
11 minute read
THE SILENT PANDEMIC
The Silent Epidemic of Lyme Disease Understanding Risks, Infections and Treatment
Think of Lyme disease as a silent pandemic. The CDC reports there are 300,000 new cases every year in the US, while other estimates put the number much higher. More than 80 countries have reported cases of Lyme disease. Testing is unreliable, there is no human vaccine available and while it does not spread through casual human-to-human contact, it can spread from pregnant mother to fetus and may be sexually transmitted. It was the fastest growing infectious disease in the US and Europe prior to the COVID-19 outbreak, is grossly underfunded compared to other diseases and is underappreciated by the “conventional” medical community. Connecticut, the epicenter of Lyme disease since the 1970s when it was first identified, continues to suffer the worst of it.
Advertisement
Connecticut at High Risk
Data in a recent report from the Connecticut Agricultural Experiment Station (CAES), with funding from the Centers
by Keith Yimoyines
for Disease Control and Prevention (CDC), indicates that 2019 was a particularly bad year for ticks across the state. Over 2,500 ticks, including 2,068 deer ticks (Ixodes scapularis) and 467 American dog ticks (Dermacentor variabilis) were collected, and all female deer tick samples were tested for several pathogens that cause disease in humans. The results were alarming, and experts warn that a mild winter can contribute to a larger boom in the tick population, so 2020 potentially could be a more active year. Out of the adult deer tick samples tested, 46% carried Borelia burgdoferi (the bacteria that causes Lyme disease), 13% were positive for Babesia microti (Babesiosis), 9% for Anaplasma phagocytophilum (Anaplasmosis), 2% for Borrelia miyamotoi (tick-borne relapsing fever) and 1% for Powassan virus. Given the prevalence of disease-causing microbes in our tick population, first-line prevention of Lyme disease requires vigilant tick-bite prevention. Avoid wooded, shaded or bushy areas and tall grasses. Wear light-colored clothing and tuck your pants into your socks. Use a tick repellent, of which there are many—both chemical and natural—on the market. Check your clothes and body thoroughly for ticks, including your hair and skin-folds. Washing clothes in hot water or putting them in the dryer on high heat for 10 or more minutes will kill ticks.
Why Antibiotics Don’t Always Work
In the ideal situation, a person bitten by a tick and infected with Borrelia burgdorferi displays the common Lyme disease symptoms, including bull’s eye rash, headache, joint pain, muscle pain, fever and chills. That person would be promptly treated with a proper course of antibiotics and recover with no lingering effects. An integrative approach, incorporating herbs (astragalus is particularly helpful to enhance the immune response) and diet and lifestyle changes (a whole food, antiinflammatory diet, restful sleep and stress
management) will increase the chances of a speedy recovery. In our less perfect world, tick bites often go unnoticed. Only about 30% of people infected get the tell-tale bull’s eye rash, and symptoms range widely from person to person. This predicament leads to delayed or missed diagnosis and the potential for the bacteria to persist in the body or cause lingering effects due to the highly inflammatory state caused by the infection.
Persister Bacteria and Biofilms
Borrelia burgdoferi has a particular ability to change its genetic expression as its environment changes. The bacteria can respond to changes in temperature, pH, nutrient content and changes in the host’s defense. A 2019 study in the journal Parasites and Vectors examined “persister” bacteria that can evade antibiotics, and potentially cause long term complications for patients, even after Lyme disease treatment. Most concerning, the Lyme bacteria has shown a better ability than other infections to resist antibiotic treatment. Under pressure from antibiotics or environmental changes, the Lyme spirochete (the common corkscrew shape) can change to a less mobile, round body (cyst form) and other forms, making it less susceptible to antibiotics. After antibiotic treatment has ceased, the round bodies can revert back to the spirochete form. Even in the round body form, Borrelia is still able to infect the host, and reversion to the spirochete form helps explains the high frequency of antibiotic treatment failure. Other studies have shown that round bodies themselves develop resistance to multiple antibiotic agents. Doxycycline, the most commonly used antibiotic in early Lyme disease treatment, was shown to reduce spirochete forms by about 90%, but doubled the number of round bodies.
Borrelia burgdorferi can also form colonies or biofilms in response to pressures, making it more difficult to eradicate. Biofilms, which are formed by most bacteria (for example, the plaque on your teeth), are sticky tangles of sugars and other substances that provide protection and community, facilitating the transfer of oxygen and nutrients, and making individual bacteria less susceptible to treatment. Five common antibiotics researched only reduced biofilm formation by 30 to 55%, and a majority of those biofilms contained the viable spirochete form of Borrelia. Prior studies have established the utility of specific antibiotic combinations and stevia leaf extract to break down biofilms with success, with more research ongoing.
Lyme Treatment Demands an Integrative Approach
The most important factor to consider in Lyme disease treatment is that Lyme is a multi-system infection. It can affect joints and connective tissue, the brain and nervous system, the heart and cardiovascular system, the gastrointestinal system, the thyroid gland, adrenal glands and the rest of the endocrine system, and on and on. To complicate the picture, Borrelia rarely travels alone. Co-infections such as Babesia, Anaplasma, Ehrlichia, Bartonella, and co-existing conditions like viral infections, heavy metal or environmental toxicity, bad bacteria and yeast in the gut, disturbances in the balance of beneficial bacteria (potentially caused by antibiotics), mold toxicity, and nutrient deficiencies make Lyme disease one of the most challenging conditions to treat. For patients with persistent symptoms, this is not a one-infection-one-antibiotic solution. A Lyme and tick-borne disease-literate practitioner works with their patient to establish which co-infections are present, which organs are affected and which complicating factors need to be addressed. The goal of treatment should be to return the body to equilibrium, limit the inflammation caused by Lyme and eradicate the underlying infections.
Dr. Keith Yimoyines is a licensed naturopathic doctor who has been practicing in the state of Connecticut since 2011, with a focus on Lyme and tick-borne diseases. He recently joined the team at Tolk Chiropractic & Wellness at 102 Hopmeadow St, Weatogue. For more information or to make an appointment, call 860-651-3521 or visit TolkWellnessCenter.com.
ANSONIA NATURE CENTER
104 acres of wooded hills and grassy fields, miles of nature trails, streams, a two-acre pond, wet meadows, upland swamp, butterfly & hummingbird garden, woodland wildflower and fern garden, community gardening, childrens’ playscape, visitor center, animals & nature exhibits, classes and more!
(203) 736-1053 AnsoniaNatureCenter.org


LYME DISEASE Pitfalls of a Broken System
by Paula Jackson Jones
When it comes to Lyme disease, there are many pitfalls. Often, we are blinded by trust or our desire to feel better, so we don’t see things as they are until we look back. Sometimes we have no idea that the medical providers we trust don’t know what we’re experiencing, let alone how to properly treat it. Patients face so many hurdles when it comes to diagnosing and treating Lyme disease. Where tick-borne disease is concerned, we have a broken system. Given what we’ve been experiencing the past few months with the novel Coronavirus, this concept may unfortunately feel more “A search for truth seems to me to be full of pitfalls. We all have different understandings of what truth is, and we’ll each believe—or we are in danger of believing— that our truth is the one and only absolute truth, which is why I say it’s full of pitfalls.” ~ Jocelyn Bell Burnell familiar to some of you now, while others who have already been dealing with Lyme may have wearily recognized the problems as more of the same.
Pitfall #1: Physician Knowledge
Knowledge and experience are all over the map, and many providers may hold fast to their beliefs without considering the opinions of their patients and other providers. Many patients, who receive inconclusive diagnoses, are left wondering if they need to find a different provider, one who will treat their infection properly. In truth, not all medical providers are knowledgeable about tick-borne disease. Some still use outdated protocols that science has proven ineffective.
Pitfall #2:
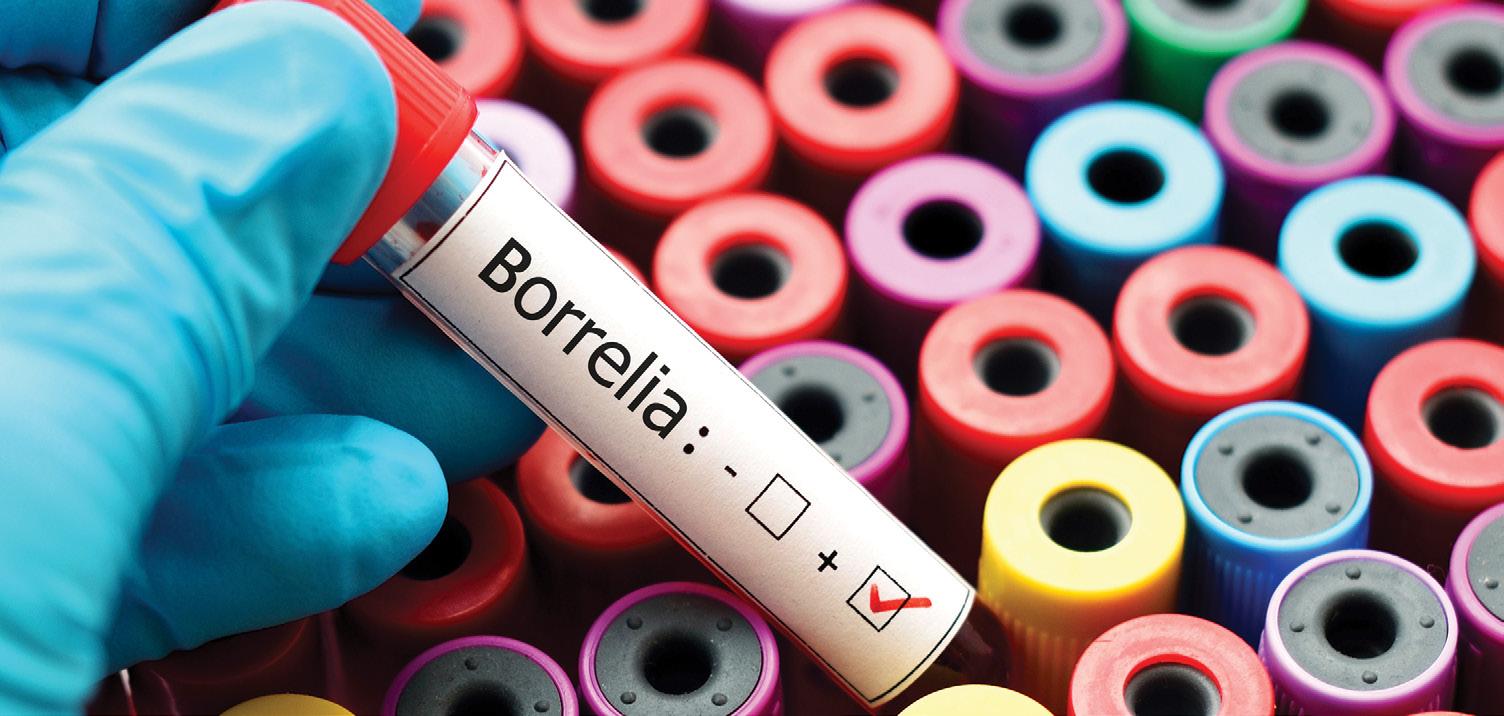
What are you treating? If you don’t know what you have, how can your provider possibly treat it? Many doctors give their patients one-size-fits-all diagnostic tests and treatment. But as leading pediatric Lyme specialist Dr. Charles Ray Jones says, “If they are not looking for it, they won’t see it.” In some cases, unreliable diagnostic tools are still being used because most medical providers think that they can use one test for all tick-borne diseases. Rather, each tick-borne disease has its own test and its own treatment. The ELISA and Western Blot tests only identify one strain of Borrelia (Lyme disease), but there are multiple strains. Additionally, some tick-borne diseases initially present a certain way, and while staying married to the idea of a tick bite (or the presence of a tick bite), patient and providers automatically think it’s Lyme Disease. In the author’s home state of Maine, Relapsing Fever looks like Lyme and acts like Lyme, but the test for Lyme is always negative. Some providers will treat it, others will not, and all the while, the patient remains sick with a tick-borne infection that no one can name.
Pitfall #3
Even when a patient does receive a clear, accurate diagnosis, they may not be able to afford to treat it. Insurance companies are directed on treatments and coverage by various governing entities. If a medical provider tries to operate outside those boundaries, claims are denied, and the patient pays out of pocket until they no longer can. Then treatment stops or they self-medicate in whatever manner they can afford, which is both ineffective and unsafe.
Pitfall #4
The following statement will not be pleasant to read: There is no test that proves that you are better, and any provider that runs a follow-up ELISA or WB following an antibiotic regime does not fully understand tick-borne disease. The ELISA and WB are antibody tests. Antibiotics suppress your immune system and, therefore, when taking them, the body won’t produce antibodies. So an antibody blood screening immediately following a round of antibiotics will almost always produce a negative result even in the presence of an active tick-borne infection. Early infection—as early as 48 hours post-tick-bite—requires a PCR test (like a DNA test) that will detect the most miniscule cell of infection. Medical Diagnostic Labs (MDL) offers both the PCR test as well as the antibody test that is highly recommended at the six-to-eightweek point (without antibiotic use). Most Lyme-literate providers offer these tests, and the good news is that MDL accepts all insurances including Medicare. More good news? As a patient, you have the right to determine where your bloodwork goes, so when suspecting a tick-borne disease, you should choose a lab, like MDL or Igenex, that has over 20 years of experience dealing with tick-borne infection.
Pitfall #5
There is a saying in the Lyme community that “you won’t get it until you get it,” meaning you won’t fully understand how devastating a tick-borne disease can be until you experience it first-hand as a patient or caregiver. The many misdiagnoses, the treatments that fail to get you better, the denial letters from your insurance company refusing to pay for treatment, arguments with your spouse on how to afford treatment, the lack of support from friends and family that walk away— it unfortunately needs to be experienced to truly be understood. These are the realities that patients with tick-borne diseases face every day. They wake not knowing if they can make it to work, stay at work, if they will continue to have a job, if their medical provider will refill a prescription and if their insurance will cover it. They wake to find relationships torn, friendships strained, their children ostracized at school and notices of debt collection in the mail. But there are nuggets of hope, stories of inspiration, messages to hang on to, if patients can find advocates, good information, and a supportive community. Recovery is possible.
Paula Jackson Jones is the president of Midcoast Lyme Disease Support and Education, the 2018 co-chair of the Access to Care Services and Patient Support subcommittee of the Federal HHS Tick-borne Disease Working Group, the Maine partner of the national Lyme Disease Association, member of Maine’s CDC Vector-borne Workgroup and is active in Maine’s Lyme legislation. You can reach her at paula@mldse.org or visit MLDSE.org.
GROW Your Business







