
16 minute read
OpCen Reports
Insight’s OpCen Reports highlight examples of outstanding responses to Triple Zero (000) calls by our dedicated staff at Operations Centres around the state.
Emily Gordon
Advertisement
Emily provided great support and reassurance to the caller, who was the mother of a disabled child with an apparent partial airway obstruction. Emily’s constant reassurance and clear instructions enabled her to keep the mother calm and focused on her child.
This rapport helped Emily maintain control of the call when the partial obstruction became a complete obstruction with the patient subsequently arresting. Emily quickly recognised the complete obstruction selecting the ProQA ‘COMPLETE Obstruction (Conscious)’ fast track button and commencing Pre-Arrival Instructions (PAIs).
During the CPR effort, the obstruction was dislodged, and the patient began breathing again. The crew arrived on scene and provided feedback that there was a positive patient outcome as a result of Emily’s actions.
Southport
The crew advised that ‘the work of the EMD on the phone and the instructions provided have quite literally saved this patient’s life and he is expected to have a good outcome’. The crew wished to express their gratitude to the EMD for their efforts on this case.
Call Lesson
This call highlights the crucial link EMDs play in the Chain of Survival. Triple Zero (000) call taking is not just about gathering information for responding crews. The instructions that our EMDs provide can literally mean the difference between life and death. Regular practice of the delivery of PAIs helps ensure confidence when navigating these cases in usually highly emotive circumstances. In this instance, Emily was literally the ‘first First Responder’.
Andrew Smith
Newly signed off Brisbane student EMD Andrew Smith received a call from two young men needing assistance after running out of fuel and water in the Jimna forest.
Andrew was able to obtain accurate GPS coordinates from his caller, and then utilise Google Maps to direct the men out of the forest to awaiting responders. Andrew demonstrated the skills of a veteran EMD in confirming battery life, acquiring alternate phone contacts, gathering geographical coordinates and landmarks, and thoroughly documenting notes for the Maroochydore dispatcher.
When it became clear battery life was becoming an issue, Andrew, under the guidance of his OCS, instructed them to hang up and he would call back every 20 minutes to update their status. Andrew and the Brisbane OCS arranged for screenshots of the patients’ location
Mark Steven
Maroochydore Operations Centre Supervisor Mark Steven got to see how the other side live when a patient presented at the Operations Centre complaining of shortness of breath.
Within two minutes of her arrival the patient arrested. Mark and CDS Simon Hansson sprang into action performing CPR. With the aid of a defibrillator they were able to get ROSC on the patient who was subsequently transported to hospital.
Brisbane
from Google Maps to be sent to the Maroochydore OCS by email to further assist with locating them. An hour and half later the patients were found safe and well as a result of Andrew and his OCS’s out of the box thinking.
Call Lesson
Whether it relates to location information, patient condition or situations involving potential risk, the importance of accurate documentation cannot be understated. Dispatchers, OCSs, CDSs, responding crews and even allied services rely on the information provided by our call takers in their decision-making processes.
Maroochydore
Lesson
With the proximity of most Operations Centres to ambulance stations, there is always a chance that a patient may present at an Operations Centre needing assistance. Ensuring that all OpCen staff have currency in their clinical skills is essential. Just as practising the delivery of PAIs assists in confidently and competently instructing a caller, regular practice of clinical skills can assist in these unexpected events whether they be in the work context or in our home lives.
Countdown on for 30 year celebrations
Where were you 30 years ago on Monday, 1 July 1991?
On this day the Queensland Ambulance Transport Brigade (QATB) transitioned to the new statewide ambulance service under the title of the Queensland Ambulance Service (QAS). This year, as we approach July 2021, the QAS is preparing to mark its 30 years of community service to Queenslanders and we are as proudly Queensland as our mighty Maroons reports QAS Heritage and History Manager Mick Davis.
From its beginnings in September 1892, the Queensland ambulance has always enjoyed a close connection with Queensland communities. As the service spread across the state in the early 1890s, each new QATB centre was established by the local community, administered and resourced by the local community and funded through local community sources that attracted a government subsidy. By 1991, there were 98 of these local administrating QATB Committees with a range of local QATB centres and sub-centres that were collectively overseen by the Queensland Ambulance Services Board (QASB). The board of 12 members was formed in 1986 having been streamlined from a previous QATB State Council of 24 QATB committee representatives. The QASB moved quickly to modernise the service and the scope of clinical practice of the state’s ambulance officers. But the local QATB Committee administrative model made it difficult to achieve standardisation of ambulance service quality, equipment and clinical practices across the state. There was also concern at state governnment level that the value of an ambulance subscription varied from QATB centre to centre. Thus, the Queensland Government established the ‘Parliamentary Select Committee of Inquiry into Ambulance Services’ which reported to Government in December 1990 (The Elder Report). The major recommendation being to amalgamate these 98 Local QATB centres into a statewide service headed by a qualified ambulance officer as Commissioner and with seven geographic regions each headed by an Assistant Commissioner who was also a qualified ambulance officer. The QATB had been moved from under Queensland Health in 1989 to be a division of the new Bureau of Emergency Services, which later became the Department of Emergency Services. Here ambulance shared equal status as a division with the Queensland Fire Service. Bureau Director Howard Baker oversaw the transition of QATB to QAS prior to and after 1 July 1991.


QAS achievements in the first 10 years
The inaugural and newly appointed QAS Commissioner Noel Gillard, from the Australian Capital Territory Ambulance, set about quickly to establish a new QAS leadership team with Dr Gerry FitzGerald (Queensland) as Medical Director, John McPherson (Queensland) and Peter McMurtrie (Victoria) as the executive team with a blend of Queensland QATB Superintendents and senior interstate ambulance appointments as the Regional Assistant Commissioners and head of Ambulance Education. Other ex QATB Superintenents and senior QATB officers were appointed District Superintendents and Officers in Charge.
The most significant initial change to Queensland ambulance was that ‘the closest ambulance would be dispatched to an emergency’. This was
Top to bottom
■ QAS 10 year Anniversary Cake. ■ QAS Heritage and History Manager Mick Davis. ■ The Ipswich Control Room.
difficult to achieve under the QATB Committee model as the expectation was that money raised locally for the QATB ambulance service would be applied locally. A number of QATB Committees were averse to their ambulance units attending cases outside of their designated area. A consequence of this change was a better opportunity for the new regional ambulance leaders to move the administrative focus from a resource focus to a patient focus. A new ‘QAS’ logo and insignia was also prepared to identiy the new statewide service.

Local Ambulance Committees
The government of the day needed to ackowledge the experience and service of those community members serving on the QATB Committees, as their administrative powers had been removed, the resources and finance that they had worked so hard to provide had now been rolled into the statewide ambulance resources and finances. Into Part 4 of the new Ambulance Services Act 1991 was drafted an important provision that served to retain the close and enduring connection between the Queensland Ambulance and the Queensland community. It was the establishment of Local Ambulance Committees (LACs) with the key function of liaising between the community that they represent and the QAS. Over the past 30 years, the support of LACs for the QAS has been outstanding. Education, qualification, scope of clinical practice

It had long been recognised and advocated that the credibity of an ambulance clinical practitioner was directly linked to both the available ambulance education and the attainable ambulance qualification. Improvement in this area of Queensland ambulance was also an important recommendation from the Elder Report to government. The Associate Diploma of Applied Science (Ambulance) had been prepared in time for the recruit intake of 1 July 1991 to be the first to undertake this course. Simultaneously, a statewide upgrade program was released for serving officers to upgrade their ambulance qualifications. A range of specialised courses established under the QASB since 1986 also were continued, enhanced and complimented. Among these were the QAS Traineeship program for younger recruits, a range of substance adminstration practices and rescue, driving and disaster management programs. Significant change included the change to regional and district level administration. This change brought about a rationalisation of communications and dispatch facilities to facilitate a more efficient application of resources across a wider area. The 98 autonymous QATB Committees each operated their own local QATB ‘Control Room’.

Vehicles and Equipment
Ambulance vehicle and equipment modernisation and standardisation was a feature of the many achievements in the first ten years. QATB Committees had procured a range of diverse ambulance vehicles and equipment with the result that a stretcher may not have been interchangeable when one ambulance transferred a patient to another.
By 1996, a Diploma of Applied Science (Ambulance) was ready for new recruits and an Intensive Care Paramedic Program (ICP) was commenced. The ICP program was a significant advancement that, for the first time in a decade, brought the Queensland ambulance into line with the other Australian and New Zealand ambulance services. By 2001 work had already commenced on a paramedic science degree qualification in universities for ambulance paramedics in Queensland.
Ambulance Operations
As mentioned earlier, a key change in ambulance operations occurred from day one of the new QAS and that was that the closest ambulance could be dispatched to a case. The next two decades

The first ten years set the foundation for QAS to become the first-class ambulance service that it is today. Rapid advancements in clinical standards, training, communications, equipment, vehicles and the use of drugs soon led to QAS becoming one of the nation’s leading ambulance services.
Top left to bottom left, clockwise
■ New QAS Commissioner Gillard with OIC and staff from Pittsworth Ambulance Station. ■ QAS Brisbane Control Room 1992. ■ Ford modular white ambulance in 1991. ■ Training scenario in 1991.




QAS rises to the occasion with successful Fever Clinic deployments
The first part of 2021 proved to be an intense period of pandemic activity for the QAS with rising concern about community transmission of COVID-19 post-Christmas prompting the deployment of two QAS Fever Clinics, the mass evacuation of a quarantine hotel, and the rollout of the COVID-19 vaccination to frontline staff. Andrew Kos reports on how the QAS has responded to the ongoing pandemic.
Left
■ Testing stations being prepped at the Noosa
Fever Clinic.
Right, top row
■ The Noosa Leisure
Centre was transformed into a temporary fever clinic.
Right, bottom row from left to right
■ Thousands came to get tested at the 24‑hour Eight Mile
Plains clinic. ■ EMU were deployed to set‑up the fever clinics.
The new year had just dawned and festive cheer was still in full swing when on 8 January a snap three-day lockdown was ordered for greater Brisbane.
Just days before, as holiday-makers travelled around the country, there was a rising concern about growing interstate clusters, prompting a call from Chief Health Officer Dr Jeannette Young for people to get tested. With demand on testing clinics peaking, the QAS was called in to assist on the Sunshine Coast and Noosa became the location of the QAS’ second fever clinic, following the first at Redbank Plains in September 2020. Emergency Management Unit (EMU) Senior Operations Supervisor Emma McKenzie said within 18 hours of a request being made, officers were testing patients presenting to the Noosa clinic. “After the success of our Redbank Plains Clinic last year we were always prepared should we be called upon again, so everything was in place for a possible deployment,” Emma said. “Working closely with the Noosa Shire Council and the Sunshine Coast HHS, we took over the Noosa Leisure Centre, transforming the indoor basketball courts into a temporary clinic. “There are a lot of pieces in the fever clinic puzzle to make it run smoothly and it’s a combined effort from many areas of the QAS including EMU, the Medical Director’s Office, the State Incident Management Room, ICT Services and the LASNs.
“Whether it was swabbing, labelling, or administrative duties, staff enthusiastically threw themselves into whatever role they were called upon to undertake.”



Just two days after the Noosa Clinic was stood-up another request came in, this time from Metro South HHS to take over one of its clinics at Eight Mile Plains.
“This was a slightly different deployment to Noosa in that the site was already operational, though we still needed to bring in our own ICT equipment and repurpose the set-up for our needs,” Emma said.
“Within a little over five hours of the request, we were accepting patients and began a 15 day, 24-hour operation.” More than 130 operational and administrative staff were rostered across the Clinic’s operational period with support coming from all areas of the QAS.
Two of those included Human Resources Officer Temika Monti and QASEC Curriculum Development Writer Kayla Markey, who both volunteered for administrative roles which included checking patients in for their tests, labelling paperwork and assisting with whatever else was needed.
“It was a great opportunity to help the organisation as well as learn new skills and I also appreciated the chance to network with staff I wouldn’t usually deal with,” Temika said. “I loved the experience - helping the QAS assist the community was super rewarding, it was nice being customer facing and dealing with members of the public to see the difference we make. “I was fortunate enough to meet some great staff that I wouldn’t usually have exposure to.” Kayla, a former paramedic, said it was rewarding to be part of something so unique. “To see how effective the team was at setting up the clinic so rapidly and watching the processes evolve as the days went on was really great to see,” Kayla said. “It feels good to be able to play a small role in the QAS response to a situation that is out of the ordinary and also to see some familiar faces from my time on-road and to meet new people from different areas of the service was great.”
During the operational period, more than 5,500 tests were performed at the Eight Mile Plains clinic by QAS officers. As this edition of Insight goes to print it is evident the pandemic is far from over, with greater-Brisbane placed into another three-day, pre-Easter lockdown following cases of community transmission stemming from Princess Alexandra Hospital clusters. The QAS had to again adapt to the changing situation with increased safety measures, surveillance testing and PPE protocols put into place for officers dealing with known COVID-19 patients.
Left, top row from left to right
■ More than 5,500 swabs were conducted at the Eight Mile Plains clinic. ■ Tests being prepared to be sent off for analysis.
Left, bottom row
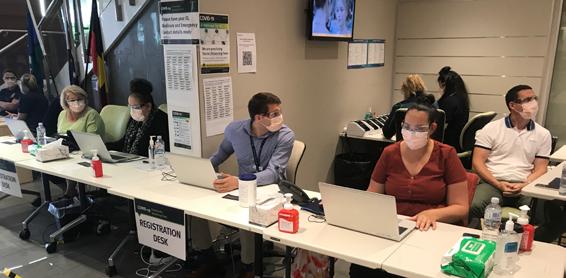
■ Admin staff ready to welcome patients at the Eight Mile Plains
Fever Clinic.
Right
■ Kayla Markey and
Temika Monti welcome patients at the Eight
Mile Plains clinic.
Grand Chancellor Evacuation
With the QAS busy running the two Fever Clinics, another major incident occurred requiring QAS assistance. Queensland Health identified potential transmission of COVID-19 between quarantined guests at the Hotel Grand Chancellor leading to a decision to have all guests evacuated to another quarantine facility so an investigation could be undertaken.



COVID-19 Vaccination rollout
The first QAS officers to be vaccinated for COVID-19 rolled up their sleeves on the Gold Coast in February.
Since then it’s been encouraging to see a positive uptake from staff eligible for Phase 1a and 1b across the state getting vaccinated as it’s become available in their region.
Staff are encouraged to get vaccinated and can contact their LASN for information on the options available. It’s important you complete a COVID Vaccination MACH Form following each dose.


Clockwise, from top left
■ Torres and Cape officer Deidree Whap gets her vaccination. ■ North West LASN Manager Brad Hardy rolls up his sleeve. ■ Gold Coast LASN officers were the first to be vaccinated.

The evacuation took place on 13 January with the QAS pivotal in the successful and safe transfer of the 126 guests over a 12-hour period.
Several dozen staff and vehicles were utilised, and our Infection Prevention Nurses and Supervisors were on site at both locations, playing an integral role in ensuring the safety of all staff, particularly in the donning, doffing and decontamination process of each transfer. Commissioner Russell Bowles said the effort and professionalism of all staff involved ensured a safe, smooth and efficient relocation of the hotel guests, something acknowledged by our colleagues at Queensland Health and allied services.
■ News clippings of the evacuation from News Corp and Nine
Entertainment Co.



■ QAS representatives at the Premier’s
Awards for
Excellence.
Premier’s Awards for Excellence

In February the QAS was named as a finalist in the Premier’s Awards for Excellence under the ‘Keep Queenslanders Healthy’ category. The QAS Demand Surge and COVID-19 Planning Team were recognised for their efforts in keeping all Queenslanders safe during the COVID-19 pandemic.
Unfortunately we didn’t take out the final gong but were extremely humbled to have been considered for the award and nominated as a finalist. The Premier’s Awards for Excellence recognises the exceptional work of individuals, initiatives and teams in driving and implementing change across the Queensland public sector and our state.







