The Equine Veterinary Practitioner
The Official Publication of the New Zealand Equine Veterinary Association

Podiatry
NZERF





The Official Publication of the New Zealand Equine Veterinary Association

Podiatry
NZERF




Joe Mayhew (Editor) 2 Owen Road, Gisborne 4010 evp.editor@gmail.com
Rabecca McKenzie (Convenor)
Emma Gordon (Secretary)
Lotte Cantley
HawkerLuca Panizzi
Mobile: 027 437 3651 Home: 06 927 7263
Rabecca@tevs.co.nz
Shelly Hann
Gareth Fitch
Barbara Hunter Trish PearceLucy Russell
Erica Gee
Lucy Holdaway (NZEVA Executive Rep.)
Papers for publication in The Equine Veterinary Practitioner (EVP) should be sent to the Editor in electronic form. Authors are requested to follow the usual EVP format for the front page of a paper including name(s) and address and email for contact author. The Editor must be made aware of any copyright matters and any appropriate acknowledgments.
Please direct all advertising inquiries to Tony Leggett (NZ Farm Life Media) on 027 4746 093 or tony.leggett@nzfarmlife.co.nz A full media kit for the publication is available on request.
The “Equine Veterinary Practitioner” is published by the NZ Equine Veterinary Association (NZEVA) a branch of the NZ Veterinary Association Incorporated (NZVA). The views expressed in the articles and letters do not necessarily represent those of the editorial committee of the NZEVA, the NZEVA executive or the NZVA, and neither NZEVA nor the editor endorses any products or services advertised. NZEVA is not the source of the information reproduced in this publication and has not independently verified the veracity of the information. It does not accept legal responsibility for the truth or accuracy of the information contained herein. Neither NZEVA nor the editor accepts any responsibility whatsoever for the contents of this publication or for any consequences that may result from the use of any information contained herein or advice given herein. The provision is intended to exclude the NZEVA, the NZVA, the editor and the staff from all liability whatsoever, including liability for negligence in the publication or reproduction of the materials set out herein.
WANDA LU (by REMIND) with rider Elise, working ahead of SNORKEL (by I AM INVINCIBLE) with rider Toni, from Isola Stables on early morning training ride at Karioitahi beach.
“I took this photo on 2nd August, 2022 around 7am at Karioitahi beach. The moon was setting, just before the sun rose. I slept at Waiuku in a motorhome with my friend because we were going to photograph meteor showers. But the moon was too bright for that so we went to the beach early in the morning. We were so lucky to meet these horses and people at the beach on such a beautiful day”.
 Catherine Song Castor Bay Auckland
Catherine Song Castor Bay Auckland
The EVP Editorial Group would like to invite NZEVAmembers contribute to the photographic art we display on the front covers, so please feel free to send any potential photos to evp.editor@gmail.com. These may be of an artistic, clinical, industry, social or humorous theme as long as they relate to Equidae. We may even spring for a prize for best contribution each year! So get your cameras out, scrutinise your hard disks and contribute.











Brendon Bell (President) nzevapresident@gmail.com 027 484 6378
Lucy Holdaway (Secretary) nzevasecretary@gmail.com 027 541 1294
Grace Reed (Treasurer) Shelly Hann Melissa Sim
Ronan Costello Pip Hendron Alex Fowler
Dentistry
Emergency Management & Horse Ambulance
Katie Kindleysides katiekindleysides@gmail.com Glenn Beeman mountainviewequinenz@gmail.com
Peter Gillespie peter@vetequine.co.nz
Endoscopy Ivan Bridge ivan@vetassociates.co.nz
EVP Journal Rabecca McKenzie Rabecca@tevs.co.nz
Groom Scheme Ivan Bridge ivan@vetassociates.co.nz
Insurance Brendon Bell brendonb@vetsouth.co.nz
Medication Andrew Grierson andrew@aucklandvets.co.nz
Parasitology Holly Blue info@bluebloodequine.co.nz
Young Members Pip Hendron pip.hendron@swvets.co.nz
LIAISON WITH
NZ Equine Health Association Ivan Bridge ivan@vetassociates.co.nz
NZ Equine Research Foundation Tim Pearce timpearce@srvs.co.nz
Racing Authorities Andrew Grierson andrew@aucklandvetcentre.com
Sport Horse Celia Grant vet@helpmyhorse.co.nz


Brendon Bell, NZEVA
President nzevapresident@gmail.comAs equine veterinarians we are in the middle of the busy season now - I hope everyone is coping well with things the silly season throws at us.
I have attended several NZVA MAG (Membership Advisory Group) meetings. Things of note are that we are looking at NZVA Policies (outline of general agreement on a subject) and Position Statements (universal agreement on a subject). Any of these that are outdated will be looked at and deleted if unnecessary or updated. This will be performed across all NZVA SIBs and the executive will be tasked with looking into all equine policies and position statements. I've also been involved in the Veterinary Council (VCNZ) Professional Standard Committee which helps to look at how the code of professional conduct is reviewed and applied. The Code dictates how we all practice on a daily process and I’ve found it interesting to be involved in the process to keep this relevant to clinical practice.
We are looking to secure equine stream speakers for next year's conference. This will be the NZVA centenary conference and will be a MEGA one with other streams, to be held in Wellington. The CPD committee has contacted speakers and are awaiting to hear back regarding confirmation. The conference will have a medical theme and our sessions may be somewhat truncated due to combined plenary sessions with other streams. VetPD are looking to return this year with a lab to be held at Massey, tacked onto the end of the conference, covering topics yet to be confirmed.
You may have noticed emails from the VCNZ regarding a survey on associated veterinary para professionals as the Vet Council looks into reviewing the Veterinarians Act. I have participated in meetings on this review with other SIB representatives and allied para veterinary professions. For equine Vets this legislation could help regulate Equine Dental Technicians in particular, so I encourage you all to participate and complete the survey.
The report in this edition by Peter Gillespie from the Equine Ambulance Trust is very inspiring. The trust has done a great job in fund sourcing then constructing these state-of-the-art Equine Ambulances that we all see at race meetings. This has been a labour of love for those involved over many years and the system we have now is a real credit to all this hard graft. Tremendous effort.
As this issue comes out close to Christmas, I wish all members good fortune over the holiday period. I hope you are not too busy over the festive season and can find time to enjoy the festivities with friends and family.
Kind regards, Brendon Bell nzevapresident@gmail.com
Arango-Sabogal JC et al. Date of birth and purchase price as foals or yearlings are associated with Thoroughbred flat race performance in the United Kingdom and Ireland. Vet Rec Open. 2022 Dec; 9(1): e43.
Purchas price as foal or yearling and performance figures were studied for 6,666 [UK] and 9,456 [IRE] horses in flat racing by the end of their second and third years of life. Prize money and prize money per start decreased with each additional day beyond 1st January (official TB foal birth date in UK & IRE) that the foal was born on. Purchase price was negatively associated with the number of races run, while it was positively associated with prize money and prize money per start by the end of the third year of life. Differences were more marked among males than females. The more expensive foals and yearlings ran fewer races but earned more prize money and prize money per start as 2- and 3-year-old racehorses than less expensive foals and yearlings. These findings may help inform management practices aiming to maximise horses' racing performance potential and increase financial returns.
Like many of you, I certainly have experienced incivility in the workplace, and heaven forbid, I may have been guilty of it myself! Incivility may be thought of as a forerunner of bullying. Displays are usually rude and discourteous, displaying a lack of regard for others and include interruptions and use of condescending tones and unprofessional terms of address (J Occup Health Psychol 2009; 14(3): 272-288) Amy Irwin and colleagues from the University of Aberdeen recently studied the frequency, impact and mitigation strategies for problematic incivility in veterinary practices in the UK (Vet Rec. 2022; 191(7): e2030). They determined that workplace incivility was very common and that incivility from senior colleagues predicted increased turnover intention for veterinary surgeons and predicted reduced job satisfaction for veterinary nurses. Also, client incivility received from clients increased the risk of professional burnout. Although only suggestions, the authors considered that veterinary practices should outline expectations in terms of civil behaviour, provide additional staff within problematic client consultations, and arrange regular reflective team meetings, all to help prevent incivility interfering with a happy, productive professional environment. Only on very large properties with quite valuable animals is equine blood typing likely to be economically feasible. Notwithstanding, most clinicians will at times face a need for blood/RBC transfusion – not simply plasma, available commercially – and we not always are well prepared for this. Fortunately, Camilla Jamieson and colleagues from Equine Veterinary Medical Center, Doha, Qatar have given us a nice review of blood transfusions in horses (Animals. 2022; 12(17): 2162) that covers the physiology and pathophysiology of conditions requiring transfusion, as well as step-by-step transfusion guidelines for practitioners. It has been a while since I have had to give blood/RBCs to a foal or whole blood to an adult horse, so this paper is a timely ready reckoner on the process. Notwithstanding, there are a few here some aides-mémoire that may be of use to readers.
- Only ~10 % of horses have naturally occurring alloantibodies, so crossmatch testing before blood transfusion is not always performed.
- Survival times for compatible RBCs is ~20-30 days.
- Survival time for incompatible RBCs is ~3-5 days.
- Laboratory-based complete major and minor compatibility testing for horses is not routinely available.
- A slide agglutination test (SAT) can be performed in many labs but just tests minor compatibility (donor serum vs recipient RBCs).
- It is haemolytic not agglutinating antibodies that are the major culprit in neonatal isoerythrolysis (NI) and in immunemediated haemolytic anaemia (IMHA).
- RBCs coated in antibodies, as in NI and IMHA, are very fragile and can lyse with any further minor insult.
- Whether blood typing, cross matching or going blind, it is the TPR-response of the recipient over the first ~15 minutes of slow administration that determines whether or not one is doing the best for the patient.
I am sure we will be reading much more in future about genetic manipulation, both for treating genetically related disorders and in detecting unlawful practices. Tozaki et al. have been looking at means to detect fraudulent forms of genetic manipulation in TB racehorses and their recent results (Genes. 2022; 13(9): 1589) indicate that gene-editing tests such as searches for single-nucleotide variants (SNVs) are useful to identify genetically modified racehorses, such as foals that have been produced by somatic cloning or by embryo transfer.
I am poor at interpreting statistics in papers, though I do tend to remain rather sceptical of claims made. However, we can get really excited about a new published finding indicating that treatment X is statistically significantly superior to a standard therapy Y [P ≤ 0.01]. Well, because of the huge misunderstandings associated with interpretations of P-values, confidence intervals and other statistical analytes, some journals have banned their publication. In fact the litany of 25 misinterpretations of such a finding [P ≤ 0.01] is quite unbelievable, as outlined in a paper by a large group of international experts in statistics and epidemiology (Eur J Epidemiol. 2016; 31: 337–350). This is not a paper for reading in bed, but a couple of Mayhewisms taken from the paper were that irrespective of any P-value, the hypothesis is still either right or wrong, depending on how well data measurement, collection and analysis followed correct processes, and what error-prone assumptions were accepted. And far too often we deduce ‘no difference’ from ‘no significant statistical difference’; WRONG.
But if readers are interested in delving further in to stats, The ASA Statement on p-Values (Am Statist 2016; 70(2): 129133) gives far more critique than the editor is capable of and addresses six (mis)conceptions and (mis)uses of the P-value: 1. P-values can indicate how incompatible the data are with a specified statistical model.
2. P-values do not measure the probability that the studied hypothesis is true, or the probability that the data were
produced by random chance alone.
3. Scientific conclusions should not be based only on whether a P-value passes a specific threshold.
4. Proper inference requires full reporting and transparency.
5. A P-value, or any measure of statistical significance, does not measure the size of an effect or the importance of a result.
6. By itself, a P-value does not provide a good measure of evidence regarding a model or hypothesis.
And while on the subject of trying to interpret data sets and association verses causality, I was interested in a commentary by a colleague James Meyer on a recent paper by Bennett and Parkin on risk factors for sudden death in racehorses appearing ahead of print at J Am Vet Med Assoc 2022 Oct 20; 1-7. The paper authors were quoted as saying that the use of furosemide (Lasix) in a race increases the risk by ~62%. This was based on the adjusted odds ratio (1.62; 1.01 to 2.61, p= 0.047), being a relative risk. Meyer points out that the data actually indicates an absolute risk of 0.005%, being rather less dramatic than 62%. On this basis, one more horse receiving furosemide would die, compared to those horses not receiving furosemide, over 20,000 race starts. Perhaps this is ano example of my simple dictum of wanting to look at the primary data rather than some derived statistic? So you think that we need more vets in our discipline and
recent graduates are ill-prepared for your practice discipline? Well, why not suggest an apprenticeship route to graduating? It appears that the UK National health Service is working towards adding such a route to graduating as a human doctor, so why not vets? This has been mooted in the Vet Rec recently by vet consultant Matt Ashford who confirms that standards of training and exams could remain the same, though there likely would be a shift to species specialisation within the programme. It would likely be applicable to only those practices with a high case load and staffing but imagine a few keen young horse industry workers being able to assist and learn on employment with say 2 days a week taking courses, both on-line and on resident teaching practicals. Wouldn’t they more likely stay in the industry? Worth pondering on, don’t you think?
I trust the spring has been enjoyable and readers can manage to take some time off during the summer period.
Kia kaha, nä Joe evp.editor@gmail.com
The


The British Equine Veterinary Association has made available to NZEVA Members much of its resource material including full current EVE and EVP papers, podcasts and discussions. You do not need to be a BEVA member to have a BEVA account - it's just you get more if you're a member. Registering as a NZEVA Member on the BEVA website will allow you to access resources, book CPD including BEVA Congress, and sign up for a BEVA membership.
To set up an account please fill in details and press the Register button on the login page here: https://www.beva.org.uk/Login?returnurl=%2fMembership%2fInternational-Partners

Proximal enteritis is a differential for horses presenting with signs of colic, systemic inflammatory response and gastric reflux, but is not commonly described in New Zealand. This report describes a case of suspected proximal enteritis and secondary mesenteric venous thrombophlebitis in a 7-yearold Welsh pony gelding. A full reference listing on proximal enteritis is offered.
A 7-year-old, 300kg Welsh pony gelding presented to Massey University Equine Veterinary Clinic with a history of colic and progressive signs of systemic illness persisting over 24 hours. There was no reported pyrexia or diarrhoea. Approximately 10 hours prior to admission, the gelding was seen by the referring veterinarian. At this visit, the gelding had marked tachycardia (88 bpm) and was given 2 mg/kg flunixin IV and 2 L of enteral fluid with electrolytes via nasogastric tube.
On presentation, the gelding was quiet with marked tachycardia (120 bpm) and tachypnoea (88 brpm). Mucous membranes were hyperaemic, dry with a CRT of 3 seconds. Jugular fill was delayed, borborygmi were absent in all quadrants, rectal temperature was 37.6 oC, and the digital pulses were difficult to palpate. The pony’s body condition score was estimated to be 7/9 (Henneke et al., 1983)
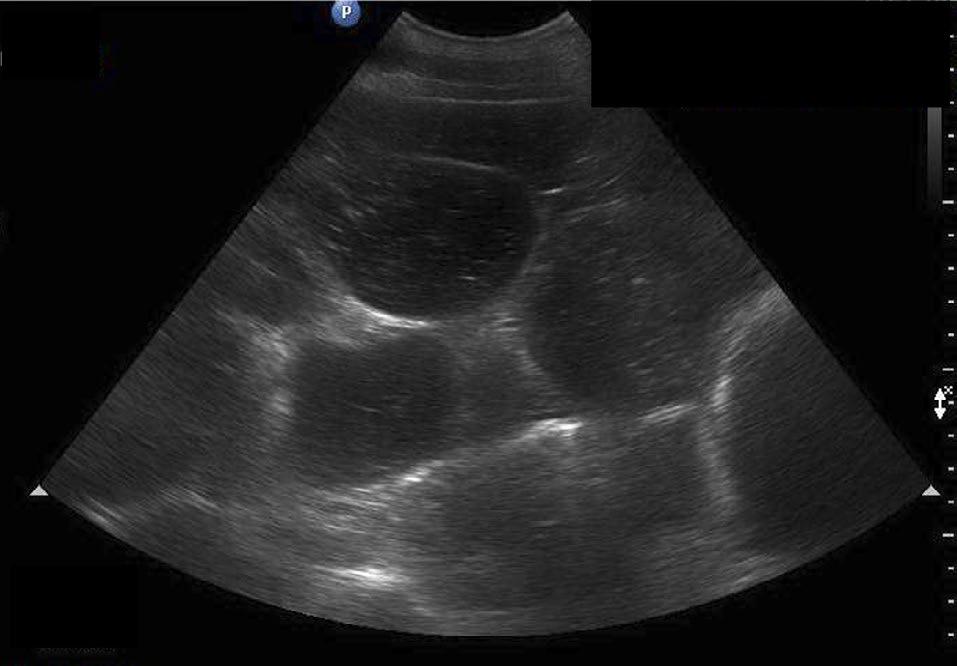
An abdominal ultrasound of the patient was performed using the “fast localised abdominal sonography of horses” (FLASH) approach (Busoni et al., 2011). The stomach was distended with fluid, with the caudal gastric axis extending to the 15th intercostal space. Nasogastric intubation was performed immediately, which liberated spontaneous, malodorous, dark green gastric reflux with a total net volume of 20 L. Continued FLASH examination revealed multiple, distended, amotile loops of small intestine (SI) in all quadrants of the abdomen (Figure 1); these loops measured 6-7 cm in diameter, and all wall thicknesses measured <3mm. There was a moderate increase in anechoic peritoneal fluid. The heart rate reduced to
108 bpm after gastric decompression and the pony’s attitude became increasingly dull. Blood analysis stall-side showed a packed cell volume of 62%, total protein of 88 g/L and lactate of 4.6 mmol/L. A jugular vein catheter was placed and a 6L bolus of Hartmann’s solution was administered. Muscle fasciculations developed and progressively worsened; 0.33 mg/kg xylazine was administered IV.
Abdominocentesis was performed and the peritoneal fluid obtained was serosanguinous in colour with a lactate of 12.5mmol/L. Venous blood gas analysis and biochemistry were performed following fluid resuscitation. These showed hypochloraemia (92 mmol/L), hyperglycaemia (11.1 mmol/L), hyperlactatemia (9.91 mmol/L), azotaemia (urea 17.6 mmol/L, creatinine 373 µmol/L) and an increased anion gap (20 mmol/L). Palpation per rectum was not performed due to the small patient size.
Dehydration of the patient was estimated to be at least 10%. The marked tachycardia persisted following gastric decompression, likely due to a combination of visceral pain and hypovolaemia. Additionally, the patient met the clinical criteria for systemic inflammatory response syndrome (SIRS) in adult horses (Roy et al., 2017), but, routine haematology
was not assessed in this case. The large volume of gastric reflux was indicative of a mechanical or functional small intestinal obstruction. Ultrasound findings were suggestive of diffuse small intestinal dysfunction, and intestinal hypomotility was supported by the absence of borborygmi on auscultation. High peritoneal fluid lactate (12.5 mmol/L) and peritoneal fluid lactate to blood lactate (PFL: BL) ratio of 2.7 (using initial blood lactate value), in combination with grossly serosanguinous peritoneal fluid, was highly suggestive of a strangulating intestinal lesion requiring surgical intervention (Shearer et al., 2018, Delesalle et al., 2007).
The azotaemia was thought to be a combination of pre-renal and renal, with the history of high dose non-steroidal antiinflammatory (NSAID) medication, along with hypovolaemia and SIRS putting this case at increased risk for acute kidney injury (Divers, 2022). No urine was passed during patient evaluation.
Strangulating and ischaemic lesions of the SI are a surgical emergency. Although exploratory laparotomy was offered, this was declined by the client due to financial considerations and the guarded prognosis for long-term survival (Delesalle et al., 2007, Hassel et al., 2009, White, 2017c). Thus, humane euthanasia was elected.
A diagnosis of mesenteric (jejunal to ileal) thrombophlebitis was made following gross and histological examination postmortem. No small intestinal pedunculated lipoma, volvulus, entrapment, displacement, intussusception, mechanical obstruction, or perforation were discovered. Grossly, the SI was diffusely distended with watery green fluid (most consistent with a functional ileus), with one exception, there was one 30cm segment of the ileum that had additional gross lesions. These included serosal haemorrhage, mural thickening and a dark red to grey appearance of the mucosa. Based on the above, a diagnosis of proximal enteritis was made.
Microbial polymerase chain reaction (PCR) was performed on fresh jejunal contents, the sample tested positive for Clostridium perfringens enterotoxin-A gene. The sample was PCR negative for Salmonella sp., C. difficile, Lawsonia intracellularis, C. perfringens NetF positive strains, and equine coronavirus.
Differentiating between a strangulating small intestinal lesion and proximal enteritis can be challenging due to similar clinical presentations and diagnostic findings (Arroyo et al., 2017). Common physical exam findings for proximal enteritis include abdominal pain, pyrexia, tachycardia, hyperaemia and marked gastric reflux (Archer, 2017). Typically, proximal enteritis cases have abdominal pain that is replaced with dullness following gastric decompression, compared to small intestinal obstruction cases that tend to become increasingly painful despite gastric decompression (Archer, 2018).
Proximal enteritis, otherwise known as duodenitis proximal
jejunitis (DPJ), is a syndrome of sporadic, acute inflammation of the duodenum and proximal jejunum. Overseas, the severity of this condition has been shown to range geographically (Steward et al., 2020). Anecdotally, there are also variations in prevalence geographically, yet there is a paucity of published reports of proximal enteritis in New Zealand horses.
The aetiology of proximal enteritis remains unknown, however, infectious agents such as C. difficile, C. perfringens, mycotoxins, and Salmonella spp. have been hypothesised (Arroyo et al., 2018, Edwards, 2000), all being anecdotal other than C. difficile. Inoculation of C. difficile toxins in healthy horses is reported to induce clinical signs and histological lesions consistent with naturally occurring proximal enteritis (Arroyo et al., 2017). In New Zealand, definitive diagnosis of these clostridial pathogens is limited due to the lack of ELISA testing for the different clostridial toxins (Uzal et al 2022). Alternatively, identification of clostridial DNA via PCR is available in New Zealand, as was performed in this case. Clostridium spp. can colonise the gastrointestinal tract of healthy horses, thus, a positive PCR result for clostridial toxins should be interpreted with caution as gene presence does not equal causation of disease (Schoster et al., 2012). In healthy colonised individuals, it is suggested that toxigenic strains of Clostridium spp. do not produce disease due to inhibitory actions of protective commensal microbiota (Mullen et al., 2018). One study investigating the presence of C. difficile and C. perfringens in different intestinal compartments of 15 healthy horses did not identify C. perfringens in any small intestinal compartment of the enrolled horses (Schoster et al., 2012). The results of this study are consistent with previous studies reporting a low prevalence of C. perfringens shedding in healthy adult horses. Thus, whether C. perfringens Type A in the present case indicates aetiological cause of proximal enteritis or simply is a result of opportunistic proliferation of this organism is unclear.
Horses with severe, acute gastrointestinal disease often develop SIRS as a result of systemic exposure to lipopolysaccharide (i.e., endotoxin) of enteric gram-negative bacteria (Archer, 2018). In both human and veterinary medicine, SIRS is known to have many deleterious sequelae, including vascular dysregulation, glucose and insulin dysregulation, coagulopathies, and multiple organ dysfunction (Dallap Schaer and Epstein, 2009). Additionally, laminitis is a common sequalae of SIRS in horses. Hyperglycaemia, as was observed in this pony, can be seen in equine patients with SIRS and is a negative prognostic indicator (Archer, 2018, Hassel et al., 2009). Horses with SIRS have a tendency to become hypercoagulable, which favours thrombosis development (Dallap Schaer and Epstein, 2009). Furthermore, obese, insulin dysregulated horses can be hypercoagulable compared to healthy controls (Lovett et al., 2022). As such, our patient might have had an increased risk for thrombosis being a predisposed breed for insulin dysregulation (Welsh pony) and being overweight (BCS 7/9). Importantly, although the mesenteric thrombophlebitis was significant in this case, the authors consider that it was most likely secondary to a SIRS-associated coagulopathy, as opposed to being the
primary inciting lesion of non-strangulating intestinal ileus and ischaemia.
The diagnosis of proximal enteritis was made at post-mortem. This was strengthened when jejunal fluid tested PCR positive for C. perfringens enterotoxin-A gene. False-negative PCR results for Salmonella spp. and equine coronavirus is possible in this case. However, due to the high sensitivity of PCR testing, and the clinical presentation of this pony not being consistent with the literature for equine coronavirus, it remains an unlikely aetiologic agent (Pusterla, et al,. 2012, Pusterla, et al., 2009). Additional infectious disease testing on faeces could have aided in further elucidating the role of these pathogens, for example, faecal PCR for equine coronavirus and culture of faeces for Salmonella spp. Salmonella spp. can be intermittently shed in the faeces of infected horses (Shaw et al., 2018), therefore, repeated faecal testing would have been valuable, although not possible in this case.
Blood lactate in normal horses is <1.5mmol/L, with peritoneal fluid lactate always less than venous blood lactate in healthy horses (Moore et al., 1977). Peritoneal and plasma lactate are significantly higher in colic cases with intestinal ischaemia (~8.45 mmol/L) compared to non-strangulating obstruction cases (~2.09 mmol/L), and peritoneal fluid lactate >9.4 mmol/L is associated with non-survival (Seahorn et al., 1992, Moore et al., 1977). Peritoneal fluid lactate (PFL) to blood lactate (BL) ratio (PFL: BL) > 2 indicates a strangulating intestinal lesion (Shearer et al., 2018). Serosanguinous peritoneal fluid is more likely to be seen with strangulating compared to non-strangulating small intestinal lesions. However, in severe cases of proximal enteritis diapedesis can occur, also resulting in serosanguinous peritoneal fluid (Shearer et al., 2018). With no evidence of a strangulating lesion on post-mortem examination, this case represents the potential limitations with interpreting peritoneal fluid lactate in severe, acute colic cases.
In conclusion, this case demonstrates how severe proximal enteritis can be difficult to differentiate from strangulating intestinal lesions in the horse. While the significance of enterotoxigenic C. perfringens in this case is difficult to define due to test limitations in New Zealand, it remains a plausible aetiologic agent.
Thank you to Dani Aberdein and Emma Gulliver, Veterinary Pathologists, for the detailed post-mortem examination, anda special thanks to Luca Panizzi, Equine Surgeon, for his help with the case.
Archer DC. 2017. Diseases of the small intestine. Ch 52 in The Equine Acute Abdomen, 3rd Ed, AT Blikslager, NA White II, JN Moore and TS Mair, Eds. John Wiley & Sons, Inc. NJ. 704-736.
Arroyo LG, Costa MC, Guest BB et al. 2017. Duodenitis-Proximal Jejunitis in Horses After Experimental Administration of Clostridium difficile Toxins. J Vet Int Med, 31, 158-163.
Arroyo LG, Gomez DE & Martins C. 2018. Equine duodenitis-proximal jejunitis: A review. Canad Vet J, 59, 510-517.
Busoni, V., Busscher, V. D., Lopez, D., Verwilghen, D. & Cassart, D. 2011. Evaluation of a protocol for fast localised abdominal sonography of horses admitted for colic. Vet Rec, 188, 77-82.
Dallap Schaer, B. L. & Epstein, K. 2009. Coagulopathy of the critically ill equine patient. J Vet Emerg Crit Care, 19, 53-65.
Delesalle, C., Lefere, L., Deprez, P., Dewulf, J., Lefebvre, R. A., Schuurkes, J. A. J. & Proot, J. 2007. Determination of lactate concentrations in blood plasma and peritoneal fluid in horses with colic by an accusport analyzer. J Vet Int Med, 21, 293-301.
Divers, T. J. 2022. Acute Kidney Injury and Renal Failure in Horses. Vet Clin Nth Mer Equine Pract, 38, 13-24.
Dunkel, B., Chan, D. L., Boston, R. & Monreal, L. 2010. Association between Hypercoagulability and Decreased Survival in Horses with Ischemic or Inflammatory Gastrointestinal Disease. J Vet Int Med, 24, 1467-1474.
Edwards, G. B. 2000. Duodenitis-proximal jejunitis (anterior enteritis) as a surgical problem. Equine Vet Edu, 12, 318-321.
Freeman, D. E. (2000). Duodenitis-proximal jejunitis. Equine Vet Edu, 12(6), 322–332.
Hassel, D. M., Hill, A. E. & Rorabeck, R. A. 2009. Association between hyperglycemia and survival in 228 horses with acute gastrointestinal disease. J Vet Int Med, 23, 1261-1265.
Henneke, D. R., Potter, G. D., Kreider, J. L., & Yeates, B. F. 1983. Relationship between condition score, physical measurements and body fat percentage in mares. Equine Vet J. 15(4), 371-372.
Johnstone, I.B., & Crane, S. 1986. Haemostatic abnormalities in horses with colic — Their prognostic value. Equine Vet J, 18: 271-274.
Lovett, A.L., Gilliam, L.L., Sykes, B.W. and McFarlane, D., 2022. Thromboelastography in obese horses with insulin dysregulation compared to healthy controls. J Vet Int Med, 36(3), 131-1138.
Moore, J., Traver, D. & Turner, M. 1977. Lactic acid concentration in peritoneal fluid of normal and diseased horses. Res Vet Sci, 23, 117-118.
Mullen, K.R., Yasuda, K., Divers, T.J. and Weese, J.S., 2018. Equine faecal microbiota transplant: Current knowledge, proposed guidelines and future directions. Equine Vet Edu, 30(3), 151-160.
Pusterla, N., Mapes, S., Wademan, C., White, A., Magdesian, K. G., Ball, R., Sapp, K., Burns, P., Ormond, C., Butterworth, K., & Bartol, J. 2012. Emerging outbreaks associated with equine coronavirus in adult horses. Vet Microbiol, 162, 228–231.
Pusterla, N., Mapes, S., Magdesian, K. G., Byrne, B. A., Hodzic, E., & Jang, S. S. (2009). Use of quantitative real-time PCR for the detection of Salmonella spp. in fecal
samples from horses at a veterinary teaching hospital. Vet J, 186(2), 252–255.
Roy, M. F., Kwong, G. P. S., Lambert, J., Massie, S. & Lockhart, S. 2017. Prognostic Value and Development of a Scoring System in Horses With Systemic Inflammatory Response Syndrome. J Vet Int Med, 31, 582-592.
Sanchez C. 2018. Duodenitis-Proximal Jejunitis, in Ch 12 Disorders of the Gastrointestinal System, Equine Internal Medicine, 4th Ed, Reed SM, Bayly WM & Sellon DC eds. Elsevier, St. Louis, Mo. 738-741.
Seahorn, T. L., Cornick, J. L. & Cohen, N. D. 1992. Prognostic Indicators for Horses with Duodenitis‐Proximal Jejunitis 75 Horses (1985–1989). J Vet Int Med, 6, 307-311.
Schoster, A., Arroyo, L.G., Staempfli, H.R., Shewen, P.E. and Weese, J.S., 2012. Presence and molecular characterization of Clostridium difficile and Clostridium perfringens in intestinal compartments of healthy horses. BMC Vet Res, 8, 1-6.
Shaw, S. D., & Stämpfli, H. (2018). Diagnosis and Treatment of Undifferentiated and Infectious Acute Diarrhea in the Adult Horse. Vet Clin Nth Amer Equine Pract, 34(1), 39–53.
Shearer, T. R., Norby, B. & Carr, E. A. 2018. Peritoneal Fluid Lactate Evaluation in Horses With Nonstrangulating
Versus Strangulating Small Intestinal Disease. J Eq Vet Sci, 61, 18-21.
Steward, S. K. T., Hassel, D. M., Martin, H., Doddman, C., Stewart, A., Elzer, E. J. & Southwood, L. L. 2020. Geographic Disparities in Clinical Characteristics of Duodenitis–Proximal Jejunitis in Horses in the United States. J Equine Vet Sci, 93, 103192
Uzal, F. A., Arroyo, L. G., Navarro, M. A., Gomez, D. E., Asín, J. & Henderson, E. 2022. Bacterial and viral enterocolitis in horses: a review. J Vet Diag Invest, 34, 354-375.
Van Den Boom, R., Butler, C. M. & Sloet van Oldruitenborgh-Oosterbaan, M. M. 2010. The usability of peritoneal lactate concentration as a prognostic marker in horses with severe colic admitted to a veterinary teaching hospital. Equine Vet Edu, 22, 420-425.
White II, N. A. 2017a. Decision for Surgery and Referral. Ch 24 in The Equine Acute Abdomen, 3rd Ed, AT Blikslager, NA White II, JN Moore and TS Mair, Eds. John Wiley & Sons, Inc. NJ. 285-288.
White II, N. A. 2017c. Prognosticating Equine Colic. Ch 25 in The Equine Acute Abdomen, 3rd Ed, AT Blikslager, NA White II, JN Moore and TS Mair, Eds. John Wiley & Sons, Inc. NJ. 289-300.
Readers might enjoy viewing video lectures on the following topics at the two links below. These are produced for the Beaufort Cottage Educational Trust and sponsored by the Gerald Leigh Family Trust.

Welcome and introduction - Nick Wingfield Digby
Sales selection - The trainer's view point - Sir Mark Prescott
The Sales Exam - The veterinary viewpoint - Mike Shepherd
Do foal injuries and diseases compromise sales and racing performance - Celia Marr
Radiography at the Sales - Are findings associated with future performance Pt1 - Debbie Spike-Pierce
Radiography at the Sales - Are findings associated with future performance Pt2 - Debbie Spike-Pierce
Does conformation affect gait - Objective assessmentRenate Weller
Genomics and performance profiling - Where are we heading - Des Leadon
9. A personal view on producing and selecting horses for racing and breeding - Luca Cumani
1. Radiographic findings in Juvenile Orthopaedic DiseaseDebbie Spike Pierce
2. Soft tissue injuries of the foot are there red flags on plain radiography - Marianna Biggi 3. Has advanced imaging changed the management of proximal suspensory desmitis - Sue Dyson 4. Imaging & clinical management of suspensory branch injury in racing thoroughbreds - Pete Ramzan 5. Third phalangeal cysts in the Thoroughbred RacehorseTom O'Keeffe
6. Imaging the equine back - Marianna Castro Martins 7. Fractured ribs - Diagnosis and prognosis - Billy Fehin 8. Pelvic ultrasonography - Sarah Boys Smith 9. Sub clinical imaging findings in the elite sport horseHow do we determine relevance - Sue Dyson
nzevasecretary@gmail.com

As part of the NZEVA executive’s role, we are asked to consider, comment, and advise on a range of topics affecting equine practitioners including policy review, current equine welfare concerns, member resources, and current issues being experienced by practitioners. Where appropriate we consult NZEVA/NZVA members with expertise in the relevant area, usually via our sub-committees. Although many of these matters are brought to us by scheduled review within our subcommittees, or delegated to us by the NZVA, we also receive correspondences from equine practitioners directly throughout the year. If there are topics affecting you in equine practice that you would like to raise, the following are the best ways to get in contact: Email nzevapresident@gmail.com or nzevasecretary@gmail. com. Currently these are attended to by President Brendon Bell and Secretary Lucy Holdaway.
• Contact any member of the executive in person: the current members are listed on our NZVA SIB page
(https://www.nzva.org.nz/branches/equine/) and at the front of each EVP issue.
You can also contact us to express an interest in being involved with the NZEVA executive; we require new members annually as we rotate through three-year cycles. Monthly meetings are held over ZOOM in the evening with the AGM being held in person at conference each year. We also have regular correspondence, mostly via email, between meetings.
If you would like to be more involved in equine collegial discussion on mostly clinical cases, Rabecca Mackenzie has set-up the ‘New Zealand Veterinary Practitioner Group’ on Facebook to support EVP and give NZ vets working with horses a place to get feedback on a variety of unusual and routine cases and procedures. If you would like to join, please contact Rabecca via Facebook or email myself. Existing members of the group can also invite their friends to the group; verification they are a vet working in New Zealand will be made before new members can join.
•


•
•
•
•
• Digital Radiography
• Ultrasonography
• Scintigraphy (Bone Scan)
• Shockwave Therapy

Equine endometritis is a significant problem in breeding mares and causes major financial losses for the equine industry due to loss of income at sales and increased veterinary cost. Equine endometritis is diagnosed via an endometrial sample such as a swab, cyto-brush or low-volume lavage taken during estrus and submitted for both cytology as well as aerobic microbial culture. To increase the sensitivity of the culture, most samples are taken in late estrus, however, to improve the breeding efficiency, clients and veterinarians are expecting a short turnaround time to allow the mare to be bred on the same cycle if the sample comes back clean. Because of this time constraint and the relative long turnover time when endometrial samples are sent to a commercial laboratory, many equine practitioners will perform in-house microbial cultures.
Most practitioners use a combination of MacConkey, blood, and Brilliance™ chromogenic agar plates to allow for easy and quick identification of the most cultured microbes such as S. zooepidemicus, E. spp. in house. Once the bacteria have been identified some practitioners treat the mare without sensitivity testing, some perform sensitivity testing in house and others submit the culture plate to a commercial laboratory.
Leigh de Clifford BVSc CertAVP PGDipVPS MVSc Barbara Hunter DVM MS DAVCS-LA
362 Hinuera Road West Matamata (07) 888 8193 matamatavets.co.nz
samples to Sydney, NSW, Australia for capsule typing.

For a limited time ISELP are offering a selection of Free Lectures that are excerpts from the 2019 ISELP Sports Medicine & Rehabilitation Module. Since EVP press time, more videos may be added.
• Improving Radiology of the Hock - Kurt Selberg
• Radiology of the Stifle - Sarah Puchalski
• Shoeing - Stephen O'Grady
• Equine Rehabilitation: Can We Make A Difference? - Melissa King

• Tendon and Ligament Injury with an Eye on Rehabilitation - Duncan Peters
As well as several GLOBAL SPONSOR
Liquid supplement containing Glucosamine, Chondroitin & Biotin suspended in Omega Oil for bone & joint health,
Dear Colleagues.
Did you know that you are eligible to apply for EVP funds to assist you in obtaining equine veterinary experience, training, travel, CPD etc? This is an annual sum of money is set aside each year by the NZEVA EVP Editorial Group to establish a Continuing Education (CE) fund.

These funds can be for use within Aotearoa. Possible uses of funds include attending the NZVA/ NZEVA conference or short courses, spending time at specialist equine clinics and learning new skills from other (non-clinical) sources e.g., veterinary pathology laboratory.
The two main purposes of this fund are:

• facilitating continuing education and/or specialist training for all paid up NZVA members and EVP Editorial Group members
• disseminating information resulting from such funding that is of benefit to New Zealand equine practitioners through publication in the Equine Veterinary Practitioner journal


Applicants seeking assistance from the CE fund must adhere to the following guidelines:
Added nutrients per 30mls of oil (minimum):
Crude Fat 85% Omega 3 2208 mg
Vitamin A 4050 iu Biotin 4.9 mg
Vitamin D 255 iu Niacin 5.6 mg
Vitamin E 45 mg Calcium Pantothenate 6.2 mg
Vitamin B1 1.05 mg Folic Acid 0.12 mg
Vitamin B2 1.3 mg Selenium 0.1mg
Vitamin B6 0.55 mg Glucosamine Sulphate 2010 mg
Vitamin B12 13 µg Chondroitin Sulphate 501 mg
Omega 6 3948 mg
1. Present a complete budget for the proposed CE project and identify all sources of funds being sought and the planned use of any funds awarded from this fund.
2. Demonstrate that funds awarded under this scheme were used for the stated purpose.
3. Normally present a verbal report to the NZEVA EVP Editorial Group at a convenient EVP meeting held after completion of the CE project, or at the next NZEVA Annual Conference.
4. Within 60 days of the applicant completing, and/ or returning to NZ from, the CE project, submit to the Editor of the EVP a concise report of the project, identifying key new practical items of interest and value to NZ equine practitioners.
5. Applications can be made in writing to and will be assessed by two members of the EVP Editorial Group [currently JM and BH], who are NOT eligible for funding.
6. The application must include a signed statement: “I have read and understand my obligations to the EVP Editorial Committee.”
7. Approved applications can access up to 75% of awarded funds prior to undertaking the proposed travel. The remaining 25% will be paid upon receipt of an acceptable written report.
8. Except in exceptional cases, the amount awarded to any individual applicant will not exceed 50% of the available funds.
The organisations currently represented on the New Zealand Horse Ambulance Trust [NZHAT] and their representatives are:
• Racing Integrity Board: Mike Godber (Chairman)
• New Zealand Thoroughbred Racing: Alice Riggins
• Harness Racing New Zealand: Liz Bishop
• Equestrian Sports New Zealand: Wally Niederer
• New Zealand Equine Veterinary Association: Peter Gillespie & Murray Brightwell.
In August of this year Bill Bishop stepped down as one of the two NZEVA representatives on the Trust although he continues to be actively involved with fund-raising.
The Trust employs a part-time operations and marketing manager and five part-time ambulance drivers.
It is almost four years to the day since the first ambulance deployment at the 2018 New Zealand Cup Day at Riccarton. Over this period, NZHAT has funded the construction and operation of a further eight ambulances, including purchase of nine Ford Ranger tow-vehicles.
The Trust has sold one ambulance to Canada, and we are currently negotiating the sale of two units to Western Australia. The nine ambulances are currently situated at:
• Auckland: Alexandra Park & Pukekohe
• Waikato: Matamata & Cambridge
• Taupo: National Equestrian Centre
• Central Districts: Palmerston North (Awapuni)
• Canterbury: Christchurch (Addington
Raceway & Majestic’s Yaldhurst Depot)
• Otago/Southland: Invercargill (Ascot Park)
During the 2021/22 season, ambulances attended 546 race meetings, 95 NZTR trial meetings and 20 ESNZ events. We were involved with nine SPCA welfare rescues and 22 nonrace day horse transfers. Many of the latter were the transfer of injured horses to and from veterinary referral centres. Most of our operational funding - $260,000 in the 2021/22 season - comes from NZTR and HRNZ, and we continue to engage with ESNZ to increase their financial contribution.
The NZHAT continues to advance the NZEVA’s animal welfare role within the New Zealand equine industry. The Trust is currently in discussions with Fire and Emergency NZ to fund technical rescue equipment throughout the country; currently there are only two FENZ brigades (Silverdale & Kumeu) equipped to attend large animal rescues.
NZHAT are looking to raise $250,000 to procure and distribute 20 sets of rescue equipment and two sets of training equipment (including full-sized horse mannequins) so that both FENZ and NZEVA members are better trained and resourced to work together in this space.
NZHAT are aware that of the important role NZEVA members play in ambulance deployments and the need for good lines of communication with those veterinarians working at race meetings and equestrian events.

There is still work to be done but I’m confident we can continue the momentum of the last four years.
Quere E
Complications
with Superior and Inferior Subpalpebral Lavage Treatment Systems Placed in 61 Equine Eyes (2004-2021). J Equine Vet Sci. 2022: 104076. https:// pubmed.ncbi.nlm.nih.gov/35830905/
Sixty horses were included in the study representing 61 sub-palpebral lavage (SPL) treatment administration systems. Median duration of SPL treatment was 7.5 days. Uneventful outcomes occurred in 53 cases (87%) and complications were recorded for seven upper eyelid systems (23%) and one complication for lower eyelid systems (4%). The easier placement and removal and the possibly lower recorded frequency of complications
All you need to do is write a clinical report that is published in the EVP, and your contribution may be eligible for one of several prizes of $150.00 that the EVP has available each year.
The EVP Editorial Group wish to promote the sharing of your interesting cases and practice tips with the wider equine veterinary community, so please contribute. Every case, technique, test and interpretation are different, no matter how experienced we are or how routine the case is, so there is always something for us to learn from each other.






Take photos, dig out your diaries, get keyboard tapping and share your views with colleagues. You could be $150.00 richer for it!
Please send your clinical reports to the EVP Editor for consideration. Joe is happy chat with you about any articles or ideas you might have. Please contact Joe at evp.editor@gmail.com or on 027 437 3651.

Podiatry Pages is a 7-part series overviewing some commonly seen hoof abnormalities in sport and racehorse practice using case examples demonstrating an approach to their treatment and management. Topics discussed include:
• Approach to the physical examination of the hoof

• Caudal failure and negative palmar/plantar angles
• Contracted heels and other capsular deformities
• Thin soles, weak walls
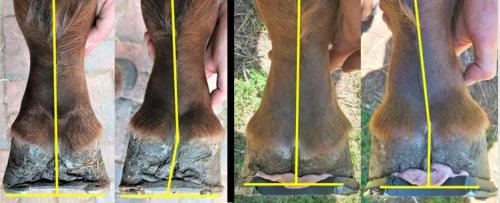
The previous instalment of Podiatry Pages discussed the aetiology of caudal failure, an extremely common abnormality seen in shod horses. However, a smaller population of horses have hoof capsule deformities that go the opposite direction when shod, developing upright, contracted heels or uneven, “sheared” heels. Though these capsular distortions can be seen in barefoot horses as well, with 8% of feral horses affected1, there is an overrepresentation of these defects amongst the shod population, ranging between 65%-95% depending on study parameters and population of sport horses.2,3,4,5 One theory behind heel contraction is that steel shoes have been shown to limit movement and expansion of the caudal structures of the foot,6,7,8,9 which can reduce circulation to the foot causing atrophy of the digital cushion and frog structures, leading to contraction.10 However, more recent research has demonstrated that, though there is some correlation between shoes and contracted heels, the cause is more multifactorial, incorporating, genetics, environment, bodyweight, conformation, application of farriery, etc.11 Pain can also contribute to development of contracted heels, with 3.3x more horses diagnosed with hoof pain having concurrent heel contraction.12 This is postulated to be caused by toe-first landing or other biomechanical factors reducing pressure to the caudal half of the foot.13
Signalment: 12yo Hanoverian mare training Grand Prix Dressage. Initially 2/5 lame right fore with effusion in both front fetlocks and a bilateral positive response to distal limb flexion, worse on the right fore. Radiographs of both fetlocks were taken which revealed bilateral osteochondral fragments on the sagittal ridge of the third metacarpal bone, visible only on flexed lateral views. The mare had arthroscopic surgery
• High-low syndrome
• Angular limb deformities affecting hoof balance
• New technologies and materials – the future of equine podiatry
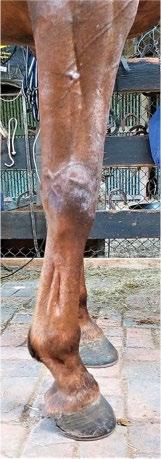
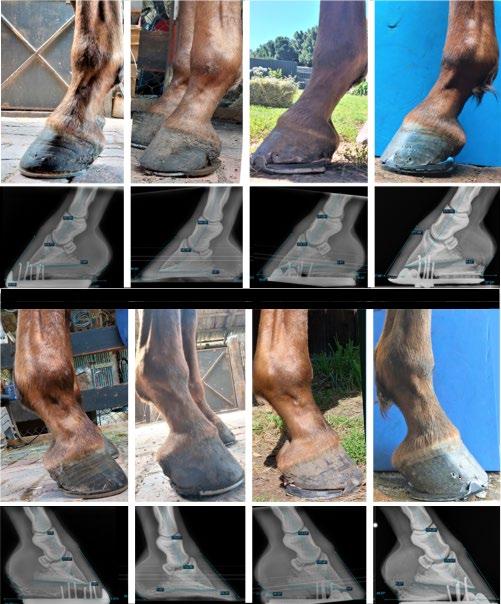
to remove the fragments and was treated with intra-articular injection of mesenchymal stem cells 2 months and 5 months post-operatively. She remained sound during her recovery and rehabilitation programme, however the owner noticed that the mare had gradually become tighter through her forelimbs and over at the knee, especially on the right forelimb (Figure 1).
Examination: The mare was examined for the progressive contracture 6 months after surgery. Comprehensive assessment of her conformation revealed a bilateral fetlock varus conformation (worse on the right forelimb), with laterally offset cannons, and some thickening of the lateral aspect of the left carpus (Figure 2). She had upright, contracted hooves, especially on the right fore. There was extreme tension of the antebrachial and pectoral musculature, and the mare was over-at-the-knee slightly on the right forelimb (Figure 1). She had a mild degree of “High-Low Syndrome,” with the left fore being lower in heel height than the right fore, and the right fore was more contracted and mediolaterally imbalanced than the left forelimb. There was no gradable lameness observed and no painful response to flexion of the forelimbs.
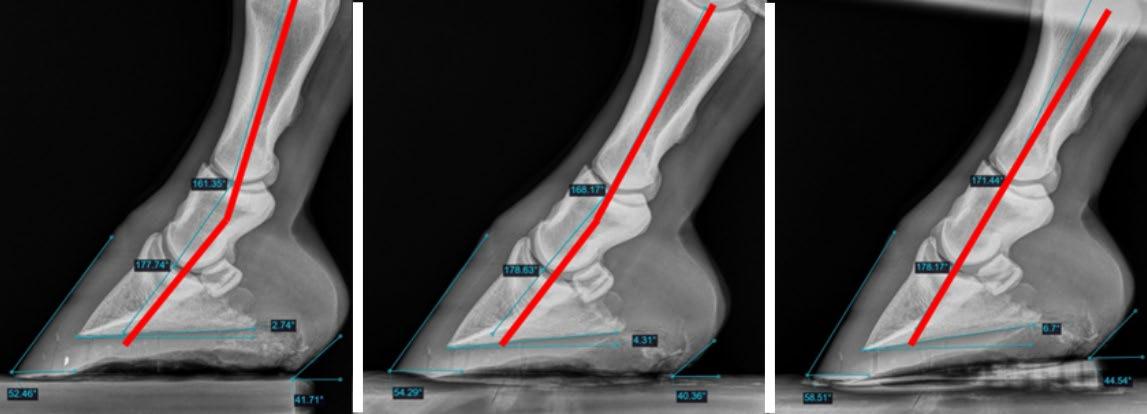
Radiographic examination revealed above average linear bony column alignment of the distal phalanges (P1, P2, P3) with a palmar angle of 3.7o on the left forelimb and 6.4o on the right forelimb. There were no significant mediolateral imbalances radiographically.
Plan: Usually it is preferred to remove the shoes to allow contracted heels to relax down an expand outward over the course of a few months to try to correct the issue. However, the owner wanted to continue progressing through the postsurgical rehabilitation programme and was not open to going barefoot for a short time in this instance because the mare was nearly back in full work. The decision was made to
Figure 1: Mare exhibiting tension through the antebrachial muscles and contracture through the carpus, upright pasterns, and toed-in conformation.
mimic barefoot biomechanics and remove heel restriction as much as possible using a “FlipFlop” pada and an aluminium breakover shoeb cut in half (Figure 3). The mare remained in the “Flip-Flops” for 3 months with no reported issues in lameness or performance observed during this time. Follow-up examination was performed prior to the 3rd set of shoes being placed. The mare’s heels had visibly lowered on both front feet, especially the lower left forelimb. Radiography showed that the mare was now at a zero-degree palmar angle on both front feet. However, physically, her limbs had relaxed and her
Figure 3: Example of the initial shoeing package.

Image: American Farriers Journal.
carpus was fully engaged. The owner, who was very diligent and observant, stated that there was only progress in her movement and demeanour and was pleased with the response, despite the obvious deterioration in palmar angle observed radiographically. There are many factors that may have been at play with this occurring: 1) the original farrier was injured during this time and an apprentice was shoeing the horse, 2) the shoeing changes occurred during a very wet winter which may have contributed to softening of the hoof capsule, 3) anecdotally, I have often observed sound, barefoot horses to have ground-level palmar angles but having wide heel bulbs and the appearance of a healthy frog and digital cushion, so more research into average palmar angles in shod versus unshod horses may be needed in the future to define what truly is “normal.” However, the vast amount of research showing a straight hoof-pastern axis and linear phalangeal alignment being the target biomechanical “ideal” has the most merit to maintaining soundness in performance horses and is still the goal for this horse.
Though there was an over-correction in the heel height, there was improvement in the width and substance of the heel bulbs and digital cushion, as well an in improvement in the angles of the quarters, which improved the imbalance of the right forelimb quite dramatically (Figure 4).
Due to the deterioration in palmar angles, it was necessary to change the shoeing package to a 3-degree frog-support padc to support the heels and allow the palmar angle to return to normal. Photos of the mare were taken with the new shoeing package placed and the relaxation in the forelimbs is visible when compared with the mare’s original posture (Figure 5) even though the internal phalangeal alignment and palmar angle is radiographically similar.

The horse remained in the new shoeing package for 6 months
and 5 shoeing cycles (Figure 6). The owner reported no issues with lameness and emphasized that the mare seemed to be improving month-on-month. A follow-up exam was performed at 6 months. There was improvement in palmar angles on both front feet, with the left forelimb at 2.7o and the right forelimb at 6o. The overall hoof quality had improved, with minimal evidence of horn tubule compression and abnormal growth rings. The right fore had made the most dramatic improvement and was moved to a flat frog-support pad at this stage. The left forelimb was trimmed to a 4-degree palmar angle but still required a degree pad (Figure 6) to restore phalangeal alignment based on this horse’s conformation.

Figures 7 and 8 present sequences of images summarising the transformation process. Given the High-Low syndrome that became more evident as the hoof rehabilitation cycles when on, there are still some further modifications to be made in the future, and perfect symmetry may never be achieved. However, the mare has only showed continued muscular relaxation, comfort, and improvement in performance throughout the process, which hopefully means we are on the right path.
1. Hampson BA, MA de Laat, PC Mills, CC Pollitt (2013). The feral horse foot. Part A: observational study of the effect of environment on the morphometrics of the feet of 100 Australian feral horses. Aust Vet J, 91: 14-22
2. do Canto LS, FD de La Corte, KE Brass, MD Ribeiro (2006). Frequência de problemas de equilíbrio nos cascos de cavalos crioulos em treinamento. Braz J Vet Res Anim Sci, 43: 489
3. De Melo UP, RMFW Santiago, RA Barrêto, C et al (2011). Biometry and hoof balance alterations in horses used to vaquejada. Acta Vet Bras, 5: 368-375
4. Maranhão RDPA, MS Palhares U Pereira de Melo, HH Capuano de Rezende, C Ferreira (2007). Avaliação biométrica do equilíbrio podal de eqüídeos de tração no município de Belo Horizonte. Cienc Anim Bras, 8: 297-305
5. Sampaio BFB, CESN Zúccari, MYM Shiroma, et al (2013) Biometric hoof evaluation of athletic horses of show jumping, barrel, long rope and polo modalities.
Rev Bras Saúde Prod Anim, 14: 448-459
6. Brunsting J, M. Dumoulin, M. Oosterlinck, M et al. (2019) Can the hoof be shod without limiting the heel movement? A comparative study between barefoot, shoeing with conventional shoes and a split-toe shoe. Vet J, 246: 7-11

7. Roepstorff L, C. Johnston, S. Drevemo. (2001). In vivo and in vitro heel expansion in relation to shoeing and frog pressure. Equine Vet J, 33: 54-57
8. Colles CM. (1989). The relationship of frog pressure to heel expansion. Equ Vet J, 21: 13-16
9. Yoshihara E, T Takahashi, N Otsuka et al. (2010) Heel movement in horses: comparison between glued and nailed horse shoes at different speeds. Equ Vet J, 42: 431-435
10. Teskey TG. (2005). The unfettered foot: a paradigm change for equine podiatry. J Equ Vet Sci, 25: 77-83
11. Senderska-Płonowska M, P Zielińska, A Żak, T Stefaniak. (2020) Do Metal Shoes Contract Heels? A Retrospective Study on 114 Horses. J Equ Vet Sci, 95:
Figure 8: Upper 2 rows – LF, clinical and radiographs. Lower 2 rows – RF, clinical and radiographs. Left to right clinical and radiographic pairs of images - Day 1 before new shoes; 3 months with Flip-Flops; first caudal support package; after 6 months in caudal support. Notice the health and integrity of the hoof walls (column 4) relative to the original photos (column 1). 103293. https://doi.org/10.1016/j.jevs.2020.103293.
12. Turner TA, C. Stork. (1988). Hoof abnormalities and their relation to lameness. Proc 34th Annu Conv Am Assoc Equ Pract, San Diego, 34: 293-297
13. Baxter GM, T. Stashak, C. Hill (2011) Conformation and movement. Adams & Stashak’s Lameness in Horses. Wiley-Blackwell, pp. 73-108
a. Grand Circuit® Flapper Pad - https://grandcircuitproducts.com/ b. Mustad® Equilibrium Shoe - http://www.Mustad.com c. 3DHoofcare® Half Mesh Pad - http://www.3DHoofcare.com

Pearce.patricia@gmail.com
What is your practice area, and how many years have you been doing this?
Panic! Rebecca and Joe want this by tomorrow so instead of being witty and succinct you will get the garbled barebones. I am currently Veterinary Advisor to the NZ Equine Health Association but have a few other equine roles including sitting on the Racing Integrity Board.
Where did you obtain your veterinary degree, and did you take on any post-graduate studies?
I migrated to Massey from small town Gore. I recall standing at the letterbox with my dad with the acceptance letter into the vet course in my hand feeling very relieved, proud, and excited while my poor father looked at me perplexed and asking if I was sure I didn’t want to be an architect? He was a builder so I wonder if he was worried about succession planning and as the youngest in the family I was his last hope. But no, of course I had to be a vet! I obviously also desperately must have wanted to be a wife too as I quickly seduced the local talent and married a classmate before I graduated in 1982 - but only after a year off to taste the delights of North America.
Why did you choose this area of practice?
My eventual areas of practise were not what I had planned at all. Most vets employed in rural NZ in 1982 did everything. Two jobs were on offer in rural Rangitikei in 1981, Tim my super talented spouse got one of them, but I seemingly wasn’t a contender for the other. The opposition Vet Club was sure Tim would poach their clients if I worked for them, which if analysed probably meant they thought I’d be bloody useless and he was supa-dupa!
As a fresh graduate I took a job working for MAF at the Borthwicks Meat works in Feilding fully intending for it to be short term. I didn’t think it was a good plan to work in the same business as Tim, and after a year or two my confidence that I could easily swap into equine practice waned, so I carried on working for MAF. The plus was I got better work life balance and got home in the daylight and could ride lots of horses. Soon Tim and I were spending all our spare time riding, competing, secretarying in equestrian events and selecting and bringing on showjumpers; this didn’t change for 40 years. By the 1990s I had switched to becoming a “field vet” working in the Wanganui area and that work was varied and way more interesting. It included involvement in quarantine programmes for new sheep and goat breeds, joining flights of horses into NZ, and participation in national disease eradication programmes which included curly
challenges such as attempting to allay community concern about aerial 1080 drops. It was in this job that I became heavily involved in Animal Welfare promotion and enforcement. I was a regional animal welfare coordinator and in this role worked with David Bayvel, a canny capable Scot, who joined the long list of wonderful mentors I benefited from. In that very long list I have to name Peter Jacques and Brian Goulden - and there are another 100 - but in the interests of brevity I will leave you to guess. In fact, if you are still reading this there is a very good chance that you might be one of them.
Any bumps and hurdles along the way to get here?
I don’t know if children are bumps in one’s career, but I found it really difficult working full time and trying to raise humans, in spite of having a pretty strong contributor as a spouse. I sometimes reflected that believing I could work and raise unscrewed up children was a big con. That thought is probably reinforced largely from the loss of our son Cameron who committed suicide when he was 19 years old. I still want to cry as I write that. Juggling work and family is a big job and if you don’t change your expectations, like me, then you can get sucked into thinking that anything that goes wrong is because you did neither very well. Alex my daughter blows that theory to bits though as she is smart, pragmatic, sane and of course beautiful. Life is full of bumps and I don’t have the answers but family and friends are very handy to pull you out of the mud and should the task be too monumental for them then time softens most things.
Outline the data and knowledge sources that are most useful to staying current in your areas of practice.
While working at the meat works, I started a Diploma in Meat Technology and didn’t finish. I also didn’t sit my membership exams in Epidemiology after wading through the course as I spent the day in labour - about as much fun! I did however enjoy and complete the first round of membership exams in animal welfare with the Australian & New Zealand College of Veterinary Scientists a few years later. I continued to
be immersed in Animal Welfare stuff, helping develop the training material for MAF Animal Welfare Inspectors and was assigned to verify that the welfare impacts of the Kaimanawa horse muster were minimised when population management efforts commenced to address the impacts of over 2000 horses on the fragile volcanic plateau at that time. When MAF was restructured I also restructured and moved sideways into Animal Welfare and Biosecurity related auditing then into MAF Emergency Management. During this time I won a Continuing Education award that sponsored my costs to complete a Masters Degree which I chose to do at Victoria Uni in Strategic Studies. This might be seen as a bit left field, but it widened my thinking, slightly improved my writing skills and gave me an introduction into what governance was all about.
All through my working life it was often the ‘spare time’ equine industry-related voluntary roles that gave me most pleasure. In the 90’s I joined the committee of the New Zealand Equine Health Association as the representative for Equestrian Sports. After 10 years on the committee, I took up the Chair role then took up a part time advisory role. This job has grown and grown and is the most diverse, challenging but best fun job I’ve had so far. The role has grown my skills in epidemiology, microbiology, virology, immunology, communications, project management and lots more.
What is the most challenging part of your job?
A lot of my job has demanded doing things I’ve never done before. Getting an equine biosecurity levy gazetted probably would not thrill the average vet as an achievement for example. When I started on it, I had no idea what to do, and only half believed it could be accomplished, but it will be the key that enables the equine sector to manage imminent and likely future disease threats. When one considers that we import more live horses than any other livestock sector, and from countries that have 10 times more diseases than NZ, we must accept that we need to stay invested in a solid risk management strategy. Climate change will not make disease exclusion any easier. Living without disease is one of the most important welfare benefits we can afford our horses, so the unique challenge of this job is describing and advertising the benefit of not having something!
Working alone would have been a lot more challenging without the support of a great committee. The current Chair, Ivan Bridge is a really dedicated, hardworking, generous boss, and when I’ve hit the wall on what to do next he has always been available and seemingly free to chat.
What advice would you give to someone thinking of following your line of practice?
I have a fantastic job and luckily NZEHA is growing. Should our BVSc [Massey] programme include substantial species or discipline specialization, or should that be mainly left to post-graduate training periods?
Who as a student has a clear view of where their career will
take them over the next 40 plus years? There is so much that could be jam packed into a degree, but I am so fortunate that I was not sent down a narrow track of specialisation based on an uninformed decision I had to make at aged 20!
What are your passions outside of work?
As well as attempting to stay on top of horses I enjoy farming, especially on the sunny days when the troughs are working, the fences are all tight and well stapled, and it’s not hailing during lambing. I am slightly addicted to buying plants and I quite like weeding. I have an e-bike and a set of skis that I will dust off soon.
Share your best practice tip
GSI. (Get Someone In…usually Tim) Give us a Tweet on Brexit, Trump, Putin… or anyone/thing else you like. Wordle is the new Tweet
Sporting event/concert you travel back in time for: Pink Floyd’s The Wall concert in Berlin
Last memorable meal: Tim’s fish pie
Best-ever or best-tentative dinner party guests: The book club ladies
First-ever concert: Monty Python at Hollywood Bowl
Favourite ever album/band: Queen
Finish the sentence: no woman/man should ever wear… Holey socks Beer or wine/Stones or Beatles: Both, I’m a very rounded person! Hazy beer and cardinay Like the Stones’ endurance and energy, but the Beatles lyrics What was the last lie you told? “Yes, I saw you pass me on the road”
Most interesting surgery you have done: Does a post-mortem count? Best self-defence tip: Watch carefully
Person(s) who influenced you most in your life: This list is very long…. some are mentioned in the epistle above
Best life lesson/life motto: “Failure is part of the process; you just have to learn to pick yourself back up”. Michelle Obama
Final personal story/comments I think I’ve gone on long enough…..
All you need to do is write a clinical report that is published in the EVP, and your contribution may be eligible for one of several prizes of $150.00 that the EVP has available each year. The EVP Editorial Group wish to promote the sharing of your interesting cases and practice tips with the wider equine veterinary community, so please contribute. Every case, technique, test and interpretation are different, no matter how experienced we are or how routine the case is, so there is always something for us to learn from each other.
Take photos, dig out your diaries, get keyboard tapping and share your views with colleagues. You could be $150.00 richer for it!
Please send your clinical reports to the EVP Editor for consideration. Joe is happy chat with you about any articles or ideas you might have.
Please contact Joe at evp.editor@gmail.com or on 027 437 3651.
The US Jockey Club has released its 2021 Edition of the Fact Book.
The online Fact Book is a statistical and informational guide to Thoroughbred breeding, racing and auction sales in North America that also features a directory of international organizations including NZ Thoroughbred Racing.
Of some note is that import/export and sales trends have been affected by the COVID-19 pandemic. When compared to 2019, the 2020 imports decreased 23%, exports decreased 36%, and mean yearling price decreased 20%.
The Brian Goulden Perpetual Trophy will be awarded annually and presented at the Annual Dinner of the NZEVA conference.
This annual prestigious prize is awarded to members or past members of the NZEVA who have shown leadership, enterprise, contribution to knowledge or education, and have made significant contributions to the equine veterinary profession in New Zealand.

Please send name, address and qualifications of your nominee, along with any supporting information, whom the nominator considers merits the award. This can include curriculum vitae, letters of support and documentation of achievements etc.
Send all details AT ANT TIME to nzevasecretary@gmail.com.
Brendon Bell NZEVA President nzevapresident@gmail.com

AUSTIN TX. USA 23-25 JUNE 2022
Here we offer selected, curated clinical extracts from papers and abstracts presented at the Hybrid ACVIM Forum, 2022.
Environment: The first approach is to use feedstuff and bedding that generate low dust levels. The second approach is to increase removal of airborne particles by improving ventilation in the barn or stall. The ideal environment for horses with severe asthma (RAO) is pasture. If the horse cannot be kept on pasture, ventilation in the barn and stall, the type of bedding, feedstuff, and general management should be scrutinized to minimize allergen exposure. Most horses improve clinically 1 to 2 weeks after being turned outside on pasture. Medical therapy helps speed up recovery. Horses with summer pasture-associated asthma are generally affected in late summer and the recommended environment for these horses during the summer is low-dust indoor housing. Some horses suffer both from classic and summer pasture-associated asthma.
Antibiotics: A large proportion of racehorses suspected of respiratory disease because of poor performance, cough, or nasal discharge are treated with antimicrobials mostly without evidence of bacterial infection. Available data shows no association between response to treatment and antimicrobial medication used. Only a proportion of racehorses diagnosed with mild asthma respond in part to a single course of antibiotic therapy.
Systemic Corticosteroids: These are potent inflammation inhibitors proven to be effective for the treatment of severe asthma (Table 1). Beware of risk of complications such as laminitis. Maximal benefit may take a week.
Inhaled Corticosteroids: Recommended dosages for the off-label inhaled corticosteroids are summarized in Table 2. The latest and only inhaled corticosteroid approved for the treatment of severe equine asthma is ciclesonide (Aservo® Equihaler®; Boehringer Ingelheim). Improved clinical signs, decreased airway hyperresponsiveness, and reduced pulmonary inflammation are usually detectable within 2 weeks of therapy. Therapy with inhaled corticosteroids results in faster improvement of clinical signs and lung function as compared to environmental management alone.
Corticosteroids
Dexamethasone 0.04–0.1 mg/kg IV or IM 0.08–0.165 mg/kg PO Once per day or every 2 days
Dexamethasone 21-isonicotinate 0.04 mg/kg IM Every third day
Isoflupredone acetate 0.03 mg/kg IM Once per day
Prednisolone 1.1–2.2 mg/kg PO Once per day
Triamcinolone acetonide 0.04–0.09 mg/kg IM No less than 3-month interval
Bronchodilators
Aminophylline 5–12 mg/kg IV 6 mg/kg PO Every 12 hours
Clenbuterol 0.8–3.2 µg/kg PO Every 12 hours Furosemide 0.5–1 mg/kg IV Every 8–12 hours
Glycopyrrolate 0.0022–0.007 mg/kg IV Once Isoproterenol 0.1–0.2 mg/kg IV Once N-butyl scopolammonium 0.3 mg/kg IV Once
Pentoxifylline 35 mg/kg PO Every 12 hours Theophylline 5–10 mg/kg PO Every 12 hours
Systemic Bronchodilators: These should not be used alone for extended periods of time because they have no anti-inflammatory properties and do not reduce airway hyperresponsiveness. Some bronchodilators (e.g., beta-2 agonists) induce airway receptor downregulation that renders the drug less effective, prevented by combined use of beta2 agonists with corticosteroids. Use of the three classes of bronchodilators available are summarised in Table 1. Oral absorption tends to be very variable and effects short lived.
Beclomethasone 80 µg HF EADDa 1–3 µg/kg, q 12 h
Ciclesonide 343 µg Soft Mist™ Aservo EquiHalerc 2744 µg q 12 h for 5 days; 4116 µg q 24 h for 5 days
Fluticasone 220 µg HFA AeroMaskb 2–6 µg/kg, q 12 h
Albuterol 120 µg HFA EADD 360–720 µg 1–3 h AeroHippusb/Equine Halerc 1–2 µg/kg
Ipratropium
20 µg 200 µg/capsule 0.02% solution for nebulization
CFC# DPI 2.5-ml vial
AeroMaskb EquiPoudred Ultrasonic nebulizer
0.2–0.4 µg/kg 2–3 µg/kg 2–3 µg/kg 4–6 h
Fenoterol 200 µg CFC# AeroMaskb 1–2 mg 4–6 h
Pirbuterol 200 µg CFC# EADD 600 µg 1 h
Salmeterol 50 µg CFC# AeroMaskb 210 µg 6–8 h
Cromones
Cromolyn sodium 0.02% solution for nebulization 2-ml vials Jet nebulizer Ultrasonic nebulizer 200 mg q 12 h 80 mg q 24 h
Inhaled Bronchodilators: Main classes of inhaled bronchodilators that have been used in the horse are beta-2 agonist and anticholinergic drugs (Table 2). The effects of anticholinergic drugs on airway smooth muscle are additive to beta-2 agonists.
Other Therapies: Supplementation of diet with omega-3 polyunsaturated fatty acids in combination with reducing exposure to dust results in improved clinical signs and lung function, as well as reduced airway inflammation. Sodium cromoglycate (cromolyn) improves clinical signs and decreases bronchial hyperresponsiveness when administered to horses with mild asthma only in cases characterized by a high mast cell count in BAL fluid.
NOTE: The diagnosis of mild asthma in racehorses is based solely on BAL fluid cytology so anything irritating the airway may cloud the diagnosis in those responding to antibiotics.
involuntary muscle contractions and stiffness that leads to a stiff gait and can progress to an inability to stand, seizures, fevers, and tachycardia. Parathyroid hormone concentrations are low or ‘inappropriately’ normal (i.e., they should be high due to the hypocalcaemia). A definitive diagnosis can be made via genetic testing. Calcium supplementation may suppress seizures in affected foals, but there is no cure for EFIH.
Equine Juvenile Degenerative Axonopathy (EJDA): In 2020, six related Quarter Horse (QH) foals (4 female, 2 male) were identified that had developed an acute onset of severe ataxia at 1–4 weeks of age. Clinicopathologic findings will be discussed, along with necropsy results and an up-to-date genetic analysis, which suggests an autosomal recessive mode of inheritance to this newly described disease.
Finno
UC Davis. CA, USA
Equine Familial Isolated Hypoparathyroidism (EFIH) is an autosomal recessive, fatal condition of TB foals up to 35 days of age. Affected foals suffer from hypocalcaemia, resulting in
Toby L. Pinn-Woodcock et al. Cornell University, Ithaca, NY, USA
Healthy horses from 9 locations in mainland USA were classified by latitude zone: northern (n=36), central (n=85), and southern (n=33), and plasma ACTH was measured once
to twice monthly. The ACTH upper reference limits were higher during July–November [equivalent to Jan–May in NZ] compared to December–June [June–Dec in NZ] in all latitude zones (p<0.0001), but no significant differences were detected between latitude zones. Horses >15 years of age exhibited higher ACTH upper reference limits during the late summer/fall compared to younger horses (p<0.0001). The results indicate that plasma ACTH concentrations are elevated in healthy horses during late summer/autumn throughout the USA and age is likely to be an important factor when interpreting ACTH results during late summer/autumn months.
Forty-three of 135 horses (32%) were positive on faecal PCR for ECoV, and 17 horses (13%) developed clinical signs. Colic occurred in 46% of affected animals. Three horses had small colon impactions, two of which required surgical intervention. Significant risk factors for having positive PCR results included presence of clinical signs (OR 56, 95% CI 8.3–594.6), being primarily stalled (OR 167.1, 95% CI 26.4–1719.0), housing next to a positive horse (OR 7.5, 95% CI 3.1–19.0), being in work (OR 26.9, 95% CI 4.573–281.9), being fed a ration of hay vs. ad libitum hay (OR 418, 95% CI 36.8–4438.0), being fed alfalfa hay (OR 418, 95% CI 36.8–4438.0) and levothyroxine supplementation (OR 7, 95% CI 2.7–18.7).
Cornell University, Ithaca, NY, USA
Common variable immunodeficiency (CVID) that occurs in horses of both sexes and different breeds, is a rare, lateonset immunologic disorder of B-cell depletion and/or dysfunction with resultant inadequate antibody production. Clinical signs appear at an average age of 12 years (range 2-27 years). Hypogammaglobulinemia leads to recurrent infections and fevers, with the most common presentations being pneumonia, sinusitis, meningitis, ataxia, peritonitis, gingivitis, sinusitis, hepatitis, diarrhoea, GI parasitism, uveitis, conjunctivitis, and/or skin lesions. There is persistently low serum IgG concentration (<800 mg/dL) and serum IgM concentrations are markedly reduced (<25 mg/dL) in most patients, suggesting the inability to elaborate primary immune response. Serum IgA and IgE concentrations may also be very low. Neutrophilia and hyperfibrinogenaemia are present during active infections, but persistent lymphopenia (<1,200 cells/µL) is common. An important differential diagnosis is lymphoma since some forms of this type of cancer may alter lymphocyte distribution and function, including B-cell lymphopoenia and hypogammaglobulinaemia. Management of horses with immunodeficiency can be difficult and impacts on the decision of euthanasia, with only rare cases being managed for a few years when serum IgG concentration remains above 600 mg/dL.
Rod Bagley
Iowa State University, Ames, IA, USA
In this study, 146 young horses treated with enrofloxacin were divided into three groups: 12–24 months (group 1); 6–12 months (group 2); and 0–6 months (group 3). Racing records for surviving animals and maternal siblings were compared. Median treatment duration was five days (range 1–63). 107/146 (73%) cases survived to discharge. Survivors did not differ from maternal siblings with regard to percentage of starters for all groups. Number of wins was significantly lower for foals from group 3 compared to their siblings, however, no significant difference was observed between cases and siblings in groups 1 and 2. Earnings per start were significantly lower compared to siblings for foals in groups 2 and 3. It appears that surviving juveniles receiving enrofloxacin were as likely to start races as their untreated siblings, but age <6 months at treatment resulted in fewer starts and lower earnings. These outcomes are similar to that reported for neonatal ICU survivors.
Some of the more common cognitive errors, usually hidden from perception, that misdirect clinical judgment and decision-making include Availability Bias, Confirmation Bias, Overconfidence Bias, Hindsight Bias, and Memory Errors. In trying to address the negative effects of cognitive errors, firstly, clinicians must accept that these biases occur regularly to effect bad clinical decision making. A balance must be struck between confidence and overconfidence, which allows the clinician to function, but with humility. Rather than following the tendency to attach to only one explanation, a switch to a more sceptical and questioning approach can help prevent some of these errors. These cognitive errors should be a component of teaching clinical decision-making and critical thinking, to instil the clinical skill required to increase diagnostic accuracy and ultimately, benefit to the patient.
Amen. We all can admit to succumbing to all these errors of judgement – knowingly and unknowingly.
Click on The HORSE – Podcast website HERE and listen to many 20-60 minute audio talks from The Horse. You may need to LOGIN/SIGNUP.

You can go to a selection of these topics directly by Ctrl+Clicking on the following:
• Older Horses. Amanda Adams
• Racetrack Surfaces. Mick Peterson
• Bits, Bridles, and Equine Welfare Hilary M. Clayton
• Mare Reproductive Cycles and Anxiety. Jenny Beard Biehunko
• Calming Horses: Education and Options. Camie Heleski
• The Best Forage for Insulin Resistant Horses. Stephen Duren
• African Horse Sickness Peter Timoney
• Vitamin E: Carrie Finno
• What Does Vitamin Deficiency in Horses Look Like?
• Why Do Horses Need Vitamin
• Vitamin E and Selenium: What’s the Relationship?
• Which is Better: Skin or Blood Test for Equine Allergies? Susan White & Ann Rashmir
• Mowing Horse Pastures to Keep Them Healthy. Krishona Martinson
• Old Gray Horses and Melanomas. Bryan Waldridge
• Basic Anatomy of the Equine Neck and Back Kevin Haussler


The history of this scholarship dates back over twenty years, when it was identified by horse owners and veterinarians on the NZ Equine Research Foundation Board that the delivery of a unified approach to horse feet issues was sadly lacking in New Zealand. This was despite many excellent farriers and vets working on hoof issues, it was largely a piecemeal approach, and the need for a more cooperative team dealing with these problems was obviously needed. Hence the scholarship was set up with the key goal of providing educational opportunities for a vet and a farrier to organise in tandem. It was also a recommendation to have the pair from a similar geographic area, with the aim of improving the future working relationship of the selected team. The opportunities were promoted by financial assistance to attend approved podiatry conferences and/or to study with recognised specialist podiatry clinics. Our teams have been very fortunate over the last 15 years to have frequently been hosted by Dr Scott Morrison and his podiatry specialist team at the Rood & Riddle clinic in Lexington, Kentucky. Dr Morrison’s team has hosted at least a dozen recipients, and all have thoroughly enjoyed their experience and benefitted from the exposure tremendously. Covid-19 has interrupted that relationship somewhat, but we are very grateful for their help to date. Currently Felicity Wade and Richard Evans are booked to spend 2 weeks of intense podiatry experience at Rood & Riddle as soon as Covid restrictions ease. To date this scholarship has been awarded to 40 people, and without exception has achieved the aim of creating great ‘vet-farrier teams’ around the country. To date, the NZERF has invested $120,000 in achieving this and believe it has been money well spent. In the future we are very fortunate that the NZEVA and the NZ Farriers Association have agreed to fund this scholarship. It is still envisaged that NZERF will still do the administration. All NZEVA practitioners involved in a significant equine caseload should definitely consider applying and this should be done in tandem with a local farrier who is a NZFA member. Depending on covid restrictions we would expect the closing date for the next round of Scholarships will be 31st January 2023.
For further information contact NZERF: nzerf@xtra.co.nz
Tim Pearce Chairman NZERF

The NZERF Bulletin for Winter 2022, Vol 27 (2) will be available August 2022 via NZERF website at https://www.nzerf.co.nz/
NZERF are also developing brief educational videos on topics of interest. Further videos
The first of these videos, presented by Paul Fraser, is on Strangles and is available HERE.
https://www.youtube.com/ watch?v=pbbXQ347LbU
The second, also presented by Paul Fraser is on Laminitis, is available HERE. https://www.youtube. comwatch?v=FKZQs2d7Tx4&t=16s



And the latest to be released is on Gastric Ulcers, presented by Ben Sykes, available HERE. https://www.youtube.com/ watch?v=eQT-2_wij4M
Secretary
NZ Equine Research Foundation Inc P O Box 52, Palmerston North 4440 nzerf@xtra.co.nz | 021 555 954
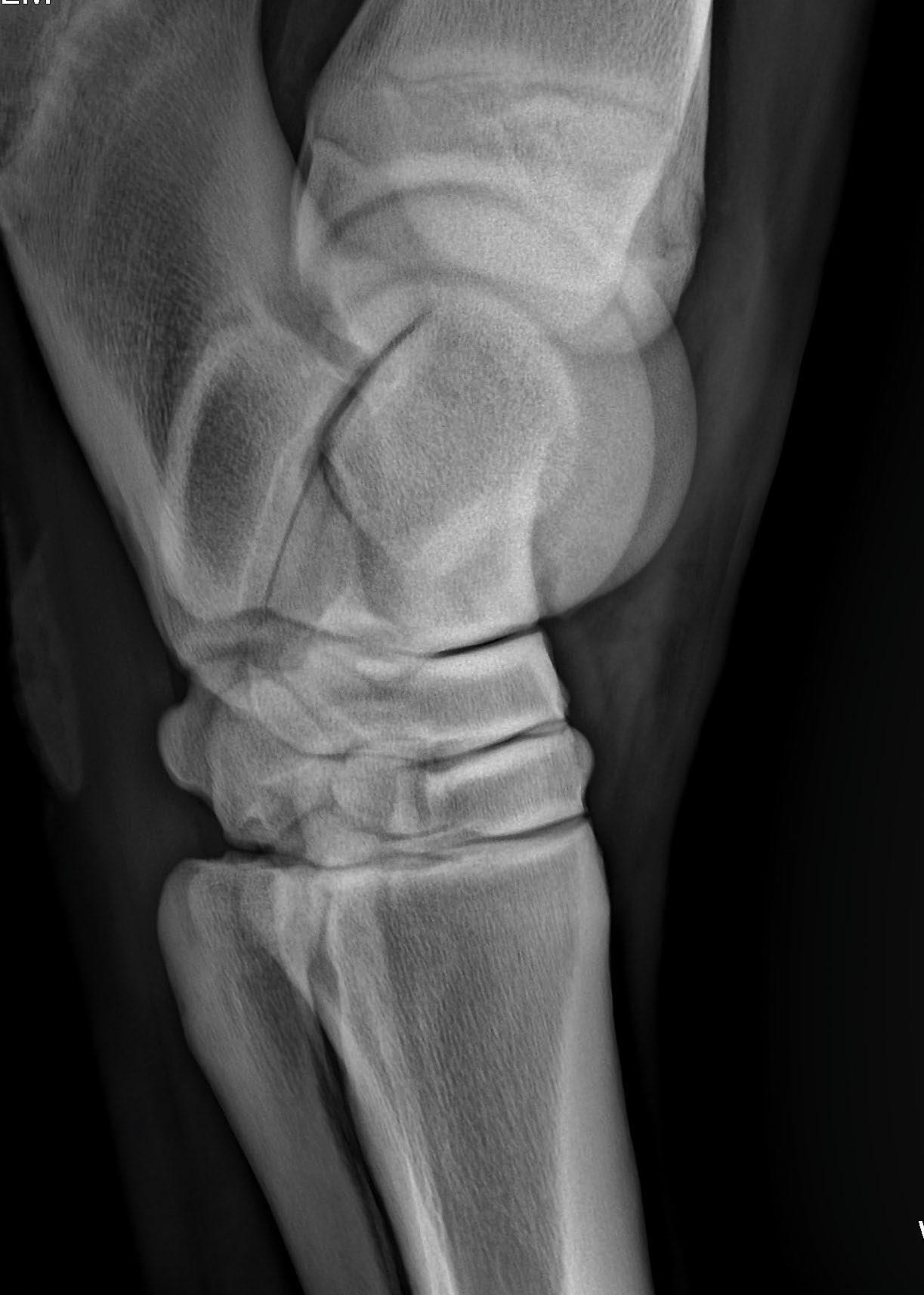







Image courtesy of Michelle Dicken michelle_dicken@hotmail.com
Equine metabolic syndrome (EMS) is currently defined as a collection of risk factors including obesity, insulin dysregulation and a genetic predisposition which results in an increased susceptibility to laminitis (Frank et al; 2010; Durham et al; 2019). Laminitis is the primary clinical consequence and most significant morbidity associated with EMS. Data pertaining to the prevalence of the whole syndrome are lacking though a recent study of 339 animals in the UK found a prevalence of 23.3% (Carslake et al 2021), this reflects the epidemiology of the individual components of the syndrome and is therefore likely to be an accurate estimate of disease burden in other populations.

Obesity in humans is defined by the World Health Organization as increased adipose tissue deposition which negatively impacts health. Whilst we have not clearly defined a critical point at which adipose deposition impacts health in horses most would consider a body condition score of >7/9 as “obese” (Dugdale et al 2011; Dugdale et al 2012). Obesity has been identified as one of the biggest welfare concerns facing the equine industry in several countries. Some studies report up to 70% of equids to be overweight or obese but the prevalence varies across the world and with season and management (see Table 1).
We are still unsure of the underlying pathology of obesity in equids, whilst the classic concept of energy intake exceeding energy expenditure holds true, we don’t know if intake or expenditure or both are genetically determined or the relative contributions of either. We must also consider the fact that a great many of our horses now reside in “obesogenic” environments (Furtado et al 2021) which not only makes obesity more likely but also make management more challenging for owners and vets. Adipose tissue is the largest endocrine organ contributing both
to the production of adipokines such as leptin and adiponectin and the metabolism of hormones such as glucocorticoids and sex steroids. It follows that dysfunction of the adipose tissue impacts the systemic metabolic profile and has remote effects on the liver, muscle and pancreas. The differential impact of specific adipose depots is well defined in humans with subcutaneous adipose often referred to as much “safer” than visceral adipose because of the enhanced ability of the subcutaneous adipocytes to store lipid. Again, the situation is much less clear in the horse, but some refer to neck crest adipose as the “dangerous depot” with a clear association between neck crest size and insulin dysregulation (Fitzgerald et al 2019) and laminitic risk (Carter et al 2009) however this could just reflect whole-body fat deposition given that neck crest adipose itself consists primarily of fibrous connective tissue (Reynolds et al 2019). Visceral adipose tissue in hoses with insulin dysregulation and the syndrome of EMS has been found to be markedly dysregulated with large hypertrophic, inflamed adipocytes present (Figure 1) (Reynolds et al 2019). Whether this is a cause or consequence is unclear but if we take lessons from our human counterparts, we can conjecture that unhealthy or dysfunctional adipose contributes significantly to the development of insulin dysregulation.
Figure 1: Adipose from a lean horse (Left) and from a horse with Equine Metabolic Syndrome and obesity (Right) that shows marked adipocyte hypertrophy [same mag.].
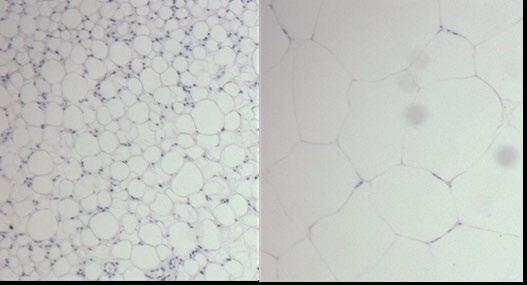
A clear breed predisposition to EMS has been demonstrated with, for example, British native breeds, Arabian and Morgan horses most at risk compared with Thoroughbreds (Carslake et al 2021; Carter et al 2009; Johnson 2002) (Figure 2). Like human metabolic syndrome it is a complex polygenic trait and some of its clinical features have been shown to have moderate to high heritability (Norton et al 2018). Endeavours to pinpoint functional and biologically plausible genetic variants driving the pathogenesis have not yet proven fruitful but are ongoing. Efforts are likely hampered by the complex nature of the disease and our poor understanding of the chronology of the pathogenesis. It is unclear whether breed predispositions are for EMS as a whole syndrome or for the individual components such as obesity or insulin dysregulation development in obesity. It may be that we will gain more incite by looking at the individual features of the syndrome. Recent work in dogs, for example, has shown that food motivation, which is higher in obese Labradors, is driven by genetic variation in the POMC appetite signalling (Raffan et al 2016). It is also important to consider epigenetic factors in the development of metabolic diseases. The in-utero environment is a critical determinant of future metabolic health in many species including horses, acute maternal stressors or insidious stressors such as obesity can impact the offspring significantly and these effects may not be identified until much later in life. It has been shown that in-utero exposure to glucocorticoids impacts pancreatic function later in life and that these differences are sex-dependent (Fowden et al 1998). Maternal obesity has been shown to alter the inflammatory profile in yearlings and increase the risk of osteochondrosis though we do not know about other metabolic effects (Robles et al 2018).
Insulin is the critical regulator of glucose homeostasis. Responding to post-prandial hyperglycaemia (and elevation in amino acids and free fatty acids) insulin acts predominantly on skeletal muscle and liver to initiate the uptake of glucose and normalise plasma glucose concentrations. In an obese state insulin signalling can become dysregulated; this can be caused by the development of insulin resistance or abnormal
insulin responses to glucose loads. Insulin resistance refers to a state in which target tissues of insulin, primarily muscle, liver and adipose become refractory to its effects. Tissue insulin resistance can develop because of a change in the number or substrate affinity of insulin receptors or defective intra-cellular signalling in response to insulin binding. Persistent impairment of a tissue’s response to insulin results in compensatory increases in pancreatic secretion of insulin and hyperinsulinaemia. In humans this often progresses to pancreatic exhaustion and insulin-dependent type 2 diabetes, but this is rare in the horse (Durham et al 2019). Alternatively,
Figure 2: Horses of two breeds kept in identical environments with markedly different body condition scores.

the pancreatic response to glucose may be altered as the primary pathology resulting in an abnormal or exaggerated secretion of insulin and insulin clearance may be impaired. Collectively these pathogeneses are known as insulin dysregulation in horses, and each may be present to a greater or lesser extent. The causative relationship between obesity and insulin dysregulation is complex, multi-factorial and poorly understood in humans let alone in the horse. Adipose dysfunction, ectopic lipid accumulation, alteration to the entero-insular axis, activation of the hypothalamic-pituitaryadrenal axis, oxidative stress, changes in the gut microbiome, changes to the lipidome and low-grade systemic inflammation all play a role in humans and most likely horses (Reynolds et al 2019, Janessen et al 2022, Zhang et al 2013, Zak 2020, Elzinga et al 2016).
Insulin dysregulation presents clinically in several ways; 1) persistent hyperinsulinaemia, 2) an exaggerated post-prandial insulin response or 3) an inappropriate and yet inadequate
insulin response to intravenous glucose. The result of each of these is persistent or recurrent exposure of tissues to high levels of insulin and whilst critical for life insulin has significant adverse effects when present in excess. For example, insulin acts on blood vessels, particularly affecting the endothelium and nitric oxide action with hyperinsulinaemia resulting in endothelial dysfunction in humans (Perkins et al 2015) and horses (Morgan et al 2016). In humans, hyperinsulinaemia is linked to a plethora of metabolic disorders including dyslipidaemia but also non-metabolic conditions such as pancreatic cancer (Zhang et al 2020) and even hearing loss (Koca et al 2020). In horses, insulin dysregulation is the key driver in development of endocrinopathic laminitis and thus early identification and treatment are key to mitigating laminitic risk.
There is ample evidence now that insulin dysregulation is the link to laminitis in both equine metabolic syndrome and pituitary pars intermedia dysfunction. Clinically recognisable insulin dysregulation is associated with a marked increase in laminitic risk and one of the best predictors of laminitis development in otherwise naive animals (Knowles et al 2022). In addition, infusion of insulin at supraphysiological concentrations results in the development of laminitis with a high degree of consistency (Asplin et al; 2007; de Laat et al; 2010).
While there is a reasonable consensus in the field that persistent or repeated exposure to increased insulin results in laminitis there is much debate as to why this happens. Ideas of insulin induced glucose deprivation (Asplin et al; 2011), glucotoxicity (deLatt et al; 2012), matrix metalloprotease upregulation (de Laat et al; 2011) and increased blood flowinduced hyperthermia (de Laat et al; 2012b) have largely been debunked as we gain more understanding of insulin receptor signalling in the hoof. The two most popular theories currently include 1) inappropriate activation, by insulin, of IGF receptors inducing direct changes to the epidermal cells and 2) changes in blood flow resulting from insulin-induced endothelial dysfunction (Morgan et al; 2016). Both of these and probably many more mechanisms contribute to the development of laminitis over time. As we understand more about laminitis development it becomes clear that the acute clinical signs we
see are most likely the manifestation of a tipping point after repeated or sustained insults to the lamellae rather than an acute disease process itself.
Systemic cardiovascular effects
There is evidence to suggest that endothelial dysfunction is not confined to the lamellar vessels in EMS but is widespread (Morgan et al 2016) which raises the question of other cardiovascular consequences of the condition. In human metabolic syndrome there is a clear association between the components of the syndrome and increased cardiovascular risk including microvascular dysfunction, coronary atherosclerosis and calcification, cardiac dysfunction, myocardial infarction, and heart failure (Tune et al; 2017). Overt cardiac disease is not commonly encountered because of EMS but there is some evidence to suggest that ponies with EMS or those with induced obesity have higher resting heart rate, higher systolic and mean arterial blood pressures and increased left ventricular wall thickness compared to controls (Heliczer et al; 2017) (Bailey et al; 2008) (Fonseca et al; 2021). Some recent work suggests that EMS may also induce a state of hypercoagulability and that this may warrant more vigilant catheter care during critical illness in these cases (Lovett et al; 2022).
In humans, obesity and insulin resistance can be associated with increased androgen production and the development of polycystic ovary syndrome which has marked effects on fertility. In horses there is some evidence to suggest that obesity and/or insulin dysregulation may impact cyclicity and oocyte health (Salazar-Ortiz et al 2011, Sessions et al 2004).
There has been a significant recent advance made in our understanding of the pathophysiology of EMS but much remains unclear. EMS is a complex interaction of risk factors and clinical development of laminitis. Further research is essential to better understand the syndrome.
All references for Part-1 and Part-2 will be available with Part2 in March 2023 EVP.
Burns JJ, MacMillan KM, John EE. Retrospective review of atrial fibrillation in Standardbred racehorses at a tertiary care facility in Atlantic Canada. Can Vet J. 2022; 63(10): 1051-1056. https://pubmed.ncbi.nlm.nih.gov/36185789/
Overall, 16 out of 22 horses (73%) with atrial fibrillation (AF) in which conversion to normal rhythm was attempted with enteral quinidine sulphate were successful. No significant difference was detected in racetrack earnings or number of top-3 finishes for each horse that raced at least 5 times pre- and post-conversion. The authors consider this to be the first published review to assess the athletic ability of Standardbred racehorses following cardioversion with enteral quinidine sulphate. Based on this study, it does not appear that treatment of AF with quinidine sulphate affects future athletic performance in horses that achieved cardioversion.
Image credit: ACVECC
CHECK WEBSITES FOR COVID-UPDATES
• To access further details for the following, CTRL-CLICK on hyperlink or insert name and location of event into your search engine.
• Listed events are delivered in English
• For additional events see https://www.ivis.org/home.asp
• And keep abreast of opportunities on VetPD and NZVA calendar sites
• Aware of an upcoming equine event? Please inform the editor evp.editor@gmail.com
JANUARY
January 25-27
FEBRUARY
Rossdales Mare and Stallion Reproduction Course. Newmarket, UK
February 28-March 1 Advanced Mare Reproduction. Lectures/Practical. VetPD. EquiBreed, NZ
February-November Veterinary Clinical Reproduction and Fertility. ONLINE COURSE. Massey University
JUNE
June 15-17
American College of Veterinary Internal Medicine Forum. Philadelphia, PA. USA
June 28-30 NZVA Centenary Conference. Tākina Wellington Convention and Exhibition Centre
JULY
July 6-8 European College of Veterinary Surgeons Annual Mtg. Cracow, Poland
July 10-14
13th International Symposium on Equine Reproduction. Foz do Iguaçu, Brazil
July 14-18 AVMA Convention 2023. TBA, USA
AUGUST
August 1-10
SEPTEMBER
September 7-11
OCTOBER
October 27-28
DECEMBER
December 2-6
Toothfest 2023; Aug 1-5, Coffs Harbour; Aug 8-10, Wet Lab, South Grafton, NSW
International Veterinary Emergency & Critical Care Symposium. Denver, CO. USA

Advances in Equine Podiatry – Practical Course. VetPD. Ocala, FL. USA
AAEP Annual Convention. San Diego, CA. USA2023

Veterinary Scholarships and Grants
http://www.nzerf.co.nz/
For any travel relating to research and development in the NZ horse industry http://www.nzerf.co.nz/travel_awards Applications received any time
Veterinarian – Farrier Scholarships
Arrangements yet to be confirmed. Please check website for details http://www.nzerf.co.nz/travel_awards
Valachi Downs Young Achiever Award
Closes 31st January, 2023
$15,000 available annually to assist an individual under the age of 35 in their career in the equine industry. http://www.nzerf.co.nz/valachi downs young achiever Closes 31st January, 2023
Jonathan Hope Equine Veterinarian Scholarship
$10,000 in total to be available to help young at heart equine practitioners travel, either nationally or internationally, to “see practice” and improve their practical skills. http://www.nzerf.co.nz/hope_scholarship Closes 31st January, 2023
Applications from interested people for funding for projects in the field of equine research. http://www.nzerf.co.nz/research_grants Closes 30th April annually
Applicants should apply in writing/email to: The Secretary NZ Equine Research Foundation, P O Box 52, Palmerston North Email: allan.fenwick@xtra.co.nz
See the Summer 2022 NZERF BULLETIN HERE
Greening L & McBride S. A Review of Equine Sleep: Implications for Equine Welfare. Front Vet Sci; 2022; 9: 916737. https://www.frontiersin.org/articles/10.3389/ fvets.2022.916737/full
Sleep profiles differ between species dependent upon a range of biological and environmental factors (see table). This review consolidates current information on equine sleep, to determine whether changes in equine sleep quantity and quality reflect changes in the animal's welfare, and to recognize the primary factors that affect the quantity and quality of equine sleep. The review then sets the direction of future equine sleep research with the aim of improving equine performance and welfare. The conclusions from this review are also contextualized within the current discussions around the social license of horse ownership from a welfare perspective.
Species
Horse (Equus caballus
NREM (h/day)
REM (h/day)
Total sleep (h/day)
2.98 0.67 3.85
Cow (Bos taurus) 3.2 0.8 4.0
Sheep (Ovis aries) 3.3 0.6 3.8 Goat (Capra aegagrus)) 4.7 0.7 3.8
Pig (Sus scrofa) 6.4 1.9 8.4
Dog (Canis familiaris) 7.1 1.6 10.7
Cat (Felis silvestris) 10.0 3.2 13.2
House mouse (Mus musculus) 11.9 1.3 12.8
Human (Homo sapiens) 6.1 1.9 8.0
A 14-year-old Quarter Horse mare with ulcerative keratitis of the right eye was referred to Massey University Equine Veterinary Clinic for further evaluation and treatment. The patient had been treated on-farm for approximately 4-weeks prior to presentation, initially with an ocular ointment containing chloramphenicol five times per day. However, the patient became refractory to the application of ocular ointment after approximately one week of treatment and a subpalpebral lavage (SPL) system was placed by the referring veterinarian. Further treatments included: compounded gentamicin, atropine, and tetanus antitoxin solution topically via the SPL five times per day, as well as oral phenylbutazone and oral trimethoprim/sulphadimidine. The decision was made to refer due to a lack of clinical response.

On presentation, general physical examination findings were within normal limits. The right eye was held approximately 50% open with an obvious 17x13mm opaque lesion of the right centrolateral cornea (Figure 1). Ophthalmic examination and sample collection were performed under standing intravenous sedation of 0.01mg/kg detomidinea and 0.008mg/ kg butorphanolb, and an auriculopalpebral nerve block (20mg mepivacaine hydrochloridec). The secondary uveitis was mild, with mild aqueous flare of the anterior chamber and miosis, and corneal oedema surrounding the plaque. The right eye had a positive menace response and pupillary light reflex (direct and indirect). The left eye had a horizontal lesion appreciated in the endothelial layer with no other significant findings. The cornea was anaesthetized topically with 10mg tetracaine hydrochlorided and debrided with a sterile cotton swab to remove undermined tissue and to collect samples for both cytology and culture. Fluorescein sodiumd was applied topically with positive uptake of the entire opaque regions with some underrunning of stain medially.
The patient was admitted to hospital for empirical medical therapy, meanwhile test results were pending. Topical ophthalmic treatments were administered via the SPL line, these included 1% voriconazole solutione, 0.3% ciprofloxacin hydrochloridef, 1% atropine sulphate monohydrateg and 0.3% EDTAh solution. Atropine treatment was administered q2h until pupil dilation was achieved, then as needed to maintain maximal dilation of the pupil. Voriconazole and ciprofloxacin treatments were given q4h until resolution (see Figure 1). All drugs were given at a volume of 0.1mL and flushed into the eye with 1mL of air. The patient received systemic NSAIDs;
either meloxicam 0.6mg/kg SID or flunixin megluminek orally or intravenously at 1.1 or 0.5mg/kg BID while in hospital based on patient discomfort.
The sample submitted for cytology revealed large mats of fungal organisms, degenerate neutrophils and necrotic background material with few epithelial cells and fungal hyphae. Fungal culture confirmed growth of Aspergillus fumigatus. Samples submitted for bacterial culture resulted in no growth. Based on these test results, a diagnosis of ulcerative keratomycosis was made.
The eye was debrided with cotton swabs, needle, the blunt end of a scalpel blade or scissors under sedation and local anaesthesia twice weekly while in hospital. To monitor for the possible side effects associated with NSAID therapy in equine patients, both serum creatinine and albumin levels were monitored from the beginning of hospitalisation. These values remained within the normal reference ranges and the trends for both these values remained stable over time. After 14 days of treatment, systemic itraconazolel at 5mg/kg PO BID was initiated. All antimicrobials, including the antifungals, were discontinued on day 25 due to resolution of the infection. Between days 9 and 18, the patient developed an episode of reduced faecal output and reduced borborygmi. Although no abnormalities were palpated per rectum during this period, an impaction of the large colon was suspected. This was managed by withholding feed, enteral fluids with electrolytes administered via nasogastric tube (NGT), polyethylene glycolm 0.25g/kg PO BID for 10 days and famotidinen 1mg/kg BID for 4 days via the NGT then PO on-going. Enteral fluids consisted of 1g/kg MgSO4 SID for two days, with the addition of 40L isotonic fluids over 4 hours on the second day and 80L over 8 hours on the third day. Soft faeces started to pass on day 3 of enteral fluid therapy and refeeding was commenced with grass only. Normal faecal output resumed 72 hours after discontinuation of enteral fluid therapy. During this time, the patient’s feeding was increased to ad lib fresh grass, but was not refed hay for the remainder of hospitalisation.
On day 28 of hospitalisation, the patient had a strong menace response bilaterally, the corneal lesion was fluorescein stain negative, and the affected corneal region had developed a prominent bed of pink granulation tissue (see Figure 1). The patient was discharged from hospital, with recommendations that the affected region would likely have permanent scarring which should reduce in size over time. Despite the possibility
of a corneal scar, prognosis for vision and athletic use was still deemed good. Continued therapy at home included atropineg 0.1mL topically via the SPL BID for 24 days and meloxicam 0.6mg/kg PO SID for 5 days.
On patient follow up, the owner reported that the patient has no noticeable visual deficits 5 months after discharge and was back in full work.
Equine keratomycosis in New Zealand has not been previously reported in the literature, although anecdotal reports exist. This is remarkable given the presence of fungi and mycotic disease reported in a variety of species including equine guttural pouch mycosis (Archer, Knight et al. 2012) and keratitis in humans (McAllum and McGhee 2003). Overseas, keratomycosis is often described in the horse (Clode 2010, Mustikka, Grönthal
et al. 2020), with Aspergillus spp. most commonly isolated (Utter, Davidson et al. 2009, Brooks, Plummer et al. 2013). This is unsurprising given that Aspergillus spp. are commonly found in the conjunctiva of healthy horses (Andrew, Nguyen et al. 2003). It is hypothesized that equine keratomycosis might occur more frequently after treatment with ocular corticosteroids, antibacterial drugs or with prior injury to the cornea (Scotty 2005, Clode 2010). This hypothesis might be relevant in this case due to the history of prior extended treatment with antibacterial drugs and lack of response to this therapy. Keratomycosis can become a surgical condition requiring conjunctival transposition or even enucleation, particularly in cases where severe keratomalacia develops. However, keratomycosis can also be managed successfully without surgical intervention (Utter, Davidson et al. 2009), as was described in this report.
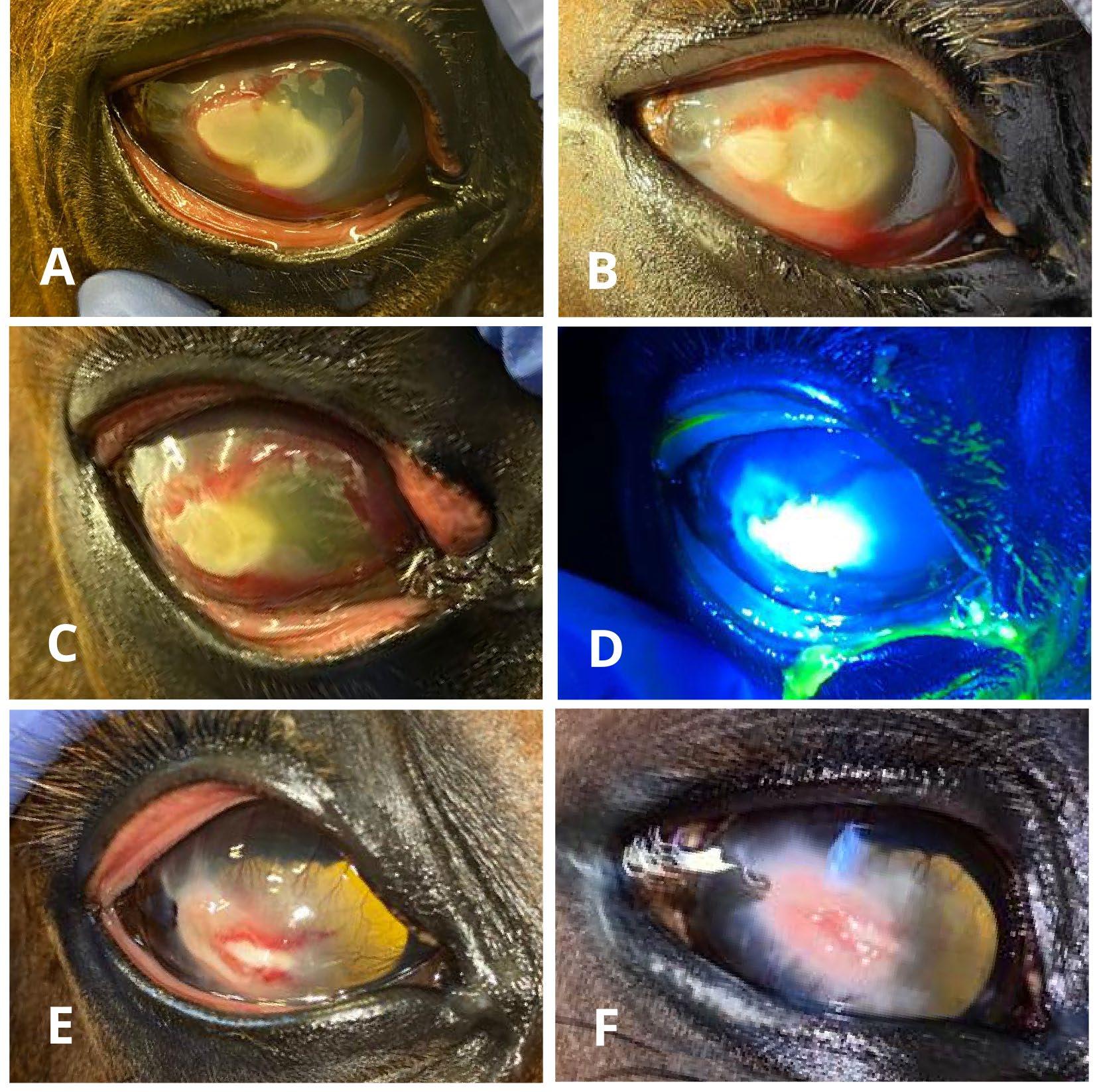
Susceptibility to voriconazole, a triazole antifungal agent, has been shown for Aspergillus fumigatus (Pearce, Giuliano et al. 2009). Additionally, there is evidence that EDTA acts synergistically with multiple triazoles for treatment of equine keratomycosis (Weinstein, Moore et al. 2006), as well as having fungistatic properties as a solo agent (Ruhil, Kumar et al. 2014). Another described use for EDTA in cases of ulcerative keratitis is to antagonise collagenases to aid in the prevention of keratomalacia (Ollivier, Brooks et al. 2003). The continued use of topical antibacterial in this case was to empirically treat a suspected concurrent bacterial infection as well as for prophylaxis against secondary infection. This was performed despite a negative bacterial culture. There are many reports in the human literature describing the sensitivity of bacterial culture in keratitis cases to be around 90%, reduced further by previous antimicrobial administration as in this case (Dunlop, Wright et al. 1994). The antibacterial ciprofloxacin was chosen based on common clinical isolates, normal conjunctival flora and the susceptibilities of these in referral bacterial keratitis (Andrew, Nguyen et al. 2003, Sauer, Andrew et al. 2003, Keller and Hendrix 2005, Galán A, MartínSuárez EM et al. 2009).
Due to the appearance of deeper tissue involvement on day 14 of hospitalisation, the systemic antifungal agent itraconazole was added to the patient’s treatment plan. This was elected at this time point because the extent of neovascularisation to the lesion was advanced (vessels from the limbus had reached the lesion’s perimeter), hence, indicating likely adequate drug delivery to the site via circulation as distribution in aqueous bodies such as tears is poor (Prentice and Glasmacher 2005). The itraconazole dose of 5mg/kg PO BID was extrapolated from a pharmacokinetic study performed by Davis et al. (2005) to target levels above the MIC for Aspergillus fumigatus (Pfaller, Messer et al. 2003, Davis, Salmon et al. 2005).
Atropine was given for mydriasis as needed to limit synechiae formation (Bistner and Riis 1979, Gelatt, Gelatt et al. 2021), as well as for cycloplegia to limit pain associated with ciliary spasm (Schwink 1992, Herring, Pickett et al. 2000). Equine patients hospitalized for ocular conditions are statistically more likely to develop gastrointestinal-related complications while in hospital (Patipa, Sherlock et al. 2012), the potential for topical ophthalmic atropine to cause gastrointestinal stasis is controversial. Wehrman et al. (2017) found that topically applied atropine did not slow gastrointestinal transit time in healthy horses and Strom et al. (2021) found that dosing every 6 hours had no side effects (Wehrman, Gemensky-Metzler et al. 2017, Ström, Dalin et al. 2021). The authors propose that the pain associated with ocular disease and stress of hospitalisation likely contributed to the observed episode of reduced faecal output in our case. During this period of feed withdrawal, suppression of stomach acidity with famotidine was elected due to famotidine’s short duration of action (Murray and Grodinsky 1992), as itraconazole bioavailability relies on the low pH of stomach fluid(Prentice and Glasmacher 2005). Accordingly, famotidine was administered 2 hours after itraconazole to allow adequate absorption of itraconazole before induction of acid suppression.
The volume of an ophthalmic drug needed in the equine tear film for intended treatment efficacy is well supported in the literature for volumes of 0.1mL or less (Hendrix, Stuffle et al. 2007, Czerwinski, Lyon et al. 2012). The efficacy of using 0.1mL per treatment was demonstrated by observing the mydriasis achieved by atropine in this case. Using a smaller volume of drug topically also limits dilution of drug by the tear film (Chrai, Makoid et al. 1974) and is more cost-effective, this is particularly noteworthy for voriconazole (being an expensive drug).
In summary, a fungal aetiology should be considered in any case of equine ulcerative keratitis seen in New Zealand, just as it is overseas. Certain temperate regions may have higher or lower risks of such fungal infection, however, fungi are ubiquitous in the environment (Bridge Cooke 1968) and opportunistic infection cannot be ruled out entirely on the basis of geographical location. It is also possible that the incidence of fungal infections might increase with the current understanding of climate change in New Zealand with Moore et al. (2005) showing presentation of equine keratomycosis occurs more frequently after periods of higher heat and without rainfall (Moore, Dietrich et al. 2005, Lake 2018, Vallee, Wada et al. 2020)
The authors would like to thank the staff and students at the Massey Equine Veterinary Clinic for their tireless efforts working with this case, and the owners who were incredibly committed to a positive outcome.
Andrew, S. E., A. Nguyen, G. L. Jones and D. E. Brooks (2003). Seasonal effects on the aerobic bacterial and fungal conjunctival flora of normal thoroughbred brood mares in Florida. Vet Ophthalmol 6(1): 45-50.
Andrew, S. E., A. Nguyen, G. L. Jones and D. E. Brooks (2003). Seasonal effects on the aerobic bacterial and fungal conjunctival flora of normal thoroughbred brood mares in Florida. Vet Ophthalmol 6(1): 45-50.
Archer, R. M., C. G. Knight and W. J. Bishop (2012). Guttural pouch mycosis in six horses in New Zealand. N Z Vet J 60(3): 203-209.
Bistner, S. I. and R. C. Riis (1979). Clinical aspects of mycotic keratitis in the horse. Cornell Vet 69(4): 364-374.
Bridge Cooke, W. M. (1968). Fungi and Their Environments. Amer Biology Teacher 30(6): 521-526.
Brooks, D. E., C. E. Plummer, B. G. Mangan and G. Ben-Shlomo (2013). Equine subepithelial keratomycosis. Vet Ophthalmol 16(2): 93-96.
Chrai, S. S., M. C. Makoid, S. P. Eriksen and J. R. Robinson (1974). Drop size and initial dosing frequency problems of topically applied ophthalmic drugs. J Pharm Sci 63(3): 333-338.
Clode, A. (2010). Therapy of equine infectious keratitis: A review. Eq Vet J. Suppl 42; 37: 19-23.
Clode, A. B. (2010). Therapy of equine infectious keratitis: A review. Eq Vet J 42: 19-23.
Czerwinski, S. L., A. W. Lyon, B. Skorobohach and R. Léguillette (2012). Pharmacokinetic analysis of topical tobramycin in equine tears by automated immunoassay. BMC
Vet Res 8(1): 141.
Davis, J. L., J. H. Salmon and M. G. Papich (2005). Pharmacokinetics and tissue distribution of itraconazole after oral and intravenous administration to horses. Am J Vet Res 66(10): 1694-1701.
Dunlop, A., E. Wright, S. Howlader, I. Nazrul, R. Husain, K. McClellan and F. Billson (1994). Suppurative corneal ulceration in Bangladesh. Austral NZ J Ophthalmol 22(2): 105-110.
Galán A, Martín-Suárez EM, Gallardo JM and Molleda M (2009). Clinical findings and progression of 10 cases of equine ulcerative keratomycosis (2004–2007). Eq Vet Edu 21(5): 236-242.
Gelatt, K., J. Gelatt and C. Plummer (2021). Veterinary Ophthalmic Surgery, 2nd Ed. Elsevier.
Hendrix, D. V. H., J. L. Stuffle and S. K. Cox (2007). Pharmacokinetics of topically applied ciprofloxacin in equine tears. Vet Ophthalmol 10(6): 344-347.
Herring, I. P., J. P. Pickett, E. S. Champagne, G. C. Troy and M. Marini (2000). Effect of topical 1% atropine sulfate on intraocular pressure in normal horses. Vet Ophthalmol 3(2-3): 139-143.
Keller, R. L. and D. V. Hendrix (2005). Bacterial isolates and antimicrobial susceptibilities in equine bacterial ulcerative keratitis (1993--2004). Eq Vet J 37(3): 207-211.
Lake, R. B., A. Brightwell, G. Cookson, A. Benschop, J. Burgess, S. Tait, A. (2018). Adapting to climate change: Information for the New Zealand food system. MPI Project. Sustainable Land Management and Climate Change Fund # SLMACC 405204. Accessed Nov 2022 from: direct (mpi.govt. nz)
McAllum, P. J. and C. N. McGhee (2003). Prescribing trends in infectious keratitis: a survey of New Zealand ophthalmologists. Clin Exp Ophthalmol 31(6): 496-504.
Moore, P. A., U. M. Dietrich, M. H. Barton, C. B. Mosunic, M. J. Chandler, K. P. Carmichael and D. E. Stooksbury (2005). The Influence of Rainfall and Temperature on the Frequency of Equine Fungal Keratitis. Invest Ophthalmol Vis Sci 46(13): 5067-5067.
Murray, M. J. and C. Grodinsky (1992). The effects of famotidine, ranitidine and magnesium hydroxide/aluminium hydroxide on gastric fluid pH in adult horses. Eq Vet J 24(S11): 52-55.
Mustikka, M. P., T. S. C. Grönthal and E. M. Pietilä (2020). Equine infectious keratitis in Finland: Associated microbial isolates and susceptibility profiles. Vet Ophthalmol 23(1): 148-159.
Ollivier, F. J., D. E. Brooks, M. E. Kallberg, A. M. Komaromy, M. E. Lassaline, S. E. Andrew, K. N. Gelatt, G. R. Stevens, T. D. Blalock, G. B. van Setten and G. S. Schultz (2003). Evaluation of various compounds to inhibit activity of matrix metalloproteinases in the tear film of horses with ulcerative keratitis. Am J Vet Res 64(9): 1081-1087.
Patipa, L. A., C. E. Sherlock, S. H. Witte, G. D. Pirie, R. D. Berghaus and J. F. Peroni (2012). Risk factors for colic in equids hospitalized for ocular disease. J Am Vet Med Assoc 240(12): 1488-1493.
Pearce, J. W., E. A. Giuliano and C. P. Moore (2009). In vitro susceptibility patterns of Aspergillus and Fusarium species isolated from equine ulcerative keratomycosis cases in the midwestern and southern United States with inclusion of
the new antifungal agent voriconazole. Vet Ophthalmol 12(5): 318-324.
Pfaller, J. B., S. A. Messer, R. J. Hollis, D. J. Diekema and M. A. Pfaller (2003). In vitro susceptibility testing of Aspergillus spp.: comparison of Etest and reference microdilution methods for determining voriconazole and itraconazole MICs. J Clin Microbiol 41(3): 1126-1129.
Prentice, A. G. and A. Glasmacher (2005). Making sense of itraconazole pharmacokinetics. J Antimicrob Chemother 56 Suppl 1: i17-i22.
Ruhil, S., V. Kumar, M. Balhara, M. Malik, S. Dhankhar, M. Kumar and A. Kumar Chhillar (2014). In vitro evaluation of combination of polyenes with EDTA against Aspergillus spp. by different methods (FICI and CI Model). J Appl Microbiol 117(3): 643-653.
Sauer, P., S. E. Andrew, M. Lassaline, K. N. Gelatt and H. M. Denis (2003). Changes in antibiotic resistance in equine bacterial ulcerative keratitis (1991–2000): 65 horses. Vet Ophthalmol 6(4): 309-313.
Schwink, K. L. (1992). Equine uveitis. Vet Clin North Am Eq Pract 8(3): 557-574.
Scotty, N. C. (2005). Equine Keratomycosis. Clin Tech Eq Pract 4(1): 29-36.
Ström, L., F. Dalin, M. Domberg, C. Stenlund, U. Bondesson, M. Hedeland, P. L. Toutain and C. Ekstrand (2021). Topical ophthalmic atropine in horses, pharmacokinetics and effect on intestinal motility. BMC Vet Res 17(1): 149.
Utter, M. E., E. J. Davidson and K. L. Wotman (2009). Clinical features and outcomes of severe ulcerative keratitis with medical and surgical management in 41 horses (2000–2006). Eq Vet Edu 21(6): 321-327.
Vallee, E., M. Wada, N. Cogger, V. Kelly, J. Marshall, J. Benschop, G. Macara and T. A. (2020). Effects of climate change on grazing livestock health in New Zealand. MPI Technical Paper No: 2021/10. ISBN No: 978-1-99-100384 (online). Accessed Nov 2022 from: Effects of climate change on grazing livestock health in New Zealand (mpi.govt.nz) Wehrman, R. F., A. J. Gemensky-Metzler, A. E. Zibura, A. B. Nyhart and H. L. Chandler (2017). Objective evaluation of the systemic effects of topical application of 1% atropine sulfate ophthalmic solution in healthy horses. J Am Vet Med Assoc 251(11): 1324-1330.
Weinstein, W. L., P. A. Moore, S. Sanchez, U. M. Dietrich, R. E. Wooley and B. W. Ritchie (2006). In vitro efficacy of a buffered chelating solution as an antimicrobial potentiator for antifungal drugs against fungal pathogens obtained from horses with mycotic keratitis. Am J Vet Res 67(4): 562-568.
A group of our colleagues consisting of Holly Blue, Peter Gillespie, Grace Reed, and Tony Parsons started up a specialised Equine Draft Breed Hospital. There were patients of four different draft breeds booked in for the first day of appointments.
1. Tony’s case was a Clydesdale
2. Regarding Grace and the Vet having the 11am appointment, one saw a Clydesdale and one saw a Percheron.
3. The appointment for the Haflinger was for one hour after Holly’s case. Using these clues and the adjacent grids, can you work out which Vet saw which patient at what time?
9am 10am 11am Noon BREED
TIME
CLYDESDALE SHIRE
See page 61 for answers
Kim J & Yoon M. The effect of serotonin and oxytocin on equine docility and friendliness to humans.
J Vet Behav. 2022; 50: 18-22. https://www.sciencedirect.com/science/article/pii/ S1558787822000144?via%3Dihub
Blood samples were collected from 20 university-owned mares and 9 geldings, comprising Thoroughbred, pony, Warmblood and Haflinger breeds and grouped into post-pubertal, adult, and aged horses. Plasma concentrations of serotonin [5-HT] and oxytocin [OXT] was measured by ELISA. The temperament of each horse was evaluated by three staff familiar with all the horses. The [5-HT] of Warmbloods, and the [OXT] of Warmbloods and Thoroughbreds were significantly higher than those of ponies. The [OXT] in the aged horse was considerably higher than that of post-pubertal horses. There was a positive correlation between the [5-HT] and [OXT]. Also, [5-HT] showed a positive correlation with horses' docility and friendliness toward humans. Perhaps plasma [5-HT] and [OXT] can be used as parameters to identify a horse's docility and friendliness to humans?


We thought you might appreciate having a listing of useful URL links to allied contact groups in your E-EVP - so here is a start. Please contact us to add or change any address.
AAEP - American Association of Equine Practitioners

ANZCVS - Australian & NZ Col lege of Veterinary Scientists



BEVA - British Equine Veterinary Association
ESNZ - Equestrian Sports NZ

EVA - Equine Veterinarians Australia

EVJ - Equine Veterinary Journal
Fédération Équestre Internationale Harness Racing NZ Massey Equine Veterinary Clinic
NZERF - NZ Equine Research Foundation


NZEVA - New Zealand Equine Veterinary Association NZVA - NZ Veterinary Association
SPCA – Society for the Preven tion of Cruelty to Animals-NZ

Thoroughbred RACEHORSE OWNERS Federation NZTR - NZ Thoroughbred Racing





RCVS - Royal College of Veteri nary Surgeons
SAEVA - South African Equine Veterinary Association

The Donkey Sanctuary https://www.vetpd.com/

Equine Dentistry and Maxillofacial Surgery
Edited by Jack Easley, Padraic Dixon and Nicole du Toit
This is the largest and most comprehensive textbook on equine dentistry and maxillofacial surgery ever published. It is a must-have for all readers interested in Equine Dentistry.
Equine Dentistry and Maxillofacial Surgery - Cambridge Scholars Publishing
The Beaufort Cottage Educational Trust is a small charity that aims to support educational projects and events for all those involved in the care of horses and disseminate knowledge of the best veterinary and management practices and thereby enhance horse welfare.

The BCET makes available many educational resources on a wide selection of topics and these include the recent Gerald Leigh Memorial Lectures that were added in 2021.
Watch the latest seminar here: Reproductive Efficiency in the Thoroughbred
Previous seminars are available at:
Angular limb deformities in foals and yearlings by Matt Coleridge, and What is OCD and how do we diagnose it? By Rhiannon Morgan
Other useful presentations can be viewed at:
• Gastrointestinal Disease in Foals
• Herpes Virus
• Foal Injuries and Diseases
• Radiography at the Sales
• Juvenile Orthopaedic Disease
• Proximal Suspensory Desmitis
• Suspensory Branch Injury
• Third Phalangeal Cysts
• Imaging the Neck and Back
• Fractured Ribs
• Pelvic Ultrasonography
• Wobbler Surgery
• Recurrent Laryngeal Neuropathy
• URT Function in the Young TB For Sale







At the time of writing this update, the current final year BVSc class is completing their final examinations before graduating as fully-fledged veterinarians. I’m sure they will be especially welcome this year as we seek to fill the deficiency in veterinary numbers in New Zealand. Despite challenges with staff and student absences due to COVID-related illness, we are delighted to
Recent photo of Vet Tower being removed.
In response to the need to supply more veterinarians for our growing client base, the School of Veterinary Science has received approval to train more veterinarians. This means that we will now have 175 allocated positions for training veterinarians starting in 2023. With this increase in student numbers, it is anticipated that we will need more staff, and to develop approaches to teaching larger numbers in our complex programme. This comes at a time when the veterinary curriculum is undergoing review and consultation across the profession, aiming to deliver one oriented toward competency-based outcomes. This is part of an international trend in veterinary education (https://cbve.org/).
And our Vet Tower (circa 1963) is no more!
Congratulations to Amy Lovett on her recognition as a Fellow of the Higher Education Academy (FHEA). This internationally recognised achievement reflects the focus of Amy and other colleagues at the School on the effective, high-quality teaching of our veterinary students. This HEA is part of an international move towards improving the teaching skills of university educators (https://www.advance-he.ac.uk/ fellowship/fellowship).
Our equine medicine resident, Jess Vokes, recently completed an externship at the University of Illinois, followed by attendance at the 28th International Veterinary Emergency and Critical Care Symposium. The proceedings make fascinating reading!

Luca Panizzi recently returned from Portland, USA, where he attended the October 2022 American College of Veterinary Surgeons symposium. His dedication to surgical excellence is appreciated by clients and referring veterinarians. Recently Luca assumed the role of Group Leader - Equine Academic at the School.
Sadly, Professor Chris Riley left Massey at the end of November after 10 years of service. Chris has been Equine Group Leader and Service Chief of the Equine Veterinary Clinic for several years and contributed to the training and
Recent photo of Vet Tower being removed.
professional development of many interns, residents and junior academics over the years. Chris is most proud of three of his many accomplishments, namely, working with Government in influencing the management of animals during disasters and incidents through the Veterinary Emergency and Rescue Team (VERT), his collaboration with Māori in Teaching and Learning, and editing the 3rd edition of Fraser’s Behaviour and Welfare of the Horse, Riley CB, Cregier SE, Fraser AF, eds., CABI, Wallingford, UK.
Chris has taken up a position as Chair of the Department of Clinical Studies at the Ontario Veterinary College, University of Guelph, Canada. Like many of us, travel restrictions and family difficulties internationally during COVID were a cause for consideration of family priorities. He and his family will move closer to his partner’s family in Ontario. He will be missed by his many colleagues and friends in New Zealand,
and we wish him the best for this new important step in his career. We just hope he has a thick winter jacket for the frozen North.
Many of the best research ideas come from private practice and industry. Please get in touch with us if you need advice on study design, applying for research funding, or potential collaborators. With the upcoming season of research funding rounds, it is hoped that we can soon announce our new projects for 2023.
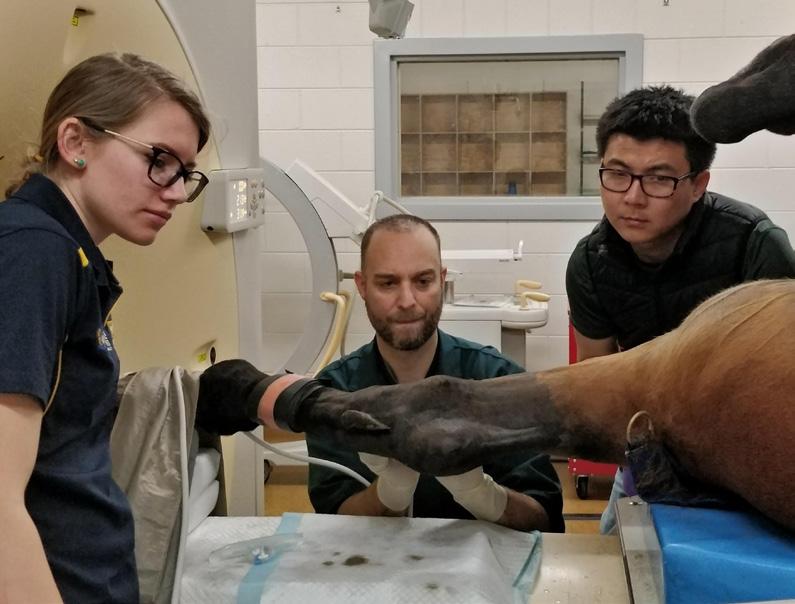
Legg KA, Bolwell CF, Gee EK, Gibson MJ, Rogers CW. Risk factors for horse falls in New Zealand Thoroughbred jumps racing. The Veterinary Journal, 2022, 105915.
Azarpeykan S, Gee EK, Thompson KG, Dittmer KE
Undetectable vitamin D3 in equine skin irradiated with ultraviolet light. Journal of Equine Science, 2022, 33(3), 45-49.
Legg K, Cochrane D, Gee E, MacDermid P, Rogers C physiological demands and muscle activity of jockeys in trial and race riding. Animals (Basel). 2022 Sep 8;12(18):2351. doi: 10.3390/ani12182351. PMID:
A multi-speciality group of vets and researchers with a broad range of expertise and knowledge

Our specialised services include:
• Elective and emergency surgery including but not limited to: Arthroscopy Colic surgery Airway surgery including laser surgery
• Investigation and treatment of: Lameness Poor performance Weight loss Respiratory disease Colic
• Neurology
• Ophthalmology
• Neonatology
• Cardiology
• Theriogenology
• Advanced imaging including: Digital radiography Ultrasonography Videoendoscopy and Gastroscopy Dynamic endoscopy Computed Tomography (CT)

Here we offer a synopsis of a general survey of (female) equine vets in Aotearoa on the tribulations and joys of pregnancy in relation to working in equine practices throughout the country. This survey was conducted via your NZEVA Executive with particular guidance from Katie Kindleysides and with editorial input from NZVA.

referred to the Department of Employment website (https:// www.employment.govt.nz/leave-and-holidays/parental-leave/ how-to-apply-for-parental-leave/). However, Health & Safety policies usually require clinical veterinary employees to inform their employer of a pregnancy as soon they are aware. Regardless, ‘the sooner they know, the sooner you can be kept safe’ (Crowe, 2014). This can be a positive discussion that helps alleviate some early anxiety around risks at work, despite negative fears you may have. Previously pregnant vets share their thoughts and experiences of early discussions with employers [Text Box 1].
Text Box 1: ‘Early in my first pregnancy I received a kick to the abdomen on farm. I hadn’t told anyone I was pregnant, so I didn’t feel I could talk about it then, either. Luckily it was so early my pregnancy was well protected, but I could have avoided the stress if I’d let my employer know.’
‘I was also offered a new job when I was openly trying to get pregnant/early pregnancy which was amazing to me at the time and will always be grateful for……. I can see it from both sides as pregnancy is a huge inconvenience for a practice especially if your job involves a lot of x-raying etc. From my experiences though I think having open conversations about this at the time of employment is the better way to go, however it does leave females more open to be discriminated against, no easy answer.’
‘When I told my employer about my pregnancy, they immediately made plans for me to avoid x-rays and anaesthesia and the team was incredibly supportive. They looked out for mine and my baby’s safety better than I did!’
Realising you’re pregnant can be an exciting yet daunting time for all. Alongside accommodating usual pregnancy concerns, equine vets and nurses must consider what changes are needed to minimise the additional risks our work brings to ourselves and our unborn children. Here we hope to address a few of the common concerns, using examples from previously pregnant, Kiwi equine vet mums and giving links to helpful advice.
The legal requirements on when to inform employers of your pregnancy are related to parental leave and readers are
‘When pregnant in practice with my first, the support and enthusiasm for starting a family from my bosses was lovely. On a day-to-day basis it sadly was not matched by a concern about how I was coping with working whilst pregnant. My advice to others would be to communicate clearly with your employers, know the legal info around pregnancy, take a support person to meetings and take notes of what is said.’
Many risks can be mitigated by delegation to or assistance by colleagues or nurses/technicians [Figure 1]. This time can be
Figure 1: With the use of adequate restraint, such as a suitable crush, and the availability of extra handlers, pregnant veterinarians can reduce the risks of physical injury due to trauma. (Photo courtesy of Pip Hendron)
Text Box 2: ‘Each time I've been pregnant I have happened to have had a new grad or young vet who does all the bits I can't do. Feedback from these vets on this has been good as they get collegial support but hands on experience and responsibility on trickier cases whilst the preggo vet is in the background giving advice, critiquing X-rays and scans where needed. Plus, the younger vet can get a good rapport with the client and massively improve on their clinical skills.’
a great opportunity to mentor students or recent graduates, as one vet found during her pregnancies, which then helped the team during her parental leave period [Text Box 2].
Worksafe (2017) advises employees have the right to refuse to work in situations which are hazardous or unhealthy, and in such circumstances they must inform the health and safety officer. Despite this, the below stories indicate pregnant equine vets can feel pressured to put themselves in situations they consider unsafe [Text Box 3]. Given the variation between individuals, it may not be clear to others which calls are suitable to attend as pregnancy progresses (Dickinson, 2016). Regular opportunities to discuss with management which procedures and jobs are not suitable for the pregnant practitioner (or require extra assistance) need to be made and
Text Box 3: ‘My boss was really understanding and accommodating of changes I needed, but I felt pressured to attend calls I wasn’t comfortable with when they were booked where there was limited ability to reschedule with someone else.’
‘I had no mentor, no one to check in with, no health and safety advice from work, my midwife, or GP. All that fell to me to manage my calls, equipment/help from colleagues, and I felt a huge sense of responsibility to keep doing everything I could’
‘I felt like I was burdening others if I couldn’t do something, and still the drive to prove girls can do anything in a male dominated (stud work) industry remained, but that’s my fault! All in all, I was treated very fairly while pregnant and did not have pressure put on to do anything unsafe’
outcomes shared with everyone in the equine team (especially those booking calls). A mentoring system as discussed by one previously pregnant vet can be useful to build trust for a truly honest conversation [Text Box 4].

Below is a non-exhaustive list of aspects of equine practice posing specific health and safety risk during pregnancy. Risks for each area are identified but specific recommendations have been purposely avoided as individual needs will vary. Where relevant, quotes have been included from previously pregnant working vets to give examples of how they mitigated risk or what they feel could have been done differently during their own pregnancies. Pregnant individuals should discuss risks of their clinical duties with their midwife/obstetrician as well as their employer/team when considering a personal Health & Safety plan.
During pregnancy accidental exposure to hormone products, in particular exogenous prostaglandin, may lead to complications such as miscarriage or premature labour (Scheftel et al., 2017). Many pregnant vets will continue to handle and administer these medications during pregnancy using gloves, but examples of needle stick injuries causing harm to pregnancy (Morris, 2000) remind us that extreme caution is needed. Although primarily used for treatment of gastrointestinal pathology, equine practitioners are reminded that misoprostal is a potent prostaglandin used heavily in human medicine for pregnancy management and is readily
Text Box 4: ‘Where I am we have a mentoring program with regular vet-to-vet coffee catch ups in work time. This is where all vets can have informative catchups with chosen mentors or just other colleagues to make sure they are happy how they are going. It's really nice for the younger vets too.’
absorbed across mucus membranes as well as via the gastrointestinal tract (Tang et al., 2007).
General information on many medications and their safety in pregnancy can be found on the BUMPS website (https:// www.medicinesinpregnancy.org/Medicine--pregnancy/) .
The information is aimed at those taking medications during pregnancy, but it is useful to help identify which compounds may be harmful to a pregnancy with accidental uptake.
Cytotoxic medications (including topical sarcoid therapies) carry significant potential harm to unborn children, who can be exposed via absorption by their mother. Home | WorkSafe New Zealand (2020) advises that pregnant workers are to be informed of the risks and offered alternative duties. Although beyond the scope of this article, there is concern cytotoxic agents can be transferred to infants via breastmilk (Albin, 2010) therefore caution around their use may remain upon return to clinical duties.
A successfully leak-tested circuit with active scavenging is considered very low risk for any personnel in theatre, but inhalation of unscavenged anaesthetic vapour is a significant risk to a pregnancy (Shirangi et al., 2009). The highest risk during equine anaesthesia is during connection and disconnection of the endotracheal (ET) tube to the circuit, as well as potentially during set-up, dismantling, and cleaning of the anaesthetic unit. Horses will also continue to exhale anaesthetic gases for a period post-surgery, especially where no washout period has occurred prior to the end of surgery. Considering comments made below regarding physical injury, there is a significant risk to especially heavily pregnant personnel involved in any anaesthetic induction or recovery (including for in-field procedure) due to working closely with ataxic/falling horses.

The maximum level of ionizing radiation for operators (set within the Radiation Safety Act 2016) is lowered to 1mSv annually for pregnant workers (Ministry of Health, 2022). Although the risks of high exposure are very low with safe radiographic technique, as it is usually an elective procedure that can be delegated, and dosimeter readings only give
Figure 2: Being able to sit comfortably for long procedures can help to reduce the risks of prolonged standing and prevent crouching, which can be more challenging during pregnancy. (Photo courtesy of Marieke van den Enden).
information after the event of high exposure, many feel it is safest for pregnant veterinarians and nurses/technicians to avoid radiography and scintigraphy all together. If clinical veterinary workers choose to remain working with radiography, stringent following of safety procedures is required, including keeping as far away from the primary beam as possible (i.e. no direct plate or generator holding). Where relevant, risks of scintigraphy are also to be assessed for pregnancy and the risk of handling of radionucleotides needs to be extended to those who are breastfeeding.
The UK’s Health and Safety Executive (HSE) has provided a useful guide on operator safety for use of ionizing radiation during pregnancy and breastfeeding, which is available at https://www.hse.gov.uk/pubns/indg334.pdf. The reader is advised to consider differences between UK and NZ legislation when consulting this document.
Individual lifting ability throughout each stage of pregnancy is variable and overloading can risk adverse pregnancy events
Text Box 5: ‘It is a difficult one and I took risks I shouldn’t have when pregnant, but it was my choice, and I was always supported by my employers to not to in terms of [avoiding] physical risks. I have had more close calls and near misses when not pregnant just due to the nature of the job and years I’ve been doing it. I worry more about something happening to me now that I have kids that need and depend on me than I did when pregnant (rightly or wrongly).’
‘I got kicked in the chest scanning a mare when I was pregnant. I think at that time (over 13 years ago) I was probably in the mindset of having to prove I could still be of use as a pregnant woman because there was quite an undercurrent of it being substandard. I didn’t want to let anyone down I guess.’
‘I remember a colleague telling me bending down for distal limb exams was one of the hardest things to continue doing as pregnancy progresses. I stopped doing foot exams during second trimester during one pregnancy as it was too uncomfortable but continued into third trimester the next time.’
‘I finished doing clinical duties at 34 weeks, on my final day I had a mini dental booked - thankfully it was the best mini mouth I’d ever seen and hardly needed any work as crouching that low was becoming almost impossible.’
(MacDonald et al, 2013). When making decisions on the physical limits of a pregnant veterinary worker it’s noted that estimations of loads lifted when working with animals are difficult to predict (Scheftel et al., 2017), and only a pregnant individual can identify what amount of physical loading on their body feels safe for them at any given point.
Current recommendations for physical exercise (including weights lifted) are focused on your fitness level prior to pregnancy rather than arbitrary limits and RANZCOG (2020) have produced a helpful fact sheet on this, which is available HERE. This guide also identifies how to spot harmful levels of exertion during pregnancy. In addition, pelvic floor physiotherapists (name withheld, 2022) advise pain, any leakage of urine, or a heavy/dragging feeling in the vagina during strenuous activity indicates overloading and a need to adapt. Related to injuries from overloading, relaxin hormone release in pregnancy starts in the first trimester and rises throughout pregnancy to increase joint laxity (Healthline.com, 2020). Along with a changing centre of balance, all of this equates to an increased risk of injury from physical exercise/ work during pregnancy, alongside the risks of pregnancy related pelvic injury, such as prolapse.
Horses are no more likely to kick, rear, or rush forward when those around them are pregnant, but pregnancy leaves the body more exposed, and the consequences of injuries are higher. Before 12 weeks gestation the pregnant uterus is well protected within the pelvis but becomes more exposed throughout the second trimester and the resultant expansion of the abdomen becomes physically restrictive, particularly into the third trimester. This alongside the changing centre of gravity, which may affect balance, contributes to a lowered ability to move quickly and safely out of the way, particularly when bent/crouched down. Previously pregnant vets shared several experiences and thoughts on how pregnancy affects the risks of equine work [Text Box 5 and Figures 2 & 3].
Tiredness and exhaustion can be regular concerns of those in equine veterinary roles, but pregnancy contributes to this with generalized exhaustion and potential sleep disturbance. Prolonged standing and shift/night work has been associated with negative outcomes in pregnancy (Mozurkewich et al., 2000) and the long hours of vet work specifically have been found to increased risk of adverse outcomes of pregnancy (Shirangi et al., 2009). Regardless of physical ability and safety concerns, exhaustion alone may be the driver of a change in after-hours duties and work hours as well as an increase in sit-down breaks. Vets sharing their personal experiences discussed needing to reduce hours as a consequence [Text Box 6].

Keep
Being on your feet too long is unhealthy in pregnancy, but so is being overly sedentary (RANZCOG, 2020). In practice
Text Box 6: ‘Working part-time throughout pregnancy meant I could cope with the long days on my feet better as when I wasn’t in work I could take it easy and recoup.’
‘I was surprised how tired I was and had to take it easier in terms of hours and workload as a result.’
this is unlikely to be a concern but needs consideration if you temporarily move to an administrative role. For ambulatory vets, long frequent car journeys can be problematic. Keep cool & hydrated (and make space for pit stops!)
It’s common knowledge that pregnant women feel the heat more and related to this is an increased risk of dehydration that can present risks to your pregnancy’s health (Tommy’s, 2022). The need to keep hydrated only adds to the expected increased frequency of urination so be prepared to build regular bathroom breaks into your day. Heat exhaustion is most of concern to those doing physical outside calls during summer [Text Box 7].
Morning sickness or hyperemesis gravidarum is hugely variable both between women and between repeat pregnancies. In severe cases it is rather devastating as
Text Box 7: ‘‘Working an ambulatory role during summer was hardest during the first trimester as I was still doing as much as pre pregnancy, I was exhausted and dehydrated really quickly, and owners didn’t expect it as they didn’t know I was pregnant. We had to put limits on things like how many dentals I could do at each call.’
Text Box 8: ‘I struggled to keep water down without vomiting for the first trimester so was hospitalised on fluids and was so sick I couldn’t work at all for the 1st 3 months before I had a big belly. So, I had to take 3 months of my maternity leave before I even looked pregnant! This was a total shock to me as I was super fit and doing long distance running before I got pregnant. I presumed I’d just cruise through pregnancy and keep working till I dropped, but no such luck! I had to take dry rice crackers with me to nibble on all day in the car and at the clinic, when I did get back to work later in my pregnancy, to stave of the nausea! Not everyone feels sick, and I was always so envious of those who could eat normally and enjoyed being pregnant! My 2nd pregnancy was worse that the 1st with extreme nausea. My girls always say they nearly killed me before they popped out to say hello!’
attested to by one colleague [Text Box 8] and may well have been the demise of Charlotte Bronte
12% pregnant women have a high level of depression (this doesn’t include those with anxiety or mild levels of depression). It’s acknowledged 50% women who suffer depression in pregnancy will suffer from post-natal depression. In addition, 1 in 50 men have been found to have symptoms of depression prior to the birth of their child, 4.3% of fathers are known to suffer from depression in the post-natal period (PADA, 2017). In an industry where mental health concerns are already high throughout; it seems
Text Box 9: ‘One of the cool things is how women [in practice] actually support each other and pick up the slack when someone else has stuff going on. Also, so many guys have young kids, so they really understand.’
pertinent to remind us all to be aware of the signs personally and in those around us and be prepared to offer support and direct them to appropriate help. Finally, PADA is a site focused on ante- and post-natal mental health where further information can be found for expectant and current parents [Text Box 9].
Below equine vets have given some great insight into when they stepped back during their pregnancies alongside what allowed them to keep going and what indicated a change was needed. Although examples from the likes of peers can be helpful guides to plan when to step back from various clinical duties, as shown below, each pregnancy can be very different and listening to your body is vital [Text Box 10].
As a pregnant veterinarian you may hit a point where even a clinical examination doesn’t feel comfortable, but you may not feel ready to step out the clinical environment all together and wish to still contribute to the team. Below are some ideas on areas clinical where workers can assist as their physical needs required them to step back. They have come from personal experience, experiences of peers, and suggestions from Carolyn Crowe’s BEVA presentation (2014) [Text Box 11].
• Mentoring students and recent graduates
-Allows learning from your experience whilst providing the pregnant individual with an extra pair of hands, especially during higher risk procedures.
• Clinical administrative task
-Is the radiography manual up to date? Do you need to audit some services/prices? Does your newsletter archive need an update?
-Whether it’s for compliance, general management, or marketing, all of these activities make good use of a practitioner’s brain and can be financially beneficial to a veterinary practice, but they are often the non-urgent tasks that get side-lined.
• Call triage and client communications.
-Can be useful support for customer service workers especially during vet shortages when scheduling appointments may be trickier.
-Can be an opportunity to use an experienced practitioner to train other members of the team on appropriate length of time for appointments determining the priority of a call.
-A non-clinical veterinarian can also be used to report the likes of laboratory reports to client where the case vet feels it is appropriate.
For some working less hours (as needed) through pregnancy can be the best option to remain active in practice for as long as you wish to. This may involve taking leave or a temporary change in contracted hours depending on how it can be accommodated by your employer.
Whether leave starts as you’d plan or is brought forward unexpectedly, walking away from vet practice for a prolonged period is often unknown territory. For some, it’s so full of new challenges and social interactions that little thought is given to our careers, but for others it’s monotonous, isolating and
Text Box 10: ‘I did repro work until 2 weeks pre-partum, and general first opinion work till 3 days pre-partum - was meant to have 2 weeks off, but baby arrived early.’
‘I was working until around 7 months gestation. Timing worked out so I was off clinics during first trimester. Then avoided x-raying and physically rough situations. Easier as we had so many students and residents though.’
‘During both pregnancies I noticed a change in my physical ability and energy levels around 32 weeks that initiated conversations about taking a step back. Until then I’d felt fine with long workdays but suddenly everything was harder and more uncomfortable.’
‘Employers and clients were great, looked out for me, were cautious about what they asked me to do. I was probably happier carrying on than I needed to be, but I was only small and still felt comfortable and stable in most situations. I stopped doing yearling work, wrestling foals, and dealing with limbs/flexions etc. by about 6 months, and was very fussy about the people I had holding and handling horses for me.’
‘My final after hours weekend (at 28weeks) involved treating a stallion and I was really grateful a colleague was available to take on the care as I just didn’t feel safe even injecting him.’
‘It was easier when pregnant with my second child as I took the role during the first trimester with everyone being aware. I was an extra person so although I still felt guilty for not being able to contribute as much as I could have, it wasn’t as hard as taking a step back in a busy team and watching my workload get added to a colleague's day list. Ultimately in an industry that tends to have overworked employers working within a close team, it's hard to feel OK about putting yourself first to take a step back whether it’s for pregnancy, injury, or mental health - it’s something we all need to get better at doing and accepting of in our peers.’
there’s a wish to be back using their vet brain. Often it differs from our expectations. Prior to heading on leave there is value discussing with your employer whether you wish to have contact and at what level throughout your leave, including how to manage clients that contact you directly. Would you still
Text Box 11: ‘Later in pregnancy when I stepped back from clinical duties on my own request, I could still be involved in cases by working closely with reception to triage and provide veterinary advice to clients alongside reporting clinical progress and lab results to clients for general matters. I was also able to act as a sounding board to the new grad.’
‘I was fortunate to be working part-time throughout pregnancy, having a break midweek really helped me cope with the long days and I had to plan at least one of my non-workdays each week to do nothing but rest.’
like to attend clinical discussion or be available to assist for certain procedures? Would you like to receive practice emails or prefer to not be contacted? Just as for pre-birth plans, accept thoughts on this may change and regularly review if
Text Box 12: ‘Once I was on leave it was as if I’d left. I was grateful there was no pressure for back to work discussions, but I also felt isolated from the team and lost my feeling of purpose within it.’
‘When I went on maternity Ieave, I and my mentee would stay in touch if they ever had something they wanted to discuss (which I found nice as I felt needed and useful as a horse vet not just as a mum).’
your original decisions are still right for you. Below are two differing experiences of work contact during parental leave [Text Box 12].
For employed workers on paid parental leave there is the option to discuss use of ‘Keep in Touch (KIT) days’ with your employer, details are available at https://www.employment. govt.nz/leave-and-holidays/parental-leave/types-of-parentalleave/keeping-in-touch-days-2/. These can be useful to keep you involved with the team whilst you are away from clinical duties and help you gauge if you’re ready to return to work earlier than originally planned.
It feels incomplete to not touch on the difficulties so many sadly face when hoping to start or expand a family. It’s estimated over a quarter of New Zealanders will face infertility as some point (Fertility NZ, 2022) and at least 1-2 of every 10 pregnancies end in loss (Ministry of Health, 2022). Often these heart-breaking situations occur before many are aware a couple is trying to get pregnant. This can result in the devastation being compounded by the feeling that their tragic experiences can’t be shared, and many would-be parents continue to work as they face the physical and emotional pains. We work in client facing roles among a workforce strong in those of childbearing age; such personal grief can be very difficult to manage when others’ obvious pregnancy journeys are visible around us and clinical situations can be triggering where they echo personal difficulties. When those walking infertility or loss journeys experience pregnancy, many of the risks we face working in the veterinary industry can drive additional anxiety, so a more cautious approach may be taken. This isn’t always understood by management or colleagues who may not be aware of the story. In Text Box 13 are some experiences of such losses from equine practitioners: Fertility New Zealand (https://www.fertilitynz.org.nz/) offer
Text Box 13: ‘When I had my miscarriage no one apart from some of the directors knew, it was devastating’ ‘I had 3 miscarriages before 12 weeks that my employers all new about, in a normal job they would have been none the wiser.’
‘I delivered a stillborn baby during second trimester after an unexpected complication. Clients had only just started to be aware of my pregnancy. Returning to work I didn’t know who knew and who didn’t so it was really important to me to have everyone made aware of the loss to avoid someone putting their foot in it. Even though the complication wasn’t work related, I was much more anxious during the next pregnancy and found everyone’s excitement for me difficult.’
information and support to those affected by infertility. SANDS New Zealand is a charity focused on supporting bereaved parents through miscarriage, baby loss, and infant death. Readers are also reminded that you now have a legal right to use bereavement leave for a loss at any point in pregnancy (Employment New Zealand, 2021).
Pregnancy is an individual journey that can bring up the unexpected, be prepared that what you envisaged yourself doing and what you’ve witnessed others do may not end up being what you do. Plan for frequent communication with your employer and understand they cannot know how you are doing without open and honest discussion. In return employers must also be accepting that their previous experiences of pregnancies are a guide not a precedent. Where challenges rise all must be prepared to look for solutions and understand some compromises may be needed to accommodate specific requests but ultimately, it’s about keeping everyone safe.
With many thanks to the equine vet mums of Aotearoa NZ who kindly took time to openly share their tribulations and joys of pregnancy to make this article possible, the power of your stories is a gift to our future vet parents.
Albin, K. (2010). Administering Chemotherapy: is it safe for pregnant or breast-feeding veterinary technicians. Vet Tech October 2010 (E1-E5)
Crowe, C. (2014). Equine Practice and Pregnancy. [Online Lecture] BEVA, April. Available at: https://cpd. ebeva.org/course/view.php?id=168 (Accessed: 20th Sept 2022).
Dickinson, A. (2016). Pregnancy in Practice. VetScript, 29(4), pp.54-57.
Employment New Zealand (2021) Bereavement Leave to Cover Miscarriage/Stillbirth [Online] Available at:https://www.employment.govt.nz/about/news-and-
updates/bereavement-leave-to-cover-miscarriagestillbirth/#:~:text=The%20law%20change%20allows%20 an,ends%20by%20miscarriage%20or%20stillbirth (Accessed 19th October 2022).
Fertility NZ (2022). Trouble Conceiving [Online]. Available at: https://www.fertilitynz.org.nz/information/troubleconceiving/ (Accessed 15th October 2022).
Health & Safety at Work Act 2015. Available at: http:// www.legislation.govt.nz/act/public/2015/0070/latest/ DLM5976660.html (Accessed: 15th October 2022).
MacDonald, L.A., Waters, T.R., Napolitano, P.G. et al. (2013). Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol, 209(2), pp.80-88.
Ministry of Health (2022) Miscarriage and Stillbirth [Online]. Available at: https://www.health.govt.nz/yourhealth/pregnancy-and-kids/services-and-support-duringpregnancy/miscarriage-and-stillbirth (Accessed 15th October 2022).
Morris, S. (2000) Health and Safety in Practice. In: Proceedings of the annual seminar of NZ Veterinary Nurse Association: NZVA Conference, 8-11th June 2000, Auckland, NZ. Pp.85-94.
Mozurkewich, E.L., Luke, B., Avni, M. and Wolf, F.M. (2000). Working conditions and adverse pregnancy outcome: a meta-analysis. Obstet Gynecol, 95(4), pp.623635.
RANZCOG (2020). Exercise during Pregnancy. Available at: https://ranzcog.edu.au/wp-content/uploads/2022/05/ Exercise-during-pregnancy.pdf [Accessed 5th October 2022].
Scheftel, J.M., Elchos, B.L., Rubin, C.S. and Decker, J.A. (2017). Review of hazards to female reproductive health in veterinary practice. J Am Vet Med Assoc, 250(8), pp.862872.
Shirangi, A., Fritschi, L. and Holman, C.D.A.J. (2009). Associations of unscavenged anesthetic gases and long working hours with preterm delivery in female veterinarians’. Obstet Gynecol,113(5), pp.1008-1017.
Tang, O.S., Gemzell-Danielsson, K. and Ho, P.C. (2007). Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynecol Obstet, 99, pp.S160-S167.
Tommy’s (2020) How Much Water Should I Drink in Pregnancy [Online], Available at: https://www.tommys.org/ pregnancy-information/im-pregnant/nutrition-in-pregnancy/ how-much-water-should-i-drink-pregnancy (Accessed 15th October 2022).
Worksafe (2017). Your Rights and Obligations. Available at: https://worksafe.govt.nz/managing-health-and-safety/ workers/your-rights-and-obligations/ (Accessed: 15th October 2022).
Worksafe (2020). Cytotoxic Drugs: Good Practice Guide. Available at: https://www.worksafe.govt.nz/ topic-and-industry/health-and-safety-in-healthcare/ cytotoxic-drugs/#:~:text=Exposure%20to%20cytotoxic%20 drugs%20can,related%20waste%2C%20are%20at%20risk (Accessed: 5th October 2022).

Listen to these audio PodCasts that are discussions with the authors of selected EVE papers on topics including:
Small intestinal intussusception
Hydroxyethyl starch solutions in fluid therapy
Sand enteropathy
Distal limb cellulitis Renal disease
Responsible antimicrobial use Difficult Horses
Tracheal Perforations
Cannabinoids
White line disease
Hindlimb proximal suspensory desmopathy
Stifle radiography
Normal radiographical variants Cutaneous squamous cell carcinoma Multimodal strategies for equine analgesia
Electroacupuncture
Listen on your phone with the Podbean Podcast App & Player

Equine odontoclastic tooth resorption Atypical myopathy
Equine rhabdomyolysis syndrome
Large colonic impactions
Whisenant KD et al Prognosis for survival to discharge and racing performance in Thoroughbred foals treated for single joint septic arthritis (2009-2016). Eq Vet J 2022 Oct: DOI 10.1111/evj.13892
Data were collected from one large KY equine hospital records for 95 cases of TB foals 6 months of age or less suffering from a single septic joint of presumed haematogenous origin without recognised systemic sepsis or other serious comorbidity, compared with a group of maternal sibling control foals. Overall, the prognosis for survival was high (93%). The last measured synovial cell count prior to hospital discharge or euthanasia (OR 0.5, p = 0.002, 95% CI: 0.3-0.8) was an indicator of poor prognosis for survival to discharge. Total winnings per career were the only statistically significant racing performance variable between cases and paired controls (IRR 0.7, p = 0.05, 95% CI: 0.5-0.99). Thus, while total winnings were reduced compared with maternal siblings, these TB foals with single joint septic arthritis had a favourable prognosis for survival and for starting in a race.
NOTE: There were many limitations to this retrospective study including great variation in prior therapy, specific joint involved, antimicrobial selection, varied absence of full clinical data, and use or not of a surgical procedure. The data also informs that 62 of the 95 affected foals (65%) subsequently raced, whereas 147 of 190 maternal sibling, matched control foals (77%) subsequently raced.

Following on from our paper on the practical aspects of euthanasia by Emma Gordon [Equine Euthanasia, EVP June 2022; 47(2): 41-43] we offer a discussion in two parts on the issues surrounding any decision for euthanasia. The first part is a bibliographic review given here, and the second part on page 59 is on reasons for, and considerations to have, at the time of a request or need for euthanasia.
“Euthanasia is available to the veterinarian when assisted death is believed to be in the best interests of the animals’ welfare relative to other practical options” (Yeates, 2010).
Utilising a welfare assessment tool can help with deciding whether a horses’ welfare or quality of life (QoL) is able to be improved or sustained at its current level or to inform a decision about euthanasia (Long, et al., 2022). The most up to date model of assessing animal welfare is the 2020 version of the five domains model where a person can consider a horse’s wellbeing according to these areas: 1. Nutrition
The first three domains are known as the “survival-critical effects”, while domain 4 focusses on the animals’ interaction with the environment, non-human animals and humans; and domain 5 is the resulting animals’ perception in response to external circumstances (Mellor, et al., 2020). This model considers the positive and negative experiences that influence the horse’s wellbeing (Bell & Rogers, 2021).
Often welfare models are used informally and are based on the knowledge and intuition of an experienced health professional and/or horse owner. Utilisation of objective and subjective measures and adjustment of criteria weightings allow welfare models to be tailored to individual cases (Long, et al., 2022). Whole animal indicators such as general attitude or a Qualitative Behaviour Assessment (QBA) can also be utilised, where indicators such as anxiousness, aggression or restfulness can indicate the horse’s general wellbeing (Long, et al., 2022).
In a presentation given by Dr Kathleen Anderson at the Pan American Racing Conference (2017), she described a method for assessing the physical wellbeing of a horse using movement, eating, drinking and weight. These four aspects of
wellbeing can be graded according to quality i.e. easy to move and good weight, through deteriorating, and to being unable to mobilise with poor condition (Anderson, 2017).
Table 1 gives the decision-making guidelines for euthanasia that are recommended by Dr Anderson and contained in the AAEP guidelines.
A horse should not have to endure the following:
• Continuous or unmanageable pain from a condition that is chronic and incurable.
• A medical condition or surgical procedure that has a poor prognosis for a good quality of life.
• Continuous analgesic medication and/or box stall confinement for the relief of pain for the rest of its life.
• An unmanageable medical or behavioral condition that renders it a hazard to itself or its handlers.
Research suggests that the majority of the time, horses are euthanised due to physical reasons, ‘old-age’ or age-related conditions (Bell & Rogers, 2021; Ireland, Clegg, McGowan, Platt, & Pinchbeck, 2011). Studies have reported laminitis related problems (25% of participants), colic (21%), and lameness (20-24%), age-related deterioration (20%) are the most common physical causes of euthanasia (Pollard, Wylie, Newton, & Verheyen, 2020; Ireland, Clegg, McGowan, Platt, & Pinchbeck, 2011). Having poor owner-perceived hoof quality further increased the rate of euthanasia.
Research done by Bell & Rogers (2021) shown in Figure 1, shows that of the 211 horses included in the study, owners reported the majority were euthanised due to physical causes, except for 11 horses that were deemed to be ‘dangerous. This research was a questionnaire of people who had had a horse euthanised in the past, which revealed that colic, arthritis, and lameness (19% each), pain, old age, or general
Figure
quality of life (15%) were the main causes reported (Bell & Rogers, 2021).
Colic is shown to be main cause in younger horses, as demonstrated in a euthanasia stress response study of 40 horses aged 6 to 24 years which revealed 16 horses were euthanised due to colic (Gehlen, Loschelder, Merle, & Walther, 2020). Another study of 55 horses admitted to hospital for colic symptoms 18 were euthanised: 4 during surgical intervention, 4 during medical management, 3 from catastrophic injuries in anaesthetic recovery, 2 following a second round of surgical intervention. The average age of these horses was of 13.6 years range (6-21 years) (Lightfoot, Burford, Bowen, & Freeman, 2021).
Ireland, Clegg, McGowan, Platt & Pinchbeck (2011) described other factors which increased the risk of mortality in older horses included being underweight, increased clinical signs, and pain limiting normal daily activities. Age has a considerable influence with horses aged over 30 years are five times more likely to be euthanised than horses in the 15-19 years age group (Ireland, Clegg, McGowan, Platt, & Pinchbeck, 2011). Age related conditions such as Pituitary Pars Intermedia Dysfunction (PPID), diseases where age is a risk factor and declining immunity may contribute to mortality in geriatric horses (McFarlane & Holbrook 2008, Freeman & Schaeffer 2001, Garcia-Seco et al, 2005, cited in Ireland, Clegg, McGowan, Platt, & Pinchbeck (2011).
It is understood that horses are more likely to be euthanised for

All you must do is write a clinical report that is published in the EVP, and your contribution may be eligible for one of several prizes of $150.00 that the EVP has available each year.
The EVP Editorial Group wish to promote the sharing of your interesting cases and practice tips
euthanasia. From Bell & Rogers, 2021.
physical reasons rather than issues relating to the horses’ affective state or behaviour although some horse owners may choose to euthanise due to dangerous behaviour (Bell & Rogers, 2021). There is a suggestion that dangerous or aggressive behaviour is linked to possible underlying physical issues. Aggression can be an indicator of pain and prolonged stress can lead to physical issues (Long, et al., 2022; Green, 2022). When humans’ safety is compromised, due to a horse that has become dangerous and/or the horse is no longer of “use” then euthanasia may be implemented (Green, 2022; Jones, 2022). Assessment of the horsemanship ability of an owner caring for a dangerous horse is important when considering euthanasia.
Further, changes to a horse’s mental health may include depression and distress due to box rest or loss of a companion. Horses which are showing obvious signs of distress, with little or no improvement may be euthanised. Some abnormal behaviours such as crib biting, wind sucking or weaving have become normalised within the industry, associated with stabling/routine management, therefore owners often don’t recognise these behaviours as early indicators of pain, fear, and stress (Bell & Rogers, 2021). It is not unusual for two horses to be euthanised together to avoid a stressful experience for the horse left behind if an alternative suitable companion cannot be found (Jones, 2022).
Euthanasia can be seen as a “positive welfare decision”

with the wider equine veterinary community, so please contribute.
Every case, technique, test and interpretation are different, no matter how experienced we are or how routine the case is, so there is always something for us to learn from each other.
Take photos, dig out your diaries, get keyboard tapping and share your views with colleagues. You could be $150.00 richer for it!
Please send your clinical reports to the EVP Editor for consideration.
Joe is happy chat with you about any articles or ideas you might have.
Please contact Joe at evp.editor@gmail.com or on 027 437 3651.
in terms of being “able to end an animals’ suffering” and/or prevent a lifetime of suffering. Changes in an owners’ situation such as redundancy or illness may mean they are no longer able to care for a horse, this can be further complicated by horses that are not viable to be rehomed or sold e.g. horses that require high levels of care, months of box rest, expensive treatment (Green, 2022). Consideration needs to be taken of the horses’ future QoL (Long, et al., 2022). Where a horse has lost its utility i.e., able to be ridden, used for competition/ racing, a situation arises where the horse has insufficient value to justify the costs of upkeep (unless the horse has significant sentimental value). Some horses have an alternative use such as mares being used in the broodmare paddock. In one study, other factors influenced the rate of euthanasia including being a cross bred vs being pure bred which resulted in higher mortality rates on multivariate analysis in older horses (Ireland, Clegg, McGowan, Platt, & Pinchbeck, 2011).
While the reasons for euthanasia quite clearly show the most probable cause is physical issues, the research available is limited to owner-reported data. The study conducted by Pollard et al (2020) included only horses with laminitis while Ireland et al (2011) included only horses over the age of 15 years. Further there is no NZ based research in this regard.
It is important to consider the timeliness of euthanasia, with ethical and welfare implications to consider where euthanasia is delayed, particularly the prolonged suffering of the horse (Cameron, et al., 2022; Anderson, 2017). Reports suggest that people are reluctant to decide on implementing euthanasia for reasons including: “financial cost, emotional attachment, peer pressure, negative attitudes towards killing, poor recognition of pain and stress indicators” (Anderson, 2017; Bell & Rogers, 2021). A person may not be able to afford the cost of treatment required to sustain life, the cost of euthanasia or may not want to put the horse to sleep, leading to welfare being compromised (Jones, 2022; Lightfoot, Burford, Bowen, & Freeman, 2021; Jones, 2022). Studies have highlighted the concept of “responsibility guilt”- where a person feels guilty for putting a horse down (Clough, Roshier, England, Burford, & Freeman, 2021). Further it has been identified that some horse owners showed an inability to recognise pain or stress in horses leading to further delays in euthanasia. Consideration must also be given to the owners’ willingness and resources to continue intervention (Long, et al., 2022). It is not acceptable to allow a horse to die an emaciated death from natural causes (Anderson, 2017). Therefore, veterinarians must ensure that owners have a clear understanding of the options presented to them.
Anderson, K. (2017). Compassionate considerations
for end of life. Pan American Conference. Washington. Retrieved August 15, 2022, from https://www.youtube.com/ watch?v=tNAmp4tvWhA
Bell, C., & Rogers, S. (2021). Attitudes of the equestrian public towards equine end of life decisions. Animals, 11(6), 1176. Retrieved August 15, 2022, from https://www.ncbi. nlm.nih.gov/pmc/articles/PMC8232243 /
Cameron, A., Pollock, K., Wilson, E. et al. (2022). Scoping review of end-of-life decision making models used in dogs, and cats and equids. Vet Rec, 191(4). Retrieved August 22, 2022, from https://doi.org/10.1002/vetr.1730
Clough, H., Roshier, M., England, G., Burford, J., & Freeman, S. (2021). Qualitative study of the influence of horse-owner relationship during some key events within a horses lifetime. Vet Rec, 188(6). Retrieved August 22, 2022, from https://doi.org/10.1002/vetr .79
Gehlen, H., Loschelder, J., Merle, R., & Walther, M. (2020). Evaluation of stress responses under standard euthanasia protocol. Animals, 10(485), 2076 - 2615. doi: 10.3390
Green, S. (2022, April 14). Making an end of life decision for your horse: how to know when its time. (S. Green, Interviewer) Retrieved August 22, 2022, from https://www. youtube.com/watch?v=ZnnuWMmAfI8
Ireland, J. L., Clegg, P. D., McGowan, C. M., Platt, L., & Pinchbeck, G. L. (2011, Sept). Factors associated with mortality of geriatric horses in the United Kingdom. Prev Vet Med, 101(3-4), 204-218.
Jones, E. (2022). Horse and Hound. Retrieved from Better a week early than a day late: the hows and whens of equine euthanasia: Horse and Hound https://www. horseandhound.co.uk/news/better-a-week-early-than-a-daylate-the-hows-and-whens-of-equine-euthanasia-784923
Lightfoot, K. L., Burford, J. H., Bowen, I. M., & Freeman, S. L. (2021). Prospective study exploring factors assocaited with the euthanasia of horses referred for colic. Eq Vet Edu, 33, 46. Retrieved August 2022, 20
Long, M., Durnberger, C., Jenner, F. et al. (2022). Quality of Life within Horse Welfare Assessment Tools: Informing decisions for chronically ill and geriatric horses. Animals, 12(1822). doi: https://doi.org/10.3390/
Mellor, D. J., Beausoleil, N. J., Littlewood, K. E. et al (2020). The 2020 Five Domains Model: Including humananimal interactions in assessments of animal welfare. Animals, 10(10). Retrieved August 30, 2022, from https:// doi.org/10.3390/ani10101870
Pollard, D., Wylie, C. E., Newton, J. R., & Verheyen, K. L. (2020). Factors associated with euthanasia in horses and ponies enrolled in a laminitis cohort study in Great Britain. Prev Vet Med, 174. Retrieved August 15, 2022, from https://www.sciencedirect.com/science/article/abs/pii/ S0167587719305720
Yeates, J.W. (2010), When to euthanase. Vet Rec, 166: 370-371. https://doi.org/10.1136/vr.c226


Following on from our paper on the practical aspects of euthanasia by Emma Gordon [Equine Euthanasia, EVP June 2022; 47(2): 41-43] we are offering a discussion in two parts on the issues surrounding any decision for euthanasia. The first part, a bibliographic review appeared on page 55, and the second part given here is on reasons for and considerations to have at the time of a request or need for euthanasia arises.
When owning or caring for a horse we need to consider a range of issues to ensure we can meet the responsibilities of the duty of care. These include having suitable facilities to keep the horse and being able to meet the cost of feeding and maintaining a healthy and happy horse.
When owning any animal we must consider the five domains of Nutrition, Environment, Health, Behaviour and Mental State. The owner, or person responsible (PR), must also realise that situations will arise where there will need to be a discussion around euthanasia. Few horses genuinely die of old age. Man has usually intervened prior to that either on welfare or economic grounds.
The Animal Welfare Act 2015 recognises the horse as a sentient being. We must treat them with respect and in a way avoids suffering and maximises their well-being. It is our responsibility to take action to avoid or minimise and alleviate any pain or suffering.
Horses need to be fit for purpose. They need to be safe for everyone to be around. They need to be reliable and affordable.
From time to time there will be a discussion around a situation that a horse is in and when the decision to euthanise should be made.
Considering the horses current and future overall well-being, the person responsible should ask, from the horses' point of view: ‘Is this a good life?’
For each reason we may be considering euthanasia there are a range of things that need to be considered that may help in the decision-making process. These reasons for euthanasia and considerations to be undertaken at the time of euthanasia are discussed below.
Old age is often the reason for a talk about euthanasia. The horse's ability to display normal behaviour is important. It should be able to move about, lay down and get up as it
wants. It should have suitable feed available and be able to easily eat. It should not have any difficulty urinating or defecating.
It is better to make the decision to euthanise when the PR is in control of the situation rather than it becomes an emergency. The quote “Better a week too early than a day too late” should be the mantra for the PR to bear in mind.
An emaciated horse requires immediate action to alleviate the situation. This requires fixing the cause of the poor body condition and providing a suitable feeding plan. If this cannot be done with the PR, or re-homing immediately, then euthanasia should be considered.
Many diseases can be cured but the cost/resources required, as well as the future suitable purpose of the horse, need to be fully understood.
Horses are a herd animal. Isolation and/or confinement can lead to behavioural issues. Occasionally these behavioural issues can lead to a horse being unrideable or dangerous to handle. The Animal Welfare Code states that horses should be kept with at least one other social companion, or at least where they can see or hear other horses. This also raises the question of what to do with the “paddock mate” who is left alone when the main horse dies.
While some behaviours will be tolerated in one situation, they may make a horse unsuitable to re-home. For example, a good racehorse who is professionally handled, but with the knowledge that it randomly kicks out, will not be suitable to rehome to an inexperienced rider or family home. Horses need to be safe, predictable, and reliable to be around.
We need to clearly understand the pathway for any horse
that is in a compromised situation to getting it back to being healthy, happy, safe, and suitable for purpose.
If this pathway is not clear and fully understood, and achievable by all those involved in the care of the horse then euthanasia must be considered.
All the considerations need to fit within the five domains model of animal welfare. There must be adequate nutrition. The environment and health status of the horse, along with it having the opportunity to display normal behaviour, must be considered. Together, all of these should allow the horse to be in a situation of having a positive mental experience.
Future suitability for primary use.
Many horses are bred for a specific purpose. If the horse is no longer suitable for the purpose, or it’s unlikely it can be returned to that state, and there is no realistic option to rehome, then euthanasia is a sensible choice.
Future alternate purpose – this owner of re-homed.
Many horses may have another use or purpose after they retire from the activity they were originally bred for. This may be with the current owner or there may be re-homing opportunities.
The pathway needs to be clear and achievable within a timeframe that does not leave the horse in a compromised situation unduly long.
Re-homing should not be an opportunity to pass the
responsibility of any disclosed, or undisclosed issue on to someone else, without the new PR fully understanding the requirements to care for that horse.
Impact on the horse during recovery.
With any injury or medical condition there must be a full conversation prior to starting treatment about the prospects for the horse. Particularly in the case of recovery from injury, there may be significant periods of pain and/or discomfort for the horse and there may need to be major changes to its management.
If long term pain relief is required, then the cost and any side effects need to be considered. Not all horses are used to being boxed/yarded which may be required during treatment. Some horses can be difficult/dangerous to handle when confined. Resources to reach the goal.
This is an area that is often overlooked when dealing with horses in a welfare compromised situation. Recovery from injury or disease, correcting poor body condition and any management and behavioural issues all require significant resources. The cost of any recovery plan needs to be fully considered by all parties.
The experience level and ability of the PR to carry out any plan needs to be considered, as well as their having the time to commit to the care of the horse. The facilities need to be suitable so the horse can be properly managed.
It is often a difficult decision to euthanise a horse but if there is doubt about being able to meet all the requirements in being able to give that horse an on-going good life then the decision to euthanise should be made. Euthanasia must be carried out in a humane manner by a trained person. Both NZ Thoroughbred Racing and Harness Racing NZ have people involved in re-homing horses. These links may be helpful:
https://loveracing.nz/Welfare/Thoroughbred-Welfare/Acknowledged-Retrainers.aspx https://loveracing.nz/News/34369/NZTR-launches-Acknowledged-Retrainers-network.aspx https://www.hrnz.co.nz/industry-information/hero/ Legg KA, Bolwell CF, Gee EK, Gibson MJ, Rogers CW Risk factors for horse falls in New Zealand Thoroughbred jumps racing. Vet J. 2022; 289: 105915. https://www.sciencedirect.com/science/article/pii/ S1090023322001307?via%3Dihub
Incidence rates for race-day horse falls in jumps races from 2005/6 through 2018/19 racing seasons (n = 13,648 race day starts) were calculated per 1000 starts. The incidence rate of horse falls in jumps races was 42 (95 % CI, 39 - 45) per 1000 starts. Horse falls in steeplechase races were 1.6 (95 % CI, 1.4 - 1.9) times more likely than hurdle races. The incidence rate ratio (IRR) for horses falling at the last three jumps in comparison with the first three jumps was 3.1 (95 % CI, 2.8 - 3.5) for hurdle and 4.4 (95 % CI, 3.9 - 5.0) for steeplechase races. Greater jockey (age, P = 0.02) and horse experience (P = 0.001) were associated with a lower IRR of falls (P = 0.05). Longer races (P = 0.02) and those held in autumn compared to winter (IRR 1.4; 95 % CI, 1.0 - 1.8; P = 0.05) were associated with a higher rate of falling in steeplechase races. A regulatory change enhancing discretionary ability of jockeys to pull up during the race was associated with reduced horse falls (IRR 0.65; 95 % CI, 0.51 - 0.82; P = 0.001). It was concluded that pragmatic rule changes within the industry can have a positive effect on reducing risk and improving equine welfare.


Each year the Beaufort Cottage Educational Trust runs the Gerald Leigh Memorial lectures in Newmarket. The focus of the 2022 lectures was Thoroughbred Reproductive Efficiency. There was an international line-up of presenters, including Dr Charles Love from Texas A&M who gave an excellent presentation on stallion fertility and reproductive efficiency, including reinforcement breeding. Dr Mandi de Mestre from the Royal Vet College London gave two great lectures on early embryonic loss, and umbilical cord torsion (a commonly diagnosed cause of abortion in the UK). Dr Karen Wolfsdorf from Hagyard Equine Medical Institute, Kentucky gave two excellent presentations on managing the high-risk pregnancy, and management of the barren mare for optimal fertility. These timely topics will be of interest for many equine vets in New Zealand.
All the lectures and discussion panels are available for viewing online at no cost. The presentations are professionally recorded, so you can see the lecture slides and watch the presenter. The sound quality is excellent, and each lecture is 30 to 45 minutes long. If are looking for accessible, free veterinary continuing education in current equine reproduction topics this is great place to start!

Connect to resources at: https://www.beaufortcottage.com/resources

You can enjoy your E-EVP Current Issue and E-EVP Archive at your NZVA login pages.
1. Go to http://www.nzva.org.nz/ and sign in 2. Click on: > FOR VETERINARY PROFESSIONALS > Branches > New Zealand Equine Veterinary Association [on left] > NZEVA Documents [on left] 3. There you have Current and Archive for E-EVP 4. Or you can View the E-EVP catalogue on SciQuest and download individual pages/articles
 Bill Bishop bill.bishop@xtra.co.nz
Bill Bishop bill.bishop@xtra.co.nz
In March 2020 I was fortunate enough to travel to the Antarctic Peninsula as a team supporter and mentor with a group of Inspiring Explorers# from NZ. This programme is run under the auspices of the Antarctic Heritage Trust.
Seven young New Zealanders aged from 18 to 26 made the trip. There was a rich diversity of cultural backgrounds, skills and experiences, and during the expedition the young explorers, instructors and supporters developed a great camaraderie. The trip was not without drama. During the latter part of the expedition we were stranded on our expedition ship in Ushuaia harbour at the southern tip of Argentina. After a week’s quarantine we finally negotiated seats on the very last flight to NZ out of a ‘CoViD shutdown’ South America.
Our time together on the expedition melded us into an enthusiastic and supportive group. It was inspirational seeing these young people develop their social skills and confidence in what was an unforgiving yet hospitable environment. Our last night on the ship was truly memorable and will remain with me forever. Our disparate group made up of Samoan, Māori, Muslim and Pakeha kiwis performed a haka for the 300 crew and passengers. There was a stunned silence during the haka then an immediate uproar demanding a repeat. The hubbub took minutes to die down and on finishing we all formed a magic circle and embraced, with most of us and many of the ships company in tears. I felt proud to be a Kiwi.
To see these young people flourish and grow was remarkable, but the legacy of the trip continues. All the young explorers returned home with a growing sense of their own identity and have subsequently shared their experiences and stories with friends, colleagues and others in a variety of publications and presentations.
One young woman, Ihlara McIndoe, a multi-talented lawyer and musician, composed on her return to NZ a suite of music based on her experiences in this dramatic, remote yet full of life landscape complemented by her own sound recordings above and below the sea. We attended a presentation of the Antarctica Suite at The Piano concert hall in Christchurch. The music was transposed with dramatic video footage by Anthony Powell. This is a remarkable piece of music. The quiver of
the flute echoing the wind vibrating a guy line on a tent and highlighting the constantly changing landscape, the cracking and moving of the ice reflected in the acoustic tapping on the guitar, the breathing in and out with the soft surges of the sea then peace and quietness suddenly broken by the call of an albatross or a gust of wind - it’s all here. Breathe in the peace and let the music transport you.
This Antarctica Suite performance lasts 70 minutes so please savour it by choosing a time and place where you will be uninterrupted and just immerse yourself in the experience. This is a precious passage back in time. You do not need any supplements to appreciate this Suite, but should you choose to do so only one taste experience accompanying this Suite is appropriate. Contact Whiskey Galore in Christchurch and arrange for a bottle of Shackleton’s Whiskey to be shipped.
#Inspiring Explorers Programme is at https://nzaht.org/ encourage/ where you can find out more about the exciting activities undertaken. If you are of a philanthropic bent, as we all should be, then this Registered charity is an ideal way to help secure the future of Antarctica and develop a sense of wonder and curiosity of the world around us in all our young kiwis.
Watch the full programme, A Musical Journey to Antarctica with Antarctic Heritage Trust Inspiring Explorer Ihlara McIndoe on Vimeo, at https://vimeo.com/709320556

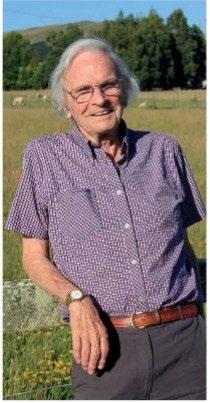
The Brian Goulden Perpetual Trophy will be awarded annually and presented at the Annual Dinner of the NZEVA conference. This annual prestigious prize is awarded to members or past members of the NZEVA who have shown leadership, enterprise, contribution to knowledge or education, and have made significant contributions to the equine veterinary profession in New Zealand.

Please send name, address and qualifications of your nominee, along with any supporting information, whom the nominator considers merits the award. This can include curriculum vitae, letters of support and documentation of achievements etc.
Send all details AT ANT TIME to nzevasecretary@gmail.com.
Brendon Bell NZEVA President nzevapresident@gmail.com

All you must do is write a clinical report that is published in the EVP, and your contribution may be eligible for one of several prizes of $150.00 that the EVP has available each year.
The EVP Editorial Group wish to promote the sharing of your interesting cases and practice tips
with the wider equine veterinary community, so please contribute.
Every case, technique, test and interpretation are different, no matter how experienced we are or how routine the case is, so there is always something for us to learn from each other.
Take photos, dig out your diaries, get keyboard tapping and share your views with colleagues. You could be $150.00 richer for it!
Please send your clinical reports to the EVP Editor for consideration.
Joe is happy chat with you about any articles or ideas you might have.
Please contact Joe at evp.editor@gmail.com or on 027 437 3651.
Main SC et al. Metabolomic Profiles in Starved Light Breed Horses during the Refeeding Process. Animals. 2022; 12: 2527. https://doi.org/10.3390/ani12192527
Ten aged and malnourished horses (BCS ≤ 2) surrendered via authorities, auctions and privately were fed specific diets over the rehabilitation period consisting of the critical care period (CCP; days 1-10 of rehabilitation) and the recovery period (RP; days 11+) were monitored. Potentially toxic compounds, analytes related to liver, kidney, and muscle function, as well as energy-related metabolites were altered during the refeeding process. These findings may provide some evidence that the refeeding process has a significant impact on the equine metabolome.
NOTE: In fact, 4 of the 10 horses succumbed to colic and respiratory disease leaving only 6 data sets to analyse. Afraid I couldn’t take a lot away from reading this article and the supplementary data. The refeeding syndrome can be a killer and initial careful monitoring of PO4-3, K+, Ca++ and Mg++ is very important during the CCP of refeeding, and vitamin B1 supplementation probably is indicated. A fine review is available at Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008; 336(7659): 1495-8. Incidentally, the study was part funded by, and two authors are employed by, Purina Animal Nutrition; maybe a refeeding diet is in the bag?
Through the generosity of the McLaren family and in memory of Don McLaren and the huge contribution he made to our profession through his drug company, Bomac, a fund is available to further veterinary research and education. A significant proportion of this money is allocated to the equine sector. A total of up to $10,000 is available for equine research and education each year, and applications are now invited for 2023.
Priority will be given to veterinary practice-based projects, especially involving young veterinarians. Consideration will also be given to broader-based equine research work or suitable education-related applications.
Applications close 30th June and the successful applicant(s) will be notified by 1st August 2023.
Please apply in writing to:
Leanne Fecser
New Zealand Veterinary Association, PO Box 11212, Wellington nzva@vets.org.nz
Applications must include: (a) Details of the proposal (b) Curriculum vitae