4 minute read
SOAPBOX
from Insight May 2022
by Prime Group
ACCELERATING TREATMENTS FOR IRDs
BY A/PROF FRED CHEN
Researchers, including myself, at Lions Eye Institute (LEI) are developing treatments for genetic eye diseases, including gene replacement therapies for Usher syndrome and novel drugs for retinitis pigmentosa (RP) and Stargardt disease.
Until now, our work to discover new treatments and cures for these inherited retinal diseases (IRDs) has gone well, but progress is set to accelerate rapidly once the first stem cell robot in Western Australia for eye research arrives at LEI, thanks to a generous $750,000 donation. Cell culture automation will free researchers from the most repetitive tasks, allowing us to focus on the business of understanding and treating blinding diseases.
To understand the function and purpose of a stem cell robot, first it’s important to remember IRDs are the most common cause of blindness in children and working aged adults. They are caused by mutations in genes only expressed in the retina. However, access to retinal tissues from IRD patients for research is limited.
Skin or blood cells are an alternative tissue source to study these diseases. While there are some things we can learn about gene expression from skin and blood, to understand what is happening in the eye we need access to retinal cells.
To gain access to retinal cells derived from patients with blinding diseases, the Ocular Tissue Engineering Laboratory has established WA’s first cellular reprogramming facility at LEI.
Skin cells harvested from our patients can be reprogrammed into stem cells, which can then be converted into retinal cells, as well as other human cell types. These retinal cells share the same genetic profile as the patient who donated the skin cells, including the genetic determinants of their retinal disease, making them an ideal tool for uncovering the molecular mechanisms of the disease and screening of potential treatments.
But cellular reprogramming and stem cell differentiation are timeconsuming, laborious processes.
Like embryos, stem cell cultures must be nurtured by prolonged daily routines during the three- to fourmonth reprogramming and validation process. Once stem cell lines have been generated, production of retinal cells can take an additional three to eight months of culture work.
These heavy demands have led to the development of several robotic systems that take over the burden of repetitive daily tasks such as feeding cells. In 2014, Melbourne’s Centre for Eye Research unveiled the country’s first stem cell robot, ‘Pierre’, which was heralded as a significant new asset for Australia’s research community.
In 2018, I met Bronwyn and Andrew Doak and their sons Eamon and Kealan, who have been diagnosed with Usher syndrome. It’s an exceptionally rare and cruel disease. Babies are born deaf, and towards their teens become affected by RP that causes night-blindness, loss of peripheral vision (or tunnel vision) and, eventually, blindness.
The Doak family was excited to hear about the cutting-edge research taking place in our laboratory and made it their mission to ensure we had the resources necessary for achieving the goal of developing IRD treatments.
In 2020, Eamon became a Telethon Star, sharing his story to promote funding of Usher syndrome research. After hearing this at the 2021 Telethon Leeuwin Lunch, philanthropist Rhonda Wyllie generously pledged to fund WA’s first stem cell robot at LEI.
With Rhonda’s support, LEI has partnered with laboratory automation company TECAN to develop a stem cell robot for our laboratory. The acquisition of this high-tech machinery will dramatically increase the amount of cell culture work that can be performed, fast-tracking sight-saving research into treatments for patients with IRDs.
We are extremely grateful for Rhonda Wyllie’s generous support, which will help ensure WA remains at the forefront of translational research.
Because the stem cells being produced at LEI can potentially be converted into any cell type, the stem cell robot will likely
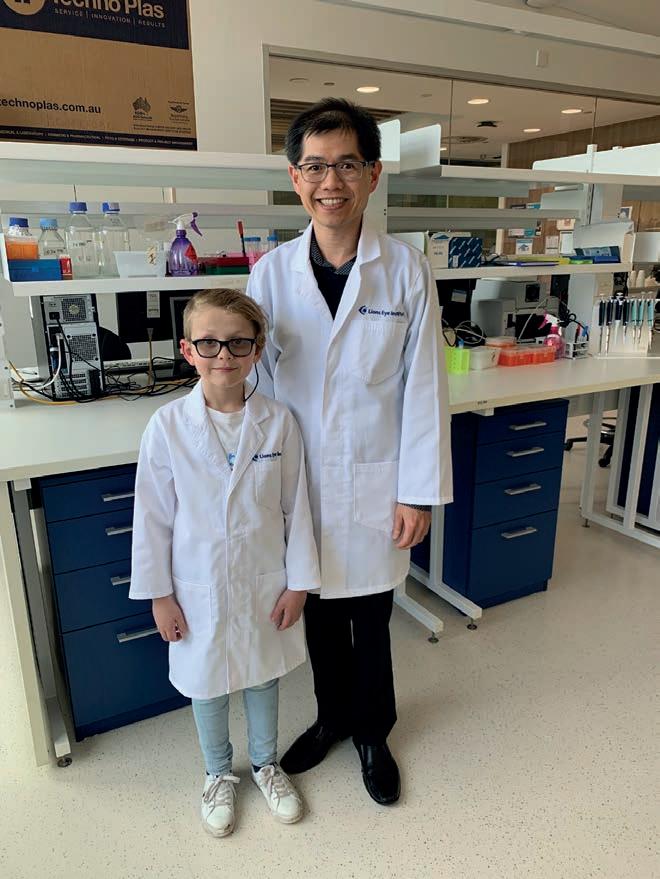
A/Prof Fred Chen with Eamon Doak who has Usher syndrome.
impact other areas of research in WA. LEI scientists are collaborating with researchers at the Ear Science Institute Australia, who are producing inner ear tissues from LEI’s Usher patient stem cell models to examine disease biology in the ear, as well as the eye.
Automation of retinal and inner ear organoid production on the stem cell robot will help to establish WA’s world-leading position in Usher syndrome research. In the future, we hope to extend our disease modelling capabilities to include other organs, such as brain, heart and liver and offer hope to patients who previously were resigned to a lifetime of illness. n
Name: A/Prof Fred Chen Qualifications: MBBS (Hons), PhD (London), FRANZCO Organisations: LEI, Centre for Ophthalmology and Visual Science, The University of Western Australia, Royal Perth Hospital, Perth Children's Hospital. Position: Head of Ocular Tissue Engineering Laboratory, consultant ophthalmic and vitreoretinal surgeon. Location: Perth Years in profession: 20, clinical practice and research. IN THE FUTURE, WE HOPE TO EXTEND OUR DISEASE MODELLING CAPABILITIES TO INCLUDE OTHER ORGANS, SUCH AS BRAIN, HEART AND LIVER.






