36 School of Nursing 1st awarded associate member status of United Nations NGO 20 Care Corner provides space designed to support student success 13 Addressing suicide risk among ethno-racially minoritized youth CULTIVATING RESILIENCE IN NURSING STUDENTS AACN awards pilot grant to foster leadership, wellbeing NURSING MINNESOTA A publication of the University of Minnesota School of Nursing SPRING/SUMMER 2023
07 New research uncovers how pandemic affected Black, American Indian women experiencing violence
Mkandawire-Valhmu’s research focuses on those with greatest vulnerability, greatest difficulty accessing health care
ON THE COVER
16
Cultivating resilience in nursing students
AACN awards pilot grant to foster leadership, wellbeing




22
‘Every day, we’re here for patients’
Raines, VP and CNO for M Health Fairview U of M Medical Center, adds DNP to her resume


38 An advocate for patients and the profession
As the nurse-midwifery program celebrates 50 years, alum Futrell Carter says the profession is where she's meant to be

www.facebook.com/umnnursing www.twitter.com/umnnursing
www.instagram.com/umnnursing
www.linkedin.com/school/umnnursing www.youtube.com/user/umnnursing

Read Minnesota Nursing online at www.nursing.umn.edu/magazine
To receive a notice when the current issue is posted on the school’s website, send an email to nursenews@umn.edu.
This publication is available in alternative formats upon request. Direct requests to the managing editor at nursenews@umn.edu.
The University of Minnesota is committed to the policy that all persons shall have equal access to its programs, facilities, and employment without regard to race, color, creed, religion, national origin, sex, age, marital status, disability, public assistance, veteran status, or sexual orientation.
The University of Minnesota is an equal opportunity educator and employer.
2 | MINNESOTA NURSING 38 22 07 SPRING/SUMMER 2023
SECTIONS 04 From the Dean 07 Research 16 Education 36 Outreach 44 School News 54 Alumni News FOLLOW US
UNIVERSITY OF MINNESOTA SCHOOL OF NURSING
OUR VISION
Optimal health and wellbeing for all people and the planet.
OUR MISSION
To generate knowledge and educate diverse leaders to shape the future of nursing and advance equitable health care to improve the health and wellbeing of all.
DEAN
Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP
SENIOR EXECUTIVE ASSOCIATE DEAN FOR ACADEMIC PROGRAMS
Christine Mueller, PhD, RN, FAAN, FGSA
ASSOCIATE DEAN FOR RESEARCH
Diane Treat-Jacobson, PhD, RN, FAAN
ASSOCIATE DEAN FOR FACULTY AFFAIRS
Wendy Looman, PhD, APRN, CPNP-PC
COOPERATIVE CHAIRS
Donna Bliss, PhD, RN, FAAN, FGSA
Wendy Looman, PhD, APRN, CPNP-PC
Jenna Marquard, PhD
DEAN'S NATIONAL BOARD OF VISITORS
David Aanonson, pastor (ret.); Clara Adams-Ender, chief nurse executive, Army Nurse Corp. (ret.); Cyrus Batheja, National Medicaid Vice President - Policy and Clinical Solutions UnitedHealthcare Community & State; Jeannine Bayard, United Health Group (ret.); Michael Bird, past president, American Public Health Association; Shonda Craft, dean, School of Health and Human Services, St. Cloud State University; Jessica Drecktrah, chief nursing officer, Faith Community Nurse Network; Melanie Dreher, dean emeritus, Rush University College of Nursing; Peter Klein, CEO, Educated Change; Rahul Koranne, CEO, Minnesota Hospital Association; Richard Norling, senior fellow, Institute for Healthcare Improvement; Laura Reed, chief nurse executive and COO, M Health Fairview; Jeannine Rivet, executive vice president, UnitedHealth Group (ret.); Michael Rohovsky, Associate Corporate Office of Science & Technology, Johnson & Johnson, (ret); Franklin Shaffer, president and chief executive officer, CGFNS, (ret.); Jessica Sylvester, nursing executive and chief executive officer, Call Light Health; Dee Thibodeau, senior executive in information technology; Sylvia Trent-Adams, president, The University of North Texas Health Science Center at Fort Worth; Charlotte Weaver, former senior vice president and chief clinical officer, Gentiva Home Health & Hospice; Cathleen Wheatley, president, Atrium Health Wake Forest Baptist Medical Center and senior vice president of clinical operations; and Jonathan M. Zenilman, chief, Infectious Diseases Division, Johns Hopkins Bayview Medical Center and professor at Johns Hopkins University School of Medicine
DIRECTOR OF STRATEGIC COMMUNICATIONS
Steve Rudolph
SENIOR EDITOR
Brett Stursa
PHOTOGRAPHERS
Darin Kamnetz, Tom Steffes, Scott Streble
DESIGNER
Tammy Rose
CONTACT US
Minnesota Nursing
University of Minnesota School of Nursing
5-140 Weaver-Densford Hall
308 Harvard Street S.E.
Minneapolis, MN 55455
Email: nursenews@umn.edu
Website: www.nursing.umn.edu
Minnesota Nursing is published semi-annually by the University of Minnesota School of Nursing for alumni, faculty, students and friends of the school.
©2023 Regents of the University of Minnesota. All rights reserved.
Desmond discusses Poverty, by America
The School of Nursing hosted Matthew Desmond, the Pulitzer Prize-winning, bestselling author of Evicted: Poverty and Profit in the American City, to discuss his latest book Poverty, by America at an event in April at Northrop. In his new book, which debuted at #1 on the New York Times Best Sellers list, he reimagines the debate on poverty, making the argument about why it persists in America: because the rest of us benefit from it.

www.nursing.umn.edu | 3
Photo: Darin Kamnetz
FROM THE DEAN
Nursing impact — from local to global
Dear Friends,
A phrase you’ll often hear at the School of Nursing when we’re discussing our intended impact is “from local to global.” This spring/summer issue of Minnesota Nursing magazine magnificently captures examples of the many ways our students, staff, faculty and alumni are engaged in our own backyard, such as the mentoring program with middle- and high-school students in Columbia Heights showcased in Partnering for Health. This issue also shares the news of the Katharine J. Densford International Center for Nursing Leadership becoming the first school of nursing in the world to be awarded associate member status in the Conference of Non-Governmental Organizations in Consultative Relationship with the United Nations.
We share the research of two recently hired, remarkable professors. Professor Lucy Mkandawire-Valhmu, PhD, RN, FAAN, studies how the pandemic affected Black and American Indian women who were experiencing intimate partner violence. Another feature in the research section introduces Professor Jenna Marquard, PhD, the Cora Meidl Siehl Chair in Nursing Research for Improved Patient Care, who is leading the effort to bring nursing and engineering together to improve health outcomes.
Our cover story focuses on the school’s efforts to cultivate resilience in nursing students. The University of Minnesota
was one of 10 schools nationwide that received a pilot grant from the American Association of Colleges of Nursing to develop a competency-based approach to leadership development and resilience for nursing students. In subsequent pages we share how our Office of Student and Career Advancement Services is implementing innovations to provide students support for their success.
This year, 2023, marks the 50th anniversary of our nurse-midwifery program. What was first established as an option within the master’s degree program would become the first Doctor of Nursing Practice program in the country to be approved in 2009. In this issue we profile one of the countless alums who is making an impact in the field, Sakeena Futrell Carter.
We appreciate your readership and support and welcome your reflections, suggestions and shared wisdom in advancing our school, nursing and health.

In gratitude,
Connie White Delaney Professor and Dean

4 | MINNESOTA NURSING
PARTNERING FOR HEALTH
Mentoring program with Columbia Heights schools focuses on wellbeing
The School of Public Health and School of Nursing joined with Columbia Heights Public School District to improve the health of middle- and high-school students while providing college students with experiential learning opportunities.

The program, called DiscoverU, is funded with $800,000 from the Centers for Disease Control and Prevention as part of its Whole School, Whole Community, Whole Child framework, which seeks more collaboration among education leaders and health sectors.
“This mutually beneficial partnership between Columbia Heights Public Schools and two schools at the University of Minnesota is a great example of how community-engaged research can tackle real-world challenges and improve overall health and wellbeing of adolescents within our local community,” says School of Nursing Associate Professor Barb McMorris, PhD, the grant’s co-principal investigator.
The goal of DiscoverU is to integrate social-emotional learning, physical activity and nutrition into an out-ofschool program. Social-emotional learning includes working on self-awareness, social skills, self-management, relationship skills and responsible decision-making.
GOOD TIMING
The program comes at a time when school districts need it most, says School
continued on page 6
www.nursing.umn.edu | 5
School of Public Health Assistant Professor Katie Arlinghaus, right, and School of Nursing Associate Professor Barb McMorris, center, lead the grant that funds DiscoverU. SPH student Mary Onchiri, left, coordinates the program.
of Public Health Assistant Professor Katie Arlinghaus, PhD, the grant’s co-principal investigator.
“Kids’ emotional and mental health is at high risk coming out of the pandemic, and there’s a great need for this program,” says Arlinghaus. “We’re seeing a lot more violence, stress, rates of anxiety, depression, and suicide ideation, as well as declines in a lot of physical health markers, including a significant increase in Type 2 diabetes.”
Arlinghaus says that as schools struggle with resources and families are unable to participate in separate programs, DiscoverU has the practical effect of being more efficient and supportive by simultaneously addressing all aspects of health.
Kristen Stuenkel, MEd, director of community education and communications with Columbia Heights Public School District (CHPS), co-created DiscoverU with Arlinghaus and says that CHPS is a perfect fit for the program. It’s a relatively small school district with 3,400 students, and it is also racially, ethnically and socioeconomically diverse. More than 33% of students are English learners and 70% qualify for free or reduced lunch.
“Many people within those demographic characteristics have higher risks for health disparities,” she says. These disparities are often systemic, and tied to racism and other social determinants of health.
DiscoverU is designed for communities with concentrated poverty for whom health and educational programming is often less accessible and who typically carry a disproportionate health burden.
DISCOVERING THE MENTOR WITHIN
DiscoverU uses a tiered mentoring system where undergraduate students, most from the University of Minnesota, are trained to mentor high-school students, who in turn mentor middleschool students.

The program runs after school two days per week for 16 weeks. Initially, college mentors meet with middle- and highschool students separately. After the highschool students gain some mentoring skills, the middle-school students join them, says Mary Onchiri, DiscoverU project coordinator and School of Public student. During each session, students participate in at least two physical activities, ranging from weightlifting to a popular game called Gaga ball. CHPS also has a robust school garden, which has allowed students to learn from mentors about nutrition firsthand and to have an opportunity to make their own snacks and pickle vegetables.
Students take part in large and small group discussions and talk about what Onchiri calls “big feelings” and how to handle them. They set health goals and identify their core values, such as family, respect, honesty or faith. They also talk about challenges that they've run into, how to overcome those, and how to navigate conflict and cope with stressful situations. “We are giving them skills on the front end to hopefully set them up for a healthier
life in the future, not just physically, but also emotionally,” says Onchiri.
As the college and high school mentors model these skills and behaviors, the younger students develop a greater understanding of their importance for their overall health and future success.
“Students really enjoy hearing what the college students have to say,” says Stuenkel. “It’s more fun for them than just engaging with other adults, because college students are kind of in between adults and high school students, so they serve as a bridge to adulthood.”
DiscoverU began in the spring of 2022, and the most recent iteration ended in March 2023.
“Kids are facing a lot right now in schools,” says Arlinghaus. “And so, having programs like this where they feel that they belong and are safe is really important.”
PARTNERING FOR HEALTH is a recurring feature that highlights a school partnership working to advance health care to improve the health and wellbeing of all.
6 | MINNESOTA NURSING
DiscoverU Columbia Heights students and their mentors.
continued from page 5
NEW RESEARCH UNCOVERS HOW PANDEMIC AFFECTED BLACK, AMERICAN INDIAN WOMEN EXPERIENCING VIOLENCE

Mkandawire-Valhmu’s research focuses on those with greatest vulnerability, greatest difficulty accessing health care
by Brett Stursa
Lucy Mkandawire-Valhmu says that because nurses are so trusted as a profession they have an opportunity to significantly address violence in women’s lives.
www.nursing.umn.edu | 7
RESEARCH
continued on page 8
Photo: Darin Kamnetz
Prior to the COVID pandemic, Black and American Indian/Alaska Native (AI/AN) women disproportionately experienced intimate partner violence while at the same time experienced some of the greatest difficulty accessing the health care system.
With the pandemic’s social distancing, quarantines and isolation measures, researchers at the University of Minnesota are seeking to understand how the pandemic affected Black and AI women who were experiencing intimate partner violence.
“With the ongoing COVID-19 pandemic, help-seeking for American Indian and Black women has become even more complicated amidst a global concern among advocates that social distancing, quarantine and isolation measures are inadvertently endangering women experiencing intimate partner violence,” says Professor Lucy Mkandawire-Valhmu, PhD, RN, FAAN, who was awarded a National Institute on Minority Health and Health Disparities grant to study the issue. “To our knowledge, while anecdotal evidence shows that the COVID-19 pandemic has complicated women’s experiences of violence with a possible rise in levels of violence resulting in lethal outcomes, no systematic studies exist that track women’s experiences of intimate partner violence during this pandemic.”
Mkandawire-Valhmu is partnering with University of Wisconsin Assistant Professor Jeneile Luebke, PhD, RN, an enrolled member of the Bad River Band of Lake Superior Chippewa Indians, to better understand women’s experiences during the pandemic.

Mkandawire-Valhmu and Luebke are conducting a community-engaged research study informed by Indigenous and Black feminist thought that includes both qualitative and quantitative methods. Ultimately, they will systematically describe the unique and intersecting structural, economic and interpersonal facilitators and barriers to help-seeking for intimate partner violence among AI and Black women in Wisconsin during the COVID-19 pandemic. Additionally, Mkandawire-Valhmu recently applied for a supplement to also include the experiences of Black and AI women in Minnesota. They are conducting two waves of surveys with a total of 600 AI and Black women, and individual and focus group interviews with a total of 300 AI and Black women to track women’s experiences, patterns of help-seeking and barriers to help-seeking.
“Our ultimate goal through this study is to create a platform where women’s voices can then inform health practice and health policy while also drawing from a community advisory board constituted of advocates and other key members of AI and Black communities in Wisconsin to provide actionable recommendations for addressing the urgent problem of intimate partner violence in the lives of AI and Black women,” says Mkandawire-Valhmu.
MKANDAWIRE-VALHMU MOVES MINNESOTA TO BROADEN RESEARCH IMPACT
Mkandawire-Valhmu came to the University of Minnesota in 2022 because she wanted to broaden the impact of her research. “Minnesota is a central location for
8 | MINNESOTA NURSING
Lucy Mkandawire-Valhmu with colleagues at Lac Courtes Oreilles.
research I hope to conduct in the Dakotas, as well as Minnesota and Wisconsin. I am eager to contribute to the health of women in Minnesota,” says MkandawireValhmu. “The experiences of Black women in Minnesota are a little different than the ones of where I was in Wisconsin, so I hope to understand the differences in women’s experiences and what we can learn across those differences.”
Already, Mkandawire-Valhmu was awarded a University of Minnesota Sustainable Development Goals research grant for Achieving gender equality for women experiencing the deepest vulnerability: A focus on gender based violence in the lives of childbearing refugee women in Dzaleka refugee camp, Malawi.
She is partnering with Associate Professor Sarah Hoffman, PhD, MPH, RN, on a mixed methods study that will provide foundational knowledge about the experiences of gender based violence in the lives of childbearing women living at Dzaleka refugee camp in Malawi.
“I want to continue to work with women who experience the greatest vulnerability,” says Mkandawire-Valhmu.
GREATEST VULNERABILITY, GREATEST DIFFICULTY ACCESSING HEALTH CARE
Early on in Mkandawire-Valhmu’s nursing career, when she was earning her first nursing degree living in Malawi in southeast Africa, she observed how women were
affected by violence. “I really wanted to understand that and determine as a nurse how I could contribute to addressing their experiences of violence so that they could live healthier lives and they could contribute more meaningfully without the burden of the experiences of violence,” says Mkandawire-Valhmu.
As she earned a PhD – her dissertation focused specifically on violence in the lives of women who work as domestic workers in other people’s homes — and after moving to the United States, she has developed a research portfolio that has deepened the understanding.
“I’ve developed an expertise with women who experience the greatest vulnerability and have the greatest difficulty accessing the health care system,” says MkandawireValhmu.
With that in mind, and with her nurse’s sensibility, she strives to make recommendations that are realistic, practical and efficient within the health care system.
“For me, it’s important that nurses are more aware,” says Mkandawire-Valhmu. “Nurses are considered a trusted profession, so we have an opportunity to significantly address violence in women’s lives.”
www.nursing.umn.edu | 9
• • •
“ The experiences of Black women in Minnesota are a little different than the ones of where I was in Wisconsin, so I hope to understand the differences in women’s experiences and what we can learn across those differences.”
– Lucy Mkandawire-Valhmu, PhD, RN, FAAN

10 | MINNESOTA NURSING
Jenna Marquard is working at the intersection of engineering and nursing to improve health outcomes.
Photo: Darin Kamnetz
A FRUITFUL ALLIANCE
Marquard aims to advance patient care through nurse-engineer collaboration
by Susan Maas
With her background in engineering and her understanding of a nurse’s sensibility, Jenna Marquard, PhD, is a rare breed.
But she shouldn’t be, she believes, and she’s working to make nurse-engineer partnerships more common—and seamless—than they currently are. Marquard, who joined the nursing school faculty in 2021, is featured in the March issue of American Journal of Nursing, along with a handful of colleagues who are at the intersection of engineering and nursing. They’re leading a movement toward bringing these two professions together to enhance patient care and health outcomes. Her master’s degree and her PhD, both from the University of Wisconsin-Madison, are in industrial and systems engineering. “My specialty is human factors engineering. Basically, the premise is that anytime you’re engineering a product or technology or system, there are people who will be using it,” Marquard explains. “So you need to be thinking about who those end users are, what they want to do, and the context where they will be using what you are designing.”
She came to the U from the University of Massachusetts Amherst, where she helped lay groundwork for the institution’s new Center for Nursing and Engineering Innovation. Marquard quotes one of her colleagues, who now codirects that center, as observing that “nurses are the biggest users of technology in health care, and they’re mostly left out of the conversation.” Her mission is to change that.
COMPLEMENTARY STRENGTHS
“Engineers are hard workers. They are ingenious. But they don’t always start with the problem,” Marquard says. “And nurses are so focused on the difficult work that they’re doing, they don’t always even know or have time to wonder if it’s possible to do something differently.”
Marquard, who knew about the U of M nursing school’s nursing informatics group from conferences and their research track record, says she reached out to Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP, and faculty to gauge interest in having an engineer on faculty. “They see things out of the box,” she says.
Her interest in health care goes back decades. Her field, often referred to as nursing informatics, is built on the supposition that “we can use data and information
continued on page 12
www.nursing.umn.edu | 11
to help empower people to make better decisions or carry out healthier behaviors,” Marquard says. “We have access to a huge amount of data right now. That can really be beneficial” — both to patients and to the professionals caring for them — "if it’s analyzed and displayed to the end users in thoughtful ways.”
And most patients’ knowledge about their own health and habits could be deployed to their advantage, but often isn’t. “Patients have so much information and data about themselves that’s not making it into the clinical conversation,” Marquard says. “The information you have about yourself and your health is as important as the single blood pressure reading they take at the clinic; it tells a story about you.”
NURSES ARE KEY TO PROBLEM SOLVING
Marquard has engaged with nurses to help improve sleep and decrease fatigue in patients with chronic illness. She’s also studied the use of eye-tracking technology to understand how nurses obtain information from electronic health record notes, detect patient identification errors and execute clinical workflows.
And she recently focused on a project with individuals who have HIV and AIDS, the essence of which was “trying to help them track their medication-taking. And trying to figure out ways to do that unobtrusively”— because the tools and systems she develops must be seamless to be used. Implementing enhancements in care cannot involve further burdening nurses or their patients, she says. “Just having more data isn’t helpful. You need to figure out how to distill it and display it in ways that are understandable and actionable,” she says.
Marquard relishes opportunities to foster and participate in collaborative relationships, beyond nurses and engineers to include physicians, neuropsychologists, computer scientists, mathematicians and others. She’s excited to build more models for such collaboration.
“And I want to figure out some creative ways to bring more students into our courses from outside of nursing,” she says. “Even more than research, I would say that’s my lifelong passion: to get engineering and nursing schools to talk to each other more.”
The Twin Cities native, who enjoys running, biking and cross-country skiing with her husband and three sons, is excited to be back in Minnesota. And she’s thrilled to be in the University of Minnesota School of Nursing. “It was clear that this was going to be a really great place to work, a place where I could be highly productive. I felt I could contribute in some pretty significant ways,” Marquard says. “It’s going to be good.”
12 | MINNESOTA NURSING • • •
“
The information you have about yourself and your health is as important as the single blood pressure reading they take at the clinic; it tells a story about you.”
– Jenna Marquard
ADDRESSING SUICIDE RISK AMONG ETHNO-RACIALLY MINORITIZED YOUTH
HRSA grant supports research to identify risk, protective factors
by Brett Stursa
Eunice Areba, Michelle Mathiason Moore, Patricia Jewett and Iris Borowsky.

www.nursing.umn.edu | 13
continued on page 14
Photo: Tom Steffes
With current data suggesting otherwise, researchers from the University of Minnesota are seeking to understand risk and protective factors associated with repetitive non-suicidal self-injury, suicidal ideation and suicidal behaviors among adolescents, with a focus on ethno-racially minoritized youth.
Clinical Assistant Professor Eunice Areba, PhD, RN, PHN, is leading an interprofessional team of researchers that was awarded funding from the Health Resources and Services Administration (HRSA) for their project, Centering the Margins: Addressing Suicide Risks among Ethno-Racial Minority Adolescents.
“The findings from the 2019 study are concerning, so we are trying to find out why,” says Areba. “Our longterm goal is to identify the role of family, school and community factors on risk for suicidal behaviors to develop interventions and foster environments that may reduce suicidal thoughts and behaviors.”
IDENTIFYING RISK, PROTECTIVE FACTORS
Their project involves analyzing cross-sectional data and links several state level datasets to identify student-reported family, school and community risk and protective factors associated with repetitive non-suicidal self-injury, suicidal ideation and suicidal behaviors. They also will examine differences across ethno-racial groups, such as Black/African American, American Indian/ Alaska Native, Hispanic/Latino, Middle Eastern and North African, as well as more granular ethnic groups
such as Somali and Hmong. The analysis will focus on students aged 15-19 years. The project will also identify school policies and resources associated with repetitive non-suicidal self-injury, suicidal ideation and suicidal behaviors. It will examine shifts in these factors pre- and post- the COVID-19 pandemic.
“We already know there was a huge increase in kids reporting to ERs with self-harm behaviors, especially at the peak of the pandemic. So we wouldn’t be surprised to see that reflected in the data, especially among girls,” says Areba. She suspects that the data may show different experiences for minoritized youth.
“Even before the pandemic, we had huge issues in terms of access to mental health specialists and resources,” says Areba. “There are cultural considerations that are often not accounted for by health care providers when providing care to minoritized youth. So even before we factored in COVID, we’ve seen differences across those groups.”
14 | MINNESOTA NURSING
When a New York University-led team published findings in 2019 indicating suicide attempts increased 73% among Black adolescents — and increased faster than any other group — it was unexpected to many as Black youth have historically not been considered at high risk for suicide or suicidal behaviors.
• • •
“ Our long-term goal is to identify the role of family, school and community factors on risk for suicidal behaviors to develop interventions and foster environments that may reduce suicidal thoughts and behaviors.”
– Eunice Areba
WHO IS CONDUCTING THE RESEARCH MATTERS
Areba says it matters who is conducting the research, noting that the NYU-led research team in the 2019 study had Black representation. “It is extremely important who is guiding the research process,” says Areba. “Because the way I am asking the questions and looking at the data is very different from someone who does not have the lived experience I have as a Black woman.”
In addition to Areba, the project team includes Michelle Mathiason, MS, Patricia Jewett, PhD, Lindsay Taliaferro, PhD, MPH, and Iris Borowsky, MD, PhD.

“The team really exemplifies team science,” says Areba. “People are trained differently. We have training in public health, psychology, nursing, medicine (pediatrics and adolescent health), epidemiology and statistics. When we all work together, you can really see each of our areas of expertise and how they complement each other.”
The team not only has a diversity of training, but also a diversity of backgrounds.
“We have diversity in racial and ethnic identity, nativity, and experience and rank in the academy, geography, and lived experience, which has been very helpful with this project,” says Areba. “Those backgrounds
are very important in how you prepare and construct the data for analysis, how you present and discuss the findings, and how you contextualize them.”
DEVELOPING BETTER SCREENING, SURVEILLANCE TOOLS
Areba expects to continue this research by seeking input from young people and community members about protecting adolescent mental health and preventing self-harm to develop broad-scale interventions to reduce suicidal behaviors using upstream approaches. Ultimately, she expects to make recommendations around screening in primary care settings. “Preliminary data show that current surveillance is working better in identifying non-Hispanic white girls, but not as much for other youth,” says Areba. “We need to answer why the current tools are missing these kids, and what we need to do to have better screening and surveillance tools and resources to help us with this work.”
www.nursing.umn.edu | 15
• • •
“We have training in public health, psychology, nursing, medicine (pediatrics and adolescent health), epidemiology and statistics. When we all work together, you can really see each of our areas of expertise and how they complement each other.”
– Eunice Areba
Lindsay Taliaferro

16 | MINNESOTA NURSING EDUCATION
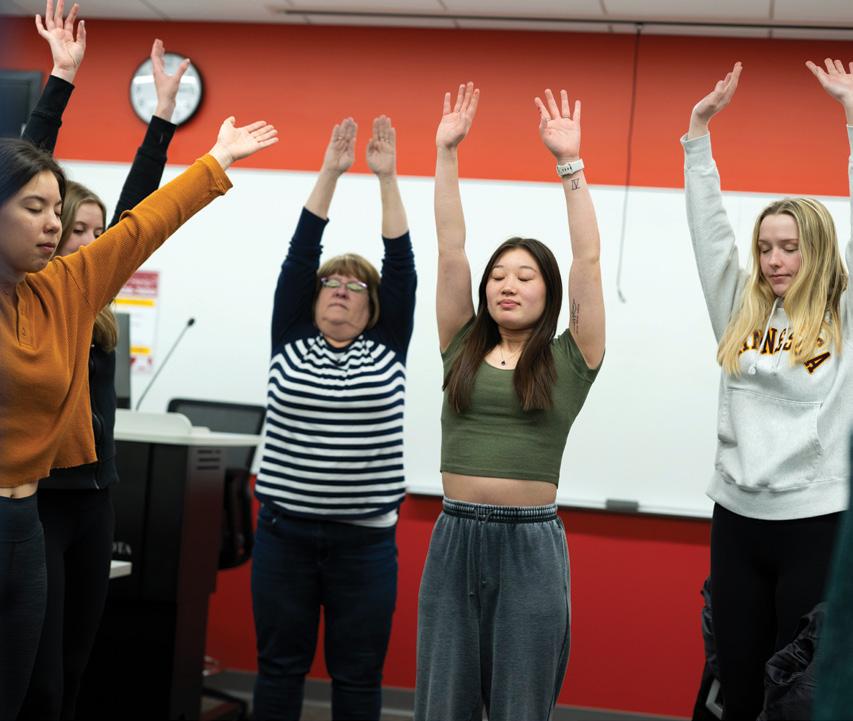
Clinical Associate Professor Donna Eull leads BSN students in a bird breathing exercise, involving controlled breathing and arm flapping.
Photo: Scott Streble
CULTIVATING RESILIENCE IN NURSING STUDENTS
AACN awards pilot grant to foster leadership, wellbeing
by Brett Stursa
As Clinical Associate Professor Donna Eull, PhD, RN, CHPPN, ends a practicum debrief course for seniors in the Bachelor of Science in Nursing (BSN) program, she leads students in a bird breathing exercise that involves controlled breathing and arm flapping.
In another course, she begins the class with a guided meditation. These activities aren’t breaks from learning, they are lessons in resilience, selfcare and wellbeing. Those lessons are becoming increasingly more critical in preparing student nurses to succeed as professional nurses.

Eull saw firsthand the importance of these lessons when she onboarded new and early career nurses at Children’s Hospital in Minneapolis. “So many new nurses hadn’t thought about self-care. There was so much focus on the skills and the technical information of being a nurse, but there wasn’t a focus on nurses as human beings and what it takes to do this job over the long trajectory of a career,” says Eull. Without the skills in resilience and self-care, Eull saw that nurses weren’t remaining in the profession. The data backs up Eull’s observations. Many took notice of a 2014 study that found that 50% of new nurses leave the field within two years. “That study was startling to me but I saw it in the nurses we were onboarding,” says Eull, who says it motivated her to earn a PhD and become nursing faculty. “I wanted to have a hand in how we prepare new nurses to deal with the rigors of a really tough job,” says Eull.
continued on page 18
www.nursing.umn.edu | 17
continued from page 17
SCHOOL 1 OF 10 AWARDED AACN PILOT GRANT
Nationally, organizations like the American Association of Colleges of Nursing (AACN) understand the importance of teaching student nurses resilience, self-care and wellbeing. It launched an initiative last year designed to prepare the next generation of nurses with these skills to meet the competency expectations outlined in the new AACN Essentials.
The University of Minnesota School of Nursing was one of 10 schools across the country to be awarded a pilot grant by the AACN for A Competency-Based Approach to Leadership Development and Resilience for Student Nurses, funded by Johnson & Johnson.
“Preparing nurses with the skills needed to foster wellness, self-care, and resilience in themselves and others is imminently important in today’s health care system,” says Deborah Trautman, PhD, RN, FAAN, AACN president and chief executive officer. “AACN is proud to be working with these 10 schools of nursing and their practice partners to advance innovative
curriculum and clinical experiences that will prepare nurses entering professional practice with the skills needed to thrive across care settings.”
Initially, the AACN convened an expert advisory board to develop new learning strategies and assessment measures related to personal, professional and leadership development, including activities and self-reflection that foster health, resilience and wellbeing. With research expertise in mindfulness-based interventions that promote resilience and mitigate stress among clinicians and family caregivers, Clinical Professor Sherry Chesak, PhD, RN, is serving on the initiative’s advisory board.
“There is a significant recognition right now that there is need to support clinicians. If anything, COVID shone a light on that,” says Chesak. “As clinicians we witness a lot
of suffering and we take on that suffering. If we don’t have a way to work through the impact of that, that’s when burnout and compassion fatigue occur. But there are tools clinicians can use to work through the emotional labor of the job, and it’s so critical, now more than ever, that they learn those practices.”
PILOT BUILDS ON STUDENT WELLBEING ALREADY IN THE CURRICULUM
Clinical Associate Professor Laura Kirk, PhD, RN, and Eull are leading the school’s pilot to integrate resilience, wellbeing and leadership development learning and

18 | MINNESOTA NURSING
• • •
“ As clinicians we witness a lot of suffering and we take on that suffering. If we don’t have a way to work through the impact of that, that’s when burnout and compassion fatigue occur. ”
– Sherry Chesak
Sherry Chesak
assessment strategies into the curriculum during the spring 2023 semester. Assistant Dean for Pre-licensure Programs Carol Flaten, DNP, RN, PHN, and Clinical Assistant Professor Erica Timko Olson, PhD, RN, have consulting roles. Even before the pilot, the School of Nursing emphasized student wellbeing in the BSN curriculum, with students engaged in self-reflection, guided imagery, mindful moments, stretching and breathing exercises. Discussions about how to integrate The Wellbeing Enhances Learning Model, developed by faculty in the Earl E. Bakken Center for Spirituality and Healing, into the BSN curriculum are underway. “This project will help us mobilize the resources we already have and give us some new tools as well,” says Kirk.
The project is being piloted with seniors in the BSN program in their leadership and practicum debrief courses. Faculty are utilizing a variety of wellbeing assessment tools and ideas, including those provided in the AACN toolkit. Wellbeing lessons are incorporated

into reflection assignments and weekly goals. Pre and post measures are being collected to assess the impact on student competency. “Once we determine what resources work the best or resonate the most for students, the goal will be to weave this through all of the curriculum, starting as sophomores,” says Kirk.
Meanwhile, faculty from the 10 schools in the pilot are meeting monthly to share successes and lessons learned to build off of each other’s efforts, and AACN will disseminate findings after determining outcomes so that schools across the country can integrate these lessons into the curriculum.
Integrating resilience, wellbeing and leadership development into the curriculum not only serves the student nurses, but also improves patient outcomes. “Patients do better when they feel genuinely cared for. If a nurse is burnt out or fatigued, they are not going to be able to accomplish that,” says Eull. “The feeling of being genuinely cared for, respected, and affirmed improves patient outcomes, and nurses need to have personal resilience to provide that kind of care.”
www.nursing.umn.edu | 19
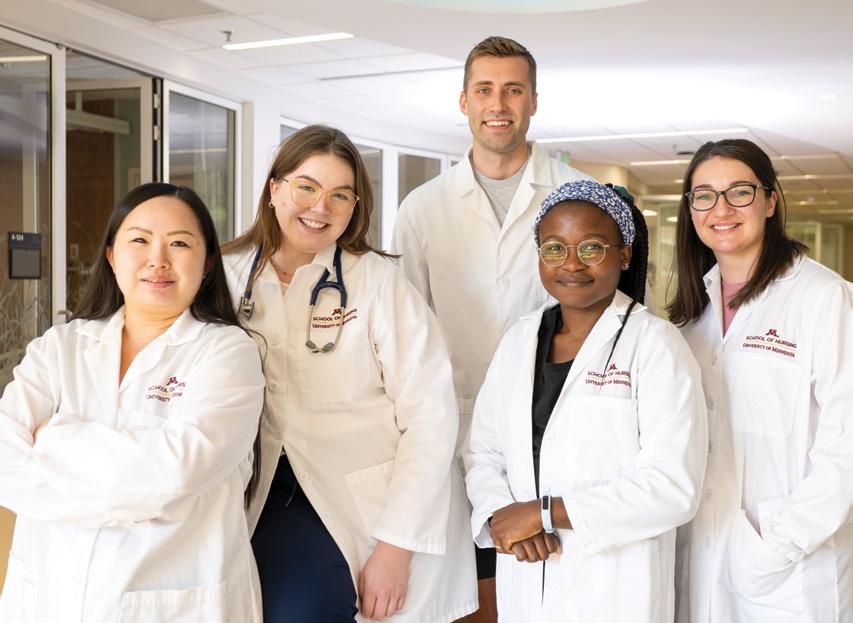
From left, Assistant Dean for Pre-licensure Programs Carol Flaten and Clinical Assistant Professor Erica Timko Olson have consulting roles, while Clinical Associate Professor Donna Eull and Clinical Associate Professor Laura Kirk are leading the school’s pilot to integrate resilience, wellbeing and leadership development learning strategies into the curriculum.
ENSURING STUDENTS THRIVE ON CAMPUS
Care Corner launches to provide students support for their success
by Brett Stursa
As students returned to oncampus learning, Kathryn Schwartz Eckhardt, director of the Office of Student and Career Advancement Services (OSCAS), noticed that students weren’t visiting the OSCAS office with the same frequency they did prior to COVID.
“They were using virtual advising so some students didn’t know that we were here or where our location was,” says Schwartz Eckhardt.
In an effort to encourage more visits to the office, as well as encourage students to see the OSCAS office as a source of support, Schwartz Eckhardt launched the Care Corner. It offers snacks, like granola bars and beef jerky, as well as on-the-go meal options like mac and cheese cups and acai bowls.
“The Care Corner is there to make sure students have something to eat if they come to campus and realize they forgot their lunch, need a little extra help stretching their food budget or just need a granola bar to give them the energy they need to take an upcoming exam,” says Schwartz Eckhardt.
The goal of the OSCAS Care Corner is to give students a reason to want to come to the office and to show them that the office is a caring space designed to support their success. “Sometimes the most needed
support is providing guidance on course selection or other things most typically associated with a student services office. Other times, the most meaningful support we can provide is a yogurt or granola bar to help them focus and get through a busy day on campus,” says Schwartz Eckhardt.
CARE CORNER CONTINUES TO EVOLVE TO SUPPORT STUDENTS
Since launching, the Care Corner has grown to also include items like ibuprofen and period products, as well as scrubs. The scrubs came from the Master of Nursing class that graduated in December, and there are plans to collect scrubs on an ongoing basis from graduating seniors. “From sustainability to a financial perspective, there are so many reasons to do this,” says Schwartz Eckhardt. They will soon be purchasing hijabs for the Care Corner as well.
While the scrubs are donated, the food and other items at the Care Corner are supported through contributed funds. The entire OSCAS team helps support the operations of the Care Corner with everyone restocking the area as supplies run low and greeting students as they come in. As word has spread about the Care Corner, usage continues to tick up, and Care Corners have sprouted up across health sciences schools at the University.
“Our hope is students see our office as a place that they associate with positive things and that they will come to us without hesitation when need us,” says Schwartz Eckhardt.
MENTAL HEALTH ADVOCATES
Schwartz Eckhardt developed the Care Corner as she completed the Mental Health Advocate training through Boynton Health. Mental Health Advocates are staff and faculty volunteers who are part of a community working to implement public health strategies to promote student mental health. About a dozen School of Nursing faculty and staff have completed the training.
“Our school really cares about students and their wellbeing,” says Schwartz Eckhardt. “We have a good faculty and staff participation, and now we are trying to mobilize.”
Schwartz Eckhardt says that when students are struggling, OSCAS is one of the first places they need to go to receive support. “So how students feel about our office is really important. If they see us as cold and inaccessible, it may make it harder for them to address issues of wellness on campus,” says Schwartz Eckhardt. “We want our students to know we care about them.”
The feedback she’s heard from students indicates that the Care Corner is achieving that goal, as they’ve told her it makes them feel like the school cares about them and that it makes OSCAS feel more welcoming and supportive.
“We have a lot of procedures and processes in place to support our students’ academic success but we don’t have a lot in place to support them more holistically as a person to thrive on this campus,” says Schwartz Eckhardt. “This is small step to more wrap around services.”
20 | MINNESOTA NURSING

www.nursing.umn.edu | 21 Students pick up snacks from the Care Corner in the Office of Student and Career Advancement Services.
Photo: Tom Steffes
After assisting in opening one of the nation's first dedicated COVID-19 hospitals, Maria Raines enrolled in the Doctor of Nursing Practice program. She says it cemented her passion for ongoing innovation and problem solving.

22 | MINNESOTA NURSING
‘EVERY DAY, WE’RE HERE FOR PATIENTS’
Raines, VP and CNO for M Health Fairview U of M Medical Center, adds DNP to her resume
by Susan Maas
Had any doubt ever existed about the creativity, adaptability and fortitude of nurses, the COVID pandemic quickly dispensed with it.
Maria Raines — vice president and chief nursing officer for M Health Fairview University of Minnesota Medical Center since 2021 and recent graduate of the Doctor of Nursing Practice (DNP) Post-Master’s program — is a powerful case in point.

In March 2020, as the crisis exploded across the U.S. after erupting in Asia and Europe, Raines, DNP, APRN, ACNS-BC, was charged with a daunting mission: to
swiftly open and lead one of the nation’s first dedicated COVID-19 hospitals. In under three weeks, Raines and her “amazing” team went from planning to opening Bethesda Hospital in St. Paul as a 100-bed center of care for a still-mysterious disease with a terrifying mortality rate.
Obviously, there was no template for pulling this off.
“I would say there were two, maybe two and half weeks from when we started the planning to when we were able to open it,” Raines says. “The rallying of teams from all these other hospitals — the providers, infection control, therapy, spiritual care — was just amazing.” Bethesda’s 82 percent hospital-wide survival rate, 74 percent
continued on page 24
www.nursing.umn.edu | 23
continued from page 23
ICU survival rate, and its exceedingly low nurse and physician infection rates were astonishingly good compared to similar efforts around the U.S.
PASSION FOR INNOVATION
Somehow, Raines began her DNP program in the midst of it all. “My husband thought I had lost my mind,” she laughs. “I told him, ‘I need to start. I feel this is the time for me to do it.’” Her program specialty — health innovation and leadership (HIL) — fit well with Raines’ work experiences at the time. And it cemented her “passion for ongoing innovation and problem solving,” Raines says.
A native of Colombia, Raines came to the U.S. as a teenager with her family. She completed her undergraduate work at a private university in Illinois, then came to the University of Minnesota for her master’s degree as a clinical nurse specialist and in nursing education. Both remain close to her heart; for her DNP project, Raines led the implementation of a dedicated education unit model to better support students in their clinical experiences.
“I think of the model as a triangle: you have the student, who is learning and going through that clinical experience. You have the School of Nursing faculty member, who is teaching and helping support the student. Then you have the professional nurse, who’s bringing in their experience, their skills, their knowledge,” she explains.
• • •
“The professional nurse essentially becomes the clinical instructor. We found that students in the first cohort really felt they were part of the unit — they felt that camaraderie — and that their learning needs were really supported.” Moreover, the clinical nurses (“we call them ACE nurses: academic clinical educator,” Raines says) found that they were “more professionally engaged in their own development. They’re feeling, ‘I am able to help the next generation.’”
‘LOOKING AT WHAT IS POSSIBLE’
Raines thinks a lot about helping young nurses weather the field’s challenges, which COVID underlined and exacerbated, enabling them to grow. “How do we support that next generation?” she says. “How do we help them develop those skills of managing change and of looking at what is possible?”
Prior to building the COVID center at Bethesda, Raines helped redesign the inpatient mental health program
at St. Joseph Hospital in St. Paul. That experience “really helped me understand that engaging our nurses and physicians in the entire process was crucial to making the program successful,” Raines says. She began in her current role in January 2021; since then Raines has helped restructure M Health Fairview U of M Medical Center nursing teams and nursing departments.
For her leadership with Bethesda, Twin Cities Business magazine named Raines a 2021 Notable BIPOC Executive. And last year, Raines earned a leadership award from the Women's Health Leadership Trust. She’s enjoying a phase of her career in which she feels equipped to “give back” — including joining the Nursing Alumni Society Board of Directors. “I’m just so grateful for the opportunities I’ve had,” Raines says.
“I want to find ways to help coach and mentor the next generation” in the profession she loves more than ever. “Every day we’re here for patients, we’re here for staff — and if you keep that as your mission, you’re able to overcome anything.”
24 | MINNESOTA NURSING
“I would say there were two, maybe two and half weeks from when we started the planning to when we were able to open it. The rallying of teams from all these other hospitals — the providers, infection control, therapy, spiritual care — was just amazing.”
– Maria Raines
Structured for your success
Want to transform your career and the health care system but don’t have the tools to do so?
Become a full-practice provider and an innovative systems leader with a Doctor of Nursing Practice (DNP) degree from the University of Minnesota.
• Co-created learning experiences in one of 12 specialties
• Hybrid-by-design program that maximizes education with flexibility
• Worry-free and relevant practicum placements with trusted preceptors
• Strong support from faculty advisers, professional academic staff and our alumni network
Learn more and apply at z.umn.edu/DNP
www.nursing.umn.edu | 25
FINDING HIS NURSING NICHE
by Kelli Billstein
Zach Taylor, MSN, CMSRN, thrives

work and strategic thinking.
A career in nursing that straddles both worlds is one of the primary things that drew him to enroll in the Doctor of Nursing Practice (DNP) program in the adult/ gerontological clinical nurse specialist (CNS) specialty. He’s now about to graduate, balancing direct patient care and systems-thinking leadership to promote change in his field.
Having recently started a new position as a diabetes clinical program coordinator at Abbott Northwestern Hospital, his nursing career is already taking off in exciting new ways. What makes Taylor’s career especially interesting, though, is that his path to arrive at this point has been nonlinear, requiring him to refine his expertise and occupational identity over the years.
“My journey toward nursing was a long and winding road,” Taylor says. In undergrad at the U, he majored in fine arts with a painting focus and minored in French studies. After graduation he worked in graphic design and finance, then spent a year in France teaching
English. Upon return to the U.S., he began exploring health care, taking the prerequisite courses necessary to attend medical school. It was while shadowing a friend in a hospital progressive care unit that Taylor fully realized nursing was the career he’d been searching for.
“What I remember liking about that experience was how well they got to know their patients, identifying their needs and partnering with them to reach their goals,” Taylor says. “Nursing also draws heavily on cognitive, affective and psychomotor skills — a combination that was exciting to me.”
After earning a master’s degree in nursing, he began serving in general medicine at the M Health Fairview University of Minnesota Medical Center. Following three years as a full-time RN, he chose to deepen his expertise by enrolling in the DNP program to become a CNS. “What attracted me to the CNS role was the flexibility. As a CNS you can work similarly to a nurse practitioner seeing patients, but also in a clinical strategizing space, engaging in quality and process improvement, project management and leadership,” he says.
continued on page 28
26 | MINNESOTA NURSING
As a DNP student, Zach Taylor is finding his passion for health equity and planetary health
when he’s able to engage in both hands-on
Photo: Tom Steffes
As a descendant of the Flandreau Santee Sioux Tribe in South Dakota, Zach Taylor participates in the Doctoral Education Pathway Program for American Indian/ Alaska Native nurses, which seeks to grow the number of Indigenous advanced practice nurses and create community among them.

continued from page 26
Effectively through the DNP, Taylor had found his nursing niche — a specialized place to thrive. As a CNS he’d learn to exercise that full range of what he found exciting about nursing in the first place.
His doctoral courses helped to augment his skills and interests. Impressed by the overall polish and professionalism of the DNP program, Taylor was especially engaged in his translation-to-practice and quality improvement courses, as well as a course in health policy leadership. “I think policy is an uncomfortable area for a lot of nurses,” Taylor says. “It's not traditionally an area where nurses have felt like they have a lot of power or much of a voice. So I’ve enjoyed learning how to better engage and figure out strategies for being an effective policy agent, by communicating with legislators or being on committees.”
As a descendant of the Flandreau Santee Sioux Tribe in South Dakota, he’s also involved in the Doctoral Education Pathway Program for American Indian/ Alaska Native nurses, which seeks to grow the number of Indigenous advanced practice nurses and create
community among them. For Taylor, who didn’t grow up on a reservation but was taught to value and appreciate his Indigenous heritage, the chance to embrace the intersection of his Native heritage with his profession as a nurse has been meaningful.
“There’s a representation problem in health care right now,” Taylor says. “Frequently the nursing workforce doesn’t reflect the demographics of the community that it serves. People of color and folks who identify as LGBTQ are underrepresented in the nursing profession. Here in Minnesota, we serve a fairly large Indigenous population, but Indigenous nurses make up an exceedingly low proportion of the total workforce. The
28 | MINNESOTA NURSING
• • •
“Here in Minnesota, we serve a fairly large Indigenous population, but Indigenous nurses make up an exceedingly low proportion of the total workforce. The Pathway Program helps address this issue by increasing mentorship and support, and hopefully increases the number of practicing Indigenous nurses.”
– Zach Taylor
Pathway Program helps address this issue by increasing mentorship and support, and hopefully increases the number of practicing Indigenous nurses.”
In addition to meeting others and participating in community events, the Pathway Program inspired Taylor to begin learning the Dakota language. As busy as he is these days, the Dakota phrase he often practices is: “Pez˙uta sápa wacin” (Peh-ZHOO-ta SAH-pah wa-CHIn), which translates to “I want some coffee.”
As he looks ahead to graduation, he’s passionate about carrying forward two important areas of focus in his profession: health equity and planetary health. In the realm of health equity, Taylor is driven to increase access to high quality health care for all populations, addressing head-on the health disparities that exist today. He says, “I think about health equity and representation a lot. On a personal level, several underrepresented identities intersect within me — being part Indigenous, being gay and being a male in the nursing profession. I have frequently worked with groups who have different health outcomes than the rest of the population due to racism,
stigma and/or socioeconomic inequities. Advancing health equity by working with and empowering people who have been underserved in this messy and broken health care system is something I really do want to have an impact on.”
When it comes to planetary health, Taylor is equally passionate about making sustainability improvements to support a healthier planet that, in turn, supports healthier populations. He does this by joining green committees that make incremental progress within hospitals. “There's just so much waste, pollution and energy use inherent in our current health care system,” Taylor says. “The green committees I’ve been part of make little changes to reduce waste, move to different products and help raise awareness of the problem. In the future, I hope to get involved in organizations that are making larger, concerted efforts toward the health of our planet and all living populations.”
Eager to make an impact in areas he’s passionate about, Taylor is poised to graduate and lean into causes and projects where he can be a catalyst for positive change.
LEARN MORE
To learn more about the Doctoral Education Pathway Program for American Indian/Alaska Native nurses, visit z.umn.edu/NursingPathway
www.nursing.umn.edu | 29
ANSWERING THE CALL

Paramedic-turned-nurse Nathan Koranda is responding to mental health and addiction needs in his local community and abroad
by Tom Ziemer
Standing in an ambulance bay outside Hennepin County Medical Center in Minneapolis, Nathan Koranda tried to process a death that tore open his deepest of wounds.
Koranda didn’t know the victim, at least personally. But about a year earlier, Koranda had been one of the paramedics who had reversed that same individual’s overdose. And the man’s profile and circumstances had reminded Koranda of his own brother’s death from a heroin overdose, a tragedy that pushed Koranda to become a paramedic in the hopes of reversing a single overdose. He wound up handling nearly 100 over six years in the field.
The heartbreaking outcome not only conjured up painful personal memories; it forced him to consider how his profession was stuck in the midst of a seemingly unending opioid epidemic.
“We’re saving lives, but there’s not really that much on the other end of things to keep people locked into sobriety and keep them alive,” says Koranda, who identifies as being in long-term recovery from addiction for the past 15 years.
In nursing, he saw a different role—one he’s occupied for the past five years as a psychiatric nurse at PrairieCare in Brooklyn Park, Minnesota. And he’s currently taking the next step in his nursing career as a student in the Doctor of Nursing Practice (DNP) program in the psychiatric/mental health nurse practitioner specialty.
continued on page 32
30 | MINNESOTA NURSING
From a paramedic to an RN, Nathan Koranda says nursing opened up many opportunities for him. He's now a DNP student in the psychiatric/mental health nurse practitioner specialty.

www.nursing.umn.edu | 31
Photo: Darin Kamnetz
continued from page 30
“You’re working with people for a longer period of time, and you’re caring for them in a different capacity. That's something I wanted to be a part of,” says Koranda, BS, RN, PHN, who will graduate in May. “As far as advanced practice nursing goes, I honestly believe that’s the future of health care. Granted, I’m biased, but I think that as a profession we’re going to continue to grow in some pretty remarkable ways, and I want to be a part of that.”
Koranda has already made his own remarkable contributions to the world, even before entering the DNP program. In 2018, he and a fellow paramedic traveled to Arusha, Tanzania, to lead six weeks of education and training around emergency medical services for local doctors and nurses. Arusha, like many other cities in the east African country, lacks a formal emergency medical services system, with those responsibilities generally falling to police officers.
“If you look globally, trauma in general takes more lives than HIV, malaria and tuberculosis combined, but receives only 1% of the world’s global funding for care,” says Koranda.
That first trip to Tanzania turned into the nonprofit KOPI, which Koranda launched in 2019 to bring together emergency medical services education and mental health training. KOPI teams have returned

to Arusha three more times to train police officers, partnering with a local psychologist to incorporate mental health components. KOPI already has plans to expand its work into another region in Tanzania in 2024.
“All of the concepts are developed locally by the stakeholders out there. We’re just the instrument that’s used to carry some of that out,” says Koranda, who is KOPI’s executive director. “I believe that they would be successful without KOPI. We just happen to be lucky enough to be participants in that work.”
32 | MINNESOTA NURSING
Nathan Korda launched KOPI to bring together emergency medical services education and mental health training to Arusha, Tanzania.
Closer to home, KOPI has partnered with a host of local entities to create the Minneapolis Addiction Recovery Initiative (MARI) Safe Station project. Funded by a federal grant through the Comprehensive Opioid, Stimulant, and Substance Use Program, the project allows individuals experiencing substance use disorder to visit designated fire stations, where they’re evaluated, paired with a peer recovery coach in a matter of minutes, and connected to a host of resources and services.
“It’s a new entry point into the system that’s hopefully breaking down a barrier to care,” says Koranda, who learned about a similar program in Rhode Island while presenting on a panel in Washington, D.C., in 2017.
KOPI is filling a void—something Koranda also hopes to do through his work as an advanced practice nurse in the psychiatric, mental health and addiction treatment space. According to a 2020 survey by the Substance Abuse and Mental Health Services Administration, less
than half of U.S. adults with a mental illness received treatment. More than 155 million people in the U.S. live in areas with a shortage of mental health professionals, per statistics from the Health Resources and Services Administration.
Koranda sees himself among a wave of nurses who are willing to respond to that need.
“Nursing has opened up a lot of opportunity for me,” he says. “It really allows a lot of flexibility for me to chase after all of this stuff that I care about that I have never had that opportunity before. I feel very lucky and blessed to be a part of the profession. I think about it often. Yeah, sure it’s a lot of work, but it’s a lot of really good work, and I wouldn’t want to be doing anything else right now.”

www.nursing.umn.edu | 33 • • •
“As far as advanced practice nursing goes, I honestly believe that’s the future of health care. Granted, I’m biased, but I think that as a profession we’re going to continue to grow in some pretty remarkable ways, and I want to be a part of that.”
– Nathan Koranda
Participants in an emergency medical services training practice new skills.
Warda Hussein talks about her path to nursing and her experience as a nursing student at z.umn.edu/Warda

34 | MINNESOTA NURSING
PATH TO NURSING PAVED BY FIRSTHAND EXPERIENCES
MN grad Warda Hussein committed to health equity so patients feel heard, understood
by Brett Stursa
Warda Hussein, MN, RN, says two events put her on the path to nursing. The first occurred when as a worried 14 year old whose mother was headed to surgery, a nurse ensured Hussein could visit her mother before being taken to the operating room and ensured her mother had a scarf to cover her head while in a patient gown. “The nurse asked if there was anything she could do to make me comfortable and to make sure our religious practices were respected. It was only after I reflected on it years later did I realize how profound it was,” says Hussein. The second event occurred her freshman year as a pre-med student majoring in biology at the University of Minnesota. While shadowing an obstetrician, she had the opportunity to observe a patient from Myanmar, who needed an interpreter, deliver a baby. ”Although I was there to shadow the doctor, I found myself watching the nurse instead,” says Hussein, who was impressed that the nurse made sure the woman understood what was happening. “She looked at the patient to ask questions rather than the interpreter, which I know can be difficult sometimes, as I come from a community where languages are spoken outside of English,” says Hussein. “As a daughter of Somali immigrants, I grew up hearing from family about how they didn’t feel heard or understood when they went to the clinic or hospital. Sometimes the language
barrier became too great for them to receive care that they felt was adequate — not by any fault of the medical system but just that there was that gap. So I became dedicated to making people feel heard regardless of who they were or where they came from. It was both fascinating and validating to see that dedication and action from that nurse.”
Now, as a recent graduate of the Master of Nursing (MN) program, Hussein says her time as a nursing student only reinforced she’s on the right path. The rigorous, 16-month program was challenging, but she felt supported and encouraged. She says it’s unlikely she would have been able to pursue the degree if it hadn’t been for the Ned and Noreen Zimmerman Nursing Scholarship. “The scholarship meant a lot. I come from a low income background and I was raised by a single mom, so the scholarship alleviated a lot of stress and made it possible,” says Hussein. “I’ve met my benefactors and told them they are the reason I am becoming a nurse. From this point on, whatever I do as a nurse it is because of their generosity and their graciousness.”
As a nursing student, Hussein found her niche in pediatric critical care. She spent her capstone in her last semester completing 200 hours on the neonatal intensive care unit at the M Health Fairview Masonic Children’s Hospital. “I really fell in love with pediatrics and
neonatal care,” says Hussein. She enjoyed including family in care and learned the importance of communicating with them — from explaining the beeps and pumps to answering their questions.
For two months she provide care to one baby with significant medical needs, learning his schedule, his meds and other needs to meet his goals for the day.
“Babies can’t talk, so I learned to pay close attention to his body language,” she says. “I really got to know him and understand his care.” Ultimately, the baby passed away. The experience left her questioning if critical care, where deaths can be more common, was the right specialty for her.
“After I cried and talked about it, I realized that I really can’t imagine doing anything else,” she says.
After graduating in December 2022 and passing the NCLEX, Hussein began her first nursing position at Children's Minnesota hospital's pediatric intensive care unit. “I am looking forward to the variety and age ranges. I’m really excited to learn care at different developmental levels,” says Hussein.
Long term, she has her eye on earning a doctoral degree and becoming faculty so she can be there for students the way faculty were there for her as a student. But for now, her focus is on becoming a critical care nurse. “As I nurse, I finally reach my goal of helping people,” she says.
www.nursing.umn.edu | 35
SCHOOL OF NURSING FIRST IN THE WORLD TO BE AWARDED ASSOCIATE MEMBER STATUS OF
UNITED NATIONS NGO
Commission on the Status of Women panel focuses on big data and health
by Brett Stursa
The Katharine J. Densford International Center for Nursing Leadership at the University of Minnesota School of Nursing was awarded associate member status in the Conference of Non-Governmental Organizations in Consultative Relationship with the United Nations (CoNGO).
It is the first school of nursing to achieve the status in the world.
“The associate member status in the Conference of Non-Governmental Organizations in Consultative Relationship with the United Nations provides yet another potent pathway for the School of Nursing to create and participate in a multitude of opportunities to co-create health at a global level,” says Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP. “It brings visibility of nursing and academic nursing to the top of the United Nations and is an important achievement for the school and nursing.”
As a non-governmental organization in general consultative status with the United Nations Economic and Social Council, CoNGO’s work relates to the entire United Nations system: the secretariat, agencies, treaty bodies, regional commissions, institutes, summits and world conferences. The associate member status provides opportunities to participate in a range of United Nations events, meetings and conferences, and includes opportunities for leadership.
One of the Densford Center’s first contributions after receiving CoNGO status was hosting a Commission
on the Status of Women Parallel Event Innovative Approaches to Informatics and Big Data for SDGs and Health on March 17 with faculty and international panelists. Additionally, planning is underway to create an immersion experience for Doctor of Nursing Practice students.
“We can participate in committees as members, thought leaders and problem solvers and reach out to the entire UN community,” says Holly Shaw, PhD, RN, a Densford Center director with extensive nursing leadership within the United Nations. “Nurses have the skills and the expertise to be able to be critical thought leaders, negotiators and problem solvers. I think our input is very badly needed in the UN system in many areas.”
Faculty and students participated in UN programs even before receiving CoNGO status. Clinical Professor Teddie Potter, PhD, RN, FAAN, FNAP, Densford Center director and director of Planetary Health, presented at several climate change events and students have attended various events and conferences. The school assisted in transitioning what was scheduled to be an in-person 2020 World Health Day event celebrating the work of nurses and midwives to a virtual one at the beginning of the COVID pandemic, when the UN wasn’t accustomed to hosting virtual events. “That was an important contribution,” says Shaw, who says the associate member status was the next step to further engage with the United Nations.
“Traditional thinking equates nursing with health care,” says Potter. “The more radical way of thinking is that nursing is everywhere because health is everywhere. Nurses shouldn’t just be on the health committee, they need to be on all of the committees — transportation, housing, women’s rights, the status of children. We need to be at the table because health is at the table.”
36 | MINNESOTA NURSING
OUTREACH
Clinical Professor Judy Pechacek, Densford Center Director Teddie Potter and Densford Center Director Holly Shaw at the United Nations in New York City.


38 | MINNESOTA NURSING ALUMNI SPOTLIGHT
Sakeena Futrell Carter talks with a new mom at the Park Nicollet clinic in Minneapolis.
Photo: Darin Kamnetz
AN ADVOCATE FOR PATIENTS AND THE PROFESSION
by Brett Stursa
Sakeena Futrell Carter, DNP, APRN, CNM, was a labor and delivery nurse for 10 years before deciding to earn a Doctor of Nursing Practice degree at the University of Minnesota and leave labor to become a women’s health nurse practitioner.
“I wanted a little bit more Monday through Friday, 9 to 5 in my life, but after seven years of that, I missed birth,” says Futrell Carter, who returned to the University of Minnesota to earn a graduate certificate in nurse-midwifery.
“I missed that in labor and delivery and during birth, you develop this really intense, close relationship. It’s, most of the time, the most significant point in a person’s life and to be a part of it is always a blessing. I always thank my patients after,” says Futrell Carter. “It doesn't get old. It gets tiring and exhausting, but it does not get old.”
PARTNERING WITH PATIENTS
Futrell Carter currently practices with a group of 14 nurse-midwives at Park Nicollet, at clinics in Minneapolis

and St. Louis Park. “We’re pretty busy. We do on average just under 800 births a year just within our group of midwives,” says Futrell Carter, who says she averages about 50 births a year. She has a call day every week and she’s in clinic seeing patients for prenatal care, postpartum care, full scope annual visits and problem visits.
Futrell Carter says being a good nurse-midwife takes compassion, listening and the ability to anticipate someone’s needs. An appreciation for the partnership between provider and patient is also key. “People will say, ‘Do I have to do that?’ And I'm like, ‘You probably won’t hear me ever say that you have to do anything. Wrap your heart around the plan, that's my big thing. Whatever we're doing, I need you to wrap your heart around it or it's not going to work.’”
She can’t imagine being a nurse-midwife without the labor and delivery experience she had as a Registered Nurse, but being an Advanced Practice Registered Nurse is a distinctly different experience. “You are in charge of the room as the midwife,” she says. “You’re not in charge of the patient and her family, but you have to see everything and also be very present in what’s happening with that birthing person.”
continued on page 40
www.nursing.umn.edu | 39
Futrell Carter says being a nursemidwife is what she’s meant to be
continued from page 40
While the majority of the clinic’s patient population is Caucasian, she says she tends to draw women of color because they seek her out. “I think it's amazing. They’ll come in and say, ‘I’m seeing you specifically because I looked up your profile and you’re a woman of color.’”
There are four midwives of color in her group, which isn’t by luck. “I happen to be fortunate enough to work within a very receptive group of midwives, and so I talk a lot within our group about diversifying,” she says.

Another important piece to being a Black midwife for Futrell Carter is raising awareness about the fears that women of color experience. “I have women come in and they’re like, ‘I know that as a Black woman, I’m more at risk to die because of this pregnancy.’ And I tell them, ‘I can't promise you that I’ll be there for your birth. What I can promise you is that I truly trust this group of women around me who might potentially be caring for you. I promise that they will honor you and take care of you to the best of their abilities.’”
A COMMITMENT TO ADVOCACY
Hand in hand with her commitment to catching babies is her commitment to advocacy. She’s supported doulas of color and raised awareness that people who are
pregnant in Minnesota qualify for health insurance, so that they know that cost shouldn’t be a barrier to receiving care.
During her term on the Minnesota Board of Nursing, she advocated for more diversity on the board and for the board to govern certified midwives, who are not nurses. “There’s a significant cost benefit in not having to become an RN and then transition into a master’s program, which opens up the profession of midwifery to more people,” she says. Eventually it gained the board’s support, although there is not a certified midwife program in Minnesota.
She’s served on the Maternal Mortality Review Committee for the state of Minnesota, which involved analyzing every maternal death in the state. “None of it is good, none of it is happy. The outcomes are never good. But you know that you’re being part of hopefully preventing this from happening to another birthing person,” she says.
Futrell Carter also serves as First Lady of Minnesota’s Capitol City. She enjoys working alongside her husband, Saint Paul Mayor Melvin Carter, and feels fortunate that their passions and goals align.
40 | MINNESOTA NURSING
Sakeena Futrell Carter holds a baby with the new mom and Park Nicollet clinic health professionals.
WHERE NURSE-MIDWIFERY IS HEADED
As she looks at the future of nurse-midwifery she sees that people are becoming more aware of midwifery care and the benefits of it. She also sees that nurse-midwives and physicians are developing better relationships. “I only know my practice, but I strongly feel like we’re developing better relationships with our physician partners,” she says. “I don't know if that’s unique to our practice or just the trust we’ve built, or maybe, hopefully, that's happening nationwide and worldwide.”
She hopes that as a profession, nurse-midwifery grows in diversity, with more men, people of color and people of varying socioeconomic statuses, all the while focusing on patient outcomes. “I hope that we continue to do what we’re doing in practice that helps those mortality rates to come down,” she says.
As the field of nurse-midwifery continues to grow and evolve, Futrell Carter knows she’ll be experiencing it firsthand. “I love my work. I love my patients. I love my partners,” says Futrell Carter. “Truly, and I tell my husband this all the time, for both of us, we truly feel like we are living what we were put on this Earth to do. And that's amazing. I don't know that everyone has that feeling in life.”
Nurse-midwifery program celebrates 50th anniversary
The University of Minnesota’s nursemidwifery program is celebrating its 50th anniversary. The program was first established in 1973 as an option within the master’s degree program. In 2009, nursemidwifery transitioned to the Doctor of Nursing Practice (DNP) program, becoming the first in the country to be approved as a DNP program.
Over the years, the program directors have included Sharon Rising, Kathleen Dineen, Mary Rossi, Melissa Frisvold and Melissa Avery. Melissa Saftner currently leads the program. The program has earned a national reputation, and it is ranked second in the nation by U.S. News and World Report.
www.nursing.umn.edu | 41
• • •
“You are in charge of the room as the midwife. You’re not in charge of the patient and her family, but you have to see everything and also be very present in what’s happening with that birthing person.”
– Sakeena Futrell Carter, DNP, APRN, CNM
LEADING BY EXAMPLE
Good’s enthusiasm for psych/mental health nursing inspires daughter to earn DNP degree
by Steve Rudolph
Beth Good, DNP, APRN, PMHCNS, has always been a leader. A self-proclaimed early adopter, she was drawn to the Doctor of Nursing Practice Program’s psychiatric/ mental health specialty while teaching psychiatric nursing classes at the University with professor emeritus Merrie Kaas, who would later become her adviser.
Good went on to implement her doctoral project of integrating depression care management into the primary care setting in Mora, Minnesota, and started integrated behavioral health at Welia Health System before launching her own, community-based practice to make an even bigger impact.
What she didn’t realize at the time was the influence she was having on her daughter, Alexis Grieves, DNP, APRN, PMHNP-BC.
Although some of her earliest memories are of accompanying her mom to campus when she taught psychopathology, including a recollection of handing out Easter candy to her mom’s students, Alexis wasn’t interested in nursing. She wanted to go into fashion design.
“I was super passionate about it and my parents were always very supportive,” said Grieves. “Never once were they like ‘you should really think about going into nursing or consider this instead.’”
In her senior year of high school Grieves reached conclusion that fashion wasn’t her path and realized what she truly liked was listening and talking to people.
“Well, my mom’s been doing this her whole life,” she recalled thinking at the time. And that was when she realized there might be a future in nursing for her.
It was at that point that mother shared with daughter how she could still be creative in a nursing role working with patients and in treatment plans.
Grieves enrolled at the College of Saint Benedict, where her choice to become a nurse was quickly affirmed, although perhaps somewhat differently than many of her classmates.

“I’d tell all my preceptors in undergrad that I’m not a big fan of blood and needles so if I pass out, that’s probably what it is. They’d respond, ‘And you want to become a nurse?’ I’d remind them there’s another kind of nurse, psych mental health.”
TAKING THE NEXT STEP
Not surprisingly, Good also played a role in Grieves’ decision to pursue her DNP at her alma mater. She invited her daughter to be her guest at the School of Nursing’s All School Reunion in 2017. There they met Katherine Todd, DNP, MBA, RN, who was receiving the Alumni Society’s
42 | MINNESOTA NURSING
Beth Good, a psychiatric/mental health clinical nurse specialist, celebrates the graduation of her daughter Alexis Grieves, who is now a psychiatric/mental health nurse practitioner.

Rising Star Award and her daughter who was finishing her DNP degree at the School of Nursing.
“Alexis was able to meet these other women who were in the field already making positive connections and creating change in systems,” Good recalls.
Those encounters and the University’s focus on research encouraged Grieves to enroll at the School of Nursing. She earned her degree in 2022. Now a psychiatric/ mental health nurse practitioner herself in Honolulu, Hawaii, Grieves has an even greater appreciation for her mother’s impact, not just on herself but the profession.
“My mom is very inspiring and has been very inspiring to me,” says Grieves. “There’s something about giving people hope and inspiration about this field that my
mom is excellent at. When I would meet people at work thinking about nursing, I’d say ‘you should talk to my mom and you’ll be convinced you should become a psych mental health nurse.’”
Still in Cambridge, Good continues to pave the way helping create resources for her patients, advocating for psych NPs in rural practices and passionately precepting students.
“I've had an administrative role, I've had the practitioner role, been an educator, and now I can put all of that together and just create a really rich experience for students because I can come from all those different roles that we can do,” she says. “At this point in my career, I feel like my job is to help as many people get into the profession.”
www.nursing.umn.edu | 43
PRAIRIECARE, SCHOOL OF NURSING FORM COLLABORATORY TO IMPROVE MENTAL HEALTH CARE
PrairieCare and the University of Minnesota School of Nursing announced the formation of a collaboratory to facilitate working together to improve nursing practice, education and patient outcomes as it relates to mental health care.

The collaboratory will serve as a nursing think tank and incubator for creativity and innovation that will engage faculty, staff and students in the development of strategies to enhance education, research and practice.
“Nursing is integral in meeting the increased demand for mental health services, particularly in rural communities,” says Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP.
“Preparing more psychiatric/mental health nurse practitioners is a top priority for the School of Nursing and
we are thrilled to be able to work with PrairieCare to meet the care needs of our community.”
“Amazing things happen when two organizations of excellence join forces to make a difference,” says Mandy Dageford, MSN, CENP, chief nursing officer of
PrairieCare. “PrairieCare is excited to partner with the University of Minnesota School of Nursing to create innovative strategies that will enhance and uplift the profession of nursing within the mental health field and positively impact our patients and our communities.”
SCHOOL OF NURSING, MAYO CLINIC FORM COLLABORATORY TO ADVANCE NURSING
and support the health of individuals and their families through research and evidence-based practice. The partnership also will address nursing workforce needs for Mayo Clinic throughout the U.S. and support a smooth transition of graduates into practice.
The University of Minnesota School of Nursing and the Mayo Clinic Department of Nursing formed a collaboratory to facilitate working together to generate, disseminate and apply knowledge for the improvement of nursing practice, education and patient outcomes. The partnership will engage nursing faculty,

staff and students in the development of strategies to enhance nursing education, research and practice.
Initially, the partnership will center on fostering innovative undergraduate, graduate and post-graduate education experiences at Mayo Clinic and advancing nursing knowledge to improve
The collaboratory will build on the partnership the School of Nursing and the Department of Nursing have had since the school first began educating Bachelor of Science in Nursing students in Rochester in 2002. All School of Nursing students in Rochester complete their clinical education at Mayo Clinic and learn from clinical instructors and preceptors who are Mayo nurses. In 2020, the School of Nursing and Mayo Clinic collaborated to provide a first-ofits-kind clinical leaning experience by creating a dedicated education unit in an ambulatory care setting.
44 | MINNESOTA NURSING
SCHOOL NEWS
MHA, SCHOOL OF NURSING FORM COLLABORATORY TO ADDRESS WORKFORCE NEEDS
The Minnesota Hospital Association (MHA) and the University of Minnesota School of Nursing announced the formation of a collaboratory to facilitate working together to improve nursing practice, education and patient outcomes. The collaboratory will serve as a nursing think tank and incubator for creativity and innovation that will engage nursing faculty, staff and students.
Specifically, the School of Nursing and MHA will strategize how to address current and future nursing workforce needs for the hospitals and health systems and support a smooth transition of graduates into practice through collaboration between the school and MHA members and statewide committees, including the MHA Chief Nursing Officers Group.
“The School of Nursing is committed to a transformative collaboration with MHA and their Chief Nursing Officers Group to

address urgent workforce needs, nursing equity and excellence,” says Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP. “The issues facing nursing and nursing education require cooperation and coordinated efforts.”
Additional areas of focus will be advancing nursing knowledge to improve and support the health of individuals and their families through research and evidence-based practice, as well as fostering innovative undergraduate, graduate and post graduate education experiences at hospitals and health systems.
“The worsening workforce crisis in health care requires an urgent and all-handson-deck approach in order to preserve access and support innovation in care,”
says Rahul Koranne, MD, MBA, FACP, president and CEO, Minnesota Hospital Association. “MHA is excited to dial up our long-standing partnership with the University of Minnesota School of Nursing through this collaboratory to strengthen the pipeline of health care professionals needed to care for our patients and communities for generations to come.”
SHUKUTOKU, MINNESOTA UNIVERSITIES SIGN AGREEMENT OF COOPERATION
The University of Minnesota School of Nursing and Shukutoku University School of Nursing and Nutrition in Japan signed a five-year agreement for cooperation and exchange to promote the wellbeing of the people of both countries.
“We are delighted to be in partnership with you,” said Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP, at a virtual signing in November. “We know that this exploration and relationship formalized through our MOU will not only be enriching for our students, but also our faculty and our research and human health.”

Possible areas of collaboration are exchanges of faculty members, exchanges of students, joint research activities, exchanges of research results and joint conferences.
Already, Clinical Associate Professor Huong Nguyen, PhD, MA, conducted a workshop on Buddhist nursing at Shukutoku University in November.
“We are all very excited to have an MOU with your university. We are very happy to work together with you,” said Dean Kaoru Shigeno, PhD.
www.nursing.umn.edu | 45
DURENBERGER, BOARD OF VISITORS EMERITUS, PASSES AWAY
Former U.S. Sen. David Durenberger passed away in January at the age of 88. Durenberger served 16 years in the U.S. Senate, after first being elected in 1978 and serving until 1995. He championed health care reform and was the original sponsor of the Americans with Disabilities Act.
After his service in the Senate, Durenberger continued serving the public in various roles, including teaching courses in health policy and serving as chair of the National Institutes of Health Policy and other national health commissions and boards. Durenberger served on the inaugural University of Minnesota School of Nursing Dean’s Board of Visitors.

A service was held for Durenberger on Feb. 7, 2023, at Saint John’s Abbey Church in Collegeville, Minnesota.
BRIEFLY
New aging education toolkits available
New resources for teaching introductory aging content are available from the Minnesota Northstar Geriatrics Workforce Enhancement Program, including toolkits created by School of Nursing faculty. Professor Emeritus Merrie Kaas, PhD, APRN, PMHCNS, FAAN, wrote Suicide in Older Adults, which teaches learners how to assess and prevent suicide in older adults. Professor Kathleen Krichbaum, PhD, RN, FGSA, ANEF, FAAN, wrote Addressing Ageism in Healthcare, which helps learners reflect on ageism and understand better how it affects the care and health of older adults. Learn more by visiting mngwep.nexusipe.org/toolkits.
Looman named inaugural associate dean for faculty affairs
Professor Wendy Looman, PhD, APRN, CPNP-PC, was named the inaugural associate dean for faculty affairs. The associate dean for faculty affairs has primary responsibility for matters related to faculty affairs in the School of Nursing, with a focus on faculty promotion, tenure, leaves and professional development. The position supports and promotes the School of Nursing’s priority on advancing a culture of wellbeing as well as in promoting recognition and inclusion for the success of all members of the faculty.
46 | MINNESOTA NURSING
BRIEFLY
3 Minnesotans honored with ANA Innovations Awards
Three Minnesotans received recognition by the American Nurses Association and the American Nurses Foundation, which announced the winners of the 2023 ANA Innovation Awards. The awards highlight, recognize and celebrate exemplary nurse innovators who improve patient safety and health outcomes.
Roxanne McMurray, DNP, APRN, CRNA, and the McMurray Team received the Nurse-led Team Award. McMurray, who is a former faculty member, leads the team that developed the Distal Pharyngeal Airway (DPA), which is a breathing tool that stents open throat tissue to maintain adequate ventilation for surgery or other medical procedures. McMurray and her team saw a gap in available and effective airway management tools for populations who suffered from breathing complications, which led to the creation of DPA.
11 new Global Health Scholars named
Associate Professor Mary Fran Tracy, PhD, RN, Clinical Associate Professor Carol Flaten, DNP, RN, PHN, Clinical Assistant Professor Stephanie Gingerich, DNP, RN, CPN, Professor Carolyn Porta, PhD, MPH, RN, SANE-A, FAAN, FNAP, Clinical Associate Professor Huong Nguyen, PhD, MSW, MA, Clinical Assistant Professor Olof Indridadottir, DNP, AHN-BC, CRRN, Clinical Associate Professor Dorcas Kunkel, DNP, RN, PHN, CNW, CPHIMS, CDIP, Clinical Assistant Professor Joanne Donnelly, DNP, APRN, CRNA, Professor Lucy Mkandawire-Valhmu, PhD, RN, FAAN, Clinical Professor Judith Pechacek, DNP, RN, CENP, and Professor Mary Hearst, PhD, were named Global Health Scholars and joined the Global Health Faculty Scholars’ Community of Practice. The program supports the advancement of global health through meaningful partnerships around the world.
Kevin Smith, DNP ‘14, FNP, FAANP, was named the recipient of the Individual Nurse Award. Smith, who graduated from the University of Minnesota’s Doctor of Nursing Practice program in 2014, is the creative mind behind The Good Clinic, a Minnesotabased, modern primary care model that provided patients age 12 or older with holistic wellness.

Assistant Professor Robin Austin, PhD, DNP, DC, RN-BC, FAMIA, FNAP, received an honorable mention in the Individual Nurse Award category for MyStrengths + MyHealth: A Comprehensive WholePerson Health & Resilience Assessment.


Post-graduate certificate program approved
The University of Minnesota Board of Regents approved the addition of an Adult Gerontological Acute Care Nurse Practitioner Specialty to the school’s post-graduate certificate program. The first students in the program will begin their students in the summer 2023 semester.
www.nursing.umn.edu | 47
AWARDS AND HONORS
Clinical Assistant Professor Jane Anderson, DNP, APRN, ANP-BC, FNP-BC, was named the recipient of the Nurse Practitioner Award for Excellence for the state of Minnesota by the American Academy of Nurse Practitioners.



Assistant Professor Cynthia Bradley's article More than a Meme: The Dunning-Kruger Effect as an Opportunity for Positive Change in Nursing Education published in Clinical Simulation in Nursing was selected as one of the Society for Simulation in Healthcare (SSH) Articles of Influence for 2021-22. Bradley, PhD, RN, CNE, CHSE, was featured in a special session at the 2023 International SSH annual conference.

Associate Professor Siobhan McMahon, PhD, MPH, APRN, GNP-BC, received the Distinguished Educator Award from the National Hartford Center of Gerontological Nursing Excellence. The award recognizes educators with knowledge and skills needed to provide excellent care to older adults and competence to engage all learners and inspire positive attitudes toward older people.
Assistant Professor Mary Whipple, PhD, RN, PHN, was selected as an associate editor for Vascular Medicine. Her three-year term began in January 2023. Whipple was also selected as a Finalist for the Jay D. Coffman Young Investigator Award Competition at the 2022 Society for Vascular Medicine Scientific Sessions.
Clinical Associate Professor Misty Wilkie, PhD, RN, FAAN, was appointed to serve a three-year term on the Department of Veterans Affairs Special Medical Advisory Group (SMAG), which provides advice to the Secretary of Veterans Affairs and the Under Secretary for Health on matters relating to the care and treatment of veterans and other matters pertinent to the operations of the Veterans Health Administration. Wilkie also was elected to the Minnesota Organization of Registered Nurses Board of Directors.

48 | MINNESOTA NURSING
NEW FACULTY JOIN THE SCHOOL


Sherry Chesak, PhD, RN, joins the school as clinical professor. She maintained funded research while at the Mayo Clinic and has held leadership positions at both Mayo and Riverland Community College. She brings extensive research, teaching and clinical/practice experience, with a focus on care for the caregiver and engendering a sense of belonging among health care workers. Chesak earned a PhD from the University of Wisconsin–Milwaukee and bachelor’s and master’s degrees in nursing education from Winona State University.
NEW APPOINTMENTS
Elizabeth Meyers, PhD, joins the school as a clinical assistant professor, with a joint appointment with the Institute for Health Informatics. Previously she served at the National Committee for Quality Assurance, and she served for five years active duty with the Army Nurse Corps. Her primary research interest is decision science. She earned a PhD from the University of Minnesota in health informatics, a master’s degree in technology management from University of Wisconsin–Stout and a bachelor’s degree in nursing from the University of Minnesota.

Bridget Apitz, MA, joins the school as an executive office and administrative specialist on the Rochester campus. Apitz earned a bachelor’s degree in philosophy from Toronto Metropolitan University and a master’s degree in education from Augsburg University. She has experience in governmental and non-profit sectors as a policy administrator and customer service specialist where she worked to modernize policies for a Homelessness and Housing Support Program.
Jillian Rowan, MA, joins the school as the American Indian/Alaska Native Pathways recruiter and adviser. She previously was employed by St. Olaf College and the University of Minnesota. She earned a master’s degree in American Indian Studies from UCLA and a bachelor’s degree in American Indian Studies from the University of Minnesota.

Julia Steiner, MPH, joins the school as a research professional for the Mobile Market study. Previously, she served as a diet interviewer for the CARDIA study at the School of Public Health. She earned a master’s degree in public health from the University of Minnesota School of Public Health, a master’s degree in international education from Columbia University Teachers College and a bachelor’s degree in Russian from Georgetown University.

www.nursing.umn.edu | 49
Renee Sieving, PhD, RN, FAAN, FSAHM
CENTER FOR ADOLESCENT NURSING
Reducing self-harming thoughts and behaviors among American and Australian young adults
Building upon, and extending, cross-national longitudinal research from the International Youth Development Study (IYDS), School of Nursing Associate Professor Barbara McMorris, PhD, recently coauthored a new analysis exploring which risk and protective factors during adolescence predict deliberate selfharm (DSH) thoughts and behaviors in young adulthood. Former postdoctoral fellow Lindsay Taliaferro, PhD, University of Central Florida, is first author with coauthors from the University of Washington and the University of Melbourne, Australia.
“Young people worldwide are in mental health crisis,” says McMorris. “It’s critical that we find out what factors during adolescence impact DSH later when they are young adults.”
Beginning in 2002, the IYDS surveyed adolescents in both Washington State and Victoria, Australia during middle school and again at age 25.
McMorris and team focused their analysis on protective factors. “Current DSH research is limited and often focuses only on risk factors during either adolescence or young adulthood, not both. By looking at both protection and risk, and expanding the timeframe, we are helping to fill the gaps in the literature and improve our understanding of this critical issue,” says Taliaferro. The team found that adolescent adaptive coping strategies, positive recognition from one’s community/neighborhood, and prosocial behavior were all protective against DSH in young adulthood. Understanding these protective factors, while also continuing to address key risk factors (depressive symptoms, poor family management/connections), could help inform the creation of programming and interventions used to reduce the prevalence of DHS thoughts and behaviors in young adulthood.
McMorris and Taliaferro are excited to share the results, in press in the Journal of Adolescent Health. “Promoting resilience through coping strategies and positive connections with adults, in addition to managing depressive symptoms and enhancing family connections, will provide the tools adolescents need to reduce or prevent DSH thoughts and behaviors in adulthood,” says McMorris.
CENTER DIRECTOR: Wendy Looman, PhD, APRN, CPNP


CENTER FOR CHILDREN WITH SPECIAL HEALTH CARE NEEDS
Resources for applying a life course perspective
Two core values of the Center for Children with Special Health Care Needs are centering care on family systems and using a life course lens in the care of children and families. This column features a national partner in this work, the Life Course Intervention Research Network (LCIRN). Funded by the Maternal and Child Health Bureau of the Health Research and Services Administration, LCIRN is a collaborative of researchers, service providers and thought leaders who support researchers and providers in developing, implementing, and evaluating interventions to help children and families thrive and achieve optimal health development. Through LCIRN, center members and their collaborators and stakeholders can access a broad set of resources for applying a life course perspective in research and practice with children and youth with special needs and their families. Three particularly useful resources to advance equity, partnership and measurement centered on the family are listed below. To access the LCIRN's full set of tools and resources, visit lcirn.ucla.edu.
1. Engaging Families and Communities in Life Course Intervention Research
lcirn.ucla.edu/advancing-lcir/
Clarissa Hoover and colleagues provide a framework for planning and implementing interventions in true partnership with families.
2. Life Course Intervention Researcher Core Competencies
z.umn.edu/lifecourseintervention
Emily Hotez and colleagues outline 29 competencies across five domains for life course intervention research and training.
3. Compendium of Family Functioning Measures
lcirn.ucla.edu/resources/familyfunctioning
This compendium provides a matrix of 40 validated family functioning tools that assess different aspects of family measurement such as organizational processes, belief systems and communication processes.
50 | MINNESOTA NURSING
CENTER DIRECTOR:
Barbara McMorris
Lindsay Taliaferro
CENTER DIRECTORS:
Christine Mueller, PhD, RN, FGSA, FAAN


 Siobhan McMahon, PhD, APRN, GNP-BC
Siobhan McMahon, PhD, APRN, GNP-BC
CENTER FOR
AGING SCIENCE AND CARE INNOVATION
5 faculty are Distinguished Educators in Gerontological Nursing

The National Hartford Center for Gerontological Excellence (NHCGNE) recognizes nurse educators for their exemplary contributions to gerontological nursing education. Through teaching excellence, and advanced knowledge and skill for providing high-quality care to older adults, the Distinguished Educators in Gerontological Nursing awardees make contributions toward preparing the future nurse workforce to care for diverse aging populations. The School of Nursing has five faculty who are Distinguished Educators in Gerontological Nursing.
Siobhan McMahon, PhD, APRN, GNP-BC
McMahon, a co-director of CASCI, is the most recent awardee. As an advanced practice registered nurse in gerontological nursing, her teaching and research focuses on improving the health and wellness of older people. She mentors and advises undergraduate and graduate students whose projects center on improving nursing care for older adults. She engages with community partners and interdisciplinary colleagues to promote health and prevent falls among older people.
Niloufar Hadidi, PhD, APRN, ACNS-BC, FAHA

As coordinator for the adult/ gerontological clinical nurse specialist specialty, Hadidi guides and mentors students to engage in gerontological nursing scholarship and quality improvement initiatives to improve the care of older adults. Hadidi participates in the health sciences Interprofessional Geriatric Case Competition as a judge.
Kristine Talley, PhD, RN, GNP-BC Talley co-directs the Minnesota Northstar Geriatric Workforce Enhancement Program, where she leads the creation of interprofessional education resources to teach Age-Friendly Care. These freely accessible resources offer nurse educators and preceptors access to digital learning modules. She developed and teaches a course on advanced practice nursing care for older adults for the adult gerontological nurse practitioner and clinical nurse specialist students.
Mary Goering, PhD, RNBC Goering has led and facilitated student practicum experiences related to gerontological nursing. She served as the Geriatric Nursing Champion for the BSN and MN programs since 2009. In this role, she works with faculty to ensure that gerontological nursing is integrated in the programs. Goering created teaching resources related to caring for older adults, and she has served as an adviser for DNP projects for students in the adult gerontological nurse practitioner specialty.
Christine Mueller, PhD, RN, FGSA, FAAN Mueller served as the co-director for the Minnesota Hartford Center for Gerontological Excellence. She was part of a team that developed a national faculty development program to prepare nursing faculty to teach gerontological nursing. She was awarded a grant from the Health Resources and Services Administration to develop exemplary clinical experiences for students in nursing homes. This initiative prepared nursing faculty from nursing schools in four states through workshops to develop clinical experiences in nursing homes. She served on national expert panel that developed competencies for gerontological nurse educators and led the validation process to finalize the competencies.
www.nursing.umn.edu | 51
CENTER DIRECTORS:
Robin Austin, PhD, DNP, DC, RN-BC, FAMIA, FNAP
Connie Delaney, PhD, RN, FACMI, FAAN, FNAP

 Martin Michalowski, PhD, FAMIA CENTER FOR
Martin Michalowski, PhD, FAMIA CENTER FOR
NURSING INFORMATICS
On the leading edge of national, international initiatives
Center for Nursing Informatics faculty are at the leading edge of nurses’ involvement in several national and international initiatives. We look forward to the 11th annual Nursing Knowledge: Big Data Science (NKBDS) conference June 7-9, 2023, focused on The Value of Nursing This conference brings together experts and participants who will challenge each other’s thinking about the value of nursing and the ways informatics can foster improvements in nursing practice, research, education and leadership. Learn more at z.umn.edu/bigdata.
Contributing to the center's history as an International Classification Nursing Practice (ICNP) of the International Council of Nurses (ICN) Research and Development Center (z.umn. edu/icnp), Robin Austin, PhD, DNP, DC, RN-BC, FAMIA, FNAP, and Dorcas Kunkel, DNP, RN, PHN, CNE, CPHIMS, CDIP, will serve as the co-directors of this effort and recently joined the ICNP’s Editorial Board. Kunkel will be presenting at the ICN and attending the ICNP Consortium meeting this July in Montreal, Canada.
Martin Michalowski will conduct a workshop this summer leading efforts on artificial intelligence (AI), 2nd Workshop on Artificial Intelligence in Nursing (AINurse23). AINurse23 is co-located with the 21st International Conference on Artificial Intelligence in Medicine (AIME2023), in Portoroz, Slovenia, on June 15, 2023. The workshop will focus on AI in nursing and provide a platform for discussions about the recent advances, cutting edge AI methods, and chart a path forward for nursing AI. More details are available at the workshop’s website https:// sites.google.com/view/ainurse23/home/
The center would like to welcome new informatics faculty, Assistant Professor Christie Martin, PhD, MPH, RN -BC, LHIT-HP, PHN, Clinical Assistant Professor Dorcas Kunkel and Clinical Assistant Professor Elizabeth Meyers, PhD, RN, CPHIMS. If you would like more information about these initiatives please contact center faculty at quis0026@umn.edu.
CENTER DIRECTOR: Jayne Fulkerson, PhD


CENTER FOR CHILD AND FAMILY HEALTH PROMOTION RESEARCH
Interrupting health inequity with communitydriven solutions
Healthy beginnings are important and can provide strong foundations for optimal health. Yet, healthy beginnings are elusive. Worldwide, the under-5 mortality rate is 40.8 deaths per 1,000 live births, with the highest rates in low-and middle-income countries, according to the World Health Organization. Worldwide, 8 million children live in orphanages, 1 billion children lack access to education, health, housing, nutrient and sanitation or water, and there are 240 million children with disabilities, according to UNICEF. In the U.S., access to equitable opportunities for education, employment, housing, transportation, food and health care is vastly different between white populations compared to Black, Indigenous and People of Color (BIPOC) communities, deeply impacting children, families and optimal life chances for all.
Mary Hearst, PhD, MPH, is a professor and center member, and her research interests aim to address these inequities. Her strategies for interrupting the social, structural, political and economic structures that interfere with health equity include community-driven solutions that create system change, using positions of power and privilege to elevate voices of the BIPOC community, and assuring families have holistic support for their children. Hearst, colleagues from St. Catherine and St. Thomas University, SPOON Foundation, and the Catholic Medical Mission Board–Zambia implemented Kusamala+. This community-driven solution including community health workers, health facility staff and local project managers alters the community-based stigma towards children with disabilities in Zambia by changing the health system practices around prevention and intervention, and build family and community support through home visiting. Hearst and colleagues elevate underrepresented voices in the U.S. and their daily life experiences coping with systemic racism and isolation. Finally, Hearst and colleagues have implemented interventions that provide holistic support to children and families domestically and internationally.
52 | MINNESOTA NURSING
Mary Hearst
Elizabeth Meyers
Christie Martin
Dorcus Kunkel
CENTER DIRECTORATE
Shirley Brekken, MS, RN, FAAN
Siobhan McMahon, PhD, MPH,
Vincent Peters, MASW
Teddie
Holly
GNP-BC
Potter, PhD, RN, FAAN, FNAP
Shaw, PhD, RN
KATHARINE J. DENSFORD INTERNATIONAL CENTER FOR
NURSING LEADERSHIP Densford Center hosts UN event
On March 17, the School of Nursing Katharine J. Densford International Center for Nursing Leadership hosted a virtual parallel event during the United Nations Commission on the Status of Women’s (CSW) 2023 annual two-week session. Engaging the expertise of the School of Nursing and interdisciplinary and global informatics faculty and partners, the panel focused on the relationship of digital technology and meeting the 17 UN Sustainability and Development Goals SDGs. More than 100 people attended the event from 13 countries.

The panel described how information, technology, resources from academia, practice and health systems, and research can achieve health improvements to service the SDGs and co-creation of the highest level of health for individuals, families and communities. Members highlighted an interdisciplinary, interprofessional model using and disseminating digital technology to innovate, create efficiencies, generate knowledge, and operationalize massive information so it can be understood by all and, thus ensure equity, access and quality health care across continuums, transitions and diverse systems. In keeping with the CSW purpose, particular attention on climate, women’s health and women’s leadership were interwoven into the presentation.
The UN Commission on the Status of Women is the principal intergovernmental body exclusively dedicated to the promotion of gender equality and the empowerment of women. The Densford Center was approved to host a parallel event because it was awarded associate member status in the Conference of Non-Governmental Organizations in Consultative Relationship with the United Nations (CoNGO). This membership brings the School of Nursing to the table to engage in policy and action at the international level. Parallel events such as this, organized outside the formal
program of the session of the commission, provide an excellent opportunity for member states, UN entities and NGOs to discuss themes of the commission.
Dean Connie White Delaney, PhD, RN, FAAN, FACMI, FNAP, coordinated the panel presentation, titled Innovative Approaches to Informatics and Big Data for SDGs and Health. University of Minnesota panelists included Sripriya Rajamani, PhD, MPH, MBBS, FAMIA, Jenna Marquard, PhD, Martin Michalowski, PhD, FAMIA, Christie Martin, PhD, MPH, RN-BC and Dorcas Kunkel, DNP, RN, PHN, CNE, CPHIMS, CDIP. Global panelists included Edwin Beyan DHSc, MSNEd, BSc, RN; Moher Patern College of Health Sciences in Liberia; Ernesto Morais, MScHEM, RN, CHN, Porto School of Nursing in Portugal; Hyeoun-Ae Park, PhD, RN, FACMI, FAAN, Seoul National University in Korea; Selda Secginli, PhD, RN, Istanbul University – Cerrahpasa, Istabull in Turkey; and Merve Altiner Yas, PhD RN, Istanbul University –Cerrahpasa, Istabull in Turkey.
LEARN MORE
A recording of Innovative Approaches to informatics and Big Data for SGDs and Health can be viewed at z.umn.edu/csw67
www.nursing.umn.edu | 53
The webinar Innovative Approaches to Informatics and Big Data for SDGs and Health was a parallel event during the United Nations Commission on the Status of Women annual session.
ALL SCHOOL REUNION MOVES TO FALL HOMECOMING
Kick off homecoming weekend with the 2023 All School Reunion, Nursing, Voices of Change. After listening to feedback from alumni, the reunion will now be held in the fall with other homecoming events. The dinner will be held at McNamara Alumni Center in Minneapolis on Thursday, Sept. 28, 2023, at 6 p.m. Convenient parking and valet will be available for all reunion guests. Come and network with other alumni, current students, as well as professors past and present. Reunite with classmates and make new friends before a weekend of homecoming activities. For more information, visit z.umn.edu/nursingreunion.
NOMINATE AN ALUM FOR AN AWARD
Celebrating the outstanding accomplishments of our alumni is a highlight of the All School Reunion. Do you know a fellow alumni who deserves to be recognized? Nominations for the Rising Star Award, Distinguished Alumni Humanitarian Award and Excellence in Practice Award are open. To find out more and nominate a colleague visit z.umn.edu/nursingalumniawards.
NURSING ALUMNI SOCIETY BOARD OF DIRECTORS
Tucker Annis, DNP ‘21, BSN ‘15 UCare, Clinical Informaticist Lead
Connie White Delaney, PhD University of Minnesota School of Nursing, Professor and Dean
Laura Kirk, PhD ’08, MS ’97, BSN ’95 President Elect
University of Minnesota School of Nursing, Clinical Associate Professor
Susan Lampe, MS’77
Heritage Committee Representative Retired
Cheryl Lanigan, BSN ’73 President
Grace University Lutheran Church, Faith Community Nurse
Quinn Mccormick, BSN ‘20
Abbott Northwestern, Cardiovascular ICU Registered Nurse
Jonathan Nghiem, BSN ’20
M Health Fairview – UMMC East Bank, ICU Registered Nurse
Maria Raines, DNP ’22, MSN ‘04, M Health Fairview - UMMC and Masonic Children’s Hospital, Chief Nursing Officer
Caroline Rosdahl, MA ’68, BSN ’60, ALA ‘57
Hennepin County Medical Center and Anoka Technical College, Retired
Nick Schuler, BSN ‘18
M Health Fairview – UMMC East Bank, Cardiovascular ICU Registered Nurse
Susan Schumacher, MS ‘92
HealthPartners - Methodist Hospital, Retired
Kathryn Schwartz Eckhardt
University of Minnesota School of Nursing, Director - Office of Student and Career Advancement Services
Susan Strohschein, DNP ’16, MS ’80, BSN ‘68
Public Health Nurse Consultant, Retired
Maura Talwalkar
MNSB Student Representative
Lexie Tremble
DNP Student Representative
Allina Health – St. Francis Hospital, Wellness Coordinator and Registered Nurse
Teri Verner, DNP ‘12
Walker Methodist Health Center, Director of Nursing
Earl E Bakken Center for Spirituality and Healing, Graduate Faculty
Megan Holle Whipps, BSN ‘12 Secretary
Park Nicollet Health Services, Pre and Post-Operative Registered Nurse
Savannah Zins, PhD ‘17
Mayo Clinic, Nursing Education Specialist
54 | MINNESOTA NURSING ALUMNI NEWS
CLASS NOTES
Caroline Rosdahl, BSN ’60, was a panelist in the College of Liberal Arts event Trailblazers: A Celebration of Women in the “Pride of Minnesota.”
Jill Guttormson, PhD ’11, MS ’05, was named dean of the Marquette University College of Nursing.
Shanda Demorest, DNP ’17, BSN ’13, published Climate, Health, and Nursing Tool (CHANT): A confirmatory factor analysis in Public Health Nursing.
Shanda Demorest, DNP ’17, BSN ’13, and Katie Huffling, DNP ’21, collaborated on the Nurses Climate Challenge, a project with Health Care Without Harm and the Alliance of Nurses for Health Environments. The initiative met its target of educating 50,000 health professionals on climate and health by 2022.
IN MEMORY
Pat K. Skelton, BSN ‘43
Janet Ahart, BSN ‘45
Shizuko D Aka, BSN ‘47
Evelyn S March, BSN ‘47
Mary E Michaels, BSN ‘47
Margaret M Nelson, BSN '47
Eileen J Clifford, BSN '48
Jeanne L Cochrane, BSN ‘48
Marguerite A Kellett, BSN ‘48
Virginia Mc Larnan, BSN '51
Ethel E Demaree, BSN ‘52
Margaret W Nichols, BSN ‘52
Phyllis R Engstrom, BSN ‘54
Phyllis A Boler, BSN ‘55
Mary L Larson, BSN ‘55
Gena R Nelson, BSN '55
Carol H Gilfry, BSN '56
Martha M Marchand, BSN '57
Doris M Sterner, BSN '58
Lois Gantriis, BSN ‘59
Kristin Verhoeven, DNP ’19, BSN ’14, started a new role as the co-director of psychiatry, clinical operations supervisor at Boynton Mental Health.
Abigail Frith, DNP ’22, MN ’15, started a new role as a neurology nurse practitioner at Park Nicollet/Methodist Hospital.
Anthony Weis, DNP ’22, accepted an informatics specialist position at Mayo Clinic.
David Wrobleski, DNP ’22, MN ’16, presented a poster at the American Psychiatric Nursing Association conference and won second place for practice posters.
George Hirschboeck, DNP ’20, started his practice as an independent CRNA in Sleepy Eye, Minnesota. He serves at four hospitals and with four other CRNAs
to help provide call coverage at sites in rural southwest Minnesota, including OB services, general surgery, orthopedics, ENT, endoscopy and cataracts.
Ryne Wilson, DNP ’22, was a featured panelist at the National Comprehensive Cancer Network’s conference on Best Practices and Policies for Addressing the Health Needs of LGBTQ+ Cancer Patients and Survivors.
KEEP
US UP TO DATE
Have you recently received a promotion, been hired for a new position or honored with an award? Or have you moved or changed email addresses? Keep us up to date and let us know by visiting www. nursing.umn.edu/alumni.
Ruth W Felker, BSN ‘59
Carol A Brache Jakway, BSN ‘63
Jane T Adams, BSN ‘64
Vernee A Stevenson, BSN ‘64
Shirley K Jones, BSN '67
Merodie C Nielsen, BSN ‘67
Ellie Slette, BSN ‘68
Teresa M Swanson, BSN ‘70
Sharon M Connelly, BSN '72
Maureen J Watson, MSN ‘72, BSN ‘67
Judith Schultz, BSN ‘73
Janice M Anderson, MS '74, BSN '72
Joann A Anton, BSN ‘77
Sandra E Blair, BSN ‘77
Choonja Lee, BSN '78
Ruth J Behrens, MSN ‘87
Suzanne K Beltz, MS '90
Clifton E Roberts, MSN ‘92
Steven J Mund, DNP ‘11, MSN ‘98
Judith L Miller, BSN ’60, passed away peacefully on Jan. 13, 2023. Throughout her 50-year career, she was an ardent advocate for public and community health with a special focus on childbearing age families. She worked tirelessly for them. This passion for young children and mothers won her numerous awards and recognition, including the first ever Pediatric Nurse of the Year from the American Nurses Association. In addition to her love of nursing she was an avid outdoorswoman. At YMCA Camp Widjiwagan she became the first female trail counselor to lead a group of teenage girls through the Boundary Waters Canoe Area Wilderness without the aid of a male counterpart. Her last role at Widji was that of camp nurse.
www.nursing.umn.edu | 55
INSPIRED, WITH A PASSION FOR THE FUTURE OF NURSING
The School of Nursing Foundation Board of Trustees plays a dynamic role in shaping the future of nursing and advancing health care to improve the health and wellbeing of all. Comprised of alumni and friends of the school, trustees are volunteer leaders who advance the school’s mission in Minnesota and in alumni communities around the country. In partnership with the school’s Office of Development and Alumni Relations, the Board of Trustees promotes nursing excellence and builds relationships with current and future benefactors and alumni.
Every trustee is unique and so are the gifts they bring to the School of Nursing. Trustees are an essential part of our school and reflect the communities with whom we partner and serve. Each trustee’s path to board service involved steps from different walks of life. Together, they champion a unified commitment to foster optimal health and wellbeing for all people and the planet.
“Serving as a trustee provides me an opportunity to give back to an institution that has been pivotal in shaping my career. I would not be the nursing leader that I am today without the education and relationships I formed at the School of Nursing, and those that have supported and guided me along the way. The board
provides a space that embraces diversity, with a lens pointed at the future, that allows me the opportunity to share my voice and perspectives authentically,” says Allysia Jenkins, DNP ’18, BSN ’07.

BECOME A TRUSTEE
Interested in a meaningful and rewarding volunteer opportunity? The school is looking for changemakers nationwide who are passionate about providing future nurses with a worldclass opportunity to learn, leading and discovering in a dynamic teaching and research environment. Applicants from all geographic locations are welcome. To learn more, please email Andrew McIlree, director of Development & Alumni Relations, at mcilree@umn.edu.
SCHOOL OF NURSING
FOUNDATION BOARD OF TRUSTEES
Bernie Aldrich
Treasurer
Rimage Corporation, Retired
Jeannine Bayard
UnitedHealth Group, Retired
Ann Garwick
University of Minnesota School of Nursing, Retired
Allysia Jenkins
Humana
Cynthia Jurgensen
Past Chair
UnitedHealth Group, Retired
Meri Beth Kennedy
Planned Parenthood North Central States, Retired
Lisa Martin
University of Minnesota School of Nursing
Christine Mueller
University of Minnesota School of Nursing
Nancy Olson
Abbott Northwestern Hospital, Retired
Marjorie Page
Chair Elect
M Health Fairview, Retired
David Rothenberger
Secretary
University of Minnesota Department of Surgery
Sharyn Salmen
Salmen Consulting
Nancy DeZellar Walsh
Chair
DeZellar Walsh Consulting LLC
EX-OFFICIO MEMBERS (WITH VOTING PRIVILEGES)
Andrew McIlree
Chief Development Officer
University of Minnesota School of Nursing
Connie White Delaney
Professor and Dean
University of Minnesota School of Nursing
TRUSTEE EMERITI
Sandra Anderson
Dawn Bazarko
Mary Lou Christensen
Susan Forstrom
Patricia Kane*
Marilee Miller
Carolyn Schroeder
Jack Spillane
56 | MINNESOTA NURSING
DEVELOPMENT
*Indicates trustee emeriti who are deceased
Allysia Jenkins
Earn your PhD the way you want
NEW DELIVERY MODEL OFFERS GREATER FLEXIBILITY
Find the answers to the questions facing nursing and improve the health of patients and the community with a PhD in Nursing from the University of Minnesota. Our HyFlex instruction format allows you the option to attend class in-person or remotely through video connection. Whether on campus or not, you’ll be mentored by nationally-renowned faculty and provided research opportunities only a tier-one institution ranked in the top 10 can provide. Full-time students receive full funding for their first two years.
Learn more at www.nursing.umn.edu/PhD
www.nursing.umn.edu | 57
PHOTO FINISH
Nurse anesthesia students volunteered at Open Arms of Minnesota, chopping 245 chicken breasts and 62 pounds of peppers and packing more than 600 meals.

Doctor of Nursing Practice students gained an understanding of the socio-cultural factors affecting the health and wellbeing of Guatemalans during a global health experience in Guatemala in January.

A group of American Indian/ Alaska Native students from the schools of medicine, dentistry, pharmacy, veterinary medicine and nursing gathered in March in an effort to build a community of support for Indigenous scholars.

SCHOOL NEWS
58 | MINNESOTA NURSING
Minnesota Student Nurses Association members and nursing student volunteers hosted Scrubs Day at Adams Spanish Immersion Elementary School in St. Paul. Kids learned how to put on PPE, listen to their hearts and lungs, make first aid kits, test their hand washing skills, and make x-ray crafts of their hands. Volunteers included Katie Hinzman, Claire Furlong, Lalina Leung, Abby Grund, Alfonso Amores, Mardi Marek, Thompson Nguyen and Anna Schumann.

Associate Professor Erica Schorr was a panelist at the International Conference on Prevention and Management of Chronic Conditions hosted by Ramathibodi School of Nursing, Mahidol University, which is a University of Minnesota School of Nursing global partner.

PHOTO FINISH
Dallas Ducar, president and CEO of Transhealth, discussed gender-affirming care at the Doctor of Nursing Practice Enhancement and Enrichment Programming Day in January.

www.nursing.umn.edu | 59
www.nursing.umn.edu | 75

Nonprofit Org. U.S. Postage PAID Twin Cities, MN Permit No. 90155 #6 DOCTOR OF NURSING PRACTICE PROGRAM U.S. News and World Report
5-140 Weaver Densford Hall 308 Harvard Street S.E. Minneapolis, MN 55455 www.nursing.umn.edu
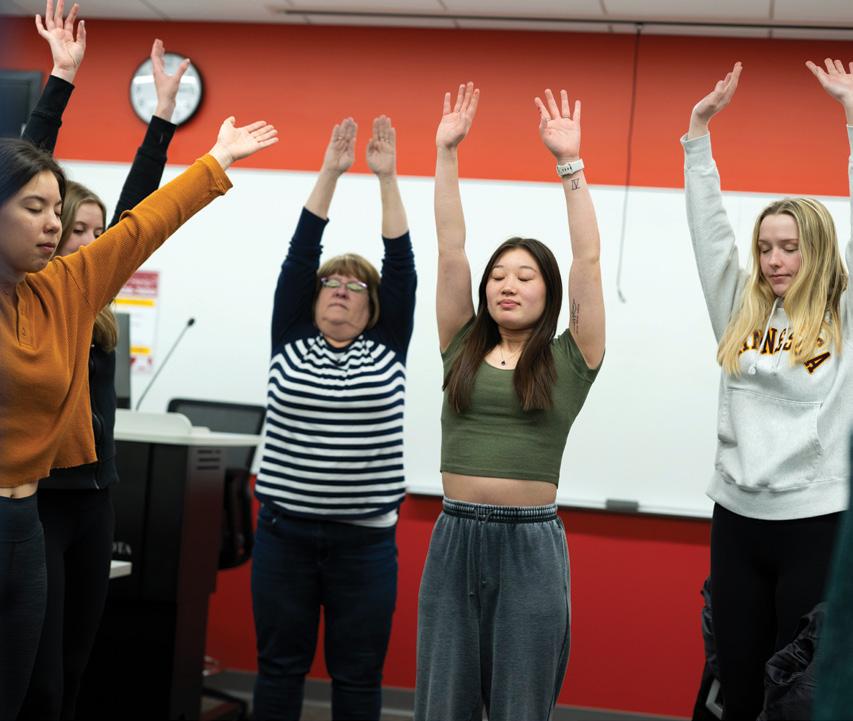
























































 Siobhan McMahon, PhD, APRN, GNP-BC
Siobhan McMahon, PhD, APRN, GNP-BC



 Martin Michalowski, PhD, FAMIA CENTER FOR
Martin Michalowski, PhD, FAMIA CENTER FOR