
15 minute read
HEALTHCARE HEROES
HEALTHCARE Heroes Meet the New Jersey nurses who risk their own health every day to help others during the COVID-19 pandemic. By Ronnie Koenig

Julianne Palardy, BSN, RN, CCRN Cardiothoracic ICU RN, Saint Barnabas Medical Center, Livingston Hometown: Essex Fells
Julianne Palardy has been a nurse for 17 years, following in her mother Joanne Anscher’s footsteps, who was also a nurse at Saint Barnabas Medical Center until she retired.
“Nursing has been part of my life since childhood with my mom practicing as a labor and delivery nurse for most of her life,” she says.
Palardy says her mother risked her own health to take care of her granddaughters during the pandemic so Palardy could go to work. “Our Cardiothoracic (open-heart) ICU was converted into a COVID ICU,” she says. “We all worked hard as a collaborative team to provide the greatest evidence-based care to each patient.”
Palardy says the hardest part of work during COVID-19 was holding the hands of sick patients when their families couldn’t be with them.
“As a team, we said prayers to initiate each shift,” she says. “We needed that uplifting start because at the end of the day you were so emotionally exhausted from the amount of tragedy you had witnessed that you were unable to grieve. We were strong when our coworkers needed us, holding them as they cried, and they were there when we were the person needing to be consoled. However, we all pushed through it facing each day at a time and on most days, each moment at a time. Although most of us were filled with fear, we put on brave faces for each other, our patients and ourselves.”
Palardy, who suffers from Lupus, said she didn’t realize the big impact she made on her own daughters until her eldest, Gabby, gave her a letter.
“Until my daughter wrote me a beautiful letter about how much I meant to her, I remained stoic,” she says.
I hope you stay healthy and never get sick. I hope you know that I really appreciate you and your hard work. I know it’s hard to go to work for 13 hours straight and not to see your family. You’re the best Mom I could ever have in the world.
Even though she’s her daughters’ hero, Palardy still thinks healthcare workers share the credit with everyday citizens, like her own mother.
“Healthcare workers have been seen as being heroes in this pandemic, and rightfully so, but it’s also taken a whole village of people to keep us going through these times,” she says. “The unseen heroes of this pandemic are our children and families that have also risked their lives for us to do our job each and every day.”

Theresa Dobbin, RN, WCC, CCRN Critical Care Nurse, Robert Wood Johnson University Hospital Rahway Hometown: Clark
Theresa Dobbin has been a nurse for more than 30 years. She was born at Robert Wood Johnson University Hospital, where she now works, and as a 5-year-old, was treated for pneumonia there.
“I wanted to be a nurse from then on,” she says.
Dobbin says that she’s seen so much support from the community throughout the coronavirus crisis.
And although she misses having her big Sunday dinners with her family, she’s made some incredible connections with strangers during the crisis, including a woman she saw standing alone in the hospital parking lot.
“One evening, after a long day, I was walking out of work. As I was heading to my car in the parking lot, I noticed a young woman standing still, silently staring up at the hospital. I asked if I could help. I found out that her dad was in the hospital as a patient and she was not able to visit with him.”
When the woman told Dobbin her father’s room number, Dobbin told her she was in the wrong place and directed her to the other side of the building.
The next day, she reached out to staff to tell them about the woman standing vigil outside the hospital and asked them to put a sign in the window so the woman would know where her father was.
“Within five minutes, a friend of mine and fellow nurse responded. ‘I’m here,’ she says. ‘I’m going to do it right now.’ She taped a heart to the window and let the woman know. That was now many weeks ago. But just watching that woman look up at that hospital window made me realize that we are all in this together and that could be any one of us.”
Dobbin wants people to know that the place she goes to for work is so much more than a building.
“Over this pandemic, we have come together as a team to care for those affected with this horrible virus,” she says. “We have seen death, but we have also celebrated those that have survived. We have seen many new faces that have come to help us during this pandemic. Many are shocked when they hear how many years some of us have been here. But we are family. We are Rahway strong!”

Jeanne Horsey, MSN, APN Pediatric Nurse Practitioner, Madison Pediatrics Hometown: Madison
Horsey has been a registered nurse for 26 years and a nurse practitioner for 20 and says it’s been amazing to be a part of the team at Madison Pediatrics as the practice has quickly adapted to these unprecedented circumstances.
COVID-19 has been tough on the Horsey family—with four children, one a graduating high school senior and one moving up to high school, both needed to have virtual graduations.
Horsey shares a strong connection with her patients and was surprised when one family reached out to help during COVID-19.
“As soon as it became clear that PPE (personal protective equipment) was going to be a critical piece to keeping health care workers and patents safe, one of our own families, the Fitzpatricks, reached out to me to ask if they could help,” she says.
Horsey wants patients to know that she is looking forward to seeing them in person again soon.
“Throughout this event, everyone throughout Atlantic Health System, including our team at Madison Pediatrics, never missed a beat,” she says.

Craig Davis, RN Nurse, inpatient unit at Children’s Specialized Hospital, New Brunswick Hometown: Plainfield
Davis is a pediatric nurse in a rehab facility and says that he can’t picture himself doing anything else, even with the added stress and restrictions brought on by coronavirus.
“I’ve worked here a little over three years and it’s one of the most rewarding and fulfilling jobs,” he says. Davis has been a nurse for four years and is motivated each day when he sees young patients get better—and knows he’s a part of that.
“Some days are tougher than others,” he says. “When coronavirus happened, we saw more of the after-effects of kids who have been in the hospital and needed that extra strengthening and conditioning. Some of the stories of resilience that kids have—you talk to them and listen to things they have overcome. They might not understand the magnitude of what they’re going through and they talk with childlike innocence. It pushes you further.”
Davis says he treats all of his patients like they’re “my little brothers and sisters.” He says there’s a lot more to nursing than just the medical needs of patients.
“One thing that made it more difficult during coronavirus was the visiting restrictions,” he says. “Family members and siblings couldn’t really visit.” Instead, in-person visits were replaced by video chats. He tried to do everything he could for kids recovering from brain and spinal injuries and relearning to move their limbs or walk again.
He remembers a young girl who came from another country where she experienced hardship, and was inspired by her strength. “Just hearing her story and what she went through and to come here in the middle of all this,” he says.
Davis takes a lot of “mental health breaks” and vitamins, eats healthy, stays active and tries to get enough sleep. His friends and family, and in particular, his girlfriend, lent their support which made all the difference.
Davis says that when he sees a child walk or move again when experts said they wouldn’t, it makes his job worth it. He says the kids are “truly inspiring. Words can’t describe it.”
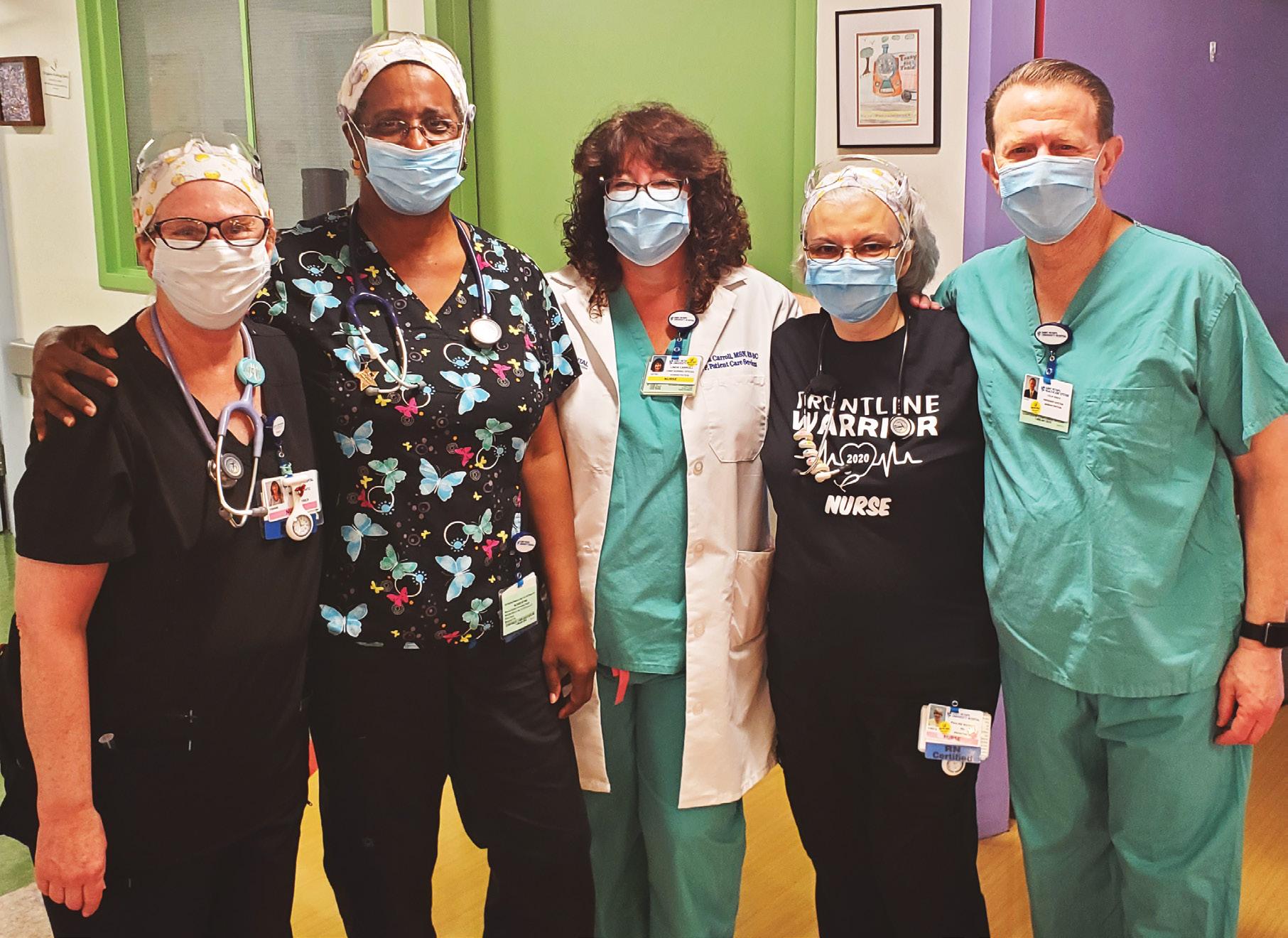
Linda Carroll, Chief Nursing Officer, pictured, center, with Saint Peter’s Healthcare System President and CEO Leslie D. Hirsch, pictured at right, along with nurses from the hospital’s pediatrics unit.
Linda Carroll, MSN, RN-BC Chief Nursing Officer and Vice President for Patient Care Services, Saint Peter’s University Hospital, New Brunswick Hometown: Colonia
We’re starting to get back to normal,” says Carroll, who has worked at Saint Peter’s for 36 years. She started as a nurse and now oversees all clinical staff, making sure the hospital is upto-date on all the PPE it needs.
During the coronavirus outbreak, the majority of hospital patients were those who tested positive for the virus. All areas of the hospital were mobilized to deal with the influx and staff from other areas stepped in where needed. Carroll says procedures such as proning, where patients are placed on their stomachs, lessened the need for many to be on ventilators.
“We would prone them with the hope that it would prolong or eliminate need for a respirator. Our clinical nurses came from all over the hospital. Anyone with critical care background pitched in,” she says.
Carroll says the way she and her staff got through the tough times were by finding little things to celebrate.
“At 6:30 in the morning and then again at 6:30 at night, all admin staff greeted our staff as they came into the hospital,” she says. There were treats handed out such as energy bars, compression stockings and meal cards for McDonald’s.
“It was emotionally stressful,” she says. “Any time a patient was discharged who was COVID-positive we would play a song,” she says. Recently, ‘Here Comes the Sun’ was played as a patient left the hospital healthy.
“We set up a Zen room where we had massage chairs donated, aromatherapy [and] we would have TVs with ocean sounds playing, lounge chairs for staff to take a break,” she says. A staff-driven support group, Masks Off, where staff could get together and support each other, was particularly important.
One of the most difficult things were the restrictions on visitors for sick patients. “We purchased iPads so families could stay connected and communicate through technology,” she says. “Our staff put their fears aside and were bedside with dying patients who didn’t have anyone.”
Carroll, who has a husband and three children, ages 24, 19 and 17, says that although it was a scary time, she liked having all of her children home during the quarantine.
“One day, my youngest started crying at the table and we got up and took a hike at Cheesequake Park. That’s something we would normally never do. We did more things as a family,” she says.

Kathy Armstrong, BSN, RN-BC Wound Care Specialist, Bayshore Medical Center, Holmdel Hometown: Neptune
Kathy Armstrong retired from nursing in December only to return a few months later in April to help with COVID-19.
Armstrong was placed in a per diem position doing wound care and soon returned to her old job. “I was welcomed back by my colleagues with open arms, a wonderful feeling amidst the severe illness I was about to be a part of,” she says.
Her family had mixed feelings about her going back to nursing but in the end, they were supportive. “I reassured them I would do everything I could to be safe, taking every precaution, making decisions with careful thought and be the nurse I am helping others to help those in need,” she says. “Nurses have a way of making the best of a bad situation. My extended family and friends offered support and concern for my safety as well. Today, my family and friends are proud of my decision as I update them regularly of the progress I see, the support of my colleagues and that I have patients recover and be discharged.” Armstrong says she saw many patients she’d treated in the past and that they were happy to see she had returned.
“At Bayshore, when a COVID-19 patient is discharged, overhead speakers throughout the hospital play, ‘Here Comes the Sun’ by George Harrison. That song has an effect on everyone, including the patient. We stop for a few minutes, smile, talk to each other who are near or just sing the song to have some relief. Special moments are when the song is played several times a day.”
Armstrong went back into retirement in July, but she won’t ever forget the experience of working during the pandemic.
“I will always remember the true commitment of teamwork, support, gratitude, humanity, sacrifices, grief, despair, frustration, love, hope and endurance that nurses and doctors have experienced together,” she says. “Nursing is a strong and resilient profession that will move forward, being more prepared if COVID returns. Whether I return, I will have to assess at that time. I know my decision will be from my heart.”

Pamela Grosso, RN, OCN Regional Director Oncology Clinical Operations, Summit Medical Group Cancer Center, Florham Park Hometown: Florham Park
Grosso chose nursing “because it brings together my love of science and desire to make an impact and a difference in people’s lives.”
After being an oncology nurse for 38 years, Grosso was diagnosed with breast cancer shortly before the novel coronavirus outbreak. But that didn’t stop her from caring for patients—after chemotherapy and a lumpectomy, she was back at work.
“The COVID-19 pandemic made it that much more important to protect the vulnerable oncology patient population,” she says.
“At Summit Medical Group, we were taking proactive actions at the beginning of the pandemic to ensure the safety of our patients, care teams and employees, including masking policies, screening anyone entering the cancer center, and testing our chemotherapy patients before their treatments to avoid giving chemotherapy to asymptomatic COVID-19 positive patients which could cause them to become very ill.”
As for how she found the strength to help others while going through her own cancer ordeal, Grosso says it actually helped her.
“After the surgery, I felt good enough to be back to work eight days later. The truth is that I found refuge in my work, where I have an amazing tribe who helped me through my own cancer journey. Getting back to work helped me to focus on something other than myself and concentrate on the greater good of our patients. I’ve had the unique opportunity to battle cancer both as a nurse and as a patient during this unusual time.”
Grosso says that when it comes to helping patients, science is the starting point, but that there’s an “art” to caring for patients.









