
10 minute read
Standing up for Science
From the beginning, NYSNA nurses and health professionals worked tirelessly to make sure science and the precautionary principle weren’t casualties of this pandemic. early evidence made it clear that this virus required airborne precautions and appropriate respiratory protection for any healthcare worker in contact with CoVID-19 patients, not just during aerosolizing procedures. through town hall meetings and well-researched fact sheets, NYSNA’s health and safety experts helped members push for more effective engineering controls, including better ventilation and expanded use of negative pressure rooms, as well as improved administrative controls, like expanded telehealth consultations, outdoor screening tents, and separately cohorting CoVID-19 patients. We consistently fought for our institutions to use ppe as the last line of defense, and follow the well-established hierarchy of controls for dealing with workplace hazards.
NYSNA was an early and outspoken proponent of reusable respiratory protection such as elastomeric respirators, and powered air purifying respirators. We also educated members on the dangers of “decontamination” techniques for N95s, and laid out the science of airborne transmission months before the Centers for Disease Control acknowledged the risks.
mobilizinG on The Job
Hundreds of NYSNA members joined CoVID Action teams, organizing to improve ppe, testing, staffing, and ensure safe workplaces and fair treatment. And when hospitals thrust more and more staff nurses into critical care, we provided hundreds of NYSNA members with Med-Surg and ICu practice workshops, and helped them collectively advocate for more training and appropriate delegation of assignments.
We also deployed cutting edge digital organizing tools to engage tens of thousands of NYSNA members, documenting conditions on the ground through member surveys, helping protect our practice and report exposures through CoVID Daily Diaries, and helping close to five thousand members notify their employers of potential workers’ compensation claims from CoVID-19 exposure.
Using town hall meetings, on-the-job organizing, and timely, well-researched materials, NYSNA members forced health and safety improvements at hospitals across the state.
Documenting the Springtime Surge
More than ten thousand NYSNA members participated in NYSNA surveys in March and April, documenting conditions during the first COVID-19 surge. Below are some key findings:
Mar 22 Apr 5 Apr 12
Definitely Exposed 40% 73% 79%
Possibly Exposed 84% 92% 94%
Have Adequate PPE 25% 33% 35%
Tested for COVID-19 7% 18% 28%
Showing COVID-19 – 27% 38% Symptoms
COVID-Positive 2% 18% 19%


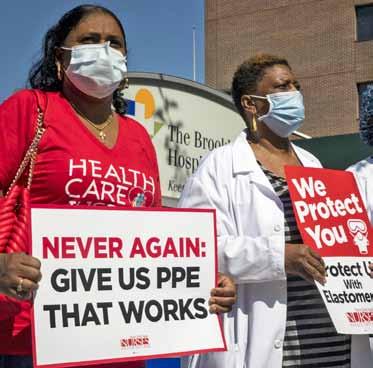

Above: NYSNA members at Brooklyn Hospital mobilized for reusable PPE. Right: NYSNA Health and Safety bulletins provided hands-on tools and cutting-edge information.
RULES OF THE ROAD Getting and Conserving Respirators and Protective Equipment APRIL 6, 2020 A Guide for Frontline Staff During the COVID-19 Crisis
PROTECTIVE EQUIPMENT IS THE CRISIS WITHIN A CRISIS The failure to provide proper protective equipment to frontline staff is a crisis within a crisis, and it will lead to many more COVID-19 cases that could have been avoided. Contrary to every infection control principle, almost all our facilities are using just one or two strategies to manage shortages of critical supplies like N95 respirators: limit the use of PPE or force staff to reuse disposable PPE. Multiple strategies are, in fact, available and they all must be used to their fullest extent before turning to conservation measures. NYSNA has created this guide to help members understand infection control best practices and demand hospital procedures that can truly protect healthcare workers on the frontlines of the COVID crisis. You can find this guide, our short COVID Protection Bulletins, along with other key health and safety re-sources on the NYSNA website: nysna.org/covid. CDC Props Up Unproven “Cleaning” Methods for N95 RespiratorsCDC GOES TO THE “LAUNDROMAT” On April 1, 2020 the CDC posted guidance that endorses the unproven, and potentially danger-ous, practice of what they call “decontaminat-ing” disposable N95 respirators. An array of business interests has backed the concept of cleaning N95 respirators for some time. Because federal and state officials have refused to order PPE manufacturers to hand over existing stockpiles and start producing large numbers of N95s, the idea of cleaning disposable respirators has been gaining traction. There is no credible evidence that it is possible to disinfect disposable N95 equipment and retain the protective effectiveness of the respirator. In fact, one of the largest producers of filtering face piece respirators (FFP), 3M, has stated: According to 3M, in order to effectively decontaminate and reuse a disposable respirator four criteria would have to be met. 3M’s criteria for any decontamination process includes the following: • Be effective against the target organism, such as the virus that causes COVID-19; • Not damage the respirator’s filtration; • Not affect the respirator’s fit; and • Be safe for the person wearing the respirator (e.g. no off-gassing of chemicals into the breathing zone). BIASED “SCIENCE” Unfortunately, the CDC has shown how deeply it’s willing to cave in to business interests during this crisis, citing flawed and biased “studies” to prop up the idea of decontamination. Their main piece of evidence is a 2016 study from Battelle, a multi-billion-dollar research institute based in Columbus, Ohio. Battelle’s study heavily touts disinfection equipment manufactured by Bioquell Corporation, but it turns out that Battelle is also getting into the “decontamination” business. On March 29th the company announced that it had been authorized by the FDA to market its “Critical Care Decontamination COVID-19 PROTECTION BULLETIN Get the latest COVID updates: nysna.org/covidLast Revised: April 14, 2020 “As of March 27, 2020 no disinfection method has met all four of these key criteria, and without all four, the method is not accceptable.” — Statement from 3M Corporation Bioquell and other manufacturers of hydrogen peroxide vapor machines are angling to make a fortune from “decontaminating” single-use N95 respirators. Healthcare worker safety — and public health — took another blow on Monday, March 16, when the New York State Department of Health issued a directive, releasing healthcare facilities from the 14-day quarantine requirement for staff who have been exposed to SARS-CoV-2/COVID 19. The Department of Health’s advisory stated that “HCP [health care professionals] who are asymptomatic contacts of confirmed or suspected [COVID-19] should self-monitor twice a day (temperature, symptoms), and undergo temperature monitoring and symptom checks at the beginning of each shift and a least every 12 hours.” LOOSENED QUARANTINE STANDARD CREATES DANGEROUS EXPOSURES 1 According to the DOH, if you are a healthcare worker who has been exposed to COVID-19 and are asymptomatic, you should continue working. The advisory also states that HCP with confirmed or suspected COVID-19 can return to work after maintaining isolation for at least 7 days after the onset of illness, provided they have been feverfree for at least 72 hours fever-free, with other symptoms improving. This means an infected HCP can return to work after less than the 14-day quarantine required for the general public. NYSNA believes these are dangerous practices that can result in further spread of COVID-19 to healthcare colleagues and patients. Just like the CDC rollbacks around personal protective equipment (PPE) this change in protocol is not based on science, but driven by pressure from employers, who in large part are unprepared to protect core staff from exposure to the virus. Most facilities jumped on the bandwagon and started applying these dumbed-down standards and announcing that exposed, un-symptomatic staff were to return to work and self-monitor their temperatures. Meanwhile, a new study in the Annals of Internal Medicine has reaffirmed the need for the current standard of 14-day quarantine. These findings indicate that about 97.5 percent of people who develop symptoms of SARS-CoV-2 infection will do so within 11.5 days of exposure. Researchers estimated that for every 10,000 individuals quarantined for 14 days, only about 101 would develop symptoms after being released from quarantine. RELAXED QUARANTINE RULES PUT WORKERS, PATIENTS, AND COMMUNITY AT RISK Continued on reverse>> Dept. of Health Shortens Quarantine Time for Healthcare Workers, Contrary to World-wide 14 Day Quarantine Standard “ New study on COVID-19 estimates 5.1 days for incubation period. Median time from exposure to symptoms affirms earlier estimates and supports CDC’s current 14-day quarantine period.” —Science Daily, March 10, 2020. GETTING OFF THE N95 TREADMILL Transitioning to Reusable Respirators One survey of healthcare workers found that between 53% and 95% used disposable N95 respirators, between 23% and 77% used PAPRs, and between 24% and 28% used elastomeric half face respirators (EHFRs).25,26 Better equipment is slowly making its way to the frontlines, which is a positive development. Research shows that EHFRs provided a “feasible and acceptable” alternative to N95s.27 Healthcare workers “can be rapidly fit-tested and trained to use the reusable elastomeric half face respirator.”28 One medical center reported that an EHFR provides “better respiratory protection, is cost efficient, and is less time consuming for fit testing. All persons in direct patient care receive an elastomeric half-mask respirator with N95 particulate filters. Cartridges are changed when dirty, saturated with fluids, difficult to breathe through, or damaged, or during annual fit testing. For individuals unable to wear half mask respirators, PAPRs are available on site . . .”29 POWERED AIR PURIFYING RESPIRATOR (PAPR) ELASTOMERIC REUSABLE HALF-FACE N95 BETTER EQUIPMENT is Available, With a Solid Track RecordAirborne Transmission of SARS-CoV-2 Virus WHAT HEALTHCARE WORKERS NEED TO KNOWEvidence supporting the possibility of airborne transmission of COVID-19 is mounting. NYSNA’s position is all healthcare facilities must put in place airborne precautions for treating COVID-19 patients and PUIs. LATEST SCIENTIFIC FINDINGS According to a recent National Academies of Sciences, Engineering and Medicine letter to President Trump’s Office of Science and Technology Policy, multiple studies have supported airborne (aerosolized) transmission of the CO-VID-19 virus, even from breathing alone.1 This evidence contradicts the CDC’s contention that workers only need to wear an N95 or higher protection respirator during aerosolgenerating procedures such as intubation. The modes of transmission of an infectious disease determine the control measures that can prevent its spread. Understanding how the SARS-CoV-2 virus is transmitted is key to pre-venting COVID-19 disease in healthcare work-ers and in the general population. There are 3 modes of transmission in which inhalation is a concern: COVID-19 PROTECTION BULLETIN Figure 2. After some time (time=1), the particles begin to disperse and larger particles begin to settle from the air. Person B will continue to inhale particles of all sizes. Figure 1. When an aerosol is initially emitted (time=0), the particles are clustered near the source at location A. Someone near the source (location B) may receive large-particle spray and inhale particles of all sizes. Carlyn Iverson/CIDR APGETTING OFF THE N95 TREADMILL Transitioning to Reusable Respirators A Guide for Frontline Staff During the COVID-19 Crisis APRIL 30, 2020 5Droplet Transmission: Large respiratory droplets are generated when a person coughs, sneezes, or talks. Large droplets descend rap-idly and travel only short distances. Inhalation of large droplets may also be possible.2 Droplet transmission is understood to be a primary mode of transmission of the SARS-CoV-2 Get the latest COVID updates: nysna.org/covidLast Revised: April 11, 2020 1 COVID-19 DEMONSTRATES THE NEED FOR BETTER ALTERNATIVES PAPR FROM THE BACK Figure 3. After more time (time = 2), the small particles are uniformly dis-persed and more of the larger particles have settled from the air. Persons B and C will inhale particles that are generally smaller, have a smaller size range, and are at a lower concentration than at time = 0. This pandemic has exposed a number of weak-nesses in the nation’s emergency preparedness. One significant problem has been hospitals’ inability to provide frontline healthcare workers with enough respiratory equipment that is safe, clean and effective. This failure stems from a single-minded reliance on just one type of respiratory protection: the dis-posable N95. NYSNA believes that now is the time to abandon our total reliance on disposable N95 respirators and increase the use of reusable elastomeric air purifying respirators and powered air purifying respirators (PAPRs). This equipment can provide higher levels of protection and improved comfort during extended use sessions. At the same time, it could get us off the N95 treadmill and on the path to greater resil-iency during times of crisis.










