6 minute read
Gene therapies present AS MANY CHALLENGES AS OPPORTUNITIES
by Prime Group
Gene therapies represent the next frontier in ophthalmology, with a multitude of drug development programs progressing towards market clearance off the back of the breakthrough approval of Luxturna for RPE-65-mediated inherited retinal dystrophies (approved in Australia in August 2020).
These next-generation, potential one-time therapies aren’t limited to inherited retinal diseases either. Programs are looking into more-complicated-to-treat conditions like neovascular age-related macular degeneration (AMD) and geographic atrophy where the defect isn’t always necessarily down to one genetic fault.
With so much happening in this space, it can be challenging to remain abreast of the most promising techniques that fall under the gene therapy umbrella. There are also major challenges to address in terms of patient safety, drug delivery systems and scalability.
Moorfields Eye Hospital London consultant retinal surgeon Professor James Bainbridge demystified many of these issues in the Retina Update at the recent RANZCO Congress in Brisbane, offering a bird’s eye view of the gene therapy landscape.
He’s well accomplished in the area himself, performing the world’s first retinal gene therapy in 2007 and winning awards for his work developing such therapies for Leber congenital amaurosis.
How Gene Therapy Is Being Applied In Ophthalmology
Bainbridge commenced his RANZCO presentation by outlining the three main gene therapy techniques being tested in ophthalmology – each with their benefits and drawbacks. In essence, gene defects can be addressed by:
1. C ompensating by supplementation (Luxturna, the first and only approved gene therapy in ophthalmology)
2. C ompensating by silencing
3. C orrection by gene editing, which offers the most promise.
Ultimately, gene therapies are developed according to the impact of the gene defect on the protein that it encodes.
In the case of ‘supplementation’ – the simplest and most common approach – Bainbridge said the patient’s condition can be improved by simply providing synthetic copies of the healthy gene to the cells that need them. This does not correct the gene defect, but establishes a sustained separate expression system inside the cell that compensates for the deficiency.
This approach has enjoyed a rapid rise, with the first proof-of-concept recorded in 2000 before the first in-human delivery in 2007 and eventually market approval in the US by 2017.
In contrast, therapies based on ‘silencing’ are designed for when a gene defect produces a protein that has an abnormal toxic function. Protection might be offered by blocking or interfering with the RNA.
“However, these approaches must both silence the toxic gene efficiently and specifically, if they’re to avoid harm by interfering with the expression of the healthy gene. And this combination of efficiency, expression and specificity presents a serious challenge.”
Gene editing, which encompasses the famous CRISP-Cas9 platform that exploits an ancient bacteria anti-viral system, has become more feasible in recent years. This form of therapy offers the most potential by correcting the exact genetic fault to permanently produce a healthy protein.
While this shows the most promise, issues remain with the two methods being applied.
The non-homologous end joining approach involves cutting out the target defect, before the DNA strands join back together – while this is efficient it can be imprecise. The alternative method, homology directed repair, allows for pasting of a new sequence into the double stranded breaks to correct for an existing defect or to add a new one –however this process is inefficient and doesn’t work particularly well in the non-dividing cells of the eye.
Challenges To Overcome
To realise the potential of gene therapies, Bainbridge pointed to several challenges that need addressing.
For example, the supplementation of large genes will depend on new vector systems, while optimal safety and efficacy will demand improved control of both genetic dosing and harmful inflammatory responses. There’s also the need to avoid off-target effects and overcome inefficiencies in the techniques.
To compensate a gene defect through supplementation, the working copy of the gene needs to be delivered through a special vehicle, most commonly the adeno-associated viral vector. Viruses are highly evolved for this function to deliver the gene, and can be disabled to prevent the spreading of infection.
“Viral vector systems can efficiently deliver genes of a certain size to target surviving photoreceptor or RPE cells, if the vector is delivered closely in contact with those cells, for example by subretinal injection. This is conventionally achieved using a pars plana vitrectomy approach, but alternative routes are being explored,” he said.
“In addition to single gene defects, similar vectors are being used in trials to establish sustained local expression of therapeutic proteins in complex acquired diseases, principally AMD. These include expression of aflibercept for neovascular AMD and expression of compliment factor I in geographic atrophy.”
But Bainbridge said currently available vectors that can target photoreceptor cells have limited capacity and cannot accommodate larger genes like those involved in Stargardt disease and Usher syndrome, or indeed some of the gene editing components necessary for CRISPR-Cas9.
“So alternative strategies are needed for this,” he said.
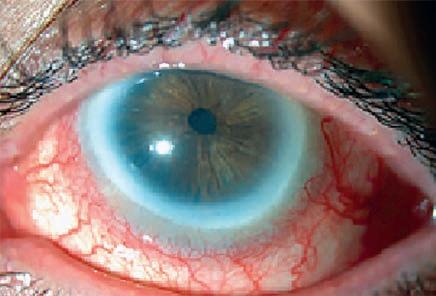
“It’s also perhaps not surprising that the delivery of billions of copies of viruses into the eye causes inflammation and this has been anticipated. This does appear to present a risk of harm.
“For example, there’s increasing awareness of inflammatory events following injection subretinally of Luxturna and this is just one example. A recent report with 12 patients receiving Luxturna, according to the appropriate methods, showed a number developed vitritis and a number developed areas of atrophy which are not limited to the bleb itself but appear to evolve in areas outside the bleb.”
Bainbridge said the exact mechanism of this was not clear, but seemed to relate to a sub-acute or chronic immune process. To date, there doesn’t appear to be evidence that it actually causes harm in terms of the overall functional effect, but there is a likelihood it could in the longer term.
“So this is something which needs to be addressed. And in terms of safety of the vector itself this could include modifying the capsid (the protective protein shell), or perhaps the route of delivery can be changed and consideration of alternative immune suppression techniques is going to be important.”
With this in mind, Bainbridge said intravitreal injection remained an attractive opportunity for gene therapy delivery – even though this method has had difficulty targeting the outer retina. But there are potential methods to modify the capsid to make this possible in small experimental models at present.
Gene Therapy Delivery Mechanisms
Nevertheless, gene therapies still rely on being delivered in the subretinal space, which is conventionally done by a transvitreal approach. According to Bainbridge, this is efficient and offers the ability to accurately target the therapy, but has the disadvantage of being invasive.
“In terms of scalability in the long term, it’s difficult to imagine how this can be performed cheaply and easily for everybody that might benefit – so there are alternative ways to try to deliver genes to the subretinal space,” he said.
These include a transscleral approach which is performed in conjunction with a cannula that can be inserted anteriorly and fed posteriorly behind the macula with a needle that is inserted through the choroid and into the subretinal space, avoiding the side effects of vitrectomy.
But Bainbridge said this approach introduced other concerns; for example, it might be difficult to target the macula if that is what’s required.
The other alternative is suprachoroidal or transchoroidal that involves delivery of a therapy to the suprachoroidal space using microneedles past anterior to the pars plana.
“This is potentially scalable but not targeted, and has uncertain systemic dissemination and immunogenicity. This pathway may prove to be a viable alternative for the treatment of acquired retinal diseases where cell specificity is not a priority. Trials of this device are ongoing with the use of Regenxbio’s product in AMD. This demonstrates widespread expression in preclinical models and is being investigated in patients.”
The final challenge that must be addressed to allow broader use of gene therapies relates to the design of clinical trials to evaluate their impact. Bainbridge believes they must adopt reliable and relevant outcome measures that demonstrate improved quality the challenge of confidently measuring rod function and understanding how children in a reliable manner while performance and learning effects.
“We need relevant, sensitive patient reported outcomes that includes quality of life. We also especially where we might see improvements and function which
“We also need to consider whether it’s feasible and ethically acceptable to include sham injection, or some form of placebo control. And finally, we need to consider how we can get rapid outcomes: where we expect an improvement in function we hope this can be measured quickly with confidence, but in many of these conditions we rely on slowing or arresting of degeneration that may become evident only after many years.
“Ideally, we would have some sort of surrogate measure that might be easy to measure, such as imaging, or electrophysiology, but this is going to take some time to develop.”
An Exciting Prospect
In summary, Bainbridge said there has been significant progress in the gene therapy space, with supplementation for deficiencies now a reality. Meanwhile, silencing can improve the affected site temporarily, and the prospect of gene editing to not just compensate for gene defects, but to correct them in vivo, is “a really exciting prospect”.
“Having said that, there are major challenges to be faced, including targeting and dosing of these new products, managing and understanding some of the immune responses, optimising some of the surgical delivery techniques for safety, efficiency and upscaling, and, finally, optimising trial design in order to be able to make these improvements rapidly and reliably,” Bainbridge concluded.