
17 minute read
Alumni Profi les: Q &A with Dr. Robert Poirier ’90
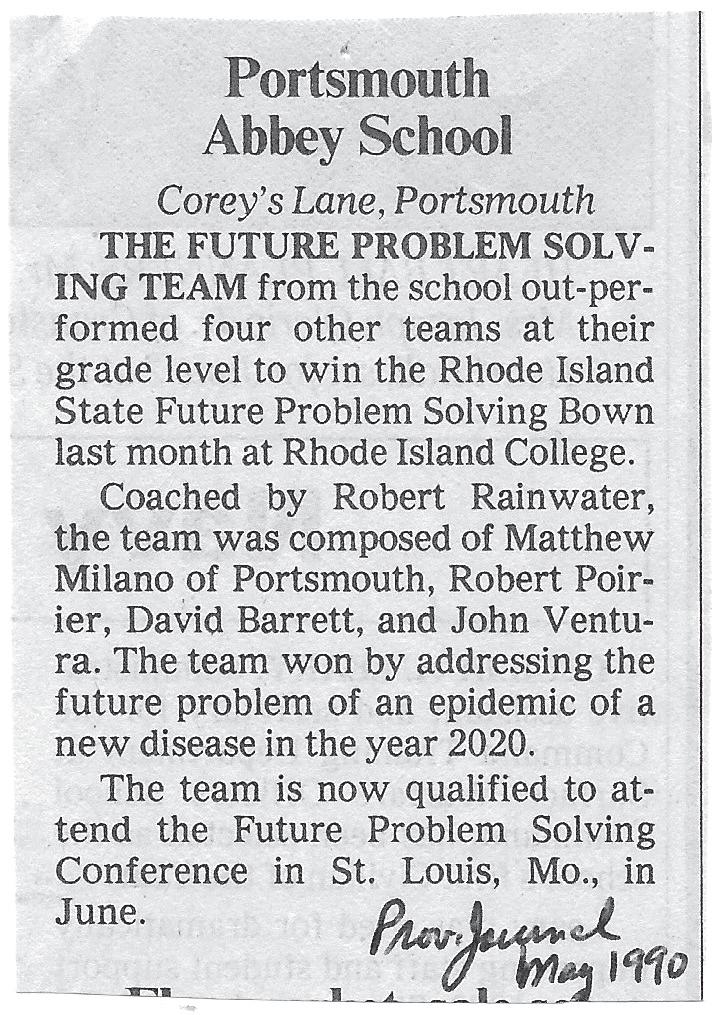
Providence Journal clipping courtesy of Carlene Ventura P ’91 ’93 ’99
IN HIS SIXTH-FORM YEAR AT PORTSMOUTH ABBEY,
Rob Poirier ’90 and classmates Matthew Milano ’90, David Barrett ’91 and John Ventura ’ 91 won the state Future Problem Solving Bowl. Their challenge: addressing the future problem of a new disease epidemic in the year 2020. The win qualified the team to compete in the national competition in St. Louis, MO.
Today, Poirier is clinical chief of the Emergency Department (ED) at the Washington University School of Medicine in St. Louis, confronting COVID-19, a new virus that is the cause of a global pandemic. Truth, as they say, is stranger than fiction.
Poirier recently spoke with the Office of Development & Alumni Affairs about that prophetic Future Problem Solving Bowl challenge, his experiences in the current pandemic, and the ways in which his time at the Abbey prepared him for a successful career in emergency medicine.
Q:What do you remember about that 1990 Future Problem Solving Bowl challenge? Did you feel that a pandemic was possible or even imminent at that point? A: I do not remember feeling at that time a pandemic was imminent. It wasn’t until I became involved in clinical research with antivirals that I realized the potential impact novel viruses could have on the world.
I would love to see what solutions our team wrote 30 years ago to the problem we now face, but from what I remember, we modeled our solutions after some of the learnings from the 1918 influenza worldwide pandemic. We predicted technology would be significantly advanced in 30 years and beneficial to managing/controlling the new 2020 epidemic. I remember we focused on solutions concerning disease testing, scientific efforts to find cures/vaccines, isolation, quarantine, law enforcement powers, ethics, public education, public hygiene, national logistical and manufacturing coordination for supplies, supporting the economy, supporting public health and retraining unemployed workforce to help with containment efforts. We talked about computer tracking/tracing (computers were in their infancy still in 1990). We modeled potential solutions from learnings about what worked and did not work from the 1918 pandemic. The cycle goes around; we can learn a lot from history. Q: Did the competition experience spur your interest experience spur your interest in the world of medicine? A: Since I was a young child, I have always asked a lot of questions. I have a curious mind by nature and an unrelenting inner drive to figure things out. I think it drove my parents nuts at times. We did not have Google back then, so I was told often to seek answers at the school or public library. Eventually we acquired a set of encyclopedias which I would often read. Joining the Future Problem Solving team at the Abbey just felt natural.
In medicine there are unlimited questions to be asked and answered along with problems to solve. Early on in college at Georgetown I took a course to become an EMT and work for the campus, student-run volunteer ambulance group called GERMS (Georgetown Emergency Response Medical System). My work study job was in the hospital. Later I became an emergency department technician and secretary and student president of the GERMS organization. My interest in becoming a doctor began at the Abbey and resulted in my choosing pre-med at Georgetown. My passion to become a physician only strengthened through my college experiences.
Q: What are your current responsibilities as clinical chief of Washington University’s Emergency Department? A: Within Emergency Medicine (EM), we have 56 EM residents (one of the largest EM residencies in the country); 80+ physician faculty; 40+ Nurse Practitioners and Physician Assistants; and 40+ administrative and research employees. This team serves a high-volume, high acuity inner-city Emergency Department seeing 90,000+ patients a year along with the St. Louis Children’s Hospital Emergency Department and two community Emergency Departments. Together, these operations serve 200,000+ patient encounters a year.
Additionally, I am the principal investigator on numerous day with COVID-19-like symptoms, although test shortresearch clinical trials evaluating new antibiotic and antiviages did not allow us to test everyone for COVID until the ral medication; I teach undergraduate, medical students, end of April. and residents regularly; and I serve as a Physician Advisor to executive teams at Washington University School of As ED physicians, we evaluate patients, performing lab Medicine and Barnes-Jewish Hospital. tests and radiology diagnostics to determine if admisQ: After completing your medical degree, you decided COVID crisis, volume in our main ED dropped by about 30 to earn your MBA as well. What motivated that decision? percent. Similar and higher reductions in ED patient visit A: Working in the Emergency Department of a large volume were seen throughout the country as most surgeries were stopped and patients were afraid to come to the complex hospital, you soon realize there’s a lot that can hospital for care. be further optimized clinically, administratively, and operationally. As chief resident and later faculty here at WashWe completely revamped our ED operations to manage ington University/Barnes-Jewish Hospital, I was tasked COVID-19 patients safely. COVID-19-suspected patients with many projects to improve operations, teamwork, were seen in different areas of the ED, separate from patient safety/quality, patient experipatients with no COVID-19 ence, and community outreach. I personally learned calming and symptoms. We analyzed what was happening overseas and Large, prestigious academic instituwellness techniques through prayer and in hard hit areas like New York tions like Washington University are meditation; both are stabilizing in times City and Washington State complex organizations. Washingand quickly implemented ton University and Barnes-Jewish of crisis and when quick decisions need to new strategies to protect our Hospital function as two companies be made. The Abbey monks taught these staff and patients. COVID-19 working as one to serve a large and testing supplies and Personal diverse patient population here in valuable techniques to students who were Protective Equipment shortthe Midwest. Together, our instituopen to the concepts. ages proved challenging. tions are a $4+ billion-a-year nonEmergency physicians are profit operation. Teamwork and significant political navigaconsidered the “MacGyvers” in the medical field. We tion are crucial to execute on performance improvement were innovating with new processes and equipment daily and efficiency projects at the institution. to best handle patients who had the virus.
Understanding the business side of medicine is vital to the success of our ED operations. I decided to pursue an MBA so I could improve my understanding and better speak the language of business needed to continue successful growth while also improving care for patients seeking emergency care.
Q: What has a typical day been like for you since the COVID-19 outbreak? A: A “normal” pre-COVID-19 day in our main ED would involve seeing average of 250 patients a day. We had our first test-proven COVID case around March 14th. A few days later, our ED was seeing 60 to 80 new patients every sion to the hospital is warranted. During the height of the Our ED admitted 20-30 patients each day with serious COVID-19 symptoms to the hospital. At the height of our first viral wave, as many as five patients a day might require intubation because of severe respiratory failure. The intubation procedure (putting a breathing tube into a person’s airway and taking over breathing for them) aerosolizes the virus and poses the most danger to our medical staff, so we had to learn new ways to intubate patients safely while also protecting ourselves and staff caring for these very sick patients.
In the beginning of May, we began to see slow reductions in patients with COVID-19-like symptoms. Reductions continued through May with only a few days of

small, manageable spikes in cases after social distancing and stay-at-home orders were relaxed. COVID-19 case numbers stabilized further in June and as of June 11 were slowly going down again.
We’re very proud that after almost three months of seeing COVID-19 patients, we did not have any spread of COVID-19 from patient to staff, staff to staff, or staff to patient. Protection measures we put in place for staff and patients are working!
Q: When did your cases peak and where are you in the cycle today? A: We experienced our first-round peak in St. Louis cases between April 10 and May 5. Our highest volume, most intense day was April 21. As of June 11, our COVID volume and census rested at half the peak and continued to decline slowly. Our non-COVID-19-related patient volume is returning, and we are now seeing an average of 220 patients coming through the ED each day.
We are seeing an uptick in visits for domestic violence, gun violence, behavioral and mental health issues, and suicide attempts along with drug/alcohol intoxication related issues. We have introduced new stressors into society with stay-at-home orders, social distancing, and furloughs/layoffs. Tensions have continued to rise as some want to ignore the new social distancing rules while others want everyone to follow new guidelines to reduce viral spread. Tension from police issues along with a focus on longstanding racism has further increased societal stress.
Q: Have you felt fear during this uncertain time? A: I have not felt fear particularly but have felt worried for others and have been frustrated that we were not fully prepared to handle the coronavirus impact.
My training and experience have prepared me to deal with situations like this in a calm, measured way. Portsmouth Abbey taught me how to solve problems, innovate, and think outside of the box. The Abbey instills a reverence for faith and all humans along with a respect for learning and order, teachings I have used throughout my career and try to teach to others.
Although the shared experience for community life has changed with social distancing, it should still be practiced to the best of our ability. I personally learned calming and wellness techniques through prayer and meditation; both
are stabilizing in times of crisis and when quick decisions need to be made. The Abbey monks taught these valuable techniques to students who were open to the concepts.
To be meditative, faith-filled, optimistic, persevering, and resilient is all a credit to my many teachers at Portsmouth Abbey, including Mr. Robert Sahms, my most significant mentor and role model at the Abbey. He was like a second father to me throughout my four years. He instilled in me a passion for science and using the scientific method to find answers to my many questions.
These characteristics have been tested and fortified during my many life experiences throughout college, medical school, residency, and my career. Without the Abbey’s spiritual, leadership, and service focus, I do not believe I would be doing what I continue to do today.
The Emergency Department where I work is always in a state of controlled chaos. We see and treat five-to-ten patients a day with gunshot wounds. We treat, support and connect to services five-to-ten patients a day suffering from heroin/opioid overdoses. Life and death hang in the balance almost every minute of the day.
I absorbed much through the Benedictine experience at the Abbey and later through Jesuit teachings at George

town. Stay energized; treat others how you would want to be treated; BE HUMBLE; be a life-long learner; approach problems with openness and problem solve using logic, skills and all the tools you have acquired –all were seeds planted in me by the Abbey. Reverence, Respect, Responsibility: the mission of Portsmouth Abbey still rings true in my heart even though I graduated 30 years ago.
Q: You’ve shared that at the Abbey you learned calm through prayer and that this helps ward off fear for you. Are you able to transfer that feeling of calm to your hospitalized patients who are fearful, and if so, how? A: Yes. I have used faith and prayer with patients and families when end of life has been reached or when there seems to be no hope. I routinely help patients and their families find inner peace, wellness, and calmness when very distressed by unexpected emergent conditions. Connecting to people through emoting that you care and have faith is helpful when guiding patients/families through grief and fear.
Q: Do you feel you it is important to share this gift with young medical students and residents?
A: Definitely. Practice is needed and you do not always Q: Any insight into a possible recurrence of the virus in get it perfect. But patients don’t want perfect, they just the fall of 2020 and can you offer any advice for prevention? want to know they are being cared for and others care about them. A: I cannot be exactly sure what things will look like Q: How do you teach medical students and residents to restrictions for social gatherings loosen, we will likely see have hope? some rebound in COVID-19 numbers. We still have a lot A: Incorporating physical, mental, and spiritual wellness to learn from this novel virus. I think we will get a bit of a break from high viral prevalence in the warmer months of techniques into physician education provides healthcare summer and fall but once it gets cold again late fall/early workers with the tools to prevent burnout, build resilience, winter, I do believe we will see another significant spike in reduce compassion fatigue, and maintain passion for the cases. I would not be surprised to see a need for stay-atprofession. Faith and hope run together. Teaching student home orders and more strict social distancing once again physicians to have faith in themselves, in their profession, during our seasonal winter viral season in the U.S. in their colleagues, in community, in people, in their religion going forward, but as stay-at-home orders expire and (if they have one), and in life are In terms of prevention and limiting all keys to internal well-being and hope. The Abbey taught me that. The Emergency Department where I work spread, we should all be washing our hands often and wearing masks is always in a state of controlled chaos. when in public and not able to Q: How has your faith served We see and treat five-to-ten patients a day socially distance. We should avoid you during this pandemic? touching our face, mouth, and nose. A: In all the ways mentioned above as well as in practical with gunshot wounds. We treat, support and connect to services five-to-ten patients We should avoid large crowds and gatherings until we have identified a successful protective vaccine and ways now available to me. Prayer a day suffering from heroin/opioid overfurther enhanced our COVID-19 is highly correlated with minddoses. Life and death hang in the balance treatment measures. Everyone fulness. Mindfulness is crucial during times like these. I have almost every minute of the day. should seek evaluation and possible treatment when feeling symptomatic missed seeing and hearing the with fever and shortness of breath. Abbey Masses over the years. Being able to watch reThose feeling symptomatic can seek out testing that corded vespers and holy Masses at the Abbey’s Church should be more readily and widely available soon. Selfof St. Gregory the Great is a source of inspiration and quarantine to prevent the spread to others will be impormindfulness. tant. Contact tracing and notification play a valuable role Although socially distanced in this COVID-19 time, we in limiting spread. We will beat this virus, but it is going have learned ways to become more connected through to be a marathon over the next couple of years, not a few Zoom, Teams, and other technologies, making it easy to months’ sprint over a finish line. connect our past and present. Many messages of inspira tion and hope are out there in our new world. Technology Q: The term “the new normal” is now ubiquitous. What and COVID-19 have shown us we can access these mesdo you see as the new normal, and what do you think will sages whenever we need to and want to. I recommend be the most challenging adjustments we will all have in fellow Alumni go to https://portsmouthabbeymonastery. our lives? org/ and experience once again the spiritual wellness and A: The “new normal” will not be so normal for many mindfulness of the Abbey Mass with its special Benedicof us…at least for a while. We are going to be dealing tine hymns and chants. with COVID-19 in one way or another for the next several
years. Naturally, we all want to go back to what we considered “normal” pre-COVID-19, but there is significant community risk if we do not take precautions that reduce the spread of the virus, at least until we find a successful vaccine that reduces morbidity and mortality among the most vulnerable of our society. Benefits must ultimately outweigh any risks.
Prevalence of the virus in our communities will wax and wane over the next few years. We must all do our part to prevent the healthcare system from becoming overwhelmed by surges that occur. This means we must enact reasonable measures to slow the spread, the practice known as flattening the curve. Some in our community, such as the elderly and those with multiple chronic medical problems, will be more heavily impacted by the virus. Consistent social distancing, which we must perform to the best of our ability when virus is in our community, will be a challenge. More challenging will be stay-at-home orders that may continue to come and go based on the toll the virus is taking in our local community at any one point in time.
If we follow the ten hallmarks of Benedictine education, along with its core values, we as a society will do well. Using technology will help us remain connected during these times where social distancing is required for the common good. Perceived loss of some freedoms we had pre-COVID-19 will challenge many. With discipline, humility, and innovation we will learn to overcome these challenges. We will eventually get used to wearing masks when around others and it is not possible to remain socially distanced. We will get used to having our temperature checked often and undergoing testing when feeling sick with potential COVID symptoms.
Despite our best efforts, we are not going to stop the continual spread of the virus long-term; we will only slow it, thus giving us time to adapt. When and if we get sick with COVID-19, we will need to quarantine ourselves to limit spread to others. Making sure we have capacity to provide the best medical care to all those who suffer ill effects from the virus is the goal. Fortunately, it appears the young are minimally impacted by the virus. Severe illness from COVID-19 fortunately is rare among this group in the population, but not zero percent. Humans are innovators by nature; we will find new ways to live life to the fullest in this new COVID-19 age. We will survive this crisis and it will eventually pass. Ultimately, we will come out of this stronger and more knowledgeable.
Q: Any final thoughts to offer our Raven community? A: I encourage people to take holistic care of themselves, with a focus on your physical, mental, and spiritual health and wellbeing. When feeling physically ill, do not be afraid to seek medical attention. There are many avenues through which to do this now. Telehealth will become more common and accessible. Call 911 if experiencing any acute emergency. I have seen some who waited too long to seek care throughout this crisis and now have permanent disability; some ended up dying. Healthcare settings have established preventative strategies to make seeking evaluation and care safe during this new COVID-19 era.
Exercising, lowering stress levels, and eating well balanced, nutritious meals strengthens your immune system. It is OK to cheat and splurge now and then, but not too often. With respect to your mental health, you should immerse yourself in something you feel passionate about. Go back to arts, music, literature, and hobbies you may have given up previously. Find things that make you happy and offer a mental break from the regular stress of the day. Spiritual health plays a HUGE role in your overall wellness and can have a significant impact on how you approach/perceive things. Prayer, faith, and meditation are crucial to your spiritual health but also provide significant benefit to your physical and mental wellness. It is all connected, just as we were taught at the Abbey.
Q: Any advice for students seeking to get the most out of their Portsmouth Abbey experience? A: Try to learn just as much from your teachers outside of class–mentors, coaches, house-parents, Abbey employees, and fellow students–as you do within the classroom. Try anything and everything you might have an interest in; you may not get another opportunity in the future. Be OK with failure and remember to fail forward, not backwards. Take time to discover and find out what your passions are in life. The Abbey is the perfect place to experiment.










