3. Equality and Diversity Statement
All patients, employees and members of the public should be treated fairly and with respect, regardless of age, disability, gender, marital status, membership or nonmembership of a trade union, race, religion, domestic circumstances, sexual orientation, ethnic or national origin, social & employment status, HIV status, or gender re- assignment.
All Provide policies and procedures must comply with the relevant legislation (nonexhaustive list) where applicable:
• Equality Act (2010)
• Employment Relations Act (1999) Rehabilitation of Offenders Act (1974) Human Rights Act (1998)
• Trade Union and Labour Relations (Consolidation) Act (1999)
• Part Time Workers - Prevention of Less Favourable Treatment
• Regulations (2000)
• Fixed Term Employees - Prevention of Less Favourable Treatment
• Regulations (2001)
• Health & Safety at Work Act (1974)
4. Equality Impact Assessments
Provide is committed to ensuring that none of its policies, procedures, services, projects or functions discriminate unlawfully. In order to ensure this commitment all policies, procedures, services, projects or functions will undergo an Equality Impact Assessment.
Reviews of Equality Impact Assessments will be conducted in line with the review of the policy, procedure, service, project or function. The Equality Impact Assessment is attached at Appendix 4
5. Environmental Impact Assessments
The environmental impact of this policy has been considered and no further action is required at this time.
6. Definitions
Practitioner: doctors and dentists are referred to throughout this document as ‘practitioners’.
Responsible Officer (RO): The role of RO is designated in legislation. Each doctor will be linked to a RO, who will make a recommendation to the GMC, usually every five years, about whether that doctor should be revalidated. The RO is also responsible for ensuring that systems of clinical governance and appraisal in their organisation are working and are appropriate for revalidation. At Provide the RO role is undertaken by a medical practitioner.
Programme Supervisor: will assist the practitioner (with the RO) in compiling a Practitioner Improvement Plan and will oversee the clinical aspects of the programme as a whole, reporting to the RO on progress against objectives. The Programme Supervisor must be a senior manager nominated in agreement with the practitioner.
Clinical Supervisor: may be required to provide close supervision of a practitioner during a clinical placement, and to monitor and report on progress to the programme supervisor. The Clinical Supervisor must be a consultant or clinician nominated in agreement with the practitioner. The role of the programme supervisor is distinct from that of the clinical supervisor who may be required to provide close supervision of a practitioner during a clinical placement, and to monitor and report on progress to the programme supervisor. While the roles are distinct, it may be possible in some instances for the same individual to carry both the role of programme supervisor and clinical supervisor.
7. Remediation Procedures
Provide will offer early intervention when justifiable concerns emerge over the capability, conduct or health of a practitioner, with the aim wherever possible of remediation, reskilling or rehabilitation. All concerns should be dealt with quickly and appropriately and inevitably some programs will be more straightforward than others.
Guiding Principles for Remediation
Provide will offer early intervention when concerns emerge over the capability, conduct or health of a doctor, with the aim of remediation wherever possible. The process will follow the procedure outlined in Provides’ Capability Policy (HRPOL29) and will also utilise the following principles of best practice build on the widespread experience of Practitioner performance advice(PPA) and its guidance document ‘Back on Track’(published by NCAS 2010 awaiting updating)
https://resolution.nhs.uk/resources/back-on-track-a-good-practice-guide/
Principle One – Clinical governance and patient safety
Patient safety should be the paramount consideration in any return to work programme. Remediation must ensure the safety of patients and the public, whilst aiming to secure:
• the needs and care of patients
• the governance and integrity of the clinical service
• the needs and well-being of the doctor
Principle Two - A single framework governing individual programmes
The framework governing individual return to work programmes should use common principles and approaches, and be applicable, as far as possible, across different organisational settings and types of case.
Principle Three – A comprehensive approach
This will involve:
• clarifying and addressing the key stakeholders’ expectations and aspirations, taking into account the need at all times to protect patient safety
• addressing fully the doctor’s training needs as well as all the factors that may be affecting performance, whether these focus on the individual, the immediate clinical team or the wider organisation
Principle Four – Fairness, transparency, confidentiality and patient consent
As far as possible, the confidentiality of the doctor and the immediate clinical team should be protected. However, this need for confidentiality should be balanced against the need to ensure that information is passed to relevant colleagues and to fulfill our obligations under the Duty of Candour
Principle Five – On going and consistent support
Any return to work programme should include personal and professional support for the doctor, for the team they are working with and for the organisation managing the programme.
Principle Six – Success and failure
Any framework must recognise and address the possibility of failure as well as success.
Principle Seven – Local resolution drawing on local and national expertise
Local structures, policies and programs should support local resolution of a case and provide opportunity for local sharing of expertise with access to national expertise
8. Actions where a Concern Arises
At Provide the management of performance is a continuous process, which is intended to identify any capability issues as they arise.
Concerns relating to a doctor’s performance may be identified in a number of ways:
• Concerns expressed by other NHS professionals, health care manager, students or non-clinical colleagues
• Review of performance against job plans, annual appraisal, revalidation
• Monitoring of data on performance and quality of care
• Clinical governance, clinical audit and other quality improvement activities
• Informal or formal complaints about care by patients or relatives or their representatives
• Incidents recorded on Datix
• Information from the regulatory bodies
• Legal claims following allegations of negligence
• Information from the police or coroner
• Court judgements
• The doctor in question self-identifying
Provide recognises unfounded and malicious allegations can cause lasting reputational and career prospect damage. Therefore all allegations or concerns raised must be properly investigated to verify the facts
Provide will work with the relevant organisations to ensure that jointly agreed procedures are in place for dealing with any concerns about doctors with honorary contracts.
Concerns about the capability of doctors in training should be considered initially as training issues and the Medical Adviser should be involved from the outset.
9. Initial Course of Action Meeting
A course of action meeting will be held with the Line Manager to decide and document the appropriate course of action in each case. At this meeting the concern will be categorized to determine if it should be treated as an attendance, capability or disciplinary issue. The Provide Policy to be followed will be agreed at this meeting.
First Meeting to Address Concerns
The Responsible Officer, or delegate, will arrange a first meeting to address concerns with the doctor at the earliest practicable opportunity. This meeting will be to address the substance and accuracy of the concern with the doctor The exceptions will be as those outlined in MHPS, for example in criminal or fraud cases.
After the first meeting to address concerns, the RO will write to the doctor to confirm the course of action to be taken.
It is recognised that some cases will cover more than one category, e.g. conduct and capability, and these may be combined under a capability process However, there may be occasions where it is necessary to pursue a conduct issue separately, in which case these issues will be conducted in line with the Provides’ Disciplinary Policy (HRPOL14). Although it is for Provide to decide on the most appropriate way forward having consulted PPA, the doctor is also entitled to use the grievance procedure (HRPOL15) if they consider that the case has been incorrectly classified.

Advice from PPA will help Provide come to a decision on whether the matter raises questions about the doctor’s capability as an individual (health problems, behavioral difficulties or lack of clinical competence) or whether there are other matters that need to be addressed. If the concerns about capability cannot be resolved routinely by management, the matter must be referred to PPA before it can be considered by a capability panel (unless the doctor refuses to have his or her case referred). Provide will also involve PPA in any potential disciplinary cases.
https://resolution.nhs.uk/resource-services/practitioner-performance-advice/
Wherever possible, Provide will aim to resolve issues of capability (including clinical competence and health) through on going assessment and support. Early identification of problems is essential to reduce the risk of serious harm to patients.
PPA will be consulted for advice to support the remediation of a doctor. Provide will use the PPA document ‘Back on Track’ and PPA resources as the framework for the remediation strategy.
https://resolution.nhs.uk/resource-services/practitioner-performance-advice/
10.Exclusion and Restrictions
The opportunities to consider exclusion and restriction occur during the Initial Course of Action Meeting, First Meeting to Address Concerns or during case investigation. Therefore the decision to formally exclude a practitioner must be taken by the Responsible Officer or delegate. The case will be discussed fully with the CEO (or CEO-Delegate), the Director of Human Resources, PPA and other interested parties (such as the police where there are serious criminal allegations or the Counter Fraud & Security Management Service) prior to the decision to exclude a practitioner.
In the rare cases where immediate exclusion is required, the above parties must discuss the case at the earliest opportunity following exclusion, preferably at a case conference.
Immediate and formal exclusion procedures will be managed and reviewed in line with MHPS Section 1 and 2 as applicable.
An immediate time limited exclusion may be necessary
• to protect the interests of patients or other colleauges
• where there has been a breakdown in relationships within a team which has the potential to significantly endanger patient care
The PPA must, where possible, be informed prior to the implementation of an immediate exclusion. Such exclusion will allow a more measured consideration to be undertaken.
The Responsible Officer will also consider if it is necessary for the doctors practice to be restricted during the investigation. This restriction may be limited to place of work, type of clinical work or other senior professional roles, for example being an appraiser.
11.Remediation
Remediation may be agreed as an outcome from both capability and conduct investigations alongsideacting down, working at different sites, direct or indirect clinical supervision or other agreed actions.
All doctors agreeing to remediation, either within or outside Provide, will need to agree to
• a senior clinician within Provide and their specialty to act as a mentor
• OHS review
• to provide regular feedback to their clinical manager
The doctor and their clinical manager will agree at the start of any remedial action a plan that will include the frequency of review of their progress and a time frame and criteria by which the doctor should be ready to return to full clinical activity.
The Responsible Officer, CEO and Group Chief People Officer should be updated.
12.Appraisal, Support and Follow Up
The documentation from the return to work programme should be shared with the practitioner’s appraiser so that it can inform the practitioner’s personal development plan for the subsequent year. The personal development plan should have a focus on preventing a recurrence of any problems which led to concerns about performance.
It may also be necessary to provide further support to the practitioner through mentoring or the provision of further training after completion of the programme. Provide will meet the costs of recommended training directly relevant to the clinical role.
The practitioner should resume involvement in normal departmental activities, such as clinical audit and review of serious untoward incidents.
13.Evaluation
The RO may wish to evaluate the process and outcome of the return to work programme and capture the lessons for the organisation.
14.Appeal Process
The appeal process will follow the relevant procedure set out in the Capability policy (HRPOL29), and Disciplinary policy (HRPOL14) as below:-
15.Advice
Advice on the application of this Policy is available from Provide HR Department and also the Clinical Performance Group.
Advice is also available from the LNC and the BMA.
16.Records
Records will be held in accordance with the General Data Protection Regulations.
Appendix 1 – NPSA ‘Back on Track’ Framework https://resolution.nhs.uk/resources/back-on-track-a-goodpractice-guide/
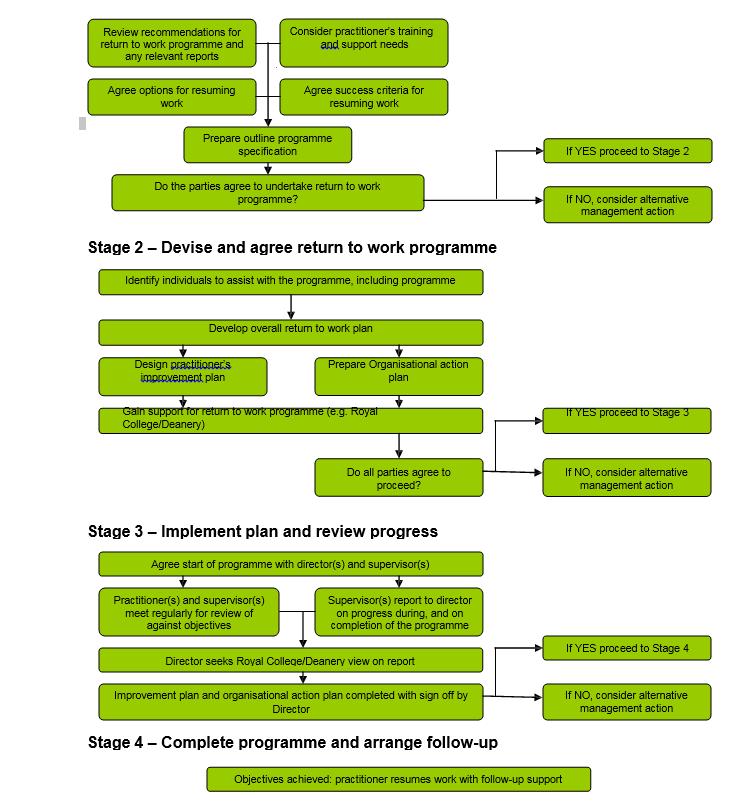
Stage 1 – Entry to return to work programme
Start: Responsible Officer (RO) reviews the recommendation for return to work programme, including information from assessment, investigation or review.
RO Considers the practitioner’s training and support needs arising from the relevant reports.
RO agrees options for resuming work and success criteria to achieve these, including prospects for success.
RO summarises the options for resuming work in an outline programme specification.
Finish: Agreement in principle to proceed to Stage 2.
Training and support needs:
Where the entry point to the return to work programme is local investigation, Royal College review or PPA or regulatory body assessment, the findings and recommendations will determine the content of the return to work programme. The report of any investigation, review or assessment should be made available to the practitioner and those who are assisting to plan the programme so that a detailed statement of training needs can be prepared. The report should define clearly who has had access to it and the duty of confidentiality.
For all practitioners it will be necessary to ensure that all significant training and development needs have been adequately identified; Some practitioners may need a return to work programme after a prolonged absence, following, for example, exclusion or restriction of practice, removal from a Performers List, suspension/erasure by the GMC/GDC or after a career break, a period overseas or ill health. They will normally need additional approaches to identifying training needs e.g., through a period of supervised practice or review undertaken by a Deanery or Royal College.
Feasibility of the Programme and Ability of the Practitioner to Change:
In considering whether to support a return to work programme, Provide will bear in mind the sensitivity of the situation and any possible dispute. Provide will consider the likelihood of success which relates to such factors as:
• The extent to which the practitioner is able to acknowledge the difficulties identified
• The progress made in any previous attempts to improve practice
• The practitioner’s demonstrated commitment to change
• Significant physical or mental health problems which impact on patient safety and cannot be remedied
• Availability of resources and support the relationships between all parties; including the sensitivity around possible victimisation
• The seriousness and scope of the concerns identified. Provide will consider the potential involvement of the LNC, MSC and BMA to support the RO on an informal basis at this stage
In some cases Provide may decide not to support a programme, but normally it will be appropriate for a practitioner to have the opportunity to demonstrate their ability to progress. This will be provided through a structured programme with clear goals, success measures and review dates. If progress is not satisfactory, then Provide, through the Clinical Performance Group, will decide on an alternative course of action.
Where a practitioner is not currently attending work the feasibility of a return to work programme will depend on finding a suitable placement. Where a practitioner has been suspended, or his practice restricted, feasibility will depend not only on finding a suitable placement but also on ensuring that adequate safeguards are in place to protect patient safety to allow the practitioner to work under supervision.
Addressing health problems:
Significant physical or mental health issues will be assessed before progress can be made on other areas of the return to work programme. Provide will provide access to occupational health advice and, through this, to further specialist referral, the practitioner may be on medical exclusion during this period. If there are health concerns, Provide will ensure information is included and considered throughout the return to work programme. Health problems that are unlikely to impact on the outcome of the programme may be addressed during its course.
Provide commitment to re-entry:
Provide, as the employer, will consider how they will support the practitioner’s re-entry to the workplace following successful completion of the programme. They will consider whether specific action will be required to rebuild relationships between the practitioner and their team practice, including external facilitation where necessary.
Agreement to desired outcome:
Following review of the needs identified, all relevant parties need to agree that the return to work programme is required and is appropriate. The desired outcome should be defined. This may include, for example, the practitioner returning to full duties in their previous post, or, alternatively, taking up a post with more limited scope or responsibility.
In some cases the practitioner and Provide may agree that s/he should leave.
Offer personal support to the practitioner:
Provide should remind the practitioner of the need for personal support and suggest options for how this support may be provided.
Where there is no agreement:
In some cases Provide will consider other options which may include mediation; alternative work location; the use ‘Maintaining High Professional Standards in the Modern NHS (MHPS)’ frameworks in England and Northern Ireland; or another HR process.
It may be appropriate at this stage to offer the practitioner specialist careers advice through PPA.
Agreement to proceed:
If agreement is reached, (even if it is provisional), on a way forward, Provide will conclude Stage 1 and proceed to consider the return to work programme in more detail.
Stage
2 – Devise and agree return to
work programme
Start: RO Identifies individuals who will assist with the return to work programme, including a Programme Supervisor.
The Programme Supervisor develops the overall return to work project plan based on the output of Stage 1, to include; as deemed appropriate:
Practitioner’s Improvement Plan, based on training needs;
• Organisational action plan.
• Gain support from relevant authorities (e.g. Royal College, Deanery) to the aims, design, objectives, methods and resource requirements for the programme.
Finish: Agreement of all parties to proceed with the programme.
Identify roles and responsibilities for handling the programme:
A small team of individuals, including the line manager and clinical lead, will need to be convened to help devise and implement the return to work programme. Their roles need to be clear and their work coordinated by a senior management lead. At Provide this will be the Responsible Officer (RO). The team may include a lay non-executive Board member to bring a wider organisational and lay perspective. The RO should take advice from the Deanery or Royal College to identify the individual who will act as the programme supervisor for any clinical retraining.
The programme supervisor will assist the practitioner (with the RO) in compiling a Practitioner Improvement Plan and will oversee the clinical aspects of the programme as a whole, reporting to the RO on progress against objectives.
The local Deanery and/or appropriate Royal College may be invited to provide expert advice on training goals, standards to be reached/competencies to be demonstrated and the measures for reviewing progress and outcome of the programme. These will need to take into account the post to which the practitioner is returning.
The Postgraduate Medical or Dental Dean or Director of Postgraduate GP Education should be informed of the department/practice where a practitioner is undertaking a return to work programme, as this may impact on accreditation of the department for training of substantive trainees.
For general medical or dental practitioners, the Local Medical or Dental Committee may have a role. For dental practitioners the Practitioner Advice and Support Scheme (PASS) group may help.
Develop the action plans:
The practitioner will need a clear plan to address improvements required in their practice (‘Improvement Plan’ (IP)). In addition, Provide will need to devise a plan to ensure that re-entry arrangements are in place for the practitioner on completion of any training programme and that measures are taken to address any team or organisational factors (‘organisational action plan’).
The practitioner’s Improvement Plan will need to cover such issues as:
• a clear statement of what the programme is seeking to achieve
• prioritized objectives
• training resources required
• timescales for interim review and completion of the programme
• how achievement of the objectives will be assessed
• funding requirements and how these will be met
• location of programme
• arrangements for support
• how the ‘sign off’ process will be managed
• a statement of the action to be taken if the programme is not satisfactorily concluded or if concerns are identified which suggest a serious risk to patient safety
• details of the post to which the practitioner is likely to return
Agree where training will take place and arrangements for any placement:
The RO should agree with the practitioner where the clinical retraining programme will take place, taking into account the views of the panel.
For practitioners currently at work, the programme may take place wholly or partially at the practitioner’s normal place of work. Where this is not appropriate or where the practitioner is not at work, a placement will be required. Provide and the practitioner should work together to identify a clinical placement. The RO will normally seek advice from the Deanery or Royal College as to the suitability of the placement. If there is evidence that the practitioner is not willing to accept a reasonable offer of a placement, Provide may need to take other steps to resolve the case.
Formal agreement for the placement will be required between the employer, practitioner and Trust/provider organisation/practice providing the placement. This should cover the objectives of the placement, supervision requirements, and arrangements for informing patients, information to be passed to the placement
provider, funding arrangements for the placement provider and the practitioner and indemnity.
Courses, coaching and training interventions:
In addition to supervised work, the practitioner should be encouraged to attend tutorials, workshops and courses, and undertake focused reading on specific topics. Where there are behavioral concerns, skilled coaching may be required.
It is likely that a combination of learning options will be required. The choice of intervention will depend on the needs and learning style of the practitioner and local availability of resources. The programme supervisor can help the practitioner make the most appropriate choice of resources to meet needs, and ensure that a coherent and balanced programme is achieved.
Personal support:
Support may be provided to the practitioner through confidential mentoring.
Provide will ensure the practitioner has access to adequatetreatment and follow-up support for managing their health concerns, through occupational health, general practitioner or specialist services.
Funding arrangements:
Provide will meet the costs of recommended training directly relevant to the clinical role.
The RO will ensure that the funding arrangements to support the programme are clarified, and the responsibility of the Provide and the practitioner are agreed. No programme can proceed without a clear view of the costs and how they will be met.
Organisational action plan:
The RO should manage the organisational re-entry programme or delegate this task to a named individual of sufficient seniority within the employing organisation.
The organisational action plan will need to cover:
• re-entry arrangements for the practitioner on completion of any training programme
• communications
• preparatory work in the department to which the practitioner will return
• measures to address other organisational factors. Each of these is considered in the following paragraphs
Re-entry arrangements for the practitioner on completion of any training programme. This will need to include
• individualised induction/orientation required to provide an update on any organisational or service changes
• how re-engagement with clinical activities will be managed, for example, reestablishing GP referrals, outpatient clinics, theatre lists, secretarial support and any changes in professional /managerial accountability
• how the practitioner will be phased back into the clinical role, particularly where acting-up arrangements are in place
Communications will include:
• internal communication for those involved in the return to work programme (e.g. clinical and programme supervisors, responsible director, placement provider)
• internal communication within the wider organisation on a ‘need-to-know’ basis (e.g. to colleagues and patients)
• any external communication requirements (e.g. in response to media enquiries or to the general public)
• external communication to relevant parties (e.g. regulatory bodies such as the GDC/GMC)
The practitioner should be informed about the proposed communications.
Preparatory work in the department will likely need to cover the following:
• preparation of and on-going support to the team the practitioner will be rejoining; team development or facilitation may be required where relationships have been strained
• agreement on how any changes in the practitioner’s job plan are communicated to colleagues
• other factors that may need to be addressed, such as attending to the difficulties of split-site working, reviewing the management structures within the team, leadership development
Other organisational factors:
Provide may also need to address other more general organisational issues identified through local investigation, review or assessment. These may include, for example: addressing any bullying or victimisation; a review of human resources policies; improving employeef training or induction procedures to help prevent similar problems occurring in the future.
Stage 3 – Implement plans and review progress
Start: Implement plans.
Review by programme supervisor of progress against objectives according to plans.
Report by programme supervisor to responsible officer on the extent to which the plans have been successfully completed.
RO seeks view from relevant authority (e.g. Royal College, Deanery) on supervisor’s report.
Finish: Sign-off by responsible officer of extent of completion of individual and organisational action plans.
Progression to Stage 3 will require satisfactory completion of Stage 2.
Implement plan for the individual:
The programme supervisor and RO will agree the start of the programme with the practitioner.
Review meetings:
The programme supervisor will meet and review the practitioner’s progress at intervals throughout the programme, to a timetable agreed at the outset. At each review the programme supervisor should summarise progress (or note that progress has not been made) and formally record the achievement of objectives where necessary.
Where clinical supervisors, specialist trainers or educationalists are involved, they should send an update on progress against objectives to the programme supervisor in accordance with the agreed timetable. The practitioner should have opportunity to comment on their progress at review meetings and to contribute to the feedback through self-assessment.
The responsible director and programme supervisor will need to consider the action to be taken if progress against objectives is not satisfactory during the course of the programme
The RO should brief the practitioner about the progress of the organisational action plan.
Implement plan for the organisation:
The organisational action plan should be implemented and reviewed in line with the arrangements outlined in this section.
Stage 4 – Complete programme and arrange follow-up
Start: If programme has been successful, RO agrees with responsible parties detailed arrangements for practitioner to resume employment under the terms agreed in Stage 1.
If programme has been unsuccessful, RO takes alternative management action which may include redeployment or disciplinary action.
Finish: Following successful completion of the programme RO agrees follow-up arrangements with practitioner.
Progression to Stage 4 will require satisfactory completion of Stage 3
Completion:
The assessment of whether the programme has achieved the desired outcomes will normally be through a process of documented assessment reports from the different stakeholders involved (Programme Supervisor, Clinical Supervisor) in the programme. This information will then inform the decision by the RO as to whether clinical/organisational re-entry has been successful.
This decision should be confirmed in writing to all parties (including external stakeholders such as the GDC/GMC or PPA).
The independent expert adviser from the Royal College/Deanery (see Stage 2) may advise the RO on the extent to which the return to work programme has followed the agreed method, providing some external validation of the process.
The RO should also ensure that the organisational action plan has been completed and that any outstanding organisational/team issues that need to be addressed during the re-entry stage are addressed (e.g. mediation, team facilitation).
The RO and the practitioner will then confirm the detailed arrangements for return to work, including start date, duties and any supervision requirements.
Appendix 3 – PPA Resource Practitioner Action Plan
Resource Practitioner action plan
This template and the accompanying guidance can be used to develop an action plan following PPA assessment or to develop a local action plan The template was developed by NCAS and partner organisations as part of the Back on Track project to bring more consistency and rigour to return-to-work programs The template is designed to be used by both primary and secondary care organisations. For further guidance please see the Back on Track Framework Document (2010) which also gives definitions of terms used in the template such as “responsible director ‟ and “supervisor ‟ .
The document is provided in Word so that users can adapt it easily. Remove the header and footer and this introductory section but keep the „Confidential ‟header, as well as adding an appropriate organisational header of your own The template is in four parts:
• Part 1 sets out the agreement – who is party to the plan and in what role etc.
• Part 2 sets out the objectives. An example objective is included for guidance which should be deleted before the plan is used or signed A blank objective template appears
• after the example which can be copied as many times as necessary
• Part 3 records how the practitioner is progressing, objective by objective As before, this needs to be copied to match the number of objectives set Summary scores are used to demonstrate progress: 0 = no progress, 1 = partial progress, 2 = objective fully achieved
• Part 4 is used to sign off the plan when completed
The template also includes two summary annexes so that objectives can be seen alongside each other (Annex 1) and key milestones and target dates can be fitted together to ensure that work is reasonably spread through the life of a programme (Annex 2)
As with all Toolkit resources, PPA cannot accept responsibility for the consequences of using this template
PART 1 – AGREEMENT
Name of practitioner
Profession and specialty
Registration number
Employing/contracting body
Address
For PPA cases PPA case number
Dr / Mr / Mrs / Ms / Miss Delete as necessary
Purpose of this plan
The purpose of this plan is for the practitioner to address the performance concerns identified by [PPA/local procedures/College or other educational body/health regulator – Add or delete as necessary]
The content of the plan has been arrived at by discussion and agreement by all the participants in this process The plan is expected to last [Add duration] months Progress will be formally reviewed by the Responsible Director and by the Programme Supervisor every [Add interval] months
Roles and responsibilities for management of this plan4
The Responsible Director identified by the employer/contracting body is: Name
Job title
The Programme Supervisor is: Name
Job title
The Educational Adviser is5: Name
Job title
Organisation
Post to which the practitioner is likely to return
On successful completion of the plan it is proposed that Dr/Mr/Mrs/Ms/Miss
Delete as necessary
Will continue in practice or return to practice in theclinical post/area described below6 . Name of post
Broad description of post/clinical area
4 Roles and responsibilities are explained in the Action Planning Guidance download already referred toandinthe
Back on Track Framework Document (2010) If a plan defines any additional roles they should be specifiedhere
5 To be used if there is a College, Deanery or other educational adviser in addition to the Programme Supervisor
6 Post, responsibilities and seniority may not be the same as those applying at the time of the concerns resulting in the assessment process
Employer/Contractor
Progress Review
At each review date and at the end of this plan there will be a review of progress by the [Responsible Director – insert name] and/or [Programme Supervisor – insert name] [The practitioner – insert name] should be able to demonstrate satisfactory and incremental progress throughout the programme and continuing ability to reflect and learn from [his/her] own and [his/her] colleagues’ practice.
The [Responsible Director – insert name] will consider taking management action in the following circumstances, if the expected progress towards objectives is not demonstrated:
1. Where failure to progress occurs at the first or second milestone, continuing with the action plan but re-assessing objectives can be considered A change of objective will only be agreed to where there is clear evidence of progress even though falling short of the performance standard defined in the plan The overall time allotted to the action plan will not be extended
2. A failure to progress in achieving the agreed objectives may result in [sanctions – add relevant possibilities such as Performers List action, use of disciplinary action, use of disciplinary/capability procedures, referral to regulatory body] and/or a new final employment goal such as redeployment These possibilities will be considered if, in the opinion of the clinical supervisor and programme supervisor, the objectives are not likely to be met in the remaining time allocated to the action plan despite the practitioner having ample opportunity to demonstrate progress
3. If a failure to progress raises concerns in relation to patient safety or professional probity, the clinical supervisor may make a referral to the [Add relevant regulator].
4. If a failure to progress is related to sickness absence, it may be appropriate to defer the plan’s completion date. The normal quota of annual leave may be taken during the period of the action plan, but this must be pro-rata. Any period of sickness absence greater than that covered by self-certification must be supported by a doctor’s certificate.
A cumulative absence due to illness of more than [Add – for example, two weeks in six months] will trigger a referral to the Occupational Health Service unless seen as unnecessary in the opinion of the clinical supervisor and programme supervisor Reasons for not making an OH referral will be given
Where an organisational action plan has been agreed (in addition to this plan for the individual practitioner) progress will be reported to the practitioner at review points. [Delete as necessary
Agreement
This plan has been developed with the cooperation of all parties who are satisfied that the identified objectives reflect the issues identified in:
• the decision of the regulator when this body is involved and/or
• the assessment report and recommendations for PPA cases and/or
• the review report and recommendations from the Royal College and/or local investigation
Add or delete as necessary
All parties agree to the objectives set out in the plan and will take forward the programme as set out in the plan, adhering to the accompanying notes. If further objectives need to be added to the plan during the course of the programme, these may be added following agreement of all parties.
Name and organisation Signature Date
Practitioner
Chief Executive of employer/contractingbody
Responsible Chief Officer on behalfofChiefExecutive
Programme Supervisor (on behalf of competent body or employer/contractingbody)
Appointed representative of practice/pharmacy where applicable
Additionalparticipantsas necessary
Additional participants as necessary
PART 2 – OBJECTIVES
See also Annex 1 for summary of objectives template and Annex 2 for summary timetable template.
OBJECTIVE - EXAMPLE – DELETE BEFORE USE
Area to be addressed: This is usually the area of Good Medical Practice identified in the NCAS report recommendations e g infection control, record keeping, communication etc
Specific objective(s)
This should be a high level objective which sets out what you want the practitioner to achieve e g “For Dr X to demonstrate his/her ability to at the standard expected of…in a modern NHS”
How will this objective be achieved?
How
Where
e g what interventions will be used to help the practitioner meet the objective
Observation of others
Supervision of practice [direct, indirect, distant] with constructive feedback and time for reflection
CME
Working 1:1 with coach/counsellor/mentor etc.
e g existing employing body/practice or host Trust (may be different for each objective)
Supervisor(s)
Resources required
[Including funding and provider of funding]
Timescale
Note that these should be named individuals who have relevant experience and again may be different for each objective The supervisor will be responsible for signing off the objective
What physical resources are required? Who is going to pay for what? NCAS advocates that the practitioner makes a reasonable contribution to their own remediation [Back on Track 2006 para 5 5]
How many weeks/months is it anticipated that it will take to achieve the objective? This needs to be realistic and, at the beginning of the programme, a fixed period of time so there is a definitive expected end point which may be re-negotiated [up or down] as the plan progresses [with agreement] Again this may be different for each objective
How will progress be recorded and achievement measured?
Milestones
Supportive evidence
Individual responsible for monitoring/sign off
To enable progress to be monitored throughout the remediation/reskilling process and not at the just at the end identify what is expected to be achieved at timely stages e g
By the end of month 1
By the end of month 2 etc.
What evidence will support the monitored progress [or not] and achievement of [or inability to achieve] the objective e g monthly progress reports, reflective learning log, certificates of successful completion of courses, documented case based reviews, final summary report etc.
This is usually the named clinical supervisor.
OBJECTIVE TEMPLATE – COPY AS NECESSARY, FOR EACH OBJECTIVE Area to be addressed:
Specific objective(s)
How will this objective be achieved? How
Where Supervisor(s)
Resources required [Including funding and provider of funding]
Timescale
How will progress be recorded and achievement measured? Milestones
Supportive evidence
Individual responsible for monitoring/sign off
PART 3 - OBJECTIVE COMPLETION - REVIEW DOCUMENTATION –COPY FOR EACH OBJECTIVE AT EACH REVIEW
Summary sheets – for use at agreed review points and at completion of the programme
Summary Score: 0 = no progress, 1 = partial progress, 2 = objective fully achieved
OBJECTIVE 1
Review Date
Clinical Supervisor comments
Practitioner comments
Signed:
Date: Proposed Summary Score:
Signed:
Date: Programme Supervisor comments
Signed:
Date: Agreed Summary Score:
Responsible Director comments
Signed:
Date: Agreed Summary Score:
PART 4 – FOR COMPLETION AT END OF PROGRAMME
The signatures in this document confirm the completion of the plan by the practitioner, who agrees to make this document available with the future appraiser/appraising body In this way, progress can be maintained and the appraisal process is informed by the plan
Please sign below to indicate your agreement to the above: Name Signature Date
Programme Supervisor
Practitioner
Final comments
Responsible Director
Final comments
Final comments
Other parties should sign here, as necessary
Name Organisation Signature Date
SUMMARY OF OBJECTIVES
Objective 1
Mechanismtoachieveobjective
Where the education/training will takeplace
Resourcerequirement
Named person/organisation to help achievetheobjective
Evidence demonstrating that the objectivehasbeenmet
Timescaletoachieveobjective
Objective 2
Mechanismtoachieveobjective
Where the education/training will takeplace
Resourcerequirement
Named person/organisation to help achievetheobjective
Evidence demonstrating that the objectivehasbeenmet
Timescaletoachieveobjective
Objective 3
Mechanismtoachieveobjective
Where the education/training will takeplace
Resourcerequirement
Named person/organisation to help achievetheobjective
Evidence demonstrating that the objectivehasbeenmet
Timescaletoachieveobjective
Objective 4
Mechanismtoachieveobjective
Where the education/training will takeplace
Resourcerequirement
Named person/organisation to help achievetheobjective
Evidence demonstrating that the objectivehasbeenmet Timescaletoachieveobjective
TIMETABLE SUMMARY – EXAMPLE – DELETE BEFORE USE Month 1 Month 2 Month 3 Month 4 Month 5 Month 6
Objective 1 Start Review Complete
Objective 2 Start Review Review Complete
Objective 3 Start Review Complete
Objective 4 Start Review Complete
Objective 5 Start Review Complete
Objective 6
TIMETABLE SUMMARY - TEMPLATE
2
Objective 1
Objective 2
Objective 3
Objective 4
Objective 5
Objective 6
3
4
5
6