






20232024
Contents
Introduction from the chief executive
Statement of directors' responsibilities
About this report
Governance arrangements
Care Quality Commission rating
Priorities for quality improvement in 2024-25
Statement relating to the quality of care
provided
Progress against priorities set for 2023-24
Our patients
y Infection prevention and control
y Quality improvement
y Patient experience and engagement
y Our Patient Panel
y Improving care for vulnerable patients
y Learning from safety incidents
y Improving medicine safety
Our people
y Recognising our amazing people
y The national NHS Staff Survey
y Equality, diversity and inclusion
Our performance
y Performance against NHS constitutional standards
y Participation in clinical audits
y Research and development
y Alex Health
Our places
y Improving our estate
y Sustainability
Statements from stakeholders
Glossary of terms
Appendix 1 - Statements of assurance from the Board – prescribed information
Welcome to the Quality Account 2023-24 for The Princess Alexandra Hospital NHS Trust (PAHT). The year has seen our dedicated teams across each of our clinical sites – The Princess Alexandra Hospital in Harlow; Herts and Essex Hospital in Bishop’s Stortford and St Margaret’s Hospital in Epping, continue to work hard with a clear commitment to provide quality care to our patients. My thanks go to all the teams at PAHT who each play an important part in ensuring our patients receive the safe, quality care they need.
This report demonstrates our commitment to patient care, our depth of monitoring, progress on meeting our aims and our breadth of improvement initiatives, all of which are a real recognition of what sits behind the decisions and transformation being undertaken across the trust.
Our nine Quality Account priorities for 2023-24 were set in-line with the quality elements of our trust objectives that focus on our patients, our people, our performance, our places and our pounds. This report shares the details and achievements and, importantly, it notes areas where we can continue to learn and to improve further through our objectives and ongoing plans for the year to come.
Significantly, this year we have achieved a strong improvement in the hospital standardised mortality ratio (HSMR). This improvement can be seen from October 2023 when our HSMR was assessed to be ‘lower than expected’ for the first time ever; this has been maintained and our HSMR is currently third best in the East of England region. Continuous improvement in the care for our patients and robust reviews of deaths which include key categories such as sepsis, acute kidney injury (AKI), chronic obstructive pulmonary

disease (COPD), fractured neck of femur and diabetes underpin the HSMR improvement. We have also continued to see improvements in key quality indicators including reductions in the number of falls and the number of pressure ulcers per 100,000 bed days. This means safer care and positive outcomes for our patients.
We are only able to provide the care we do thanks to the skill, dedication, passion, and compassion of our 4,200 colleagues and volunteers, and through our partnership working with primary care, community services, mental health and social care colleagues.
As always, I am grateful to the many people who continue to provide high quality care and who have contributed to this report. I am proud of our achievements and ongoing transformation and commend this Quality Account to you. I confirm that, to the best of my knowledge, the information and details in this account are accurate.
Best wishes
Lance McCarthy Chief executive
The Trust directors are required under the Health Act 2009, amendments published in the Health and Social Care Act 2012 and the Quality Account FAQ published in 2021/2 Annex 1, to prepare a Quality Account for each financial year.
The Department of Health has issued updated guidance regularly on the form and content of the annual Quality Account, which incorporates the above legal requirements.
In preparing the Quality Account, directors are required to take steps to satisfy themselves that:
y The Quality Account presents a balanced picture of the Trust’s performance over the reporting period y The performance information in the Quality Account is reliable and accurate
y There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice
y The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review. The Quality Account has been prepared in accordance with Department of Health guidance
The directors confirm that, to the best of their knowledge and belief, they have complied with the above requirements in preparing the Quality Account.
By order of the Board
Every year all NHS hospitals in England must write a report for the public about the quality of their services; this is called the annual Quality Account. The purpose of the report is to make the hospital more accountable to you and drive improvement in the quality of our services.
At The Princess Alexandra Hospital NHS Trust, we are committed to ensuring that we keep our patients and our people safe. Our focus has been to ensure we can provide all necessary care and treatment in the safest possible way, at the right time and in the right place for our patients. Through this, we are making our pledge to you about the improvements we intend to make over the period 202425 by committing to our Quality Account improvement priorities.
This report will tell you how well we performed against the quality priorities and goals we set for the period of April 2023 to March 2024 and the areas we have improved through this year.
We will describe to you the areas where we have reviewed our patient care in order to evaluate the quality of services provided. This report will contain mandated information from our Board, along with statements from our commissioners and partners. We will also provide a glossary of terms.
Our Quality Account is prepared in line with the Quality Account toolkit guidance with additional information included in line with advice received by NHS England as follows:
y Details of ways in which staff can speak up (including how feedback is given to those who speak up), and how the Trust ensures that staff who speak up do not suffer detriment
y A statement regarding progress in implementing the priority clinical standards for seven-day hospital
y A statement that evidences an improvement plan to reduce rota gaps for NHS doctors and dentists (Schedule 6, Paragraph 11b of the terms and conditions of service for NHS doctors and dentists in training (England) 2016)
The report is published following internal and external partnership engagement. The information was reviewed by the Trust Board in June 2024, with delegated authority given to our Quality and Safety Committee for final approval.

The most recent inspection of the Trust completed by the Care Quality Commission (CQC) was an unannounced focused inspection over the summer of 2021. This included a review of the Trust-wide Well Led Key Line of Enquiry. The care services inspected were:
y Maternity care
y Medicine (including elderly care)
y Urgent and emergency care (emergency department) services
The most recent specific focused inspection was of the urgent and emergency care department
The CQC completed an unannounced focused inspection of the urgent and emergency care department in March 2023 to monitor our progress against the Trust action plan and review our performance against their Key Lines of Enquiry standards.
The report was received in mid-June 2023 and we were pleased to note the CQC improved the rating for the urgent and emergency care department to Requires Improvement.
The CQC noted improvements had taken place in the department for:
y Delivery of safe care to patients and the department meeting the standards for leadership covering the area of Well Led
y The rating for the department overall has been improved to meet the standard of Requires Improvement
y We are pleased that the CQC stated we deliver outstanding practice for the provision of care for patients in a mental health crisis. The Trust ensures a registered mental health nurse is rostered on every shift to meet the needs of patients and ensure timely risk assessments are completed
Figure 1: Our overall Trust rating

The recommendations received from the CQC were collated into individual projects and were updated by the relevant divisional teams using our quality improvement methodology to enable a consistent and sustained approach to the achievement of these objectives. Each project has a designated executive, a senior responsible officer (SRO) and we have appointed a quality project management team to provide additional support.
We used our CQC quality improvement plan as a dynamic document; during the year we have added additional improvement topics as we identified further areas that required improvement. The quality improvement plan is monitored monthly through the clinical quality improvement group that reports into the Trust compliance group and onto the Quality and Safety Committee.
Our people use the CQC inspection outcomes as the foundation upon which to critically examine our services and focus on how we plan and deliver the fundamental aspects of safe care. We have taken decisive action to change everyday activities, which have led to significant improvements.
The new CQC inspection framework has been amended during the spring of 2024 and going forward will undertake inspections against quality statements. The Trust is actively working across all our clinical services to measure our current performance position and identify the evidence we have in place to support each quality statement.
Quality Account priorities for improvement during 2024-25
Our nine Quality Account priorities for the next year are identified in line with the quality elements of our Trust objectives, which focus on our patients, our people, our performance, our places and our pounds
We have developed these through consideration of the factors that matter the most to our patients which is to improve safety, reduce harm and waiting times and learn from their feedback. Also, taking into consideration how we deliver improvements for our people who are responsible for face to face patient care. This process has been supported by the clinical leadership team and members of the Trust board.
Our patients and our performance 1. We will maintain the Trust Hospital Standardised Mortality Rate (HSMR) within the as expected range and we will continue learning from every death. This will improve quality of care for all patients.
2. We will continue to deliver high quality care in the right place and at the right time for our urgent and emergency care patients, working towards achieving the 76% emergency care quality standard. This will be measured and reported on national submissions of the four-hour access standard.
3. We will reduce the number of complaints or patient advice and liaison service (PALS) concerns that detail communication as a theme by 10%. We will focus on identifying that our feedback from patients demonstrates an improvement in communication with them. This will improve the experience for all patients.
4. We will reduce inpatient falls with moderate and severe harm to less than 0.5 per 1,000 occupied bed days. We will continue to learn from each of these
incidents. This will improve the quality of care for patients at risk of falling.
5. We will reduce the numbers of patients that sustain a pressure ulcer by reducing all pressure ulcers that could not otherwise be avoided to less than 3 per 1,000 occupied bed days. This will improve the quality of care received by our patients at risk of developing pressure ulcers.
6. We will reduce the number of patients waiting longer than a year for their elective treatment by improving the efficiency and utilisation of our clinical resources such as theatres and outpatient clinics. This will be measured and reported by national submissions of patient waiting times.
7. Our developing change strategy is aligned with our core values of everyday excellence as we move forward on our journey to becoming a learning organisation. We will foster a culture of continuous learning, adaptability and knowledge sharing, to not only deliver successful and effective transformation, but also to empower our people and teams to evolve and thrive in their delivery of everyday excellence.
Our people
8. We will improve our people’s satisfaction measured through the annual NHS Staff Survey. This will benefit the Trust through the improved wellbeing of our people and support our continued focus to drive a positive culture.
Our places
9. We will continue to work in partnership to improve our hospitals and health infrastructure for our patients.
Our pounds - nil
By improving the quality of care as detailed in the priorities above, we will deliver greater value for money for our patients.
These priorities will be monitored using our existing governance structures; this will include being monitored through our Quality and Safety Committee.
Statements relating to the quality of care provided
PAHT is a 418 bedded hospital with a full range of general acute services, including; a 24/7 accident and emergency department (A&E), an intensive care unit (ICU), a maternity unit (MU) and a level II neonatal intensive care unit (NICU).
We serve a core population of around 350,000 and are the hospital of choice for people living in east Hertfordshire and west Essex. In addition to the
communities of Harlow and Epping, we serve the populations of Bishop's Stortford and Saffron Walden in the north, Loughton and Waltham Abbey in the south, Great Dunmow in the east, and Hoddesdon and Broxbourne in the west. The extended catchment areas incorporate a population of up to 500,000. We own the main hospital site in Harlow, and operate outpatient and diagnostic services at Herts and Essex Hospital, Bishop's Stortford, and St Margaret’s Hospital, Epping. The operation of these facilities forms part of the longer-term strategy of bringing patient services closer to where people live and making services, where appropriate, that are more accessible and easily available to patients. We operate over 64 different services to meet the needs of our patients (see the service portfolio in table 1).



Children and women's services
Antenatal and newborn screening
Early Pregnancy Unit
Children’s ward including patient at home (23/24 delivered by community provider)
Foetal medicine
Colposcopy and hysteroscopy services
Community midwifery
Infant feeding support
Newborn hearing screening
Gynaecology ambulatory service
Neonatal critical care – special care baby unit and neonatal community nurses
Gynaecology including termination of pregnancy services
Maternity: Antenatal clinics
Ultrasound scanning
Labour Ward
Antenatal Ward
Postnatal Ward Maternity Assessment
Centre (Maternity Triage and Day Assessment Unit)
Birth Centre
Community midwifery services
Homebirth service
Maternity bereavement services
Specialist antenatal services
Obstetrics
Paediatric diabetic Medicine
Tongue tie service
Clinical support services
Audiology Blood tests
Breast surgery
Paediatrics – inpatients, outpatients, assessment services
Chemotherapy
Clinical haematology
Interventional radiology
Oncology services
Dermatology
Medical oncology
Outpatients
Dietetics
Mortuary and bereavement services
Patient appliances
Pharmacy services
Physiotherapy and occupational therapy
Tissue viability Transfusion services
Medicine
Cardiology
Genito-urinary medicine
Oncology services relevant to medical care
Diabetic medicine
Geriatrics including frailty
Respiratory medicine
Radiology
Infection prevention and control services
Neurology
Pathology: microbiology, cellular pathology, blood sciences, biochemistry
Speech and language therapy
Endocrinology
Medical inpatient wards
Rheumatology
General medicine
Older people's assessment and liaison (OPAL)
Specialist palliative care and end of life services
Surgery and critical care
Day surgery
Gastro enterology
Maxillo-facial surgery
Colorectal services
Ear, nose and throat
General surgery High Dependency Unit
Ophthalmology
Oral surgery
Endoscopy services
Intensive Care Unit
Perioperative
Medicine
(Anaesthetics and ICU)
Urgent and emergency care
Adult assessment services incorporating same day emergency care and urgent 'hot' clinics
Integrated Urgent Treatment Centre - in collaboration with Stellar Health, Stort Valleys Federation, Essex Partnership University NHS Trust and Herts Community Trust
Emergency department Paediatric emergency department
Patient at home, adult (23/24 delivered by community provider)
The review of services and all associated data is undertaken through the Trust governance structure. This includes monthly meetings reviewing information covering patient experience and engagement, patient safety, learning from deaths, vulnerable patients and the Infection Prevention and Control Committee and bi-monthly Clinical Effectiveness and Compliance Groups. All of these groups report monthly into the Quality and Safety Committee, a subcommittee of Trust Board.
Review of each service's performance (Appendix 1) within the Trust has been monitored through the Performance and Finance Committee, with external review undertaken by both Essex and Hertfordshire commissioners at the monthly Service Performance and Quality Review Group.

Our patients and our performance
1. We will maintain the Trust Hospital Standardised Mortality Rate (HSMR) within expected and we will continue learning from every death. This will improve quality of care for all patients.
Outcome: Achieved The trust has shown a significant improvement in HSMR, Standardised Mortality ratio (SMR), in the national and regional position in the current financial year (April 2023 – April 2024).
During this current financial year, the trust has consistently submitted fully coded data on a monthly basis with particular improvements in the capture of comorbidity reporting and palliative care. Continuous improvement in care for patients and robust review of deaths have seen the trust return to "as expected" level in historical outlier categories such as sepsis, AKI, COPD, fracture neck of femur and diabetes.
HSMR for the period April 23 to October 23 is 83.4 and “lower-than-expected” (see figure 3 below and HSMR for October 23 and divided by months in the figure 4).

PAHT have the second lowest HSMR value in the region (see figure 5).
Figure 5: Regional HSMR is 96.3 and “lower-than-expected”

PAHT remains in a good position when compared with national data for similar organisations (see figure 6).
Figure 6: National HSMR for the period April 23 to October 23 is 96.0 and “lower-than-expected” (confidence intervals 95.3 – 96.6)

The SMR of the first 7 months of this financial year remains” lower than expected” (see figure 7).
Figure 7: SMR for the period April 23 to October 23 is 85.0 and “lower-thanexpected”, SMR for Oct-23 is 81.5 and “within expected”

In summary:
y There has been a significant improvement during the current financial year of the main mortality indices
y Compared to the previous financial year, there has been an improvement in mortality rates and in the position of the historical categories of outliers (sepsis, acute kidney injury (AKI), diabetes and respiratory diseases)
y Since the beginning of this financial year, PAHT has remained in a favourable position compared to peers in the regional and national context
Learning from deaths does not rely only on the mortality indices. The following processes complement the mortality data:
y The Telstra data set includes diagnosis-specific mortality outliers. All of the patient deaths within each outlier group are reviewed by the clinical specialty leads and the coding leads
y All deaths are scrutinised by the Medical Examiner team
y 25% of deaths are further reviewed using the structured judgement review approach and learning shared through regular departmental mortality and morbidity meetings
y Any concerns raised through or external to these processes are scrutinised by the incident management group by reporting using the Trust Datix system
y Regional networking has commenced,
in order to improve learning and benchmarking for national and local processes.
The SMART database was implemented in July 2021 and is fully embedded at the Trust.
y This is used for the completion of Medical Examiner independent reviews and the recording of Structured Judgement Reviews
y The database produces a mortality dashboard, which can be filtered to individual specialities or divisions. This allows teams to review mortality over defined periods of time
y This has proved a useful tool in pulling themes and trends in order to understand the Trust's mortality status and where improvements may be required. It also provides a useful digital platform for the management and standardisation across the Trust of the learning about Mortality and Morbidity meeting
Next steps:
y The Strategic Learning from Death Group continues to support and enable the mortality programme in order to facilitate continued improvement of care of our patients
y The palliative care, coding and mortality teams continue to work closely to deliver training for clinical staff on the importance of accurate documentation and the impact this has on the Trust's clinical data quality
y An associate medical director for
mortality and risk has been appointed early this financial year. They work closely with Mortality Matron to oversee the learning from deaths programme
y The Deteriorating Patient Group has been re-established and is working closely with all divisions to improve both early identification and the quality of care delivered to the deteriorating
Our patients and our performance
2. We will continue to deliver high quality care in the right place and at the right time for our emergency and urgent care patients. This will be demonstrated through an improvement in our emergency department care.
The Trust closed respiratory ED during the year, following appropriate guidance from our infection prevention and control team relating to the changes to Covid-19 management nationally.
The Trust worked with system partners including the Integrated Care Board (ICB) to provide an Integrated Urgent Treatment Centre (UTC) with a new provider collaborative.
y The collaborative includes both of the local GP federations, Stellar Healthcare and Stort Valley, Essex Partnership University NHS Foundation Trust (EPUT), Hertfordshire Community Trust (HCT) and us (PAHT)
y The UTC now operates on an appointment system and we have seen a significant improvement in reduced waiting time for patients attending the UTC. The appointments can be accessed via NHS 111 or by attending the emergency department (ED), with appropriate patients having been clinically reviewed as suitable to be streamed across to the UTC service rather than needing ED care
y The service has the capacity to see 110 patients a day between the hours of 8am-10pm. Outside of these hours, suitable patients can be streamed to the GP out of hours service at Lister House which is provided by Herts Urgent Care
patient across the trust
y Further implementation of the SMART system will help to standardise and extend the mortality and morbidity programme to all services across the trust
y Enhanced networking with regional peers and primary care will continue to support learning across the system
The CQC undertook an unannounced inspection of the urgent and emergency care department in March 2023, and the Trust was notified in June 2023 that we were to be removed from special measures. Colleagues in the department were delighted that the work they had undertaken had resulted in a notable improvement that was recognised by our regulator. This has had a positive impact on staff morale and the way in which our teams work together, identifying further opportunities to sustain these substantial improvements to patient safety and patient experience.
During this year, our UTC is able to see, treat and discharge all of the patients referred to it within 4 hours and are currently reporting 100% compliance against the 4-hour standard.
The Trust is participating in a national pilot with NHS England to optimise our initial assessment processes. This project and other improvements have ensured that we are able to triage and take observations on our patients within 15-20 minutes of attendance, figures 8-11.

UTC is able to see, treat and discharge all of the patients referred to it within 4 hours and are currently reporting 100% compliance against the 4-hour standard.
The Trust is participating in a national pilot with NHS England to optimise our initial assessment processes. This project and other improvements have ensured that we are able to triage and take observations on our patients within 15-20 minutes of attendance, figures 8-11.
Figure 8: Average minutes after arrival until time of triage in ED (arrival by ambulance)

Figure 9: Average minutes after arrival until time of triage in ED (arrival by another route)

Figure 10: Average minutes after arrival until observations are completed ED (arrive by ambulance). This demonstrates a sustained improvement during March and April 2024

Figure 11: Average minutes after arrival until observations are completed ED (arrive by another route)

Attendances have remained within normal variation, and we continue to work hard to reduce the length of time patients stay in the UEC department, figures 12-15. In order to do this, we have developed a comprehensive improvement plan to support further improvements.
Figure 12: Attendances total

13:



The Trust has worked with system partners and stakeholders to support the timely handover of patients arriving by ambulance. Whilst we still have improvements to make, we are confident that the improvement plans we have will continue to deliver sustainable change, figure 16.

We have implemented a trust-wide Same Day Emergency Care (SDEC) steering group to further develop the service within the trust, allowing more patients to be managed in a non-admitted pathway.
y Medical SDEC services have continued to deliver an average length of stay of 5 hours for patients whilst in the department
y The Trust is working collaboratively with the ED team to ensure that all appropriate patients are managed away from ED
y The SDEC team have successfully implemented a surgical hub within the SDEC building, which is enabling surgical patients to be managed away from the ED
y SDEC have continued to provide a urology hot clinic services and ultrasound services for our patients
y The continued collaboration with EPUT on the implementation in January 2024 of a community led deep vein thrombosis (DVT) pathway is enabling patients to be treated closer to home
The Acute Admissions Unit (AAU) has continued to provide medical specialist assessment services for patients who are unable to attend SDEC, and have managed to maintain an average length of stay of 1.2 days. However, the length of stay is reflective of some trust-wide barriers to patient flow through and out of the hospital.

3. We will reduce the proportion of complaints or patient advice and liaison service (PALS) concerns that detail communication as the main concern. We would like to see evidence from patients’ feedback that communication with them is improving.
Outcome: Partially achieved
As a result of our work to support improvements in communication with patients, three quantifiable improvements have taken place in year.
y PALS concerns relating to communications have reduced from 24% of all PALS in 2021-22 to now being 16% in 2023-24
y Complaint numbers have reduced from 262 to 176 over the last two years. Complaints regarding communication
2
reduced from 28 to 26 cases per year
y In year the Trust has trained 911 staff in SAGE and THYME – our communication skills course. This is 67% of all nursing, midwifery and allied health professional (AHP) staff
4. We will reduce the number of moderate and severe harms inpatient falls. We will continue to learn from each of these incidents. This will improve quality of care for patients at risk of falls.
Outcome: Partially achieved
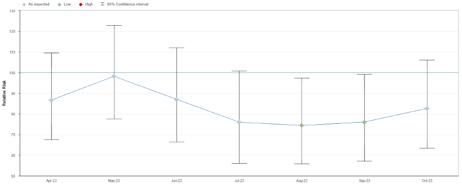
In year there was a small increase in the numbers of inpatient falls resulting in moderate and severe harms, table 2, figure 17, 18.
*The Trust grades all incidents that result in a fractured neck of femur as severe harm.
The total number of falls that have occurred have reduced over the last three years
y Comparison with total numbers in 2022-23 has reduced by 2.5%
y In comparison with 2021-22 the numbers have reduced by 3%. It should be noted that data for this period still had an impact resulting from Covid-19
y Patient deaths resulting from an inpatient fall during 2023-24 have reduced to zero
y Mandatory falls awareness training has been maintained at over 90% compliance
Figure 17a: All falls with harm (moderate/severe/death) per 1000 bed days

Figure 17b: All falls with (moderate/severe/death) per 1000 bed days

Figure 18: All falls per 1000 bed days

Highlights from 2023/4
y Introduced the Falls Investigation Oversight group – to review all moderate and above harm falls. Themes from this are being built into our new falls strategy for this financial year
y Maintained mandatory falls awareness training at over 90% compliance each month
y Reviewed and updated the falls multifactorial risk assessment – and this has been built in to CERNER
y Reviewed and updated the enhanced care risk assessment and this has been built into CERNER
y Developed an action plan to address the national alert regarding bed rails –including training programme and updates to CERNER and Nervecentre
y Strengthen the governance around the provision of enhanced care – including reviews of Level 4 patients and accuracy of data recorded on Safecare
y Continued to recruit to the enhanced care team
y Worked with the new manual handling lead to start to better align falls training and manual handling training (including the use of the hoverjack equipment)
y Continued with the programme to encourage the reconditioning of our patients
y Continued to work with the lead frailty pharmacist to encourage the
deprescribing of culprit medication
y Undertaken the pilot study of new bed sensor technology (with Cognito and Medstrom)
y Undertaken a deep dive review of falls leading to cerebral bleeds
y Continued with the bi-monthly meetings of the Improving Essential Care – Falls Prevention Group


5. We will reduce the numbers of hospital acquired pressure ulcers resulting in moderate & severe harm and continue to learn from each of these incidents. This will improve the quality of care received by our patients at risk of developing pressure ulcers.
Outcome: Not achieved
In year, the inpatient moderate harm pressure ulcers appear static. However, it should be noted that there are 21 incidents with initial harm grading of moderate in this category and two incidents with initial harm grading of severe. This will likely result in an increase of the harms that occurred this year when compared with the year 2022-23 data once the 23 investigations currently in progress are completed, table 3 and figure 19-20. Table 3
21 incidents from 23-24 are under investigation and not validated and
2 incidents from 23-24 are under investigation and not validated and closed
By undertaking gap analysis of completed investigations this year, we have identified specific thematic contributory factors towards the development of hospital acquired pressure ulcers.
This resulted in the implementation of a new process as part of our quality improvement initiatives that will go live in May 2024.
y This aims to reduce the time to complete an investigation having reviewed what we already know, and focus primarily on implementing improved care.
Figure 19 details our pressure ulcers rate within March 2023 until March 2024. From February 2024, our categorisation process aligned with national guidance requiring two categories of pressure ulcers to be changed and the exclusion of moisture lesions reported as these are not pressure injuries. Therefore, the downward trend in all pressure ulcers and total pressure ulcer rate per 1,000 occupied bed is due to the change in reporting methodology aligned to the national guidance.

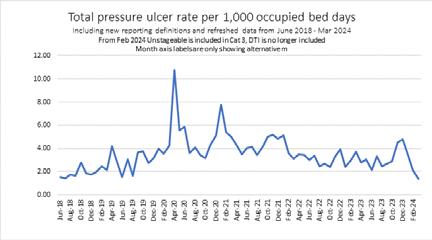
The National Wound Care Strategy Programmes ‘Pressure Ulcer Guidance and Clinical Pathway (2023)’ recommends within this, the pressure ulcer categories will no longer include deep tissue injury, instead replaced with ‘vulnerable skin’ and/or category 3 on assessment, this will impact the total number of pressure ulcers reported and potential severity of ulcer and harm level.
Purpose T will give an earlier identification via screening of those patients most at risk, from the start of their journey into the hospital through to discharge. The training tool is in progress along with training Trust wide and linked to the planned digital programme of Alex Health.
Tissue viability is aligned to the Patient Safety Incident Response Framework (PSIRF) with our new process for investigating hospital acquired pressure ulcers being approved and implemented in 2023. This process supports staff to identify why a pressure ulcer has occurred and what the impact of the pressure ulcer is on the patient. This will be used for investigating pressure ulcer categories 2,3 and 4 regardless of harm level. Moisture associated skin damage is not routinely classified as a harm.
During the year, the Trust implemented a Pressure Ulcer Investigation Oversight Group (PUIOG) as a sub group of the Improving Essential Care Group which is part of the Trust quality governance process, this group has oversight of:
y All hospital acquired pressure ulcers within the Trust, but primarily categories 3 and category
y Any themes that have been identified
y Clinical areas requiring quality improvement action plans (pressure ulcers) and ensuring they are reviewed in a timely manner
y That all risks that have been identified are reported
PUIOG ensures new themes are recognised and addressed, either through local action plans, strategic action plans, quality initiative or held on a risk register. PUIOG is continually evolving to meet investigation requirements robustly and addressing quality improvement strategies in a timely manner.
Implementation of the National Wound Care Strategy Programme recommendations and establishing a robust investigation and quality improvement plan process, will help to achieve improved patient outcomes for reducing pressure ulcer harms.
To demonstrate our commitment to patient safety improvement we have developed a Pressure Ulcer Prevention Strategy which will assist in improving quality of care delivery to our patients over the next 3 years (2023-27). The forward view is aligned to the PACE ward accreditation programme and the fundamentals of care work implemented will go towards delivery of these objectives, we have:
y Implemented a new tissue viability team structure including a dedicated pressure ulcer prevention practitioner
y Developed mandatory pressure ulcer prevention training
y Implemented a new national audit for pressure ulcers
y Increased thenumber of pressure ulcer study days for registered and healthcare assistant nursing staff
y Implemented new categorisation of pressure ulcers to the Trust
y Conducted a mattress sensor trial to alert staff when patients require repositioning
The Trust is supporting the National Wound Care Strategy Programme (NWCSP) by implementing a new Pressure Ulcer Guidance and Clinical Pathway. The recommendation is to provide clear advice to health and care practitioners, service managers and commissioners about the fundamentals of evidence-informed care for people who have or are at risk of developing pressure ulcers. The recommendations outline a pathway of care that promotes early risk identification and preventative care, enabling fast access to evidence-informed therapeutic interventions, with escalation of treatment or service provision for people requiring more complex care.

6. We will improve our people’s satisfaction, measured through the annual NHS Staff Survey. This will benefit the Trust through the improved wellbeing of our people.
This year we had the highest response rate ever at PAHT, with over 1,900 of our people taking the opportunity to give feedback. We also had a response rate that was 5% above the average response rate for acute and community Trusts in the country.
Feedback shows that there have been improvements in all seven of the NHS People Promises, with significant improvement in 6 of the 7.
Feedback also shows that we have improved significantly in both of the NHS themes (staff engagement and staff morale).
We will improve our people’s satisfaction measured through the annual NHS Staff Survey. This will benefit the Trust through the improved wellbeing of our people.
Our Feedback to action programme was our approach to acting upon the insights and feedback from the Staff Survey. The programme ran between March – August 2023 (6 months). Activities included:
y 14 programme sponsors were overall accountable for programme implementation within their division or corporate sub-division
y 33 facilitators were trained to support the divisions
y 100 group members were confirmed at the beginning of the programme
y All divisional groups continued with their plans and adopted full, condensed or localised approaches to the programme
All divisions and corporate areas committed to plans at the beginning of the programme and submitted
divisional summaries at the close of the programme.
The activities included in Feedback to action plans (2023) related back to the trust-wide Staff Survey 2022 improvement priorities which were:
y health and wellbeing, learning and safety culture and psychological safety
y management and leadership, and effective staffing
Some of the activities included:
y Listening events with key stakeholder groups
y Caring and co-working in a culture of diversity
y Inter-department shadowing
y A Day in the Life Of programme was extended to all of our people, giving a holistic understanding of interlinking departments and activities
y Suggestion boxes implemented
y There were multiple nominations for stands at This is Us Week to celebrate and showcase work
y Employee of the month
The Trust has a culture to support our people who speak up, to include the following commitment:
y Colleagues at all levels within the trust feeling equally encouraged and empowered to speak up. They feel safe to speak up without fear of detriment, that is without experiencing disadvantageous and/or demeaning treatment as a result
y All of our people are confident that their voices will be heard and our managers across PAHT feel confident to listen and act when someone speaks up and improvements will happen as a result. These are communicated back to those who raise matters
y Leaders are seen to promote Freedom to Speak Up through actively demonstrating positive behaviours
y We have expanded our Freedom to Speak Up team this year by appointing 27 Freedom to Speak Up
Ambassadors and provided them appropriate training and support to equip Freedom to Speak Up leads to actively support the Freedom to Speak Up Guardian
y There have been notable improvements in staff morale and culture. Well-being focus week for staff included Diwali celebrations, African Day, Birthday and Retirements – improved staff morale and team engagement
y The positive impact of the Professional Nurse Advocate role in addition to career clinics supports our people and links into the equality diversity and inclusion element of the Quality Account


7. We will continue to work in partnership to improve our hospitals and health infrastructure for our patients.
The funding for a new hospital has been announced and approved and we have started to recruit our design team. A build schedule will be set by the National New Hospital Programme, which we are preparing ourselves to ensure we can move as quickly as possible. The need for a new hospital for the local area is well established and will serve local people for years to come. It will also provide the best place to work for our clinical and corporate teams and enable us to make a real difference to healthcare in our community and will appeal to new people to join PAHT.
A clinical model to support the needs of our population now, and in the future, is currently under development and led by a range of clinical teams from across our organisation and wider health and care system. Once agreed, this clinical model will also allow us to recognise opportunities for further community-based health care provision and set us on a
path to developing our off-site estate, as well as the new hospital build.
Our staff continue to work in partnership with a wide stakeholder group of experts to deliver a Community Diagnostic Centre at St Margaret’s Hospital in Epping. As part of this programme, we are also developing a spoke CDC site for extended diagnostic access at Herts and Essex Community Hospital. Across these two sites we have refurbished three X-ray rooms and, from September 2023, have extended access to patients for plain film X-ray, non-obstetric ultrasound and MRI.
As the lead organisation for our CDC programme, we are committed to delivering an innovative and fit for purpose Community Diagnostic Centre by refurbishing and extending existing NHS estate. The CDC will provide additional scanning and diagnostic testing at the weekend and longer opening times during the week. This development brings diagnostic tests closer to patients, increases the number of appointments and extends the days of the week that tests are available, which will support local people.

Infection prevention and control
Respiratory viruses including COVID-19
2023 - 2024 has seen an ongoing reduction in the impact of coronavirus (COVID-19). COVID-19 testing and documented outbreaks have reduced throughout the course of the year, with a shift towards managing COVID-19 as part of a wider group of respiratory viruses. This UK Health Security Agency (UKHSA) recommendation was implemented in our Trust, with surveillance and monitoring of influenza, respiratory syncytial virus (RSV) and seasonal respiratory viruses as in previous years.
The likelihood of being admitted to hospital due to COVID-19 has greatly reduced with the vaccinations, with testing in health care settings mainly targeted at informing clinical care. The acceptance of COVID-19 vaccination by patients over 75 years of age was noted nationally and locally, together with a trend for significantly reduced uptake by health care staff. Infection prevention and control (IPC) precautions in hospital, were as stated in the national IPC manual.
Testing for COVID-19 (in patients as well as health care staff) reduced gradually over the course of the year. Only symptomatic patients were tested for COVID-19, either by lateral flow tests or using rapid diagnostic testing. We documented a total of 32 COVID-19 outbreaks across our wards in 20232024, compared to 41 in the previous year.
Our COVID-19 Medicines Delivery unit (CMDU) continued to dispense medication recommended by NICE. They used a limited number of oral treatments, or IV medication delivered via our Same Day Emergency Care (SDEC) Unit, to manage non-hospitalised highrisk patients. From April 2024, local
delivery of COVID-19 treatments will be changing, with some aspects of the service being managed through the 111 service.
Our in-house microbiology laboratory responded to the changing requirements for management of respiratory infections in our patients, and by early 2024 introduced polymerase chain reaction (PCR) testing using a wide respiratory panel. Previously only COVID-19, Influenza A and B and respiratory syncytial virus (RSV) were tested for, in and out of hours. Now, apart from the latter four viruses, adenovirus, human metapneumovirus, parainfluenza (1-4), enterovirus, rhinovirus, parechovirus and bocavirus are tested for, including in our paediatric population.
Respiratory syncytial virus (RSV) testing using point of care testing (Abbott ID) continued over the winter season. Point of Care testing helped clinicians adhere to the latest guidance from the Royal College of Paediatrics to isolate children with respiratory viruses appropriately, whilst protecting immune-compromised children.
As we approach the summer months, we note there is a reduced burden across our health care setting associated with respiratory viruses, including COVID-19, Influenza and RSV. Hospital inpatients, and the population as a whole have moved towards learning to ‘live safely with coronavirus’.
A total of 48 hospital and community onset health care associated C. difficile cases were reported during the year 2023-24, as shown in the C.difficile table below. Of these, 38 were hospital-onset, health care associated (HOHA), detected three or more days after hospital admission, and 10 were communityonset healthcare associated (COHA), detected in the community, or within two days of admissions, and the patient had been an inpatient in the Trust in the previous four weeks. This compares with a total of 36 cases in the previous year, 28 of which were HOHA, and eight were
Although the Trust did exceed its trajectory, in terms of its position against the East of England (EoE) region, the Trust had an almost identical rate (very slightly above at 34.26 per 100,000 occupied bed days, compared with a rate of 33.56 average for all 14 Trusts in EoE).
Cases were reviewed as part of the root cause analysis (RCA) process at the bi-monthly Incident Review Panels, identifying any trends/themes and sharing of learning. Panel reviews include the monitoring of key Infection Prevention and Control (IPC) measures for the control of C.difficile including isolation, sampling, environmental cleaning, hand hygiene, use of appropriate personal protective equipment (PPE), and the careful prescribing of antibiotics. In the second half of the year, the IPC team developed a new investigation tool, aligned to the Trust moving towards adopting the Patient Safety Incident Response Framework (PSIRF), in responding to patient safety incidents.
A thematic review of the healthcareassociated C.difficile cases in 2022-23 and the contributory factors identified, were used to inform and develop a comprehensive, Trust-wide collaborative action plan to improve practice and patient safety. The investigation tool and the action plan are now being used by clinical areas to provide greater clinical ownership of their cases. A further thematic review of the cases from 202324 is currently underway.
There is a link between C.difficile infection and antibiotic use, particularly broad-spectrum antibiotics. The total antibiotic consumption in the organisation continues to be high, with the latest manually calculated define daily doses/1000 admissions reported as being one of the highest in the East of England (EoE) region. The digitally calculated figure of 5,282.0 (15th worst performing non-specialist trust in England, against a national average of 4,601) is incorrect, as there is a large discrepancy between the Trust admission data, and that published
by NHS Digital. This is currently being investigated by the PAHT Business Intelligence (BI) team. Unfortunately, NHS Digital cannot correct the 2024 data until June - September 2024, and they also cannot correct 2023- 2024 data.
In addition, Trusts are benchmarked against the number of antibiotics used with a high risk of antimicrobial resistance and C.difficile (categorised as ‘Watch’ and ‘Reserve’ antibiotics in the World Health Organisation's ‘AWaRe’ classification). The Princess Alexandra Hospital NHS Trust (PAHT) currently use 3077 DDD/1000 admission, the 7th highest non-specialist trust in England, against a national average of 2234. These figures will be monitored by our BI team in 2024 and more accurate figures should be available for 2024 - 2025. However, our Watch list antibiotic usage needs to be reduced. We are doing well with our Reserve list antibiotics, although Carbapenem use needs to be controlled better this year. Reducing antimicrobial burden and the use of these specific antibiotics are a key priority for the Trust going forward.
Following on from last year’s external peer review, we continue to work through the action plan which includes reducing antibiotic burden, reviewing treatment protocols and reducing course lengths, monitoring antibiotic use in hospital and improving medical engagement with the antimicrobial stewardship (AMS) agenda. We are excited to share our work with the NHS England regional team when they visit the Trust in May 2024.
The C. difficile threshold for the 2024-25 year is not yet known, but it is expected that there will be some changes to definitions to reflect the new protocols from UKHSA. Control of C.difficile will remain a top priority for our clinical teams, the Infection Prevention and Control (IPC) Committee, and the Antimicrobial Stewardship Group in 2024-25, as well as for the region.
Table 4: C.difficile cases 2023-24

Meticillin Resistant Staphylococcus Aureus (MRSA) Bacteraemia Infections
There was one case of HOHA MRSA bacteraemia this year, and no COHA cases. This was the first HOHA MRSA bacteraemia case that the Trust has had in 18 months (the last case was December 2021). PAHT is below the EoE regional average rate per 100,000 occupied bed days (0.70 for the Trust, compared to 1.57 for the EoE region), and also has the lowest rate of the three acute Trusts within the Integrated Care System (ICS) for MRSA bacteraemia cases.
Whilst it is reassuring that the Trust continues to have low numbers of MRSA bacteraemia cases, it is important that we continue to learn from the case this year (and from our MSSA cases), particularly in relation to the management and care of intravenous (IV) peripheral devices due to the risks associated with blood stream infections.
There is also a zero tolerance to hospital onset MRSA bacteraemia; where cases do occur, a full review of the incident is undertaken between the IPC and clinical teams, with clear actions required to reduce the risk of further avoidable cases.
Table 5: MRSA Bacteraemia cases 2023-24

Methicillin Sensitive Staphylococcus Aureus (MSSA) Bacteraemia Infections
Unlike some other alert organisms, there is no trajectory in place for MSSA bacteraemia, however, the Trust has continued to closely monitor and review its cases. PAHT previously had low rates of MSSA bacteraemia cases, however, over the last few years there has been an increase. This is reflective of national data, with some infections significantly increasing during the COVID-19 pandemic. This year however, there was a total of 11 HOHA and one COHA cases in 2023-24 (as seen in the below table), which is a significant reduction compared to the 19 cases last year (15 HOHA cases and four COHA). In comparison to the region, the Trust is considerably below the EoE average rate per 100,000 occupied bed days (8.39 for the Trust, and 13.95 for the EoE region), and also has the lowest rate of the three acute Trusts in the Integrated Care System (ICS).
This progress may be reflective of the blood stream infection improvement plan that the IPC team have been leading on, which has included several work streams including Trust-wide IV peripheral device audits, the appointment and development
of IV Champions in all clinical areas, education and training, and new and more meaningful audit tools to be used by the clinical areas. Additionally, the formation of a Task and Finish group, with divisional membership, as well as the practice development team and medical education. The purpose of the group is to oversee the work streams to ensure learning and appropriate actions are taken. Additionally, as with C.difficile, a thematic review of our MSSA cases, and the development of a BSI Improvement Plan and investigation tool are currently being progressed and is expected to be implemented in the early part of 2024-25.
Cases have been reviewed as part of the IPC Incident Review Panels and IV peripheral devices have been the source of infection in several; therefore, although a reduction in numbers is reassuring, this remains a priority for the Trust to ensure there is engagement from all divisions (medical and nursing colleagues) in further reducing BSIs.
Table 6: MSSA Bacteraemia cases 2023-24

In line with the ambition to reduce the incidence of gram-negative bloodstream infections (GNBSI) in England, the IPC team have been monitoring trends in GNBSIs throughout the year. Our local data matches national trends, except we report more respiratory source infections. The IPC team plan to review respiratory source infections in 2024 – 2025, and monitor this trend.
The largest number of GNBSI patients are those of urinary origin; various strategies have been used to reduce infections over the past few years. These include sepsis prevention, UTI and catheter-related UTI prevention, better dissemination of patient information (hygiene, good hydration), improved education and training of staff, antimicrobial stewardship (improved antibiotic management of UTIs), and surveillance.
Another significant GNBSI patient group are those with hepato-pancreato-biliary (HPB) disease. NHSE have made recommendations about this patient group.
y Gallstone disease is the most prevalent cause of HPB GNBSI. In almost 80% of cases of symptomatic gallstone disease prior to a GNBSI episode, and contrary to NICE recommendations, cholecystectomy had not been performed. Operations should be carried out soon, rather than through an elective waiting list. There is a wide variation amongst hospitals in relation to laparoscopic cholecystectomies performed as an emergency. In addition, patients presenting with biliary disease in the community, should be referred for a laparoscopic cholecystectomy.
Other strategies to reduce HPB associated GNBSIs include:
y Intra-operative cholangiography during laparoscopic cholecystectomy, to reduce the incidence of residual bile duct stones after cholecystectomy
y For operable HPB cancers, omitting pre-operative biliary drainage or stenting to reduce GNBSI during surgical delays
y Draining malignant biliary obstruction with self-expanding metal stents, rather than plastic stents
In 2024 - 2025 the IPC team would like to also direct their focus towards this group of HPB patients, and work with colleagues as part of a wider MDT to reduce GNBSIs in this patient group.

Table 8

Table 9

Norovirus
Norovirus is a common cause of diarrhoea and vomiting outbreaks in hospitals (and other close contact settings) during the winter months. Incidences have risen at this time nationally, most likely because people are now having more contact again, and reducing IPC precautions in the community.
There were four outbreaks of confirmed Norovirus in the Trust during 2023-24. There were also four ‘periods of increased incidence’ of diarrhoea in the summer months, where no organism was identified from any of the patients. Following a case by case analysis, it was concluded that that most symptomatic patients had other reasons for having diarrhoea. The IPC team met with Integrated Care Board (ICB) colleagues to discuss whether there were any themes/learning outcomes from these outbreaks (the source could not be confirmed although in one outbreak, two patients tested positive for Rotavirus).
The microbiology laboratory is now undertaking viral polymerase chain reaction (PCR) testing on stool
specimens on site, which is helpful in receiving results much more promptly, and for decisions to take place in a much timelier manner around bed closures/opening. Previously samples were having to be sent off site for testing which caused delays as positive/ negative results are crucial to aid decision making.
Increased cases of measles are currently causing a public health concern, and the UKHSA have recently issued several briefing notes on actions required to avert measles resurgence. Large outbreaks have been reported in the Midlands and case numbers in London are increasing. Towards the end of 2023-24, the EoE also started to see a rise in cases, and although numbers are small, the Trust had two confirmed cases admitted (one adult and one paediatric case, both unvaccinated) in total for 2023-24 in the community, however, case numbers are higher and particularly in certain communities where vaccination uptake is low. It is likely we will see more cases going into 2024-25.
The Trust has reviewed its local process against the actions required in the briefing notes, and the IPC team have taken a number of measures, including:
1. Ensuring the provision of oral fluid test kits are in place (or alternative viral swabs when they aren’t)
2. Development of a measles admission pathway
3. Working with the staff health and wellbeing (SHaW) team to ensure there is knowledge of staff vaccination against measles in high risk areas.
4. IPC progressing development of a measles policy
5. Ensuring clinical areas are aware of changes to guidance in the IPC national manual which states staff must be fit tested and wear an FFP3 mask
6. Working with ED to ensure prompt recognition of cases and supporting reception staff to identify potential cases (new measles posters)
7. Incident review meetings held for suspected/confirmed cases
8. Director and deputy director of IPC to attend a round table discussion on measles in the region, arranged and facilitated by the (ICB) in April 2024
Group A Streptococcus (GAS)
Prior to the COVID-19 pandemic, there were a number of seasons with elevated incidence of scarlet fever and iGAS, in particular in 2017-2018. During the COVID-19 pandemic (2019-2020 and 2021-2022), there was a significant reduction in notifications.
GAS can cause severe illness and, unfortunately with mortality in a small number of cases. Nationally, after the high case numbers during last winter (2022-23), scarlet fever notifications throughout 2023 stayed at the top end of normal seasonal levels. GP consultations for scarlet fever towards the latter part of 2023-24, demonstrates an increasing trend comparable to the previous season, but lower than the 2017-18 season. There is a normal seasonal pattern, with a slight December elevation followed by a slightly larger February/March increase.
As with scarlet fever, the rate of iGAS infection in the early part of the current season has followed a normal seasonal pattern, but at the higher end of the range. Rates were highest in those aged
75 years and older (8.8 per 100,000, higher than in the previous five years where the range was 1.5 to 3.9), followed by those under 1 year old (6.4 per 100,000), and 65 to 74-year olds (4.0 per 100,000). The lowest infection rate was in 10-14-year olds (1.1 per 100,000). The rates for different age groups are not the same as the unusual pattern in children in 2022/23. The median age nationally for iGAS infection this season is 56 years, in line with the range in the preceding six seasons (51 to 59 years).
Our local case numbers attending the urgent and emergency care department are lower in both adults and children compared to last year. For adults admitted, numbers are very similar to last year, whilst for children, less were admitted this year than last.
Total community cases for both adults and children were noted to be higher in 2023-24 than in than in the previous year. The highest number of cases was observed in December 2023, January 2024 and February 2024, with a reduction in the March 2024 cases.
The number of patients requiring admissions was low. Invasive GAS numbers were low, but with serious outcomes for some patients. The impact on IPC measures (e. g. side room allocation) within our inpatient areas was minimal. Cases will continue to be closely monitored.
As the year comes to an end, we continue to follow the national steer on managing respiratory viruses, in line UKHSA guidance and recommendations in the national IPC manual.
In 2024-25, the priorities for the Trust will be to continue with our improvement plans for the reduction of C.difficile cases, including the provision of AMS leadership. In addition, reducing the number of avoidable bloodstream infections for MRSA and MSSA with support from the Task and Finish group, and for Gram Negative BSI, a particular focus on HPB patients.
We continue to monitor other organisms including Measles and group A streptococcal infections, responding to these infections to control spread, and continuing to maintain nationally recommended IPC practices.
improvement
At PAHT we define quality improvement as: ‘Working together in partnership to make the sustainable changes that lead to us being modern, integrated and outstanding for our patients, people, places, performance and pounds.’
y Quality First team (QI and PMO
The Quality First team are based at The Princess Alexandra Hospital and include the quality improvement team, the programme management office and Alex Health transformation team. Together, we are dedicated to working alongside our people, patients and wider health and care partners, to ensure that everyone is equipped and enabled to deliver improvement and transformation.
y Quality improvement (QI) team
We inspire our people to put quality first for the benefit of our patients, our people and wider community. We achieve this by developing capability, strengthening confidence and enabling capacity to support and guide the organisation through continuous improvement and to achieve our strategic priorities, namely PAHT2030.
The quality improvement team has two key functions:
i) Lead PAHT’s Improvement Partnership, we build our people’s confidence and capability in delivering quality improvement and transformation.
ii) Centrally coordinate and facilitate for the delivery of quality improvement and transformation programmes and projects that:
1. address significant risks in the organisation
2. support the delivery and realisation of our strategy, namely PAHT2030
Next year’s focus will be to further strengthen and improve the improvement

partnership model to make it increasingly meaningful and valuable for our people to help increase engagement and involvement in quality improvement and transformational change at PAHT. Now, more than ever, this is important to help ensure we achieve the strategic aims and objectives outlined in our PAHT2030 strategy.
To deliver quality improvement capability building we use an Improvement Partnership approach that has enrolled, engaged, involved and developed our people in quality improvement and transformation. The Trust delivers two training programmes - leading change training and leading projects to continually educate and encourage new people to participate.
i) 2023/24 programme highlights The following paragraphs outline some of the projects and programmes that the quality improvement team have supported this year.
Improving patient outcomes (mortality improvement)
PAHT had been an outlier for hospital standard mortality rates (HSMR) for more than 36 months. We became ‘as expected’ for HSMR for the 12 months between April 2020-March 2021 and continue to be as expected.
Summarised below are the key highlights/progress related to mortality improvement over the previous year.
Aspiration Pneumonia
y Launch of shallow screening tool pilot on OPAL
y Development of a number of patient leaflets including modified diets and fluids, risk of feeding
y Mouth care audits in partnership with ward-based teams to target improvement efforts.
y This has now been handed over to business as usual led by the speech and language team
Fractured neck of femur
y Following NHSE visit recommendations shared with key stakeholders
y The emphasis continues to be on improving the time it takes for this cohort of patients to be transferred from the emergency department to Tye Green. Some improvements were seen following the early identification of patients, including use of a ‘femur fracture alert group’ on Alertive to ensure fast track transfer of patients to wards
y The focus next year will be on improving time from ED to the appropriate ward utilising the recommendations from the NHSE report
Acute kidney injury (AKI)
y There were plans to introduce an e-referral in collaboration with the Lister Hospital, but this has been put on hold with the expectation that this will be addressed by introduction of new electronic healthcare record (EHR)
y Sepsis and AKI nurse recruited and in post and leading on training and relaunching of sepsis and AKI champions from March 24
y Ongoing development of sepsis digital assessments for both adult and paediatric patients to support their treatment using the sepsis 6 screen protocol
y Adult assessment went live in February 2024 - this should improve collection of data on compliance of sepsis 6
y Plans for paediatric assessment to go live within Q1 next year
y Support to relaunch the Deteriorating Patient Group
Outpatients
Patient initiated follow up (PIFU)
y This pathway allows patients to
determine whether their condition requires clinical intervention and allows access to a specialist when needed. In turn, this reduces the number of follow up appointments needed
y This pathway is now available to all specialties and circa seven thousand appointments have been saved. Fracture, neurology and physiotherapy are all exceeding the 5% target for PIFU
y Plans are being developed for 24/25 to explore further the use of the pathway for those patients who are admitted into hospital rather than automatically booking an outpatient appointment for review
Long term condition – patient managed pathway
y This pathway will allow our patients with long term conditions, who cannot be discharged from secondary care, to determine when their condition requires clinical intervention, allowing rapid access to a specialist when needed
y The pilot has been live since 10 October 2023 within gastroenterology for those patients with inflammatory bowel disease (IBD). As at 6 February 2024, this pathway had seen 70 patients placed, of which 13 had accessed the nurse specialist for support via a virtual consultation
y Breast cancer surveillance patients will follow as part of the pilot following a review of review requirements
y Due to the implementation of EHR, this pathway will not be extended further across all appropriate conditions as planned. The teams are working closely together with the Alex Health transformation team to understand the pathways in place following the introduction of EHR. At this point, this pathway will be expanded.
y We need to ensure people are treated in the right setting with the right clinician in a timely manner
y Ophthalmology have tested referral assessment services (RAS) to triage
referrals to the right clinic with the right diagnostics and refer back those patients who can be managed in primary care with specialist advice for managing their care. 17.5% of those referred in received advice on how to manage the patient's care
y In line with best practice, other referral optimisation methods are being explored and a pilot in Advice and Refer (A&R) went live in March 2024. Benchmarking from other Trusts has shown this has improved the rate of patients being supported in the community setting
Urgent and emergency care improvement programme
IN Improvement Programme
y Enhanced triage methodology and digital solutions have led to improvement from 60 minutes to below 30 minutes average time from arrival to triage/observations
y Emergency department (ED) streaming kiosk – development of the directory of service to facilitate the implementation of the kiosks to support alignment of patients to the correct area
y In (Assessment) – Implementation of a ‘back to assessment’ model in the Adult Assessment Unit (AAU) to facilitate greater flow through the emergency department
y In (Frailty) – Development of a plan to recover the core functionality including pulling patients from the front door. Development of a ‘back to assessment’ model
y In (ED) – Implementation of a further assessment model including increased assessment space for clinicians. Reduced patient safety risks by bringing decision making closer to the front door with the introduction of the Manchester Triage System
OUT Improvement Programme
y SAFER and R2G – Implementation of the SAFER Patient Flow Bundle ‘to make maximum use of capacity within acute care settings to support patient safety
y Criteria led discharge - Embed criteria led discharge (CLD) into practice across our inpatient wards,
implementation of a pilot process on the respiratory ward to improve patient and staff experience
y Site team and transport – Development of a standard operating procedure to facilitate the establishment of a new discharge lounge including changing the skill mix of the staff
y Integrated discharge – Moving from <30% to >80% Single Referral form first time acceptance has demonstrated improvements in quality as a result of training and targeted feedback
y Care Coordination Centre (CCC) and Virtual Ward. Pilot work with the Integrated Discharge Team to establish proof of concept for discharge pathways that enable a move from a push to a pull model for pathways 2 and 3. Working with virtual ward team to support a new way of working
y To take away medications (TTAs) –Implementation of a portering service to support earlier discharge on the wards
Nerve centre ED module
y Implementation of the Nervecentre Emergency Department (ED) dedicated solution in both adult and paediatric EDs. To support improving patient safety, patient experience and patient outcomes. The module and functionality enable us to address concerns raised by our clinical staff and by the CQC in repeated reports
y Moving from three ways of documenting patient information in ED to one single solution which releases time to care for staff, avoids duplication of documentation and will help to ensure patients are seen within the national four-hour standard. The solution enables swifter assessment, treatment and departure of patients. Teams will also have better visualisation and oversight of patients, Improving patient prioritisation and flow
y This has now been handed over to business as usual to the urgent and emergency care (UEC) team

Patient and clinical administration
The aim of the project is to deliver patient and medical administration function that is modern, integrated and outstanding (PAHT2030) embracing digital solutions where possible to reduce duplication, human error and provide efficient and effective care for patients and an enhanced experience for our people.
The two key elements that are being focused on are digital dictation and the workforce.
General Medical Council (GMC) improvement programme
The team worked in collaboration with the medical director and director of medical education to develop a programme to comply with the GMC and HEE standards and requirements for the delivery of all stages of highquality medical education and training. In addition, this was to support an improvement in the experience of our trainees to positively influence the results of the GMC survey and to ensure we benchmark nationally at average or better.
The main elements supported by the team were implementation of a “too tired to drive” policy, improvements to local inductions, availability of appropriate equipment in ED resus, continuity with escalation of clinical concerns out of hours and facilitation of listening events. These were handed over to business as usual in September 2023.
The programme outcomes are monitored though the monthly GMC enhanced monitoring meeting chaired by the medical director.
Integrated Musculoskeletal (MSK) Service
Summarised below are the key highlights/progress related to the Integrated MSK Service.
y Full pathway review undertaken by the partnership
y Efficiencies within the contract identified. Agreement on services that will be commissioned from April 2024
y Improved communication between the partnership
y Audit undertaken of referral routes to ensure referrals are going via the MSK community hub service. The audit showed that referrals from Primary Care are going via the MSK community hub
y Community Extended Scope Practitioners (ESP) have increased their capability and can now carry out ultrasounds and ultrasound guided injections
y All First Contact Practitioners (FCPs) are now in place across the patch, providing an extra 4110 contacts with a physiotherapist at the point of accessing primary care
y New shoulder pathway has been developed between community and secondary care allied health professionals (AHPs)
y Rheumatology are triaging review list patients and moving stable patients out to the community GP with Specialist Interest (GPSI)
y Shared decision making (SDM) training has taken place across the partnership
y Hip and knee replacement length of stay has improved from 7 days in Q4 2022/23 to 3 days in Q3 2023/24
y Processes in place to ensure more patients go to joint school before surgery
y Hotline and hot clinics set up for postoperative issues
y Post-operative hip and keen rehabilitation classes moved to the community
Summarised below are the key areas of focus for next year for the Integrated MSK Service.
y Develop a new reporting dashboard in line with contract changes
y Review spinal pathway and criteria with a view to set up a spinal multidisciplinary team (MDT) meeting between community and secondary care to reduce discharge at first appointment and increase conversion rate
y Implement GIRFT outpatient templates, when available.
y Increase PIFU usage to 5%
y Reduce DNA rates to 5%
y Reduce discharge at first appointment
y Increase conversion rate
y Increase the number of nurse and AHP clinics
y Review pathways and criteria, working alongside all MSK providers in the ICS
Theatres optimisation
The aim of the theatre efficiency programme is to improve theatre utilisation to 85% by April 2024. There are three primary drivers which include:
y Weekly meetings to ensure fully utilised theatre sessions and lists locked down at two weeks. This is now supported by an updated 642 Standard Operating Procedures (SOP)
y Monitoring and escalation process for on the day cancellations
y Monitoring of fallow sessions to allow reallocation to other specialities
y Next steps - fallow sessions to be redistributed based on demand
Pre-operative assessment
y High risk anaesthetic waiting list has been through validation
y Cardiopulmonary Exercise Test (CPET) has been installed and is now being utilised in conjunction with the High-Risk Anaesthetic Clinic (HRAC)
y Next steps – implement standby patient pilot with urology
y All specialities utilising theatres dashboard to inform of activity at Consultant Only Group (COG) meetings or service reviews
y Consultants aware and more engaged with data
y Utilisation has been gradually improving and reached 77% and 78% during November and December 2023.
y January 2024 has seen a drop in utilisation mainly due to winter pressures and beds and ITU availability, estates issues with theatres (e.g. leaks) which have required patients to be cancelled on the day or at short notice resulting in an inability to backfill these slots
y Targeted approach by speciality for test of change
y Deep dive into late starts in ADSU
y Explore standby patient or overbooking lists to ensure theatre time not lost due to on the day cancellations.
y GIRFT to revisit ophthalmology in March 2024 to support dedicated cataract lists
y Trauma and orthopaedic (T&O) Getting it Right First Time (GIRFT) revisit in six months

Electronic Health Record (Alex Health) transformation
There are three key elements (figure 1) that will underpin our approach to EHR transformation and they are communications, training and change management. These three distinct areas will need to work together to ensure our people fully embrace the EHR and associated new ways of working. This is critical to us achieving the successful implementation of the EHR and associated benefits realisation outlined in the business case.
Communications and engagement as well as education and training will need to be targeted and informed by outcomes of change management efforts, so they best meet the needs of our people in the delivery change. A huge amount of work has already been completed and there is a strategy and plan in place to support transformation go-live, adoption and optimisation efforts, which is tracked formally via the implementation and programme board for Alex Health.

Programme Management Office (PMO)
The PMO is an independent, trusted advisor and support service that enables the Trust to do the right thing, at the right time, using the best practice project management tools and techniques that support the delivery of organisational goals.
The PMO operates flexibly across PAHT sites, whilst maintaining an ‘engine room’ on main site to drive delivery programmes. The PMO has expanded both its remit and responsibilities since its inception to support and respond to the Trust's ambitions and strategic priorities.
Essentially, the PMO, as part of the wider quality improvement team, enables the Trust to become modern, integrated and outstanding.
The PMO provides assurance, oversight and governance to the Trust Board, executive team and wider stakeholders of the key projects and programmes undertaken at PAHT. The PMO ensures there is an effective framework and governance for the management of project and programme deliverables, ensuring sustainable change is implemented and benefits are identified, monitored, managed and ultimately realised in a timely manner. The PMO focuses on driving, embedding and sustaining quality improvement through an evidence-based approach and work with a wide range of stakeholders across the Trust and wider system to enable and drive the successful delivery of key projects and programmes.
The PMO employs an appreciative enquiry and engagement approach which is supportive, collaborative and empowering. The PMO have embedded a standardised approach to project and programme management across the Trust and have established clear and robust governance processes in relation to delivery, responsibility and accountability, underpinned and utilising the Trust's Accountability Framework (AF).
The PMO works with stakeholders to codesign and co-produce programmes of work, ensuring a balance of top down and bottom up approaches. The PMO provide and analyse benchmarking data from a variety of tools including Model Health and GIRFT to identify opportunities, inform Trust and divisional delivery and improvement plans, track the delivery of key metrics and enable informed and evidence-based decision making. The divisions utilise the outputs from the PMO to inform their patients, quality, productivity (PQP), quality improvement (QI) and wider programmes of work.
PM3, programme and project management
The PMO continue to utilise a project management system called PM3 to track the delivery of projects and programmes. The PM3 system is fully managed by the PMO enabling project leads, project managers and project teams to effectively manage, document, report and deliver projects and programmes of work. In turn, the PM3 system enables the PMO to track and report on the delivery and monitor progress, issues and risks effectively, enabling the PMO to track hundreds of projects using the system's reporting functionality. There are currently 234 trained PM3 users, and a total of 956 projects captured on the system, of which 320 are currently active and 280 have been delivered and closed with measurable benefits delivered, with the remainder in pipeline for future delivery.
The PMO have supported and driven the delivery of the key major projects and programmes at PAHT over the past two years. This includes driving the delivery of the five strategic priorities of PAHT2030 (transforming our care, our culture, digital health, new hospital, corporate transformation) and the various projects and programme there within, including the production of the Trust's 28 clinical strategies, overseeing the planning of the new hospital, a high level oversight of the implementation of
the new electronic health record (EHR), monitoring the development of the ‘our culture’ programme and overseeing the delivery of the corporate transformation programme.
The PMO work with the wider QI team to enable and report on the delivery of quality improvement initiatives undertaken across the Trust, including those quality improvements led, supported and facilitated by the Quality Improvement team. Work is also continuing in partnership with the wider QI team and the business intelligence team to produce the Trust's Outcomes Framework.
The PMO work closely with the Trust's patient safety and quality team as part of the Quality PMO, jointly overseeing QCIG (Quality Compliance Improvement Group), which oversees the delivery of regulator improvement actions.
The PMO have also led the successful delivery of the 2023/24 Patient, Quality and Productivity (PQP) programme, which has seen measurable patient safety and quality improvements across all divisions, as well as substantial financial and productivity improvements totalling £16.5m in year. The PMO have also overseen the production of the 2024/25 PQP programme plans.

The patient advice and liaison service (PALS) are the public’s first contact service and in total responded to 4410 concerns in year, this has increased by 162 cases when compared with 2022-23.
The service has been proactively developing a number of new ways of interacting with members of the public, including a main entrance reception PALS service (pictured, bottom right), drop-in service, flyers and pop-up banners, as well as supporting Alex, our digital receptionist (pictured, top right) who can respond to your questions when we are not available.
Every year, the Trust must make a statement under Section 18 of the NHS Health and Social Care Act 2009 about how many complaints it received, whether or not they were well founded, their subject, the issue they raise, and any actions taken. This report is intended to satisfy that requirement.
The Trust received 172 complaints in 2023-24, this has reduced by 34%.
Of the 207 complaints closed during the year 2023-24 (the point at which we can determine if the complaint is upheld)
y 6 complaints fully upheld
y 158 complaints were partially upheld
y 9 complaints were not upheld
y 7 complaints were not raised by our patient so they were asked to consent to the investigation and failed to return their consent
y 23 ended contact with the Trust.
y By identifying a case as upheld, we mean that at least one of the concerns raised meant action was required by the Trust to address the issue
Of the 172 complaints raised against the Trust, the most frequently occurring themes related to:
a. Medical care with 28 cases
b. Communication issue with 26 cases
c. Nursing care with 24 cases
d. Other subjects are noted as in the



What actions are being taken in response to the subjects of complaints
Medical care related actions
y One of the biggest changes planned in how we deliver care is about to begin, driven by patients, our follow up on the Electronic Health Record (EHR) and multiple disabilities event on 21 June 2023, with the patient portal workstream lead and subject matters experts coming from that workshop
y We ran an event to better understand how we could support long-waiters, awaiting planned care, this was on 20 July 2023 and that data is
now informing the support package patients and their families get while they are waiting, targeting the 20000+ patients in our system awaiting a first appointment
y We continue to share compliments and complaints with the CMO and senior medical staff to alert senior colleagues to the concerns and compliments
Communication related actions
y The patient experience team now offers a service co-located at the main reception every morning so that anyone who is coming into the hospital in the morning can speak to someone in person as soon as they arrive. We are also working on improving the experience at the front entrance so everyone a patient or their family might need is available at the first point of contact
y The Trust is running communication simulation workshops working with HealthWatch Essex Ambassadors and Patient Panel members and including people with physical and sensory impairments
y Communication training led by the patient experience team (PET), (SAGE and THYME) achieved 67% compliance. As a result, we have a one third drop in PALS concerns relating to communication (just 16% of all cases now relate to communication)
y Partnership working with HealthWatch Essex on the Accessible Information Standard is ongoing, with support for the identify, record, flag and share process
y Ongoing outreach events in children’s centres and the African community working with the Maternity Voices Partnership (MVP) have been delivered with new events being planned with the MVP chair
y Outreach events in the community with the Patient Panel – at Bishop's Stortford and Epping
y A cancer outreach project run by the patient experience team with our primary care colleagues concluded the year with an event for 300 members of the primary care networks, with the intention of bringing services together around patient experiences of the cancer pathway
Nursing care related actions
y The noise at night project is nearing completion. It launched in April 2024 with posters, pop ups, and ward level noise measurement on four wards
y A partnership to support carers' needs with Governance International is nearing its conclusion, with new groups contributing towards a carers' panel
y We will continue to deliver and develop the PACE ward accreditation programme to reduce unwarranted variation in patient care and improve the quality of care given. This is undertaken through the identification and sharing of good practice in one overarching framework and a clear set of standards. PACE further supports the development of shared governance within the Trust
y The Fundamentals of Care work stream launched across the inpatient ward areas with an initial focus on teaching and audits of mouthcare, continence, nutrition and pain management. Further plans are in place for continuation of this work during 2024/5, with a launch of a Trust wide communication and education campaign from summer 2024, with a focus on patient posters and leaflets and our review of monitoring progress using our PACE process that will include monitoring the fundamental care
y A new patient satisfaction system (we call this FFT) is being implemented across the hospital
Complaints and PALS process improvements workshops
y Complaints are down from over 160 open cases at the peak to now 103 cases open
y A revised way of checking complaints (we call it CMG (complaints management group) is now embedded and has supported the resolution of 60 complaints raised by families, improved response times and improving the coordination of investigations across clinical divisions
y We are repeating a face to face training offer in May and June 2024 on developing effective written responses to complaints in healthcare, which was well received with 62
Compliments
374 compliments were received during April 2023 to March 2024, these related to care given in the following services:
y Surgery division (143)
y Medicine division (79)
y Clinical support services (64)
y Urgent and emergency care (34)
y Child health and women’s services (30)
Case studies
These are case studies presented at the patient experience group, which takes place every other month. At each meeting, one division provides a detailed update on its current learning from complaints and its process that has taken place as a direct result of our patients’ feedback to us. The following four case studies were presented during the year.
Clinical support services division
y A patient waited 5 months for a skin biopsy, which was recognised once reviewed as a possible malignant melanoma (a type of skin cancer)
y The patient had previously been seen by an outsourcing company and treated with antibiotics, but follow up care was delayed for 3 months, and only addressed as the condition was not improving
Learning and actions taken
y All dermatology clinicians have undertaken a new university–led ‘dermoscopy’ course to enhance diagnostics
y Monthly metrics on diagnostic accuracy captured and action plans in place for clinicians where needed
y Diagnostic accuracy discussed at monthly Clinical Service Group meeting, medical photography and all clinicians have been given their own iPad to facilitate this
y A new dermatology standard operating procedure (SOP) has been written and in-depth training carried out with all the team
y Training for multi-disciplinary team (MDT) trackers to ensure they can
escalate if incorrect process is followed regarding ‘off cancer pathway’ Surgery and critical care division
y Patient attended the emergency department (ED) after advice from his GP as he was passing blood in his stools and had changed bowel habits
y Following examination, the patient was advised to attend the Same Day Emergency Care (SDEC) Unit the following day for a CT scan
y When the patient attended SDEC the following day, the CT scan was rejected by the radiography team and the results from the examination performed by a surgical doctor differed from the previous examination
y Patient was advised to return to his GP and ask to be put on the colorectal pathway
y The patient decided to be treated in the private sector, he had surgery to treat lower rectal cancer
y Patient did then receive a follow up colorectal appointment 7 months after his ED attendance
y The patient experienced poor communication in terms of his complaint being handled and a long delay in receiving a written response
Learning and actions taken
y The complaint was presented at the surgical mortality and morbidity meeting (attended by many clinical and non-clinical services intended to understand the patterns of care outcomes for patients, including death and disease progression), session in February 2024
y This informed a discussion for junior doctors on how to perform a good rectal examination and which diagnostic tests needed to be booked following a rectal examination
y The service has a plan to review and improve the pathways between the emergency department and the surgical team to ensure cancer referrals can be made directly
y The case has been shared with primary care services through to refer to speciality if there is a suspected cancer diagnosis delegates participating from across the organisation last year.
Medicine division
y A 78-year-old man with a learning disability (LD) attended the emergency department (ED) after advice from his GP as he was passing blood in his stools and had a change in bowel habits
y Patient lived a full and active life for 30 years in the same care home, and was only admitted to hospital after developing swallowing difficulties due to recurrent aspirational pneumonia
y The family were aware of the deterioration in his condition and supported plans for palliative care, visiting frequently. He developed an unstageable pressure ulcer which had a significant effect on his outcomes. Sadly, following transfer to a new care home, he died the same day
Learning and actions taken
y A number of errors were made, his condition being recorded as dementia, not a learning disability, and so he lacked specialist support, this is being addressed through new training with the learning disabilities nurse specialist
y Having a learning disability, the patient should have been considered a vulnerable person and since he was unable to comment on his wellbeing, his care plan should have taken this into account
y Changes made include the tissue viability nurses (who are responsible for making plans to protect the skin of our most vulnerable patients), support to ensure that all staff have the correct training and information is available
y Ensuring daily ward manager assurance audits complete a review of one set of healthcare records each day to ensure quality of documentation is good
y Launch of care colour circles as a visual guide at a glance to identify those patients who need repositioning and when to support with the prioritisation of care.
Children’s services
y Patient attended the children’s emergency department twice and was discharged both times. 24 hours
later the child presented to Broomfield where they were admitted for suspected sepsis
y Patient was treated for cow's milk protein allergy and discharged with advice and safety netting
y 24 hours later the child presented to Broomfield hospital where the child was admitted for suspected sepsis
Learning and actions taken
y Patients require a repeat set of observations and review by medical teams prior to discharge
y As a result, we have now implemented a discharge proforma to ensure all patients are safely discharged. This includes a set of observations and review by a senior doctor and changes in how sepsis is managed on our health record system
y We have now added three sepsis link nurses in our emergency department who audit sepsis data and keep colleagues updated with learning and changes in practice
y Practice development nurses focus on sepsis training and awareness for each team every quarter, and during paediatric simulation training, sepsis is one of the focus subjects

This past year has been a period marked by both successes and challenges, and our Patient Panel’s commitment to serving our patients has remained steadfast.
This year, there have been significant strides in enhancing patient care through initiatives that covered many areas from nutrition and hydration, accessible information and accessibility around the general hospital site.
Our Patient Panel celebrated its 10th anniversary with a short film covering this period, available via the QR code (right).
Working with our estates and facilities team, the Patient Panel supported the installation of a new bus shelter and lovely flower boxes which have been placed throughout the hospital grounds (pictured, right). These were implemented as a direct result of feedback received from the Patient Led Assessments of the Care Environment (PLACE) review at PAHT. Any member of the public can join this year’s visit.


The panel has continued its work on nutrition and hydration, the foundation for which was established by late panel member Mollie Pattenden, who sadly passed away last year. As a result, patients and visitors are now able to obtain refreshments 24 hours a day in the main hospital restaurant and the Trust is working towards a plan to have hot, healthy meals available to patients, visitors and staff during the out of hours period following a major refurbishment of the hospital restaurant that is underway from March to June 2024.
and the public, because it’s Good to Talk
Our Patient Panel have hosted events to support service users to meet Patient Panel members and talk to them about healthcare for our community - known as “Good to Talk” - with the aim to gather feedback about the hospital services. So far there have been events held in Harlow Central Library in January 2024 and The Harvey Centre in Harlow in February 2024. These were supported by the chair of the Trust Board, and further event planning is underway to meet in Jackson Square, Bishop’s Stortford and Epping High Street. More details will be shared via social media, including X (formerly Twitter_ @panel_patient).
On 12 March 2024, the Patient Panel, together with our cancer outreach project ‘One Step at a Time’, hosted a cancer pathways event for over 300 primary care professionals at the Great Parndon Community Association in Staple Tye. This is already yielding benefits, with discussions about better collaborations between primary and secondary care. This event arose following evidence received following a meeting to support cancer professionals on 29 November 2023 which revealed gaps in the knowledge of hospital staff about how cancer pathways and care operate in the community.

Fundraising
The Patient Panel hosted a fundraising stand at the front of the hospital, supporting the Royal British Legion charity, ahead of Remembrance Day. Staff from across PAHT volunteered to help raise funds, consistent with our commitment to the Armed Forces Covenant, signed on 27 October 2023. This demonstrates our commitment to supporting veterans across all areas. The team raised just over £1,600 in five days. In addition to this, once again wreaths were laid by the chief nurse and members of staff who are former veterans on Remembrance Day.
Financial overview
Financially, through prudent management of the small budget, the Patient Panel have ensured that their resources were directed towards improving patient information and services. They continued to provide at least one conference each year on items that are of interest to the local community. The panel also support the hospital divisions with the Patient Panel awards.
Challenges and adaptations
The year also brought its share of challenges, particularly with the moving of phlebotomy to Gibberd Ward. However, additional Blue Badge spaces were installed and information was shared across our communications channels to ensure the local community were aware of this change.
Looking ahead
The Patient Panel have started work looking at:
y The role of unpaid carers, who are recognised to contribute an incredible amount of support to our patients when they are in hospital and we want to support them
y The reception area in the main hospital entrance, to make it work better for patients and visitors
y Working with the Integrated Care Board colleagues to work jointly with our neighbouring services and providers
y Working on a patient portal, as part of our new electronic healthcare record (EHR), Alex Health, focusing in particular on digital inclusion
y Discharge process, as we know from talking to patients, this is an area of concern
y New hospital
Achievements
y Part of the work of the Patient Panel is to review complaints. Some of the evidence they saw showed how as panel members they can support problem solving through early intervention, which they called ‘nipping it in the bud’
y As a result of this, the Trust listened to their views and provided access to the patient advice and liaison service (PALS) at the main entrance Monday to Friday on the main desk. Since this was commenced, the panel have seen evidence that complaints are falling and this year alone went from 262 to 176

y Communication workshops, which have involved patients with a visual impairment, and the newest members of the panel as part of a new clinical simulation programme working with the PAHT medicine division
y The panel were winners of the ‘Fork Handles’ (The Two Ronnies’ sketch) Award for their work on nutrition and hydration. They presented a poster about this work which showed how we should design malnutrition out of the system. That video can be viewed via the QR code, right
y Ann Nutt, chair of the Patient Panel, won Volunteer of the Year at the National Unsung Heroes Award for NHS staff in March 2024
The panel had an increased workload in the last year and unfortunately, lost a few panel members. They recruited five new members, which has enabled them to become more diverse as a group and bring people with a diverse range of knowledge, skills and experience to their work. The new members are bringing needed skills to the panel and they would welcome more volunteer members. To get involved in any of this work – please email: paht.patient.panel@nhs.net
The panel members would like to extend their heartfelt gratitude to all of the hospital's dedicated volunteers, and the staff, senior managers and consultants who support them and work with them in their panel role. Your unwavering support has been the cornerstone of the Patient Panel's success.

Improving care for patients with delirium and dementia
We have made good progress on our goal to deliver the very best possible care for our patients with dementia, in line with national policy. We have in place an integrated dementia strategy, which has key performance indicators in the following areas and is monitored through our dementia and delirium steering group.
y Find, assess and refer pathway
y Person-centred care (recording of ‘This is Me’)
y Comparison of harm related incidents for patients with dementia (development of a dashboard)
y Training plan
We have recently participated in round 6 of the national audit of dementia care in general hospitals, The Royal College of Psychiatrists (2019). Initial feedback from family carers about their experience of hospital care and the recommendations will inform part of our clinical strategy document.
Our dementia clinical nurse specialist (Caroline AshtonGough), has converted to an Admiral Nurse, supported by Dementia UK. Caroline’s role within the Trust is now supported with monthly clinical supervision and access to other training and learning opportunities and will support the strategic development of dementia care at PAHT. Her role will still provide clinical nurse specialist support. The Admiral Nurse role supports patients and their family carers with dementia/suspected dementia, supporting approximately 50 patients/staff and families per month.

In 2019, we undertook a project to introduce singing for the brain into the hospital setting. The aims were to reduce the social isolation that patients often experience during a stay in hospital, to improve wellbeing and mobility. Music therapy is known to play a crucial role in the care of many people with or without dementia, helping to minimise apathy, anxiety, restlessness and depression.
Following the successful pilot, we now provide a weekly music therapy session, which is facilitated by the clinical nurse specialist for dementia and volunteers. The sessions are delivered at the bedside if required on a 1-1 basis or in small groups. The plan for the early part of 2024/5 is to look at expanding the variety of these sessions (a ukulele band are visiting in May).
Delirium (sometimes called ‘acute confusional state’) is a common clinical syndrome characterised by disturbed consciousness, cognitive function or perception, which has an acute onset and fluctuating course (NICE 2010). The risk of mortality following a delirium episode in a person with dementia is more than 40%. To support our staff in the care of patients presenting or developing delirium in hospital, we now have established new pathways and guidelines. We also have a leaflet designed to be given to patients and their families or carers. There is a plan to have an electronic assessment.
Dementia training for our people is delivered face to face at new colleagues’ induction to the Trust. To support our patients, we have introduced mandatory training on delirium, as well as creating dementia and delirium simulation training. This has
received excellent evaluation and we have helped to set this up at the Lister Hospital. This training complements the dementia training that already exists for our people and we are proud of our virtual dementia tour, which enables our people to experience what it may be like to have dementia, and learn how to work with people living with dementia. Tier 2 dementia training has now been introduced into our preceptorship programme and healthcare support worker programme, and is available to all of our people who have regular contact with people with dementia.
Namaste care “to honour the spirit within" offers a respectful and supportive approach to care for those living with advanced dementia, integrating compassionate nursing and therapeutic activities. Working closely with St Clare’s Hospice, we have introduced Namaste care at PAHT with the support of the dementia clinical nurse specialist (Namaste champion), who will develop the role of Namaste volunteers in partnership with PAHT volunteers. A dedicated room space will need to be identified. Currently, Namaste care sessions are delivered weekly and we are embedding a Namaste approach to delivering compassionate care in everyday nursing care. The Dementia CNS works closely with St Clare's Hospice (SCH) and supports with the Namaste training.
We were successful in obtaining funding through NHS Charities Together (NHSCT) to recruit a carers' lead, this was a Band 6 role with a view to extension if successful. Future plans will be to develop a business case for a substantive role. A carer’s information stand, when possible, is available Monday-Friday lunchtimes, this has proved successful and enhanced the communication between carers and ward staff and has resulted in more family carers being supported. A Dementia Information Hub has been set up, running almost weekly dependent on leave, this hub is available for family carers and staff at PAHT and will be extended to the wider community.
This project continues to provide such wonderful moments for our patients and our people. The project was developed during 2021/22 and started on 6 April 2022, led by our voluntary services. Ward visits with therapy dogs provide reminiscence, conversation, loving touch and comfort.
We have a robust focus and governance process in place to monitor safeguarding concerns. We have a team that oversee provision of advice, guidance and training to our people to ensure we provide care that maintains patient safety. Our specialist safeguarding team work collaboratively with our community partners to ensure this important aspect of patient care is delivered to a high standard.

We were successful in a bid to NHSCT for £88,000 to develop three therapeutic garden spaces: a dementia sensory garden, a spiritual garden, and staff gardens. The Princess Alexandra Hospital Charity are match funding this project. This
exciting project is in the planning phase. It will involve the wider community and provide opportunities for volunteers, including those living with dementia.
We recognise the environment in hospital can be unsettling for our patients with dementia and delirium. We are working closely with our Patient Panel, our Trust Board, estates team and external companies to enhance our environment. While some progress has been made, there are challenges around infection control and plans for ward refurbishment. An audit by The King's Fund is soon to be undertaken alongside Harlow Dementia Friendly Communities.
The Trust supports the use of Hospital Passports and the Purple Folder (which contain valuable information about each patient) that will support our people to provide personalised care to those who have a learning disability or are autistic.
Wherever possible, the Trust will support adjustments such as giving double time for an outpatient appointment to allow for a meaningful discussion, or allocating a quiet area for a patient to wait whilst in the outpatient department. Support is given to patients on our wards by allowing input from their family and carers to assist them to feel more comfortable when being cared for in an unfamiliar environment. This will support patients with a learning disability or who are autistic to access and use our hospital services.
The Trust has a learning disability team and their role is to specifically support our patients with a learning disability or who are autistic to ensure that we fully utilise the valuable information stored within the documents our patients bring into hospital with them, such as the passport, and this will support our outpatient and ward staff to make adjustments to how they deliver care wherever they are needed.
The Trust will promote Oliver McGowan training, which is focused on learning disabilities and autism. This is part of a nation-wide rollout across England to ensure our people have the right skills and knowledge to provide safe, compassionate and informed care to autistic people and people with a learning disability.
The training is named after Oliver McGowan, whose story and death in 2016 has shone a light on the need for health and social care staff to receive better training in understanding, communicating and treating people with a learning disability and autistic people. The training has been co-produced and co-delivered by trainers with lived experience.

Patient safety is our priority and we continuously work to ensure that incidents are managed effectively, promptly and most importantly that we learn from them and share the improvements arising with relevant colleagues.
A patient safety incident or adverse incident is defined as ‘any unintended or unexpected incident which could have, or did lead to harm for one or more patients receiving NHS funded care’. This includes all terms such as adverse incidents, adverse events and near misses, where an incident was recognised and averted.
For the year 1 April 2023 to 31 March 2024, 13,496 incidents were reported on the Trust’s Datix incident management system; this is comparative to the previous year’s reporting. Figure 24 below shows the spread of incidents arising across our divisions.
Figure 24: Incident reporting data for period 1 April 2023 – 31 March 2024

A large proportion of our incidents are not about patient safety and these are detailed in Table 10 below.
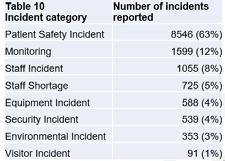
The top 10 categories of patient safety incidents reported in this financial year are summarised in Figure 25, with themes of care incidents detailed separately in figure 26. These are reported to the National Reporting and Learning System (NRLS) to enable learning and comparison with similar sized organisations across the country to occur.
Figure 25: Top 10 categories of patient safety incidents for 1 April – 31 March 2024

Figure 26: Top 10 themes of care in patient safety incidents given for 1 April –31 March 2024

The Trust raised 19 serious incidents (SIs) during the period 1 April 2023 to 31 March 2024. 3 of these incidents have been raised since January 2024, when the Trust commenced management of incidents using the national Patient Safety Incident Response Framework, these incidents are now called Patient Safety Incident Investigations (PSII). Figure 27 shows the comparisons of incidents raised in 2023-4 against those in the previous year.
Figure 27: Number of serious incidents reported - a 2-year comparison of

Once an SI/PSII investigation is concluded, an action plan is developed to capture the learning and recommendations that need to be undertaken to prevent a reoccurrence. The Trust uses a sharing the learning report to ensure all relevant staff are aware of:
y the key issues that occurred in this incident
y the changes to practice either implemented or being completed y what the learning from the incident is to prevent reoccurrence
This is presented and shared widely within the local teams where the incident occurred and if relevant to other clinical areas with divisions across the Trust. This information is reported in a Trust wide report that is taken to monthly or quarterly quality governance meetings, including the sub-committee of Trust Board, the Quality and Safety Committee.
Of the 19 SIs/PSIIs raised during 2023/4, three were Never Events. The investigation has concluded for two of these incidents with robust action plans completed and shared. A subsequent audit to confirm the actions are embedded into staff practice has given assurance this work was completed. The remaining Never Event investigation is ongoing, immediate actions were developed and implemented until the conclusion of the report is completed.
Examples of changes implemented as part of learning from incidents
Pressure ulcers
Repositioning of patients in a timely manner and accurate maintenance of records supports pressure ulcer prevention. The implementation of a project called ‘Care Colour Circles’ provides a visual aid to staff that enables prioritisation of patients according to their pressure ulcer risk. This initiative was introduced onto three inpatient wards. There is now a plan in place to introduce this onto all inpatient wards at the Trust.
E-consent has been implemented at the Trust, which allows clinicians to complete an electronic consent form during virtual clinic appointments, rather than on the day of surgery when both the doctor and patient are face to face.
Improvement work by the practice development team has taken place to ensure that nursing staff have gained the appropriate competency for undertaking and interpreting neurological observations.
Improvement work has been undertaken in the accurate recording and monitoring of insertion, removal and ongoing care of invasive devices. The practice development team have updated the peripheral cannula insertion training. Training has been supplemented by additional training provided by infection control for staff new to the organisation. Auditing is in place to ensure that this procedure is carried out to the required standard.
Improvement work has taken place to ensure that female patients of child bearing age receive the correct information and counselling to avoid pregnancy when taking a drug for a skin condition that would be harmful to a baby. The improvement work has involved:
y Pregnancy testing for all female patients of child bearing age that are prescribed these drugs
y Training has been provided to ensure that a patient’s electronic record shows that a patient is prescribed a high-risk drug
y Pregnancy prevention information and reminder cards have been made available to all clinicians
Medicines safety and reducing avoidable harm from medicines is of worldwide significance, with both the launch of the World Health Organisation’s ‘Medication without Harm’ initiative as well as NHS England’s recently launched Medicines Safety improvement programme.
Regionally, medicines safety is a core priority as services and pathways begin to become more seamless in the newly formed Integrated Care System (ICS).
Despite the increased service demands and challenges around staff resource, medicines safety continues to be a clinical and quality priority for the Trust, with improvements seen throughout the organisation. Medicines safety will continue to form a key driver of improvement within pharmacy and the wider organisation, as we strive to ensure our patients receive the most appropriate, most effective, and best value treatments, free from avoidable harm.
Medicines agenda and clinical priorities going into 2024/25 Medicines are the most common intervention in medical care. Medicines play a crucial role in maintaining health, preventing illness, managing chronic conditions and curing disease. In an era of significant economic, demographic and technological challenge it is crucial that patients get the best quality outcomes from medicines.
Medicines optimisation ensures a patient-focused approach to getting the best from and use of medicines, focusing on a holistic approach, an enhanced level of patient centred professionalism, and partnership between clinical professionals and the patient. In order for medicines optimisation to flourish, it must be patient-centered, based on the most up-to date available evidence, and work collaboratively across the whole ICS. This is the underpinning framework of our medicines strategy.
Our medicines strategy consists of four key objectives:
y Developing our workforce
y Optimising medicines at ward level
y Expanding the pharmacy workforce
y Ensuring seamless integration with the wider ICS
Within each objective, there are a number of workstreams aimed at ensuring medicines use at PAHT is patient-focused, evidence based, and safe from harm.
Developing the workforce
A well developed, informed workforce where learning from incidents are shared and where staff are empowered to escalate concerns and ideas for improvements, will result in a safer environment concerning all aspects of medicines management. This will include various e-learning and updates in medicines management, insulin safety, antimicrobial stewardship, opioids and patient group directions, as well as various competencies in medical gases and discharge procedures.
Optimising medicines at ward level
Ensuring patients get the best value from their medicine is a key objective for the 2024/25 year. Any quality improvement or financial savings need to factor in from not just a PAHT perspective, but ensure value across the whole ICS.
Key areas include:
y Use of biosimilar medicines in rheumatology, ophthalmology, neurology, dermatology and gastroenterology
y Ensuring best value medicines are used in anticoagulation, diabetes management and other chronic conditions
y Horizon scanning and moving to generics when available
y Utilising patients own drugs (PODs) to ensure regular medication is not dispensed unnecessarily
Expanding the pharmacy workforce
Utilising pharmacists and pharmacy technicians at the top of their licence is vital to ensuring patients get the best out of their medicines. Both play an active role in the safe reconciliation of medicines at admission, the monitoring and safety of therapies while in hospital, and facilitating discharge back to primary care. Various strategies are in development and include:
y Recruitment of specialist pharmacists in areas such as respiratory medicine, that can also support with discharge medicines
y Introduction of division technicians to support clinical governance
y Developing a framework for both prescribing and non-prescribing pharmacists to enhance care and correct errors at ward level
y Develop a pharmacy workforce plan, identifying areas of need, mapped to national best practice
Ensuring seamless integration with the ICS
Care and communication across the interface is one of the biggest risks to a
patient's treatment and working with GPs, commissioners, community pharmacy and other healthcare trusts is vital to ensure free flowing, responsive communication between all providers. At PAHT we aim to:
y Be an active, enthusiastic participant in key decision making within the ICS
y Share learning from incidents that encompasses more than one healthcare provider
y Improve referrals to community pharmacies for the new medicines service, postdischarge medicines use reviews, and managing chronic conditions
Developing the roles of our pharmacy team
Pharmacists, pharmacy technicians and pharmacy support workers play an integral role in optimisation of pharmaceutical care and delivery at PAHT, maintaining a safe, effective supply chain of medicines. Expanding on their current roles can play a vital role in optimising patient care, reducing wastage, and maintaining patient and medicines safety. Within the ICS, the boundaries between primary care, secondary care, community pharmacy and primary care network pharmacists and pharmacy technicians are slowly being withdrawn, giving rise to potential new roles and care pathways.
The Carter Review (2016) and the subsequent hospital pharmacy transformation programme encourages pharmacists to spend the majority of their time carrying out clinical functions in support of medicines optimisation and the clinical care of patients to reduce the amount of resource devoted to infrastructure services.
Pharmacist and pharmacy technicians in the Trust have seen their roles expanded considerably with the introduction of specialist roles (e.g. gastroenterology, dermatology, haematology, rheumatology and neurology) as well as the introduction of a specialist pharmacy technician in antimicrobial stewardship.
In order to ensure that medicines safety remained at the core of all patient services, the pharmacy workforce strategy was developed.
The pharmacy workforce strategy should meet the demands of the ICS medicines optimisation strategy, the Trust's medicines optimisation strategy, and the PAHT2030 strategy.
Overall, we must ensure the pharmacy workforce:
y Are suitably equipped and trained to perform their role
y Are supported by the right governance structure, policies and procedures and organisational leadership to provide the best everyday care for their patients
y Are inspired and equipped to get the best outcomes for patients
y Are a valued member of the wider MDT, contributing to healthcare agendas within their respective fields
y That staff are proud of their work, with job satisfaction, inspiring future leaders, clear career progression and succession planning embedded throughout our practice
y That we enhance, integrate and optimise use of the pharmacy workforce
y That we collaborate with key stakeholders in the ICS, working towards the development of more interface roles
y That we create a shared vision for the medicines strategy, ensuring everyone’s voice is heard
y That we promote and champion good practice through both national and local networks, highlighting some of the outstanding work being done
Antimicrobial stewardship (AMS)
The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics.
In 2019 WHO identified 32 antibiotics in clinical development that address the WHO list of priority pathogens, of which only six were classified as innovative. Furthermore, a lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are affecting countries of all levels of development and especially in healthcare systems. The UK Government has developed a 5-year National Action Plan (NAP), to contain and control these drug resistant bacteria by 2040. As part of this strategy, the use of antimicrobial drugs is heavily scrutinised.
According to the benchmarking results comparing hospitals it has identified that The Princess Alexandra Hospital are the worst performing hospital in our region and have one of the highest prescribing rates in comparison with patients’ length of days in hospital.
Figure 28: Our antibiotic use over 2023-24, compared with other local Trusts of a similar bed size

The numbers in figure 28 are the abbreviations for all acute hospitals within the East of England region.
To follow on from these results, the Trust has developed an antimicrobial action plan that has five key components:
Optimising antimicrobial use
y Reduce duration of antibiotic use: This is the mainstay of our stewardship programme and provides evidence-based advice on the effective and safe treatment of infections commonly presenting at PAHT. The guideline also promotes the use of narrow-spectrum and ‘access’ antibiotics in preference to broad-spectrum antibiotics where appropriate.
y Improve the number of patients switched from intravenous to oral antibiotics within 48 hours: An antimicrobial intravenous-to-oral switch (IVOS) decision aid was co-produced through a UK-wide consensus process involving 279 multidisciplinary participants. This tool has been uploaded onto the MicroGuide application to help clinicians when switching to oral antibiotics. IVOS is an important antimicrobial stewardship intervention. Research evidence confirms several IVOS benefits, including decreased risk of bloodstream and catheter-related infections, reduced equipment costs, carbon footprint and hospital length-of-stay, increased patient mobility and comfort, and released nursing time to care for patients. In addition, a daily consultant led anti-microbial stewardship (AMS) ward round takes place with a consultant microbiologist and lead antimicrobial pharmacist
y Reduce antibiotic wastage: Actioned in December 2022
Organisation development
y Establish AMS engagement across all divisions: The chief pharmacist has written to each divisional director asking for a medical representative to attend our newly formed AMS meeting group, and also that AMS to be added to the regular agenda items discussed at each divisional board meeting
y Establish oversight of the Trust teams' use of antibiotics led by the divisional directors: The chief pharmacist has written to each divisional director asking for a medical representative at the AMS and for AMS to be added to the agenda at divisional board level
y Create antimicrobial champions: Created and the names of the antimicrobial champions are available on AlexNet
Support prescribing
y Update our electronic system to ensure antibiotics chosen are in line with Trust and local standards: Regularly updated in line with the antibiotic guidelines
y Monitor use of antibiotic prescribing on our electronic drug prescription system: Interventions are made during AMS ward rounds and also by the ward pharmacists
Develop the AMS workforce
y Empower our multi-profession team members such as physician associates to be the beacons of antimicrobial excellence: Physician associates, antibiotic champions, nurses and ward pharmacists are working together with the consultants within the Trust to comply with the antibiotic guidance
y Create a consultant pharmacist role for antimicrobial stewardship.
Improve training and education
y Essential AMS training for all healthcare staff: The training package developed for clinical staff has been submitted for approval by the learning and organisational development team
y Incorporate AMS shared learning into the Grand Round: Teaching sessions have taken place at the Grand Round and Medical Advisory Committe (MAC). Teaching also takes place at ward level when the consultant microbiologist and lead antimicrobial pharmacist are undertaking AMS ward rounds
Electronic Prescribing and Medicines Administration (EPMA)
In the last year, the EPMA team expanded the use of the ChemoCare system to all areas that require drugs to be manufactured within our pharmacy technical services units.
We were able to introduce electronic prescribing and administration for biologics used in speciality areas such as gastro-enterology and rheumatology, oncology and haematology clinical trials.
We have been recognised as an exemplar site for sending discharge medicines referrals to the community pharmacies via the PharmOutcomes platform when patients are discharged. We refer approximately 1000 discharges per month.
We started working on the configuration of our new EPMA system, Oracle Health, which is a module of the Trust’s electronic health record (EHR), rather than a standalone EPMA system. The change to the new system will give us improved functionality to support antibiotic stewardship, allow prescribing of complex continuous infusions and remove the need for any remaining paper prescriptions in our inpatient areas. The go-live of the new system, Alex Health, is scheduled for October 2024.
Medication incidents
There are two metrics that are nationally reported to measure medicines safety and governance.
a) These are Medication Incidents Rate per 1,000 bed days
b) Percentage Medication Incidents Reported as Causing Harm or Death/All Medication Errors
A trust that is frequently reporting medication incidents, with a low percentage of incidents causing harm, is recognised as having a good organisational ethos with regards to patient safety.
These are also reported as part of hospital pharmacy’s benchmarking process, known as ‘model hospital’.
Figure 29: Number of reported medication incidents/per 1000 bed days



Key themes:
Medication on admission
There have been incidents, resulting in patient harm, where medication as part of a patient’s drug history are missed on admission to hospital resulting in unintentional omitted doses. This has included insulin, antihypertensives and antiepileptics. Staff are reminded of the importance of good reconciliation of medicines on admission.
Venous thromboembolism (VTE) prevention and the anticoagulation report The addition of a VTE report on Fleming Ward has highlighted potential incidents before they occur, this allows our staff to resolve the issue of patients not being given their anticoagulants because of finished courses of fondaparinux (a drug used to prevent VTE). This is now to be potentially expanded to other areas such as for Parkinson’s medication, where a patient receiving a modified release cobeneldopa instead of immediate-release levodopa, resulting ineffective treatment and exhibiting symptoms will be reduced.
Amiodarone
A patient developed phlebitis from an amiodarone infusion given peripherally. Staff are reminded on the need for central line for continuous infusions unless in exceptional circumstances.
A large number of prescribing errors, particularly teicoplanin and gentamicin, both antibiotics that have a narrow therapeutic window, meaning the effective dose at which they both act and produce a toxic effect resulting in renal impairment or ototoxicity (causes hearing and balance problems). Outside of endocarditis, gentamicin should be prescribed once daily, at 5mg/kg (max 400mg) for a maximum of 5 days unless under microbiology advice.
There have been a number of incidents around the prescribing of teicoplanin. Teicoplanin is a glycopeptide antibiotic which is used to treat serious staphylococcal and streptococcal infections. Due to its long half-life (the length of time it stays active in the bloodstream), teicoplanin requires the administration of loading doses to achieve satisfactory serum levels. Dosing is individualised based on weight and renal function to achieve target pre-dose (trough) level. There are three steps to the prescribing. A loading dose, a continuation to day 4, and a dose adjustment dependent on renal function.
The ability to aseptically prepare chemotherapy for our patients is vital for any organisation that treats cancer. In June 2023, we opened our new Aseptic Unit, a modern, fit for purpose facility which allows us to manufacture treatments to the highest standard. During September 2023, there was an audit carried out by the regional quality assurance inspector and the unit received the highest approval rating, which meant the inspection period was extended from 18 months to 2 years.

This is Us Week is our spectacular annual event with an exciting mix of sessions and activities to recognise, celebrate and develop our amazing PAHT people.
The 2023 programme included guest speakers at the Breafast with... sessions; opportunities to find out more about a range of topics at the Learn about... sessions; and wellbeing and information and discussions at the Wellbeing o'clock series of sessions.

Colleagues got involved with the fun at the Board games; joined the Schwartz Round to reflect on what great teamwork looks and feels like; and even droppedin to see demonstrations of the da Vinci robot which is used for robotic assisted surgery; and much more.
Thank you to everyone involved.




Some of the events during This is Us Week 2023
This is Us: Our Amazing People Awards and Long Service Awards
We celebrated our amazing people during This is Us Week with two special awards ceremonies.
Colleagues enjoyed the Long Service Awards on 26 June 2023 and the This is Us: Our Amazing People Awards on 27 June 2023; both of which were hosted at That Amazing Place in Harlow.
At the Long Service Awards, 30 people were presented with certificates and a pin badge to mark 20 years of service at PAHT; with a further 21 people presented with certificates and pin badges to mark 25 years of service at PAHT.
Recognised for 20 years of service
y Ben Rikhotso
y Claire Stroud
y Dawn Chapman
y Dawn Williams
y Eleanor Cuthbert
y Hannah LeMar
y James Campbell
y Jenny Harding
y Julie Hendy
y Karen Abraham
y Katie Randall
y Kim Stevens
y Kuo Man
y Lisa Reed-Langley
y Maureen McGowan
y Michelle Bradford
y Nitsa Menicou
y Paul Gonzales
y Rafael Silva Ros
y Randy Paguiligan
y Renee Hesketh
y Rowena Bravo
y Sally Trussler
y Samantha Hancock
y Samantha Morton
y Stuart Searle
y Susan Harrington
y Susan Marder
y Toni Sylvester
y Tracy Lynch
Recognised for 25 years of service
y Alison Gillman
y Andy Dixon
y Barbara Best
y Belinda Harvey
y Carolyn Barbet
y Edwina Lee
y Fiona Tredgett
y Julie Reeder
y Karl Beard
y Kim Murrell
y Lisa Flack
y Lorraine Nixon
y Michelle Penney
y Natasha Jacobs
y Sandra Duncan
y Sarah Cowley
y Sarah Needham
y Susan Malt
y Susan Whitmore
y Tracey Burgess
y Yvonne Haddow
For the This is Us: Our Amazing People Awards, 101 shortlisted nominees (from 490 nominations received) were recognised across 12 award categories that included:
y Kindness Award
y Safety Award
y Speaking Up Award
y Learning Award
y Commitment Award
y Improvement Award
y Teamwork Award
y Engagement Award
y Inclusion Award
y Managing for Excellence Award
y Emerging Leader Award
y Inspiring Leader Award
Highly commended: Gary Fordham, ward clerk
Winner: Ana Sofia Gomes, ward manager Adult Assessment Unit
Safety Award
Highly commended: Mylene Aran, healthcare worker
Winner: Caitlin Knight, midwife
Highly commended: Petya Ivanova, midwife.
Winner: Nichola Lane, theatre practitioner.
Learning Award
Highly commended: Kelsea Rickman, theatre practitioner.
Winner: Hershernpal Basra, consultant radiologist
Commitment Award
Highly commended: Beena George Winner: Edmon Masih, front of house staff in the Alexandra Restaurant
Improvement Award
Highly commended: Louise Lopez, senior biomedical scientist and pathology IT super-user
Winner: Dr Tamam Rifai, consultant in radiology
Teamwork Award
Highly commended: Frailty team (OPAL and REACT)
Winner: ICT design and development team
Highly commended: Kieran Burn, strategic people business partner Winner: Billie-Jo Croft, information governance officer
Inclusion Award
Highly commended: Karl Wolpert, dermatology consultant Winner: Shikha Sharma, practice development nurse (ED)
Managing for excellence award
Highly commended: Marie Parsons, consultant clinical scientist (biochemisty)
Winner: Jennifer Hibionada, ward manager on Harold Ward
Emerging leader award
Highly commended: Cherie Beckett, senior biomedical scientist Winner: Katherine Sebarillo, maternity nurse
Inspiring leader award
Highly commended: Sue Lord, lead practice development nurse in theatres Winner: Hanna Deman, lead EPMA and pharmacist IT development pharmacist
The events were also live streamed, with colleagues joining to celebrate online.
Congratulations to the nominees, highly commended and award winners - take a look overleaf.


Winners who collected their award on the night...






Highly commended who collected their award on the night...











Ann Nutt, chair of the PAHT Patient Panel, won an NHS Unsung Hero Award in the category of Individual Volunteer of the Year (pictured, right).
The awards aim to shine a spotlight on the extraordinary contributions of non-clinical and non-medical NHS colleagues and volunteers.
Ann (pictured, right) was also awarded the British Empire Medal (BEM) in His Majesty The King’s Birthday Honours announced on 15 June 2024 in recognition of her work with the NHS. The BEM is a prestigious award given for an outstanding achievement or service to the community that has had a long-term, significant impact.
The informatics team was shortlisted in the 2024 HSJ Digital Awards under the category ‘driving change through data and analytics’.
The HSJ Digital Awards celebrate excellence in digitising, connecting, and transforming health and care; and recognise innovative digital projects that are transforming care delivery, enhancing efficiency, and improving patient outcomes.



A surgeon at PAHT was awarded an honorary degree from Anglia Ruskin University in recognition of his outstanding contribution to healthcare.
Mr Ashraf Patel, associate specialist in breast surgery, received the award of Honorary Doctor of Health Sciences at the graduation ceremony at Chelmsford Cathedral on 22 November.

Committed nurse Kristle Bravo attended a royal reception hosted by His Majesty The King on 14 November.
The reception, that took place at Buckingham Palace, was an opportunity to celebrate the contribution of nurses and midwives working in the UK’s health and social care sector. Kristle, international nurse educator and manager at PAHT, was nominated to attend the reception by her senior nursing management team.
Nursery nurse Suela Porja received a Chief Midwifery Officer Award in November for her hard work and dedication in her previous role as a maternity support worker.
The Chief Midwifery Officer Awards have been developed to reward the significant and outstanding contribution made by midwives in England and has been extended to recognise the exceptional contributions of maternity support workers.
The emergency department team received the Gems of Harlow Award for their hard work and dedication.
The event, hosted by Harlow Council on Monday 6 November, celebrated the achievements of local organisations, services, charities and people who make a real difference in the community.
Our teams were shortlisted for six Academy of Fabulous Stuff Awards in recognition of their commitment to enhancing care and experiences for our patients and people.
The Academy of Fabulous Stuff, set up by Roy Lilley in 2015, is a social movement for sharing health and social care ideas, services and solutions.




The key performance indicators monitored by the people team are detailed in table 11 (below).
Table 11: People KPI

The annual NHS Staff Survey (NSS) is recognised as an important tool for ensuring that the views of people working in the NHS are used to help inform local improvements. The feedback is useful in helping highlight strengths, and improvements that will make PAHT a better place to both work and be treated.
Achievements of the Feedback to Action plan are reflected in the positive outcomes of the national NHS Staff Survey benchmark report for 2023.
y 1,953 employees completed the National Staff Survey 2023. This was a 50% response rate, noted as a record high for PAHT and a 5% increase on the comparable median rate, again higher than the previous year.
y 26% of respondents shared a freetext comment, which offered further insights about specific issues important to our people
y Significantly, we achieved an improvement on the previous NHS Staff Survey results across all People Promise elements, staff engagement and morale
Critical improvement measures for the trust are in figure 32:
y Would you recommend PAHT as a place to work? 50%, up from 44% last year
y Would you be happy with the standard of care if a friend or relative needed treatment at PAHT? The response was 47%, up from 42%
Figure 32: Critical improvement measures

The report findings from the 2023 NHS Staff Survey were presented to the People Committee and the senior management team in March 2024. The results were communicated to the wider organisation through an all user email from Lance McCarthy, chief executive, on the day of the national results release (7 March 2024). This was followed up with an InTouch briefing (webinar) on 12 April 2024. Divisional level results are also being communicated to colleagues by divisional senior management teams.
The NHS People Promise continues to be important as we strive to deliver care in line with our values and our quality and patient safety strategy. Representatives from every team in the organisation will be encouraged to join a divisional Feedback to Action group, to share their views on the results and inform improvement actions.
Building on the previous year, a Feedback to Action 2.0 programme has been developed for each division to fully review the findings and commence the development of Staff Survey improvement plans. The divisional engagement plans align to three priority improvement actions identified by the Trust (building on the momentum achieved in 2023).
y People Promise: We are always learning
y People Promise: We are safe and healthy
y This is Us management practices and leadership promise in our ways of working
The agreed Feedback to Action 2.0 programme:
y Ensures employee engagement is always on the agenda
y Aligns engagement improvement actions with divisional priorities and workplans that support PAHT2030
y Focuses on quality improvements over quantity
y Measures improvement actions with specific targets
y Builds accountability into established governance structures
y Empowers divisional leads to involve our people and recognise them in continuous improvement work
Our vision is to have a naturally inclusive organisation where everyone feels valued and is treated with respect.

To achieve this, our EDI strategy was approved in 2023 and features our aims to:
y Ensure the voice of our people, patients and the communities we serve are heard
y Promote equality of opportunity, dignity and respect for all our patients, service users, families, carers and our people
y Value and harness people’s differences

This will achieve our goals to:
y Put equality, diversity and inclusion at the heart of our organisation
y Recruit, retain, develop and support a diverse workforce
y Improve patient experience for people with protected characteristics and those who experience marginalisation
y Engage our diverse communities across our services and pathways.

To embed and transform the EDI strategy:
y An EDI delivery group was established with clinical triumvirates to ensure divisional plans incorporate EDI and, more specifically, have actions aligned to the goals and objectives outlined in the EDI strategy
y The EDI steering group meets bi-monthly to help shape the organisation’s strategies and policies to improve the experience of our people and patients with protected characteristics. The group consists of a diverse range of representation from teams and departments across PAHT and regularly reports progress to the People Committee, as a sub-committee of the board, to ensure visibility and scrutiny of all interventions
y Three staff networks, the Disability and Wellbeing Network (DAWN), the Race Equality and Cultural Heritage (REACH) Network and the LGBTQ+ Network, were formed in response to feedback from our people and a review of Staff Survey findings. These groups continue to meet to ensure the needs of all of our people and patients with protected characteristics are considered, and such needs are fed into the divisional plans
Programmes and initiatives which promote inclusion for our people
Disability Confidence scheme
We are ensuring we achieve the actions we put in the Disability Confidence scheme self-assessment/accreditation for level 2.
Rainbow Badge scheme
We continued to promote the pledges, including with information leaflets, and had interactive events on inclusion and intersectionality at This is Us Week in June 2023.
Unison Anti-Racism pledge
We are committed to ensuring that we meet the requirements set out in the pledge.
Colleagues were identified and trained to be disability champions.
Our recruitment team reviewed our training and supported training for Inclusion Champions who sit on all interview panels for Band 8a and above.
Training
EDI sessions were built into the corporate induction programme. Managing Inclusively became part of our Ready to Manage development programme. We also ran 60-minute virtual bitesize sessions around disability.
We supported employment opportunities for young adults with a learning disability and/or autism spectrum condition. In total, 11 interns commenced the programme in October 2023.
The Race, Equality and Cultural Heritage (REACH) Staff Network ran a cultural festival for our people in September 2023, a colourful Diwali celebratory event was held in November and in February we celebrated LGBT+ History Month.
The cultural festival is pictured below - the event was held on 16 September at Our Lady of Fatima Church Hall in Harlow.

The Trust’s monitoring of operational performance against national constitutional standards and local standards is monitored and reviewed at:
y Regular Divisional Review Meetings between members of the executive team and each division or department
y The Urgent Care Board
y The Access Board
y The Cancer Board
y Senior Management Team meetings
y The Performance and Finance Committee
y Trust Board meetings
An Integrated Performance Report is presented to the Performance and Finance Committee, Quality and Safety Committee and Trust Board meetings. Externally, the Trust is held to account for its operational performance by NHS England/ Improvement and its commissioners.
Delivery of all national standards has continued to be impacted by the increased elective waiting lists caused by the Covid-19 pandemic, industrial action and high numbers of emergency patients requiring care. The Trust has established infection prevention and control processes that minimise bed closures for Covid-19, influenza and norovirus.
The Trust has focused on improving the efficiency of services to ensure that as many patients receive appointments and treatment as possible with the facilities and staff available. Full elective operating was delivered for a second winter period with only a two-week closure of the orthopaedic ward to support the increased emergency admissions. Critical care capacity has been challenged during 23/24 with a number of elective critical care cases requiring rescheduling due to emergency pressures, and developments to increase capacity are being developed, figures 33-34.
Figure 33 Referral to Treatment access target – Incomplete standard


The 18-week Referral to treatment (RTT) standard was impacted by the long waiting times for treatment for patients, with 48% of our patients waiting over 18 weeks for routine treatment. The Trust continues to book patients in clinical priority order with urgent and cancer treatments continuing to be delivered in under 18 weeks.
The Trust has also reduced the number of long waiting patients over 78 weeks, however the aim was to have no patient waiting this long by July 2023, this was not achieved due to the impact of industrial action and the requirement to prioritise increased cancer and urgent patient treatments. This aim remains a focus for the Trust along with the requirement to have no patients waiting longer than 65 weeks by 30 September 2024.
Delivery of the national cancer standards has continued to be impacted by the number of patients waiting over 62 days for their treatment, however significant progress has been made in reducing the long waits. The Trust only slightly missed the target set by the national team for numbers of patients waiting longer than 62 days for treatment as the year-end was across the Easter holiday period and aims to exceed the March 2025 standard set for 24/25.
Figure 35 – 62 Day cancer backlogs

The Trust has achieved the national standard of 75% for the Faster Diagnosis Standard for more than 6 months and is one of the top performing Trusts in the East of England for this clinical safety standard that ensures patients with suspected cancer receive a diagnosis of cancer or no cancer within 28 days of referral, figure 36.
Figure 36 – 28 day Faster Diagnosis Standard

Diagnostic performance
Diagnostic performance has also been impacted by backlogs of routine patients waiting longer than 6 weeks for their diagnostic and significant increases in referrals such as MRI increases of 34% and 18% in ultrasound. The opening of additional capacity at the St Margaret’s site for the Community Diagnostic Centre and ongoing additional capacity from temporary diagnostic services has contributed to a steady improvement in the number of patients receiving their radiology diagnostic within 6 weeks, figure 37. Additional capacity in the audiology service has improved waiting times for patients and the endoscopy service is also delivering additional capacity in 23/24 and has significantly improved performance.
Figure 37 – Diagnostic times – Patients seen within 6 weeks

Urgent and emergency care performance
The proportion of patients treated within 4 hours in the emergency department has remained lower than the national target. Demand for urgent care services has remained high in 23/24 and flow through the hospital wards is challenged. This impacts the swift movement of patients to the most appropriate clinical ward and the off-loading of ambulances into the department. The Trust has implemented a number of improvements to ensure patients can transfer to wards such as a larger discharge lounge with longer opening hours, a “golden patient” initiative to expedite morning discharges and a reverse boarding policy. In addition, working closely with East of England Ambulance colleagues the Trust has made improvements in hours lost to handover, figures 38-39.
Figure 38 – Proportion of patients treated within 4 hours in the emergency department

39 – the number of hours lost to handover from ambulance to PAHT


The Trust is committed to undertaking effective clinical audit across all clinical services and recognises this is a key element for developing and maintaining high quality patient-centred services.
During 2023-24 the Trust participated in 90% of the eligible national clinical audits. Of the 5 national confidential enquiries, the Trust has participated in 4, (80%) of the studies which it is eligible to
participate in. The national clinical audits and national confidential enquiries that the Trust participated in and for which data collection was completed during the 2023/24 period are listed below alongside the current stage/reasons for not taking part to each audit or enquiry where known, Table 12 below.
Table 12 National audits the Trust considers participating in Provider organisation Participation Stage/submission details
Adult Respiratory Support Audit
BAUS Nephrostomy Audit
Breast and Cosmetic Implant
Registry
British Hernia Society Registry
Case Mix Programme (CMP)
British Thoracic Society Yes 15 cases (no minimum / maximum)
The British Association of Urological Surgeons (BAUS) Not applicable
British Hernia Society
Intensive Care National Audit & Research Centre (ICNARC)
Child Health Clinical Outcome Review ProgrammeJuvenile Idiopathic Arthritis National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
Child Health Clinical Outcome Review Programme –Testicular Torsion National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
Not applicable
Table 3 Programme / work stream (AZ)
Cleft Registry and Audit Network (CRANE) Database
Elective Surgery (National PROMs Programme)
Emergency Medicine Quality Improvement
a. Care of Older People
b. Mental Health (Self-Harm)
Epilepsy12: National Clinical Audit of Seizures and Epilepsies for Children and Young People
Falls and Fragility Fracture Audit Programme
a. Fracture Liaison Service Database (FLSDB)
b. National Audit of Inpatient Falls (NAIF)
c. National Hip Fracture Database (NHFD)
Improving Quality in Crohn's and Colitis (IQICC)
[Note: previously named Inflammatory Bowel Disease (IBD) Audit]
Provider organisation Participation Stage/ submission details
Royal College of Surgeons of England (RCS) Not applicable
NHS Digital Yes
Royal College of Emergency Medicine
a. Yes
Continuous data submission
a. Data submission period still open
b. Yes
Royal College of Paediatrics and Child Health
Royal College of Physicians a. Not applicable
b. Yes c. Yes
IBD Registry Yes
b. Data submission period still open
- 4 cases
Data submitted during 2023. Registry closed January 24.
Table 3 Programme / work stream (A-Z) Provider organisation
Learning from lives and deaths of people with a learning disability and autistic people (LeDeR)
Maternal, Newborn and Infant Clinical Outcome Review Programme
a) Perinatal mortality surveillance
b) Maternal morbidity confidential enquiry
c) Maternal mortality confidential enquiries
d) Maternal mortality surveillance
Medical and Surgical Clinical Outcome Review Programme
a) Endometriosis
b) Community acquired pneumonia
c) End of life care
Mental Health Clinical Outcome Review Programme
University of Oxford/ MBRRACEUK collaborative
a) Yes
b) Yes
c) Yes
d) Yes a) 100% b) 100% c) 100% d) 100%
National Confidential
Enquiry into Patient Outcome and Death (NCEPOD)
a) Yes
b) No
c) Yes a) 100% c) 100%
The University of Manchester / National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH)
Not applicable
Table 3 Programme / work stream (A-Z)
National Adult Diabetes Audit (NDA):
a) National Diabetes Footcare Audit (NDFA)
b) National Diabetes Inpatient Safety Audit (NDISA)
c) National Pregnancy in Diabetes Audit (NPID)
d) National Diabetes Core Audit
National Asthma and COPD Audit Programme (NACAP):
a) Chronic Obstructive Pulmonary Disease (COPD) Secondary Care
b) Pulmonary Rehabilitation
c) Adult Asthma Secondary Care
d) Children and Young People’s Asthma Secondary Care
National Audit of Cardiac Rehabilitation
National Audit of Cardiovascular Disease Prevention in Primary Care (CVD Prevent)
Provider organisation Participation Stage/submission details
NHS Digital
a) Yes
b) Yes
c) Yes
d) No
Royal College of Physicians
a) No
b) Not applicable
c) Yes
d) No
University of York Not applicable
a) Data submission period still open
b) Continuous data collection
c) 100%
d) Insufficient software
NHS Benchmarking Network Not applicable
c) 15 cases
Table 3 Programme / work stream (A-Z) Provider organisation
National Audit of Care at the End of Life (NACEL)
National Audit of Dementia (NAD)
National Audit of Pulmonary Hypertension
National Bariatric Surgery Registry
National Cancer Audit Collaborating Centre -
National Audit of Metastatic Breast Cancer
National Cancer Audit Collaborating Centre -
National Audit of Primary Breast Cancer
National Cardiac Arrest Audit (NCAA)
NHS Benchmarking Network Yes
Royal College of Psychiatrists Yes
NHS Digital Not applicable
British Obesity & Metabolic Surgery Society Not applicable
Royal College of Surgeons of England (RCS)
Royal College of Surgeons of England (RCS)
Yes
Data submission period still open
100% Round 5 - 102 cases (target 40)
Intensive Care National Audit & Research Centre (ICNARC)
Yes
Yes
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD)
Continuous data collection

Table 3 Programme / work stream (A-Z) Provider organisation Participation Number/ % submitted
National Cardiac Audit Programme (NCAP):
a) National Adult Cardiac Surgery Audit (NACSA)
b) National Congenital Heart Disease Audit (NCHDA)
c) National Heart Failure Audit (NHFA)
d) National Audit of Cardiac Rhythm Management (CRM)
e) Myocardial Ischaemia National Audit Project (MINAP)
f) National Audit of Percutaneous Coronary Intervention (NAPCI)
g) National Audit of Mitral Valve Leaflet Repairs (MVLR) [estimated start date April ‘23]
h) The UK Transcatheter Aortic Valve Implantation (TAVI) Registry
National Institute for Cardiovascular Outcomes Research (NICOR) hosted at NHS Arden and Greater East Midlands CSU
a) Not applicable
b) Not applicable
c) Yes
d) Yes
e) Yes
f) Not applicable
g) Not applicable
h) Not applicable
c) Continuous data collection
d) Continuous data collection
e) Continuous data collection

Table 3 Programme / work stream (A-Z)
National Child Mortality Database (NCMD)
National Clinical Audit of Psychosis (NCAP)
National Comparative Audit of Blood Transfusion:
a) 2023 Audit of Blood Transfusion against NICE Quality Standard 138
b) 2023 Bedside Transfusion Audit
National Early Inflammatory Arthritis Audit (NEIAA)
National Emergency Laparotomy Audit (NELA)
National GastroIntestinal Cancer Audit Programme (GICAP):
a) National Bowel Cancer Audit (NBOCA)
b) National Oesophago-Gastric Cancer Audit (NOGCA)
University of Bristol Yes
100%
Royal College of Psychiatrists Not applicable
NHS Blood and Transplant
a) Yes
b) Yes
British Society for Rheumatology No
Royal College of Anaesthetists Yes
Royal College of Surgeons of England (RCS)
a) Yes b) Yes
a) 10 cases
b) 100% - 21 cases
Capacity issues
Continuous data submission
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD)
Table 3 Programme / work stream (A-Z)
National Joint Registry
National Lung Cancer Audit (NLCA)
Provider organisation Participation Number/ % submitted
Healthcare Quality Improvement Partnership (HQIP)
Royal College of Surgeons of England (RCS)
Yes
Yes
National Maternity and Perinatal Audit (NMPA)
National Neonatal Audit Programme (NNAP)
National Obesity Audit (NOA)
National Ophthalmology Database (NOD) Audit
National Cataract Audit
National Paediatric Diabetes Audit (NPDA)
National Prostate Cancer Audit (NPCA)
Royal College of Obstetricians and Gynaecologists
Royal College of Paediatrics and Child Health
Yes
Yes
NHS Digital Not applicable
The Royal College of Ophthalmologists (RCOphth)
Royal College of Paediatrics and Child Health
Royal College of Surgeons of England (RCS)
No
National Vascular Registry (NVR)
Out-of-Hospital Cardiac Arrest Outcomes (OHCAO)
Paediatric Intensive Care Audit Network (PICANet)
Royal College of Surgeons of England (RCS)
Yes
Yes
Yes
University of Warwick Not applicable
University of Leeds /University of Leicester Not applicable
Continuous data submission
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD)
Continuous data collection
Automatic data submission
100%
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD)
Continuous data submission
Table 3 Programme / work stream (A-Z) Provider organisation
Perinatal Mortality Review Tool (PMRT)
Perioperative Quality Improvement Programme
Prescribing Observatory for Mental Health ( POMH)
a) Use of medicines with anticholinergic (antimuscarinic) properties in older people's mental health services
b) Monitoring of patients prescribed lithium
Sentinel Stroke National Audit Programme (SSNAP)
Serious Hazards of Transfusion
UK National Haemovigilance Scheme
Society for Acute Medicine Benchmarking Audit
The Trauma Audit & Research Network (TARN)
University of Oxford / MBRRACEUK collaborative
Royal College of Anaesthetists
Royal College of Psychiatrists
a) Not applicable
b) Not applicable
King's College London Not applicable
Hazards of Transfusion (SHOT)
for Acute Medicine
The Trauma Audit & Research Network (TARN)
UK Cystic Fibrosis Registry Cystic Fibrosis Trust Not applicable
UK Renal Registry Chronic Kidney Disease Audit
UK Renal Registry National Acute Kidney Injury Audit
UK Kidney Association Not applicable
Kidney Association

Figure 40 above shows that there were 7 commercial portfolio studies open throughout 2023-24. 4 are still open to recruitment, 3 are closed to recruitment but in follow up.
The Trust had 63 non-commercial studies open in total for 2023-24. 44 of these are still currently open to recruitment, 17 are closed to recruitment but in follow up and 2 were open during the year but have since closed.


Figure 41 and table 13 show the overall recruitment for 2023/24, our target was 1,000 accruals and we managed to exceed this, recruiting in total 1,236 participants into our studies.


Our new electronic health record (EHR) goes live on 12 –13 October 2024 and it’s called Alex Health. Alex Health is a major transformation project - one of the biggest PAHT has ever seen. It is a key part of the digital strategy and essential to the efficient delivery of care. Alex Health is also a critical step forward in our aim to be modern, integrated and outstanding before we move into our brand new hospital.
An electronic health record is a single digital record of a patient’s care, drawing together information from all systems that store a patient’s data. This includes a patient’s health history, treatments, medical conditions, and allergies. Hospital clinicians and patients will get fast and easy access to this data.
We are using the Cerner Millennium system (an IT solution from Oracle Health) to power Alex Health. Cerner Millennium has been successfully used by hospitals across the world, including many NHS Trusts in England.
During the last 12 months there has been a huge amount of work on the project, led by specialists and clinicians from across PAHT.

Summer 2023: Project launch
In July 2023 the project formally kicked off with engagement activities across the Trust to support our people to find out more about Alex Health and how it will benefit their work.


During August 2023, the team ran 100s of workshops with our PAHT people and Oracle Health professionals to share knowledge and build an accurate picture of how PAHT currently operates.
The workshops helped identify how operations might need to be changed or adapted to allow the Millennium system to work effectively. It was an important learning exercise to enable the Trust to make the most of Alex Health to deliver even safer, more effective and joined up care in the future.

Photo: The Alex Health team demonstrating Alex Health to clinicians.
Autumn 2023: Adapting Alex Health to be the best fit
In the autumn the team held a further 70 workshops with our people to look at different parts of a patient journey so that the team at Oracle Health could demonstrate how Alex Health will actually work for our people as users.
This was followed by weeks of localisation and data collection, which saw our people work with Oracle Health colleagues to shape and adapt the system to fit PAHT's policies, procedures and guidelines across the many workstreams that focus on patient care.
Winter 2023/4: Finalising the design and build
In January 2024, the team reached a major milestone with two weeks showcasing all the hard work that had been done to make Alex Health the best fit across all patient care workstreams.
This was a chance for the specialist teams - from prescribing to women’s health to emergency care (and more) - to come together to see the whole system for the first time.
The fortnight was a huge success and paved the way to start testing Alex Health and importantly, sharing what it looks like with our people across PAHT.


Photos: A demonstration in action (left) and the whole team at the end of the fortnight’s demonstrations (above).
Spring 2024: First look at Alex Health
Following the successful design and build phase, throughout spring the Alex Health team have been running a First Look campaign across PAHT to share demonstrations and presentations of Alex Health in action.


The Alex Health team engaging our clinical people.
Alongside a wide range of engagement with our people, there have been several months of testing to make sure the system is ready for our people to be trained in its use in August 2024.
The Alex Health team have also started to engage patient groups and GPs and clinical leaders in Hertfordshire and West Essex.
The wider community, including patients, will learn more about Alex Health and what it will mean for them in the summer when we roll out our external engagement campaign.
In the meantime, the key information patients need to know is included below.
Alex Health: benefits for patients
How does Alex Health improve care?
y Alex Health will help clinicians make better decisions about patient care, informed by a secure, single patient data record that provides a broad view of a patient’s medical history and health information
y The intelligent computer system follows best-practice ‘care pathways’ and takes the information clinicians put into it to suggest next steps in the care of a patient. This will help us to ensure patients always receive the right care and that decisions are applied with equity
y Computers can never replace the knowledge and good judgement of a clinician; however, they can support care, alert healthcare staff to what they should look out for and act as a guiding hand in their work. Alex Health will also alert staff if a dose of medicine has been missed or a patient is due for an observation or test. There are a number of other tools built into the system to support clinical decision-making
What information is on a patient’s Alex Health record?
y A patient’s Alex Health record will show their health history, medications, treatments and any other relevant information. This information can also be accessed by GPs and other health services providers
How will Alex Health improve the patient experience?
y With one patient record, there will be a reduced need for repeat testing as all clinicians will have access to any test results. Similarly, patients won’t have to repeat themselves to different clinicians each time they visit
y Clinicians will already be aware of any allergies and additional needs, as well as pre-existing conditions and treatment plans, which could reduce hospital attendances and admissions
y When the full patient portal is rolled out, patients will be able to access appointment booking, including rescheduling their appointments
How will patients access their Alex Health record?
y Patients will access their Alex Health record via a new patient portal accessible from computers, tablets and other hand-held devices.
y On 12-13 October (go-live) we will introduce patient portal ‘lite’. Via the NHS App, you will be able to access all your personal information and see your appointments and test results.
y A few months after go-live we will introduce the full version of the patient portal. At that point, you will also be able to schedule appointments, request medication and message clinicians.
Will there be support for digitally excluded patients, carers and families?
y We recognise that some people will not be able to use digital technology, and therefore might not be able to access their electronic health record via the patient portal. There will be support provided for those people, including working closely with Essex County Council, to enable patients and carers to access the portal via the NHS App through drop-ins at Harlow Library and on site at the hospital.
Is a patient’s personal data safe?
y Yes. Alex Health will process personal information fairly, lawfully and transparently under data protection legislation. Only those directly involved in a patient’s care will access a patient’s Alex Health record and a secure login will always be required when anyone needs to access it.
Further information on Alex Health and how it will benefit patients will be available on the PAHT website (www.pah.nhs.uk) by the summer of 2024.

To be a modern, integrated and outstanding hospital, our estate requires significant ongoing investment to enable us to provide the best services possible. During the last year, the Trust invested in the estate, transforming a number of key sites that have since brought significant improvements to our operations.
This is not just about investing in spaces and places, it is about investing in our people and our patients; listening to their needs, understanding what we can do better to provide and maintain the very best environment to deliver and receive care.
We have a responsibility to invest to improve the health of the planet too, and during the last year we have introduced a number of initiatives to reduce our environmental impact in line with wider NHS green targets.
In 2023-24, the PAHT estate was remodelled and maintained to improve the experience for everyone in the hospital by:
y improving the management of buildings and engineering systems
y providing excellent and sustainable facilities
y ensuring safety and security at all times
Capital highlights 2023/2024
y Phase 1 - orders in place for equipment that will provide clean electrical supplies, uninterrupted to key clinical sockets serving medical equipment to ensure the safety of our patients should a full mains failure on power occur and the Trust electrical generators do not kick in. This will provide mitigation plans and business continuity for our emergency department, High Dependency Unit and Neonatal Intensive Care Unit
y Water remedial works completed this year to remove redundant dead leg pipework (that allows organisms to grow), renewal of ageing heating
and hot water systems serving key hospital areas that provides improved monitoring and are in line with governing regulations
y Medical gas Area Valve Service Units (AVSU) renewal programme across the site to ensure clinical areas' alarm systems are linked to our main switchboard that will allow pressure monitoring for compliance with governing regulations
y Upgrade of the emergency department that included new coved sealed flooring, renewal of wall cladding to aid cleaning, full decoration throughout, door protection and frames and new medical gas installation for resilience and compliance


Pictured: The emergency department before the refurbishment (top) and after (below).
y Upgrades to the discharge lounge in the emergency department and the creation of a second space in the old therapy area that received new heating, a disabled toilet, kitchenette, flooring, decoration and new air conditioning
y Funding agreed for commencing work on fire stopping, fire door renewal and detection systems
y Main kitchen fridges and freezers upgrade, and completed upgrade of the main hospital restaurant
y Completion of a new in-house fit testing room for the infection prevention and control (IPC) team to complete staff tests from on the main site (pictured right)
y Creation of new mental health side room on Charnley Ward to ensure the clinical area is safer for this group of patients
Capital Projects sitewide:


y Supporting provision of offsite X-ray equipment upgrade projects at Herts and Essex Hospital
y The Trust has appointed a main contractor with the scheme in the final design stage reached to complete the new Community Diagnostic Centre at St Margaret’s Hospital, aiming for completion by autumn 2025
y Supporting pharmacy with the creation of an area to be used to place the temporary dispensing area pharmacy ahead of the new pharmacy dispensing robot that is due to be in place later this year
y Supporting IT with the installation of new 4G equipment in the telephone switch room
y Installation of new sitewide wayfinding signage to common areas of the Trust, both externally and internally
y Creation of additional parking bays, including disabled bay provisions at Gibberd Ward and the Williams Day Unit

In line with targets set by Greener NHS and targets in our green plan, we continued working towards achieving net zero by 2040 for emissions we control directly and by 2045 for emissions we can only influence i.e. supply chain emissions.
y The Trust was successful with its application for the NEEF – phase 2 LED lighting and Solar PV grant. The Trust was awarded £390,116 for an LED lighting upgrade across the hospital site. The project will procure, install and commission LED lighting across the site, with the expectation that the project yields benefits in reducing energy consumption, reduction in carbon footprint and cost savings. This work is continuing and due for completion during quarter 1 in 2024/5
y Following approval of funding for developing a heat decarbonisation plan for the Trust, the estates department have commissioned Low Carbon Europe (LCE) to produce the HDP. The trajectory to achieve net zero by 2040 and recommend decarbonisation actions are planned.
Electric vehicles delivery
We have taken delivery of the first three electric vehicles for the facilities team, the remaining three will be delivered in early March
These vehicles replace our old dieselpowered fleet and form part of our sustainability strategy to help reduce our carbon footprint and to comply with greener NHS guidance.
The vehicles will be used to transport pathology samples, medical record blue boxes, pathology supplies, CSSD instruments, pharmacy items; and will transport items between the main hospital site, St Margaret’s Hospital and
Herts and Essex Hospital. They will also be used to travel to local GP surgeries and to transport medical records between buildings and off-site to Cold Harbour Road.
The revenue generated from EV charging on site is £8,308.43 for the period of July – December 2023.
We are currently reviewing proposals to install more EV chargers on site to help reduce our travel related carbon footprint and to increase EV charging provisions for our people and patients.
Following a penalty imposed by our clinical waste supplier (Stericycle), the Trust has implementing the following action plan to resolve the waste segregation issues:
y Increase in face-to-face and one to one staff training for clinical and facilities colleagues
y Staff induction training for nursing staff
y Weekly awareness road shows
y Weekly contract management/update meetings with the contractor
y Contractors’ (Stericycle and Sharpsmart) support through educational materials, roadshow and re-set

Healthwatch Essex

Healthwatch Essex is an independent organisation that works to provide a voice for the people of Essex in helping to shape and improve local health and social care. We believe that health and social care organisations should use people’s lived experience to improve services. Understanding what it is like for the patient, the service user and the carer to access services should be at the heart of transforming the NHS and social care as it meets the challenges ahead of it.
We recognise that Quality Accounts are an important way for local NHS services to report on their performance by measuring patient safety, the effectiveness of treatments that patients receive and patient experience of care. They present a useful opportunity for Healthwatch to provide a critical, but constructive, perspective on the quality of services, and we will comment where we believe we have evidence – grounded in people’s voice and lived experience – that is relevant to the quality of services delivered by PAHT. In this case, we have received no additional feedback, and so offer only the following comments on the Quality Account.
y What is encouraging to see, is that there is a priority focus on reducing the number of complaints and patient advice and liaison service (PALS) concerns that detail communication as a theme by 10%. Understanding the importance of communication is vital when it comes to engagement with patients
y It is interesting to see the work highlighted on falls at PAHT. It is great to see there is a Falls Investigation Oversight group introduced to review all moderate and above harm falls. Also making falls awareness training at over 90% compliance each month mandatory is pleasing
y With over 1,900 respondents providing feedback and a response rate 5% above the average response rate for acute and community Trusts in the country this is pleasing that there have been improvements made in all seven of the NHS People Promises. There is also a clear passion to improve staff engagement and staff morale which the annual NHS Staff Survey will measure
y Complaints are always going to be made so it is important to see next steps and lessons learned at hospitals where possible. Of the 172 complaints raised against the Trust, the most frequently occurring themes related to medical care, communication issues and nursing care. It would be encouraging to see a focus on what learning came from these cases and what is put in place moving forward. This could include how patients can be used to share their lived experience to work together to improve services
y It would be pleasing to see the number of cases reduce in relation to complaints throughout each calendar year
y Listening to the voice and lived experience of patients, service users, carers, and the wider community, is a vital component of providing good quality care and by working hard to evidence that lived experience we hope we can continue to support the encouraging work of The Princess Alexandra Hospital.
Dan Potts Engagement Manager
17.05.2024
Healthwatch Hertfordshire
Healthwatch Hertfordshire values the relationship with The Princess Alexandra Hospital NHS Trust and the opportunities to discuss matters that impact on patient experience and quality of care.

The Trust has been particularly supportive in helping us to engage with internationally recruited staff to understand their experiences by sharing our survey and other opportunities for engagement. Retaining and supporting staff to provide high quality care is crucial to ensuring patient safety and a good patient experience and we look forward to sharing the outcomes from this research with them. We look forward to continuing to work closely with the Trust, patient experience team and Patient Panel including supporting the quality priorities outlined in this Quality Account.

Neil Tester
Chair Healthwatch Hertfordshire
May 2024


NHS Hertfordshire and West Essex Integrated Care Board (HWE ICB) response to the Quality Account of The Princess Alexandra Hospital NHS Trust 2023/2024
NHS Hertfordshire and West Essex Integrated Care Board (HWE ICB) welcomes the opportunity to share this feedback statement on The Princess Alexandra Hospital NHS Trust (PAHT) Quality Account for 2023/24. The ICB would like to thank the Trust for preparing this Quality Account, developing future quality priorities, and acknowledging the importance of quality at a time when they continue to deliver services during ongoing challenging periods. We recognise the dedication, commitment, and resilience of staff, and we would like to thank them for this.
HWE ICB is responsible for the commissioning of health services from PAHT. During the year the ICB has been working closely with PAHT in gaining assurance on the quality of care provided to ensure it is safe, effective, and delivers a positive patient experience. In line with the NHS (Quality Accounts) Regulations 2011 and the Amended Regulations 2017, the information contained within the Quality Account has been reviewed and checked against data sources, where this is available, and confirm this to be accurate and fairly interpreted to the best of our knowledge.
The Trust has identified nine priorities for 2024/25 that are fundamental elements of their ‘Five P strategy: our patients, our people, our performance, our places, and our pounds’. This includes continuing the work to reduce the mortality rate, reducing the number of moderate or severe harm from inpatient falls and the number of hospital-acquired pressure ulcers, and to improve staff well-being. The Trust has provided transparent information regarding the 2023/24 priorities that were not met and remain ongoing, as well as the next steps going forward for these priorities. Progress against all the priorities will be monitored through the Trust’s Quality and Safety Committee.
Regarding the delivery of the national cancer standards, these have continued to be impacted by the number of patients waiting over 62 days for treatment, however significant progress has been made in reducing the long waits. The Trust has achieved the national standard for the faster diagnosis standard for more than 6 months and is one of the top performing Trusts in the east of England for this clinical safety standard.
The Trust has provided a transparent account of the Care Quality Commission (CQC) inspections they have received in-year, and the outcomes, including the CQC improved grading for the urgent and emergency care department which has an improved rating of “Requires Improvement”. The elements of care which needed review and improvement are detailed in the Quality Account. The Trust continues to focus on their improvement plans and regularly report progress to the Trust’s Quality and Safety Committee, to the ICB and to the CQC.
The Trust has identified many departments and speciality teams within which improvements have been made in the last year, including the teams caring for patients with dementia, actions taken in relation to learning from complaints and the continued wide ranging and constructive work of the Patient Panel.
The 2023 NHS National Staff Survey results demonstrated the Trust achieved improvements across all People Promise elements, staff engagement and morale and the ICB recognises the ongoing work and commitment within the Trust in progressing the Staff Survey findings.
The Trust reported three “Never Events” in-year, of which, two investigations have been completed with significant learning and changes in practice to mitigate against a recurrence. The remaining Never Event remains under investigation at the time of writing this statement, and the ICB look forward to receiving updates on this in due course. Significant learning from patient safety incidents has been demonstrated, including in relation to implementing a pressure ulcer project, improvement work related to high-risk drugs, and the implementation of electronic consent at the Trust.
The ICB would like to recognise PAHT for their readiness and successful implementation of the Patient Safety Incident Response Framework (PSIRF), which sets out a shift in approach for how the NHS responds to patient safety incidents for the purpose of learning, improving patient safety and outcomes for our population. The ICB looks forward to working in partnership with PAHT and across the system as we collectively take forward PSIRF and the National Patient Safety Strategy.
During the year the ICB have been working closely with PAHT, gaining regular assurance on the quality and safety of provision to ensure a positive patient experience. Looking forward to 2024/25, the ICB supports PAHT priorities, and we look forward to a continued collaborative working relationship, building on existing successes and collectively taking forward needed improvements to deliver highquality services for this year and thereafter.

Toni Coles
Place Director, West Essex
Hertfordshire and West Essex ICB

Allied health practitioners - Healthcare professionals working in dietetics, occupational therapy, physiotherapy, operating department assistants, radiography and speech and language therapy. This is distinct from nursing, medicine, pharmacy and healthcare scientists.
Ambulatory care - Medical care provided on an outpatient basis, includes diagnosis, observation, consultation, and treatment.
Amiodarone – A medication used to treat certain types of serious irregular heart rhythms.
Antenatal – This is the care you receive from health professionals during your pregnancy.
Antimicrobial resistance - The ability of a bacteria to resist the effects of medication (antibiotics) that once could successfully treat the infection.
Antimicrobial stewardship - A coordinated intervention designed to improve and measure the appropriate use of antimicrobials by promoting the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and route of administration.
Audiology - The study of hearing and balance.
Bacteraemia – An infection of bacteria in the blood.
Cardiac arrest – Sudden loss of blood flow from failure of the heart to pump effectively.
Cardiology - The branch of medicine that deals with diseases and abnormalities of the heart.
Care Quality Commission (CQC) - CQC is an executive non-departmental public body of the Department of Health United Kingdom. Established in 2009, it is the independent regulator of all health and social care services in England. Chemical pathology – A branch of
pathology dealing with biochemical basis for disease.
Chemotherapy - The treatment of disease by the use of chemical substances, especially the treatment of cancer by cytotoxic and other drugs.
Chronic obstructive pulmonary disease (COPD) - The name for a collection of lung diseases including chronic bronchitis, emphysema and chronic obstructive airways disease.
Clinical audits - A process aimed to improve quality of patient care and outcomes through systematic review of care against explicit criteria and the implementation of change.
Clinical coding - The process by which patient diagnosis and treatment is translated into standard, recognised codes that reflect the activity that happens to patients.
Clostridium difficile (C.difficile)Clostridium difficile, also known as C. difficile, or C. diff, is a type of bacterial infection that can affect the digestive system.
Community-onset healthcare associated infection (COHA) – is when an infection is detected when a patient is at home but they have only arrived home within two days of admission to hospital, and the patient was an inpatient in the Trust in the previous four weeks.
Colorectal care - Treatments for patients with symptoms of the gastrointestinal tract including colorectal cancer and inflammatory bowel disease.
Colposcopy and hysteroscopy services - A procedure used to examine the cervix and inside of the womb (uterus).
CQUIN - Commissioning for Quality and Innovation is a system introduced in 2009 to make a proportion of healthcare providers’ income conditional on demonstrating improvements in quality and innovation in specified areas of care.
Datix - Software used in healthcare to collect patient safety incidents and for reporting adverse events.
Delirium - Is a state of mental confusion that can happen if you become unwell. It is also known as an acute confusion.
Dementia champions - A group of staff who have had specific training in dementia care. Their aim is to make other colleagues more understanding of why a patient may be more challenging and encourages them to tailor therapies accordingly.
Dermatology - The branch of medicine concerned with the diagnosis and treatment of skin disorders.
Diagnostics - Tools used to help identify disease and illness.
Dietetics – A branch of healthcare concerned with the diet and its effects on health, especially with the practical application of a scientific understanding of nutrition.
Endocrinology - The branch of physiology and medicine concerned with endocrine glands and hormones.
Endoscopy - A procedure that allows a view the inside of a person's body.
ENT clinics – An area where diagnosis and treatment are provided to conditions of the ear, nose and throat.
Eneterovirus – a common cause of infection in people of all ages.
Escherichia coli (E.coli) bacteraemia - Type of bacterial infection and a blood stream infection.
Frailty service – Reviews frail older people using a holistic assessment of physical, mental and social needs.
Friends and Family Test (FFT) - Test aimed at providing a simple headline metric which, when combined with follow-up questions, is a tool to ensure
transparency, celebrate success and galvanise improved patient experience. It asks “How likely are you to recommend our services to friends and family if they needed similar care or treatment?” with answers on a scale of extremely likely to extremely unlikely.
Gastroenterology - The branch of medicine which deals with disorders of the stomach and intestines.
Genito-urinary - The branch of medicine relating to the genital and urinary organs.
Governance - Establishment of policies, and continuous monitoring of their proper implementation, by the members of the governing body of an organisation.
Gram negative blood stream infections (GNBSIs) - Type of bacterial infection and a blood stream infection.
Gynaecology - The branch of physiology and medicine that deals with the functions and diseases specific to women and girls, especially those affecting the reproductive system.
Haematology - The branch of medicine involving the study and treatment of the blood.
Healthcare associated infections (HCAI) - Infections that are acquired as a result of healthcare. The burden of healthcare-associated infections has mainly been in hospitals where more serious infections are seen.
Health Overview and Scrutiny Committee – Local authority committees that scrutinise health issues and care in their area.
Healthwatch – Obtain the views of people about their health needs and experiences of having care and social services.
Hepato-pancreato-biliary (HPB)involved in the management of gallstone disease along with benign and malignant diseases of the liver, pancreas and gall bladder.
Hospital onset healthcare associated infection (HOHA) – this is an infection that is detected three or more days after admission to hospital therefore considered to be hospital acquired.
Hospital Standardised Mortality Ratio (HSMR) - Calculation used to monitor death rates in a Trust.
Integrated Care Partnership and System (ICP and ICS) – are alliances of NHS providers that work together to deliver care by agreeing to collaborate rather than compete.
Inflammatory bowel disease – The name for a group of conditions that cause the digestive system to become inflamed.
Intravenous – Giving fluids or drugs directly into a vein.
Klebsiella bacteremia - Type of bacterial infection and a blood stream infection.
Laparotomy - A surgical incision into the abdominal cavity, used for diagnosis or in preparation for major surgery.
Maternal and Fetal Assessment UnitOutpatient Antenatal Unit offering planned appointments for assessment of the mother and unborn baby in pregnancy.
Maxillofacial department – An area where diagnosis and treatment is provided to conditions of the mouth, face and adjacent structures.
Medical examiner – senior medical doctors who are contracted for a number of sessions a week to undertake medical examiner duties outside of their usual clinical duties. They are trained in the legal and clinical elements of death certification processes.
Medicines optimisation - Is the process of ensuring patients are on the most effective and fewest medications.
Methicillin-Resistant Staphylococcus Aureus (MRSA)/Methicillin-Sensitive Staphylococcus Aureus (MSSA) –
A specific bacterial infection.
Morbidity and mortality (M&M)Meetings established to review deaths as part of professional learning.
Myocardial ischaemia - When blood flow to your heart is reduced, preventing the heart muscle from receiving enough oxygen.
National Confidential Enquiries (NCEPOD) - National Confidential Enquiry into Patient Outcome and Death.
National Reporting and Learning System (NRLS) - A central database of patient safety incident reports.
Neonatal (NICU) - New-born children and new-born intensive care unit.
Nervecentre – electronic data base where observations are recorded.
Neurology - The branch of medicine or biology that deals with the anatomy, functions, and organic disorders of nerves and the nervous system.
NHS Digital – the national information and technology partners to the health and social care system.
NHSE/I - NHS England and Improvement is responsible for overseeing Trusts and NHS services, as well as independent providers that provide NHS-funded care.
NICE - The National Institute for Health and Care Excellence provides guidance, which supports healthcare professionals and others to make sure that the care they provide is of the best possible quality and offers the best value for money.
Norovirus - A type of viral infection that can affect the digestive system.
Nosocomial – a disease originating in a hospital.
Obstetrics - The branch of medicine that deals with the care of women during pregnancy, childbirth, and the
recuperative period following delivery.
Oesophago-gastric care – Treating patients with problems of the gullet (oesophagus) and stomach.
Oncology - The study and treatment of cancer and tumours.
Ophthalmology - The study of the structure, functions, and diseases of the eye.
Orthopaedic - The branch of medicine that deals with the prevention and correction of injuries or disorders of the skeletal system and associated muscles, joints, and ligaments.
Paediatrics - The specialty of medical science concerned with the physical, mental and social health of children from birth to young adulthood.
Palliative care - An approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.
Parechovirus – a common cause of mild infection in people.
Pathogen – microorganisms that cause disease.
Pathology - The scientific study of the nature of disease and its causes, processes, development and consequences.
Patient Advice and Liaison Service (PALS) - Offering confidential advice, support and information on health-related matters. Provides a point of contact for patients, their families and their carers.
Patient Panel - A group of volunteers who represent patients, families and carers of The Princess Alexandra Hospital NHS Trust.
Perioperative medicine - care of
patients from the time of contemplation of surgery through the operative period to full recovery.
Personal protective equipment (PPE) - will protect the user against health or safety risks at work, examples are FFP 2/3 face masks medical grade.
Polymerase chain reaction (PCR) testing - a method widely used to look for genetic code of the COVID-19 virus, this involves taking a swab of the throat and nose. The test will confirm if a person with symptoms has the virus currently.
Pressure ulcer – injury to the skin and underlying tissue primarily caused by prolonged pressure on the skin.
Pseudomonas – a specific bacterial infection.
Rapid Assessment and Treatment (RAT) - A treatment model used in emergency care to provide an early senior assessment and early treatment.
Radiology - The branch of medicine that deals with the use of radioactive substances used in the diagnosis and treatment of disease.
Referral to Treatment (RTT) – A constitutional standard that trusts are measured against in which a person’s waiting time starts on the day the hospital receives the referral letter from a GP to the time of first appointment or treatment.
Respiratory medicine – The branch of medicine that deals with the act of breathing.
Respiratory Syncytial Virus (RSV) – Respiratory syncytial virus is a contagious infection causing infection of the respiratory tract.
Rheumatology - The study and treatment of arthritis, autoimmune diseases, pain disorders affecting joints, and osteoporosis.
Rhinovirus – a common cause of infection in people of all ages.
SAFER care bundle – practical tool that
uses five elements of best practice.
Sepsis and septicaemia - Sepsis is a serious blood stream infection. A serious complication is septicaemia, which is when inflammation occurs throughout the body, which can be life-threatening.
Serious Incidents (SIs) - An unexpected or unplanned event that caused harm or had the potential to cause harm to a patient, member of staff, student, visitor or contractor.
SMART – mnemonic for objectives that are Specific, Measurable, Achievable, Realistic and Timely.
Stakeholders - A stakeholder is anyone with an interest in a business. Stakeholders are individuals, groups or organisations that are affected by the activity of the business. They include owners who are interested in how much profit the business makes.
Standard Operating Procedures – A set of step-by-step instructions compiled to help workers carry out complex routine work, aimed to achieve efficiency and uniformity of performance.
Standardised Mortality ratio (SMR) and Summary Hospital-level Mortality Indicator (SHMI) - Ratio between the actual number of patients who die following treatment at the trust and the number that would be expected to die, based on average England figures given the characteristics of the patients treated there.
Streptococcus – a type of bacteria causing infection.
Structured judgement review – allows trained reviewers to identify and describe the quality of care received and in so doing can create a score of that quality.
Trauma Audit and Research Network (TARN) – An audit where information is collected and analysed for patients who are moderately or severely injured after an injury. Data is submitted by trusts and a comparison can be undertaken.
UK Health Security Agency (UKHSA) –responsible for protecting every member of every community from the impact of infectious diseases.
Urology - The study of urinary organs in females and the urinary and sex organs in males.
Vascular surgery – Specialists that treat people with diseases of the circulation, which can be conditions affecting arteries, veins and where there are blockages to the flow of blood.
Venous thromboembolism (VTE) - A condition where a blood clot forms in a vein, most commonly in a leg where it is known as deep-vein thrombosis (DVT), a blood clot in the lungs is called a pulmonary embolism (PE).
VTE prophylaxis/ thromboprophylaxis - The giving of a medicine or treatment to prevent a VTE.

Prescribed
1. The number of different types of relevant health services provided or subcontracted by the provider during the reporting period, as determined in accordance with the categorisation of services:
(a) Specified under the contracts, agreements or arrangements under which those services are provided or
(b) In the case of an NHS body providing services other than under a contract, agreement or arrangements, adopted by the provider.
During 2023/24, The Princess Alexandra Hospital NHS Trust (PAHT) has provided a range of health services listed in the directory of services, table 1. Services are provided by the Trust to the Integrated Care Partnership (ICP) and are usually commissioned under standard form NHS contracts.
The payment mechanism applicable to most NHS contracts for patient care for the Trust post COVID-19 is an aligned payment and incentive contract (API). It is a blended payment, made up of a variable element which funds the majority of elective care and a fixed element which is a stable, pre-agreed value for activity outside of the scope of the variable element. These arrangements will remain in place for the whole of 24/25 until we receive further guidance from the national team.
Subcontracted activity: During the year 23/24, the Trust subcontracted a small number of services to private or other NHS providers. Services are generally subcontracted where there is a short-term capacity constraint and the response to COVID-19 has required additional resources. Examples of subcontracted services were for a Dermatology Minor Ops service by the provider called Remedy (now called Medinet Clinical Services).
The Trust is also the lead provider

1.1
1.2
The Trust has subcontracted arrangements in place from our local mental health provider (EPUT).
Prescribed information Form of statement
The number of relevant health services identified under entry one in relation to which the provider has reviewed all data available to it on the quality of care provided during the reporting period.
The percentage that the income generated by the relevant health services reviewed by the provider, as identified under entry 1.1, represents of the total income for the provider for the reporting period under all contracts, agreements and arrangements held by the provider for the provision of or subcontracting of, relevant health services.
We have reviewed all the data available on the quality of care provided by the services listed in table 1.
In 2023-24, £331.9m (97%) of the total income of £342.0m was received for patient care activities for services listed in table 2. Including this reimbursement, 89% of income related to patient care.
The most significant element of nonpatient income (£11.1m) related to provision of education and training.

2. The number of national clinical audits and national confidential enquiries which the Trust collected data during the reporting period and which covered the relevant health services that the provider provides or subcontracts.
2.1 The number, as a percentage, of national clinical audits and national confidential enquiries, identified under entry two, that the provider participated in during the reporting period.
During 2023-24 there were 50 national clinical audits relevant to the Trust that had data collected and 4 national confidential enquiries covering relevant health services.
2.2 A list of the national clinical audits and national confidential enquiries, identified under entry 2.1, that the provider participated in.
During 2023-24, the Trust participated in 50 audits out of 56 that we were eligible to participate in, which is 90% of national clinical audits.
The Trust participated in 4 of the 5 national confidential enquiries, which is 80% that were relevant to participate in.
The national clinical audits and national confidential enquiries that we have participated in during 202324 are detailed in Table 12.
2.3 A list of each national clinical audit and national confidential enquiry that the provider participated in, and which data collection was completed during the reporting period, alongside the number of cases submitted to each audit, as a percentage of the number required by the terms of the audit or enquiry.
2.4 A list of each national clinical audit and national confidential enquiry that the provider participated in, and which data collection was completed during the reporting period, alongside the number of cases submitted to each audit, as a percentage of the number required by the terms of the audit or enquiry.
The national clinical audits and national confidential enquiries that we have participated in, and for which data collection was completed during 2023-24, are listed alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Detailed in Table 12.
The national clinical audits and national confidential enquiries that we have participated in, and for which data collection was completed during 2023-24, are listed alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry, detailed in table 3.

2.5 The number of national clinical audit reports published during the reporting period that were reviewed by the provider during the reporting period.
2.6 A description of the action the provider intends to take to improve the quality of healthcare following the review of reports identified under entry 2.5.
The reports of 4 national clinical audits were reviewed by the provider in 2023-24.
2.7 The number of local clinical audit (a) reports that were reviewed by the provider during the reporting period.
2.8 A description of the action the provider intends to take to improve the quality of healthcare following the review of reports identified under entry 2.7.
y Falls training is mandatory for nursing staff
y Two sets of flat lifting equipment are available in the Trust
y Treatment escalation plans are in place
y An advanced care planning guideline is being developed
y A gold standards framework initiative is being introduced (initially to 3 of our wards), this includes completing a ceilings of care assessment and end of life planning
y Supported by an e-learning module
The reports of 19 local clinical audits were reviewed by the Trust in 2023-24.
y Education and IT solutions to reduce inappropriate drug omissions
y Education and standardised protocol to support appropriate use of oxygen therapy
y Teaching sessions on metastatic spinal cord compression pathway
y Education and training on carbapenemase producing enterobacterales (CPE) screening process
y New vascular surgery referral proforma available electronically
y Use of e-consent to support inclusion of chronic pain and other significant risks when consenting for inguinal hernia
y Increase ultrasound lists (for neck region) to reduce average waiting times
y Use of IT to support compliance with the guidance for the investigation and treatment of babies born to mothers with HIV, hepatitis or syphilis
y Provide OASIS care bundle (obstetric anal sphincter injury) to all clinicians in maternity
y Junior doctor teaching on VTE assessment and prescribing
3. The number of patients receiving relevant health services provided or subcontracted by the provider during the reporting period that were recruited during that period to participate in research approved by a research and ethics committee within the National Research Ethics Service.
4. Whether or not a proportion of the provider’s income during the reporting period was conditional on achieving quality improvement and innovation goals under the Commissioning for Quality and Innovation (CQUIN) payment framework agreed between the provider and any person or body they have entered into a contract, agreement or arrangement with for the provision of relevant health services.
The number of patients receiving relevant health services provided or subcontracted by PAHT in 202324 that were recruited into research studies during the period and approved by a research ethics committee was 975.
In 2023-24 the Commissioning for Quality and Innovation (CQUIN) payment was included within the fixed element of the contract.
4.1 If a proportion of the provider’s income during the reporting period was not conditional on achieving quality improvement and innovation goals through the CQUIN payment framework, the reason for this.
Not applicable for 2023/24.
4.2 If a proportion of the provider’s income during the reporting period was conditional on achieving quality improvement and innovation goals through the CQUIN payment framework, where further details of the agreed goals for the reporting period and the following 12-month period can be obtained.
Not applicable.
5. Whether or not the provider is required to register with the CQC under Section 10 of the Health and Social Care Act 2008.
5.1 If the provider is required to register with the CQC: whether at end of the reporting period the provider is:
(i) registered with the CQC, with no conditions attached to registration.
(ii) registered with the CQC with conditions attached to registration.
If the provider’s registration with the CQC is subject to conditions, what those conditions are, and whether the CQC has taken enforcement action against the provider during the reporting period.
6. Removed from the legislation by amendments made in 2011.
7. Whether or not the provider has taken part in any special reviews or investigations by the CQC under Section 48 of the Health and Social Care Act 2008 during the reporting period.
7.1 If the provider has participated in a special review or investigation by CQC:
(a) the subject matter of any review or investigation (b) the conclusions or requirements reported by the CQC following any review or investigation
PAHT is required to and is registered with the Care Quality Commission.
The Trust is not subject to any enforcement action during the reporting period.
PAHT has not participated in any special reviews or investigations by the CQC during the reporting period.
Not applicable.
(c) the action the provider intends to take to address the conclusions or requirements reported by the CQC and (d) any progress the provider has made in taking the action identified under paragraph (e) prior to the end of the reporting period.
8. Whether or not during the reporting period the provider submitted records to the secondary uses service for inclusion in the hospital episode statistics, which are included in the latest version of those statistics published prior to publication of the relevant document by the provider.
8.1 If the provider submitted records to the secondary uses service for inclusion in the hospital episode statistics which are included in the latest published data:
(a) the percentage of records relating to admitted patient care which include the patient’s:
(i) Valid NHS number
(ii) General Medical Practice Code
(b) The percentage of records relating to outpatient care which included the patient’s:
(i) Valid NHS number
(ii) General Medical Practice Code
(c) The percentage of records relating to accident and emergency care which included the patient’s.
PAHT submitted records during 2023-24 to the secondary user service for inclusion in the hospital episode statistics, which are included in the latest published data.
The percentage of records in the published data which include valid percentage:
(a) the percentage of records relating to admitted patient care which include the patient’s:
(i) valid NHS number - 99.8%
(ii) General Medical Practice Code – 100%
(b) the percentage of records relating to outpatient care which included the patient’s:
(i) valid NHS number - 100%
(ii) General Medical Practice Code - 99.9%
(c) the percentage of records relating to emergency care which included the patient’s:
(i) valid NHS number - 99.4%
(ii) General Medical Practice Code - 99.9%
9. The provider’s Information Governance Assessment Report overall score for the reporting period as per the Data Security Protection Toolkit (DSPT) grading criteria.
10. Whether or not the provider was subject to the payment by results clinical coding audit at any time during the reporting period by the audit commission.
10.1 If the provider was subject to the payment by results clinical coding audit by the audit commission at any time during the reporting period, the error rates, as percentages, for clinical diagnosis coding and clinical treatment coding reported by the Audit Commission in any audit published in relation to the provider for the reporting period prior to publication of the relevant document by the provider.
11. The action taken by the provider to improve data quality.
PAHT Information Governance: Assessment Report via the Data Security Protection Toolkit has an overall score for 2023-24 as Standard Met. PAHT received a substantial assurance with high confidence rating outcome for the associated internal audit.
PAHT was not subject to the payment by results clinical coding audit during 202324 by the audit commission. However, an internal clinical coding information governance audit was undertaken by an NHS Digital qualified clinical coding auditor.
Not applicable for 2023/24.
PAHT will be taking the following actions to improve data quality:
a) a full suite of data quality reports produced daily/weekly and circulated to operational teams for resolution of issues
b) data quality issues are monitored and addressed through the data quality group
c) data quality updates are provided to the Performance and Finance Committee, Information Governance steering group and System Access Board
d) respond in full to externally reported data quality issues from NHS England and our commissioners. The NHS England Data Quality Maturity Index score is 95.3% for December 2023; the national average is 81.2%
e) Conducts full user and refresher training to support the capture and recording of good quality data, operational processes are reviewed and aligned to system functionality. Furthermore, system user training guides are regularly reviewed and updated
f) Complies with the data quality standards within the data security and protection toolkit
12.
(a) The value and banding of the summary hospitallevel mortality indicator (‘SHMI’) for the trust for the reporting period; and
(b) The percentage of patient deaths with palliative care coded at either diagnosis or specialty level for the Trust for the reporting period.
a. SHMI banding is 99.73 for period January 2023 to December 2023, as published on May 2024. This result is consistent with previous months, and represents an improvement on our data from the same period last year.
A major national data integrity issue has been identified. NHS England and Digital are aware of the issue impacting data quality on Hospital Episode Statistics Information during Months 10 and 11 (January and February) that has an impact on the SHMI data. Recently NHS England have confirmed they have identified the source of the issue and a fix will be in place for the publication of the next release of information (expected in July of each year).
The Trust's HSMR for the period April 23 to October 23 is 83.4,- this is categorised as “lower-thanexpected” (see figure 4-7) and has seen also an improvement from our position last year.
b) Palliative care coding was 5.56% at either diagnosis or speciality level
Mental health Trusts
Ambulance Trusts
Ambulance Trusts
Ambulance Trusts
Mental health Trusts Not applicable to our Trust.
18. The Trust’s patient reported outcome measures scores (PROMs) for: (i) groin hernia surgery (ii) varicose vein surgery (iii) hip replacement surgery and (iv) knee replacement surgery during the reporting period.
Monitoring of PROMs for groin hernia and varicose vein surgery was paused in 2022, therefore no data is available.
EQ5D Index
Hip replacement: 91.30%
Knee replacement: 71.43%
EQ-VAS
Hip replacement: 83.33%
Knee replacement: 57.89%
National
EQ5D Index
Hip replacement: 94.50%
Knee replacement: 88.87%
EQ-VAS
Hip replacement: 79.10%
Knee replacement: 71.42%

19. The percentage of patients aged:
(i) 0 to 15 years
(ii) 16 years and over
That were readmitted to the Trust within 28 days of being discharged from our hospital, that forms part of the same organisation during the reporting period.
20. The Trust’s responsiveness to the personal needs of its patients during the reporting period.
21. The percentage of staff employed by, or under contract to, the Trust during the reporting period who would recommend the Trust as a provider of care to their family or friends.
22. Friends and Family Test – patient. The data made available by the National Health Service Trust or NHS Foundation Trust by NHS Digital for all acute providers of adult NHS funded care, covering services for inpatients and patients discharged from accident and emergency (types 1 and 2).
Please note: there is a not a statutory requirement to include this indicator in the Quality Account reporting, but provider organisations should consider doing so.
(i) Percentage of 0 to 15 years readmitted was 7.7%
(ii) 16 years and over readmission rate was 13.4%
The patient advice and liaison service are our first contact and point of care resolution service and in total responded to 4410 cases this year which was a 4% increase from the previous year (4248 in 2022-23).
The Staff Survey 2023 results found that 47% of staff would be happy with the standard of care provided by the organisation if a friend/relative needed treatment.
The patient Friends and Family Test continued throughout 2023/2024.
Our service users receive a link via text within 24 hours of being discharged or attending their appointment.
The Trust has seen an increase in responses received due to this new way of collecting data.
Total annual FFT for 2023/2024 showed that 76% of 12,272 patients rated services as good or very good.

23. The percentage of patients who were admitted to hospital and who were risk assessed for venous thromboembolism during the reporting period.
24. The rate per 100,000 bed days of cases of C.difficile infection reported within the Trust amongst patients aged two or over during the reporting period.
Data for the period 2022-23 was previously suspended due to Covid and has not been restarted at this time.
The plan is to re-instate monitoring from April 2024.
There were 49 hospital onset cases of Clostridium Difficile reported to the national surveillance database for period April 2023 to March 2024
Rate per 100,000 bed days is 28.88 (based on our own Trust data) as this information has not been published by UKHSA).
25. The number and, where available, rate of patient safety incidents reported within the Trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death.
April 2023 to March 2024: The total number of incidents was 13496 with 8546 for patients.
Validated harms:
Severe harm incidents: 20 (0.002%)
Death incidents: 1 (0.0001%)
26. Statement on seven-day hospital services.
The Trust is reviewing the workforce and service requirements across the 7-day week.
This will identify where service gaps exist, whether there is a service need to operate across 7 days and the resources required. This will feed into future business and service plans in line with the PAHT2030 strategy.

27.1 The number of its patients who have died during the reporting period, including a quarterly breakdown of the annual figure.
From 1 April 2023 to 31 March 2024, 1,237 of The Princess Alexandra Hospital NHS Trust patients died. This comprised the following number of deaths each quarter:
Quarter 1: 261
Quarter 2: 208
Quarter 3: 276
Quarter 4: 303
27.2 The number of deaths included in item 27.1 which the provider has subjected to a case record review or an investigation to determine what problems (if any) there were in the care provided to the patient, including a quarterly breakdown of the annual figure.
In relation to 1048 deaths (item 27.1):
y 203 case record reviews (SJRs) were completed
y 39 incidents were raised on Datix for patients that died:
y 28 are closed of which one was confirmed as a death harm
The number of deaths in each quarter for which a case record review, a serious investigation or a Patient Safety level II (PSII) was carried out are:
Quarter 1:
y 64 case record reviews
y 11 incidents were raised:
y 10 concluded no harm
y 1 concluded death harm – SI launched
Quarter 2:
y 36 case record reviews,
y 8 incidents were raised with harm confirmation of: 6 no and 1 moderate harm
y 1 remains under investigation
Quarter 3:
y 55 case record reviews
y 9 incidents were raised with harm confirmation of: 5 no harm, 1 minor and 1 moderate harm
y 2 remain under investigation
Quarter 4:
y 48 case record reviews
y 11 incidents were raised with harm confirmation of: 3 no harms
y 8 remain under investigation
27.3 An estimate of the number of deaths during the reporting period included in item 27.2 for which a case record review or investigation has been carried out which the provider judges as a result of the review or investigation were more likely than not to have been due to problems in the care provided to the patient (including a quarterly breakdown), with an explanation of the methods used to assess this.
Of the 2023/24 completed case studies and incident investigations into patients who had died, one was found to be a result of problems in the care provided to the patient. In relation to each quarter, this consisted of:
Quarter 1: 1 incident had a serious incident investigation and SJR
Quarter 2: None
Quarter 3: None
Quarter 4: None
Cases referred for a structured judgment review (also called case record review) have data captured on an electronic system called SMART. All of these cases are rated with an avoidability rating of:
Score 1: Definitely avoidable
Score 2: Strong evidence of avoidability
Score 3: Probably avoidable (more then 50:50)
Score 4: Possibly avoidable (less than 50:50)
Score 5: Slight evidence of avoidability
Score 6: No evidence of avoidability
All cases with an avoidability score of 1 or 2 are referred for:
y a review by the Trust’s learning from deaths panel
y are logged on Datix as a clinical incident and investigated through the Trust incident process
y Reviewed by the Trust’s Incident Management Group that determines what level of investigation is required
y Discussed and learning completed at the specialty mortality and morbidity meeting

27.4 A summary of what the provider has learnt from case record reviews and investigations conducted in relation to the deaths identified in item 27.3.
Learning identified from completed case record reviews:
y Improvements required with communication between speciality teams
y Improvements required with escalation to speciality teams
y Improvements required with clinical documentation
y Improvement required with accuracy in antimicrobial usage
y Improvements required with adherence to DNACPR and TEP document completion
y Complications identified with prolonged hospital stay and nosocomial infections
Learning identified from the confirmed death harm incident investigation:
y There should be clear, consistent recording and monitoring of insertion, removal and ongoing care of invasive devices
y Visual infusion phlebitis (VIP) score of peripheral lines is to be checked as per trust and evidence-based guidance
y VIP monitoring allows staff to ensure timely collection of blood cultures is completed when signs of infection are noted
y Timely administration of stat dose antibiotics in line with prescribing to be completed with clear documentation of rationale if this is not undertaken
y Appropriate prescribing of antibiotics or advice to be sought when infective markers are noted to be raised
y Antimicrobial wash to be prescribed and provided on admission
y Appropriate escalation of any changes and increases in NEWS score to enable appropriate actions to be taken

27.5 A description of the actions which the provider has taken in the reporting period, and proposes to take following the reporting period, in consequence of what the provider has learnt during the reporting period (see item 27.4).
The following actions from case reviews that continues to be embedded:
The process of Mortality and Morbidity (M&M) meetings have been reviewed, allowing junior clinical staff to attend and present cases to senior clinicians. An increased attendance at these meetings has been identified.
Sharing the learning from case reviews at wider forums where clinical staff of all levels are invited.
Nosocomial cases are investigated as a case review with the learning shared at M&M and with the Infection, Prevention and Control group, in order to triangulate learning.
Improved and enhanced service for referring patients to endoscopy teams out of working hours.
Re-launch of the deteriorating patient group to share and improve patient care across all specialities.
Anti-microbial guidelines reviewed and amended and shared at M&M meetings.
Improvement and enhanced service for the Non-Invasive Ventilation (NIV) service.
Sepsis mortality working group continues to support projects to further embed the Sepsis 6 bundle.
Monthly meetings are held to discuss the Trust's mortality indices, in order to gain a greater understanding of the Trust's

27.5 A description of the actions which the provider has taken in the reporting period, and proposes to take following the reporting period, in consequence of what the provider has learnt during the reporting period (see item 27.4).
mortality data and identify medical outlier groups, which are reviewed monthly, in order to identify care and treatment concerns or issues with coding.
The following actions from the serious incidents continues to be embedded
y Teaching and discussion on the sepsis six bundle has been commenced and is ongoing
The topics that are highlighted are:
y To act on a spike in temperature
y Collect blood cultures as soon as possible
y The Infection Prevention and Control (IPC) team have additional sessions in place for new staff to discuss invasive devices insertion and ongoing care
y There is a high impact audit in place looking at record keeping for inserted devices
y The PDT have updated the peripheral cannula and insertion training delivered
y IV champions launched and in place in each clinical area
27.6 An assessment of the impact of the actions described in item 27.5, which were taken by the provider during the reporting period.
The impact of the actions from review of cases are as follows:
y There is a greater understanding of inpatient deaths across all specialities due to dissemination of information across M & Ms and involvement from the multidisciplinary team
y Fewer incidents logged in delays of patients receiving endoscopies due to enhancement of the service
y Reduction of incidents logged due to inappropriate use of antibiotics due to the dissemination of the antimicrobial guidelines across numerous forums

27.7 The number of case record reviews or investigations finished in this reporting period which related to deaths during the previous reporting period but were not included in item 27.2 in the relevant document for that previous reporting period (2022/23).
27.8 An estimate of the number of deaths included in item 27.7 which the provider judges as a result of the review or investigation were more likely than not to have been due to problems in the care provided to the patient, with an explanation of the methods used to assess this.
27.9 A revised estimate of the number of deaths during this reporting period stated in item 27.3, and for that previous reporting period, taking account of the deaths referred to in item 27.8.
Two incident investigations were closed during this reporting period relating to deaths:
y Fall incident: death harm confirmed
y Child death incident: death harm confirmed
Two SIs investigation reports have concluded that the deaths were more likely than not due to issues in the care provided.
y One case detailed in 27.3
y Two deaths in 27.8
y Total: 3

28 In response to the Gosport Independent Panel Report, provide details of ways in which staff can speak up (including how feedback is given to those who speak up) and how we ensure staff who speak up do not suffer detriment. This disclosure should explain the different ways in which staff can speak up if they have concerns over quality of care, patient safety or bullying and harassment.
There are a number of ways in which our people can speak up. One of these may be via the Freedom To Speak Up service (F2SU). This may be to raise concerns about behaviours, patient or staff safety, either as an individual or as a witness or to give suggestions for improvements.
There is a lead guardian who is clinical with a further two clinical guardians and two non-clinical guardians. We have now trained a total of 27 Freedom to Speak Up Ambassadors. Their role is to support staff to speak up, raise the profile of the service and be accessible to a wider range of staff. They come from a wide range of ethnic backgrounds and a variety of roles within the Trust.
We have a Freedom to Speak up vision and strategy and the vision states: “We are striving to ensure that our people feel enabled to speak up in order to support and improve patient safety and quality, the health and wellbeing of our people, and staff experiences."
The focus of Speak Up Month this year was removing barriers to people speaking up. A number of initiatives have continued or taken place in year to raise the profile of speaking up and to remove barriers.

28 In response to the Gosport Independent Panel Report, provide details of ways in which staff can speak up (including how feedback is given to those who speak up) and how we ensure staff who speak up do not suffer detriment. This disclosure should explain the different ways in which staff can speak up if they have concerns over quality of care, patient safety or bullying and harassment.
These include:
y Junior doctor drop in sessions.
y FTSU newsletters
y Increasing the number of ambassadors
y Presentations for all new staff
y Video on AlexNet featuring an example of speaking up
y Attending wards/departments
y Posters with contact details
y Listening events
y Support at health and wellbeing events
The Guardians submit a quarterly report to the National Guardians' Office detailing the numbers of referrals and themes. A more detailed report is presented to the People Committee and the Trust board bi-annually. This shares numbers and themes of concerns raised to them but also the actions taken or required to happen to improve staff and patient experience and safety. The number of referrals continues to increase which is a good indication that more staff are feeling supported and safe to speak up.
The Trust endeavours to triangulate all speaking up avenues and the lead guardian collaborates with a range of key individuals across the Trust to promote this.

28 In response to the Gosport Independent Panel Report, provide details of ways in which staff can speak up (including how feedback is given to those who speak up) and how we ensure staff who speak up do not suffer detriment. This disclosure should explain the different ways in which staff can speak up if they have concerns over quality of care, patient safety or bullying and harassment.
Staff can also contact a range of people directly within the organisation who can signpost them to advice and support. These include:
y The people team
y Staff side
y Equality, diversity and inclusion lead
y Line managers
y Tutors
y Organisational development team
y Staff health and wellbeing
y Mental health first aiders
y Professional nurse/midwife advocates
y Guardian for Safer Working
y Freedom to Speak Up ambassadors
Anyone who speaks up is always thanked for doing so. They are assured of confidentiality and encouraged to report immediately if they suffer any detriment from speaking up. This is taken very seriously and will be formally investigated. They are kept informed of progress of any actions taken to improve or resolve issues and asked to feedback on their experience.
An internal audit was undertaken to review the Freedom to Speak up service within the Trust in February 2024 and the findings were that the design of the service was green (substantial evidence) and design effectiveness was amber (moderate evidence). We will focus to ensure the evidence on the services effectiveness is also substantial.
Staff surveys and regular pulse surveys are undertaken to monitor the impact of any changes made to improve experience and actions are monitored locally and centrally for themes and improvements.

29 Following the terms and conditions of service for NHS Doctors and dentists in training (England) 2016 requires a consolidated annual report on rota gaps and the plans to reduce rota gaps.
The Trust did not complete an annual report in 2023/24.

The Princess Alexandra Hospital NHS Trust, Hamstel Road, Harlow, Essex, CM20 1QX 01279 44 44 55




The Princess Alexandra Hospital NHS Trust