9 minute read
Nursing's next generation
Nurse Residency preps new grads for future at NWH

On her very first day on the Labor and Delivery unit at Newton-Wellesley, Jillian Levesque, RN, remembers feeling instantly at home. Seeing the nurses in action, she thought to herself, “Oh, this is exactly what I want to do.”
It was July 2022. Just having graduated at the top of her class from nursing school, she had seized the opportunity to join the first cohort of the hospital’s brand-new Nurse Residency program.
As the daughter of a nurse, she’d always known the difference that nurses make in people’s lives—and how being a nurse changes one’s own life.
Today, Jillian is one of 73 nurses to complete the program so far—and 104 more are in the midst of preparing to join our family of caregivers. “It’s a special thing to be a nurse at Newton-Wellesley,” she believes. Working nights as a Labor and Delivery nurse, she reminds herself to pause and take in how truly special it is.
For every birth that she’s part of, Jillian puts a bead in a keepsake jar. So far, it’s filled with more than 100 beads, one for each birth story. “In every way, my job is filling my jar,” she smiles to say.
The future of nursing
Having just welcomed its fifth cohort, the Nurse Residency program continues to provide new graduates like Jillian with a yearlong opportunity for intensive experiential learning at Newton-Wellesley.
NWH nursing leaders trace the program’s roots to The Future of Nursing, a landmark report published in 2011. It called for fundamental changes in nurses’ roles, responsibilities, and education nationwide. Residency training was a core educational suggestion for ensuring that nurses were prepared for what’s ahead.
While the report was an impetus for developing NewtonWellesley’s program, “we also did it because it was the right thing to do for our nurses,” notes Lesley Adkison, PhD, RN, Nursing Practice Innovation Leader and one of its guiding forces.


The report was spurred in part by an awareness of shifting demographics and baby boom retirements on the horizon. What it didn’t take into account was COVID, explains Tricia Crispi, PhD, RN, NPD-BC, Nurse Director, Quality, Safety & Professional Development.
The pandemic heightened the sense of urgency, as nurses left their jobs in greater numbers than anticipated. Staffing challenges have strained hospital finances across the country. The Bureau of Labor Statistics projects more than 200,000 annual openings for RNs nationwide through 2031, further highlighting the need for new approaches to recruiting and retaining the workforce of the future.
At the same time, during COVID, most graduates coming out of nursing schools had only limited opportunities at best for clinical experience and senior-level preceptorship.
The first two NWH cohorts began in July and September 2022, while all hospitals were still under pandemic emergency restrictions. The nurse residents came into the world of healthcare at an incredibly challenging time, including an increase in acuity among those seeking care.
All of these factors have made the Nurse Residency experience even more vital—and even more attractive to new graduates poised to begin their careers.
At Newton-Wellesley, the team of nurse educators from across the hospital have nurtured and readied them for what’s ahead. “What the residency does is create a healthy working environment where they know they’re supported,” Tricia explains.
Tara Tehan, PhD, MBA, RN, NE-BC, Associate Chief Nurse, describes it as a clear signal of Newton-Wellesley’s investment in them. Importantly, “an investment in our workforce is an investment in our patients,” she explains.
Providing the best patient care
As the idea for the Nurse Residency emerged, Sharon Keogh, MSN, RN, NPD-BC, PCCN, stepped up to take on the role of director. She came to nursing herself as a second career. With a strong belief in continuous learning, she gravitated to a role of nurse educator.
When she thinks about the nurse residents, “they are our future,” she says. “I want them to take the foundational skills that we’re teaching them and build on them to provide the best patient care.”
Jillian echoes Sharon’s point. From her perspective as one of NWH’s newest nurses, “that’s our priority: to deliver the best possible care to every patient.”
Instilling a sense of the hospital’s distinctive culture starts on day one of the program. “We’re talking about how we at Newton-Wellesley see ourselves and deliver care,” says Tricia.
In the first month, they spend 16–24 hours per week together in training. By month two, they meet for four hours a week and dive more deeply into orientation on their assigned units. By month three, as unit-based learning becomes their daily focus, they meet only once a month as a full cohort.
By the end of the program, 90 percent feel prepared to complete their job responsibilities. At a time when turnover of first-year nurses has been a concern nationally, they stay on in their roles. In the program’s inaugural year, NWH nurse residents had a retention rate of close to 85 percent as compared to 72 percent nationally.
Retention takes “feeding them personally and professionally,” reflects Lesley. As they learn and grow, she envisions cohorts building bonds across the hospital. “We want them to see themselves as change agents in their own right, using their voices to advocate for patients” she adds.
Continually learning
When they begin as nurse residents, “their brains are on fire,” Lesley reflects. “They’re continually learning.”
Tricia sees it as a natural extension of their education in nursing school. While they may have acquired extensive knowledge from coursework, “their education doesn’t stop when they graduate.”
For her part, Sharon values watching them grow professionally.
On their very first day, they’re asked to “tell me something you’ve never done.” It’s a long list. At the start, there are many skills that many have yet to do. That’s been especially true for those who’ve had their nursing education altered by the pandemic.
They each write narratives at three, six, and 12 months, reinforcing the experiential lessons in patient-centered care. By the time of their completion ceremony, they can look back at their narratives to see how much they’ve grown.
For any nurse, the learning never stops. “You’ll always see something different, and you’ll always be challenged,” Sharon says. Developing these clinical judgement skills will help nurse residents rise to the challenges.
Connected forever
As nurses, “we’re a relationship-based profession,” reflects Tara. “Relationships are key.” That understanding shapes the program’s cohort design.
For Sharon, “watching all of the nurse residents build supportive relationships is one of the highlights.”
She enjoys seeing the friendships blossom. When she walks into the Allen-Riddle living room at 7 a.m. for a monthly cohort gathering, she’s struck by the noise level. Everyone is busy chatting and catching up with one another after being busy working on their units. “I see how much they’ve bonded.”
By design, group experiences such as a required quality improvement project add to their bonds. They work collaboratively with other nurse residents on their unit. Their focus can be on anything that is going to improve patient care. “It’s about promoting the health of our community,” Sharon notes.
At the same time, “they’re building the support that every nurse needs,” she reflects.
Day by day and month by month, “they come to know each other,” adds Lesley. Thanks to a strong cohort model, “they’ll be connected forever.”
The best nurses they can be
Having transitioned from the residency’s first cohort to full-time nurse, “I’m still learning every single day,” Jillian reflects. “Part of being a good nurse is knowing there’s always room to grow.”
The residency is a huge learning year. To her, “it’s a time of finding yourself as a nurse.” She remembers how “Sharon and Lesley always told us you are so capable. You are RNs. You earned this. You can do this.”
Sometimes there would be hard days. Throughout, “they instilled confidence in us. They were constant reminders that people have faith in you to do the job well. From day one, we were told that they wanted us to succeed.”
Moreover, Jillian senses that the hospital’s leaders “want this new generation of nurses to succeed.”
From the frontlines of nursing, she sees the enormous need.
Looking to the future, “I think it’s so important that nursing remains a thriving profession, and we give back to our own,” she says. “We should want to invest in them being the best nurses they can be.”


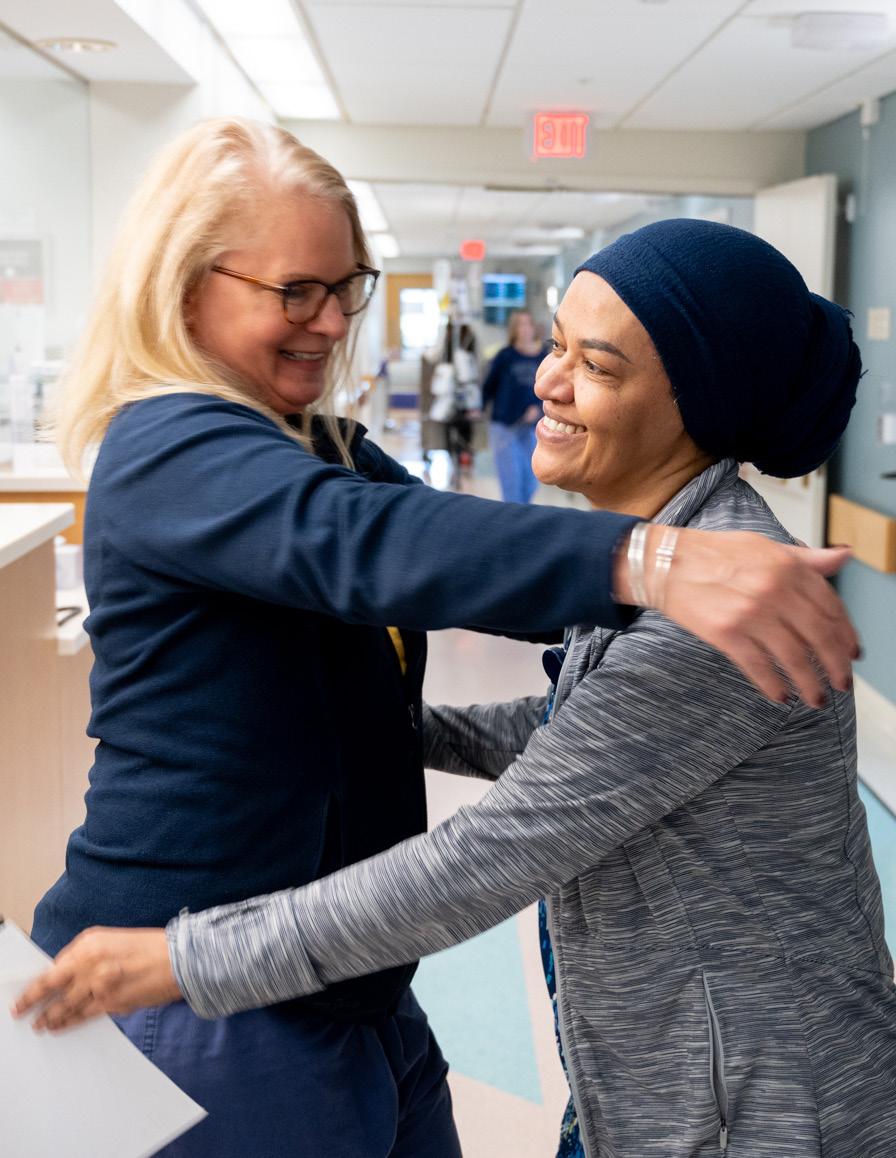
When they start at NWH, each nurse resident is paired with an experienced preceptor. “They all have an RN on their unit who’ll work with them and teach them everything they need to know,” Sharon explains.
Kelly Carter, RN, volunteered to take on the role of preceptor and guide new graduates on the hospital’s 6 West unit for medical/surgical inpatients.
Now in her 22nd year in the field , “I’ve wanted to be a nurse since I was 5 years old,” Kelly says. Looking back on the start of her career, she remembers being precepted for only two weeks. It was a struggle. “I think our nurse residency is such a great opportunity,” she says. “I’m jealous,” she adds with a laugh.
In first trying to help patients, she knows that everything might be new for a nurse resident. “As a preceptor, you have to be in the mindset: I was here once, too.”
One of her nurse residents, Isaac Yi, surprised her with a T-shirt after his closing ceremony, celebrating her as an “Elite Preceptor.” Looking back, “I cherish the time
that I had with Kelly and always remain grateful that she was the one who molded my practice,” he says.
“We were a great match,” Kelly recounts. She valued how receptive he was to learning. Isaac, in turn, appreciated their honest and open communication.
In his first few days on the unit, he did more observing, seeing how she would assess patients and communicate with them. Gradually, he moved to taking the lead on one patient, then two. She oversaw his work and reviewed his notes with him. “By the end, he was running the show,” she says.
Now, Isaac and Kelly work as fellow nurses on the same unit. He sees communication as one of the essential lessons that he’s carried with him from the residency into his day-to-day work.
“When it comes to teaching, it’s not just me, it’s all of us,” Kelly adds. “Every nurse on the whole unit is part of the education. Everyone’s supportive."






