Management of Blood Borne Viruses (BBVs) Policy
Version: V9
Ratified by: Quality and Safety Committee
Date ratified: 19/07/2023
Job Title of author: Specialist Infection Prevention Nurse
Reviewed by Committee or Expert Group Infection Prevention Group
Equality Impact Assessed by: Specialist Infection Prevention Nurse
Related procedural documents

LDPOL03 - Statutory and Mandatory Training Policy
LDPOL02 – Policy for the Management of Corporate and Local Induction Training
IPPOL18 – Management & Safety of Sharps
IPPOL21 – Policy on Standard Infection Control Precautions (SICPs) and Transmission Based Precautions (TBPs)
Review date: 19/07/2026

It is the responsibility of users to ensure that you are using the most up to date document template – i.e. obtained via the intranet.

In developing/reviewing this policy Provide Community has had regard to the principles of the NHS Constitution.
Version Control Sheet
Version Date

Author Status Comment
V2 April 2009 MEHT Occupational Health: kind permission to use Ratified Revised by Infection Prevention Lead Nurse
V3 March 2011 Infection Prevention Lead Nurse Ratified General review and CECS CIC status
V4 October 2013 Infection Prevention Lead Nurse Ratified Revised by Optima Health Infection Prevention Lead Nurse
V5 September 2016 Optima Occupational Health Ratified Reviewed by Infection Prevention Committee (virtual panel)
V6 January2017 Headof Infection Prevention Ratified Reviewedby Infection Prevention (virtualpanel)
V7 March2019 Specialist Infection Prevention Nurse Ratified
V7.1 May2020 Specialist Infection Prevention Nurse Ratified Updateof Optimacontact details
V7.2 September 2021 Specialist Infection Prevention Nurse Updateof Optimacontact Details page 8 andpage16
V8 September 2022 IPC Consultant/ Medigold Regional Associate Director of Nursing Review & Update and change OH provider details toMedigold
V9 July2023 Specialist Infection Prevention Nurse Ratified


1. Introduction
The Department of Health states that ‘although the risk of acquiring blood borne viruses through occupational exposure is low, the consequences can be serious’.
It is the policy of Provide to minimise the risk to patients, staff and the public from blood borne infections.
All staff should make themselves familiar with this policy to ensure ‘best practice’
The aim of this policy is to:
• Ensure that clear guidance is given to all healthcare workers on how to minimise the likelihood of exposure to a blood borne virus (hereafter BBV)
• Ensure that all healthcare workers are aware of the action to take in the event of a needle stick or sharps injury and that these are managed in a timely, appropriate and consistent manner
• Ensure that all patients are protected against the risk of acquiring a BBV from an infected healthcare worker
For this purpose action to be taken by the individual, Occupational Health Department, Accident and Emergency Department, and clinical staff are included.
Provide is committed to improving the quality of care throughout the organisation and the promotion of high standards of infection prevention and control practice.
All staff must possess an appropriate awareness of their role in the prevention and control of infection including BBVs in their area of work. Not only is this part of their professional duty of care to the patients with whom they are involved, but it is also their responsibility to themselves, to other patients and members of staff under the Health and Safety at Work Act 1974.
2. Purpose
The purpose of this policy is to give clear guidance to staff in the management of sharps and exposure to blood borne viruses, thereby limiting injuries and the risks associated with accidental exposure to blood borne viruses. This policy applies to all employees of Provide Group, and all service users who will come under the direct care of the service and reflects all current national guidance.
3. Definitions
Exposure Prone Procedures (EPPs) are those invasive procedures where there is risk that injury to the worker may result in exposure of the patient’s open tissues to the blood of the worker. These include procedures where the worker’s gloved hands may be in contact with sharp instruments, needle tips or sharp tissues (e.g. spicules of bone or teeth) inside a patient’s open body cavity, wound or confined anatomical space where the hands or fingertips may not be completely visible at all times.

Mucocutaneous Exposure
When blood- or blood-stained fluids contaminate non-intact skin (cuts, abrasions, sores, chapped skin etc), conjunctivae or mucous membranes. Mucocutaneous exposures occur more frequently than percutaneous exposure; however, the transmission risk after a mucocutaneous exposure is lower than that after a percutaneous exposure.
Percutaneous Exposure
When a sharp instrument (needle, scalpel, scissors etc.,) that is contaminated with someone else’s blood or other blood-stained body fluid penetrates the skin. Sharp tissues such as spicules or bone or teeth may also pose a risk of injury. A bite which causes bleeding or other visible skin puncture also falls into this category.
Source patient
The source patient is the individual involved in the incident and whose blood has the potential to cause injury and/or disease to the injured person (staff member).
4. Duties
The Chief Executive of Provide has overall responsibility for ensuring that the organisation has the necessary management systems in place to enable the effective implementation of all Provide policies. The Service will be responsible for ensuring that the requirements of all pertinent health and safety legislation are met.
Management Responsibilities
To assess the risk of transmission of Blood-borne viruses (BBVs) in each clinical area and take all reasonably practicable measures to prevent transmission based on the principle of standard infection control precautions (SICPs).
To ensure that the COSHH Regulations are complied with in relation to BBVs.
To ensure that new and existing healthcare workers are aware of the principles of SICPs relevant to their work area and that adequate resources are available to allow precautions to be applied.
To ensure that all healthcare workers receive the appropriate information, instruction and training on BBVs and accidental exposure.
It is the responsibility of an injured member of staff’s line manager/on-call manager to undertake an initial risk assessment of the type of injury sustained with the affected staff member and then direct them to A&E if appropriate (appendix 2) with an incident referral form which they also need to send to OH for follow-up post-assessment.
Where deemed appropriate (following initial assessment by A&E) it is the relevant managers responsibility to contact the source patient (if known) for bloods to be taken if the injury is assessed as significant – a decision will be made by A&E following staff members attendance. See section 9 for further details.

Employee Responsibilities
To co-operate with all measures taken by the organisation to protect them from BBV transmission including Hepatitis B immunisation (where appropriate) together with resources in place for the avoidance of sharps injuries using safer sharps (safety devices) where appropriate.
To report all incidents of potential exposure to BBVs to their line manager and to follow the instructions in the flow chart (appendix 1) to determine their next action in discussion with their line manager.
All healthcare workers who have direct patient contact have a duty to keep themselves informed and updated on the codes of professional conduct and guidelines on HIV infection as laid down by the regulatory bodies.
Occupational Health Department Responsibilities
The effective management of occupational health services in the NHS requires employers to ensure a comprehensive occupational health service is provided either in-house or outsourced to an occupational health provider. This service should include the provision of specialist advice in all aspects of the prevention and management of bloodborne virus transmission. Currently this service is sub-contracted to Medigold Health (Occupational Health and Wellbeing).
Accident and Emergency Department Responsibilities
The role of the A&E department is to undertake an assessment of HCWs who have sustained a sharps injury that may, on assessment be deemed to have led to potential exposure to a BBV and to follow up assessment with initial treatment if deemed necessary If bloods are needed, the line manager (of the injured staff member) should make the referral to OH using the BBV Exposure Form which is available on the Provide Community platform. See section 9 for further guidance.
5. Consultation and Communication
This policy has been developed in consultation with advice from Occupational health provider ‘Medigold’ to Provide CIC and the policy distributed to members of the infection Prevention group for approval.
6. Monitoring Monitoring
Provide monitors all infection control incidents, and in particular needle stick incidents every month via the Incident Reporting procedure (Datix). The Quality and Safety team report all recorded events / trends to the Quality & Safety Committee as part of the regular incident reporting. All needle stick / sharps injuries are monitored by the Quality & Safety team. Where it is recognised that there are significant trends identifying poor practice these issues will be reported to Assistant Director of the relevant service, accountable for the risk. The number and location of incidents is monitored by the Quality & Safety Committee.

Auditing
The Quality and safety team may audit sharps injuries reported via the datix system if there are identified themes or trends that present a risk to staff, service user and/or environment. These audits will be monitored through the Organisational audit programme reporting to the Quality Committee.
7. Risk of Transmission and Types of Exposure
Risk of Transmission
The risk of transmission to a healthcare worker from an infected patient following an injury has been shown to be:
• 1:3 When a source patient is infected with Hepatitis B and is ‘e’ antigen positive
• 1:30 When a source patient is infected with Hepatitis C
• 1:300 When a source patient is infected with HIV
There is no evidence to suggest that BBVs transmitted by blood can contaminate intact skin or contaminate by inhalation or by faecal-oral contamination.
The risk of transmission of BBVs is greater from patients to healthcare worker than healthcare worker to patient. It is proportional to the prevalence in the local population, the infectivity of the source patient and the type and degree of exposure. Transmission most commonly occurs in the healthcare setting after percutaneous exposure to the patient’s blood by needle stick or other sharps injury.
The occupational risks of transmission of BBVs can also arise from the potential exposure to other body fluids and tissues contaminated with blood from an infected patient.
Not all patients with blood borne viruses have had their infections diagnosed and certain groups of individuals are considered to be “high risk”. For HIV, “high risk” groups include intravenous drug users, men having sex with men (MSM), Sex Workers, natives of Africa or Southeast Asia and sexual partners of the above.
The same groups are “high risk” for hepatitis viruses with the addition of persons with a history of hepatitis and natives of Asia and the Middle East.
Types of Exposure
Types of exposure within the healthcare environment associated with risks include:
• Percutaneous injury (from needles, instruments, bone fragments)
• Mucocutaneous injury from a human bite or scratch that breaks the skin
• Exposure of broken skin (abrasions and cuts which are less than 24 hours’ old)
• Eczema with breaks in the skin
• Exposure of mucous membranes including the eye and mouth

8. Measures to Reduce the Risk of Occupational Exposure
Refer to IPPOL18 Management of Sharps
9. Action Required Following Sharps Injury
Immediate first-aid following injury:
• Encourage the wound to bleed by applying light pressure around the site
• Wash the wound under warm running water for up to two minutes (this will encourage bleeding and clean the site). Do not scrub the skin
• Do not suck the wound or press directly onto the wound site
• Cover the wound site with an appropriate dressing
• Inform your manager or senior colleague and complete risk assessment form at earliest opportunity to determine actions required post-injury
Please refer to Appendix 2: Sharps / Needle Stick Risk Assessment Form.
• If further action is required due to the nature/risk associated with the injury, visit local A&E department at the earliest opportunity. Take a copy of the risk assessment form with you.
• Complete Datix risk event form but prioritise seeking further assessment/treatment initially
Contact / attend your local hospital A & E department at the earliest opportunity if risk assessment (appendix 1) deems you need to seek further medical advice
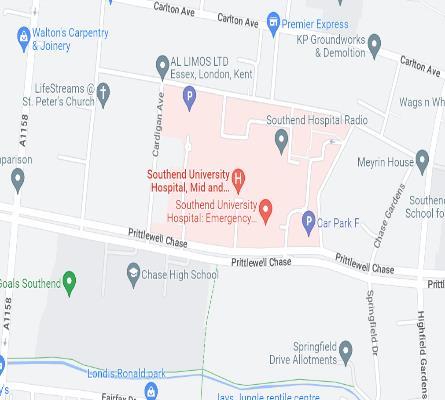
See Appendix 3 for all information on local hospitals with A&E departments
• Send completed needlestick risk assessment form (Appendix 2) to Medigold together with details of treatment/advice provided by A&E (if attended).
• Occupational health will review the treatment that you have been given and provide staff with further advice if required.
• Please send copy of risk assessment form to Medigold on the next working day even if you do not attend A&E.
• Medigold email: clinical.resources@medigold-health.co.uk

10.Consent from source patient (if known) for bloods to be taken
Once the level of risk associated with the exposure incident has been assessed, it may be necessary for the employer/line manager of the injured staff member to contact the source patient (if known) to further assess the risk and, where deemed necessary, to obtain a sample of blood after informed consent has been obtained. This step should only be taken when further risk assessment of the injury has been undertaken by A & E who have deemed it necessary to have a sample of source patient blood. Where informed consent is refused or cannot be obtained these cases must be referred to the Provide safeguarding team provide.safeguarding@nhs.net
11.Training
Provide is committed to ensuring that all staff including senior management and the Board receives information, instruction and training appropriate to their role.
Training on the risks associated with needle stick and sharps injuries are provided in accordance with the Provide training matrix (Mandatory training policy). Current BBVs awareness training is provided to all new employees as part of their corporate induction and then subsequently as part of the mandatory infection prevention training programme.
12.References
1. Directive 2010/32/EU Prevention from sharp injuries in the hospital and healthcare sector (directive 2010/32/EU) updated (2021) Accessed 07.06.23
2. UK Health Security Agency (2021), Integrated guidance on health clearance of healthcare workers and the management of healthcare workers living with bloodborne viruses (hepatitis B, hepatitis C and HIV) Accessed 07.06.23
3. Health and Safety Executive (HSE), Blood-borne viruses (BBV) Accessed 07.06.23
4. UK Health Security Agency and Department of Health and Social Care (2021), Immunisation against infectious disease (the ‘Green Book’) Accessed 07.06.23

Management of Exposure to blood borne virusesClient Actions