


“Our community can feel confident that our nurses worked tirelessly to provide high-quality, evidence-based, compassionately connected nursing care.”




“Our community can feel confident that our nurses worked tirelessly to provide high-quality, evidence-based, compassionately connected nursing care.”
It is with great honor and appreciation that I share the 2023 Bismarck Nursing Annual Report. This year has been a particularly amazing year full of accomplishments and growth. We achieved our fourth Magnet designation with a number of exemplars which will be showcased later in this report.
Our community continued to see growth and a desire for high-quality health care which resulted in the need to increase services and access within the Sanford Bismarck Region. With that growth, we experienced record volumes in deliveries, surgeries, emergency room visits, and our second-largest year of overall admissions. I am proud to report that nursing was at the forefront of that growth. Nursing collaborated with our interdisciplinary team members to offer exceptional care while remaining flexible, efficient and adaptable. Our quality of care, clinical outcomes, research and educational offerings served us well as we worked toward improving the health of our communities. Safety and quality remained the pillars in driving that work.
Our community can feel confident that our nurses worked tirelessly to provide high-quality, evidence-based, compassionately connected nursing care. We can be proud of our accomplishments in 2023.
As your nursing leader, I look forward to 2024 as another great year of innovation and technological advances in virtual care, all while keeping the patient at the center of our care. Our construction and facilities crews will be hard at work with projects such as the expansion of the Sanford Broadway Same Day Surgery Center’s endoscopy/procedural rooms, 36 additional beds on floors three, four and five of the Legacy Wing of the medical center, the Sanford Southridge Downtown Walk-in Clinic, phase-two renovation of the emergency department’s trauma bays, and the Sanford East Century Ave Clinic’s addition of a multi-specialty clinic. Through it all, we will look ahead and build on the talents, experiences and beliefs of our employees to improve the lives of the diverse community of patients we serve.

With gratitude,
Wendy Kopp, PhD, MSN, RN, CENP Chief Nursing Officer, Sanford Bismarck Medical Center and ClinicsDedicated to sharing God’s love through the work of health, healing and comfort.
Improving the human condition at every stage of life through exceptional care, spiritual enrichment, innovation and discovery.
Calling
Demonstrating enthusiasm for those we serve, our vocation and the organization’s mission.
Courage
Having strength to persevere, innovate, use our voices and take action.
Family
Celebrating the connection and commitment we have to each other through it all.
Community
Providing care in a diverse range of settings and environments with a focus on the wellness of individuals.
Service
Sharing God’s love through actions that reflect compassion, acceptance, love, humility and sincerity in keeping with the common Lutheran heritage of our legacy organizations.
Resolve
Adhering to systems that align actions to excellence, efficiency and purpose.
Advancement
The pursuit of individual and organizational growth and development.
Sanford Health, the largest rural health system in the United States, is dedicated to transforming the health care experience and providing access to world-class health care in America’s heartland. Headquartered in Sioux Falls, South Dakota, the organization serves more than one million patients and nearly 200,000 health plan members across 250,000 square miles. The integrated health system has 45 medical centers, 2,900 physicians and advanced practice providers, 540 active clinical trials, 160 Good Samaritan Society senior living centers, and world clinics in nine countries around the globe.
Sanford Health includes:
45 medical centers
211 clinic locations
160 Good Samaritan Society senior care locations
152 skilled nursing and rehab facilities
Nearly 200,000 Sanford Health Plan members
44,000 employees
2,900 physicians and advanced practice providers and 7,944 registered nurses delivering care in more than 80 specialty areas
Centers of Excellence:
Sanford Cancer Center
Sanford Children’s
Sanford Heart
Sanford Orthopedics & Sports Medicine
Sanford Women’s
Sanford Health’s annual patient statistics for 2023:
5.8 million outpatient and clinic visits
80,880 admissions
143,217 surgeries and procedures 9,541 births
224,223 emergency department visits
Quick facts about Sanford Bismarck in 2023:
nursing staff members
Female 9% Male
Average age: 38 14,016 admissions 258,795 operation visits 37,896 emergency department visits 1,235 deliveries
Average daily census of 173.84 patients
Average length of stay (LOS) of 4.44 days
Case mix index (CMI) of 1,633
248 licensed beds (excluding three observation beds and three psychiatric seclusion rooms)
Additionally, there are 20 nursery bassinets and 28 unlicensed NICU beds




At Sanford Health, we believe quality health care should be available close to home for everyone, everywhere.
From our roots in the Midwest, we are proud to set the standard for delivering world-class care. By building on the talents, experiences and beliefs of our employees, we aim to improve the lives of patients and residents throughout the diverse communities we serve. Through our shared commitment we can become the nation’s most connected, widestreaching health care system, shrinking the distance between every patient and their best, healthiest life.



In November of 2023, Sanford Bismarck celebrated a 4th American Nurses Credentialing Center Magnet designation – an arduous feat that recognizes the high caliber of nursing professionals within the organization. Receiving this designation required a rigorous document submission that spanned over 2,400 pages and a thorough site visit that spanned two and a half days. In September of 2023, Sanford Bismarck hosted the Magnet appraisal team for an in-person site visit. The appraisal team consisted of three accomplished nursing leaders, whose soul objective was to affirm that Sanford Bismarck lived up to the high standards that Magnet demands. During the site visit, the Magnet appraisal team interviewed over 200 nurses, leaders and health care professionals and visited every inpatient unit and ambulatory area in which nursing is practiced. This scrupulous visit corroborated that Sanford Bismarck is among an elite group that provides the highest quality of care. To that end, Sanford Bismarck was recognized for four exemplars including:
• Maintaining greater than 80% of professional registered nurses who have earned a baccalaureate or higher degree in nursing.
• The unit-level data for MRSA outperformed the vendor’s national mean, median or other benchmark statistic and comparison cohort for the majority of eight quarters on 100% of the units.
• The ambulatory setting nurse-sensitive clinical indicator PERCENTAGE OF STEMI PATIENTS WITH FIRST MEDICAL CONTACT TO DEVICE IN < 90 MINUTES data outperformed the benchmark statistics for all eight quarters.
• The ambulatory setting nurse-sensitive clinical indicator ELECTRONIC CLINICAL QUALITY MEASURE (eCQM) FOR HYPERTENSION CONTROL data outperformed the benchmark statistics for the majority of eight quarters on 100% of the units.
From the Nursing Administration team, we want to extend a heartfelt “thank you” to all that participated and provided support throughout this Magnet journey. We look forward to the next.

Poor engagement, dwindling attendance and confusion regarding ambulatory’s shared governance structure marred the nursing voice in the ambulatory setting. After meetings with leadership and discussions with the ambulatory council cabinet group, it was decided that the ambulatory council needed a “reboot.” This reboot included a name change, new meeting format, a central location for agenda items and minutes, stronger leadership presence and administrative assistance.
The first step towards this reboot included a name change. This name change helped the group to clarify its role and further define its mission. The council moved to change the group’s name from Ambulatory Shared Governance to simply Ambulatory Council. This aligned with the other council names in the organization such as Night Council, Professional Management Council, Education Council and Magnet Council. This decreased confusion among staff and leadership.
The next step was modifying the platform for meetings. Previously, all meetings were held online via Webex, which was a major catalyst for decreased attendance and engagement at the meeting. Thus, the decision was made to move to in-person attendance with lunch for the council being provided. Since this change occurred, attendance, contribution and interactions within the council have increased significantly. Moreover, the council has grown and has seen representation from almost all clinics.
Lastly, a team was created in Microsoft Teams to serve as a central location for all agenda items, handouts and past-meeting minutes. Wanda Wahl, executive assistant, ensures the Teams site is up to date, provides the meeting packets, sends out the meeting invites and ensures that the cabinet is prepared to present to the council. Wanda’s contributions have increased the council’s overall efficiency. This reboot has promoted the council so significantly that ambulatory staff are willing and excited to join. Moreover, the ambulatory nursing voice has been elevated exponentially, revitalizing the essence of shared governance in all spaces of the organization.
Sanford Bismarck is committed to providing top-quality, guideline-driven care for STelevation myocardial infarction (STEMI) patients. Since 2019, Sanford Bismarck has held and maintained Chest Pain Center Accreditation through the American College of Cardiology (ACC). We have been a Platinum Award recipient in the Chest Pain –Myocardial Infarction (CP-MI) registry for five years in a row, indicating our high level of performance.
Sanford Bismarck has a dedicated STEMI and Chest Pain Coordinator, Aprille Luger, BSN, RN, CV-BC, CPHQ. Duties of this role include managing the CP-MI and CathPCI registries, maintaining Chest Pain Center Accreditation requirements, overseeing quality improvement projects and providing education and feedback to frontline staff members.
One example of how nurses have made a difference in patient care is first medical contact (FMC) to device time within 90 minutes or less for patients with STEMI. The importance of timely coronary reperfusion (performance of percutaneous coronary intervention (PCI)) is well established in the literature for patients experiencing STEMI. Sanford Bismarck outperforms the national comparative benchmark in eight out of eight quarters (100%). Nurses are critical to this measure by expediting care and transfer to the Cardiac Cath Lab, starting with early recognition of STEMI by 12-lead EKG. The goal of obtaining an EKG in under 10 minutes or less from patient arrival for patients experiencing chest pain is a continuous quality improvement project, ensuring early identification of STEMI. Once STEMI is identified via EKG from ED walk-in or EMS LifeNet system, rapid communication to the interventional cardiology physician and 24/7 on-call Cath Lab team is done through an app called Pulsara, newly implemented in 2023 to replace the paging system. In some instances where STEMI is identified by EMS, ED can be bypassed and the patient can be directly admitted to the Cath Lab to save time. Red STEMI folders containing flow sheets and check lists exist as a tool for nurses to decrease clinical variation and enhance documentation efficiency. Lastly, feedback is given to all STEMI team members from the coordinator to evaluate and identify any improvement areas.
In 2023, the Nursing Senate Retreat was held at the Bismarck State College Bavendick Room. The theme was “Finding Joy in the Journey,” and the overarching emphasis was promoting one’s own wellness, self-care and positivity in order to deliver excellent care to our patients. Attendees engaged in presentations and sessions that explored different facets of wellness – emotional, physical, financial and work-life balance. Speakers presented content that inspired attendees to seek out the good in each situation, and approach each challenge with a positive attitude to further increase chances of success and personal fulfillment. Staff in attendance also participated in chair yoga, crafts, socializing and an evening of trivia!
The afternoon working session of the retreat brought leaders and senators together in an activity, “Open Spaces,” in which all brainstormed and worked through potential content for the Nursing Strategic Plan. From these great ideas and brainstorming sessions, initiatives and tactics were developed and placed into the 2024 Bismarck Nursing Strategic Plan.



The Sanford Student Nurse Internship Program (SSNIP) is an opportunity for nursing students to have a hands-on, 10-week internship to expand their clinical skills and knowledge under the guidance of an experienced nurse preceptor. Sanford Bismarck hosted 37 nurse interns in the summer of 2023. Students were placed across 17 departments throughout the medical center and surgery clinic in Dickinson. The students came from North Dakota State University, University of Mary, University of Jamestown, Dickinson State University and University of North Dakota.
Sixteen interns extended their experience into the school year and 23 students have accepted an RN position. Sanford Bismarck currently has a 62% conversion rate and continues to connect with future graduates about RN opportunities. The Sanford Student Nurse Internship Program is a great pipeline for the organization. To that end, students enjoy the hands-on experience that strengthens their clinical skills and confidence as aspiring nurses.
Sanford Bismarck currently has 109 internationally educated nurses (IEN) working in the medical center. Onboarding began in 2022 with 20 nurses accepting offers and 100 nurses accepting offers in 2023. Sanford Bismarck plans to continue international recruitment well into 2025 to support the medical center and, in the future, the clinics. Onboarding our IENs is rigorous – nurses learn the same information as any other nurse coming to work for Sanford Health, but also much more. The official areas that we focus on are health care in the U.S., nursing practice, communication, computer application, HIPPA, nurse-sensitive indicators, physical assessment, medication administration, IV skills, benefits and insurance information, and general skills. These areas help verify that when they get to the floor, their nursing skills are sharp and ready to meet the expectations of work in this location.
I particularly enjoy a section of teaching that presents typical slang and sayings that IENs may hear, and they guess the meanings. For example, to “bite the bullet,” or “it’s raining cats and dogs.” They always have wonderful guesses. All this information gets covered before they start on the floors.
To help continue their growth as nurses and in community integration, we offer monthly fellowships that last for six months. At these fellowships, we cover the transition to practice, communication and patient education, health care and patient outcomes in the U.S., the culture of safety and respect, ethical awareness and moral distress, bedside leadership and professional development. In each fellowship, we also address personal physical, spiritual and social health. Although we cover some great information, a fair amount of time is spent talking and storytelling to not only help talk through issues but also so IENs can share tips and tricks. The very best part is when we have potlucks and get to sample food from their homelands. We have a great time strengthening the bonds between the IENs and the educators at the lead.

On September 29, 2023, 35 inpatient educators, leaders and LEAD Center team members came together to learn, network and have fun at the Bismarck Educator Retreat. The purpose of this retreat was to support education across the continuum using SAFE relationship and reliability skills. It was a forum to share best practices, increase information sharing and gain mutual understanding of each other’s work and purpose while creating shared accountability for addressing gaps in practice and performance.
Both Clinical Learning and Development/Unit educators and the LEAD Center shared an overview of clinical orientation and skill development on the unit. The result was a greater understanding of purpose, process and best practices. The group participated in a professional development session focused on unleashing our team’s potential through coaching. Finally, the knowledge gained from the retreat was used to complete a “Start-Stop-Continue” closing activity. During this culminating work, the group identified next steps that will lead to new opportunities and improved experiences (Start), activities that no longer add value (Stop) and best practices that should be repeated (Continue).
A comparison of the pre- and post-retreat surveys demonstrated an overall increase in confidence with an anticipated positive impact on educator knowledge, competency and performance.
Action was set in motion to complete the identified next steps. One of the most significant deliverables was the creation of a guiding principles document that can be used to guide the identification of learning needs and planning for skill-based nursing
The concept of a Behavioral Emergency Response Team (BERT) is not new to health care, nor to Sanford Health. BERT teams have been successfully implemented throughout numerous health care settings including other Sanford facilities. Literature actively supports the creation and implementation of BERT-like teams/resources to support not only behavioral health in the medical setting, but also support workplace violence prevention through helping patients and staff work through escalating stress and the tensions people face during medical and acute crises. For this reason, a workgroup of risk management, security and behavioral health professionals created the BERT Team in Bismarck with a go-live in September 2023.
For a successful implementation and maintenance of a BERT program, resources, workflows and education all had to align prior to go-live. The BERT work group focused on addressing real world concerns from our core providers, nurses and CNAs who work on the units and deal with workplace violence and high-stress patients. After viewing literature and workflows from other locations, the BERT work group felt something critical was missing. The other locations/workflows that were reviewed followed a one-and-done BERT approach, meaning the BERT team would only interact with the patient upon the initial BERT call. Our team believed that true behavioral change, clinical support and therapeutic coping skills are not learned in one session, so we created our workflow with a deviation from others. It’s also important to note that clinical staff are not consistent and change shift-to-shift and day-to-day – so what does it look like for BERT to be as fluid as staffing?
To address those concerns, we created our core BERT response to include a minimum of two visits – the initial call and a minimum of one follow-up the next shift. After four months of data collection, we have an average follow-up of seven visits per BERT call. This allows the rounding BERT Nurse & Security Team member to provide continual support across shifts, days and fluctuations in the patient’s mood/circumstances throughout the day. Following up gave the BERT team the ability to reinforce behavior expectations and provide therapeutic support to not only the patient, but the variable staff caring for them. In four months, we have had 72 initial BERT calls and 325 followup visits. We see a balance of calls between the day and night shifts, but the highest call volume comes at the afternoon/evening shift change hour. The BERT team has brought additional support and resources directly to the clinical team members and nurses throughout the hospital. With the elevated focus of patient-centered care, therapeutic relationship building and therapeutic boundary setting, we have seen a four-month decline in workplace violence events on our inpatient units!
Staff working in a critical care setting are frequently exposed to episodes of stressful and potentially traumatic events. All too often, when these events are over, nurses and other team members are left with little to no physical, mental or emotional support. There was an apparent need to foster an environment that supported knowledge sharing and improved teamwork during and, particularly, after these events. A literature search centered on clinical post-event debriefing provided the background information used to develop the 2023 ICU Performance Improvement Project. A hot debrief is conducted shortly after the events occur and all involved staff have the opportunity to participate and provide feedback. The goal of implementing hot debriefs is to strengthen support and relationships for all team members, increase knowledge sharing, decrease compassion fatigue and improve code blue efficiencies. The Sanford Bismarck ICU team began conducting hot debriefs in March of 2023.
Implementing hot debriefs showed improvements in communication and role identification during code blues, particularly for recorder roles, streamlined code blue workflows and staff support. The ICU has advanced patient-centered care with more efficient codes and decreased adverse events through education and open discussion during hot debriefs. The ICU team members have gained pillars of confidence, unity and honesty, along with a culture of continuous transformation through embracing each other as humans and recognizing the need to support individual and team growth.


The DAISY Award is an international program that rewards and celebrates the extraordinary clinical skill and compassionate care given by nurses every day. Patients, visitors, families, volunteers and all employees may nominate a deserving nurse.







 Dickinson Same Day Surgery
Dawn Huber, BSN, RN
Olivia Holly, BSN, RN
Whitney Leingang, BSN, RN
Kyla Schock, BSN, RN
Sandee Padilla, BSN, RN
Talyssa Carufel, BSN, RN
Kat Teske, LPN
Dickinson Same Day Surgery
Dawn Huber, BSN, RN
Olivia Holly, BSN, RN
Whitney Leingang, BSN, RN
Kyla Schock, BSN, RN
Sandee Padilla, BSN, RN
Talyssa Carufel, BSN, RN
Kat Teske, LPN





Kim Ledger, BSN, RN, CNOR, CRNFA
Distinguished Wisdom Keeper

Connie Aberle, PCT Friend of Nursing

Breanna Meckle, BSN, RN Structural Empowerment

Social Work Department Friends of Nursing (Team Award)

Emily Smith, DNP, RN, CNE Exemplary Professional Practice

Michael Quast, MD Friend of Nursing

Robin Bowlinger, MSN, RN, CPHQ Structural Empowerment

Cheryl Page, BSN, RN
Jan Kamphuis Spirit of Nursing

Naomi Schmidt, BSN, RN Florence Nightingale Award

Alex Gatt, MSN, RN
New Knowledge, Innovation and Improvements Award

Shauna Voigt, MSN, RN Structural Empowerment

Ron Montgomery, LPN Florence Nightingale Award

Whitney Leingang, BSN, RN STAR Performance
COVID-19 and the Current State of RN
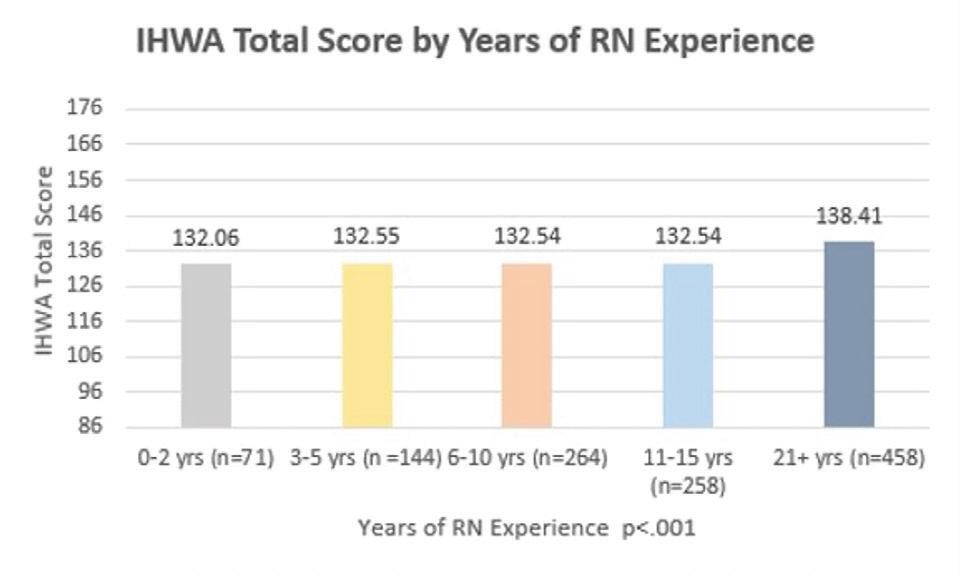
Written by: Emily Smith, DNP, RNThe past three years have been extremely stressful for nurses working in COVID-19 environments, having an emotional impact on nurses’ health, well-being and overall wellness. In a recent study, 19 frontline nurses in the Upper Midwest described feelings of being overwhelmed, role frustration related to the chaos in the care environment, and abandonment by their leaders, families and communities. An enterprise nursing research team including Bismarck representatives Marth Stow, ASN, RN; Nick Hillman, MSN, RN; and Emily Smith, DNP, RN, CNE, came together to explore the topic of nursing wellness. Extensive review of COVID-19 pandemic literature revealed a gap in describing the RNs’ experience with wellness. To fill the gap, the enterprise research team implemented a mixed methods research study.
The research questions included:
1. What is the wellness level of RNs working in rural America inpatient and outpatient settings?
2. What are the current barriers these Upper Midwest RNs are experiencing to maintain or enhance their wellness?
3. What interventions are recommended by these RNs to promote wellness in the workplace?
The mixed methods research study included two phases. Phase one was the quantitative part of the study with a non-experimental descriptive survey design. Phase two includes a qualitative design using focus groups to understand the lived experiences of the participants. The research study received full approval from the Sanford Institutional Review Board.
Phase one was implemented in April 2023 in the four regional tertiary medication centers in the Upper Midwest. A valid survey titled Integrative Health and Wellness Assessment (IHWA V2 2022) with a 36-item tool was given to all frontline RNs, advanced practice nurses and supervisors/managers/directors. Eligibility criteria included consenting RNs of any age, gender, race or ethnic group, and employed by Sanford Health. Travel nurses, agency/contract nurses and current extended leave of absence nurses were excluded. The survey also included demographic information and additional questions addressing barriers to maintaining wellness and recommendations to promote wellness in the work setting. Phase two started in December 2023 and will continue into 2024.
Results: Identified Barriers to Wellness included:
1,429 (20.4%) RNs completed all items on the IHWA V2 2022



Not enough time
Busy home and work life, inadequate breaks, exhaustion
Work environment
Negative, unrealistic expectations, lack of support, short-staffed, stressful, unhealthy food options
Family responsibilities
Marriage, children, caregiving, guilt prioritizing family before work
Emotional concerns
Hopelessness, guilt prioritizing self, feeling like a number
Accessing resources
Limited gym/fitness access dependent on locations and shift work
Finances
Cost of living, gym/fitness membership fees, health care expenses
Underlying health issues
Anxiety, PTSD, chronic illness, weight concerns, chronic stress
The results helped to form the questions for the qualitative portion of the study. Next steps include six focus groups to include cohorts of clinical RNs, advanced practice nurses and supervisors/ managers/directors in tertiary care and critical access/rural hospitals – these will be convened virtually to better understand the RNs’ experiences with wellness in their professional and personal life. Additionally, the results are a resource for nursing leaders within Sanford Health to help inform future interventions that may be helpful to impact RN wellness.
CEA Healthcare’s Apollo is the newest simulator at the Sanford Simulation Center in Bismarck. Apollo is a high-fidelity, tetherless and fully wireless adult patient simulator with modeled physiology to allow for more realistic patient behavior with responses to real time interventions. When using high-fidelity patient simulators, Apollo sets the standard for reliability, quality and value in health care education.
A large portion of use for Apollo is for code blue and emergency response simulations and education. As shown in the 2023 data, many staff participated in a code blue/ emergency response simulation. With the continued use of Apollo and other high-fidelity simulators for ongoing education, we can prevent errors, improve performance and enhance patient care.




Apollo is the newest simulator at the Bismarck Sanford Simulation Center. CAEs Apollo is a high-fidelity, tetherless and fully wireless adult patient simulator with modeled physiology to allow for more realistic patient behavior and responses to real time interventions. Apollo sets the standard for reliability, quality and value in healthcare education using high fidelity patient simulators. Apollo has many features and benefits, below are just a few to mention.
Airway (assess & manage airway
• Bag-valve-mask ventilation
• Head tilt/chin lift & Jaw thrust
• Tongue swelling
• Bronchial occluder
• Surgical cricothyrotomy
• Needle cricothyrotomy
• Laryngeal mask airways
Neurological
• Blinking and reactive pupils with multiple setting
• Seizures
Circulation (assess and manage perfusion status)
• Defibrillation and cardioversion using live defibrillators.
• Pacing
• 12-lead dynamic ECG display ECG monitoring posts and interface with real ECG monitor
• Adequate chest compressions result in simulated circulation, cardiac output, central and peripheral blood pressures, carbon dioxide return
• Hand-placement detection
Respiratory (assess and manage breathing)
• Intubation: orotracheal, nasotracheal, retrograde, fiber optic
• Mainstem intubation detection
• Gastric distention with esophageal intubation
• Laryngospasm Airway occluder
• Bilateral needle decompression and chest tube insertion

As a group (nursing manager, dietitian and diabetes educators), we identified a concern at one of our monthly meetings. We noted that many patients did not see a diabetic educator. We also noted that many patients were having therapy adjustments because of Hemoglobin A1C% (HA1C%) values alone. This raised huge safety concerns for our patients. To see the full picture of the diabetic patient’s needs, all glucose levels must be reviewed. A great example is a patient with an HA1C% of 8% would automatically get a basal insulin increase recommendation from a provider to help bring the HA1C% down. Often, when these patients get a continuous glucose sensor trial, there are low blood sugars overnight or at other times of the day, and their insulin dose has just been increased based only on their HA1C%. This is not the best management for our diabetic patients.
The American Diabetes Associate (ADA) “Standards of Medical Care in Diabetes” current clinical practice guideline recommends patients should self-monitor glucose levels to help providers properly assess the effectiveness and safety of a management plan. Evidencebased practice recommendations have included self-monitoring of blood glucose (SMBG) as a key component to overall diabetes management. SMBG is a useful tool for guiding medication interventions, nutrition therapy, physical activity, hypoglycemia prevention and medication adjustments (particularly insulin doses). There is a direct correlation between greater SMBG frequency and lower HA1C% values.
Our goal was to encourage providers to request their patients to ALWAYS bring their diabetic devices (glucose meter, sensor, insulin pump, etc.) to their diabetic follow-up appointments to have the device uploaded for review. We implemented the nursing staff’s assistance with contacting patients before clinic appointments to remind them to bring their devices to their upcoming appointment. Additionally, we recently trained a CNA in our diabetes department to specifically help with diabetes device uploads. After implementation, we saw an increase in provider, diabetes educator and patient interaction regarding diabetes care management for our patients. We provided a much more individualized plan of care for each patient when reviewing their blood sugars with them at a follow-up appointment. This project impacted our patients immediately with a noted 3.6% decrease in overall HA1C% over a three-month period. Our main goal was to provide better diabetes management to our diabetic patients. Our patients commented that they felt “valued and cared for.” We are so thankful for all the assistance with getting this implemented at our clinics and we cannot wait to see continued progress for our patients.


Written by: Nick Hillman, MSN, RN, Manager of Quality and Safety, and Jess Leibel, BSN, RN, Director of Quality and Safety
On November 7, Sanford Bismarck held their annual Performance Improvement Symposium at the Radisson Hotel Bismarck. The event’s purpose is to showcase quality and performance improvement in various areas of our regional footprint. This year Sanford Bismarck reached a record of 71 posters submitted. Additionally, attendees were treated to various guest speakers, highlighting and showcasing the importance of quality health care in our region.
Below are the event’s winning individuals and teams: Clinical Care
1st – Dear Depression, Not Today (Bismarck Internal Med) – Heather Weaver, MS, RN 2nd – Feeling Blue? Let us help you (Dickinson Oncology) – Anne Berguin, BSN, RN/ Kahla Giese, BSN, RN
3rd – Caring for Catheters (4NE) – Renata Hegle, BSN, RN
Evidence-Based Practice
1st – The Future is NOWS: Improving Outcomes for Infants with Neonatal Opioid Withdrawal Syndrome – Danielle Thurtle, MD 2nd – Tubed and Lubed (NICU) – Sydney Pexa, BSN, RN/Taylor Privrafsky, BSN, RN/ Madison Johnson, BSN, RN
Sanford Experience
1st – Put Some P.E.P. in Your Step (Patient Experience) – Mikayla Atchison 2nd – Get Engaged, Asking the Right Questions to Improve the Patient Care Experience (Outpatient PT) – Bruce Belland
Communication
1st – Let’s Rock This Joint (Orthopedics) – Kalcey Schneider, BSN, RN/Gina Pich, ADN, RN 1st – It’s My Code and I’ll Cry if I Want To (ICU) – Kimberly Stearns, MSN, RN
2nd – A Selfie a Shift Keeps the Rift Raft Amiss (2SE) – Kimberly Stearns, MSN, RN
Safety
1st – Let’s “Connect 4.” Improved Patient Safety and Satisfaction (4SE) –Natalie Pape, BSN, RN
2nd – Who Sent the Cord Blood Down? A Mislabeled Lab Specimen Quality Improvement Project (Birth Center) – Natasha Hildebrand, BSN, RN
Quality of Life
Baby’s Next Steps (Care Management) – Kayla Roberson, BSN, RN
Cost
1st – Taking a Bite Out of Sepsis (CDI) – Lois Mosbrucker, ADN, RN
2nd – Reducing Length of Stay (LOS) for Metabolic and Bariatric Surgical (MBS) (Bariatric Surgery) – Alicia Huizenga, BSN, RN
