7 minute read
WHAT THE EYES tell us about the brain
by Prime Group
PROF HELEN DANESH-MEYER was ranked by Ophthalmologist magazine as one of the top 100 most influential people in the world of ophthalmology in 2022. Several aspects of her research have influenced and altered clinical management strategies, particularly in the field of neuro-ophthalmology.
As early as 1986, a team at the University of Southern California undertook a post-mortem study in deceased patients with Alzheimer’s disease and observed that eight of their 10 samples demonstrated varying levels of optic nerve degeneration.
But due to the study’s very small sample size, and limited post-mortem histological methods, determining the relevance of this observation had to wait 20 years, when in 2006, Professor Helen Danesh-Meyer’s research team reported the first study on this topic in living patients.
“We started the efforts a few years earlier with the Heidelberg Retina Tomograph (HRT), a scanning laser ophthalmoscope. At the time, the HRT was the only technology available that could quantitatively image the optic nerve,” she said.
“We correlated optic nerve measurements and retinal nerve fibre layer with cognitive function and risk of Alzheimer’s disease in 90 participants. Our study found a clear dose-response relationship between optic nerve head thinning and lower cognitive function, including a threefold excess of Alzheimer’s disease and patients with extreme thinning. Importantly, this was in the absence of any measurable optic nerve visual dysfunction.”
The fascinating insight is an example of the way in which technological advances have opened opportunities for novel ocular biomarkers into brain function and disease, which was the focus of Danesh-Meyer’s Dame Ida Mann Memorial Lecture at RANZCO’s 53rd Congress in Brisbane in late 2022.
Ultimately, her team’s work helped establish the concept of optic nerve biomarkers and their ability to give insight into central nervous system injury. But it also raised new questions about whether future advances in technology would support the clinical translation of their findings, given the inherent limitations of HRT.
The answer was ‘yes’.
About The Speaker
“More than a decade after the publication of our group’s results, a team lead by Moorfields Eye Hospital combined OCT, and serial cognitive testing in over 32,000 participants in the UK Biobank population study. Their findings confirmed our observations,” Danesh-Meyer explained.
“Thinner retinal nerve fibres were associated with worse cognitive function, but they also made an additional intriguing observation. Retinal nerve fibre layer thinning is associated with a doubling of risk of future cognitive decline.”
Further research from her team and others has generalised these observations showing that the link between the optic nerve biomarkers and cognitive decline are not an isolated example.
“Accumulating data also show that ocular biomarkers are an indicator of a wide range of neurodegenerative diseases. Such findings will be useful in clinical trials of novel agents in neurodegenerative conditions and have already been incorporated into some trials.”
M ultimodal imaging of the optic nerve is advancing the diagnosis and management of patients with a range of neuro ocular conditions. But Danesh-Meyer believes a challenge in the coming years will be to identify imaging and other biomarker signatures that are specific to neuro ocular conditions.
Eye Tracking And Concussion
According to Danesh-Meyer, recent advances in software and hardware technology have opened major opportunities for examining the efferent visual system.
“Over the past three years Dr Matthew McDonald, a PhD student in my group, has built a state-of-the-art eye tracking system using 3D printed glasses. The device is compact and mobile and allows a patient’s gaze to be mapped with high precision and accuracy,” she said.
Professor Helen Danesh-Meyer is the first female Professor of Ophthalmology in New Zealand and is Sir William and Lady Stevenson Professor of Ophthalmology Chair at the New Zealand National Eye Centre, University of Auckland.
As a neuro-ophthalmologist, she pioneered quantitative evaluation of the optic nerve and its morphological changes using many optic nerve imaging modalities such as OCT.
Several aspects of her research have influenced and altered clinical management strategies in the international arena, in particular her work on imaging of the retinal nerve fibre layer and chiasmal compression.
Over the last 20 years, Danesh-Meyer has established the Optic Nerve Research Laboratory at the University of Auckland which investigates mechanisms of injury and repair in the optic nerve head and retina.

Examining the issue of concussion, McDonald worked with Matai Medical Research Institute (Gisborne, NZ) to recruit 40 high school rugby players who were tested at the beginning and end of the season, as well as following any concussion.
Each player also wore a mouthguard accelerometer, which allowed McDonald to quantify the amount of force sustained to their heads throughout a season.
Initial pre- and post-concussion eye tracking results were striking, demonstrating micro saccadic intrusions invisible to the human eye, occurring in less than 20 milliseconds, but a characteristic of concussion.


“These gives us a glimpse into the omnipause neuron function and the pathology that occurs with concussion,” Danesh-Meyer said.
Given that the US National Institute of Health recently acknowledged a causal link between concussion and chronic traumatic encephalopathy, such readily available tools for diagnosing and managing concussion are likely to play a major role both in amateur and professional sports in years to come, she said.
Disease Prognosis
There’s also evidence to suggest that the eye has a role in prognosis. In 2006, together with collaborators from Wills Eye Hospital, and Dr Peter Savino, Danesh-Meyer’s team reported the first study to compare structure function correlation of retinal nerve fibre layer thinning in patients with chiasmal compression, taking advantage of the newly available OCT at the time.


They found that temporal and nasal quadrants showed thinning of nearly 50% in patients with complete bitemporal hemianopias.

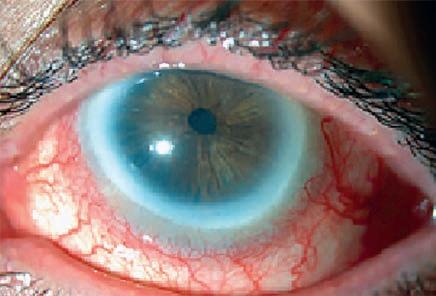
However, in some patients there is a glaring mismatch between a normal-appearing OCT and a dense bitemporal defect, dismissed in some instances as poor scanning technique, or the unsuitability of OCT in neuropathy, she explained.
“Rather than interpreting our results as artefacts we believed the mismatch told the meaningful biological story, something essential about the nature of compressive optic neuropathies,” she said.
“We hypothesised that our findings demonstrated that compression at the chiasm was analogous to one’s arm falling asleep; after sitting on it for a period of time, function is lost, but structure remains intact. So, if we freed the compression, such as with pituitary surgery, the function should improve. To us, this interpretation explained why the OCT was measuring a normal retinal nerve fibre layer and the presence of a complete bitemporal loss.”
Along with neurosurgeons in Auckland, and at Wills Eye Hospital, Danesh-Meyer and her team designed a prospective study to test if OCT could predict recovery of vision following chiasmal compression.
“Remarkably, we found that the degree of recovery of visual dysfunction was related to the thickness of the retinal nerve fibre layer as a measure of OCT,” she said.
“We had identified a biomarker that predicted degree of visual recovery after surgical intervention. In particular, patients with a complete bitemporal defect, who had recovery of greater than 10 decibels, had an OCT thickness of greater than 75 micrometres.”
To investigate the temporal pattern of visual recovery following pituitary tumour resection in eyes with and without preoperative retinal nerve fibre layer (RNFL) thinning, they then conducted a 10-year prospective study of 230 patients in collaboration with the neurosurgical department at the University of Melbourne.
“We found that eyes with normal retinal nerve fibre layer thickness at baseline experienced most of the recovery within the first six weeks. However, eyes with a thin RNFL had whatever recovery they were going to have at a much slower rate,” Danesh-Meyer said.
“We’ve subsequently extended this work and developed a multivariable risk prediction model, which has now been widely adopted for patients counselling and prognostication, making a real-world impact.”
Dynamic Injury
While advances in imaging have allowed visibility of detail previously invisible to the naked eye, Danesh-Meyer said there is another invisible world to be visualised: tiny motion.
“Our assumption about aetiology of disease has been dominated by what we see in static 3D because that is what available technology can resolve. But perhaps this paradigm needs to be challenged,” she said.
“We now have tools to see the brain in motion. Eulerian magnification relies on computation rather than optics, and it is already having an impact on biology, structural analysis, and mechanical engineering – and it is poised to make a major contribution to clinical neuroscience.”
Dr Samantha Holdsworth at the University of Auckland has recently taken this technology and applied it to MRI to create a new imaging processing tool called Amplified MRI, to study eye brain connections.

“Our initial focus is to develop a non-invasive technique to measure intracranial pressure, and we are working towards being able to incorporate a four-minute amplified MRI (aMRI) sequence that will accurately estimate intracranial pressure,” Danesh-Meyer said.
“Motion maps from patients pre and post lumbar puncture are allowing us to build a computational model that predicts brain pressure. We are also using this technology to help understand how microscopic movements impact different eye and brain diseases.”
Danesh-Meyer and her team are applying aMRI to two conditions where the translaminar pressure gradient plays a significant role –glaucoma and idiopathic intracranial hypertension (IIH) – and shared some preliminary unpublished data at RANZCO.
“In patients with IIH, there are three interesting observations post lumbar puncture. First, the optic nerve sheath diameter is visibly smaller. Second, the sheath is more collapsible. And third, the entire optic nerve seems more mobile in the orbit following lumbar puncture,” she said.
“In glaucoma, it appears there’s no significant difference between pre and post IOP but we need to recruit a few more patients to confirm this. However, in the orbit, there seems some intriguing observations. In one case, a patient had an IOP of 27 millimetres of mercury prior to treatment, and then we applied latanoprost and brimonidine to lower the IOP to 15. The pre-treatment eye with high pressure shows significant greater anterior posterior movement while, in contrast to IIH, the diameter of the sheath is greater after drops. We’re still to unravel the full implications of these findings so watch this space.”
In closing, Danesh-Meyer highlighted Ida Mann’s scientific collaborations with leading authorities worldwide across multiple fields, including Nobel Prize winning pathologist Sir Howard Florey and biochemist Sir Hans Adolf Krebs.
“As I have observed through my own research experiences, diverse collaborations enrich perspectives and help maximise the scope and impact of scientific discoveries,” she concluded.
“Visual science is increasingly a global team sport, or in the words of Ida, ‘We use research in order to answer the age-old question: what makes you get what you get, when you get it, and why?’. And nothing could be more rewarding than that.”