Before I begin to highlight the many wins and innovations we have seen this year produced within the Queensland Ambulance Service, I want to start with saying thank you.
Thank you for caring for Queenslanders through the worst COVID-19 waves we had ever seen throughout this pandemic. We know 2022 has brought unprecedented challenges for the sector and the QAS has certainly borne its share.
I am constantly in awe and appreciation of your resilience, empathy and dedication and I know the community is too.
QAS has produced some exceptional patient outcomes and some of the country’s leading innovations in emergency care.
Some of these include the continued growth of the Mental Health Co-Responder program, the continued work of HCC’s 13HEALTH triage call centre and – one of my prouder moments this year – the was announcement of the Clinical Hub expansion. I know this expansion will make all the difference to outcomes for Queenslanders. While having a secondary triage system and different avenues for care will of course help with demand, the benefit the Clinical Hub brings to the patient is the most invaluable asset we have.
Another important innovation has been the establishment and growth of the Cultural Safety Unit to ensure equitable access to health care, bringing with it better long-term outcomes for all Queenslanders.
It’s also very pleasing to see QAS’s Strategy 2022-2027 being embedded – a great body of work providing the foundations for our future work to build on.
Over the year I have enjoyed reading stories of paramedics and EMDs saving the lives of people in our communities, including mums, dads, sisters, brothers, grandparents and children.
I thank you again for another year of great achievements in the face of great adversity.
I wish each and every one of you only the best for 2023.
Sincerely,
Honourable Yvette D’Ath MP Minister for Health and Ambulance ServicesAs the year draws to a close, it’s a great opportunity to reflect on what we have seen, experienced, achieved and learned throughout 2022.
Our workforce persisted through three COVID-19 waves, one of the worst influenza seasons in half a decade and ongoing pressures on our health system.
We were on the ground during floods right across the state. But we’ve also managed to stay focused on the road ahead and welcomed key milestones for us as an organisation.
In July we launched the QAS Strategy 2022-27, informed by thousands of conversations across the organisation, many I had myself with those of you who attended one of our Workforce Forums. This document will pave the way for us to become better clinicians, better colleagues, and better leaders. We will improve the way we work within, and contribute to, the broader health system. Our new initiatives will allow us to innovate, to find new ways to care for our patients and achieve even better outcomes.
As we implement the QAS Strategy 2022-27, our efforts will focus on five main objectives. These are:

You will see throughout this version of Insight, we have tagged many different stories with one of these objectives to show how what we do directly aligns with our objectives as an organisation.
I want to thank each and every one of you for your time and patience this year. Despite the many challenges we have faced, I am proud of the care, dedication and professionalism you have displayed while we care for patients and provide our state with the best possible emergency care.
I hope you have a happy and safe festive season and New Year.
Kind regards,
 Craig Emery ASM QAS Commissioner
Craig Emery ASM QAS Commissioner
 The
The
Box 1425, Brisbane QLD 4001.
If you know of a QAS ‘quiet achiever’ or an event or program with a story worth sharing with our colleagues, please get in touch with INSIGHT editor Caroline Page by email (above) or phone 3635 3900.









Summer 2022–23 edition contributors: Caroline Page, Trinette Stevens, Madolyn Sushames, Matt Stirling, Melissa Mangan, Dr Claire Bertenshaw, Jo Roy, Dr Bec Brady, Alex Thompson, Hayley Grant, Liz Brookes, Philippe Vipathkun, Corey Wakefield, Serah Steemson, Claudia Reagan-Knights, Jo Mitchell, and Michael Augustus.
Designed by: Paper & Desk
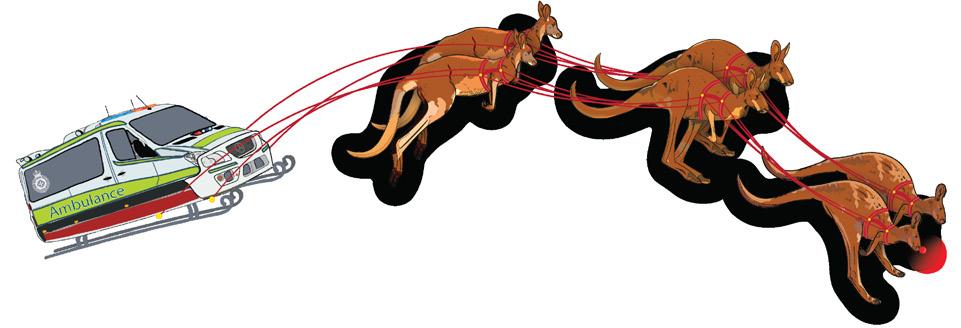
Front cover: The QAS unveiled its bright new car wraps in Cairns during a Ministerial announcement of our Cultural Safety Unit in September. These wraps feature our very own artwork, “Caring for mob together”. To read more about our Cultural Safety Unit and the new wraps, see page 13.
Over the last few months, the Queensland Ambulance Service’s Commissioner Craig Emery has announced a series of statewide appointments.
These new roles include Deputy Commissioners, Assistant Commissioner and Regional Assistant commissioners.
Deputy Commissioner roles report directly to the Commissioner, providing executive leadership within their portfolios of responsibility and contribute to the strategic direction of the QAS as a member of the senior executive team which also includes the Medical Director and Deputy Commissioner Operations, South.
Stephen Zsombok has been appointed Deputy Commissioner, Corporate and Statewide Services. This is a relatively new role within the QAS, following the organisational design changes in 2021. This role ensures statewide corporate service functions such as Finance, Human Resources, Workplace Health and Safety, Infrastructure and Procurement are delivered, and is also responsible for leading statewide operational systems and functions including the Health Contact Centre and Strategic Operations.
Stephen brings with him more than 28 years’ experience at QAS after holding various positions within QAS, including Assistant Commissioner, Darling Downs, Assistant Commissioner, Strategic Operations and most recently as Acting Deputy Commissioner, Corporate and Statewide Services.

Kari Arbouin has been appointed Deputy Commissioner Operations, North and Rural and Remote. This position was also introduced into the QAS management system after the 2021 organisational structure review. This role works closely with the Assistant Commissioners of Far Northern, Northern and Central Regions to ensure delivery of ambulance services in our central and northern communities. Importantly, this role will drive our regional, rural and remote ambulance service agenda, enabling a strong focus on ensuring local services and solutions are right for those communities.
(You can read more about Kari on page 4.)
Regional Assistant Commissioners lead all aspects of ambulance operations at a regional level, including frontline service delivery, communications and coordination and functions such as business and clinical support and workforce planning.
Regional Assistant Commissioners report to one of the Deputy Commissioners of Operations (North and Rural and Remote or South) and contribute to the QAS strategic leadership as members of the Senior Executive Management team.
Rita Kelly has been appointed Far Northern Region’s Assistant Commissioner. Rita has more than 12 years’ experience within the QAS and has worked in various roles including the Operations Centre, Clinical Education and as District Director throughout Cairns and Torres and Cape Districts in Far Northern Region.


Matthew Green is the new Northern Region’s Assistant Commissioner. Matt has more than 30 years’ experience within the QAS, most recently as Acting Assistant Commissioner Metro South Region. Matt has worked across Metro North and Metro South in various roles including Acting Assistant Commissioner, State Operations Centre and Metro North Region.

Tony Armstrong is the new Metro North Region’s Assistant Commissioner. Tony has nearly 19 years’ experience within the QAS, most recently as Acting Assistant Commissioner, Darling Downs and South West Region. He has worked across both Metro South and Gold Coast Regions as Acting Assistant Commissioner for the past four years.

Drew Hebbron has been appointed the Gold Coast Region’s Assistant Commissioner. Drew has more than 21 years’ experience within the QAS, most recently as Director, West Moreton District and has undertaken various acting opportunities as Assistant Commissioner at Cairns, Gold Coast and Metro South Region.

Michelle Baxter has been appointed Darling Downs and South West Region’s Assistant Commissioner. Michelle has more than 21 years within QAS, serving most recently as the Assistant Commissioner for the Far Northern Region and has taken on various acting Assistant Commissioner roles across a number of regions.

David Hartley has been appointed Assistant Commissioner, Strategic Operations. This position is based at Kedron and supports the Statewide Operations of our service through the oversight of portfolios including Fleet and Equipment, Statewide Workforce Management, State Operations Coordination Centre, State Communications Development, Service Planning and Emergency Management.
David has nearly 23 years’ experience within QAS, most recently as Acting Assistant Commissioner, Metro North Region since April 2021. David has also worked across Metro South and Metro North Regions and State positions including as Acting Assistant Commissioner, State Operations Centre.
Scott Revell has been appointed South East Queensland Operational Planning and Coordination’s Assistant Commissioner. The role of Assistant Commissioner South East Queensland Operational Planning and Coordination is a new position and will report to the Deputy Commissioner, Operations South.

This new role will drive operational coordination through leadership of planning, logistics and formulation and delivery of key operational initiatives which span multiple regions in the busy southeast corner of Queensland.
Scott joins the QAS from the Department of Defence and has worked across various roles, most recently as Head of Operations within the Department of Defence.
This new Assistant Commissioner role will join the QAS Senior Executive Management (QAS SEM) team, which includes my role as Commissioner, the Deputy Commissioners and Medical Director, all Assistant Commissioners and Executive Directors. The QAS SEM meets regularly to discuss issues of significance and formulate appropriate strategic responses to those issues.
District Directors or Executive Managers are responsible for the delivery of all aspects of frontline operational ambulance services within the District reporting to the Regional Assistant Commissioners.
As members of their respective Regional Leadership Team, the appointment of the District Directors provides the next step in the QAS’s significant undertaking to advance our leadership capability, support and engage our workforce and ensure we remain capable, delivering ambulance services to our communities into the future.
These new appointments are:
• Far Northern Region, Cairns District - Manjeet Singh
• Northern Region, Townsville District – Amanda Harper
• Central Region, Central Queensland District – Darren Pirie
• Sunshine Coast and Wide Bay Region, Sunshine Coast District –Hayley Salethorne
• Sunshine Coast and Wide Bay Region, Wide Bay District –Warren Painting (Grant Williams currently relieving)
• Darling Downs and South West Region, Darling Downs District –Russell Cooke
• Darling Downs and South West Region, South West DistrictGavin Trembath
• Metro North Region, Moreton District – Lisa Dibley
• Metro North Region, North Brisbane District –Sally Wuersching
• Metro South Region, South Brisbane District – Anthony Hose

• Metro South Region, Logan District – Peta Thompson (Kelsie Pelka currently relieving in this role)
• Metro South Region, West Moreton District – Jessika Brind
QAS’s new Deputy Commissioner Operations, North and Rural and Remote Kari Arbouin may hail from Glasgow, the Friendliest City in the World, but her early career move in 1990 to Julia Creek nearly 15,200km away created the perfect foundation for this role.

Kari took over the reins from Gerard Lawler in June and has hit the ground running, travelling around the region meeting staff and reinvigorating her health network contacts.
While she may not have a paramedic background, health has been a common thread and passion throughout Kari’s career.
“After narrowly missing out on a competitive medical place at Glasgow University, I was instead offered a place in Dentistry which I found unappealing so at last minute I switched to nursing, not really sure that at the time it was what I wanted to do either,” Kari said.
“Nursing in Glasgow was pretty intense, and I gained lots of experience in trauma, working in the Emergency Department at the Royal Glasgow Infirmary, the busiest ED in Western Europe.
“After a few years, including a year working with a French pharmaceutical company in marketing, I bought a oneway ticket to Australia, a place I had always wanted to travel around, but with the intention of coming back to Scotland, confidently telling my Mum and Dad I would be back in nine months.
“Leaving Scotland, I felt confident about what I would do, but arriving in Melbourne I felt lost and homesick with only $400 to my name,” Kari said.
“After two days I landed a job teaching children swimming (having competed at a national level in Scotland and with a father who was a world champion polo player) until my nursing registration came through and then took on relief nursing jobs throughout Victoria before working my way north through New South Wales and into Queensland.
“I arrived in Townsville close to running out of money and agreed to a six-week position at Julia Creek.
“Shortly after I got there, cyclone season hit and the surrounding areas flooded, the roads were cut, and I was asked to stay on for a few more months.”
Kari grew up in a 270-year-old manse to a castle in the middle of a wood with a graveyard at the bottom of the garden, and where in winter she’d enjoy skiing in the Scottish Highlands and skating on the pond – a stark contrast to the 40-degree heat, dirt and dust of the Julia Creek landscape.
“I didn’t think I’d last 6 weeks,” Kari remembers.
Six months later, the outback town and its people had grown on her and Kari found herself applying and being successful in the role of Director of Nursing.
But what was it about working in that rural and remote region that kept Kari there?
“I’d worked in large hospitals in Glasgow where all my patients were strangers to me,” Kari said.
“The experience is so very different in a small rural community.
“I quickly got to know every patient and their families, and through time, their life stories.
“I was present when they had their children and sadly, I was there too when they lost family and well-loved community members.
“As a health team we were everything we could be to the community; councillor,
pharmacist, radiologist, sometimes even requiring to be the local vet or dentist.
“In real emergencies everyone chipped in with off duty nurses turning up to the hospital, the paramedic staying on and even the cook and cleaning staff turning up to make food or clean up.
“I had never experienced such community spirit.”
Kari’s achievements shone through with the Australian Council of Healthcare Standards (ACHS) awarding Julia Creek Hospital full accreditation hospital; an accomplishment no other western Queensland hospital had managed to do. “I wanted to show that the small hospitals could have a comparable standard of care to those larger metro hospitals and with a team of committed nursing staff and GP, and we did it.”
She remembers the lead up to the survey as one of her biggest challenges.
“When we were frantically preparing for the day the surveyors arrived, I was pregnant at the time, with my due date being the actual date of the survey and I promised my team I wouldn’t go into labour,” she said.
“I remember sitting on the floor of my office night after night, writing procedure manuals on a typewriter because it was the most comfortable position.”
In case you’re wondering, Kari didn’t go into labour on survey day, and later, she went on to assist many of the other North West rural hospitals gain their accreditation.
Kari said the team also would get involved in community events, providing first aid support or health promotion talks to help the community.
But one year during her tenure, Kari earned a new and unusual title … of Champion Bog Snorkeller.
“The Dirt and Dust Triathlon started when I was working out there, and as usual, myself and other staff would provide first aid and would also get involved in the competition,” Kari said.


“One year the organisers brought out the world bog snorkelling champion from Ireland to compete and I beat her, so I won the title of Champion Bog Snorkeller which I held onto for three or so years.
“She wasn’t too impressed about that, but I believe I was the legitimate champion particularly as my bog snorkelling win involved having cane toads thrown onto me by the local kids while I was swimming!”
Kari’s time in Julia Creek lasted seven years and her achievements during this time, were recognised with an Australia Day award and a Queensland Health award for outstanding service.
She said while she and her family left the community when her children were young, the connection has remained, and they are still considered very much part of the community whenever they return.
Kari then went on to take on the Director of Clinical Services role at a private Townsville-based hospital in the late 1990s.
“One of the great things about nursing is that so many of its skills are transferrable – in many ways it’s similar to paramedicine – you learn how to deal with a range of people often at the worst time of their lives and work through this negotiating conflict, empathising and working towards the best clinical solution and always with the best interests of the patient. Kari said.
After years of being on call 24/7 call and with a young family, Kari decided to take a break from health before moving into the university sector in the early 2000s.

“This type of work, as passionate as you might be about it, does takes a toll and I needed some time away from health, so I worked at James Cook University in a variety of senior leadership roles and really loved expanding my experience
to a sector I didn’t really know,” she said.
For example, I worked for several months as interim CEO of JCU’s Singapore campus, where I had a great experience in Singapore.
“It taught me valuable lessons in working with a different culture and the need to listen and be open to a variety of perspectives.”
Another role at JCU included overseeing the university’s boating and diving infrastructure, along with managing Orpheus Island’s research station.
“This was something a little out of the box given my background, but my partner is a marine biologist, so it was a great way to understand the needs of the researchers who worked there, and of course, I became the honorary research assistant when needed.”
In 2000 Central Queensland University approached Kari to develop a business case for a campus in Townsville and Cairns, which she did successfully, taking on the role of Associate Vice Chancellor for the Townsville campus and Northwest, overseeing the building of the campus, and delivering a range of courses starting with paramedicine.
“Paramedicine was popular with students right across the North, who were studying by distance, but then had to travel to Rockhampton for their clinical skills,” Kari said.
“I felt sure that if we had a campus which could support their study there would be a greater chance of them not only being successful due to this, and having family support close by, but that they remained and committed to working in this region.
Kari maintained a close link to health during this time, taking on board and committee roles with the Northwest Hospital
and Health Service until 2020 when she was appointed the newly established Office of Rural and Remote Health’s inaugural Executive Director at Queensland Health.
Kari said on taking this Deputy Commissioner role for the North, her focus will also be on the Rural and Remote communities.
“I have a passion for these communities, and I believe we need to focus on what each community needs and work together as health professionals if we are ever to improve the health outcomes for these communities,” she said.
Given how well she knows the North and has lived and worked in Townsville, Kari said she’s currently focussed on getting to know and supporting her new Assistant Commissioners based in Rockhampton, Townsville and Cairns.
Kari said she would like to quickly get out to as many of the rural and remote communities as she can, particularly the areas with the single-officer station communities to better understand their unique challenges.
“I’m hoping to use these first few months to learn and build a better understanding of the services that QAS services in the North and meet the staff and local ambulance committee members,” Kari said.
“I am really excited about the new QAS Strategy.
“From past experience this strategy, which I can see has lots of input from our workforce, is a great opportunity to focus all of QAS on one vision.
“I want to ensure I provide clarity to that vision and support the Assistant Commissioner, Directors and staff in understanding how they can contribute to making QAS the best service it can be.
“I intend to lead with courage and curiosity: to ask the hard questions about what we do as a service and why we do things the way do. I hope then that this encourages my team in the North to do the same and in turn have their staff challenge how we might do things differently.
“We’ve gone through challenges over the last few years with COVID, but there are significant opportunities for us to consider how we can use these experiences to change health care and deliver high quality services smarter, particularly in the rural and remote communities where access to services can be inequitable.”
Kari said in previous organisations culture had been extremely important and she identified the need for a strong culture to support each other.
“As health professionals we’re often very good at being compassionate about our patients but not so good at looking after ourselves and each other so I’m hoping to contribute to developing a culture that emphasises health, safety and wellbeing so that our people flourish,” Kari said.
“I’m here to bring an external perspective to QAS and I want to see what I can do to really support that in the leaders here – to build capacity of an organisation which is only limited by the capacity of its leaders and to look at how we can have our leaders flourish.”
Kari’s use of the word “flourish” coincidently takes us back to her birthplace – it appears unconsciously she has brought a little bit of “home” to share in her own way with QAS, as Glasgow’s coat of arms motto is Let Glasgow Flourish.
■ Since leaving Scotland, Kari has continued her strong sense of adventure from diving with bull sharks in Fiji, hiking to Everest Base Camp and the Inca trail to Machu Pichu and swimming with Piranhas in the deepest Amazon. She is an avid skier and snowboarder and is always chasing the next outdoor adventure.



There are so many more deals to choose from, and so many more ways you could save thanks to a novated lease with RemServ. Call 1300 73 14 29 or visit remservlease.com.au/vehicle-offers to find out more.

the novated lease is based on vehicle quotations RemServ has received within the last 45 days and does not include any optional extras. Any optional extras that you choose will affect the cost of the novated lease and residual value. If you purchase the vehicle on termination of the novated lease, GST will apply on the purchase price you pay at that time. The novated lease offer is based on the assumption outlined above, and is an indicative cost approximation of the selected vehicle and model shown and the amounts may change at the time the novated lease quotation is completed and finalised. Your individual circumstances have not been taken into account as this will affect the overall weekly cost amount and the benefits of a novated lease. These specials cannot be used in conjunction with any other offer.
**BMW Service Inclusive - Basic is based on the vehicle’s condition based service monitoring system for 3 years from the date of first registration or up to 60,000 kilometres, whichever occurs first. Normal wear and tear items and other exclusions apply. Scheduled servicing must be conducted by an authorised BMW Dealer.

^Savings shown are indicative and reflect estimated tax savings over the full-term of the lease. The total amount saved is a comparison between a novated lease based on the assumption outlined above and the purchase of a vehicle and payment of running and maintenance costs using post-tax earnings. Actual savings will depend on your personal circumstances.
Things you need to know: The implications of salary packaging a motor vehicle through a novated leasing arrangement, including tax savings will depend on your individual circumstances. The information in this publication has been prepared by RemServ for general information purposes only, without taking into consideration any individual circumstances. Before acting on any information or entering into a novated leasing arrangement, you should consider your objectives, financial situation and needs, and, take the appropriate legal, financial or other professional advice based upon your own particular circumstances. The Queensland Government strongly recommends that you obtain independent financial advice prior to entering into, or changing the terms of, a salary packaging arrangement.
Conditions and fees apply, along with credit assessment criteria for lease and loan products. The availability of benefits is subject to your employer’s approval. RemServ may receive commissions in connection with its services. Actual vehicle price is based on specific vehicle and accessories, prices and savings may vary based on additional options selected with vehicle. RemServ does not act as your agent or representative in respect of the purchase of any vehicle. RemServ does not provide any advice or recommendations in relation to the purchase of any vehicle. Remuneration Services (Qld) Pty Ltd | ABN 46 093 173 089 (RemServ)




In October the Queensland Ambulance Service (QAS) welcomed Retrieval Services Queensland (RSQ) into our ranks.
This transition is part of the Department of Health’s Business Case for Change initiative and QAS is thrilled to have such a highly respected team on board.
RSQ is responsible for the clinical and logistic coordination of all aeromedical patient retrievals and transfers from parts of Northern New South Wales to the Torres Strait Islands, including coordinating all aeromedical resources as part of Queensland’s major incidents response and is also embedded in the State’s Disaster Coordination Centre.
It not only provides statewide clinical and operational leadership and governance for Queensland Health’s contracted and Hospital and Health Service retrieval services and aeromedical transport providers, but also delivers specialist telehealth emergency clinical support, training and education to clinicians working in

rural, regional and remote emergency departments with a focus on initial resuscitation and preparing patients for aeromedical transfer.
RSQ also provides the supporting business, publishing, project, policy, procurement, data and applications management that ensures the various aeromedical services that are tasked are safe, responsive, efficient and support equity of access to our communities and patients.
RSQ’s leadership team includes Executive Director Dr Mark Elcock PSM, Medical Director Dr Brett Hoggard, Nursing/Service Director Donna McLean and Governance and Performance Director Michael Cussen.
Mark said RSQ’s move to QAS made good sense.
“This is a strategic and sensible integration of statewide front line clinical services,” Mark said.
“We are excited about joining QAS as it will provide further opportunities to improve our clinical support to rural, regional and remote patients and their communities.”
According to QAS Commissioner Craig Emery, RSQ’s move to QAS also speaks to one of the QAS’s most innovative strategic objectives in Health System Integration.
“It speaks to our service’s growing role in the broader health system and our ongoing commitment to ensuring the right care to the right patients at the right time,” Craig said.
Stay turned for our next edition when we’ll put the leadership team in the spotlight!
The QAS Strategy 2022-27 was finalised and released in the second half of this year.
We wanted a document that truly captured the requirements of a modern ambulance service, and the conversations we had with people across the state at our Workforce Forums.
We had a lot of those conversations. All together, we ended up speaking with more than 3000 paramedics, emergency medical dispatchers and call takers, patient transport officers, managers, supervisors and support staff across Queensland.
We also had conversations we hadn’t had before.
We met with Health Consumers Queensland representatives, who rightly pointed out we hadn’t spoken to enough patients about how they saw the ambulance service evolving into 2027.
We are, after all, a service designed to care for patients first, so we included those perspectives too. Eventually, we landed on a document that to implement the five key Strategic Objectives. Some of these are obvious priorities we have always aligned ourselves with.
Caring for Queenslanders is something we have always excelled at, and which speaks to the core of our public image. This remains unchanged, but now we look to ways to innovate and grow in this space, to ensure we are always providing the right care, to the right people, at the right time.
Other strategies, like Health System Integration, will build upon existing partnerships to strengthen and move our organisation forward. As we evolve and retain our place as a leader in emergency medical care, it is critical that we move beyond the days of a ‘lights and sirens’ response and look deeper into the needs of our individual patients, and the needs of the broader health system. Initiatives like our Clinical Hub (page 54) does just that. Working within Queensland’s health system, instead of an addition to it, is our way forward.
You will hear countless highlights and examples of ways we are aligning ourselves with these strategic objectives over the years.
To help make this journey a little easier, we are operationalising the strategy and taking it on the road. So far, we have and will continue to bring Regional Roadshows to locations such as Townsville, Cairns, Mackay, Bundaberg, Rockhampton, Roma, Gold Coast and Ipswich to speak to operational staff about workforce planning. Our goal is to make this a very real, workable reality with tangible results.
As we turn the strategy into a tool kit, we want staff to consider three core questions as we hold ourselves to account against the values and ethos of the organisation:
1. What should we continue doing?
2. What should we stop doing?
3. What else could we be doing?
Our hope is that this helps each of you understand the focus of our organisational direction, and your contribution to where we see the QAS in 2027.
With Clinical Manager Amanda Martin and OIC Dean Hay
• Amanda and Dean identified the need to empower officers with the tools they need to not only achieve their potential, but excel as productive innovative supervisors
• The pair have designed and implemented training guides for supervisory roles, focusing on what already works, what QAS should start doing, and what we should stop

• This platform was founded via a 2022 Workforce Forum following feedback from staff about the need for improved training and development
• The four Development Phases break down barriers to empower the individual acting supervisor to have ownership over their own development through reflection and feedback
• The Pilot Program has informally begun in Mackay, led by Amanda
Three thousand people in 150 days covering 48 pages – one strategy for one service.
This year has seen the formal establishment of the Queensland Ambulance Service’s Aboriginal and Torres Strait Islander Cultural Safety Unit, a major milestone in QAS’s steps to improve its cultural capability to ensure it delivers excellent health care to all Queenslanders.

QAS’s commitment to Aboriginal and Torres Strait Islander peoples forms part of our Strategy 2022-2027 and recognises the need for equal access to our health system and the need for us to provide a culturally safe and responsive service for all Queenslanders.
This unit is responsible for growing greater cultural awareness, competency, and safety within the Additionally, the CSU manages the QAS Indigenous Scholarship Program, the Indigenous Paramedic Program and the Indigenous Liaison Network.
The Unit sits within the Office of the Commissioner and comprises of Executive Manager Trish Murray, two Senior Advisors, Angela Perry and Mindy Thomas and three Cultural Safety Support Officers who are based out in the regions.
Trish said through her upbringing she formed a strong connection to Aboriginal and Torres
Strait communities, particularly across the Gulf, Cape, and Thursday Island.
“My Father instilled upon me a deep respect for these cultures and their communities, he taught me to listen to their wisdom, honour their customs and connection to this country,” Trish said.
“This sentiment stays with me today.”
Trish has had a varied career, overcoming health challenges and then the adventures of being an interstate truck driver before becoming a paramedic with the QAS in 2008, where she has served at many stations across Queensland before moving to Kedron in 2019 to take on a more focused role of supporting the QAS to develop its Aboriginal and Torres Strait Islander Cultural Safety agenda.

Trish said she sees the QAS’s commitment to building long-term and sustainable approaches to being a culturally safe organisation and supporting initiatives for Aboriginal and Torres Strait Islander peoples within the health industry.
Trish said since the new unit’s inception the team’s initial work has been to create stable foundations for the agenda and strong partnerships with our regions.
“Cultural safety is every one’s responsibility. Each of us can make a difference by starting positive conversations and seeing how you can get involved and engage with your local community,” she said.
Supporting Trish at Kedron Park are Senior Advisors Angela Perry and Mindy Thomas.
Through her mother’s side of the family, Angela has connection to the Yiman people of Central Queensland.
Continuing the previous hard work of Sunshine Coast Paramedic Emma Williams, Angela has been working in the office with Trish since October 2021 helping to get the unit established.

Angela joined the service in 2005 as a Patient Transport Officer and has since held roles as a paramedic and OIC, working mostly across the lands of the Jagera, Yuggera and Ugarapul People in West Moreton.






“When I joined the QAS I wanted to make a difference to people and improve their health and wellbeing,” Angela said.
“When I was on the road that difference was achieved one patient at a time.
“In my new role I am lucky enough to be a part of a team contributing to a more culturally safe workplace for all my colleagues and better service delivery to Aboriginal and Torres Strait Islander communities. It is really the best of both worlds.”
Mindy Thomas has worked at QAS for 22 years, the last 14 of those in Operations Centres as a call taker, dispatcher and in various supervisory roles, most recently within the Brisbane OpCen.

Mindy is a proud Birri Gubba, Gungalu woman and the co-Chair of the QAS’s Aboriginal and Torres Strait Islander Leadership Committee.
Mindy comes from a family with a rich tradition of activism and brings her advocacy skills, on top of her organisational knowledge, to her role in the CSU.
“One thing I have learnt from my family is the value of persistence and to not only consider what’s been achieved by those before us, but how we can continue to grow and enhance that legacy.
“I feel that we all play a part in ensuring that we leave a space better than when we found it.
“By working together, we can all contribute to a culturally safe organisation, where everyone is supported to succeed on your chosen pathway.”
Based out in our regions are three Aboriginal and Torres Strait Islander Cultural Safety Support Officers (CSSOs)

Claine Underwood, Gemma Armit and Trent Jackson who cover North, Central and South Queensland respectively.
The CSSO are a pivotal resource in growing the cultural awareness and safety of our organisation.
The CSSOs’ roles are to promote culturally safe practices; to support their managers and supervisors build their own capacity of working in a culturally safe and responsive manner; and to provide holistic, culturally appropriate advice and consultation.
Their roles are also designed to support our Aboriginal and Torres Strait Islander staff’s welfare, engage with Aboriginal and Torres Strait Islander communities, and identify our service delivery gaps, and overall, to support the CSU, policy reform and strategic initiative development.
Claine Underwood is the CSSO for North Queensland, covering the Torres and Cape York, Cairns and Hinterland and the North West districts, and has been working with the QAS since January 1996.




He is a proud Ydinji (Cairns region) man and Yarrabah local and paramedic, and has been a long-time cultural safety advocate, particularly promoting employment pathways for people from Aboriginal and Torres Strait Islander communities.







“I am very proud of being involved in the IPP having had two cadets at Yarrabah in the early days and to see how far the program has come is very pleasing,” Claine said.
“As a CSSO I can continue to support all cadets and help them achieve what they want to achieve in the QAS.
“I am also looking forward to working with all QAS staff to work towards cultural safety within the QAS.”
Proud Bwgcolman (Palm Island) and Kuku Yalanji (Mossman to Cooktown) woman Gemma Armit is QAS’s Central CSSO, covering Townville, Mackay, Central Queensland and Central West districts and has been working with QAS since 2008.









Gemma has always worked in the region and has always been proud of her Aboriginality and her people, especially working on Palm Island.
“After having a child, I feel like I’m now ready in my career to foster change as I now feel I have the age and experience and perhaps a trusted face to now represent our people, culture and our own Indigenous officers and to work to rebuild trust in our health system,” Gemma said.



Trent Jackson is a proud Muruwari and Yuwaalaraay man who grew up just north of Brisbane and has been working with QAS since 2012, working out of Ipswich.





Trent is CSSO for Queensland’s South, including the Wide Bay, Sunshine Coast, Metro North, Metro South, Gold Coast, West Moreton, Darling Downs and South West districts, where around 38 per cent of the state’s Aboriginal and Torres Strait Islander population live.
Trent said for many years he didn’t speak out about his cultural background simply because he didn’t feel confident drawing any extra attention to himself.
“I am really excited to head out and start to form better relationships with our Indigenous communities, improve the experiences for our Aboriginal and Torres Strait Islander Staff and patients, as well as meet with all the Regions Leadership teams to see how we can work together to improve Cultural Safety within the QAS,” Trent said.


Supporting these roles throughout the state is a strong QAS Indigenous Network currently comprising 51 Indigenous Liaison Officers (ILOs) and 68 Cultural Capability Champions (CCCs) whose ranks will continue to grow over time.
The Network was formed as an initiative out of the QAS Cultural Capability Action Plan (CCAP) 2019-2022 to improve the organisation’s workforce cultural safety to improve Aboriginal and Torres Strait Islander people and communities’ health outcomes.
ILOs are QAS employees of Aboriginal and or Torres Strait Islander descent who are passionate and committed to guiding positive cultural change in Aboriginal and Torres Strait Islander people’s health care delivery – they work across all areas of the organisation.
In short, they’re QAS’s primary contacts for cultural capability and cultural safety in their Districts.
They also support the CCAP’s initiatives at a local and state level and report back to the broader Network and QAS managers on areas either demonstrating excellence or needing improvement.
The CCCs are QAS employees who don’t identify as being of Aboriginal and or Torres Strait Islander descent who are equally passionate and committed to guiding positive cultural change in the healthcare delivery for Aboriginal and Torres Strait Islander peoples.
Like ILOs the CCCs are also a key point of contact for cultural capability initiative support, advocating for initiatives at a local level in their workplace.
They also support ILOs and QAS employees in communicating effectively and sensitively with Aboriginal and Torres Strait Islander stakeholders, communities, and our patients.
Network members advocate, support and promote local and state cultural capability initiatives across QAS, provide advice and feedback to the QAS leaders and Network members around strategies to improve cultural capability and safety.
To find out more about QAS’s cultural capability or to join the network, click here or to get in touch with the unit, click here












In September, Health Minister Yvette D’Ath announced the QAS’s Cultural Safety Unit in Cairns, at the same time, using the opportunity to inspect vehicles freshly decorated with designs based on our very own “Caring for mob together” artwork.



These wraps will be used on cars heading out into communities and will play their part in breaking down barriers, to improve health equity and foster better engagement across all Queensland communities.
During the Minister’s announcement, QAS Deputy Commissioner Kari Arbouin presented the Minister with her own Caring for mob together artwork.
Top and bottom
■ Special
■
-

Fifty-five cadets across 34 Queensland communities have gone through our Queensland Ambulance Service (QAS) Indigenous Paramedic Program (IPP) since it started 10 years ago, thanks to the passion and dedication of the Cultural Safety Unit.

Our IPP is one of the only programs in the country which trains locals to work in their own communities and creates a precedent for other streams across the wider health system.
It now includes the Culturally and Linguistically Diverse Program (CALD) under its umbrella, to help more cadets achieve their full potential and the first of these graduates were presented with their epaulettes at a special ceremony last year.
We sat down with the Executive Manager Trish Murray to see how the program has evolved since its inception...
1. What is the Indigenous Paramedic (IPP) and Culturally and Linguistically Diverse (CALD) Program?
This program creates opportunities in education and employment and offer multiple pathways for Aboriginal, Torres Strait Islander and Samoan peoples to engage in nationally accredited healthcare qualifications, while working on the frontline in the field next to their paramedic mentors.
The IPP and CALD cadets work to support our QAS teams to provide respectful and culturally safe care to our patients.
Embedded within our communities, our IPP and CALD programs aim to reflect the diverse culture and belonging of our Queensland communities.
2. How did it come into being?
The program started off small in 2012, with only a couple of cadets in discrete communities because the QAS recognised a gap in local people having opportunities to care for their own mob.
We identified the need to provide better pathways in communities and to focus on recruiting local people to develop their skills and capabilities to provide healthcare to their community.
Several cadets have graduated from the program and are now registered paramedics working in their communities and some have gone on to be the Officer in Charge of their stations.
The program demonstrates the importance of buildingcapacity within Aboriginal and Torres Strait Islander communities.
3. What are the benefits for the QAS?
The program helps build respect, trust, and safety within the remote communities where our cadets come from.
This creates the foundation to empower healthcare decisions, and work towards health equity.
4. How does it help the wider health system?
The program is tailored to meet the individual learning needs of cadets and offers a scaffolded approach to achieving paramedic qualifications that aligns with the paramedic registration requirements.
There are serval qualifications cadets can access both in the vocational learning space, as well as tertiary level higher education.
We have found there is a strong bond and friendship amongst the cadets
and supporters of the program and these relationships are pivotal to helping unleash potential and form the pillars of support to assist individuals to reach their goals.
By providing more responsive and supported pathways to access employment and education within the healthcare industry, our workforce better represent the communities we serve and strengthens our ability to provide culturally safe and competent healthcare.
5. What are the benefits for our patients and broader communities?
The program’s aim is to build community capacity and to keep people on country and to achieve this, we bring the education and employment to the community, limiting the need for people to leave home, which also improves the community’s economic engagement.
Working with the community to employ local talent and providing the platform to build on skills and capability is empowering for individuals and their communities.
If you can see it – you can be it! The younger generation see their
■
■
■
culture represented in professional healthcare roles – this is inspiring, and the program provides a pathway of opportunity. Our cadets are role models, not only for the QAS, but importantly also for their community and their culture.
6. What will the IPP/CALD program look like in the future?
Our program continues to strengthen, and we hope in time we will broaden it to include more functions across our organisation, including our communication roles, the public service and corporate environment as well.
And what do our cadets think?
Jane-Sa Mose (pictured on the right) comes from a background in education and had already started her paramedicine degree when she found out about the Culturally and Linguistically Diverse Program.
“I just love the facilitators we’ve had and hearing about their experiences and knowledge,” she said.
“I find that really beneficial along with meeting people already in the field sharing their firsthand experiences in treating patients and their patient care.
“Being from a culturally and linguistically diverse background it’ll be great to be another representation of culture out in the community and being able to advocate for them as well.”
Joel Hartgrove (pictured on the right) brings a wealth of experience from the Australian Defence Force and has enjoyed the transition to the Queensland Ambulance Service.

“I take a lot of pride in my work being from defence and this is sort of similar in that aspect,” he said.

“The point of this program is to have good role models in the Indigenous community and other cultures, as well to have a face and someone they can look up to.
“Some people don’t exactly have good role models so it’s nice that I may be able to cross paths with them one day and inspire them to go down any pathway they want to.”

When Meandarra Station OIC Allison Doyle hatched a plan for a small NAIDOC Week celebration for 25 local school students, little did she know this small event would balloon into an all-day community-wide cultural event.
Meandarra in the state’s Western Downs region is a quiet, blink-andyou-miss-it town in grain, cattle and sheep country on the main road between Tara and Surat.
It comes alive during harvest time, bulging at the seams to house backpackers and farm workers, but most of the year around 250 people call it home – around 50 in the township and the rest on properties in the surrounding area.

Allison has been based at Meandarra for the last few years and in that time, noticed during a book reading session at the local school in Reconciliation Week there had never been a NAIDOC Week celebration.
“The initial plan was to open our doors, throw on a sausage sizzle and include some dreamtime stories,” she said.
Allison got cracking and applied for some grants with her LAC’s support and invited some local schools to come along.
“While I invited a few schools close by, the word spread, and others contacted me to see if they could join in too.
“Our community here has no Elders left in it, but I had a great response to a call-out I posted on social media, and we ended up with a wonderful dance troupe from Oakey, and Elders from Roma, Chinchilla and Miles sharing their knowledge.
“So, on Tuesday 12 July Meandarra proudly hosted its first ever NAIDOC Week celebration on Barrunggam country.”
Allison said their tiny town swelled with around 150 local school children from Meandarra, Meandarra Kindergarten, Glenmorgan, Westmar and Hannaford Primary Schools, alongside community members, to watch a fabulous day sponsored by the Meandarra LAC, Shell QGC, GrainCorp and The Sara St Café.
“The day kicked off at 9am with a smoking ceremony and the sounds of the didgeridoo to welcome guests into the hall performed by Uncle Greg Locke from Miles,” Allison said.
“In the hall the Mura Biri Gururu Aboriginal Dancers entertained everyone with a welcome to country and traditional dancing.
“While the dancing was hard to top, the children split into groups and rotated through a presentation of weapons and tools with Uncle Greg, as well as a workshop on playing the didge and clap sticks for the girls, and one lucky boy from Westmar was named best didge player and got to take it home.
“The second workshop for the day was with Auntie Susie Klein from Roma who did indigenous face painting and crafts with the children and once they were all painted up, they even made a Torres Strait Islander headdress (Dari).”
Allison said after a BBQ lunch for everyone, Chinchilla artist Uncle Brett Parker “Billyara”, helped the children design and paint their own school mural to take home with them, which was thoroughly enjoyed.
“The painting didn’t end there, with some beautiful boomerangs being painted and taken home,” Allison said.
Meandarra QAS also designed and had printed a special NAIDOC t shirt for the day and a goodie bag for every child - even a few parents got something special to take home.
“It was such a great day, and everyone had such a brilliant time,” Allison said.
“The level of community involvement just warms my heart – we have found Elders who are keen to continue our new connection and talk about our country here, its scar trees and its legends to our children and young people – they’ll be back in Spring to do that.
“Our local community also benefited with all the event’s food and supplies sourced from local businesses too.”
While the day lasted from 9am to 3pm, it could have continued until midnight. “I’m just thrilled it worked so well and now our community is already starting to discuss plans for next year’s event!” Allison said.














This edition looks at an unlikely wooden box containing a carbon dioxide resuscitator comprising a resuscitation face mask and a whole pile of carbon dioxide cannisters.
A century ago, when it was invented, it was believed pushing carbon dioxide into a patient’s lungs may kick-start their breathing – no surprise – it was unsuccessful, and its use was somewhat short-lived.
Click here or scan the code to hear more about this unique device from QAS History and Heritage Manager Mick Davis.


The Queensland Ambulance has a long heritage to celebrate and so much history for us to discover.
Queensland Ambulance Service announced its support for Queensland Health’s commitment to become a Child Safe Organisation in July this year and as a result, has developed a series of processes to ensure we protect the state’s most vulnerable people – children and young people with a disability.

The Medical Circular outlines how it’s now mandatory for all adults in Queensland to take positive and proactive steps to protect children under 16 years and people with an impairment of the mind, from sexual and physical abuse, including neglect, and harm.
Our child protection policy statement was developed in line with the Australian Human Rights Commission’s National Principals for Child Safe Organisations, and collectively, these principles provide guidance for our staff and volunteers to create a culture promoting the wellbeing of children and proactively adopts and implements harm prevention strategies.
QAS Paramedic Matt Bidgood is a Springfield-based ACP who has had a couple of cases which have stayed with him.
While neither case was a child safety sexual offence concern, Matt was certainly worried about the overall health and wellbeing and safety of his patients, noticing some potential signs of neglect and inadequate care.

As members of the community, and as QAS employees and volunteers, regardless of role, we all have a legal duty to protect children from abuse, and this includes if there is a reasonable belief someone may be at risk of sexual abuse.
For more information about our Child Protection policy, how to report and who to contact, see our Child Protection Framework on our Portal. For Clinicians, please refer to the CPG for Suspected Abuse.
Click here or scan the QR code on the right to listen to the discussion which includes an introduction from QAS’s Mental Health Response Program Director Sandra Garner.
The extreme rain event and flooding early this year brought many challenges for Queensland Ambulance Service, but there’s one job three of our paramedics won’t forget for a long time.

On 2 March, during yet another dreadful deluge, Flight CCP Prue Snedden and ACPs Brad Stokes and Joshua Lee were called out to a critically ill worker on a container ship stationed off the Sunshine Coast.

Normally based at Archerfield, Prue was on transfer at the Sunshine Coast and was working night shift when the call came through just after 8.30pm.
The weather was too dangerous for a helicopter winch, so Prue, along with a flight doctor, geared up and boarded a police vessel to follow paramedics Brad and Joshua to perform a difficult and dramatic overnight rescue from the container ship during this major weather event.
Prue said the first report from the QAS about *Mehir (not his real name), detailed he’d been unwell for two to three weeks but was being treated for a shoulder wound for the last fortnight before their callout.
“He had apparently received a medical consult from Italy and later a telehealth session with a Melbourne-based doctor, but all container ships were unable to dock because of the flooding and were instead sitting out in the channel off Maroochydore, so he’d been unable to get to shore for further checks and treatment,” she said.
“The QAS had contacted the water police anticipating the weather conditions were too rough for the helicopter unit.
“Initially the plan was for both teams to attend via the police boat, but, due to time to scene, the ACP crew was sent out first as they arrived at the water police depot quickly and had a plan to attempt to retrieve the patient and return to rendezvous with the medical team at the water police depot.”
“Out on the bay the conditions were abysmal – it was bucketing rain and the water was very rough, so getting onto the ship itself was a challenge.
“On arriving at the boat and boarding, it was obvious there would be delays in getting the patient off, and the deckhands’ descriptions of the patient indicated he was in a critical condition.
“Josh and Brad boarded and sent the Police boat back to retrieve us to bring more critical resources to the patient.
“Brad and Josh really made the first steps in getting to the patient safely and gave an amazing situation report which set the scene for the whole case.”
The pair faced a critically ill patient with a Glasgow Coma Scale (GCS) of 8, a severely infected, fungating wound on his shoulder and “dark coffee grounds” vomit near his bedside, suggestive of a possible gastrointestinal bleed.
“Despite the challenging conditions, everyone – especially the crew – wanted Mehir off the ship, so Brad and Joshua gave him fluids and an antiemetic in preparation for his extrication.
“From his clinical presentation, vital sign survey and brief ‘interpreted’ clinical history, it was obvious he had severe sepsis and was acidotic with fatiguing respiratory compensation.
“When Mehir was strapped into a Robinson Stretcher ready for highlining to the rescue boat, Brad rang me to discuss the logistics and that he wasn’t sure he liked them,” Prue said.
The combination of dangerous conditions, no flotation and Mehir’s rapidly deteriorating condition from that restrictive stretcher thwarted their attempts to transfer him, so Prue boarded the container ship to join the ACPs to care for him.

By the time Prue arrived on the container ship’s deck which was only minutes after getting off the phone, the patient had progressed into cardiac arrest.
Brad and Joshua had repositioned him, removed the restrictive stretcher the crew had applied, placed a Laryngeal mask airway (LMA) and were performing CPR on him.
Further care included a single adrenaline bolus and treating reversible causes, which the team had identified as sepsis, acidosis and respiratory restriction and fatigue.
“Mehir was in arrest for no more than 10 minutes before they got his pulse back,” Prue said.
“Post ROSC they continued to focus on oxygenation and ventilation until he started to self-ventilate, improve in his GCS and enable removal of his LMA.”
Prue and the ACPs then pulled together their “Plan B”, which meant managing the patient until morning on board the ship, as there was no way off with the patient in this state.
“Before I arrived Brad and Joshua had been resuscitating Mehir with a very helpful, non-English speaking crew standing around them, which was a little intimidating,” Prue said.
“Brad and Joshua stabilised Mehir and coordinated the crew to move him an enormous 600m to the other end of the top deck in the pouring rain to the first aid room, as we’d decided this was the best place to continue his treatment until morning.

“Overnight Brad and Josh did almost all of the clinical intervention, while I was concentrating on the logistics and worked the phones to see what we could do,” Prue said.
Their main challenge was to ensure their equipment and supplies lasted until help arrived the next morning.

The team created a makeshift ICU and Mehir slowly started to improve –meanwhile the weather had worsened and the police vessel along with the doctor on board had to return to port.
“Firstly, we needed to ensure we had enough oxygen – a big tank – to last until help arrived as one of the oxygen cylinders had fallen overboard earlier in the night,” Prue said.
Mehir was placed on an adrenaline infusion and given IV antibiotics, and Prue was able to get more of his medical history from his managers.
They told Prue he’d had three weeks of infection from a large shoulder wound –a staph infection – and conjunctivitis.
He had received oral antibiotics and was due to be reviewed in Brisbane by a medical team for further care.
“We made up a fluid solution for him and then warmed him up and changed his clothes which were not only wet but also soiled,” Prue said.
“We then took stock and started planning – we had six hours of power left on our monitor, 12 hours on our syringe driver, and placed him on a fluids regime in consideration of what we had on board and the risks of fluid overload.
“Knowing we had a minimum six-hour wait until a helicopter could winch him out, we checked his blood pressure and pulse manually so we could conserve equipment power for a time when we might really need it.”
Prue said Mehir improved over the next four hours … but it wasn’t to last.
“His antibiotics (Ceftriaxone) had been working and he’d improved to a GCS 13, but then at around 5am, he started decompensating,” she said.

“The severe sepsis and acidosis meant his body had used all its reserves and had nothing left – so he needed to be ventilated and intubated – impossible for us to do as we didn’t have the equipment or medication to do it safely or efficiently.
“I then contacted RSQ (the lead agency) as we believed Mehir was going into respiratory failure.”
Meanwhile RSQ had been working to coordinate a team to remove Mehir from the ship, but they’d hit some snags - the weather was still too unsafe for a helicopter winch, and they needed winch-certified staff as Prue’s fatigued state ruled her out of being safe to winch.
A third plan was hatched, and the police vessel was reactivated with a fresh team sent out in it with new batteries and oxygen supplies with a helicopter to follow.
As the team had anticipated, Mehir had a seizure at 6am and went into cardiac arrest, his second in their care, but the team intubated him and was able to get his ROSC back using adrenaline within minutes.
“We then worked out a strategy to keep him alive while the poor weather continued to delay the fresh RSQ team’s arrival,” Prue said.
“So from 6am until 9.40am we had to hand-ventilate him and his adrenaline had to continue and because he was being ventilated, he had to be next to an oxygen tank.
“We then had to make the big journey with him still intubated and ventilated to the other end of the ship where the HELO extrication zone had been identified.
“There was rain and water everywhere and by this stage we only had enough oxygen to last him another 30 mins while we waited for the Helicopter team to arrive.
“There were further delays and we had to continue to bunker down and bring resources to the extrication zone to continue care.”
Prue said when the fresh team arrived by the Helicopter just after 9.40am, she and the ACPs had never been so excited to see them.
“Compto (Anthony Compton) and Rick Harvey, the rescue crewmen brought bloods and monitoring equipment with them. Overnight Mehir’s belly had become increasingly distended, and he’d gone very pale – validating our initial diagnosis of a potential gastrointestinal haemorrhaging,” she said.
“We were then able to stabilise Mehir with four units of blood and calcium and got him into a winch stretcher, hyperventilating him as he needed respiratory compensation.”
“The pilot did an amazing job – the extrication itself was also impressive as Mehir was winched overhead from a gap between the lines of containers.”
Prue said the team’s overriding emotion when Mehir was winched out was relief and shortly after, the team was packed up and loaded safely onto the police vessel for their return trip.
Mehir managed to make it to Sunshine Coast Hospital and was later transferred for more treatment in Brisbane but despite how very ill he was, is still alive and is at home in Tanzania.
“It’s amazing he survived,” Prue said.
“He had necrotising fasciitis and to our knowledge, he underwent surgery with a large portion of his back cut out to manage the infection, and subsequently received extensive reconstructive surgery.”
Reflecting on the job, Prue said she believed had Brad and Josh not got to him when they did, he wouldn’t have survived.
“Both Brad and Joshua took on very proactive roles, they were so engaged in owning this case and providing excellent patient care in a very austere environment,” Prue said.
“They embraced new skills out of their scope to ensure the longterm management of the patient, allowing me to cognitively off load responsibility
“I am so privileged to work alongside so many great and dedicated paramedics.
“This is such an amazing example of how early communication, great clinical care, continual risk assessment and teamwork can change the trajectory of a situation and can result in remarkable outcome,” Prue said.
Kawana Station graduate paramedic Josh was in his fourth week out on the road when he and his senior partner Brad were called to the Mooloolaba wharf to get to the container ship.
Despite having had a few different careers before becoming a paramedic, this job on the eve of his 29th birthday was one he says will stay in his mind for a very long time.
“We left at around 10pm after electing to go out to the ship first because of the weatherrelated despatch delays with the flight crew,” Josh said.
“I have never been out on a boat in that type of situation, and I was a bit excited as I knew this wasn’t a typical job and there was certainly a bit of risk in it which also had to be taken into account.”
That risk started with boarding the container ship when the team was met with a rope ladder with planks, combined with a 1-2 metre swell and heavy rain.
“It was a bit daunting as you had to time your move with the peak of the wave to get onto the ladder, so you weren’t knocked off by the boat as it lifted again with the next wave,” Josh said.
“You didn’t want to end up between the two boats in pitch black water.”
Josh said the language barriers which came with the non-English speaking crew also complicated their efforts at times.
But for Josh, this job provided a precious opportunity for him to develop critical lifesaving skills so early in his career.
“I believe this was my first cardiac arrest, so, managing such a sick patient on top of his arrests; being able to ventilate him and putting in an LMA, doing compressions, putting in intravenous lines and do all the other assessments, as well as coordinating with Brad to get Prue our CCP on board and work out the best way of extrication – this is just gold for a junior ACP as there was so much involved both clinically and logistically,” Josh said.
As for his learnings, Josh said being on top of his primary and secondary assessments while studying and then being able to apply them and really get on top of them ensured he gained a strong understanding of what was going on with a patient.
“It was huge for me to be able to become familiar with the critically ill patient assessments,” he said.
“From a more clinical perspective, it was good to learn the importance of timeliness and communication, for example, Mehir was so sick he was difficult to canulate, and we urgently needed to get fluids into him and a canular into veins at the same time someone’s running iv lines ready for action, so being aware of who’s doing what in a short time span, communicating priorities and who’s doing what was an essential learning.
“The greatest highlight to me came afterwards, considering all the things we did for this man who’d gone into cardiac arrest twice, seeing how sick he was and the time we spent with him unconscious being hand-ventilated before being winched out and flown to ICU at hospital and then learning he’d been discharged later – that was such a huge highlight for me.”
“I don’t believe he would have survived another hour if we hadn’t got to him when we did, he was so critical even by then.”
With 19 years of paramedic experience behind him, Josh’s senior partner and ACPII Brad Stokes agreed this was a once-in-a-lifetime job for all involved.
“At the time it was just a case, but a few days later when I had a chance to reflect on what we did, it was so far outside the norm,” Brad said.
“Even the way the job started, because boarding the ship was going to be fairly challenging, I felt it wiser to take only what was necessary and leave the extra equipment on the boat ready for the return trip with the patient.
“But the combination of the poor weather, the language barriers and our patient’s deteriorating condition and our limited supplies saw us having to work around so many obstacles for much longer than we anticipated.
“Even the next morning the weather was so bad, when we were preparing our patient for airlifting, we weren’t just dealing with heavy rain and rough seas, there were literally waterfalls coming off the sides of the stacked containers.”

But Brad said teaming up with a fresh graduate in Josh, particularly while they waited for Prue to arrive certainly wasn’t one of those challenges.
“Josh was very good – he’s quite a knowledgeable young man,” he said.
“Some graduates are lucky to get the (learning) opportunity straight after their degrees and he was quite easy to manage and understood what needed
to be done and everything flowed really well.
“But we certainly had many long hours on our knees and crouching on the deck next to our patient, having to do things manually for hours to conserve our battery supplies, coming up with workarounds and using even the boat’s medical supplies to keep him alive and that was a huge learning curve.”
Brad said on reflection, Mehir’s survival was remarkable.

“He was so sick, and he arrested twice – it’s crazy to think he survived this,” he said.
“I went home the next morning thinking how sad it was to see a man so far away from the comforts of his family and his home, who had clearly been working very hard for a very long time to provide for his family.
“It was quite exhilarating to know he would see his loved ones again – I feel so happy for his family too knowing he’ll be returning to them.
“It’s just great to know our hard work paid off – it really was something movies are made of.”
Click on the image, or scan the QR code to view the LifeFlight footage of the helicopter rescue.
Pru, Brad, Josh and Anthony’s outstanding work saw them win the Working Together category in this year’s QBank Everyday Hero Awards held in October.
QAS was also incredibly proud to see two more staff –emergency despatchers – announced as finalists.
Gold Coast EMD Tilly Hersel was nominated as a finalist in the Ownership category for her contribution to saving the life of a 74-year-old man who had fallen off a roof, suffering multiple fractures and who then went into cardiac arrest.


Tilly talked the man’s partner through CPR until the paramedics arrived.
The man was flown to Brisbane’s Princess Alexandra Hospital with critical injuries but survived.
Cairns EMD Richard Lopes was also nominated as a finalist in the awards in the Achievement category for his behind the scenes work to improve the Cairns Operations Centre’s ethos and to foster positive cultural change within its teams.

You’ll read more about Richard’s work in the next article…
Since he switched jobs 16 years ago from a corporate role to working at the Cairns OpCen, Richard has focused on the small ways he can improve his colleagues’ daily workplace experience.
“I’ve always been interested in team dynamics and during my career change, I discovered our OpCen roles can have their struggles at times, and it took a while to feel the work I did was useful,” Richard said.
“I don’t think this was unique to me as I’ve since discovered many EMDs and ECTs struggle to come to grips with their job and this was one of the reasons I started doing what I do.”
Richard’s quest to strengthen culture and build a team ethos struck gold five years ago when he contacted Melbourne Storm’s General Manager People and Culture Michelle Young to see what he could learn from a team which had demonstrated and maintained high standards and success, and she offered him a personal tour of their Melbourne head office.
Cairns Operations Centre Emergency Medical Dispatcher Richard Lopes may be a quiet achiever, but his goal is to leave Queensland Ambulance Service a far better place than when he started – not that he intends to leave any time soon.
When little things count: EMD captures opportunities to build a positive cultureQAS AC Met North Tony Armstrong, Prue Sneddon, Tilly Hersel, Josh Lee, Richard Lopes, Anthony Crompton, Brad Stokes and AC Strategic Operations Dave Hartley at the awards. Tilly Hersel receives her QBank Award
“I wanted to know how you get people from diverse backgrounds and with different attributes and mould them together – this was my main question,” Richard said.
“What struck me straight away was when you walk into the reception area, you ring a bell and anyone, even the CEO, will come out to reception to greet you.
“The club’s commitment to safety is highly visible with an Acknowledgement of Country on the wall in the reception and there was even a WHS message in the reception about physical safety too.”
During his visit Richard met the CEO, some of the coaches, and learned the team had a high percentage of players with Polynesian or Melanesian backgrounds and how it ensured they had the support they needed, including employing welfare officers on staff with shared cultural links.
“It was the care they showed not just for the players and staff but also their families too which really stuck me, for example, holding Community Days for athletes and their families, as well as all the supporting and corporate staff and their families too, and we can learn something from that as well,” he said.
“The Cairns OpCen is one work area I believe we can develop that team spirit or ethos as we’re all together and this drives my continuing learning,” Richard said.
“Every day we come to work, do our work and go home, and often we forget while there’s the 40-or so of us in that OpCen– our family and friends are also living our work with us despite the fact we can’t discuss it in any great detail.
“It would be great if we could show our loved ones what the QAS does for the community and for us as staff.”
Since his Melbourne Storm visit, Richard has made it his business to try build that team spirit within the diverse OpCen, whether its through a simple chat, or through his much-loved rituals for new call takers.
“Maybe because we’re so protocol driven and measured, we forget about the human side of things,” he said.

“But I feel it’s important to celebrate our wins (and mourn losses) as a group.”
One of Richard’s rituals is celebrating call takers’ graduations when they’ve finished their mentoring period.
He said he does this to make the student EMDs feel welcome.
“I want them to know they start with us from a place with respect and trust they’ve been recruited for the right reasons,” Richard said.
“When our student EMDs complete their 6-9 months mentoring, I had this idea we host a morning tea when a senior EMD or I would talk to them about what it means to work in the Cairns OpCen and these are personalised for each staff member.
“For example, we had an EMD who had been an international pilot second officer and this gave us the perfect opportunity to kick it off like a Captain’s announcement and I then spoke about our code of conduct and what it means for us – it’s been really well received and I’d love to see it happen in the other OpCens.
“So far I have done this for around 10 people and I’d like to extend this and once an EMD goes from communications officer, to a senior communications officer, it would be lovely if they could have their epaulettes presented to them by someone special noting their achievements along the way.
“Suicide has touched many people both professionally and personally and every October one of our EMDs gets together a group to walk for the Black Dog Institute.
“Last year they raised over just over $5,000 and the end of the month I ran a BBQ and surprised them with a plaque and their names.
“I made the plaque up because it’s a visual reminder of what our people do and if we can create a tradition where new people walk in and see these things, it gives them an opportunity to think they can contribute.
“It also gives us a connection to the community which is something we often forget we have as we’re sitting in a room on the end of a phone, often quite removed from it all.
“We’ve got a community out there which we represent and serve, and I want to ensure our teams don’t become insular in our thinking, which is easy to do when we’re in a room distanced from an emergency.
“OpCen work is not a job for everyone; I’ve seen people come and go and I’d like to think when people do move on, they leave with a better set of skills and leave better people than when they started.”
Cairns Operations Centre Executive Manager Brina Keating said Richard does everything he can in his own power to influence up and within his peers to make Cairns OpCen a better place to work.

“Richard cares about our workers – even being a WHS supervisor for us and attending all meetings; he wears his heart on his sleeve and is passionate about making the OpCen a place we want to go to work,” Brina said.
“He has old-school values and thinks outside the box to demonstrate his care for our people.
“Over time Richard has collaborated with everyone here to create a series of rituals and beliefs for our OpCen and a lot of thought has gone into creating our culture from the ground up – not just from the top down – and we are all the richer for his work over the years.”
In October, Gary and his Sydney-based best friend Trevelyan Bale proudly rolled over the finishing line at St Leonards North Sydney, completing their last 1200kms for Kids ride from Brisbane along with 13 other cyclists and 6 support crew.

So far from this ride alone, the team raised nearly $95,600 for the Humpty Dumpty Foundation with donations still coming in.
Gary said he had so many emotions completing this final ride with Trev and the team.
“Trev and I spent many hours riding side by side reminiscing on this trip and were again riding next to each other as we reached our destination,” Gary said.
“Some of the cyclists who rode with us on our first trip joined us again just to be part of our final ride and that was incredibly special.”
The two old friends formed the 1200kms for Kids charity ride in 2006 after both had young children who’d needed hospital treatment.
“Then when I became a paramedic, the QAS’s support in kind for our venture was also brilliant, and I thank QAS from the bottom of my heart,” he said.
“Also a giant thank you to our wonderful ride paramedics over the years, James Whelan, Steve Morrish, Keith Taylor, Mick Bielby and Rene Grenfell – we couldn’t have ridden safely without them and their support and care has been amazing.”
The 1200km ride has fundraised through ride sponsorship and donations, with each participant responsible for fundraising.
“We wanted to give something back after that experience, so given we both loved cycling and because Trev and his family lived interstate, we decided to ride to each other’s hometowns,” Gary said.
“It’s easy to forget every year just how much it punishes your body because you recover and get on with life.
“You forget how much pain you put your body through for that week, but you become numb to the pain because you’re being driven by a greater need.”
“When we started this project, I was working for Virgin and we were fortunate to have Richard Branson backing us,” Gary said.
“We’ve been incredibly fortunate over the years with word-of-mouth through the cycling community ensuring we’ve got plenty of people wanting to participate,” Gary said.
And a number of those have been cycling and sporting greats keen to help.

“The first year we had Olympic, Australian and World Cup champion, Commonwealth Games medallist, the wonderful Sara Carrigan OAM join us and it was just fabulous for everyone on the trip to be able to get to know her.
“Another year, Aussie great – former professional cyclist and triple Tour de France points jersey winner Robbie

After 16 years of organising and riding gruelling annual charity bike rides, Beerwah Station’s Acting Officer in Charge Gary Richardson has hung up his helmet, knowing he’s helped raise more than $1.8 million to help seriously ill children and their families.
Gary saddles up for his last charity ride
McEwan threw his weight behind our cause and auctioned off a heap of Gran Fondo jerseys he’d signed as a special surprise – we thought he was providing just one for the auction!”
This year all but one cyclist finished the ride, bowing out with bike problems.
Gary said the ride also saw one very special person join the support crew for one last time as the group rode from Newcastle to Sydney.


“In 2010 we had a very sick girl with Cystic Fibrosis called Olivia, who with her parents’ and hospital’s consent, became an ambassador for us and who designed a leadership jersey to be awarded to those who’d battled but prevailed on the ride,” Gary said.
Most people have a special item of clothing – for some it’s a t-shirt or a signed scarf, but one of Gary’s treasured items would probably pass unnoticed by anyone who doesn’t ride.
This treasured item is a six-year-old jersey designed by indigenous artist Eileen Thompson which was signed by all the participants of that year’s ride.
Over the last 16 years the ride has raised much-needed funds for various areas of paediatric need including medical research for childhood leukemias, cystic fibrosis, childhood cancers, and has also funded much needed medical equipment for neonatal and paediatric use.
Gary said since 2016, the ride has raised money for the Humpty Dumpty Foundation, a well-recognised children’s charity which purchases essential and life-saving medical equipment for sick and injured children in hospitals.

“This collaboration made good sense as a lot of the larger hospitals have formed their own fundraising units over the years, but Humpty Dumpty steps in for the other hospitals which don’t have those fundraising units,” Gary said.
“Olivia is now nearly 19 years old and despite being recently very sick and receiving a double lung transplant, she donated $1000 through our charity to Humpty Dumpty.
“Olivia was in tears during her speech at the end of the trip as she felt we were part of her family now.”
While the charity will continue to operate after Gary and Trev retire, Gary said it may even evolve to an online ride.
“The time is right for us to retire – it’s a huge commitment to organise the event each year and COVID has hit hard,” Gary said.
“Working as a paramedic in this Covid climate means I just don’t have the time and traditional fundraising has simply become too difficult.”
As for his future cycling challenges, Gary said he’s already starting to think about Pedal for Paramedics, so he’s definitely not hanging up his helmet in the near future.
“I love this because Eileen was pleased to design this jersey for us and its design is based on the turtle,” he said.
“She explained to me the turtle’s story and how it represents life and is recognised for its resilience and determination to survive.
“Each ride we have special jerseys presented to participants perhaps for outstanding efforts each day or money raised and somehow I ended up being presented with one, so I got everyone to sign it as a memory of that ride which adds to the meaning of the image on the jersey especially why we created our charity and have kept doing these rides for so many years,” Gary said.
But, my story isn’t so much about my work, but my life with Multiple Sclerosis (MS).
MS is an incurable auto-immune disease that presents itself differently with each patient.
I was diagnosed with MS in April 2016, after noticing some strange things happening with my body.
Everything was innocuous to start with; some leg heaviness, some night blindness, some lack of balance –nothing that I really tied together as being a problem.
I was 52 and obviously old age was kicking in.
In December 2015, another seemingly minor occurrence, kicking two toes on a door, gave me a “stubbed-toe” sensation, but it never went away.
In fact, it spread over my foot and up my leg and it was at this point I saw my GP, who did some initial tests, largely regarding balance.
A computerised axial tomography (CAT) scan was done, followed by a quick referral to a neurologist. A magnetic resonance imaging scan (MRI) soon after confirmed a diagnosis of MS. I was lucky, as it was an early diagnosis.
It took around 12 months for a suitable treatment to be found, that my body would accept. By this time, that “stubbedtoe” sensation was up to my chest and spreading into my hands.
This was not going away and these days I receive an infusion every six months to keep my symptoms under control.
In January 2018, I was reading the MS QLD newsletter, where a very small story
on the last page caught my eye about an event called the “Oceans of Hope Challenge”, being held in New Zealand later that year.
This event was designed to bring sailing to people with MS and was being held on the Spirit of New Zealand tall ship, sailing for a week in the waters around Auckland. The concept of the event caught my eye, this was something I could still do.

I don’t have a history of sailing, but I was drawn to the idea.
My disease at this point had progressed but then regressed following treatment – I still had mobility, albeit with some wobbles, I had arm strength still but I had lost reading vision in my right eye, which is still the same now.
My family was totally supportive of my intention to head to New Zealand and it was just a case of time and money now.
An adjustment to my leave was approved, and I managed to gather enough funds to cover the trip.
That was it, I was going sailing.
Oceans of Hope was started by Danish doctor, Mikkel Anthonisen who had been treating a patient who was building a sailing boat when diagnosed with MS.
His patient thoughts his dreams of sailing were over, but with encouragement from Dr Anthonisen, he continued to complete his boat, and managed to fulfill his dreams.
Dr Anthonisen then decided to take this idea of sailing for MS patients further and in 2014/2015, the sailing boat, Oceans of Hope circumnavigated the globe crewed by people with MS, along with a skipper and first mate.

The crew stayed with the boat from legto-leg and changed crew along the way.
MS patients had to complete all tasks associated with sailing around the world – raising sails, navigation, cooking, cleaning – all aspects of sailing.
The beauty of a sailing boat for someone with MS, is that there are many grab points and hand holds around the boat, so mobilising becomes less of an issue.
People with MS often feel they are unable to live a normal life, unable to mobilise normally, and often experience depression because of this.
Being able to participate and contribute to life on board a boat/ship, makes you feel less disabled, and more able to participate in activities and this was certainly the case for me.
My goal on boarding the Spirit of New Zealand was to determine if I was normal for someone with MS.
I commenced my service with QAS in January 2012 as an EMD at Southport OpCen and am now a PTS dispatcher at PTS Spring Hill, having been here since early 2021, Ray Holden writes.
I had never met anyone else with MS, so did not know if what I was experiencing was “normal”.
I quickly discovered I was very normal for an MS patient and this took a great load off my shoulders – I was okay.
Following the NZ challenge, I wanted more. Something inside me was stirred.
I had spoken to some other sailors about a previous challenge in Turkey and a few other sailors and I decided if a challenge in Turkey was to happen again, we would go.

In October 2019, five of us travelled together to southern Turkey, to sail in the Mediterranean Sea, in the waters around Fethiye.
What a trip! We sailed on 45-foot sailing boats that were very luxurious, compared to the large wooden tall ship in New Zealand.


We spent three weeks in Turkey, taking the opportunity to visit Gallipoli, Istanbul, and hot air ballooning in Cappadocia and it was an amazing journey.
Following this was a journey back to New Zealand, this time aboard the worldrenowned racing yacht Steinlager 2, an 86-foot ocean racing yacht.
It was very different sailing, but also very fast and very exciting. Obviously, my appetite was whetted. I was hooked and looking to see what was coming next.
Unfortunately, no one saw Covid-19 coming and along with the rest of the

world, all sailing plans were put on hold and I wasn’t going anywhere.
Fast forward to early 2022, and the world has started opening again.
We refer to Oceans of Hope as the “mother-ship” as this is where it all began, and something was drawing me back to her. Finally, I had an opportunity to sail again.
I recently returned from three weeks in Denmark in July comprising two weeks of exploring Denmark by train by myself, and a week sailing.

What a great trip and a great country to visit!
The Danes are very accommodating, and they live a life very similar to our own and their summer weather is much like a Brisbane winter, even warmer.
We sailed with a crew of five, with six MS patients on board, some Danes, some Dutch, and a lady from Portugal. We had a great time and new friendships grew.
We sailed overnight from Denmark to Sweden, where we stayed 2 nights –it was a new world for me, somewhere I’d never been.
Had someone told me five years ago, this what I would be doing, I would have thought them crazy as my life was very safe, very secure and very risk free.
The Oceans of Hope program has been life changing for me.
It has given me new hope, a purpose for doing what I do, and certainly a view into my future life – I have discovered “me” again.
As for how I manage work with MS. Well, initially it was a matter of adjusting my shifts, so that I was only doing one night shift, not two and when I went to Laru dispatch in Kedron, my latest finish was midnight.
Now at PTS my latest finish is 2200, so home by 2300.
A big factor for me, is fatigue. So, night shifts are out, doctors’ orders. I manage to work full time, and a certain amount of overtime and I seem to be surviving this way.
When not working, I do have my share of nanna naps. I just know to stop when needed.
With the sailing, while it doesn’t directly assist my work, there are psychological benefits to knowing that working hard will bring some reward, eg, an overseas trip.
It gives me a goal to focus on and I guess, some resilience training, to know I can overcome adversity. There are always challenges while sailing, solutions to be found, difficulties to endure.
What is my next move? I am off again to New Zealand in November, sailing on Steinlager 2 for a week and a great chance to catch up with some old friends, and certainly make some new ones.
We are hoping to hold an event in Australia in the future but in the meantime, Turkey sounds nice next year.
I have to take every opportunity as it presents itself as I don’t know what course my health will take, or what the future holds for me.
If I have learned anything from this, it is firstly to listen to your body. If something seems off, get it checked. Take any opportunity you are given, as it may never come again.
If anyone has MS or a friend or family member with MS, please consider reading up on the Oceans of Hope, or the Oceans of Hope Challenge UK. Even if you have never sailed before, it doesn’t matter, you will fit in.
A Kawana Station ACPII, Emma is a Wakka Wakka woman (Gayndah and Eidsvold area), a QAS Aboriginal and Torres Strait Islander Leadership Committee Member and an Indigenous Liaison Officer.
Emma said she decided to embark on this journey to support her partner James McAlloon, whose original plans in 2020 to walk from coast to coast across Australia were thwarted at the halfway mark by the continuing COVID-19 Western Australia border closures.

“James works in travel and his 2020 walk raised $30,000 for those in the South American travel industry who had lost work due to the pandemic and were plunged into poverty,” Emma said.
This year, James and Emma set off on the second part of the trek from Alice Springs on a new path to Broome, bush camping on their way north to the Indian Ocean – still matching the distance James had originally planned to walk.


“This time, as part of our walk ‘Footsteps for Good’, we raised funds and awareness for Purple House, an Indigenous-owned and run Alice Springs-based health service which has 18 remote clinics through the Northern Territory including a mobile dialysis unit, called the Purple Truck,” Emma said.
“We chose Purple House as its focus is on getting patients back home so families
and culture can remain strong, and it contributed directly to the communities we travelled through.”
Emma and James had previously taken on longer walk challenges, but this was Emma’s first significant trek.
“About 18 months ago, we walked unsupported, 230km over four days (with about 6000m of elevation) from Merimbula to the summit of Mt Kosciusko – one of the Sea to Summits on the seven continents,” Emma said.
“For the Alice to Broome trip we trained for about two months, just walking, which seemed really tedious as I prefer to run, swim and cycle – I had to shift my mindset and get used to walking up to 30kms a day and be able to back it up the next day which thankfully, shift work allowed for.”
The couple’s route followed the 1000km iconic red road of the Tanami Track, which included 700kms of dirt, sand and gravel road running through the Tanami Desert between Alice Sprints and Halls Creek.


“It’s a well-known track but it’s difficult logistically because of how remote it is, so we had to be very focused on our food and water consumption and where we could restock,” Emma said.


“At one stage we had 550 kilometres between points to restock our food and water supplies.
“While there was no phone service, we did have a satellite phone and two emergency position indicating radio beacons (EPIRB), just in case.”
Emma said there were only a few hairy moments during their trek – one at around 500kms between resupply points when they were low on food despite some rationing and became a little calorie depleted by the time they got to their next shop.
“We bought Nutella and peanut butter and calorie overloaded when we were able to stock up,” she said, “Although I haven’t eaten it since!”
The couple’s logistics were made somewhat easier thanks to their “engineering genius” flatmate who built them special trolleys for their luggage, equipment, and supplies.
“James knew what we needed and had learned from the negatives in the first half of his challenge,” Emma said.
“The trolleys had to be sturdy enough to carry up to 60 litres water and needed 26-inch mountain bike wheels, as they’re easy to fix in the middle of nowhere.
“We started with a trolley prototype and made modifications over the training period.
“Their total weight empty was 26kg, so we were able to take 40-60 litres each of water, 5-7kg of clothes, swags (about
10kgs) and about 15-20kg each of food (reducing daily).
“When fully loaded, they weighed around 100kg.”
Because of the trolleys’ weight, Emma said it was easier to push rather than pull them on the dirt roads.
“Pushing the trolleys through the sand was difficult because they were big and heavy, but if you got the right roll, you could go through the corrugations.
“The rocky surface was more difficult, as you could never get an even roll,” she said.

The couple was wary of the traffic as the road trains were huge and travelled at faster speeds.
“On the Tanami the traffic was okay –you had plenty of notice as you could see the dust kicked up by the road trains for kilometres.
“The road train drivers were great and if they could, they’d drive right over on the side of the road to factor in their dust trail, so we weren’t covered with it.
“We never felt threatened by anyone, and everyone was so friendly it was incredible.
“On the Tanami track, everyone was curious and engaging, but as soon as we got out on the bitumen of the Great Northern Highway, compared with the trucks, the motorists weren’t quite so considerate, and we had a couple of close calls from caravaners’ side mirrors.”
Emma said wildlife wasn’t a concern because of the desert ecology and there just weren’t a lot of animals around.

“There were occasional dingos, but they didn’t give us any trouble,” she said.
“We camped one night in a field of cows who were a bit curious, and James didn’t see a couple of the big tiger snakes we walked past – but all in all, we felt safe.”
One thing which didn’t cease to amaze Emma was the landscape.
“It was so refreshing to be disconnected from technology and to reconnect yourself with just being on country, in the middle of nowhere and enjoying that experience for what it was,” Emma said.
“The stars were spectacular, the magical sunrises and sunsets, and the sheer number of different colours – they were absolutely breathtaking.
“In the city we don’t take the time to stop and look at them and often, we’re in such built-up areas, we don’t have the real darkness, the space or time to stop and look around.
“Being out there, getting up at dawn and finishing at dusk it was all out on show and the skies were so clear and the stars were so bright.”
And how did the couple’s relationship survive the trek?
“No one got buried in the desert!” Emma laughed.
“There were always going to be difficult periods because it was physically and mentally challenging.
“But we worked as a team, so when one of us was down, the other picked us up.
“We never argued… but we had days when one of us wouldn’t want to walk as far, or was a bit cranky.
“We knew we could always walk a little apart – there was certainly plenty of space out there and we would always sort it out over dinner that night.”
Emma said they certainly got excited, and their spirits lifted when they finished the dirt section just south of Halls Creek – seeing the bitumen and knowing they only had 700kms to go to Broome.


“Once on the sealed road our legs were fine, but the trolleys got a lot more punctures,” she said.
“We went through three inner tubes each and needed an emergency dash to a shop at the end to get more!
“Walking along sealed roads meant we were able to punch out 45-50km days (instead of 35-40) which got us to Broome ahead of time.
“One day we chose to walk 57kms just to get to a free campsite which had tables and chairs – a bit of luxury compared with our fold out camp stools – so we worked hard to get there.”

Emma said the pair was extremely grateful to have finished their walk in one piece and uninjured.
“We finished five days ahead of schedule and were therefore able to explore and enjoy the beautiful Yawuru Country,” she said.
“A huge highlight on our arrival was receiving a Welcome to Country and smoking ceremony from Local Elder Aunty Pat Torres – it was lovely after travelling so far to know we were welcome to explore her beautiful Country.”
Emma said she and James were thrilled to be able to contribute to the great service Purple House provides and hoped to raise more funds for this important cause.
If anyone would like to contribute, click here
As for their future plans… it’s clear Emma and James won’t be storing their swags for long.
“James is already planning his Sea2Summit Antarctica which will be a world first in November 2023,” Emma said.
“For me, I am considering cycling from Alice Springs to the Sunshine Coast so I can also complete an unsupported transAustralian crossing….watch this space!”
of the trusty handmade trolleys loaded up and ready for action
If a member of our ambulance family passes away, QAS Legacy Scheme is there to help the spouse and children who have been left behind.

The scheme strives to ensure no surviving spouse, partner, or child will ever feel forgotten.

The QAS Legacy Scheme does not receive any government funding and is funded by donations and fundraising which is predominantly through fortnightly tax-deductible payroll contributions from current members.
Other funding comes from bequests and tax-free donations, often from retired paramedics or members of the public expressing appreciation for work done by ambulance staff in the community.
You can help QAS Legacy Scheme continue to provide its valuable programs by donating. Donations of $2 and over are tax-deductible and will assist with the ongoing support of all ‘QAS Legacy families’.
If you’re interested in donating, or would like to find out more, go to www.qaslegacy.org.au.

We are a compassionate charitable organisation providing a range of services to QAS families who have suffered the loss of a loved one, ensuring they are supported in times of need.

Motorists are now legally required to move over and slow down after new laws aiming to keep our frontline workers safe were introduced on 16 September this year.
The Queensland Government’s Move over, slow down road safety campaign recognises our emergency services and roadside assistance workers do an incredible job and play a critical role in responding to roadside incidents.

The campaign’s safety messages include:
• If you see flashing lights at the roadside, it’s as easy as moving over and slowing down
• If you are travelling on multi-lane roads, this means that you will need to change lanes to give as much space to the roadside incident as possible, or if it’s a single lane, then move over as far as possible within your lane and slow down to a safe speed.
While many motorists already do this, the rules send a clear message that workers and the people they’re helping can expect to be safe from harm.
The new rule applies to ambulances, police cars, fire trucks, and transport enforcement vehicles, as well as breakdown assistance providers such as RACQ, tow trucks and assistance vehicles.
Penalties for not moving over and slowing down will cost offenders $431 and three demerit points.
For more information, visit the StreetSmarts website.

A casual information session at Queensland AFL Girls Academy
turned into a perfect yarning circle for Far Northern
Leeanne Gray.
Ian is a Cultural Capability Champion for the Far Northern region and when QAS was invited to attend the Academy’s information session in June, Ian jumped at the chance to chat with students what a career in the service could look like.
“We wanted to give them a bit of an idea about what it’s like to be a paramedic and gauge some interest on whether some of the girls would be keen on a career path with QAS,” Ian said.
“We gave them all the options and spoke to them about what they could do.
“A lot of these girls come from Cape York and very remote areas in Queensland, so they don’t get the opportunity to talk to paramedics as a lot of these places are coordinated by
Queensland Health, so it was the first time a lot of them saw an ambulance without it being an emergency.
“They were a little bit shy and reserved at first, but once it opened up into more of a yarning circle, they opened up to us and it went really well.”
Ian said that’s when the questions started to flow.
“We spoke about all the scholarships available to students and everything to do with the QAS and paramedics in general, from communications to first aid training all the different things they could aspire to,” he said.
Then they took the group through the ambulance and gave a demonstration of the different pieces of equipment.
“That was the best part, they became very interested in all the equipment,
what it was used for and what circumstances we would use it in,” Ian said.
“At the end a couple girls came up to me said they were now starting to think about career path with QAS.
“It’s really important they get out there now and fly the flag at their schools to promote first aid safety, how to call Triple Zero (000) and the career path opportunities there are, especially for those from a culturally diverse background to get into QAS.”
Ian said he and Leanne were already planning their next visit with the AFL Academy to hopefully inspire more young girls to choose a career they’re passionate about.
“It was a really good opportunity to speak to the girls, it was a real hit,” he said.
at Redlynch paramedics Ian Day andFor two of our staff members, Jan’s emergency was a first for them in their early careers.
On 9 April, 58-year-old Jan and her sister sat in the audience watching a band at Mansfield Tavern when her sister noticed she had gone limp and stopped breathing.
Bystanders rushed to her aid and called Triple Zero (000) –Jan was suffering a cardiac arrest.
Emergency Medical Dispatcher Monique Bolton answered, and this was her first time talking someone through CPR.
Monique guided bystanders through compressions while they used an AED to deliver two shocks before the ambulance arrived.
before transporting Jan to the Prince Charles Hospital for further treatment.
This was also Critical Care Paramedic intern Alex Cattaneo’s first time using the MCCD and he said it was very effective.
“We put the mechanical device on straight away, so we didn’t have to coordinate changeovers and that was quite effective,” Alex said.
“We only conducted CPR for a brief period, about three minutes of compressions and two shocks.”
Alex said this was all that was needed for crews to regain a pulse after about 15 minutes of downtime supported by CPR.
Jan spent about two and a half weeks in hospital and about month later walked through the Capalaba Ambulance Station’s doors to thank the crews who helped save her life.

Jan and her sister presented the paramedics with a certificate of appreciation.
“If it wasn’t for Alex and the other paramedics, I wouldn’t be here now,” she said.
“I can’t remember anything from that day, but I understand there were doctors and nurses at the tavern at the time –I was just lucky they were there too.
Alex said it was interesting she remembered little of the day. “The first thing she remembered was some vague memories after she was extubated at the Redcliff Intensive Care Unit,” he said.
As soon as paramedics Alexander Cattaneo, Tricia McIntyre, Aishah Ahmed, Sandra Cowley and Julie Hughes arrived, they took over resuscitation, using the mechanical compression device (MCD) and delivered five more shocks
“It was great to meet Jan looking so well and if anything, her case emphasised the extremely important role the bystander played with their early CPR and Defibrillation which certainly contributed to her positive outcome,” Alex said.
Left and right
■ Card from Jan
■ Paramedics Tricia and Alex with patient Jan and EMD Monique.

Frontline workers don’t do what they do for praise, so when cardiac arrest survivor Jan Williams contacted QAS to thank the crew who saved her life, they jumped at the chance to meet her again – properly.
In May, the Queensland Ambulance Service (QAS) joined a major multiagency exercise at the Brisbane Airport to test and hone response capability in a steady-state and elevated crisis management stance.
Crews faced the scenario of a major aircraft crash at the busy airport involving multiple patients with varying degrees of injuries including fractures, wounds, grazes, burns, head, and crush injuries.

Several crews, including Critical Care and the High Acuity Response Unit (HARU), were tasked with assessing, triaging, and treating about 50 patients before deciding which hospitals to transport them to.
QAS Major Events Coordinator Luke Bamford said for this exercise, the QAS and Queensland Health’s focus was on the triaging process during a prolonged incident.
“It was not only about the response to mass causalities at the incident site but to work with Queensland Health staff to coordinate the greater distribution of these causalities in the health network while considering
the demand of business-as-usual workload,” he said.
“Both teams worked well together, with the QAS working as the primary medical triage and response agency, backed up by the Queensland Health’s Metro North team.”
But the biggest challenge the teams faced was the weather.
“The exercise was held in extreme weather conditions involving heavy rain throughout the entire exercise, so it felt very real,” Luke said.
“Brisbane Airport was also an active live environment during the exercise, so safety and security measures had to be put in place.
“If a significant incident such as a plane crash did occur at the airport, you would expect the airport would be shut down to would give us greater access to the area.
“It’s always difficult to make the exercise world feel real and not roleplaying, but I think we achieved it with realistic scenarios and injuries that required treatment and patient distribution coordination.”
Luke said practice like this ensures crews are ready to hit the ground running with QAS’ emergency service colleagues if (or when) they happen.
“Working with established partners like the other emergency services goes smoothly because of the amount of work we do together daily,” he said.
“Creating new relationships requires a bit more work to understand each other’s capacities and capabilities, so this is why we hold exercises and discussions – to be prepared and ready for when we need to stand up and respond to a real-life incident.
“Being able to explore Queensland Health’s response support capabilities both on-site and through the Health Emergency Operations Centre (HEOC) to assist with large volume and critical patient flow into the hospital network was also hugely beneficial.”
Training exercises are vital to ensure emergency services get it right in real life, no matter how big or small the scenarios are, Madolyn Sushames writes.
As an Advanced Care Paramedic (ACP), Troy Heise’s job is to help save lives. Now, the lasting legacy of his 12-year-old son Flynn is doing the same after a tragic accident cut his life short, Madolyn Sushames writes.
Flynn’s heart, lungs, liver, kidneys, and eye tissue were all donated to help save several lives following his passing in early 2021.

“The fact Flynn was able to keep fighting meant he passed away during surgery and he still lives on in others,” Troy said.
“I’m a paramedic, but my little boy saved lives.”
Troy and his family shared their story with The Project which went to air nationally for DonateLife Week (24-31 July) in the hope it encouraged more families to consider organ donation.
“We had a strong view if we shared Flynn’s story it would encourage families to talk, and our aim was to highlight children need to be involved in that conversation,” Troy said.

“We wanted people to think and act and it appears they’re doing that.”
Within five minutes of Troy and Flynn’s story going to air, there were 1300 new organ and tissue donor registrations.
Their story was viewed more than 80,000 times and continues to inspire many more.
It only takes a minute to register as an organ and tissue donor at www.donatelife.gov.au.
Troy said everything he has been through has shaped the way he now approaches his role as a paramedic, saying you couldn’t go through a tragedy like this and not be changed.
“I’m very aware of the fact that a family will listen to every word I say because not that long ago I was that family,” he said.
“I feel like maybe I might just be the right person at the right time to support that family going through what they’re going through because of my life experience.”
Troy said it had also changed the way he saw what some people deem to be negative patient outcomes.
“If someone has made it back to a health service and that family is able to have a few more hours or days with them to grieve or talk or share, that’s a win because there are many times that doesn’t even happen,” he said.
“As paramedics we’re around death more than the average person and it has raised how do we cope with that and how can we make death not-so-dark.
“It’s something we need to talk about and highlights that we need to look after each other. Every paramedic needs to look after themselves, their family and their friends.”
Above
■ Flynn Heise. Inset
■ Troy and Flynn Heise.
Michael was a fresh second-year ACP finishing his shift on the night of 12 October 2002 when a patient presented with burns and a fractured arm, saying he’d come off a plane from Kuta where there had been an explosion.
“Our initial reaction was that were hesitant to believe him,” Michael said.
“There was just so much confusion, but his injuries were compatible with an explosion, but no one knew about it.”
By lunchtime the following day, that had all changed, and Michael was being called back into work – it was all handson deck.
“I remember gathering at our station and there was this air about,” he said.
“We didn’t really know what had happened and we were being drip fed information because we had no technology.
“Then it started to filter through that something had happened, and it was an attack.”
Michael and his colleagues were told planes full of survivors would be landing at Darwin Airport and it was their job to triage, treat and transport them to hospital.
“At the time there were only three ambulances on at any given time in Darwin,” he said.
“When we drove up to airport I saw 13 ambulances and I had never seen that many.
“But when the first person we pulled off the plane went into cardiac arrest, that’s when we knew it was really bad.”
Michael said the whole of Darwin worked together that day.
“There were hardly any Triple Zero (000) phone calls over that weekend, motorists would stop when they saw you driving past and flash their lights to show respect,” he said.
“There were so many patients in hospital who weren’t related to the blast who saw the news and went home.
“A woman from Adelaide ordered 100 pizzas to the hospital for us.
“As awful and nervous as were were and as scary as it was, it was reassuring to know there are good people out there.”
It’s a lesson Michael has kept coming back to throughout his career as part of the response team to the Christchurch Earthquake in 2011 and working on the same day as the Melbourne Bourke Street incident.

He said it was jobs like these that show you what you’re truly capable of.
“When the heat is on and you have a situation, you get to the point where you transcend the everyday and you just figure it out,” Michael said.
“The other realisation I had was that whatever problem you’re facing you will figure it out and you will go home.
“A lot of paramedics aim for perfection and that’s great, but I don’t think the perfect job exists – you just do the best you can.”
Michael spent time reflecting on his experience in Darwin at a recent reunion with his former colleagues.
He said while the actual event wasn’t discussed much, the lessons learnt shone through.
“At that point in my career I was just a baby and I thought this is what ambos did, I don’t think I gave it the respect it deserved until recently,” Michael said.
“I see it here at work now with graduate paramedics when we go to heavy jobs and I ask if they’re ok, they’ll say yeah they’re fine but perhaps don’t really process it.
“You will see trauma over your career as a paramedic and it might be in the first year or two and it doesn’t take away from the fact that it’s trauma.
“You will see horrible things and be tested and stressed out but you will see some good, even if it’s just that feeling of comraderie or working together to achieve common goals or the kindness of others.”
There are some cases that you go to or calls that you may take that you may never forget. This is normal when you experience something that is out of the ordinary. The cases that Michael is referring to are certainly out of the ordinary.
Exposure to potentially traumatic events may change your perspectives on life. Michael’s experiences have helped him to recognise that he is resilient and can face significant difficult events.
Likewise, through these events, he has also recognised that perfection is not always possible and that sometimes you just do the best that you can.
These are all signs of the potential for Post Traumatic Growth.
This is where we may not just become more resilient but experience positive changes as a result of trauma and extremely difficult life events.
Michael also talks of how he supports his colleagues by asking them if they’re okay and of recognising the importance of comradery and kindness.
These are protective factors in the context of exposure to potentially traumatic events.
Being able to talk to a trusted colleague about your experiences of a difficult event can provide an opportunity to downregulate your sympathetic nervous system and allow your brain to make meaning of something that may otherwise be extremely confronting. Who is your go-to person?
Sometimes you may still have intrusive thoughts and hyperarousal following a potentially traumatic event and this can be very normal. If this continues for more than a couple of weeks, then this is a good time to access additional psychological supports.
Michael Holmes may have been a paramedic for more than 20 years, but few things will ever compare to the day the first of the Bali Bombing victims began to land in Darwin, Madolyn Sushames writes.
Wynnum Station’s Acting Officer in Charge Joshua O’Grady represented the paramedics to also thank the Rickwoods and wish them well.
“I’d like to thank you both for all you’ve done to make life easier for us over the years and we certainly appreciate all the extra work you and the LAC have done at the station,” said Josh.
QAS Heritage and History Manager Mick Davis said the Rickwoods had also been the lynchpins of the Wynnum Museum.
“Ray and Monika Rickwood brought to the Wynnum Local Ambulance Committee and the Wynnum Heritage Ambulance Station, a well-established relationship with, and the respect of, people of the Wynnum area,” Mick said.

“They had a business in Wynnum’s CBD that served the local community every day for many years.
“This local knowledge was a significant asset to both the LAC and QAS Heritage, no matter what local issue or questions might arise.
Beside him stood his wife Monika, happy to let Ray do the talking as usual, but equally emotional.
After many years, Ray and Monika, both Wynnum residents and Local Ambulance Committee (LAC) stalwarts, have decided to hang up their hats and retire from their volunteering to take some long-overdue time out for themselves.
A master plumber by trade, Ray joined the Wynnum LAC more than 26 years ago, and Monika followed close to a decade ago, “to make up the numbers”.
Their daughter Michelle is also a member of the same LAC and joined around the same time as Monika.
Metro South’s then Acting Assistant Commissioner Matthew Green was at the gathering to farewell Ray and Monika and thanked them on behalf of the QAS and Wynnum communities and presented the couple with Certificates of Appreciation and a plaque to Ray for his 26 years of service.
“The Wynnum Museum and Station are a credit to Ray and Monika and all our LAC volunteers who do all this work volunteering so many, many hours of service,” Matt said.
“The void Ray and Monika leave will be difficult to fill – if ever.”
“Ray has overseen many changes here (at the Museum), improving our lighting to LED, adding carpets, changing rolling doors to window, installing air conditioners, fans, but also provided a lot of support to the Station too like providing shades in the car park.
“All this work has added value well beyond QAS’s budget – not just for our own comfort, but more importantly to improve our visitors’ experience,” Mick said.
“The work Ray did in the auditorium area of the Museum has made a huge difference and makes it so much easier for the broader Queenslander community to come and listen to our history.”
Ray is a former Wynnum Chamber of Commerce President and initially joined the LAC because he met then LAC President David Lloyd at a function, and he invited him to join.
“I said yes of course, because I was interested in what the ambulance did and thought I’d like to be able to help out,” Ray said.
“Over the years we were able to raise a lot of money for our local station and the museum and we’ve been very proud of this.”
Mick said while the LACs’ larger role has changed over time it still acts as a liaison between the QAS stations and their local communities.
“Ray’s background as a master tradesman ensured works done at the Wynnum Heritage Ambulance Station (Museum) were of the highest quality, and he was expert in dealing with tradies and repairers as well as architects and engineers.
“Monika’s experience in customer service shone brightly when helping visitors look through the ambulance heritage station or taking phone bookings to arrange a visit.
“Both spent many hours volunteering to make the Wynnum Heritage Ambulance Station a place people would want to visit and enjoy while they were there,” Mick said.

■
■
An emotional Ray Rickwood stood in front of a small gathering of people at the Queensland Ambulance Service’s Wynnum Museum for most likely his last time earlier this year.Background and inset Ray and Monika in the old treatment room at the Wynnum Museum - he says he was treated on the bed behind him in his youth. Met South Acting Commissioner Matt Green (centre) presented Ray and Monika with parting tokens of thanks for their many years of volunteering.
The Queensland Ambulance Service (QAS) develops Ambulance Management Plans (AMPs) to improve assessment and treatment for individual patients whose management either falls outside the QAS Clinical Practice Manual’s scope, or if they have special needs, Alex Thompson writes.
AMPs are developed on an exception basis and QAS Medical Director Dr Stephen Rashford approves them after consultation with the patient’s treating clinical team.
QAS’s first AMP was implemented 15 years ago, in February 2007 after a request from a major oil refinery in Brisbane to have its authorised registered nurses travel with the refinery’s patients to hospital in the ambulance, and to continue ongoing treatment with calcium gluconate gel for patients exposed to hydrofluoric acid.
As part of this package, the refinery staff were also provided with a script for calling Triple Zero (000), to advise the EMD the QAS Medical Director had pre-authorised a Code 1C immediate response, and to contact the Clinical Deployment Supervisor.
In the 15 years since this first AMP, over a thousand plans have been developed, amended, and removed as required and currently, there are more than 150 formal AMP documents in circulation.
These include plans for several specific cohorts of patients with very complex needs.
Examples include:
• patients awaiting cardiac transplants who are on Ventricular Assist Devices
• patients with pulmonary hypertension requiring continual epoprostenol infusions,
• paediatric patients with tracheostomies and/or ventilators, and
• patients with Functional Neurological Disorders who require individualised management of their presenting condition.
Our AMPs have historically prompted the development of more generalised Clinical Practice Guidelines.
For example, prior to the introduction of hydrocortisone for Advanced Care Paramedics (ACPs), the QAS had a large number of AMPs for specific children with adrenal disease.
These AMPs authorised ACPs to administer hydrocortisone in times of illness or injury.
Following many successful cases, and supported by endocrinology experts, the QAS approved wide spread use of hydrocortisone by ACPs.
Until now, the actual AMP document outlining the specific patient management was held by the patient’s family or carer and was shown to the attending paramedics on arrival.
A copy was also kept in the local Opcen with the CDS, who could relay the information to the crew as required.
A medical caution note was also added to the CAD system to notify the
EMD and the attending crew that an AMP was in place.
This caution note advised only the most important details of the plan –for example, the dispatch code, or a critical variation in drug dose.
Since early 2022 QAS clinicians registered with the Australian Health Practitioner Authority (Aphra) can access to the Queensland Health’s “The Viewer” system, after completing the requisite training.
The Viewer is a powerful tool which enables paramedics to review a patient’s history while providing clinical care, and for undertaking clinical follow-ups for the patients they provided earlier clinical care to.
Not only does The Viewer allow QAS paramedics to view information about the patient entered by Queensland Health staff, it also allows QAS to upload QAS-specific information.
All QAS internal AMP documents are now on The Viewer, allowing paramedics to review an AMP in real time on their operational iPad, even before arrival at the scene in some instances – a significant improvement to our patient care. We now have in excess of 4,000 patients with AMPs, CAD notes and other treatment recommendations listed in The Viewer.
The existence of a QAS AMP for a particular patient will be notified to attending crews via a “caution note”, in line with current practice.
After entering the patient’s name and date of birth in The Viewer app on the iPad, a “pop-up” will appear to alert there is an AMP in place, which can then be located under the “Care Plans” tab.
If a caution note is not triggered for a particular patient who has an AMP (for example, if the patient is located in a public space), The Viewer can be used to check if the patient has an AMP if the patient is identifiable once on scene – another considerable improvement on the current process. It is envisaged The Viewer will be the sole access point of AMPs for operational staff.
Having a single online source of information will greatly enhance version control and ensure our paramedics are accessing the very latest version, thereby mitigating clinical risk.
Clinical Deployment Supervisors will also have access to the AMPs via their own Viewer access.
So, if a paramedic’s iPad is out of data range or has some other technical difficultly, the paramedic can default to the current situation and contact the CDS who can relay the information.
The Clinical Hub and the QAS 24/7 Clinical Consultation and Advice Line
doctors and senior paramedics will also have access to AMPs via The Viewer, allowing advice more tailored to the patient’s specific situation.
It is important to note the QAS is only uploading QAS-generated AMPs.
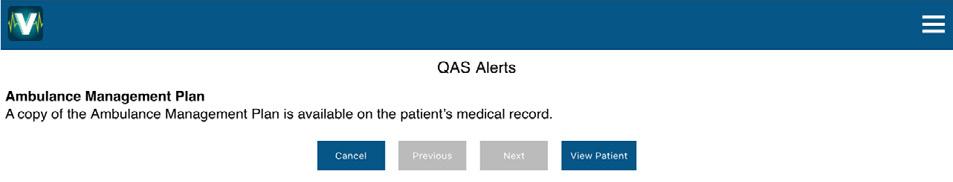
All other plans developed by other agencies, (such as Emergency Department Acute Management Plans, Mental Health Plans etc), are the responsibility of those other agencies, with their uploading onto The Viewer to continue as per their current procedures.
A limited number of other relevant documents will continue to be held in the OpCens and referred to in the caution note.
The ability to access timely and accurate information in The Viewer is an important step for QAS in our continuing integration with the wider health system.
Work is in progress for future enhancements, which will provide QAS clinicians with even more access to patient-specific information.

• Access to The Viewer is available for Ahpra registered QAS clinicians only.
• The training package can be accessed via QASLCO –Clinical Information Systems.
• Following successful completion of the package Ahpra registered QAS clinicians (excluding communications and corporate staff) will be provided access to The Viewer. This process can take up to 2 weeks after successful eROA completion. If after this time you encounter problems, please contact FSG Mobility via email.
Severe traumatic brain injury (TBI) has a poor prognosis that has not improved significantly in the last two decades despite improvements in research, prehospital and ICU care, Hayley Grant writes.
But an aggressive approach to prevention of secondary brain injury in the hyper-acute phase of injury may reduce morbidity and mortality.
Severe TBI is a High Acuity Low Occurrence (HALO) scenario for most paramedics in Queensland.
This results in the potential for suboptimal management as clinicians may not have managed a patient in this condition or reviewed the practice guidelines for some time.
Primary traumatic brain injury is the initial disruption of cerebral tissues due to external forces. These forces result in the direct compression, destruction or shearing of tissues. The primary injury is complete at the time of impact and isn’t reversible. Secondary brain injury develops in the minutes and hours following initial injury, with the damaged brain tissue commencing a neuro-electro-chemical cascade that ultimately ends in neuronal cell death. Managing or preventing the effects of this cascade is the goal of prehospital intervention (Murray & Lopez, 1997).
PROMPT is a state-wide study and includes patients suspected of suffering a severe TBI (as defined by a Glasgow Coma Score of equal to or less than 8) following head trauma and who are treated by all levels of QAS clinicians (from volunteer first responders to QAS Medical officers). This study will provide a baseline assessment of clinician compliance with international best practice recommendations, followed by a focused educational package to improve on any areas that require it. A post intervention analysis will then determine the effectiveness of the educational package. A convenience sample of all patients presenting within both study periods (pre and post educational package) will be collected. With TBI incidence data extrapolated to the state population we anticipated collecting data for between 500 and 700 patients. All data is extracted from QAS eARF software. In the first phase, retrospective patient data provided a baseline assessment of compliance with the Brain Trauma Foundation Guidelines about physiologic measures.
Hypotension: The current recommendations are to avoid hypotension (systolic blood pressure <90mmHg) and hypoxia (oxygen saturations of <90%) (Badjatia et al., 2008). Interestingly, the updated fourth edition of the general guidelines recommend a higher systolic blood pressure of 110mmHg be used as the lower limit of hypotension, with thresholds changing with age groups (Brenner et al., 2012). This is based on a large retrospective study by Berry et. al in 2012 that analysed 15733 patients with isolated moderate to severe TBI. They concluded that patients should be considered hypotensive if their systolic blood pressure is <110 mmHg at any point. Further research should confirm this new definition of hypotension, however 90mmHg is still the recommendation for prehospital providers.
Hypoxia: A relationship between reduced brain tissue oxygenation and poor outcome following severe traumatic brain injury has been reported in observational studies (Manley, 2001) yet a report by Stahel et al., 2007 found hypoxia to be less devastating than hypotension. The current Brain Trauma Foundation guidelines advocate that oxygenation must be monitored continuously and that hypoxaemia should be avoided (defined by a PaO2< 60 mmHg). For obvious ethical reasons, no prospective randomised controlled clinical trials have been, or probably ever will be, conducted to compare the effect of hypoxia and hypotension on the outcome after TBI. Advancements in the recognition and treatment of TBI are focussing on improved monitoring of the head injured patient’s oxygen levels beyond oxygen saturations. The Brain Tissue Oxygen Monitoring and Management in Severe Traumatic Brain Injury trial (BOOST-III) has demonstrated a significant reduction in hypoxia during hospitalisation in the targeted treatment group. The BOOST-III trial aims to evaluate the clinical efficacy of a treatment protocol based on brain tissue oxygenation (PbtO2) monitoring compared to treatment based on intracranial pressure (ICP) monitoring alone (Okonkwo et al., 2017). Whilst PbtO2 and ICP monitoring isn’t currently relevant to prehospital management, the outcome of the trial may help clarify the importance of avoiding hypoxia in the head injured patient.
Co2: In the setting of acute brainstem herniation following TBI, the use of hyperventilation to reduce intracranial pressure may be life-saving (Badjatia et al., 2008). However, undue use of hyperventilation is thought to increase the incidence of secondary brain injury through direct reduction of cerebral blood flow. A retrospective study of 65 patients following severe TBI found that any attempt at hyper or hypoventilation during prehospital care resulted in an increase in the in-hospital mortality (Dumont et al., 2010). The authors suggested that implementation of universal normoventilation of patients with TBI is the optimal prehospital management until an initial evaluation by neurosurgery can be carried out.
Airway management: An airway should be established in the most appropriate manner available to ensure adequate airway maintenance and prevent hypoxaemia. If endotracheal intubation is used, then in-line end tidal carbon dioxide monitoring should be used to confirm tube placement and guide a ventilation strategy that ensures ETCO2 is maintained between 35-40mmHg.
Education: The Brain Trauma Foundation guidelines emphasise prevention and treatment of hypoxia, hypotension, and hyperventilation. These recommendations are based on observational studies demonstrating increased TBI mortality from these insults. However, the supporting evidence remains weak, as there are only a few studies available that review the impact of prehospital guidelines and educational programs on patient outcome.
Phase one data was collected between 1 January 2020 and 31 December 2021. Initial capture was 917 patients meeting criteria, which was cleaned to a final patient group of 304. The gender breakdown was 206 males to 98 females, which is consistent with the higher male representation of TBI in the literature. Ages ranged from 18 to 101, with a mean age of 45. The breakdown of presenting regions across the state is presented in Figure 1.

The clinical parameters we measured were systolic blood pressure, oxygen saturations, blood glucose level, temperature, and airway management e.g. ETT, LMA, OPA, NPA. The first and last set of vital signs were measured to demonstrate trends in patient management. All call cycle times were recorded as per eARF.
Overall, management of critical physiological parameters such as hypoxia and hypotension were managed consistently well state-wide. The majority of patients had SPO2 measured, and of the 31 hypoxic patients only 7 remained hypoxic following intervention. Despite glucose being critical to brain function, only 120 patients had an initial BGL recorded, with 12 having results outside normal. The data indicted only 3 patients received additional BGL checks despite abnormal initial reading. Only 125 of 304 patients had a temperature recorded at initial presentation with none being recorded have having further assessment following treatment. Figure 2 shows the clinical parameters recorded at initial presentation and Figure 3 shows the final set of clinical parameters recorded.
The regions where HARU operate are also the largest regions by population and therefore had the highest number of patient presentations, and the highest cohort of intubated patients. We did not request pharmacological data, so have no way of ascertaining which patients received RSI – this was intentional, as this study examines the overall management of severe TBI. Figure 4 describes the use of airway adjuncts across the state.

Figure 1: Incidence by region (represented as LASN due to data collection period)
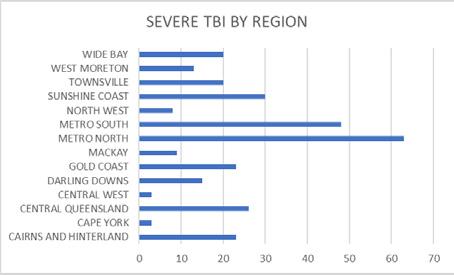 Figure 2: Clinical parameters at presentation
Figure 2: Clinical parameters at presentation
Badjatia, N., Carney, N., Crocco, T., Fallat, M., Hennes, H., & Jagoda, A. et al. (2008). Guidelines for Prehospital Management of Traumatic Brain Injury 2nd Edition. Prehospital Emergency Care, 12 (Supplement 1), S1S52. https://doi.org/10.1080/10903120701732052
Brenner, M., Stein, D., Hu, P., Aarabi, B., Sheth, K., & Scalea, T. (2012). Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. The Journal Of Trauma And Acute Care Surgery, 72(5), 1135-1139. https://doi.org/10.1097/ta.0b013e31824af90b
Severe traumatic brain injury is a low occurrence event, but the early management is critical in preventing the secondary injury. Careful monitoring and correction of hypoxia and hypotension can reduce the morbidity that occurs following TBI. Relatively few patients presenting with severe TBI were found to have clinical parameters outside the recommended range and these were management appropriately on most occasions by paramedics. Areas of potential improvement include improved monitoring of BGL and temperature.

Less than 40% of patients across the state had an airway adjunct used in their management despite hypoxia remaining present amongst some patients. There are several factors that may preclude the use of an airway adjunct and the use of manual techniques to maintain patency may be an appropriate course of action.

The data used in this study was retrospective and relied on input by treating clinicians which may not always occur. Reassessment of BGL and temperature may have occurred and not entered into the patient record.
Despite severe TBI being a confronting patient cohort, the prehospital management of it is inherently simple. Whilst high-quality data may be lacking, large retrospective studies suggests that without prompt, aggressive treatment, patients are more likely to suffer the potentially devastating consequences of secondary brain injury. Any deviation from homeostasis remains easily recognisable and treatable in the prehospital setting, reducing avoidable secondary insults which are associated with worse outcome after TBI. Strict adherence to national and international guidelines by all levels of practitioner may be associated with improved outcome. Free, online access education may be the key to ensuring prehospital providers remain up to date in the appropriate management of these devastating injuries.

Manley, G. (2001). Hypotension, Hypoxia, and Head Injury. Archives Of Surgery, 136(10), 1118. https://doi.org/10.1001/archsurg.136.10.1118
Murray, C., & Lopez, A. (1997). Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. The Lancet, 349(9064), 1498-1504. https://doi.org/10.1016/s0140-6736(96)07492-2
Okonkwo, D., Shutter, L., Moore, C., Temkin, N., Puccio, A., & Madden, C. et al. (2017). Brain Oxygen Optimization in Severe Traumatic Brain Injury Phase-II. Critical Care Medicine, 45(11), 1907-1914. https://doi.org/10.1097/ccm.0000000000002619
Figure 3: Clinical parameters after QAS management Figure 4: Airway adjunct usage amongst severe TBI patients


Upon examination, the patient was GCS 15, interacting verbally, tachypnoeic with a respiratory rate of 35/min and a SpO2 of 88% on room air. His chest wall was bilaterally tender to palpation, demonstrating splinting with subtle right sided hyperinflation, shallow breathing but with no subcutaneous emphysema present. The patient had multiple superficial horizontal lacerations to the posterior triangle of his neck bilaterally with no active haemorrhage. A 3cm laceration superior to the sternal notch in the midline had an active slow ooze, however nil clinical evidence of aerodigestive injury. Dressings and soft collar were applied to his neck. A weak radial pulse was present and the patient was cool peripherally. The patient was hypotensive, with a blood pressure of 74/35mmHg and tachycardic with a heart rate of 120bpm. His abdomen was soft to palpation, non-distended but with generalised tenderness. Upon gentle palpation of his pelvis whilst simultaneously applying a pelvic binder he complained of significant pain globally.
His left distal leg had an open, angulated fracture and his left forearm also was deformed. The patient was log-rolled to 15 degrees to facilitate extrication off the ground to the stretcher, with no obvious injuries to

his back being identified. Verbally, the patient advised the team that he could not feel or move his lower limbs.
The patient was given aliquots of 25mcg IV fentanyl for analgesia, transfused 1 unit of fresh frozen plasma (FFP) and 1 unit of packed red blood cells (PRBC) to improve haemodynamics.
A rapid sequence induction/intubation (RSI) was performed with 50mg ketamine and 100mg rocuronium IV. It was an uncomplicated intubation and the patient had simultaneous bilateral finger thoracostomies to decompress the chest. En route to the major trauma service he had his left ankle splinted, a Focussed Abdominal Sonography in Trauma (FAST) was scanned which was negative for intraabdominal haemorrhage, and his point of care International Normalised Ratio (INR) was completed. The INR was 1.3, which indicated significant early coagulopathy. He was given 2g fibrinogen concentrate to attempt to correct the early coagulopathy, 1 further unit of PRBC, 1g Tranexamic Acid and 4.4mmol Calcium IV. Small aliquots of metaraminol, a synthetic alpha receptor agonist were administered for the persisting hypotension given the concerns for spinal injury and neurogenic shock.
At hospital a “Trauma Respond” team had been assembled, and his arrival observations were a blood pressure of 112/86mmHg, heart rate 140bpm, SpO2 86% on 100% FiO2. Repeat FAST scan was negative, he had bilateral intercostal catheters inserted to prevent reaccumulation of potential underlying pneumothoraces through the finger thoracostomy sites and he was sent for a CT scan to further delineate his injury profile. In the CT he had recurrence of haemodynamic instability and further Fibrinogen
An ACP crew, CCP and HARU team were dispatched to an alert and breathing 34-year-old male following a presumed fall of a significant height from the 7th floor. The ACP crew arrived first, noted the patient was alert and conversive but with obvious head, chest, neck and orthopaedic injuries. The ACPs had attached patient care monitoring and were establishing peripheral IV access and commencing 250mL IV 0.9% sodium chloride upon the CCP and HARU team arrival.and 4 units of PRBC were administered. The patient was then to the operating theatre for laparotomy and pelvic packing.
His injuries included multiple bilateral rib fractures, including a flail segment on the right side, bilateral pneumothoraces (right > left), small volume pneumomediastinum, large bowel haematoma, femoral head fracture, two lumbar spine transverse process fractures, C7 spinous process fracture, open left distal tibia + fibula fracture, right calcaneal fracture, left radius/ ulna/ scaphoid fractures, and multiple complex, comminuted, displaced pelvic fractures with associated retroperitoneal haematoma.
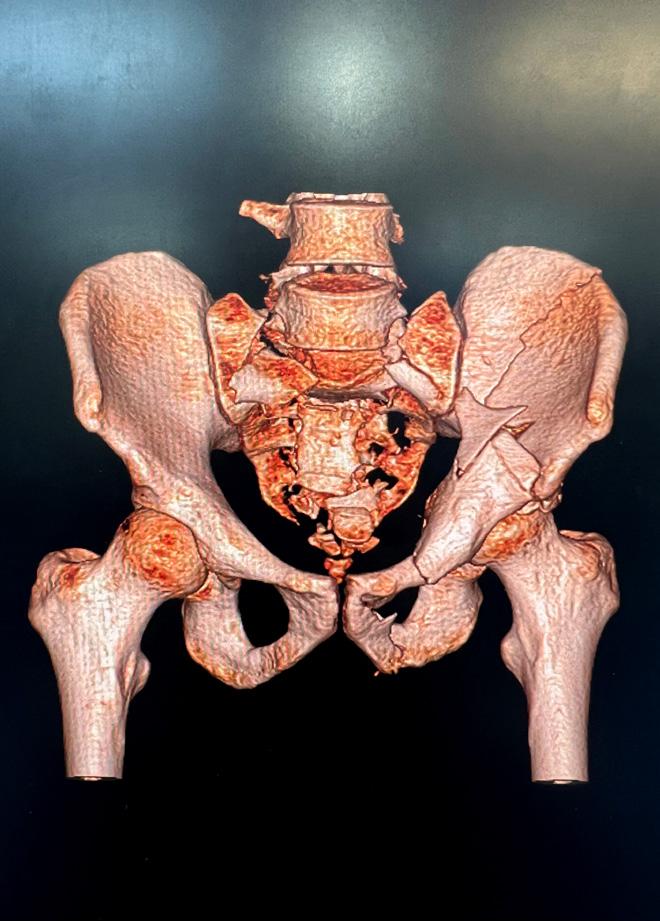
The patient was admitted to the Intensive Care Unit post operatively and underwent a total of seven operations during his stay, including spinopelvic fixation, staged orthopaedic repairs of his wrist and bilateral distal lower limb fractures, and rib fixation surgery. The patient has since been discharged from the ICU and admitted to the Spinal Injury Unit for rehabilitation, due to the finding of reduced use of his lower limbs secondary to the extent of his lumbosacral fractures.
1. The trauma care journey begins with excellence in prehospital assessment and care.
2. It is important to ensure comprehensive documentation of
the patient’s presenting status, especially an accurate neurological assessment.
3. The QAS provides a multi-tiered approach to trauma care, with each clinician providing an important contribution to treatment.
4. Identification and treatment of early coagulopathy in the prehospital environment is becoming increasingly important, with the QAS undertaking both novel research and providing state of the art care.
5. Recovery from a major trauma may take 18 to 24 months. Attention to ensuring first class basic and advanced prehospital care may be a critical difference for the standard of recovery that occurs.
The Medical Directors office has recently set up a LARU Community of Practice Team on MS Teams to achieve improved flow of information and have clinical discussions related to complex patient presentations relevant to LARU paramedics.


This team is designed to the support professional standards and care
provided by LARU paramedics across the state and is run by clinical LARU staff.
This team will be holding professional development meetings which will be open to all LARU paramedics and will explore complex clinical reasoning and differential diagnostic skills in the out of hospital environment.
For more information, please contact Alex Thompson alex.thompson@ ambulance.qld.gov.au
The Graduate Certificate team have recently had 10 eligible LARU officers working through the EARWOU004 Wounds unit to complete their foundation LARU course. These officers recently completed the workshop and are now credentialled to use their skills on-road.
■
Back, from left to right ■ Liz Brooks, Warren Smith, Anthony Downes, Colin Oxlade, David Krygger, Naomi Knight, Tina Sattler, Blake Rhodes Front, from left to right Kerrie Fissenden, Nicole Beesley, Nancy Brown, Hope Carson, Teresa Smith









We’ve all been there; called by a nurse to a Residential Aged Care Facility (RACF) to see an elderly, demented, significantly co-morbid and immobile patient who has had a recent change in their behaviour.
Our first instincts too often assume that the patient is too complex. Too difficult to assess, lacks the local resources for care and is simply just easier to pat slide to your stretcher for transport to the nearest Emergency Department.
But what if, with a small amount of lateral thinking, team building and supported decision making, we could keep this patient within the RACF for care? This can happen and the below case in an example of the importance of critical thinking and care planning in the setting of complex geriatric patients.
Case: Dispatch code 2C to 92yom in RACF has been refusing to eat -1/7.
PMHx: MI, COPD, Mixed type dementia (non-verbal), immobility, prostate CA, AF.
MEDn: Heaps!
Allergies: Penicillin
Normal functioning state: Bed bound, immobile, non-verbal, high care patient
RN called because the patient has been refusing to eat for the past -1/7 since discharge from ED where he was dx with an active COVID-19 infection. He has had no food or fluid intake since yesterday. No physician review has been conducted within the RACF prior to calling QAS.
Nursing staff on scene stated the patient has not been eating since returning from hospital yesterday but is otherwise presented normally. His vitals were unremarkable, and the 12-Lead ECG was his expected controlled AF. A detailed and thorough respiratory, gastrointestinal and cardiovascular examination did not find anything unusual or unexpected (normal poor tidal volume due to COPD noted), but the patient did not appear in any respiratory distress or behaving abnormally. He has not opened his bowels today but had a small motion yesterday.
General poor or reduced appetite is not unusual in geriatric patients but acute decline in appetite may be a symptom of a concerning diagnosis. Causes can include changes in “physiological or psychological health; social circumstances and acute or chronic
disease” (Pilgrim et al, 2015 pg 30).
Furthermore, acutely reduced appetite can be a sign the patient is starting the dying process and may be in the final stages of his life (nhsinform website).
Either way, nursing staff were correct to recognise the red flag symptom early and seek help.
In the setting of normal vitals and unremarkable physical examinations, it becomes a challenge to differentiate the cause.
The most common cause of acutely reduced appetite in geriatric patients is constipation which effects more than half of RACF patients (Pilgrim et al, 2015 pg 30). Due to geriatric “anatomical and nervous system changes in the colon, sphincter and rectum” (Lucak et al, 2021), constipation should be ruled in/out.
Investigations include blood pathology - metabolic profile, thyroid function, anaemia, CBC; and medical imaging –x-ray and/or CT (Lucak et al, 2021).
These tests can also aid in diagnosis of other bowel disorders including obstruction, lesions, inflammatory diseases, and mesenteric ischaemia;
but pain is commonly present in these conditions.
Either way, these required investigations are not immediately available onsite at the RACF staff or even a general practitioners office.
A significantly co-morbid elderly patient with an active COVID-19 infection who has stopped eating a day ago with a differential diagnosis (possible) of acute constipation, COVID-19 complications or end of life symptomology.
What does this patient need? Acutely he needs blood work, medical imaging and rehydration. Results to which will guide further management.
This patient has not documented any end of life or advanced health care directives and the power of attorney (son) has in the past requested full care. So, what do we do? Transport to ED potentially.
But is this the correct option for this patient, or even for the system at whole? What can be done to bring care to the patient?
A transport which will trigger complex and expensive isolation requirements due to the active COVID-19 infection; not to mention perhaps not being in the best interest holistically for this individual.
When considering these issues, it is important remember geriatric patients rarely exist without any supporting medical teams.
This is especially true of patients within an RACF as many RACFs in SE QLD have access to expert in-call specialist services offered by a local hospital. In the case of the Gold Coast the Residential aged-care Support Service (RaSS) which is run by the Geriatric Emergency Department Intervention team (GEDI – cool name) offer a service overseen by consultant geriatric physicians and senior RNs.
But before exploring this option we should determine the son’s expectations for care, including discussing what options of care exist.
Does he want the patient admitted to ED, or would he be happy for us to explore locally available support?
The son indicated to me over the phone that his preference is to keep him in the RACF if care can be provided, I informed him that I can explore those options and liaise back to him.
While I spoke with the RaSS Consultant the RACF RN called the patient’s GP.
Through a four-way phone conversation, LARU Paramedic/GP/Nurse/RaSS
Geriatrician we collectively agreed the services this patient needs for diagnostics could be provided within the nursing home, including a portable x-ray.

This would be provided by a RaSS RN attending the RACF the following morning.
SUBCUT fluids were charted for this evening as was a COVID-19 anti viral medication.
We re-contacted the son and informed him initial care could be provided within the RACF, but if his father deteriorates, he may need an in-patient admission. The son remained happy and very thankful.
The RaSS Geriatrician also undertook to discuss advanced health care directives with the son at the earliest opportunity. On reflection, it is possible that this patient’s condition may worsen in the coming days.
But it is possible this would occur irrespective of whether he remained in the RACF or was transported to ED.
In this case the services of the ED were rallied in support of the patient, the RACF and the wider healthcare system.
Ultimately a patient-centred approach to his complaint facilitated high quality and multi-disciplinary out of hospital care.
Clinical reasoning does not only encompass how to treat and transport a patient to ED, but also to explore what options may be available locally
and how to best advocate for your patient’s healthcare journey.
A patient-centred approach and appropriate clinical reasoning could be the difference between pre-hospital versus out-of-hospital thinking.
Ratnaike, R. N., & ProQuest Ebooks. (1999;2009;). In Ratnaike R. N. (Ed.), Diarrhoea and constipation in geriatric practice. Cambridge University Press. https://doi.org/10.1017/ CBO9780511545818
Pilgrim, A. L., Robinson, S. M., Sayer, A. A., & Roberts, H. C. (2015). An overview of appetite decline in older people. Nursing Older People, 27(5), 29-35. https://doi.org/10.7748/nop.27.5.29.e697
NHSInform – Body Changes at the End of Life – https://bit.ly/3C291SL
Lucak, S., Lunsford, T. N., & Harris, L. A. (2021). Evaluation and treatment of constipation in the geriatric population. Clinics in Geriatric Medicine, 37(1), 85-102. https://doi.org/10.1016/j. cger.2020.08.007
Each year International Academy of Emergency Dispatch (IAED) recognises Australasian individuals who have made the most significant contributions to further the values and missions of the Academies through personal action. Jo Roy writes.
The IAED Dispatcher of the Year award is the highest honour an accredited EMD can be awarded.
Nominees of this prestigious award must consistently demonstrate the following qualities:
• compliance with Medical Priority Dispatch System (MPDS) protocols
• a commitment to teamwork
• initiative to further professionalism and education
• the ability to function well under highly stressful situations.
The award is issued each year at the Australasian Navigator Conference, and this year, it was held in November in Melbourne.
Queensland Ambulance Service had one nominee for the highly coveted award – Rockhampton EMD Sasha Dobbs.
Sasha commenced her career with the Queensland Ambulance Service (QAS) in February 2022, taking up a position at the Rockhampton Operations Centre (OpCen).
Despite being in the service for only nine months, Sasha has been an enthusiastic and diligent staff member with a focus of excellence in the delivery of patient care.
A recently qualified Paramedic, Sasha displays excellent situational awareness and provides enhancing actions/ reasons statements to provide strategies to aid the caller in caring for the injured or sick patient.
Sasha seems to attract high priority incidents. This includes 10 response priority 1A incidents in her first 16 shifts; four of these incidents requiring CPR with two resulting in ROSC when the responding crews arrived on scene.
Sasha received high praise from Paramedics for her quick recognition and delivery of effective Pre-Arrival Instructions. She displays a real passion for our patients and is a quiet achiever who is always ready to assist others without any fanfare or need for recognition.
Sasha has become a valued member of the team and the Rockhampton Operations Centre.
We look forward to seeing what comes next as she continues her career with the QAS.
Above
■ Rockhampton OpCen’s Sasha Dobbs.
Insight’s OpCen Report highlights examples of outstanding responses to Triple Zero (000) calls by our dedicated staff at Operations Centres around the state. Jo Roy writes.
Toowoomba CairnsWhen Toowoomba ECH, Abbie Batzlof received a call from a woman who had fallen and hurt her back, she knew something just wasn’t right.
“I’ve had had an argument with my partner and I’ve taken a fall with my back,” the caller stated.
The caller then said something strange: “I have a comma on the inside of my wrist if you understand what that means.”
Abbie was aware of the semicolon used as a message of affirmation and solidarity against suicide, depression, addiction, and other mental health issues, but she had not heard about a “comma” on the inside of the wrist before.
The caller’s insistence that she had the “comma”, and that the paramedics needed to be advised of the comma convinced Abbie there was more to this picture.
Click here to hear a sample of the call.
Managing Triple Zero (000) calls is so much more than asking a series of scripted questions. Our emergency call takers use a variety of skills, knowledge, experience, instruction and instinct to ensure our patients get the help they need. Abbie expertly used her intuition, verbal queues from the caller and conversations heard in the background to ensure an appropriate response to this patient who was later confirmed as having experienced domestic violence.
Cairns ECH Laura Long quickly recognised the signs of agonal breathing and was able to get “hands on chest” for a 60-year-old male who went into arrest approximately 16 minutes into a call.
Initially called in as a conscious patient who had collapsed, the patient continued to deteriorate throughout the call.
The caller in this instance was the patient’s very concerned wife.
They were home alone and knew they were “about 15 minutes” from the closest ambulance station.
Understandably the caller was very worried about her husband, but the information she provided required further clarification.
Wherever doubt existed, Laura ensured she confirmed the information using clarifying questions.
Whilst the first unit was assigned in less 2 minutes and responded in less than 90 seconds the patient’s location meant a code one response time of almost 20 minutes.
As the responding units were on route Laura correctly identified ineffective/agonal breathing and immediately commenced CPR pre arrival instructions (PAIs) which continued until the first crew on scene could take over.
The first crew arrived on scene approximately eight minutes later and after administering one shock the crew advised the OpCen they had ROSC.
Click here to hear a sample of the call.
Laura ensured the patient was constantly monitored and was about to commence another breathing diagnostic test when the caller stated he was no longer responsive, and he could “Hardly breathe. It’s all nasally or something? He’s taking deep breaths like a fish through his mouth”. At this point recognising the caller’s description of agonal breathing Laura was able to get hands on chest quicker than if she had proceeded with the breathing diagnostic tool.
How many seconds she saved, we cannot be sure but what we can be sure of is that every second counts.
The Clinical Hub performs an active role in QAS patient encounters in various and diverse ways. Stationed within the Clinical Hub are paramedics with specialist training, an Emergency Medicine Dispatcher and Operations Centre Medical Officers including Emergency Medicine Consultants and the HARU Fellows.
The Clinical Hub role includes:
1. Performing call backs to pending cases with the goal of providing clinical advice to the patient and their family.
2. Supporting patients through the discussion and exploration of alternate pathways for care.
3. Supporting paramedics via phone and video conferencing with advice and support for direct patient care.
4. Providing advice and support via the COVID referral line to paramedics on road.
5. Secondary triage of pending jobs that may need to be up-graded or down-graded depending on further clinical information obtained through clinical history in case notes or on call back to the scene.

The selection of cases below highlights the different abilities within the Clinical Hub and when they can be of assistance.
Medical officer call back to a pending 2A case
Patient: a 75-year-old male patient who’d had a fall from an office chair.
When family arrived home the patient was still on the floor with a sore neck, back and shoulders with weakness in the arms most notably the hands. He was moved to his bed by family. On discussion with the patient and their family the weakness was only in his arms, sensation was preserved, he was suffering from an intense pain over his upper back and shoulders down his arms. The presentation was concerning for central cord syndrome which was relayed to the treating paramedics via the MDT. The case was upgraded, and the patient was transported to hospital with analgesia, spinal precautions, and monitoring with the paramedic team. A diagnosis of central cord syndrome was confirmed on MRI and the patient is currently recovering in hospital.
The varied examples below demonstrate the interventions from the Clinical Hub are beneficial for both patients and paramedics.
When working on road the Clinical Hub is contactable via the QAS consult line by selecting option 3. Please contact us if you think we may be able to help with alternate pathways for care.
Paramedic
Patient: A 46-year-old male patient with vertigo which was a persistent problem for the patient, who had run out of medication prescribed by his General Practitioner who had previously assessed his vertigo.
A Clinical Hub Paramedic performed a call back and telephone risk assessment and concluded there were no new findings or symptoms. The patient was able to mobilise without assistance; there were no red flags or high-risk symptoms of stroke or other sinister pathology. He was not able to access his usual GP so the patient consented to referral to Mater @ Home Direct via the Clinical Hub. Mater @ Home Direct completed a telehealth appointment with a medical practitioner. Prochlorperazine was delivered to the patient’s home and a physiotherapist attended for a home visit within 2.5 hours of referral to complete a vestibular assessment and maneuvers. The case was placed in a holding pattern while the process was undertaken to inform the Emergency Dispatchers that a referral process was underway and not for dispatch currently. The clinical hub was able to facilitate an alternate pathway that met the medical needs of the patient and supported this care occurring in the community.

Incoming call: Paramedic with COVID patient in remote location of far Northern QLD
A paramedic called the Clinical Hub requesting decision support for a high-risk patient declining transport to hospital despite paramedic assessment and recommendations.
The patient was a 34-year-old female with a COVID positive Rapid Antigen Test (RAT). There was no phone reception due to remoteness, but she could make calls using WiFi. Our paramedic had assessed the patient but had to leave the scene to get phone reception.
The Clinical Case was presented to Clinical Hub Practitioner via COVID referral line:
Identified High Risk COVID patient due to risk factors including unvaccinated status and asthma compounded by remoteness. Symptoms included headaches, malaise, fevers and chest pain. Assessment- 34-year-old female. Symptomatic for 4 days. Positive RAT 1 day ago. Afebrile. SBP 123/82, HR 80, RR 14, chest clear, SpO2 99% no desaturation or increased work of breathing when completing the 40-step test. Able to maintain nutrition and self-care. Living at home with family.
The Clinical Hub was able to help mitigate any risk by linking in with the Cairns and Hinterland HHS who accepted the referral to their COVID virtual ward. The paramedic drove back to inform the patient of the COVID virtual ward admission. The COVID virtual ward contacted the patient daily over WiFi and performed a telehealth clinical assessment. Feedback from the COVID virtual ward confirmed the referral system worked well, the patient benefitted from the daily review and was able to be cared for at home for the duration of their infection.

Paramedic clinical call back to a pending code 2A with scene support
Patient: A 50-year-old male with over 18 hours of chest discomfort while out at sea on a prawn trawler. He’d been attempting to make his way back to Port Douglas, but inclement weather was setting in and his pain was increasing.
Call back to scene from Clinical Hub Paramedic: the patient’s central chest pain was worsening throughout the day and with exertion. He had no previous cardiac history but was overweight and was a smoker. He was also intermittently feeling dizzy, with shortness of breath and was in a hurry to pack up his trawler and return to land. His partner was on the boat too but did not speak much English and couldn’t drive it. Our advice was to limit exertion and self-administer analgesia, including paracetamol and aspirin which he had on board while awaiting paramedic arrival.
The case was upgraded to a 1C and poor weather meant the meet up was challenging. Clinical Hub staff liaised with the local OCS to organise Volunteer Marine Rescue (VMR) to transport a paramedic crew to the trawler. OCS had liaised with Retrieval Services Queensland (RSQ), but no local aeromedical assets were available.
The Clinical Hub Paramedic remained in regular contact with the patient while waiting for the VMR and paramedics. Our paramedics assessed him and brought him back to the mainland. His ECG did not show any signs of ischaemia and he was safely transported to hospital. VMR assisted with the ongoing management of the trawler.
These documents aim to provide guidance for employees looking to affirm their gender in the workplace and managers looking to support their employees through this process.
Queensland Health Gender Affirmation Guideline’s vision and plan is:
“Every employee has the right to safe, inclusive and supportive workplace free from discrimination, bullying and harassment – one that promotes respect, equity and a place where all employees know “It’s okay for you to be you””

Gender Identity, in addition to sexuality, is protected under both State legislation (QLD Anti-Discrimination Act 19911) and Commonwealth legislation (Sex Discrimination Act 19842). Workplaces therefore must ensure employees with diverse gender identities are provided with a workplace environment that is free of discrimination, bullying and harassment.
The Queensland Public Service Commission LGBTIQ+ Action Plan 2018-20223 clearly outlines the need for workplaces to be inclusive and supportive of transgender, gender diverse and non-binary employees through the supportive workplace cultures and Inclusive policy and practice levers.
“Developing guidelines or policies to support gender diverse employees through transition in the workplace”
Gender affirmation means transgender, gender diverse and non-binary people can thrive as their authentic selves.
The process is unique to the individual employee but usually involves one or more of the pictured processes. There is no right way to affirm one’s gender.
Under the Queensland Health Gender Affirmation Guideline the employer should help facilitate name and pronoun changes, ensure access to facilities (bathrooms and
The Queensland Health Gender Affirmation Guideline and accompanying plan were released on Transgender Day of Visibility (31 March) this year after significant community and workforce consultation and collaboration.The Queensland Health Gender Affirmation Guideline outlines the responsibilities of an employee’s manager and/or case manager during the process of gender affirmation. An employee’s manager may also be their case manager however an external case manager can be appointed (for example a HR representative or LGBTIQ+ network member). The responsibilities broadly are;
•
•
•
•
•
•
•


The QAS has a proud history of supporting our LGBTIQ+ workforce and community and is committed to building an inclusive workplace where all employees feel safe, valued and supported.
Being able to come to work each day and be your authentic self, is not always a given. For our LGBTIQ+ workforce this means being out and not having to hide who they are from their families, friends and colleagues, which isn’t always the case.
August
Wear It Purple Day was launched in 2010 in response to global stories of young people taking their own lives following bullying and harassment resulting from the lack of acceptance of their sexuality or gender identity.
This year’s theme “Still Me, Still Human” aimed to reinforce that behind the labels, politics, new stories, and data that the LGBTIQ+ community includes your neighbours, friends and our young people.

The theme seeks to remind us that behind every story there is a human being who is worthy of love, respect and acceptance, and that our differences can unite us instead of dividing us.
The QAS invited staff to send through photos of themselves and their colleagues holding Wear it Purple signs in their work setting as a visible sign of support for the LGBTIQ+ community.




























 and September were bumper months for the QAS LGBTIQ+ community with two days of significance celebrated by the organisation including Wear it Purple Day and Brisbane Pride.
and September were bumper months for the QAS LGBTIQ+ community with two days of significance celebrated by the organisation including Wear it Purple Day and Brisbane Pride.

The QAS participated in the Brisbane Pride March and Fair Day on 24 September, and all levels of staff showed their support for the march from Orleigh Park to Musgrave Park in West End.








The QAS contingent was joined by Assistant Commissioner Gold Coast Region Andrew Hebbron and the Bicycle Response Team.
Participation at Brisbane Pride is a fantastic occasion for staff to celebrate their professional and personal identities and be proud of their whole selves.
It also serves as an opportunity for the QAS to help improve the health and wellbeing for all LGBTIQ+ people by showing our visible support for the community.

Annually the LGBTIQ+ PSO Network have a workshop, followed by attendance the following day at the Pride March and Fair.
This year the LGBTIQ+ PSO Network enjoyed a day focussed on addressing challenges, acknowledging achievements, and planning for the coming year.

Future activities based on education, improving visibility and accessibility of the PSOs in the LGBTIQ+ Network and establishing broader networks with various community groups are part of the exciting direction planned for this PSO Network in 2023.
It was an absolute pleasure to welcome PFlag+ President Jane Hopkins to speak with the network at the workshop. Jane spoke about PFlag+ work supporting parents of children who identify as LGBTIQ+, as well as ways the PSOs can access
assistance and support for QAS staff from PFlag+, and a number of other community organisations. We greatly appreciate Jane’s time in speaking with the group and the valuable work being undertaken by PFlag+.







Compassion fatigue in its simplest definition is the “cost of caring” (emotional costs, psychological costs, and physical costs). Also referred to as Secondary Traumatic Stress, compassion fatigue develops when clinicians re-experience the trauma their patients have experienced. Symptoms of compassion fatigue include decreased compassion for patients, feelings of hopelessness, increased stress and anxiety, difficulties with sleep, and decreased ability to experience pleasure. If you currently experience these symptoms, please discuss this with your Priority One Regional Counsellor or check in with one of our highly dedicated external counsellors for support.
In comparison, burnout tends to be driven by organisational factors which leads to long term exhaustion and a diminished interest in workplace activities.
It is considered there are generally six areas of work life which contribute to experiences of burnout. These are:
• Workload
• Control
• Rewards
• Community
• Fairness, and
• Values.
If these areas are improved the experiences of burnout amongst employees will be reduced.
A less known concept is that of Compassion Satisfaction however, from what I have seen within the QAS, it is very prevalent. The term Compassion Satisfaction describes the positive experiences associated with the work employees perform.
Take a moment to reflect on these questions:
• I find that I learn new things from those I care for
• I have good peer support when I need to work through a highly stressful experience
• Working with those I help brings me a great deal of satisfaction
• Some people I help are particularly enjoyable to work with
• I like my work as a helper
If you can endorse one or more of these items, you are indicating compassion satisfaction. This factor is what keeps us going when our levels of compassion fatigue and burnout are high. Manager support is a key contributor with high levels of manager support leading to higher levels of compassion satisfaction.
Clark, P., Holden, C., Russell, M., & Downs, H. (2022). The impostor phenomenon in mental health professionals: relationships among compassion fatigue, burnout, and compassion satisfaction. Contemporary Family Therapy, 44(2), 185-197.
Hunsaker, S., Chen, H. C., Maughan, D., & Heaston, S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of nursing scholarship, 47(2), 186-194.
Pérez-Chacón, M., Chacón, A., Borda-Mas, M., & Avargues-Navarro, M. L. (2021). Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. International Journal of Environmental Research and Public Health, 18(2), 611.

Ray, S. L., Wong, C., White, D., & Heaslip, K. (2013). Compassion satisfaction, compassion fatigue, work life conditions, and burnout among frontline mental health care professionals. Traumatology, 19(4), 255-267.
Sprang, G., Clark, J. J., & Whitt-Woosley, A. (2007). Compassion fatigue, compassion satisfaction, and burnout: Factors impacting a professional’s quality of life. Journal of loss and trauma, 12(3), 259-280.
During my time as Regional Staff Counsellor, I have had staff refer to feelings of compassion fatigue or burnout. Often these concepts have been used interchangeably to describe the experience of exhaustion or an increase of cynicism related to the workplace, however, there are specific differences between compassion fatigue and burnout.Above
Use the resources available on the portal to support you to manage stress within the workplace. Take the time to notice which strategies work for you and implement these in your daily life.
Do more of the things you love. Find a hobby, if you don’t have one, ask others in your workgroup what they do outside of work. Try a new class and you may stumble across a talent you didn’t realise you had.
Finding just one thing you like about the most challenging clients can made it much easier to work with them and provide a positive experience.
Change your view regarding Imposter Syndrome
Pass it forward
Keep up to date with your knowledge and skills in your field. Those who felt confident regarding the work they did were more likely to experience Compassion Satisfaction.
Imposter Syndrome can be a positive and protective characteristic as you are more likely to improve your knowledge and skills to provide better services to the patients you see.
When staff are not provided positive feedback regarding the work they perform, it can be harder for them to experience compassion satisfaction. Where possible, pass on praise and acknowledgement to those behind the scenes in the contributions they made to ensuring the job runs smoothly.
Take time to reflect
Recall or record the good times
Take a moment and think of a time where you felt really satisfied at work. What happened, who was around you, where were you in your progress within the organisation? What inspired you to work in this field, what are the things important to you?
Write down or record the jobs that gave you the most amount of satisfaction. Review these regularly or reflect with colleagues about some of the positive experiences and positive challenges you have faced in your roll.
Where do I find help?
24-hour telephone counselling 1800 805 980
QAS Priority One Director 0419 707 397
QAS Staff Counsellors 0408 191 215 or 0417 079 679 or 0409 056 983
QAS Priority One State Office 3635 3333
LGBTIQ+ support service 3830 5888
Chaplaincy service 0439 788 485 or Office 3835 9923
Local Priority One Peer Support Officers or Counsellors See list in each QAS Station or on QASPortal

The Health Contact Centre went live with the Nurse Triage service in 2006 and registered nurses have been providing health assessment and information to Queenslanders every day since then.
The Triage nursing team receives around 1,200 calls every day and call volumes are typically higher in the evenings and on weekends when GP clinics are closed.
With more than 75 per cent of callers to 13 HEALTH being recommended to self-care or to visit their GP, the Triage service plays a vital role in keeping emergency departments for emergencies, and Queenslanders out of waiting rooms.
Triage team member Jackson Jones (pictured) took this milestone call, and the caller was experiencing flu-like symptoms including a high temperature and confirmed they already had a negative PCR.
Jackson used the HCC’s Clinical Decision Support System to assess the symptoms, and in the absence of other risk factors, recommended self care at home unless their symptoms worsened.
Congratulations

The Health Contact Centre (HCC)’s Quitline team headed to the North Coast during Reconciliation Week to raise awareness for its Yarn to Quit smoking program.
The team joined the North Coast Aboriginal Corporation for Community Health (NCACCH) at its Well Persons Health Check Day, held at The Pavilion Conference & Reception in Gympie on Saturday 4 June 2022.

More than 900 people attended the event this year, where Quitline telephone counsellors Gwen (pictured) and Michelle hosted a community stall to talk about quitting smoking and Quitline’s Yarn to Quit program. “Meeting face to face was a great experience and allowed people to see our smiling faces. A few people expressed their thanks for Quitline’s help and support.” Gwen, Aboriginal and Torres Strait Islander Team Member
The Yarn to Quit program provides free quit support to Aboriginal and Torres Strait Islanders including multiple support calls and up to 12 weeks of free combination nicotine replacement therapy. Quitline also has a dedicated team of Identified Telephone Counsellors, both male and female, who clients can elect to speak with if they would prefer.
“Having the option to talk to an Aboriginal and Torres Strait Islander team member is important as it allows our community to connect with confidence.” Peter, Aboriginal and Torres Strait Islander Team Member.
Queenslanders can call 13 HEALTH for access to advice from a registered nurse 24/7 all year round and recently the Health Contact Centre’s service received its five-millionth call.
HCC and thank you for Queenslanderssupporting to receive appropriate care as we face growing demand in health services throughout the state.
The Remembrance Service was held this year on 9 September in the lead-up to Foundation Day on 12 September, to commemorate our 36 fallen officers whose names appear on the QAS Roll of Honour.
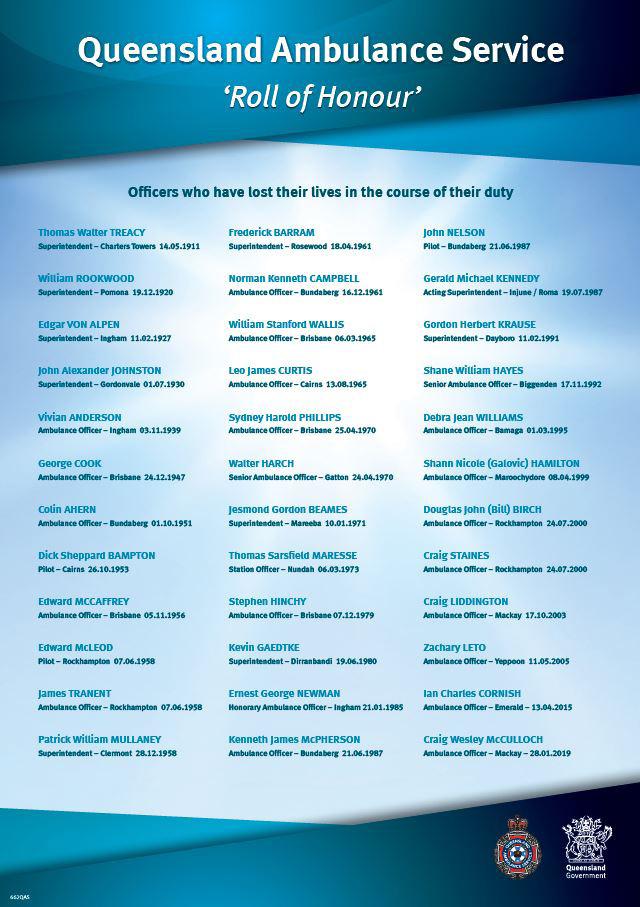
On 12 September in 1882, QAS’s ancestor organisation was born after a group of concerned citizens met to establish the City Ambulance Transport Brigade (CATB).
While a lot has chanced since then, what hasn’t changed is our staff and volunteers’ dedication and commitment to delivering timely and quality patient focussed ambulance services to all Queenslanders.
This year all QAS staff and volunteers were able to watch a special QAS Remembrance Day Service video presented by QAS Commissioner Craig Emery with the service conducted by Chaplain Daniel Ollis – you can watch it here


In September this year we honoured and paid our respects to the 36 ambulance officers who lost their lives in the course of their duty during a Remembrance Day Service.






 Rita Kelly and Health and Ambulance Service Minister Yvette D’Ath with the family of former officer Debra Williams who accepted her Posthumous National Medal.
Father Tom Stephen blessing the plaque
Health and Ambulance Service Minister Yvette D’Ath officially opens the new Thursday Island Station with Assistant Commissioner Rita Kelly.
Auntie Deidree Whap with Debra Williams’ niece Mary Mills who accepted her Posthumous National Medal on her family’s behalf. (Debra was one of Deidree’s mentors.)
Health and Ambulance Service Minister Yvette D’Ath presents QAS Field Officer Deidree Whap with her 30 year Long Service Medal
Rita Kelly and Health and Ambulance Service Minister Yvette D’Ath with the family of former officer Debra Williams who accepted her Posthumous National Medal.
Father Tom Stephen blessing the plaque
Health and Ambulance Service Minister Yvette D’Ath officially opens the new Thursday Island Station with Assistant Commissioner Rita Kelly.
Auntie Deidree Whap with Debra Williams’ niece Mary Mills who accepted her Posthumous National Medal on her family’s behalf. (Debra was one of Deidree’s mentors.)
Health and Ambulance Service Minister Yvette D’Ath presents QAS Field Officer Deidree Whap with her 30 year Long Service Medal
Australia’s most northern ambulance station was rebuilt several years ago, but thanks to COVID-19 pandemic delays until September this year the station was missing a vital cultural link – a blessing ceremony.
The station is home to five Advanced Care Paramedics, an Officer-inCharge and most importantly for this community, two Indigenous cadets. A blessing ceremony is an important cultural way of recognising the Torres Strait Islander Community’s connection and affiliation with the facility.

The official opening and blessing were timed so the Health and Ambulance Minister Yvette D’Ath and Father Tom Stephen could open and bless the station together.
Far North Region Assistant Commissioner Rita Kelly, who took on the day’s MC role said the Thursday Island team had gone above and beyond to ensure its station was ready for this special community celebration, with woven palm fronds decorated with flowers on the front gates signalling the special gathering and a largely home-made tasty morning tea to follow.
More than 30 attendees joined the special event, representing community members, QAS staff and the LAC, as well as the local fire and police services.
Father Tom Stephen was invited to open the morning’s event with a prayer and later blessed the commemorative plaque, the driveway, and the front door.
The Minister said the official opening was another exciting step in keeping Queenslanders healthy, no matter where they live.
“Thursday Island has a rich heritage, and the health-care needs of Aboriginal and Torres Strait Islander people is important for any government committed to ensuring equity for all.”

Ms D’Ath said the blessing ceremony of was an important part of recognising the Torres Strait Islander community’s connection and affiliation with the facility.
Deidree is the longest serving Torres Strait Islander in the QAS and has been instrumental in building connections between the QAS and the community.
She has also been a trailblazer for the ongoing support of the QAS Aboriginal and Torres Strait Islander initiatives.
Also honoured with a Posthumous National Medal was the late QAS Officer Debra Williams, who also happened to be one of Deidree’s mentors.
A proud Torres Strait Islander woman, Ms Williams passed away in 1995 after falling ill while on a training course with the QAS.
With the day’s preparations nearly complete, Deidree Whap, Rita Kelly and Ollie Ford sneak in a happy snap together
“We know Thursday Island and Torres Strait residents live a remote lifestyle in beautiful surrounds and the Queensland Government is committed to delivering the best care when people find themselves in need of an ambulance, regardless of the secludes of island life,” Minister D’Ath said.
The event was also exceptional because it included the presentation of two very special awards – a 30-year Long Service Medal was presented to Thursday Islander Elder and long-time staff member Deidree Whap, and a Posthumous National Medal was presented to the family of QAS Officer Debra Williams.
This award presentation was particularly significant for the team, as it was the first time Thursday Island staff have been recognised in front of their own community.
Debra had served communities in Cairns, Bamaga and Thursday Island for more than a decade prior to her passing.
Debra’s family attended the ceremony to accept her medal and brought her hat and photographs to commemorate her life in the service.
Debra’s niece Mary Mills said the presentation to Debra’s family was immensely important for the family as it meant her many years of service to the community was properly recognised.
Debra’s grave can be found on Thursday Island and is a lasting testament to her dedication to the QAS – with each tile decorated with the QAS logo, all made in Innisfail.
Click here to hear Deidree’s and Rita’s thoughts in their own words on the day’s event.
Thursday Island paramedics and the community had several reasons to celebrate in September, with the official opening and blessing of its station, and staff recognition and a Ministerial visit.





 Thursday Island’s old ambulance station
Thursday Island’s new ambulance station
The Thursday Island team. From left – Warren Martin, Majella Filewood, Adam Marston, Lucy Searle, Deidree Whap, Minister Yvette D’Ath, Rita Kelly and Beryl Wilson (LAC).
Auntie Deidree Whap cutting the ribbon while Father Tom Stephen blesses the station.
Thursday Island’s old ambulance station
Thursday Island’s new ambulance station
The Thursday Island team. From left – Warren Martin, Majella Filewood, Adam Marston, Lucy Searle, Deidree Whap, Minister Yvette D’Ath, Rita Kelly and Beryl Wilson (LAC).
Auntie Deidree Whap cutting the ribbon while Father Tom Stephen blesses the station.
The ASM recognises distinguished service by the men and women of Australia’s ambulance organisations.
Grant began his career as an Honorary Ambulance Officer for the Queensland Ambulance Transport Brigade in 1984 and was made a permanent Ambulance Officer the following year.
Since then, Grant has taken on a variety of senior clinical roles including Clinical Support Officer and Regional Operations Supervisor before completing his training as a Critical Care Paramedic.
Grant has also acted in senior roles across the organisation, from the Local-area Assessment and Referral Unit and the Kedron Operation Centre’s Clinical Hub.
His expertise and experience saw Grant deployed during Tropical Cyclone Debbie in 2017 and contribute
to several key projects across the service.
Grant said he felt honoured and humbled by the news of his selection.
“Everyone has a role to play in the ambulance service and it’s humbling because I am just one person contributing alongside many others. We all come together to provide this service to the community,” Grant said.
“I’m humbled by it, I greatly appreciate it, but I also know it’s just not me who does the job.”
QAS Commissioner Craig Emery said the prestigious award was a mark of recognition of Grant’s unfailing commitment and dedication to excellence in patient care.
“Grant’s dedication to education and training has enabled him to provide authoritative advice to junior staff,
After 38 years of service
Gold Coast Critical Care Paramedic Grant Gamble was announced as an Ambulance Service Medal (ASM) recipient in the Queen’s Birthday 2022 Honours List.
patients and carers, his peers and higher management during highly complex and extremely challenging incidents and environments,” Commissioner Emery said.
“Grant has served Queenslanders through his work at the QAS for nearly four decades and he continues to demonstrate the professionalism representative of today’s paramedic profession – and we’re immensely proud of him.”
Listen to Grant’s full reaction to his award announcement here…

This year Queensland Ambulance Service (QAS) celebrated a significant milestone in its long and distinguished history, marking 130 years of ambulance services in the state.
The award recipients this year were:
It’s quite remarkable to think about how much has changed since that time.
What hasn’t changed is the dedication and commitment of QAS staff and volunteers to deliver timely and quality patient focused ambulance services to Queenslanders.
As part of Foundation Day (12 September 1892) which is marked annually, the QAS holds both the Remembrance Service and our
Commissioner’s Achievement Awards close to this day.
This year QAS Commissioner Craig Emery announced the 2022 Commissioner’s Achievement Awards recipients on 12 September.
These awards recognise projects, initiatives, teams, individuals and volunteers who have demonstrated an outstanding commitment to the QAS, our patients and the community we serve.
Highly Commended Health Contact Centre Covid-19 Contact Tracing Efforts Initiative Customer Focus (Joint Winners) June Nielsen Local Ambulance Committee Member, South Brisbane and Logan Districts, Metro South Region
Sonia Tracey Administration Officer, West Moreton District Metro South Region
Fostering Innovation – Winner Dr Nhut (Tan) Doan Research Fellow Cardiac Coutomes Program, Information Support Research and Evaluation, Medical Director’s Office
Excellence in Performance –Winner William (Doug) Buchanan Officer-in-Charge, Chermside, Metro North Region
Courage and Integrity –Winner Health Contact Centre – Nursing Services Redesign and implementation of a new approach to nursing call quality and evaluation
Lisa Courtney, Nurse Unit Manager, Acute Care Anne-Marie Kinsella, Nurse Unit manager, Child Health Helen Lester, Nurse Unit MANAGER, Self Management of Chronic Conditions (SMOCC)
Kay Colley, Clinical Nurse Consultant Quality
Kelly Wigginton, Nurse Educator
Melissa Surrey, Clinical Nurse, SMOCC
Pamela McErlean, Director of Nursing Dr Kim McFarlane, Director of Clinical Safety and Quality
Execellence in Leadership –Winner Mei-Lin Dean Officer in charge, Kingaroy, Darling Downs and South West Region
Young Heroes of the Year –Joint Winners Chelsea Kucks and Maddison Jennings
Commissioner’s Achievement Award – Winner Angela Beatson Advanced Care Paramedic II, Central Queensland District, Central Region
Watch the video for the announcement and to find out more about each of the recipients.










 Communicable Diseases Team June Nielsen
Doug Buchanan
Chelsea Kucks
Maddison Jennings
Tan Doan
Mei-Lin Dean
Sonia Tracey
Nursing services
Communicable Diseases Team June Nielsen
Doug Buchanan
Chelsea Kucks
Maddison Jennings
Tan Doan
Mei-Lin Dean
Sonia Tracey
Nursing services
In November we celebrated some of our very special researchers’ milestones with their awards presented to them by our Medical Director Dr Stephen Rashford.
Congratulations to Research Officer Louise Sims who received her 10 years Long Service Badge, Operational Research Officer Nathan Daley who received his Long Service Medal 2nd Clasp (30 years) and Cardiac Outcomes Program Research Fellow, Tan Doan who received the Commissioner’s Award for Fostering Innovation.

This vital work our researchers do fosters innovation and understanding, and links directly to the high quality of care the QAS provides to all Queenslanders.
Wynnum Station celebrated a very special milestone for Wynnum Station’s ACP Russell Weeks, with AC Peter Warrener presenting him with several medals including his National Medal 1st and 2nd clasp for 25- and 35-years’ service, as well as the QAS Long Service Medal 2nd and 3rd clasp recognising 30 and 40 years of meritorious service with the QAS.
Russell began his career at Spring Hill in March 1978 with the QATB where he worked until 1988 before taking a break before returning to Beenleigh Station in January 1989 as an ambulance officer.
A decade later he transitioned to the position of Paramedic, working at stations including Pimpama, Nambour and Kawana before transferring to Wynnum in 2020. He’s also performed periods of higher duties as Officer in Charge in Biggenden.
Russell said he still loves his job and that’s why he’s stayed in it so long.
“The thing I love most about this job is the people I work with,” he said. “But none of us could do our jobs without the teamwork, and a good partner means the world.
Metro South saw a group of exceptional people recognised for long service during its awards presentation at Beenleigh Station, including mother and daughter duo Marcia and Jodie Love, who clocked up more than 60 years of service between them.

Met South Assistant Commissioner Peter Warrener presented Marcia with her National Medal 2nd Clasp (35 years) and Jodie with her National Medal 1st Clasp (25 years).

Jodie was able to share with us some photos taken of the pair when she first started in 1994 at Wynnum as an honorary ambulance officer, and also with sister Amanda when she was a paramedic too.


Jodie said she was so proud of her mum’s trailblazing work for gender equality in the days when women were a minority at QAS.
“Mum worked so hard to pave the way for the rest of us to come through, and we’re all so grateful for this,” Jodie said.
Marcia said she was incredibly proud of Jodie and all she’s achieved in her career so far.
“It’s a very special person who comes into this job – they need to show a lot of empathy and feeling, and we all need a lot of assistance and backup from our partners so there’s a lot of give and take in our roles.”
“My job has been helping people, and I love helping people and making a difference to someone’s life.
“Patients and their families look at you with trust – you never see a look like that from people – the public places so much trust in us, so anyone doing this job is a very special personI take my hat off to them all.
Russell was thrilled to have his family there to see the award presentation.
“In this job your family is everything – they’re our support crew when we’re not on the road.”
Russell said one of the best innovations he has seen over the years in QAS is the inclusion of Priority One into the organisation.
“We deal with so much out on the road, and it does take its toll with PTSD, so the extra focus on our own mental wellbeing has certainly been welcomed,” he said.
Russell Weeks and his family























In the 1920s, an Arrol-Johnston motorcar began transporting Nambour’s sick and injured in a defining milestone for the recently established ambulance centre.

During a centenary commemoration in April 2022, generations of Nambour residents were once again taken on a trip in the Arrol-Johnston, this time through history.
When Thomas Beech was officially appointed the first superintendent of an independent Queensland Ambulance Transport Brigade (QATB) centre in Nambour, a glimpse into the modern service that now stands a century later would have been unfathomable.
While Nambour ambulance has evolved into a beehive of operations servicing the Sunshine Coast hinterland, staff are proud to say they have maintained the family atmosphere of a smaller team.
For evidence, look no further than the meticulously planned and well-attended commemoration events that paid tribute to those who have served over the past 100 years.
A private twilight function on the Friday provided a space for former and current staff and volunteers to reminisce on the vast changes before an open day on Saturday provided a wonderful occasion to embrace the wider Nambour community.

While the modern ambulance station can be found on Rigby Street, the Ambulance Centenary Open Day was held at the Nambour Tram Terminal to cater for the large turnout, CPR sessions and a heritage display.

An integral part of Nambour ambulance’s success and longevity is owed to its Local Ambulance Committee (LAC), which has donated more than $200,000 in education and equipment to its local QAS staff. It also frequently engages with the community in CPR and AED awareness.

On Friday 12 May the HCC celebrated International Nurses Day which involved several activities but with its main one fundraising, which raised close to $2,000 to donate to nurses in the Ukraine.
 Mick Davis, OIC Joy Reitze, AC Stephen Gough and Manager Clinical Education Alexis Hughes
Mick Davis, OIC Joy Reitze, AC Stephen Gough and Manager Clinical Education Alexis Hughes
In May the QAS teamed up with Queensland Police and Queensland Fire and Emergency Services to launch National Road Safety Week.

QAS Petrie Officer in Charge Dermot Kelly joined his emergency services colleagues at the media launch, held on the side of the busy Bruce Highway at the Caboolture Service Station to urge all Queenslanders to take the pledge to drive to survive.
“Our joint effort of raising awareness for Road Safety Week each year is important as it shows a united front from the emergency services because it affects all of us too,” Dermot said.
“If we can reduce road accidents, it frees us up to get to the other unpreventable jobs.”
Dermot said the most difficult thing about responding to crashes was that
99 per cent of them were preventable.
“Most of them are caused by speed, lack of concentration or not driving to weather or road condition or being aware of your surroundings,” he said.
Dermot has responded to countless road accidents during his time as a paramedic and knows firsthand the impact road traffic crashes can also have on first responders.

“Even some of the most senior officers can be affected, especially when you’re treating kids around the same age as your own,” Dermot said.
“The good thing after an incident is over is to debrief and talk to people to help you rationalise what happened reaffirm what you do actually helps people.”
The QAS has support available to all staff in all regions and encourages everyone to access it – whether it’s through Peer Support, our
non denominational Chaplaincy Service, or Priority One. Staff can also call our 24hr Telephone Counselling Service 1800 805 980. For more information click here.
Like many of the small mining towns dotting regional Queensland, Baralaba’s ambulance service was borne through the necessity of remoteness and carried through the decades by the blood, sweat and tears of a tight-knit township.

Since its first building was funded and completed in 1923, Baralaba’s ambulance station has remained a monument of a community that takes pride in everyone pitching in to look out for one another.
QAS officers joined QFES, QPS and SES in a joint exercise at Clump Point Lookout at Mission Beach with a scenario of a search for a person who had been fishing at the Point but failed to return and was reported missing.
The QPS team coordinated the search, while QFES established safe access to the search area and then SES, QFES and QPS started a ground search over difficult terrain. SES also had a boat out on the water involved as well.

The missing patient was successfully located with serious leg injuries and our QAS team stabilised and treated them before all agencies worked together to extract them back to the lookout before a debrief was held.
On 25 June about 100 local community members turned out to celebrate Baralaba Station’s centenary, where previously unseen photos and memorabilia were on show, a tribute garden was with a very special plaque were unveiled, along with a 20-year pin presentation to long-serving LAC member John Lawson.

The garden serves as a tribute set in stone for a town which once saved its ambulance service during the Great Depression when the General Secretary of the Queensland Ambulance Transport Brigade, Captain E Pike, arrived in 1933 intending to close the service and relocate its vehicle to a nearby town.
At the time, the townspeople rallied in support of their local committee, and it was decided the car would remain in Baralaba with the local service functioning as an Honorary Centre.
Brisbane’s Ekka finally made its post-COVID return to entertain the crowds for the first time in three years in August and the QAS was there encouraging people to learn valuable life-saving skills.

This year the Ekka ran from 6 to 14 August 2022 but was slightly different to previous years with capped visitor numbers and increased infection control measures.
As part of the Queensland Government Precinct, the QAS display encouraged visitors to learn important skills including hands-only CPR, using an Automated External Defibrillator, calling Triple Zero (000) and downloading the Emergency+ app in case of emergency.
The Mechanical Chest Compression Device (MCCD) was also on show.
The QAS teams based at the display also fielded many different questions from visitors.
FAST FACTS – QAS EKKA DISPLAY
• 3 years without an Ekka
• 9 days for Ekka 2022
• 81 hours the QAS display was open
• 10 Aug Busiest day (Brisbane public holiday)
• > 340,000 Visitors to the Ekka
• > 52,000 Visitors to the Queensland Government Precinct
QAS engagement and community education – priceless!
The Health Contact Centre (HCC) has won one the Advancing First Nations Health Equity Category in this year’s Queensland Health and Department of Health Awards for Excellence.

The award was presented during a live cross to the HCC offices on Friday 26 August and the HCC won its category for its contribution to the delivery of state-wide targeted First Nations prevention and health promotion strategies.

The CAA Women in Leadership Forum
The CAA Women in Leadership Forum was held on 11 August in Sydney and Queensland Ambulance Service’s Senior Operations Centre Supervisor, Mindy Thomas won the Leadership Scholarship at the CAA Gala Awards dinner.

The Queensland Ambulance Service also was successful in winning the Leadership Award for our pandemic response.
Congratulations to Mindy and our leadership team!
These awards recognise initiatives and teams who have demonstrated a commitment to excellence when supporting or delivering health services to Queenslanders during 2020-21.
Well done team!
Gympie Station marks 120 year milestone
Gympie Ambulance Station quietly marked a very special milestone in September –120 years of ambulance services in the region.
Long-time Officer in Charge (OIC) Wayne Sachs said a low-key celebration was held on 17 September at the station to celebrate which included a staff barbeque.
A proud chronicler of the Gympie Station’s history and author of ‘Gympie Ambulance 1902-2002’, Wayne holds a wealth of knowledge of the region and its rich paramedic history.
From its humble beginnings in 1902, Gympie Station has transformed along with the ‘town that saved Queensland’ to become the state-of-the-art service it is today.
The station has had several moves over the years and can currently be found on the corner of King and Alfred Streets where it started operating on Monday 4 September 2006, before being officially opened on 15 January 2007.
This station sits on Gympie’s first cemetery, which operated from 1867 to 1869, a total of 86 people were buried at the site and their
names are now listed on its wall.
Past and present officers have reported a spooky presence in the station after dark, but Wayne explains this away saying the staff are just having some fun.
Since a 1922 public meeting was held to establish a Queensland Ambulance Transport Brigade (QATB) centre, community support in has been the bedrock for sustaining Boonah’s ambulance service over the following century.
The Boonah Ambulance Station officially celebrated its 100-year milestone on 1 October 2022, with local staff rolling up the station doors to host a public heritage display in a tribute to the last century.

Today’s Boonah paramedics continue to benefit from a strong sense of community that sees them working alongside volunteers from the Boonah First Responder Group and Boonah Local Ambulance Committee (LAC).

Boonah Officer in Charge Russell Pavey addressed the attendees of the Open Day to express his pride in the station and the staff in which he works alongside.
“Boonah Ambulance has seen it all, from pandemics, floods, road traffic crashes, aircraft and boating incidents, sporting,
farming and misadventure injuries located anywhere from home to the bush, lakes and mountains,” Russell said.
“With all the changes, the purpose of the ambulance service has remained the same as 100 years ago, we still get the patient and take them to hospital or appropriate medical care, in ideally a better condition than when we found them.”
Melissa kicked off Mental Health Week early by joining in on the Conquer the Corrugations Walk in Coen to shed a light on mental health, particularly in remote and isolated communities.

More than 150 people from all walks of life trekked 42km through the blistering North
Queensland heat and red dirt from Coen Information Centre to the Archer River Roadhouse, supporting each other every step of the way.

Well done to Melissa and everyone involved!
#mentalhealthweek2022
(And how good does our new car wraparound look?!)
QAS Flappers and Sheiks got their glamour on for a good cause
QAS staff managed to “dud up”, find a “sharpshooter”, and enjoyed some “cat’s pyjamas” “whangdoodle” – or got dressed up, found themselves a great dancing partner and enjoyed some great jazz – for a good cause in November.
QAS staff from the Sunshine Coast area helped organise the Great Gatsby Gala, a formal event held at the Sunshine Coast Convention Centre, Novotel Twin Waters on Saturday 19 November to raise around $18,000 for the Sunshine Coast Hospital and Health Service’s (SCHHS) End of Life Care Research Program.

Officers past, present and future joined eager members of the public to help celebrate the Sandgate Ambulance Stations Centenary on Saturday 5 November.


Sandgate, as a Sub Centre of the Queensland
Ambulance Transport Brigade (QATB), was first suggested at a public meeting in the local Town Hall in February 1922. The new committee held its first meeting on 8 February and a house on Brighton Road was rented as a temporary Station called ‘Laguna’.
The first purpose-built ambulance station in
Sandgate officially opened in August 1924 and in November 2001, Sandgate Ambulance moved to Bracken Ridge where the service is located today.
The day marked a ‘covid delayed’ celebration for this station and its hardworking members, including Craig Claassen one of Sandgate’s longest serving officers.

He has been with the Queensland Ambulance Service (QAS) for almost 40 years and said it was very special to be involved with the celebrations.
From members of the public walking through the middle of the station to where it is today, the Sandgate Ambulance Station has come a long way.
Teaching CPR to young Sandgate community members Met North AC Tony Armstrong Sandgate LAC volunteers helping out on the day Joy Reitze (OIC Nambour), Alexis Hughes (MCE Sunshine Coast District), Kevin Smith (Buderim Station) in their glad bags. Thumbs up!The QAS took time out in May to thank our wonderful volunteers and recognise the vital work they do for the service and their communities. Meet some of our wonderful volunteers –
Powerhouse mother and daughter duo Jenny and Rachael Floyd have a combined 50 years of volunteering for the Kirwan Local Ambulance Committee.

Jenny joined in the early 90s and Rachel joined soon after to be a younger voice in the Committee and is now LAC President while her Mum is now the LAC Treasurer.
“Like everything, emergency services need to have some backup from the community,” Jenny said.

Rachael said her father’s heart attack reinforced how important CPR skills were.
Jason has been supporting the QAS response in Barcaldine and surrounds for a decade now and has never looked back.
“It helps people, you never know when you’ll be in that position,” he said.
Their dedication to QAS only strengthened when their husband and father suffered a heart attack in 2006 and had to be airlifted to hospital – and Jenny says he owes his life to the medical help that day.
“Now as a Peer Trainer I can pass on CPR Awareness to others, which is very important for anyone at any age if you’re ever put in that situation,” Rachael said.
They both share a passion for passing on their knowledge and skills to the next generation.
Zach works full time, has volunteered with the QAS for the last two years, and also volunteers with the local Rural Fire Service (RFS) and State Emergency Service (SES) crews.
“Seeing the smile on someone’s face when you turn up to a job in their darkest time,” he said.
“They’re just looking for someone to give them a helping hand and guide them and it’s such a good way to give back to the community.”
Wendy went from having no medical experience to saving lives as a volunteer with QAS and is one of the longest standing volunteers in her region, after joining about a decade ago when she and her husband moved from Mackay to Woodgate to retire.

“We went to a community meeting, and we went along just to meet people, and someone came up and said, ‘you would be a good First Responder’, I had no idea what a First Responder even was!” she said.
She has since been to countless jobs, saved someone’s life by delivering effective CPR and is a huge part of her community.
Glenn volunteers on the water, on the roads and everything in between as a Volunteer Marine Rescue (VMR) First Responder, starting 26 years ago before the .
He had volunteered with his local VMR crew at Southport for 26 years, so when they joined forces to introduce QAS’ First Responder program 11 years ago, he jumped at the chance to be involved.


Our paramedics work closely with VMR who help us get to and from patients as quickly as possible.
“I always had an interest in water and fishing, and I just love helping people,” Glenn said.
Everyone has different levels of success. For me, success can never be achieved unless you have the desire to initiate it. The amazing work and commitment from staff that continuously results in appreciation letters we receive from members of the public, makes me constantly aware of what accomplishments we have made as an organisation.
From Keren from Griffin...
This month has seen an influx of thank you letters, with 304 letters received this year to date and 609 letters and emails of thanks sent to staff members.

I cannot thank you enough for all your hard work.
Russell Bowles ASM QAS CommissionerReading the submissions of gratitude and praise written about our staff and services, it provides me the opportunity to reflect on the critical work that the QAS performs. I would like to thank each of you, for your dedication and passion to meet the increasing community demand for healthcare delivery. Your hard work is recognised by the members of the community and your colleagues, and it is a highlight to send these through to you.
Between 1 April 2022 and 31 October 2022, a total of 521 appreciations were received. Once received, I sent 562 emails onto the deserving officers, attaching a copy of the appreciation.


 Craig Emery asm QAS Commissioner
Craig Emery asm QAS Commissioner
I just wanted to send a message to say thank you to Darcy and Sam who were working on Tuesday the 10th May that came out on Tuesday evening to help my daughter Anna on her 3rd birthday who was having trouble breathing. They were absolutely amazing and kept her completely at eze and comfortable. So professional. They made an awful experience somewhat joyful and kept my daughter happy. Thank you so much. I also hope Sam had a great wedding. If you can pass on my gratitude to them would be very much appreciated. You are lucky you have such great staff. Thank you very much :) D’arcy and Sam
Just want to say a big thank you to the ladies (Corinne Wilkes, Kate Olive and Candice Boileau) that came to my house this morning (July 19) for my little girl and the dispatch guy (Jamaine Prieditis) who helped me stay very calm. They do an amazing job and I really appreciated them being so fantastic.
Kristie, MorningsideFrom Jess from Hervey Bay...
I wasn’t sure how to pass along a giant ‘Thank You’ to one of your amazing Paramedics based in Hervey Bay and could be passed along to his bosses.



My son was being seen to in the Hervey Bay ER last Friday when a Paramedic by the name of Normie had walked past us and returned to our cubicle where he spoke beautifully to my 8-year-old son and proceeded to pull a knitted blue teddy from his pocket and hand to my son. Normie, with a great big smile tapped him on the shoulder and wished him well and went on his way.

From Kerri from Bellara...
I would like to take the time to express our thanks to various QAS officers for their attendance and assistance at our unplanned home birth on 4/9/2017. I commend the Triple Zero officer (Julie Ricardo) for her efficiency and ability to reassure us that help was on the way and clear instructions in the meantime. Tammy (Olsson) arrived on scene approximately 5 minutes following the birth of our son Woody and I would like to commend her professionalism, calm in the situation and ability to treat me as a fellow being rather than just a patient. She was caring, compassionate and efficient. I appreciate Tammy arranging for our transfer through to Hervey Bay Hospital. I believe Arto (Hirsimaki) and another officer (Andrew Rach) assisted with my transfer

Thank you to Yorky and Neil the BEST paramedics who transported my son Rain to Caboolture hospital this morning. So kind, caring and funny. You are amazing!!! And to Erin in the Paediatric ward tonight and the private room we got! We are very happy, warm and comfortable. Thank you so much :) you all went above and beyond!! Hoping to go home tomorrow Yorky and Neil
I want to send a quick thank you to the paramedics (Chantal Greaney and Melissa Dajic) who assessed my son and took him to hospital on Wednesday night (July 12). It was the first time I have ever had to call the ambulance and I was quite nervous in doing so – worried I was overreacting and wasting the paramedics time. The two ladies who attended our home were so calm and reassuring. They quickly assessed my son and took us to Lady Cilento, all the while distracting my son with Wiggles videos and calming a nervous and panicked mum. Thank you for such excellent service and care!!! I don't believe this service gets the recognition it deserves for all the work your paramedics do.
What Normie did not realise at that time was my son had just had a massive bleed at home from a tonsillectomy 14 days post op and had lost a lot of blood. We had just rushed into the ER where they briskly took us out the back to be seen and assessed (yes we should have called an ambulance but I thought I could get him quicker to the hospital than the ambulance would get to us). I was still in panic mode and my son was in a little bit of shock, therefore Normie coming over to us and handing over this teddy made the next few hours and days a little less traumatic for my son as he had this little blue teddy to hold onto and comfort him.
Just want to give a shout out to the LARU officer who attended my home on Monday (August 21). His name was Steve (Kliese) and we are in the Ipswich area. He was prompt, caring, compassionate, empathetic, funny and the list goes on. He had me reassured within minutes. If my thanks could be passed to his OIC that would be appreciated.
From Nicole from Calamvale...
Courtney and Angela from Munruben station came out to visit myself and nearly 4yo son Jackson tonight for croup with a stridor. Jackson has only just gone to bed now (good old steroids) but he has been talking about the “nice girls” since they left. They even showed him their flashing lights (which I’m sure Jackson’s twin brother who was fast asleep in bed is going to be annoyed he missed haha). And as soon as they drove off he said “Mummy, it was nice to see Courtney and Angela” Hats off to the amazing work all the staff do but if you are able, can you pass this special message onto the girls at Mubruben. They were so friendly, knowledgeable and great with Jackson. If I ever have another call out, I secretly hope to get them again.
Courtney and Angela
After Normie had left us, we were moved quickly to the resus unit and a Life Flight helicopter was organised to transfer us to the QLD Children’s Hospital. As I was walking through the ER just as the flight doctor and nurse arrived to prepare us to fly, I came across Normie in the corridor. I thanked him again, confirmed his name and explained what was happening to my son and that his random act of kindness has made his last few hours there just a little bit easier. Normie popped his head into us as my son was being moved onto the helicopter bed to give a smile and wave to my son. Again, just a beautiful gesture from him.
My son named the teddy ‘Normie’, and ‘Normie’ has had one hell of an expedition over the weekend. My son cuddled him the entire flight and the time we were away and now has a special spot on my son’s bed.
To some it may just be a teddy, but for me that teddy took away some of the scary stuff my son had to deal with for the first time ever.
Thank you Normie for your random act of kindness that made a world of difference for Brax!!! You are a true credit to your patients, team and community!!
Normie
From Andrew from Nundah
Just like to thank you for the quick response to my call for my neighbour at Nundah. It was under 10 minutes, and they were here taking over. My wife and two other neighbours were sharing CPR until they arrived and my 30+ years of yearly CPR training as an Electrician was a great help in keeping everyone on track until the ambulance arrived, as well as the lady on the phone was great. Unfortunately, I was informed by our neighbour’s son-in-law that she did pass away, but he thanked our efforts as they are from New Zealand and it helped keep her alive long enough for them to fly over and say their good byes while she was alive. Our neighbour was also able to donate some organs to someone in need which her family mentioned at her funeral. Thanks again!
John, Bryce, Brad, Andrew, Gabrielle and Sascha (ECH)
From Marietta from Capalaba...
I’d like to send a BIG hugs and Thankyou to Capalaba Ambos who were on duty last Sunday afternoon around 2:30. I had a car accident on Redland Bay Road (my first at age 66 and 7months!) and “Brucey” (with a very funny sense of humour!) and Michael were wonderful helping me in every way possible. They drove me to Mater Private to be under the care of their Medical Staff. Loved their sense of humour, even though I was in too much pain (with a cracked sternum) to laugh! I’m home now and resting with more medical tests by my GP! Lovely blokes. Bruce and Michael
From Jennifer (and Cynthia) from North Ipswich...
I would just like to thank you for looking after my Mother Cynthia Brook twice a week when she has to go and have Cancer treatment In South Brisbane. I know it must be so hard for you all when you have emergencies that need you, but you are booked for transport to other sick patients. Thank you for what you do always. I really appreciate your work always no matter what you do. (Mum also gets some great recipes from the grew along the way to and from her treatment at Icon South Brisbane.)
John, John, Indira, Marcus, Martin, Seru, Daniel, Christine, Emma and Danielle
From Kevin from Thornlands...

A big shout out to the two paramedics who took me to Redlands Hospital this morning after my bike accident in Fitzroy St Cleveland. I can’t remember their names but thank you so much. Very caring and so professional.
Jennifer and Ian
From Kate from St George...
Thanks for a great morning at St George Careers Expo. The ladies were lovely and kids had a great time. Claire and Hallie are both potential future paramedics in western Queensland.

I just wanted to send a big thank you to the paramedics and student paramedic that attended to me early this morning. I’m currently going through a medical condition that is a bit strange and is being investigated but the paramedics that attended were so compassionate and treated me with the upmost respect even though the service was extremely busy and under pressure last night (21 June 2022).
Thank you again for everything you do for Queenslanders to help us in our times of need, even when that means sacrificing time with your own families Hayley, Jason and Tomos
On the 26 October 22 my almost five month old baby had stopped breathing she had a few moments of not breathing, paramedics were called straight away, we had two ambulance and a critical care as well, and one paramedic in particular Troy, was an absolute godsend, he helped calm me down from being so emotional, we got taken to the Prince Charles Hospital in the childrens ED, later that night Troy had brought in another unwell child, and he took the time to come and see my baby. We were still in the ED awaiting on test results, she unfortunately has pneumonia and rhinovirus, I would just like to pass on my absolute gratitude to Troy and the other lovely paramedics who did their best yesterday for my baby, and mainly Troy for remembering my baby Indiana. We were from Murrumba Downs.
Troy, Melanie, Samuel, and Robert
From Brett from Eastern Heights...
Big shout out to Kelvin (Ipswich) and Letitia who were the paramedics that attended to me with a suspected heart attack today at Eastern Heights. Bloody brilliant, reassuring and so professional. Thank you so much.... your care and concern was outstanding.
Kelvin and Leetasha
NAME
Position Title
Years
Edwin (Tom) Roberts Paramedic 50 Central Region
Mark Smith Paramedic 27 Central Region
Heather Johnson Paramedic 33 Central Region
Melanie Smith Emergency Medical Dispatcher 10 Central Region - Rocky OpCen
Jessie Kerswell
Local Ambulance Committee Member 30 Central Region - Bowan LAC
Ronald Pont Pesident 27 Central Region - Gemfields LAC
Jessie Pont Local Ambulance Committee Member 31 Central Region - Gemfields LAC
Janelle Boto Local Ambulance Committee Member 13 Central Region - Wowan/Dululu LAC
Timothy Turvey Paramedic 15 Darling Downs and South West Region
Andrew Kajewski Patient Transport Officer 17 Darling Downs and South West Region
Jon Emberg Paramedic 16 Far Northern Region
Kerry Hill Paramedic 12 Far Northern Region
Morris Mitchell Paramedic 32 Far Northern Region
Sarah May McGurk Paramedic 11 Gold Coast Region
Ian Tucker Paramedic 20 Gold Coast Region
Darren Williams Paramedic 22 Gold Coast Region
Glen De Kleyn Emergency Medical Dispatcher 23 Gold Coast Region - Southport OpCen
Lawrence Lambie First Responder 13 Gold Coast Region
Brett Rogers Project Officer 25 Office of the Medical Director
Jennifer McCormick Learning Management System Administrator 35 Office of the Medical Director
Graeme Hodges Prinicpal Fleet Technical Officer 23 Corporate and Statewide Services
Jody Elson Principle Business Analyst 12 Corporate and Statewide Services
Catherine Bishop Business Support Officer 20 Corporate and Statewide Services
John Hammond Assistant Commissioner 23 Corporate and Statewide Services
Anthony King Director 37 Office of the Commissioner
Alan McGrath Manager, Patient Transport Services 40 Metro North Region
Desley Jozefowski Local Ambulance Committee Member 15 Metro North Region - Bribie Island LAC
Derek Greaves Paramedic 19 Metro North Region
Natalie Roberts Paramedic 12 Metro North Region
Harriet Stevens Paramedic 10 Metro North Region
Julie Robert Emergency Medical Dispatcher 17 Metro North Region - Brisbane OpCen
Melissa Jackson Emergency Medical Dispatcher 13 Metro North Region - Brisbane OpCen
Ray Rickwood Local Ambulance Committee Member 26 Metro South Region - Wynnum LAC
Wayne Sylvander Paramedic 12 Metro South Region
Pink Brian Patient Transport Officer 12 Metro South Region
Paul Morris Workforce Planning Officer 23 Metro South Region
David Newman Paramedic 47 Metro South Region
John Borowski Paramedic 41 Metro South Region
Ian Pask First Responder 11 Metro South Region
Dorothy Collingqwood Local Ambulance Committee Member 17 Metro South Region - Macleay LAC
Kahli Ball Emergency Medical Dispatcher 10 Northern Region - Townsville OpCen
Allan Wallman Paramedic 37 Northern Region
Susan Hall Emergency Medical Dispatcher 12 Northern Region - Townsville OpCen
Anna Balestrieri Patient Transport Officer 13 Sunshine Coast and Wide Bay Region
Michael Williams Paramedic 14
Sunshine Coast and Wide Bay Region
Helen Lloyd-Jones Patient Transport Officer 18 Sunshine Coast and Wide Bay Region
David Raine Local Ambulance Committee Member 34 Sunshine Coast and Wide Bay Region - Caloundra LAC
Julie Ann Kleeman Paramedic 34
Sunshine Coast and Wide Bay Region
Robyn Boyd Clinical Support Officer 25 Sunshine Coast and Wide Bay Region
Leona Olsen Local Ambulance Committee Member 15
Mervyn Olsen Local Ambulance Committee Member 15
Sunshine Coast and Wide Bay Region - Turkey Beach LAC
Sunshine Coast and Wide Bay Region - Turkey Beach LAC
Lyle Oppermann Paramedic 29 Sunshine Coast and Wide Bay Region
Shane Foley Patient Transport Officer 31 Sunshine Coast and Wide Bay Region
Melissa Connolly Paramedic 18 Sunshine Coast and Wide Bay Region
Adam Gaffel
Principal HR Advisor Metrics & Reporting
Reflects activities during the period from 27 April 2022 to 1 November 2022.
Appointed date Location
23-May-22 HR Analysis and Reporting
Amanda Harper Director 4-Jul-22 Townsville District
Andrea Thompson Principal HR Consultant 25-Jul-22 Workforce Reform
Andrea Whelan Officer In Charge 21-Mar-22 Agnes Water Ambulance Station
Andrew Davidson Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Angela Perry Senior ATSI Cultural Safety Advisor 29-Aug-22 ATSI Cultural Safety Unit
Anthony Hose Director 4-Jul-22 South Brisbane District
Ashleigh Hourigan Support Officer 24-Feb-22 Service Planning
Ben Clarke Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Blake Karas Manager Clinical Education 5-Sep-22 Gold Coast Region
Bradley Woodward ICT Enterprise Architecture and Planning 4-Jul-22 ICT Governance Strategy and Performance
Cindy Pepperdene Executive Services Officer 8-Sep-22 Executive Services
Claire Bertenshaw Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Craig Pearce Principal Management Accountant 14-Feb-22 Management Accounting
Cristal Drew Senior HR Consultant 5-Sep-22 Northern Region
Darren Pirie Director 18-Jul-22 Central Queensland District
David Hartley Assistant Commissioner 20-Jun-22 Statewide Services
Desmond Cannon Senior Advisor Health and Safety Management 8-Aug-22 Workplace Health and Safety
Drew Hebbron Assistant Commissioner 20-Jun-22 Gold Coast Region
Emma Waghorn Clinical Team Leader 31-Oct-22 Statewide Services
Glenn Ryan Senior Medical Clinical Coordinator OpCen 26-Sep-22 Office of the Medical Director
Gulnaz Caplice Procurement Officer 9-May-22 Procurement
Hayley Salethorne Director 1-Aug-22 Sunshine Coast District
Jacqui Kelsey Operational Support Officer 26-Sep-22 Frontline Services Group
James Symes Procurement Officer 23-May-22 Procurement
Jessica Kranenburg Operations Supervisor 19-Sep-22 Metro South Region
Jessika Brind Director 18-Jul-22 West Moreton District
Joanne Selby Operations Supervisor 16-May-22 Far Northern Regional Office
John Glasheen Senior Medical Clinical Coordinator OpCen 26-Sep-22 Office of the Medical Director
Joshua McGuigan Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Kari Arbouin Deputy Commissioner Operations - North and Rural & Remote 13-Jun-22 Northern Regional Office
Kassandra
Kanagaratnam Counsellor 8-Aug-22 Far Northern Regional Office
Kate McCoist Principal HR Consultant 23-May-22 HR Recruitment
Kelly Anderson Counsellor 23-May-22 Central Regional Office
Kim Lai Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Kristie Van Fleet Operations Manager Frontline Services 8-Aug-22 Frontline Services Group
Leah Jorgensen Executive Support Officer 23-Jun-22 Metro South Regional Office
Linda Gallegos Executive Manager Financial Accounting 18-Jul-22 Financial Accounting
Lisa Dibley Director 4-Jul-22 Moreton District
Lisa Walker Principal HR Consultant 18-Jul-22 Workforce Reform
Louise Sing HR Advisor Metrics and Reporting 23-May-22 HR Analysis and Reporting
Lyn Bassett Operations Centre Supervisor 31-Oct-22 Cairns Operations Centre
Malcolm Veal Officer in Charge 28-Mar-22 Wandoan Ambulance Station
Mandi Kittel Senior ICT Purchasing Officer 17-Oct-22 ICT Programs and Service Management
Manjeet Singh Director 4-Jul-22 Cairns District
Matt Bourne Technical Project Officer 11-Apr-22 Application Development Services
Matthew Green Assistant Commissioner 20-Jun-22 Northern Region
Michael Gaskin Manager Workforce Planning 3-Oct-22 Central Region
Michelle Mantgaris Operations Centre Supervisor 31-Oct-22 Cairns Operations Centre
Miranda Thomas Senior ATSI Cultural Safety Advisor 29-Aug-22 ATSI Cultural Safety Unit
Neil Slabbert Senior Medical Clinical Coordinator OpCen 31-Oct-22 Office of the Medical Director
Paige Harris Clinical Team Leader 31-Oct-22 Office of the Deputy Commissioner - South Queensland
Patricia Murray Executive Manager ATSI Cultural Safety 16-May-22 ATSI Cultural Safety Unit
Peta Thompson Director 4-Jul-22 Logan District
Rita Kelly Assistant Commissioner 20-Jun-22 Far Northern Region
Robin Crittenden Counsellor 8-Aug-22 Far Northern Regional Office
Sally Wuersching Director 1-Aug-22 North Brisbane District
Sam Anstee Principal HR Consultant 29-Aug-22 HR Services
Samantha Herring Clinical Team Leader 31-Oct-22 Statewide Services
Sarah Dickson Human Resource Consultant 19-Oct-22 HR Services
Scott Cooper Manager Clinical Education 15-Aug-22 Far Northern Regional Office
Scott Revell Assistant Commissioner 11-Jul-22 Office of the Deputy Commissioner - South Queensland
Stacie Ramanah Executive Manager Recruitment 23-May-22 HR Recruitment
Stephen Walsh Senior Medical Clinical Coordinator OpCen 26-Sep-22 Office of the Medical Director
Stephen Zsombok Deputy Commissioner Corporate and Statewide Services 16-May-22 Corporate and Statewide Services
Steven Ball Health and Safety Advisor 29-Apr-22 Northern Regional Office
Steven Miller Principal Business Intelligence Analyst 17-Oct-22 Operational Business Intelligence & Planning
Stewart Watkins Clinical Team Leader 31-Oct-22 Service Planning
Teresa Leung Operational Support Officer
26-Sep-22 Frontline Services Group
Thomas Hassall Product Manager Frontline Communications 12-Sep-22 Frontline Services Group
TJ Gueco Operational Support Officer 26-Sep-22 Frontline Services Group
Tony Armstrong Assistant Commissioner 20-Jun-22 QAS Spring Hill
Verity Ney Executive Manager Corporate and Statewide Services 21-Jul-22 Corporate and Statewide Services
Vicki Puplett Principal Awards & Reporting Officer 8-Sep-22 Executive Services
Warren Painting Director 1-Aug-22 Wide Bay District
Wayne Loudon Clinical Team Leader 31-Oct-22 State Operations Coordination Centre