


Ria
Rita
Andre
Yiping




Ria
Rita
Andre
Yiping
As this report discusses, critical barriers to health access and equity exist in New Mexico, due to the lack of trust, staggering health disparities, and inadequate service delivery in indigenous communities. We recognize that the relationship between government entities and indigenous communities is complex and painful, with a long history of broken promises and mistrust. We specifically want to recognize this harsh reality in the context of Princeton University’s role in the Manhattan Project, which produced the world’s first nuclear weapons during the Second World War.
At the time, the U.S. government recruited talented scientists in institutions of higher learning throughout the country, and professors from Princeton University in physics and chemistry joined the project as consultants.1 Members of the Navajo Nation and the Southwest Pueblos in New Mexico were displaced from their lands for the creation of what became the Los Alamos National Laboratory and for uranium mining needed during the project.2
After the Trinity Test which marked the first detonation of an atomic bomb, people in the State of New Mexico who were exposed to the radiation fallout experienced health issues as a result of exposure and contamination. As we studied health inequities that persist among indigenous communities in New Mexico as part of our evaluation of the Native American Premium Assistance Program (NAPA), we acknowledge that both the effects of nuclear testing and the efforts of the project itself have led to environmental and health impacts in the area. This history of nuclear tests may have furthered health inequities and overall mistrust among indigenous communities.
“We recognize that the relationship between government entities and indig enous communities is complex and painful, with a long history of broken promises and mistrust.
We wish to clarify that this statement does not reflect the views of Princeton University, the Princeton School of Public and International Affairs, Princeton University staff or administrators, or the State of New Mexico, and are the collective opinion of the nine students who co-authored this report.
Respectfully,
Mary Grace Darmody
Ria Hanson
Laura Hausman
Rita Fernandez
Andre Jimenez
Yiping Li
Raj Mukherji
Brontë Nevins
Gillian Tisdale
This report was prepared by graduate students at Princeton’s School of Public and International Affairs. The report incorporates research, data analysis, and insights from interviews, most of which were conducted in New Mexico from October 16 – October 20, 2023. We are grateful to New Mexico’s Office of the Superintendent of Insurance for the opportunity to collaborate on this project.
This report fulfills Princeton’s graduate requirements for the Master in Public Affairs degree, which requires that all students conduct research and produce an actionable policy proposal for a client. We wish to express our gratitude to our instructors Heather Howard and Dan Meuse, who were so generous with their time, insights, and experience throughout the course of this project. We also wish to thank the many topic experts and contacts in New Mexico who shared their valuable perspectives with us as we created this report.
Secretary Kari Armijo, Cabinet Secretary, Human Services Department
Nick Autio, General Counsel, New Mexico Medical Society
Colin Baillio, Deputy Superintendent of Insurance, New Mexico Office of the Superintendent of Insurance
Sara Bencic, Colorado Option Director, Colorado Department of Regulatory Agencies
Tom Betlach, former Arizona Medicaid Director
Nathan Bush, Director of Government Relations, The University of New Mexico
Cynthia Cisneros, Public Outreach Coordinator, New Mexico Office of the Superintendent of Insurance
Troy Clark, Chief Executive Officer, NM Hospital Association
Nick Cordova, Healthcare Director, New Mexico Center on Law and Poverty
Brent Earnest, Chief Operating Officer, beWellnm
RubyAnn Esquibel, University of New Mexico Health System
Bruce Gilbert, Chief Executive Officer, beWellnm
Sahar Hassanin, Economist, New Mexico Office of the Superintendent of Insurance
Bill Jordan, Interim Co-Director and Government Relations Officer, New Mexico Voices for Children
Annie Jung, Executive Director, New Mexico Medical Society
Loreli Kellogg, Acting Medicaid Director, New Mexico Human Services Department
Pamela Kirby Blackwell, Director of Government Relations and Communications, NM Hospital Association
Jessica Lopez Collins, New Mexico Program Director, Forward Together
Juliette McCoy Program Manager of Population Health, Presbyterian Healthcare Services
Carrie Robin Brunder, Chief Lobbyist, New Mexico Medical Society
Chrissy Robinson, Program Coordinator, New Mexico Office of the Superintendent of Insurance
Maria Rodriguez, Health Equity & Outreach Specialist, Colorado Department of Regulatory Agencies
Javier Rojo, Senior Research and Policy Analyst, New Mexico Voices for Children
Julia Ruetten, Director of Government Regulation and Reimbursement Policy, NM Hospital Association
Alex Sanchez, Director of Communications, beWellnm
Divya Shiv, Research and Policy Analyst, New Mexico Voices for Children
Jacqueline Smith, Director of Public Policy and Government Relations, Presbyterian Healthcare Services
Rep. Reena Szczepanski, Majority Whip, New Mexico House of Representatives
Barbara Webber, Executive Director, Health Action New Mexico

This report was prepared for New Mexico’s Office of the Superintendent of Insurance (OSI) as the state seeks to boost health insurance coverage and make transformational investments in access to high-quality, affordable health care. New Mexico’s efforts come at a critical juncture; the impacts of COVID-19 and the Medicaid “unwinding” process have exacerbated issues in the health landscape for providers and patients alike. At the request of OSI, this report evaluates:
1. Health access and cost issues in New Mexico (based on available literature, stakeholder interviews, and OSI survey data) and pathways to address these issues
2. The health equity impact of various policy initiatives and recommendations for future implementation, including:3
a. The Native American Premium Assistance program (NAPA)
b. The Coverage Expansion Plan (CEP)
c. Medicaid Forward, and
3. Policies that OSI could adopt to address provider shortage issues in New Mexico.
New Mexico’s health care landscape presents several overarching challenges for coverage and health access. First, the state is among the most rural in the nation; ensuring provider access in sparsely populated areas remains a key challenge. Second, high premiums and out-of-pocket costs can make plans on New Mexico’s exchange, beWellnm, unaffordable for many who do not qualify for Medicaid due to income thresholds or immigration status. Additionally, indigenous and undocumented communities in New Mexico face unique barriers to access. Uptake of Medicaid and marketplace plans (which are often required to supplement care at Indian Health Service facilities) has been low in indigenous communities, due to historic mistrust and barriers to ongoing outreach. Undocumented residents, meanwhile, cannot access care on either Medicaid or New Mexico’s marketplace; care is only available via the New Mexico Medical Insurance Pool (NMMIP) and private markets, both of which can be unaffordable.
The state has implemented and proposed various ideas to address these issues and improve health access. This report focuses specifically on NAPA, CEP, and Medicaid Forward, before discussing ways to approach New Mexico’s provider shortage. Insights and recommendations related to these proposals are based on data analysis, literature reviews, and stakeholder interviews with advocates, legislators, state officials, providers, and carriers.
NAPA aims to enhance the affordability of marketplace plans for indigenous New Mexicans by offering zero-dollar premiums for individuals below 300% of the federal poverty level (FPL) and reduced premiums for those earning below 400% FPL. This supplement to the Indian Health Service (IHS) is critical, as it provides access to care beyond what the IHS can offer, particularly for indigenous New Mexicans living or commuting outside of reservation territory. Despite its potential, NAPA has seen limited enrollment during initial implementation. At the time of writing, approximately 1,000 indigenous New Mexicans participated, a small fraction of the state’s indigenous population. Language barriers, limited outreach, and a pervasive distrust in government programs among indigenous communities all limit enrollment.
A strategic shift in outreach and implementation can improve NAPA’s effectiveness. Opportunities exist to prioritize relationship-building with tribal communities and to leverage existing community programs that have already built trust with pueblos. The state should clearly communicate the specific benefits of NAPA, especially in relation to the services provided by (and limitations of) IHS. Furthermore, ensuring the continuity of NAPA’s funding will be vital to improving access and fostering trust with indigenous communities over time.
CEP is a key initiative to cover uninsured individuals who do not have access to other, affordable coverage options, most likely due to immigration status. The plan targets residents earning up to 200% FPL and similar to New Mexico’s Medicaid program, will cover essential health benefits. Individuals with incomes up to 138% FPL will not pay a deductible or premium, whereas individuals with incomes between 138-200% FPL will pay a modest deductible.
CEP is expected to attract between 6,250 and 12,000 new enrollees in its first year, assuming 25-40% of eligible individuals enroll. Effective outreach and enrollment processes are critical to the success of CEP. New Mexico should collaborate with beWellnm to integrate enrollment, conduct outreach and education with communities, and provide robust customer support and language access resources. Successful implementation hinges on managing administrative burden, ensuring sustainable funding, and conducting comprehensive stakeholder engagement. If optimally implemented, CEP could meaningfully reduce uninsurance in New Mexico, improving overall health equity in the state.
Medicaid Forward has been proposed by lawmakers to expand health access and reduce uninsurance in New Mexico. The program would raise the current income cutoff for Medicaid eligibility (138% FPL) and could cover New Mexicans with incomes up to 400% FPL or more. Medicaid Forward would also be available to all residents, regardless of their immigration status. Early estimates from the Urban Institute suggest that Medicaid Forward could reduce the state’s uninsurance rate from 13.1% to approximately 5.75% and is anticipated to enhance the member experience by reducing insurance churn and offering stable, reliable coverage.
The legislature passed HB 400 in 2023, which commissioned a study to assess the potential impacts of Medicaid Forward. This study will likely address different implementation strategies, necessary adjustments in provider reimbursement, funding sources, and coverage eligibility. Successful implementation of Medicaid Forward could make New Mexico’s health care system more equitable and could significantly benefit residents who have been excluded from public coverage under current parameters. For the effective implementation of Medicaid Forward, several key considerations have been highlighted. These include ensuring sustainable funding, careful consideration of impacts on existing providers and provider networks and insurers, and taking care to avoid unintended consequences. The report also recommends continuous evaluation and adjustment of the program to meet evolving health care needs and to navigate the dynamic federal regulatory environment.
Provider scarcity is a critical issue in New Mexico, particularly in rural and underserved areas, as discussed in the Health Access subsection of the report. Although shortages exist across the entire health care system, provider scarcity is particularly acute in primary care and mental health services. Provider scarcity negatively impacts health access and quality for all of New Mexico’s residents, and exacerbates health disparities among rural, indigenous, and low-income communities. The rural nature of New Mexico, combined with socioeconomic challenges and gaps in broadband coverage (which impede telehealth delivery) all pose challenges to provider access.
The report discusses a series of policy recommendations to address provider shortages. Shortterm solutions include increasing reimbursement rates, addressing medical malpractice premiums, and streamlining credentialing processes for providers entering the state. Other solutions could include creating a limited license process for foreign-trained physicians; expanding graduate medical education (GME) and residency programs, particularly in underserved specialties and areas; and enhancing post-residency retention through incentives such as enhanced loan forgiveness. Implementing these strategies will require collaboration among policymakers, medical schools, and health care organizations, to address the growing urgency of ensuring access to providers for New Mexico’s residents.





As New Mexico emerges from COVID-19, the state is making a concerted effort to advance equal access to high-quality, affordable health care. Several initiatives that address health access and affordability are at different stages of discussion and implementation, including NAPA, CEP, and Medicaid Forward. To be effective, these initiatives require buy-in from a broad array of stakeholders, including legislators, advocacy organizations, providers and carriers, and the state agencies charged with implementation.
As discussed, this report 1) analyzes the current landscape of health access and affordability in New Mexico 2) evaluates the health equity impacts of NAPA, CEP, and Medicaid Forward, and 3) makes recommendations to address New Mexico’s provider shortage. Recommendations related to these topics are informed by data provided by OSI, independent research based on available literature, and conversations with stakeholders across New Mexico’s health care ecosystem. The perspectives of legislators, state agencies, providers, carriers, and health advocates all informed this report. Additionally, we conducted interviews with health care policymakers from neighboring states (Colorado and Arizona) to learn from their experiences.
Health equity, access, and affordability are critical themes that emerge repeatedly throughout this report. Accordingly, the following background section defines these concepts and applies them to the unique health care environment in New Mexico.
“Gun violence is a public health issue. Poverty is a public health issue. Environmental consequences from energy is a [sic] public health issue. [...] All of these disenfranchised populations, all of the equity barriers, are all public health issues. And when we address those, our economy is better, our families are stronger, our risks are fewer.” - Govenor Michelle Lujan Grisham5
According to the New Mexico Office of Health Equity, health equity is achieved when people of all identities, backgrounds, and geographic locations have the same opportunity to be as healthy as possible.6
Health equity is the goal; health disparities are how we measure it. Disparities are avoidable, unjust differences between health outcomes, and inequities are their underlying causes.7 Although disparities may arise in the health care system based on differences in access to and affordability of care, they also arise upstream, resulting from structural inequities embedded in previous and ongoing policies. These disparities manifest in inequitable opportunities for nutrition, public safety, housing, education, and employment. As Governor Lujan Grisham states in the quote above, health impacts all aspects of life, and myriad social and economic conditions impact health.
We believe that OSI is well-positioned to address some factors that impact health equity –specifically, disparities in health care access and affordability. Accordingly, this report focuses on how OSI can advance access and affordability for a selection of underserved populations: indigenous communities, uninsured individuals who do not have access to other coverage options, and lower-income families. The following sections illustrate the different experiences of access and affordability faced by these communities, and proposes policy solutions to close these gaps.
New Mexico is home to a diverse population of residents. According to the United States Census Bureau, the state’s population was approximately 2,117,522 as of July 2022. Among New Mexicans, 50.2% of the population identifies as Hispanic or Latino, 11.2% as Native American or Alaskan Native, 35.7% as White alone, 2.7% as Black or African American alone, 2.0% as Asian alone, and 0.02% as Native Hawaiian or other Pacific Islander.8 As will be discussed, New Mexico is predominantly rural, and many of the state’s residents are geographically dispersed.
Twenty-three tribes and Pueblos are located in New Mexico, including several Apache tribes and the Navajo Nation. These indigenous communities comprise slightly over 11% of the state population, per the U.S. Census.9 It should be noted, however, that there was an undercount of indigenous individuals living in reservations during the 2020 Census.10
In 2021, New Mexico’s median household income was $54,020; per capita income, however, was $29,624 in the same year. New Mexico’s median household income was substantially lower than the national median real household income ($74,580 in 2022)11. Although approximately 17.6% of the state’s population lives below the poverty line, New Mexico’s unemployment rate was 3.7% in September 2023, slightly lower than the national rate as of October 2023.12
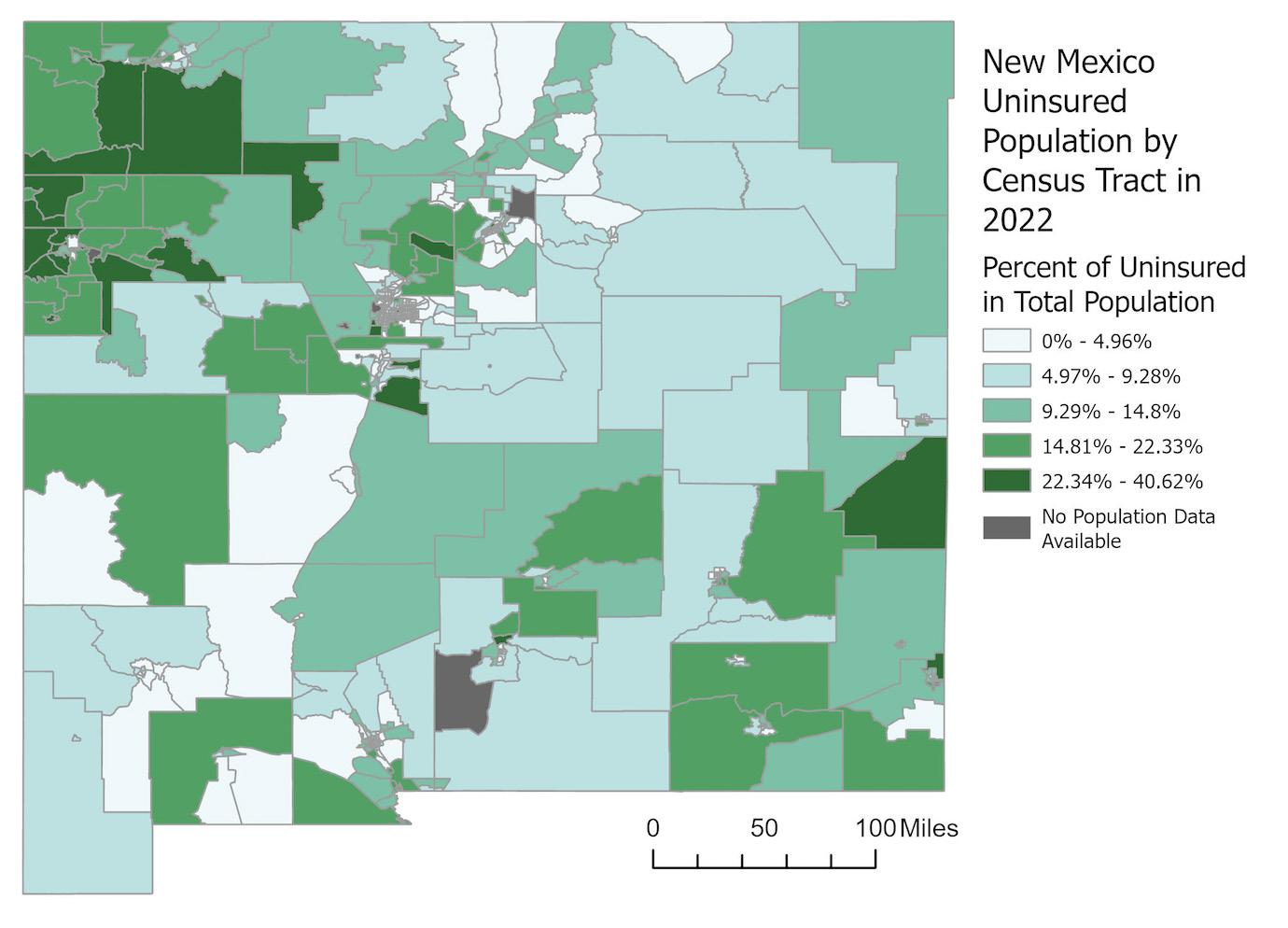
New Mexico has made significant progress in insuring the state’s population since the ACA was enacted in 2010. Nevertheless, approximately 10% of the state’s population remains uninsured.13 New Mexicans who are insured rely on a mix of coverage. In 2022, 36% of New Mexicans obtained coverage through their employers, 33.5% through Medicaid, 15.8% through Medicare, and 3.2% through the military.14
Rural Communities
New Mexico is the nation’s fifth-largest state by land area, but fifth-smallest state in terms of population.15, 16 With roughly 2,100,000 residents, New Mexico ranks 46th in population density. The combination of an expansive geographic area and a relatively diffuse distribution of residents presents formidable challenges in providing equal access to affordable and highquality health care. The New Mexico Department of Health’s Indicator-Based Information System (IBIS) defines 26 of New Mexico’s 33 counties as non-urban.17 Roughly one third of the state’s population resides in these rural or frontier areas.18
Rural and frontier areas are underserved in many ways. Critically, of the nearly 25% of New Mexican households which lack reliable internet access, a disproportionately large share reside in rural and frontier areas. This inhibits access to medical care, as digital access is critical to enrolling in health insurance, booking medical appointments, and accessing any form of telehealth services. Nearly 60% of McKinley County residents, for example, do not have broadband access.19 Some rural and frontier areas that are designated as tribal lands, furthermore, lack basic and essential services, including running water.20
Finally, rural and frontier areas suffer from a dire shortage of providers. The Health Resources and Service Administration uses the term “Healthcare Provider Shortage Areas” (HPSAs) to identify areas with a shortage of primary, dental or mental health care providers. HPSAs can be geographic areas, populations, or facilities.21
There are three types of geographic and population HPSAs for primary care: whole county, sub-county, and low-income population (the population of a county or sub-county that is below 200% FPL). All of New Mexico’s 14 Small Town Rural counties are whole-county primary care HPSAs. Of New Mexico’s 14 Large Town Rural counties, five are whole-county HPSAs and seven whole counties have a low-income population designation. By contrast, only one of New Mexico’s three Small Metro Counties has a whole-county primary care HPSA.22, 23
Source: U.S. Census Bureau
Source: HRSA, U.S. Census


Compared to urban areas, rural regions have higher poverty rates, higher unemployment, and greater uninsurance.24 These deep disparities affect every corner and chapter of life. Rural regions have a lower life expectancy, more years of life lost to premature death before age 75, and disability rates that are over 20% higher than those in urban areas. Rural areas also have a 50% higher adolescent birth rate, a higher rate of preterm births, and a lower rate of births with first trimester prenatal care.25
The health disparities experienced by indigenous people stem from “the negative impacts of colonization.”26 Tribes have endured forced assimilation, removal from tribal homelands, and relocation to reservation lands. This history has contributed to an environment of distrust between indigenous communities and
the state of New Mexico, which makes it challenging to promote enrollment in services such as Medicaid and the beWellnm marketplace.
One direct threat to health is inadequate access to health care providers, due in large part to the continued underfunding of IHS. In 2018, IHS had a 30% vacancy rate across all providers for the Albuquerque and Navajo regions, with a 45-52% vacancy rate for physicians.27 Another ongoing threat is the lack of access to culturally competent care, as accessing non-indigenous providers may create linguistic barriers to obtaining high-quality care and many communities look to tribal healing in a manner that is integrated with Western medicine.
A significant portion of uninsured individuals who lack access to alternative coverage options in New Mexico are believed to be undocumented residents; these individuals may encounter distinct barriers to health access. Under federal law, undocumented residents are ineligible for traditional Medicaid regardless of income; Medicaid is restricted to U.S. citizens or certain qualified non-citizens, such as lawful permanent residents outside of the five-year bar, discussed below.28 Undocumented residents also cannot obtain coverage on the marketplace and do not qualify for federal subsidies.
More broadly, undocumented residents face legal barriers to accessing federal public benefits under the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) of 1996.29 This law established strict eligibility criteria for immigrants seeking public assistance and it bars undocumented immigrants from most federally-funded public benefits.
The five-year bar applies to documented immigrants who became ‘qualified immigrants’ within the last five years. Immigrants in the five-year bar are ineligible for federal meanstested programs, including Medicaid, CHIP, SSI, and SNAP. Individuals subject to the fiveyear bar, however, are eligible to purchase coverage on the marketplace; the Affordable Care Act’s marketplaces extend coverage to most lawfully present noncitizens. A special rule exists that permits immigrants with incomes below 100% FPL to access subsidized marketplace coverage, which is often needed in cases where immigration status renders individuals ineligible for Medicaid.30
Furthermore, the risk of becoming a “public charge” – meaning an individual who is likely to become primarily dependent on the government for subsistence – is a potential deterrent to undocumented immigrants accessing public benefits. In 2019, President Trump’s administration issued a Public Charge Rule that expanded the criteria for determining whether an immigrant applying for a visa or seeking adjustment of status (such as obtaining a green card) would be considered a “public charge.” Although this rule was struck down in several courts and removed from the federal register in 2021, this rule change has had a chilling effect on the immigrant community, further increasing the barriers to obtaining health care coverage.31 Undocumented immigrants and mixed-status families (who have individual family members that are undocumented) can be reluctant to seek services they are eligible for, out of fear that they will be identified to the federal government or could face penalties for using public benefits.
The result of this policy environment is that affordable health insurance is often inaccessible for most undocumented New Mexicans. Undocumented immigrants have the option of purchasing coverage via NMMIP or pursuing private options, which are expensive and have their own barriers to access. These barriers to insurance access create profound health disparities, as they deter individuals from seeking maintenance medication and preventative services. We heard
from stakeholders in New Mexico that undocumented individuals often only seek emergency care, resulting in higher rates of disability and health disparities.
Health affordability includes a variety of costs that increase the price of accessing health care services. Costs related to insurance (premiums, deductibles), out-of-pocket costs charged by health care facilities (copayments and coinsurance), time off from work, and transit all impact health affordability.32 These different costs accrued in accessing health services, therefore, are important factors to consider for all New Mexicans.
Health affordability is a pressing challenge in New Mexico, where 17.8% of the state’s population lived at or below the federal poverty level in 2022.33 Among the fifty states, only Louisiana and Mississippi reported higher proportions of individuals at or below the federal poverty level. Public health insurance provides a critical safety net for low-income New Mexicans; 51.2% of the state’s population relied on public coverage in 2022, the highest proportion in the nation.34
For New Mexicans with incomes too high to qualify for Medicaid, premiums and out-ofpocket costs may be unaffordable. Although the 2021 American Rescue Plan Act included financial assistance to make marketplace coverage more affordable, these enhanced subsidies are scheduled to expire after 2025, which would raise the cost of insurance for many.35 Even with this assistance, 56% of respondents in a 2022 survey reported foregoing medical care in the past two years due to cost.36 When New Mexicans do seek medical care, the ensuing bills are often prohibitive. The Consumer Financial Protection Bureau reported that ~18% of New Mexicans had medical debt in 2022.37 This debt summed to approximately $881 million, or $2,692 per individual, creating a substantial financial burden on the state’s residents.
Indigenous people have treaty rights to health care from the US federal government, which is primarily supplied via IHS.38 Despite this, the underfunding of IHS leads to significant medical debt for indigenous individuals. Limited success in insuring the indigenous community through Medicaid and the beWellnm marketplace exacerbates cost barriers by putting more financial strain on IHS, which would otherwise be reimbursed by Medicaid and private payers. Furthermore, some indigenous individuals are unable to access care at IHS facilities due to geographic distance or service availability. The consensus from the stakeholders we interviewed is that more effective outreach is required to enroll indigenous communities into marketplace plans. Even then, plans may still straddle indigenous people with considerable costs associated with deductibles, coinsurance, and copays, leaving them vulnerable to acquiring medical debt.
Among uninsured individuals without access to other coverage options, undocumented residents are prohibited from enrolling in Medicaid or obtaining coverage through the beWellnm marketplace. This lack of access to coverage leads to high medical debt for these residents and increased uncompensated care expenditure for hospitals and providers.
Those who do not qualify for Medicaid due to their immigration status are eligible for Emergency Medicaid Services for Aliens (EMSA).39 EMSA provides coverage for emergency medical care, encompassing services such as labor and delivery. EMSA may not entirely cover emergency medical expenses, and many individuals depend on charity care from hospitals to avoid medical debt. NMMIP was originally created in the late 1980s to cover the “uninsurable” population.40 While the Affordable Care Act (ACA) has now made it possible for individuals who were previously uninsurable to obtain coverage, undocumented immigrants, excluded from the ACA’s options, are still able to seek coverage through NMMIP.
This form of coverage is notably expensive; accordingly, NMMIP offers a Low Income Premium Program (LIPP) program that provides a premium reduction of 25%, 50%, or 75% depending on the applicant’s annual income.
Given the existing landscape of health access and affordability in New Mexico, the state government and legislature have proposed several programs to address these issues. NAPA, CEP, and Medicaid Forward are in various stages of implementation and are discussed below as elements of New Mexico’s health policy landscape.
Under NAPA, indigenous people who are members of a federally recognized tribe are eligible for either a zero-premium plan on the marketplace (for those earning up to 300% FPL) or a reduced premium plan (for incomes between 300 and 400% FPL). As of 2023, 300% FPL is $40,770 for an individual, $54,930 for a couple, or $83,250 for a family of four.41 Concurrent with the introduction of NAPA, there has been a doubling of health insurance enrollment on the beWellnm marketplace, from 500 to 1,000. While this may not be fully attributable to NAPA, recent action does seem to be increasing indigenous enrollment.42 While the increase in uptake was a promising development, estimates show that 90% of indigenous New Mexicans eligible for premium assistance remain without coverage.43
Utilizing resources from the New Mexico Health Care Affordability Fund (HCAF), OSI has proposed establishing a collaborative initiative with NMMIP to introduce CEP. This plan aims to mitigate affordability and access challenges currently experienced by uninsured New Mexicans and low-income NMMIP enrollees without access to other coverage options. Under OSI’s proposal, individuals may qualify for CEP if they:
• Reside in the State of New Mexico and earn up to 200% FPL.
• Lack access to Medicaid, Medicare, beWellnm, or employer-sponsored insurance (ESI).
• Are either uninsured or enrolled in LIPP-75%.44
CEP will mirror the state’s Medicaid program and will encompass the ten essential health benefits, with HSD continuing to cover services eligible for federal matching dollars under Emergency Medicaid. Premiums and out-of-pocket costs will be income-dependent, with Plan A catering to individuals with incomes up to 138% FPL and will closely resemble beWellnm’s Turquoise 1 Plan (99.2% actuarial value) which includes a $0 deductible. Plan B covers those with incomes between 138-200% FPL, mirrors beWellnm’s Turquoise 2 Plan (95.1% actuarial value) and offers a $100 deductible.45
The ACA requires non-grandfathered health plans in the individual and small group markets to cover essential health benefits, which includes the following ten benefit categories: (1) ambulatory patient services; (2) emergency services; (3) hospitalization; (4) maternity and newborn care; (5) mental health and substance use disorder services including behavioral health treatment; (6) prescription drugs; (7) rehabilitative and habilitative services and devices; (8) laboratory services; (9) preventative and wellness services and chronic disease management; and (10) pediatric services, including oral and vision care.
Drawing from comparable programs in other states, data indicate that enrollment typically ranges from between 25-40% of eligible individuals. According to modeling commissioned by OSI, CEP could potentially attract between 6,250 and 12,000 new enrollees in the first year, assuming take-up rates fall within the 25-40% range.
New Mexico is considering expanding the availability of publicly-run coverage to more residents through Medicaid Forward. Medicaid Forward, a legislative proposal that is currently under study, would provide residents above the current cutoff of 138% FPL with the option to buy into the state’s existing Medicaid program. Residents earning above 150% FPL would likely pay modest premiums and other cost-sharing requirements. Washington, DC has implemented a similar program up to 210% FPL;46 New Mexico’s proposed program, on the other hand, may raise the limit to 400% FPL or more.47
The Urban Institute estimates that this program would reduce the uninsurance rate from 13.1% to approximately 5.75%.48 It has the potential to improve member experience by eliminating churn and providing New Mexicans with a stable, reliable source of coverage, regardless of income or employment status. Critically, it would also be available to all residents regardless of immigration status.
In early 2023, the legislature passed HB 400, which tasked the Secretary of Human Services with studying the impacts of Medicaid Forward.49 This study will suggest detailed implementation and operational plans, necessary provider reimbursement changes, funding sources, and coverage eligibility. These findings are due in October 2024 and will inform the future of Medicaid Forward.
The policies above are part of a complex existing policy landscape. While the policies below are not the focus of this report, they interact with the proposed solutions and are important to understand when analyzing how the proposed policies will impact health equity.
HCAF was created in 2021 to serve the needs of underinsured New Mexicans.50 This fund collects $165 million each year using a state version of a recently expired federal fee on insurers.51
Currently, HCAF has three components:52
1. NAPA guarantees the availability of $0 premium plans for up to 200% FPL and lowers premiums for those between 200-400% FPL.53 This is one of the policies examined in the report.
2. The Native American Affordability Fund completely buys down the premiums for those <300% FPL and reduces premiums for those within 300-400% FPL.
3. The State Out of Pocket Assistance Program makes utilizing coverage on Tur quoise Plans more affordable by reducing cost-sharing and improving behavior al health coverage.54, 55 Although these plans significantly reduce the amount of out-of-pocket costs, they do not necessarily ensure affordable coverage or elimi nate the possibility of medical debt.
HCAF builds on the premium subsidies and marketplace structure that the ACA created to establish more affordable coverage for low-income and indigenous groups.
Initially authorized in 2013,56 New Mexico’s marketplace, beWellnm, officially launched in 2021 for 2022 plan year enrollment, transitioning fully from the federal marketplace.57 BeWellnm is a source of affordable coverage for over 40,000 enrollees,58 most of whom do not receive ESI but are not eligible for Medicaid. Marketplace coverage is particularly important due to the comparatively low rate of ESI in New Mexico.
New Mexico’s Medicaid program, called Centennial Care or, as of 2024, Turquoise Care, is a pillar of health coverage in the state.59 New Mexico has the highest proportion of its population enrolled in Medicaid among all states60 and was among the first wave of states that expanded Medicaid in 2014.61 According to survey results from 2022, residents hold Centennial Care in high regard, with 67% saying it is a high-quality, trusted program.62 It is centrally administered by HSD, which contracts with four Managed Care Organizations (MCOs) to provide health benefits.63 The overwhelmingly positive perception of the state’s Medicaid program would provide a strong foundation for Medicaid Forward’s image, if the proposal were to proceed.
During the public health emergency (PHE) resulting from the COVID-19 pandemic, a condition of receiving federal relief dollars was that states could not disenroll individuals from Medicaid except under very limited circumstances. The Consolidated Appropriations Act, 2022 ended this continuous coverage requirement as of April 1, 2023 At that point, states began the process of “Medicaid unwinding,” or disenrolling people from the program who were no longer eligible.
Medicaid unwinding has been a challenging process across the country. Stakeholders in New Mexico mentioned staffing constraints in the Human Services Department (HSD), which is facing an estimated 40% vacancy rate, as a challenge to keeping up with the workload and avoiding procedural disenrollment.
Procedural disenrollment occurs when someone is removed from Medicaid for administrative reasons, such as outdated contact information or failing to respond to re-enrollment paperwork. Individuals who are procedurally disenrolled may still be eligible for the program.
Programmatic disenrollment occurs when someone is no longer eligible for Medicaid due to income or health status changes.
As of November 2023, 96% of people disenrolled from Medicaid in New Mexico had been removed for procedural reasons.64 Of the more than 60,000 disenrolled by July 2023,65 30,000 procedurally disenrolled people have re-enrolled in Medicaid coverage. People who no longer qualify for Medicaid should be shown a zero-dollar premium plan, for which the majority are eligible. Although beWellnm is notified when people are disenrolled from Medicaid in the unwinding process or otherwise, only a small portion sign up for marketplace coverage. Transitioning those disenrolled from Medicaid to marketplace plans is a problem nationwide, with states struggling to reach newly uninsured families about their options. Those who do not sign up for Medicaid or a marketplace plan frequently remain uninsured.
As of the writing of this report, New Mexico is currently seeking a five-year 1115 Medicaid waiver (under the name “Turquoise Care”) that would add several new programs, including continuous eligibility for children under six, expanded access to home-visiting and supportive housing, Medicaid for high-need (serious mental illness, substance use disorder, or intellectual disability) justice-involved people 30 days before release, traditional healing benefits for Native Americans, and home-delivered meals.66
The continuous eligibility provision means that no form of recertification would be required to children under six. As New Mexico has a particularly high procedural disenrollment rate from Medicaid, the continuous eligibility provision would prevent detrimental, early-life disruptions in coverage due to missing paperwork.67
In terms of traditional healing, Native Americans with Medicaid and a nursing facility level-of-care need may currently receive up to $2,000 of annual culturally-appropriate therapies, including dance, song, plant medicines, participation in sweat lodges, or other care provided by a community-recognized healer.68 The new waiver would provide $2,500 of traditional healing to all Native American Medicaid members.69
Through Section 1115 of the Social Security Act, the Secretary of Health and Human Services can approve budget-neutral demonstration programs to assess improved ways of serving Medicaid patients.70 Savings from one aspect of the demonstration can be used to fund another component.71
As discussed, a unique component of New Mexico’s care infrastructure is its highrisk pool, founded in 1987 to cover ‘uninsurable’ populations.72 Uninsurable people, historically, were those with preexisting conditions. Although individuals with preexisting conditions are now insurable thanks to the ACA, the high-risk pool is still used to cover undocumented immigrants, who are left out of the ACA’s options.
74
73 It is an expensive form of coverage and some of the policies discussed below cover similar populations to those currently on NMMIP plans with more affordable options.
IHS is another critical component of care in New Mexico. IHS provides care at its facilities75 but a Purchase/Referred Care agreement is necessary for those traveling or seeking specialized care that is unavailable at IHS facilities.76 This lack of comprehensive coverage can be a barrier for indigenous people in accessing care.77 The Tribal Budget Formulation Work Group estimates that IHS would need a 700% budget increase over its 2022 budget to provide perfectly comprehensive health care to indigenous people of New Mexico.78 The Urban Indian Health Centers, which are designed to care for indigenous New Mexicans in metropolitan areas outside of tribal land, are similarly chronically underfunded (1% of IHS funding goes to these centers).
Additionally, Forward Together found in a survey that over a third of indigenous New Mexicans are uncomfortable receiving care at an IHS facility, primarily due to challenges obtaining an appointment and poor quality of care.79 According to Dr. Lucero (Zia Pueblo Tribe), the high turnover rate at IHS facilities leads to additional issues as there is no consistency in providers over time. Accordingly, “The concern is more than just having a provider who knows you; it is also about having a provider who understands your community, culture and beliefs.”80 This high turnover rate also undermines efforts to train providers in even basic cultural competency, exacerbating challenges around building trust in the health care system.
Sample
Between September to November 2023, the authors of this report conducted 15 interviews. Two interviews were with government agencies from neighboring states that have experience with similar policies to those New Mexico is considering. The remaining 13 interviews were with representatives from government agencies, advocacy groups, providers, and carriers in New Mexico.
The faculty advisors, Heather Howard and Dan Meuse, conducted the initial outreach to all interviewees. The authors of the report met with each group for 30 to 60 minutes in-person or over Zoom. The authors informed all interviewees that the notetaking was for factual information, not for attribution. The authors went back and obtained permission for all attributions made throughout the report during the writing process.
In addition to insights from the interviews, the report also analyzed administrative data and incorporated a review of academic and professional literature.
Approach
This report examines the three programs requested by OSI (NAPA, CEP, and Medicaid Forward) and evaluates their potential for closing health disparities and achieving health equity in New Mexico. The report also examines the provider shortage issue in New Mexico and makes recommendations to increase provider availability. Each section of the report proceeds in the following manner:
• A problem statement that lays out the health equity issues that each proposal seeks to address;
• Background that provides additional context on issues facing the policy in New Mexico and programmatic details;
• Recommendations that identify the opportunities for each policy to maximize its impacts on achieving health equity; and,
• Considerations to keep in mind when implementing the policy as is or any recommendations proposed by the authors of this report.
Evaluative Criteria
For each of the three policies and the provider shortage issue, the authors sought to address the following questions that fit into two broad categories:
1. Health Equity
a. How does the program promote coverage access?
b. How does the program enhance affordability for its consumers?
c. How does the program address the provider shortage issue in New Mexico?
d. Is the community involved in the design of the program?
2. Implementation
a. What is the administrative burden on the state?
b. What is the financial impact of the program? Is it cost-effective?
c. What is the political feasibility of the program to receive continued funding or to become a reality?
d. How might the program be impacted by the dynamic federal environment? How reliant is it on federal funding sources and authorizations?
One limitation of this report is the lack of representation of indigenous communities in New Mexico among the interviewees. The faculty advisors contacted one Pueblo based on recommendations from New Mexico state officials, but were unsuccessful in setting up a meeting. The authors sincerely regret the lack of inclusion of the lived experiences of indigenous communities in New Mexico and take full responsibility. The authors’ failure to include indigenous voices in this report also speaks to the greater issue of need for trustbuilding with these communities given the history of the United States. Trust is a challenging word…because there has been such a long history of broken promises. - Tom Betlach, former Arizona Medicaid Director, when asked about how Arizona approaches conducting outreach to indigenous communities
The report therefore only is limited to discussions of the observable experience of indigenous communities interacting with the health care system in New Mexico and commentary from advocates working on issues related to indigenous experiences. Furthermore, this report focuses on the interactions on indigenous individuals with the health care system administered by the New Mexico state government, rather than a comprehensive overview of their interaction with IHS or tribal health providers and state-based health care. The report does not seek to present a whole picture but rather focuses its attention on aspects of health inequities that can be addressed from the lens of the three programs examined and the provider shortage issue.
““Trust is a challenging word... because there has been such a long history of broken promises.” — Tom Betlach81


Problem Statement
As of 2019, the indigenous peoples of New Mexico had the highest uninsurance rate of all racial and ethnic groups in the state. Of the 187,000 non-elderly uninsured residents, almost 20% are indigenous. Approximately 75% of uninsured indigenous people earn less than 400% FPL.82 NAPA aims to increase the affordability of health insurance to enrolled tribal members by offering zero-dollar premiums for marketplace plans to indigenous people earning under 300% FPL and reduced premiums for indigenous consumers between 300 to 400% FPL. BeWellnm estimates that the average monthly subsidy through NAPA is $14.92 per month.83
This section provides background information concerning the Native American health insurance and care landscape and discusses relevant policy considerations concerning the efficacy of NAPA in improving health equity.
Indigenous communities in New Mexico experience health disparities due to lack of access to providers, uninsurance and underinsurance, and a combination of poor outreach and historical injustice. Uptake of NAPA remains low, with our fieldwork suggesting that approximately 1,000 indigenous individuals (~0.05% of the entire indigenous population in New Mexico) are currently enrolled in a marketplace plan.84 Our research and fieldwork highlighted four drivers of limited NAPA uptake. First, NAPA does not improve physical access to providers, one of the major challenges facing indigenous people. Second, some individuals who are served by IHS believe that it provides more comprehensive coverage than it actually does.85 Given this, there is little demand for a marketplace plan on top of the coverage they believe IHS provides, thus contributing to low NAPA uptake. Third, nascent outreach around the NAPA program has had low efficacy so far, and has run into pervasive distrust of government-run programs in the target communities. Finally, NAPA alone does not completely solve the issue of affordability for all plans that an individual might choose, as it focuses on the issues of premiums, rather than large medical debt contributors, namely coinsurance and deductibles.
Lack of access to qualified providers is a pervasive problem in New Mexico, even if individuals are insured. The impacts are especially extreme for New Mexico’s indigenous populations, who frequently rely on the underfunded IHS system and live in rural or small towns with significant provider shortages (73% of indigenous New Mexicans live in rural or small towns).86 The NAPA program is intended to address the affordability of health insurance premiums; while it does not directly address this accessibility issue, expansion of insurance coverage is associated with better access to care. According to the 2017-2021 Behavioral Risk Factor Surveillance System Survey (BRFSSS), only 60% of indigenous New Mexicans had a primary care provider, as compared to 70% of all New Mexicans.87
The geographic accessibility challenges that make health care access difficult are exacerbated by chronic underfunding of IHS. Funding constraints mean IHS struggles to fund enough providers across specialties. The Tribal Budget Formulation Work Group estimates that IHS would need a 700% budget increase over its 2022 budget to provide perfectly comprehensive health care to indigenous people in New Mexico.89 This underfunding of IHS leads many indigenous people to postpone care for the next fiscal year, as they are unable to receive care at an IHS facility when IHS has exhausted its budget.90
In addition to the difficulties of simply accessing a primary care provider or relevant specialist, indigenous New Mexicans also face challenges in receiving care from a trustworthy and culturally competent provider. There are only 3,400 indigenous doctors in the entire United States, and only 3% of New Mexico’s mental health providers are indigenous.91 The lack of cultural competence among non-indigenous providers can lead to negligence and harm, including the
Source: NM RGIS, U.S. Bureau
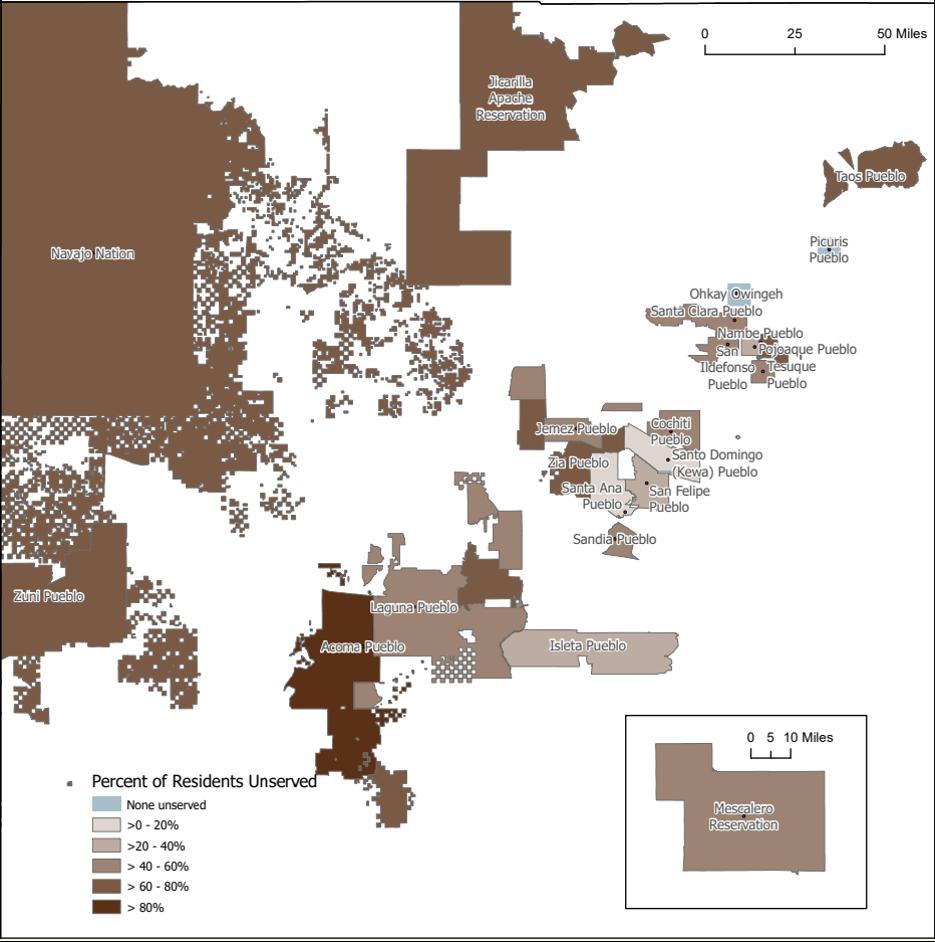
A network analysis conducted in ArcGIS Pro created a 30-minute driving distance service area of medical facilities, FQHCs, and IHS available from RGIS NM. Using the area of land covered and applying the percentage to the population in each tribal land or pueblo, an estimate of individuals living in an area outside of the service area is calculated. Because population density is not taken into consideration, the estimates here are merely suggestive.
2023 death of a Navajo speaker in New Mexico who was not provided an interpreter and whose altered mental state was thus missed by hospital staff.92
Due to these access issues, indigenous New Mexicans have worse outcomes on a number of preventable health indicators, including a 2.6 times higher age-adjusted mortality rate from diabetes and a 3.3 times higher age-adjusted alcohol-related mortality rate.93 While diabetes and alcohol abuse disorder are related to many other facets of colonization, including poverty and loss of traditional lifeways, the high mortality rate implies a failure of health care. In 2020, these inequities meant an indigenous person born in New Mexico could expect to live ten fewer years than the average New Mexican.94
During the COVID-19 pandemic, indigenous communities in New Mexico were particularly hard-hit, with the Navajo Attorney General Doreen N. McPaul stating that “We’ve had some really sad situations where COVID-19 has wiped out almost an entire family.”95 A University of New Mexico Hospital study found that their indigenous patients were more than three times as likely to be severely ill and more than twice as likely to die.96 The study also found that these patients had fewer preexisting conditions than other racial or ethnic groups, and were significantly younger. The authors of the study suggested that a lack of early intervention could be a contributing factor, again highlighting the lethal toll of inadequate health care access.97
In New Mexico, 16.2% of indigenous people are uninsured.98 While IHS provides health care to many indigenous people, the dramatic underfunding of IHS leads to insufficient health care provision for uninsured individuals. IHS primarily provides preventative care (“direct care” at IHS or tribal facilities) and refers people to specialist care through the “Purchased/ Referred Care” (PRC) program, if their tribe has bought into the PRC program.99 For example, the IHS Santa Ana Health Center only provides care for general medicine, diabetes, pediatrics, women’s health, and audiology.100 The diabetes and women’s health clinics take place once per month, and general medicine is provided 2.5 days of the week. For any other kind of care, or more frequent access to care, an individual may need to visit a non-IHS facility. According to Dr. Lucero, underfunding of IHS has led to essentially rationed care, with IHS only willing to pay for “Priority One” (immediate loss of life or limb) PRC reimbursements towards the end of the fiscal year.101 This results in uninsured patients either going without care until their condition becomes life-threatening, or paying out of pocket.
The burden for paying for care outside of IHS facilities frequently falls upon the uninsured individual, according to the IHS website, as all referrals are subject to final determination by IHS before payment.102 In sum, indigenous people are often stuck with the bill if IHS denies the claim or exceeds funding. Due to this high uninsurance rate and lack of adequate IHS funding, the New York Times found that between 2016-2019, indigenous people accumulated over $2 billion in medical debt.103
Since the ACA’s expansion of Medicaid, New Mexico has made significant strides in better insuring indigenous people through Medicaid. Medicaid recipients do not pay a premium, deductible, or coinsurance, and thus face significantly lower cost barriers than uninsured people.104 In addition, Medicaid reimbursement of IHS and tribal providers can provide spillover benefits to indigenous communities and nations by freeing up additional budget space. In 2013, 36.5% of nonelderly indigenous New Mexicans were covered by Medicaid, as compared to 60.2% in 2022.105 Despite this progress, over half (57.8%) of uninsured indigenous people in New Mexico are eligible for Medicaid and not enrolled, suggesting that there are thousands of people who are currently forgoing care or paying out of pocket for care that could otherwise be covered by Medicaid.106
Source: U.S. Census Bureau

Our interviews with key stakeholders and review of the data indicate that beWellnm has a far lower uptake than Medicaid in indigenous communities. In 2019, 37.3% of indigenous people who were eligible for marketplace insurance were uninsured, while the uninsurance rate was half of that (13.2%) for people eligible for Medicaid.107 This highlights the need for more outreach to focus on marketplace options and accessibility. In total, around 11,000 nonMedicaid-eligible indigenous New Mexicans could receive some kind of premium assistance through NAPA. BeWellnm estimated in our conversation that they are currently serving 1,000 indigenous people.108 Thus, we estimate that they are currently serving less than 10% of the eligible indigenous population. Given the relative nascency of the benefit, we expect that beWellnm should be able to continue expanding access to NAPA in the upcoming years.
A major component of uptake when introducing an assistance program is ensuring that the target audience knows the program exists and that it is meant for them. Successful outreach around NAPA must both be extensive and effective, reaching rural communities and clearly communicating the need the program addresses, to promote uptake. Three key barriers to effective outreach emerged from our meetings with stakeholders: language barriers, methods used to reach populations, and a lack of trust.
1. No matter how well-constructed a health care platform, navigating a complicated system full of terminology and nuanced choices is challenging.109 These challenges are exacerbated for indigenous populations because of language barriers, including a lack of support in their native languages.
2. Our conversations also indicated that outreach methods in general were limited. In multiple conversations, online resources and mailing efforts were highlighted as the primary outreach strategies. Many indigenous populations do not have consistent access to broadband which reduces the applicability of online resources. Additionally, lower-income populations tend to move addresses more frequently, making it harder for mailed resources to reach their intended recipient. BeWellnm is making new efforts to increase community engagement, including texting and calling, as well as facilitating outreach through trusted members of communities.110 As these efforts are recent, the outcomes of these strategies are still unknown. However, according to our fieldwork, beWellnm reported that in a recent survey prior to their new outreach efforts, the majority of New Mexicans surveyed were unaware of beWellnm or its outreach efforts. BeWellnm attributes much of this visibility issue to the organization’s previous lack of a year-round community presence.
3. Lastly, there is a pervasive and well-justified distrust of government-run programs among indigenous populations. A history of federally run medical and scientific studies that were conducted in unethical ways on indigenous populations have created a significant culture of mistrust and skepticism that the New Mexican government must now overcome.111 Further negative experiences of indigenous individuals in Western doctor’s offices, from sterilization to discrimination, have also rightfully increased mistrust.112
Out-of-pocket costs may remain high for plans on the marketplace, even with NAPA subsidies that fund zero-dollar or reduced premiums. While NAPA can make higher quality (lower outof-pocket, likely gold or platinum) plans more affordable on a monthly basis, NAPA reduces premiums for any plan that someone selects. The premium assistance provided by NAPA could allow someone to buy a “better” plan that has lower out-of-pocket costs, but out-ofpocket cost-reduction is not a direct benefit of NAPA. An individual would need to have a
thorough understanding of health insurance terms (i.e., what “deductible” means) in order to use the NAPA program to select a plan that actually guarantees affordable care. Thus, without familiarity with health insurance terms or adequate navigation guidance, a chronically ill person may select a plan with high costs that does not effectively reduce the out-of-pocket costs of their continuing care needs. Ideally, beWellnm should consider guiding all NAPA recipients to use their premium assistance to purchase a gold or platinum plan with zero or very low deductibles and no coinsurance.
Given the complexity of choosing a marketplace plan, beWellnm has an opportunity to assist indigenous consumers to use NAPA assistance most effectively. Currently, different marketing materials state both that there is a “zero cost-sharing” plan available to indigenous communities and that plans “can reduce your premiums, copays or deductibles to zero” (emphasis added).113, 114 If indigenous consumers believe that NAPA alone will fully reduce their out-of-pocket burden, they may be less careful to pick a plan that minimizes coinsurance, copays, and deductibles. Marketing materials also state that with marketplace plans, indigenous consumers do not need to pay copays, deductibles, coinsurance at IHS, despite the fact that indigenous people never need to pay these out-of-pocket fees at IHS facilities, regardless of insurance status. BeWellnm should consider unifying the messages about NAPA to best support indigenous communities’ trust and understanding of the marketplace.
We continue our discussion with policy recommendations and limitations for OSI to consider as they continue their work on health equity in New Mexico, and specifically, to increase the uptake and efficacy of NAPA. We note that the following policy considerations may have transferability beyond the NAPA program.
First, we recommend that OSI undertake and support other entities in pursuing a more comprehensive approach to culturally competent outreach in indigenous communities. Personal relationships and trust between insurance providers and Native Americans are important parts of this outreach. We suggest building an outreach strategy that funds deputized members of indigenous communities as outreach agents, utilizes existing relationships between community programs and indigenous communities, and prioritizes relationshipbuilding with tribes.
As part of our research, we spoke to states neighboring New Mexico, including Arizona, that have seen higher rates of health insurance uptake by indigenous people. We sought advice and insight into building trust and open communication channels between indigenous populations and the government. We also studied other states across the United States that have more robust relationships between indigenous peoples and the federal, state and local governments, like Washington and Alaska. Our goal was to understand what has been done differently, and what may be applicable to New Mexico.
1. Use community programs that already have existing relationships with tribes. This allows work to progress rapidly, instead of spending time building new relationships and trust before working on health insurance uptake. Existing relationships and familiar community programs will also add legitimacy to outreach efforts, as it is not the federal government coming in alone, but rather actors who know and care for the indigenous communities, introducing opportunities for better health care.
2. Collaborate with tribal leaders, enabling them to be direct spokespeople for their tribes. In a similar vein, this strategy recognizes the importance of trust and strong relationships in generating uptake. According to Kenneth Lucero, a Pueblo scholar,
“tribal leadership is responsible for looking after the community as his children.”115 Native American communities are more likely to trust that NAPA and other health insurance programs can improve their quality of life if the messaging comes from a familiar and trusted leader, as opposed to a stranger who has not invested in their community before. This also reduces the lift of program administrators to educate one or a few leaders, as opposed to trying to reach an entire population.
3. Come to the tribes on their terms. In practice, this looks like prioritizing traveling out to the tribes, as opposed to having them travel to Santa Fe. Currently the Native American Technical Advisory Committee (NATAC), which is composed of representatives from the Tribes, Pueblos and Nations, has the opportunity to meet in-person with HSD’s Medical Assistance Division Director on a quarterly basis to discuss health care. These meetings, however, are conducted on-site at the department, and in a Western framework.116 Former Arizona Medicaid Director Tom Betlach recommended that senior staff both be educated by trial liaisons around the history of broken promises to tribes and that senior staff travel in person to respectfully listen to tribal leaders speak about their priorities. In his words, “presence matters,” and it is fully worth driving multiple hours so that senior staff can hear from indigenous people directly.117 Meeting the tribes on their terms also means spending time understanding needs from their point of view and considering policy adaptations based on their feedback. Currently, few sovereign tribal nations provide notable input into their own health care policy.118 By including indigenous voices in the development of assistance programs, rather than keeping them only on the receiving end of the programs, we can create policies that better reflect community needs. Betlach recommended that instead of entering conversations with the aim of “problem solving,” the true job of state officials is to listen respectfully to tribal representatives speaking and to then shape policies around this feedback.119
4. Improve coordination between state and health entities who work with New Mexico’s indigenous peoples. Throughout stakeholder conversations, we found that there is little coordination between different entities working with New Mexico’s tribes. Outreach coordination between entities like OSI, beWellnm and the Office of the Tribal Liaison within the NM Department of Health could allow entities to build on existing relationships and see outreach improvements on a shorter timeline than if they worked alone.
Over time, OSI and other administrators of health insurance programs should strive to strengthen direct relationships with tribes, resulting in a comprehensive understanding of needs and tools to address those needs.
Outreach efforts need to address:
1. How IHS interacts with health insurance coverage, and what services insurance coverage provides that IHS does not: Although beWellnm provides a pamphlet outlining the differences, these resources need to be supplemented with effective and thoughtful outreach to their intended populations.120 Another possible challenge here is that even when made aware of the gaps in IHS care, indigenous populations may not see a need for greater coverage.
2. The specific help NAPA provides: If the benefits of NAPA are misrepresented or misunderstood, this runs the danger of increasing distrust in US government-run “aid” programs. Specifically, outreach should outline what insurance covers and what obligations remain with the covered individual.
3. The status of access to culturally competent care and traditional healing through
insurance coverage vs IHS coverage: As a baseline, “many AI/AN believe that their health care providers need to know about the history and culture of their tribe before they can accept them and respect them as individuals.”121 Additionally, there is a demand for traditional healing as well as Western medicine.122 For individuals who prefer or seek out traditional care, there is little motivation to buy Western health insurance. Thus, communication also needs to focus on the value of access to Western medicine if and when a person may need it, as well as ongoing work to pay for traditional healing through Medicaid.
In order to build trust with indigenous communities, it is crucial that NAPA has consistent and sufficient funding. As Dr. Heather Sauyaq Jean Gordon (Iñupiaq, Nome Eskimo Community), Dr. Deana Around Him (Cherokee Nation), and Elizabeth Jordan write, the “chronic underfunding” of IHS and resource inadequacy of other health programs undermine trust and indigenous self-determination.123 Given historical relationships with indigenous communities, it will take time to build authentic relationships. Similarly, global health decolonization efforts emphasize that “in contexts of exclusion and marginalization,” policy change “requires time and sustained support that allows for the reconfiguration of societal-level power dynamics.”124
Rather than cutting back NAPA due to current poor uptake, we advocate for increased funding. New Mexico should consider the following:
1. Fully address affordability concerns As discussed in the Affordability section, NAPA does not address deductibles, coinsurance, or copays. NAPA could be expanded to cover these out-of-pocket costs for any plan that an indigenous person may choose to buy.
2. Increase navigation resources. New Mexico should consider hiring several more year-round indigenous community health workers (CHWs) who can assist individuals in enrolling in insurance. As an example, Diné College and Northern Arizona University worked together to train 35 Diné College students to provide vaccine safety education – a similar approach could be taken with insurance enrollment.125
3. Provide financial resources directly to tribes. As seen with the COVID-19 pandemic, supporting tribal sovereignty and providing resources directly to tribes is an effective way to enhance public health.126 For example, the Navajo Nation used a culturally relevant communication approach (responsibility to elders and ancestors), intense health messaging (including in the Navajo language), trust building through role models and participation in the vaccine trials, and a doorto-door mobile vaccination campaign.127 A similar approach could be taken with insurance enrollment, if sufficient funding was provided to tribal entities.
4. Ensure that there is continuity of funding. In order to increase people’s awareness and use of NAPA, NAPA must remain a reliable, adequately funded program.
5. Consider a continuous enrollment process and improve communication between Medicaid and beWellnm. Currently, individuals must re-enroll and re-select a health plan on the marketplace every year. If a person’s income has slightly changed, this also leads to benefit cliffs. For example, if a person is now at 139% FPL instead of 138%, they will need to shift over to the marketplace instead of Medicaid. Re-enrollments and changing between insurance providers causes attrition, as currently seen with Medicaid Unwinding. We advise that New Mexico consider a continuous enrollment process and develop infrastructure to warmly hand off people between programs. Rather than spending on funds on renewal and recertification, it may be more cost effective to ensure that people maintain insurance. Medicaid Forward may be one way to create more continuous coverage.
Meaningfully addressing health inequities will require the commitment of substantial funds to NAPA. We advise that the state meet with tribal representatives, indigenous-led community organizations, and indigenous health experts to hear feedback on NAPA. If there is consensus that NAPA has the potential to be a meaningful program in addressing health inequities, we advise that New Mexico take steps to ensure that NAPA has sustainable funding for complete enrollment going forward. This approach would be distinct from making the program available to a limited number of individuals based on the variable amount of revenue generated by the insurance surtax. If outreach is successful, the state must be prepared for exponential growth in enrollment. Similarly, we recommend that New Mexico consider the political climate across levels of government around programs aimed only at indigenous people. New Mexico should take steps to advance long term funding continuity of the program, so as to be able to ensure that program provision does not fluctuate with external political changes.
““Meaningfully addressing health inequities will require the commitment of substantial funds to NAPA.”
A major recurring theme in all New Mexico health equity conversations is the provider shortage. No matter which way the issue is sliced, the bottom line is clear: New Mexico needs more providers. In the specific context of NAPA, and improving indigenous health outcomes and access in general, we reduce the scope of the problem to the following: New Mexico needs more indigenous providers, as well as providers educated in indigenous cultural competency. While cultural competency training is a step in the right direction, having indigenous care providers supporting indigenous communities is even better. We highlight a few of suggestions below to this end:
1. Establish middle school or high school programs that get local students interested in health care from a young age. Early exposure to potential career paths, especially ones that can be brought back to a community could lead to more indigenous youth moving into the health care sector.
2. Develop financial support structures for providers who do want to return to their communities as health care workers. Currently, providing health care in rural areas is prohibitively expensive for an individual provider. Thus, even if a trained provider has the desire to return and open a practice in their community, it is economically infeasible. Financial programs to support such providers could pay dividends to the state of New Mexico for years to come in the form of improved health outcomes throughout the state.
3. Expand CHW programs targeting participation from indigenous communities, and develop a community health worker to more accredited provider pipeline. CHW training and accreditation is a relatively quick process, but can simultaneously help address provider shortages and start indigenous people on the path to becoming a more accredited health care provider.

Problem Statement
New Mexico faces a pressing challenge in ensuring equitable health care access for uninsured individuals without access to common forms of coverage (such as Medicaid and the beWellnm marketplace). These individuals, some of whom are undocumented, constitute a significant portion of the state’s diverse communities and contribute meaningfully to the state’s economy and cultural vibrancy. However, disparities in health care access persist, creating a critical need for targeted policy interventions.
Access issues arise from the complex interplay of federal regulations, which impose significant barriers to health care access for uninsured, undocumented individuals. Legal restrictions, compounded by fear and uncertainty stemming from evolving federal policies, create a chilling effect within the undocumented community, hindering their ability and willingness to seek essential health care services. The existing health care landscape further exacerbates the problem, as uninsured individuals are currently ineligible for federal public benefits, including Medicaid. Despite the state’s efforts to bridge the coverage gap through proposed initiatives like CEP, challenges persist in determining eligibility criteria, ensuring effective outreach, and addressing language barriers that impede access to vital health care information. Additionally, potential volatility in funding, specifically the surtax used for HCAF, raises concerns about the sustainability of programs like CEP in the long term. Without secure and permanent funding, the state risks compromising the continuity of essential health care coverage for vulnerable populations.
In summary, the problem at hand encompasses multifaceted legal, policy, and systemic barriers that hinder uninsured individuals without access to Medicaid and marketplace coverage from accessing critical health care services. Addressing this issue requires a comprehensive and sustained effort, involving policy adjustments, community engagement, and the establishment of secure and permanent funding mechanisms to ensure the enduring success of health care initiatives like CEP.
New Mexico has a strong immigrant community; almost one in ten residents were born abroad, and one in nine residents are native-born U.S. citizens with at least one immigrant parent.128 As of 2018, the state was home to 198,522 immigrants, comprising 9% of the population. These individuals hail primarily from Mexico (72%), followed by the Philippines, India, Germany, and Cuba. These immigrants actively contribute to various industries and enrich New Mexico’s diverse communities as neighbors, business owners, taxpayers, and workers.
Approximately 60,000 undocumented immigrants lived in the state as of 2016, constituting 29% of the state’s immigrant population and 3% of the state’s total population. Additionally, around 5,690 active DACA (Deferred Action for Childhood Arrivals) recipients have resided in New Mexico as of March 2020.129 Mixed status households are also prevalent in New Mexico; 35% (21,000) of undocumented residents currently live with a U.S. born child under the age of 18, and 17% (11,000) are married to a U.S. born spouse.
Immigrants play a vital role in the state’s economy, contributing hundreds of millions of dollars in taxes and adding billions of dollars to consumer spending. Nearly 19,000 immigrant entrepreneurs in New Mexico generate substantial business revenue ($319.5 million).130 Overall, immigrants are integral contributors to the state’s economic, social, and cultural fabric.
In our discussion of health care access for undocumented residents, it is crucial to differentiate between undocumented and lawful residents. Although both groups are immigrants and foreign-born, their levels of health care access differ significantly, especially in regard to Medicaid eligibility.
An undocumented resident, also commonly referred to as an undocumented immigrant, is an individual who resides in a country without the legal authorization to do so. This lack of legal status typically means that they entered the country without proper documentation or that their legal status has expired. Undocumented residents face challenges accessing certain benefits and their presence in the country is not officially recognized by immigration authorities. Undocumented residents still typically pay taxes and contribute to the local economy.
A lawful resident has legal authorization to reside in a country. In the U.S. context, this often refers to someone with a legal immigration status, such as a green card holder (lawful permanent resident) or someone with another type of authorized visa. Lawful residents have undergone a legal process to enter or remain in the country and are granted specific rights and privileges, such as the ability to work and access certain public services. Lawful residents are recognized by immigration authorities, and their presence in the country is in accordance with the laws and regulations governing immigration.
For the purposes of this report, we choose to focus exclusively on undocumented residents as they face the highest barriers to health care access and affordability.
Undocumented residents in New Mexico encounter distinct challenges in accessing health care. Even if these residents meet the state’s income eligibility criteria, they remain ineligible for Medicaid, based on federal law. Medicaid mandates that recipients must be lawful residents of the state where they receive health care. This generally restricts access to U.S. citizens and certain qualified non-citizens, such as lawful permanent residents outside of the five-year bar.131
These barriers extend beyond Medicaid; undocumented residents face legal obstacles to accessing various federal public benefits due to the regulations established by the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) of 1996. This legislation established stringent criteria for immigrants seeking public assistance, resulting in the general exclusion of undocumented immigrants from most federally funded public benefits.
Furthermore, the Public Charge rule implemented during the Trump administration marked a significant policy change. This rule expanded the criteria for determining whether an immigrant applying for a visa or seeking adjustment of status, such as obtaining a green card, would be considered a “public charge.”132
A “public charge” is an individual likely to become primarily dependent on the government for subsistence, demonstrated by the receipt of specific public benefits.
The Public Charge rule was struck down in legal challenges across various courts, and the Biden administration removed it from the federal register in March 2021.133 Its impact, however, persists. The rule change has created a chilling effect within the undocumented community, exacerbating concerns about health care access. This complex web of legal restrictions and policy changes underscores the multifaceted access challenges faced by undocumented residents in New Mexico.
In a 2023 national survey, half (50%) of likely undocumented immigrant adults and one in five (18%) lawfully present immigrant adults identified a lack of health insurance as their highest concern. These figures are a stark contrast to corresponding data points of 6% for naturalized citizens and 8% for U.S.-born citizens.134 Noncitizen immigrants are more likely to be uninsured, as they often work for employers that do not provide health benefits. Additionally, eligibility restrictions for federally funded coverage options – including Medicaid, the Children’s Health Insurance Program (CHIP), Marketplace coverage and subsidies (beWellNM), and Medicare –contribute to this disparity.
Those eligible for coverage among noncitizen immigrants encounter various enrollment barriers, including fear, confusion about eligibility rules, and challenges related to language and literacy. The higher rate of uninsurance among noncitizen immigrants translates into a greater likelihood of encountering obstacles in accessing health care, leading to instances of skipping or postponing necessary care. The limited access and utilization of health care services among immigrants result in lower health care expenditures compared to their U.S.born counterparts.
To combat these significant limitations to access, the Biden administration in 2022 increased funding for navigator programs, offering crucial support for enrollment assistance; these programs are especially helpful for immigrant families seeking to secure coverage. However, in 2023, an overwhelming majority of immigrant adults, including 90% of those likely to be undocumented, expressed uncertainty regarding the potential impact of utilizing non-cash assistance programs on their immigration status. Many mistakenly believe that such usage might diminish their prospects of obtaining a green card in the future. An estimated 27% of likely undocumented immigrants and 8% of lawfully present immigrants refrained from applying for food, housing, or health care assistance in the past year due to concerns related to immigration.135
Affordability remains the primary obstacle to obtaining health coverage for those without insurance. For undocumented residents who are ineligible to purchase insurance through the marketplace (and cannot use existing, generous subsidies for coverage) this policy landscape contributes significantly to health inequity and places strain on the state’s health care providers, who frequently provide uncompensated care to fulfill the needs of their communities.
For many uninsured individuals in New Mexico, NMMIP has served as a vital safety net for decades, acting as a last resort for those unable to find coverage elsewhere. While NMMIP offers income-based discounts, the coverage remains prohibitively expensive for a considerable portion of lower-income individuals. Consequently, only those with the most critical health needs find enrollment worthwhile. This dynamic underscores the ongoing challenges in ensuring affordable health care for all residents, emphasizing the need for comprehensive solutions to address the gaps in coverage and enhance health equity.
To address this coverage gap, Governor Lujan Grisham signed the HCAF legislation in 2021.136 This legislation grants OSI funding for a variety of objectives, including offering an affordable insurance alternative to uninsured individuals who lack access to other coverage options.
Considering the limitations imposed by federal regulations on Medicaid and the beWellnm marketplace, this report assumes that the target population New Mexico aims to assist is significantly composed of undocumented residents. As undocumented residents are ineligible for Medicaid and federal subsidized health care options, they stand to benefit under CEP.

The map is an estimate created by examining the portion of residents estimated to be undocumented in the state of New Mexico and the breakdown of country of origin for undocumented residents from the Center for Migration Studies. The percentage figures are applied to the 2021 5-year American Community Survey population data of residents in New Mexico with a foreign country of origin. Therefore, the estimates here are only suggestive.
As OSI works to finalize CEP’s design and implement the program, we offer recommendations below to ensure that CEP is efficient, affordable, and sustainable for many years to come.
Given the critical nature of the services CEP provides, OSI should avoid placing constraints on the number of individuals who can enroll in the program. The enrollment structure should also be similar to that of Medicaid, which is done on a continuous basis, as opposed to a more limited “open enrollment” period. This will help OSI scale up the program gradually, allowing the agencies time to build up enrollment, rather than having designated enrollment periods in which staff at OSI could be overwhelmed with a surge of sign-ups. Continuous enrollment would also benefit CEP enrollees, as it will grant them flexibility to sign up throughout the year, in light of any major life changes.
Individuals who do not qualify for any other form of insurance will sometimes apply to beWellnm initially before realizing they do not qualify. Collaborating with beWellnm and creating a system for “warm handoffs” would serve to promote CEP among eligible populations. BeWellnm should also post information on the website to connect eligible New Mexico residents to the program and promote CEP as one of New Mexico’s health care options. Figure five below can help inform an outreach plan to reach areas with a greater number of undocumented residents. Additionally, some CEP enrollees will reside in mixed status families, in which some but not all members are undocumented. These communities will require a more coordinated approach to connecting all members of each respective family with the benefits for which they best qualify.
As CEP enrollment grows, OSI should both prepare for new applicants to CEP. According to OSI’s 2023 CEP summary, 6,250-12,000 new individuals could enroll in CEP in the first year if uptake rates range from 25-40%. Given these numbers, it is important that OSI scale up staffing and all internal resources needed to keep up with this increase.
It is also crucial for OSI to have a comprehensive language access strategy when implementing CEP outreach. Connecting members to CEP services will be complex because these populations are often hard to reach, and will have doubts about approaching a government agency for assistance. OSI can address these challenges by utilizing a comprehensive language access strategy that takes into consideration the diverse and varied language needs of New Mexico’s immigrant population. This can be streamlined by identifying the top ten languages spoken in New Mexico and ensuring that all CEP materials, communications, and digital assets going forward are produced in those ten languages. OSI, however, should be prepared to offer additional translated materials as needs arise, which is another reason why the translation service provider contracts will be instrumental in expanding language services capabilities.
Agencies must also ensure that customer service and appeal and grievance processes are accessible, regardless of language. Oftentimes, businesses or government offices may rely only on translating materials into Spanish when conducting outreach with the immigrant community, thinking that bilingual services sufficiently cover outreach needs. However, immigrant communities are diverse and often speak languages other than Spanish. OSI should consider contracts with language translation services as part of their outreach strategy for CEP, including written translations, in-person interpretation, and over-the-phone translations for people who call in with questions. Many translation companies offer their services throughout the United States. This should enable OSI to choose among a variety of translation service contractors, rather than just those located in New Mexico.
The enrollment process for CEP should be easy to navigate.The application should not ask for a Social Security Number (SSN), and instead should simply verify income for purposes of eligibility. An Individual Tax Identification Number (ITIN) can be requested in lieu of an SSN, but should not be required as not all applicants will have an ITIN. The most important requirement for the program is establishing residency in New Mexico, which can be done through employment verification.
While CEP will serve as a separate program managed by OSI, identification cards for members should not be easily discernible from other health insurance cards issued by the state. For example, if CEP plans mirror Turquoise Plans 1 and 2, enrollees’ insurance cards should not be visually identifiable from those of other plans. Plan differences should only be distinguishable on the back-end when viewing benefit details.
As OSI decide on their redetermination processes, it is important that redetermination (if adopted) not be overly prescriptive nor burdensome, as frequent fluctuations in income could drop people from coverage that they still need. If, for example, a member goes from 190% FPL to 220% FPL, this may mean that according to CEP guidelines, they become ineligible. In reality, however, this only represents a slight increase in income; it does not mean that this family no longer requires assistance. For these reasons, the OmniSalud program which serves undocumented communities in Colorado (and is discussed more below) has chosen not to utilize annual redetermination. While there are challenges inherent to this approach, it is important to remember that if members in New Mexico are dropped from CEP due to a slight increase in income, they will not have any additional coverage options available. Oftentimes, these populations experience many fluctuations in their incomes; incomes may increase slightly one month to reach above 200% FPL, just to fall below 200% FPL again in the following month. OSI should consider providing members whose incomes exceed 200% FPL a grace period of about 6-12 months before dropping them entirely. This grace period would also provide families some time to prepare for the transition off of CEP.
Community outreach will be crucial to the successful implementation of CEP. Many of the populations that would benefit most from this program will be hard to reach given years of fear and distrust toward government programs, and a lack of awareness about coverage options. OSI will need to engage in a proactive campaign to educate New Mexico’s residents about the benefits of CEP and to assuage concerns.
In OSI’s 2023 report, the agency identified a one-year preparation period for outreach leading up to implementation.138 It is very helpful to set up this dedicated time for implementation –OSI should also work to continue this critical outreach beyond the initial preparation period.
Given that a number of non-profit organizations and advocacy groups have established trust with undocumented immigrant populations, we recommend that OSI outsource much of the outreach to these organizations. Organizations that deploy “promotoras” can play a crucial role in helping to enroll vulnerable communities, as these organizations are often trusted and established in the community already. OSI should set expectations for outreach and enrollment, while seeking input from these organizations about strategies that would be the most helpful in reaching these populations.
Another important component of community outreach will be the explanation of benefits, and how they can benefit immigrants and their families. Because members that are used to the LIPP-75% may be accustomed to only seeking out medical services on an emergency basis, explaining the advantages of preventative care may improve population health.
As CEP implementation moves forward, OSI should stress the importance of offering health services to all residents, regardless of immigration status. CEP is expected to bring both health care benefits and considerable savings to the state. According to OSI’s own projections in a memo from August 18th, CEP will save the state approximately $23 million, as cost sharing with HCAF provides a more cost-effective option to cover individuals who qualify for LIPP75%. Providers, businesses, and related stakeholders should be transparently briefed on the reimbursement rates and other benefits that CEP will provide.
As the state prepares to implement CEP, its immediate focus should be on allocating funding and implementing a community-oriented plan that centers outreach. In the longer term, the state should work to build up CEP as a permanent program, by creating a permanent carveout for CEP within HCAF. OSI should also ensure that funding requests from the Legislative Finance Committee staff align with CEP needs, so funding streams do not fluctuate and negatively impact service delivery.
As CEP becomes more established and the state can measure its impact, OSI should consider widening the program’s eligibility criteria to include other income brackets that currently participate in LIPP. CEP is currently designed to include anyone participating in LIPP-75%, which includes individuals below 200% FPL. However, LIPP also offers coverage at 50% for people under 300% FPL and 25% for those under 400% FPL. If OSI wishes for more NMMIP enrollees to participate in CEP, it should create a longer-term plan to include individuals under 400% FPL.
OSI should be mindful that federal immigration policy is subject to change, and has experienced many restrictions in previous years. These changes affect the way in which immigrants apply to state and local programs. Even though state and local programs are not tied directly to the federal government, immigrants may wish to avoid identifying themselves to any government agency.
OSI should conduct their outreach in a way that is mindful of these concerns. Additionally, there should be robust plans in place to protect data and information gathered about vulnerable populations. We advise that OSI not collect immigration information as this could dissuade enrollment. More broadly, the agency must ensure that all data and information collected on new members and existing members participating in CEP and NMMIP is secure and not shared with the federal government.
As stated above, securing permanent funding for CEP is critical to establish the longevity of the program and to ensure its permanence. The state’s Legislative Finance Committee has secured only $10 million of the $23 million that was requested for CEP. If the surtax used to fund HCAF is seen as volatile, this could impact the overall funds provided to programs including CEP. A permanent appropriation included in the state’s budget would ensure longer-term, sustainable access to health coverage.

Problem Statement
Medicaid Forward has been proposed as a solution to persistent uninsurance and underinsurance in New Mexico. Although uninsurance in the state was more than halved between 2009 and 2019 due to the state’s implementation of the ACA, 10% of New Mexicans under 65 still lacked coverage as of 2022.139 New Mexico will face further challenges in insuring the state’s population as individuals and families lose coverage due to the Medicaid unwinding process.
Many New Mexicans whose incomes are greater than 138% FPL (and therefore do not currently qualify for Medicaid) may struggle to afford plans on the beWellnm marketplace. Affordability has certainly improved in recent years, through both federal and state-led efforts. In 2021, the American Rescue Plan increased financial assistance for marketplace plans, and the Inflation Reduction Act extended this assistance through 2025.140 Due in part to these enhanced subsidies, four in five Healthcare.gov customers will be able to purchase coverage for $10 per month or less, for the 2024 plan year.141 These federal efforts have been supplemented by New Mexico’s assistance for the state’s residents. Through New Mexico’s Turquoise plans, households below 300% FPL can now access coverage with low- or no-cost premiums, although some cost-sharing is still required.142
Nevertheless, New Mexicans may struggle to afford the cost-sharing associated with these plans, even if premiums are low. New Mexicans at slightly higher income thresholds, who do not qualify for Turquoise plans, may also struggle to afford more expensive premiums, as assistance decreases at relatively higher incomes. These residents may access enhanced Premium Assistance through the stated above federal subsidies; yet, these may be insufficient to buy a plan that reduces cost-sharing to affordable levels. Many individuals may, therefore, opt for the Bronze or Silver-tier marketplace plan with the lowest possible premium, which typically demand higher out-of-pocket payments. Even if affordable plans are available, sifting through multiple options to minimize out-of-pocket costs requires time and a preexisting knowledge of the health care system which many New Mexicans lack.
In addition to these affordability issues, challenges in the existing insurance marketplace contribute to uninsurance, in spite of the efforts of beWellnm, the state’s ACA marketplace. When individuals lose Medicaid eligibility (due to variations in pay, such as a slight pay increase that leaves a person slightly over 138% FPL for example, or cyclical unemployment) they lose insurance through Medicaid and must proactively seek insurance on the marketplace to avoid becoming uninsured. Without a mechanism for automatic enrollment in a marketplace plan, some individuals lose coverage as their income and employment status changes, making them ineligible for Medicaid. Uptake on the beWellnm marketplace, as reflected in marketplaces across the country, has not accounted for all individuals losing Medicaid coverage. Additionally, open enrollment only takes place once per year; if an individual misses their special enrollment period, they are forced to remain uninsured until the following year.
Furthermore, churn imposes burdens on patients who may lose access to their existing providers as they change insurance networks, potentially disrupting continuity of care. This churn also burdens health care providers, who must manage billing and administration across a plethora of insurance carriers, as their patient population switches coverage.
Finally, uninsurance remains persistent in New Mexico among undocumented individuals, who, as discussed, are ineligible for both Medicaid and insurance plans on the beWellnm marketplace based on federal restrictions. Even if an individual becomes documented and meets the Medicaid eligibility requirements, he or she often must wait five years before applying to the Medicaid program, creating another barrier to insurance access.143
The New Mexico legislature has proposed a solution to these issues: Medicaid Forward. Medicaid Forward would provide residents above the current cutoff of 138% FPL with the option to buy into the state’s existing Medicaid program. The Urban Institute estimates that Medicaid Forward could reduce the state’s uninsurance rate from 13.1% to approximately 5.75%.144 The program could also improve member experience by reducing program churn and would also be available to all residents regardless of immigration status.
An income cap or other eligibility restrictions are not yet set for the program. The ACA allows states to expand coverage with no upper limit, leaving it to New Mexico to decide who will be eligible.145 If covered, Medicaid Forward would provide families earning between 138-400% FPL with a more stable and affordable alternative to the programs within HCAF reviewed in our background section, including the Premium Assistance and the State Out of Pocket Assistance Program, as well as the Native American Affordability Fund for indigenous populations. While HCAF programs somewhat offset the premium and out-of-pocket costs of marketplace options, Medicaid Forward would provide an entirely state-run plan for these families. Participants in Medicaid Forward earning above 150% FPL may be charged modest premiums or other costsharing requirements, which we expect to fall below marketplace alternatives. Cost-sharing requirements have not yet been determined for the program.
In Medicaid’s current form, residents without documentation, within the ‘five-year bar’, or otherwise lawfully present but not qualified are ineligible to participate. Under Medicaid Forward, however, all residents of the state who meet income limitations would be eligible for the program without exceptions based on immigration status. This would preempt the need for CEP, discussed above, as Medicaid Forward would provide state-run, subsidized coverage for immigrant populations.
New Mexico has one of the country’s highest Federal Medical Assistance Percentage (FMAP) rates for Medicaid of about 73%, meaning that for every dollar the state spends, the federal government contributes $2.65.146 New Mexico will be able to receive this subsidy for all expansion populations except for those who do not qualify for traditional Medicaid based on immigration status.147
According to estimates from the Urban Institute, the state share of the expanded program could total several hundred million dollars annually.148 Multiple sources of revenue would compensate for this gap:
• Implementing Cost Sharing: New Mexico may charge premiums or other costsharing, such as copays and deductibles, for populations earning above 150% FPL.149 Total cost sharing may not exceed 5% of family income.150 Comparatively, according to 2020 data, the average family covered under ESI spends 4.7% of household income on their deductible alone.151
• Covering State Employees: Employees of New Mexico are currently covered under a state health plan, which is expensive for the state to administer. Employees would be transitioned onto Medicaid Forward, enabling the federal match to apply to their health coverage.
• Reducing Uncompensated Care: Uncompensated care for uninsured populations amounts to nearly 3% of hospital budgets.152 These expenses are passed onto insured populations, which has historically driven up the cost of treatment and coverage. Furthermore, the Uncompensated Care Pool is authorized to spend up to $68.9 million on reimbursement for uncompensated care.153
• Redirecting Other Assistance: HCAF and other assessments that support the high-risk pool and state-based marketplace (SBM) programs would be diverted to Medicaid Forward. It would require legislative action to convert these funds to Medicaid Forward.
• Increasing Base for Payor Fee: New Mexico currently assesses a fee on marketplace plans and Medicaid MCOs to fund HCAF. Self-insured plans are exempt from these fees. By moving covered lives from self-insured ESI to Medicaid Forward, New Mexico would increase the base on which the fee is assessed.
• Oil and Gas Revenue: New Mexico is in the midst of an oil and gas boom, benefitting state budgets. Governor Lujan Grisham recently signed SB 26 to lessen budget volatility and invest these dollars for future use.154 Numerous stakeholders mentioned potential overreliance on these revenues for the state budget since they are unreliable and operate in a cyclical market.
The Urban Institute also estimates that revenues may originate from employers through two channels. First, employers in competitive markets may pass through a portion of the savings from no longer offering ESI to employees through increased wages, thereby increasing the state’s income tax base. This, of course, is predicated on an assumption of competitive markets that may not materialize, based on the state of New Mexico’s economy at the time of implementation. Second, there may be an opportunity for the state to impose a tax on employers to fund the program; this would require additional legislation and is not included in our analysis.
Compared to traditional Medicaid, the program could also impose cost-sharing requirements on participants, offsetting some of the cost through premiums and out-of-pocket payments.
HB 400 was signed into law in April 2023, passing the Senate with 24 yes-votes (out of 42 seats) and the House with 57 yes-votes (out of 70 seats).155 This bill requires Secretary of Health and Human Services Kari Armijo to submit a study to two legislative committees by October 2024 with recommendations for Medicaid Forward. The Secretary, in consultation with the Superintendent of Insurance, Medical Advisory Committee, and other stakeholders, is tasked with evaluating the effects on existing insurance markets, including individual, group, self-insured, and state plans. She is also tasked with determining the effect on the provider landscape and necessary changes to Medicaid reimbursement rates to maintain sufficient provider supply under Medicaid Forward. Finally, she is tasked with determining the operational needs, funding, and economic implications of the plan.
The planning of Medicaid Forward rests with HSD in the creation of this proposal, which will include the coverage design and feasibility of the program.

Medicaid Expansion, Basic Health Program, or Public Option?
Other states have tried various solutions to address coverage of their population that makes too much to qualify for Medicaid (over 138% FPL) but cannot afford health insurance even with marketplace subsidies. Some, like New Mexico’s HCAF, have added incentives on top of federal subsidies to expand the populations that can access $0-premium plans and reduce cost sharing. Others have created publicly-funded programs, run by the state, that cover middle-income populations.
As discussed above, Medicaid expansions above 138% FPL are allowed under the ACA.156 In this system, enrollees utilize the same structure as those qualifying for traditional Medicaid with the option to add limited cost sharing requirements. The District of Columbia has implemented longterm Medicaid expansion above 138% FPL akin to Medicaid Forward.157 In DC, residents earning up to 215% FPL can qualify for Medicaid, with higher thresholds for parents with dependent children and pregnant women.158 Immigrants can obtain coverage through a separate, more limited program called DC Health Care Alliance. Oregon recently implemented a temporary expansion of Medicaid income limits up to 200% FPL as a stopgap measure while they await approval of their basic health program (BHP) to avoid temporarily dropping people from Medicaid during unwinding. The funding for this population is only approved until July 2024 when they expect their BHP to be operational.159 Delaware evaluated expanding their Medicaid income limits in 2019 but decided against it due to financial and operational concerns.160 Other states, such as Connecticut, have elevated income limits for certain populations, such as pregnant women and parents of dependent children.161
The ACA provided states with the opportunity to run health plans for residents earning between 133% and 200% FPL. Lawfully present immigrants under the five-year bar are eligible to participate in a BHP.162 States receive 95% of what the federal government would have paid in marketplace subsidies for this population, which is benchmarked to the second lowest cost silver plan.163 As a result, states with high marketplace premiums and low Medicaid plan costs are best positioned to run effective BHPs. Although BHPs must be at least as affordable as their marketplace alternative, they typically provide more generous coverage and states have the option to eliminate cost-sharing altogether. Minnesota and New York have implemented BHPs with generous coverage. Oregon expects to launch its BHP in 2024 164 and Kentucky submitted an application to CMS for approval.165
Three states – Colorado, Washington, and Nevada – have launched public options through public-private partnerships with carriers.166 The scope of what public options can encompass is varied. For example, Colorado requires carriers to offer Colorado Option plans with reduced premiums. Through this program, they run OmniSalud, which provides a limited number of Option plans for people who do not qualify for other forms of coverage based on immigration status.
The majority of New Mexico residents have favorable views of the current Medicaid program and view it as a “quality, trust[ed] source of health insurance.”167 If implemented successfully, Medicaid Forward has the potential to help remedy existing health disparities in New Mexico. As discussed, the 2023 Urban Institute study on Medicaid Forward estimates that between 130,000 and 142,000 New Mexicans would gain access to insurance via the program, prompting the state’s uninsurance rate to more than halve (dropping from 13.1% to ~5.4-6.1%).168 Meaningfully improving insurance access across the state would create a stronger safety net for future health emergencies. The COVID-19 pandemic, for example, deepened health disparities; broadbased access to insurance would leave New Mexico better prepared to weather future shocks.
Medicaid Forward could also ease financial and access burdens on New Mexicans who have historically faced barriers to care. The Urban Institute estimates that household spending on health care would fall, with those living at or below 138% FPL experiencing the largest reductions. (Although many individuals at or below 138% FPL have access to Medicaid, some out-of-pocket costs are still involved, and access remains restricted for undocumented individuals.) These projected reductions in out-of-pocket spending would help alleviate health disparities faced by low-income New Mexicans. More individuals would have access to preventative care, and fewer individuals would delay care as access becomes more affordable. In contrast, polling shows that 56% of New Mexicans have delayed care over the past two years due to cost concerns.
“...between 130,000 and 142,000 New Mexicans would gain access to insurance via the program, prompting the state’s uninsurance rate to more than halve
Medicaid Forward could also improve health equity in New Mexico by eliminating the administrative complexity that individuals face in navigating health care markets. If more New Mexicans had the option to utilize a stable source of health insurance that was not linked to their employer or current income levels, churn across the insurance markets would decrease. This has important consequences for health equity as churn is associated with disruptions in care, medication adherence, and increased emergency department visits.169 Individuals with less stable sources of employment would not lose coverage between jobs. Furthermore, obtaining and retaining coverage would be simpler for individuals who may have difficulty navigating health insurance markets due to issues such as language barriers or broadband access.
As discussed throughout this report, indigenous communities face unique health disparities and barriers to care. It may be difficult to promote Medicaid Forward uptake among indigenous communities, given existing distrust and the perception that insurance beyond the IHS system is unnecessary. (As mentioned in the NAPA section, the state sees persistent underutilization of Medicaid by indigenous individuals who currently qualify.) Robust community outreach and trust-building will be required to generate buy-in for Medicaid Forward; with successful implementation, the program could improve access to high-quality, affordable care outside of the IHS system.
Similarly, Medicaid Forward could be transformational for undocumented New Mexicans, who are currently barred from participating in Medicaid or the beWellnm marketplace. Thoughtful outreach would be required among undocumented and mixed-status families, to restore trust and encourage Medicaid Forward participation. Any Medicaid Forward program would also need to be carefully designed to ensure that enrollment data cannot be weaponized against undocumented communities in the future, given the dynamic federal policy environment.
Medicaid Forward would also be accessible to qualified non-citizens in New Mexico, who currently cannot access Medicaid benefits due to the “five-year-bar.” Medicaid Forward could alleviate health disparities that these individuals face, due to systemic barriers to insurance coverage.
Importantly, however, the health equity impacts of Medicaid Forward are hypothetical at this stage. Several stakeholders in New Mexico raised concerns that Medicaid Forward could negatively impact health equity, if:
• Provider shortages intensify due to low reimbursement rates, particularly in rural areas that are already suffering from provider shortages;
• The size and accessibility of the Medicaid provider network is more restrictive than currently available commercial plans, particularly during the transition period in which individuals switch to Medicaid Forward;
• Funding streams (either federal or state) become unreliable in future years and are unable to continuously maintain Medicaid Forward.
To deliver greater health equity for New Mexicans, Medicaid Forward implementation would need to address these concerns.
The HSD report will outline implementation and operational needs for their vision of Medicaid Forward. As the primary agency responsible for the program, they will have the most intimate understanding of its needs and their capacity. There are, however, two key operational issues to highlight: the need for new cost-sharing systems and administrative capacity at HSD.
Centennial Care does not currently collect premiums – it is statutorily prohibited from collecting premiums on people making below 150% FPL. As a result, HSD presumably does not have the existing technological infrastructure to operationalize enrollment. Therefore, it is important that any implementation plan includes time and budget for building out premiumcollecting systems. Other cost-sharing requirements, such as copays, would be collected through the Medicaid MCOs, which currently collect modest copays and should have this infrastructure in place.
The Human Services Department will be responsible for administering Medicaid Forward, yet it is widely understood that they have significant staffing vacancies. This has impeded their ability to avoid ex parte disenrollment during Medicaid unwinding and HSD is facing issues hiring sufficient staff. Medicaid Forward will increase staffing needs.
Finally, the state should consider the reliability of revenues used to support Medicaid Forward, including any reliance on oil and gas revenue. Some stakeholders we spoke to estimated that the current boom is expected to last approximately ten years, after which the state budget may be more constrained.
Medicaid Forward may have unintended consequences for insurance markets, state budgets, and health systems, which must be considered as part of any implementation plan.
Given the small size of New Mexico’s insurance market, it may become difficult to sustain commercial insurance plans absent markedly higher premiums if enough individuals opt into Medicaid Forward.
The Urban Institute estimates that the number of New Mexicans enrolled in ESI could decline by 31.9% to 50.1%, as employees opt for Medicaid Forward.170 Employers-based plans, whether self-insured Administrative Services Only (ASO) or fully commercial, may become less attractive to employees and stop being offered.
On the beWellnm marketplace, participants moving to Medicaid Forward could lead to insufficient risk pooling, driving up premiums and creating a “death spiral.” If commercial insurance becomes unviable, Medicaid Forward would need to accommodate all New Mexicans, beyond any income limits originally set by Medicaid Forward. Furthermore, the state government would need to work with individuals and insurance carriers displaced by changes to the current insurance market.
Hospitals and providers expressed concern about the possibility of cannibalizing the ESI market with Medicaid Forward. ESI provides reimbursement rates that are sometimes above 250% of Medicare rates, according to the New Mexico Hospital Association.171 Gaining the support of hospitals and providers could hinge on the program’s ability to either raise Medicaid reimbursement rates or put guardrails on residents with ESI (which has the highest reimbursement rates) moving onto the program.
One key question for Medicare Forward, therefore, is whether the policy can sufficiently drive participation and reduce uncompensated medical care to compensate hospitals and providers for the loss of commercial insurance reimbursement rates. Stakeholders were concerned that rural hospitals in particular would be vulnerable to insolvency and closure if Medicaid Forward eats into commercial insurance payments. Raising reimbursement rates – and perhaps adding in facility fees and adjustments for rural hospitals – may alleviate some concerns related to provider reimbursement.
Sustainable financing for Medicaid Forward will be critical to the success of the program, if implemented. As New Mexico cannot run a deficit year-to-year, the state must plan ahead for the budgetary demands imposed by Medicaid Forward to avoid running out of funds or needing to adjust provider reimbursement rates if they experience a budget shortfall. Creating an emergency fund, perhaps by using existing oil and gas revenue could create breathing room for New Mexico going forward, to alleviate financial pressure during years when state revenue is less plentiful.
As greater numbers of New Mexicans become insured, utilization of health care services could increase. Given that New Mexico already faces a provider shortage, simply providing access to insurance may not guarantee access to health care, if providers cannot support the demand for services. Furthermore, increased utilization of health services may increase the financial demands placed on the state in providing Medicaid Forward. While it may be possible to limit demand by adding copays that would limit utilization, such a policy decision would involve trade-offs with health equity. Studies have repeatedly shown, for example, that even $5 copays can lower health care utilization.172 New Mexico should apply co-pays judicially, therefore, as additional out-of-pocket costs may limit the use of preventative care, create poor health outcomes, and perpetuate health disparities.
As discussed above, employers stand to save significant benefits dollars on ESI if their employees switch to Medicaid Forward. In particular, small-to-medium sized enterprises may presently struggle to afford ESI, and employers under the mandatory threshold (<50 employees) may be unable to compete for employees against larger companies without offering these benefits.173 Medicaid Forward, therefore, may change New Mexico’s employment landscape, if ESI becomes a less essential benefit within employer benefit offerings. Further research could help better understand the precise implications of this shift.
Finally, current policy planning around Medicaid Forward assumes a constant level of federal support for the program and state policymakers should be cognizant of the dynamic federal landscape. If new federal administrations change policy regarding FMAP reimbursement or public charge rules, for example, the sustainability and health equity impacts of Medicaid Forward would be altered. Furthermore, expanding existing Medicaid programming to those above 138% FPL and adding premiums according to income requirements would not require federal approval, but any deviation from this structure would require an 1115 waiver.174 Any withdrawal of benefits due to federal policy would result in distrust and upheaval in New Mexico’s insurance landscape.
As HSD completes its study of Medicaid Forward, the department may wish to consider different policy levers that could improve the financial sustainability and impact of the program.
As mentioned previously, states have the option to run BHPs for residents earning between 133-200% FPL. States receive 95% of what the federal government would have paid in marketplace premiums for BHP recipients to enroll these residents in a state plan. As a result, a BHP benefits states with high marketplace premiums but low provider reimbursement rates. This setup, therefore, could be advantageous for New Mexico; it could allow the state to provide generous coverage to low-income New Mexicans while maximizing federal dollars. Furthermore, a BHP could provide affordable, highquality coverage for income-eligible, lawfully present immigrants who may otherwise be subject to the “five-year-bar” on utilizing Medicaid benefits.175
Previous states have also implemented BHPs to reduce churn between Medicaid and the commercial marketplace.176 As many individuals perceive marketplace coverage to be too expensive (a perception beWellnm is trying to combat), a BHP can promote enrollment for individuals with incomes just above the Medicaid cutoff. If New Mexico does implement Medicaid Forward, however, Medicaid Forward would provide an equivalent path for reducing churn.
Stakeholders throughout New Mexico suggested a range of reimbursement rates to make Medicaid Forward feasible for providers (which will be discussed more in the following section). Reimbursement rates will be a critical lever for policymakers to consider, as they seek to cultivate physician and hospital buy-in. Likewise, price transparency from hospitals and physicians can help justify and make the case for increased reimbursement rates.
New Mexico could consider variable reimbursement rates for rural providers, to help address the acute rural provider shortage. An enhanced reimbursement factor designed to target rural facilities could help make Medicaid Forward sustainable among rural and frontier clinics which may operate on thinner margins.
Implementing Medicaid Forward would require robust coordination across different agencies in New Mexico’s state government. BeWellnm, contacts responsible for state employee insurance plans, and tribal liaisons, for example, would all need to coordinate closely with HSD to ensure a successful transition to Medicaid Forward. Additional resources and implementation capacity would be essential to HSD’s success in spearheading an initiative as large and as complex as Medicaid Forward.


Problem Statement and Background
New Mexico has a striking provider shortage, which stems from both recruitment and retention issues.177, 178 Among New Mexico’s 33 counties, 32 are designated Healthcare Professional Shortage Areas.179 Between 2017 and 2021, New Mexico lost a staggering 30% of its primary care provider workforce. In 2021, New Mexico experienced a net loss of providers across several areas, including OBGYNs, psychiatrists, registered nurses, dentists, and certified nursemidwives. To meet minimum national provider-to-population benchmarks, New Mexico requires hundreds more providers. As of 2023, meeting these benchmarks would require an estimated 264 additional primary care physicians, 235 additional dental care providers, and over 90 additional mental health providers.180
Shortages are growing increasingly acute in New Mexico because providers–and the population at large–are aging.181 New Mexico’s providers are, on average, substantially older than the national average. The state’s primary care providers are 52.8 years old on average, nearly 13 years older than the national mean of 40. Troublingly, specialists such as general surgeons and psychiatrists are even older (54.9 and 58.2, respectively). This aging provider population indicates mass retirements are likely within the next ten years.
New Mexico’s residents, like its providers, are also aging.182 By 2030, over 22% of New Mexicans will be over 65 years old.183 This is roughly consistent with national trends, which forecast that 20% of the population will surpass 65 by 2030.184 New Mexico’s oldest counties are also some of its most rural. For example, 43.3% of the population in Catron County, New Mexico’s third least-populous county, are 65 or older.185 Aging providers are struggling to care for an aging patient population with increasingly complex conditions.
The provider shortage is particularly severe in rural and frontier areas of New Mexico. Among the state’s 2.1 million residents, 31% reside in rural counties.186 Furthermore, rural areas have specific and complex needs, making the provider shortage more difficult to address. Rural and frontier areas require providers with specialized training across multiple practice areas, due to the long distance from fully equipped hospitals.
The potential of telehealth to blunt the impact of provider shortages is limited by broadband issues in the State. The Governor’s Office reports that nearly one quarter of households in New Mexico lack reliable internet access; 16% of households have no broadband access whatsoever.187 The areas without reliable broadband access are disproportionately rural. For example, in McKinley County, which overlaps with Navajo Nation, 60% of residents lack broadband access.
There are many drivers of the provider shortage in New Mexico. Low Medicaid reimbursement rates relative to neighboring states, the medical malpractice environment, tax policies affecting providers in the state, and inadequate investment in the provider pipeline all exacerbate the provider shortage.188 For providers, New Mexico’s reputation is unmistakable: in three of the past four years, the Becker Hospital Review has ranked New Mexico among the five worst states in which to practice medicine.189, 190, 191
Compared to neighboring states, New Mexico has high caps on medical malpractice damages. New Mexico’s Medical Malpractice Act of 2021 increased the cap on medical malpractice damages from $600,000 to $4,000,000 for hospitals and outpatient health care facilities. This cap will increase even further, and will reach $6,000,000 by 2026.192 The Medical Malpractice Act also increased the cap on independent providers from $600,000 to $750,000. Comparatively, neighboring Texas has a medical malpractice cap for independent providers of just $250,000. These policies have made liability insurance expensive, especially compared to neighboring states.193, 194, 195 This discrepancy makes it difficult for New Mexico to compete with neighboring states for providers.
New Mexico’s unique tax policy is also less hospitable to providers than those of neighboring states that compete for talent. New Mexico imposes a gross receipt tax (GRT) on medical services; this means that all of a practice’s transactions are subject to a 7% tax.196 While GRT deductions are available for services rendered through Medicare, MCOs, and government insurance programs such as TriCare, GRT deductions for co-pays and deductibles were not permissible until July 2023.197, 198 This 7% tax – combined with longstanding limitations on GRT deductions that were only lifted this year–constitute a financial burden for independent medical practices in New Mexico. No other state in the Southwest has a GRT on medical services.199
Finally, New Mexico has a limited student loan repayment program that provides little support for those in the medical provider pipeline. The Health Professional Loan Repayment Program offers up to $25,000 in student loan forgiveness, but the fund is not large enough to meet applicant demand. Of the 600 plus health care professionals who applied for the Program, less than 8% of applicants received any form of student loan relief.200
There are multiple challenges in recruiting and retaining talent. In rural areas particularly, the provider shortage is a self-compounding issue: the scarcity of providers effectively increases the patient load per provider and the length of time for which each provider needs to be on call. These factors worsen the quality of life for providers in New Mexico and, in turn, deters others from practicing in New Mexico. For example, rural providers are more likely than urban providers to report working 40 or more hours weekly and spending all of their work hours in direct patient care.

Increase Reimbursement Rates
According to some of our interviewees, the disproportionate percentage of Medicaid patients and uncompensated care in New Mexico’s payer mix causes unsustainable operating margins for providers. Compounding this issue, New Mexico’s Medicaid reimbursement rates are comparatively lower than in neighboring states. We heard from stakeholders, for example, that a 125% of Medicare reimbursement rate in New Mexico still resulted in lower reimbursement for providers than a 100% of Medicare reimbursement rate in Texas. Comparatively low margins are the most significant obstacle to attracting and retaining providers. This discrepancy should underpin comparisons of reimbursement rates with competitor states. The New Mexico Health Care Workforce Committee proposes the state “increase Medicaid reimbursements by ensuring any percentage increases to the Medicaid budget are matched, proportionately, to an increase in provider reimbursement rates in both Centennial Care plans and fee-forservice reimbursement schedules. Each Medicaid reimbursement must be a minimum of 125% of Medicare rate and updated annually.”201
If Medicaid Forward provides reimbursement rates that are sustainable for providers, the financial case for practicing medicine in New Mexico, particularly as an independent practitioner, would improve. Furthermore, increasing insurance coverage would reduce uncompensated care, further helping providers. It is worth noting, however, that the exact reimbursement rates required for provider sustainability are uncertain and would vary based on patient volume.
In interviews, the state’s health systems and the New Mexico Medical Society repeatedly pointed to HB 75 (passed in 2021, which overhauled previous medical malpractice laws) as driving physicians out-of-state and warding off new practitioners, due to increased malpractice insurance premiums. Independent outpatient facilities and certain clinics are now subject to the same professional liability coverage requirements as acute care hospitals (an increase in potential exposure from $600,000 to $4,000,000, eventually rising to $6,000,000), making coverage out of reach for many providers.202, 203 Some carriers are reportedly refusing to insure independent practitioners who perform in-office colonoscopies or in-office surgeries due to the new exposure.204 Meanwhile, neighboring Texas caps malpractice liability at $250,000, and premiums are far cheaper in all of New Mexico’s neighboring jurisdictions.
The Legislature should examine the impact of HB 75 and determine whether the law requires further amendments to mitigate the impact of rising professional liability insurance premiums, especially for independent providers and outpatient facilities. New Mexico could also consider implementing a state-run malpractice insurance plan or supplemental insurance program, to promote rural practice. Indiana, New York, and Pennsylvania all offer excess or primary coverage options to reduce the cost of malpractice insurance for in-state providers.205
Although New Mexico enacted legislation in 2016 to streamline and expedite credentialing decisions by insurers (which must be rendered within 45 days of a provider’s application), insurers routinely fail to comply with these deadlines. Insurers often blame late reimbursements for any delays in adding credentialed providers into their payment systems, disrupting provider revenue cycles.206 To address the state’s physician shortage, the New Mexico Medical Society and the New Mexico Health Care Workforce Committee have recommended amending the 2016 law to require insurers to load provider information into their payment systems within the 45-day period (as proposed by SB 182 from 2022). OSI could also advocate for the Legislature to buttress enforcement of the existing law and add tougher penalties for violating the 45-day timeline to ensure effective implementation of the timeline.207 Provider enrollment in Medicaid and credentialing for hospital privileges should also be further streamlined.
Hospitals throughout the United States have a long history of successfully relying upon foreign-trained doctors to bolster their physician workforces.208 Requirements that physicians work in rural or underserved areas for at least three years have created significant demand for immigration “national interest waivers.” However, most states’ licensing rules require foreigntrained physicians to complete residencies in the United States or Canada.209 This compels many international physicians to repeat residency training they have already completed abroad.210 While immigration-related barriers to attracting foreign physicians are not within the state’s purview, New Mexico could explore joining its neighbor Colorado along with Idaho, Illinois, and Tennessee by simplifying the path to licensure for immigrant physicians while contemporaneously mitigating the impact of the physician shortage in New Mexico’s Health Professional Shortage Areas (HPSAs). These foreign-trained physicians would still be required to pass U.S. medical licensing examinations, assuaging concerns about their qualifications to practice in accordance with American standards.211
With both the second-worst projected physician shortage ratio and the oldest physician workforce in the country, New Mexico should focus on both retaining talent and attracting young physicians.212 Since Medicare has capped the number of funded residencies in 1997 (at a time when Congress feared a physician surplus), the number of qualified medical school graduates who have passed their licensing exams now outstrips the number of available residency slots by the thousands, annually, New Mexico could enact legislation modeled after laws in Arkansas, Kansas, Missouri, and Utah to provisionally license M.D.’s and D.O.’s who have not successfully “matched” to a residency.213 Such provisional licenses would require these providers to treat patients under the supervision of practicing, conventionally licensed collaborating physicians and require them to work in rural or underserved parts of the state.
General Medical Education and Residency Expansion (Including Implementation of House Bill 480)
Similar to the challenges posed by the retirement of older doctors and an aging population, the misallocation of physicians is a national concern. It is critical for the state to send providers where they are most needed, given the large proportion of New Mexico designated as rural and underserved. Most efforts to combat physician shortages fail to address a fundamental missed opportunity in how Medicare funds residencies (98% of which are situated at urban, metropolitan teaching hospitals): future physicians are far more likely to settle down and practice medicine where they train.214
General Medical Education (GME) expansion and the creation of additional residency slots in New Mexico – especially in underserved, rural areas and areas near tribal communities – can even be achieved by state funding for new residencies. Wisconsin, North Carolina, West Virginia, and California have implemented this model at rural clinics and federally qualified health centers (FQHCs) to address shortages in underserved areas. The first increase in GME funding from Medicare in a quarter-century was enacted as part of the Consolidated Appropriations Act of 2021. This federal funding, combined with new opportunities arising from the Resident Physician Shortage Reduction Act, creates an opportunity for New Mexico to leverage federal dollars, expand residencies, and buttress state funding for provider deserts.215 While most U.S. residencies are Medicare-funded, this is not required; residencies only need to be accredited.216 The State already received CMS approval in 2021 to provide Medicaid GME funding for rural clinics and FQHCs as residency training sites.217 New Mexico’s Medicaid GME program includes a rural training track for residents to increase access to rural care.
The New Mexico Legislature previously funded nine state residencies in response to the New Mexico Health Care Workforce Committee’s 2014 recommendations (in Fiscal Years 2015 and 2016), but this funding was temporary.218 Subsequently, House Bill (HB) 480, the Graduate Medical Education Expansion Grant Program Act, tasked HSD with the creation of a GME grant program to encourage the establishment or expansion of residency programs focused on general internal medicine or family medicine, general psychiatry, and general pediatric medicine.219 The laudable work of the GME Expansion Review Board & Advisory Group has led to a strategic plan which, upon implementation, would result in training an additional 149 residents over a five-year period.220 Since several of these GME programs already have a footprint, further expansion could build on this foundation.
Residency expansion could involve direct state funding for additional slots, with a focus on FQHCs, rural clinics, and additional specialties where a demonstrated critical need exists. State-funded graduate medical education can better train practitioners for a state’s distinct needs. And the more residents train in New Mexico, the likelier they are to stay in New Mexico.
New Mexico’s loan repayment incentives require that health care professionals work two years in an underserved area. These requirements are more modest than the debt forgiveness incentives provided by neighboring states (Texas, Arizona, and Colorado).221 The Legislature and the Governor increased funding for the Health Professional Loan Repayment Program (which only had funding last year to approve 60 out of 649 applications) for payments capped at $25,000 annually. This new funding extends loan repayments from two to three years and expands the program to include specialists.222 Nevertheless, with hundreds of eligible new physicians’ applications being rejected, while neighboring states provide more generous packages, we would recommend restructuring to create a loan refinance program capped at $200,000 ($40,000 per year for five years). This program should defer principal and loan interest payments for five years, during service in a New Mexico HPSA. Loans can then be forgiven upon completion of the five-year period, with an option to reapply until the entirety of a physician’s medical school debt is forgiven. (This is a variation of a recommendation from the New Mexico Health Care Workforce Committee’s 2022 Report; the Committee recommended the Health Professional Loan Repayment Program cap be doubled to $150,000 over three years with the option to reapply until the entire loan balance is repaid.)223
As New Mexico invests in its provider pipeline, it is important to remember that investments will take years to materialize. This chapter describes a series of recommendations, however, which could result in a stronger and more diverse healthcare workforce, if New Mexico makes critical investments in recruiting and retaining talent.224
It will be critical to build a coalition in support of some of these reforms. Addressing the provider shortage may require reforms to medical malpractice policy, which may not be politically feasible. Bills that have previously proposed modest limitations on medical malpractice payouts for independent providers struggling to operate have languished in the Legislature.225 It remains to be seen if pressure for reforms will increase, as the provider shortage becomes even more acute.
Despite these limiting factors, New Mexico has ample opportunity to address the provider shortage with creative and thoughtful investments in its provider pipeline, its existing providers, and the methods by which care is delivered and compensated.

New Mexico is at a critical juncture in its work to make health care more accessible, affordable and equitable for the state’s residents. Several dynamics specific to the state’s health care landscape make this goal challenging. As a rural state, it can be difficult to ensure access to providers throughout New Mexico. New Mexico’s high premiums and out-of-pocket costs can make insurance policies available on the exchange unaffordable for some. Plans on beWellnm are unattainable for many due to income thresholds or immigration status requirements. Alternatives to the exchange, which include NMMIP and private markets, are often prohibitively expensive. New Mexico’s large indigenous and immigrant populations may be skeptical of state institutions and face unique barriers to accessing health care.
To meet these challenges, New Mexico has proposed several innovative health access initiatives. This report has examined the impacts of NAPA, CEP and Medicaid Forward.
• We recommend that New Mexico consider a strategic shift for NAPA, to prioritize outreach and relationship-building with tribal communities. This outreach would be most effective if the state partnered with existing community programs that have built trust and partnerships with indigenous populations.
• For successful CEP implementation, New Mexico’s strategy should include robust outreach, customer support, language accessibility, adequate funding, an enrollment process that is accessible and integrated with beWellnm’s system, and sustained stakeholder engagement to remain responsive to potential enrollees.
• We conclude that Medicaid Forward could make health care more inclusive if it is buttressed by sustainable funding, carefully considers its impacts on providers and carriers, and conducts continuous program evaluation to keep pace with evolving health care needs and a dynamic federal regulatory environment.
Addressing the provider shortage is foundational to the success of all of these programs. New Mexico can begin to address the provider shortage through several measures designed to make the state more attractive to providers, relative to its neighbors. These measures include increasing reimbursement rates, addressing medical malpractice premiums, streamlining credentialing processes, and making insurers accountable for adding new providers to their payroll systems in a timely manner.
New Mexico is ready to meet these formidable challenges with strong, creative, and responsive solutions.
ACA Affordable Care Act
ASO Administrative Services Only
BHP Basic Health Program
BRFSSS Behavioral Risk Factor Surveillance System Survey
CEP Coverage Expansion Plan
CHIP Children’s Health Insurance Program
CHW Community Health Worker/Aide
CMS Centers for Medicare and Medicaid Services
COVID-19 Coronavirus Disease 2019
D.O. Doctor of Osteopathic Medicine
DACA Deferred Action for Childhood Arrivals
EMSA Emergency Medical Services for Aliens
ESI Employer-Sponsored Insurance
FMAP Federal Medical Assistance Percentage
FPL Federal Poverty Limit
FQHC Federally Qualified Health Centers
FTE Full-Time Employees
GRT Gross Receipt Tax
HB House Bill (New Mexico House of Representatives)
HCAF Health Care Affordability Fund (New Mexico)
HSD Human Services Department (New Mexico)
HSPA Healthcare Provider Shortage Area
IBIS Indicator-Based Information System (New Mexico)
IHS Indian Health Service
ITIN Individual Taxpayer Identification Number
LIPP Low-Income Premium Program (Managed through NMMIP)
M.D. Doctor of Medicine
MCO Managed Care Organization
NAPA Native American Premium Assistance
NATAC Native American Technical Advisory Committee
NMMIP New Mexico Medical Insurance Pool (also known as ‘High Risk Pool’)
OBGYN Obstetrician and Gynecologist
OSI Office of the Superintendent of Insurance (New Mexico)
PHE Public Health Emergency
PRC Purchased/Referred Care
PRWORA The Personal Responsibility and Work Opportunity Reconciliation Act of 1996
RGIS Resource Geographic Information System (New Mexico)
SB Senate Bill (New Mexico State Senate)
SNAP Supplemental Nutrition Assistance Program
SSI Social Security Insurance
SSN Social Security Number
UNM University of New Mexico
Data
OSI tasked the University of New Mexico with administering a statewide survey to learn more about health care and health insurance access among state residents. The survey was administered from May 3-30, 2023 to 2,000 New Mexican residents. This report examines the data from the survey to draw further conclusions about the state of health care and health insurance access across different demographics.
Health Professional Shortage Areas (HPSA)
This report also used the Health Professional Shortage Area data from Health Resources and Service Administration (HRSA). HRSA identifies HPSAs as areas, facilities, or populations as medically underserved through a scoring process.226 The report focuses on shortages in primary care.
New Mexico Resource Geographic Information System (RGIS) Program and Clearinghouse
The report used GIS data from RGIS compiled by a team at the University of New Mexico (UNM). The New Mexico legislature tasked UNM with creating and maintaining a database of digital geospatial data in 2013.227 The RGIS depository includes a multitude of datasets on boundaries, locations, census data, and other datasets related to the topography of New Mexico. All datasets used for this report are publicly available on the RGIS website.
Figure 6 | 30-minute driving distance coverage of medical facilities, FQHC, and IHS
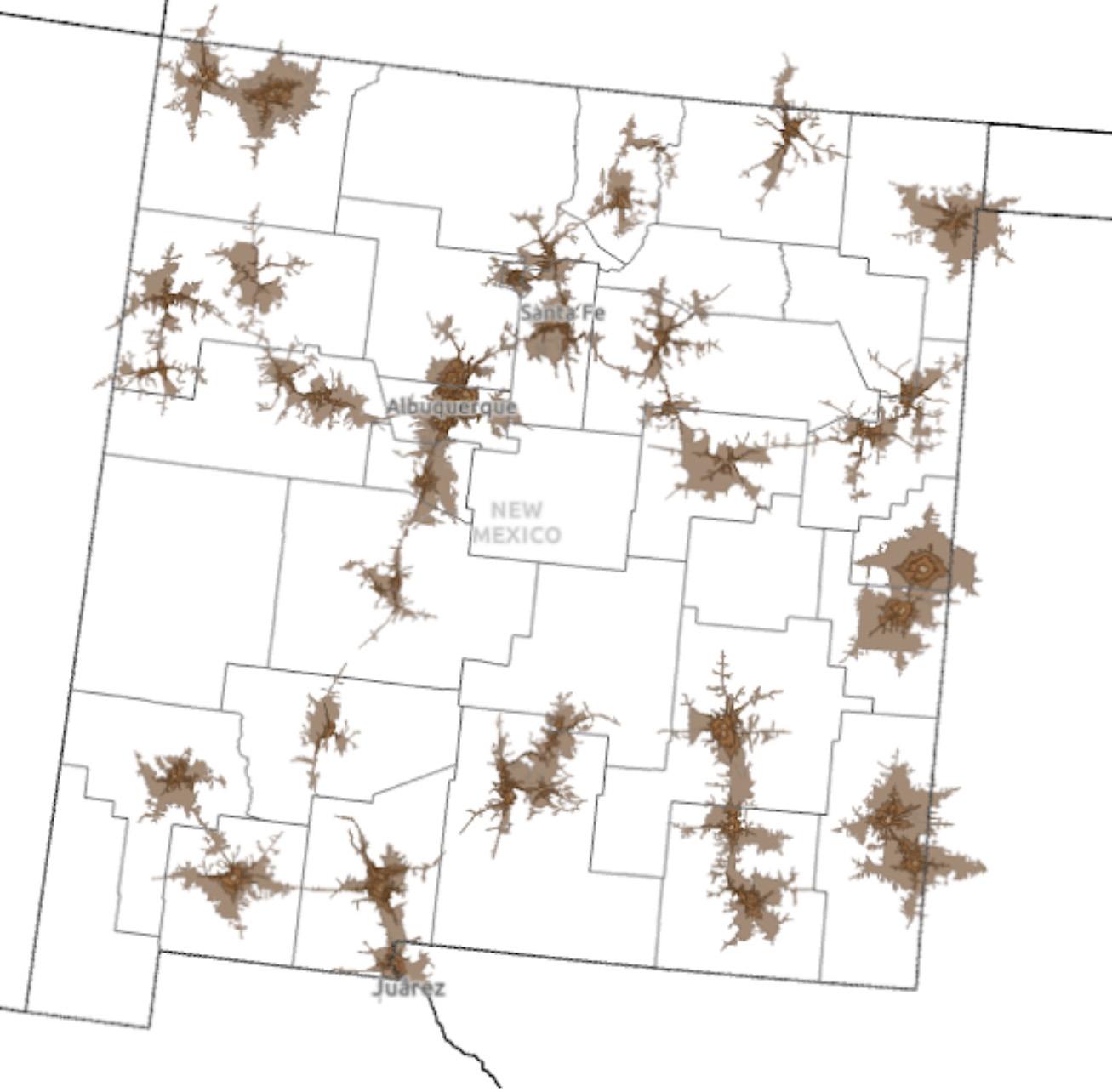





Heather Howard is a Professor of the Practice at Princeton University’s School of Public and International Affairs, where she co-directs the Global Health Program and is a faculty affiliate of the Center for Health & Wellbeing. She is also director of the State Health and Value Strategies program, a Robert Wood Johnson Foundation-funded program focused on assisting states with transforming their health care systems to be affordable, equitable and innovative. She served as New Jersey’s Commissioner of Health and Senior Services from 2008-2010. She also has significant federal experience, having worked as Senator Jon Corzine’s Chief of Staff, as Associate Director of the White House Domestic Policy Council and Senior Policy Advisor for First Lady Hillary Clinton, as an Honors Attorney in the U.S. Department of Justice’s Antitrust Division Health Care Task Force, and for the U.S. Representative Nita Lowey (D-NY). She received her B.A. from Duke University and her J.D. from NYU School of Law.
Dan is the Deputy Director of the State Health and Value Strategies program where heassists in managing and coordinating the technical assistance providers serving the states and works with states to identify their assistance needs and policy goals. He was deeply involved in the implementation of the Affordable Care Act at the state level as Deputy Chief of Staff for Rhode Island’s Lieutenant Governor. Dan also served as the principal subject matter expert for the Rhode Island Healthcare Reform Commission on Health Insurance Exchange and project director for the State Innovation Model (SIM). Dan serves as a Lecturer in Public Affairs at the School of Public and International Affairs at Princeton University. He received a MBA from Providence College and his BA from Brown University.
Mary Grace is a graduate student in Princeton’s Master in Public Affairs program, focusing on international relations and public health. Prior to coming to Princeton, she worked to expand the global affordability of and access to critical women’s health commodities at the Clinton Health Access Initiative. Mary Grace grew up in Miami, FL and graduated from Harvard College in 2017 with a degree in Social Studies. Her interest in health policy began as an intern in the Obama White House, where she read and responded to constituent mail concerning the Affordable Care Act.
Ria is a second year MPA student, focused on international relations and Arctic policy at Princeton. She was born and raised in Alaska, USA, splitting her time between Hope, a small gold mining town and Anchorage, the big city. She received her undergraduate degree in economics from Williams College in Massachusetts. Prior to Princeton, Ria commercially fished out of Larsen Bay, Kodiak for three summers, and worked as an economist for the Alaska Department of Revenue the rest of the year. At the Department of Revenue, she provided forecasts of the State’s non-petroleum revenue, produced revenue analyses that served as the foundation for budget negotiations, and performed fiscal policy analysis for proposed legislation. Her work spanned tax policy, natural resource policy, international market impacts, and economic development. In her free time, Ria enjoys hiking, cross-country skiing, live music, and any excuse to be on a boat.
Laura graduated summa cum laude in 2020 from Princeton’s Politics department with a certificate in American Studies. She received the John G. Buchanan Prize in Politics, which is awarded to the senior who has attained during junior and senior years the highest standing in the department and was elected to Phi Beta Kappa. Laura’s summer internships include working for Springboard Collaborative, a nonprofit dedicated to closing the literacy gap; for Senator José Rafael Nadal Power of Puerto Rico; and for federal Magistrate Judge Cheryl L. Pollak in the Eastern District of New York. Her senior thesis focused on how U.S. voters respond to disclosures of mental illness experiences from candidates seeking elected office. Laura is also a scholar in the Princeton Scholars in the Nation’s Service Initiative (SINSI).






Rita was born and raised in the U.S.-Mexico border region of San Diego County and is the daughter of Mexican Immigrants. She served in the Washington, D.C. office of Rep. Juan Vargas (CA-51), where she worked closely on immigration and border issues as a press aide and special assistant. Rita later worked in the office of Los Angeles Mayor Eric Garcetti as Associate Director of Immigrant Affairs, helping lead major programs and initiatives to support immigrant and refugee communities in Los Angeles. More recently, Rita served as Executive Director of the City of San Diego’s Office of Immigrant Affairs, an office created by Mayor Todd Gloria to advance San Diego’s welcoming policies. She also served as Director of Global Affairs for Mayor Gloria, overseeing subnational diplomacy issues, San Diego’s Sister City relationships, and growing economic development ties with other countries. During her spare time, Rita enjoys working on her writing projects including short stories and screenplays.
Andre’ is a master’s student in Public Affairs at Princeton University. He earned his Bachelor’s in Law and Policy from the University of Washington. With experience in state and local government, Andre has worked on criminal justice reform, reentry, workforce development, and education. Recently, he has continued to develop his expertise in building safe and equitable communities through his work with the cities of Chicago and Philadelphia. He graduated from the University of Washington with a BA in Law and Policy. In his free time, Andre enjoys being with his wife, Jazmyne, and their four children.
Yiping was born in Shenzhen, China, and raised in the Southside of Chicago. During undergraduate, Yiping discovered her passion for rigorous empirical research methods through her major in psychology. After college, she pivoted from using puppet shows to study infants’ perception of causality to using randomized controlled trials to examine the effectiveness of anti-poverty policies in the United States. Yiping came to Princeton after three years at J-PAL North America, an economic research center that sits at MIT. There, she supported state and local governments in designing and implementing randomized evaluations to answer priority policy questions. She also synthesized academic research into accessible products for a general audience. In her free time, Yiping enjoys trading skincare tips with her peers while sipping on perfectly brewed loose-leaf teas.
A fifth-term state lawmaker in New Jersey, where he serves as a State Senator, Raj was the first Indian-Bengali state legislator elected in American history and the second South Asian American to be elected in New Jersey. He is committed to defending democracy and human rights and providing a voice for vulnerable and marginalized communities. A former healthcare and technology entrepreneur, Deputy Mayor of Jersey City, and local prosecutor, Raj enlisted in the U.S. Marines as a reservist two weeks after the September 11th attacks and served in military intelligence as a Sergeant. In the State Legislature, he has been a primary sponsor of numerous enacted laws focused on sustainability and environmental protection, expanding mandatory insurance coverage of healthcare services and prescription benefits, protecting reproductive autonomy, and myriad other issues. Raj spends most of his spare time with his wife Natasha and their two children.
Brontë is a second year master’s student in Public Affairs at Princeton University. She has previously worked at the Johns Hopkins Poverty and Inequality Research Lab and served as the manager of community health at Central Kenilworth Avenue Revitalization Community Development Corporation. Most recently, she has been working with the federal Administration for Children and Families, evaluating anti-poverty pilot programs including the Diaper Distribution Demonstration and Medical-Legal Partnerships Plus. When not working, Brontë enjoys quilting with her partner and failing to teach her greyhound to retrieve a ball.
Gillian is a Master in Public Affairs student at Princeton SPIA pursuing concentrations in domestic and health policy. She recently completed an internship on the health policy team at the Center for American Progress, where she was sponsored by the Peter G. Peterson Foundation. Prior to Princeton, she built a career as a market strategist in the healthcare sector, most recently as the Director of Product Marketing at a caregiver support solution. She graduated from Smith College with a BA in Philosophy and Logic. In her spare time, she acts in theater productions and plays with her two cats.
1. “Nuclear Princeton - People,” Nuclear Princeton, n.d., https://nuclearprinceton.princeton.edu/people-manhattan-project.
2. “Nuclear Princeton: Impacts on Indigenous Communities,” Nuclear Princeton, n.d., https://nuclearprinceton.princeton.edu/resources.
3. NAPA and CEP are two of the three initiatives that comprise the Health Care Affordability Fund (HCAF), a law that provides state financial assistance to income-eligible New Mexicans. The program components are: (1) individual market premium assistance and out-of-pocket subsidies, (2) a small business premium relief program that subsidizes employers with 50 employees or fewer who provide health insurance to their employees with a 10% reduction in premiums, and, (3) CEP, a program that provides state financial assistance to individuals who do not qualify for insurance coverage from other sources.
4. New Mexico Office of Superintendent of Insurance. In discussion with authors. October 2023.
5. Morgan Lee, “Governor of New Mexico Sees Progress on Health, Poverty,” AP News, May 5, 2023, https://apnews.com/article/new-mexico-governor-health-abortion-6acbd4f4d5a0d7740e3f5a9eff2272a3.
6. New Mexico Department of Health, “Office of Health Equity,” accessed November 3, 2023, https://www.nmhealth.org/about/asd/ohe/.
7. State Health & Value Strategies, “Talking about Anti-Racism and Health Equity: Discussing Racism,” August 2021, https://www.shvs.org/wp-content/uploads/2021/08/TalkingAbout-Anti-Racism-Health-Equity-1-of-3.pdf.
8. U.S. Census Bureau, “U.S. Census Bureau QuickFacts: New Mexico,” n.d., https://www. census.gov/quickfacts/fact/table/NM/RHI325222#RHI325222.
9. “History | NM Indian Affairs Department,” New Mexico Indian Affairs Department, n.d., https://www.iad.state.nm.us/about-us/history/.
10. “US Census: Census Bureau Releases Estimates of Undercount and Overcount in the 2020 Census,” n.d., https://www.census.gov/newsroom/press-releases/2022/2020-census-estimates-of-undercount-and-overcount.html.
11. “US Census: Income in the United States,” n.d., https://www.census.gov/library/publications/2023/demo/p60-279.html.
12. “US Bureau of Labor and Statistics,” n.d., https://www.bls.gov/lau/.
13. U.S. Census Bureau, “U.S. Census Bureau QuickFacts: New Mexico.”
14. KFF, “Health Insurance Coverage of the Total Population,” 2022, https://www.kff.org/ other/state-indicator/total-population/?currentTimeframe=0&selectedRows=%7B%22sta tes%22:%7B%22new-mexico%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
15. U.S. Census Bureau, “U.S. Census Bureau QuickFacts: New Mexico.”
16. StatsAmerica, “Population Estimate for 2022,” StatsAmerica, accessed November 21, 2023, https://www.statsamerica.org/sip/rank_list.aspx?rank_label=pop1&ct=S18.
17. LHHS New Mexico Rural Health Plan. IBIS uses two categories for rural areas: Small Town Rural (counties containing towns no larger than 10,000 people) and Larger Town Rural (counties containing towns larger than 10,000 people). The IBIS has no “frontier” designation. The National Rural Health Association defines “frontier” as a service area with a population density of fewer than or equal to 6 people per square mile. By pop-
ulation density, frontier areas are more dense than Small Town Rural counties (which have a population density of 2 people per square mile), but less dense than Larger Town Rural counties (which have a population density of 11 people per square mile). (https:// www.ruralhealth.us/getattachment/Advocate/Policy-Documents/NRHAFrontierDefPolicyPaperFeb2016.pdf.aspx)
18. Marjorie Childress, “Lawmakers Tackled New Mexico’s Crisis of Rural Health Care Workers. It Wasn’t Enough. | New Mexico In Depth,” New Mexico In Depth, October 11, 2023, https://nmindepth.com/2023/lawmakers-tackled-new-mexicos-crisis-of-ruralhealth-care-workers-it-wasnt-enough/.
19. Stephanie Chavez, “Federal Map Shows Disparities in Broadband Access across New Mexico,” KRQE News, June 20, 2021, https://www.krqe.com/news/new-mexico/federal-map-shows-disparities-in-broadband-access-across-new-mexico/.
20. Becky Sullivan, “The Navajo Nation’s Water Rights Are at the Center of a Supreme Court Case : NPR,” NPR, March 20, 2023, https://www.npr.org/2023/03/20/1164852475/ supreme-court-navajo-nation-water-rights.
21. Bureau of Health Workforce, “Scoring Shortage Designations | Bureau of Health Workforce,” Bureau of Health Workforce, accessed November 19, 2023, https://bhw.hrsa.gov/ workforce-shortage-areas/shortage-designation/scoring.
22. Childress, “Lawmakers Tackled New Mexico’s Crisis of Rural Health Care Workers. It Wasn’t Enough. | New Mexico In Depth.”
23. Rural Health Planning Workgroup, “New Mexico Rural Health Plan,” accessed November 16, 2023, https://www.nmlegis.gov/handouts/LHHS%20092519%20Item%202%20 New%20Mexico%20Rural%20Health%20Plan.pdf.
24. Rural Health Planning Workgroup, “New Mexico Rural Health Plan” (New Mexico Legislature, 2019), https://www.nmlegis.gov/handouts/LHHS%20092519%20Item%202%20 New%20Mexico%20Rural%20Health%20Plan.pdf.
25. Rural Health Planning Workgroup, “New Mexico Rural Health Plan” (New Mexico Legislature, 2019), https://www.nmlegis.gov/handouts/LHHS%20092519%20Item%202%20 New%20Mexico%20Rural%20Health%20Plan.pdf.
26. Regina Eddie et al., “Practicing Tribal Sovereignty Through a Tribal Health Policy: Implementation of the Healthy Diné Nation Act on the Navajo Nation,” Preventing Chronic Disease 19 (November 23, 2022): 220106, https://doi.org/10.5888/pcd19.220106.
27. United States Government Accountability Office, “Indian Health Service: Agency Faces Ongoing Challenges Filling Provider Vacancies” (United States Government Accountability Office, August 2018), https://www.gao.gov/assets/gao-18-580.pdf.
28. Medicaid.gov, “Medicaid Eligibility,” Government, Medicaid.gov, n.d., https://www.medicaid.gov/medicaid/eligibility/index.html.
29. “Personal Responsibility and Work Opportunity Reconciliation Act of 1996,” Pub. L. No. Public Law 104-193 (1996), https://www.congress.gov/104/plaws/publ193/PLAW104publ193.pdf.
30. “Health Coverage for Lawfully Present Immigrants,” HealthCare.gov, accessed November 11, 2023, https://www.healthcare.gov/immigrants/lawfully-present-immigrants/.
31. Shelby Gonzales, “Efforts to Repeal the Biden Administration’s Public Charge Rule Harm Children and Families Living in the United States,” Center on Budget and Policy Priorities, June 13, 2023, https://www.cbpp.org/blog/efforts-to-repeal-the-biden-administrations-public-charge-rule-harm-children-and-families.
32. David Beal and Karen J. Foli, “Affordability in Individuals’ Healthcare Decision Making: A Concept Analysis,” Nursing Forum 56, no. 1 (2021): 188–93, https://doi.org/10.1111/ nuf.12518.
33. “Distribution of Total Population by Federal Poverty Level,” Kaiser Family Founda-
tion, accessed November 11, 2023, https://www.kff.org/other/state-indicator/distribution-by-fpl/.
34. Conway, Douglas and Branch, Breuna, “Health Insurance Coverage Status and Type by Geography: 2021 and 2022,” Census.gov, accessed November 11, 2023, https://www. census.gov/library/publications/2023/acs/acsbr-015.html.pset
35. “Marketplace Plan Year 2024 Open Enrollment Fact Sheet | CMS,” CMS.gov, October 25, 2023, https://www.cms.gov/newsroom/fact-sheets/marketplace-plan-year-2024open-enrollment-fact-sheet.
36. New Mexico Together for Healthcare, “Poll Finds New Mexicans Want Action on Affordable Healthcare Reforms,” New Mexico Together for Health Care (blog), March 24, 2022, https://nmtogether4health.org/media-press/poll-finds-new-mexicans-want-action-on-affordable-healthcare-reforms/.
37. “What We’re Hearing from Consumers in New Mexico,” Consumer Financial Protection Bureau, August 10, 2023, https://www.consumerfinance.gov/about-us/blog/what-werehearing-from-consumers-in-new-mexico/.
38. “Basis for Health Services | Fact Sheets,” accessed November 9, 2023, https://www.ihs. gov/newsroom/factsheets/basisforhealthservices/.
39. New Mexico Center for Law and Poverty, “Resource List: Health Care for Immigrants in New Mexico,” New Mexico Center for Law and Poverty, October 2013, https://nmpovertylaw.org/wp-content/uploads/2020/07/Handout-Resource-List-Health-Care-Immigrants-Final-2014-07-07.pdf.
40. New Mexico Medical Insurance Pool, “Who We Are,” accessed October 8, 2023, https:// www.nmmip.org/about-us/who-we-are/.
41. “Federal Poverty Level (FPL),” HealthCare.gov, accessed November 9, 2023, https:// www.healthcare.gov/glossary/federal-poverty-level-fpl/.
42. beWellnm staff in discussion with the authors, October 18, 2023.
43. Jessica S Banthin et al., “The Uninsured in New Mexico” (The Urban Institute, December 2019), https://www.urban.org/sites/default/files/publication/101427/the_uninsured_ in_new_mexico_final_v2_1.pdf.
44. The Low-Income Premium Program (LIPP) was designed to help persons who qualify for NMMIP coverage remain on pool coverage by offering a reduced premium. LIPP offers reduced premiums of between 25-75%, based on household size and income. Individuals enrolled in the LIPP would qualify for CEP in the absence of that program. LIPP enrollees will have the option to participate in CEP.
45. Office of the Superintendent of Insurance, “The Coverage Expansion Plan,” August 18, 2023, file:///Users/andrejimenez/Downloads/CEP%20Proposal_230821.pdf.
46. NM Together for Healthcare, “HB 400: ‘State Administered Health Coverage Plan,’” n.d., https://nmtogether4health.org/wp-content/uploads/2023/03/Revised-HB-400-OnePager-3.06.2023_FINAL.pdf.
47. “2023 Regular Session - HB 400,” 400, accessed October 30, 2023, https://www.nmlegis. gov/Legislation/Legislation?chamber=H&legType=B&legNo=400&year=23.
48. Matthew Buettgens et al., “Medicaid Forward in New Mexico: Health Coverage, Health Care Spending, and Government Costs” (Urban Institute, September 2023), https:// www.urban.org/sites/default/files/2023-09/Medicaid%20Forward%20in%20New%20 Mexico.pdf.
49. “2023 Regular Session - HB 400,” 400, accessed October 30, 2023, https://www.nmlegis. gov/Legislation/Legislation?chamber=H&legType=B&legNo=400&year=23.
50. Office of the Governor Michelle Lujan Grisham, “Gov. Establishes Health Care Affordability Fund, Eliminate Copays for Behavioral Health Services | Office of the GovernorMichelle Lujan Grisham,” April 8, 2021, https://www.governor.state.nm.us/2021/04/08/
gov-establishes-health-care-affordability-fund-eliminate-copays-for-behavioral-health-services/.
51. Forward Together, “New Mexico Healthcare Affordability Fund,” Forward Together, 2020, https://forwardtogether.org/tools/new-mexico-healthcare-affordability-fund/.
52. “Office of Superintendent of Insurance.” Accessed February 11, 2024. https://www.osi. state.nm.us/pages/misc/health-insurance-marketplace-affordability-program; The New Mexico Office of Superintendent of Insurance. “Health Care Affordability Fund Annual Report to the State Legislature.” The New Mexico Office of Superintendent of Insurance, October 31, 2023.
53. beWellnm, “New Mexico’s Health Insurance Marketplace Affordability Program,” November 3, 2022, https://nfpnewmexico.my.site.com/knowledgebase/s/article/ New-Mexico-Health-Insurance-Marketplace-Affordability-Program.
54. beWellnm, “Turquoise Plans,” November 3, 2022, https://nfpnewmexico.my.site.com/ knowledgebase/s/article/Turquoise-Plans.
55. Office of the Governor Michelle Lujan Grisham, “Gov. Establishes Health Care Affordability Fund, Eliminate Copays for Behavioral Health Services,” April 8, 2021, https://www.governor.state.nm.us/2021/04/08/gov-establishes-health-care-affordability-fund-eliminate-copays-for-behavioral-health-services/.
56. beWellnm, “Mission & History,” accessed October 8, 2023, https://bewellnm.com/mission-history/.
57. Centers for Medicare & Medicaid Services, “Kentucky, Maine, and New Mexico Launch State Marketplaces for 2022 Coverage,” October 4, 2021, https://www.cms.gov/newsroom/press-releases/kentucky-maine-and-new-mexico-launch-state-marketplaces2022-coverage.
58. Louise Norris, “New Mexico Health Insurance Consumer Guide,” healthinsurance. org, September 19, 2023, https://www.healthinsurance.org/states/health-insurance-new-mexico/. Updated numbers are available on beWellnm dashboard at: Open Enrollment Data | beWellnm, https://bewellnm.com/open-enrollment-data/.
59. “New Mexico Medicaid Releases Request for Proposals for New Turquoise Care Contracts | New Mexico Human Services Department,” New Mexico Human Services Department, accessed November 27, 2023, https://www.hsd.state.nm.us/2022/10/03/ new-mexico-medicaid-releases-request-for-proposals-for-new-turquoise-care-contracts/.
60. Kenneth Finegold et al., “Trends in the U.S. Uninsured Population, 2010-2020” (Assistant Secretary for Planning and Evaluation, February 11, 2021), https://aspe.hhs.gov/ sites/default/files/private/pdf/265041/trends-in-the-us-uninsured.pdf.
61. KFF, “Status of State Medicaid Expansion Decisions: Interactive Map,” KFF (blog), October 4, 2021, https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.
62. Perry Undem, “How New Mexicans Feel about Affordability and Healthcare Reform,” February 2022, https://nmtogether4health.org/wp-content/uploads/2022/03/NM-Affordability-Report-1.pdf.nt
63. New Mexico Human Services Department, “Centennial Care Overview,” accessed October 8, 2023, https://www.hsd.state.nm.us/lookingforassistance/centennial-care-overview/.
64. KFF, “Medicaid Enrollment and Unwinding Tracker,” KFF (blog), November 1, 2023, https://www.kff.org/report-section/medicaid-enrollment-and-unwinding-tracker-overview/.
65. Austin Fisher, “Nearly 60,000 New Mexicans Purged from the Medicaid Rolls (so Far),” Source New Mexico (blog), July 12, 2023, https://sourcenm.com/2023/07/12/nearly-
60000-new-mexicans-purged-from-the-medicaid-rolls-so-far/.
66. “Medicaid 1115 Waiver Renewal | New Mexico Human Services Department,” accessed November 7, 2023, https://www.hsd.state.nm.us/medicaid-1115-waiver-renewal/.
67. KFF, “Medicaid Enrollment and Unwinding Tracker.”
68. Nicole Comeaux, “New Mexico Centennial Care 2.0 Medicaid 1115 Demonstration” (New Mexico Human Services Department, 2020), https://www.medicaid.gov/sites/default/files/2020-07/nm-centennial-care-ca.pdf.
69. “Tribal Health Spotlight | FTI Consulting,” accessed November 7, 2023, https://www. fticonsulting.com/insights/articles/tribal-health-spotlight-strategies-traditional-healing-medicaid.
70. “About Section 1115 Demonstrations | Medicaid,” accessed November 19, 2023, https:// www.medicaid.gov/medicaid/section-1115-demonstrations/about-section-1115-demonstrations/index.html.
71. “Section 1115 Research and Demonstration Waivers : MACPAC,” accessed November 19, 2023, https://www.macpac.gov/subtopic/section-1115-research-and-demonstration-waivers/.
72. New Mexico Medical Insurance Pool, “Who We Are,” accessed October 8, 2023, https:// www.nmmip.org/about-us/who-we-are/.
73. Colin Baillio, Meeting between Colin Baillio and Princeton University, September 25, 2023.
74. Louise Norris, “Health Insurance and High-Risk Pools,” healthinsurance.org, accessed October 8, 2023, https://www.healthinsurance.org/obamacare/risk-pools/.
75. Indian Health Service, “For Patients,” accessed October 8, 2023, https://www.ihs.gov/ forpatients/
76. Indian Health Service, “Purchased/Referred Care (PRC),” Indian Health Service, June 2016, https://www.ihs.gov/newsroom/factsheets/purchasedreferredcare/.
77. beWellnm, “How Native Americans Can Get No-Cost to Low-Cost Health Insurance in 2023,” accessed October 8, 2023, https://bewellnm.com/get-answers/health-plan-howtos/how-native-americans-can-get-no-cost-to-low-cost-health-insurance-in-2023/.
78. “New Indian Health Service Funding Provides Stability, but Long-Standing Issues Remain - OPB,” accessed November 9, 2023, https://www.opb.org/article/2023/01/20/ new-indian-health-service-funding-provides-stability-but-long-standing-issues-remain/.
79. “The Road to Reproductive Justice: Native Americans in New Mexico - Forward Together,” accessed November 10, 2023, https://forwardtogether.org/tools/the-road-to-reproductive-justice-native-americans-in-new-mexico/.
80. Kenneth Lucero, “Improving the New Mexico Indian Health Care System: Pueblo Core Values and Federal Policy” (Arizona State University, 2015), https://core.ac.uk/download/pdf/79576239.pdf.
81. Tom Betlach, Zoom interview with authors, November 13, 2023
82. Banthin et al., “The Uninsured in New Mexico.”
83. Email exchange with beWellnm staff, December 8, 2023.
84. beWellnm staff in discussion with the authors, October 18, 2023.
85. beWellnm staff, Center on Law Poverty, Office of the Superintendent of Insurance, Tom Betlach, and University of New Mexico Hospital in conversations with the authors, October 16 - 19, 2023 and November 13, 2023.
86. Sarah Dewees and Benjamin Marks, “Twice Invisible: Understanding Rural Native America,” Research Note (First Nations Development Institute, April 2017), https://www.
usetinc.org/wp-content/uploads/bvenuti/WWS/2017/May%202017/May%208/Twice%20 Invisible%20-%20Research%20Note.pdf.
87. New Mexico’s Health Indicator Data & Statistics, “Percentage of Persons with a Primary Medical Provider by Race/Ethnicity, New Mexico, 2017-2021,” November 2, 2023, https://ibis.doh.nm.gov/indicator/view/HlthCarePriProv.RacEth.html.
88. A network analysis conducted in ArcGIS Pro created a 30-minute driving distance service area of medical facilities, FQHCs, and IHS available from RGIS NM. Using the area of land covered and applying the percentage to the population in each tribal land or pueblo, an estimate of individuals living in an area outside of the service area is calculated. Because population density is not taken into consideration, the estimates here are merely suggestive.
89. “New Indian Health Service Funding Provides Stability, but Long-Standing Issues Remain - OPB.”
90. Jenny Chiang, “Medical Debt Implications in Native American Communities,” Community Catalyst, April 28, 2022, https://communitycatalyst.org/posts/medical-debt-implications-in-native-american-communities/.
91. Usha Lee McFarling, “There Aren’t Nearly Enough Native American Physicians. A Crash Course in Medicine Seeks to Change That,” STAT, July 21, 2022, https://www.statnews. com/2022/07/21/native-american-physicians-crash-course-in-medicine/.
92. Jeanette Dedios, “Larry Williams Wasn’t given a Navajo Translator to Speak to His Doctor; He Died after His Visit,” Source NM, March 3, 2023, https://sourcenm. com/2023/03/03/larry-williams-suffered-a-serious-medical-episode-and-needed-anavajo-interpreter-to-speak-to-his-doctor-that-didnt-happen-and-he-died-after-hisvisit/.
93. New Mexico’s Health Indicator Data & Statistics, “American Indian/Alaska Native Race/ Ethnicity Community Report,” NM-IBIS, accessed November 9, 2023, https://ibis.doh. nm.gov/community/indicators/HealthStatusOutcomes/RacEthDOH.
94. “New Mexico,” Centers for Disease Control and Prevention, accessed November 19, 2023, https://www.cdc.gov/nchs/pressroom/states/newmexico/nm.htm.
95. Elizabeth Hlavinka, “COVID-19 Further Strains Care Disparities Among Native Americans,” Medpage Today, May 21, 2020, https://www.medpagetoday.com/infectiousdisease/covid19/86633.sec
96. Ivy Hurwitz et al., “Disproportionate Impact of COVID-19 Severity and Mortality on Hospitalized American Indian/Alaska Native Patients,” PNAS Nexus 2, no. 8 (August 1, 2023): pgad259, https://doi.org/10.1093/pnasnexus/pgad259.
97. Tommy Lopez, “New Research Shows COVID-19 Impacted Otherwise Healthy Native Americans Disproportionately,” KOB 4, September 7, 2023, https://www.kob.com/ new-mexico/new-research-shows-covid-19-impacted-otherwise-healthy-native-americans-disproportionately/.
98. Banthin et al., “The Uninsured in New Mexico.”
99. Indian Health Service, “Purchased/Referred Care (PRC).”
100. “Santa Ana Health Center,” Indian Health Service, accessed November 9, 2023, https:// www.ihs.gov/Albuquerque/healthcarefacilities/santaana/.
101. Kenneth Lucero, “Improving the New Mexico Indian Health Care System: Pueblo Core Values and Federal Policy.”
102. Indian Health Service, “Purchased/Referred Care (PRC).”
103. Mark Walker, “Fed Up With Deaths, Native Americans Want to Run Their Own Health Care,” The New York Times, October 15, 2019, https://www.nytimes.com/2019/10/15/us/ politics/native-americans-health-care.html.
104. New Mexico Human Services Department, “Centennial Care Overview.”
105. KFF, “Medicaid Coverage Rates for the Nonelderly by Race/Ethnicity,” accessed November 9, 2023, https://www.kff.org/medicaid/state-indicator/nonelderly-medicaid-rate-by-raceethnicity/?currentTimeframe=0&selectedRows=%7B%22states%22 :%7B%22new-mexico%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
106. Banthin et al., “The Uninsured in New Mexico.”
107. Ibid.
108. beWellnm staff in discussion with the authors, October 18, 2023.
109. Kenneth Lucero, “Improving the New Mexico Indian Health Care System: Pueblo Core Values and Federal Policy.”
110. beWellnm staff in discussion with the authors, October 18, 2023.
111. Dana Hedgpeth, “How Native Americans Were Vaccinated against Smallpox, Then Pushed off Their Land,” Washington Post, March 28, 2021, https://www.washingtonpost. com/history/2021/03/28/native-americans-vaccine-smallpox-covid/.
112. Gabriel R. Sanchez and Raymond Foxworth, “Native Americans And COVID-19 Vaccine Hesitancy: Pathways Toward Increasing Vaccination Rates For Native Communities,” Health Affairs Forefront, accessed November 11, 2023, https://doi.org/10.1377/forefront.20210723.390196.
113. beWellnm, “Health Insurance for Native Americans,” 2021, https://www.bewellnm.com/ wp-content/uploads/2021/11/Native-American-Cost-Sharing-Flyer-2021.pdf.
114. beWellnm, “How Native Americans Can Get No-Cost to Low-Cost Health Insurance in 2023,” accessed October 8, 2023, https://bewellnm.com/get-answers/health-plan-howtos/how-native-americans-can-get-no-cost-to-low-cost-health-insurance-in-2023/.ase
115. Kenneth Lucero, “Improving the New Mexico Indian Health Care System: Pueblo Core Values and Federal Policy.”
116. “Native American Technical Advisory Committee,” New Mexico Human Services Department, accessed November 19, 2023, https://www.hsd.state.nm.us/about_the_department/native-american-technical-advisory-committee/.
117. Tom Betlach, Zoom interview with authors, November 13, 2023
118. Eddie et al., “Practicing Tribal Sovereignty Through a Tribal Health Policy.”
119. Tom Betlach, Zoom interview with authors, November 13, 2023
120. beWellnm, “Health Insurance for Native Americans.”
121. Mim Dixon, Strategies for Cultural Competency in Indian Health Care (Washington, D.C. : American Public Health Association, 2006), http://archive.org/details/strategiesforcul0000dixo.
122. Kenneth Lucero, “Improving the New Mexico Indian Health Care System: Pueblo Core Values and Federal Policy.”
123. Heather Sauyaq Jean Gordon, Deana Around Him, and Elizabeth Jordan, “Federal Policies That Contribute to Racial and Ethnic Health Inequities and Potential Solutions for Indigenous Children, Families, and Communities,” ChildTrends, November 3, 2022, https://www.childtrends.org/publications/federal-policies-contribute-racial-ethnic-health-inequities-potential-solutions-indigenous-children-families-communities.
124. Moses Mulumba et al., “Decolonizing Health Governance,” Health and Human Rights 23, no. 1 (June 2021): 259–71.
125. “Diné College Public Health Students Provide Vaccine Education to Navajo Nation Residents through Study,” Northern Arizona University, October 20, 2021, https://nau.edu/
cher/dine-college-nau-rave-study/.
126. Jackie Powder, “Keys to the Navajo Nation’s COVID-19 Vaccination Success,” Johns Hopkins Bloomberg School of Public Health, August 5, 2021, https://publichealth.jhu. edu/2021/keys-to-the-navajo-nations-covid-19-vaccination-success.
127. Terry Tang, “Tribes Credited with Elevating Vaccinations in Rural Arizona,” Associated Press News, May 7, 2022, https://apnews.com/article/covid-health-pandemics-public-arizona-19b7d4293982fafccbf58c5375c49f2a.
128. American Immigration Council, “Immigrants in New Mexico,” American Immigration Council, 2020, https://www.americanimmigrationcouncil.org/sites/default/files/research/immigrants_in_new_mexico.pdf.
129. United States Citizenship and Immigration Service, “Approximate Active DACA Recipients,” March 31, 2020, https://www.uscis.gov/sites/default/files/document/data/Approximate%20Active%20DACA%20Receipts%20-%20March%2031%2C%202020.pdf.
130. American Immigration Council, “Immigrants in New Mexico.”
131. Personal Responsibility and Work Opportunity Reconciliation Act of 1996.
132. Shawn Fremstad, “Trump’s ‘Public Charge’ Rule Would Radically Change Legal Immigration,” November 27, 2018, https://www.americanprogress.org/article/trumps-public-charge-rule-radically-change-legal-immigration/.
133. Gonzales, “Efforts to Repeal the Biden Administration’s Public Charge Rule Harm Children and Families Living in the United States.” https://www.cbpp.org/blog/efforts-to-repeal-the-biden-administrations-public-charge-rule-harm-children-and-families
134. Kaiser Family Foundation, “Key Facts on Health Coverage of Immigrants,” September 17, 2023, https://www.kff.org/racial-equity-and-health-policy/fact-sheet/key-facts-onhealth-coverage-of-immigrants/.
135. Kaiser Family Foundation, “Key Facts on Health Coverage of Immigrants,” September 17, 2023, https://www.kff.org/racial-equity-and-health-policy/fact-sheet/key-facts-onhealth-coverage-of-immigrants/.
136. Office of the Superintendent of Insurance, “The Coverage Expansion Plan.”
137. The map is an estimate created by examining the portion of residents estimated to be undocumented in the state of New Mexico and the breakdown of country of origin for undocumented residents from the Center for Migration Studies. The percentage figures are applied to the 2021 5-year American Community Survey population data of residents in New Mexico with a foreign country of origin. Therefore, the estimates here are only suggestive.
138. Office of the Superintendent of Insurance, “The Coverage Expansion Plan.”
139. U.S. Census Bureau, “U.S. Census Bureau QuickFacts: New Mexico.”
140. “Marketplace Plan Year 2024 Open Enrollment Fact Sheet | CMS,” CMS.gov, October 25, 2023, https://www.cms.gov/newsroom/fact-sheets/marketplace-plan-year-2024open-enrollment-fact-sheet.
141. Ibid.
142. Natasha Murphy, “How States Can Use Section 1332 Waivers To Improve Health Care Affordability and Access,” Center for American Progress (blog), October 23, 2023, https://www.americanprogress.org/article/how-states-can-use-section-1332-waivers-toimprove-health-care-affordability-and-access/.
143. “Health Coverage for Lawfully Present Immigrants,” HealthCare.gov, accessed November 11, 2023, https://www.healthcare.gov/immigrants/lawfully-present-immigrants/.
144. Matthew Buettgens et al., “Medicaid Forward in New Mexico: Health Coverage, Health Care Spending, and Government Costs,” v.
145. Medicaid and CHIP Payment and Access Commission, “Medicaid Buy-In: Program Options and Considerations,” April 2020, https://www.macpac.gov/wp-content/uploads/2020/04/Medicaid-Buy-In-Program-Options-and-Considerations.pdf.
146. KFF, “Federal Medical Assistance Percentage (FMAP) for Medicaid and Multiplier,” accessed November 6, 2023, https://www.kff.org/medicaid/state-indicator/federal-matching-rate-and-multiplier/.
147. NM Together for Healthcare, “HB 400: ‘State Administered Health Coverage Plan.’”
148. Matthew Buettgens et al., “Medicaid Forward in New Mexico: Health Coverage, Health Care Spending, and Government Costs,” ix.
149. New Mexico Together for Healthcare Campaign, “Medicaid Forward: Medicaid Expansion above 133% FPL,” August 25, 2022, 2.
150. Medicaid and CHIP Payment and Access Commission, “Medicaid Buy-In: Program Options and Considerations,” 2.
151. “Percent of Median Income Spent on Health Plans U.S. 2020,” Statista, accessed November 29, 2023, https://www.statista.com/statistics/631987/percent-of-income-spent-onhealth-plan-by-us-employees/.
152. Matt Broaddus, “Uncompensated Care Costs Well Down in ACA Medicaid Expansion States | Center on Budget and Policy Priorities,” Center on Budget and Policy Priorities, October 21, 2020, https://www.cbpp.org/blog/uncompensated-care-costs-well-down-inaca-medicaid-expansion-states.
153. “Uncompensated Care in New Mexico After the Affordable Care Act” (Legislative Finance Committee, October 27, 2015), https://www.nmlegis.gov/entity/lfc/Documents/Health_ Notes/Uncompensated%20Care%20in%20New%20Mexico%20After%20the%20Affordable%20Care%20Act.pdf.
154. “Governor Signs Bill to Bolster State’s Financial Stability – Senate Bill 26 Redirects Excess Oil and Gas Revenue to Protect against Volatility,” Office of the Governor Michelle Lujan Grisham (blog), March 18, 2023, https://www.governor.state.nm.us/2023/03/18/ governor-signs-bill-to-bolster-states-financial-stabilitysenate-bill-26-redirects-excess-oil-and-gas-revenue-to-protect-against-volatility/.
155. New Mexico Legislature, “An Act Relating To Health Care; Requiring A Study On The Feasibility Of Creating And Implementing A State-Administered Health Coverage Plan; Requiring Reporting.,” HB 400 § (n.d.), https://www.billtrack50.com/billdetail/1570116.
156. Medicaid and CHIP Payment and Access Commission, “Medicaid Buy-In: Program Options and Considerations,” April 2020, https://www.macpac.gov/wp-content/uploads/2020/04/Medicaid-Buy-In-Program-Options-and-Considerations.pdf.
157. NM Together for Healthcare, “HB 400: ‘State Administered Health Coverage Plan.’”
158. Louise Norris, “Medicaid Eligibility and Enrollment in DC,” healthinsurance.org, November 3, 2023, https://www.healthinsurance.org/medicaid/dc/.
159. Amelia Templeton, “Oregon Becomes 3rd in Nation to Seek Federal Approval for a Basic Health Program,” OPB, September 12, 2023, https://www.opb.org/article/2023/09/12/oregon-basic-health-plan-insurance-doctor-authority-affordable-care-act/.
160. Medicaid and CHIP Payment and Access Commission, “Medicaid Buy-In: Program Options and Considerations,” 3.
161. Louise Norris, “Medicaid Eligibility and Enrollment in Connecticut,” healthinsurance. org, November 3, 2023, https://www.healthinsurance.org/medicaid/connecticut/.
162. “Basic Health Program,” Medicaid.gov, accessed November 8, 2023, https://www.medicaid.gov/basic-health-program/index.html.
163. Sabrina Corlette et al., “The Basic Health Program: Considerations for States and Lessons from New York and Minnesota” (Urban Institute, April 26, 2023), https://www.urban.org/
research/publication/basic-health-program.
164. Natasha Murphy and Sarah Millender, “How States Can Build Bridges by Smoothing Medicaid-to-Marketplace Coverage Transitions,” Center for American Progress (blog), February 14, 2023, https://www.americanprogress.org/article/how-states-can-buildbridges-by-smoothing-medicaid-to-marketplace-coverage-transitions/.
165. “Basic Health Program - Cabinet for Health and Family Services,” Team Kentucky, accessed November 8, 2023, https://www.chfs.ky.gov/agencies/dms/member/Pages/bhp. aspx.
166. Christine Monahan, Justin Giovannelli, and Kevin Lucia, “Update on State Public Option-Style Laws: Getting to More Affordable Coverage,” The Commonwealth Fund, March 29, 2022, https://doi.org/10.26099/5fjh-kw48.
167. Perry Undem, “How New Mexicans Feel about Affordability and Healthcare Reform,” February 2022, https://nmtogether4health.org/wp-content/uploads/2022/03/NM-Affordability-Report-1.pdf.
168. Matthew Buettgens et al., “Medicaid Forward in New Mexico: Health Coverage, Health Care Spending, and Government Costs.”
169. Benjamin D. Sommers et al., “Insurance Churning Rates For Low-Income Adults Under Health Reform: Lower Than Expected But Still Harmful For Many,” Health Affairs 35, no. 10 (October 2016): 1816–24, https://doi.org/10.1377/hlthaff.2016.0455.
170. Matthew Buettgens et al., “Medicaid Forward in New Mexico: Health Coverage, Health Care Spending, and Government Costs” (Urban Institute, September 2023), https:// www.urban.org/sites/default/files/2023-09/Medicaid%20Forward%20in%20New%20 Mexico.pdf.med
171. The New Mexico Hospital Association, interview with authors, October 19, 2023.
172. Brian Schilling, “Hitting the Copay Sweet Spot,” The Commonwealth Fund, accessed November 14, 2023, https://www.commonwealthfund.org/publications/newsletter-article/hitting-copay-sweet-spot.ch
173. “New Research About Small Businesses Offering – and Not Offering – Health Insurance,” NFIB, April 5, 2023, https://www.nfib.com/content/analysis/national/new-research-about-small-businesses-offering-and-not-offering-health-insurance/.
174. Medicaid and CHIP Payment and Access Commission, “Medicaid Buy-In: Program Options and Considerations,” April 2020, https://www.macpac.gov/wp-content/uploads/2020/04/Medicaid-Buy-In-Program-Options-and-Considerations.pdf.
175. Corlette et al., “The Basic Health Program: Considerations for States and Lessons from New York and Minnesota.”
176. Stan Dorn and Jennifer Tolbert Published, “The ACA’s Basic Health Program Option: Federal Requirements and State Trade-Offs,” KFF (blog), November 25, 2014, https:// www.kff.org/health-reform/report/the-acas-basic-health-program-option-federal-requirements-and-state-trade-offs/.
177. ABQJournal News Staff, “NM Needs to Act Quick to Attract and Keep Physicians,” ABQJournal, January 30, 2023, https://www.abqjournal.com/news/nm-needs-to-act-quickto-attract-and-keep-physicians/article_ea73424c-957e-586f-ab6f-a60ad2a4710e.html.
178. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report,” 2022.
179. Vanessa G. Sánchez, “Where Have All the Doctors (and Nurses) Gone?,” Searchlight New Mexico, February 8, 2023, http://searchlightnm.org/where-have-all-the-doctors-andnurses-gone/.
180. “Bureau of Health Workforce Health Resources and Services Administration, U.S. Department of Health and Human Services, Fourth Quarter of Fiscal Year 2023 Designat-
ed HPSA Quarterly Summary,” n.d., accessed November 21, 2023.
181. New Mexico Medical Society, “Provider Shortage in New Mexico: The Challenges of Recruitment and Retention of Physicians and Proposed Solutions,” https://www.nmlegis.gov/handouts/LHHS%20091422%20Item%2017%20Addressing%20Physician%20 Shortages.pdf.
182. Administration for Community Living, “New Mexico Policy Academy State Profile” (Administration for Community Living, April 2, 2012), https://acl.gov/sites/default/files/ programs/2016-11/New%20Mexico.pdf.
183. “New Census Data Shows New Mexicans Are Getting Older,” UNM Newsroom, accessed December 2, 2023, http://news.unm.edu/news/new-census-data-shows-new-mexicansare-getting-older.
184. US Census Bureau, “2020 Census Will Help Policymakers Prepare for the Incoming Wave of Aging Boomers,” Census.gov, accessed December 2, 2023, https://www.census. gov/library/stories/2019/12/by-2030-all-baby-boomers-will-be-age-65-or-older.html.
185. “Catron County | NM Counties,” accessed December 2, 2023, https://www.nmcounties. org/counties/catron-county/.
186. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report.”
187. “Map Shows Broadband Issues across New Mexico,” accessed November 21, 2023, https://www.krqe.com/news/new-mexico/federal-map-shows-disparities-in-broadband-access-across-new-mexico/; Megan Gleason, Source New Mexico July 10, and 2023, “NM Broadband Officials Figure out How to Use $675M for Broadband Expansion, despite Federal Errors,” Source New Mexico (blog), July 10, 2023, https:// sourcenm.com/2023/07/10/nm-broadband-officials-figure-out-how-to-use-675m-forbroadband-expansion-despite-federal-errors/.
188. New Mexico Legislative Finance Committee, “Medicaid 2023 Accountability Report” (New Mexico Legislature, 2023).
189. New Mexico Medical Society, “Provider Shortage in New Mexico: The Challenges of Recruitment and Retention of Physicians and Proposed Solutions.”
190. Molly Gamble, “The 15 Best, Worst States for Physicians in 2022,” Becker’s Hospital Review, March 21, 2022, https://www.beckershospitalreview.com/rankings-and-ratings/ the-15-best-worst-states-for-physicians-in-2022.html.
191. Paige Twenter, “10 Best, Worst States for Healthcare,” Becker’s Hospital Review, October 13, 2023, https://www.beckershospitalreview.com/rankings-and-ratings/10-best-worststates-for-healthcare-3.html.
192. “SB0333,” Pub. L. No. SB0333 (2011), https://www.nmlegis.gov/sessions/11%20regular/ bills/senate/SB0333.html.
193. Medical Society Meeting Notes, October 19, 2023
194. Kelly Gooch, “5 Best, Worst States for Physicians to Practice in 2021,” Becker’s Hospital Review, May 24, 2021, https://www.beckershospitalreview.com/rankings-and-ratings/5best-worst-states-for-physicians-to-practice-in-2021.
195. Twenter, “10 Best, Worst States for Healthcare.”
196. Medical Society Meeting Notes, October 19, 2023
197. New Mexico Medical Society, “Provider Shortage in New Mexico: The Challenges of Recruitment and Retention of Physicians and Proposed Solutions.”
198. REDW, “New Mexico GRT Deduction Update for Medical Practitioners,” REDW Financial Advisors & CPAs, August 3, 2023, https://www.redw.com/insights/new-mexico-grt-deduction-update-for-medical-practitioners/.
199. Medical Society Meeting Notes, October 19, 2023
200. New Mexico Medical Society, “Provider Shortage in New Mexico: The Challenges of Recruitment and Retention of Physicians and Proposed Solutions.”
201. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report.”
202. New Mexico Medical Society. “The Challenges of Recruitment and Retention of Physicians and Proposed Solutions.” Presentation, September 15, 2022. https://www.nmlegis. gov/handouts/LHHS%20091422%20Item%2017%20Addressing%20Physician%20Shortages.pdf.
203. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report.”
204. New Mexico Medical Society, “The Challenges of Recruitment and Retention of Physicians.”
205. Thomas Waldrop and Emily Gee, “How States Can Expand Health Care Access in Rural Communities” (Center for American Progress, February 9, 2022), https://www.americanprogress.org/article/how-states-can-expand-health-care-access-in-rural-communities/.
206. Sánchez, “Where Have All the Doctors (and Nurses) Gone?”
207. Albuquerque Journal Editorial Board, “Editorial: NM Lawmakers Need to Stop Doctor Exodus to Resuscitate Health Care System,” Albuquerque Journal, February 11, 2023, https://www.abqjournal.com/opinion/editorials/editorial-nm-lawmakers-need-to-stop-doctor-exodus-to-resuscitate-health-care-system/article_fd1ecba89716-54b8-81ae-5ae837fc0806.html.
208. Xiaoming Zhang et al., “Physician Workforce in the United States of America: Forecasting Nationwide Shortages,” Human Resources for Health 18 (February 6, 2020): 8, https://doi.org/10.1186/s12960-020-0448-3.
209. Silva Mathema, “Immigrant Doctors Can Help Lower Physician Shortages in Rural America,” Center for American Progress (blog), July 29, 2019, https://www.americanprogress.org/article/immigrant-doctors-can-help-lower-physician-shortages-rural-america/.
210. Jonathan Wolfson, “Op-Ed: Addressing Rural Physician Shortages – the Urgent Need for Licensing Reform,” The Center Square, October 9, 2023, https://www.thecentersquare.com/opinion/article_baf26fce-66e0-11ee-a2c5-7b63f909e968.html.
211. Silva Mathema, “Immigrant Doctors Can Help Lower Physician Shortages in Rural America.”
212. Zhang et al., “Physician Workforce in the United States of America.”
213. Dayaratna, Kevin D., PhD, and John O’Shea, MD. “Addressing the Physician Shortage by Taking Advantage of an Untapped Medical Resource.” Backgrounder, No. 3221, The Heritage Foundation. https://www.heritage.org/sites/default/files/2017-06/BG3221_0. pdf.
214. Dylan Scott, “How to Bring Back the Small-Town Family Doctor,” Vox, June 23, 2023, https://www.vox.com/policy/23753724/physician-doctor-shortage-primary-care-medicare-medicaid-rural-health-care-access.
215. Association of American Medical Colleges. “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034.” Prepared by IHS Markit Ltd. Washington, D.C., June 2021. https://www.aamc.org/media/54681/download.
216. Scott, “How to Bring Back the Small-Town Family Doctor.”
217. New Mexico Human Services Department. “Graduate Medical Education Ex-
pansion in New Mexico Five Year Strategic Plan.” January 2022. https:// api.realfile.rtsclients.com/PublicFiles/6c91aefc960e463485b3474662fd7fd2/559d9767-951e-4240-a21a-6a462e3c8096/2022%20NM%20GME%20Expansion%20 Strategic%20Plan.
218. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report.”
219. New Mexico Human Services Department. “Graduate Medical Education Expansion in New Mexico Five Year Strategic Plan.” December 2019. https://burrell.edu/wp-content/ uploads/2020/10/HSDGME-StrategicPlan-Final2020.pdf.
220. New Mexico Human Services Department, “Graduate Medical Education Expansion” (2019).
221. Sánchez, “Where Have All the Doctors (and Nurses) Gone?”
222. Childress, “Lawmakers Tackled New Mexico’s Crisis of Rural Health Care Workers. It Wasn’t Enough.”
223. University of New Mexico - Health Sciences Center, “New Mexico Health Care Workforce Committee 2022 Annual Report.”
224. Sánchez, “Where Have All the Doctors (and Nurses) Gone?”
225. “Another Medical Malpractice Fix Bill Tabled - NM Political Report,” March 3, 2023, https://nmpoliticalreport.com/nmleg/another-medical-malpractice-fix-bill-tabled/.
226. Bureau of Health Workforce, “Scoring Shortage Designations | Bureau of Health Workforce.”
227. “NM RGIS – New Mexico Resource Geographic Information System Program,” accessed November 19, 2023, https://rgis.unm.edu/.

