts of the body, dividing and sub-dividing and becoming smaller and smaller until they are known as capillaries.
FIG 57 CAPILLARIES FIG. OF VEIN SHOWING VALVES FIG. (Open)Capillaries are very small blood-vessels with an averag e diameter of about 1/3000 of an inch. The two outer coats of the arteries gradually disappear leaving the thin inner coat, which allows the passage of fluids and the diffusio n of gases to and from the tissue cells.
Veins are formed by the joining up of the capillaries . The smaller veins unite to form larger veins until they termin a te in the upper and lower venae cavae as these enter the right auricle. The structure of the vein is much strong er than that of the capillary, but a vein does not contain as mu c h muscular or elastic tissue as an artery. Most vein s have numerous valves which allow the blood to flow toward s the heart, but prevent its flowing in the opposite direction.
BLOOD PRESSURE
The pressure of the blood in the arteries is called the blood pressure and is maintained by the force of the heart's contraction, the elasticity of the arteries and the for ce required to push the blood through the capillary section of the circulation. It follows, therefore, that if an artery is cut , blood will spurt out with considerable force, varying according to the size of the artery. The pressure decreases in the small arteries and capillaries owing to their large sectional area. Blood pressure is, therefore, greatest in the arterie s, less in capillaries and least in the veins.
BLOOD
Blood is the liquid which flows in the blood-vessels and is carried in them to all parts of the body tissue with the exception of a few like cartilage, outer layer of the skin, nails and hair. It consists of a transparent yellow fluid

91
called blood plasma in which float large numbers of bloodcorpuscles. These are of two types, red and white, the being comparatively small in number. . Blood carnes nutritive matter from digested foodstuffs In the bowel to all cells and tissues of the body. It also carries waste matter to the excretory organs, oxygen to the tissues, and the oxidi sation product (carbon dioxide) from the tissues to the lungs, where as already explained the interchange of gases takes place. Blood carrying bright red colour and blood carrying carbon diOXIde IS dark red ill colour.
Blood tends to clot when it escapes from the blood-vessels and clots formed should never be disturbed when present over a wound as they serve to keep blood in and germs out.
CHAPTER VII
WOUNDS AND HlEMORRHAGE
A wound is a break in the continuity of the tissues of the body which thus permits the escape of blood and the entrance of disease-producing germs or other injurious agents.
WOUNDS
Wounds may be classified as follows :-
1. Incised Wounds, which are caused by a sharp Instrument, such as a razor, and bleed freely because the blood-vessels are "clean cut."
2. Lacerated Wounds, which have torn and irregular They are caused by such things as machinery, a pIece of shell or the claws of an animal. As the bloodvessel.s torn through, lacerated wounds bleed less freely mCIsed wounds, and the bleeding may be delayed for a tune.
3: . Contused . Wounds, which are accompanied by brUlsmg of the. tIssues, and are caused by a direct blow by some blunt mstrument or by crushing.
4· . Punctured Wounds, which have comparatively small openmgs, but may be very deep and are caused by a stab from any sharp-pointed instrument, such as a needle, knife or bayonet.
Gun-shot wounds come under one or more of the aboveheadings.
HlEMORRHAGE
Hremorrhage or bleeding may vary in intensity from severe to slight.

Severe Hremorrhage comes from a torn artery or tom vein or both combined. Many large arteries and veins lie close together and are frequently injured together.
Blood from an artery in the systemic circulation is bright red. If the injured artery is near the skin, the blood is seen to spurt out in jets corresponding with the pulsations of the heart.
Blood from a vein is dark red. It flows in a steady continuous stream.
Arterial and venous hremorrhage combined usually gushes out from the depth of the wound.
Slight Hrernorrhage comes usually from injured capillaries and may flow briskly in a continuous stream or merely ooze from all parts of the wound. This type of bleeding is much more easily controlled than severe hremorrhage.
INFECTION
Infection (s epsis) is the presence of disease-producing germs in the tissues of the body. Germs are invisible to the naked eye and can be seen only with the aid of a microscope. They exist in soil, dust, water and in many other places including the skin and intestinal tract of both man and animal. Germs are living organisms and need water, suitable food and a favourable temperature in order to live and multiply. Disease-producing germs find ideal conditions in the tissues of the human body and, when they enter a wound, multiply rapidly and produce the characteristics of infection.
Cleanliness is essential in the prevention of infection, and everything which comes in contact with the wound (han ds, skin, lotions, dressings) must be scrupulously clean.
The hands are best cleaned by thorough scrubbing with soap, water and a nail brush, much attention being paid to the nails.
If scrubbing or washing is not possible, the hands may be rendered sterile (germ-free) by the application of an antiseptic.
An antiseptic is a chemical preparation which has the power of restraining the growth of germs. Certain antiseptics may be used in and around wounds, but it is essential that only those which will not irritate the tissue cells and cause delay in healing be applied. These non-irritating antiseptics may be used in the form of antiseptic creams or lotions. Antiseptic creams contained in collapsible tubes may be used in any circumstances, the cream being squeezed on to the wound before the application of the dressing; but lotions should be used only where circumstances favourable to their preparation are present.
Water may be rendered sterile by boiling and may then be kept hot or allowed to cool.
GENERAL RULES FOR TREATMENT OF WOUNDS ACCOM. PANIED BY SEVERE HlEMORRHAGE
I. Place the patient in a suitable position, bearing in mind that blood escapes with less force when the patient sits and still less when the patient lies down.
2. Elevate the bleeding part, except in the case of a fractured limb.
3· Expose the wound, removing only whatever clothing may be necessary.
4· Do not disturb any blood clot already formed.
5· Remove any foreign bodies which are visible and easily removed.

. h the thumb or thumbs,
6 Apply direct pressuhre WIt f the wound from which . d ' f '1 ble to t e part 0 . . over a pa 1 aVal a, c· body or proJectrng . . When a 10relgn . . the blood IS . h wound press alongsIde It broken bone IS presentb{n ; . e point not readily visible, and not over it. If thed ee squeeze it tightly. This grasp the whole woun bleeding for a time; and by will nearly always contro ,
FOREIGN
bl din points will be found relaxing the grasp slowly, the w1th the thumb. so enabling to .be app le
7· Apply an bantlseptlc. substitute pressure as follows :-
8. For thum pressure. . ro 'ecting broken bone, (a) Wh en th er e. 15 no boc;r the wound, press apply a suitable-slzed dressldng an h Pa firmly in position (see them firmly down and ban age t em
Rule 9) .
FIG. 62
TREATMENT OF WOUND IN WHICH A FOREIGN BODY IS PRESENT FIRST STAGE-COVERING WITH DRESSING .

FIG. 63
TREATMENT OF WOUND IN WHICH A FOREIGN BODY IS PRESENT SECOND STAGE-BuILDING UP PADS
97
Deep wounds may need further pads on top of the first) thus pressing the dressing into the depth of the wound. Ensure that pads project well above the level of the skin in order to provide adequate pressure on the torn ends of the blood-vessels.
(b ) When a foreign body which cannot be easily remo'ved or a projecting broken bone is present in a wound ( Fig. 6 1):(i) When gauze or lint dressings are being used) cover the wound with the dressing ( Fig. 62 ) and build up
FIG. 64
TREATMENT OF WOUND IN WHICH A FOREIGN BODY IS PRESENT. THIRD STAGE-BANDAGE ApPLIED
the pads around the wound to a sufficient height (Fig. 63) to allow for pressure to be applied by the bandage referred to in Rule 9 without pressing on the foreign body or projecting broken bone (Fig. 64).
(ii) When sterile are being used, bUIld them up m cone fashion around the wound to a sufficient height to cover the wound and to allow for pressure to be applied by the diagonal bandage referred to in Rule 9 without pressing on the foreign body or projecting broken bone.
(c) In the case of wounds involving fracture of the dome of the skull, a ring pad must be used.
9 · 0e pads firmly in position. When a foreign body or proJectmg broken bone is present in a wound, it may be advantageous to apply the bandage diagonally (Fig. 64) to prevent pressure on the foreign body or projecting broken bone.
with a tape attachment at the end for fastening. At the end of every 20 minutes the bandage must be relaxed; if bleeding has not ceased, the bandage must be re-tightened. This constrictive bandage (Fig . 65 ) when used should never be covered by subsequent bandages. A note must be made of the application and time applied .

66
CAROTID ARTERY
A . Sterno-Mastoid Muscle
B . Carotid Artery
65
CONSTRICTIVE BANDAGE ROLLED TO SHOW ATTACHED TAPES
. The .bandage should not be applied more tightly than IS sufficIent to stop the bleeding. If blood still soaks through, apply further pads on top with a fresh bandage but do not remove the original bandage and pads. '
10. If bleeding is not controlled by the application of pressure, apply a firm bandage round the limb a few Inches above the wound. It is preferable to use a rubber bandage about four feet long and about 2i- inches wide
I I. Where a limb ha3 been amputated, no time should be wasted in attempting to apply direct pressure, but a constrictive bandage should be immediately applied a few inches above the stump wound .
12 When it is impossible to apply direct pressure successfully for the arrest of arterial hremorrhage, and when the constrictive bandage cannot be used, apply indirect pressure to the appropriate pressure point (see page 100).
FIG.
13· Immobilise the injured part: when the wound is near a joint immobilise the joint.
14· When bleeding has stopped, keep the patient warm ' and give him plenty of fluids, especially warm tea sweetened with sugar.
PRESSURE POINTS
A pressure point is one where an artery can be compressed against the underlying bone to prevent the flow of blood beyond that point.
Carotid Pressure Point. The carotid arteries (Fig. 66 ) are branches of the aorta and pass up on either side of the wind-pipe to supply the head area. To apply digital pressure, place the thumb in the hollow between the lower parr of the larynx and the sterno-mastoid muscle running up the side of the neck and compress the artery below the level of the wound (Fig. 67).
It may also be necessary to apply pressure with the other thumb above the wound, e.g., to arrest the flow of blood from the main vein in the neck (jugular) which runs alongside the carotid artery and is often wounded at the same time.

DIGITAL PRESSURE ON SUBCLAVIAN PRESSURE POINT
Subclavian Pressure Point. The subclavian arteries (Fig. 68) are branches of the aorta and pass from a point behind the inner ends of the collar-bones across the first ribs to the armpits. To apply digital pressure, bare the patient's neck and upper part of his chest; depress his shoulder and incline his head to the injured side. Press one thumb on top of the other in the hollow behind the collar-bone and compress the artery against the first rib (Fig. 69)·
103
Brachial Pressure Point. The brachial arteries (Fig. 70) run along the inner sides of the biceps muscles. The inner seams of the coat sleeves roughly indicate their course. They are the blood supply to both upper limbs. To apply digital pressure place your fingers under the patient's arm and compress the artery against his humerus (Fig. 7I.)
DIGITAL PRESSURE ON BRACHIAL PRESSURE Ponn
Note the taking of the pulse at the wrist
Femoral Pressure
Point. The femoral arteries (Fig. 72) are continuations of the iliac arteries which are branches of the abdominal aorta. They pass into the lower limbs at a point corresponding to the centre of the fold of the groin and run in a line from there to the inside of the knee for two-thirds of the distance at which point they pass to the back of the knees. They are the blood supply to both lower limbs. To apply digital pressure, flex the patient's knee, grasp his thigh with both hands and press directly downwards in the centre of the groin with both thumbs one on top of the other against the brim of the pelvis (Fig. 73).

73
DIGITAL PRESSURE ON FEMORAL PRESSURE POINT
GBNERAL RULES FOR TREATMENT OF WOUNDS ACCOMPANIED BY SLIGHT HlEMORRHAGE
I. Expose the wound, removing only whatever clothing may be necessary.
%. Do not disturb any blood clot already formed.
3. Remove any foreign bodies which are visible and easily removed.
4. Apply an antiseptic.
5. Apply a dressing and appropriate pad.
6. Bandage firmly.
WOUND OF THE ABDOMINAL WALL TREATMENT
A. When there is no protrusion of organs
I. Keep the patient on his back, draw his knees well up and raise his head and shoulders.
2. Apply the general rules for treatment of wounds as far as applicable.
3. Give nothing by the mouth.
B. When internal organs such as the intestines protrude through the wound.
I. Keep the patient on his back, draw his knees well up and raise his head and shoulders.
2. Make no attempt to replace organs, but cover the area with a large piece of lint or a soft towel wrung out of sterilised hot water (at the normal temperature of the bodY,9 8.4 °F .) to which may . be added, if readily available, salt in the proportion of one teaspoonful to a pint of water. Change the application every fifteen minutes.
3. Cover the application with cotton wool or soft clean flannel.
4. Keep the patient warm, but avoid undue pressure to the abdomen when applying hot water bottles to the sides of the body.
5. Give nothing by the mouth.
6. Remove the patient to hospital as speedily as possible.

CHAPTER VI II
HlEMORRHAGE FROM SPECIAL REGIONS
HlEMORRHAGE FROM AN INTERNAL ORGAN
Hremorrhage from an internal organ may result from injury, such as a crush, blow, fracture of a rib, of the pelvis or of the skull, or may be caused by a stab or bullet; or it may be due to disease, in which case no external cause is apparent.
SIGNS AND SYMPTOMS
I. Pallor of the face and lips, and cold clammy skin.
2. The patient complains of thirst and becomes excitable and talkative.
3. Giddiness and faintness, especially when the upright position is assumed.
4. The breathing is hurried and 1aboured and accompanied by yawning and sighing.
5. The pulse fails and may altogether disappear at the wrist.
6. Air hunger, i.e., distressed efforts to breathe characterised by throwing the arms about, tugging at the clothing and calling for air.
7. Finally the patient may become totally
Hremorrhage from an internal organ becomes visible in the following cases :
From the lungs.-Blood is coughed up. It is bright red and frothy.
From the stomach.-Blood is vomited. It sometimes has the appearance of coffee grounds.
From the upper bowel.-Blood is mixed with the freces and gives the stools a black tarry appearance.
From the lower bowel.-Blood in the stools is fresh m appearance.
From the kidneys.-Blood escapes with the urir:e and may be smoky in appearance. There may be pam over the kidney area.
From the bladder.-Blood is present in the urine which is often passed with difficulty. (See page I40-Fracture of the Pelvis).
Hremorrhage from an internal organ remains concealed in the following cases:
From the liver, spleen or pancreas.-The bleeding takes place into the abdominal cavity and does not appear outside the body. It may be a very type of bleeding and should be suspected where the SIgns and symptoms of hremorrhage from aD: internal .organ are present following a crush or blow m the regIOn of the liver, spleen or pancreas.
TREATMENT
1. Remove the patient to hospital at the earliest possible moment.
2 . Give nothing by the mouth.
3 Apply an ice-bag or cold compress over the suspected area .
4 . Pay special attention to the treatment of shock.

109
HlEMORRHAGE FROM THE CHEEK, THE TONGUE, THE GUMS, THE SOCKET OF A TOOTH, OR THE THROAT
Hremorrhage from any of these regions must not be confused with hremorrhage from the lungs or stomach.
TREATMENT
Give ice or cold water to hold in the mouth.
If bleeding from the front part of the cheek or the tongue is excessive, compress the part by a piece of clean lint held between the finger and thumb.
If the bleeding is from the socket of a tooth, plug the socket with a piece of clean lint or cotton wool; over this place a small cork or other substance of suitable size, and instruct the patient to bite on it.
HlEMORRHAGE FROM THE NOSE
TREATMENT
r. Place the patient in a SIttIng position in a current of air before an open window, with his head thrown slightly back and his arms raised above his head.
2. Undo all tight clothing around his neck and chest.
3. Instruct the patient to keep his mouth open, and so avoid breathing through his nose.
4. Apply cold over his nose and also to the spine at the level of the collar; place his feet in hot water.
5. Warn the patient not to blow his nose.
Hl£MORRHAGE
FROM THE EAR CHANNEL
Blood issuing from the ear channel generally indicates a fracture of the base of the skull.
TREATMENT
1. Make no attempt to plug the ear.
2. Incline the head to the affected side and apply a dry dressing over the ear and bandage lightly.
BRUISES
A blow anywhere on the surface of the body may cause extensive capillary hzemorrhage beneath the skin, without breaking it-a "black eye" is an instance. The injury is accompanied by discoloration and swelling.
TREATMENT
Apply pieces of lint soaked in equal parts of spirit and water, or a cold compress.

CHAPTER IX
FRACTURES
DEFINITION
Fracture is the term used to indicate that a bone is broken or cracked.
CAUSES OF FRACTURE
Fractures may result from a variety of causes of which the most common is some form of force or violence :-
1. A fracture may result from direct force when from a severe blow, impact of a bullet, crush by a wheel, etc., a bone breaks at the spot where the force is applied.
2. A fracture may result from indirect force when a bone breaks at some distance from the spot where the force is applied. In such cases the force is the intervening bones which may themselves escape InJury.
3. A fracture may result from the force due to muscular action, e.g., the knee-cap and the bones of the forearm are occasionally broken by a sudden viol ent contraction of the muscles attached to them.
TYPES OF FRACTURE
Fractures may be classified as :-
1. Simple or Closed-when there is no wound leading down to the broken bone (Fig. 74).
2. Compound or Open-when there is a wound leading down to the broken bone or when the fractured ends protrude through the skin, thus allowing disease-producing

FIG. 74
SIMPLE FRACTURE
FIG. 75
COMPOUND FRACTURE
germs to obtain access to the seat of the fracture (Fig. 75). This ty pe of fracture is therefore always more serious than the simple variety.
II3
3. Complicated-when there is associated injury to some important internal structure such as brain, spinal cord, nerve, lung, liver, spleen, kidney, major blood-vessel, or when a fracture at a joint is associated with a dislocation.
FIG. 76
COMMINUTED FRACTURE
There are other varieties of fracture which cannot nor. mally be diagnosed by the First-Aider. These include :(a) Comminuted-when the bone is broken into severa] parts (Fig. 76).
(b) Impacted-when the broken ends are driven into one another (Fig. 77).

FIG. 77
IMPACTED FRACTURE
(c) Greenstick-in the case of children the bone is partially broken and bent without breaking completely across (Fig. 78).
Cd) Depressed-when, in the case of a fracture of the upper part or sides of the skull, the broken part of the bone is driven inwards (Figs. 79 and 80).
lI5
GENERAL SIGNS AND SYMPTOMS OF FRACTURE
1. Pain at or near the seat of fracture.
2. Tenderness or discomfort on gentle pressure over the
FIG . 78 GREENSTICK FRACTURE affected area.
3. Swelling about the seat of fracture.
Swelling frequently renders it difficult to perceive other signs of fracture and care must therefore be taken not to treat the condition as a less serious injury.
4. Limitation of natural movements. The injured part cannot be used normally.
79
DEPRESSED FRACTURE
FIG. 80
lIb

5· of the limb. The limb may assume an unnatural posltlon and be misshapen.
The contracting muscles may cause the broken ends of the bone to override thereby producing shortenin CT of the limb. I:>
6. Irregularity of the bone.
If the fracture is near the skin, the irregularity of the bone may be felt.
7· Crepitus (bony grating) may be heard or felt.
8. Unnatural movement at the seat of the fracture.
The last two signs should never be sought deliberately, but they may be noted during examination.
All signs and symptoms may not be present: those which are may vary in degree.
Comparison with the uninjured side will assist ill the diagnosis.
In addition to these sign s and symptoms, mark s on the clothing or skin may serve to locate the fracture. The snap of the bone may have been heard or felt .
Doubtful cases should be treated as fractures.
GENERAL RULES FOR TREATMENT OF FRACTURES
1. As far as possible attend to the fracture on the spot. No attempt must be made to move the patient until his movements are restrained unless life is in immediate danger from some other cause.
2. Wounds and hremorrhage must be dealt with before the completion of the fracture treatment.
3· Steady and support the injured parts from the outset that movem.ent is impossible, thus preventing further ffiJury; otherwIse the ends of the bones may damage blood-vessels or nerves or pIerce the muscles and skin.
4. In the case of a fractured limb, place the limb with great care and without using force in as natural a position as possible.
5. Immobilise the fracture by the application of bandages using the patient's body as a means of support. Adequate p adding must be used to secure comfort and maintain immobilisation.
( a ) Bandages must be applied sufficiently firmly to prevent harmful movement s, but not so tightly as to prevent the circulation of the blood. In the case of a fractured limb further swelling may occur, causing the bandages to become to o tight. Should thi s occur, the bandages mu st at once be loos ened sufficiently to allow the normal circulation to return.
( b) \'{lhen the pati ent i s in the recumbent position, double th e bandage over the end of a splint to pa ss it under the tr unk or lower limos , u sing the natural hollows of the body (t he neck, loins, knee s and region just above the heels ) . Avoid jarring the patient while working the bandages into t h eir correct position.
(c) In those rare cases where splints are required they mu s t be firm, long and wide enocgh to keep the joints immediately above and below the fractured bone at rest. They should, if practicable, be well-padded to fit accurately to the limb and be applied over the clothing. Ample width is very desirable in a splint, but a splint may be improvised from a walking stick, umbrella, billiard-cue, broom or brush handle, policeman's truncheon , rifle, folded coat, piece of wood, cardboard, paper firmly folded, a rolled-up map, or in fact, anything that is firm, long and wide enough to keep the joints immediately above and below the fractured bone at rest.

u8
SPECIAL TREATMENT IN SPECIAL CASES
FRACTURE OF THE SKULL
A fracture of the skull may injure the brain and nervous system causing concussion and compression (see page 164). There may be two varieties of fracture of the skull:-
(a) Fracture of the Upper Part or Sides
This is generally caused by direct violence, e.g., a blow or fall upon the head. There is generally swelling with linear or circular irregularity of the bone. The fracture may be depressed.
(b) Fracture of the Base
This is generally the result of indirect violence, e.g., a fall on the feet or lower part of the spine or a severe blow to the lower jaw. Blood or fluid may issue from the ear channel, escape from the nose, or it may be swallowed and afterwards vomited. The fracture may involve the orbit causing a bloodshot eye.
TREATMENT
I. Lay the patient on his side in the three-quarters prone position (half-way between side and face down position) and ensure that the throat and lungs are free from obstruction.
2. Support the patient in this position with a pad in front of the chest. If no pad is available draw up the patient's upper knee
3 · If there is still any tendency to choke, the patient should be placed in the full prone position with the head LOwer than the feet and turned to one side.
4· Keep a continuous and careful watch on the patient.
5. Make no attempt to rouse the patient.
FRACTURE OF THE LOWER JAW
This is always due to direct violence and in most cases is compound as there is usually a wound inside the mouth. II9
Sometimes there is a wound leading down from the chin. e.g., when the jaw is fractured by a bullet. fracture is usually confined to one side, but on rare occaSIOns both sides may be in vol ved.
SPECIAL SIGNS AND SYMPTOMS
I. Pain which is increased by speaking, by jaw movements and by swallowing.
2. Irregularity of the teeth.
3. Crepitus may be noticed by or by the First-Aider on steadying and SUPPOrtIng the Jaw.
4. Excessive flow of saliva which is frequently blood -stained.
When there has been extensive jaw damage, e.g., as a result of a bullet wound, the tongue is liable to slip backwards and interfere with breathing.
There may also be hremorrhage from a wound involving the tongue.
TREATMENT
L Warn the patien. not to speak.
2. Instruct the patient to lc:an forward Place the palm of your hand against the injured bone and press It gently agamst the upper Jaw.
3 Place the centre of a narrow bandage under the patient's chin; tie a single hitch on tOP of his head (Flg. 81); draw one loop forwlI!d one backwards well down the back of his head until. form a . turf round his head meeting the loop under the chin tn a half-hitch m ront 0 each ear (Fig. Take the free ends and tie . them in a reef knot on the top of his head (Fig. 83). (The above bandage IS generally referred to as the "ba rrel bandage for the jaw". ) .
[f the narrow bandage is too short to be used as a barrel bandage, Its centre
should be placed under the patient ' s chin and the ends tied off with a ree f knot on top of his head . Tie the knot as far forwards as poss ible without danger of its slipping.
4· If the patient shows any indication of being about to vomit, remov e the bandage, turn his head to the sound side and support his jaw with the palm of your hand Re-apply the bandage when t he vomiting ha s ceased

BANDAGE FOR LOWER JAW
On the rare occasions when the jaw is broken on both sides and the tongue has consequently lost its normal support, do not apply any bandages as these might cause further displa cement of the fracture.
TRANSPORT
(a) If the patient is able to travel in a slUmg posztzon, instrUCt him to sit with his head held forwards and downwards to prevent his tongue from slipping backwards into his throat. 121
(b) If the patient is to be transported as a stretcher case (e.g., when the jaw is broken on both sides) and when the treatment of other important injuries will not preclude the following routine, turn the patient face downwards on a blanket, lift
TRANSPORT WHEN BOTH SIDES OF LOWER JAW ARE FRACTURED
him by the "blanket lift" (see page 209) and place him on the stretcher with his head projecting over the canvas end, his forehead supported by bandages running between the stretcher handles and his chest placed in position on a folded blanket to allow his head to hang forward (Fig. 84). The utmost care must be taken to ensure that the patient's face
and upper limbs are not injured. The patient must be loaded into the ambulance feet first. A lower berth should be selected so that blood and vomit may be collected in a bowl.
FRACTURE OF THE SPINE
The vertebral column may be broken either by direct or indirect violence. Examples of direct violence are the fall of a heavy weight across the back, or falling from a height on the back across a bar, causing fracture at th e site of impact. Examples of indirect violence are a broken neck which may result from a fall on the head, and fracture in the lumbar region due to sudden overflexion or jerking of the spine. An occasional grave complication of fracture of the spine is injury to the spinal cord or to the nerves issuing from it. Such injury is caused by pressure from displaced bony fragments resulting in complete or partial loss of power and sensation (paralysis ) in all parts of the body below the site of the injury.
Fracture of the spine should be suspected in all cases in which there is a history of accident or injury to vertebral column with pain and shock, even if there are no indications of paralysis. All cases of fracture of the spine must be regarded as serious emergencies and all doubtful cases must be treated as fractures.
GENERAL TREATMENT OF CASES OF SPINAL INJURY
I. Immediately warn the patient to lie still.
2. If the patient is unconscious, ensure that breathing does not become obstructed by the tongue.
3· A. If medical aid is readily available:-
(i) Without moving him, keep him as warm as possible

12 3 by means of blankets and hot water in mind that the trunk and limb, may be msensltlve and so easily burned. . .
(ii) Keep the patient under careful observatIon pending arrival of medical aid.
B. If m e dical aid is not r e adily available :-
(i ) Place pads between the patient's ankles, knees and .
(ii ) Apply a bandage in the manner of a of eIght round his ankles and feet, the knot bemg tIed under the soles of the feet.
(iii) Apply broad bandages round his knees and thighs over the intervening pads.
(iv) Empty side- and back-pockets.
(v) Make preparations for the removal of patient to shelter.
TRANSPORT
Preparing the Stretcher
I. The entire bed of a "Furley" type of strelc her must be stiffened, preferably with a series. <;>f short transverse boards. (The metal bed portion of a C:1V1l Defence stretcher is sufficiently rigid and does not reqUIre extra support). If no stretcher is available, a narrow shutter, door ?r board of at least the same width and length as the patIent may be used.
. Cover the stretcher with a folded blanket and then "blanket" the stretcher by one of the methods shown on pages 205-207 . . .,
2. Irrespective of the site of m)ury, place ill readiness on the stretcher, in a position to support the neck and small
of the back of the patient, pillows or pads sufficiently large, but not too large, to preserve the normal curves of the spine..
Preparing the Patient
I. In all cases of fracture of the spine, the patient roust be transported ON HIS BACK, i.e., in the supine, or face-upwards position. If found in any other position, he roust slowly and evenly be rolled on to his back, with the greatest possible care, using all available assistance.
at the feet by grasping the patient's ankles from their outer sides (Fig. 85). (Traction at the head and the feet must be continued until the patient has been placed on the stretcher, so as to ensure that the whole length of his back, his head and lower limbs are kept straight) .

2. In moving or lifting the patient, he must not be bent, twisted or over-extended at the site of injury. This is particularly important in cases of fracture-dislocation, especially in the movable parts of the spine, i.e., the cervical and lumbar regions.
Whenever the patient is about to be moved, it is necessary for one bearer to apply gentle traction at the head by placing the palms of his hands on the patient's ears, with the fingers at the back of the neck and the thumb over the angle of the jaw; and for another bearer to apply gentle traction
3. When the patient is not already lying a blanket or rug and one is available, he must be placed on It as follows:Place the blanket or rug on th: ground in .line :vith the patient, and rolled lengthwIse for half Its WIdth.
(b) While the two bearers maintain traction to the head and feet other bearers very carefully turn the patient on to hls side, every precaution being taken against movement at the site of the fracture. Place the rolled portion of the blanket or rug close. to the patient's back (Fig. 86) and gently roll him over the roll until he is lying on his opposite side. Unroll
the rolled portion of the blanket or rug and gently lower the patient on to his back so that he lies in the centre of the open blanket or rug . The bearers at the head and feet conform to the rolling of the patient throughout.
Loading the Stretcher
There are two methods of loading the stretcher, a Standard Method (when there is a blanket under the patient) and an Emergency Method (when there is no blanket under the patient and none is available ) . In cases in which the stretcher is pushed under the patient, it will be necessary for the bearer at the feet to keep his legs wide apart to allow the stretcher to be placed between them. In case s in which the patient is carried to the stretcher, the head of the stretcher should be placed as close to the feet of the patient as convenient before proceeding to lift.
1. Standard Method ( when th er e is a blanket under the patient )
( a ) Roll the two edges of the blanket up against the patient's sides.
(b) Place the patient on the stretcher feet first as follows:-
(i) If 7 bearers are available. While two bearers maintain traction, four others should stand two on each side of the patient facing one another. On the word of command they raise the patient by grasping the rolled edges of the blanket and, acting together , carefully and evenly lift the patient to a sufficient height to enable the remaining bearer to push the stretcher underneath.
(it')
If only 6 bearers ar e available, they should act .as in (i) above, but move with short even until the patient is directly over the stretcher ( FIg. 87).

( iii) If only 5 bearers are avat'lable. While two bearers maintain traction, two other bearers should stand one on each side of the patient facing each other. The two bearers who maintain traction at the head and feet must momentarily relax traction in order to incorporate the rolled edges of the blanket in their
grasp. On the word of command the bearer on each side of the patient grasps the nearest rolled edge of the blanket with the hands wide apart opposite the patient's shoulder and thigh. Acting together they carefully and evenly lift the patient to a sufficient height to enable the remaining bearer to push the stretcher underneath.

STANDARD METHOD FOR LOADING CASE OF SPINAL INJURY ( FOR FOUR BEARERS)
(iv) If only 4 bearers are available, they should act as in (iii) above, but move with short even paces until the patient is over the stretcher (Fig. 88).
2. Emergency Method (when there is no blanket under the patient and none is available)
(a) Open out the patient's coat and roll it firmly so that t he roll is close to his side.
(
b) Place the patient on the stretcher feet first adopting the same procedure as described for the Standard Method when 7, 6, 5 or 4 bearer s are available, except that the bearers grasp the rolled-up coat and / or the clothing and / or t he bandage round the patient's thighs instead of the rolled edges of the blanket. When the clothing is insecure, a broad bandage must be placed round the body just below the shoulder for the bearers to grasp.
Subsequent Action
I. In the case of cervical lll)uries, place firm supports such as sandbags on each side of the head to steady it.
2. Place a -fo lded blanket beneath the calves so as to re lieve pressure on the heels.
3. Wrap the patient as in Fig . 132 or Fig . 13;3· .. .
4. If he is to be carried over rough ground, his body movements by binding him firmly, but not too to the stretcher with broad bandages round the pelvls, t highs and calves.
5. On reaching shelter, do nothing further until the arrjval of medical aid .
FRACTURE OF THE RIBS
The ribs usually fractured are the sixth, seventh, eighth and ninth, the fracture generally occurring midway between the breast-bone and spine.
Ribs may be fractured by :-
A. Direct force.
This drives the broken ends of the bone inwards, so that frequently a complicated fracture results. The organs most commonly involved are the lungs, and less frequently the liver or spleen.
Every case of complicated fracture involving the lungs must be regarded as compound, since the broken ends of the bones are in contact with the air through the lungs.
B. Indirect force.
This is produced by pressure to the front and back of the chest, as in crushing, the broken ends of the bones being driven outwards. -Usually more than one rib is involved.
SPECIAL SIG S AND SYMPTOMS
1. There is a sharp cutting pain at the site of fracture, which is increased by deep breathing or coughing.
2. The patient takes short, shallow breaths in an attempt to decrease the pain.
Crepitus may occasionally be discovered when a hand is placed over the broken ribs, but the patient must on no account be instructed to take deeper breaths.
3. If the lungs, liver or spleen are affected there will be signs and symptoms of hremorrhage from an internal organ.
An open wound in the chest wall over the fracture may allow direct access of air to the lungs, the air being sucked in and blown out as the patient breathes. This is a grave complication.
13 1
TREATMENT
A. When the fracture is unromplicated
I. Apply two broad bandages round the chest, firmly enough to afford support, with the centre of the first immediately above, and that of the second immediately below, the site of The lower bandage must overlap the upper to ha.lf Its extent. The bandages may be applied over the clothing, after removal of the coat or jacket.

2. Instruct the patient to breathe out. Tie the knots firmly, rather to front of the opposite side of the body.
3. Support the limb of the injured side in an arm slino(Fig. 89).
B. When the fracture is complicated
0
1. Lay the patient down, with his body inclined towards
2
the injured side and supported in this poslUon, e.g., by means of a folded blanket applied lengthwise to his back. (Bandages are not applied ) .
2. If .air is being sucked into the lungs through an open wound m the chest wall, cover the wound with a dressing and pild, and bandage lightly.
3· Place the limb of the injured side in an arm sling.
TRANSPORT
Transport the patient as a stretcher case.
FRACTURE OF TH E BREAST-BONE
This is relatively uncommon, but is attended by great danger masmuch as the underlying chest organs and blood-vessels may be involved.
TREATMENT
I. Undo tight clothing about the neck, chest and waist.
2. Place the patient on his back in the most comfortable position.
3· Keep the patient warmly covered.
TRANSPORT
Transport the patient as a stretcher case.
FRACTURE OF THE COLLAR-BONE
This fracture is often caused by indirect force such as a fall on the point of the shoulder or on the pahn of the hand when the arm is outstretched to the side.
SPECIAL SIGNS AND SYMPTOMS
The arm on the injured side is partly helpless and the patient usually supports it at the elbow with the hand of
the uninjured side and inclines his head towards the injured side.
On examination the broken ends of the bones may be felt to overlap, the outer fra gment being the lower.
T R EATM ENT
I. Remove the coat and wai stcoat and undo the brace (if worn) on the injured o r side s .

TREATMENT OF FRACTURE OF ONE OR BOTH COLLAR-BONES ( FIRST STAGE)
2. Support the arm of the injured side or sides with the help of an as sistant. ( If only one collar-bone is broken tho patient himself may be able to assist).
3: Around. each shoulder pass a narrow bandage with thelI m front and tie each off at the back so as to form two rmgs.

TREATMENT OF FRACTURE OF ONE COLLAR-BONE (FINAL STAGE)
. 4· Pass a third narrow bandage through the two rings and tle o.ff over a fiat pad adjusted between the shoulders, thus bracmg the shoulders backwards (Fig. 90).
. 5· (a) If only one collar-bone is broken, support the upper limb of the affected side in a St. John Sling (Fig. 9 1 ).
(b) If both collar-bones are broken, cross the patient's forearms across his chest. Apply a broad bandage around the body enclosing both forearms and tie off in front just below the wrists (Fig. 92).
TREATMENT OF FRACTURE OF BOTH COLLAR-BONES ( FINAL STAGE!
TRA TSPORT
(a) When only one collar-bone is broke:z,. and there is severe shock, transport the patient as a slttmg case or assIst him as a walking case .
(b) If both collar-bones ar e broken, transport the patient as a stretcher case .
3. Apply adequate padding between the limb of the injured side and the trunk.
4. Fix the hand in position with a collar and cuff sling, taking care that there is no constriction at the wrist.
s. Secure the limb firmly to the chest by two broad bandages :-
(a ) the first with its upper border level with the top of the shoulder ;
(b) the second with its lower border level with the tip of the elbow.

F IG. 93
TREATMENT OF FRACTU RE OF UPP ER LIMB OR SHOULDER - BLADE ( FIRST STAGE )
FRACTURE OF EfE SHOULDER-BLADE
This fracture is relatively uncommon and is usually due to direct force, e.g., a severe blow or crush.
TR E ATMENT
1. Carefully remove the patient's coat if possible and unfasten the brace, if worn, on the injured side.
2. Bend the patient's elbow and lay the limb of the injured side against his chest with the fingers just touching the opposite shoulder.
. 94
TREATMENT OF FRACTURE OF UPPER LIMB OR SHOULDER-BLADE ( FINAL STAGE)
Tie off both bandages at the opposite side of the body (Fig. 93).
6. Replace the coat and button it if possible (Fig. 94).
FRACTURE OF TIm UPPER LIMB
A. Fracture of the Arm
This may occur (a) close to the shoulder, (b) near the middle of the shaft, (c) close to or involving the elbow joint.
B. Fracture of the Forearm
Shortening is unlikely to be observed unless both bones are broken.
Fracture of the lower end of the radius (Colles's fracture) is extremely common, and frequently results from a faU on the outstretched hand or from "backfire" when turning the starting handle of a motor car. It is frequently mistaken for a sprain of the wrist.
In severe cases of fracture of the lower end of the forearm the deformity is marked.
C. Fracture of the Hand and Fingers .
This fracture is frequently accompanied by severe bleeding from the palm of the hand.
TREATMENT OF ALL FRACTURES OF THE UPPER LIMB
(a) When the elbow can be bent without difficulty or increasing pain
1. Carefully remove the patient's coat if possible.
2. Bend the patient's elbow and lay the injured limb against his chest, with the fingers just touching the opposite shoulder.
3· Apply adequate padding between the limb and the trunk.
4· Except in the case of a Colles's fracture, for the treatment of which see Fig. 95, fix the hand in position with a collar and cuff sling, taking care that there is no constriction at the wrist.
5. Secure the limb firmly to the chest by two broad bandages:-
(i) the first with its upper border level with the top of the shoulder;
(ii) the second with its lower border level with the tip of the elbow.
Tie off both bandages at the opposite side of the body (Fig. 93).

TREATMENT Of COLLES'S FRACTURE
6. Replace the coat and button it if possible (Fig. 94)·
(b) When the elbow cannot be bent without difficulty or increasing pain
I. Place the limb by the side, palm to thigh, whh adequate intervening paddinjr.
2. Secure the limb to the trunk and lower limb by three broad bandages tied:one round the arm and trunk, one round the elbow and trunk and one round the wrist and thighs. Transport the patient in the recumbent po sition.
(c) When both upp er limbs are fractured
Adopt Rules ( b) I and 2, and transport the patient in the recumbent position.
FRACTURE OF THE PELVIS
This is nearly always the result of direct violence, e .g., a heavy fall of debris. It is very occasionally caused by indirect violence, e.g., falling from a height and landing

TREATMENT OF FRACTURE OF PELVIS
heavily on both feet when the lower limbs are held stiffly. When the pelvis is fractured, the pelvic organs, especially the bladder and urinary passages, may possibly be injured.
141
SPECIAL SIGNS AND SYMPTOMS
I. Severe pain in the region of the hips and loins, increased by moving or coughing.
2. Inability to stand, despite the absence of any injury to the lower limbs.
3. Pos sibly a desire to pass water frequently though with diffi c ulty.
TR E ATMEN T
1. Lay the patient in whatever position is found to give the greate s t ease. This should be preferably on his back with the kn ees straig ht . If he desires to bend his knees slightly, they should be supported on a folded blanket.
2. Warn the patient not to pass water if he can avoid it.
3. Gently apply two broad bandages round the pelvis, overlapping by half, and with their centres in line with the hip joint of the affected side. Tie off on the opposite side of the body, so as to avoid any painful parts. When the site of the fracture is doubtful tie off in the must comfortable position. The bandages must be sufficiently firm to support the part, but not so tight as to press the broken ends of the bones further inwards.
4. Apply padding between the ankles and knees.
5. Apply a bandage as a figure of eight round the ankles and feet, and a broad bandage round both knees (Fig. 96).
TRANSPORT
Transport the patient as a stretcher case ill the faceupwards position.
FIG. 97
FRACTURE OF NECK OF FEMUR

FIG. 98
FRACTURE OF SHAFT OF FEMUR
99 POTT'S FRACTURE
FRACTURE OF THE LOWER LIMB
A. Fracture of the Thigh Bone
The thigh bone may be broken anywhere along its length. Fracture of the neck of the bone (Fig. 97) occurs in elderly people, frequently from a relatively slight cause, and is often mistaken for a badly bruised hip.
Shortening is often noticeable, varying from half an inch to three inches; and apart from the general indications of fracture, a prominent sign is the position of the foot which lies on its outer side.
This fracture must always be regarded as a serious injury because of the great shock which accompanies it and the possibility of hcemorrhage into the surrounding tissues.
B. Fracture of the Leg
One or both bones may be broken. When both are involved, all the general indications of fracture are usually present, put when only bone is broken deformity is not always noticeable. A fracture of the leg two or three inches above the ankle (Pott's fracture ) (Fig. 99) is frequently mistaken for a sprain or even dislocation of the ankle.
TREA TME T OF FRACTURE OF THE THIGH OR LEG
(a ) When the fractur e is confined to one limb
1. Steady the limb by holding the ankle and foot.
2. Cautiously, but not so as to increase pain, draw the foot as nearly as possible into line with the sound limb.
3. Place adequate padding between the ankles and feet and apply a bandage as a figure of eight round them.
4. Place adequate padding between the thighs and legs.
5. Bandage the knees together with a broad bandage, tied off on the outer s ide of the uninjured limb.

. 100
1'REATMENT OF FRACTURE OF ONE THIGH (LEFT)
.bIG. 101
TREATMENT OF FRACTURE OF ONE LEG (LEFT)
6. Apply two bandages (narrow or broad according to the size of the patient) one above and one below the fracture, tied off on the outer side of the uninjured limb (Figs. 100 and IOI).
FIG. 102
TREATMENT OF FRACTURE
().F BOTH LOWER LIMBS ( FIRST STAGE)
145
In the case of a fracture near the. hip- or ankle-joints, the application of the bandage nearest the joint may have to be modified.
In certain cases, as mil7ht oCC:.ll" b m mmes or when the patient has to be carrieci :Ong distances over rough or uneven ground, it may be ne cessary to u se a splint for additional immobilisation. Trearment in such cases must be carried out as follows ;-
(i) Adopt Rules I to 4 above.
(ii) Apply a splint of adequate length on the outer side of the injured limb.
(iii ) Apply the bandages mentioned in Rules 5 and 6 in the same order round the splint, and tie them off over the splint.
(iv) Tie a figure of eight bandage around the feet at ankles .
(b) When both thighs are fractured.
I. Place a well-padded splint between the limbs extending from the crutch to the foot (Fig. 102).
2. Gently draw down the feet and bring them as nearly as possible into line without using force or causing pain.
3. Apply a bandage as a figure of eight round the ankles and feet (Bandage A).
4. Pass seven bandages under the patient in the following order:
The chest, just below the armpits (B) .
The pelvis, in line with the hip -joints (C).
Both ankles and feet (D). (This covers bandage A).
Both thighs, above the fracture (E) .
Both thighs, below the fracture (F).
Both legs (G).
Both knees (H) (a broad bandage).
D

I03
TREATMENT OF FRACTURE OF BOTH THIGHS (FINAL STAGEFirst View)
5. Place a splint along each side of the patient from the armpit to just beyond the foot.
6. Secure the splints by tying the bandages in the same order. The bandages must be tied over the splint on the side showing least injuries, except D, which must be applied 147
as a figure of eight and tied under the soles of the feet (Figs. 103 and 104) .
(c) When both legs are fractured and assistance lS available
1. Place a well-padded splint between the limbs extending from the crutch to the foot (Fig . 102).
2. Steady the limbs by holding the ankles and feet.
3. Gently draw down the feet and bring them as nearly as possible into line, without using force or causing pain, and do not let go until the splints have been fixed.
4. Apply splints on the outer side of each leg, reaching from above the knee to beyond the foot.
5. Secure the splints by bandages: (A ) above, ( B) below the fractures, (C) immediately above the knees,
I04
TREATJ\'lENT OF FRACTURE OF BOTH THIGHS ( FINAL STAGESecond View)
105
TREATMENT OF FRACTURE OF BOTH LEGS WHEN ASSISTANCE IS AVAILABLE ( FINAL STAGE-First View)

(D) round the ankles and feet as a figure of eight, (E) a broad bandage round both knees.
The bandages (except D) must be tied over the splint on the side showing least injury (Figs. 105 and 106).
FIG. 106
TREATMENT OF FRACTURE OF BOTH LEGS WHEN ASSISTANCE IS AVAILABLE (FINAL STAGE-Second View)
(d) When both legs are fractured and no assistance is available
I. Place a well-padded splint between the limbs extending from the crutch to the foot (Fig. 102).
2. Steady the limbs by holding the ankles and feet.
3. Gently draw down the feet and bring them as nearly as possible into line, without using force or causing pain.
4. Tie the ankles and feet together.
5. Apply bandages above and below the fracture, immediately above the knees and a broad bandage round both knees.
C. Fracture of the Knee-cap
The knee-cap may be broken by direct violence, but more frequently it is broken by muscular action causillg it to snap in two (Fig. 107).
FIG. 107
FRACTURE OF KNEE-CAP
SPECIAL SIGNS AND SYMPTOMS
The limb is quite helpless. There may be marked swelling of the joint, some irregularity, and a gap may be felt between the broken fragments of the bone.
TREATMENT
1. Lay the patient on his back, raise well and support his head and shoulders, straighten and raise the injured limb.
2. Apply a splint along the back of the limb reaching from the buttock to beyond the heel. The splint must be well-padded under the natural hollow of the ankle so as to raise the heel from the splint.
3. Secure the splint by bandages round the thigh (A) and leg (B).
4. Apply a narrow bandage with its centre immediately above the knee-cap, cross the ends behind over the splint, pass them again to the front of the limb just below the knee-cap and tie them (C).
D. Fracture of the bones of the Foot or Toes-Crushed Foot
This injury is co.m.monly caused by the passage of a heavy weight over the foot, and should be suspected when there is pain, swelling and loss of power.
TREATMENT
(a) When no wound is present or suspected (Fig. 1 0 9)
I. Do not remove the shoe or boot.
2. Apply a cold co.mpress.

TREATMENT OF FRACTURE OF KNEE-CAP
5. Raise the uninjured limb and bring it into line with the injured limb. Place adequate padding between the ankles and feet and fasten them together with a figure of eight bandage (D) tied under the soles of the feet. This will embrace the splint on the injured side.
6. Support the feet well off the ground by pillows or rugs (Fig. 108).
7. Apply a cold compress over the fracture.
109
TREATMENT OF CRUSHED FOOT WHEN NO WOUND IS PRESENT OR SUSPECTED
3. Apply the centre of a bandage (narrow or broad, according to the size of the foot) under the centre of the sole of the foot, cross the ends in front of the ankle, carry once round the ankle and tie off in front.
(b) When a wound is present or suspected (Fig. IIO)
I. Remove the shoe or boot and stocking.
2. Treat the wound.
3· Apply adequate padding all round the foot.

£'11J. 110
TREATMENT OF CRUSHED FOOT WHEN A WOUND IS PRESENT OR SUSPECTED
4· Apply the centre of a bandage (narrow or broad, according to the size of the foot) under the centre of [he sole of the foot, cross the ends in front of the ankle, carry once round the ankle and tie off in front.
153 CHAPTER X
INJURIES TO JOINTS AND MUSCLES DISLOCATIONS
A dislocation is the displacement of one or more bones at a joint. . The joints most frequently dlslocated are those of the shoulder, elbow, thumb, fingers a.nd lower jaw, the last nam.ed resulting sometimes from yawrung or a blow on the chin.
DISLOCATION OF SHOULDER
FIG. 112
DISLOCATION OF ELBOW

II3-(Back View)
1I4-( Side View)
DISLOCATION OF FINGER
SIGNS AND SYMPTOMS
I. Pain of a severe sickening character at or near the joint.
2. Loss of power in the limb.
3. Fixity of the joint.-The limb cannot be moved at the joint either by the patient or by the First-Aider.
4. Deformity of the limb.-The limb assumes an unnatural position and appears misshapen at the joint.
5. Swelling about the joint.
In many cases it will prove difficult or even impossible to distinguish between a dislocation and a fracture by the means ordinarily at the disposal of the First-Aider, and both may occur simultaneously. The following table will help to distinguish between the two in a straightforward case:-
Dislocation
Always occurs at a joint.
There is fixity of the joint.
Crepitus is absent.
If the end of the bone can be felt, it is smooth and rounded.
Fracture
May occur anywhere in the bone.
Unnatural movement may be accidentally discovered. Crepitus may be accidentally discovered . If the broken end of the bone can be felt, it is sharp and angular.
TREATMENT
1. Make no attempt to reduce a dislocation.
2. (a) In the case oj a limb
When the accident occurs out-oj-doors, steady and support the limb jn the position which gives most
ease to the patient, using padding where necessary in order to lessen the effects of jolting during transport.
When the patient is indoors:-
(i) Place the patient on a couch or bed in the position which gives most ease.
(ii) When the injury is painful expose the joint and, if treated early, apply a cold compress. When an interval occurs between the injury and treatment, apply a hot compress so as to relieve congestion and / or pain.
(b) In the case of the lower jaw
(i) Remove the patient's dentures if he wears them.
(ii ) Afford support to the lower jaw.
DISPLACED CARTILAGES OF THE KNEE
In sudden wrenches of the knee such as occur in football and other games or slipping on a step, the semi-lunar cartilages may be displaced or torn.
The signs (with the exception of deformity) and symptoms are the same as those of a dislocation.
TREATMENT
Apply the rules for treatment of dislocation of a limb.
SPRAINS
When, by a sudden wrench or twist, the ligaments and parts around a joint are stretched or torn, the joint is said to be sprained.

SIGNS AND SYMPTOMS
I. Pain at the joint.
2. Inability to u se the joint without increasing the pain.
3. Swelling and , later, discoloration.
TREATMENT
I. Pla ce the limb in the most comfortable position, preferably elevated, and prevent movement.
2. Expose the joint and apply a firm bandage.
3. Wet the bandage with cold water and keep it wet.
4. When this ceases to give relief, take the bandage off and re-apply it.
In all doubtful cases treat as a fracture.
If the ankle is sprained and circumstances compel the patient to walk, apply the rules for treatment of sprains and replace the boot or shoe befo r e rhe increa sin Q: s \ve llin g makes this impossible.
STRAINS AND RUPTURED MUSCLES
When, during severe exertion, muscles or tendons are over-stretched, they are said to be strained, or if they are actually torn, they are described as ruptured.
The so-called strain in the groin (sometimes referred to as a rupture or hernia) is an injury of a totally different nature (see page 182).
SIGNS AND SYMPTOMS
I. There is a sudden sharp pain at the seat of injury.
2. In the case of a limb, the muscles may swell and cause severe cramp. If the back is affected the patient may be unable to stand upright.
3. Further exertion is difficult or impossible.
TREATMENT
1. Place the patient in the most comfortable position, and afford support to the injured part.
2. When the injury is treated immediately, apply a cold compress to the injured part. When an interval occurs between the injury and the treatment, apply a hot compress.

CHAPTER XI
INSENSIBILITY
THE NERVOUS SYSTEM
Two systems of nerves, the cerebro-spinal and the autonomic, regulate and control the movements and functions of the body.
THE CEREBRO-SPINAL SYSTEM
The cerebro-spinal system is made up of the brain, spinal cord and nerves; through its agency sensations are received and the will causes the action of the voluntary muscles. For example, when a part is injured a sensation of pain is conveyed to the brain by the sensory fibres of the nerve, thus affording an indication of the seat of injury or a warning of a possible danger of further damage. On attention being directed to the injury, motor fibres of the nerve convey a message to the muscles, and an attempt is instantly made to ease the pain by moving the injured part.
The Brain, situated within the cranium, is the seat of intellect, the emotions and the will; it is the organ where impressions brought by sensory nerves are received and from which orders are given through the motor nerves.
The Spinal Cord, coming from the brain, consists of nerve tissue and lies within the spinal canal. It leaves the brain through an opening in the base of the skull, and extends to the second lumbar vertebra.
The Nerves proceed from the brain and spinal cord it: pairs as pearly-white trunks, and their branches can be traced throughout the of the body. When a nerve is

115
SECTION THROUGH BRAIN AND SPINAL CORD
severed there is loss of power and sensation in the region in which its branches are distributed.
161
THE AUTONOMIC SYSTEM
The autonomic system consists of a network of bodies of nerve tissue (ganglia) and connecting nerves; it controls the involuntary muscles, and regulates the vital functions of the body. The main part of the network (solar plexus) is situated in the upper part of the abdomen behind the stomach; when it is struck, as in "winding" in football and boxing, severe collapse may The autonomic system is not under the control of the will, and acts alike during sleep and activity.
INSENSIBILITY
Insensibility is loss of consciousness due to interruption of the action of the brain brought about by some interference with the functions of the nervous system. It is an important indication not only of of or injury to the brain, but of many other serious injuries or diseases of the body.
There are two degrees of insensibility apart from sleep;-
Partial (stupor).
Complete (coma).
The degree of insensibility may be determined by the following tests;-
(i) In stupor the patient can be roused with difficulty yarying with the degree of stupor present. In coma there IS no response.
(ii) In stupor the patient objects to the eyeballs being touched, as evidenced by contraction of the eyelids. In

coma he does not object. (The corner of a clean handkerchief should be used for this test.)
(iii) If a bright light is flashed into the eyes, or if the eyes are shaded and the shade suddenly removed, the pupils become smaller in stupor, but remain fixed in coma. This reaction also varies with the degree of stupor present.
The pupil of the eye is the dark circle surrounded by a coloured muscular ring (iris). Stimulation by a bright light causes the muscles of the iris to contract and the size of the pupil is diminished. In the dark the pupil becomes dilated.
GENERAL RULES FOR TREATMENT OF INSENSIBILITY
I. Ensure that air can enter freely into the lungs.
2. If breathing has stopped, turn the patient into the prone position and commence artificial respiration.
3. If breathing is noisy (bubbling through secretions), turn the patient into the three-quarters prone position.
Support the patient in this position with a pad in front of the chest. If no pad is available draw up the patient's upper knee.
If the patient is on a stretcher, raise the foot of the stretcher about 12 inches to drain secretions from the lungs.
4. If breathing is not obstructed and the injuries of the patient make the prone position unsuitable, lay the patient in the most convenient position and be prepared, if necessary, to modify the position should breathing become difficult.
5. Undo all tight clothing about the neck, chest and waist.
6. Keep a continuous and careful watch on the patient. Do not leave him until he has been placed in the charge of another responsible person.
7· Ensure an abundance of fresh air by opening windows ana. doors; keep back a crowd; remove from harmful gases or impure atmosphere.
8. Adopt the special treatment for the condition which has caused the insensibility.
9: .Remove the patient ,to shelter in the appropriate recumbent posltlon as soon as expedient.
10. Give no food or fluids whatever by the mouth while the patient is insensible.
,II. returns to consciousness water may be glven to drmk m SlpS., If the pulse is feeble give hot strong tea or coffee sweetened wlth sugar, unless hremorrhage is apparent or hremorrhage from an internal organ is suspected.
CAUSES OF INSENSIBILITY
A. Commoner Causes of Insensibility
(i) Shock (s ee Chapter IV)
(ii) Asphyxia (see Chapter V)
(iii ) Hremorrhage (see Chapter VIII)
(iv) Poisoning (see Chapter XII )
(v) Direct injury to the brain causing concussion or compression
(vi) Apoplexy
(vii) Epilepsy
(viii) Hysteria
Infantile convulsions
(x ) Effects of excessive heat.

B. Less Common Causes of Insensibility
(i) Diabetes
(ii) Insulin overdose
(iii) U rremia
(iv) Starvation
(v) Brain turnour or abscess
(vi) Meningitis
(vii) Infantile paralysis.
In some cases of insensibility convulsions are present. These are spasmodic and involuntary contractions of the muscles of the body and limbs. They may be general affecting the whole body or they may be limited to the limbs or one side of the body.
A. The Commoner Causes of Insmsibility not dealt with in other Chapters
DIRECT INJURY TO THE BRAIN
This may bring about concussion and /or compression.
(a) Concussion is a condition of widespread disturbance of the functions of the brain which comes on as the result of injury. It is not necessarily associated with any changes in the brain substance. "Brain shaking" is a good description of what occurs. A blow on the head, a fall from a height on to the feet, falling forcibly on the lower part of the spine or a blow on the point of the jaw may all cause concussion.
SIGNS AND SYMPTOMS
The patient may be insensible immediately or the insensibility may develop at a later stage. The face is pale, the skin is cold and clalTIlTIY, the breathing is shallow, the pulse is quick and weak indicating lowered blood pressure.
(b) Compression is a condition due to actual pressure on some portion of the brain within the skull by blood clot or piece of bone in fracture of skull. I t may supervene on concussion or may come on after a lucid interval or recovery from concussion.
SIGNS AND SYMPTOMS
The patient may be insensible immediately or the in.sensibility may develop at a later stage. The face may be flushed and the body temperature may be raised. The breathing is stertorous (i.e. snoring in character). The pulse is strong and slow indicating raised blood pressure. The pupils of the eyes are dilated and fixed or may sometimes be unequal. Dependent on the site of the pressure, there may be paralysis of one side of the body.
SPECIAL TREATMENT OF CONCUSSION AND COMPRESSION
I. Apply the rules for fracture of skull (page 118) and the general rules for insensibility ( page 162). In particular ensure that air is entering freely into t he lungs.
Z. Apply warmth (blankets, hot water bottles) to the abdomen and lower limbs.
3. On no account attempt to rouse the patient.
NOTE
After minor concussion the patient may act automatically and may appear to be "drunk" and unreasonable. This may lead to difficulties if not appreciate d . After recovery thex-e is often a gap in his memory for this period, and also for a few seconds before the injury, so that he cannot remember how it happened.
No case of head injury should be regarded lightly and all unnecessary movement should be avoided. A caution should be given to a patient who has been

unconscious even for only a moment not to resume physical or mental activity without the consent of a Doctor.
APOPLEXY
. This usually occurs in or elderly people with high blood pressure and IS due to the rupture of a diseased causing hremorrhage into the brain tissue. I t IS commonly called "stroke." Signs of injury to the head are not necessarily present.
SIGNS AND SYMPTOMS
The signs and symptoms are identical with those of compression and, in fact, the condition is a form of compression. The age of the patient and the absence o f history or signs of injury help with the diagnosis.
TREATMENT
The treatment is the same as that of compression.
EPILEPSY
. This is a condition which may occur at any age but usually m persons. There are two types of enileo sy, minor and major.
(a) Minor Epilepsy
The patient may become pale with eyes fixed and staring and may. unconscious. He may then resume his pre:,lOUs aCtiVIty as though nothing had occurred.
All that a FIrst-Aider can do is to keep a watch for the presence of post-epileptic automatism which is described on page 167_
(b ) Major Epilepsy consists of the true epileptic fit.
SIGNS AND SYMPTOMS
The patient may have a premonition that he is going to have a fit . He may experience a sense of strangeness accompanied by headache, irritability, re stlessness o.r a feeling of lethargy-the "dreamy state". These sensatlons are known as the "aura."
The epileptic fit consi sts of four stages :-
(i) The patient sudd enly loses consciousness and falls to the ground, possibly with a cry. . '
(ii ) He remains rigid for a few seconds and durmg this stage the face becomes flushed. .
(iii ) The convulsions start. During this stage the patient may injure himself by striking a hard object. His face becomes livid and he froths at the mouth. He may bite his tongue . He will not have control of his bladder nor rectum and may pass urine and freces involuntarily (incontinence ) .
(iv ) The convulsions cea se and the patient may be dazed and confused or sometimes act in a strange manner without realising what he is doing (post-epileptic automatism) . This condition varies in duration.
T REATM EN T
1. Apply the general rules for the treatment of insensias fa r as applicable.
2. Do not forcibly restrain the patient because the forcible restraint of an epileptic has been known to result in dislocations or even fractures. When possible remove any objects on which the patient might injure himself.
3. As opportunity arises, place the handle of a spoon or other hard object wrapped in a handkerchief between his teeth to prevent the patient from biting his tongue.
4. Wipe away the froth from his mouth.
s. Keep a careful watch for a possible recurrence, and do not leave him until you are satisfied with his menta l condition or until he is placed in the care of another responsible person.
HYSTERIA
This occurs in nervous people, more frequently in females , although males are sometimes subject to it.
SIGNS AND SYMPTOMS
It is sometimes characterised by "convulsions." Th e hysterical "convulsion" is a dramatic performance demanding an audience and does not occur, therefore, when the patient is alone. Hysteria may be brought about by a shock or mental stress. The onset of the attack is more gradual than in epilepsy. The patient in falling to the ground takes care not to injure himself. Alternate laughing and crying or the utterance of words or phrases take the place of the epilepti cry. The movements which comprise the "convulsion" consist of voluntary movements such as tearing of the hair or clothes, clutching at bystanders or rolling on the ground . There is never complete loss of consciousness. The tongue is not bitten nor is there incontinence of urine or freces.

TREATMENT
Avoid sympathy with the patient. Speak firmly to him. Leave him alone in a room if possible as segregation is often a successful form of treatment.
INFANTILE CONVULSIONS
These occur in infants as a result of teething, some stomach or chest trouble or when sickening for an illness such as an infectious disease.
SIGNS AND SYMPTOMS
There is general twitching or tremor of the muscles; extreme pallor and later blueness of the face; occasional squinting or upturned eyes; holding of the breath; and fr oth may appear at the mouth.
TREATMENT
Wrap the child in a warm blanket and follow the general ru les for the treatment of insensibility where applicable.
EFFECTS OF EXCESSIVE HEAT
(a) Heatstroke and Sunstroke. The cause of heatstroke
1S exposure to excessive heat either in hot buildings or from urnaces or boilers (e.g., the stokehold of a steamer in the ro pics). The cause of sunstroke is exposure to bright hot sun light without adequate protection. Moist heat is said .0 be a more frequent causative factor in both conditions.
SIGNS AND SYMPTOMS
The patient is usually unconscious, his face is livid· skin is hot and dry.; his pulse is bounding; his IS stertorous; and his temperature is excessively high; it may be as much as 110 °F.
TREATMENT
I. Apply the general rules for the treatment of insensibility as far as applicable.
2. Place the patient in a cool shady spot with a free circulation of air and strip him to the waist.
3. Fan him vigorously.
4: ice-bags to his head and spjne continuously untll his temperature falls to just above normal C9 8 .4 °F .).
5· Sponge his body with very cold water or rub him over with ice, if available, continuously.
6. When consciousness returns, give Epsom or Glauber salts, a teaspoonful to a tumblerful of water, and drinks of cold water.
7. Remove him to hospital.
(b) Heat Exhaustion. The causes of this condition are similar to those which produce heatstroke, but the symptoms are not so severe.
SIGNS AND SYMPTOMS
The patient may have fainted but unconsciousness is of only short duration. He will complain of weakness, possibly cramp in the legs, dizziness, faintness, headache and nausea. There may be diarrhoea and vomiting. The pulse is rapid and feeble, the skin hot and dry and the temperature is high, but not so high as in cases of heatstroke and sunstroke.
TREATMENT
I. Rest the patient in a shady, cool, well-ventilated room and strip him to the waist.
2. Fan him vigorously.
3. Sponge him with tepid water.
4. Give cold water to drink freely.
B. The Less Common Causes of Insensibility
DIABETIC COMA AND INSULIN OVERDOSE
SIGNS AND SYMPTOMS
Diabetic Coma
Skin is dry
Distressed breathing
Breath smells of acetone (musty apples)
Insulin Overdose
Skin is moist with perspiration
Shallow and quiet breathing
Breath odourless
In insulin overdose the patient's pockets should be sea rched for lumps of sugar which are often carried by diabetics on insulin treatment. Signs of recent injection on the arm or thigh may be present. Sometimes patients ca rry a card indicating their insulin dosage.
In diabetic coma the patient may be suffering from some in fection such as a boil or carbuncle.
TREATMENT
Diabetic Coma
Apply the general rules for the treatment of insensibility as far as applicable

Insulin Overdose
Apply the general rules for the treatment of insensibility as far as applicable
Obtain the services of a Doctor immediately or if this is not possible remove the patient to hospital.
Obtain the services of a Doctor immediately or if this is not possible remove the patient to hospital.
Feed with sweet substances -jam, sweets or dissolved sugar. These should be fed by teaspoon when the swallowing reflex is present. When the swallowing reflex is absent nothing must be given by the mouth. (The patient's ability to swallow must be tested by introducing a teaspoonful of cold water at a time between the gums and the cheek.)
URlEMIA
1 hIs is a condition due to defective action of the kidneys . There may be a history of scanty urine or even at times of increased frequency in passing urine. The patient will be pale and will show a desire to go to sleep or be somewhat drowsy. Convulsions may occur.

173
TREATMENT
Apply the general rules for the treatment of insensibility as far as applicable.
STARVATION
The history is the only real guide in this condition, but the appearance of patient (emaciated) may help.
TREATMENT
Apply the general rules for the treatment of insensibility as far as applicable. On return to consciousness give food sparingly.
BRAIN TUMOR OR ABSCESS, MENINGITIS, INFANTILE PARALYSIS
These are outside the scope of First Aid so far as diagnosis is concerned.
TREATMENT
Apply the general rules for the treatment of insensibility as far as applicable.
CHAPTER XII
POISONS
b p.oison is. any substance which when taken into the y suffikclent. quantity is capable of destroying life (m)a y e ta en eIther accidentally or intentionally ._ .
a Through the lung b b hi . . fu . s, y reat ng pOIsonous gases or .I?es.. This portal of entry is put first because gas POIsobr:mg d causes more deaths than all other poisons com Ine .
(b) By the mouth, i.e., swallowed (c) By injection under the skin. .
hold a ) Gas pOhisoning occurs mainly from breathing house gas or t e fumes of fire tthe smoke generated fr nils, s motor or L.t: . om co agratIOns or explosIOns decel If by asphyxia. Sufferers may appear w'll), ve y we . unless. very. severely poisoned, when they 1 e unconscIOus WIth difficult breathing.
poisons chiefly exert their dangerous
direcJlY fon the/ood passages, causing retching, . ' pam. an .0 ten diarrhcea. Poisons in this class n:etallic pOIsons., poisonous fungi and berries and omposmg fc:od . Partlcularly severe symptoms are caused by corrosIves (strong acids and alkalis) which burn the ltps, mouth, gullet and stomach and cause intense pain.

175
(ii) Or on the nervous system after absorption into the blood, usually causing coma and sometimes asphyxia. The most important of these poisons are alcohol (beer, wine, spirits) taken in excessive amount, and the many drugs, taken as tablets or draughts, to relieve pain (e.g ., aspirin and opium derivatives) or to produce sleep (e.g., the barbiturate drugs). All patients unconscious from poisoning by drugs are seriously ill; this also applies to individuals who are insensible from alcoholic intoxication ("dead drunk"). A few poisons act on the nervous system by causing delirium (e .g., belladonna) or fits (e.g., strychnine, prussic acid).
(c) Injected poisons. These poisons are injected by hypodermic syringe; by bites from poisonous reptiles; by stings from certain insects; or by bites from rabid animals. As a result life is endangered through coma and asphyxia.
GENERAL RULES FOR THE TREATMENT OF POISONING
I. Place an unconscious patient in the prone position with the face turned to one side and not resting on a pillow. The prone position also facilitates the commencement of artificial respiration by Schafer's method.
2. Start artificial respiration instantly if the breathing is feeble or unduly slow. Keep it up till a Doctor takes charge.
3. Send for a Doctor, giving brief particulars, and preserve for his examination any remaining poison and any vomited matter.
4. DO NOT give aperients, e.g., castor oil, unless ordered by a Doctor.

ADDITIONAL TREATMENT FOR SWALLOWED
I. Induce vomiting by tickling the back of the patient's throat with a spoon or two fingers; or if this method fails, by giving an emetic, i.e., a tumbler of water containing two tablespoonfuls of salt, but in the following cases DO NOT INDUCE VOMITING :-
(a) When the patient is unconscious, because attempts to induce vomiting or to pour liquid down the throat of an unconscious person may easily cause drowning through inhalation of vomit or fluid.
(b) When the lips and mouth of any patient (conscious or unconscious) are burned.
2. Except in the case of unconscious patients, administer an antidote (to neutralise the poison) after vomiting has been injuced or, in the case of corrosive poisoning, without the production of vomiting.
ANTIDOTES
The simplest antidote for general use is milk (one pint). If milk is not available, then a pint of water may be given; water acts by diluting the poison although it has no specific neutralising action.
Special antidotes, instead of milk, may be administered in certain cases when the nature of the poison is definitely known and the antidote is hnmediately available :_
For corrosive acids, e.g., sulphuric acid (oil of vitriol), hydrochloric acid (spirits of salts), nitric acid :_
Two tablespoonfuls of magnesia powder in a pint of water. If magnesia is not available, powdered chalk may be substituted or a pint of soapy water used.
For corrosive alkalis, e.g., caustic soda, caustic potash, strong ammorua :-
Two tablespoonfuls of vinegar in a pint of water.
For carbolic acid (phenol) and carbolic-smelling disinfectants :-
Two tablespoonfuls of Epsom salts in a pint of water, or four ounces (8 tablespoonfuls ) of medicinal liquid paraffin.
For oxalic acid and oxalates (salts of lemon, salts of sorrel ) :-
Two tablespoonfuls of powdered magnesia or chalk in a pint of water.
For Iodine :-
A pint of thin starch paste. . .
All quantities mentioned above should be diVIded by. two f or children between two and eight years of age, and dIVIded b y four for infants under two years.

CHAPTER XI II
MISC E LLA NEOU S INJURIES
BURNS AND SCALDS
A Burn is an injury caused by :-
(a) Dry heat, such as fire, a piece of hot metal or the sun.
(b) Contact with any object charged with a high-tension electric current; or by lightning.
(c) Friction, caused for example, by contact with a revolving wheel (brush burn) or fast-moving rope or WIre.
(d) Corrosive chemicals :-
(i) Acids, such as sulphuric acid, nitric acid, hydrochloric acid.
(ii) Alkalis, such as caustic soda, caustic potash, strong ammonia or quicklime.
A Scald is an injury caused by moist heat, such as boiling water, steam, improperly applied poultice, hot oil or tar.
The effects of a burn or scald are the same. There may be reddening of the skin or blister formation or destruction of the skin or destruction of the deeper tissues.
There is great danger from shock (which is increased by the intense pain and aggravated by loss of body fluid), and from septic infection of the wound.
The areas of most burns and scalds, including the clothing involved, are to all intents and purposes sterile for a short period, and every effort should be made to keep them so
until medical aid is available. Prepared sterile dressings should always be used and great care must be taken in their handling and application.
GENERAL RULES FOR TREATMENT OF BURNS AND SCALDS
A. When medical aid is readily available
1. Do not remove clothing and do not break blisters.
2. Cover the area (clothing included) with prepared sterile dressings.
3. Apply a pad of conon wool.
4. Bandage firmly except when blisters are present or suspected, in which case bandage lightly.
5. Wrap the patient in blankets to keep him warm.
6. In severe cases immobilise the affected area by the application of slings, bandages or splints.
7. Give large quantities of warm fluids, preferably weak tea sweetened with sugar.
B. When medical aid is not readily available
1. Do not remove clothing and do not break blisters.
2. Saturate the area, clothing included, with warm alkaline solution (two teaspoonfuls (one dessertspoonful) of baking soda (bicarbonate of soda) to one pint of sterile water at body temperature) or warm saline solution (one teaspoonful of common salt to one point of sterile water at body temperature).
This treatment will relieve pain and thereby minimise shock.

3. Cover the area with prepared sterile dressings soaked in a similar solution and keep them moist with the solution. If the above solutions are not available, cover the area with prepared sterile dressings.
4. Apply a pad of cotton wool.
5. Bandage firmly in position, unless blisters are present or suspected, in which case bandage lightly.
6. Wrap the patient in blankets to keep him warm.
7· In severe cases immobilise the affected area by the appljcation of slings, bandages or splints.
8. Give large quantities of warm fluids, preferably weak tea sweetened with sugar.
When the face is burnt, cut from a piece of lint a dressing in the shape of a mask with a hole for breathing. Moisten the dressing with one of the solutions described in Rule B 2 and keep it moist.
A young child, when severely burnt or scalded, must be placed in a warm bath, preferably of the alkaline solution, or, if not available, saline solution, without removing his clothes, and kept there until medical aid is available. The bath must be kept warm at approximately body temperature, and must be tested frequently. Hot water must be carefully added when necessary to keep the solution at the correct temperature.
When a person's clothing catches fire, approach him holding a rug, blanket, coat or table-cover in front of yourself for protection, wrap it round the patient, lay him flat 80 smother the flames.
If a person's clothing catches fire when alone, he should roll on the floor, smothering the flames with the nearest available wrap and call for assistance; on no account should he rush into the open air.
The use of fire-guards would prevent many calamities.
SPECIAL TREATMENT OF BURNS CAUSED BY CORROSIVE CHEMICALS
A. When the corrosive is an acid
I. Bathe the part freely with an alkaline solution, such as two teaspoonfuls (one dessertspoonful) of baking soda (bicarbonate of soda) or washing (carbonate of in one pint of warm water. If the solutIon cannot be obtamed quickly thoroughly flood the burnt part with water, warm if immediately available.
2. Apply the general rules for the treatment of burns as far as applicable.
B. When the corrosive is an alkali
I. If the burn is caused by quicklime, brush off any that remains on the part.
2. In all cases, bathe the part freely with a weak acid solution, such as vinegar or lemon juice with an equal quantity of warm water. If the solution cannot be obtained quickly, thoroughly flood the burnt part with water, warm if immed i?tely available.
3. Apply the general rules for the treatment of burns as far as applicable.
In all cases of burns caused by corrosive chemicals, if a neutralising or diluting fluid is not available, remove the affected clothing immediately.
When the eyes are injured by a corrosive chemical, treat as described on page 185·
FROST-BITE
During exposure to severe cold, parts of the body (usually the feet, fingers, nose or ears) lose sensation and become first waxy white and afterwards congested and of a purple appearance. As sensation is lost in the part the patient is frequently unaware of his condition.
TREATMENT
Do not bring the patient into a warm atmosphere until, by mild friction and the application of dry moderate warmth, sensation and circulation in the affected parts are restored. Neglect of this precaution may lead to death of the tissues of the frost-bitten part. Avoid the application of moisture in any form.
The patient must not be taken into a warm atmosphere until the circulation in the affected part is restored.
ABDOMINAL HERNIA
Abdominal hernia, frequently referred to as a rupture, consists of a protrusion of some part of the abdominal content, usually the bowel, through the muscular wall of the abdomen under the skin. It occurs most frequently at the groin, but is not uncommon at the navel or through

an abdominal scar. It may appear in babies or persons of any age. The condition may be sudden in onset or may come on gradually; if the onset is sudden there is swelling and pain, followed sometimes by vomiting.
TREATMENT
1. Lay the patient down, raise and support his head and shoulders, bend his knees and place a pillow under them.
2 . Apply ice or a cold compress to the affected part.
3. Make no attempt to reduce the swelling, but seek medical aid as soon as possible.
STINGS OF PLANTS AND INSECTS
These may give rise to serious inconvenience and in some cases grave symptoms develop .
TREATMENT
1. Extract the sting if present ( e.g., bee stings ) with the point of a needle which has been sterilised by passing i t slowly through a flame.
2 . Apply freely spirit, sal volatile, weak ammonia, a solution of baking soda (bicarbonate of soda ), washing soda (carbonate of soda ) or a wet "blue bag."
3. Cover with a dry dressing.
If the sting is inside the mouth, a mouth wash of a solution of baking soda (bicarbonate of soda ), two teaspoonfuls (one dessertspoonful) to a pint of water, should be used. Apply a hot compress to the front of the neck.
FOREIGN BODY EMBEDDED UNDER THE SKIN
If a needle or other foreign body, such as a splinter of glass or fish-hook, becomes embedded under the skin, do not attempt to remove it; but treat the wound, inunobilise the part (using splints if necessary) and obtain medical aid.
FOREIGN BODY IN THE EYE
Particles of grit, coal dust, sand, metal splinters or loose eyelashes may lodge on the eyeball or under the eyelids and cause much discomfort and possibly inflammation if they are not speedily removed. Occasionally the foreign body may become embedded in or adherent to the eyeball and cause serious trouble.
TREATMENT
A. When the foreign body is not embedded in or adherent to the eyeball
I. Prevent the patient from rubbing his eye. In the case of a child it may be necessary to tie his upper limbs to his body.
2. Seat the patient facing the light and stand in front of him. Pull down his lower eyelid and, if the foreign body can be seen, remove it with a corner of a clean handkerchief, preferably white, twirled up and wetted with clean water.
3· If the foreign body has not been found and it is suspected to be under the upper eyelid, instruct the patient to blink his eyelid under water. Alternatively, lift the upper lid

forward, push the lower lid beneath and let go .both the eyelids. The lashes of the lower lId brush the mner surface of the upper one and may dislodge the foreign body. Should the first attempt be unsuccessful, repeat several times. If the foreign body is not dislodged, take the patient to a Doctor as soon as possible, but when medical aid is not available:-
( a ) Seat the patient facing the light and stand behind him, steadying his head against your chest.
(b ) Place a matchstick on the of his upper press it o-ently backwards and mstruct the patient to look do;nwards. Take hold of his upper eyelashes and pull the lid over the matchstick, thereby everting the eyelid.
(c) Remove the foreign body with a corner of a clean handkerchief as described in Rule 2.
B. When the foreign body is embedde d in or adherent to the eyeball, do not attempt to remove it but instruct the patient to close his eyelids. Apply a soft pad of cotton wool and secure it by a bandage tied sufficiently firmly to keep the eyeball steady. Take the patient to a Doctor.
C. a corrosive acid or alkali is suspected, instruct the patient to blink his eyelid under water. Apply.a soft yad of cotton wool over his eye and keep the pad ill posltlon by a shade, or bandage applied lightly, and take the patient to a Doctor.
186 (a)
FOREIGN BODY IN THE EAR CHANNEL
If an insect is in the car c hann el , 1111 the car with oil or in se rt a few drops of su rg ica l sp irit ; the insect will float and .may be remov<:d.
All other foreIgn bodies s h ould be left in position and the patiel1[ warned not to inl<:rCae with th em. In llie case of a child, it may be necessary to lie his upper limbs to hi s body.
Take the patient to a Doclor.
FOREIGN BODY IN THE NOSE
Instruct the patient to breathe throu gh the mouth. Do not interfere with the foreign body. '1'ak<: the patient to a Doctor.
FOREIGN BODY IN THE STOMACH
Pins and other sma ll objects such as coins or buttons may be accideI1lally swa ll owed. Smoolh objects need not nece ssari ly cause alarm.
Give nothing by the mouth. Take the palient to a Doctor.
FISH BONE IN THE THROAT
Take the patient to a Doctor.

CIVIL DEF SUPPLEMENT
Subjects to be added to No. (, Lecture for Civil Defence Lectures and Examination
Although the principles of first aid are the same in times ofpeac<.; and war, 11rst aid students enrolling in Civil Defence arc required to receive instruuion on certain conditions not usually encountered in time of peace.
This short supplement to the 40th edition of "First Aid to the Injured" has therdore been prepared for the use of the s tud ents as s t aled above. It will not be intluded in the standard syllabus of instruction and examination of the St. John Ambulance Association.
BURNS
A. A lOll/Ie Bomb Flash and Radialion Burns
These differ in no way from ordinary burns and should be trea ted as such.
B. Phosphorus Blirns
Phosphorous is present in several types of bomb and the resulting burns differ from ord inary burns in that phosphorus adheres to the skin and continues to burn in the presence of air.
It is particularly dangerous in the eyes.
TREATMENT
(a) Flood the part with water to extinguish any burning particles.
186 (b)
(b) Cover the part with a sterile dressing which has been soaked in water.
(c) Keep the dressing wet to ensure the phosphorus does not again burst into flame.
(d) Remove the patient speedily to hospital for special treatment.
. Special warning-Only water-soaked dressings may be used ill the treatment of phosphorus burns.
BLAST
A. Atmospheric (in the air)
SYMPTOMS
I. Pain in the ears, chest and sometimes abdomen.
2. Later coughing up blood or sputum tinged with blood.
TREATMENT
I. Treat for shock.
2. Do not attempt artificial respiration.
3. Do not allow the patient to smoke.
4. Apply broad bandage round chest.
s. Remove urgently to hospital.
B. Immersion (in water)
SYMPTOMS
These are similar to Atmospheric Blast but usually more severe, especially pain in the abdomen. Blood may be passed from the bowel.

186 (c)
TREATMENT
I. Treat for shock removing wet clothing before wrapping in warm blankets.
2. Handle very carefully and remove urgently to hospital.
TRANSPORT
Where it is necessary to secure the patient to the stretcher various methods may be used.
Special Harness
(a) "Manifold" Harness consists of longitudinal straps fastened at either end round the handles and through the runners, and transverse straps fastened round the patient and stretcher.
There are several variations of this type including a very satisfactory one used by the R.A.F. with a central controlling fastening with quick release trigger.
(b) Ropes may be used quite satisfactorily as in the "Rescue" Service.
Where stretchers are not available or where they cannot be used, in addition to the various handseats the "Trigg Lift" may be used especially when removing patients close to walls where a team has difficulty in manceuvring.
The "Trigg Lift" consists of four sets of strong webbing attached to steel wire handles.
The handles facilitate passing the canvas bands under the patient and by supporting the head and feet and with two more above and below the buttocks a patient may be moved from an awkward position to a stretcher.
187
THOMAS'S SPLINT
Details. of this can be found in Appendix VI to "F" t Aid to the InJured." Irs
LABELLING CASUALTIES
AiJie-on labels should be used whenever possible, and Firstd ers must to using the standard types an the symbols mdicatmg the various conditions Th daIS? the symbols by marking the WI m elible pencil.
X Urgent removal and examination.
T Tourniquet, time of original application and times of each release.
H Severe hremorrhage.
M Morphine. Time of administration and dose.
C Contamination by Persistent Gas.
XX Nerve Gas or Non-Persistent Gas.
P Phosphorus burn.
R Radioactivity.
DEAD BODIES
They should be removed to nearest . and covered. convement building

CHAPTER XIV
PREPARATION FOR RECEPT!ON OF ACCIDENTS
1. Select the room. Choose one which is easy of access, on the ground floor, if possible. I t should be large and airy and preferably with a fireplace which will ensure efficient ventilation. In private houses the choice is necessarily limited, but a room with a cheerful sunny aspect is desirable. The patient's own room is the best if it fulfils these requirements.
2. Clear the passage and staircase of furniture and mats as far as possible.
3. Prepare the bedroom. Light the bedroom fire and remove all unnecessary furniture. Place the bed so that both sides are easy of access.
4. Prepare the bed. A single bedstead with a firm mattress (not a feather bed) should be used. If the patient has sustained a fracture of the pelvis or lower limb place transverse boards under the mattress and have ready a bed-cradle.
Remove the upper bedclothes, pla ce a mackintosh or waterproof sheet in the bed, and a draw-sheet on that portion of the bed on which the injured part will lie. Over this place a blanket or sheet, aprons, brown paper or even new sp aper s, to keep the bed clean until the patient's soiled clothing is removed and the patient has been attended to by the Doctor.
. Place hot water bottles or hot bricks covered with flannel In the bed.
5. Prepare for the prevention or treatment of shock Have ready hot blankets, tea, coffee and other
6. ready for the Doctor a small, easily moved table, basms and small, plenty of hot and cold sterilised water, soap, naIl brush, t?wels, antiseptics, dressings , cotton wd.001, dband.ages, safety-pms, scissors, and a pail to receive Irly ressmgs.
7. Have airing by the fire clean clothing for the patient and extra bedclothes and pillows in case they should b needed. e

CHAPTER XV
TRANSPORT OF INJURED PERSONS
An injured person may be removed to shelter by the following methods:-
1. Support by a single helper.
2. Hand seats.
3. Stretcher.
4. Wheeled transport.
The method or methods adopted will depend upon the fo llowing factors:-
(a) The nature of the injury.
(b) The severity of the injury.
(c) The number of helpers available.
(d) The distance to shelter.
(e) The nature of the route to be traversed.
After the appropriate First Aid treatment has been given the following principles of tran sport must be kept in mind:-
A. The position assumed by the patient or in which he has been placed must not be disturbed unnece ssarily.
B. Throughout the transport a careful watch must be kept on:-
(i) The general condition of the patient.
(ii) Any dressings, etc., that may have been applied.
C. The transport must be safe, steady and speedy.

METHODS OF CARRYING
A. If only one bearer is available
Cradle. (To be used only in the case of light patients or c hildren). Lift the patient by passing one of your arms well beneath his two knees, and the other round his back.
Human Crutch. Standing at his injured side, assist the patient by putting your arm round his waist, grasping the clothing at his hip and placing his arm round your neck, holding his hand with your free hand (Fig. 116) .
Pick-a-Back. If the patient is conscious and able to hold on, he may be carried in the ordinary "pick-a-back" fashion (Fig. 117 ) ·
Fireman's Lift and Carry. (To be used only when the patie nt is not too hea v y for the bearer ) . Help the patient to rise to the upright position. Grasp the patient's right wrist with your left hand. Bend down with your head under hi s extended arm so that your right shoulder is level with the lower part of his abdomen and place your right arm between or round his legs. Taking the weight of the patient on your right shoulder, rise to the erect position, pull the patient across both shoulders and transfer his right wrist to your right hand, so leaving your left hand free (Fig. 118).
B. If twO or more bearers are available
HAND SEATS
The Four-Handed Seat. This seat is used when the patient can assist the bearers by using one or both arms.
FIG. r r6-HUMAN CRUTCH
I. Two bearers face each other behind the patient and grasp their left wrists with their right hands and each other's right wrists with their left hands (Fig. 119), and stoop down.
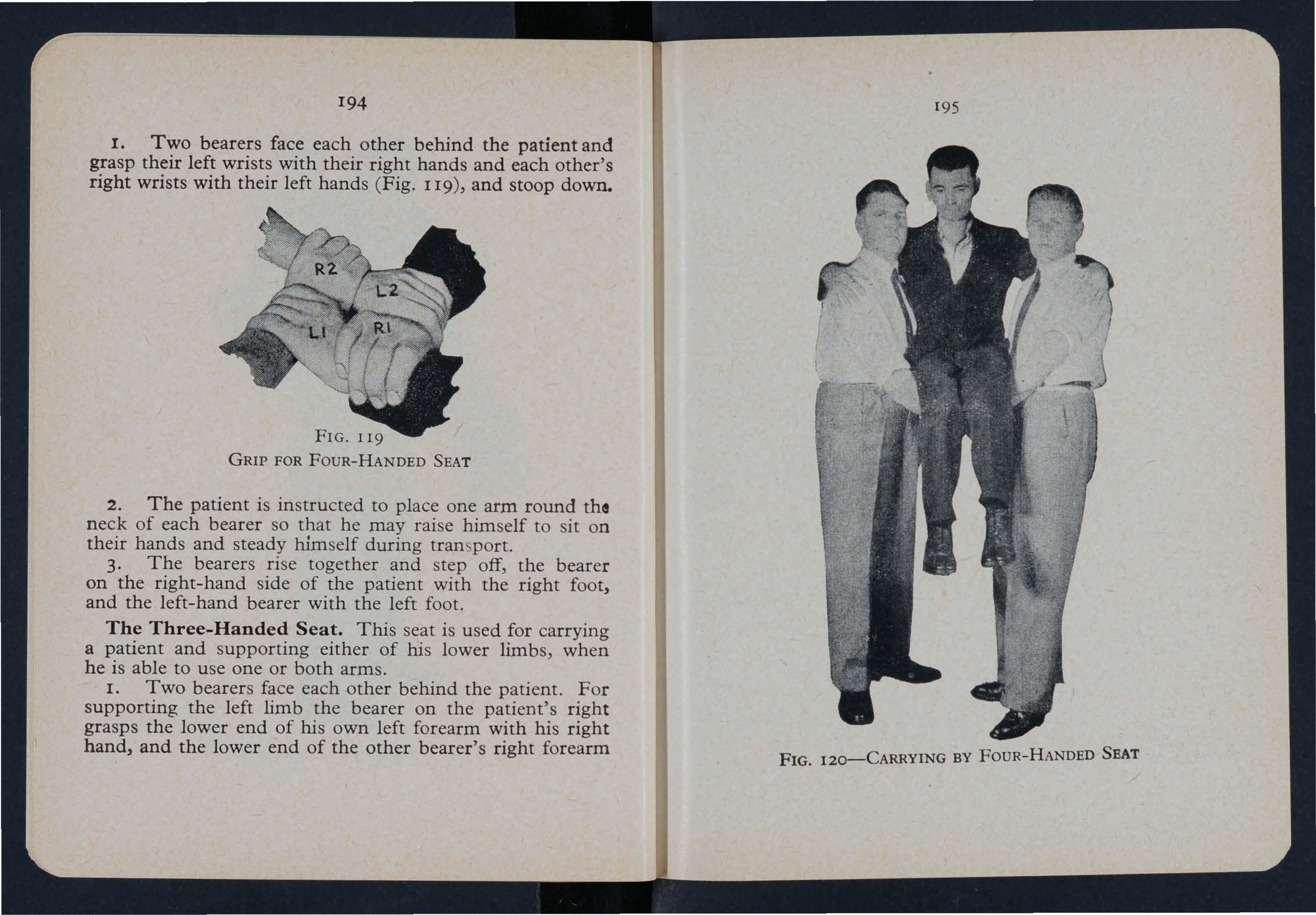
GRIP FOR FOUR-HANDED SEAT
2. The patient is instructed to place one arm round the neck of each bearer so that he may raise himself to sit on their hands and steady himself during tran sport.
3. The bearers rise together and step off, the bearer on the right-hand side of the patient with the right foot, and the left-hand bearer with the left foot.
The Three-Handed Seat. This seat is used for carrying a patient and supporting either of his lower limbs, when he is able to use one or both arms.
I. Two bearers face each other behind the patient. For supporting the left limb the bearer on the patient's right grasps the lower end of his own left forearm with his right hand, and the lower end of the other bearer's right forearm
with his left hand. The bearer on the left grasps the lower end of the first bearer's right forearm with his right hand (Fig. 12 J ). This leaves his left hand free to support the patient's left leg. For the patient's right lower limb follow the same directions, substituting "right" for "left" and "left" for "right."-In other words, if the left leg is injured

GRIP FOR THREE-HANDED SEAT
the bearer on the sound side grasps the lower end of his left forearm; if the right leg is injured, he grasps the lower end of his right forearm. The bearers stoop down.
2. The patient is instructed to place one arm round the neck of each bearer so that he may raise himself to sit on their hands and steady himself during transport.
3. The bearers rise together and step off, the right-hand bearer with the right foot, and the left-hand bearer with the left foot.
FIG. I21 I97 FIG. I22-CARRYING BY THREE-HANDED SEATThe Two-Handed Seat. This seat is mostly used to carry a patient who is unable to assist the bearers by using his arms.
1. Two bearers face each other and stoop-Cnot kneel)one on each side of the patient. Each bearer passes his

123
forearm nearest to the patient's head under the patient's back just below the shoulders} and} if possible} takes hold of his clothing. They slightly raise the patient's back} and
199
then pass their other forearms under the middle of his thighs (Fig. 123)} and clasp their hands} the bearer on the left of the patient with his palm upwards and holding a folded handkerchief to prevent hurting by the finger-nails; the bearer on the right of the patient with his palm downwards, as shown in Fig. 124 ("Hook-grip").
METHOD OF FORMING "HOOK-GRIP" (Front View)
2. The bearers rise together and step off} the right-hand bearer with the right foot} and the left-hand bearer with the left foot (Fig. 125).
In all cases of carrying by Hand Seats the bearers walk with the cross-over step and not by side paces.
THE FORE AND AFT METHOD
This method of carrying (Fig. 126) should be used only when space does not permit of a hand seat. The bearers walk in step.
FIG TWO-HANDED SEAT (FIRST STAGE) FIG. 124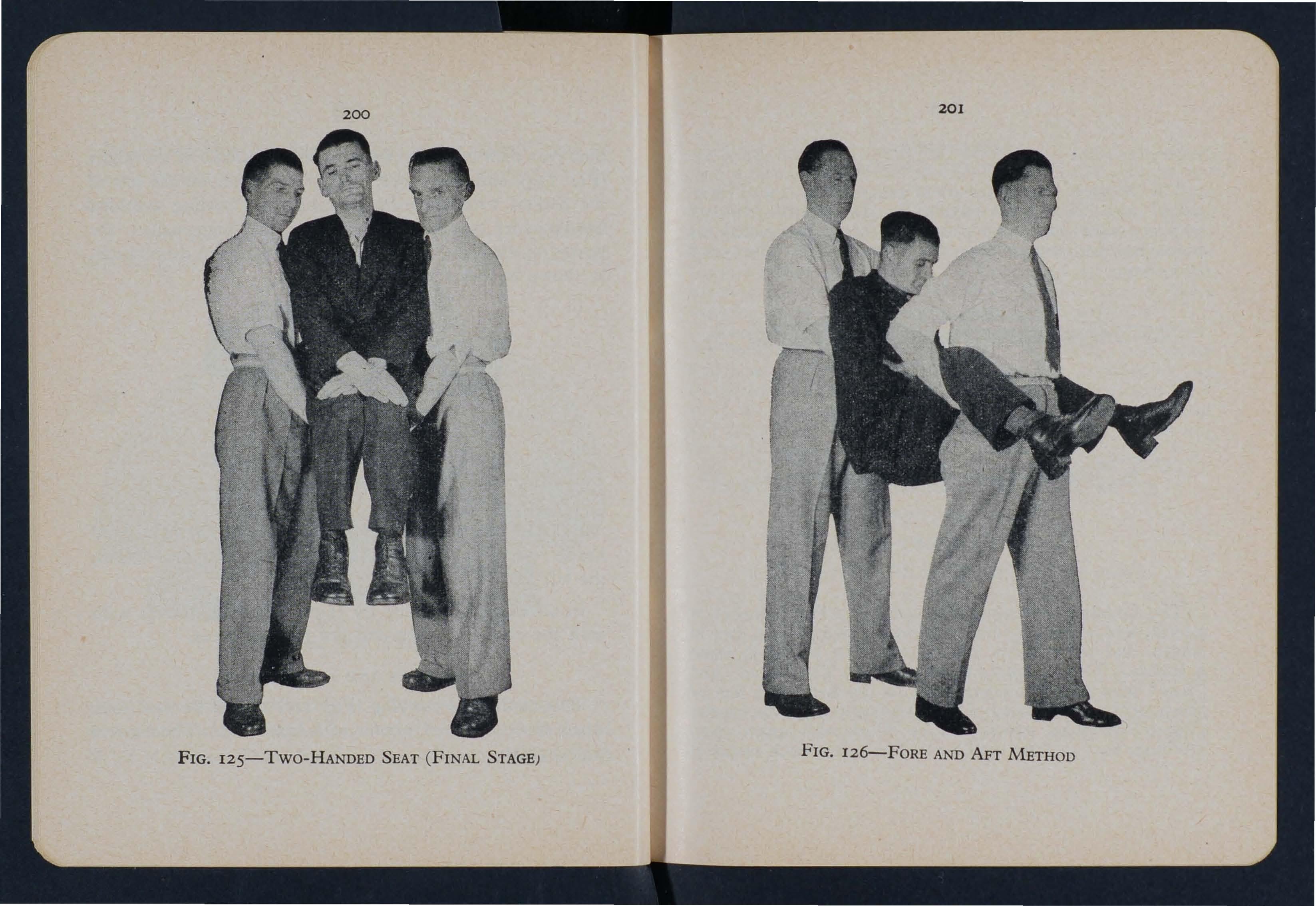
STRETCHERS
THE "FURLEY" STRETCHERS
The "Furley" Stretchers are of two patterns, viz., "Ordinary," and "Telescopic-handled." In general principle they are alike, the component parts being designated the poles, handles, jointed traverses, runners, bed, pillow-sack and slings.

TELESCOPIC-HANDLED STRETCHER ( OPEN)
The Ordinary Stretcher (Fig . 127) is 7 feet 9 inches III length, and I foot 10 inches wide. The bed is 6 feet in length, and the handles 10 k inches. The heiaht is about 6 inches. The weight is 21 to 22 lbs. The and "foot" of a stretcher correspond to the head and feet of the pat!ent. At the of the stretcher is a canvas overlay (the .pillow-sack), which can be filled with straw, hay, clothing, etc., to form a pillow. The pillow-sack opens at
203
head, and its contents can therefore be adjusted witJ:out Im due disturbance of the patient. The traverses are provIded with joints for opening or Telescopic-handled pattern (FIg. IS sImIlar, but ItS le ngth can be reduced to 6 feet by sliding the handles nea th the poles. This is of great value when working III confined spaces, or when a patient has to be taken up or down a narrow staircase with sharp turns. The St. John carrying sheet is also useful in similar circumstances.
When closed, the poles of the stretcher lie close together, th e traverse bars bein a bent inwards, the canvas bed neatly fo lded on the top of poles and held in po sition by the slings which are laid along the canvas and secured a strap which is placed transversely at the end of each sling an d passed through the large loop of the other, and round th e poles and bed.
STRETCHER EXERCISES
EXERCISE No. 1 FOR
FOUR BEARERS
1. SELECTION AND NUMBERING OF BEARERS
Four bearers will be selected and numbered I, 2, 3, 4 fro m tallest to shortest in order to give even a as possible. They will take up the pOSItIOnS shown ill
F ig. 129 . . "bl
No. I bearer is the leader of the squad and IS responsi e fo r the welfare of the patient until he is seen by a Doctor or handed over to another responsible person. All stretcherb earers must be able to undertake the duties of a No. I bearer.
20 5
2. COLLECTING BLANKETS AND STRETCHER
No. I will give the command-"No. 3 Collect Blankets, No.4 Collect Stretcher, Nos. 3 and 4 Right TurnQuick March," and the named bearers will collect the blankets and stretcher. NO.3 will fold the blankets neatly
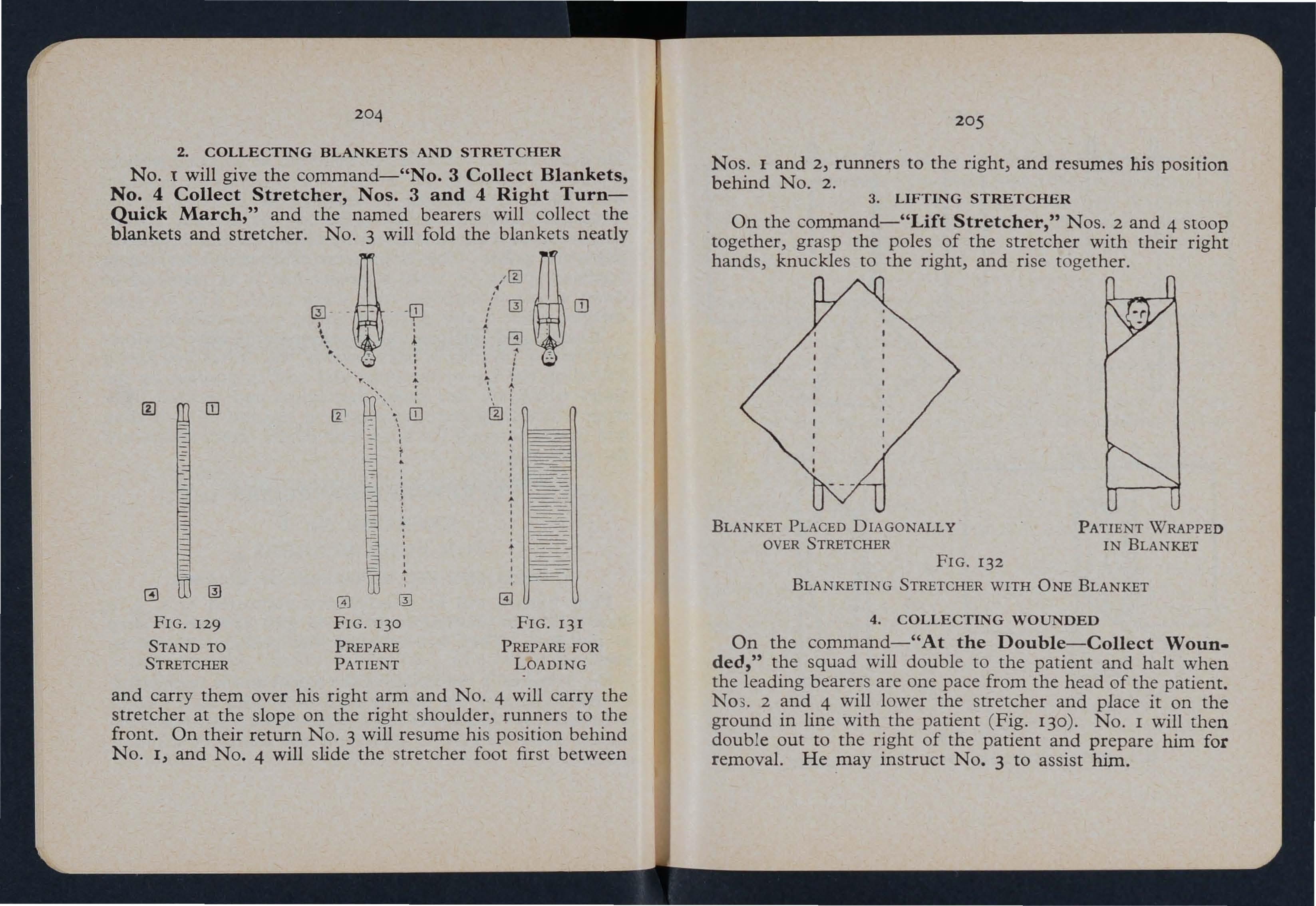
FIG. 129 FIG. 13 0 FIG. 131
STAND TO PREPARE PREPARE FOR STRETCHER PATIENT LOADING and carry them over his right arm and NO.4 will carry the stretcher at the slope on the right shoulder, runners to the front. On their return NO.3 will resume his position behind No. I, and NO.4 will slide the stretcher foot first between
Nos. I and 2, runners to the right, and resumes his position behind NO.2.
3. LIFTING STRETCHER
On the command-"Lift Stretcher," Nos. 2 and 4 stoop together, grasp the poles of the stretcher with their right hands, knuckles to the right, and rise together.
BLANKET PLACED DIAGONALLY OVER STRETCHER
FIG. 132
PATIENT WRAPPED IN BLANKET
BLANKETING STRETCHER WITH ONE BLANKET
4.
COLLECTING WOUNDED
On the command-"At the Double-Collect Wounded," the squad will double to the patient and halt when the leading bearers are one pace from the head of the patient. N03. 2 and 4 will lower the stretcher and place it on the ground in line with the patient ( Fig. 130). No. I will then double out to the right of the patient and prepare him for removal. He may instruct NO.3 to assist him.
FIG. I33
BLANKETING STRETCHER WITH Two BLANKETS

5. PREPARING AND BLANKETING STRETCHER
On the command-"Prepare and Blanket Stretcher," Nos. 2 and 4 will open the stretcher, see that the traverse bars are secure, test it and blanket it by one of the methods shown on pages 205-207 according to the number of blankets available.
Blanketing Stretcher with two blankets
I Place the first blanket lengthwise across the stretcher w ith one edge covering half the handles at the head end, and with the whole of the blanket slightly more to one side of the stretcher than the other (Fig. 133 A ) .
2. Fold the second blanket lengthwise in three and lay it on the stretcher with the upper edge about fifteen inches be low the first blanket.
3. O p en out the folds of the second blanket at the lower end fo r a bout two feet (Fig. 133 B ) .
Wrapping the patient
Place the patient on the four thicknesses of blanket on the s tretcher and :
1. Bring the foot of the second blanket up over the feet, t u c king in a small fold between the feet (Fig. 133 C ) .
2. Bring the sides of the fold s of this blanket over the fee t and lower part of the legs and tuck in.
3. Turn in the upper corners of the first blanket and bring the shorter end over the patient, then the longer end over and tuck in well (Fig. 133 D ) .
4. If a third blanket is available, it should be doubled lengthwise and laid over the patient before the patient is tucked in.

6. LOADING STRETCHER
(a) When the patient is lying on a blanket or rug (Fig. 134). The edges of the blanket or rug must be firmly rolled close up to the patient. On the command-" Load Stretcher," the bearers, two on either side, will grasp the rolls and, unless a fifth bearer is available to slide the stretcher underneath the patient, will move by side paces over the stretcher and lower the patient carefully on to it.
(
b) When the patient is not lying on a blanket or rug and a spare one is available (Fig. 135).
210
The patient must be placed on a blanket or rug as follows :-
Place the blanket or rug on the ground in line with the patient and roll it lengthwise for half its width. Nos. 2, 3 and 4 will turn the patient carefully on to his side. No. I will place the rolled portion of the blanket or rug close
NO·4 No. I NO.3 NO.2

READY TO LIFT PATIENT
to the patient's back and all the bearers will gently roll the patient over until he is lying on his opposite side on the blanket or rug. The blanket or rug will then be unrolled and the patient gently turned on to his back so that he lie s in the centre of the open blanket or rug. On the command"Load Stretcher," proceed as at 6 (a).
211
Provided four or more bearers are available, the blanketlift or rug-lift is the method of preference for loading a patient on to a stretcher owing to the smoothness of the w- hole operation .
NO.4 No. I NO.2
LIFTING PATIENT
I c) When the patient is not lying on a blanket or rug and none is available.
On the command-"Load Stretcher," Nos. 4, 3 and 2 g / ill place themselves on the left of the patient; No. 4
facing the shoulders, No. 3 facing the hips and No. z facing the knees; No. 1 will place himself on the right of the patient facing NO.3 (Fig. 131). All will go down on their left knees and place their forearms beneath the patient, paying particular attention to the seat of the injury. (If it is necessary to lift the patient from the right side, bearers will go down on their right knees. When" Standing to

PLACING STRETCHER
Stretcher" (see Movement 7) the positions of Nos. I and 3 bearers will be on the left and those of 2 and 4 on the right of the stretcher). Using the hook grip, No. 1 joins his left hand with the left hand of NO.4 and his right hand with the right hand of NO.3. No. 4 supports the head and shoulders, NO.2 the lower limbs (Fig. 136).
21 3
When No . 1 gives the order-"Lift," the patient must b e lifted gently and slowly and placed on the knees of Nos. 4, 3 and 2 (Fig . 137) . No. 1 will disengage, take hold of t he (left hand across, resting the near pole on his left hip ) and place the stretcher beneath the patient, so that when he is lowered on to it, his head will just be clear of th e metal bar at the top and will rest on the pillow if one is available (Fig. 138) . NO.1 will then resume hi s po sition .
NO.4 No.2 NO.1
L OWERING PATIENT
When NO.1 gives the order-"Lower " the patient will be raised slightly from the knees of Nos. 3 and 2 , lowered gently and carefully on to the stretcher and covered with coats (Fig. 139) . The bearers then rise and turn to face the fo ot of the stretcher.
8. CARRYING A LOADED STRETCHER
7. STANDING TO STRETCHER
On the command-"Stand to Stretcher," No. I will take up a position level with the handles at the foot of the stretcher; NO.2 will step forward opposite No. I ; and
No. I

140
HAND CARRIAGE BY FOUR BEARERS
No. 3 will double round the head of the stretcher and position himself on the right of the stretcher opposite NO.4(Fig. 129).
No. I will decide whether the stretcher is to be carried b y four or two bearers.
( a) Hand Carriag e by Four Bear ers
On the command-"Hand Carriage by Four BearersL ift Stretcher," all four bearers stoop together , grasp the p oles with their inner hand s and rise together holding the str etcher at the full extent of their arms (Fig. 140) .
AD VANC I N G
On the command-"Advance," all bearers will step off with the inner foot. The bearers must keep their knees slightly bent and walk with a relaxed gait.
R ET IRING
On the command-"Retire," a squad will retire by wheeling and not by turning.
LOW E RI NG A LO ADE D STRE TCHE R
On the command-"Lower Stretcher," the four bearers stoop, gently lower the stretcher to the ground and rI se together.
(b) Hand Carriage by Two B earers
. On the command-"Hand Carriage by Two BearersLi ft Stretcher," Nos. 2 and 4 will take a side pace over the handles of the stretcher and if they decide to use slings
will pick them up, place them over their shoulders and on the handles of the stretcher. They will then rise steadily
No. I

No 2
NO·4
141
HAND CARRIAGE BY Two BEARERS
together keeping the stretcher level. Nos. I and 3 will turn inwards to assist. No. r particularly can help to prevent
the patient's feet catching on the buttocks of No.2. Nos. I and 3 will then turn to face the foot of the stretcher (Fig. 141).
ADTUSTING SLINGS ( IF USED )
On the command-"Ad;ust Slings," Nos. I and 3 turn t o the left and adjust the slhgs of Nos. 2 and 4 respectively.
ADVAN C I N G
On the command-"Advance," Nos. I, 2 and 3 will s tep off with the left foot and NO.4 with the right . The b earer s must keep their knees slightly bent and walk with a relaxed gait.
RETIRING
On the command-"Retire)" a squad will retire by wheeling and not by turning.
LOWERING A LOADED STRETCHER
On the command-"Lower Stretcher," Nos. 2 and 4 stoop slowly, gently lower the stretcher to the around and 0 Tl se together. If slings are in use Nos. 2 and 4 will remove t hem after lowering the stretcher, step over the handles to t heir former positions, and place the loops of the folded slings over the near handles and the ends over the other handles.
9. RELIEVING BEARERS BY CHANGING 1"3' 2 --+ 1 f.4\ NUMBERS \.:V \2.J

EXERCISE No. 11
FOR THREE BEARERS
The stretcher will bid . same line as his bodye pJce the patIent's head, in the injured side left knee on his hands under the patient's I . N ees and passes egs , os. 2 and 3 kneel
NO.2 NO·3 NO,l
CHANGING NUMBERS
On the command-"Chauge Numbers," Nos. 1 and 3 will turn about and 1 1 the whole will then step off together, Nos. 3 and 2 wheeling round the ends of the stretcher and all moving round twO places clockwise. Each bearer will halt in the position of the bearer whose place he has CD 4 3 CD taken and the new Nos. 1 and 3 turn left about so that all again face the foot of the FIG. 142 stretcher (Fig. 142).
10 . UNLOADING A STRETCHER
On the command-"Unload Stretcher," the bearers will adopt a similar procedure to that carried out for loading the stretcher.
11. RETURNING BLANKETS AND STRETCHER
At the end of the exercise, NO.1 will give the command"No.3 Return Blankets, No.4 Return Stretcher, Nos. 3 and 4 Right Turn-Quick March." The procedure to be followed by Nos. 3 and 4 is similar to that carried out for collecting blankets and stretcher.
12. CLOSING A STRETCHER
On the command-"Close Stretcher," Nos. 2 and 4 turn inwards and close the stretcher by pushing in the poles after the ttaverse bars have been unlocked, folding the canvas on itself and buckling the straps tightly round the stretcher behind the traverse bars. Where slings are in use they must be placed on the canvas and the straps buckled round the stretcher behind the traverse bars.
FIG. 143
READY TO LIFT PATIENT
on their left knees on "d each other and . SI es of the patient, facing an d hips, hands his shoulders mand-"Lift " the b g by .the .hook-gnp. On the como earers WIll flse to the erect position,
and moving by side-paces, carry him head foremost over the 'foot of the stretcher, the horizontal position of his body being maintained throughout the movement, and lower him
No 3

carefully on to the stretcher. When unloading, the patient will be lifted and carried head foremost over the head of the stretcher (Figs. 143 and 144 )
EXERCISE No. III FOR TWO BEARERS
(For use in mines and narrow cu ttings w her e ::,pace is limited)
LIFTING THE PATIENT
Both bearers will stand astride the patient, No. 2 at the head, placing his forearms under th e patient"s shoulders,
N o. I about the knees, placing his left hand beneath the patient's thighs and his right below the knees. When both are ready No. 1 will give the command-"Lift."
223
ADVANCING
NO.1 will the order-"Advance," and both will step off WIth the left foot, taking short even paces, and stoopmg s? that the body of the patient is not far from the ground (FIg. 145). They will advance till the patient is over the stretcher when NO.1 gives the order-"Halt- Lower."
NO.1

FIG.I46
LOWERING PATIENT
LOWERING THE PATIENT
On the command-"Halt-Lower," the patient is lowered gently on to the stretcher (Fig. 146). Both bearers then take up position on the left of the stretcher ready for lifting, No. 2 at the head and No. 1 at the foot.
IMPROVISED STRETCHERS
Stretchers may be improvised as follows:-
(a) Turn the sleeves of two or three coats inside out; pass two strong poles through them, button the coats. The poles may be kept apart by strips of wood lashed to the poles at both ends of the bed formed by the coats.
(b) Make holes in the bottom corners of one or two sacks and pass stout poles through them keeping them apart as in (a).
(c) Tie broad bandages at intervals to two poles.
(d) Spread out a rug, piece of sacking, tarpaulin or a strong blanket, and roll two sto ut poles up in the sides. Two bearers stand on each side and grasp the middle of the covered pole with one hand, and near the end with the other. They walk sideways.
(e) A hurdle, broad piece of wood, or shutter may be used; rugs, clothing, hay or straw should be placed on it and covered with a piece of stout cloth or sacking which is useful in taking the patient off the stretcher.
Always test an improvised stretcher before use.
RULES FOR CARRYING PATIENTS ON STRETCHERS
As a general rule, carry a patient feet first. The exceptions are:-
(a) When carrying a stretcher upstairs.
(b) When going uphill with a patient whose lower limbs are uninjured.
(c) When going downhill with a patient whose lower limbs are injured.
(d) When carrying a patient to the side or foot of a bed.

(e) When 1.oa.ding .an ambulance (but see page 122), though It IS advIsable to ask the patient if he has any preference.
TO CROSS A DITCH
The stretcher is lowered with its foot one pace from the edge of ditch. Nos. 1 and 2 bearers then descend. The IS now advanced) Nos. 1 and 2 in the ditch Supportmg the front end while the other end rests on the edae of the ground above. Nos. 3 and 4 then descend. All the bearers now carry the stretcher to the opposite side and the of the stretc?er is made to rest on the edge of the ground) while the head supported by Nos. 3 and 4 in the d:tch. Nos. 1 and 2 climb out. The stretcher is lifted forward the ground above) and rests there while Nos. 3 and 4 clImb up.
TO CROSS A WALL
The stretcher is lowered with the foot about one pace from the wall; the bearers then stand to stretcher) Nos. 2 4 on the left, Nos. 1 and 3 on the right. They turn stoop .down, grasp the poles with both hands and rIse slowly, liftmg the stretcher, holding it level at the full extent o.f the arms. Then by side-paces they advance to the wall) raIse the stretcher and lift it on to the wall so that the front runners are just over the wall. No. 2 crosses the wall and takes hold of the front handles; No. 1 then crosses the wall; they grasp the poles) lift the foot of the stretcher; all the bearers then advance and lift the rear runners over the wall) resting the rear handles on the wall' )
.:ro. 4 then crosses the wall and takes hold of the left pole. '\fo. 3 then crosses the wall and takes hold of the right p ole. The bearers then advance until the stretcher is clear of the wall. The stretcher is then lowered to the ground.
TO LOAD AN AMBULANCE
The stretcher is lowered with its foot or head one pace fro m the end of the ambulance, according to the patient's d esire to travel feet or head first ( but see page 122).
The bearers now stand to stretcher.
On the command-"Load."-The bearers turn inwards, stoo p, grasp the poles of the stretcher, hands wide apart, palms uppermost; they rise slowly) lifting the stretcher, h olding it level at the full extent of the arms. They then take a side-pace to the ambulance) raising the stretcher eve nly to the level of the compartment to be loaded. The ro nt bearers place the runners in the grooves and then assist he rear bearers to slide the stretcher into its place and secure It . If slings have been used) they should be kept with their stretc her.
Many ambulances are provided with upper and lower b erths. In such cases the sequence of loading is upper left) upper right, lower left) lower right.
TO UNLOAD AN AMBULANCE
Two bearers take hold of the handles at the rear and gently withdraw the stretcher. As it is withdrawn) the othe r two will take hold of the handles at the front, and, laking the weight, lower it to the full extent of the arms; .he n by side-paces march clear of the ambulance, lower he stretcher to the ground.
LIFTING INTO BED
The stretcher is lowered at the side of the bed. The bearers take positions as for unloading stretcher, Nos. 2, 3 and 4 being on the side furthest from the bed. The patient is unloaded on to the knees of Nos. 2, 3 and 4. No. I will disengage and remove the stretcher (this may be done by pushing it under the bed). He then joins hands with NO.3. All the bearers rise to a standing position, supporting the patient on their forearms. No. I disengages and goes to the patient's head, and supports it. All bearers then step forward and gently place the patient on the bed. If the bed is narrow and there is room, the stretcher may be placed on the floor with the head close to the foot of the bed. The injured person may then be lifted over the foot and placed on the bed. If the patient is lying on a blanket and if the bed is narrow and there is room, the blanket lift should be used, the bearers lifting the patient over the foot of the bed.

INTRODUCTION TO APPENDICES
The Textbook of the Association deals primarily with First Aid rendered by an individual at the scene of the accident with such materials as may be at hand, as distinct from "organised" First Aid as by Fir.sl Aid .units trained to work together and eqwpped wIth swtable appliances.
For the benefit of First-Aiders who have opportunities of practising together, who are equipped with s:utable material and appliances and who have not to rely on Improvisation, some additional information is included in the Appendices which follow. They will be of particular. to First-Aiders who are working as members of specIalised serVIces
APPENDIX I
THE ROLLER BANDAGE AND ITS APPLICATION
ROLLER BANDAGES
Roller bandages are made of muslin, calico, domette, flannel, crepe, or any other suitable material, and may be rolled by hand or by means of a machine (Fig. 147), but
U ses of the Roller Bandage:-
1. To retain splints or dressings in position.
2. To afford support.
3. To exert pressure and so reduce or prevent swelling.
4. To drive blood from the part of the body bandaged, as in the case of extreme collapse from hremorrhage.
Sizes. The bandages are made in various widths and lengths to suit different parts of the body, e.g.:-
Fo r the head ..
F or the upper limbs ..
F or the lower limbs
F or the trunk
FIG. 147
ROLLER BANDAGE MACHINE

in either case the roll must be tight and even. When a bandage is partly unrolled, the roll is called the head and the unrolled part the free end. (Fig. 14 8).
FIG.I48
ROLLER BANDAGE SHO'NING
( 1 ) HEAD, AND ( 2 ) FREE END
2
Fo r the fingers Width Length
2 or 2t inches 3 to 6 yards. inches 3 to 6 yards.
3 inches 6 yards
4 to 6 inches 6 yards or more. I inch 1 yard.
GENERAL RULES FOR APPLICATION
I. Stand or sit opposite the patient.
2. In the case of a limb, place it in the position in which it is to be kept when bandaged.
3. See that the bandage is tightly and evenly rolled before attempting to use it.
4. Hold the head of the bandage in the right hand when bandaging a left limb and vice versa.
s. Apply the outer side of the free end to the part, and, where possible, lock it by a superimposed turn.
6. Never allow more than a few inches of the bandage to be unrolled at a time.
7. Bandage from below upwards, and from within outwards, over the front of the limb.

8. Apply each layer of the bandage so that it covers two-thirds of the preceding one.
9. Apply the bandage firmly and evenly, but not tightly enough to stop the circulation. If the edges turn up on passing the hand over them, the bandage is too loose. If, after the bandage is taken off, red lines are seen, it has not been evenly applied.
10. When finished, fix the bandage securely with a safety pin or by other suitable methods.
METHOD OF APPLICATION
There are four principal methods of applying the roller bandage:-
I. The Simple Spiral, which should only be used when the part to be bandaged is of uniform thickness, as, for instance, the finger (Fig. 156) or wrist and a short portion of the forearm above it. The bandage is carried round in a spiral direction; straight circular turns must be avoided because they interfere with the circulation.
2. The Reverse Spiral, which is made by a number of spiral turns in which the bandage is reversed downwards upon itself at each circuit of the limb. This is used in bandaging parts of the limbs where, owing to their varying thickness, it is impossible to make a simple spiral lie properly. (Figs. 164 and 165).
3. The Figure of 8, which is applied by passing the bandage obliquely round the limb, alternately upwards and downwards, the loops resembling the figure 8. It is used for bandaging at or in the neighbourhood of a joint such as the knee or elbow. (Figs. 166 and 167). It may also be used instead of a reverse spiral for a limb.
4. The Spica, which is a modified figure of 8 used for bandaging the shoulder, gr oin or thumb. ( Figs. 174 and 175 ) ·
When the methods of bandaging are understood, no difficulty should arise in covering any part of the body. The points to which attention should be directed are evenness and firmness of application rather than a completed bandage corresponding exactly with the It in be found that differently shaped limbs reqUlre slight modifications of the bandage .
APPLICATION TO VARIOUS PARTS
Capeline Bandage for Head. Take two bandages and join the free ends. Standing behind the patient, who should be seated, apply the join to the middle of the forehead just a bove the eyebrows, head s of the bandages inwards. The bandage in the right hand is called the v ertical bandage, and that in the le ft hand is called the horizontal bandage. Bring both rolls to the back of the head and cross them. (Fig. 149 ) . Carry the vertical bandage forward over the head, and the horizontal bandage round t he head and over the vertical FIG. 149 bandage in front. (Fig. 150 shows the vertical bandage carried twice forwards and once backwards). Continue to pass the vertical bandage backwards and
forwards, each time a little to the left and right alternately, locking it with the hprizontal bandage. Finally, pass the horizontal bandage twice round the head, and pin in front. (Fig. 151).

FIGS. 149-151
Bandage for the Ear. (Figs. 152 and 153). Width of bandage 2! in. This is a useful banpage for holding a dressing about the ear. Place the free end of the bandage over the affected ear and carry it horizontally across the forehead, carry it back to the starting point, round to the opposite ear and obliquely down across the back of the head, covering the lower part of the dressing . Carryon up to the horizontal turn and make a reverse. Repeat these horizontal and oblique reverse turns until the dressing is covered and finish by pinning in front.
Bandage for the Eye. (Figs. 154 and ISS). Width of bandage 2t in. This is a useful bandage for holding a dressing on the eye. Place the free end of the bandage above the ear on the same side as the injured eye and take a horizontal turn one and a half times round the forehead and the head, then obliquely across the back of the head, below the ear and upwards across the eye. Bring the bandage back to a point below the ear as shown in Fig. ISS and repeat the oblique turns until the dressing over the eye is covered. Finish by taking another horizontal turn round the head and pin the bandage in position.
Simple Spiral for the Fingers. Width of bandage I in. Course:From inner to outer :;ide of front of wrist, a sufficient length being left for tying; across back of hand to inner side of finger to be first bandaged (taking the fingers in order from the little finger side), by one spiral to root of finger nail; round the finger by simpJe spirals; thence to root of little finger and round wrist, continuing to the next finger, if necessary. When completed, tie to free end left for the purpose (Fig. 156).

Recurrent Bandage for the Finger. (Figs. 157, 15 8 and 159). Width of bandage I in. This bandage may be used to hold a dressing at the tip of the finger. Take the bandage once over the middle of the tip of the finger, holdi!lg it on each side. Agam make two more turns over the tip, one on each side of the middle. Apply a spiral from the top as far as necessary down the finger. Finish off
157 with a figure of 8 round the wrist.
FIGS. 157-159-REcURRENT BANDAGE FOR THE FINGER
Spica for the Thutnb. Width of bandage, r in. Course:Across front of wrist from inner to outer side; up between thumb and finger by one spiral to root of thumb nail; simple turn round thumb; diagonally across back of thumb and FIG. 160
FIG. 161
FIGS. 16o-161-SPICA FOR THE THUMB
hand to wrist; continue by figure of 8 round thumb and wrist until the thumb is covered. Finish by a turn round wrist and secure (Figs. r60 and r6r).
Bandage for the Hand. Width of bandage, 2 or 2! in. Course:-Across front of wrist from inner to outer side; t hen from wrist to base of little finger; once round fingers (Fig. r62 ) . Figure of 8 round hand and wrist. Repeat figures of 8 until the hand is covered, then round wrist and secure (Fig. r63).

FIG. 162 FIG. 163
FIGS. 162-163-BANDAGE FOR THE HAND
Reverse Spiral for the Foreartn. Width of bandage, 2 or 2! in. Course:-Across front of wrist from inner to outer side; across back of hand to first joint of little finger;
across front of fingers; to inner then outer side of wrist
Repeat Two or three simple spirals round wrist: Reverse spIrals on forearm and secure (Figs. 164 and 165).

FIG . 164
FIG. 165
FIGS. 164-165-REVERSE SPIRAL FOR THE FOREARM
figure of 8 bandage, as for the leg (see page 242 and FIg. 178), may be applied instead of the spiral.
Figure of 8 for Elbow, Knee and Ankle. Width "f b andage, 3 in. Course:-Round the joint and then figure of 8 alternately above and below joint (Figs. 166 and 167). Secure.
FIG. 166
FIG. 167
FIGS. 166-167
FIGURE OF 8 BANDAGE FOR ELBOW, KNEE AND ANKLE
FIG. 168
FIG. 169
FIGS. 168-169-SPICA FOR THE SHOULDER
Spica for the Shoulder (left). Width of bandage, 3 in.
Course:-Secure the free end round the arm. 1 hence from inner side of left arm, over the front of the arm· across the under the right armpit; acro ss the to the outer sIde of the arm; across the back of the arm (Fig. 168). Repeat until the part is sufficiently covered and secure (Fig. 169),
Bandage for Both Breasts. Width of bandage, 3 in.
C ourse:-From right side of back of waist; round waist; u p over front of left shoulder to right side of waist; round waist; over back of right shoulder to left side of waist; and round waist (Fig. 172). Repeat alternately over the left and right shoulders until both breasts are covered and su pported (Fig. 173). Secure.

FIG. 170
FIG. 171
I7O-17I-BANDAGE FOR THE BREAST
Bandage for the B,reast (right). Width of bandage, 3 in.
Course:-. From left sIde of back of waist; round waist; un.der nght breast; over left shoulder to right side of waist (FIg. 170); round waist; repeat until the breast is sufficiently covered and supported (Fig. 171). Seccre.
172
173
FIGS. 172-173-BANDAGE FOR BOTH BREASTS
To give added support it is sometimes more effective
0 use two crepe bandages 3 in. in width, and apply one LO ea ch breast in the manner des cribed for one breast only.
Spica for (right) Groin or Hip. Width of bandage, J in , Course:-Two turns round the thigh to fix the bandage. fork to crest of right hip; across loins to left hip; he nce to outer side of and behind right thigh. Repeat until the groin is sufficiently covered. Secure. (Figs. 174 n d 175).
Bandage for the Foot. Width of bandage, 2! in. Course: -From inner side of ankle to outer; then from inner side of ankle, over foot to root of fifth toe; round foot; two or three reverse spirals round foot; figures of 8 round the ankle and foot until the part is sufficiently covered; once round ankle, and secure (Figs. 176 and In).

243
Bandage for a Broken Collar-bone. I. Place in the armpit a pad, about 2 in. by 2 in. by 4 in.
2. Pass the end of a 4 in. bandage round the upper part of the arm to form a loop, and secure with a safety pin.
176
177
FIGS. 176-I77-BANDAGE FOR THE FOOT
174 FIG. 175
FIGS. 174-I75-$PICA FOR GROIN OR HIP
Figure of 8 Bandage for the Leg. Width of bandage, 3 in. Course:-From inner side of ankle to outer side of foot; round foot; round ankle; again round foot and ankle; and thence up the limb by reverse spiral to commencement of calf muscles and thence up the limb by ascending figure of 8, each layer covering the previous one by two-thirds (Fig. I78). Secure. The reverse spiral, as for the forearm, may be applied throughout instead.
FIG. 178-FIGURE OF 8 BANDAGE FOR THE LEG
FIG. FIG. FIG.3· Carry the bandage across the patient's back a little bel ow the arml-1its to draw the shoulder back and continue . , It round the chest to the armpit on the injured side.
4· Raise the forearm well up.
5· Carry the bandage diagonally across the back and over the uninjured shoulder (Fig. 179 ) , and round the elbow three times to raise the shoulder and support the forearm.

6. Pass the bandage three times round the body and lower end of the arm to lever out the 1>houlder.
7· Secure with a safety pin (Fig. 180).
Bandage for the Jaw. Take one yard and a half of a 3 in. bandage. Cut a small hole in the cenlre, and cut the bandage 245
f rom each end down the middle to within 11 in. of the thus producing a bandage with four tails. Apply as shown ill Fig. 181.
Barrel Bandage for the Jaw, as used in war . injuries because it maintains the lower jaw in a more p osition. Take a bandage 2 } in. wide and 2 yards III length ;
place it under the chin; tie a single hitch on top of the head (Fig. 182) ; draw one loop forward and one backwards well down the back of the head (Fig. 183 ) until they form a horizontal turn round the head, meeting the loop under
the chin in a half-hitch in front of each ear; take the free ends and tie them in a reef knot on top of the head (Fig. 184)·

182 FIG. 183
FIGS. I82-I84-BARREL BANDAGE FOR THE JAW
MANY - TAILED BANDAGES
Many-tailed bandages are valuable for fixing dressings on an abdominal wound because they give good support and remain in position extremely well. They are also frequently used for limbs since the wound can be examined or a dressing changed without undue disturbance of the patient (Fig. 186).
247
Domette, flannel, linen or other suitable material may be used and the bandage is made as follows:-
Cut a foundation strip ABCD (Fig. 185) as long as the required width AB of the final bandage and 4 in. in width
FIG. I8S-MANY-TAILED BANDAGE (how made)
AD. Strips of material 3 in. in width are laid across this, p arallel to one another and each overlapping one-third of t he preceding one; the strips are then sewn to the central found a tion.
186
MANY-TAILED BANDAGB
Many-tailed Bandage for Stump of Limb. Make the bandage as Fig. 187 from 3 in. calico, and apply as Fig . 188
FIG."T" BANDAGES
"T"-shaped bandages (Fig . 189) are used for fixing dressings over the rectum and perineum. They are usually made from 5 in. gauze bandages or from strips of calico 4 in. in width.
A horizontal piece AB is cut long enough for the waist and folded in half lengthwise. The upper end of the vertical

FIG. 187
FIG. 188
FIGS. 187-188
MANY-TAILED BANDAGE FOR STUMP OF LIMB
piece DE is folded over to make a hem 4 in. in width. In this hem two slits are cut I t in. apart and the piece AB is threaded through. The lower end of E is slit. When applied, the waist piece is fastened first and the vertical piece used to fix the pad or dressing, the narrow ends being brought to the front and tied or pinned to the waist piece.
B A Many - tailed '-----------r...L. Abdominal Binder
may have an elongated central strip as shown in Fig. 190. The ends are fixed in the same way as the vertical piece of the "T" bandage in Fig. 189 in order to keep the binder in position.
A Many-tailed Chest Bandage is made as on page 247 and to the upper edge are sewn two strips to act as shoulder straps.
FIG. 189 "T" BANDAGE
FIG. 190
MANY-TAILED ABDOMINAL BINDER \...--

APPENDIX II
SHOCK
Shock has been defined in Chapter IV as a condition of prostration of the body arising from sudden exhaustion of vital activities and varying appreciably in degree from a slight feeling of faintness to a condition of collapse in which the vital forces of the body are so exhausted that death may result. It is the degree and type (or combination of types ) of shock which determine the seriousness of a patient's condition.
Nerve Shock is a reflex action on the part of the body which happens automatically without our knowledge or consciousness and may be essentially protective. It produces rapid onset of unconsciousness which may not be serious because recovery is usually rapid and there is no loss of blood or other permanent harm to the body. The beneficial effect of the loss of consciousness enables the individual to escape from the pain, sound, sight, smell or other obnoxious stimulus which caused unconsciousness; and the accompanying fall in blood pressure and pallor of the skin prevent loss of body heat, and loss of blood if the skin is damaged, all of which can be helpful. -
Although Nerve Shock may be essentially protective, it must never be assumed that a patient having the signs and symptoms of Nerve Shock is necessarily suffering from Nerve Shock, because the signs and symptoms of Nerve Shock can be found accompanying either Hrernorrhagic or
Shockhwhich are very serious conditions. It is for . s reason t at too much stress cannot be laid on th Importance of treating shock immediately. e
f In to illustrate some of the causes and combination o vanetIes of shock the followin di h included although th ' b g agrams ave been ey are y no means exhaustive of the and of the varieties of shock. of be studied In conjunction with the text
Fig. 191-NERVE SHOCK
Point 0 in dicates the ori gin of an acci d en t o r illness resultin g in unconsciousness due to ne rve sh ock. The line OA in dicates the on set of un :on scio u sn ess, and the line AB represents re c ov ery from unconscious n ess. No t e th e rel a ti ve sl ope s of l ine s O A and AB indi c atin g that re c overy ( though rapi d , se e p age 2 5 0) is le ss rap id than the ons e t. The duration of the condition may vary from moments to a maner of

Fig. l'; '!-CO M BINATION OF NERVE SHOCK AND Hl£MORRHAGIC S H OCK
Point 0 indicates the origin of an accident involving hremorrhage. The line OA indica tes th e onset of unconsciousness, and the line AB represents recovery from unconsciou sness Complete recovery is, however, interrupted at point B by the supervention of hremorrhagic shoc k brought about by the increase of hremorrhage, the effect of which has been masked up to this point by nerve shock. C u rve BC indicates the gradual deterioration of the patient'S con dition due t o hremorrhagic shock. At point C one of two things may happen, viz. :(i ) if correct treatment has been given and hremorrhage controlled thereby, hremo rrhagic shock may be arrested and the patient will gradually recover (cu rve CD ), o r
(ii) if hrem orrhage is no t controlled, the p atient 's con di ti on d e t erior a te s f u rther at point C and coma and dea th s up erven e
255 ApPENDIX III
RESPIRATION
RESPIRATION-INTERCHANGE OF GASES
Inspiration plus expiration constitutes respiration, and the amount of air in the lungs at the various stages of respiration is shown in the following table :-
fi dal Air The amount of air inspired and expired in ordinary quiet breathing (about 30 cubic inches either way).
S upplemental Air: The amount of air which can be forcibly expired after an ordinary expiratioB has taken place (about 100 cubic inches).
R esidual Air: The amount of air remaining in the lungs after {he strongest expiration (about 100 cubic inches).
C omplemental Air: The amount of air that can be taken in after an ordinary inspiration by the deepest inspiration (about 120 cubic inches).
Vital Capacity: The total amount of air that can be expelled from the lungs after a forced inspiration by a forced expiration.
The interchange of gases takes place by diffusion, first b etween the blood and the air in the air cells, and secondly between the air in the air cells and the tidal air.

SS3NsnODSNO)Nn W 3NVld
ApPENDIX IV
THE ROCKING STRETCHER METHOD OF ARTIFICIAL RESPIRATION
(To be used when a specially devised stretcher is available an d when an assistant is present to h elp in placing the patient o n the stretcher)
I. Commence Schafer's method of artificial respiration immediately. Do not take the patient to the rocking stretcher ; have it brought to the patient.
2. On the arrival of the rocking stretcher, place the patient on it without breaking the continuity or rhythm of Schafer's method. Ensure support for the patient's head and a clear airway. Continue Schafer's method until an assistant has secured the patient's wrists and feet to the handles of the rocking stretcher by means of broad bandages .
3. When the patient has been secured in position, cease Schafer's method and start rocking with a head down tilt.
In cases of drowning do not commence the feet down tilt until the water has stopped flowing out; otherwise it might be sucked into the lungs.
4. Alternate the head down and feet down rocking movements regulating the rate to approximately nine doubl e rocks per minute, i.e., four seconds head down and three seconds feet down. Continue until natural breathing is restored unless a Doctor decides that further efforts will be of no avail.
5. The patient must be kept warm by means of blankets, hot water bottles and impervious coverings.
APPENDIX V
RESUSCITATION APPARATUS
In resuscitation work the "Novita" apparatus can be used, if available, in conjunction with Schafer's method of artificial r espiration. The apparatus cor:sists of a. steel cylinder containing oxygen, connected Wlth a fleXlble tube to a face-mask. The apparatus is fitted with hand-controlled valves. As soon as artificial respiration has been an d while it is being continued, an assistant loosens any ught clothing round the patient's neck, chest or waist, applies the o xygen face-mask and operates the apparatus.

ApPENDIX VI
THE THOMAS SPLINT
This splint (which is named not after the famous hospital in London, but after the eminent surgeon, the late Mr. H. O . Thomas) , may be used (a) for all fractures of the thighbone except where there is an extensive wound in upper part of the thigh or buttock against which the splint would pr ess and cause pain; (b) for any fracture about the kneeJoint and bones of the leg; (c) for certain cases of extensive wounds of the fleshy part of the leg or thigh.
OUTFIT
For practising the application of the splint the following ou tfit is desirable:Thomas Splint. Stretcher suspension bar.

Reversible stirrup (Sinclair's).
Stick or 6 in. nail for Spanish windlass.
Flannelette bandage, 3 yards long by 3 inches wide.
Five flannelette bandage slings and 5 safety pins.
Five triangular bandages.
Some loose woven bandages and wool.
Two pieces of Gooch splinting about 8 inches by 6 inches.
A stretcher. (Trestles on which the stretcher may be placed are convenient when practising .)
Three blankets.
To form the slings mentioned above, five pieces of fla n nelette bandage, approximately 30--36 inche s in length ar e taken and folded into two. The loop ends are pinned ov er the inner bar of the splint, rolled up and secured in po si tion by short ties of loo se woven bandage.
PERSONNEL
A team for the purpose of practice usually consists of ro u r First-Aiders, who may be numbered 1, 2, 3 and 4, an d a patient; . but three or even two are sufficient.
DRILL
The application of the Thomas Splint can most con\ eniently be taught as a drill . .
1. Prepare Stretcher. Nos. 1 and 3 proceed to the pa tient and cover him with a blanket: Nos. 2 and 4 prepare th e stretcher as described on page 205 or 207 (Figs. 132 and 13 3) ·
2. Hand Extension. NO.3 places himself at the foot of the patient facing him and opposite the injured limb. K ee ping the arms straight, he grasps the heel of the boot i th his right hand and the toe with his left, and, keeping

the foot vertical, exerts a steady pull. No. 4 steadies and supports the injured limb above and below the seat of fracture.
3. Apply Splint. NO.1 threads the ring of the splint over the boot (pointed end of ring outwards), No. 3 removing and re-applying each hand in turn to permit of this being done. While NO.4 continues to support the limb at the seat of fracture, No. I passes the splint up the limb until its further passage is stopped by the buttock. The n otched bar mu st be kept horizontal.
4. Clove Hitch. No. 2 takes three yards of flannel bandage and makes a clove hitch in such a way as to leave one end about six inches longer than the other and a double loop about ten inches in diameter. This loop is applied over the boot with the ends on the outer side of the ankle: t o allow of this being done NO.3, still carrying out hand extension, again removes and re-applies one hand at a time. The long end of the bandage is taken under the instep of the boot, up on the inner side of the ankle, threaded through the loop of the hitch and turned down outside the loop. These two ends of the bandage, one on either side of the ankle, are for use as extension bands when permanent extension takes the place of hand extension.
5. Fix Leg.
(a) The extension bands are tied round the notched bar as follows :-the outer extension band is passed over and under the bar, round the notch, drawn taut, and held over to the opposite side. The inner band is passed under and over the bar, then also round the notch, so that it crosses the first band and prevents it slipping. The two are tied off by a half bow. NO.3 may now release his hold.

a;he notched bar .is now placed on some object th limban petrol tm turned on its side, so as to st:ady ground. NO·4 will continue t o
h middle sliz:g is tied off over the outer bar behind t e(d) No: 4 the knee slightly bent.
e behind the ankle and calf are tied off so tat leg IS now .supp orted in a shallow trou gh with the on(g) ars of the splint level with the centre of the leg
e To. prevent the leg rising . off the splint, a bandage IS pla.ced across the leg Just below the knee' the ends are down between the leg and the crosshedfbehind, brought up outside the bars and tied off on t e ront of the leg.
lower limb is thus fixed in a position of extension It may be moved freely without causing pain to patIent or damage to the injured part.
. 6. Dress Wound. A wound l'f prese t . dr d ,n, IS essed ill accor ance with the general rules.
li Splinting. or other well-padded sp nts may be applied (over th dr ' 'f one piece is placed behind the limb a de essilldgsb , 1 off the re " . n secure y tymg front of two The other piece is placed in kn e thigh, care bemg taken to avoid pressure on the The dressing and the splints are kept firml in by two narrow bandages applied as follows ._ y the f e cenr.:e of bandage is placed near each' end of sPdlinthting.. The ends are taken d . an e SIde bars of the splint crosse behind and then brought h . ' bars and tied in front of the limb.uP on t e outsIde of the
8. Stirrup and Figu re of Eight. The stirrup is sprung on to the splint (care being taken to keep it clear of the extension bands) and pres sed upwards until the horizontal bar rests lightly aga inst the sole of the boot, thus preventing lat eral movement o f the foot. A narrow bandage is applied In the following manner to form a figure of eight. The centre of the bandag e is pl ac ed under the sole of the boot. T he ends are brought forwar d , crossed, taken down behind th e ankle, cros sed again, brought up outside the bars and tie d off in front of the limb.
9. Spanish Windlass. Except in the case of a compound fra cture when the bone protrudes, the extension bands are tightened and a small piece of wood or a nail may be introduced to increase the tension by twisting up as required.
10. Pad in Ring. A pad of cotton wool is placed inside th e ring on the outer side of the thigh to act as a wedge and so prevent undue movement.
I I. Suspension Bar. This is fitted to the stretcher with the grips away from the foot end, and with its horizontal part one hand's breadth in front of the foot.
The splint is slung about one hand's breadth from the horizontal iron of the suspension bar by bandages tied to the splint bars. It is also tied to the vertical irons of the suspension bar to prevent lateral movement; to prevent vertical movement of the splint, a narrow bandage is passed round the outer side of the splint below the foot and tied off to the handle of the stretcher.
12. Cover Patient. Hot water bottles are applied and the blankets adjusted as shown on page 205 or 206. The patient is now ready for removal to shelter.

WOUNDS C AU SED BY A VENOMOUS SNAKE OR RABID ANIMAL
SNAKE BITE
The bite of a venomous snake endangers life, and immediate action is necessary to prevent the spread of the venom through the body.
TREATMENT
(a) If the bite is on a limb
I. Immediately arrest all circulation in the limb by means of a constriction about the upper arm or thigh between the wound and the heart. Irrespective of where the bite is, do not apply the constriction below the elbow or the knee; this will not impede the circulation sufficiently.
The purpose of the ligature (constrictive bandage ) is to delay the entry of the venom into the circulation by obstructing the venous blood flow, so gaining time for further treatment.
Soft rubber gas tubing, elastic braces, strips of cloth or neck-ties make suitable ligatures.
The constriction may be left in position for at least two hours, provided it is relaxed temporarily every 10 or 20 minutes for half to one minute at a time, or until the skin below it becomes pink, and again tightened.
2. Many snakes dribble venom on to the surface as they bite. It is therefore necessary to identify the fang marks
and wash the surface of the wound with water or weak permanganate serious emergencies saliva may be used if water IS not available.
3 As soon as the ligature has been applied and the surface washed cut into the soft tissues in the region of the bite. Make (avoiding main ves sels ) about an inch long and up to half an inch deep along the of the fangs and in the direction of the length of the limb. Make sure the s around the bite has been well washed before cutting, otherwise venom may be introduced from the s kin surface into the tissues by the knife.
The cuts should be allowed to bleed freely, as the flow of blood will help wash out the venom.
. Where a long interval is likely to elapse before skilled treatment is available, double ligation may be employed to promote the washing out of venom from th.e cut ti ssue. A second ligature is tied loosely about an below the original one. Immediately after .the released (as described in Rule I ) the second ligature IS tlghtened so as t o obstruct the venou s but not the arterial blood flow (i.e., just enough to cause swelling and of the veins and blueness of the limb below the obstructlon) . The wound will now bleed freely and should be to d? so for about half a minute. The original ligature IS then tIghtened until all circulation ceases and subsequently relaxed periodically as described in Rule I.
(Where help from a doctor is it .may. advisable to cut away the bitten area , partlcularly If this .IS n ot on a limb. Such procedure may be dangerou s ill un s killed hands as it is necessary to excise to the depth of the fang puncture, i.e. probably about half an inch).

4. Suction of the incised tissue may be tried, especially where the bite has occurred in regions where ligature cannot be applied. If no other apparatus is available, suction may be carried out by the mouth. Never do this until the skin has been well washed and do not apply the bare lips. The safest way is to suck through a piece of thin rubber sheeting or latex. On the whole, it is probably better to rely on bleeding and washing out of the venom than on sucking, which may involve considerable risk to the operator.
5. When the bite is on the arm or leg the limb should be kept as still as possible. Movement helps the spread of venom through the veins and lymphatics. If the bite is on the lower limb, fix rhe legs together (after applying Rules 1-4) with bandages round the ankles and above the knees. When the bite is on the arm, fix the limb along the side of the body, one bandage round the wrist and body, the other round the body and the arm above the elbow. Never neglect to release the ligature temporarily at regular intervals of ten to rwenty minutes.
6. Keep the patient at rest, and try to calm him. Do not allow him to walk about, as exercise will increase the circulation and so the rate of spread of the venom.
7. Keep him warm and give him warm tea sweetened with sugar. Small amounts of alcohol may help soothe the patient; large amounts are contra-indicared.
8. If breathing is failing apply artificial respiration.
9. The patient should be seen by a Doctor and given effective antivenin serum as soon as possible. If he has to be transported he should be accompanied by an attendant
who can supervise the periodic relaxation of the ligature. Antivenin should be given only by a trained attendant or Doctor. It is not readily available in England. Elsewhere, e.g., in India and Africa, antivenin prepared for use against local snake venom should be used. Owing to the specificity of antivenin it is important wherever possible to identify the snake causing the bite.
(b) If the bite is elsewhere than on a limb
As ligation is impossible, wash the skin in the region of the bites, incise the wound and apply suction and then apply Rules 6 to 9 above.
BITE BY A RABID ANIMAL-HYDROPHOBIA
Hydrophobia is caused by the bite of an animal such as a dog, jackal, fox or wolf suffering from rabies. The virus travels from the bite along the nerves to the central nervous system, and differs entirely in this respect from snake bite where the venom is absorbed directly into the veins from the bitten tissues.
TREATMENT
1. After a person has been bitten by a rabid animal or one suspected of having rabies, every effort should be made to promote bleeding so as to wash the wound from within outwards. This is best done by:-
(a) Immediately placing a constriction (a piece of cord, tape or handkerchief) between the bite and the trunk tightly enough to cause congestion of the limb and ensure bleeding, but nor so tightly as to obstruct the arLerial circulation in which case the limb becomes
pallid, the pulse cannot be felt and bleedirlg entirely ceases.
(b) Keeping the affected part low; the upper limb should allowed to. hang down and in the case of the lower limb the patIent should be seated with the foot on the ground.
(c) Bathing the wound with warm water to which crystals of of potash have been added: the solutlon should be pale pink in colour.
2. Give alcohol such as brandy or whisky (in the case of an adult two tablespoonfuls or in the ca se of a child two teaspoonfuls) in a little water or hot black coffee.
.3 ..If it is not 'possible to obtain the services of a Doctor Within a few minutes of the person being bitten, the wound b.e cauterised. .This is done by removing the and applymg a fiwd caustic, such as carbolic or rutnc aCId a match or a piece of wood cut to a point, or lunar caustIc. To prove effective every tooth mark must be and cauterised separately, as only by so doing can the VIrUS be destroyed.
If more . than half an hour has elapsed since the per son has been proceed as in Rule s I and 2 and then remove the constrICtlOn, but do not cauterise the wound.
4. Apply a dry dressing and retain it in position with a bandage.
A which has bitten anyone should be kept under or 10--14 days to see if it develops si<YTI S of rabIes. As the incubation period can be over 6 and the to transmit the disease is only during last 10 days, this can greatly reduce anxiety in a bitten person.

ApPENDIX VIII
EMERGENCY BIRTH
(Text supplied by Ministry of Health)
If a pregnant woman complains of recurring pains of a griping character corning on at regular and decreasing int ervals ("labour pains" ), she must be regarded as an urg ent case requiring immediate professional attention by a Doctor or Midwife.
1. Send for a Doctor or Midwife or arrange for the p atient to be removed to hospital at once.
2. Make the patient as comfortable as possible on her back with a pillow to support her head, and keep her wann. She may be given a warm drink but not alcohol. Advise her not to exert undue pressure when the pains come on, but rat her to breathe quickly so as to lessen their effect. This may help to prevent or lessen a tear when the baby is bom. No thing further should be done.
3. If the baby is born before the Doctor or Midwife arrives the baby should be lifted clear of the mother (without pulling on the cord which is still attached) and placed between the mother's legs in a position in which it can breathe easily, preferably on its side. The child should be ke pt warm and covered, without being smothered.
AS A GENERAL RULE, APART FROM MAKING T HE MOTHER COMFORTABLE, THE LESS DONE T HE BETTER.
Page
Abdomen .. .. 25, 32, 39 " wound in wall of 105
Abdominal aorta. . 104 " binder, manytailed 249 " hernia 182
Abscess on brain 173
Accidents, preparation for reception of

Page
Ammonia.. 73, 177, 17 8
" as a stimulant 66
Amputated limb . . 99
Anatomy . . 25
Asphyxia, causes of Page 7 2 ,73 68 " " " definition of general rules for treatment of 74 signs and symptoms of 74
Barbiturate drugs
Bed, lifting into .. Page 175 226 " to prepare
Belladonna poisoning
Berries, poisoning by Birth, emergency .. 18 7 175
Acetone 17 1 .. 174, 176, 177, 17 8
Ankle, bandage for 239 " bone 32 " dislocation of 143 " fracture near " joint " sprained
Acids
Air " hunger, definition
" passages
" sacs
" tube .. 69, 13 2 of 107 7 2 , 73 69 69
Alcohol as a poison 175
" as a stimulant 66
" in snake-bite 266
Alkaline solution 67, 179, 180, 181
Alkalis 174, 177, 17 8
Alveoli 69
Ambulance, to load and unload .• 122, 225
Antidotes ..
Antiseptics
Aorta " abdominal .. Aperients
Apoplexy .. Approach to case Arm, bone of
fracture of
fracture of involving
sling.. 48
Arterial hremorrhage 93, 99
Arteries 69, 86, 89
Artificial respiration 78, 256
Aspirin poisoning Atlas 175 26 Aura Auricles 167 86
Automatism, post-epileptic 167
Autonomic system 161 Axis 26 Back-bone 26 46 99 48
Bandage, " " " " " " broad constrictive improvi se d many-tailed narrow .. roller .. rubber .. 246 4 6,59 228 98 "triangular 45
Bandages, roller, applica" tion of 229-249 triangular, application of 51-59
Bites by poisonous reptiles 175, 264 " by rabid animals 175, 267 "Black Eye" 110
Bladder 42 " hremorrhage from 108 " injuries to 140 20 5, 20 7
Blanketing stretcher
Blanket lift 121,2II palm of Bleeding from hand
Bleeding point
Blisters
Blood " circulation of " clot .. " corpuscles .. " pla sma " pres sure " stream " vessels .. 13 8
Page
Bottles, hot water 65
Bowel , hremorrhage from 108
" protrusion of 182
Brachial artery 103
" pressure point 103
Brain .• 25, 38, 159
" abscess .. 173
" injury to u8, 164
" tur.1our .. 173
Breast-bone 28, 30, 39, 69
" fracture of .. 132
Breasts, bandage for 240, 241
Breathing. . 22, 68
Bronchioles 69
Bronchus .. 69
Bruises
Brush-burn
Burns by corrosive chemicals 181
" by electric shock.. 78
Capillaries 42, 69, 86, 90
Capillary hremorrhage 110
Capsule 33
Carbolic acid 177
Carbon dioxide 72, 76, 88, 91
Carbon monoxide 76
Carotid artery
Page 100 100 " pressure point
Carpus 30
Carrying, methods of 191
Cartilage .. 28, 32, 33, 35 "displaced 156
Cerebro-spinal system 159
Cervical vertebrre 26
Cheek, bandage for 53
" hremorrhage from I09
Chest .. 25, 28, 30, 39, 69
" bandage for 54
" many-tailed bandage for .. 249
Childbirth, emergency .. 269
Choking .. 72, 75
Circulation of the blood, 86, II7 " to induce 65
Civil Defence miscellaneous injuries 186 (a)
" "
Clavicle
Cleanliness stretcher 123 30 93
Closed fracture
Clot, blood
Clothing on fire III .. 91, 94, 105 180
" removal of 23
Clove hitch 50
273 Page
Coccyx 28, 32
Collar and cuff sling 49, 13 8
Collar-bone 30
" bandage for .. 243
" fracture of 132
Colles's fracture 13 8
Coma 161
Comminuted fracture
" diabetic 17 1 II3
Complicated fracture
Compound fracture II3, 130 112, lI8, 130
Compress ., 44
Compression II8, 165, 166
Concussion u8, 162, 164, 165
Connective tissue 39, 69
Constrictive bandage 99
Contused wounds 92
Convulsions 167, 172
" definition of 164 " hysterical 168
" infantile 169
Corpuscles 9 1
Corrosive acids 174, 176, 17 8
" alkalis 174, 177, 17 8 " burns 181 " in eye •. 185
Corrosive poisons
Cradle
Cramp
Cranium Page 174, 176 .. 191 .. 158 25, 26
Crepitus u6, u9, 130, 155
Crush injuries of limbs 67
foot 151
39 Delirium Depressed fracture
Diabetic coma
Diagnosis . .
Diaphragm
Digital pressure
Diphtheria

175 114, u8 39 .. 17 1
Direct force " " presswe violence 20, 21, 23
39, 69, 7 1, 7 2 100, 102, 103, 104 73 III, 130, 136 95 118, 122, 140 149
Dislocation II3, 143 " definition of .. 153 " signs and symptoms of 155 treatment of .. 15S
Disposal of patient 24
Ditch, to cross with stretcher 224
Dressings. . 43
Drowning. . 75
Drugs, barbiturate 175
" poisoning by 163
Ear
" bandage for 232
" foreign body in 186
" hremorrhage from IIO, II8
Elbow 30
" bandage for 55, 239
" joint 34
" joint, dislocation of 153
Electric shock 73, 76
Emergency birth . . 269
" dressings 44
Emetic
Epiglottis
Epilepsy, major " minor
Epileptic fit
Examination of a patient 21
Expiration. . 72, 82, 85
Eye, bandage for 53, 234
Eye, "
foreign body in . . 184 pupils of 23, 162, 165 sockets 26
Face, bones of " burnt
Fainting
Femoral artery 25,26 .. 180 61, 64 .. 104
" pressure point .. 104
Femur 32, 35
Fibula 32
Finger-bones 30
Fingers, bandages for 234,235 " dislocation of .. 153
" fracture of 138
Fireman's lift and carry.. 19I
First Aid, essentials of 19 " " meaning of 17
Foot, crushed " fracture of Page 15 1 15 1
Fore and aft method of carrying ..
Forearm, bandage for " bones of " fracture of 199 237 30 13 8

Page
Fracture, general signs and symptoms of 115 " types of .. I II
Fractures, special ..
Frost-bite ..
Functions of the body
Fish-hook under skin
Fits
Food, poisoning by Foot, bandage for " bones of
First-Aider, qualifications of .. 19 " responsibility of .. 17 18 4 167, 175 .. 174 57,24 2 32
Forehead, bandage for Foreign body embedded 53 " " " " " " " " " " " under skin .. 184 in ear 186 in eye 184 in nose 186 in stomach 186 in throat .. 186 in wound 94, 95, 97, 105
Foreign fluid in air passages
Four-handed seat
Fracture, causes of " definition of 73 19 1 III III " dislocation 124 " general rules for treatment of II6
Fungi, poisonous .. "Furley" stretcher II8- 1 52 .. 182 25,4 2 159 .. 174 123, 202
Gas, inhaling poisonous 73, 174 " suffocation by poisonous ..
Gases, interchange of 69, 88, 255 43
Gauze
Germs
Glands
Granny knot 9 1 , 92 , 93, II2 39 47
Greenstick fracture 114
Gristle 28
Groin 104, 157 " bandage for 56, 241
Gums, hremorrhage from 109
Hremorrhage 43
Page

Page
Page
arterial 93, 99
capillary IIO from an Internal organ 44, 107, 130, 163 from special regions .. 107 severe 93
Hremorrhage and wounds 92, II6 " " " " " " " "
" severe, treat-
" ment of .. 94
" slight 93
" slight, treat" ment of .. 105
" venous 93
Hremorrhagic shock 62, 250
Hand 30
" bandage for 56, 237
" bleeding from palm of
" fracture of ..
" seats
Hands, sterilisation of
Hanging
Head, bandage for 19 1 94 73, 75 53
Head, bones of .. 26
" capeline bandage for 231 8 86 2 ,39,
Heartbeat . . 86
Heat exhaustion " stroke
Heel-bone ..
Hernia
" abdominal . . Hip 170 169 3 2 157 182 32
" bandage for .. 56, 241
Hip-joints. . 32, 34, 145
History, definition of 22 "Hook-Grip" 199
Hot water bottles. . 65
Human crutch
Humerus ..
Hydrochloric acid
Hydrophobia
Hysteria
Hysterical convulsions
Iliac arteries
Impacted fracture
Improvising bandages " slings " splints
Improvising stretcher 223
Incised wounds 9 2
incontinence 167
Indirect force III, 130, 13 2
" pressure 99 " violence II8, 122, 140
Infantile convulsions ., 16 9
" paralysis 73, 173
Infection .. 43, 63, 93, 17 8
Innominate bones
Insensi bili ty 32 " "
Intestines, protrusion of, through wound in abdomen 106
Involuntary muscles
Iodine, poisoning by Iris 39, 161 177 162
Inspiration
Instep causes of general rules for treatment of .. 162
Insulin overdose
Interchange of gases 71,82,84 32 ., 17 1 69, 88, 255
Internal organ, hremorrhag e " " Intestines from .. 44, 107,130, 163 injury to 65 42
Jaw, bandage for _ ., 244 " barrel bandage for 119, 245 26 " lower " lower fracture of II8 33 " InJunes to 153 Jugular vein 102
Kidneys 42, 113, 17 2
" hremorrhage from 108
Knee, bandage for 57, 239 "displaced cartilage of.. 15 6
Knee-cap .. " fracture of Knee-joint
Knot, granny " reef 32 149 32 , 35 47 47
Knuckles ..
Lacerated wounds
Larynx
Leg, bandage for ..
)) bones of " fracture of ..
Ligaments .. Lightning ..
Limb, amputated ..
" lower Page 30 242 32 143 28,33, 156 73, 17 8 99
" lower fracture of .. 30 143
" " upper 30 upper fracture of .. 138
Lint 43
Liver 28,42, II3, 130
" h::emorrhage from .. 108
Loading stretcher, "
Lockjaw
Loin
Lower jaw

Lower jaw, fracture of
Lower limb " "fracture of Lumbar vertebr::e Page II8 30 143 28, 39
Lungs 28, 39, 68, 69, 113, 130, 13 2 h::emorrhage from 107, I09
" root of 69 Lymphatic vessels 42
Many-tailed bandage 246
Marsh gas 76
Mechanism of circulation 86
Medical aid, provision for 24
Membrane 69
Meningitis
Needle, embedded
Neck Page .. 1 84 30
Nerve shock 61, 250
Nerves 25,38,39, II3, rr6,
Nervous system
Nitric acid
Nose 122, 159, 160 42, II8, 175 176, 17 8 " foreign body in 26, 69 186 " h::emorrhage from
Oil of vitriol
Open fracture
Opium poi soning
Orbit
Oxalates
Oxalic acid
" " emergency method 126, 129, 21 I " standard method 126, 209 73 28 26
Metacarpus
Metallic poisons
Metatarsus
Methane gas
Mouth
Muscles " injuries to 173 30 174 32 76 26, 69 25, 35 .. 153 " ruptured
dislocatron of 153
Muscular action .. .. 157 III, 149 279
Oxygen 17 6 II2 175 26, II8 .. 177 .. 177 42, 88, 91
Pad, ring
Palate
Palm 30 " hremorrhage from.. 138
Pancreas 42 " hremorrhage from .. 108
Paralysis .. infantile .. Patella
Pelvis " brim of )) fracture of Phalanges
Pharynx
Phenol
Physiology
Pick-a-back
Plasma
Pleura
Poisoning by drugs Page122, 165 73, 1733 2 30,3 2,39 80, 104 107, 14 0 30, 32 69 177 25 I9 f 9 f 69, 7 1 163
Poisonous berries .. 174 " fungi .. 174
" gases .. 73, 7 6 , 174-
Poisons 73, 174
Post-Epileptic automatism 167
Pon's fracture ., 143
Prepared sterile dressing.. 43
Pressure, digital 100, 102, 103, 104 " direct 95 " indirect .. 99
Pressure point, brachial 103 " " carotid IOo.
Page
Pressure point, definition of 100 " " " " femoral .. 104 subclavian 102
Prussic acid, poisoning by 73, 175
Pubes
Pulmonary artery 3 2 88 " circulation 86, 88
Pulse 23, 103
Puncturep wounds 92
Pupils of eyes 23, 162, 165
Qualifications of a FirstAider 19
Quicklime. . 178 " burn by 181
Rabid animals, bites by Rabies
Radial artery
Radius
Re-dressing of injuries
Reef knot .. 267 26 7 23 30, 13 8 17 47
Respiration .. 68, 71, 255
" artificial 78, 256
280
Respiratory centre 69, 72 ,
Respiratory mechanism " system " tract ..
Responsibility of Aider Rest First17 66
Resuscitation
Ribs 257 28, 39, 69, 71 " fracture of . . 107, 129
Ring pad .. Roller bandage
Rubber bandage ..
Rump-bone
Rupture
Ruptured muscles
Sacrum
St. John sling
Saline solution
Sal volatile
Scalds
Scalp, bandage for Scapula 59, 98 228-249 9 8 28 157, 182 .. 157 28, 32 51, 134 179, 180 66, 183 17 8 53 30
Schafer's method of artificial respiration 78
Seats, four-, three- and two-handed 191-199
281
Sepsis
Sewer gas .. Shelter
Shi n-bone .. Sho ck " electric Page 93, 178 73 21, 24 32 24, 60 , 25 0 " treatment of 73,7 6 64 116
Shortening
Sho ulder, bandage for Sho ulder- blade 55, 240 30 fracture of 136 "
Shoulder- bone 30 34
Shoulder-joint " dislocation of 153
Signs, definition of 22
Silves ter's method of artificial respiration 83
Simple fracture I I I
Skele ton 25
Skin 39
Skull, fracture of base of IIO, II8 " fracture of dome of 98 " vault of Slings " improvised 5 I
Smelling salts 66
Smoke, suffocation by 75 Smothering 73 Snake bite 264 Solar plexus
Spinal canal " " column cord 161 26, I59 25 25, 26, II3, 122, 159
Spine 26, 28, 30, 39 " fracture of .. 122
Spleen 28, 42, 113, 130 " hremorrhage from 108
Splint, Thomas .. 257
Splints .. 117
Sprained ankle 143, 157
Sprains 156
Starvation. . 173
Sterilisation of hands 94 " of water 94
Sterno-mastoid muscle 100
Skull 25 " " " base of 25,26, 72, 159 dome of .. 25 fracture of 107, II4, II8, 165 Page
Sternum . .
Stimulants
Stings Page 28, 69 65 175, 18 3
Stomach "
Strains 28, 42 foreign body m 186 hremorrhage from 108, I09 .. 157
Strangulation 73, 75
Stretcher blanketing 205, 207 " " " "

Stump, bandage for " many-tailed bandage for wound
Stupor
Subclavian artery .. Page 59 247 99 161 102 " pressure point 102
Suffocation by poi onous gas. . 76 " by smoke 75
Sulphuretted hydrogen 76
Sulphuric acid 176, 178
Thigh-bone " fracture
Thomas splint
Thoracic vertebrae
Thorax
Three- handed seat
Throa t Page 3 2 of .. 143 257 28 " foreign body in 39, 69 194 69 186 " hremorrhage from 109 swelling of tissues within . . 73, 75
socket, hremorrhage from .. 109
.. 62, 251 69 124 24, 18 9
24
bandage 45, 5 I-59
39 Tumour on brain
seat
"Stroke" carriage of 223 Civil Defence.. 123 emergency method of loading 126, 129, 2II
Sunstroke.. 169
Surroundings 20
Swallowing reflex 172
Swelling of tissues within the throat 73, 75
Symptoms, definition of.. 22
exercises 20 3-222 "Furley" 123, 202 improvised .. 223 standard m ethod of loading 126, 209 166
Structure of the body 25
Strychnine poisoning 73, 175
Synovial fluid 33 membrane
Systemic circulation "T" bandage
Tail-bone .. Tarsus Tendons Tetanus 33 86, 88
Throttling. . 73
Thumb 30 " bandage for 236 " dislocation of 153 "pressure 95
Tibia
Tissue connective 32, 35 35 39 of throat, swelling within. . 73, 75
Toe-bones 32
Toes, fracture of .. Tong ue " hremorrhage Too th .. 15 1 120, 162 from 109, II9 26
Urremia
Urinary passages. . 140
Urine 108, 167, 172
Vein, jugular Veins
Venous hremorrhage
Ventricles ..
Vertebrae ..
Vertebral column .. ..

Violence, direct 118, 122, 140 , Wounds accompanied by 149 severe hremorr" indirect !I8, 122, hage, treatment 140 of 94
Vitriol .. 17 6 " accompanied by
Voluntary muscles 35, 159 slight hage, treatment of 105
Wall, to cross with " and hremorrhage 92 , stretcher 224 II 6
Warmth 65 by bite of rabid "
Water, sterilisation of 94 animal 267
Windpipe .. 69 " by bite of veno" compression of 73 mous snake .. 264
Wound 43,92, !I8, 13 2 " varieties of 92 " of abdominal wall 105 Wrist, bones of .• ... 30


