PAGE 11 PAGE 17 PAGE 29 EnsuringCompetitioninthe HealthcareIndustry:The ProblemwithPharma's AnticompetitivePractices GraceMatwijec HealthCareandthe InflationReductionAct: Let'sBreakItDown AnnaShell TanzaniaMission:DrHärtl's NeurosurgicalAdvancements inEastAfrica JaskeeratGujral
HEAD OF DESIGN
WRITERS
Shahana Banerjee
Om Gandhi
Michael Go
Jaskeerat Gujral
Hiba Jamil
Arjan Kahlon
Nancy Lam
Grace Matwijec
Adanna Mogbo
Parthiv Patel
Angelo Petto
Austin Pothikamjorn
Anna Shell
Neil Tangal
EDITORS
Eesha Balar
Shahana Banerjee
Ashrit Challa
Siddharth Chitta
Tingting Chung
Jaskeerat Gujral
Shikhar Gupta
Srijan Kalva
Erin Lee
Amarichi Mbadugha
Adanna Mogbo
Arav Nangia
Aarsha Shah
Saraswati Sridhar
Jessica Wu
DESIGNERS
Oscar Capraro
Julia
Gerbino
Nancy Lam
Jenny Li Cherry Lin
Zachary Rentala
Dear Readers,
I cannot express my excitement enough to share this semester's journey with you. The Penn Healthcare Review Fall 2022 cohort is impressively unique and has made history as our largest, most diverse, and most talented group of students yet.
As Penn resumes normal day to day life, we look back and reflect on how much has happened in healthcare since the onset of the COVID 19 pandemic. Within a few years, we went from lockdowns to the passing of the Inflation Reduction Act and the overturning of Roe v. Wade. As such, it is only natural for us to present to you our most thoroughly explored journal theme yet.
Our articles explore topics ranging from sociocultural disparities during COVID 19 to antitrust legislation We have organized our articles this semester into subthemes for your ease of viewing: 1 Social Determinants of Health 2. Legislation & Government in Healthcare 3. Healthcare Industry and Delivery 4. International Healthcare.
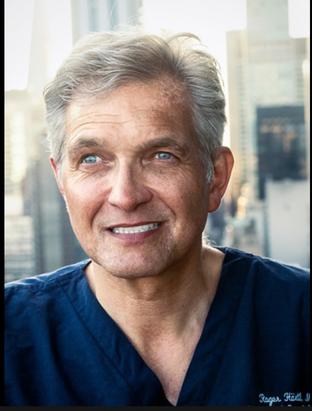
In addition, we are so excited to continue our guest feature program this semester. Starting last semester with the CEO of Butterfly Network, we are striving to feature an industry professional directly tied to at least one of our articles in each publication. This semester, we are thrilled to feature Dr Roger Härtl, a board certified neurological surgeon at Weill Cornell Medical College and the head of the Tanzania Neurosurgery Project (for more details on the project, visit page 29).
This is an exciting start to the 2022 2023 school year, and at PHR, we are proud to welcome you behind the frontlines to explore the politics, policy, and reform in healthcare domestically and abroad.

Enjoy, Kyne Wang
Editor in Chief
Please note: There articles were prepared by members of the Wharton Undergraduate Healthcare Club. The opinions do not represent the school or club's official positions on the issues. The Wharton Undergraduate Healthcare Club is an independent, student-led organization of the Wharton School of the University of Pennsylvania. All content is the responsibility of the club.
EDITOR-IN-CHIEF
Kyne Wang
VICE PRESIDENT
Om Gandhi
Julia Gerbino
SOCIAL DETERMINANTS
Medical Racism and Its Byproduct: Medical Mistrust
Written by Austin Pothikamjorn, Edited by Adanna Mogbo, Designed by Jenny Li
COVID 19: An Imbalanced Battle for the Disadvantaged
Written by Parthiv Patel, Edited by Srijan Kalva, Designed by Cherry Lin
LEGISLATION AND GOVE
The True Toll of Dobbs v. Jackson: The Overturning of Roe v. Wade
Written by Adanna Mogbo, Edited by Jessica Wu, Designed by Julia Gerbino
Health Care and the Inflation Reduction Act: Let's Break it Down
Written by Anna Shell, Edited by Saraswati Sridhar, Designed by Oscar Capraro
Removing Barriers to APRN Practice through the ICAN Act:

Written by Michael Go, Edited by Tingting Chung, Designed by Oscar Capraro
Where's My Food? A Retrospective Analysis of the Healthy, Hunger Free Kids Act of 2010
Written by Neil Tangal, Edited by Amarachi Mbadugha, Designed by Julia Gerbino
HEALTHCARE INDUSTRY
Ensuring Competition in the Healthcare Industry: The Problem with Pharma's Anticompetitive Practices
Written by Grace Matwijec, Edited by Eesha Balar, Designed by Zachary Rentala
Where's the Benefit? Addressing Exorbitant Prescription Drug Costs in the US
Written by Arjan Kahlon, Edited by Arav Nangia, Designed by Cherry Lin
$15 vs $1500: For-Profit, not For-Patient
Written by Nancy Lam, Edited by Ashrit Challa, Designed by Julia Gerbino
Changing the Dated Reimbursement Model for Bedside Nurses
Written by Angelo Petto, Edited by Jaskeerat Gujral, Designed by Nancy Lam
INTERNATIONAL HEALTHC
Scotland's Period Product Act: A Legislative Model to Address the Unequal Price of Periods.
Written by Hiba Jamil, Edited by Shahana Banerjee, Designed by Julia Gerbino
The Damaging Impact of Trade Embargos on Cuban Healthcare
Written by Om Gandhi, Edited by Aarsha Shah, Designed by Nancy Lam
Tanzania Mission: Dr Härtl's Neurosurgical Advancements in East Africa
Written by Jaskeerat Gujral, Edited by Shikhar Gupta, Designed by Zachary Rentala Russia and the Fossil Fuel Non Proliferation Treaty
Written by Shahana Banerjee, Edited by Siddharth Chitta, Designed by Jenny Li
5
7 9
11 13 15
17 19 21 23 25 27 29 31
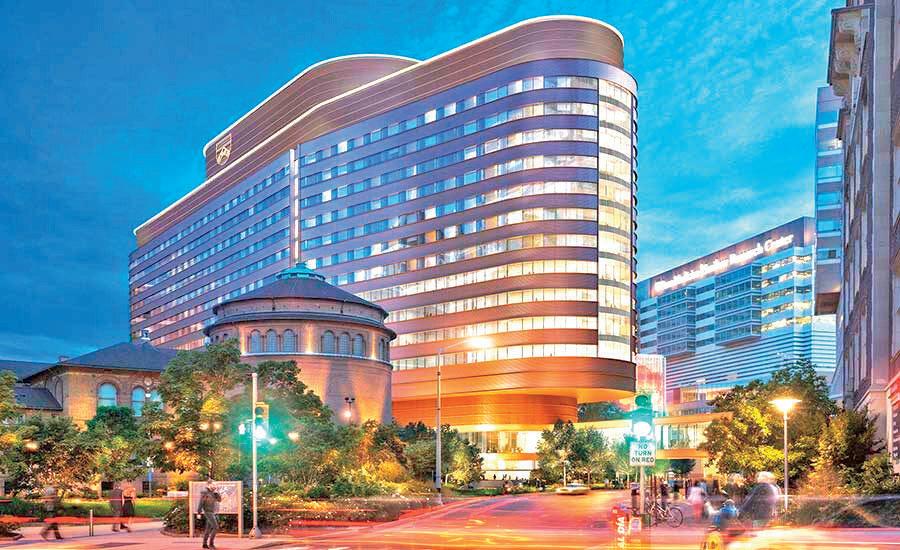
Dr. Roger Härtl
RogerHärtl,M.D.,istheHansen MacDonaldProfessorofNeurologicalSurgeryandDirectorof

Obviously me being a neurosurgeon, I was interested in neurosurgical diseases. My particular interest when I started was head injuries head trauma because that had been my research in medical school and afterwards, andIwasveryinvolvedwithguidelinesforheadinjury.In the early 2000s, there was a strong movement towards guidelines for medicine, and then also in neurosurgery more and more guidelines were published on how to treat certain diseases. For head trauma, what made a lot of uproar and caught a lot of attention were the guidelinesforthemanagementoftraumaticbraininjury. Those were the first guidelines that were made in neurosurgeryever,andtheywereaboutheadinjury.
When I traveled to Tanzania, one of the things that really were most remarkable was the incidence of traumatic brain injury, neurotrauma, spine trauma, and also head injuries. Naturally, since I was involved with the guidelines in North America, I saw this as a special opportunity to translate some of those guidelines and some of the recommendations to come to the particular challenges in Tanzania. When we started the Tanzania project,headinjurywasthefirstpathologythatwereally focused on We did that by starting to collect data on patient’s head injury in Tanzania trying to understand howmanypatientstheysee,howtheyarebeingtreated, whattheoutcomewas,andwhatarethechallenges.
How did the Tanzania mission come about and how was it supported?

The mission came about really based on the previous visit that I had as a medical student in Tanzania When I was in medical school, I spent 2 months there. I actually went to Malawi, which is a country that is adjacent to Tanzania. I was in the hospital there and I was during the later part of my medical school, and I enjoyed it a lot, and I also wanted to go back and then residency and then as a young neurosurgeon I couldn’t really figure out exactly how to make that happen. I was taking care of the president of Tanzania; he was my patient. He came to New York for treatment, and then he invited me back to Tanzania, so that's how I went back to Tanzania.
When I went to visit the president, I went to the local hospital and no it was struck by struck by the severity of the situation in terms of neurosurgical diseases, such as hydrocephalus, spinal trauma, head injuries, brain tumors, abnormalities, birth deficiencies, and children of spina bifida, and so forth. There were a vast number of patients who clearly had neurosurgical problems and they only had three neurosurgeons for the whole country so it was immediately an opportunity to kind of get involved in and then go every year. We started organizing meetings there who started having fellows go back and forth between New York and Tanzania so Tanzanians would come over here for observations and then people from New York and Eruope would go over there. The funding was based on patient donations and my own personal funding for my own traveling. I paid myself and then everything else was paid for by patient contributions.
lacking that made it seem that the country needed neurosurgicaladvancements?
SpinalSurgeryattheWeillCornellMedicineBrainandSpineCenterinNewYork,aswellasthe co directorofNewYork PresbyterianOchSpine HeisalsothefounderanddirectoroftheWeill CornellMedicineCenterforComprehensiveSpineCareaswellasWeillCornellMedicine's GlobalNeurosurgeryInitiativeinTanzania(forwhichhewasnamedAANSHumanitarianofthe Yearfor2022).HereceivedhisM.D.fromtheLudwig MaximilliansUniversityinMunich, Germany.HecompletedhisneurosurgeryresidencyatNewYork Presbyterian/WeillCornell MedicalCenterandMemorialSloan KetteringCancerCenter,afterwhichhepursued specializedtrainingincomplexspinesurgeryattheBarrow'sNeurologicalInstituteinPhoenix underDr VolkerSonntag In2004Dr Härtlreturnedtore jointheDepartmentofNeurosurgery atWeillCornellMedicalCollege
ThisinterviewdivesintoDr.Hartl'sTanzaniainitiative.
From a neurosurgical perspective the many things that come to mind. One thing would be the lack of intensive care units You know a lot about what we do in neurosurgery really relies on adequate perioperative care and that’s usually ICU care and rehabilitation after surgery, which are all really lacking in Tanzania The capital, or the big city of Dar es Salam there are some places that utilize those facilities, but if you look at the whole country, and the whole picture, it is extremely rare to have an ICU. If you do have an ICU, then it is understaffed and under equipped and it does not function very well The other thing we do in neurosurgery we really rely on a lot of infrastructure For example, we need a functional CT scan, functional MRI, you need scans for instrumentation for spine and screw placement and so forth Frequently, they don’t have that, and if they do, then patients have to pay for it. It’s not like here where you have insurance. Here, for example, if you come to the emergency room and no questions are asked. Everybody’s going to be taken care of You don’t have to prove that you were able to pay you Over there, however, you may come in with a head bleed, and you are not going to get a CT scan unless a family member comes in and pays for it, which is crazy There's a totally different attitude towards what constitutes an emergency and what's urgent and what's not.
What are you hoping to accomplish in the coming years with the Tanzania mission?
I think we are trying to establish a solid program where we have a lot of interaction by a lot of fellows going back and forth, and we already do that to a certain extent We have to coordinate efforts in Tanzania with some of the research efforts here on the ground We would like to have somebody in the department who is dedicated to the collaboration with Tanzania like an administrative person who works with Tanzanians on the variety of projects that we collaborate on.
I would like to give our residents and fellows more regular opportunities to go over there to have experiences there and to spend time in a place like Tanzania. At the end of the day, it’s all about capacity building, so we’re going to help train and educate surgeons, nurses, healthcare workers. That’s really the goal to really expand neurosurgical care in Tanzania
Read more about Dr. Härtl's Tanzania Initiative on Page 29
Thank you to our Gold Sponsor:
What do you think the health system in Tanzania could improve upon?
MMedical mistrust is not a novel issue, and with controversies regarding COVID 19 vaccinations, medical mistrust within the African American community has become more prevalent.AsofNovember2021,only
38.6% of Black Americans in the United States report having received at least one dose of the COVID 19 vaccine, whereas 45% of White Americans have done the same [1] Though this difference may have resulted from a different number of disparities (ie access to vaccination sites, vaccine misinformation, and lack of community investment), most stem from one mechanism:medicalracism[2] Medicalracismis the discrimination against people of color in medicine,whetheritbeinpracticeoraccessibility
Due to early, paternalistic forms of racism, medicalracismpropagatedthroughoutAmerican healthcare. The black community was targeted by egregious medical experiments, namely the Tuskegee Syphilis study, and generally received lowqualitycare.Thus,BlackAmericanshavegone on to distrust contemporary medicine, leading to worsehealthoutcomes.Tore establishthisbond, the patient provider relationship must be reevaluated.
MEDICAL RACISM AND ITS BYPRODUCT Medical Mistrust
WrittenbyAustinPothikamjorn
DesignedbyJennyLi
EditedbyAdannaMogbo
Medical racism can be traced all the way back to the birth of medicine During this time, discrimination against race was rampant, and inevitably felt in the realm of healthcare. The general notion that dark complexioned people were “inherently inferior and less intelligent” was spearheaded by medical forerunners such as Plato and Aristotle, lacing this racial bias throughout medical literature and research. Medical education would only further promote this proposed inferiority like those in Roman and Arabic training. As a result, anti black prejudices emerged in not only medical progression, but also medical practice. Healthcare for slaves in the pre Civil War era was the most deficient out of any group in the United States: discrimination from public hospitals, rundown medical facilities, and even medical abuse By the time Johns Hopkins opened its medical institution, racism and inequality had been implanted in every aspect of American healthcare, and would greatlyaffectBlackAmericansgoingforward[3]
TheracialprejudiceagainstAfricanAmericans in medicine can be seen throughout history and today A key instance of medical racism was the 1932 Tuskegee Syphilis study, where white researchersselected600blackmenfromMacon County,Alabamatotakepartinanexperimentto observetheeffectsofuntreatedsyphilis.
5
FIG.1IllustrationbyDianaEjaita
The exploitative study subjected the men to risky procedures and tests over 40 years, and even when penicillin, an effective cure to the ailment, was discovered, the experiment continued Eventually when the experiment’s true intentions were exposed, 128 of the men had already passed away due to the disease or its complications [4]. More generally, racism affects the healthcare provided to Black Americans. Overall, Black Americans tend to receive lower quality care than White Americans [5]. For example, in a 2007 study, black women were more likely to receive substandardchemotherapytreatmentsthanwhite women [6]. Another study reveals that black children receive fewer antibiotic prescriptions than non blackchildren,evenunderthesamephysician [7]. These disparities in treatment have naturally led Black Americans to distrust physicians and medicine. They are then less likely to get annual checkups and follow medical advice; as a result, Black Americans are more likely to report being in poor health [8] This hesitation for healthcare can beseentoday,asBlackAmericanshavethelowest COVID 19 inoculation rate out of any group in America [9] This apparent health inequity is a signal that American medical infrastructure needs to be rebuilt: it must be more inclusive of all demographics, and it begins right in the doctor’s office.

While reestablishing broader trust between African Americans and the national health system may take years of reform, rebuilding interpersonal trustbetweenpatientsanddoctorsisanadequate starting point. A key aspect of the patient-provider relationship is, of course, communication. A 2011 report claimed that on average Black Americans were less likely to have an informative healthcare experiencecomparedtoWhiteAmericans[10] This
Primary care physicians are commonly where patients go to voice their medical concerns, so ensuring the space is safe and comfortable is imperative for establishing a trusting relationship. However,implicitracialbiasescancauseproviders to talk more than usual over the patient, and a disproportionate amount may cause patients to feel overwhelmed [11]. This limits opportunities for patients to express their true issues, potentially resulting in missed diagnoses or incorrect prescriptions. To prevent this, providers should focus on allowing more time for their patients to participate,andtrainingneedstobeimprovedand standardized to reduce the bias physician patient talktimeratio Tobuildfurtheronthismethod,ashifttoamore patient centered approach should be considered It establishes a common ground between patient and provider, eliminating the intimidating power disparity Patients with medical illiteracy won’t feel scrutinized when communicating with their providers, allowing more of their participation To abide by this model, doctors should be clear with eir patients by speaking in simple language, king open ended and engaging questions, and oviding directional plans about treatment. This eofpatient-centeredcommunicationresultsin her patient satisfaction, better outcomes, and erall,anincreasedtrustinmedicine[12].
In conclusion, the national healthcare system ould look to improve the patient provider ationship as inadequate interactions can cause tient dissatisfaction and lead to worse health tcomes, especially for Black Americans. They en will be led to distrust modern medicine and edical advice, widening their health disparity in eUnitedStates
FIG 2AnursepreparesasyringeofaCOVID 19vaccine 6
Edited by Srijan Kalva
COVID-19:
AnImbalancedBattlefortheDisadvantaged


The COVID 19 pandemic significantly upended the personal and social aspects of individuals’ day to day lives It also shed light on the generational health disparities present among vulnerable communities that the US healthcare system discriminates against These populations have a disproportionate allocation of readily available resources for those suffering from the interwoven comorbidities or other external health conditions that face an amplified burden from the pandemic[1]. Their limited knowledge on the services offered within the healthcare system and current governmental infrastructure related to socio political policies empowered COVID 19 to target vulnerable communities The aftermath of the pandemic has consequently encouraged the amelioration of these disparities and the equitable allocation of healthcare resources throughout society.
The U.S. has made efforts to amend their past prejudicial wrongdoings, but the pandemic demonstrated that healthcare equalities amongst all racial communities were not a priority According to the Center for Disease Control and Prevention, the excess mortality rate engendered by crisis conditions for example, disease pandemics skyrocketed for both African American and Hispanic populations at 32.9% and 53.6% respectively. Contrastingly, the excess mortality for White persons was 11.9% the large discrepancy elucidates the racial and ethnic health inequalities[2] Furthermore, African American and Hispanic minorities comprise 31 9% of the U S demographic as opposed to the prodigious 60% of the population that
represent non Hispanic White Americans; the increasing excess mortality rate within these communities is alarming considering the small portion of the total population they represent[3]
While the bulk of these inequalities can be attributed to the discriminatory nature of the healthcare system, the systemic burdens rooted within these racial and ethnic minorities could further elucidate their healthcare disparities The socioeconomic background of vulnerable individuals predominantly underlies such burdens inherent to minorities struggling with their integration into American society The systematic inequality against those who are less economically facilitated resulted in a growing racial wealth gap and significantly impacted healthcare coverage. Given
the lower socioeconomic status present throughout African American and Latinx communities, the cost barriers present in acquiring health insurance deter these individuals from pursuing healthcare securities, consequently leading to greater out of pocket costs for immediate treatments and disincentivizing engagement in the healthcare system Even after the ratification of the Affordable Care Act implemented employer sponsored insurance plans for dsfdd

by Parthiv Patel Designed by Cherry Lin
Written
The U.S. has made efforts to amend their past prejudicial wrongdoings, but the pandemic demonstrated that healthcare equalities amongst all racial communities were not a priority.
7
minorities that struggled to afford private insurance the average rate of uninsured beneficiaries from African American and Hispanic backgrounds steadily increased throughout the pandemic[4].

The reason for this incline was associated with the growing unemployment rates within these minorities from temporary and permanent layoffs during the pandemic, jumping as high as 9 2% for African American communities alone such job and income losses consequently led to withdrawn employer contingent health coverage plans[5]. According to the Bureau of Labor Statistics, compared to the 29.9% of White individuals that are approved for teleworking, only 19 7% of African Americans and 16 2% of Latinx populations are allowed to work from home[6] Such drastic discrepancies present greater risks of exposure to COVID 19 for essential workers who are unable to socially distance or potentially reject regulatory masking mandates As such, the presence of systematic inequities related to socioeconomic and employment burdens create large disparities amongst racial minorities and their White counterparts, prohibiting these disadvantaged societies from experiencing the total services of the healthcare system Considerations towards the health and physical geography of various communities is also crucial in determining why COVID 19 had a stronger burden on certain populations across the country In the presence of various comorbidities cardiovascular disease, for example, the deleterious effects of COVID 19 are magnified within the host. Comorbidities are present a variety of racial and ethnic groups, such as Nati and Indigenous People, but also throughout populations that suffer from bein immunocompromised and therefore more vuln a pandemic setting[7] Furthermore, the location of households possesses a strong lin burdens; the discrepancy between urbanized death rates and rural community death rate respectively 132.8 deaths per 100,000 populat deaths per 100,000 population, reveals the si population distribution on health inequalities[8
While the COVID 19 pandemic seems superfic an ubiquitous effect on the U S demographic, analysis reveals an alternative narrative char discriminatory effects on disadvantaged popula
Urban areas must account for factors, such as employment and income deprivation, crime, and environmental well being, which collectively contribute to poorer health outcomes across a society For example, according to the Harvard T H Chan School of Public Health, regions with higher levels of air pollution are linked to increased hospitalizations and deaths due to COVID 19[9]. Contrastingly, while rural areas certainly contain less dense populations, they suffer from a higher prevalence of the aforementioned aging populations and limited access to healthcare providers and resources With respect to mitigatory solutions, the implementation of a support scheme similar to that of the U K ’s Coronavirus Job Retention Scheme where a large majority of salary losses are compensated by the government can mitigate the stress placed on those with lower socioeconomic status, hi h i k f l t d hi h i k f l i

8
Fig 1 Protest against the Discriminatory nature of the Healthcare System
THETRUETOLL
OF DOBBS V.
JACKSON: THE OVERTURNING OF ROE V. WADE
Written by Adanna Mogbo Edited by Jessica Wu Desjgned by Julia Gerbino
RoeV.WadeOverturned
The overturning of Roe v. Wade this summer shocked the nation On June 24, in the case of Dobbs v Jackson Women’s Health Organization, SupremeCourtjusticesruled6 to 3thatabortion is not a federally protected right under the Constitution and that the states can determine thelegalityofabortion[1]
FollowingtheDobbsv.Jacksondecision,13states now have full bans on abortion in place, with another five states having gestational limits for abortion Although the majority of these states don’t have exceptions for cases of rape and incest, all states currently have exceptions for life threatening medical emergencies [2]. However,thevaguewordingoftheseexceptions lead to a multitude of complications that can stall treatment. Women can experience grave injuries or die with even a short delay in accessing abortion care while their exceptions are processed or while doctors decide if their condition is life threatening enough to treat. Despite what many pro life activists claim, saying that only women who seek to end their pregnancies will be affected, the overturning of Roev Wadecanstillendangerwomenwhowant to keep their pregnancies but experience dire medicalemergenciesduringtheirpregnancy.
DangersPrevailInSpiteof ExceptionsforMedicalEmergencies
ECTOPICPREGNANCIES
Ectopicpregnanciesareamedicalconditionthat canturndeadlywithoutspeedyabortioncare. An ectopic pregnancy occurs when a fertilized egg implants anywhere outside of the uterus, suchasinthefallopiantubes(themostcommon implantation spot in ectopic pregnancies), the ovaries, or even the abdominal cavity [3] As a result,ectopicpregnanciesarenotviableandcan lead to ruptures or life threatening internal bleeding if not treated quickly In the US, roughly one in 50 pregnancies are ectopic, and factorslikeage,geneticpredisposition,andprior healthcomplicationscanincreasethelikelihood ofanectopicpregnancy[4].
In light of these new abortion bans, many abortion care providers now fear the risk of investigation, losing their medical license, or imprisonmentforperforminganabortiononan ectopic pregnancy at an early stage where the conditionisnotyetlife threatening Thisresults in doctors deciding to, dangerously but legally, sendwomenseekingcarebackhomeuntiltheir conditionworsens,riskingthemother’slifeand increasingthepossibilityofapreventabledeath. ObstetricianDr.AlirezaA.ShamshirsaztoldThe NewYorkTimesthatthismethodofcareislike “bring[ing]lotsofpeopletothetopofahighrise and push[ing] them to the edge and then catch[ing] them before they fall” [5] It will inevitablyleadtomanywomenlosingtheirlives duetointentionaldelaysincare.
OPINION BY ADANNA MOGBO
9
INCOMPLETEMISCARRIAGES
Spontaneous, incomplete miscarriages are another condition out of a pregnant woman’s controlandcanturndeadlywithoutspeedycare Miscarriagesarewhenafetusdiesinthewomb, oftenbeforethefetusreaches20weeks:10 20% of pregnancies end in miscarriage [6]. Miscarriagesusuallyleadtotheexpulsionofthe fetusonceitdies;butsometimes,fetusesdonot expelcompletely.Again,speedyabortioncareis neededtofullyremovethefetusorelseawoman can risk going into septic shock and dying However, similar to the ectopic pregnancy dilemma,abortioncareprovidersarehesitantto performabortions.Theyoftensendwomenhome in the hopes that the fetus eventually expels naturally or that her condition worsens, giving them more standing to perform abortions that arepermittedbytheexceptions.Inmanycases, abortion providers waste precious time by havingtoconsulthospitalethicscommitteesor lawyers[7]
The 2012 death of Savita Halappanavar, an Indian Irish dentist, demonstrates what could happen in America as these policies take place. Halappanavar sought abortion care repeatedly over the course of three days in Ireland, a Catholiccountrywithstrictabortionregulations. However,doctorsdeniedhercare althoughshe wasmiscarrying,her17 week oldfetusstillhada detectable heartbeat [8]. Similar to the policies that US doctors have now in certain states, doctors can make risky decisions by having to interpret the bounds of legislation during a medical emergency [9] Halappanavar spent “several days in agony” until the fetus’s official heartbeatstopped Thefetuswasthenremoved, butHalappanavar’shealthcouldnotrecover.She died shortly after [8]. With total abortion bans taking place, many tragedies similar to Halappanavar’s have and will continue to take placeinourcountry
1.
after a
Roe.
Consequences of Delays in
Abortion Care
The overturning of Roe v Wade and the enactment of near total abortion bans across the country threaten the lives of all women Even pregnant women who do not choose to undergoanabortionandhopetohavechildren are still vulnerable to these abortion bans due to the possibility of pregnancy complications like ectopic pregnancy or incomplete miscarriages. It is vital to vote for political representatives that protect abortion rights bothatthenationalandstate level.Anyformof delayinabortioncareaccesscanspelldoomfor patients suffering from medical emergencies, anddespitepro lifeactivistsclaimingthatthey are “saving lives” by outlawing abortion, the true toll of banning abortion continues to rise everyday.

10
FIG
Pro-choice protesters stand outside of the Supreme Court in May 2022,
draft opinion was leaked stating that a court majority approved overturning
AJune 2022 Gallup poll reported that 26% of Americans have delayed or cut back on health care services and prescription drugs. 17% of Americans reported driving less, 10% reduced utility usage, and 7% skipped meals to pay for essential health services [1]. In response to this


growing crisis, in August of 2022, Congress passed the Inflation Reduction Act The 1,000 page bill written by Senator Manchin (D WV) and Senate Majority Leader Chuck Schumer (D NY) included significant health care provisions aimed at combating ballooning costs [2].
The IRA’s health provisions can be grouped by overall targets: 1) lowering prices through drug negotiation, 2) prescription drug inflation rebates, 3) Medicare Part D improvements and out of pocket caps, 4) Affordable Care Act (ACA) subsidies, and 5) miscellaneous (including delays of rebate rules, extension of vaccine coverage, payments for biosimilar products, cost sharing improvements, and subsidy eligibility) [3]. This article will focus on elements within each of the five categories that will likely have the greatest impact on health care costs.
IRA section 11001 allows Medicare to negotiate with pharmaceutical companies for lower prescription drug prices [4] In 2003, Congress included a non interference clause within Medicare Part D that forbade the federal government from interfering in negotiations between manufacturers and sponsors or setting any form of price structure for drug reimbursement Currently, hundreds of individual plans recognized by Medicare Part D have to negotiate with pharmaceuticals individually [5] The IRA eliminates this clause and creates the Drug Price Negotiation Program, enabling price negotiation for certain single source drugs and establishing price ceilings for certain drug categories [6] Handing the bargaining power over to the Medicare program as a whole demonstrates the government’s prioritization of beneficiaries, rather than drug manufacturers
IRA sections 11101 and 11102 mandate prescription drug inflation rebates Manufacturers of drugs covered by Medicare Part B and D whose prices increase faster than inflation will have to offer rebates or else face a fine to the tune of 125% of the government determined rebate amount In essence, beneficiaries will see their drug costs rise at a pace consistent with that of other goods and services, but no faster [7].
IRA sections 11201 and 11202 redesign Medicare Part D cost sharing (how much beneficiaries pay out of pocket). Over the past two decades, out of pocket costs have doubled, increasing from $193.5 billion in 2000 to $388.6 billion in 2020 [8[. Beginning in 2025, out of pocket expenditures on Medicare Part D prescription drugs will be capped at $2000, and beneficiaries whose prescriptions meet this price ceiling in a single fill can pay in installments throughout the year [9].
Written by: Anna Shell by: Anna Shell
11
Edited by: Saraswati Sridhar by: Saraswati Sridhar by: Designed by: Oscar Capraro Designed by: Oscar Capraro Oscar Capraro
IRA section 11404 expands Medicare Part D low income subsidy eligibility [10]. Currently, under the Extra Help program, Medicare Part D beneficiaries making 135% or below the Federal Poverty Line (FPL) are eligible for “full help” subsidies These government payments cover 100% of premiums and deductibles and cap cost sharing at $4 15 per generic drug and $10 35 per brand name drug (2023 pricing) However, those with incomes between 135% 150% of the FPL are currently only eligible for “partial help” subsidies and can end up paying hundreds, if not thousands, on prescription drugs even with Part D coverage [11] The IRA raises the eligibility threshold for full help subsidies to 150% of the FPL beginning in 2024, easing the burden of cost sharing for thousands of low income Medicare Part D beneficiaries
Currently, 3 3 million Medicare beneficiaries suffer from diabetes and require insulin IRA section 11406 caps the cost of insulin products at $35 per month from 2023 2025, and $35 per month, 25% of the established maximum fair price, or 25% of a new negotiated price for 2026 and beyond [12] Thanks to these provisions, beneficiaries will finally see a significant reduction in their out of pocket spending on the life saving drug

The final provision to be discussed, second to drug price negotiation, drew some of the most attention Section 12001 of the IRA extends ACA premium tax credits through 2025 [13] The Biden administration’s 2021 American Rescue Plan expanded eligibility for subsidies by providing premium tax credits for anyone whose ACA marketplace plan premium exceeded 8 5% of their income These subsidies helped ACA marketplace plan enrollment reach an all time high in 2022, with the rate of uninsured Americans at a record low of 8% [14].
The IRA’s health provisions will significantly impact Pennsylvanian Medicare beneficiaries throughout the coming decade. Of the 2.2 million Pennsylvanians enrolled in Medicare Part D, approximately 73,000 currently incur out of pocket costs exceeding the new $2000 cap. 154,000 beneficiaries in PA used insulin products in 2020 and will now pay no more than $35 per month. Approximately 346,000 Pennsylvanians will benefit from the continuation of ACA subsidies. The
Department of Health and Human Services estimates that 76,000 additional Pennsylvanians will have health insurance as a result of the Inflation Reduction Act [15]
The health care provisions within the Inflation Reduction Act demonstrate a long needed willingness from Congress to address the staggering financial burden imposed upon Americans by a deeply flawed healthcare system. Even though many in Congress believe the price tag of the bill will be too high, there is no question that these provisions will lower the costs of health care for a significant portion of Americans.
12
Written by: Michael Go Edited by: Tingting Chung Designed by: Oscar Capraro
Context and Regulatory Debates
The US is facing a pressing healthcare staffing shortage crisis By 2034, the US is estimated to have a shortage of between 37,000 and 124,000 physicians [3]. As such, in recent years, researchers have been studying the potential efficacy of utilizing Advanced Practice Registered Nurses (APRNs) to alleviate this shortage. Nurse practitioners (NPs), the most common type of APRN, care for millions of patients and serve as “key providers” for community healthcare centers and nurse managed health clinics, especially for the underserved [7] Because of the ever increasing physician shortage, more states are considering expanding the scope of practice (SOP) of APRNs to fill the gap [1] The Improving Care and Access to Nurses Act (the ICAN Act), introduced on 09/13/2022 to Congress through Bill H R 8812, aims to allow for increased authority for APRNs to carry out a variety of treatments, such as determining if a patient is eligible for hospice [1]

At this time, 27 states do not allow for full NP practice authority [3] This debate is further pronounced between nurse/hospital (AANA, ANA, etc.) and physician groups (AMA, AAP, etc) [7, 8, 11]. Those against ICAN argue
that NPs usually have fewer years of training, that patients prefer to see physicians over APRNs, and that APRNs order more unnecessary services (ex: lab tests/imaging) [8, 12].

Autonomous: able to diagnose, prescribe medications, and oversee treatment
Removing Barriers to APRN Practice through the ICAN Act: the Debate between Access to Care and Safety.
Full Practice ReducedPractice Restricted Practice Direct supervision from another health provider Completely restricts NPs from carrying out an element of their practice Limits NPs from practicing one or more elements of NP care to full extent Requires some level of supervision 13
Scope of Practice Impacts
Access and Utilization of Primary Care
A 2014 study done by Strange defined access to care as “whether an individual had a usual source of care” and defined healthcare utilization as the number of office based visits in the past 12 months [7] A 2018 UnitedHealth Group Report predicted that 31 million more people could have access to primary care if all states allowed for NPs to practice to their full scope Strange’s study found that only by increasing NP authority and increasing the number of NPs was there a positive impact on healthcare utilization [7].
Moreover, without full SOP NPs must be supervised directly by physicians, hindering the ability for NPs to be dispatched to underserved and rural communities [7]. This problem will be further exacerbated by the fact that fewer physicians are entering primary care residencies (AAFP 2014). Evidence also shows that full SOP states have increased office visits, increased timely and convenient care, increased adults reported to be in excellent health, and decreased emergency admissions (demonstrates better preventative care) [8]
Cost of Care
Full NP SOP regulation and larger NP supply have been shown to only affect uninsured patients’ healthcare costs [7] Strange’s study showed that relaxed regulation did not affect charges per office visit, but this could be because of confounding variables such as the incentive for physicians to bill at a higher rate [7]. Additionally, another study by Hooker & Muchow in 2015 estimated that removing NP/PA SOP restrictions could save up to $729 million in Alabama from 2013 to 2022 [7]. Moreover, having full SOP for APRNs is also correlated with lower hospitalization and lower unnecessary specialty care [12]. Further, the cost of NP provided care is shown to be lower than that of physician care, even after adjusting for NPs' lower reimbursement rates [11].
Quality and Safety of Care
NPs have been shown to have similar performance to primary care physicians (PCPs) in terms of quality and safety of care despite fewer years of formal education, based on factors such as “reduction of symptoms, improvement in health and functional status, and mortality” for up to 90% of primary care services PCPs offer, and may even give patients higher satisfaction than PCPs because providers have more time and attention to listen and explain properly to patients, performing better than PCPs on patient compliance, health promotion, and disease prevention [7, 8, 9, 11]. This increase in autonomous NPs could also relieve PCPs of burnout and overload, especially seen during COVID and the 2017 opioid crisis [11]
Conclusion
In reality, the attitudes on the issue of APRN SOP are far less polarized than they seem A study on PCP and NP attitudes in Missouri noted how both physicians and NPs preferred that NPs held a higher level of autonomy given that NPs have some ability to reach a physician when needed.12 Even still, if the ICAN Act passes, it may be important to redefine stereotypes about NP autonomy for the sake of teamwork between NPs and physicians 10 Further research can focus on the development of a nationwide survey of PCPs and APRNs on these issues to provide a more accurate view of the US as a whole, as well as the impact of SOP on APRNs other than NPs.8
14
WHERE’S MY FOOD?
A Retrospective Analysis of the Healthy, Hunger-Free Kids Act of 2010
 WRITTEN BY NEIL TANGAL
EDITED BY AMARACHI MBADUGHA DESIGNED BY JULIA GERBINO
WRITTEN BY NEIL TANGAL
EDITED BY AMARACHI MBADUGHA DESIGNED BY JULIA GERBINO
Inresponsetotheirfavoritesubjectinschool,a sizable portion of students will emphatically answerwith“lunch.”Thus,understandably,there wasmuchdebatewhentheObamaadministration announcedtheHealthy,HungerFreeActof2010, whichwouldoverhaultheschoollunchprogram[1] SpearheadedbyMichelleObamaandherHealthy Schoolsinitiative,thebilllaidoutthreemainpoints: newnutritionstandards,increasedaccesstolunch, andincreasedaccountabilityforschoolsButdidit reallyimprovewhatwasalreadyinplace?
BreakingDowntheProposedLegislation
First,theHealthy,HungerFreeKidsActaimedto combat rising childhood obesity trends by modifying the National School Lunch Program (NSLP).AccordingtotheCDC,childhoodobesity rateshadjumpedfromjustfivepercentin1970toa whopping17percentby2008[2] Tocurbthis epidemic, the Obama administration looked to schoollunches.ThebillgavetheUSDAauthorityto set school lunch standards nationwide These includedwholegraincontentminimums,fruitand vegetableminimums,andcaloricandsodiumlimits [3]. The new rules were intended to work in conjunctionwitheachothertoensurethatallmeals servedwerenutritionallyappropriateforchildren


Thesecondpartofthebillaimedtochangetheway publicschoolsreceivedfundingforschoolmeals Previously,schoolswouldreceiveenoughfederal fundstocoverfreemealsforlowincomestudents. However,thisrequiredsuchhouseholdstofillout complicatedlunchforms,whichcamewithstigma andconfusion.
The new legislation sought to simplify the administrativeworkforbothschoolsandstudents: itdidawaywithpaperformsandreplacedthem withtheCommunityEligibilityProvision(CEP)[4].
ReactionstotheChanges
Thisallowedschoolsinlowincomeareastoserve free meals to all students Schools were now reimbursed by the government based on the numberofmealsservedandstudentparticipation inotherfamilyincomebasedprograms,suchasthe SupplementalNutritionAssistanceProgram(SNAP). Withlessadministrativeworkrequired,costswould decreaseandmorestudentswouldhaveaccessto healthylunch.
Ofcourse,thefirsttohavecomplaintsaboutthebill
proteinwithmorefruitsandvegetablesmeantthat portionsizesimmediatelyfeltsmaller.In2012,The
publication,“I’mabigguyIneedmorefoodthan this” FIG 1. MyPlate, the current USDA nutrition guide for balanced meals. 15
werethechildrenthemselves.Replacinggrainand
TampaBayTimesreportedthatafootballplayerat thelocalhighschoolhadconsistentlybeenbuying twolunchestosatisfyhishunger[5].Hetoldthe
He wasn’t alone: students nationwide complained thattheyleftlunchstillhungry.ThesatiricalTwitter hashtag #ThanksMichelleObama gained popularity, propagatedbystudentswhopostedblurrypictures of their school lunch Melancholic pieces of fruit and mystery mush circulated on the Internet, stirring up outrage. Some critics asserted that studentswereeatinglessfoodsincetheydidn’tlike thenewguidelines OnestudydonebytheNational DairyCouncilfoundthattheeliminationofflavored milk in some schools led to less milk consumption overall by students which was concerning as milk containskeynutrientssuchascalcium[6]
Evaluating the Bill’ s Effectiveness
But what did the act do for obesity trends? The answer is complicated Researchers from the Harvard School of Public Health evaluated the link betweenthisnewlegislationandchildhoodobesity trends [7]. The study linked BMI (Body Mass Index) of students between 2003 and 2018 with various covariates such as age, sex, and race The results were mixed: even when adjusted for different variables,thelegislationhadanon significanteffect onobesitytrendsoverall However,theyfoundthat when adjusted for income, low income students showed a marked decrease in obesity risk: without thelegislation,theriskofobesitywouldhavebeen 47 percent higher in 2018 Additionally, in one study,theCenterforPublicHealthNutritionfound that students selected healthier meals with no marked decrease in meal participation [8]. This suggested that the new guidelines were not worse for the students, but the results were not as overt aslawmakersmayhavehoped.
Thelinkbetweenthenewlegislationandaccessto school lunch has also been investigated
Researchers from the Johns Hopkins School of Public Health published a review summarizing the effects of the act and suggested various ways to improve it [9] Several studies found that the introductionoftheCEPledtoamarkedincreasein lunch participation, as well as a small increase in meal security for low income students Unsurprisingly, the CEP was associated with small gains in academic, disciplinary, and behavioral outcomes, reaffirming that access to healthier schoollunchwasextremelyimportantforstudents’ success
FIG 2. A Tweet from November 2014 showing a school lunch under the Healthy, Hunger-Free Kids Act

Additionally, the researchers suggested that streamlining the funding process for schools would greatly improve meal participation. This could be done by making it easier for schools to self identify as low income and qualify for the CEP Overall, the legislation was beneficial, especially for poorer students
The Healthy Hunger-Free Kids Act may have been loathed by school children nationwide, but the associated health benefits, and more significantly, the increase in access to said benefits, tell a different story. The plethora of studies performed throughout the decade tells us that the bill did more good than harm in terms of nutrition and food security However, more importantly, they also show us how we as a nation can revise and improve these guidelines for healthier children While the taste and variety of the food could be worked on, the Healthy Hunger Free Kids Act was a big step in the right direction. #ThanksMichelleObama.
16
Drug prices are at an all time high for Americans with the average cost per person for prescription medications at $1,300 dollars per year and per capita out of pocket drug costs are only projected to increase [1] Pharmaceutical companies have long claimed that such exorbitant pricing is due to high R&D costs associated with developing safe drugs However, pharmaceutical companies are often not transparent about the cost of bringing new drugs to market, and estimates of such costs by independent sources often conflict. While the value cost of drug development is unclear, the widespread anticompetitive conduct in the pharmaceutical industry is a well documented contributory factor to high drug prices plaguing Americans that continues to need redress.

Anticompetitive conduct refers to unfair business practices that thwart competition and free markets leading to higher market prices. Generally these practices fall under the category of monopolization, which is when a company maintains dominant market power by illegally excluding market entry to competitors, or horizontal conduct, which involves illegal agreements between companies that unfairly limit competition [2].





[4]

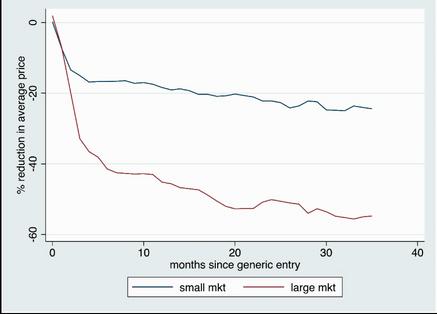
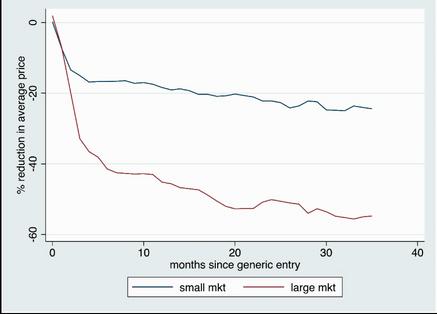
In markets with fewer firms, prices tend to be higher; therefore, prices in the pharmaceutical industry lower when originator drug patents expire and generic/biosimilar drug companies enter the previously limited market (See Figure 1) [3]. Pharmaceutical companies of originator drugs, however, impede the entry of such generics through various means, thus keeping prices high for drug payers.
For example, in the midst of the opioid epidemic, Reckitt Benckiser (now Indivior) slightly reformulated its Suboxone tablet, one of the leading addiction drugs, into a film version with “additional benefits” around the same time the patent on the tablet was set to expire. Before generics could even enter the market, production on the Suboxone tablet was halted by Indivior, and physicians were forced to switch to the patent protected film version of the drug [5]. This practice of “product hopping” prevents the entry of generics into the market and costs drug payers millions [6]. This Indivior scheme reportedly increased their profits by $1 billion while limiting patient access to this important drug due to pricing [7]. Another scheme involving Forest Laboratories’ replacement of a patent expiring Alzheimer’s drug, Namenda IR, with a slightly modified drug, Namenda XR, had a similar effect costing more than $300 million for consumers and $1.4 billion for third party payers [8]




17
Figure 1: Estimated Drop in Price for Originator Drugs after generic entry. Grootendorst, Percent Reduction in Average Price after Generic Entry
Originator drug companies also extend their market exclusivity by denying generic drug companies timely access to originator drug samples to begin production, sometimes forcing them to pay higher prices for samples, which increases generics’ R&D costs. One estimate found that 16% of generic drug companies in the Canadian Generic Pharmaceutical Association (CPGA) were delayed due to these tactics resulting in an additional cost of $57 million annually to drug payers [9]. The United States reported a similar impact and passed the CREATES Act in 2020 to provide generic drug developers an easier path to originators’ samples and a private right of action to sue originator developers that refuse to sell their samples [10]
When different pharmaceutical companies are selling similar drugs, agreements between the companies are sometimes made to maximize each other’s profits For instance, competing pharmaceutical companies producing similar drug products may agree to divide the market (market allocation), so in each respective market, there will be no competition [11]. Additionally, competitors may also agree to sell their product at the same price or coordinate with each other to determine who should win a bid for a product, known as rigged bidding. These practices are quite common in the pharmaceutical industry and lead to increased prices for consumers, prompting the Federal Trade Commission (FTC) to take action. For instance, in 2021 the FTC won a suit against Taro Pharmaceuticals USA Inc., Sandoz Inc., and Apotex Corporation for illegal price fixing among themselves, resulting in higher drug prices for federal health programs. As part of the settlement agreement, these companies paid a total of $871.9 million in civil and criminal penalties and agreed to a corporate integrity agreement (CIA), which subjects them to price transparency provisions and special monitoring [12] Given the utility of antitrust laws however, other anti competitive practices cannot so easily be pursued by the FTC, which means more systemic changes on a policy level should be pursued [13]




One such anticompetitive practice that has the potential to be reconciled on a broader level is “product hopping.” The Patent and Trademark Office (PTO) could impose stricter standards for patents that modify already existing patents to prevent pharmaceutical companies from frequently engaging in patent modification to insulate their market power The FDA can also change their standards around approval for drug market entry because their ability to keep tabs on relevant drug patents puts them in a well empowered position to detect “product hopping” schemes [14]. Moreover, the FDA could significantly help generic brand manufacturers bypass the patent abuse of pharmaceutical entities by improving access to biosimilar drugs [15].
Anticompetitive behavior, such as monopolization and horizontal conduct, is commonplace in the pharmaceutical industry and has long ranging negative impacts on consumers due to increased drug prices. As of late, the U.S. has taken legislative action such as the CREATES Act and legal action through the FTC; however, pharma’s antitrust issues are still pervasive, so taking other avenues such as patent reform could greatly benefit drug payers and the healthcare industry. Continuing to recognize and address pharma’s anticompetitive methods will promote a freer drug market, naturally lowering drug prices for the public

18
Where'stheBenefit
Where's
Addressing Exorbitant Prescription Drug Costs in the US
Written by Arjan Kahlon Edited by Arav Nangia Designed by Cherry Lin
n recent decades, patients nationwide have been faced with growing prescription medication costs. A study by the Commonwealth Fund found that “by 2015, U.S. spending on pharmaceuticals exceeded $1,000 per person and was 30 percent to 190 percent higher” than other Western countries studied including Canada, Australia, and seven European nations[1] Since then, the problem has only been exacerbated; a recent report from the U S Department of Health and Human Services notes that for over 1,200 pharmaceuticals, “price increases from July 2021 to July ddfd 2022 exceeded the inflation rate of 8.5% for that period. The average price increase for these drugs was 31.6%”[1]. Growing out of pocket costs can be attributed to many factors within the pharmaceutical manufacturing and distribution network One such factor is the immense complexity of the sale and distribution of a typical medication, which involves layers of for profit, low profile middlemen entities known as pharmacy benefit managers (PBMs)

Monkey in the Middle
However, this relatively old fashioned middleman trick isn’t the only way PBMs turn a profit. Today’s PBMs employ more complicated schemes, forming the basis of the process that helps determine pharmaceutical prices in the first place.


I
1) After
pharmaceutical
but doesn’t always
the
cost
2) Pharmaceutical manufacturers sell drugs
through wholesalers to
patients
investing in the development and testing of a drug, a
company sets a retail list price that influences,
determine,
final
to the patient.
based on list prices
pharmacies, who then dispense them to
3) 4)
The pharmacies are reimbursed by PBMs, who serve as the middlemen on such sales PBMs pay out a slightly higher price than pharmacies were originally charged, allowing them to turn a profit. The PBMs themselves are then compensated by patient copays and insurance company payments, totaling a far higher value than what the pharmacy was paid.
I
plans[1]
Ultimately, this practice, known as spread pricing, allows PBMs to pocket the difference and rake in huge profits by managing large scale health plans for insurance companies that cover both individual patients and larger groups, such as employee and prisoner healthcare
Fig1.FollowtheDollar,FlowofPaymentfora $3,000HIVMedicine 19
Drug Distribution Debauchery
When one walks into a pharmacy and picks up their prescription, the specific breakdown of their copay/insurance payment split varies from drug to drug based on its position on a formulary, which is a specific list of covered medications managed by PBMs. The cost of a drug with a higher position on the formulary is covered more by the insurance company and less by the patient, lowering end user costs, and thereby increasing sales of the drug In order to obtain a more advantageous position on the formulary, drug manufacturers pay a significant rebate of sales to PBMs A portion of this rebate is then distributed to the insurance company, which it uses to account for the higher insurance price paid as a reimbursement for the higher position on the formulary.
In this cycle, drug manufacturers are effectively forced to pay PBMs increasingly large rebates in order to maintain competitive positions on the formulary and influence the sales success of the drug As a result, drug manufacturers raise list prices to maintain profits, raising the overall price of the drug, and in turn, the copay paid by the patient. In today’s market, ensuring and improving the profitability of drugs necessitates maintaining competitive positions on formularies; pharmaceutical manufacturers are thus trapped in a cycle in which they are effectively forced to pay PBMs increasingly large rebates As a result, drug manufacturers raise list prices to maintain profits, raising the overall price of the drug and in turn, the copay and overall insurance costs paid by the patient The lack of oversight on this system allows under the radar PBMs to siphon money from the chain, which results in increased prices for patients[2].
FDA: Failure at Drug Administration


A substantial reason why PBMs are capable of unilaterally exercising control over the distribution system is a dearth of accountability and a lack of government oversight Since the FDA functions only as a safety checker and not as a value watchdog, its involvement in the pricing of new drugs entering the market is nonexistent; it essentially “allows every drug that's proven to be safe come onto market [sic]” with little scrutiny of the cost or its value proposition This stands in stark contrast to government evaluation protocols commonplace in countries ranging from Australia to Canada, and much of Europe In those countries, factors such as benefits, costs, efficacy, and other qualities are considered to determine a set purchasing price of newly launched drugs for all consumers in the country. This results in lower patient costs for the same medications[2]
Bridging the Gap
Comprehensively implementing the above system in the U.S. would be incredibly disruptive to the industry, as it would demand a sudden and massive top down change that would likely stunt future pharmaceutical R&D, as well as growth and investment in the entire sector To address rising out of pocket prices while still allowing for leniency for the many actors in the drug distribution chain, the U.S. could adopt a modified system based on expanded FDA evaluations, such that its authority more closely aligns with the functionality of regulatory bodies abroad. In such a system, the FDA would evaluate each newly developed drug before it is made available for sale, considering not only the safety of the drug but also the side effects, efficacy, treatment course, cost, and competition, among several other relevant factors
If the drug is approved, the FDA would negotiate generous but reasonable patient out of pocket/copay price caps for different levels of insurance coverage that can be re evaluated and adjusted over time[2]. Pharmaceuticals could continue to be sold to patients at rates set by insurance companies, but since a dynamic limit could be established on patients’ final copay for obtaining a medication, the cumulative cost to be paid to drug manufacturers would stabilize or decrease This decreased revenue would likely not precipitate the collapse of new drug development: Penn professor and co director of Penn’s Healthcare Transformation Institute Ezekiel Emanuel claims that even moderately large pharmaceutical manufacturers can expect to regularly see profits margins of over 30 50%, and that “even if profits were cut by a third or a half, there would [still] be sufficient incentive to assume the risks of drug development”[2] However, the outcome of this implementation would be a decrease in PBMs’ leverage, preventing them from unilaterally demanding ever increasing rebates from manufacturers who have their own profits to protect. Slowing this constant manufacturer PBM insurer cycle of increasing rebates and rising prices could prompt a voluntary restructuring of the pharmaceutical industry in such a way that all parties’ profits are distributed most efficiently to accommodate negotiated final patient costs for pharmaceuticals Mandating an established economic sector to conform to a new system would not be easy, but it may be one of the only viable methods to curb the unsustainable cost growth in pharmaceutical prices that we see today.
20
For-Profit, not For-Patient
Edited by Ashrit Challa Designed by Julia Gerbino
Introduction


With the exorbitant prices of healthcare delivery in the U.S., healthcare insurance is necessary for every American. Although the prices for healthcare services are relatively high, insurance rates vary depending on the type of healthcare service. Medicaid, a state program that uses funding to provide medical insurance for qualifying low income individuals, releases statistics regarding the fee schedules of physician services. With Medicaid, the average primary care visit costs $79 [1]. However, there is an apparent discrepancy when those prices are compared to more specific procedures that require specialists (e.g., vessel shunts, grafts, reconstructions, etc.). The costs of those services are relatively higher, with almost all costs exceeding $1000. Thus, it’s crucial to delve into different healthcare payment models and the concerns that arise due to the discrepancies in health service costs.
Healthcare Delivery within the Feefor Service Model in the United States
The fee for service model (FFS) is the most traditional payment model of healthcare services. In this model, patients are charged separately for every service that is performed Some argue that the FFS payment model leads to “overprovision, inefficiency, and uncontrollable health expenditures,” potentially pushing physicians to provide additional services solely for higher incomes [2] In many developed countries, governments form an agreement with physician associations regarding the number of services and physicians’ salaries [3]. However, in the U.S., the control over the number of services and physician salaries is in the hands of private insurance companies and providers [4].


For example, the average physician earnings in Germany is $183,000, whereas in the U S it is $316,000 [5] In an article released by the International Journal of Health Policy and Management, author Naoki Ikegami reveals: “[The FFS payment model] has allowed some physicians to earn twenty times the income of the average worker (or that of a nurse), and for cardiac surgeons to earn three times or more the income of general practitioners (GPs)” [6] The FFS system rewards physicians and healthcare providers on the number of services that are delivered, not on the quality of patient care This payment model increases healthcare inequity and bears the responsibility for the surge in costs and high utilization


 Written by Nancy Lam
Written by Nancy Lam
21
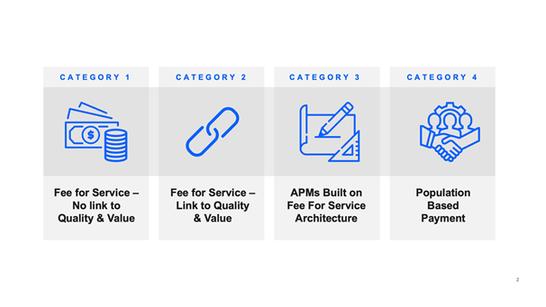
FIG 1. Healthcare payment models.
Fee For Service vs. Value Based Care
In the U S , the transition from the traditional FFS payment model to the value based reimbursement (VBR) model is currently underway The main purposes of the VBR model include controlling costs, reducing unnecessary healthcare services, and prioritizing patient health Under this model, physician payment corresponds to the quality of care delivered. Value based reimbursements are determined by analyzing quality metrics (e.g., hospital readmissions, adverse events, etc.) and overall population health improvement [7]. In contrast to the FFS payment model, the VBR model encourages physicians and healthcare providers to care for patients efficiently and effectively. Although VBR models are slowly becoming more prevalent in the U.S., it has not reached the goals that policymakers had in mind.
In a survey of the NEJM Catalyst Insights Counsel in July 2018, 38% of clinicians, 47% of clinical leaders, and 55% of executives believe that value based contracts significantly improve the quality of care [8]. The VBR model proposes promising methods to rectify the disadvantages of the FFS model; however, these low statistics may be due to a lack of substantial evidence that VBR models improve outcomes and control costs
$15 vs. $1500: Discrepancies in Costs of Healthcare Services



Arguably, the most urgent concern with the FFS payment model is that the financial incentives for delivering more services are prioritized over patient well being. In a 2012 documentary called Escape Fire: The Fight to Rescue American Healthcare, the director of the Cleveland Clinic’s Women’s Cardiovascular Center, Dr Leslie Cho, reveals some startling facts regarding the discrepancies in costs depending on the type of healthcare service Physicians get paid $15 for spending forty five minutes with the patient and delving more into the patient’s health problems by asking questions about exercise, diet, and lifestyle behaviors On the other hand, physicians get paid $1500 for spending five minutes with the patient and inserting a stent as a short term solution instead of figuring out the root of the problem This can lead to patients living with multiple stents and worrying about skyrocketing costs that accompany the stent placements
It is evident that learning about the patient’s health behaviors and educating the patient about preventions/interventions would be more beneficial for the patient However, the disparity in costs of an established patient visit versus a stent placement may influence physicians to provide patients with the latter, solely due to financial and time incentives Aware of the differences in costs depending on the type of service, Tine Hansen Turton, MGA, JD, FCCP, FAAN, President and CEO of Woods Services, and adjunct professor at the University of Pennsylvania’s School of Nursing, begs the question: "Why are we not incentivizing established patient visits rather than specialized procedures that provide short term solutions?”
Conclusion
It is evident that the U S healthcare system has shortcomings when it comes to physician reimbursements and the quality of care delivered to patients However, there is hope that the rise in VBR models can reach its goals of controlling costs, reducing unnecessary services, and improving health quality and equity The question of incentivizing primary care visits over procedures that offer short term solutions requires a thorough examination, and the collaboration of various stakeholders is essential to solving the issue of cost discrepancies in healthcare services



22
CHANGING THE DATED REIMBURSEMENT MODEL FOR BEDSIDE NURSES
Written by Angelo Petto
Edited by Jaskeerat Gujral Designed by Nancy Lam
Registered nurses are at the forefront of the American healthcare system, but are they valued as much as they should be? As nurses were integrated into the hospital setting back in the early 1900s, nursing service fees were lumped in with room and board costs, leading to the reimbursement model we have today The lack of a direct, value based reimbursement model for nurses undervalues their work and sets nursing services up as a cost to be cut, as hospitals do not bill for nursing services separately like they do for physician services The current reimbursement model makes it seem as if nurses are not valued in the hospital despite evidence nurses have a notable impact on patient outcomes and hospital costs [1]
Hospital Payment Through Medicare
To first understand reimbursement, it is important to look at how Medicare, the largest and most influential payer for hospital care, tackles hospital payments Under the Affordable Care Act, Medicare has moved away from a fee for service model of repayment, where services are paid for regardless of outcomes, to a value based model of repayment, with three different programs guiding payment based on hospital performance on various quality measures The first program is the Value Based Purchasing (VBP) scale, where hospitals can earn quality based incentive payments from a pool of withheld Medicare payments for scores on items such as patient safety, mortality, and overall patient experience. Additionally, there is the Hospital Acquired Conditions (HAC) Reduction program, where hospitals are scored on how often patients acquire conditions while they are treated in the hospital for something else and AHRQ Patient Safety Indicator scores, which provide information about the prevalence of adverse events and in hospital complications. Hospitals performing poorly will face reductions in their payment amounts Lastly, the Hospital Readmissions Reduction Program penalizes hospitals for excess thirty day readmission rates for patients with certain conditions [2]
Nursing Impact
The role of a nurse within acute care hospitals enables them to directly impact quality measures, especially those considered for the VBP and HAC scores. Researchers at Penn’s Leonard Davis Institute of Health Economics exemplify nurse impact on quality measures using the National Database of Nursing Quality Indicators (NDNQI). Two of these NDNQI indicators: Central Line Associated Bloodstream Infections (CLABSI) and Catheter Associated Urinary Tract Infections (CAUTI) are impacted by nursing interventions and are used to determine hospital VBP and HAC scores Researchers were able to calculate a percentage value designating the extent to which these outcomes contribute to hospital performance scores CLABSI was calculated to be 6 23% of the VBP performance score and 27 27% of the HAC score CAUTI was
"Nurses are at the forefront of the American health-care system, but are they valued as much as the should be?"
23
calculated to be 5 71% of the VBP score and 25% of the HAC score These percentages quantify the impact of nurses on VBP and HAC scores If nurse actions are directly associated with outcomes that determine hospital payments through Medicare, then it stands to reason nurses should be reimbursed directly for their services
The current system undervalues nurse contributions and blinds hospital administrators to nurse impact on hospital payments
Changing the Current Model
This raises the question: how can the reimbursement model be improved? Currently Medicare has benefit categories for Advanced Practice Registered Nurses (APRNs), including nurse practitioners, certified nurse midwives, certified registered nurse anesthetists, and clinical nurse specialists. Registered nurse services are typically encompassed under broader benefit categories, and payments are made to their employer [4] Codifying registered nurse actions represents a unique challenge Registered nurses perform various tasks during a shift and often care for patients that are not ‘theirs’ due to the collaborative nature of bedside nursing This makes it more difficult to codify and bill for registered nurse services than for physician or APRN services The additional time spent tracking and documenting the actions of an individual nurse on a shift by shift basis could potentially halt the care process
One model that could be used to inform a benefit category for nurses is the current model for Medical Nutritional Therapy (MNT) [5] MNT services, which are nutritional interventions for the purpose of disease management, are covered by Medicare for patients with diabetes, kidney disease, or who have had a kidney transplant in the last 3 years [6] Registered dietitians and qualified nutrition professionals bill for their services according to billing codes established by the American Medical Association Two of these billing codes consist of actions akin to what nurses do on a day to day basis, demonstrating it is possible to codify some of the actions nurses perform Specifically, codes 97802 and 97803 code for a 30 minute individual, face to face initial assessment and an additional 30 minute reassessment [7]
When nurses see a new patient, vital signs are taken and a physical assessment is performed, a process that parallels the 30 minute MNT assessment coded for by Medicare Reassessments are also performed by nurses as needed. Billing codes could be established for nursing assessments similar to the codes for assessments by dieticians and nutritionists. Use of the Electronic Health Record as the primary method of charting vital signs and physical assessment results provides a record to track these billable nursing services.

Conclusion
The value of nursing services should be recognized from a payment system lens Switching to a value based payment system where nurses can bill for their services not only prevents the devaluation of nursing services within a hospital setting, but also allows nurses to be adequately compensated for their work This model would also highlight nurses ’ value to patients, organizations, and healthcare overall
Value Based: Fee for Service: 24
Scotland’s Period Product Act

A L e g i s l a t i v e M o d e l t o A d d r e s s t h e U n e q u a l P r i c e o f P e r i o d s .
Written by Hiba Jamil
Edited by Shahana Banerjee
Designed by Julia Gerbino
For decades, American citizens and the rest of the world alike have experienced the effects of the politicization of menstruation. Yet despite these many frustrations, specifically, those regarding the increased taxation on women’s hygiene products referred to as the Pink Tax, there has been large cultural and governmental dismissal of women’s menstrual needs, resulting in inadequate legislation surrounding the crisis. In this landscape of inaction, Scotland has passed a landmark legislation, the Period Poverty Act, that established the country as the first to make period products free for all [1]. Having taken the lead, Scotland provides an important example for countries whose governments have long debated the merits of such policies. Financial and social incorporation of the Scottish model can prove beneficial to larger countries like the United States where the demand for period poverty legislation is pressing.

The Period Poverty Act (PPA) was introduced into the Scottish Parliament by MSP Monica Lennon, a lawmaker who first submitted a draft of the legislation in 2020. The unanimous vote for the act is a stark contrast from what other countries have experienced in past attempts to pass similar legislation [2]. The Period Poverty Act was not an unexpected legislative decision by the Scottish government but was preceded by several previous Scottish laws that provided free access to tampons in schools, universities, and public buildings. However, few menstrual health related policies have received as swift legislative acceptance nor have seen as large scale a policy implementation as compared to the PPA since it came into effect this year.
The Period Poverty Act is not just representative of a political change but also a cultural shift Hidden under the Scottish parliament’s unanimous acceptance of policies, omitting costs associated with menstrual hygiene is the shift in cultural paradigms that have normalized the conversation surrounding women’s struggles with their periods. In an email to New York Times, the aforementioned MLP Monica Lennon has been quoted stating, “We are witnessing a massive culture change, where period stigma is no longer being tolerated. There’s more emphasis on menstrual well being and a renewed focus on tackling medical misogyny” [3].
FIG1 A tweet by Member of the Scottish Parliament Monica Lennon on November 22, 2020 25
The increased menstrual activism in recent decades has worked to remove the taboos and hushed whispers in which the dialogue around periods has historically taken place This shift is apparent in advertisements for menstrual products, as well as across social media and other non profit campaigns which have been empowering women’s candidness about their menstrual struggles [4] Pop culture has additionally been a driving force of change, from celebrities to television shows which have removed notions regarding menstruation as unglamorous
Given this shift in social views around menstruation, there has been international frustration with menstrual health legislation with many criticizing the policies governing female bodies as largely antiquated The United States has 16 9 million people who menstruate living in poverty, and is one of the countries which has consistently worked to mobilize their government for legal remedies that policymakers have deemed “impractical” [5,6] With Scotland proving the ability to effectively execute such models, this could issue new amendments to US menstrual policies Additionally, the Scottish model of financing menstrual product supply is catered to succeed in an environment that generally emulates that of the United States For example, Scotland’s period legislation prior to the PPA is similar to current state level American policies that mandate local educational agencies to provide free menstrual hygiene supplies in California, Maryland, Washington, etc [7] Though fragmented, small scale PPA like legislation is applicable in the US
What’s promising about the implementation of the Scottish legislation is that it leverages today’s technologically driven lifestyles to maximize access to menstrual products One of the most unique features of the PPA is its delivery is made possible through a mobile app called PickMyPeriod The app allows users to determine the location most proximate to them that has period products available Additionally, for those unable to transport themselves to those locations, the app is also equipped with a home delivery service, an important consideration for those with disabilities or individuals lacking a form of transport such as a car The app will likely be especially beneficial when the legislation first goes into action seeing as it will offer clarity to users unsure about the logistics of obtaining free government funded menstrual hygiene products
These many benefits of PPA’s unique delivery model suggest that it is highly adaptable to the United States environment socially, technologically, and financially In the United States, where 85% of people own a smartphone as compared to 75% in Scotland, a technology based model of implementation is highly indicative of success to drive similar legislation in the US as the PPA [8,9] Healthcare technology has revolutionized individuals’ access to healthcare resources as well as the ability to monitor their health and seek out solutions. Such a culture is seen with the rise in users of health tracking apps and wearable devices such as Fitbits and Apple Watches which have found great popularity amongst the American public. Legislative policies intersecting with the accelerated world of health tech uncovers a novel path to creating effective public health interventions. Such a future may be what the United States needs in its approach to tackling period poverty. The technological aspects of the Scottish Period Poverty Act coupled with the similar cultural and environmental factors in both countries dissuade claims of impracticality and indicate that the adoption of similar legislation in the United States seems to hold a more optimistic future.
26
The Damaging Impact of Trade Embargos on Cuban Healthcare
Cuba’s unique healthcare model has long been upheld as the world’s gold standard in achieving exemplary outcomes with extremely limited resources [1]. However, COVID 19 has reignited the structural problems that Cuban healthcare had previously quelled: severe medical supply shortages, overworked and underpaid healthcare professionals, and limited access to US developed medical technology.
Although nations were forced to scramble for medical supplies during the early stages of the COVID 19 pandemic, the vast majority of nation states today can easily access critical medical equipment through mega exporters like the United States. But for Cuba, a trade embargo established during the Cold War makes it impossible to acquire these supplies from the US [2]


History of Cuba's Healthcare Challenges
Although Cuba’s constitution has guaranteed universal high quality healthcare since 1976, global events in the 1990s exacerbated by the trade embargo continue to negatively impact Cuba’s health system. Ronn Pineo, professor at Towson University, explains that the Cuban three tiered healthcare model prioritized direct patient treatment over medical technological innovation and domestic production of crucial medical supplies [3] As a result, Cuba was heavily dependent on foreign nations for medical technologies and raw materials. Given the presence of the US embargo since 1962, Cuba was primarily reliant on the USSR and on US subsidiaries headquartered in other nations [4]. Prior to the collapse of the Soviet Union, Cuba produced more than 80% of its medicine supply from raw materials acquired from the USSR. They also imported $719 million worth of goods and medicines from foreign based US subsidiary companies. Thus, Cuba had very few problems with healthcare supply shortages despite the trade embargo before 1992 [5]
Nigel White from the University of Nottingham believes that two separate events sharply increased the damaging impact of the embargo on Cuban healthcare. Firstly, the collapse of the USSR in 1991 rid Cuba of its main source of raw materials [6]. Then, in 1992, the US Congress passed the Cuban Democracy Act, an addition to the trade embargo that
Writer: Om Gandhi Editor: Aarsha Shah Designer: Nancy Lam
prohibited US subsidiaries from trading with Cuba [7] This had dramatic impacts that still persist today: Cuba’s access to medical products decreased by 30%, tuberculosis deaths increased by 48%, the amount of surgeries performed decreased by 30%, and contaminated water related conditions increased [8]. Therefore, for the past thirty years, the Cuban healthcare system has operated under substantial duress.
Cuba's Current Inaccessibility to Medical Supplies

Many technologies and drugs are only made by US companies and thus cannot be accessed in Cuba. For example, Prostaglandin, the gold standard drug for inducing labor and an essential medicine per the World Health Organization (WHO), is only produced by US corporations. High efficiency X ray films, recommended by the WHO for breast cancer screening, are only manufactured by Kodak, a US firm Cuba is also unable to purchase the radioactive isotope Iodine 125, which is used in areas from kidney disease to pediatric eye
 Image 1—Cuban physician travel abroad to fight COVID 19 in other nations
Image 1—Cuban physician travel abroad to fight COVID 19 in other nations
27
cancer. Substitute drugs and technologies all carry higher risks and lower efficacy [9]. The last few decades have also been marked by increasing consolidation in medical industries, further concentrating medical supply market share in the US and thus lowering Cuba’s access to potential suppliers For example, US based Blackrock bought Japanese Alinamin Pharmaceuticals (formerly a division of giant Takeda Pharmaceuticals), a leading producer in drugs that increase absorption of vitamins in the body, in 2020 [10]. None of these drugs may now be exported to Cuba. Loyola University Chicago Professor Joy Gordon explains how Pharmacia, a Swedish company, merged with Upjohn, a major US pharmaceutical company, in 1995. Pharmacia had previously been a major supplier of medical supplies to Cuba, selling a multimillion dollar array of medications such as protein purifiers, chemotherapy drugs, and growth hormones Within three months of the merger, Pharmacia’s office in Havana was closed down [11].
This all contributes to underlying structural tensions of Cuba’s healthcare system the sort of tensions that can exacerbate and prolong a crisis such as COVID 19.
Impact on Cuban Physician and Patients
TThe lack of medical supplies caused by the embargo has devastating impacts on physicians and patients in Cuba Thousands of Cuban doctors are sent to countries in need, as shown in Image 1, to have an opportunity to gain medical experience and be paid up to 25 times as much as their colleagues at home [12] Many of these doctors decide to not return to Cuba after their “tour” is over Octavio Dantes from the National Institute of Public Health in Mexico argues that the US embargo is the root cause of the exodus of Cuban physicians [13]. Since Cuban doctors have little access to medical technology or adequate resources, many leave Cuba for better medical opportunities. The remaining medical professionals are then overworked, which causes even more to either desert the profession or leave for a foreign nation [14].
Patients are also negatively impacted by both supply and physician shortages. With approximately 50,000 Cuban medical workers living abroad, queues and waiting times at clinics in Cuba are excessively long. Physicians remaining in Cuba must undertake greater responsibilities with limited resources, which translates to poorer patient outcomes, and patients sometimes have to travel long distances to find a physician [15] With the pandemic, supply shortages have resulted in many preventable deaths Alexander Izaguirre, a doctor in Cuba’s Granma province, explains that hundreds of thousands of deaths are going unreported, and that the state of Cuban hospitals is very
poor in the status quo [16]. Such a state of affairs is especially problematic in the midst of the global pandemic with a shortage of both medical professionals and equipment, the Cuban healthcare system is struggling to stay afloat
Solutions and Next Steps

While experts have identified a variety of strategies to mitigate this pressing issue, the primary solution is for the US to lift the current embargo on medical supplies to Cuba. In doing so, the US would alleviate a humanitarian catastrophe and open up a new market for medical exports.

The primary difficulty with such a policy is political Kelly Gouin from Yale University explains that Cuban Americans are highly politically motivated and strongly aligned against the current Cuban government. Given the high concentration of Cubans in a crucial swing state such as Florida, candidates from either major political party may be wary of liberalizing policies directed towards Cuba [17].
Experts argue that one way to limit the political damage of lifting the embargo on medical supplies may be to reframe lifting the embargo as a humanitarian issue Rather than openly claiming that lifting the embargo is designed to normalize US Cuba relations, it is possible to claim that the US government is taking a humanitarian action by shipping medical supplies to a country in need [18]. Furthermore, policymakers could argue that sending crucial supplies to Cuba would improve US standing in Cuba and undermine the Cuban regime’s legitimacy. Finally, experts believe that policymakers should emphasize that the embargo is not over the prohibition on the sale of weapons, consumer goods, and most other types of production is still alive [19] Rather, it would be a significant first step to help an industry crucial to human life: healthcare.
Image 2—Cuban physicians and other healthcare workers during COVID 19
"Experts argue that one way to limit the political damage of lifting the embargo on medical supplies may be to reframe lifting the embargo as a humanitarian issue."
28
Tanzania Mission: Dr. Härtl's NeurosurgicalAdvancements in East Africa
Written by Jaskeerat Gujral
Edited by Shikhar Gupta
Designed by Zachary Rentala

INTRODUCTION
Tanzania is a nation full of culture, from its vibrant music and dance to its delectable food However, one major issue plaguing many African nations, like Tanzania, is the lack of a modern neurosurgical foundation For example, trephination, a surgical procedure to perforate a hole in the skull to treat intracranial pressure, is one of the oldest procedures performed in Tanzania, considered a crucial ritual to this day [1]. The prevalence of such a surgery in East Africa can be attributed to the fact that there are only twenty seven neurosurgeons for 270 million people in East Africa, which highlights the need for neurosurgical advancements [2].
Fig 1 Picture of Dr Roger Hartl [10]
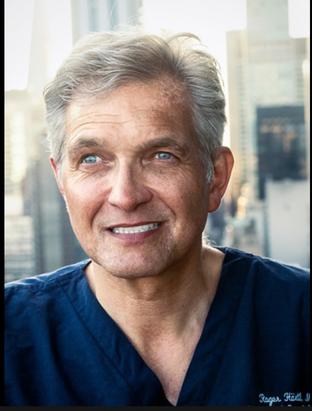
After treating a prominent figure from Tanzania, Dr Roger Härtl was invited to visit the country During his visit, he made it a priority to go to the hospital in Dar es Salaam, the largest city in Tanzania As soon he walked into the hospital, he promptly realized that the neurosurgical division of the hospital needed vast improvement There were only three neurosurgeons treating forty million people with no efficient way of treating complex cases, such as hydrocephalus, infections, and spinal disorders. Witnessing the condition that Tanzania was in, Dr. Härtl decided to found the Tanzania Mission in order to not only advance neurosurgery in the country, but also foster better health outcomes [3].
THEOBSTACLES
A few key obstacles stood in Dr. Härtl’s way, particularly the burden of disease in low and middle income countries with a lacking surgical workforce. Approximately six million people die from traumatic injuries with 89% of these deaths coming from low and middle income countries. Another challenge is surgery being the “neglected stepchild” in regards to global health. As a result, there has been an emphasized issue of lacking materials and appropriate organization. With these two challenges, it is impossible to have a successful program to treat millions of people with complex neurological conditions. The presence of community problems and the failure of primary care creates more barriers and difficulties when attempting to treat pathologies. In addition, exhaustion from the immense pressure and workload can be a major challenge, since it can take a serious toll on the physician.
29
It is unrealistic to have one neurosurgeon be responsible for millions of patients and the associated stress can lead physicians to sway away from medicine in the first place. Lastly, the concept of having a surgeon “carry the torch” is also challenging since there is a lack of proper education to put the physician in a position to mentor other surgeons [4]

THESOLUTION
To tackle these issues, Dr Härtl devised the Tanzania Mission, a program that consists of hands on training, observership in New York, local educational conferences, weekly Skype calls, research, and global neurosurgery fellowship [5].
In Tanzania, Dr. Härtl leads an annual hands on training program that involves a group of neurosurgeons, anesthetics, biomedical engineers, nurses, and students to teach local healthcare providers and surgeons. The team also gets involved in the brain and spine cases present. Dr. Härtl emphasizes the importance of Minimally Invasive Spine Surgery (MISS) because it not only creates ideal patient outcomes, but it is conducive in an environment where there are limited resources
Observership in New York serves as a way for surgeons to come to Weill Cornell and observe top quality care and neurosurgical expertise, emphasizing the importance of “carrying the torch" [6]. This past summer, Dr. Costansia Bureta, one of Tanzania’s neurosurgeons, came to Weill Cornell to both observe spinal procedures and fine tune their skull base techniques. Observership is a valuable experience because it allows for the visiting surgeons to bring what they learned during their observership back to their country.
The local educational conferences’ main purpose is to have yearly updates for participants and serve as a training opportunity [7]

The weekly skype calls are crucial as well because it allows for a way to discuss challenging cases, projects, and patient management [8]. As someone who has been part of these meetings, I know how helpful and organized they are; Dr. Härtl goes through any research projects that they were working on and discusses unique cases, which showed great organization.
Research plays a key role in this mission because it allows the surgeons to keep a database and conduct projects on the effectiveness of the program and how the newly introduced techniques are benefitting the patients in Tanzania
Lastly, a fellowship program is offered, which allows funding for a North American or European trained neurosurgeon to live in Tanzania and serve as a mentor [9]. It can certainly be said that this program has optimal structure and valuable aspects that will help neurosurgeons be more successful in giving back to Tanzania.
All in all, the training provided in Tanzania and the weekly skype calls allows the Tanzania Mission to be a great way to improve public health and policy in Tanzania The projected number of neurosurgeons in Tanzania should increase to fourteen by 2027, lessening the pressure on the current surgeons The Tanzania Mission will continue to provide help in any way possible and promote future neurosurgical advances!
30
Fig 2 Radiation oncology observership at UT Southwestern [11]
FUELING THE DECLINE OF YOUR HEALTH
Russia and the Fossil Fuel Non-Proliferation Treaty

The Fossil Fuel Non Proliferation Treaty is a global initiative implemented to phase out fossil fuels in an effort to facilitate bold and immediate action to address the impending issue of climate change The
mission has been described as “a global treaty that would end new fossil fuel exploration and expansion and accelerate equitable transition,” by the Toronto City Council. Fossil fuels have been the main cause of the climate crisis, and the Treaty’s goal is to phase out non renewable fuel production, and progress towards more sustainable and cost effective alternatives. The Treaty highlights how international cooperation is essential to tackling climate change, particularly emphasizing how wealthy countries have the resources to lead the movement [1]
In September 2022, several multinational health organizations, including the World Health Organization, World Medical Association, and World Federation of Public Health Associations, endorsed the Treaty, demanding governments to implement a strict global plan to phase out fossil fuel use The letter was a symbol of the organizations’ strong initiative to bolster the health and wellbeing of future and current generations The amended treaty would be grounded as an international task working to control three main elements known to be harmful to human health: coal, oil, and gas These elements are particularly under scrutiny from the WHO and other health
Written by Shahana Banerjee Edited by Siddharth Chitta
Designed by Jenny Li
organizations because their combustive properties release pollutants that link to early deaths, heart attacks, respiratory disorders, Alzheimer’s disease, and autism spectrum disorder A Harvard University study found that the air pollution from burning coal and gas was responsible for approximately one in five deaths worldwide [2] The risks from such fuels pertaining specifically to bodily health are immense and have continually presented severe threats to both the human and the planet’s wellbeing. The intersection of fossil fuels and population health is incredibly relevant, yet often overlooked, even though processes like mining, fracking, and processing and burning fuels for transport have been shown to injure populational health. Implementing the clean energy alternatives that evidently exist would pull communities out of poverty, support economic growth, deliver education and healthcare, and benefit social determinants of health [3][4]
Large carbon emitters like Russia have been publicly asked to use their resources to not only make the clean energy transition, but to assist developing countries in addressing the consequential health inequities While climate change poses health threats for every human, marginalized, high need groups, and people of color are disproportionately at risk;
FIG 1 Coal is burned to fuel power plants 31
the same factors contributing to worldwide inequities influence the degree to which communities face increased climate related health risks whose exposures can lead to heat related and cardiopulmonary illnesses, food , water , and vector borne diseases, and worsened mental health and stress Clean alternatives would help remote clinics, hospitals, and communities access affordable energy, while eliminating fossil fuels could massively improve indoor air quality, making buildings safer and healthier. Fossil fuels have disproportionately affected lower income and disadvantaged groups preventing
At a time where democracy and liberalism are under threat and Russia seeks to delegitimize liberal democratic norms, energy geopolitics can not be understood outside broader conflicts While the United States and Europe have attempted to isolate Russia politically and economically, it is critical to note how Russia is an essential fuel supplier In 2021, Russians crude and condensate output reached 105 million barrels per day (bpd), making up 14% of the world’s supply [9] Due to its corruption, illiberalism, and Vladimir Putin’s rejection of Western institutions, there has been a challenge in garnering international support to urge Russia to fight the climate change battle which, ironically, is a consequence of its own policies [10][11].
Russia has infamously been identified for its rigorous, non reformist political and economic culture. Its attack on Ukraine has caused changeable environmental damage, completely serting ecosystems, which will negatively affect a een transition of the Russian economy. The fossil el driven post Soviet state capitalism of Russia s barred its overdue modernization and ersification which has dismantled any ospective climate agenda With decades of such a litical history, it remains to question whether ssia will actually make amendments to abide by e Fossil Fuel Non Proliferation Treaty, and other milar movements for fossil fuel retraction Despite ssia’s actions continually attributing to the wnfall of the planet and human population’s alth, previous attempts to limit the expansion of fuels substantiates that Russia will likely remain daunted by such campaigns that diversify away from fossil fuels [12][13]
consumption, crises like the Russian invasion of Ukraine have underlined the exact opposite In Russia, fossil fuels symbolize both wealth and national pride As the battle against fossil fuel implementation peaks, all eyes are on how Russia will adapt. Overall in Russia, oil and gas have provided 39% of the federal budget revenue and made up 60% of the country’s exports. As sanctions against Russia were put in place post invasion, planetary professionals have been delving into Russia’s dependence on fossil fuels, leading to discussions about the myriad reasons for transferring away from toxic energy sources Currently, there’s a rush of divestment in all things related to Russia, including the oil industry [8]
Since the invasion, Europe’s dependency on Russian fossil fuels has revealed how the world’s renewable energy economy is deeply entailed by its geopolitically problematic supply chain


32
"While Russia’s global influence gives it the power to isolate itself and other countries from fossil fuel consumption, crises like the Russian invasion of Ukraine have underlined the exact opposite."
FIG 3 A drilling rig in the Yarakta Oil Field in Irkutsk Region, Russia
FIG 2
$55MillionGiftCreatesNew“CancerInterception”InstituteatPenn’sBasser CenterforBRCAtoStopHereditaryCancersattheEarliestStages
FundingfortheInstitutefromMindyandJonGraywillpropelearlydetectionandpreventionofbreast,ovarian, pancreatic,andprostatecancers
TheUniversityofPennsylvania’sBasserCenterforBRCAattheAbramsonCancerCenterannounceda$55milliongift fromPennalumniMindyandJonGraytoestablishtheBasserCancerInterceptionInstitute,creatinganewweaponto targethereditarycancersattheirearlieststages.

Theinstitutewillaimtodramaticallydisruptthetimelineofcancertreatment,“intercepting”diseasewhenthevery firstabnormalBRCA1/2cellsdeveloporevenstoppingcancerfromdevelopingatallratherthanreducingcancer riskthroughsurgeryortreatingcanceronceithasgrownenoughtobecomevisiblethroughimagingandtesting.The BasserteamwillpioneereffortsrangingfromdrugsandimmunebasedapproachestointerceptBRCArelatedcancers tonewmethodsofdetectingcancercellswithbiomarkersandartificialintelligence.
BuildinganInterceptionToolkit
EveryonehasBRCA1andBRCA2genes,butsomepeoplearebornwithanerror,ormutation,inoneofthesegenes. Menandwomenwitheitheroftheseinheritedgenemutationsareatincreasedriskforcertaincancers,including breast,ovarian,prostate,andpancreaticcancers.Today,optionsforpreventionofBRCArelatedcancersarelargely limitedtosurgicaloptionssuchastheremovalofhealthybreastsandovaries,bothofwhichcanbringsignificantside effectsandtradeoffsOtherpatientstypicallyundergoclosemonitoring,buttherearecurrentlynoreliableearly detectionmethodsforovarianandpancreaticcancer
Thegoalofinterception,Domcheksays,istoidentifyanddeployatoolkitofstrategiesthatcanbeusedmuchlikeHPV testingforcervicalcancerscreeningandcolonoscopiesforcoloncancer bothtestsallowidentificationofpre cancerouscellsandopportunitiestointervenebeforetheydevelopintodisease
AninterceptionplanforBRCAmutationcarrierscouldpotentiallyincludeaseriesoftimedinterventionsdesignedto keepcancerouscellsatbayInthecaseofa25yearoldwomanwholearnsshehasaBRCAmutation,forexample, futureinitialcaremightincludeclosemonitoringwith,forinstance,“liquidbiopsies”todetecteventhemost minuteamountsofabnormalcellsthatareonthepathtobecomingcancerAtage40,astheriskofcancerincreases, hercareteamcouldadministeracancervaccine,“settingback”thebiologicalclockandstoppingthegrowthof precancerouscellsAtage55,doctorscouldagainintercept,perhapswithadrugfromtheclassknownasPARP inhibitors,whicharealreadyapprovedforbothtreatmentandrecurrencepreventionofBRCArelatedcancersAtage 70,anotherinterceptionmightbeadministered,suchaspreventiveradiationorimmunotherapy
AdditionalpillarsoftheCancerInterceptionInstitute’sworkwillincludediscoveryscienceleveragingsamplesinthe BasserBiobankandtheGrayFoundationPreCancerAtlastoidentifytheearliestchangesassociatedwithBRCA relatedcancersandmarkerstotargetwithpreventionandtreatmenttacticsTheteamalsoplanstostudypathways associatedwiththesediseasesandpinpointwaystoshortcircuitabnormalcellgrowth,anddevelopnewearly detectionstrategiesemployingAIandnewformsofimagingTheGrays’giftwillalsosupportcreationofaprevention clinicaltrialsunitfornovelstudies,including“windowofopportunity”trialsdesignedtotestsafetyofdrugspriorto riskreducingmastectomiestoidentifydrugstobeusedforprevention
TolearnmoreaboutresearchandcareattheBasserCenterforBRCA,visitbasser.org.
33
Proudly Sponsored By:


Scan the QR code to access all endnote and image citations




















 WRITTEN BY NEIL TANGAL
EDITED BY AMARACHI MBADUGHA DESIGNED BY JULIA GERBINO
WRITTEN BY NEIL TANGAL
EDITED BY AMARACHI MBADUGHA DESIGNED BY JULIA GERBINO