4 minute read
Could anticancer drugs be used to treat PH?
from Emphasis Summer 2022
by phauk
Could anticancer drugs be used to treat pulmonary arterial hypertension
Researchers hope to access funding for a new study that will investigate whether a therapy to treat cancer could be repurposed for use in PAH. Here, we tell you more about what the team from University College London are trying to find out.
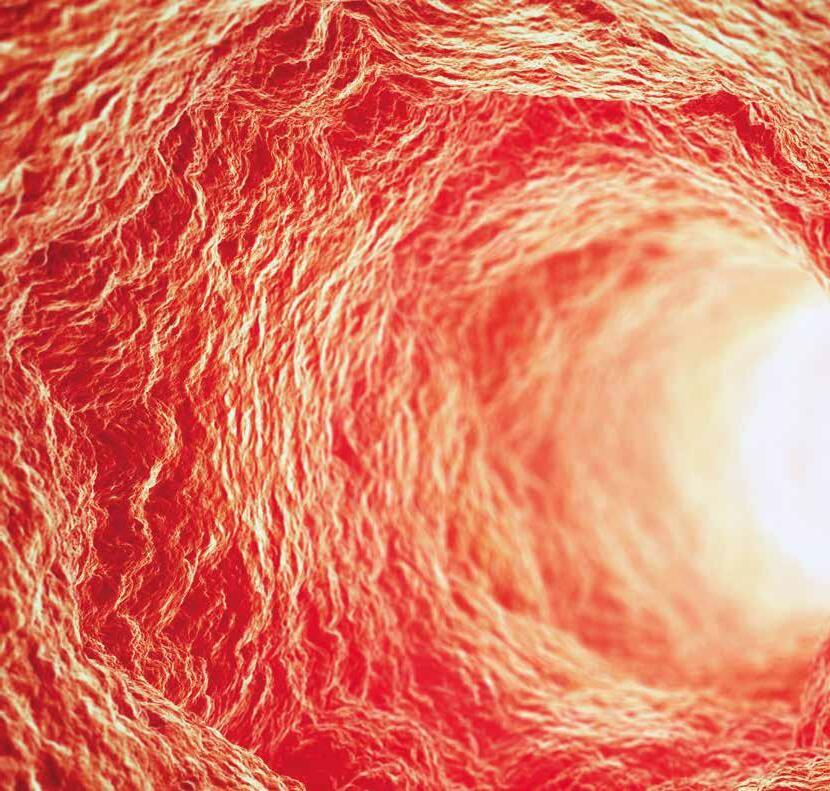
Pulmonary hypertension (PH) is caused by the small lung arteries becoming thicker, making it harder for blood to pass through these narrow channels.
A specific type of pulmonary hypertension in which the disease process occurs in the pulmonary arteries is pulmonary arterial hypertension (PAH). The condition causes the heart to struggle to pump blood through the lungs and causes high blood pressure in the lung arteries.
Currently, treatments for PH are based on drugs that relax the artery muscles to make it easier for blood to pass through. However, this doesn't address the thickening of the blood vessels – so up until now, conventional therapies have had limited impact on prolonging survival. The potential to repurpose well-known medication
Blood vessel dilators, known as ‘vasodilators’ are medications that open (dilate) blood vessels. There are several new treatments being developed and tested in combination with vasodilators to improve the disease process. Some of these drugs are approved and being used to treat other diseases such as cancer.
However, anticancer drugs cannot differentiate healthy cells from diseased cells, which leads to severe side effects for the patient. This has therefore limited their use and the problem remains a challenge for doctors and researchers.
A strategy is needed to tailor the delivery of a drug to exactly where the disease is in the lung blood vessels, to avoid the targeting of healthy cells that causes these side


effects. And as part of this, the ability to monitor the progress of the treatment in a non-invasive way is really important.
If clinicians can identify the drug is reaching the target area and evaluate this through medical imaging (for example medical resonance imaging, known as MRI scanning), they would be able to predict the response of specific tissue. This would then allow them to select the right amount of drug to be used, that would treat the disease effectively without the unwanted side effects.
Exploring a solution
Researchers believe a solution to this clinical problem is to package anticancer drugs into tiny nano-sized particles, which will help concentrate the treatment on the diseased tissue and decrease the side effects.
The study sets out to develop drug delivery strategies based on small particles (nanoparticles) that can be injected into patients. These nanoparticles will specifically concentrate in the lung arteries through a targeting molecule, that will be incorporated on the surface of the particles.
The strategies will also use medical imaging to improve and guide the treatment. This means that nanoparticles will also contain a radioactive molecule that allows them to be seen by special imaging methods – specifically a positron emission tomography (PET) scan.
This will allow doctors to evaluate how effective different doses of the drug are, so the right amount for each individual can be found. This is what’s known as ‘personalised treatment’.
The study sets out to address the challenges in treatment of PH by introducing alternative therapy, guided by imaging, through targeted delivery specific to the lung arteries. The targeting is non-invasive and medical imaging will ensure that the therapy is delivered to the thickened blood vessels only, and not to other areas of the body.
It normally takes around 10-15 years from the point of research for a concept like this to be used routinely for patients. However, because PH is a rare disease and researchers are seeking to repurpose drugs that already have regulatory approval, the team are hopeful that the process can be accelerated. The study is due to begin in October this year and a funding decision from UK Research and Innovation will be made before then. Keep an eye on our social media channels for updates. . Lecturer in Pharmaceutical Engineering at University College London

(RIGHT) DR BENJI SCHREIBER
Consultant Rheumatologist, Royal Free Hospital

The team of engineers, physicists and clinicians seeking funding for the study include Dr Maryam Parhizkar and Dr Benji Schreiber. They told us: “The outcomes of this study will have a substantial impact on our understanding of how this new nano-size drug delivery system can be further translated into the clinic, and how patients can benefit from more personalised treatment options. We are very excited about this, as we are experts from different disciplines working together to develop a highly specific therapy for PH. We believe this locally-delivered therapy for pulmonary hypertension would be a real advance for patients and will certainly be a great step towards finding a cure for this disease.”
Research studies into treatments for all types of PH are ongoing, and at the PHA UK we support these projects however we can. Although we cannot report on every piece of research, we believe it’s important to keep our readers informed of potential new treatments where possible – and our goal is that one day, we can bring you news of a cure.








