
4 minute read
BREAST
Breast Thermography Redefining Early Detection
by April Beaman
Advertisement
During the month of October, pink ribbons and an assortment of pink clothing and paraphernalia have a singular meaning to most women over age 40: schedule an annual mammogram. For all women, breast health is important, as every woman living today has a one in eight chance of developing invasive breast cancer in her lifetime. This makes screening for breast abnormalities especially important. Current methods used to detect breast cancer depend primarily on a combination of physical examination and mammography. While this approach has become the mainstay of early breast cancer detection, mammography is not the only method of detecting breast abnormalities. Since the prevention of breast cancer has not yet become a reality, every effort must be directed at detecting breast cancer at its earliest stage. When breast abnormalities are detected early, the survivability rate is up to 100%. Since most tumors take years to grow, the earliest indication of an abnormality is needed to allow for the earliest possible intervention with the least invasive treatments.
What Is the Current Definition of Early Detection?
According to traditional screening methods such as mammography, early detection is the discovery of a tumor large enough to be detected by an x-ray. Studies have shown that by the time a tumor reaches this size, it has in fact been growing for years. Is this early enough detection?
Identifying Reversible Risks
Imagine a screening tool that could detect the changes that occur in the breasts before a tumor is seen or felt in its place? Is there a way to see physiological changes BEFORE an actual tumor forms? Breast thermography is a screening tool that can detect abnormalities that may lead to cancer. It can also aid in the detection of future risk factors years before they may be found by other screening methods. Consider that if breast changes and risk factors were found early, they could be reversed by making dietary changes, removing toxins and naturally balancing hormones.
A 50-year History and FDA Clearance
Breast thermography has been around for more than 50 years. It is a non-invasive, radiation and compression-free imaging procedure that has been FDA-cleared since 1982 as an adjunct screening method for breast cancer. A medical infrared camera and a sophisticated computer are utilized to convert infrared heat emitting from the surface of the skin into electrical impulses that are visualized in color. The spectrum of colors indicates an increase or decrease in the amount of infrared heat or temperature variations, also known as “hot or cold spots” on a thermogram (thermal images). These temperature variations may be among the earliest
What is Breast Thermography? How is It Redefining Early Detection?
Breast thermography is different than other imaging tools; it is a test of physiology. It detects subtle underlying chemical and
Y
CM
nervous system signals in the body. The infrared camera detects
MY
these changes by measuring heat on the surface of the body. It can CY
provide an indication of inflammation, lymph activity, abnormal
CMY
physiology and vascular activity that is indicative of dysfunction and may lead to breast cancer.
K
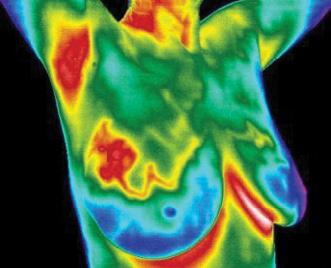

Thermography is based on the principle that blood vessel activity is almost always higher in pre-cancerous tissue and the area surrounding a developing breast cancer than in healthy breast tissue. This process,
Normal symmetrical blood vessels known as neoangiogenesis, is the formation of new blood vessels to supply nutrients and support the growth of cancer cells. The activity of these newly formed vessels and increased blood flow produces measurable amounts of heat, and an increase in surface Activated blood vessels right breast temperature of the affected regions. Additionally, the activated blood vessels have a distinct appearance that a medical, infrared camera can detect. Breast thermography has more than 800 peer-reviewed studies, involving more than a quarter of million participants over the past 30 years. An evaluation of these studies revealed that breast thermography has up to a 94% sensitivity rate for detecting early changes in the breast tissue that may possibly lead to cancer. In conclusion, the addition of thermography to the front line of early breast cancer detection brings a great deal of good news for all women. It has proven to be a valuable screening tool for women of all ages, with all breast types including dense breast tissue, fibrocystic breast tissue, implants, inconclusive mammograms, and high risk and breast cancer survivors. Thermography can also help fill the gap for younger women, especially those under the age of forty, where currently there is no breast screening methods advised as well as expecting women.
April Beaman, RDH, CTT, is a certified thermographic technician, certified by the Professional Academy of Clinical Thermology, and a professional member of Breast Thermography International. Beaman has worked in the wellness industry for over 15 years and provides thermography screenings and wellness support for both men and women. She is the owner of Farmington-based CT Thermography. For more information or to set up an appointment, connect at 860-415-1150 or CTThermography.com. See ad on page 7.
Maintain your youth with Homeopathic HGH Transdermal Gel Maximum Strength Somatropin
Unique and affordable alternative designed to support your pituitary gland! Usage may • Improve Bone and Joint Health • Improve Sleep • Increase Muscle and Reduce Fat Contact Shirley R. Bloethe 860-989-0033 or www.PassItOnLLC.com
Final Journey, LLC (Pet Euthanasia Service)
Kristen Klie, D.V.M. and Associates
(203) 645-5570 www.finaljourneyllc.com
Professional Printing Reliable Customer Service
594 Blakeslee Blvd. Dr. W. • Lehighton, PA 18235 P: 800.443.0377 - Ext. 3104 • C: 570.606.6975 E-mail: mgriffith@tnonline.com www.tnprinting.com







