Newton-Wellesley

Beyond postpartum depression
Dedicated to emergency medicine
Elevating diabetes care
“Postpartum depression is treatable, and we have many resources and strategies to help. You will get better.”
Buffy Sheff Ross, MSW, LICSW






Beyond postpartum depression
Dedicated to emergency medicine
Elevating diabetes care
“Postpartum depression is treatable, and we have many resources and strategies to help. You will get better.”
Buffy Sheff Ross, MSW, LICSW




When new moms feel persistently sad, anxious, or alone, getting the right help is vital—for themselves and their babies. Learn how thousands are finding hope and healing.
“Being a new mom of two is great, but it’s very stressful… I won’t lie,” says Mandi. Two and half years after giving birth to her first daughter, her second arrived in midMarch 2024. “Nights are especially hard with feedings every two to three hours.” Even with great support from her husband, Dan, and both of their families, having two little ones relying on her for everything fuels fear and anxiety at times.
After both births, she faced the added challenge of having her newborns arrive early and needing to spend time in the Special Care Nursery at Newton-Wellesley Hospital. While the nurses were wonderfully supportive,
“it was really sad, difficult, and stressful to have to drive home every night without our baby,” Mandi recounts.
Looking out the car window, she’d think about their baby alone, her tiny chest rising and falling, her impossibly small fingers curling and uncurling in the air.
Once their new baby came home this spring, along with the anxiety of caring for her, “I had the constant worry about her sister getting enough attention and love and not feeling displaced.”
Thankfully, Mandi realized she didn’t need to face her fears alone.
“Buffy has taught me how to give myself a bit more grace, to trust myself. Who knew how powerful that permission could be.” Mandi, a new mom receiving postpartum support
During her pregnancy, she sought help from Buffy Sheff Ross, MSW, LICSW, through the Perinatal Mood and Anxiety Disorder Initiative at Newton-Wellesley Hospital—something she wishes she had done before and after her first daughter’s birth.
“Buffy has helped me so much with coping skills like deep breathing, journaling, and asking for—and saying yes to— help from my support network. She is incredibly open and real. She tells it like it is. ‘Mandi, what’s going on?’ she’ll ask. She’ll dig in and we’ll figure it out together.”
“Buffy has taught me how to give myself a bit more grace, to trust myself,” she says. “Who knew how powerful that permission could be?”
The myth of motherhood
Look at pictures, movies, social media. Over and over, we’re bombarded with images of a new mom, blissfully nursing her angelic baby in a perfect, pastel-decorated nursery. Sure, there are many heart-expanding moments
of new motherhood, but for some, they can also seem few and far between during those first long hours, days, and sometimes weeks and months of feeling stressed, afraid, and overwhelmed.
Many women have feelings of sadness in the first few days after having a baby, most commonly due to a drop in hormones. For the 10 percent of new mothers who experience postpartum depression, strong feelings of sadness, anxiety, worry, and tiredness persist, often long after giving birth. Such feelings can make it difficult for some mothers to bond with their baby or to take care of themselves and the baby.
What can make postpartum depression even worse is the persistent shame, silence, and stigma surrounding it.
Postpartum depression is treatable
“Why am I crying all the time? Why am I not bonding with my baby? Why am I afraid to be alone with my baby? Why don’t I trust myself? Many new mothers can feel

“You will get better. You may feel overwhelmed now, but we will get you the supports you need, and you will feel better!” Buffy Sheff Ross, MSW,
LICSW
ashamed of having thoughts and feelings like these,” explains Buffy. “And asking for help seems only to compound that shame and feeling of isolation.”
“But we know that people want to feel better and get better, and our program has seen great response and outcome,” she notes. “Postpartum depression is treatable, and we have many resources and strategies to help.”
Launched in 2019, the clinical social worker’s vital role with new moms grew out of the efforts of the Maternity Services Council, a part of NWH’s Community Collaborative. It exemplifies the Collaborative’s unique community-based approach to addressing the most compelling health needs of our neighbors.
The initiative reflects the Council’s special mission to build awareness and improve treatment of pregnancyrelated depression—and was made possible in large part through the generosity of the Marriott Daughters Foundation.
The Council also sponsors online and in-person support groups for new mothers, led by Angela Rostami, MSN, CNM, a certified nurse midwife. (See story, page 6)
As an active part of the Council, Buffy shares members’ deep interest in improving services during pregnancy and after delivery. Together, they embrace education, advocacy, philanthropy, and targeted programs to best meet the needs of new mothers and families.
As with all of NWH’s efforts to respond to community health needs, relationships are key. The perinatal initiative works hand in hand with physicians and practices in identifying anyone with symptoms of or at risk for postpartum depression.
Obstetricians at three local practices—Wellesley Women’s Care, Newton-Wellesley Ob/Gyn and About Women By Women—ask their patients to complete the Edinburgh Postnatal Depression Scale at four points in time: the initial prenatal visit, the 24–30 week prenatal


appointment, the six-week postpartum visit, and six months after the baby is born. If a mom’s score on the scale is 10 or more—out of 30—she is referred to Buffy.
“Whether a mom is eager to talk to me because she acknowledges her struggles or is reluctant after a referral from her OB, I always say, ‘I’m here—anytime, you are not alone.’ I tell them I’m here to provide therapy, connect them to therapists in the community, support groups and any other concrete need they may have.”
Her clear message to them: “You will get better. You may feel overwhelmed now, but we will get you the supports you need, and you will feel better!”
Here’s what support can look like. Rather than staying silent and alone, a new mother overcomes cultural shame about therapy and seeks help to feel better and stronger. When an expectant mother has all of the emotions from a prior traumatic birth rise back to the surface, she finds support to face her past trauma and let them go. Yet another mother struggles to get out of bed in the morning after the birth of her child. In her case, Buffy asks what she did to cope before the baby. “She was a runner. So, we got her to put her sneakers back on—asked her friends and family to cover her for a small window of time each day to run—and soon her darkness dissipated.”
“Once we get people talking, once they don’t feel alone, they are on the path to feeling better and stronger,” says Buffy.
To date, Buffy and her team have helped more than 2,400 patients. The program—and the broader work of the Maternity Services Council—underscores the hospital’s commitment to the community.
“Our relationships with providers continue to grow, there is more trust as we help more women navigate the sometimes-challenging path of new motherhood, and there has definitely been strong word of mouth,” she notes. “We get women seeking our help from all over, not just those in our backyard. We know that what we are doing works and mothers are getting the assistance they need.”
As part of her role, Buffy also provides resources and strategies for mothers who may have trouble conceiving, have miscarried or had a stillbirth, or who had to terminate a pregnancy because of anomalies.
“There can be a lot of loss in the OB world, but there is also a lot of healing and joy,” she reflects. “I love what I do. People will thank me for reaching out, for helping them through a difficult time. In getting to help all these mothers and families, I think we are the lucky ones.”
“Give yourself grace and ask for help. Trust your gut. You can do more than you think you can. Listen to your baby and yourself; you will teach each other. You know how to do this!”
Those are just a few of the nuggets of advice that Angela Rostami, MSN, CNM, gives to mothers in her postpartum support groups. A certified nurse midwife, she also brings to the role the perspective of working in Labor and Delivery at Newton-Wellesley.

“What I love about our support groups is getting to see the growth,” she reflects. “You see moms emerge from feelings of unsteadiness and go on to give advice and anecdotes to the newer moms who join them.”
“I may initiate a topic, but the mothers really lead the groups and support each other through the collective insight of their experiences,” she adds.
Mothers join her groups at different times—while pregnant, still in the hospital with a new infant, six months out and still struggling, or after having a third child and needing a new layer of support.
Topics of conversation can run the gamut from how to cope with guilt around not bonding with their baby, to how to ask for and accept help, to how to handle the fear of returning to work.
“Recently, we had a new mom who was really struggling with the idea of leaving the house. She had so much fear and anxiety around driving alone with her baby, keeping him safe outside the cocoon of home,” says Angela. “Another mom who was attending again after the birth of her second child jumped right in to help. She had had the same fears after having her first child. The group had helped her take baby steps—sit
“The mothers really lead the groups and support each other through the collective insight of their experiences.”
Angela Rostami, MSN, CNM
Sponsored by NWH’s Maternity Services Council, the support groups meet twice a week online and monthly in person at the Weston Public Library. They also have a robust WhatsApp community of various chat chains that offers resources and information about meet-ups in various neighborhoods so mothers can get out of the house for a coffee or a walk and feel understood, supported, and heard by their peers.
“What I see most with mothers who are struggling after their baby’s birth is a deep feeling of lack of control,” Angela says. Without the right support, “this can spiral into anxiety and depression, which in turn can feel like a painfully stuck place.”
in the back yard with baby, sit in the car with baby, and so forth—until she had the confidence to take that first drive alone with her newborn. Just listening to the veteran mother, you could see relief and hope spread over the new mom’s face.”
Angela reminds her new mothers that there is no one correct way to mother.
“Every family unit—every mom, baby, partner—is unique,” she says. “I love working with these moms; they are strong, and they empower each other, and in so doing, themselves.”


In a time of unprecedented demand for emergency care, our ED staff is rising to the challenge. Driven by passion, the team now sees more than 75,000 patients annually.
“For the first time in my career, we had to worry about our own safety…the team didn’t miss a beat. Everyone stepped up.” David Huckins, MD, Interim Chair, Department of Emergency Medicine
To understand the capacity issues facing the Emergency Department today, “the story arc begins with COVID,” reflects David Huckins, MD, MBA, Interim Chair.
Flash back to February 2020, and Newton-Wellesley’s ED saw 165 patients a day on average. When the first wave of COVID hit that spring, volume dropped 40 percent before bouncing back a year later.
Ever since, “the increase has been unrelenting,” he says. “Over the last two years, volume has continued to build and build.”
Across his 27 years on the ED staff, Dr. Huckins has held many different roles, directing everything from EMS to research to operations. From his earliest days in emergency medicine, like many in the field, he’s appreciated how “you never have a day that you know what will happen.”
Yet nothing prepared him for the pandemic. “For the first time in my career, we had to worry about our own safety,” he shares. “Never before had I dealt with my life being in danger.”
Amid a 100-year crisis, “the team didn’t miss a beat. Everyone stepped up.”
Increasing pressure
During the post-COVID surge, all has been strained by volume. The ED staff now sees 225 patients per day on average, up by more than 35 percent since pre-COVID. On its busiest day, 256 patients sought care in a space originally designed to accommodate 150.
In explaining the impact, Dr. Huckins turns to science for an analogy: when volume increases in an enclosed space, the pressure increases.
The department has done everything it can to maximize existing space, including creating six pods carved out of space in the waiting area and using 24 stretchers as auxiliary spaces.
He appreciates how several initiatives have helped ease the pressure, such as patient progression efforts to free up beds. Ultimately, a long-term fix to space issues would require expanding the ED.
Whatever the challenge, he takes heart in the “quiet determination” of the ED staff. “Many of us have been together so long. It makes for a team that’s resilient and supportive.”
Putting patients first
Dr. Huckins credits leaders working together across the hospital—and Mass General Brigham—with helping ameliorate the problems. “The cumulative effect shows real results,” he says.
As in all facets of patient care at Newton-Wellesley, emergency medicine benefits from the hospital being part of Mass General Brigham. In January 2022, the system launched its enterprise emergency medicine service, building on a long history of collaboration and coordination across hospitals.
“The systemwide approach puts our patients first,” explains Michael J. VanRooyen, MD, MPH, chief of enterprise emergency medicine for Mass General Brigham. “Working together advances patient experience, quality and safety, and health equity across our hospitals.” It also helps in managing complex issues such as boarding and behavioral health that impact not only NWH but all hospitals today.
NWH plays a key role in the system’s capacity as Mass General Brigham’s second busiest emergency department.
Being there for kids and families
“Our connection with Mass General Brigham has always been there, but it’s grown stronger,” reflects Mollie Lebowitz, MD, NWH’s Interim Chief of Pediatric Emergency Medicine.
“We have the feel of a community hospital that’s very connected to the world around us,” she adds. At the same time, NWH has all the resources of being part of one of the world’s premier healthcare systems. “That’s a very lucky balance.”
Now in her ninth year on the team, she’s part of training a new generation of staff coming on board.
Children and adolescents account for up to a third of ED patients. As in every part of the ED, “our volume has

gone up and up,” she explains. In the winter of 2022, “the huge RSV surge was the worst I’ve ever seen,” she recounts.
The ED staff now sees 225 patients per day on average Up by more than 35 percent since pre-COVID
Children and adolescents account for up to 1/3 of ED patients
Whatever the day’s challenges, her love for patients and families and her wonderfully caring colleagues keep her going. “I’m extremely lucky to have a great team,” she reflects. As part of their community focus, “we have great relationships with the pediatricians in our area,” she adds. “They are wonderful!”
NWH is not only her workplace but also her family’s hospital of choice. “It’s where I brought my own two kids,” she says. (See related story, page 28)
Years ago, in her very first job at a local hospital, Dorothy Smith, RN, “fell in love with the ED.” One of the newest leaders on NWH’s team, she brings 40 years of experience to her nurse director’s role.
She describes the surge in ED volume as a “tsunami.” Among the many impacts of the pandemic, the stress and social isolation has spurred an influx of patients with behavioral health issues (see story, page 11). ED staff often see far sicker patients and, with people living longer, more geriatric patients.
All of this has changed the emergency nurse’s role. A natural team builder and former nurse educator, she sees one of her key goals as training the next generation of nurses.
“Caring for our patients is an honor and a privilege. I really feel lucky to be a part of this community.”
Justine Nagurney, MD, Medical Director, Home Hospital Emergency Care
Drawn to the hospital and system in part by their strength and stability, she appreciates not only the community feel and collegiality at NWH but also having the resources to take care of patients’ needs.
The extraordinary staff keeps her energized. It’s demanding work, even for those who thrive on chaos. Yet what they do can be life-saving. Being there for patients “feeds your soul,” she says.
An honor and a privilege “I work with incredible people,” Justine Nagurney, MD, says gratefully, noting how many have made NWH their professional home. “They’re committed to this place and to their patients.”
She’s approaching year four at NWH, where she serves as Medical Director of Home Hospital Emergency Care. Looking ahead, “the future of medicine is in the community,” she believes. “Newton-Wellesley is unique.” Its values align beautifully with her own belief in prioritizing seeing patients where they are.
“Caring for our patients is an honor and a privilege,” she says. “I really feel lucky to be part of this community.”
In July, Newton-Wellesley will welcome Erin Beaumont, MD, MHCDS, as Chair of Emergency Medicine. In her new leadership role, she will help guide the hospital’s ED in building on its commitment to safe, high-quality, patient-centered care as well as seamless coordination with Emergency Services colleagues across Mass General Brigham. A highly skilled physician, she brings deep clinical knowledge, proven leadership skills, and a passion for community. She joins NWH from the Cambridge Health Alliance, where she has served as site chief at the Cambridge Hospital ED and Somerville Campus Urgent Care.

As the Emergency Department’s specialists in behavioral health, the Psychiatric Triage team has had to rise to its own share of challenges.
At a time of crisis in mental health nationally, having a team of psychiatric social workers embedded within the ED creates a strong resource for patients of all ages.
“We have a great team of very seasoned clinicians,” notes Maureen Lavelle, LICSW, lead social worker. “We’re all working closely together to do whatever we can to get patients the best care.” From her perspective, NWH offers one of the best consult liaison teams across Mass General Brigham.
Elliott Martin, MD, the team’s medical director, echoes her point. When it comes to ensuring patients move on to the right next step, “I can’t say enough about the job they’ve done,” he says. “Hands down, they’re the best.”
The team does an incredible job collaborating both with psychiatrists and the wider ED staff, he adds. At the same time, “this is a very psych-friendly ED,” a distinction that he deeply values.
A decade ago, the hospital’s reputation for providing compassionate care to its most vulnerable patients drew Maureen to NWH. “The ED is like a family,” she reflects. Along with taking care of patients, “we take care of each other.”

Thanks to game-changing medicines and technology, it’s a new world for those with diabetes. Our experts are at the forefront, passionately helping patients lead fuller lives.
“I could go on and on about my team. They’re on the cutting edge. They’re knowledgeable. They’re really smart. They listen incredibly well.”
Joanne Wills, a grateful patient
Joanne Wills didn’t learn she had type 1 diabetes until her early 50s.
Often, people think of it as something surfacing in childhood. In her case, a routine checkup with her new Newton-Wellesley primary care physician led to an antibody test confirming her diagnosis.
Hoping to find care close to home, Joanne sought an appointment at NWH’s Diabetes Clinic. “I feel very lucky and grateful that Dr. Steppel-Reznik had an opening,” she says. “I see it as if someone was watching over me.”
Today, the Needham resident sees both Jeanne SteppelReznik, MD, Chief of the hospital’s Endocrinology and Diabetes Division, and Elyse Rayney, CNP, the clinic’s lead nurse practitioner. “I rely on them,” she says.
For Joanne, her own family history made the initial diagnosis unnerving. She had lost her older sister at age 51 after having lived with complications related to diabetes since her teens. Dr. Steppel-Reznik reassured her of the difference that advances in technology and medication have made—something which Joanne wishes her sister could have benefited from.
“They tell me, ‘Everybody’s diabetes is different, and in time you’ll know your diabetes best,’” Joanne notes. “That resonates with me.”
“I could go on and on about my team,” she adds. “They’re on the cutting edge. They’re knowledgeable. They’re really smart. They listen incredibly well.”
Importantly, “you’re going to people who truly care.”
When Dr. Steppel-Reznik first arrived at NewtonWellesley in 2005, she was only the second full-time endocrinologist on staff. They had one diabetes educator and one dietitian, based in a different location.
Today, as division chief, she oversees a bustling clinic specializing in diagnosing, treating, and managing a wide range of endocrine conditions, including not only diabetes but also thyroid disorders, osteoporosis, and more.
Her team now consists of seven endocrinologists as

well as a highly trained and experienced team of nurse practitioners, nurses, and registered dietitians.
“We’ve grown into a very strong division,” she notes proudly. With a focus on individualized care, “our staff stay up to date with the latest breakthroughs and offer patients the best choices for them.” A recent move to a new location within the hospital enabled staff from across the division to be in one space, taking advantage of their interdisciplinary expertise. The combination of the clinic’s team, technology, and new home position them well moving forward.
NWH has continually added to a growing array of services. The American Diabetes Association-certified Diabetes Management Program now provides individual assessments, group classes, and support groups for a large outpatient diabetes population. Over time, the division has also created a thriving nurse-practitioner based service for inpatients with diabetes.

From the start, Dr. Steppel-Reznik realized “community medicine is where my heart is.” Looking to the future, she’s always hoping to be able to provide patients with more and better options. With the growing understanding of connections between chronic diseases, she envisions more comprehensive care—and work toward prevention— that bridges fields of medicine.
Like Joanne, Dr. Steppel-Reznik has her own family history with the disease. She often shares with her patients the story of her mom’s experience after being diagnosed with diabetes at age 9 in the 1950s.
The perspective influenced her path in medicine and deepens her understanding and compassion for patients and families. Put simply, “it makes me a better doctor,” she says.
For patients like her mom, it was a very different time with far fewer options. When her brother was diagnosed with diabetes just a decade ago, the field had vastly changed.
Today, “it’s not an easy disease but it’s much easier to manage the day-to-day ups and downs and allow people to live their lives more fully,” Dr. Steppel-Reznik reflects. She’s grateful for the ongoing advances both in
“We’re at the forefront, and we’re giving people a menu of options to make sure they have access to the latest and greatest.”
Elyse Rayney, CNP
technology and medication and what they have meant for millions of patients and their families.
Through the years, she’s seen massive change in the understanding of type 2 diabetes, for example. “We’re fortunate to be blessed with new medications, which has led to tremendous improvement in treatment,” she notes. Every year they get better access to data through advances in the technology of devices. “Literally 24/7 we can monitor levels,” she adds.
At same time, the need for care locally and nationally is on the rise. In the last two decades, the prevalence of diabetes has increased at an alarming rate among US adults ages 18 or older. By 2022, nearly 30 million people had been diagnosed with diabetes, and an estimated 8.6 million others had yet to be diagnosed, according to the Centers for Disease Control and Prevention. An estimated 97.6 million US adults have prediabetes.
Embracing technology
“Diabetes impacts everyone from all walks of life,” says Elyse Rayney, CNP. She originally developed her own passion for diabetes working in research at Massachusetts General Hospital. A desire to work more directly with patients led her back to school to become a nurse practitioner.
Thankfully, “there’s now so much creativity in how we can manage diabetes,” she says. “There are so many aha moments where patients see how small changes can make a huge difference.”
Like Dr. Steppel-Reznik, she also appreciates how far the division has come. When Elyse first came on board, she was the team’s only nurse practitioner; now she’s one of four. Ever since, “I’m proud of how we’ve embraced technology and stayed ahead of it,” she says. “We’re at the forefront, and we’re giving people a menu of options to make sure they have access to the latest and greatest.”


By 2022, nearly 30 million people had been diagnosed with diabetes An estimated 8.6 million others had yet to be diagnosed
An estimated 97.6 million US adults have prediabetes
Source: Centers for Disease Control and Prevention
“There are so many aha moments where patients see how small changes can make a huge difference.”
Elyse Rayney, CNP
In an “ever-changing medication and technology landscape,” many things constantly need to be re-evaluated, she explains. Everyone on staff needs to be nimble.
The advent and evolution of continuous glucose monitors, for example, has been a “game changer.” Patients can see information in the moment as well as see how changes in behavior impact their levels. “It’s been a huge shift in the diabetes community and how we give guidance to our patients,” she says.
She’s excited to see where the field goes next. Day to day, “our team and our patients keep me energized,” she says. Importantly, every patient is an individual. The team works collaboratively with them to achieve their goals. “When you see someone succeed, it’s a great feeling.”
“What excites me is how we continue to add elevated services for our patients,” says Kim Sabada, MS, RDN, CDCES, the lead registered dietitian and American Diabetes Association (ADA) coordinator for the practice.
Along with seeing patients individually, she also helps to lead the ADAcertified program of group classes, educating patients on the day-to-day management of type 2 diabetes to allow them to live healthier, happier lives. During the pandemic, the team pivoted to virtual classes. “Our enrollment has exploded,” she says.
“What excites me is how we continue to add elevated services for our patients.”
Kim Sabada, MS, RDN, CDCES

What started as a three-part series now includes optional fourth and fifth classes. Participants are in the same cohort for their first three sessions, getting to see familiar faces and become more comfortable talking with one another.
Two years ago, Kim began offering a free, monthly support group. She’s there to moderate. Sessions typically draw 15 to 20 people, and it’s been beloved by those who attend.
The field of nutrition is ever changing, ever growing. With social media, “what’s also changing is people’s exposure to misinformation,” she adds. She strives to make sure that she’s pointing patients to good information.
One misconception: “they think that I’m here to tell them
what they can’t eat,” she says. She stresses “getting out of this all or nothing mindset.” For her, it’s about moderation. “You have to meet patients where they are,” she adds. Her key questions: How long can they sustain this? How do we not only manage your diabetes but also manage your quality of life?
Echoing Elyse’s point about continuous glucose monitors, Kim appreciates how they allow her patients to see very tangible data: “when I eat X, this is what happens.” They can feel the highs and lows with their blood sugar.
As much as she recommends that people with diabetes take advantage of newer medications, they’re not a substitute for getting nutrition and eating an adequate diet, she believes. Nine times out of ten, having good food habits also makes a medication’s side effects more manageable.
Now in her seventh year at NWH, “it’s definitely home for me,” Kim says. Both for herself and her patients, she finds the division’s team-oriented approach rewarding. She loves seeing the collaboration in action.
“Always trying to up my game”
“Our patients make us the best doctors,” Jeanne Steppel-Reznik likes to say. For her, being able to know many of her patients by following them throughout their lives adds a special dimension to her own work.
For Joanne, one of Dr. Steppel-Reznik’s hundreds of grateful patients, it’s now been seven years since diagnosis. She’s continually seen advances in the technology. “The progression in such a short time has been phenomenal.” She initially took advantage of a continuous glucose monitor. “Now I’m on a pump [for the delivery of insulin], which has been life-changing.” Hers is a wireless system, already in its fifth generation.
As Joanne recounts her experience, she notes that “today is a big day.” She’ll begin a new quick-acting insulin suggested by her team.
“They’re always trying to up my game,” she adds. “If they can make my life easier, it’s a win.”
Established in 2023, the Welsh-Loveman Family Fund for Diabetes and Endocrinology has already made a difference for patients by making possible two very important types of technology.
First, the new fund has enabled the purchase of a retinal camera, allowing patients to have images taken of the inside of their eyes as part of their visit and read by ophthalmologists. Going forward, having the technology on site will enable patients to be routinely checked each year, easing access to screening and early detection of diabetes-related eye conditions.
Second, the family’s gift has provided funding for a point-of-care hemoglobin A1C machine. This device will allow staff to get data on patients’ A1C levels as part of a routine check of vital signs.
Again, having that technology at the clinic will provide the team with the benefit of knowing more information right at the time of the visit. It will increase productivity dramatically.
Dr. Steppel-Reznik and her entire team are immensely grateful to Kathleen Welsh and Gary Loveman, PhD, for their amazing generosity. “Every year, there are new recommendations about diabetes-related technology and medication,” she reflects. For the sake of their patients, “we try very hard to stay on the cutting edge.”
Along with its timely investment in the division’s capabilities, the Welsh-Loveman Fund provides a wonderful reminder of the power of philanthropy to advance care.

“Every year, there are new recommendations about diabetesrelated technology and medication. We try very hard to stay on the cutting edge.”
Jeanne Steppel-Reznik, MD

In gratitude for life-saving care, a pediatric nurse gives back by running for Team NWH in the Boston Marathon.
Being part of the pediatric inpatient team at Newton-Wellesley, Christine Doherty, RN, loves the sense of purpose. “Everybody comes together in the moment,” she says. “We work together as a team for our patients and their families.”
This year, to support their work, she teamed up with nine other runners—and passionate NWH supporters—in raising funds for Newton-Wellesley through the 2024 Boston Marathon.
For Christine, it was her 16th straight Boston. In training, “on every run, you learn something,” she reflects. Along the way, “it’s amazing to see how far you’ve come.” For her, it’s a path to “finding my best self.”
Ever since she started running fundraising 5Ks after college, she’s been hooked. Running for Team NWH allowed her to contribute to a place that has touched her life in so many meaningful ways.
When she joined the NWH staff just over a year ago, she followed in the footsteps of her mom, who spent 30 years as a pediatric nurse at the hospital. “I feel like I grew up here,” Christine says. “It’s a hidden gem in the community.”
Along with being a source of life-saving care for family members, NewtonWellesley saved her own life, she recounts. In 2018, after being hit by a car while biking during triathlon training, “my orthopedist and hematologist never gave up on my treatment.” The way her entire NWH care team went the extra mile for her inspired her to give back.
Six years later, she still gets emotional as she talks about it. Yet the experience helped her as a caregiver to gain perspective and have more empathy for her own patients.
On Marathon Monday, she proudly crossed the finish line on Boylston Street wearing her Team NWH singlet. Every day, she concludes, “it makes me feel proud to care for and educate my patients so they can reach their own finish line.”

“It makes me feel proud to care for and educate patients so they can reach their own finish line.”
Christine Doherty, RN, pediatric nurse

Congratulations to the 10 dedicated members of Team NWH who ran the 2024 Boston Marathon on behalf of the hospital. Together, they raised more than $115,000 to support expert, compassionate care.
Avner Aliphas, MD
Ray Angelone
Ryan Daly
Christine Doherty
Carly Fay
Andrew Hinman
Mandy Holub
Samantha Newman
Leah O’Neill
Adina Taylor
Thanks, too, to the family, friends, neighbors, and staff who cheered them on at our celebration tent on the hospital lawn at Mile 17.
More than $1 million raised for Community Collaborative
At the 2024 Gala, more than 500 guests celebrated all that Newton-Wellesley means to them and to the communities they call home. Held May 3 at Boston’s Intercontinental Hotel, the event inspired more than $1 million in support of our Community Collaborative. Highlights included Michael S. Jellinek, MD, former NWH president and Collaborative co-founder, receiving the inaugural Community Champion Award, presented by Jack Connors, Jr.













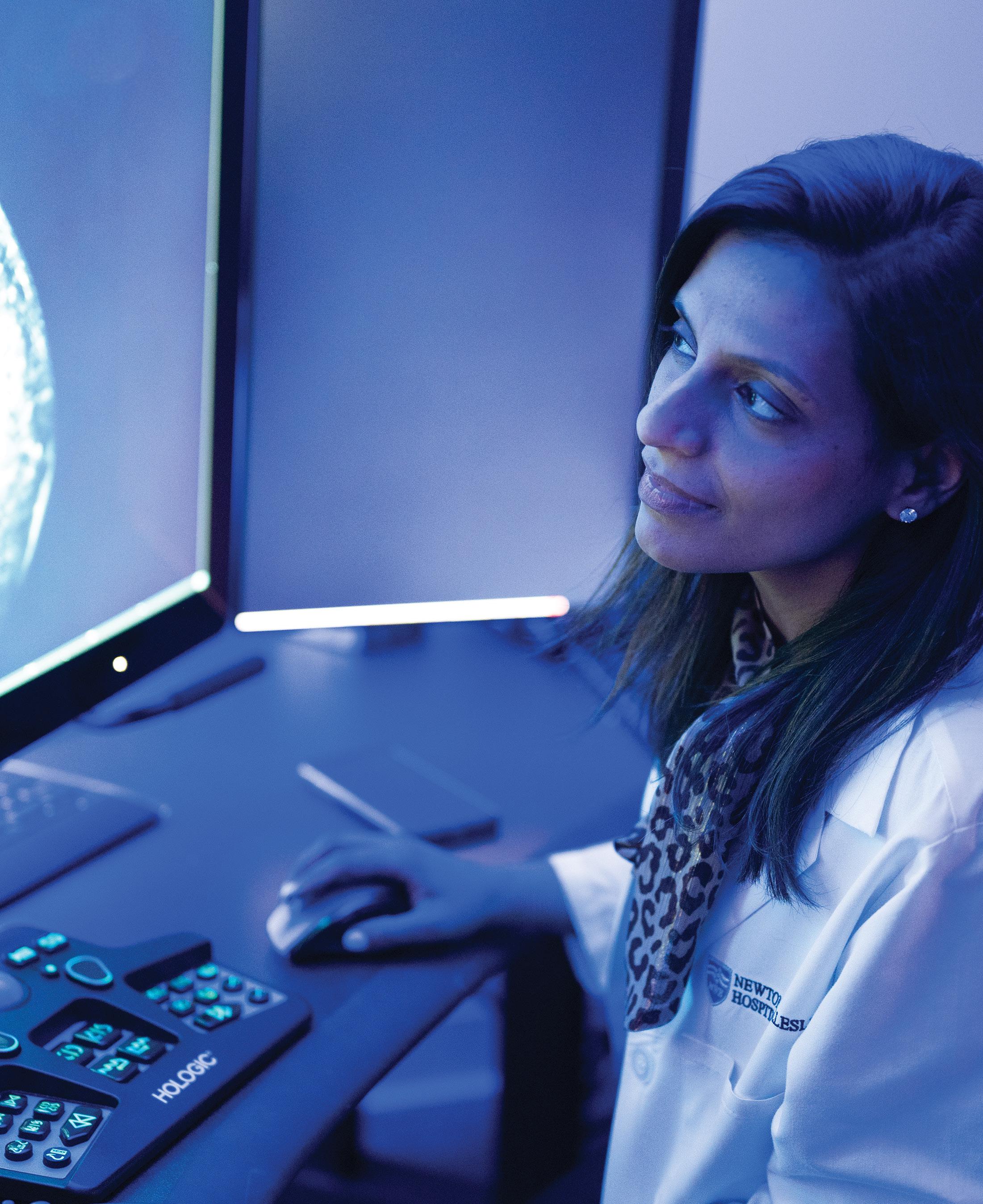
Dolores Manzi will forever have an impact on care, thanks to her thoughtful inclusion of Newton-Wellesley in her estate plans. Her bequest honors her beloved parents, Anthony and Benvenuta, whose own remarkable legacy includes a family of 18 children! She chose to support two areas close to her heart, Maternity Services and Breast Imaging. Generations of patients will be the ultimate beneficiaries.
To learn more about how to include Newton-Wellesley in your estate plans, visit giftplanning.nwh.org.

In a time of escalating needs for youth mental health, a $500,000 challenge grant from an anonymous family foundation has succeeded in inspiring powerful new endowed support of our Child and Adolescent Psychiatry team.
For those leading donors who quickly responded, the 1:1 matching challenge has made their gifts doubly impactful. Together, by investing in our caregivers, programs, and outreach efforts, they are helping to make life-changing treatment a reality for thousands of children and families.
To learn more about other opportunities for support, please contact Jaime Mulligan, Managing Director of Philanthropy, at jmulligan5@mgb.org.
Newton-Wellesley unveiled its new, state-of-the-art MedicalSurgical unit on 5 East during a special ribbon-cutting ceremony on May 17. The 24-bed unit offers the latest innovations in patient care and cutting-edge technology.
It will significantly expand our capacity at NWH and across Mass General Brigham. A testament to thoughtful planning, the project prudently made use of an existing space previously used for storage.
The unit will temporarily house our 6 West team and patients during renovations to that unit. When 6 West reopens, 5 East will formally begin operations as a new unit, playing an important role in mitigating high patient volume.


According to the American Heart Association, 436,000 Americans die from cardiac arrest in one year alone. Cardiopulmonary resuscitation (CPR), especially if administered immediately after cardiac arrest, can double or triple a person’s chance of survival.
As part of Newton-Wellesley’s ongoing commitment to improving community heart health, our Heart Health and Wellness Council has partnered with Natick and Waltham High Schools to equip all students with live-saving skills.
Between the two schools, the Council also donated 24 automated external defibrillator (AED) trainers and two CPR mannequins, and they worked with the AHA to obtain donated training videos.
“By educating more people to use CPR and AEDs, we hope to increase the likelihood that someone will step forward to help in an emergency,” explained Jane Barr, MPH, RD, LDN, Community Wellness Coordinator, who assisted with the training along with Debra Rosenberg, MBA, BSN, RN, Nurse Educator.
In Waltham, the Council collaborated with the school’s Physical Education department to ensure that CPR/AED training is part of the school’s regular curriculum moving forward. Having begun in February, training classes will reach nearly 1,800 students. In May, the Council trained Natick High’s PE teachers to bring the same skills to their 1,600 students, beginning this fall.
3,400 students to receive CPR/AED training at Waltham and Natick high schools
When you give to the NWH Fund, you make a difference every day for our patients, their families, and your community.
By contributing today, you’ll have an immediate, missioncritical impact at a time of so many urgent health needs.
You’ll keep us at the forefront of medicine—helping to build and sustain our world-class team of caregivers, cutting-edge facilities and equipment, and lifechanging community initiatives.
With a gift of $1,881 or more, you’ll be welcomed into the 1881 Pillar Society, honoring the true “pillars” of our community and the year of NWH’s founding.
To give now, visit giving.nwh.org/



Sponsor the NWH Golf Tournament today!
Join us for a day to remember on the links this fall, and contribute to a healthier future for our community and its youth.
Foursomes and sponsorships are now available for the annual NWH Golf Tournament on Monday, September 9, 2024, at Wellesley Country Club.
By participating, you’ll be directly benefiting our Community Collaborative’s Workforce Development Council, including its annual youth summer internships.
To register or learn more, visit the tournament webpage at www.nwh.org/golf.
Students from Waltham High School and the Waltham Partnership for Youth’s Teen Mental Health Alliance joined a select group of NWH clinicians and leaders for a small, intimate roundtable discussion this spring.
In sharing details from the Waltham Youth Risk Behavior Survey, the students impressed attendees with their knowledge of the data, presentation skills, and articulate and candid responses to the many, many questions raised.
“It was empowering to the students as they were very clearly the experts in the room,” reflects Lauren Lele, Senior Director, Community Health and Volunteer Services. She notes proudly that three of the four are alumni of the NWH summer internship program, including the peer leaders from this year and last.
The invite-only event grew out of goals identified by a Youth Task Force, created by the hospital’s Community Benefits Committee in response to the priorities emerging from the most recent Community Health Needs Assessment.
As a Sustaining Partner of WPY, Newton-Wellesley has a longstanding relationship with the Waltham nonprofit. In a new dimension of our active engagement, four WPY students now serve on Councils of the Community Collaborative, contributing their perspectives on both youth mental health and workforce development.


“I feel a deep sense of responsibility to ensure that my institution is living out its values in a meaningful way.”
Vincent Rougeau, JD, member, NWH Board of Trustees
For Vincent Rougeau, the lessons in community engagement started young.
“My parents were teachers and active in the Civil Rights Movement, and they never saw their achievements as essentially for themselves alone,” he recounts.
“They always reminded us of our obligation to give back. And so your education, your job, your accomplishments, your resources, are not just to benefit you. You now have an opportunity to make life better for others as well.”
Through giving back—including as a Newton-Wellesley trustee—he carries their lessons forward.
Today, as president of the College of the Holy Cross, he seeks to lead by example. “I feel a deep sense of responsibility to ensure that my institution is living out its values in a meaningful way,” he says. “And I feel the same for Newton-Wellesley.”
What sets NWH apart
Since moving to Weston a dozen years ago, his family has relied on Newton-Wellesley. As parents of three adolescent boys, Vince and his wife, Robin KornegayRougeau, MD, have gotten to know it well.
From the start, “it surprised us that people didn’t appreciate more how lucky they were to have a hospital of such high quality so close to them,” he notes.
He sees NWH as having all the attributes they’d hope to find in a local hospital: community-centered, accessible, family-friendly, and staffed by kind, helpful caregivers.
After his mother, now in her 80s, moved here to be near them, “having such a fine hospital so close to us has also given her a sense of security,” he adds.
The values we embrace
In his mind, as a healthcare institution, “NewtonWellesley provides one of the most essential things in the lives of all human beings.”
Vince first became involved with NWH while dean of Boston College Law School. Over time, “as options for being more involved emerged, it was important to me to give back in a way that reflected our admiration for the hospital.”
He joined the NWH Board of Trustees in spring 2021. In this challenging time for healthcare, he has gained a deeper perspective on changes spurred by the pandemic—and the powerful benefits of increasing collaboration as part of Mass General Brigham.
From his own experiences, he appreciates the impact on patients and their families. Being married to a Mass General Brigham pediatrician, “I’ve personally seen how the professional lives of physicians have evolved over the last few decades,” he adds.
He sees it as critical that all those we seek to serve feel seen and believe this hospital exists for them. He asks himself, are we doing our absolute best to make sure that the healthcare we give is accessible? Do patients feel treated with dignity, care, and compassion?
“These are values that I know the hospital and the community embrace,” he says.
As a lifelong academic, “It’s been a real gift to be in a position to shape young people and help them chart their future,” he reflects. “I really firmly believe they will help build a better future for all of us.”
On a typical day, “there’s so much excitement and engagement on a college campus, you can’t help but get caught up in the positive energy,” he adds. “And even when things don’t go so well, you realize over time, most of the days are good and the work is valuable.”
He looks at the hospital in the same way. “The work is so important and so many patients are thankful and grateful,” he reflects. “There’s real power in that.”

“Patient care is my passion. I love kids, and I love all aspects of making them better.”
Mollie Lebowitz, MD, Interim Chief, Pediatric Emergency Medicine
Having a continuum of care from birth throughout childhood and beyond sets NWH apart for families, reflects Mollie Lebowitz, MD. Many of her Pediatric ED patients were born at Newton-Wellesley. If a child she sees needs to be admitted, we offer our own pediatrics inpatient unit devoted to their care, unlike many community hospitals. For more on emergency medicine, see pages 8–11.
Newton-Wellesley Hospital Development Office
2014 Washington Street
Newton, MA 02462
nwh.org/giving



“Nurses are the best of the best. They helped me through my toughest times. I cannot say enough wonderful things about them.”